Comparison Between Herbal and Orthodox Medicine
VerifiedAdded on 2022/04/26
|25
|8694
|32
AI Summary
Natural medicine treats the whole person, whereas conventional medicine practitioner simply treats the symptoms. In the traditional medical practise, you meet with your doctor for around fifteen minutes to discuss your problems. After that, you'll be given a prescription for drugs to help you disguise your symptoms.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
CHAPTER ONE
INTRODUCTION
1.1 Medicines/ Drugs
Medicines are chemicals or compounds used to cure, halt, or prevent disease; ease
symptoms; or help in the diagnosis of illnesses. Advances in medicines have enabled doctors to
cure many diseases and save lives. These days, medicines come from a variety of sources. Many
were developed from substances found in nature, and even today many are extracted from plants.
Some medicines are made in labs by mixing together a number of chemicals. Others, like
penicillin, are byproducts of organisms such as fungus. And a few are even biologically
engineered by inserting genes into bacteria that make them produce the desired substance. When
we think about taking medicines, we often think of pills (Elora, 2018). But medicines can be
delivered in many ways, such as:
liquids that are swallowed
drops that are put into ears or eyes
creams, gels, or ointments that are rubbed onto the skin
inhalers (like nasal sprays or asthma inhalers)
patches that are stuck to skin (called transdermal patches)
tablets that are placed under the tongue (called sublingual medicines; the medicine is
absorbed into blood vessels and enters the bloodstream)
injections (shots) or intravenous (inserted into a vein) medicines
No medicine can be sold unless it has first been approved by the National Agency for Food
and Drug Administration (NAFDAC). The makers of the medicine do tests on all new medicines
and send the results to NAFDAC. They allow new medicines to be used only if they work and if
they are safe enough. When a medicine's benefits outweigh its known risks, the FDA usually
approves the sale of the drug (Alamgir, 2017). NAFDAC can withdraw a medicine from the
INTRODUCTION
1.1 Medicines/ Drugs
Medicines are chemicals or compounds used to cure, halt, or prevent disease; ease
symptoms; or help in the diagnosis of illnesses. Advances in medicines have enabled doctors to
cure many diseases and save lives. These days, medicines come from a variety of sources. Many
were developed from substances found in nature, and even today many are extracted from plants.
Some medicines are made in labs by mixing together a number of chemicals. Others, like
penicillin, are byproducts of organisms such as fungus. And a few are even biologically
engineered by inserting genes into bacteria that make them produce the desired substance. When
we think about taking medicines, we often think of pills (Elora, 2018). But medicines can be
delivered in many ways, such as:
liquids that are swallowed
drops that are put into ears or eyes
creams, gels, or ointments that are rubbed onto the skin
inhalers (like nasal sprays or asthma inhalers)
patches that are stuck to skin (called transdermal patches)
tablets that are placed under the tongue (called sublingual medicines; the medicine is
absorbed into blood vessels and enters the bloodstream)
injections (shots) or intravenous (inserted into a vein) medicines
No medicine can be sold unless it has first been approved by the National Agency for Food
and Drug Administration (NAFDAC). The makers of the medicine do tests on all new medicines
and send the results to NAFDAC. They allow new medicines to be used only if they work and if
they are safe enough. When a medicine's benefits outweigh its known risks, the FDA usually
approves the sale of the drug (Alamgir, 2017). NAFDAC can withdraw a medicine from the
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
market at any time if it later is found to cause harmful side effects. Medicines act in a variety of
ways. Some can cure an illness by killing or halting the spread of invading germs, such as
bacteria and viruses. Others are used to treat cancer by killing cells as they divide or preventing
them from multiplying. Some drugs replace missing substances or correct low levels of natural
body chemicals such as some hormones or vitamins. Medicines can even affect parts of the
nervous system that control a body process (Aguwa et al., 2006).
Nearly everyone has taken an antibiotic. This type of medicine fights bacterial infections.
Your doctor may prescribe an antibiotic for things like strep throat or an ear infection.
Antibiotics work either by killing bacteria or halting their multiplication so that the body's
immune system can fight off the infection. Sometimes a part of the body can't make enough of a
chemical. That can also make you sick. Someone with insulin-dependent diabetes, for instance,
has a pancreas that can't produce enough insulin (a hormone that regulates glucose in the body).
Some people have a low production of thyroid hormone, which helps control how the body uses
energy. In each case, doctors can prescribe medicines to replace the missing hormone. Some
medicines treat symptoms but can't cure the illness that causes the symptoms. (A symptom is
anything you feel while you're sick, such as a cough or nausea.) So taking a lozenge may soothe
a sore throat, but it won't kill that nasty strep bacteria (Elora et al., 2018; Aguwa, 2006).
Some medicines relieve pain. If you pull a muscle, your doctor might tell you to take
ibuprofen or acetaminophen. These pain relievers, or analgesics, don't get rid of the source of the
pain — your muscle will still be pulled. What they do is block the pathways that transmit pain
signals from the injured or irritated body part to the brain (in other words, they affect the way the
brain reads the pain signal) so that you don't hurt as much while your body recovers. As people
get older, they sometimes develop chronic or long-term conditions (Kishore, 2017). Medicines
can help control things like high blood pressure (hypertension) or high cholesterol. These drugs
don't cure the underlying problem, but they can help prevent some of its body-damaging effects
over time.
Among the most important medicines are immunizations (or vaccines). These keep people
from getting sick in the first place by immunizing, or protecting, the body against some
infectious diseases. Vaccines usually contain a small amount of an agent that resembles a
ways. Some can cure an illness by killing or halting the spread of invading germs, such as
bacteria and viruses. Others are used to treat cancer by killing cells as they divide or preventing
them from multiplying. Some drugs replace missing substances or correct low levels of natural
body chemicals such as some hormones or vitamins. Medicines can even affect parts of the
nervous system that control a body process (Aguwa et al., 2006).
Nearly everyone has taken an antibiotic. This type of medicine fights bacterial infections.
Your doctor may prescribe an antibiotic for things like strep throat or an ear infection.
Antibiotics work either by killing bacteria or halting their multiplication so that the body's
immune system can fight off the infection. Sometimes a part of the body can't make enough of a
chemical. That can also make you sick. Someone with insulin-dependent diabetes, for instance,
has a pancreas that can't produce enough insulin (a hormone that regulates glucose in the body).
Some people have a low production of thyroid hormone, which helps control how the body uses
energy. In each case, doctors can prescribe medicines to replace the missing hormone. Some
medicines treat symptoms but can't cure the illness that causes the symptoms. (A symptom is
anything you feel while you're sick, such as a cough or nausea.) So taking a lozenge may soothe
a sore throat, but it won't kill that nasty strep bacteria (Elora et al., 2018; Aguwa, 2006).
Some medicines relieve pain. If you pull a muscle, your doctor might tell you to take
ibuprofen or acetaminophen. These pain relievers, or analgesics, don't get rid of the source of the
pain — your muscle will still be pulled. What they do is block the pathways that transmit pain
signals from the injured or irritated body part to the brain (in other words, they affect the way the
brain reads the pain signal) so that you don't hurt as much while your body recovers. As people
get older, they sometimes develop chronic or long-term conditions (Kishore, 2017). Medicines
can help control things like high blood pressure (hypertension) or high cholesterol. These drugs
don't cure the underlying problem, but they can help prevent some of its body-damaging effects
over time.
Among the most important medicines are immunizations (or vaccines). These keep people
from getting sick in the first place by immunizing, or protecting, the body against some
infectious diseases. Vaccines usually contain a small amount of an agent that resembles a
specific germ or germs that have been modified or killed. When someone is vaccinated, it primes
the body's immune system to "remember" the germ so it will be able to fight off infection by that
germ in the future (Kishan et al., 2009).
Most immunizations that prevent you from catching diseases like measles, whooping
cough, and chickenpox are given by injection. No one thinks shots are fun. But the diseases they
prevent can be very serious and cause symptoms that last much longer than the temporary
discomfort of the shot. To make life easier, now you can get immunizations at many pharmacies.
Although some medicines require a prescription, some are available in stores. You can buy many
medicines for pain, fever, cough, or allergies without a prescription (Alamgir et al., 2017). But
just because a medicine is available over-the-counter (OTC), that doesn't mean it's free of side
effects. Take OTC medicines with the same caution as those prescribed by a doctor.
1.2 Sources of Medicines
1.2.1 Plants Sources
A number of plants have medicinal qualities and have been used for centuries as drugs or
drug sources. Although the earliest plant source for drugs was the leaf, other parts of plants (e.g.,
barks, fruits, roots, stem, wood, seeds, blossoms, bulb etc.) were also later exploited for drug
extraction. Where the product is used without further processing e.g., ground leaves or bark,
boiled concoctions or powdered sap, the substance is called crude drug. The world's flowering
plant species have been used medicinally. Sometimes the figure of 70,000 medicinal plant
species is cited, but this includes many algae, fungi, and micro-organisms that are not really
plants as the word is understood by botanists (WHO, 2005).
These days the term Alternative Medicine became very common in western culture, it
focus on the idea of using the plants for medicinal purpose. But the current belief that medicines
which come in capsules or pills are the only medicines that we can trust and use. Even so most of
these pills and capsules we take and use during our daily life came from plants. Medicinal plants
frequently used as raw materials for extraction of active ingredients which used in the synthesis
of different drugs. Like in case of laxatives, blood thinners, antibiotics and antimalaria
medications, contain ingredients from plants. Medicinal plants have a promising future because
the body's immune system to "remember" the germ so it will be able to fight off infection by that
germ in the future (Kishan et al., 2009).
Most immunizations that prevent you from catching diseases like measles, whooping
cough, and chickenpox are given by injection. No one thinks shots are fun. But the diseases they
prevent can be very serious and cause symptoms that last much longer than the temporary
discomfort of the shot. To make life easier, now you can get immunizations at many pharmacies.
Although some medicines require a prescription, some are available in stores. You can buy many
medicines for pain, fever, cough, or allergies without a prescription (Alamgir et al., 2017). But
just because a medicine is available over-the-counter (OTC), that doesn't mean it's free of side
effects. Take OTC medicines with the same caution as those prescribed by a doctor.
1.2 Sources of Medicines
1.2.1 Plants Sources
A number of plants have medicinal qualities and have been used for centuries as drugs or
drug sources. Although the earliest plant source for drugs was the leaf, other parts of plants (e.g.,
barks, fruits, roots, stem, wood, seeds, blossoms, bulb etc.) were also later exploited for drug
extraction. Where the product is used without further processing e.g., ground leaves or bark,
boiled concoctions or powdered sap, the substance is called crude drug. The world's flowering
plant species have been used medicinally. Sometimes the figure of 70,000 medicinal plant
species is cited, but this includes many algae, fungi, and micro-organisms that are not really
plants as the word is understood by botanists (WHO, 2005).
These days the term Alternative Medicine became very common in western culture, it
focus on the idea of using the plants for medicinal purpose. But the current belief that medicines
which come in capsules or pills are the only medicines that we can trust and use. Even so most of
these pills and capsules we take and use during our daily life came from plants. Medicinal plants
frequently used as raw materials for extraction of active ingredients which used in the synthesis
of different drugs. Like in case of laxatives, blood thinners, antibiotics and antimalaria
medications, contain ingredients from plants. Medicinal plants have a promising future because
there are about half million plants around the world, and most of them their medical activities
have not investigate yet, and their medical activities could be decisive in the treatment of present
or future studies (Krishna et al., 2011).
