Analysis of Healthcare Systems in New Zealand and Australia
VerifiedAdded on 2024/05/14
|13
|2188
|138
Report
AI Summary
This report provides a detailed overview of the healthcare system in New Zealand, comparing it with Australia. It highlights key characteristics such as health system performance indicators, healthcare funding, the role of government, and the healthcare workforce. The report notes that while New Zealand's healthcare system is comprehensive, it faces challenges in accessibility and equity, particularly for indigenous populations. It also discusses the integrated performance and incentive framework developed by the government to improve health system performance. The analysis includes a comparison of New Zealand's healthcare performance with Australia, noting areas where Australia's system is more advanced. The report concludes that both countries face workforce issues, including a shortage of indigenous health workers, and that New Zealand needs to focus on improving accessibility and healthcare outcomes.
HEALTHCARE SYSTEM IN NEW ZEALAND
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Table of Contents
INTRODUCTION..........................................................................................................................2
HEALTH CARE SYSTEM OF NEW ZEALAND.................................................................................3
HEALTH SYSTEM PERFORMANCE INDICATORS..........................................................................4
THE ROLE OF GOVERNMENT......................................................................................................6
HEALTH CARE FUNDING.............................................................................................................7
HEALTH CARE WORKFORCE.......................................................................................................8
CONCLUSION............................................................................................................................10
REFERENCES.............................................................................................................................11
1
INTRODUCTION..........................................................................................................................2
HEALTH CARE SYSTEM OF NEW ZEALAND.................................................................................3
HEALTH SYSTEM PERFORMANCE INDICATORS..........................................................................4
THE ROLE OF GOVERNMENT......................................................................................................6
HEALTH CARE FUNDING.............................................................................................................7
HEALTH CARE WORKFORCE.......................................................................................................8
CONCLUSION............................................................................................................................10
