Public Health Project: Immunization Coverage Poster and Reflection
VerifiedAdded on 2023/05/30
|14
|2796
|77
Project
AI Summary
This project focuses on designing a poster and accompanying script to promote immunization coverage rates in Australia, supported by an evidence-based reflective paper. The student has developed a poster and script, providing an overview of immunization coverage, addressing the national targets, and highlighting discrepancies in coverage among different demographics, including Indigenous Australian children. The reflective paper utilizes Rolfe's reflective model to identify the target audience for the poster and script, and the optimal locations for display to maximize impact. The paper analyzes the project's expected outcomes for the target audience and discusses the implications for future practice, considering strategies to address misconceptions, and improve vaccination rates, particularly within Indigenous communities. The project references relevant research and statistics from sources like the Australian Institute of Health and Welfare (AIHW) and the Department of Health, providing a comprehensive analysis of the topic.

Running head: IMMUNIZATION
Immunization
Name of the Student
Name of the University
Author Note
Immunization
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1IMMUNIZATION
Immunization Coverage in Australia:
Evidence based Script for the Poster:
Childhood Immunization Coverage is calculated as the percentage of children who
have received all the vaccines according to their ages as per the National Immunization
Program Schedule (Hu et al. 2015; Gibson et al. 2016). By measuring the immunization
coverage rate it is possible to keep a track of how much the people are protected against
preventable diseases. Vaccinations help the spread of diseases and help to develop ‘herd
immunity’. This type of immunity helps to protect individuals who are not vaccinated (such
as infants), people who cannot be vaccinated for medical conditions and people from whom
the vaccination did not work (Metcalf et al. 2015; Bordon 2017). Australia has a target for
immunization coverage of 95% which can help to develop herd immunity against diseases
such as measles or other diseases that can be prevented through vaccines (health.gov.au
2018a).
According to the Department of Health of the Australian Government, coverage of
immunization for children between the age of one and five years have increased since 2008,
however the target of 95% have not yet been met. As of September, 2018, the national
coverage rates were estimated to be 94.02% for one year old children, 90.63% for two year
old children and 94.62% for five year old children (health.gov.au 2018b). This has been
shown in the diagram below:
Immunization Coverage in Australia:
Evidence based Script for the Poster:
Childhood Immunization Coverage is calculated as the percentage of children who
have received all the vaccines according to their ages as per the National Immunization
Program Schedule (Hu et al. 2015; Gibson et al. 2016). By measuring the immunization
coverage rate it is possible to keep a track of how much the people are protected against
preventable diseases. Vaccinations help the spread of diseases and help to develop ‘herd
immunity’. This type of immunity helps to protect individuals who are not vaccinated (such
as infants), people who cannot be vaccinated for medical conditions and people from whom
the vaccination did not work (Metcalf et al. 2015; Bordon 2017). Australia has a target for
immunization coverage of 95% which can help to develop herd immunity against diseases
such as measles or other diseases that can be prevented through vaccines (health.gov.au
2018a).