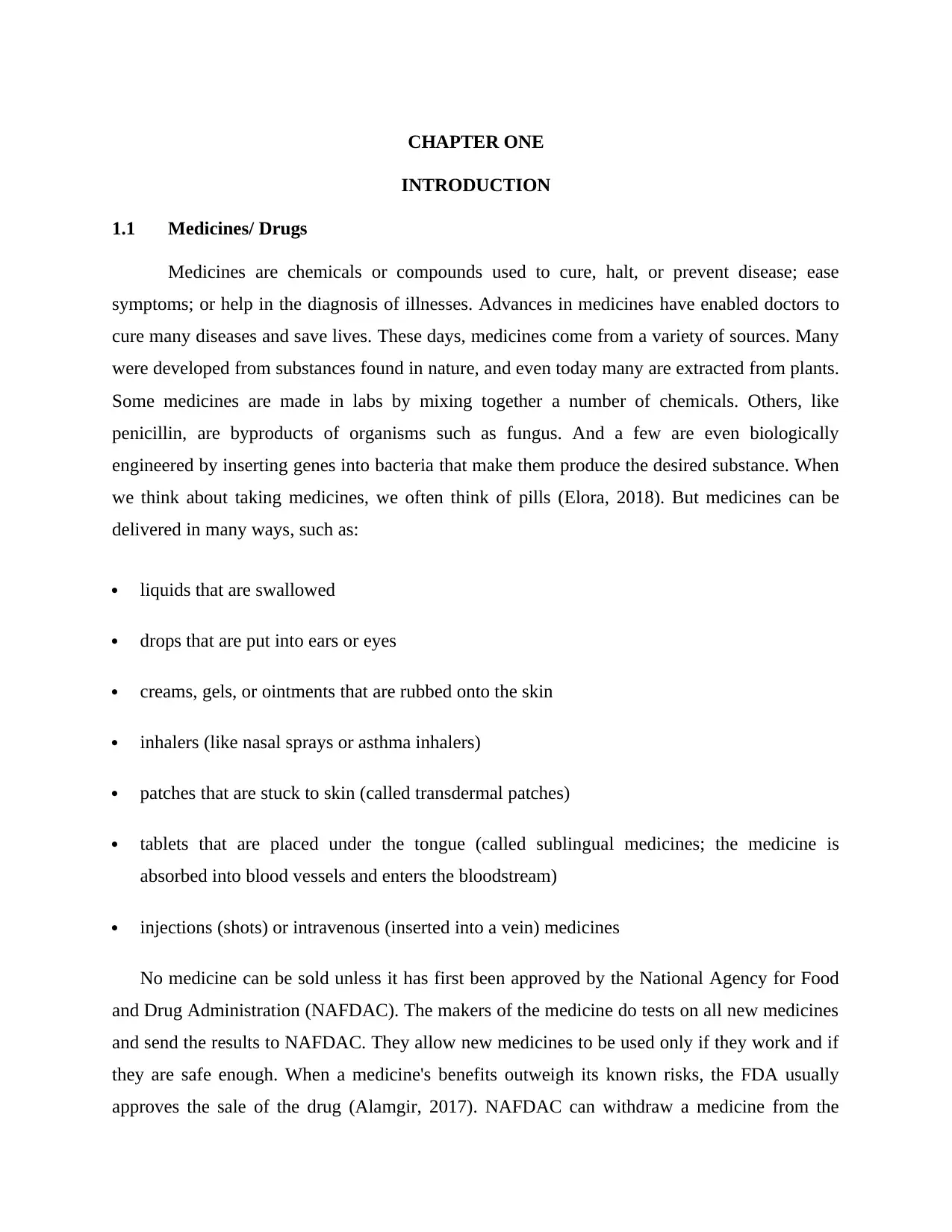
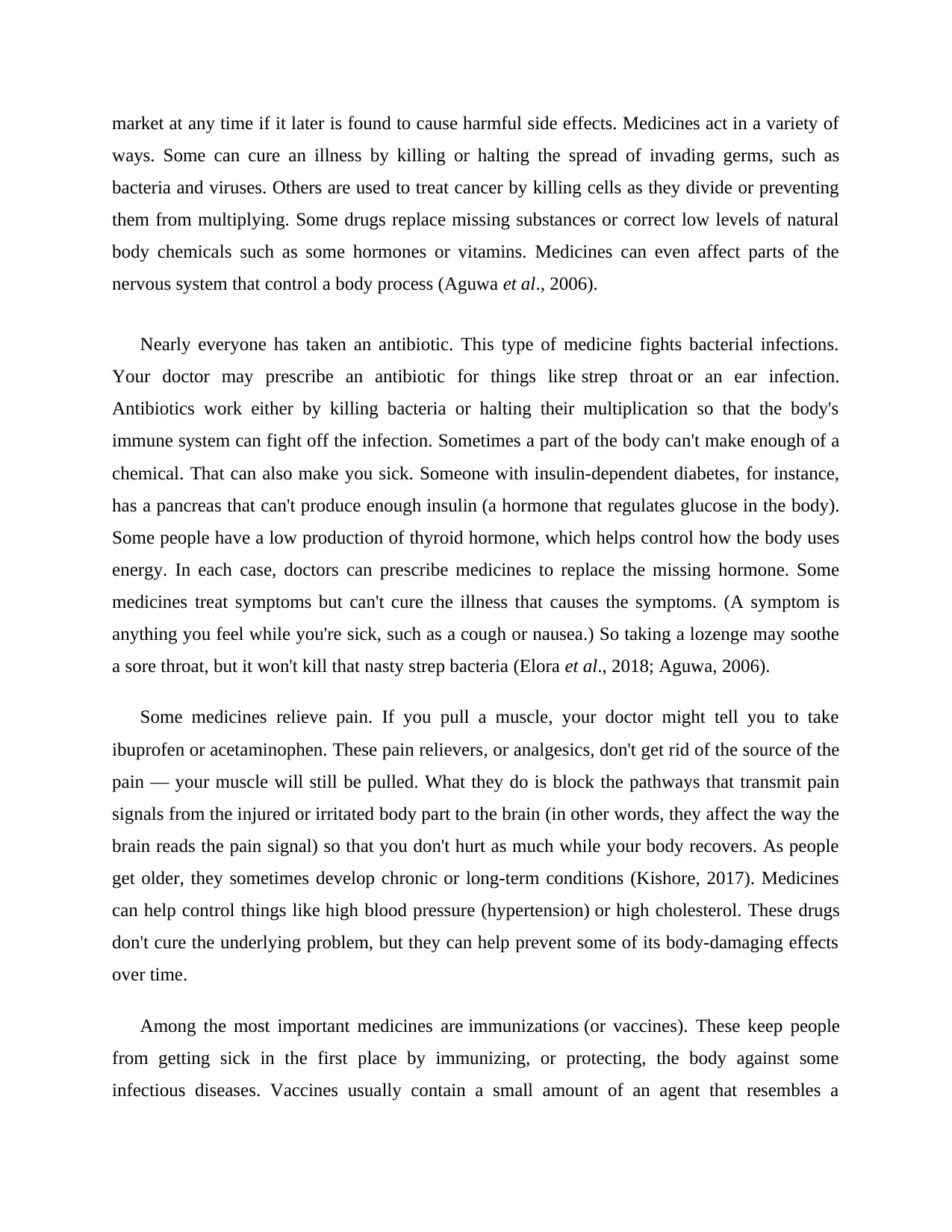
The table below shows some pharmacologically active principles or drugs derived from
various parts of a plant.
Plant part Drugs
Leaves Digoxin, digitoxin (from Digitalis purpurea/foxglove plant); atropine
(from Atropa belladonna)
Flowers Vincristine, vinblastine (from Vinca rosea)
Fruits Physostigmine (from Physostigma venenosum/calabar bean)
Seeds Strychnine (from Nux vomica); physostigmine
(from Physostigma venenosum/calabar bean)
Roots Emetine (from Cephaelis ipecacuanha); reserpine (from Rauwolfa
serpentina)
Bark Quinine (from Cinchona); atropine (from Atropa belladonna)
Stem Tubocurarine (from Chondrodendron tomentosum)
(Aguwa and Akah, 2006)
1.2.2 Animal Sources
Many important drugs are derived from animal source. In most instances, these medicinal
substances are derived from the animal’s body secretions, fluid or glands. Insulin, heparin,
adrenaline, thyroxin, cod liver oil, musk, beeswax, enzymes, and antitoxins sera are some
examples of drugs obtained from animal sources. Like plant products, drugs from animal sources
may be crude (unrefined) or refined material (WHO, 2005).
have not investigate yet, and their medical activities could be decisive in the treatment of present
or future studies (Krishna et al., 2011).
The table below shows some pharmacologically active principles or drugs derived from
various parts of a plant.
Plant part Drugs
Leaves Digoxin, digitoxin (from Digitalis purpurea/foxglove plant); atropine
(from Atropa belladonna)
Flowers Vincristine, vinblastine (from Vinca rosea)
Fruits Physostigmine (from Physostigma venenosum/calabar bean)
Seeds Strychnine (from Nux vomica); physostigmine
(from Physostigma venenosum/calabar bean)
Roots Emetine (from Cephaelis ipecacuanha); reserpine (from Rauwolfa
serpentina)
Bark Quinine (from Cinchona); atropine (from Atropa belladonna)
Stem Tubocurarine (from Chondrodendron tomentosum)
(Aguwa and Akah, 2006)
1.2.2 Animal Sources
Many important drugs are derived from animal source. In most instances, these medicinal
substances are derived from the animal’s body secretions, fluid or glands. Insulin, heparin,
adrenaline, thyroxin, cod liver oil, musk, beeswax, enzymes, and antitoxins sera are some
examples of drugs obtained from animal sources. Like plant products, drugs from animal sources
may be crude (unrefined) or refined material (WHO, 2005).
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1.2.3 Microbial Source
Several life-saving drugs have been historically derived from microorganisms. Examples
include penicillin produced by Penicillium chrysogenum, streptomycin from Streptomyces
griseus, chloramphenicol from Streptomyces venezuelae, neomycin from Streptomyces
fradiae, bacitracin from Bacillus subtilis etc. Xanthan (polysaccharide gum secreted
by Xanthomonas campestris), dextran (polysaccharide of glucose synthesized by lactic acid
bacteria Leuconostoc mesenteroides, Streptococcus mutans, Lactobacillus brevis), curdian (β-
1,3-glucan polymer, product of Agrobacterium biobar and Alcaligenes faecalis), pullulan (a
polysaccharide polymer of maltotriose units produced from starch by the fungus Aureobasidium
pullulans) etc. are all examples of drugs from microbial sources (Kishore and Kishan, 2009).
1.2.4 Marine Sources
Bioactive compounds from marine flora and fauna have extensive past and present use in
the prevention, treatment or cure of many diseases. Coral, sponges, fish, and marine
microorganisms produce biologically potent chemicals with interesting anti-inflammatory, anti-
viral, and anticancer activity. For example curacin A from marine cyanobacterium Lyngbya
majuscule, eleutherobin from coral Eleutherobia sp., discodermolide from marine
sponge Discodermia dissoluta, etc. show potent anti-tumour activity (Alamgir, 2017).
1.2.5 Mineral Sources
Minerals (both metallic and non-metallic minerals) have been used as drugs since ancient
times. Our body requires trace elements of minerals in order to maintain homeostasis. Patients
lacking an adequate level of these materials may take specific mineral-based drugs to raise the
level of minerals. Examples include ferrous sulfate in iron deficiency anemia; magnesium sulfate
as purgative; magnesium trisilicate, aluminum hydroxide and sodium bicarbonate as antacids for
hyperacidity and peptic ulcer; zinc oxide ointment as skin protectant, in wounds and eczema;
gold salts (solganal, auranofin) as anti-inflammatory and in rheumatoid arthritis; selenium as
anti-dandruff (Alamgir, 2017).
Several life-saving drugs have been historically derived from microorganisms. Examples
include penicillin produced by Penicillium chrysogenum, streptomycin from Streptomyces
griseus, chloramphenicol from Streptomyces venezuelae, neomycin from Streptomyces
fradiae, bacitracin from Bacillus subtilis etc. Xanthan (polysaccharide gum secreted
by Xanthomonas campestris), dextran (polysaccharide of glucose synthesized by lactic acid
bacteria Leuconostoc mesenteroides, Streptococcus mutans, Lactobacillus brevis), curdian (β-
1,3-glucan polymer, product of Agrobacterium biobar and Alcaligenes faecalis), pullulan (a
polysaccharide polymer of maltotriose units produced from starch by the fungus Aureobasidium
pullulans) etc. are all examples of drugs from microbial sources (Kishore and Kishan, 2009).
1.2.4 Marine Sources
Bioactive compounds from marine flora and fauna have extensive past and present use in
the prevention, treatment or cure of many diseases. Coral, sponges, fish, and marine
microorganisms produce biologically potent chemicals with interesting anti-inflammatory, anti-
viral, and anticancer activity. For example curacin A from marine cyanobacterium Lyngbya
majuscule, eleutherobin from coral Eleutherobia sp., discodermolide from marine
sponge Discodermia dissoluta, etc. show potent anti-tumour activity (Alamgir, 2017).
1.2.5 Mineral Sources
Minerals (both metallic and non-metallic minerals) have been used as drugs since ancient
times. Our body requires trace elements of minerals in order to maintain homeostasis. Patients
lacking an adequate level of these materials may take specific mineral-based drugs to raise the
level of minerals. Examples include ferrous sulfate in iron deficiency anemia; magnesium sulfate
as purgative; magnesium trisilicate, aluminum hydroxide and sodium bicarbonate as antacids for
hyperacidity and peptic ulcer; zinc oxide ointment as skin protectant, in wounds and eczema;
gold salts (solganal, auranofin) as anti-inflammatory and in rheumatoid arthritis; selenium as
anti-dandruff (Alamgir, 2017).
