Case Study: Hypoglycemia Assessment, Pathophysiology, and Care Plan
VerifiedAdded on 2023/06/10
|20
|3444
|355
Case Study
AI Summary
This case study focuses on Mrs. Anthony, a 35-year-old patient admitted to the emergency department with multiple fractures, loss of consciousness, and smoke inhalation. The case details her type 2 diabetes diagnosis and presenting symptoms, including hypotension, tachycardia, hypoxemia, and a low blood glucose level of 2.8 mmol/L, indicating hypoglycemia. The assignment explores the pathophysiology of hypoglycemia, explaining how insufficient glucose impacts brain function and triggers hormonal and metabolic responses. It also outlines a comprehensive nursing care plan, including assessment, interventions such as glucagon administration and oxygen therapy, and rationales for each intervention, aiming to restore blood glucose levels, improve vital signs, and address the patient's various symptoms. The essay also highlights the importance of glycemic control, identifying precipitating factors, regular blood glucose monitoring, patient education, and medication safety to prevent future hypoglycemic events. The case study emphasizes the need for a multidisciplinary approach and the importance of patient and family education for effective self-management of glucose levels.

Running head: CASE STUDY
Case Report Assessment 1
Name of the Student
Name of the University
Author Note
Case Report Assessment 1
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1CASE STUDY
Part 1
Introduction-
Low blood glucose or hypoglycemia occurs in instances when the levels of sugar in
the blood are found much less than the normal range. Most people diagnosed with diabetes
mellitus have a mean blood sugar level of 70 milligrams per decilitre (mg/dL). Although the
symptoms of the physiological abnormality differs among people. However, the symptoms
reported by most individuals comprise of shaky and jittery feelings, headache, blurred vision,
dizziness, confusion, pale face, irritability, and irregular or fast heartbeat. Some of the severe
symptoms of the condition encompass convulsions and seizures, unconsciousness, and the
lack of ability to drink or eat (Seaquist et al. 2013, p.DC_122480).
This condition has most commonly been associated with adverse effects of insulin and
other kinds of diabetes medications. Some of the most common medications that lead to
hypoglycaemia include meglitinides and sulfonylureas (Pfeiffer 2016, p.117). Furthermore,
failure of the affected individuals to consume adequate amount of carbohydrates, skipping or
delaying meals, vigorous physical activity and alcohol consumption increases the risks of
hypoglycaemia. This essay will elaborate on a case study about a hypoglycaemic patient,
admitted to the emergency department in a hospital. Furthermore, it will also shed light on
the pathophysiology of the condition and explain the nursing management that will be
delivered to the patient.
Assessment data-
The case study is about Mrs. Anthony, aged 35 years who has been admitted to the
HHHS Ward 1. Some of her presenting complaints that resulted in her admission to the ED
include multiple fractures, loss of consciousness, and smoke inhalation. Her past medical
history includes diagnosis of diabetes mellitus (type 2). Upon conducting an assessment risks
Part 1
Introduction-
Low blood glucose or hypoglycemia occurs in instances when the levels of sugar in
the blood are found much less than the normal range. Most people diagnosed with diabetes
mellitus have a mean blood sugar level of 70 milligrams per decilitre (mg/dL). Although the
symptoms of the physiological abnormality differs among people. However, the symptoms
reported by most individuals comprise of shaky and jittery feelings, headache, blurred vision,
dizziness, confusion, pale face, irritability, and irregular or fast heartbeat. Some of the severe
symptoms of the condition encompass convulsions and seizures, unconsciousness, and the
lack of ability to drink or eat (Seaquist et al. 2013, p.DC_122480).
This condition has most commonly been associated with adverse effects of insulin and
other kinds of diabetes medications. Some of the most common medications that lead to
hypoglycaemia include meglitinides and sulfonylureas (Pfeiffer 2016, p.117). Furthermore,
failure of the affected individuals to consume adequate amount of carbohydrates, skipping or
delaying meals, vigorous physical activity and alcohol consumption increases the risks of
hypoglycaemia. This essay will elaborate on a case study about a hypoglycaemic patient,
admitted to the emergency department in a hospital. Furthermore, it will also shed light on
the pathophysiology of the condition and explain the nursing management that will be
delivered to the patient.
Assessment data-
The case study is about Mrs. Anthony, aged 35 years who has been admitted to the
HHHS Ward 1. Some of her presenting complaints that resulted in her admission to the ED
include multiple fractures, loss of consciousness, and smoke inhalation. Her past medical
history includes diagnosis of diabetes mellitus (type 2). Upon conducting an assessment risks
2CASE STUDY
for hypoglycaemia were noticed. Some of her vital signs indicated hypotension, high pulse
rate, high body temperature and low amount of oxygen saturation. Her respiratory rate was
normal. Furthermore, the low amount of blood glucose levels were also observed in the
patient. Diastolic hypotension is evidenced by the fact that her blood pressure levels were
around 95/50. Diastolic blood pressure less than 60 mmHg is regarded as hypotension
(Halliwill et al. 2013, p.12). Abnormally reduced blood pressure results in fainting and
dizziness and can also be considered life-threatening. Her pulse rate of 120 beats per minute
indicated presence of tachycardia, a condition characterised by heart rate that exceeds the
resting or normal rate of 100 beats per minute (Fenoglio Jr et al. 2015, p.187). Presence of
type 2 diabetes can be considered as a risk factor that increased her susceptibility to report an
abnormally high pulse rate. Oxygen saturation generally measures the percentage of oxygen
binding sites that are associated with haemoglobin in the bloodstream.
The patient reported 92% SAO2, thereby indicating the presence of hypoxemia that
was characterised by an abnormal low amount of oxygen in the blood. This oxygen
deficiency results in failure to supply adequate oxygen to the blood. The normal blood
glucose levels are found to be 4.0 to 5.4 mmol/L during fasting and upto 7.8 mmol/L, after 2
hours of having a meal. The fact that Mrs. Anthony reported blood sugar levels of 2.8
mmol/L confirms the presence of hypoglycaemia that occurs when there is a drop in the
amount of blood sugar, below the normal levels. This in turn increases the risk of the patient
of suffering from trouble in talking, clumsiness, seizures, loss of consciousness, and
subsequent death. Thus, hypoglycaemia can be cited as the primary reason that resulted in her
loss of awareness, upon arrival to the ED.
Pathophysiology
for hypoglycaemia were noticed. Some of her vital signs indicated hypotension, high pulse
rate, high body temperature and low amount of oxygen saturation. Her respiratory rate was
normal. Furthermore, the low amount of blood glucose levels were also observed in the
patient. Diastolic hypotension is evidenced by the fact that her blood pressure levels were
around 95/50. Diastolic blood pressure less than 60 mmHg is regarded as hypotension
(Halliwill et al. 2013, p.12). Abnormally reduced blood pressure results in fainting and
dizziness and can also be considered life-threatening. Her pulse rate of 120 beats per minute
indicated presence of tachycardia, a condition characterised by heart rate that exceeds the
resting or normal rate of 100 beats per minute (Fenoglio Jr et al. 2015, p.187). Presence of
type 2 diabetes can be considered as a risk factor that increased her susceptibility to report an
abnormally high pulse rate. Oxygen saturation generally measures the percentage of oxygen
binding sites that are associated with haemoglobin in the bloodstream.