REFERENCES.............................................................................................................................11
1
INTRODUCTION
This report is been drafted to understand the health care system in New Zealand and
Australia. The details of the health care systems of New Zealand are represented along with
a focus on the main healthcare characteristics such as health system performance
indicators, health care funding the role of government and health care workforce (Pegasus
Health, 2014). It also depicts the difference between the health performance indicators of
New Zealand that differs from Australian health care system.
2
This report is been drafted to understand the health care system in New Zealand and
Australia. The details of the health care systems of New Zealand are represented along with
a focus on the main healthcare characteristics such as health system performance
indicators, health care funding the role of government and health care workforce (Pegasus
Health, 2014). It also depicts the difference between the health performance indicators of
New Zealand that differs from Australian health care system.
2
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
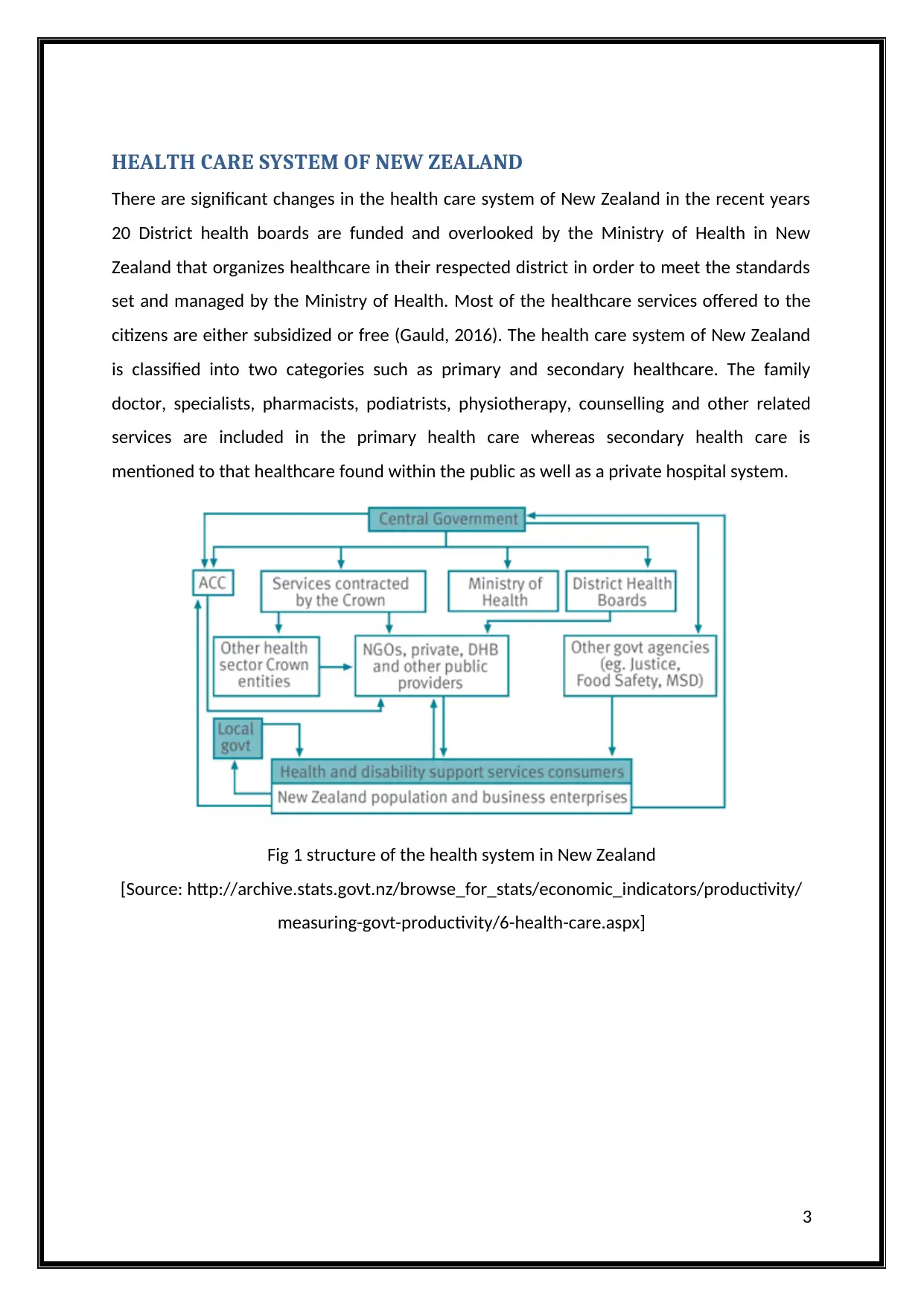
HEALTH CARE SYSTEM OF NEW ZEALAND
There are significant changes in the health care system of New Zealand in the recent years
20 District health boards are funded and overlooked by the Ministry of Health in New
Zealand that organizes healthcare in their respected district in order to meet the standards
set and managed by the Ministry of Health. Most of the healthcare services offered to the
citizens are either subsidized or free (Gauld, 2016). The health care system of New Zealand
is classified into two categories such as primary and secondary healthcare. The family
doctor, specialists, pharmacists, podiatrists, physiotherapy, counselling and other related
services are included in the primary health care whereas secondary health care is
mentioned to that healthcare found within the public as well as a private hospital system.
Fig 1 structure of the health system in New Zealand
[Source: http://archive.stats.govt.nz/browse_for_stats/economic_indicators/productivity/
measuring-govt-productivity/6-health-care.aspx]
3
There are significant changes in the health care system of New Zealand in the recent years
20 District health boards are funded and overlooked by the Ministry of Health in New
Zealand that organizes healthcare in their respected district in order to meet the standards
set and managed by the Ministry of Health. Most of the healthcare services offered to the
citizens are either subsidized or free (Gauld, 2016). The health care system of New Zealand
is classified into two categories such as primary and secondary healthcare. The family
doctor, specialists, pharmacists, podiatrists, physiotherapy, counselling and other related
services are included in the primary health care whereas secondary health care is
mentioned to that healthcare found within the public as well as a private hospital system.
