Implement and Monitor Care for a Person with Mental Health Conditions
VerifiedAdded on 2023/01/04
|14
|3767
|33
AI Summary
This document provides information on how to implement and monitor care for a person with mental health conditions. It covers the definition of mental health, objectives of mental health legislation, treatment options, management strategies, and common mental health conditions. The document also includes a case study and recommendations for providing care to individuals with mental health conditions.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
HLTENN009 - Implement
and monitor care for a person
with mental health conditions
and monitor care for a person
with mental health conditions
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Contents
PART A...........................................................................................................................................3
1...................................................................................................................................................3
2...................................................................................................................................................3
3...................................................................................................................................................3
4...................................................................................................................................................4
5...................................................................................................................................................4
6...................................................................................................................................................4
7...................................................................................................................................................4
8...................................................................................................................................................4
9...................................................................................................................................................4
10.................................................................................................................................................4
11.................................................................................................................................................5
12.................................................................................................................................................5
13.................................................................................................................................................5
14.................................................................................................................................................1
15.................................................................................................................................................1
16.................................................................................................................................................2
17.................................................................................................................................................2
PART B...........................................................................................................................................2
Case study 1.................................................................................................................................2
Case study 2.................................................................................................................................3
Case Study 3................................................................................................................................4
REFERENCES................................................................................................................................6
PART A...........................................................................................................................................3
1...................................................................................................................................................3
2...................................................................................................................................................3
3...................................................................................................................................................3
4...................................................................................................................................................4
5...................................................................................................................................................4
6...................................................................................................................................................4
7...................................................................................................................................................4
8...................................................................................................................................................4
9...................................................................................................................................................4
10.................................................................................................................................................4
11.................................................................................................................................................5
12.................................................................................................................................................5
13.................................................................................................................................................5
14.................................................................................................................................................1
15.................................................................................................................................................1
16.................................................................................................................................................2
17.................................................................................................................................................2
PART B...........................................................................................................................................2
Case study 1.................................................................................................................................2
Case study 2.................................................................................................................................3
Case Study 3................................................................................................................................4
REFERENCES................................................................................................................................6
PART A
1.
A) Mental health means condition of a person according to their psychological health and emotional well-
being.
B) Mental illness is basically where severe disorder is being caused to person’s thinking ability.
C)Delusion is a false belief which forces an individual to see things which are not actually happening.
D)Phobia: It is an extreme fear of doing something (Bronson and Berzofsky, 2017).
2.
Objectives: Mental health legislation of Australia has the objective to provide better treatment to people
suffering from acute psychotic illness.
Involuntary admission: Involuntary admission to mental health illness and treatment under the Australian
Acts now require, at a minimum the person must be suffering from any type of mental illness.
Consumer right: Receive high quality treatment, receiving appropriate treatment, giving timely treatment,
entitled to privacy of data, equal and fair access to care
Involuntary review process: In this the mentally retarded person is been detained legally and the questioning
can be done up to period of 3 months (Oddy and et.al., 2018).
Seclusion: It is being done of the mentally ill patient to prevent harm for other people and patient.
Admission procedure: Under mental health act a person can only be admitted when the authorised person is
satisfied that these people are likely to benefit from the care.
Community treatment: CTO is basically giving assistance to people suffering from mental health disorder
with the help of tribunal.
Role of mental health practitioner: Role is to provide high quality of treatment to patients in order to
enhance their well-being.
Consent: Before admitting any patient to mental health ward consent of the family member and patient needs
to be taken.
Confidentiality: Data of the patient needs to be kept confidential by following the ethical code of conduct.
3.
Recovery is self-directed: It means that patient can only heal from mental illness if they are willing to.
Recovery empowers: support must be provided to empower that individual make their own choices and
makes their own decision.
Recovery includes support from others: Nurses, family members must be engaged in giving support to
patient so there wellbeing improves.
1.
A) Mental health means condition of a person according to their psychological health and emotional well-
being.
B) Mental illness is basically where severe disorder is being caused to person’s thinking ability.
C)Delusion is a false belief which forces an individual to see things which are not actually happening.
D)Phobia: It is an extreme fear of doing something (Bronson and Berzofsky, 2017).
2.
Objectives: Mental health legislation of Australia has the objective to provide better treatment to people
suffering from acute psychotic illness.
Involuntary admission: Involuntary admission to mental health illness and treatment under the Australian
Acts now require, at a minimum the person must be suffering from any type of mental illness.
Consumer right: Receive high quality treatment, receiving appropriate treatment, giving timely treatment,
entitled to privacy of data, equal and fair access to care
Involuntary review process: In this the mentally retarded person is been detained legally and the questioning
can be done up to period of 3 months (Oddy and et.al., 2018).
Seclusion: It is being done of the mentally ill patient to prevent harm for other people and patient.
Admission procedure: Under mental health act a person can only be admitted when the authorised person is
satisfied that these people are likely to benefit from the care.
Community treatment: CTO is basically giving assistance to people suffering from mental health disorder
with the help of tribunal.
Role of mental health practitioner: Role is to provide high quality of treatment to patients in order to
enhance their well-being.
Consent: Before admitting any patient to mental health ward consent of the family member and patient needs
to be taken.
Confidentiality: Data of the patient needs to be kept confidential by following the ethical code of conduct.
3.
Recovery is self-directed: It means that patient can only heal from mental illness if they are willing to.
Recovery empowers: support must be provided to empower that individual make their own choices and
makes their own decision.
Recovery includes support from others: Nurses, family members must be engaged in giving support to
patient so there wellbeing improves.
4.
Uniqueness of the individual: It means that outcome of recovery is unique for an individual and they need to
provide with better decision making choices related to their health
Real choices Attitudes and rights: Attitude of health care professional must be positive towards patient.
Dignity and respect: Respect needs to be given to patients while providing them treatment (Pacheco and et.al.,
2017).
Partnership and communication: Health care professionals needs to make use of effective communication to
know about thoughts and feelings of patients
Evaluating recovery: Recovery must be evaluated on time to time basis.
5.
Evidence based practice is useful for treating mental health patients. In this best possible care is given to
patients by making use of holistic approach. They also include multi-disciplinary team in it.
6.
The National recovery-oriented mental health practice framework is a policy which is being implemented to
enhance the health outcome of mentally retarded patients. The main purpose is to align various hospital care
settings, government to enhance health outcome of patients (Wang and et.al., 2020).
7.
Barker's Tidal Model of Mental Health Recovery is a nursing theory that can be used to reduce mental distress
of patients. In this patient can make use of their own voice to recover the moments of their mental distress. By
this nurses can be able to know about patient’s thoughts and feelings.
8.
Social factors: Culture, background, belief
Psychological factor: Child neglect, growing up with families having domestic violence, psychological abuse
Physical factor: sexual abuse, physical health inequalities, physical abuse
Cognitive factor: Cognitive impairment, recalling memory, brain cells damage
9.
It has been analysed that social stigma and discrimination when faced by any individual can make mental
health condition worse. Various effects can be faced by an individual because of the social stigma. They can
lose confidence and also reluctant to get any type of treatment in future.
10
By developing better health promotion programme for patients with mental health issues.
Making sure that fair health services are being provided to patients with psychiatric disorders and oral
issues
Providing them equal and fair treatment to patients
Uniqueness of the individual: It means that outcome of recovery is unique for an individual and they need to
provide with better decision making choices related to their health
Real choices Attitudes and rights: Attitude of health care professional must be positive towards patient.
Dignity and respect: Respect needs to be given to patients while providing them treatment (Pacheco and et.al.,
2017).
Partnership and communication: Health care professionals needs to make use of effective communication to
know about thoughts and feelings of patients
Evaluating recovery: Recovery must be evaluated on time to time basis.