The patient reported 92% SAO2, thereby indicating the presence of hypoxemia that
was characterised by an abnormal low amount of oxygen in the blood. This oxygen
deficiency results in failure to supply adequate oxygen to the blood. The normal blood
glucose levels are found to be 4.0 to 5.4 mmol/L during fasting and upto 7.8 mmol/L, after 2
hours of having a meal. The fact that Mrs. Anthony reported blood sugar levels of 2.8
mmol/L confirms the presence of hypoglycaemia that occurs when there is a drop in the
amount of blood sugar, below the normal levels. This in turn increases the risk of the patient
of suffering from trouble in talking, clumsiness, seizures, loss of consciousness, and
subsequent death. Thus, hypoglycaemia can be cited as the primary reason that resulted in her
loss of awareness, upon arrival to the ED.
Pathophysiology
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3CASE STUDY
Showing similarity with most animal tissues, the metabolism of the brain principally
depends on glucose as the fuel. An inadequate quantity of glucose is generally obtained
from the glycogen stored in astrocyte cells, but gets consumed within less time. Thus, the
brain is highly dependent on a constant source of glucose that diffuses from the bloodstream
into interstitial cells and tissues, present within the central nervous system. Therefore,
reduction in the amount of glucose present in the blood primarily affects the brain. In most
individuals, this lowering of blood glucose level below 3.6 mmol/L (65 mg/dL) manifests in
the form of a lessening in the mental efficiency (Kovatchev & Cobelli 2016, p.508). This is
most commonly exhibited in the form of an impairment in judgement and/or action that
becomes more prominent at levels less than 2.2mmol/L (40 mg/dL). With a further reduction
in the sugar levels, seizures might also occur. The neurons enter a state of electrical silence
with a reduction in the blood glucose levels below 0.55 mmol/L (10 mg/dL), thereby leading
to coma (Bergenstal et al. 2013, p.227). These effects on the brain are together referred to
as neuroglycopenia.
There occurs huge number of hormonal, nervous and metabolic changes that occur in
the body in response to inadequate supply of blood sugar to the brain. Most of the changes
are adaptive or defensive, with an intent to increase the blood glucose levels by the process of
gluconeogenesis or glycogenolysis. Under conditions when there is a huge reduction in the
blood sugar levels, the liver is able to convert stored reserves of glycogen into glucose,
thereby releasing it into bloodstream (Cryer 2013, p.369). This in turn prevents the affected
individual from entering a state of diabetic coma. Mild or brief periods of hypoglycemia fails
to exert any lasting effects on the human brain. However, the brain responses get temporarily
altered. Severe hypoglycemia results in an impairment in motor control, cognitive function,
and/or consciousness. Majority of patients with type 2 diabetes, like Mrs. Anthony in the case
study are under the first line treatment that involves administration of compounds that
Showing similarity with most animal tissues, the metabolism of the brain principally
depends on glucose as the fuel. An inadequate quantity of glucose is generally obtained
from the glycogen stored in astrocyte cells, but gets consumed within less time. Thus, the
brain is highly dependent on a constant source of glucose that diffuses from the bloodstream
into interstitial cells and tissues, present within the central nervous system. Therefore,
reduction in the amount of glucose present in the blood primarily affects the brain. In most
individuals, this lowering of blood glucose level below 3.6 mmol/L (65 mg/dL) manifests in
the form of a lessening in the mental efficiency (Kovatchev & Cobelli 2016, p.508). This is
most commonly exhibited in the form of an impairment in judgement and/or action that
becomes more prominent at levels less than 2.2mmol/L (40 mg/dL). With a further reduction
in the sugar levels, seizures might also occur. The neurons enter a state of electrical silence
with a reduction in the blood glucose levels below 0.55 mmol/L (10 mg/dL), thereby leading
to coma (Bergenstal et al. 2013, p.227). These effects on the brain are together referred to
as neuroglycopenia.
There occurs huge number of hormonal, nervous and metabolic changes that occur in
the body in response to inadequate supply of blood sugar to the brain. Most of the changes
are adaptive or defensive, with an intent to increase the blood glucose levels by the process of
gluconeogenesis or glycogenolysis. Under conditions when there is a huge reduction in the
blood sugar levels, the liver is able to convert stored reserves of glycogen into glucose,
thereby releasing it into bloodstream (Cryer 2013, p.369). This in turn prevents the affected
individual from entering a state of diabetic coma. Mild or brief periods of hypoglycemia fails
to exert any lasting effects on the human brain. However, the brain responses get temporarily
altered. Severe hypoglycemia results in an impairment in motor control, cognitive function,
and/or consciousness. Majority of patients with type 2 diabetes, like Mrs. Anthony in the case
study are under the first line treatment that involves administration of compounds that
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4CASE STUDY
promote insulin release. Sulfonylureas has become the mainstay treatment for obtaining
glycemic control, and generates hypoglycaemia by bringing about changes that block the
potassium channels present on the beta cells, thereby altering the membrane potential and
triggering the release of insulin. Research evidences have established the fact the uptake of
brain glucose increases in response to recurrent hypoglycaemia. Owing to the fact that the
neurotransmitter epinephrine plays an essential role in tachycardia generation and
nervousness among the patients, reduction in release of catecholamine contributes to the loss
of consciousness during hypogylcemia.