1.2.6 Synthetic/Chemical Derivative
A synthetic drug is produced using chemical synthesis, which rearranges chemical
derivatives to form a new compound. The synthetic sources of drugs evolved with human skills
in the laboratory and advanced knowledge and understanding of phytochemical investigation. At
present, majority of drugs used in clinical practice are exclusively prepared synthetically in
pharmaceutical and chemical laboratory. One of the earliest synthetic drugs was sulphonamide,
which began with the synthesis of prontosil dye. Other examples include acetylsalicylic acid
(aspirin or ASA), oral antidiabetics, antihistamines, thiazide diuretics, chloroquine,
chlorpromazine, general and local anaesthetics, paracetamol, phenytoin etc. Synthetically
manufactured drugs generally have higher yields that are significantly associated with quality,
purity and low cost (Aguwa and Akah, 2006).
1.2.7 Semi Synthetic Sources
Semi-synthetic drugs are neither completely natural nor completely synthetic. They are a
hybrid and are generally made by chemically modifying substances that are available from
natural source to improve its potency, efficacy and/or reduce side effects. Sometimes, semi-
synthetic processes are used to prepare drugs when the natural sources may yield impure
compounds or when the synthesis of drugs (complex molecules) may be difficult, expensive, and
commercially unviable. In semi-synthetic drugs, the nucleus of drug obtained from natural
source is kept intact but the chemical structure is altered. Examples of semi-synthetic medicine
include heroin from morphine, bromoscopolamine from scopolamine, homatropine from
atropine, ampicillin from penicillin etc (Kishore and Kishan, 2009).
1.2.8 Biosynthetic sources (genetically engineered drugs)
This is relatively a new field which is being developed by mixing discoveries from
molecular biology, recombinant DNA technology, DNA alteration, gene splicing, immunology,
and immune pharmacology. Drugs developed using living organisms with the help of
biotechnology or genetic engineering are known as biologics, biopharmaceuticals, recombinant
A synthetic drug is produced using chemical synthesis, which rearranges chemical
derivatives to form a new compound. The synthetic sources of drugs evolved with human skills
in the laboratory and advanced knowledge and understanding of phytochemical investigation. At
present, majority of drugs used in clinical practice are exclusively prepared synthetically in
pharmaceutical and chemical laboratory. One of the earliest synthetic drugs was sulphonamide,
which began with the synthesis of prontosil dye. Other examples include acetylsalicylic acid
(aspirin or ASA), oral antidiabetics, antihistamines, thiazide diuretics, chloroquine,
chlorpromazine, general and local anaesthetics, paracetamol, phenytoin etc. Synthetically
manufactured drugs generally have higher yields that are significantly associated with quality,
purity and low cost (Aguwa and Akah, 2006).
1.2.7 Semi Synthetic Sources
Semi-synthetic drugs are neither completely natural nor completely synthetic. They are a
hybrid and are generally made by chemically modifying substances that are available from
natural source to improve its potency, efficacy and/or reduce side effects. Sometimes, semi-
synthetic processes are used to prepare drugs when the natural sources may yield impure
compounds or when the synthesis of drugs (complex molecules) may be difficult, expensive, and
commercially unviable. In semi-synthetic drugs, the nucleus of drug obtained from natural
source is kept intact but the chemical structure is altered. Examples of semi-synthetic medicine
include heroin from morphine, bromoscopolamine from scopolamine, homatropine from
atropine, ampicillin from penicillin etc (Kishore and Kishan, 2009).
1.2.8 Biosynthetic sources (genetically engineered drugs)
This is relatively a new field which is being developed by mixing discoveries from
molecular biology, recombinant DNA technology, DNA alteration, gene splicing, immunology,
and immune pharmacology. Drugs developed using living organisms with the help of
biotechnology or genetic engineering are known as biologics, biopharmaceuticals, recombinant
DNA expressed products, bioengineered, or genetically engineered drugs Examples include
recombinant Hepatitis B vaccine, recombinant insulin and others (Kishore et al., 2009).
1.3 Aim and Objectives of the Study
The aim of the study is to review the comparison between herbal and orthodox
medicines. The specific objectives are;
To review Herbal and Orthodox Medicines.
To examine the safety of both medicines.
To examine the side effects of both medicines.
recombinant Hepatitis B vaccine, recombinant insulin and others (Kishore et al., 2009).
1.3 Aim and Objectives of the Study
The aim of the study is to review the comparison between herbal and orthodox
medicines. The specific objectives are;
To review Herbal and Orthodox Medicines.
To examine the safety of both medicines.
To examine the side effects of both medicines.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
CHAPTER TWO
2.1 Herbal Medicines
Herbal medicine is a part and parcel of and sometimes synonymous with African
traditional medicine. It is the oldest and still the most widely used system of medicine in the
world today. It is used in all societies and is common to all cultures. Herbal medicines, also
called botanical medicines, vegetable medicines, or phytomedicines, as defined by World Health
Organization (WHO) refers to herbs, herbal materials, herbal preparations, and finished herbal
products that contain whole plants, parts of plants, or other plant materials, including leaves,
bark, berries, flowers, and roots, and/or their extracts as active ingredients intended for human
therapeutic use or for other benefits in humans and sometimes animals (Phua et al., 2009).
Herbal medicine is a special and prominent form of traditional medicine, in which the traditional
healer, in this case known as the herbalist, specializes in the use of herbs to treat various
ailments. Their role is so remarkable since it arises from a thorough knowledge of the medicinal
properties of indigenous plants and the pharmaceutical steps necessary in turning such plants into
drugs such as the selection, compounding, dosage, efficacy, and toxicity.
The use of herbal medicines appears to be universal in different cultures. However, the
plants used for the same ailments and the modes of treatment may vary from place to place. The
plants used for medicinal purposes are generally referred to as medicinal plants, i.e., any plant in
which one or more of its organs/parts contain substances that can be used for therapeutic
purposes, or in a more modern concept, the constituents can be used as precursors for the
synthesis of drugs. For example, a number of plants have been used in traditional medicine for
many years without scientific data to back up their efficacy. In this case, these plants, whole or
parts, which have medicinal properties, are referred to as crude drugs of natural or biological
origin. They may further be classified as “organized drugs,” if such drugs are from plant parts
with cellular structures such as leaf, bark, roots, etc., and “unorganized drugs,” if they are
obtained from a cellular portions of plants such as gums, balsams, gels, oils, and exudates.
Compared with modern allopathic medicine, herbal medicine is freely available and can easily be
accessed by all (Anoka, 2012).
2.1 Herbal Medicines
Herbal medicine is a part and parcel of and sometimes synonymous with African
traditional medicine. It is the oldest and still the most widely used system of medicine in the
world today. It is used in all societies and is common to all cultures. Herbal medicines, also
called botanical medicines, vegetable medicines, or phytomedicines, as defined by World Health
Organization (WHO) refers to herbs, herbal materials, herbal preparations, and finished herbal
products that contain whole plants, parts of plants, or other plant materials, including leaves,
bark, berries, flowers, and roots, and/or their extracts as active ingredients intended for human
therapeutic use or for other benefits in humans and sometimes animals (Phua et al., 2009).
Herbal medicine is a special and prominent form of traditional medicine, in which the traditional
healer, in this case known as the herbalist, specializes in the use of herbs to treat various
ailments. Their role is so remarkable since it arises from a thorough knowledge of the medicinal
properties of indigenous plants and the pharmaceutical steps necessary in turning such plants into
drugs such as the selection, compounding, dosage, efficacy, and toxicity.
The use of herbal medicines appears to be universal in different cultures. However, the
plants used for the same ailments and the modes of treatment may vary from place to place. The
plants used for medicinal purposes are generally referred to as medicinal plants, i.e., any plant in
which one or more of its organs/parts contain substances that can be used for therapeutic
purposes, or in a more modern concept, the constituents can be used as precursors for the
synthesis of drugs. For example, a number of plants have been used in traditional medicine for
many years without scientific data to back up their efficacy. In this case, these plants, whole or
parts, which have medicinal properties, are referred to as crude drugs of natural or biological
origin. They may further be classified as “organized drugs,” if such drugs are from plant parts
with cellular structures such as leaf, bark, roots, etc., and “unorganized drugs,” if they are
obtained from a cellular portions of plants such as gums, balsams, gels, oils, and exudates.
Compared with modern allopathic medicine, herbal medicine is freely available and can easily be
accessed by all (Anoka, 2012).
As a result, there is limited consultation with traditional healers because there is a fairly
good knowledge of common curative herbs especially in the rural areas except in the case of
treatment of chronic diseases (Anoka, 2012). Even where consultation is done, there is lack of
coherence among traditional healers on the preparation procedures and correct dosage of herbal
medicines (Wilcox and Bodeker, 2014). However, according to WHO (2005), at least 80% of
people in Africa still rely on medicinal plants for their health care. In Nigeria, and indeed the
entire West Africa, herbal medicine has continued to gain momentum, some of the advantages
being low cost, affordability, availability, acceptability, and apparently low toxicity (Parmer,
2015)
2.1.1 Plants part
A detail of plant parts used in herbal medicines is as follows:
i. Roots—i.e., the fleshy or woody roots of many African plant species are medicinal. Most
of the active ingredients are usually sequestered in the root bark rather than the woody
inner part.
ii. Bulbs—A bulb is an underground structure made up of numerous leaves of fleshy scales,
e.g., Allium sativa (garlic) and Allium cepa (onions).
iii. Rhizomes—Woody or fleshy underground stem that grows horizontally and brings out
their leaves above the ground, e.g., Zingiber officinale (ginger), which is used for
respiratory problems; Imperata cylindrica (spear grass) for potency in men and Curcuma
longa (turmeric), an antioxidant, anti-inflammatory, and anticancer drug.
iv. Tubers—Swollen fleshy underground structures which form from stems/roots, e.g.,
potatoes and yams such as Dioscorea dumetorum (ona-(igbo)) for diabetes and Gloriosa
superba for cancer
v. Bark—The outer protective layer of the tree stem or trunk. It contains highly
concentrated phytochemicals with profound medicinal properties. A host of plants have
barks of high medicinal value. 6. Leaves, stems, and flowers of many plants are also
medicinal.
vi. Fruits and seeds also contain highly active phytochemicals and essential oils.
good knowledge of common curative herbs especially in the rural areas except in the case of
treatment of chronic diseases (Anoka, 2012). Even where consultation is done, there is lack of
coherence among traditional healers on the preparation procedures and correct dosage of herbal
medicines (Wilcox and Bodeker, 2014). However, according to WHO (2005), at least 80% of
people in Africa still rely on medicinal plants for their health care. In Nigeria, and indeed the
entire West Africa, herbal medicine has continued to gain momentum, some of the advantages
being low cost, affordability, availability, acceptability, and apparently low toxicity (Parmer,
2015)
2.1.1 Plants part
A detail of plant parts used in herbal medicines is as follows:
i. Roots—i.e., the fleshy or woody roots of many African plant species are medicinal. Most
of the active ingredients are usually sequestered in the root bark rather than the woody
inner part.
ii. Bulbs—A bulb is an underground structure made up of numerous leaves of fleshy scales,
e.g., Allium sativa (garlic) and Allium cepa (onions).
iii. Rhizomes—Woody or fleshy underground stem that grows horizontally and brings out
their leaves above the ground, e.g., Zingiber officinale (ginger), which is used for
respiratory problems; Imperata cylindrica (spear grass) for potency in men and Curcuma
longa (turmeric), an antioxidant, anti-inflammatory, and anticancer drug.
iv. Tubers—Swollen fleshy underground structures which form from stems/roots, e.g.,
potatoes and yams such as Dioscorea dumetorum (ona-(igbo)) for diabetes and Gloriosa
superba for cancer
v. Bark—The outer protective layer of the tree stem or trunk. It contains highly
concentrated phytochemicals with profound medicinal properties. A host of plants have
barks of high medicinal value. 6. Leaves, stems, and flowers of many plants are also
medicinal.
vi. Fruits and seeds also contain highly active phytochemicals and essential oils.
vii. Gums, exudates, and nectars, which are secreted by plants to deter insects and grazing
animals and to seal off wounds, are very useful in the pharmaceutical industries.
Sale of herbs in form of dried or fresh plant parts is as lucrative as the prepared
medicines. They are usually displayed in markets and sold with instructions on how to prepare
them for maximum efficacy. In many areas of Africa, the knowledge of plant species used and
the methods of preparing and administering the medication, especially for serious ailments, still
reside with traditional healers. Secrecy and competition still surround the use of these
medications, with the healers often being reluctant to hand down their knowledge to anyone but
trusted relatives and initiates.
2.2 History of Use of Herbal Medicines
Historically the beneficial plants have always been thought of as the “people's medicine”.
They were often safer than chemical medicines, cheaper and more accessible to common folk.