According to the Department of Health of the Australian Government, coverage of
immunization for children between the age of one and five years have increased since 2008,
however the target of 95% have not yet been met. As of September, 2018, the national
coverage rates were estimated to be 94.02% for one year old children, 90.63% for two year
old children and 94.62% for five year old children (health.gov.au 2018b). This has been
shown in the diagram below:
2IMMUNIZATION
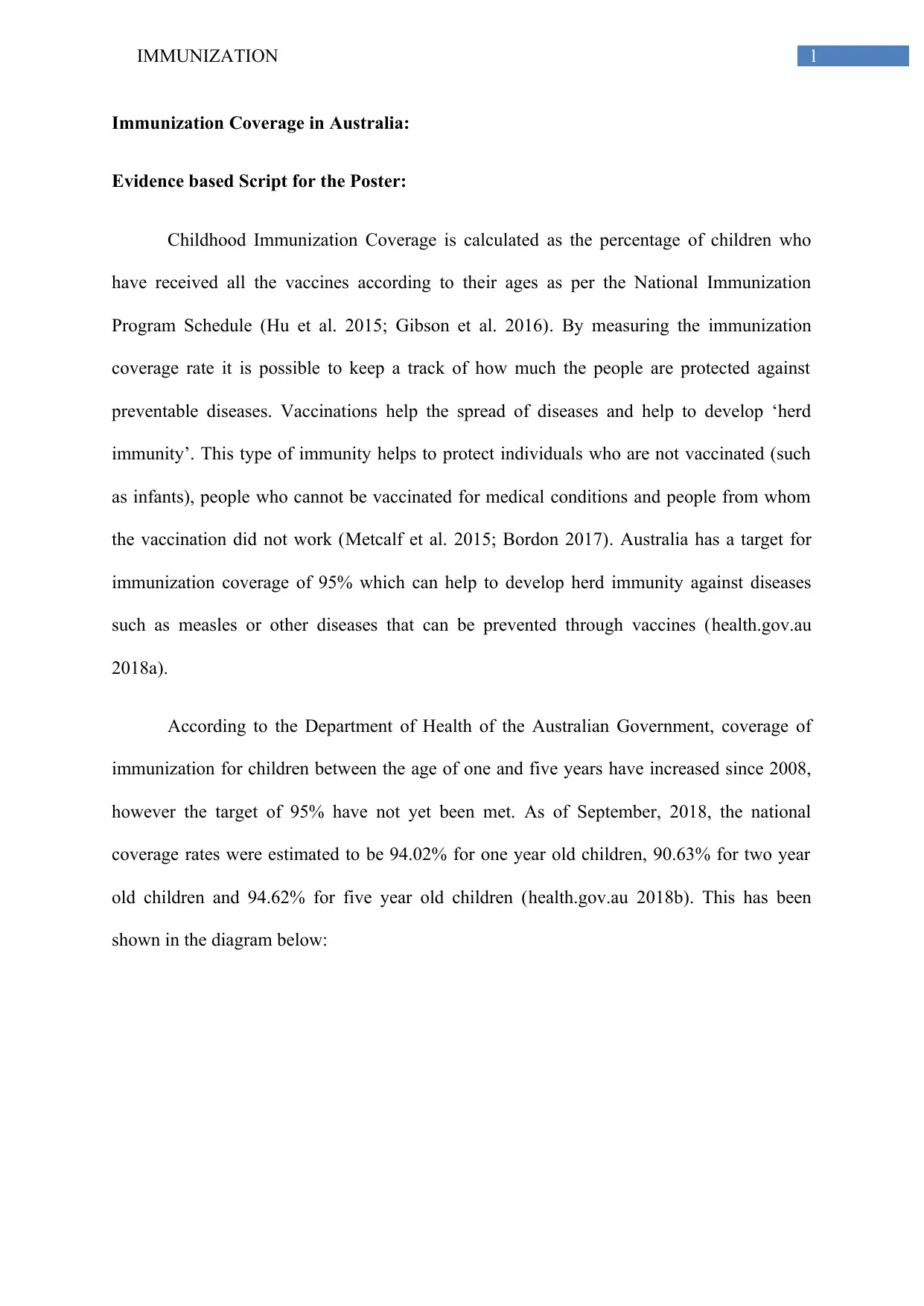
(Figure 1 National Coverage Rates from 2008 to 2018; source: health.gov.au 2018b)
The figure shows that for 1 year olds the immunization rates have significantly
increased since 2008, with major improvements being made between 2008 to 2011 after
which the rate of increase of immunization coverage have declined, while for 2 year olds, the
rates of immunization have slightly reduced since 2008 and immunization coverage of 5 year
olds have remained more or less constant (health.gov.au 2018b).