Fig 1 structure of the health system in New Zealand
[Source: http://archive.stats.govt.nz/browse_for_stats/economic_indicators/productivity/
measuring-govt-productivity/6-health-care.aspx]
3
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
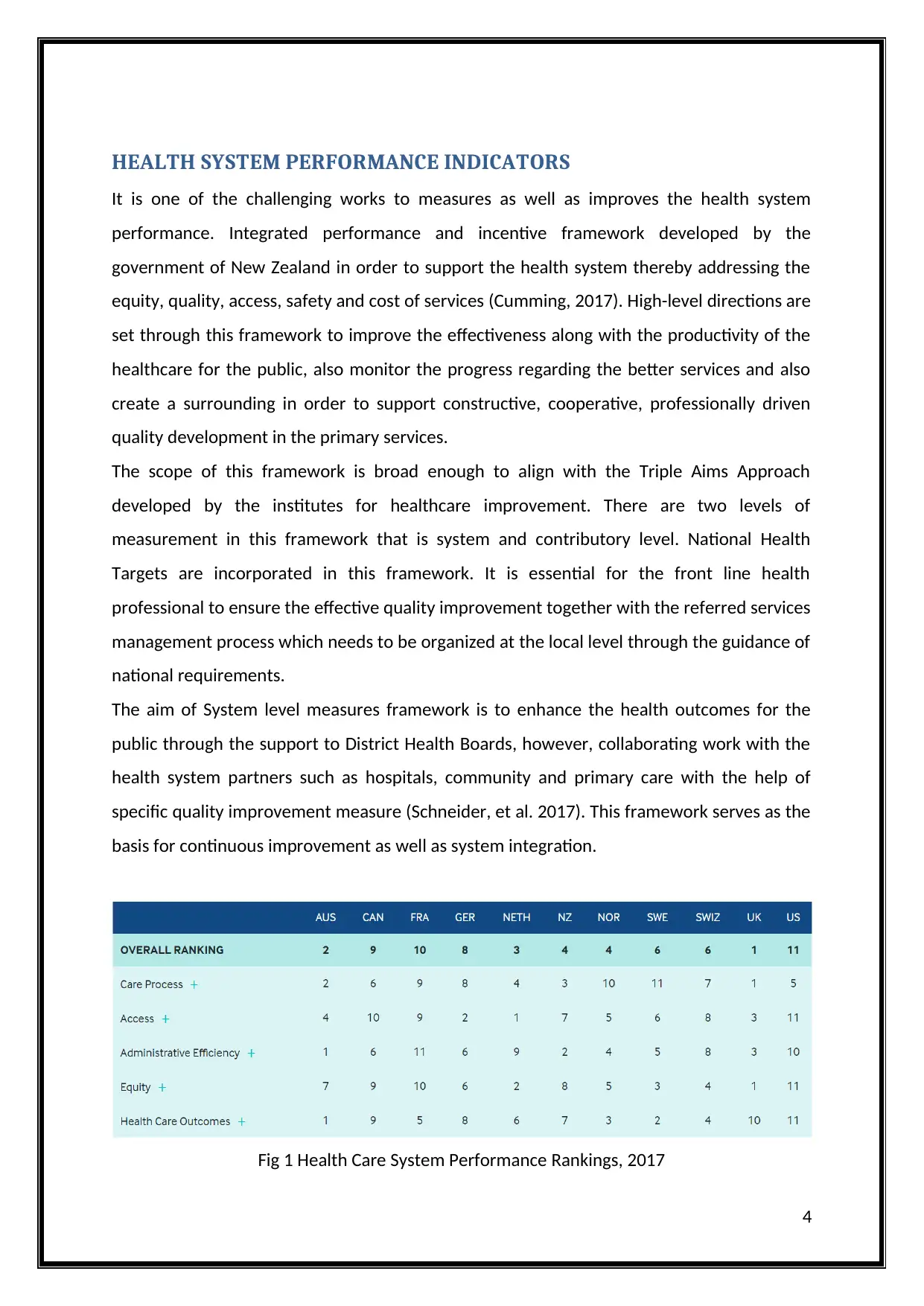
HEALTH SYSTEM PERFORMANCE INDICATORS
It is one of the challenging works to measures as well as improves the health system
performance. Integrated performance and incentive framework developed by the
government of New Zealand in order to support the health system thereby addressing the
equity, quality, access, safety and cost of services (Cumming, 2017). High-level directions are
set through this framework to improve the effectiveness along with the productivity of the
healthcare for the public, also monitor the progress regarding the better services and also
create a surrounding in order to support constructive, cooperative, professionally driven
quality development in the primary services.