5.
Evidence based practice is useful for treating mental health patients. In this best possible care is given to
patients by making use of holistic approach. They also include multi-disciplinary team in it.
6.
The National recovery-oriented mental health practice framework is a policy which is being implemented to
enhance the health outcome of mentally retarded patients. The main purpose is to align various hospital care
settings, government to enhance health outcome of patients (Wang and et.al., 2020).
7.
Barker's Tidal Model of Mental Health Recovery is a nursing theory that can be used to reduce mental distress
of patients. In this patient can make use of their own voice to recover the moments of their mental distress. By
this nurses can be able to know about patient’s thoughts and feelings.
8.
Social factors: Culture, background, belief
Psychological factor: Child neglect, growing up with families having domestic violence, psychological abuse
Physical factor: sexual abuse, physical health inequalities, physical abuse
Cognitive factor: Cognitive impairment, recalling memory, brain cells damage
9.
It has been analysed that social stigma and discrimination when faced by any individual can make mental
health condition worse. Various effects can be faced by an individual because of the social stigma. They can
lose confidence and also reluctant to get any type of treatment in future.
10
By developing better health promotion programme for patients with mental health issues.
Making sure that fair health services are being provided to patients with psychiatric disorders and oral
issues
Providing them equal and fair treatment to patients
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
11.
Side effects of medication: Some medication can cause oral health issues which can be possibly the result of
their side effects. This can reduce the health outcome of patients with mental health problem (Gao and et.al.,
2020).
Poor nutrition: Poor diets can result into worsening disorders, in this the person can become depressed and
also anxious when not consuming the better diet.
Reduced motivation for self-care: If the mental health patients are not willing to take care of their own than
their health outcome can be lowered down. In this patient must be motivated to take care of themselves as this
will positively impact their health outcome and also because of this there well being will be improved.
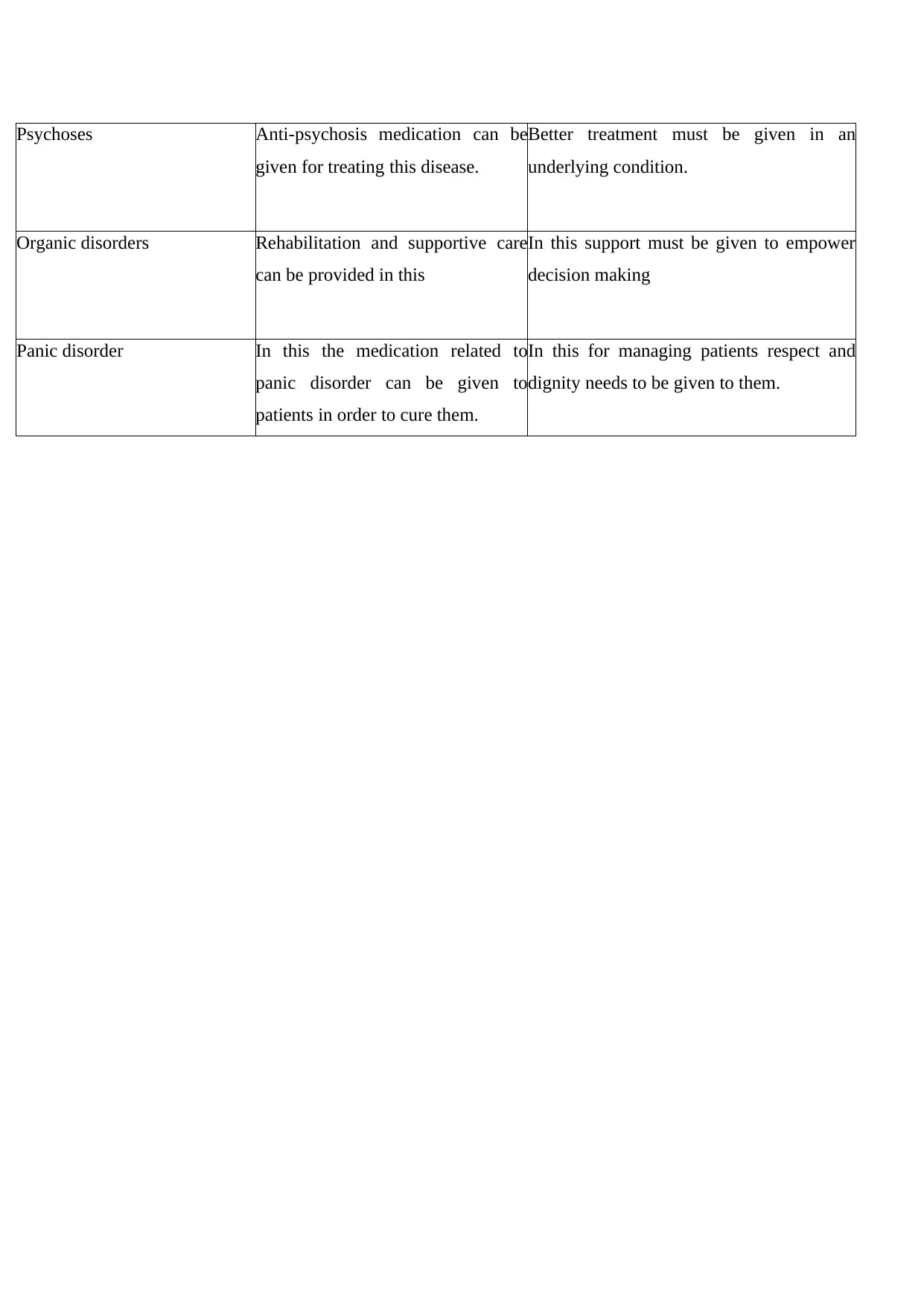
12.
Diagnostic and Statistical Manual of Mental
Disorders (DSM – 5)
International Classification of Diseases
(ICD - 10)
It is the standard classification of mental
disorder which has been used by the American
psychological association. There are various
classifications given in this manual of mental
health like anxiety disorder, bipolar disorder
and many other. In this the treatment
procedures given to mentally ill patients are
also being given.
International Classification of Diseases
(ICD - 10) is been used to design and promote
and reduced down the mortality statistics of the
people who are been dying because of mental
health disorders. In this the methods are been
defined for the injury, disease and causes of
death (Kisely and et.al., 2018).