Worldwide, it is estimated that there are 21,000 estimated medicinal plants. They are more
concentrated in the global biodiversity ‘hot-spots’ such as the Amazon rainforest of South
America, the Eastern Himalayas and Western Ghats in south Asia, and the Eastern Arc
Mountains and Coastal Forests of East Africa. Medicinal herbs, shrubs and trees are widely used
both in the developed and developing world for preparing traditional remedies that find both
domestic and commercial usage. In tropical Africa, more than 4,000 plant species are used for
medicinal purposes, and 50,000 tons of medicinal plants are consumed annually in the region.
There are more than 8,000 plant species in South Asia with known medicinal uses. Medicinal
plants are an accessible, affordable and culturally appropriate source of primary health care for
more than 80% of Asia's population (WHO).
Marginalized, rural and indigenous people, who cannot afford or access formal health
care systems, are especially dependent on these culturally familiar, technically simple,
financially affordable and generally effective traditional medicines. WHO has estimated that up
to 80 per cent of people in the developing countries depend upon traditional systems medicines
primarily because of their easy accessibility, wide affordability and cultural familiarity. In fact,
animals and to seal off wounds, are very useful in the pharmaceutical industries.
Sale of herbs in form of dried or fresh plant parts is as lucrative as the prepared
medicines. They are usually displayed in markets and sold with instructions on how to prepare
them for maximum efficacy. In many areas of Africa, the knowledge of plant species used and
the methods of preparing and administering the medication, especially for serious ailments, still
reside with traditional healers. Secrecy and competition still surround the use of these
medications, with the healers often being reluctant to hand down their knowledge to anyone but
trusted relatives and initiates.
2.2 History of Use of Herbal Medicines
Historically the beneficial plants have always been thought of as the “people's medicine”.
They were often safer than chemical medicines, cheaper and more accessible to common folk.
Worldwide, it is estimated that there are 21,000 estimated medicinal plants. They are more
concentrated in the global biodiversity ‘hot-spots’ such as the Amazon rainforest of South
America, the Eastern Himalayas and Western Ghats in south Asia, and the Eastern Arc
Mountains and Coastal Forests of East Africa. Medicinal herbs, shrubs and trees are widely used
both in the developed and developing world for preparing traditional remedies that find both
domestic and commercial usage. In tropical Africa, more than 4,000 plant species are used for
medicinal purposes, and 50,000 tons of medicinal plants are consumed annually in the region.
There are more than 8,000 plant species in South Asia with known medicinal uses. Medicinal
plants are an accessible, affordable and culturally appropriate source of primary health care for
more than 80% of Asia's population (WHO).
Marginalized, rural and indigenous people, who cannot afford or access formal health
care systems, are especially dependent on these culturally familiar, technically simple,
financially affordable and generally effective traditional medicines. WHO has estimated that up
to 80 per cent of people in the developing countries depend upon traditional systems medicines
primarily because of their easy accessibility, wide affordability and cultural familiarity. In fact,
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
as up to 40% of the world’s poor have no access to the government health services, traditional
and folk medicine is the only medicine available to them.
According to the World Health Organization (WHO, 1977) “A medicinal plant” is any
plant, in which one or more of its organ contains substances that can be used for the therapeutic
purposes or which, are precursors for the synthesis of useful drugs. This definition distinguishes
those plants whose therapeutic properties and constituents have been established scientifically
and plants that are regarded as medicinal but which have not yet been subjected to thorough
investigation. The term “herbal drug” determines the part/parts of a plant (leaves, flowers, seeds,
roots, barks and stems, etc.) used for preparing medicines (Anonymous, 2001a).
2.3 Method of Preparation and Dosage forms of Herbal Medicine
Methods of preparation of herbal medicines may vary according to place and culture. The
plant materials may be used fresh or dry. With experience, a particular method is chosen to
increase efficiency and decrease toxicity. Generally, different methods of preparation include:
Extraction—This is prepared with solvent on a weight by volume basis. Sometimes, the
solvent is evaporated to a soft mass.
Infusions are prepared by macerating the crude drug for a short period of time in cold or hot
water. A preservative such as honey may be added to prevent spoilage.
Decoctions are made by boiling woody pieces for a specified period of time and filtered.
Potash may be added to aid extraction and as preservative.
Tinctures are alcoholic infusions which if concentrated may be diluted before administration.
Ashing—The dried parts are incinerated to ash, then sieved and added as such to water or
food.
Miscellaneous—Other types include liniments for external applications in liquid, semi-liquid,
or oily forms containing the active substances; lotions which are liquid preparations intended
for skin application. Poultices are prepared from macerated fresh part of plant containing the
juice from the plant and applied to skin. Snuffs are powdered dried plant inhaled through the
and folk medicine is the only medicine available to them.
According to the World Health Organization (WHO, 1977) “A medicinal plant” is any
plant, in which one or more of its organ contains substances that can be used for the therapeutic
purposes or which, are precursors for the synthesis of useful drugs. This definition distinguishes
those plants whose therapeutic properties and constituents have been established scientifically
and plants that are regarded as medicinal but which have not yet been subjected to thorough
investigation. The term “herbal drug” determines the part/parts of a plant (leaves, flowers, seeds,
roots, barks and stems, etc.) used for preparing medicines (Anonymous, 2001a).
2.3 Method of Preparation and Dosage forms of Herbal Medicine
Methods of preparation of herbal medicines may vary according to place and culture. The
plant materials may be used fresh or dry. With experience, a particular method is chosen to
increase efficiency and decrease toxicity. Generally, different methods of preparation include:
Extraction—This is prepared with solvent on a weight by volume basis. Sometimes, the
solvent is evaporated to a soft mass.
Infusions are prepared by macerating the crude drug for a short period of time in cold or hot
water. A preservative such as honey may be added to prevent spoilage.
Decoctions are made by boiling woody pieces for a specified period of time and filtered.
Potash may be added to aid extraction and as preservative.
Tinctures are alcoholic infusions which if concentrated may be diluted before administration.
Ashing—The dried parts are incinerated to ash, then sieved and added as such to water or
food.
Miscellaneous—Other types include liniments for external applications in liquid, semi-liquid,
or oily forms containing the active substances; lotions which are liquid preparations intended
for skin application. Poultices are prepared from macerated fresh part of plant containing the
juice from the plant and applied to skin. Snuffs are powdered dried plant inhaled through the
nostrils. Dried plants may be burnt, and their charcoal is used as such. Gruels are
cereals/porridges made from grains, to which dried powdered plant or its ash is added to be
taken orally. Mixtures are sometimes prepared with more than one plant to give synergistic
or potentiating effects of the composite plants.
There are also different methods of administration. Apart from the common routes such as
oral, rectal, topical, and nasal, other methods include smoking a crudely prepared cigar
containing dried plant materials or by passive inhalation. Others are steaming and inhaling the
volatile oils exuding from the boiling plant material. These can be used to relieve congestion,
headaches, or pulmonary problems. Sitz baths are used for piles (Okafor, 2013).
2.4 Ethnobotanical Surveys
Information on plants is obtained through ethnobotanical surveys, which involves the
study of plants in relation to the culture of the people. Many plants are used in African traditional
medicine, but little information is available on their active ingredients/constituents.
Ethnobotanical surveys involve the interaction with the people and their environment and are
therefore participatory approaches, in which local people are able to contribute their knowledge
on the uses of plants within their environment. This may involve the identification,
documentation, conservation, and utilization of medicinal plants. Much of the ethnomedicinal
information is largely not validated.
In Nigeria, a number of authors have published a lot of data on plants with their curative
values (Iwu, 2014). These provide a vast array of information for scientific research and
validation. Preliminary scientific knowledge is drawn from studies on in vitro and in vivo
bioassays on crude extracts of various plants. Using plants as medicine provides significant
advantages for treating many chronic conditions. For example, information from folklore
medicine in Nigeria has it that Rauvolfia vomitoria is used for treating hypertension and other
nervous conditions while Ocimum gratissimum is used for treating diarrheal diseases. Others
include Citrus paradise seeds for resistant urinary tract infections, pure honey for chronic wound
treatment, Carica papaya seeds for intestinal parasites, Garcinia kola seeds for pain and
inflammation, and Aloe vera for skin diseases. The same is also true for plants from other
African countries (Oreagba et al., 2011). Knowledge of most of these curative properties was
cereals/porridges made from grains, to which dried powdered plant or its ash is added to be
taken orally. Mixtures are sometimes prepared with more than one plant to give synergistic
or potentiating effects of the composite plants.
There are also different methods of administration. Apart from the common routes such as
oral, rectal, topical, and nasal, other methods include smoking a crudely prepared cigar
containing dried plant materials or by passive inhalation. Others are steaming and inhaling the
volatile oils exuding from the boiling plant material. These can be used to relieve congestion,
headaches, or pulmonary problems. Sitz baths are used for piles (Okafor, 2013).
2.4 Ethnobotanical Surveys
Information on plants is obtained through ethnobotanical surveys, which involves the
study of plants in relation to the culture of the people. Many plants are used in African traditional
medicine, but little information is available on their active ingredients/constituents.
Ethnobotanical surveys involve the interaction with the people and their environment and are
therefore participatory approaches, in which local people are able to contribute their knowledge
on the uses of plants within their environment. This may involve the identification,
documentation, conservation, and utilization of medicinal plants. Much of the ethnomedicinal
information is largely not validated.