The scope of this framework is broad enough to align with the Triple Aims Approach
developed by the institutes for healthcare improvement. There are two levels of
measurement in this framework that is system and contributory level. National Health
Targets are incorporated in this framework. It is essential for the front line health
professional to ensure the effective quality improvement together with the referred services
management process which needs to be organized at the local level through the guidance of
national requirements.
The aim of System level measures framework is to enhance the health outcomes for the
public through the support to District Health Boards, however, collaborating work with the
health system partners such as hospitals, community and primary care with the help of
specific quality improvement measure (Schneider, et al. 2017). This framework serves as the
basis for continuous improvement as well as system integration.
Fig 1 Health Care System Performance Rankings, 2017
4
It is one of the challenging works to measures as well as improves the health system
performance. Integrated performance and incentive framework developed by the
government of New Zealand in order to support the health system thereby addressing the
equity, quality, access, safety and cost of services (Cumming, 2017). High-level directions are
set through this framework to improve the effectiveness along with the productivity of the
healthcare for the public, also monitor the progress regarding the better services and also
create a surrounding in order to support constructive, cooperative, professionally driven
quality development in the primary services.
The scope of this framework is broad enough to align with the Triple Aims Approach
developed by the institutes for healthcare improvement. There are two levels of
measurement in this framework that is system and contributory level. National Health
Targets are incorporated in this framework. It is essential for the front line health
professional to ensure the effective quality improvement together with the referred services
management process which needs to be organized at the local level through the guidance of
national requirements.
The aim of System level measures framework is to enhance the health outcomes for the
public through the support to District Health Boards, however, collaborating work with the
health system partners such as hospitals, community and primary care with the help of
specific quality improvement measure (Schneider, et al. 2017). This framework serves as the
basis for continuous improvement as well as system integration.
Fig 1 Health Care System Performance Rankings, 2017
4
[Source: http://www.commonwealthfund.org/interactives/2017/july/mirror-mirror/]
It is observed that the health care performance level of New Zealand is well however the
ranks of the New Zealand is at 4th position while comparing with the other nations such as
Australian healthcare system which is at 2nd position (Duckett, 2017). Australian healthcare
system is advanced and improved from that of New Zealand in terms of care process,
equity, cost of services, access and health care outcomes. The reason being growing gap
between high as well as low income earners, Majority of the people are unable to afford the
medical and dental care.
5
It is observed that the health care performance level of New Zealand is well however the
ranks of the New Zealand is at 4th position while comparing with the other nations such as
Australian healthcare system which is at 2nd position (Duckett, 2017). Australian healthcare
system is advanced and improved from that of New Zealand in terms of care process,
equity, cost of services, access and health care outcomes. The reason being growing gap
between high as well as low income earners, Majority of the people are unable to afford the
medical and dental care.
5
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
THE ROLE OF GOVERNMENT
The healthcare of New Zealand is created by an amalgamation of the private and public
system to deliver health care services. The role of the government in New Zealand is
essential to provide health care requirement and needs for the total population as per the
consensus develop through the Social Security Act 1938. Central role is played by the New
Zealand government through the health strategy of New Zealand to set the policy agenda
and service requirement along with the determining the annual health budget funded by
public (Pegasus Health, 2014). The Ministry of Health appoints 4 out of 7 locally elected
members for 20 geographical defined district health boards, who are responsible to plan,
purchase, and provide the health services and disability support to the people ageing over
65 years (Pegasus Health, 2014).
Objectives, targets and services requirements set by government are pursued by these
boards while they operate through government-owned hospitals as well as health centers.
They also provide community services and purchase services form both non-government
and private service providers (Pegasus Health, 2014). Essential health care services are
offered to the local citizens and also to the people who have a work permit valid for two or
more than two years.