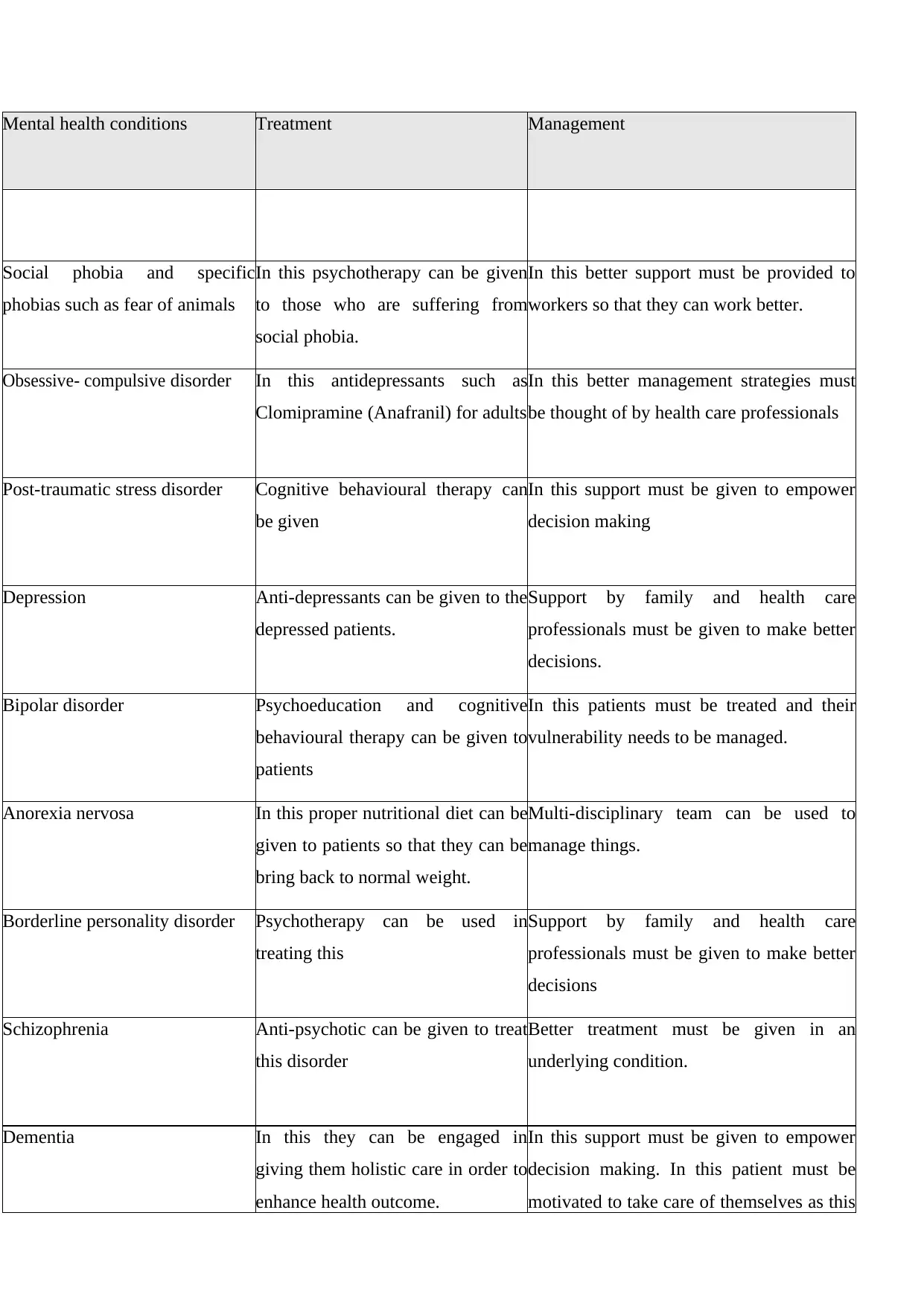
13.
Common mental health
conditions
Treatment Management
Personality disorders In this health care professionals can
be engaged in giving them
psychiatric medications and also the
mood depressants
In this health care professional needs to
manage them patiently.
Anxiety disorders This can be treated by giving
patients with better therapies like
CBT.
Management of these patients needs to be
done carefully and also in risk free
environment.
Side effects of medication: Some medication can cause oral health issues which can be possibly the result of
their side effects. This can reduce the health outcome of patients with mental health problem (Gao and et.al.,
2020).
Poor nutrition: Poor diets can result into worsening disorders, in this the person can become depressed and
also anxious when not consuming the better diet.
Reduced motivation for self-care: If the mental health patients are not willing to take care of their own than
their health outcome can be lowered down. In this patient must be motivated to take care of themselves as this
will positively impact their health outcome and also because of this there well being will be improved.
12.
Diagnostic and Statistical Manual of Mental
Disorders (DSM – 5)
International Classification of Diseases
(ICD - 10)
It is the standard classification of mental
disorder which has been used by the American
psychological association. There are various
classifications given in this manual of mental
health like anxiety disorder, bipolar disorder
and many other. In this the treatment
procedures given to mentally ill patients are
also being given.
International Classification of Diseases
(ICD - 10) is been used to design and promote
and reduced down the mortality statistics of the
people who are been dying because of mental
health disorders. In this the methods are been
defined for the injury, disease and causes of
death (Kisely and et.al., 2018).
13.
Common mental health
conditions
Treatment Management
Personality disorders In this health care professionals can
be engaged in giving them
psychiatric medications and also the
mood depressants
In this health care professional needs to
manage them patiently.
Anxiety disorders This can be treated by giving
patients with better therapies like
CBT.
Management of these patients needs to be
done carefully and also in risk free
environment.
Psychoses Anti-psychosis medication can be
given for treating this disease.
Better treatment must be given in an
underlying condition.
Organic disorders Rehabilitation and supportive care
can be provided in this
In this support must be given to empower
decision making
Panic disorder In this the medication related to
panic disorder can be given to
patients in order to cure them.
In this for managing patients respect and
dignity needs to be given to them.
given for treating this disease.
Better treatment must be given in an
underlying condition.
Organic disorders Rehabilitation and supportive care
can be provided in this
In this support must be given to empower
decision making
Panic disorder In this the medication related to
panic disorder can be given to
patients in order to cure them.
In this for managing patients respect and
dignity needs to be given to them.
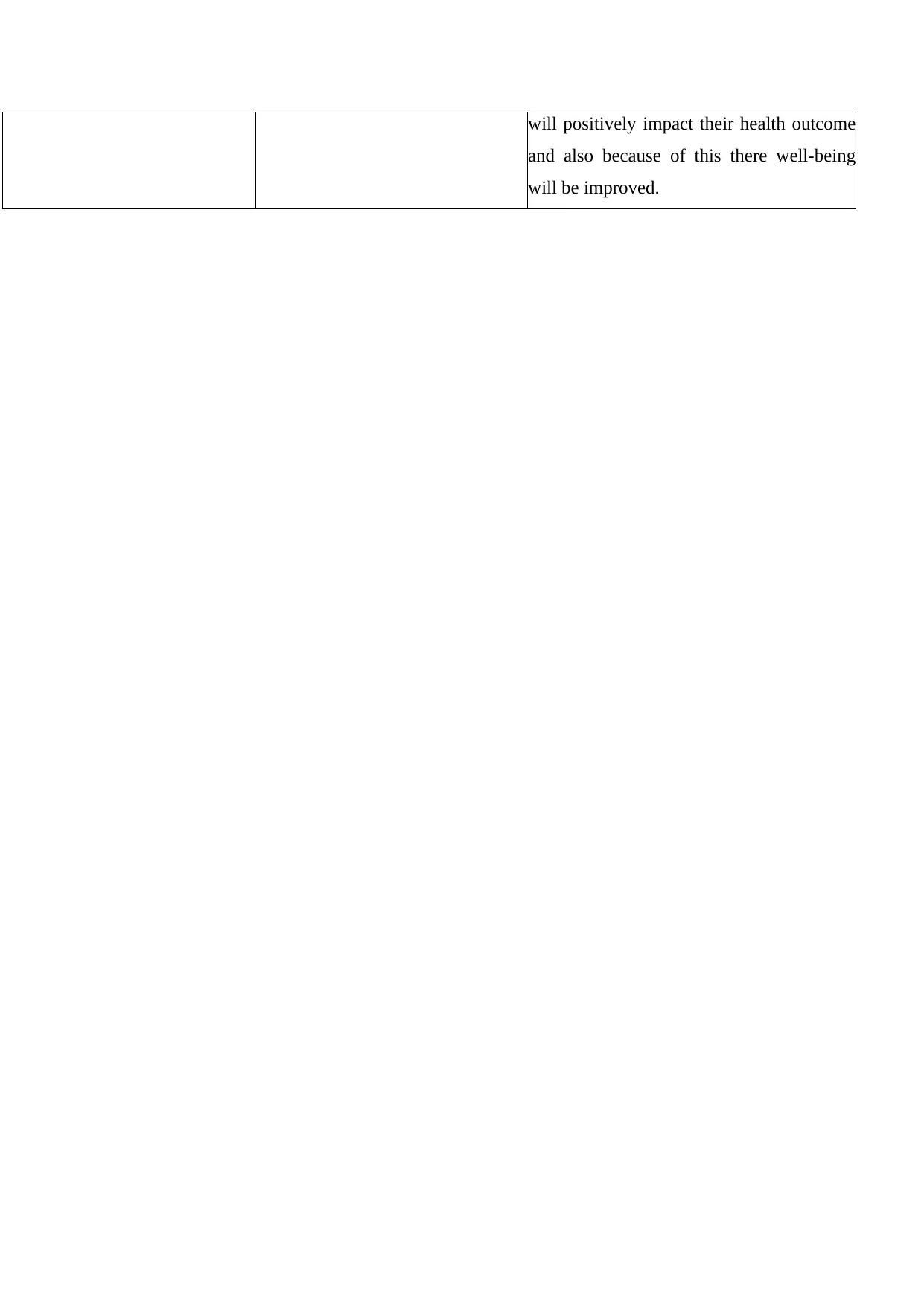
Mental health conditions Treatment Management
Social phobia and specific
phobias such as fear of animals
In this psychotherapy can be given
to those who are suffering from
social phobia.