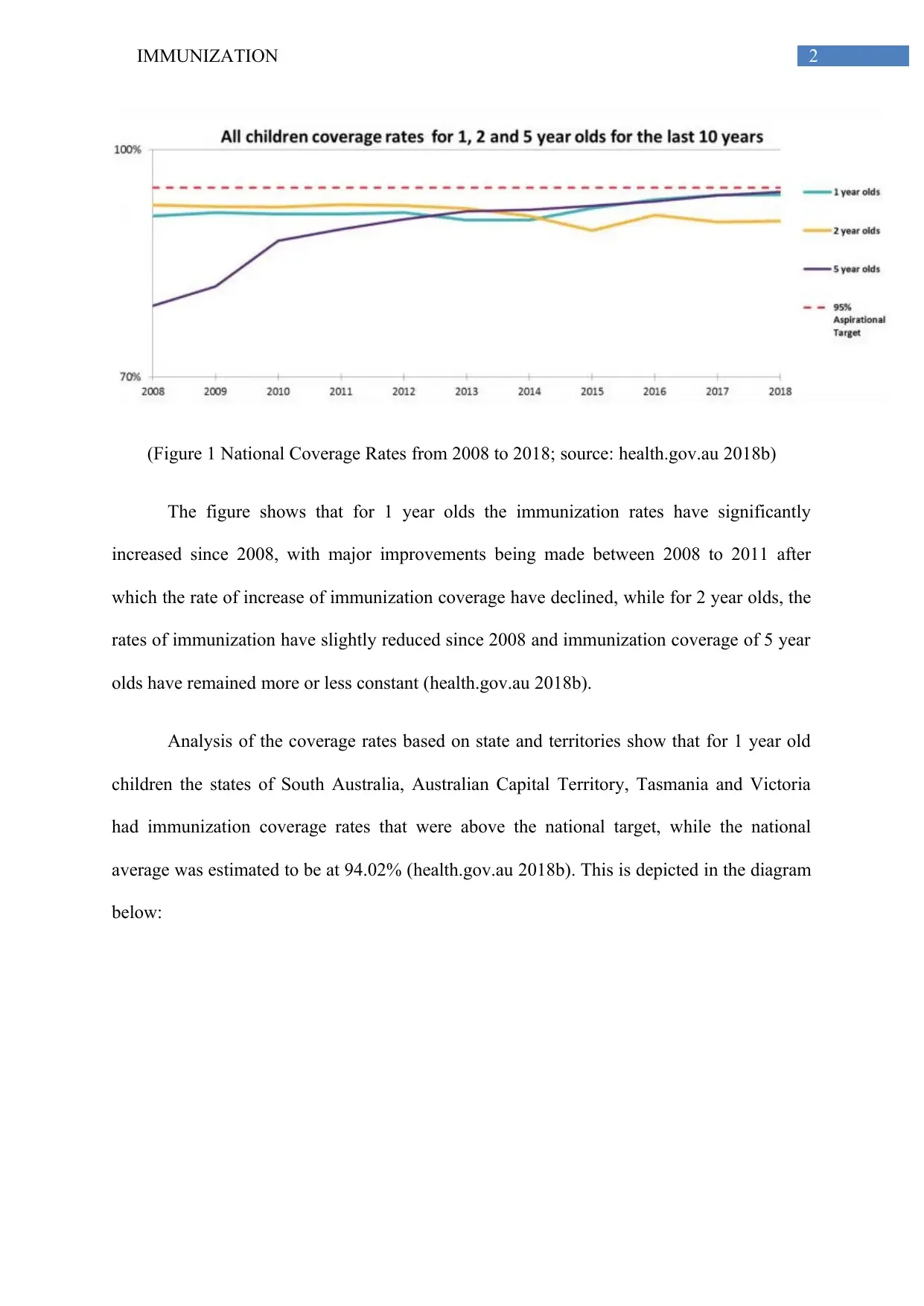
Analysis of the coverage rates based on state and territories show that for 1 year old
children the states of South Australia, Australian Capital Territory, Tasmania and Victoria
had immunization coverage rates that were above the national target, while the national
average was estimated to be at 94.02% (health.gov.au 2018b). This is depicted in the diagram
below:
(Figure 1 National Coverage Rates from 2008 to 2018; source: health.gov.au 2018b)
The figure shows that for 1 year olds the immunization rates have significantly
increased since 2008, with major improvements being made between 2008 to 2011 after
which the rate of increase of immunization coverage have declined, while for 2 year olds, the
rates of immunization have slightly reduced since 2008 and immunization coverage of 5 year
olds have remained more or less constant (health.gov.au 2018b).