It is observed that there is no or little improvement in the indigenous health over the last 10
years or more in Australia. There is greater gap in socioeconomic status between indigenous
Australian. The education system and public policies are less culturally and linguistically
diverse in Australia as compared to that of New Zealand (Medical Council of New Zealand,
2018). Some of the factors are demographics, treaties, funding inadequacies and workforce
deficiency that contribute to the lack of improvement and poorer health status of
indigenous Australians as compared to the New Zealanders.
6
The healthcare of New Zealand is created by an amalgamation of the private and public
system to deliver health care services. The role of the government in New Zealand is
essential to provide health care requirement and needs for the total population as per the
consensus develop through the Social Security Act 1938. Central role is played by the New
Zealand government through the health strategy of New Zealand to set the policy agenda
and service requirement along with the determining the annual health budget funded by
public (Pegasus Health, 2014). The Ministry of Health appoints 4 out of 7 locally elected
members for 20 geographical defined district health boards, who are responsible to plan,
purchase, and provide the health services and disability support to the people ageing over
65 years (Pegasus Health, 2014).
Objectives, targets and services requirements set by government are pursued by these
boards while they operate through government-owned hospitals as well as health centers.
They also provide community services and purchase services form both non-government
and private service providers (Pegasus Health, 2014). Essential health care services are
offered to the local citizens and also to the people who have a work permit valid for two or
more than two years.
It is observed that there is no or little improvement in the indigenous health over the last 10
years or more in Australia. There is greater gap in socioeconomic status between indigenous
Australian. The education system and public policies are less culturally and linguistically
diverse in Australia as compared to that of New Zealand (Medical Council of New Zealand,
2018). Some of the factors are demographics, treaties, funding inadequacies and workforce
deficiency that contribute to the lack of improvement and poorer health status of
indigenous Australians as compared to the New Zealanders.
6
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
HEALTH CARE FUNDING
A broad range of services is accessible to all the permanent residents that are largely
financed through general taxations. Public health providers in New Zealand charge full cost
of the services to non-residents and tourists (Ministry of Health, 2016). However, everyone
including the visitors in New Zealand is covered for any injury or accidents under the
personal injury scheme that is Accident Compensation Corporation organized by the
government covering full ranges of injuries by pay for medical or treatment fees along with
the rehabilitation costs or residential care.
Vote health is the primary sources of funding for the health and disability system in New
Zealand that is over $16.142 billion in 2016-17. Out-of-pockets and insurance are some
private sources and Accident Compensation Corporation, local government and other
government agencies are some of the other sources of funding (Ministry of Health, 2016).
About 19 per cent of the public funding is provided by the Ministry of Health in order to
fund different important services such as disability support services, specific screening
programmes, public health services, elective services and mental health services. About
$2.879 billion worth of the health, as well as disability support and services, are purchased
by the ministry of health (Ministry of Health, 2016).
About one per cent that is $196 million worth of funding from Vote Health is spent on the
functioning of ministry that supports, governs, develops and oversees the broad health as
well as disability sector (Keene, et al. 2016). It is observed by prof. Jeff Richardson that the
situations in New Zealand and Australia are parallel, however, the unsustainability myth has
occurred due to concentrating on percentages rather than on the absolute level of
resources available.
7
A broad range of services is accessible to all the permanent residents that are largely
financed through general taxations. Public health providers in New Zealand charge full cost
of the services to non-residents and tourists (Ministry of Health, 2016). However, everyone
including the visitors in New Zealand is covered for any injury or accidents under the
personal injury scheme that is Accident Compensation Corporation organized by the
government covering full ranges of injuries by pay for medical or treatment fees along with
the rehabilitation costs or residential care.
Vote health is the primary sources of funding for the health and disability system in New
Zealand that is over $16.142 billion in 2016-17. Out-of-pockets and insurance are some
private sources and Accident Compensation Corporation, local government and other
government agencies are some of the other sources of funding (Ministry of Health, 2016).
About 19 per cent of the public funding is provided by the Ministry of Health in order to
fund different important services such as disability support services, specific screening
programmes, public health services, elective services and mental health services. About
$2.879 billion worth of the health, as well as disability support and services, are purchased
by the ministry of health (Ministry of Health, 2016).