In this better support must be provided to
workers so that they can work better.
Obsessive- compulsive disorder In this antidepressants such as
Clomipramine (Anafranil) for adults
In this better management strategies must
be thought of by health care professionals
Post-traumatic stress disorder Cognitive behavioural therapy can
be given
In this support must be given to empower
decision making
Depression Anti-depressants can be given to the
depressed patients.
Support by family and health care
professionals must be given to make better
decisions.
Bipolar disorder Psychoeducation and cognitive
behavioural therapy can be given to
patients
In this patients must be treated and their
vulnerability needs to be managed.
Anorexia nervosa In this proper nutritional diet can be
given to patients so that they can be
bring back to normal weight.
Multi-disciplinary team can be used to
manage things.
Borderline personality disorder Psychotherapy can be used in
treating this
Support by family and health care
professionals must be given to make better
decisions
Schizophrenia Anti-psychotic can be given to treat
this disorder
Better treatment must be given in an
underlying condition.
Dementia In this they can be engaged in
giving them holistic care in order to
enhance health outcome.
In this support must be given to empower
decision making. In this patient must be
motivated to take care of themselves as this
Social phobia and specific
phobias such as fear of animals
In this psychotherapy can be given
to those who are suffering from
social phobia.
In this better support must be provided to
workers so that they can work better.
Obsessive- compulsive disorder In this antidepressants such as
Clomipramine (Anafranil) for adults
In this better management strategies must
be thought of by health care professionals
Post-traumatic stress disorder Cognitive behavioural therapy can
be given
In this support must be given to empower
decision making
Depression Anti-depressants can be given to the
depressed patients.
Support by family and health care
professionals must be given to make better
decisions.
Bipolar disorder Psychoeducation and cognitive
behavioural therapy can be given to
patients
In this patients must be treated and their
vulnerability needs to be managed.
Anorexia nervosa In this proper nutritional diet can be
given to patients so that they can be
bring back to normal weight.
Multi-disciplinary team can be used to
manage things.
Borderline personality disorder Psychotherapy can be used in
treating this
Support by family and health care
professionals must be given to make better
decisions
Schizophrenia Anti-psychotic can be given to treat
this disorder
Better treatment must be given in an
underlying condition.
Dementia In this they can be engaged in
giving them holistic care in order to
enhance health outcome.
In this support must be given to empower
decision making. In this patient must be
motivated to take care of themselves as this
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
will positively impact their health outcome
and also because of this there well-being
will be improved.
and also because of this there well-being
will be improved.
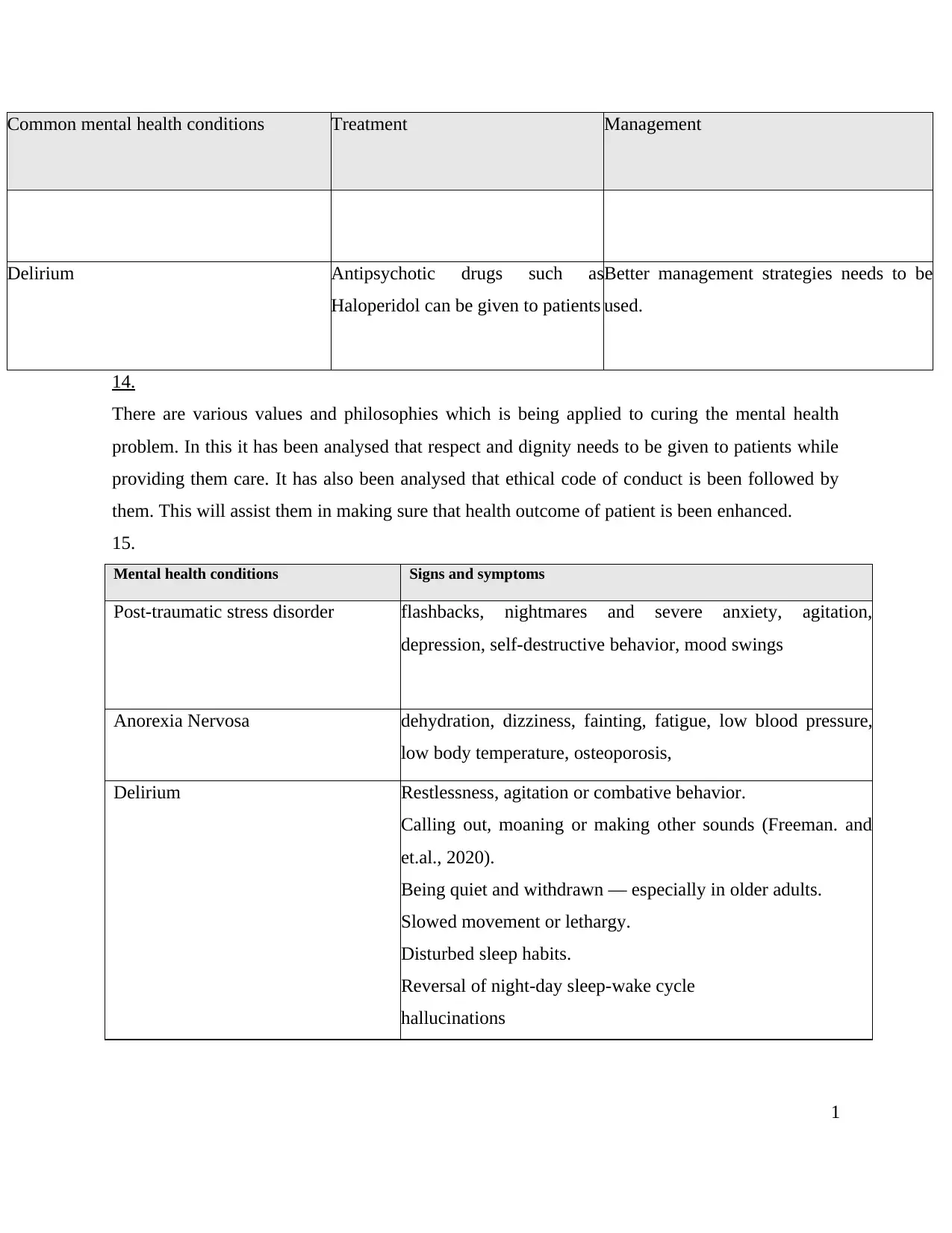
Common mental health conditions Treatment Management
Delirium Antipsychotic drugs such as
Haloperidol can be given to patients
Better management strategies needs to be
used.
14.