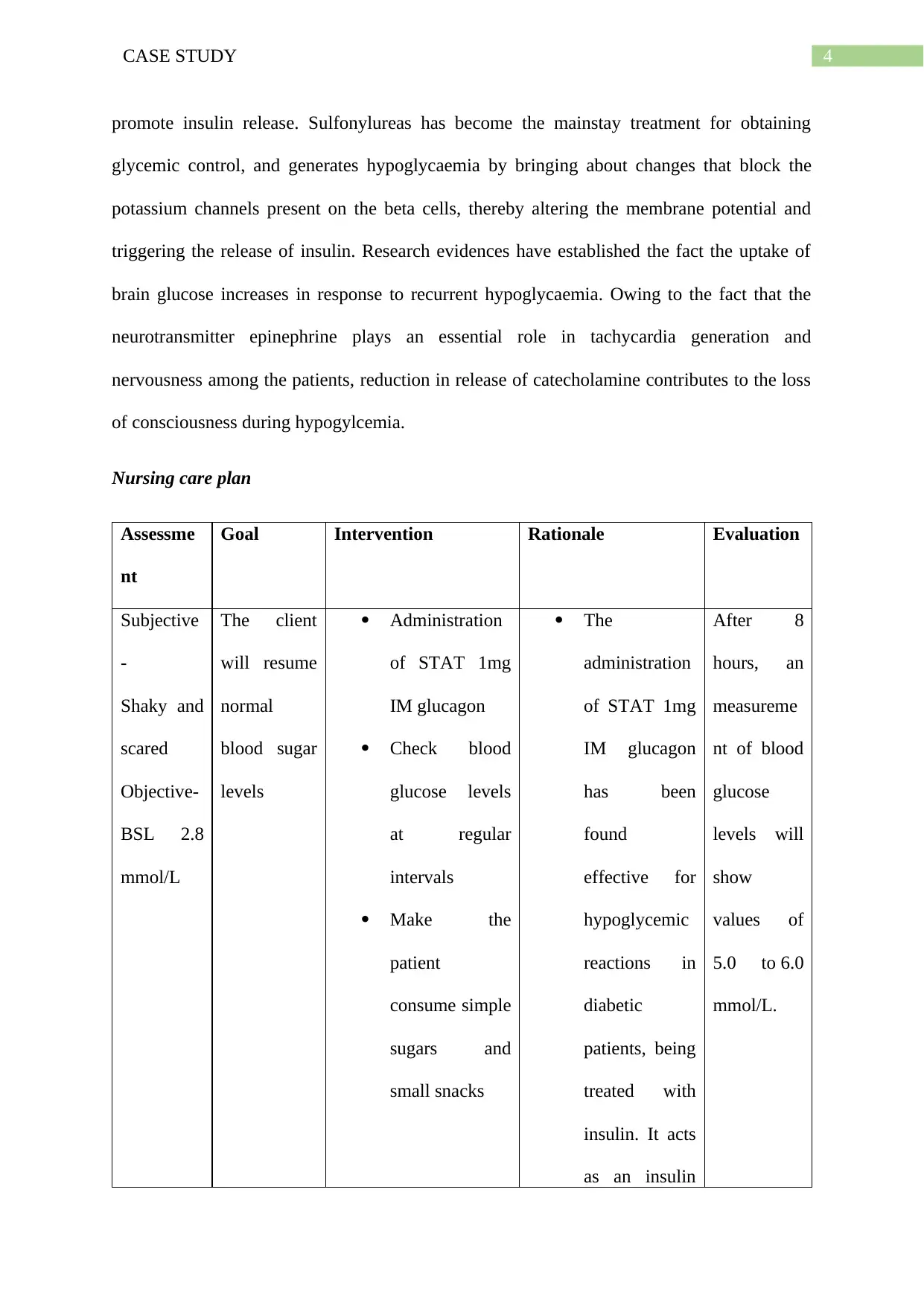
Nursing care plan
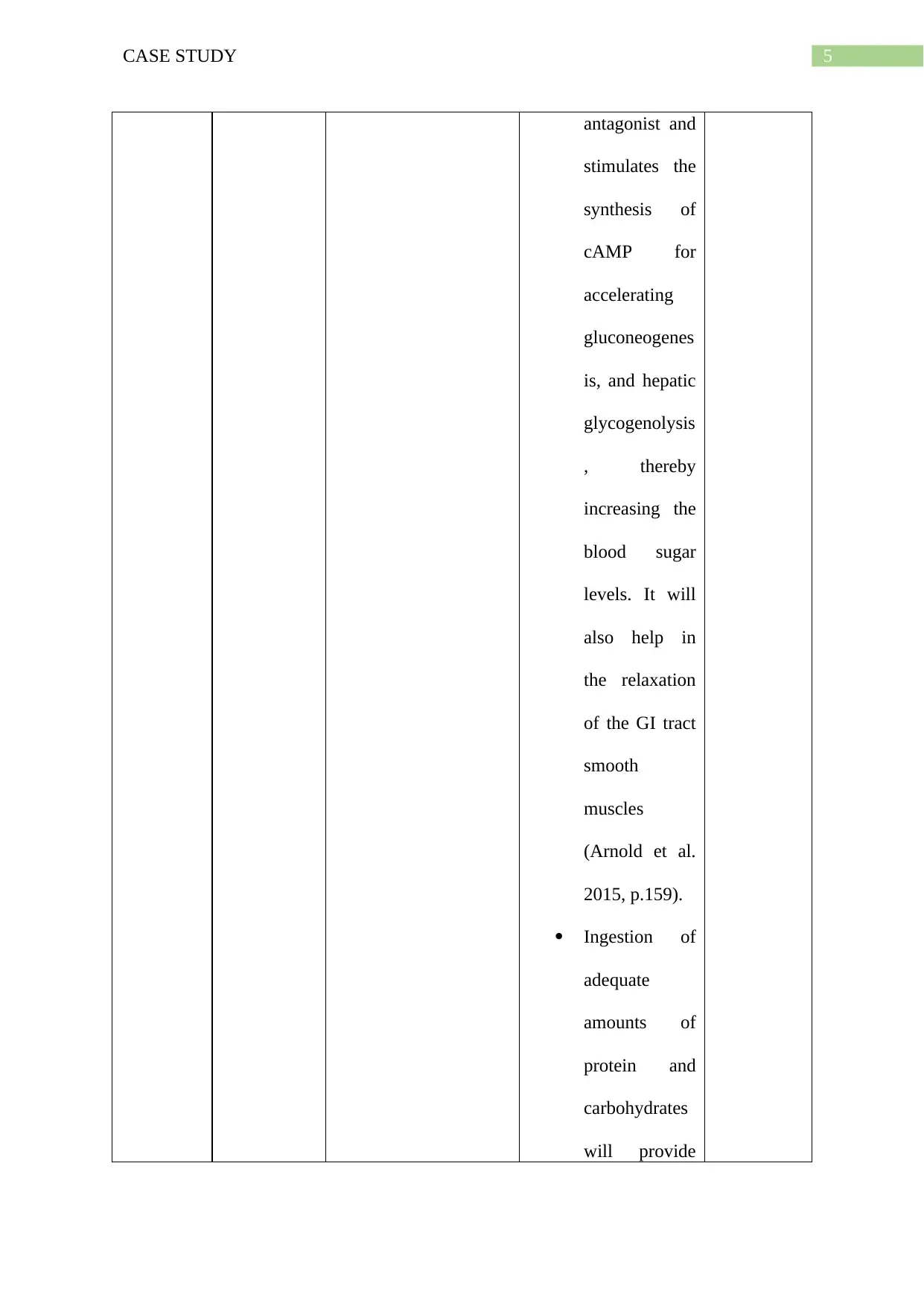
Assessme
nt
Goal Intervention Rationale Evaluation
Subjective
-
Shaky and
scared
Objective-
BSL 2.8
mmol/L
The client
will resume
normal
blood sugar
levels
Administration
of STAT 1mg
IM glucagon
Check blood
glucose levels
at regular
intervals
Make the
patient
consume simple
sugars and
small snacks
The
administration
of STAT 1mg
IM glucagon
has been
found
effective for
hypoglycemic
reactions in
diabetic
patients, being
treated with
insulin. It acts
as an insulin
After 8
hours, an
measureme
nt of blood
glucose
levels will
show
values of
5.0 to 6.0
mmol/L.
promote insulin release. Sulfonylureas has become the mainstay treatment for obtaining
glycemic control, and generates hypoglycaemia by bringing about changes that block the
potassium channels present on the beta cells, thereby altering the membrane potential and
triggering the release of insulin. Research evidences have established the fact the uptake of
brain glucose increases in response to recurrent hypoglycaemia. Owing to the fact that the
neurotransmitter epinephrine plays an essential role in tachycardia generation and
nervousness among the patients, reduction in release of catecholamine contributes to the loss
of consciousness during hypogylcemia.