In Nigeria, a number of authors have published a lot of data on plants with their curative
values (Iwu, 2014). These provide a vast array of information for scientific research and
validation. Preliminary scientific knowledge is drawn from studies on in vitro and in vivo
bioassays on crude extracts of various plants. Using plants as medicine provides significant
advantages for treating many chronic conditions. For example, information from folklore
medicine in Nigeria has it that Rauvolfia vomitoria is used for treating hypertension and other
nervous conditions while Ocimum gratissimum is used for treating diarrheal diseases. Others
include Citrus paradise seeds for resistant urinary tract infections, pure honey for chronic wound
treatment, Carica papaya seeds for intestinal parasites, Garcinia kola seeds for pain and
inflammation, and Aloe vera for skin diseases. The same is also true for plants from other
African countries (Oreagba et al., 2011). Knowledge of most of these curative properties was
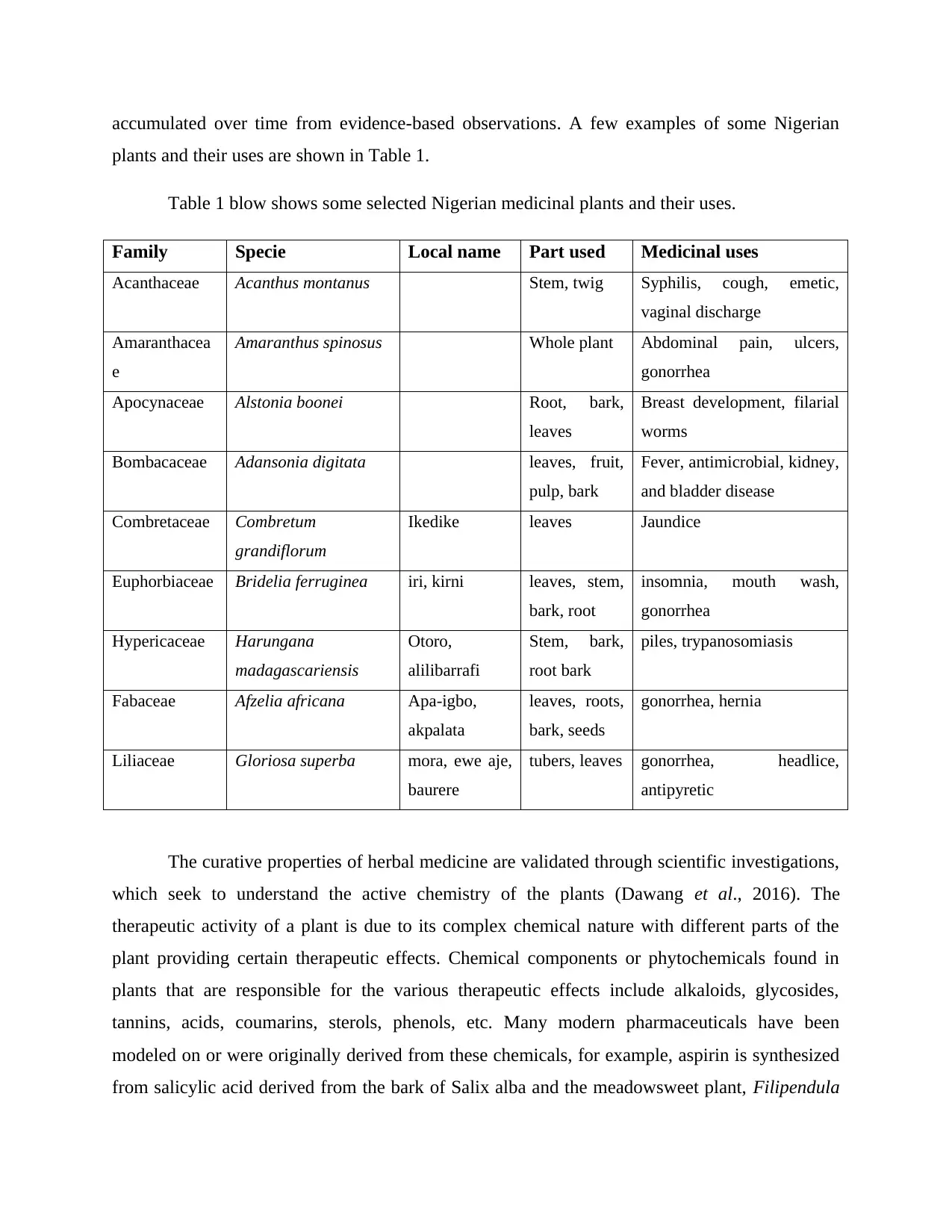
accumulated over time from evidence-based observations. A few examples of some Nigerian
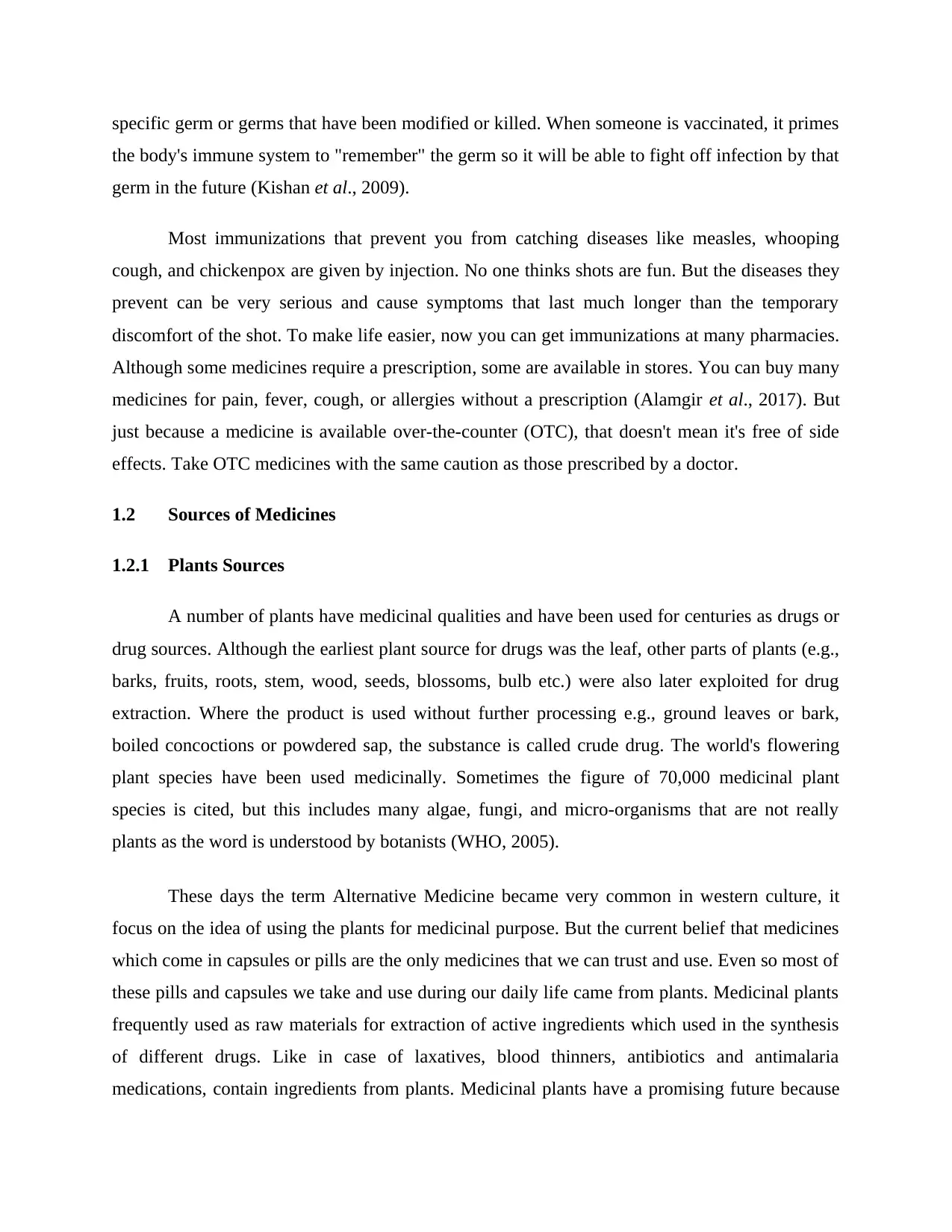
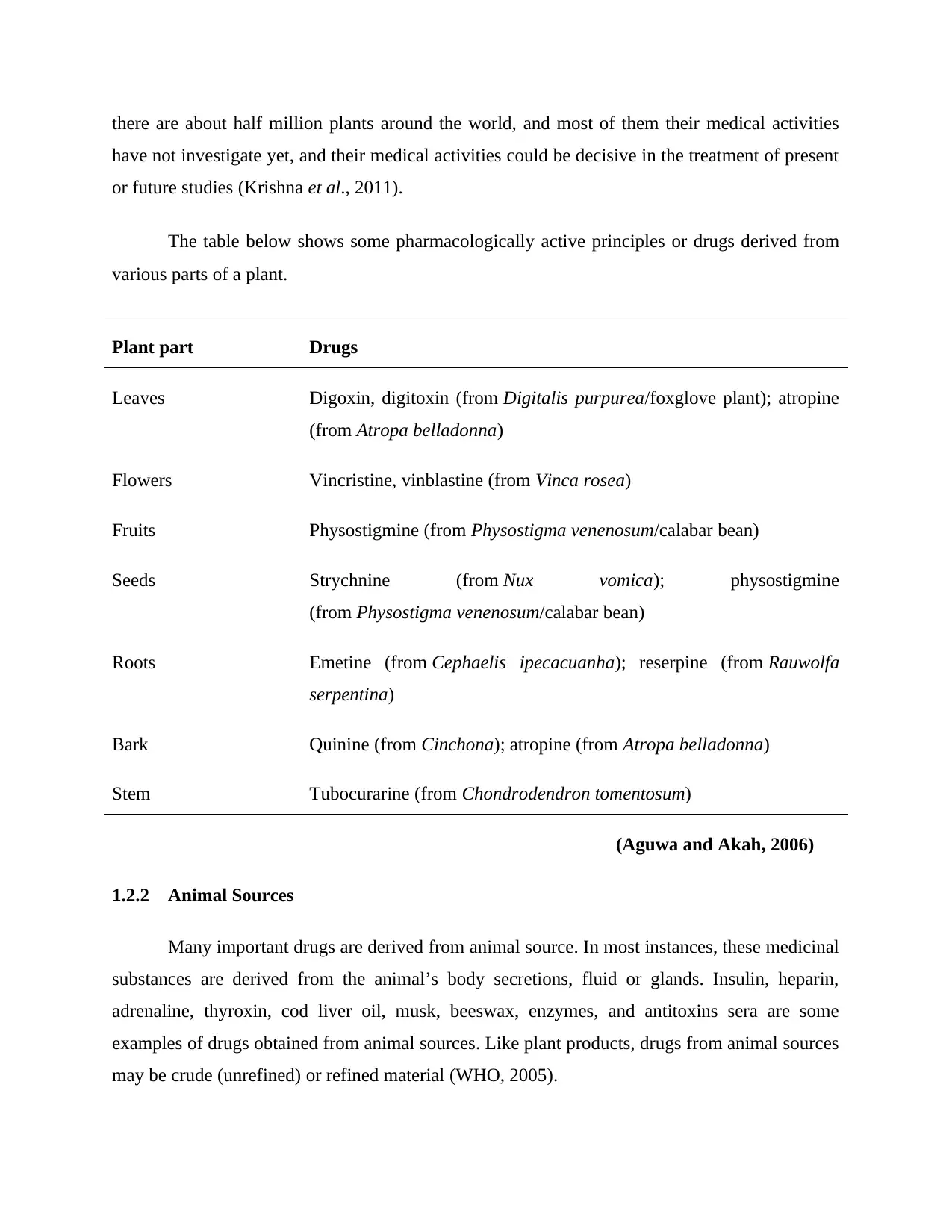
plants and their uses are shown in Table 1.
Table 1 blow shows some selected Nigerian medicinal plants and their uses.
Family Specie Local name Part used Medicinal uses
Acanthaceae Acanthus montanus Stem, twig Syphilis, cough, emetic,
vaginal discharge
Amaranthacea
e
Amaranthus spinosus Whole plant Abdominal pain, ulcers,
gonorrhea
Apocynaceae Alstonia boonei Root, bark,
leaves
Breast development, filarial
worms
Bombacaceae Adansonia digitata leaves, fruit,
pulp, bark
Fever, antimicrobial, kidney,
and bladder disease
Combretaceae Combretum
grandiflorum
Ikedike leaves Jaundice
Euphorbiaceae Bridelia ferruginea iri, kirni leaves, stem,
bark, root
insomnia, mouth wash,
gonorrhea
Hypericaceae Harungana
madagascariensis
Otoro,
alilibarrafi
Stem, bark,
root bark
piles, trypanosomiasis
Fabaceae Afzelia africana Apa-igbo,
akpalata
leaves, roots,
bark, seeds
gonorrhea, hernia
Liliaceae Gloriosa superba mora, ewe aje,
baurere
tubers, leaves gonorrhea, headlice,
antipyretic
The curative properties of herbal medicine are validated through scientific investigations,
which seek to understand the active chemistry of the plants (Dawang et al., 2016). The
therapeutic activity of a plant is due to its complex chemical nature with different parts of the
plant providing certain therapeutic effects. Chemical components or phytochemicals found in
plants that are responsible for the various therapeutic effects include alkaloids, glycosides,
tannins, acids, coumarins, sterols, phenols, etc. Many modern pharmaceuticals have been
modeled on or were originally derived from these chemicals, for example, aspirin is synthesized
from salicylic acid derived from the bark of Salix alba and the meadowsweet plant, Filipendula
plants and their uses are shown in Table 1.
Table 1 blow shows some selected Nigerian medicinal plants and their uses.
Family Specie Local name Part used Medicinal uses
Acanthaceae Acanthus montanus Stem, twig Syphilis, cough, emetic,
vaginal discharge
Amaranthacea
e
Amaranthus spinosus Whole plant Abdominal pain, ulcers,
gonorrhea
Apocynaceae Alstonia boonei Root, bark,
leaves
Breast development, filarial
worms
Bombacaceae Adansonia digitata leaves, fruit,
pulp, bark
Fever, antimicrobial, kidney,
and bladder disease
Combretaceae Combretum
grandiflorum
Ikedike leaves Jaundice
Euphorbiaceae Bridelia ferruginea iri, kirni leaves, stem,
bark, root
insomnia, mouth wash,
gonorrhea
Hypericaceae Harungana
madagascariensis
Otoro,
alilibarrafi
Stem, bark,
root bark
piles, trypanosomiasis
Fabaceae Afzelia africana Apa-igbo,
akpalata
leaves, roots,
bark, seeds
gonorrhea, hernia
Liliaceae Gloriosa superba mora, ewe aje,
baurere
tubers, leaves gonorrhea, headlice,
antipyretic
The curative properties of herbal medicine are validated through scientific investigations,
which seek to understand the active chemistry of the plants (Dawang et al., 2016). The
therapeutic activity of a plant is due to its complex chemical nature with different parts of the
plant providing certain therapeutic effects. Chemical components or phytochemicals found in
plants that are responsible for the various therapeutic effects include alkaloids, glycosides,
tannins, acids, coumarins, sterols, phenols, etc. Many modern pharmaceuticals have been
modeled on or were originally derived from these chemicals, for example, aspirin is synthesized
from salicylic acid derived from the bark of Salix alba and the meadowsweet plant, Filipendula
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ulmaria. Quinine from Cinchona pubescens bark and artemisinin from Artemisia annua plant are
antimalarial drugs.
Vincristine and vinblastine are anticancer drugs derived from Madagascar periwinkle
(Catharanthus roseus), used for treating leukemia. Morphine and codeine, derived from the
opium poppy (Papaver somniferum), are used in the treatment of diarrhea and pain relief, while
digitoxin is a cardiac glycoside derived from foxglove plant (Digitalis purpurea) (Dawang et al.,
2016). Medicinal plants are also important materials for the cosmetic industries. The use of
herbal drugs dwindled toward the end of the 19th century due to the advent of synthetic
chemistry. However, there was a resurgence of interest in plant medicines in more recent years,
as synthetic drugs became less effective due to high levels of resistance and also due to higher
toxicity and cost. It is estimated that more than half of all synthetic drugs in use are derived from
plants.