There are various values and philosophies which is being applied to curing the mental health
problem. In this it has been analysed that respect and dignity needs to be given to patients while
providing them care. It has also been analysed that ethical code of conduct is been followed by
them. This will assist them in making sure that health outcome of patient is been enhanced.
15.
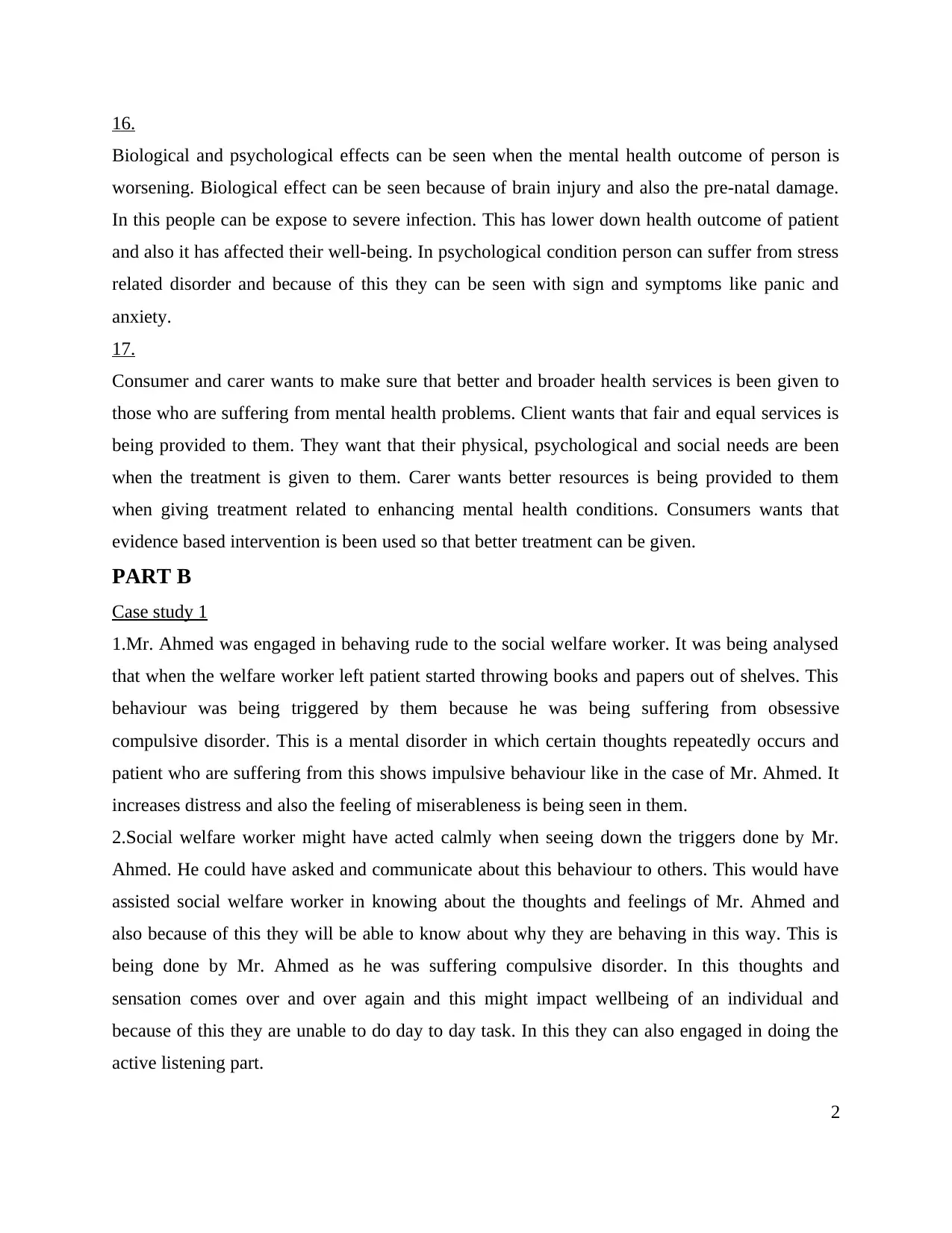
Mental health conditions Signs and symptoms
Post-traumatic stress disorder flashbacks, nightmares and severe anxiety, agitation,
depression, self-destructive behavior, mood swings
Anorexia Nervosa dehydration, dizziness, fainting, fatigue, low blood pressure,
low body temperature, osteoporosis,
Delirium Restlessness, agitation or combative behavior.
Calling out, moaning or making other sounds (Freeman. and
et.al., 2020).
Being quiet and withdrawn — especially in older adults.
Slowed movement or lethargy.
Disturbed sleep habits.
Reversal of night-day sleep-wake cycle
hallucinations
1
Delirium Antipsychotic drugs such as
Haloperidol can be given to patients
Better management strategies needs to be
used.
14.
There are various values and philosophies which is being applied to curing the mental health
problem. In this it has been analysed that respect and dignity needs to be given to patients while
providing them care. It has also been analysed that ethical code of conduct is been followed by
them. This will assist them in making sure that health outcome of patient is been enhanced.
15.
Mental health conditions Signs and symptoms
Post-traumatic stress disorder flashbacks, nightmares and severe anxiety, agitation,
depression, self-destructive behavior, mood swings
Anorexia Nervosa dehydration, dizziness, fainting, fatigue, low blood pressure,
low body temperature, osteoporosis,
Delirium Restlessness, agitation or combative behavior.
Calling out, moaning or making other sounds (Freeman. and
et.al., 2020).
Being quiet and withdrawn — especially in older adults.
Slowed movement or lethargy.
Disturbed sleep habits.
Reversal of night-day sleep-wake cycle
hallucinations
1
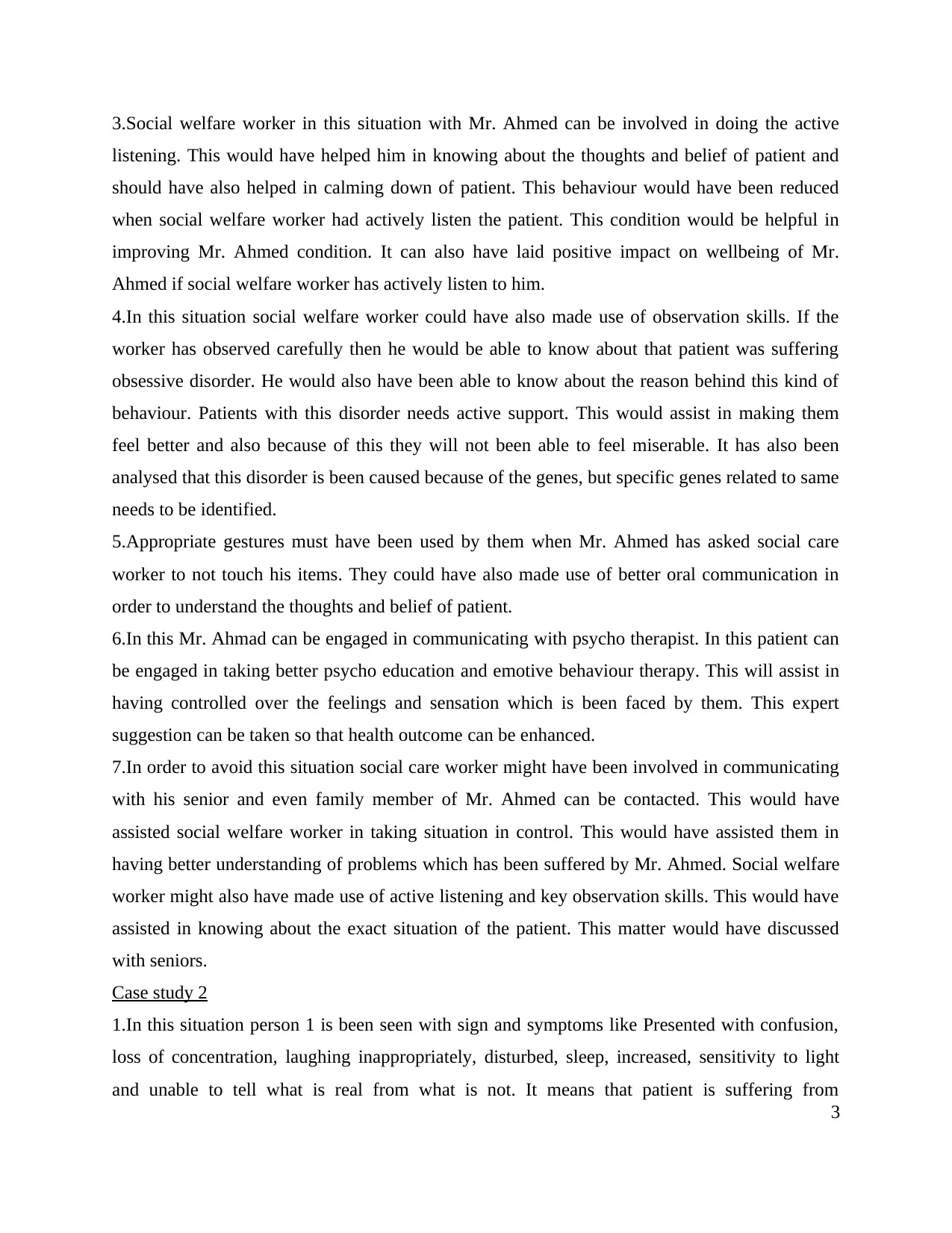
16.