Nursing care plan
Assessme
nt
Goal Intervention Rationale Evaluation
Subjective
-
Shaky and
scared
Objective-
BSL 2.8
mmol/L
The client
will resume
normal
blood sugar
levels
Administration
of STAT 1mg
IM glucagon
Check blood
glucose levels
at regular
intervals
Make the
patient
consume simple
sugars and
small snacks
The
administration
of STAT 1mg
IM glucagon
has been
found
effective for
hypoglycemic
reactions in
diabetic
patients, being
treated with
insulin. It acts
as an insulin
After 8
hours, an
measureme
nt of blood
glucose
levels will
show
values of
5.0 to 6.0
mmol/L.
5CASE STUDY
antagonist and
stimulates the
synthesis of
cAMP for
accelerating
gluconeogenes
is, and hepatic
glycogenolysis
, thereby
increasing the
blood sugar
levels. It will
also help in
the relaxation
of the GI tract
smooth
muscles
(Arnold et al.
2015, p.159).
Ingestion of
adequate
amounts of
protein and
carbohydrates
will provide
antagonist and
stimulates the
synthesis of
cAMP for
accelerating
gluconeogenes
is, and hepatic
glycogenolysis
, thereby
increasing the
blood sugar
levels. It will
also help in
the relaxation
of the GI tract
smooth
muscles
(Arnold et al.
2015, p.159).
Ingestion of
adequate
amounts of
protein and
carbohydrates
will provide
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6CASE STUDY
energy
(Choudhary et
al. 2015,
p.1018)
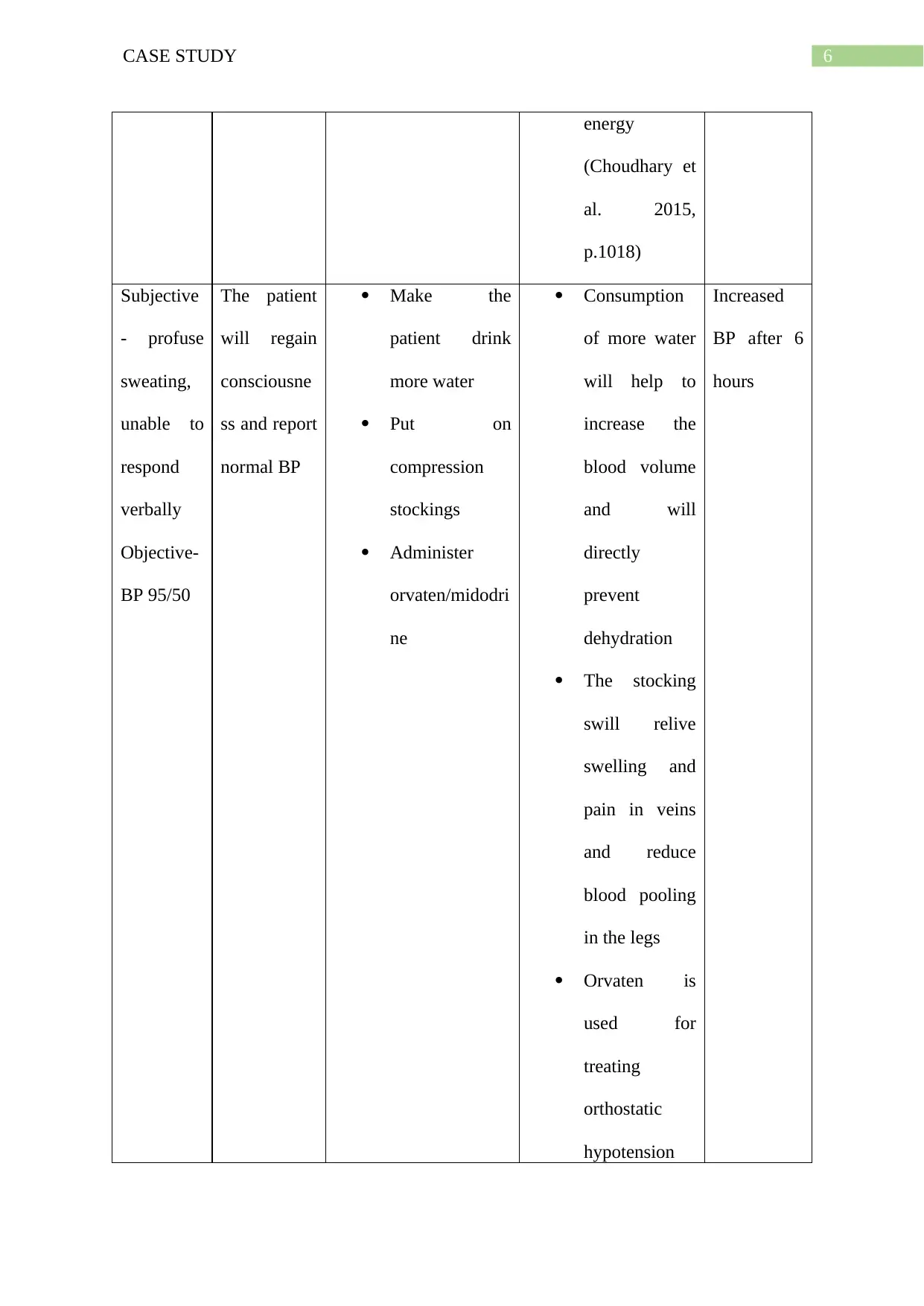
Subjective
- profuse
sweating,
unable to
respond
verbally
Objective-
BP 95/50
The patient
will regain
consciousne
ss and report
normal BP
Make the
patient drink
more water
Put on
compression
stockings
Administer
orvaten/midodri
ne
Consumption
of more water
will help to
increase the
blood volume
and will
directly
prevent
dehydration
The stocking
swill relive
swelling and
pain in veins
and reduce
blood pooling
in the legs
Orvaten is
used for
treating
orthostatic
hypotension
Increased
BP after 6
hours
energy
(Choudhary et
al. 2015,
p.1018)
Subjective
- profuse
sweating,
unable to
respond
verbally
Objective-
BP 95/50
The patient
will regain
consciousne
ss and report
normal BP
Make the
patient drink
more water
Put on
compression
stockings
Administer
orvaten/midodri
ne
Consumption
of more water
will help to
increase the
blood volume
and will
directly
prevent
dehydration
The stocking
swill relive
swelling and
pain in veins
and reduce
blood pooling
in the legs
Orvaten is
used for
treating
orthostatic
hypotension
Increased
BP after 6
hours
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7CASE STUDY
and belongs to
the alpha
receptor
agonist group
of drugs.
These
maintain
proper blood
pressure and
prevents
symptoms of
light-
headedness
and dizziness
(Izcovich et al.