2.5 Herbal Medicines in Nigeria
The various ethnic groups in Nigeria have different health care practitioners aside their
western counterparts, whose mode of practice is not unlike in other tribes. The Yorubas call them
“babalawos,” the Igbos call them “dibia,” while the Northerners or Hausas call them “boka”
(Abdullaji, 2017). Traditional/herbal medicines have impacted the lives of people, especially in
the rural areas where access to orthodox medicare is limited (Abd El-Ghani, 2016). Apart from
the lack of adequate access and the fear of expired or fake drugs, the prohibitive cost of western
medicine makes traditional medicine attractive. Various training schools exist for both herbal
medicine and homeopathy, and as such, most modern traditional health practitioners have great
knowledge of pharmaceutical properties of herbs and the shared cultural views of diseases in the
society and they combine their knowledge with modern skills and techniques in processing and
preserving herbal medicines, as well as in the management of diseases.
In oral interviews with two modern traditional medicine practitioners, Dr. Anselm
Okonkwo of Saint Rita’s Ethnomedical Research Center, Enugu, Nigeria, a Veterinary doctor,
and Mr. Uche Omengoli of CGP Herba-Medical Consultancy and Research, Enugu, Nigeria, a
medical laboratory technologist, both revealed that their knowledge and ‘gift’ of medical practice
were handed down by aged relatives who were also in the practice by both tutelage and
antimalarial drugs.
Vincristine and vinblastine are anticancer drugs derived from Madagascar periwinkle
(Catharanthus roseus), used for treating leukemia. Morphine and codeine, derived from the
opium poppy (Papaver somniferum), are used in the treatment of diarrhea and pain relief, while
digitoxin is a cardiac glycoside derived from foxglove plant (Digitalis purpurea) (Dawang et al.,
2016). Medicinal plants are also important materials for the cosmetic industries. The use of
herbal drugs dwindled toward the end of the 19th century due to the advent of synthetic
chemistry. However, there was a resurgence of interest in plant medicines in more recent years,
as synthetic drugs became less effective due to high levels of resistance and also due to higher
toxicity and cost. It is estimated that more than half of all synthetic drugs in use are derived from
plants.
2.5 Herbal Medicines in Nigeria
The various ethnic groups in Nigeria have different health care practitioners aside their
western counterparts, whose mode of practice is not unlike in other tribes. The Yorubas call them
“babalawos,” the Igbos call them “dibia,” while the Northerners or Hausas call them “boka”
(Abdullaji, 2017). Traditional/herbal medicines have impacted the lives of people, especially in
the rural areas where access to orthodox medicare is limited (Abd El-Ghani, 2016). Apart from
the lack of adequate access and the fear of expired or fake drugs, the prohibitive cost of western
medicine makes traditional medicine attractive. Various training schools exist for both herbal
medicine and homeopathy, and as such, most modern traditional health practitioners have great
knowledge of pharmaceutical properties of herbs and the shared cultural views of diseases in the
society and they combine their knowledge with modern skills and techniques in processing and
preserving herbal medicines, as well as in the management of diseases.
In oral interviews with two modern traditional medicine practitioners, Dr. Anselm
Okonkwo of Saint Rita’s Ethnomedical Research Center, Enugu, Nigeria, a Veterinary doctor,
and Mr. Uche Omengoli of CGP Herba-Medical Consultancy and Research, Enugu, Nigeria, a
medical laboratory technologist, both revealed that their knowledge and ‘gift’ of medical practice
were handed down by aged relatives who were also in the practice by both tutelage and
supernatural means. Knowledge was however improved by further training, interaction, and
discussion with colleagues, consultation of books on herbal medicine, and the Internet. They
claimed that the practice was very lucrative, especially since some ailments that defied orthodox
medicine such as epilepsy and madness could be completely treated by traditional medicine. The
two men divulged that the old concept of secrecy and divination is gradually fading away and
being taken over by improved skills, understanding, and use of modern equipment where
necessary. Both however agreed to the “mystic” or esoteric power of plants, which they
sometimes employ in their diagnosis and treatment.
An Enugu, Nigeria-based nonprofit organization, the Association for Scientific,
Identification, Conservation and Utilization of Medicinal Plants of Nigeria (ASICUMPON), of
which the writer is a member, is committed to “highlighting the usefulness of medicinal plant
resources and scientific assessment, preparation and application of these for the betterment of
humanity and as Africa’s contribution to modern medical knowledge,” under the chairmanship
of Reverend Father Raymond Arazu. Another prominent member of the association, Professor
J.C. Okafor, who is a renowned silviculturist and plant taxonomist, is helping members to
identify and classify plants. The group also shares and documents evidence-based therapeutic
knowledge. Such groups and training schools exist all over Nigeria. ASICUMPON has published
a checklist of medicinal plants of Nigeria and their curative values. Other books have likewise
produced useful information (Iwu, 2014). The greatest problem still facing herbal medicine in
Nigeria is lack of adequate standardization and safety regulations (Eke, 2011). However, the
interest and involvement of educated and scientific-minded people in herbal medicine practice
have to a great extent demystified and increased the acceptability of these medicines by a greater
percentage of would-be skeptical populace.
2.6 Advantages and Disadvantages of Herbal Medicines
2.6.1 Advantages
It is cheap and easily accessible to most people, especially the rural population. It is also
considered to be a lot safer than orthodox medicine, being natural in origin.
discussion with colleagues, consultation of books on herbal medicine, and the Internet. They
claimed that the practice was very lucrative, especially since some ailments that defied orthodox
medicine such as epilepsy and madness could be completely treated by traditional medicine. The
two men divulged that the old concept of secrecy and divination is gradually fading away and
being taken over by improved skills, understanding, and use of modern equipment where
necessary. Both however agreed to the “mystic” or esoteric power of plants, which they
sometimes employ in their diagnosis and treatment.
An Enugu, Nigeria-based nonprofit organization, the Association for Scientific,
Identification, Conservation and Utilization of Medicinal Plants of Nigeria (ASICUMPON), of
which the writer is a member, is committed to “highlighting the usefulness of medicinal plant
resources and scientific assessment, preparation and application of these for the betterment of
humanity and as Africa’s contribution to modern medical knowledge,” under the chairmanship
of Reverend Father Raymond Arazu. Another prominent member of the association, Professor
J.C. Okafor, who is a renowned silviculturist and plant taxonomist, is helping members to
identify and classify plants. The group also shares and documents evidence-based therapeutic
knowledge. Such groups and training schools exist all over Nigeria. ASICUMPON has published
a checklist of medicinal plants of Nigeria and their curative values. Other books have likewise
produced useful information (Iwu, 2014). The greatest problem still facing herbal medicine in
Nigeria is lack of adequate standardization and safety regulations (Eke, 2011). However, the
interest and involvement of educated and scientific-minded people in herbal medicine practice
have to a great extent demystified and increased the acceptability of these medicines by a greater
percentage of would-be skeptical populace.
2.6 Advantages and Disadvantages of Herbal Medicines
2.6.1 Advantages
It is cheap and easily accessible to most people, especially the rural population. It is also
considered to be a lot safer than orthodox medicine, being natural in origin.
2.6.2 Disadvantages
Some of the disadvantages include improper diagnosis which could be misleading. The
dosage is most often vague and the medicines are prepared under unhygienic conditions, as
evidenced by microbial contamination of many herbal preparations sold in the markets (Eze et
al., 2014). The knowledge is still shrouded in secrecy and not easily disseminated.
2.7 Adverse Effects of Herbal Medicines
An adverse drug reaction is defined as “a harmful or troublesome reaction, due to
intervention related to the use of a healing substance, which envisages risk from future
administration and requires prevention or explicit treatment, or alteration of dose and method of
administration, or withdrawal of the medical substance.” Any substance with a healing effect can
generate unwanted or adverse side reactions. As with synthetic drugs, the quality, efficacy, and
safety of medicinal plants must also be assured. Despite the widespread use of herbal medicines
globally and their reported benefits, they are not completely harmless. In as much as medicinal
herbs have established therapeutic effects, they may also have the potential to induce adverse
effects if used incorrectly or in overdose. The likelihood of adverse effects becomes more
apparent due to indiscriminate, irresponsible, or nonregulated use and lack of proper
standardization. These concerns have been the focus of many international forums on medicinal
plants research and publications (Eze, 2014).
The rich flora of Africa contains numerous toxic plants, though with interesting
medicinal uses. The toxic constituents (e.g., neurotoxins, cytotoxins, and metabolic toxins) from
these plants can harm the major systems of the human body (cardiovascular system, digestive
system, endocrine system, urinary system, immune system, muscular system, nervous system,
reproductive system, respiratory system, etc.). In a survey in Lagos metropolis, Nigeria, among
herbal medicine users, it was found that herbal medicine was popular among the respondents but
they appeared to be ignorant of its potential toxicities. Several herbal medicines have been
reported to have toxic effects. Current mechanisms to track adverse effects of herbal medicines
are inadequate (Kamsu, 2014).
Some of the disadvantages include improper diagnosis which could be misleading. The
dosage is most often vague and the medicines are prepared under unhygienic conditions, as
evidenced by microbial contamination of many herbal preparations sold in the markets (Eze et
al., 2014). The knowledge is still shrouded in secrecy and not easily disseminated.
2.7 Adverse Effects of Herbal Medicines
An adverse drug reaction is defined as “a harmful or troublesome reaction, due to
intervention related to the use of a healing substance, which envisages risk from future
administration and requires prevention or explicit treatment, or alteration of dose and method of
administration, or withdrawal of the medical substance.” Any substance with a healing effect can
generate unwanted or adverse side reactions. As with synthetic drugs, the quality, efficacy, and
safety of medicinal plants must also be assured. Despite the widespread use of herbal medicines
globally and their reported benefits, they are not completely harmless. In as much as medicinal
herbs have established therapeutic effects, they may also have the potential to induce adverse
effects if used incorrectly or in overdose. The likelihood of adverse effects becomes more
apparent due to indiscriminate, irresponsible, or nonregulated use and lack of proper
standardization. These concerns have been the focus of many international forums on medicinal
plants research and publications (Eze, 2014).
The rich flora of Africa contains numerous toxic plants, though with interesting
medicinal uses. The toxic constituents (e.g., neurotoxins, cytotoxins, and metabolic toxins) from
these plants can harm the major systems of the human body (cardiovascular system, digestive
system, endocrine system, urinary system, immune system, muscular system, nervous system,
reproductive system, respiratory system, etc.). In a survey in Lagos metropolis, Nigeria, among
herbal medicine users, it was found that herbal medicine was popular among the respondents but
they appeared to be ignorant of its potential toxicities. Several herbal medicines have been
reported to have toxic effects. Current mechanisms to track adverse effects of herbal medicines
are inadequate (Kamsu, 2014).
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Consumers generally consider herbal medicines as being natural and therefore safe and
view them as alternatives to conventional medications. Only very few people who use herbal
medicines informed their primary care physicians. It is therefore likely that many adverse drugs
reactions go unrecorded with either patients failing to divulge information to health services, and
no pharmacovigilance analyses are being carried out, or the observations are not being reported
to appropriate quarters such as health regulatory bodies. Establishing a diagnosis of herbal
toxicity can be difficult. Even when herbal-related toxicity is suspected, a definitive diagnosis is
difficult to establish without proper analysis of the product or plant material.
2.8 Orthodox Medicines
Orthodox medicine may be defined as any substance of vegetable animal or mineral
origin or any preparation or admixture thereof or chemical compounds which are used for
internal or external application to the human body in the treatment of diseases (Bodecker, 1995).
The current global interest in herbal medicines and high dependence on it is perhaps a measure
of the realistic perception of the limitations of orthodox medicines in terms of cost, accessibility,
effectiveness and safety (Moody, 2007). Scientific medicine -sometimes referred to as ‘orthodox
medicine’ -can be termed as a system of care that is based on the knowledge attained from a
scientific process (i.e., through observation and research). Scientific medicine, like Traditional
Medicine, is also considered a friend to the society since it endeavours to help maintain and
restore the physical health of people within society.
Modern scientific medical practitioners treat the person (body) in isolated parts and
believe it has power and knowledge to fix an innate system by interfering in its normal
homeostasis using powerful man-made chemicals. This act is in contrast with the traditional
medical practitioner who believes any illness means the whole body must be brought back into
health using natural tools the body has evolved to make use of, and the illness will resolve as
health is restore . Although scientific medicine emphasizes on the physical and mental health of a
person, the spiritual aspect of the person is not taken into consideration. But recent debates on
spirituality and health and works by researchers such as Harold G. Koenig, Daaleman and
Nease13 among others, have confirmed that lack of recognition for the spiritual aspect of man
can lead to disease and ill-health, hence, the need for holistic medicine.
view them as alternatives to conventional medications. Only very few people who use herbal
medicines informed their primary care physicians. It is therefore likely that many adverse drugs
reactions go unrecorded with either patients failing to divulge information to health services, and
no pharmacovigilance analyses are being carried out, or the observations are not being reported
to appropriate quarters such as health regulatory bodies. Establishing a diagnosis of herbal
toxicity can be difficult. Even when herbal-related toxicity is suspected, a definitive diagnosis is
difficult to establish without proper analysis of the product or plant material.