Biological and psychological effects can be seen when the mental health outcome of person is
worsening. Biological effect can be seen because of brain injury and also the pre-natal damage.
In this people can be expose to severe infection. This has lower down health outcome of patient
and also it has affected their well-being. In psychological condition person can suffer from stress
related disorder and because of this they can be seen with sign and symptoms like panic and
anxiety.
17.
Consumer and carer wants to make sure that better and broader health services is been given to
those who are suffering from mental health problems. Client wants that fair and equal services is
being provided to them. They want that their physical, psychological and social needs are been
when the treatment is given to them. Carer wants better resources is being provided to them
when giving treatment related to enhancing mental health conditions. Consumers wants that
evidence based intervention is been used so that better treatment can be given.
PART B
Case study 1
1.Mr. Ahmed was engaged in behaving rude to the social welfare worker. It was being analysed
that when the welfare worker left patient started throwing books and papers out of shelves. This
behaviour was being triggered by them because he was being suffering from obsessive
compulsive disorder. This is a mental disorder in which certain thoughts repeatedly occurs and
patient who are suffering from this shows impulsive behaviour like in the case of Mr. Ahmed. It
increases distress and also the feeling of miserableness is being seen in them.
2.Social welfare worker might have acted calmly when seeing down the triggers done by Mr.
Ahmed. He could have asked and communicate about this behaviour to others. This would have
assisted social welfare worker in knowing about the thoughts and feelings of Mr. Ahmed and
also because of this they will be able to know about why they are behaving in this way. This is
being done by Mr. Ahmed as he was suffering compulsive disorder. In this thoughts and
sensation comes over and over again and this might impact wellbeing of an individual and
because of this they are unable to do day to day task. In this they can also engaged in doing the
active listening part.
2
Biological and psychological effects can be seen when the mental health outcome of person is
worsening. Biological effect can be seen because of brain injury and also the pre-natal damage.
In this people can be expose to severe infection. This has lower down health outcome of patient
and also it has affected their well-being. In psychological condition person can suffer from stress
related disorder and because of this they can be seen with sign and symptoms like panic and
anxiety.
17.
Consumer and carer wants to make sure that better and broader health services is been given to
those who are suffering from mental health problems. Client wants that fair and equal services is
being provided to them. They want that their physical, psychological and social needs are been
when the treatment is given to them. Carer wants better resources is being provided to them
when giving treatment related to enhancing mental health conditions. Consumers wants that
evidence based intervention is been used so that better treatment can be given.
PART B
Case study 1
1.Mr. Ahmed was engaged in behaving rude to the social welfare worker. It was being analysed
that when the welfare worker left patient started throwing books and papers out of shelves. This
behaviour was being triggered by them because he was being suffering from obsessive
compulsive disorder. This is a mental disorder in which certain thoughts repeatedly occurs and
patient who are suffering from this shows impulsive behaviour like in the case of Mr. Ahmed. It
increases distress and also the feeling of miserableness is being seen in them.
2.Social welfare worker might have acted calmly when seeing down the triggers done by Mr.
Ahmed. He could have asked and communicate about this behaviour to others. This would have
assisted social welfare worker in knowing about the thoughts and feelings of Mr. Ahmed and
also because of this they will be able to know about why they are behaving in this way. This is
being done by Mr. Ahmed as he was suffering compulsive disorder. In this thoughts and
sensation comes over and over again and this might impact wellbeing of an individual and
because of this they are unable to do day to day task. In this they can also engaged in doing the
active listening part.
2
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
3.Social welfare worker in this situation with Mr. Ahmed can be involved in doing the active
listening. This would have helped him in knowing about the thoughts and belief of patient and
should have also helped in calming down of patient. This behaviour would have been reduced
when social welfare worker had actively listen the patient. This condition would be helpful in
improving Mr. Ahmed condition. It can also have laid positive impact on wellbeing of Mr.
Ahmed if social welfare worker has actively listen to him.
4.In this situation social welfare worker could have also made use of observation skills. If the
worker has observed carefully then he would be able to know about that patient was suffering
obsessive disorder. He would also have been able to know about the reason behind this kind of
behaviour. Patients with this disorder needs active support. This would assist in making them
feel better and also because of this they will not been able to feel miserable. It has also been
analysed that this disorder is been caused because of the genes, but specific genes related to same
needs to be identified.
5.Appropriate gestures must have been used by them when Mr. Ahmed has asked social care
worker to not touch his items. They could have also made use of better oral communication in
order to understand the thoughts and belief of patient.
6.In this Mr. Ahmad can be engaged in communicating with psycho therapist. In this patient can
be engaged in taking better psycho education and emotive behaviour therapy. This will assist in
having controlled over the feelings and sensation which is been faced by them. This expert
suggestion can be taken so that health outcome can be enhanced.
7.In order to avoid this situation social care worker might have been involved in communicating
with his senior and even family member of Mr. Ahmed can be contacted. This would have
assisted social welfare worker in taking situation in control. This would have assisted them in
having better understanding of problems which has been suffered by Mr. Ahmed. Social welfare
worker might also have made use of active listening and key observation skills. This would have
assisted in knowing about the exact situation of the patient. This matter would have discussed
with seniors.
Case study 2
1.In this situation person 1 is been seen with sign and symptoms like Presented with confusion,
loss of concentration, laughing inappropriately, disturbed, sleep, increased, sensitivity to light
and unable to tell what is real from what is not. It means that patient is suffering from
3
listening. This would have helped him in knowing about the thoughts and belief of patient and
should have also helped in calming down of patient. This behaviour would have been reduced
when social welfare worker had actively listen the patient. This condition would be helpful in
improving Mr. Ahmed condition. It can also have laid positive impact on wellbeing of Mr.
Ahmed if social welfare worker has actively listen to him.
4.In this situation social welfare worker could have also made use of observation skills. If the
worker has observed carefully then he would be able to know about that patient was suffering
obsessive disorder. He would also have been able to know about the reason behind this kind of
behaviour. Patients with this disorder needs active support. This would assist in making them
feel better and also because of this they will not been able to feel miserable. It has also been
analysed that this disorder is been caused because of the genes, but specific genes related to same
needs to be identified.