2014, p.12)
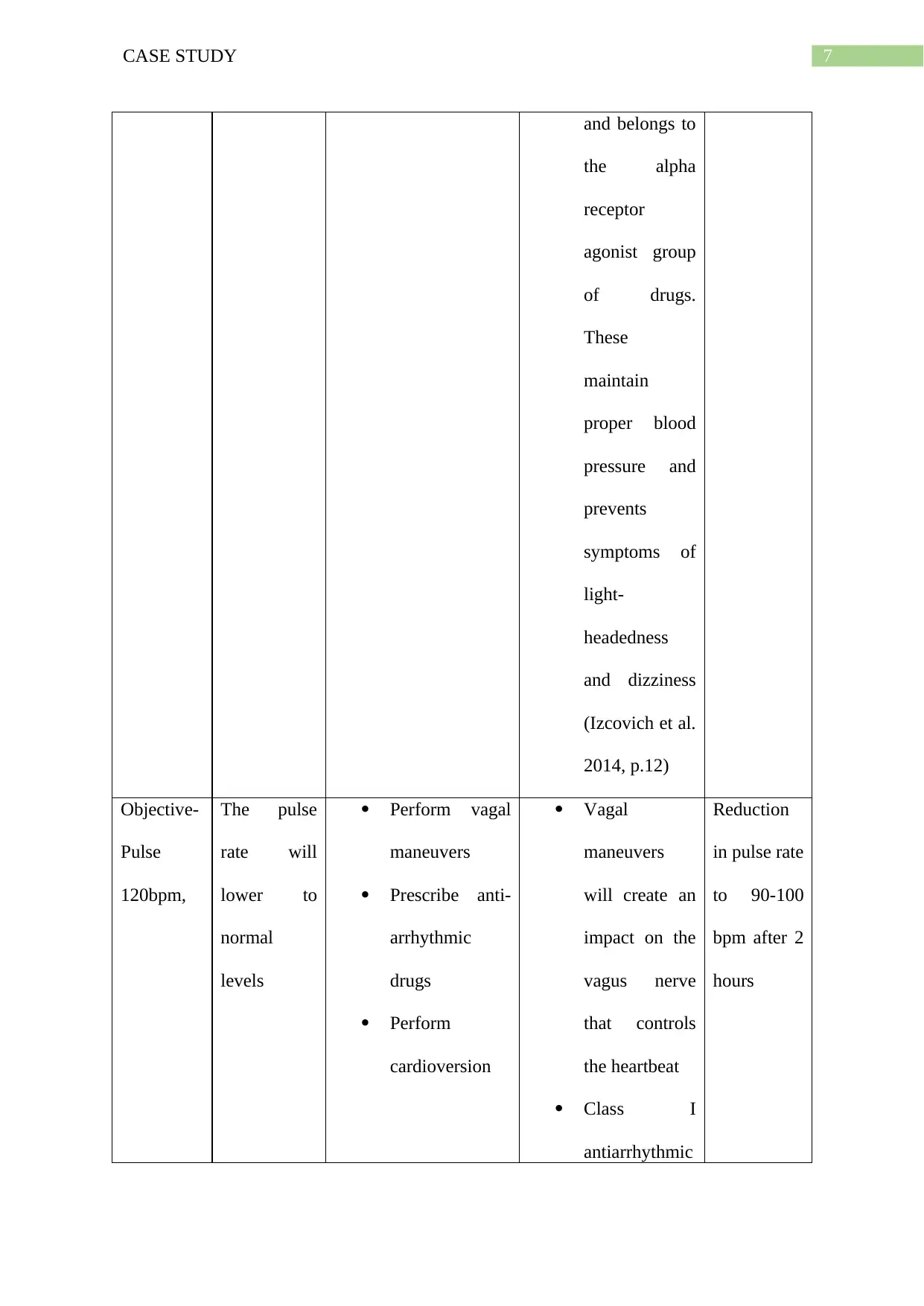
Objective-
Pulse
120bpm,
The pulse
rate will
lower to
normal
levels
Perform vagal
maneuvers
Prescribe anti-
arrhythmic
drugs
Perform
cardioversion
Vagal
maneuvers
will create an
impact on the
vagus nerve
that controls
the heartbeat
Class I
antiarrhythmic
Reduction
in pulse rate
to 90-100
bpm after 2
hours
and belongs to
the alpha
receptor
agonist group
of drugs.
These
maintain
proper blood
pressure and
prevents
symptoms of
light-
headedness
and dizziness
(Izcovich et al.
2014, p.12)
Objective-
Pulse
120bpm,
The pulse
rate will
lower to
normal
levels
Perform vagal
maneuvers
Prescribe anti-
arrhythmic
drugs
Perform
cardioversion
Vagal
maneuvers
will create an
impact on the
vagus nerve
that controls
the heartbeat
Class I
antiarrhythmic
Reduction
in pulse rate
to 90-100
bpm after 2
hours
8CASE STUDY
agents will
suppress the
abnormal heart
rhythm by
interfering
with sodium
channels
(Motoki et al.
2016, p.16).
Cardioversion
will involve
delivery of a
shock to the
chest that will
affect
electrical
impulses and
restore the
heart beat
(Cappato et al.
2014, p.3349)
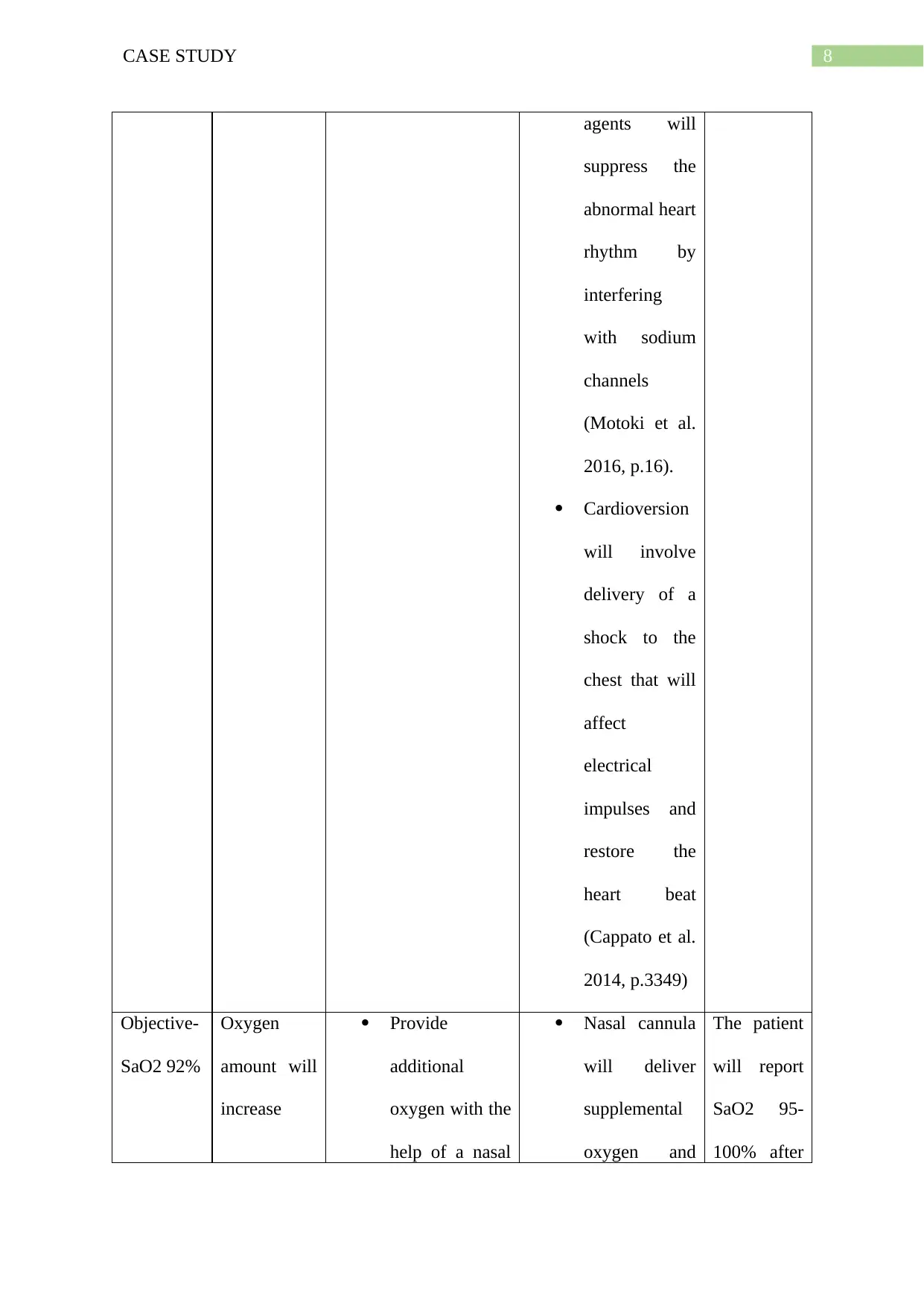
Objective-
SaO2 92%
Oxygen
amount will
increase
Provide
additional
oxygen with the
help of a nasal
Nasal cannula
will deliver
supplemental
oxygen and
The patient
will report
SaO2 95-
100% after
agents will
suppress the
abnormal heart
rhythm by
interfering
with sodium
channels
(Motoki et al.