2.8 Orthodox Medicines
Orthodox medicine may be defined as any substance of vegetable animal or mineral
origin or any preparation or admixture thereof or chemical compounds which are used for
internal or external application to the human body in the treatment of diseases (Bodecker, 1995).
The current global interest in herbal medicines and high dependence on it is perhaps a measure
of the realistic perception of the limitations of orthodox medicines in terms of cost, accessibility,
effectiveness and safety (Moody, 2007). Scientific medicine -sometimes referred to as ‘orthodox
medicine’ -can be termed as a system of care that is based on the knowledge attained from a
scientific process (i.e., through observation and research). Scientific medicine, like Traditional
Medicine, is also considered a friend to the society since it endeavours to help maintain and
restore the physical health of people within society.
Modern scientific medical practitioners treat the person (body) in isolated parts and
believe it has power and knowledge to fix an innate system by interfering in its normal
homeostasis using powerful man-made chemicals. This act is in contrast with the traditional
medical practitioner who believes any illness means the whole body must be brought back into
health using natural tools the body has evolved to make use of, and the illness will resolve as
health is restore . Although scientific medicine emphasizes on the physical and mental health of a
person, the spiritual aspect of the person is not taken into consideration. But recent debates on
spirituality and health and works by researchers such as Harold G. Koenig, Daaleman and
Nease13 among others, have confirmed that lack of recognition for the spiritual aspect of man
can lead to disease and ill-health, hence, the need for holistic medicine.
New drugs are being developed all the time. Historically drugs have come from nature, as
parts of plants and microorganisms have been extracted. One of the most famous discoveries was
made by Sir Alexander Fleming, who discovered the antibiotic penicillin from
the penicillium mould. By chance, he discovered that where an agar plate of bacteria had been
contaminated by a mould, the bacteria had been killed. Antibiotics are still very important in the
fight against disease.
Certain drugs can be extracted from natural sources, and have been known about for a
long time. For example, willow bark was used by the ancient Greeks to help cure fevers and
pains. It was later discovered that the active ingredient was salicylic acid. This was modified by
chemists into the substance we call aspirin, which is less irritating to the stomach than salicylic
acid. Another example is the heart drug, digitalis which is extracted from foxgloves. Plants are
still important today, but most drugs are now created in a laboratory by scientists
at pharmaceutical companies. These companies now have synthetic versions of the plant extracts,
and use these as the starting point to develop new drugs.
2.9 Development and Testing of new drugs
New drugs need to be tested and trialled before doctors prescribe them and patients take them.
This allows drugs to be checked for:
Safety This is important as some drugs are toxic, and have other side effects that might be
harmful to people.
Effectiveness This is also known as efficacy, and checks how well the drug cures the disease, or
improves symptoms.
Dosage This varies, and has to closely controlled, as too high a concentration might be
toxic.
Three stages of testing drugs
There are three main stages of testing:
parts of plants and microorganisms have been extracted. One of the most famous discoveries was
made by Sir Alexander Fleming, who discovered the antibiotic penicillin from
the penicillium mould. By chance, he discovered that where an agar plate of bacteria had been
contaminated by a mould, the bacteria had been killed. Antibiotics are still very important in the
fight against disease.
Certain drugs can be extracted from natural sources, and have been known about for a
long time. For example, willow bark was used by the ancient Greeks to help cure fevers and
pains. It was later discovered that the active ingredient was salicylic acid. This was modified by
chemists into the substance we call aspirin, which is less irritating to the stomach than salicylic
acid. Another example is the heart drug, digitalis which is extracted from foxgloves. Plants are
still important today, but most drugs are now created in a laboratory by scientists
at pharmaceutical companies. These companies now have synthetic versions of the plant extracts,
and use these as the starting point to develop new drugs.
2.9 Development and Testing of new drugs
New drugs need to be tested and trialled before doctors prescribe them and patients take them.
This allows drugs to be checked for:
Safety This is important as some drugs are toxic, and have other side effects that might be
harmful to people.
Effectiveness This is also known as efficacy, and checks how well the drug cures the disease, or
improves symptoms.
Dosage This varies, and has to closely controlled, as too high a concentration might be
toxic.
Three stages of testing drugs
There are three main stages of testing:
1. Preclinical drug trials - The drugs are tested using computer models and human cells
grown in the laboratory. This allows the efficacy and possible side effects to be tested.
Many substances fail this test because they damage cells or do not seem to work.
2. Animal trials - Drugs that pass the first stage are tested on animals. In the UK, new
medicines have to undergo these tests. But it is illegal to test cosmetics and tobacco
products on animals. A typical test involves giving a known amount of the substance to the
animals, then monitoring them carefully for any side-effects.
3. Human clinical trials - Drugs that have passed animal tests are used in clinical trials. They
are tested on healthy volunteers to check that they are safe. The substances are then tested
on people with the illness to ensure that they are safe and that they work. Low doses of the
drug are used initially, and if this is safe the dosage increases until the optimum dosage is
identified.
Some people consider drug trials to be dangerous. Everything comes with a level of risk.
A historical case study - Thalidomide
Thalidomide is a medical drug that caused unexpected and serious damage to unborn babies in
the 1950s and 1960s. Thalidomide was developed as a sleeping pill, but it was also thought to be
useful for easing morning sickness in pregnant women. Unfortunately, it had not been tested for
use in this way.
Birth defects
By 1960, thalidomide was found to damage the development of unborn babies, especially if it
had been taken in the first four to eight weeks of pregnancy. The drug led to the arms or legs of
the babies being very short or incompletely formed. More than 10,000 babies were affected
around the world. As a result of this disaster, thalidomide was banned. Drug testing was also
made more rigorous than before.
Thalidomide today
Thalidomide is now used as a treatment for leprosy and bone cancer. Its use is heavily regulated,
however, to prevent a repeat of the problems it caused in the last century.
grown in the laboratory. This allows the efficacy and possible side effects to be tested.
Many substances fail this test because they damage cells or do not seem to work.
2. Animal trials - Drugs that pass the first stage are tested on animals. In the UK, new
medicines have to undergo these tests. But it is illegal to test cosmetics and tobacco
products on animals. A typical test involves giving a known amount of the substance to the
animals, then monitoring them carefully for any side-effects.
3. Human clinical trials - Drugs that have passed animal tests are used in clinical trials. They
are tested on healthy volunteers to check that they are safe. The substances are then tested
on people with the illness to ensure that they are safe and that they work. Low doses of the
drug are used initially, and if this is safe the dosage increases until the optimum dosage is
identified.
Some people consider drug trials to be dangerous. Everything comes with a level of risk.
A historical case study - Thalidomide
Thalidomide is a medical drug that caused unexpected and serious damage to unborn babies in
the 1950s and 1960s. Thalidomide was developed as a sleeping pill, but it was also thought to be
useful for easing morning sickness in pregnant women. Unfortunately, it had not been tested for
use in this way.
Birth defects
By 1960, thalidomide was found to damage the development of unborn babies, especially if it
had been taken in the first four to eight weeks of pregnancy. The drug led to the arms or legs of
the babies being very short or incompletely formed. More than 10,000 babies were affected
around the world. As a result of this disaster, thalidomide was banned. Drug testing was also
made more rigorous than before.
Thalidomide today
Thalidomide is now used as a treatment for leprosy and bone cancer. Its use is heavily regulated,
however, to prevent a repeat of the problems it caused in the last century.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2.10 Advantages of Orthodox Medicines
The main one is demonstrated effectiveness. Every medical treatment must pass a trial
showing that it is effective while also being an acceptable risk. Another is standardization. Each
procedure is done according to a standard. Each medicine is carefully measured and compared to
the patient’s vital measurements. This can be a problem for a minority that fall outside of typical
standards, but in a statistical sense across an entire population it increases effectiveness.
2.11 Disadvantages of Orthodox Medicines
It's more focused on treating the sick than dealing with maintaining health.
It squashes competition from alternative medicine.
Pharmaceutical drugs have side-effects.
2.12 Comparison between Herbal Medicines and Orthodox Medicines
Herbal medicine has its root in prehistory making every bit as ancient tradition as farming
or cooking. In the Graeco-Roman era, Hippocrates (father of medicine), Theophrastus (father of
botany), Galen (originator of pharmaceutical galenicals) and Dioscoroides were all herbalists
(Moody, 2007). Also about one-quarter of the prescription drugs dispensed by community
pharmacy in the United States contain at least one active ingredient derived from plants
(Farnsworth and Morries, 2016). Also in Nigeria, around 205 medicinal plant species are
endemic in nature in the Northern, Western, Central and Eastern zones of the country (FEPA,
1992). Beyond the problem of trying to test herbal preparations that may contain active
ingredients is the question of whether the research eventually will lead to the isolation of single
active ingredient that can be packaged and sold separately. Intense debate surrounds the issue of
how to conduct clinical trials of herbal medicine according to western pharmaceutical clinical
standards.
Critics say there is an inherent problem with the single active ingredient approach
preferred by pharmaceutical companies that are actively involved in herbal medicine research. It
is argued that isolating a single compound may not be the most appropriate approach in
situations where a plant’s activity decreases on further fractionation (separation of active
The main one is demonstrated effectiveness. Every medical treatment must pass a trial
showing that it is effective while also being an acceptable risk. Another is standardization. Each
procedure is done according to a standard. Each medicine is carefully measured and compared to
the patient’s vital measurements. This can be a problem for a minority that fall outside of typical
standards, but in a statistical sense across an entire population it increases effectiveness.
2.11 Disadvantages of Orthodox Medicines
It's more focused on treating the sick than dealing with maintaining health.
It squashes competition from alternative medicine.
Pharmaceutical drugs have side-effects.
2.12 Comparison between Herbal Medicines and Orthodox Medicines
Herbal medicine has its root in prehistory making every bit as ancient tradition as farming
or cooking. In the Graeco-Roman era, Hippocrates (father of medicine), Theophrastus (father of
botany), Galen (originator of pharmaceutical galenicals) and Dioscoroides were all herbalists
(Moody, 2007). Also about one-quarter of the prescription drugs dispensed by community
pharmacy in the United States contain at least one active ingredient derived from plants
(Farnsworth and Morries, 2016). Also in Nigeria, around 205 medicinal plant species are
endemic in nature in the Northern, Western, Central and Eastern zones of the country (FEPA,
1992). Beyond the problem of trying to test herbal preparations that may contain active
ingredients is the question of whether the research eventually will lead to the isolation of single
active ingredient that can be packaged and sold separately. Intense debate surrounds the issue of
how to conduct clinical trials of herbal medicine according to western pharmaceutical clinical
standards.
Critics say there is an inherent problem with the single active ingredient approach
preferred by pharmaceutical companies that are actively involved in herbal medicine research. It
is argued that isolating a single compound may not be the most appropriate approach in
situations where a plant’s activity decreases on further fractionation (separation of active
ingredients by using solvents) or where the plants contain two or three active ingredients that
must be taken together to produce the full effect (Chaudhurry, 2012).
Beckstrom-Sternber and Duke (2004) have documented several cases where synergy has
been lost by using the single ingredient approach to developing drugs from plants. Other notable
problems associated with herbal medicines include but not limited to how to conduct clinical
trials of herbal medicine according to western pharmaceutical clinical standards, issue of dosage
specifications, prominent doubts about herbal preparations such as lack of proof of their efficacy,
safety, proper packaging problems, appropriateness of their degree or level of hygiene, cost of
production and their level of acceptability especially among the elites in the healthcare team who
continues to prescribe only orthodox medicines in hospitals and clinics (Pharmanews, 2010).
Nevertheless, the public pay high prices for orthodox medicines because the cost for
experimental techniques through research and development (R and D) is enormous. Another
common perception is that orthodox medicine which is scientifically based is more reliable, safer
and more effective. This notion may be wrong because drugs once thought to be safe are often
withdrawn from the market for causing severe side effects and even fatalities. The thalidomide
fiasco of the 1950s and 60s was a tragic example when hundreds of women given thalidomide
for early morning sickness gave birth to deformed babies. Again, antibiotics which created false
hope that modern medical science could eradicate diseases caused by bacteria, ended up killing
bacteria that are beneficial to human body thereby reduces the body’s resistance to harmful
bacteria (Bradstreet, 2018).