5.Appropriate gestures must have been used by them when Mr. Ahmed has asked social care
worker to not touch his items. They could have also made use of better oral communication in
order to understand the thoughts and belief of patient.
6.In this Mr. Ahmad can be engaged in communicating with psycho therapist. In this patient can
be engaged in taking better psycho education and emotive behaviour therapy. This will assist in
having controlled over the feelings and sensation which is been faced by them. This expert
suggestion can be taken so that health outcome can be enhanced.
7.In order to avoid this situation social care worker might have been involved in communicating
with his senior and even family member of Mr. Ahmed can be contacted. This would have
assisted social welfare worker in taking situation in control. This would have assisted them in
having better understanding of problems which has been suffered by Mr. Ahmed. Social welfare
worker might also have made use of active listening and key observation skills. This would have
assisted in knowing about the exact situation of the patient. This matter would have discussed
with seniors.
Case study 2
1.In this situation person 1 is been seen with sign and symptoms like Presented with confusion,
loss of concentration, laughing inappropriately, disturbed, sleep, increased, sensitivity to light
and unable to tell what is real from what is not. It means that patient is suffering from
3
Schizophrenia. It is a psychiatric disorder and this disease has no exact cause. It has been
believed that disease is been associated with when there is low amount of grey matter which has
been presented below the central nervous system. In this the patient can go through the situation
of hallucination affecting their mental health negatively.
2.In this case scenario person 2 is been seen with trembling hands and voice, blushing,
hyperventilation, fear, anticipatory anxiety and avoiding public places and crowds including
seeing friends and family. It means that person 2 is suffering from social phobia. Patient
suffering from this are anxious in front of public. They are unable to share their thoughts and
feeling which affects their wellbeing severely. It has also been analysed that these patients are
also unable to make their own decision and they feel invulnerable in front of every other person
which they meet. They can also feel anxious in going to crowded place.
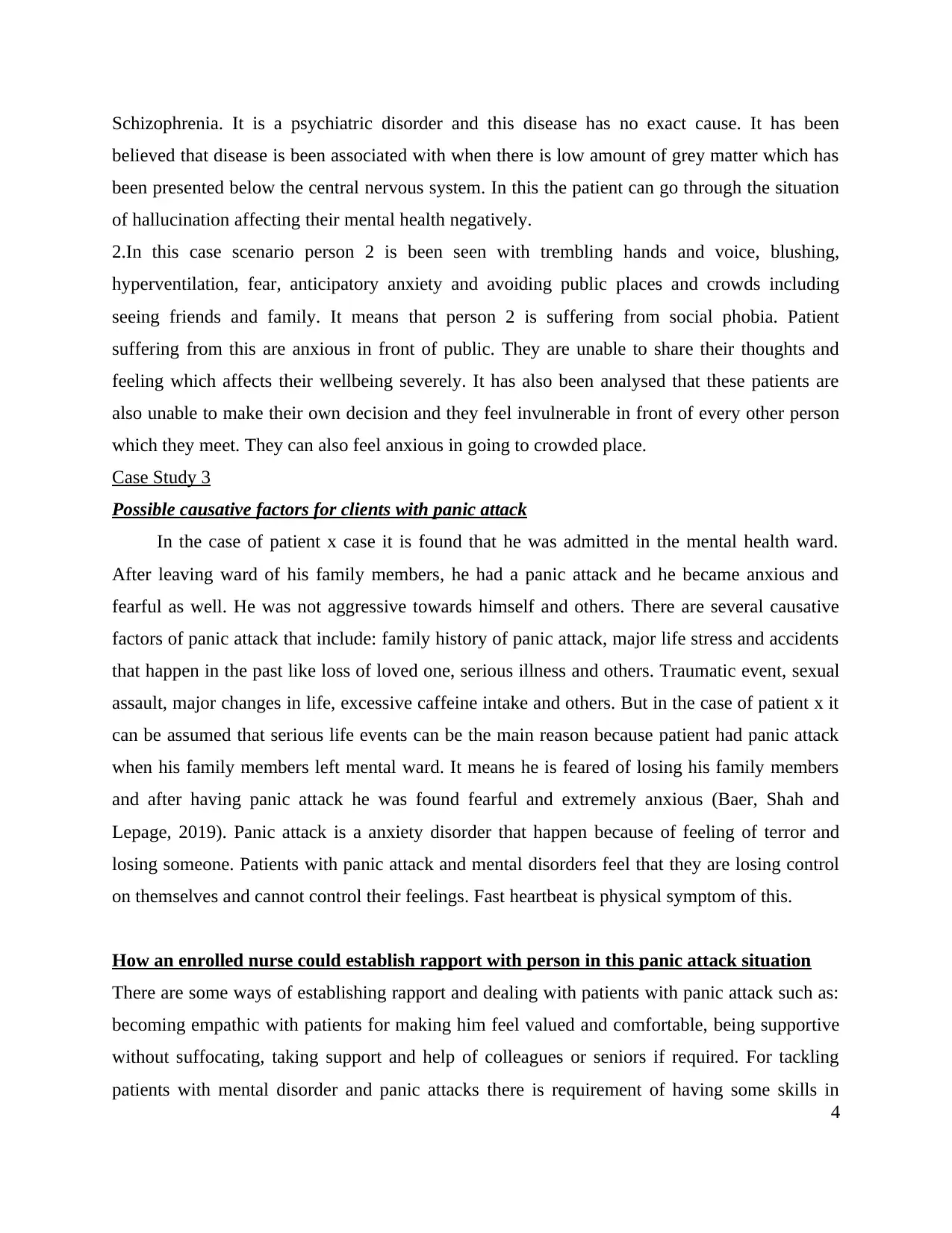
Case Study 3
Possible causative factors for clients with panic attack
In the case of patient x case it is found that he was admitted in the mental health ward.
After leaving ward of his family members, he had a panic attack and he became anxious and
fearful as well. He was not aggressive towards himself and others. There are several causative
factors of panic attack that include: family history of panic attack, major life stress and accidents
that happen in the past like loss of loved one, serious illness and others. Traumatic event, sexual
assault, major changes in life, excessive caffeine intake and others. But in the case of patient x it
can be assumed that serious life events can be the main reason because patient had panic attack
when his family members left mental ward. It means he is feared of losing his family members
and after having panic attack he was found fearful and extremely anxious (Baer, Shah and
Lepage, 2019). Panic attack is a anxiety disorder that happen because of feeling of terror and
losing someone. Patients with panic attack and mental disorders feel that they are losing control
on themselves and cannot control their feelings. Fast heartbeat is physical symptom of this.
How an enrolled nurse could establish rapport with person in this panic attack situation
There are some ways of establishing rapport and dealing with patients with panic attack such as:
becoming empathic with patients for making him feel valued and comfortable, being supportive
without suffocating, taking support and help of colleagues or seniors if required. For tackling
patients with mental disorder and panic attacks there is requirement of having some skills in
4
believed that disease is been associated with when there is low amount of grey matter which has
been presented below the central nervous system. In this the patient can go through the situation
of hallucination affecting their mental health negatively.
2.In this case scenario person 2 is been seen with trembling hands and voice, blushing,
hyperventilation, fear, anticipatory anxiety and avoiding public places and crowds including
seeing friends and family. It means that person 2 is suffering from social phobia. Patient
suffering from this are anxious in front of public. They are unable to share their thoughts and
feeling which affects their wellbeing severely. It has also been analysed that these patients are
also unable to make their own decision and they feel invulnerable in front of every other person
which they meet. They can also feel anxious in going to crowded place.
Case Study 3
Possible causative factors for clients with panic attack
In the case of patient x case it is found that he was admitted in the mental health ward.