Analysis of the coverage rates based on state and territories show that for 1 year old
children the states of South Australia, Australian Capital Territory, Tasmania and Victoria
had immunization coverage rates that were above the national target, while the national
average was estimated to be at 94.02% (health.gov.au 2018b). This is depicted in the diagram
below:
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3IMMUNIZATION
(Figure 2: Coverage rates for 1 year olds. source: health.gov.au 2018b)
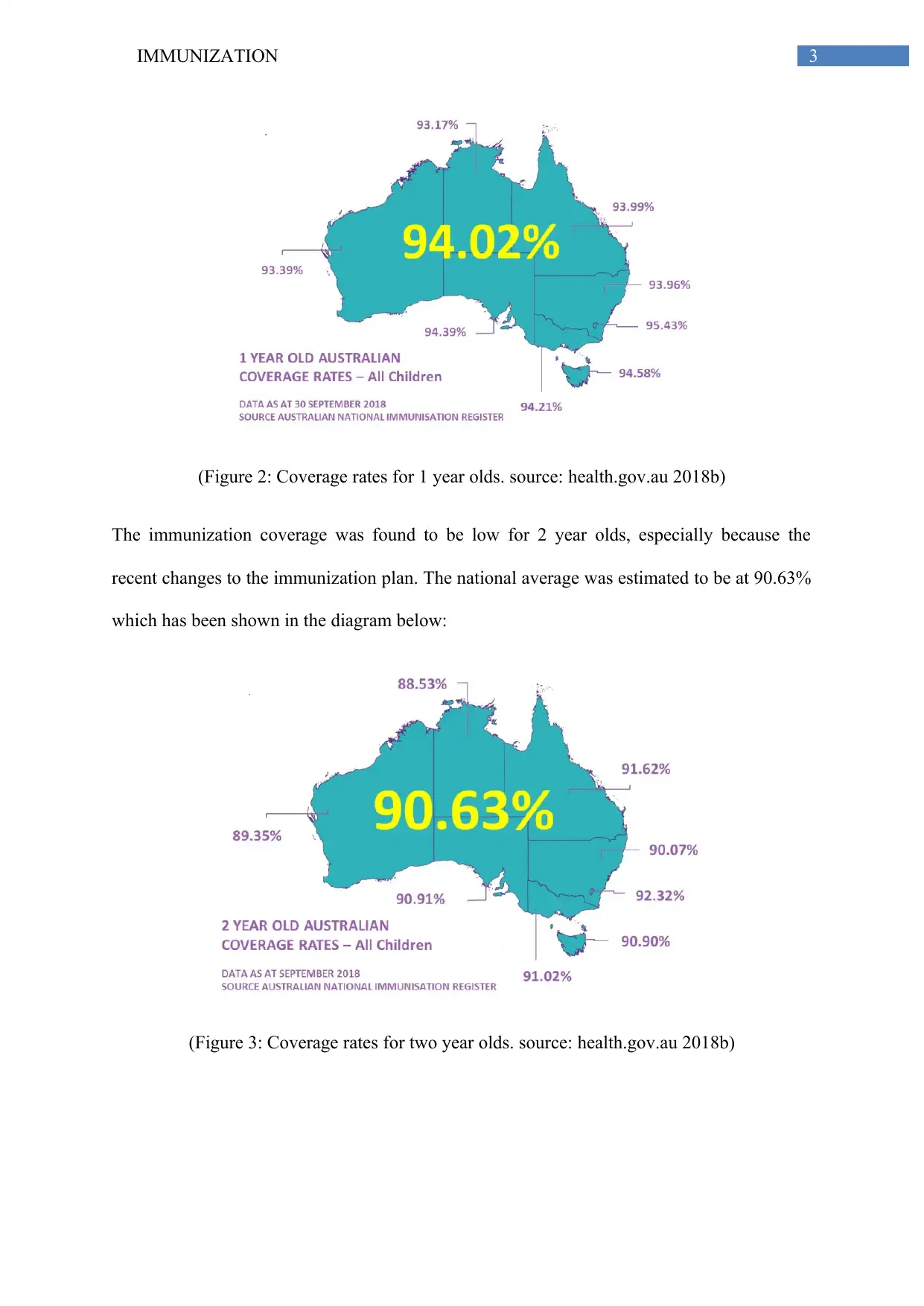