2016, p.16).
Cardioversion
will involve
delivery of a
shock to the
chest that will
affect
electrical
impulses and
restore the
heart beat
(Cappato et al.
2014, p.3349)
Objective-
SaO2 92%
Oxygen
amount will
increase
Provide
additional
oxygen with the
help of a nasal
Nasal cannula
will deliver
supplemental
oxygen and
The patient
will report
SaO2 95-
100% after
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
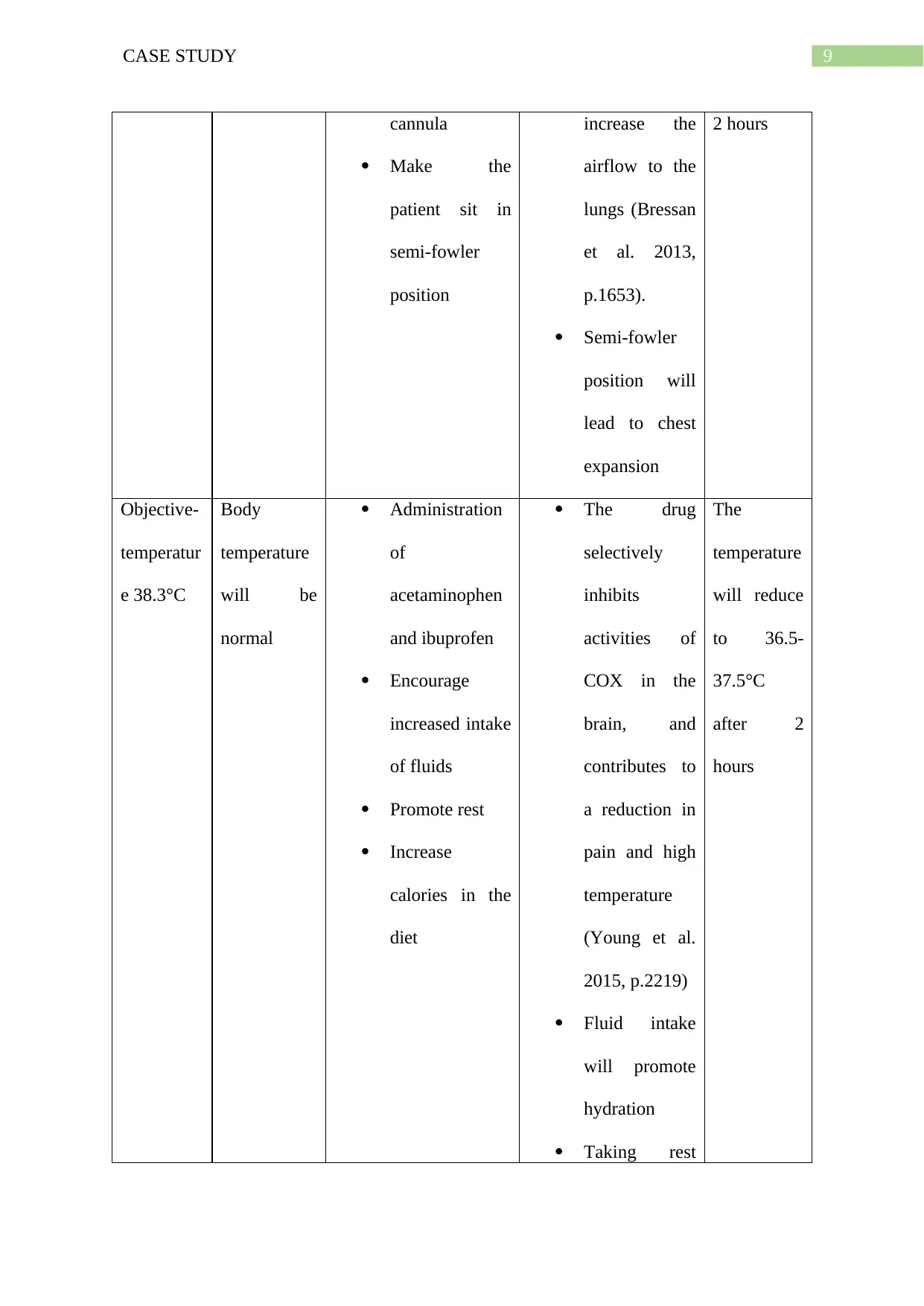
9CASE STUDY
cannula
Make the
patient sit in
semi-fowler
position
increase the
airflow to the
lungs (Bressan
et al. 2013,
p.1653).
Semi-fowler
position will
lead to chest
expansion
2 hours
Objective-
temperatur
e 38.3°C
Body
temperature
will be
normal
Administration
of
acetaminophen
and ibuprofen
Encourage
increased intake
of fluids
Promote rest
Increase
calories in the
diet
The drug
selectively
inhibits
activities of
COX in the
brain, and
contributes to
a reduction in
pain and high
temperature
(Young et al.
2015, p.2219)
Fluid intake
will promote
hydration
Taking rest
The
temperature
will reduce
to 36.5-
37.5°C
after 2
hours
cannula
Make the
patient sit in
semi-fowler
position
increase the
airflow to the
lungs (Bressan
et al. 2013,
p.1653).