After leaving ward of his family members, he had a panic attack and he became anxious and
fearful as well. He was not aggressive towards himself and others. There are several causative
factors of panic attack that include: family history of panic attack, major life stress and accidents
that happen in the past like loss of loved one, serious illness and others. Traumatic event, sexual
assault, major changes in life, excessive caffeine intake and others. But in the case of patient x it
can be assumed that serious life events can be the main reason because patient had panic attack
when his family members left mental ward. It means he is feared of losing his family members
and after having panic attack he was found fearful and extremely anxious (Baer, Shah and
Lepage, 2019). Panic attack is a anxiety disorder that happen because of feeling of terror and
losing someone. Patients with panic attack and mental disorders feel that they are losing control
on themselves and cannot control their feelings. Fast heartbeat is physical symptom of this.
How an enrolled nurse could establish rapport with person in this panic attack situation
There are some ways of establishing rapport and dealing with patients with panic attack such as:
becoming empathic with patients for making him feel valued and comfortable, being supportive
without suffocating, taking support and help of colleagues or seniors if required. For tackling
patients with mental disorder and panic attacks there is requirement of having some skills in
4

enrolled nurse such as: effective communication, empathy and others. With an effective
communication and empathy skills, nurse can interact with patient and can know the main reason
behind panic attack. It makes patients feel valued when people and nurses communicate with
them in an effective manner and try to understand their emotional aspects (Oswald and et.al.,
2018). In addition, it can also be said that patient centre care approach can also help this patient
in improving health as in this approach nurses focus on patients and understanding their needs.
Support and assistance that enrolled nurse seek from colleagues in this situation
Enrolled nurses require support and assistance from their seniors and colleagues for dealing
patients with critical mental disorders and panic attack because patients do not have in their
senses. So, in this regard, it can be said that nurse can seek for support and ask appropriate ways
of encouraging patients for participating in treatment process and relaxation exercise like deep
breathing, meditation, muscle relaxation and others. They can also ask for better and appropriate
interventions such as patient centre care, family involvement, anti depressants and panic focused
psychotherapy (Gensichen and et.al., 2019). They can also ask for ways of using communication
therapy in an effective manner like using silence in this serious cases, giving recognition, active
listening, seeking clarification etc. Seniors and colleagues can also help enrolled nurses by
telling those ways of using interventions and encouraging both patient and their family members.
5
communication and empathy skills, nurse can interact with patient and can know the main reason
behind panic attack. It makes patients feel valued when people and nurses communicate with
them in an effective manner and try to understand their emotional aspects (Oswald and et.al.,
2018). In addition, it can also be said that patient centre care approach can also help this patient
in improving health as in this approach nurses focus on patients and understanding their needs.
Support and assistance that enrolled nurse seek from colleagues in this situation
Enrolled nurses require support and assistance from their seniors and colleagues for dealing
patients with critical mental disorders and panic attack because patients do not have in their
senses. So, in this regard, it can be said that nurse can seek for support and ask appropriate ways
of encouraging patients for participating in treatment process and relaxation exercise like deep
breathing, meditation, muscle relaxation and others. They can also ask for better and appropriate
interventions such as patient centre care, family involvement, anti depressants and panic focused
psychotherapy (Gensichen and et.al., 2019). They can also ask for ways of using communication
therapy in an effective manner like using silence in this serious cases, giving recognition, active
listening, seeking clarification etc. Seniors and colleagues can also help enrolled nurses by
telling those ways of using interventions and encouraging both patient and their family members.
5
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
REFERENCES
Books and Journals
Baer, L.H., Shah, J.L. and Lepage, M., 2019. Anxiety in youth at clinical high risk for psychosis:
A case study and conceptual model. Schizophrenia research, 208, pp.441-446.
Bronson, J. and Berzofsky, M., 2017. Indicators of mental health problems reported by prisoners
and jail inmates, 2011–12. Bureau of Justice Statistics, pp.1-16.
Freeman, D. and et.al., 2020. Sleep disturbance and psychiatric disorders. The Lancet
Psychiatry, 7(7), pp.628-637.
Gao, J. and et.al., 2020. Mental health problems and social media exposure during COVID-19
outbreak. Plos one, 15(4), p.e0231924.
Gensichen, J. and et.al., 2019. Panic Disorder in Primary Care: The Effects of a Team-Based
Intervention—a Cluster-Randomized Trial. Deutsches Ärzteblatt International, 116(10),
p.159.
Kisely, S. and et.al., 2018. Child maltreatment and mental health problems in adulthood: birth
cohort study. The British Journal of Psychiatry, 213(6), pp.698-703.
Martin, A.R. and et.al., 2019. Predicting polygenic risk of psychiatric disorders. Biological
psychiatry, 86(2), pp.97-109.
Oddy, W.H. and et.al., 2018. Dietary patterns, body mass index and inflammation: pathways to
depression and mental health problems in adolescents. Brain, behavior, and
immunity, 69, pp.428-439.
Oswald, T.M. and et.al., 2018. A pilot randomized controlled trial of the ACCESS program: A
group intervention to improve social, adaptive functioning, stress coping, and self-
determination outcomes in young adults with autism spectrum disorder. Journal of
Autism and Developmental Disorders, 48(5), pp.1742-1760.
Pacheco, J.P. and et.al., 2017. Mental health problems among medical students in Brazil: a
systematic review and meta-analysis. Brazilian Journal of Psychiatry, 39(4), pp.369-378.
Wang, Y. and et.al., 2020. Epidemiology of mental health problems among patients with cancer
during COVID-19 pandemic. Translational psychiatry, 10(1), pp.1-10.
6
Books and Journals
Baer, L.H., Shah, J.L. and Lepage, M., 2019. Anxiety in youth at clinical high risk for psychosis:
A case study and conceptual model. Schizophrenia research, 208, pp.441-446.
Bronson, J. and Berzofsky, M., 2017. Indicators of mental health problems reported by prisoners
and jail inmates, 2011–12. Bureau of Justice Statistics, pp.1-16.
Freeman, D. and et.al., 2020. Sleep disturbance and psychiatric disorders. The Lancet
Psychiatry, 7(7), pp.628-637.
Gao, J. and et.al., 2020. Mental health problems and social media exposure during COVID-19
outbreak. Plos one, 15(4), p.e0231924.
Gensichen, J. and et.al., 2019. Panic Disorder in Primary Care: The Effects of a Team-Based
Intervention—a Cluster-Randomized Trial. Deutsches Ärzteblatt International, 116(10),
p.159.
Kisely, S. and et.al., 2018. Child maltreatment and mental health problems in adulthood: birth
cohort study. The British Journal of Psychiatry, 213(6), pp.698-703.
Martin, A.R. and et.al., 2019. Predicting polygenic risk of psychiatric disorders. Biological
psychiatry, 86(2), pp.97-109.
Oddy, W.H. and et.al., 2018. Dietary patterns, body mass index and inflammation: pathways to
depression and mental health problems in adolescents. Brain, behavior, and
immunity, 69, pp.428-439.
Oswald, T.M. and et.al., 2018. A pilot randomized controlled trial of the ACCESS program: A
group intervention to improve social, adaptive functioning, stress coping, and self-
determination outcomes in young adults with autism spectrum disorder. Journal of
Autism and Developmental Disorders, 48(5), pp.1742-1760.
Pacheco, J.P. and et.al., 2017. Mental health problems among medical students in Brazil: a
systematic review and meta-analysis. Brazilian Journal of Psychiatry, 39(4), pp.369-378.
Wang, Y. and et.al., 2020. Epidemiology of mental health problems among patients with cancer
during COVID-19 pandemic. Translational psychiatry, 10(1), pp.1-10.
6
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