About one per cent that is $196 million worth of funding from Vote Health is spent on the
functioning of ministry that supports, governs, develops and oversees the broad health as
well as disability sector (Keene, et al. 2016). It is observed by prof. Jeff Richardson that the
situations in New Zealand and Australia are parallel, however, the unsustainability myth has
occurred due to concentrating on percentages rather than on the absolute level of
resources available.
7
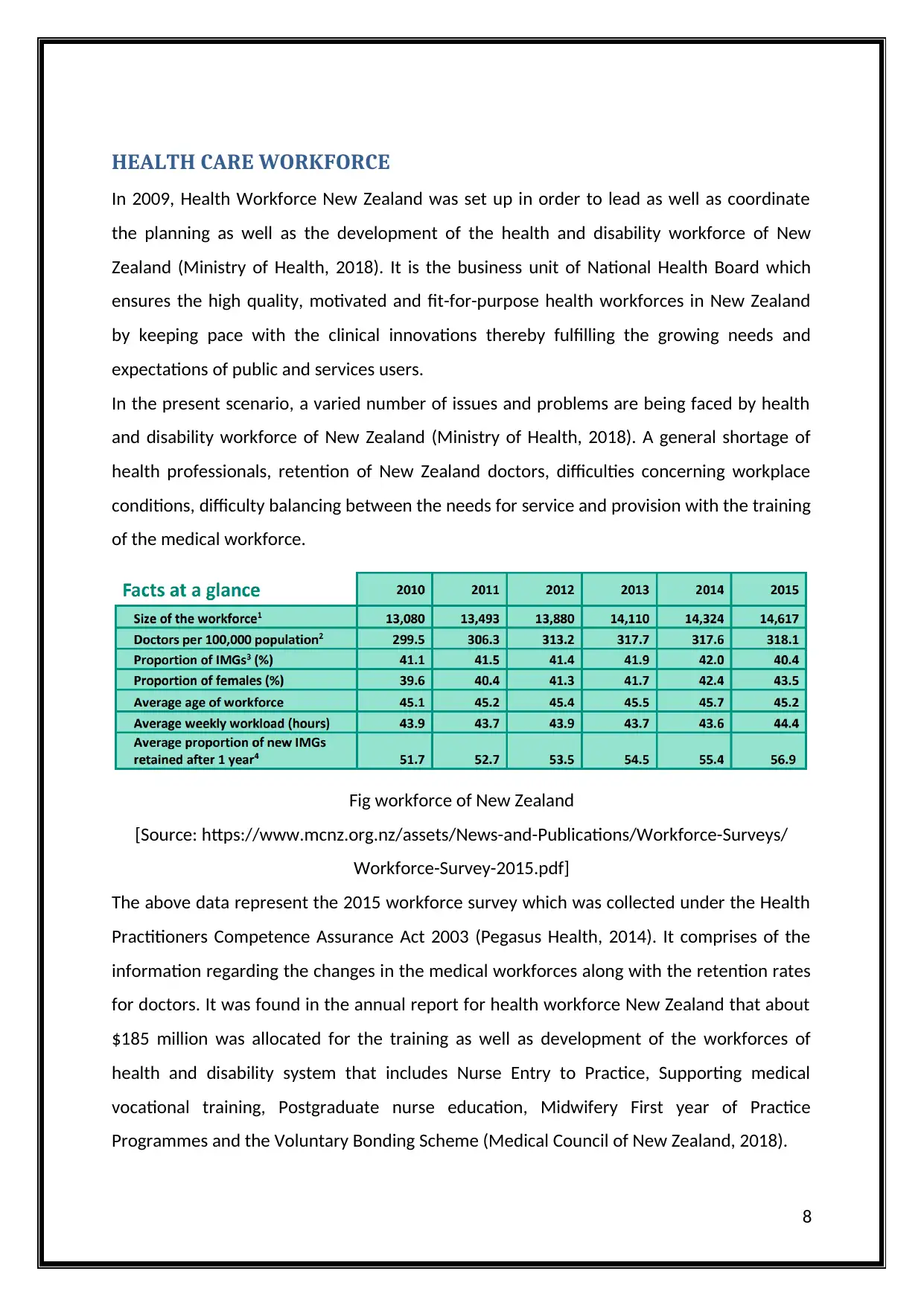
HEALTH CARE WORKFORCE
In 2009, Health Workforce New Zealand was set up in order to lead as well as coordinate
the planning as well as the development of the health and disability workforce of New
Zealand (Ministry of Health, 2018). It is the business unit of National Health Board which
ensures the high quality, motivated and fit-for-purpose health workforces in New Zealand
by keeping pace with the clinical innovations thereby fulfilling the growing needs and
expectations of public and services users.