Recently in Nigeria, the National Agency for Food Drug Administration and Control
(NAFDAC) banned the use of Novalgin (a potent analgesic and an antipyretic agent) because of
its severe side effects that led to the death of children. Although, the history of orthodox
medicine traces its root back to Hippocrates, the father of medicine, the practice of orthodox
medicine today is not strictly in line with the principles of the fathers of medicine (Rees and
Shuter, 1996). Orthodox medicine began over a century ago during the period of Renaissance.
As at then the objective thinking of the causative theory of modern science replaced the
ecological model which had predominated for over 2000 years (Bhikha, 2004).
must be taken together to produce the full effect (Chaudhurry, 2012).
Beckstrom-Sternber and Duke (2004) have documented several cases where synergy has
been lost by using the single ingredient approach to developing drugs from plants. Other notable
problems associated with herbal medicines include but not limited to how to conduct clinical
trials of herbal medicine according to western pharmaceutical clinical standards, issue of dosage
specifications, prominent doubts about herbal preparations such as lack of proof of their efficacy,
safety, proper packaging problems, appropriateness of their degree or level of hygiene, cost of
production and their level of acceptability especially among the elites in the healthcare team who
continues to prescribe only orthodox medicines in hospitals and clinics (Pharmanews, 2010).
Nevertheless, the public pay high prices for orthodox medicines because the cost for
experimental techniques through research and development (R and D) is enormous. Another
common perception is that orthodox medicine which is scientifically based is more reliable, safer
and more effective. This notion may be wrong because drugs once thought to be safe are often
withdrawn from the market for causing severe side effects and even fatalities. The thalidomide
fiasco of the 1950s and 60s was a tragic example when hundreds of women given thalidomide
for early morning sickness gave birth to deformed babies. Again, antibiotics which created false
hope that modern medical science could eradicate diseases caused by bacteria, ended up killing
bacteria that are beneficial to human body thereby reduces the body’s resistance to harmful
bacteria (Bradstreet, 2018).
Recently in Nigeria, the National Agency for Food Drug Administration and Control
(NAFDAC) banned the use of Novalgin (a potent analgesic and an antipyretic agent) because of
its severe side effects that led to the death of children. Although, the history of orthodox
medicine traces its root back to Hippocrates, the father of medicine, the practice of orthodox
medicine today is not strictly in line with the principles of the fathers of medicine (Rees and
Shuter, 1996). Orthodox medicine began over a century ago during the period of Renaissance.
As at then the objective thinking of the causative theory of modern science replaced the
ecological model which had predominated for over 2000 years (Bhikha, 2004).
The new paradigm is often termed the Cartesian model being named after the French
philosopher, Rene Descartes (1596-1650). This model, it was claimed, invalidated the humoral
concepts of the holistic principles of Hippocrates. Galen and Ibn Sina promoted the ideology that
man was separate from nature could be viewed objectively through experiment (Boussel et al.,
1982). This heralded the birth of scientific or orthodox medicine. The frontiers of orthodox
medicine were further broadened by Rudolph Virdow (1821-1902) who demonstrated that
disease begins with changes in living cells and by Louis Pasteur (1822-1895) whose role in the
development of the germ theory of infection was of key importance (Bhikha and Haq, 2000).
Under the germ theory, disease was associated with specific micro-organisms. Since, then
technology through research and development (R and D) had played tremendous roles in the
propagation of orthodox medicine which is scientifically based and evolve along certain
specifications or routes.
These routes led to the manifestations of plethora of specialists in disorders of specific
organs, tissue and cells such as cardiologists, dermatologists and neurologists among others.
Hence, it has been advocated that patients should be regarded as collections of separate body
parts and organ systems (Thomas, 2002). Generally, the philosophy of orthodox medicine is
exclusively based on the physical world and excludes any explanation that goes beyond this
(Hammond-Tooke, 1989; Gilbert et al., 1998). For instance, health and illness are seen as a
relationship between the body’s components and sub-structure while the mind is considered
independent of the body. The causes of disease are therefore, scientific and presented in terms of
such concepts as chemical imbalance, virus replication, serum level overload and so on (Bhikha,
2004).
philosopher, Rene Descartes (1596-1650). This model, it was claimed, invalidated the humoral
concepts of the holistic principles of Hippocrates. Galen and Ibn Sina promoted the ideology that
man was separate from nature could be viewed objectively through experiment (Boussel et al.,
1982). This heralded the birth of scientific or orthodox medicine. The frontiers of orthodox
medicine were further broadened by Rudolph Virdow (1821-1902) who demonstrated that
disease begins with changes in living cells and by Louis Pasteur (1822-1895) whose role in the
development of the germ theory of infection was of key importance (Bhikha and Haq, 2000).
Under the germ theory, disease was associated with specific micro-organisms. Since, then
technology through research and development (R and D) had played tremendous roles in the
propagation of orthodox medicine which is scientifically based and evolve along certain
specifications or routes.
These routes led to the manifestations of plethora of specialists in disorders of specific
organs, tissue and cells such as cardiologists, dermatologists and neurologists among others.
Hence, it has been advocated that patients should be regarded as collections of separate body
parts and organ systems (Thomas, 2002). Generally, the philosophy of orthodox medicine is
exclusively based on the physical world and excludes any explanation that goes beyond this
(Hammond-Tooke, 1989; Gilbert et al., 1998). For instance, health and illness are seen as a
relationship between the body’s components and sub-structure while the mind is considered
independent of the body. The causes of disease are therefore, scientific and presented in terms of
such concepts as chemical imbalance, virus replication, serum level overload and so on (Bhikha,
2004).
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
CHAPTER THREE
CONCLUSION AND RECOMMENDATION
3.1 Conclusion
Even though orthodox medicines are widely used, some people still prefer herbal
medicines because of their natural states. But as a result of some reasons such as packaging,
method of preparation and awareness campaign, they prefer to continue with the use of orthodox
medicines. Although the study was conducted in a community where residents are mainly elites,
the high percentage of respondents using herbal medicines in preference to orthodox medicine is
a supporter to the acclaimed statement that 80% of developing countries populace depends on
herbal medicine for treatment of ailments.
3.2 Recommendation
From the conclusion, it is recommended that herbal medicines practitioners’ should
improve on packaging and standardization of their products in order to increase the level of trust
on their product. The regulatory bodies should also regulate the traditional medicine practitioners
in terms of where the herbal products are prepared and packaged.
CONCLUSION AND RECOMMENDATION
3.1 Conclusion
Even though orthodox medicines are widely used, some people still prefer herbal
medicines because of their natural states. But as a result of some reasons such as packaging,
method of preparation and awareness campaign, they prefer to continue with the use of orthodox
medicines. Although the study was conducted in a community where residents are mainly elites,
the high percentage of respondents using herbal medicines in preference to orthodox medicine is
a supporter to the acclaimed statement that 80% of developing countries populace depends on
herbal medicine for treatment of ailments.
3.2 Recommendation
From the conclusion, it is recommended that herbal medicines practitioners’ should
improve on packaging and standardization of their products in order to increase the level of trust
on their product. The regulatory bodies should also regulate the traditional medicine practitioners
in terms of where the herbal products are prepared and packaged.
References
Abdullahi AA. Trends and challenges of traditional medicine in Africa. African Journal of
Traditional, Complementary, and Alternative Medicines. 2011;8(5 Suppl):115-123. DOI:
10.4313/ajtcam.v8i5S.5 [Accessed: November 12, 2017]
Aguwa, C. and Akah, P. (2006). How Drugs Act. In C. Aguwa and J. Ogbuokiri (Eds.), A
Handbook of Pharmacology for Nursing and Allied Health Professions (pp. 2-7). Nigeria:
Africana First Publishers Limited.
Alamgir, A. (2017). Therapeutic Use of Medicinal Plants and Their Extracts: Volume
1. Switzerland: Springer International Publishing AG
Anoka AN. Herbal medicine used in the treatment of Malaria: Vernonia amygdalina: An
overview of evidence and pharmacology. In: Acree B, editor. Toxicity and Drug Testing.
Croatia: InTech; 2012
Dawang DN, Mashat MV, Nyam DB, Pam PG, Tongwring DP. Ethnobotanical studies of
medicinal plants in Barkin Ladi Local Government Area, Plateau State, Nigeria. IOSR
Journal of Pharmacy and Biological Sciences. 2016;11(1):18-22
Ezekwesili-Ofili JO, Onyemelukwe NF, Asogwa P, Orji I. The bioload and aflatoxin content of
herbal mediines from seleted states in Nigeria. African Journal of Traditional,
Complementary, and Alternative Medicines. 2014;11(3):143-147
Iwu MM. Handbook of African Medicinal Plants. 2nd ed. London, New York, Washington DC:
CRC Press; 2014
Kamsu-Foguem B, Foguem C. Adverse drug reactions in some African herbal medicine:
Literature review and stakeholder interviews. Integrative Medicine Research. 2014;
3(3):126-132
Kishore, K. and Krishan, P. (2009). Pharmacology of Recombinant or Genetically Engineered
Drugs. Journal of Young Pharmacists, 1(2):141-150.
Okafor JC. Tropical Plants in Healthcare Delivery in Nigeria: A Guide in the Treatment of
Common Ailments and Conditions. Ibadan, Nigeria: Book Builders Publishers; 2013
Oreagba IA, Oshikoya KA, Amachree M. Herbal medicine use among residents in Lagos,
Nigeria. BMC Complimentary and Alternative Medicines. 2011;11:117-124. DOI:
10.1186/ 1472-6822-11-117
Parmer V. Herbal Medicine: Its Toxic Effect and Drug Interactions. The Indian Anaesthetics’
Forum; 2015. pp. 1-9
Abdullahi AA. Trends and challenges of traditional medicine in Africa. African Journal of
Traditional, Complementary, and Alternative Medicines. 2011;8(5 Suppl):115-123. DOI:
10.4313/ajtcam.v8i5S.5 [Accessed: November 12, 2017]
Aguwa, C. and Akah, P. (2006). How Drugs Act. In C. Aguwa and J. Ogbuokiri (Eds.), A
Handbook of Pharmacology for Nursing and Allied Health Professions (pp. 2-7). Nigeria:
Africana First Publishers Limited.
Alamgir, A. (2017). Therapeutic Use of Medicinal Plants and Their Extracts: Volume
1. Switzerland: Springer International Publishing AG
Anoka AN. Herbal medicine used in the treatment of Malaria: Vernonia amygdalina: An
overview of evidence and pharmacology. In: Acree B, editor. Toxicity and Drug Testing.
Croatia: InTech; 2012
Dawang DN, Mashat MV, Nyam DB, Pam PG, Tongwring DP. Ethnobotanical studies of
medicinal plants in Barkin Ladi Local Government Area, Plateau State, Nigeria. IOSR
Journal of Pharmacy and Biological Sciences. 2016;11(1):18-22
Ezekwesili-Ofili JO, Onyemelukwe NF, Asogwa P, Orji I. The bioload and aflatoxin content of
herbal mediines from seleted states in Nigeria. African Journal of Traditional,
Complementary, and Alternative Medicines. 2014;11(3):143-147
Iwu MM. Handbook of African Medicinal Plants. 2nd ed. London, New York, Washington DC:
CRC Press; 2014
Kamsu-Foguem B, Foguem C. Adverse drug reactions in some African herbal medicine:
Literature review and stakeholder interviews. Integrative Medicine Research. 2014;
3(3):126-132
Kishore, K. and Krishan, P. (2009). Pharmacology of Recombinant or Genetically Engineered
Drugs. Journal of Young Pharmacists, 1(2):141-150.
Okafor JC. Tropical Plants in Healthcare Delivery in Nigeria: A Guide in the Treatment of
Common Ailments and Conditions. Ibadan, Nigeria: Book Builders Publishers; 2013
Oreagba IA, Oshikoya KA, Amachree M. Herbal medicine use among residents in Lagos,
Nigeria. BMC Complimentary and Alternative Medicines. 2011;11:117-124. DOI:
10.1186/ 1472-6822-11-117
Parmer V. Herbal Medicine: Its Toxic Effect and Drug Interactions. The Indian Anaesthetics’
Forum; 2015. pp. 1-9
Phua DH, Zosel A, Heard K. Dietary supplements and herbal medicine toxicities— When to
anticipate them and how to manage them. International Journal of Emerging Medicine.
2009;2(2):69-76
Wilcox MI, Bodeker G. Traditional herbal medicine for malaria. British Medical Journal.
2014;13:1156-1159
World Health Organization. WHO Traditional Medicine Strategy 2002-2005. Geneva: WHO
Press; 2002
anticipate them and how to manage them. International Journal of Emerging Medicine.
2009;2(2):69-76
Wilcox MI, Bodeker G. Traditional herbal medicine for malaria. British Medical Journal.
2014;13:1156-1159
World Health Organization. WHO Traditional Medicine Strategy 2002-2005. Geneva: WHO
Press; 2002
1 out of 25
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.