Semi-fowler
position will
lead to chest
expansion
2 hours
Objective-
temperatur
e 38.3°C
Body
temperature
will be
normal
Administration
of
acetaminophen
and ibuprofen
Encourage
increased intake
of fluids
Promote rest
Increase
calories in the
diet
The drug
selectively
inhibits
activities of
COX in the
brain, and
contributes to
a reduction in
pain and high
temperature
(Young et al.
2015, p.2219)
Fluid intake
will promote
hydration
Taking rest
The
temperature
will reduce
to 36.5-
37.5°C
after 2
hours
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10CASE STUDY
will help to
regain energy
Calorie rich
diet will also
lower
temperature
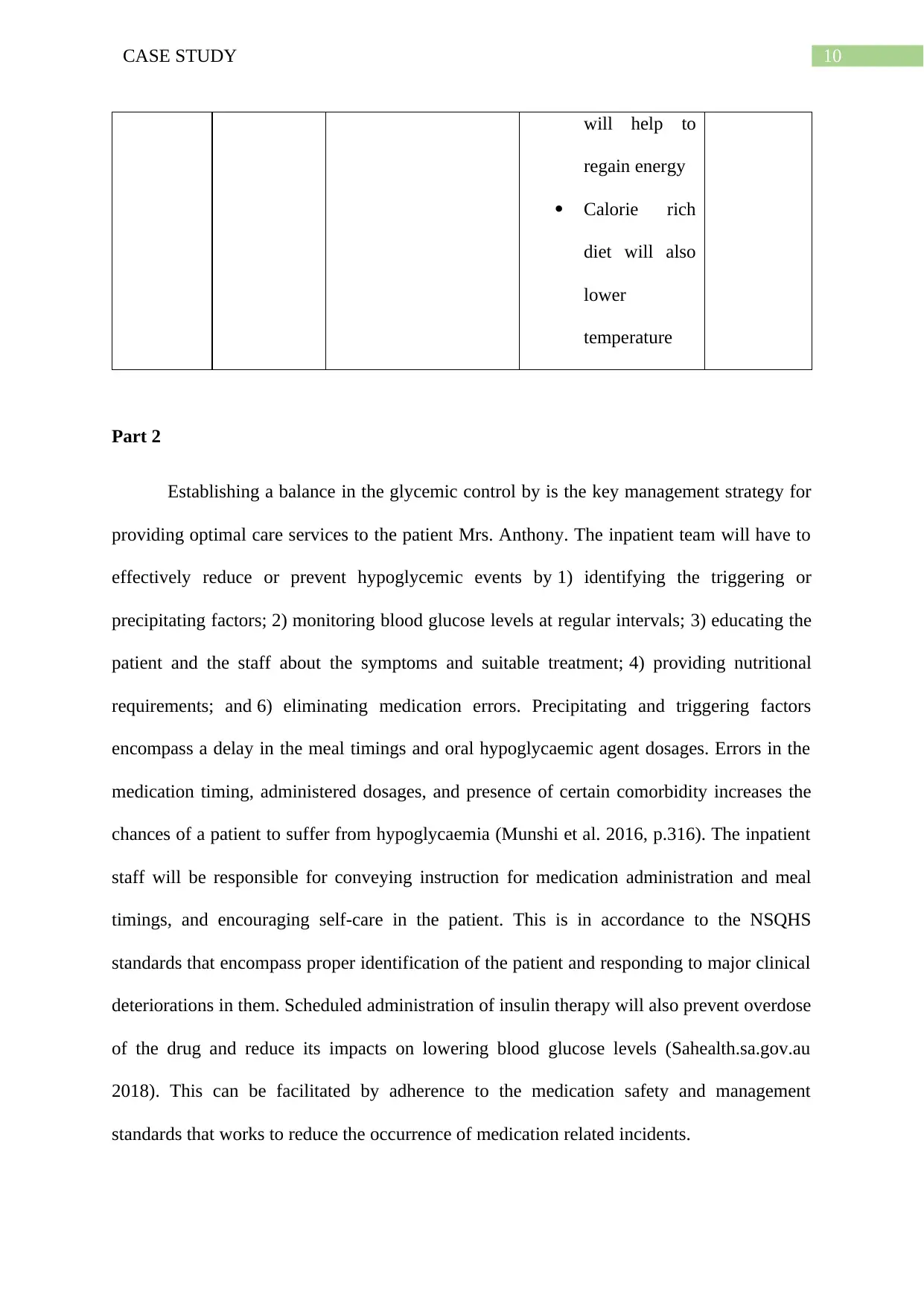
Part 2
Establishing a balance in the glycemic control by is the key management strategy for
providing optimal care services to the patient Mrs. Anthony. The inpatient team will have to
effectively reduce or prevent hypoglycemic events by 1) identifying the triggering or
precipitating factors; 2) monitoring blood glucose levels at regular intervals; 3) educating the
patient and the staff about the symptoms and suitable treatment; 4) providing nutritional
requirements; and 6) eliminating medication errors. Precipitating and triggering factors
encompass a delay in the meal timings and oral hypoglycaemic agent dosages. Errors in the
medication timing, administered dosages, and presence of certain comorbidity increases the
chances of a patient to suffer from hypoglycaemia (Munshi et al. 2016, p.316). The inpatient
staff will be responsible for conveying instruction for medication administration and meal
timings, and encouraging self-care in the patient. This is in accordance to the NSQHS
standards that encompass proper identification of the patient and responding to major clinical
deteriorations in them. Scheduled administration of insulin therapy will also prevent overdose
of the drug and reduce its impacts on lowering blood glucose levels (Sahealth.sa.gov.au
2018). This can be facilitated by adherence to the medication safety and management
standards that works to reduce the occurrence of medication related incidents.
will help to
regain energy
Calorie rich
diet will also
lower
temperature
Part 2
Establishing a balance in the glycemic control by is the key management strategy for
providing optimal care services to the patient Mrs. Anthony. The inpatient team will have to
effectively reduce or prevent hypoglycemic events by 1) identifying the triggering or
precipitating factors; 2) monitoring blood glucose levels at regular intervals; 3) educating the
patient and the staff about the symptoms and suitable treatment; 4) providing nutritional
requirements; and 6) eliminating medication errors. Precipitating and triggering factors
encompass a delay in the meal timings and oral hypoglycaemic agent dosages. Errors in the
medication timing, administered dosages, and presence of certain comorbidity increases the
chances of a patient to suffer from hypoglycaemia (Munshi et al. 2016, p.316). The inpatient
staff will be responsible for conveying instruction for medication administration and meal
timings, and encouraging self-care in the patient. This is in accordance to the NSQHS
standards that encompass proper identification of the patient and responding to major clinical
deteriorations in them. Scheduled administration of insulin therapy will also prevent overdose
of the drug and reduce its impacts on lowering blood glucose levels (Sahealth.sa.gov.au
2018). This can be facilitated by adherence to the medication safety and management
standards that works to reduce the occurrence of medication related incidents.