In the present scenario, a varied number of issues and problems are being faced by health
and disability workforce of New Zealand (Ministry of Health, 2018). A general shortage of
health professionals, retention of New Zealand doctors, difficulties concerning workplace
conditions, difficulty balancing between the needs for service and provision with the training
of the medical workforce.
Fig workforce of New Zealand
[Source: https://www.mcnz.org.nz/assets/News-and-Publications/Workforce-Surveys/
Workforce-Survey-2015.pdf]
The above data represent the 2015 workforce survey which was collected under the Health
Practitioners Competence Assurance Act 2003 (Pegasus Health, 2014). It comprises of the
information regarding the changes in the medical workforces along with the retention rates
for doctors. It was found in the annual report for health workforce New Zealand that about
$185 million was allocated for the training as well as development of the workforces of
health and disability system that includes Nurse Entry to Practice, Supporting medical
vocational training, Postgraduate nurse education, Midwifery First year of Practice
Programmes and the Voluntary Bonding Scheme (Medical Council of New Zealand, 2018).
8
In 2009, Health Workforce New Zealand was set up in order to lead as well as coordinate
the planning as well as the development of the health and disability workforce of New
Zealand (Ministry of Health, 2018). It is the business unit of National Health Board which
ensures the high quality, motivated and fit-for-purpose health workforces in New Zealand
by keeping pace with the clinical innovations thereby fulfilling the growing needs and
expectations of public and services users.
In the present scenario, a varied number of issues and problems are being faced by health
and disability workforce of New Zealand (Ministry of Health, 2018). A general shortage of
health professionals, retention of New Zealand doctors, difficulties concerning workplace
conditions, difficulty balancing between the needs for service and provision with the training
of the medical workforce.
Fig workforce of New Zealand
[Source: https://www.mcnz.org.nz/assets/News-and-Publications/Workforce-Surveys/
Workforce-Survey-2015.pdf]
The above data represent the 2015 workforce survey which was collected under the Health
Practitioners Competence Assurance Act 2003 (Pegasus Health, 2014). It comprises of the
information regarding the changes in the medical workforces along with the retention rates
for doctors. It was found in the annual report for health workforce New Zealand that about
$185 million was allocated for the training as well as development of the workforces of
health and disability system that includes Nurse Entry to Practice, Supporting medical
vocational training, Postgraduate nurse education, Midwifery First year of Practice
Programmes and the Voluntary Bonding Scheme (Medical Council of New Zealand, 2018).
8
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
A number of boards, committees and commissions such as SMO commission, RMO
commission and Medical training board have been exploring the ways to tackle the issues
related to the health and disability workforce. Workforce issues are prevalent in both
Australia and New Zealand which needs to be resolved (Medical Council of New Zealand,
2018). There is a paucity of indigenous doctors and health workers in both the regions
despite the declaration and strategies designed by the government for redressing the
shortage over the years.
9
commission and Medical training board have been exploring the ways to tackle the issues
related to the health and disability workforce. Workforce issues are prevalent in both
Australia and New Zealand which needs to be resolved (Medical Council of New Zealand,
2018). There is a paucity of indigenous doctors and health workers in both the regions
despite the declaration and strategies designed by the government for redressing the
shortage over the years.
9
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CONCLUSION
Thus the conclusion is that considering the different characteristics of health care system of
both New Zealand and Australia. There is not much difference in the healthcare
management of both the regions. The healthcare system of Australia is unique however it
needs to be accessible and efficient along with the maintaining cost of health services.
Whereas the health care system of New Zealand is comprehensive but it needs to be
accessible, equity and concern over health care outcomes (Schneider, et al. 2017).
10
Thus the conclusion is that considering the different characteristics of health care system of
both New Zealand and Australia. There is not much difference in the healthcare
management of both the regions. The healthcare system of Australia is unique however it
needs to be accessible and efficient along with the maintaining cost of health services.
Whereas the health care system of New Zealand is comprehensive but it needs to be
accessible, equity and concern over health care outcomes (Schneider, et al. 2017).
10
REFERENCES
1. Cumming, J., 2017. New Zealand’s health service performs well, but inequities
remain high [Online available at https://theconversation.com/new-zealands-health-
service-performs-well-but-inequities-remain-high-82648] [Last accessed on 29-05-
2018]
2. Duckett, S., 2017. Australia’s health system is enviable, but there’s room for
improvement [Online available at https://theconversation.com/australias-health-
system-is-enviable-but-theres-room-for-improvement-81332] [Last accessed on 29-
05-2018]
3. Gauld, R., University of Otago, New Zealand, 2016. The New Zealand Health Care
System [Online available at
http://international.commonwealthfund.org/countries/new_zealand/] [Last
accessed on 29-05-2018]
4. Keene L., Bagshaw P., Nicholls M. G., Rosenberg B., Frampton C. M., Powell I., 2016.
Funding New Zealand’s public healthcare system: time for an honest appraisal and
public debate [Online available at https://www.nzma.org.nz/journal/read-the-
journal/all-issues/2010-2019/2016/vol-129-no-1435-27-may-2016/6891] [Last
accessed on 29-05-2018]
5. Medical Council of New Zealand, 2018. Public and private health systems [Online
available at https://www.mcnz.org.nz/alpinfo/public-and-private-health-systems]
[Last accessed on 29-05-2018]
6. Medical Council of New Zealand, 2018. The New Zealand Medical Workforce in 2015
[Online available at
https://www.mcnz.org.nz/assets/News-and-Publications/Workforce-Surveys/
Workforce-Survey-2015.pdf] [Last accessed on 29-05-2018]
7. Ministry of Health, 2016. Funding [Online available at
https://www.health.govt.nz/new-zealand-health-system/overview-health-system/
funding] [Last accessed on 29-05-2018]
11
1. Cumming, J., 2017. New Zealand’s health service performs well, but inequities
remain high [Online available at https://theconversation.com/new-zealands-health-
service-performs-well-but-inequities-remain-high-82648] [Last accessed on 29-05-
2018]
2. Duckett, S., 2017. Australia’s health system is enviable, but there’s room for
improvement [Online available at https://theconversation.com/australias-health-
system-is-enviable-but-theres-room-for-improvement-81332] [Last accessed on 29-
05-2018]
3. Gauld, R., University of Otago, New Zealand, 2016. The New Zealand Health Care
System [Online available at
http://international.commonwealthfund.org/countries/new_zealand/] [Last
accessed on 29-05-2018]
4. Keene L., Bagshaw P., Nicholls M. G., Rosenberg B., Frampton C. M., Powell I., 2016.
Funding New Zealand’s public healthcare system: time for an honest appraisal and
public debate [Online available at https://www.nzma.org.nz/journal/read-the-
journal/all-issues/2010-2019/2016/vol-129-no-1435-27-may-2016/6891] [Last
accessed on 29-05-2018]
5. Medical Council of New Zealand, 2018. Public and private health systems [Online
available at https://www.mcnz.org.nz/alpinfo/public-and-private-health-systems]
[Last accessed on 29-05-2018]
6. Medical Council of New Zealand, 2018. The New Zealand Medical Workforce in 2015
[Online available at
https://www.mcnz.org.nz/assets/News-and-Publications/Workforce-Surveys/
Workforce-Survey-2015.pdf] [Last accessed on 29-05-2018]
7. Ministry of Health, 2016. Funding [Online available at
https://www.health.govt.nz/new-zealand-health-system/overview-health-system/
funding] [Last accessed on 29-05-2018]
11
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