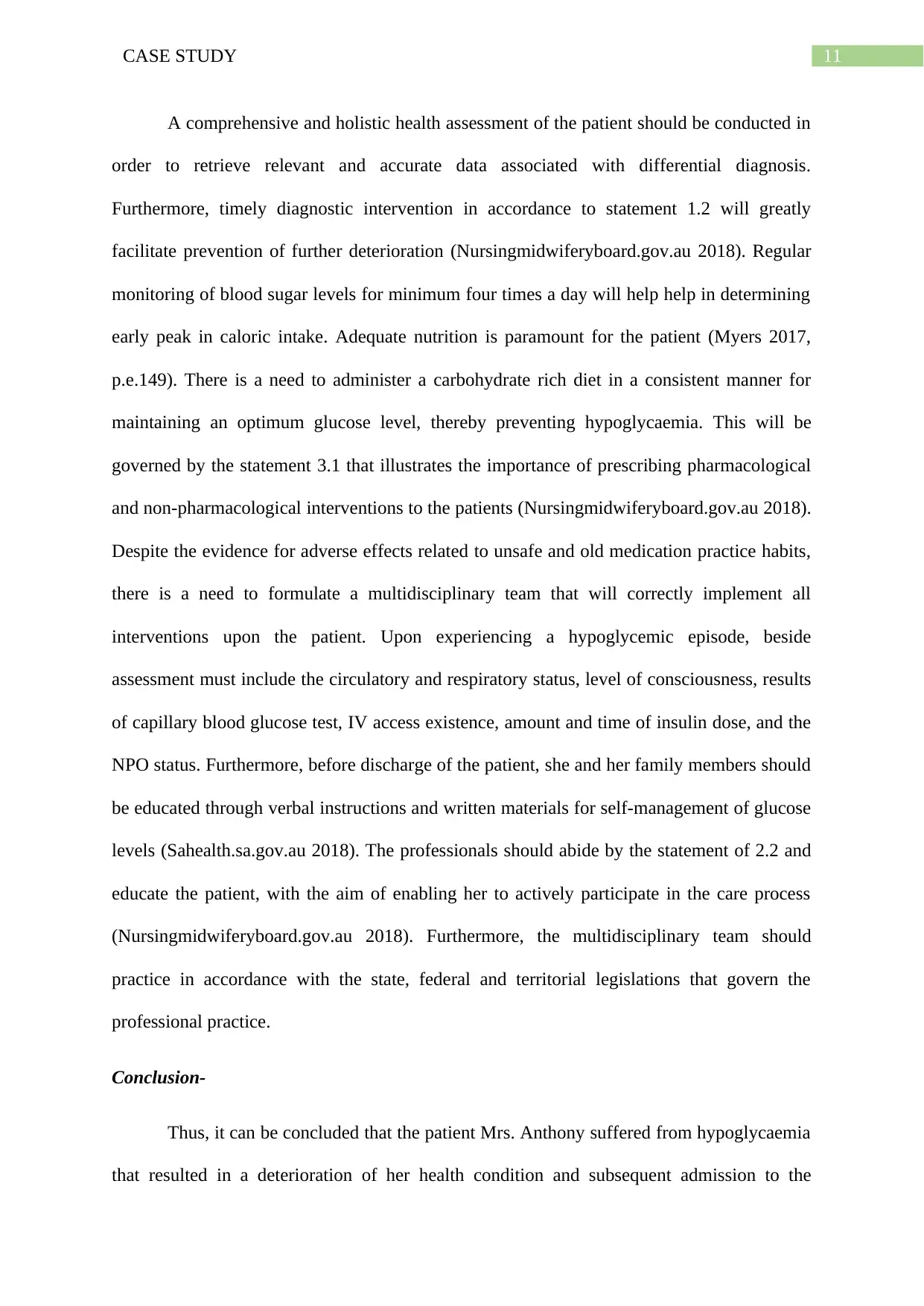
11CASE STUDY
A comprehensive and holistic health assessment of the patient should be conducted in
order to retrieve relevant and accurate data associated with differential diagnosis.
Furthermore, timely diagnostic intervention in accordance to statement 1.2 will greatly
facilitate prevention of further deterioration (Nursingmidwiferyboard.gov.au 2018). Regular
monitoring of blood sugar levels for minimum four times a day will help help in determining
early peak in caloric intake. Adequate nutrition is paramount for the patient (Myers 2017,
p.e.149). There is a need to administer a carbohydrate rich diet in a consistent manner for
maintaining an optimum glucose level, thereby preventing hypoglycaemia. This will be
governed by the statement 3.1 that illustrates the importance of prescribing pharmacological
and non-pharmacological interventions to the patients (Nursingmidwiferyboard.gov.au 2018).
Despite the evidence for adverse effects related to unsafe and old medication practice habits,
there is a need to formulate a multidisciplinary team that will correctly implement all
interventions upon the patient. Upon experiencing a hypoglycemic episode, beside
assessment must include the circulatory and respiratory status, level of consciousness, results
of capillary blood glucose test, IV access existence, amount and time of insulin dose, and the
NPO status. Furthermore, before discharge of the patient, she and her family members should
be educated through verbal instructions and written materials for self-management of glucose
levels (Sahealth.sa.gov.au 2018). The professionals should abide by the statement of 2.2 and
educate the patient, with the aim of enabling her to actively participate in the care process
(Nursingmidwiferyboard.gov.au 2018). Furthermore, the multidisciplinary team should
practice in accordance with the state, federal and territorial legislations that govern the
professional practice.
Conclusion-
Thus, it can be concluded that the patient Mrs. Anthony suffered from hypoglycaemia
that resulted in a deterioration of her health condition and subsequent admission to the
A comprehensive and holistic health assessment of the patient should be conducted in
order to retrieve relevant and accurate data associated with differential diagnosis.
Furthermore, timely diagnostic intervention in accordance to statement 1.2 will greatly
facilitate prevention of further deterioration (Nursingmidwiferyboard.gov.au 2018). Regular
monitoring of blood sugar levels for minimum four times a day will help help in determining
early peak in caloric intake. Adequate nutrition is paramount for the patient (Myers 2017,
p.e.149). There is a need to administer a carbohydrate rich diet in a consistent manner for
maintaining an optimum glucose level, thereby preventing hypoglycaemia. This will be
governed by the statement 3.1 that illustrates the importance of prescribing pharmacological
and non-pharmacological interventions to the patients (Nursingmidwiferyboard.gov.au 2018).
Despite the evidence for adverse effects related to unsafe and old medication practice habits,
there is a need to formulate a multidisciplinary team that will correctly implement all
interventions upon the patient. Upon experiencing a hypoglycemic episode, beside
assessment must include the circulatory and respiratory status, level of consciousness, results
of capillary blood glucose test, IV access existence, amount and time of insulin dose, and the
NPO status. Furthermore, before discharge of the patient, she and her family members should
be educated through verbal instructions and written materials for self-management of glucose
levels (Sahealth.sa.gov.au 2018). The professionals should abide by the statement of 2.2 and
educate the patient, with the aim of enabling her to actively participate in the care process
(Nursingmidwiferyboard.gov.au 2018). Furthermore, the multidisciplinary team should
practice in accordance with the state, federal and territorial legislations that govern the
professional practice.
Conclusion-
Thus, it can be concluded that the patient Mrs. Anthony suffered from hypoglycaemia
that resulted in a deterioration of her health condition and subsequent admission to the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 20
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