The immunization coverage was found to be low for 2 year olds, especially because the
recent changes to the immunization plan. The national average was estimated to be at 90.63%
which has been shown in the diagram below:
(Figure 3: Coverage rates for two year olds. source: health.gov.au 2018b)
(Figure 2: Coverage rates for 1 year olds. source: health.gov.au 2018b)
The immunization coverage was found to be low for 2 year olds, especially because the
recent changes to the immunization plan. The national average was estimated to be at 90.63%
which has been shown in the diagram below:
(Figure 3: Coverage rates for two year olds. source: health.gov.au 2018b)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4IMMUNIZATION
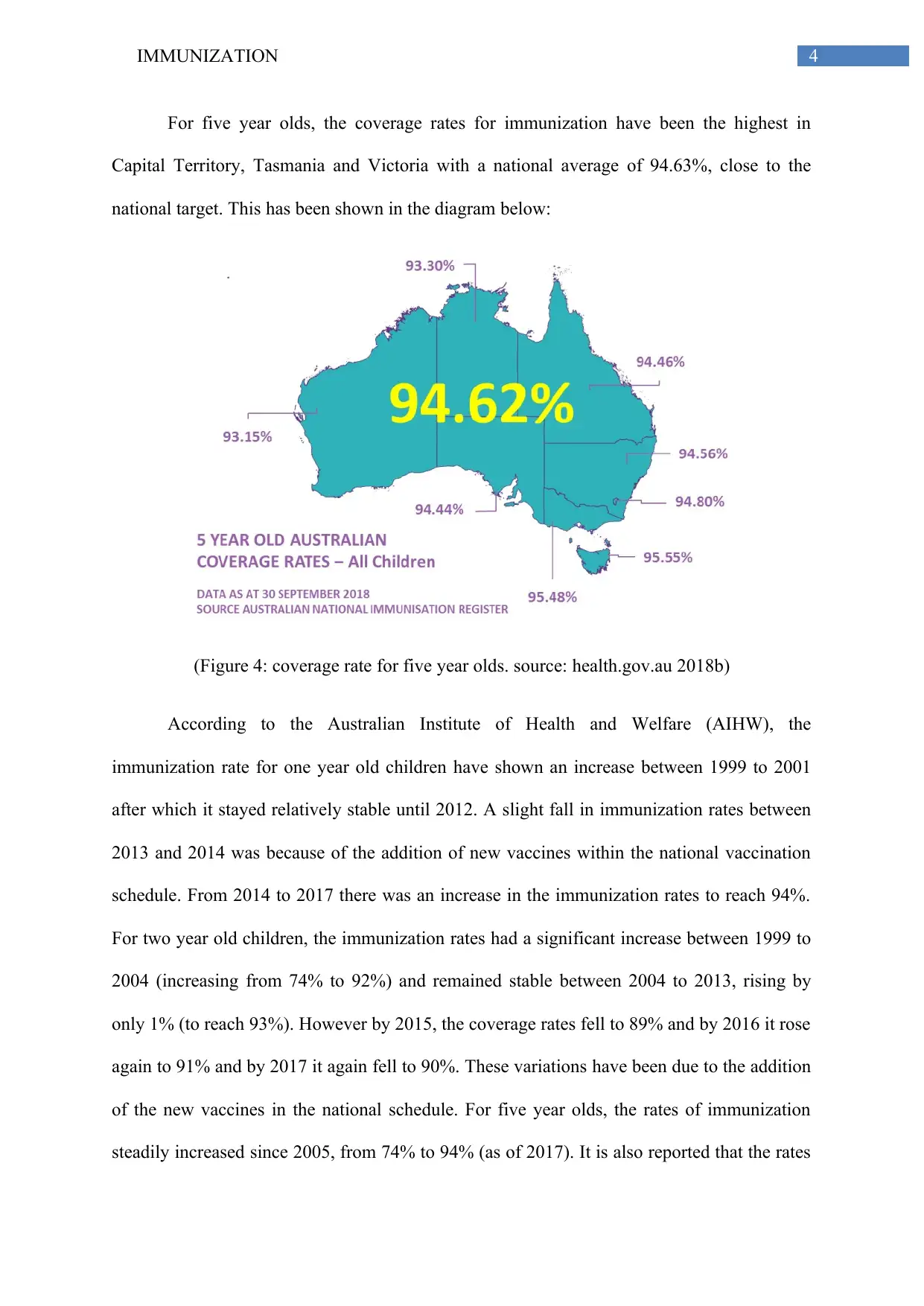
For five year olds, the coverage rates for immunization have been the highest in
Capital Territory, Tasmania and Victoria with a national average of 94.63%, close to the
national target. This has been shown in the diagram below:
(Figure 4: coverage rate for five year olds. source: health.gov.au 2018b)
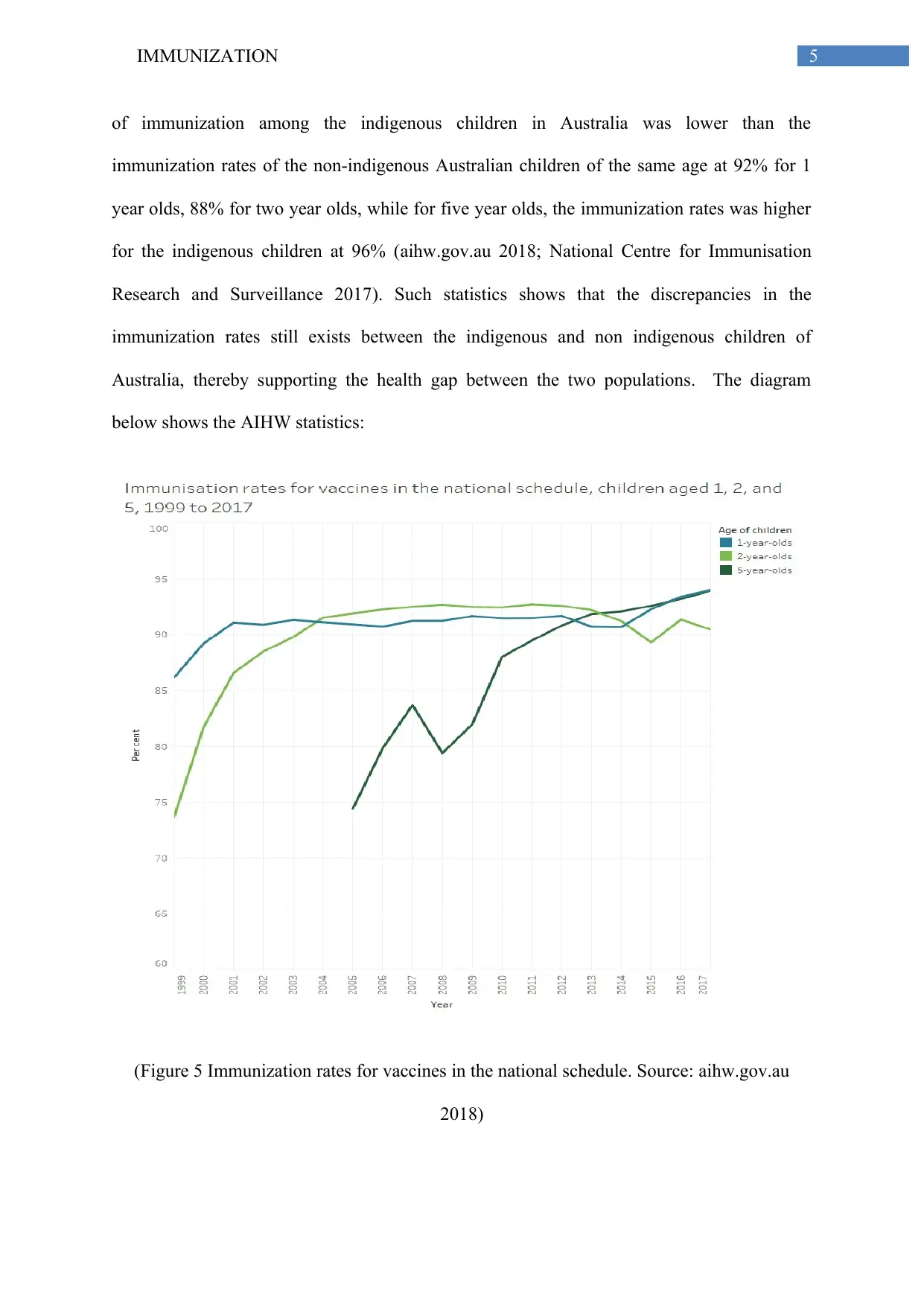
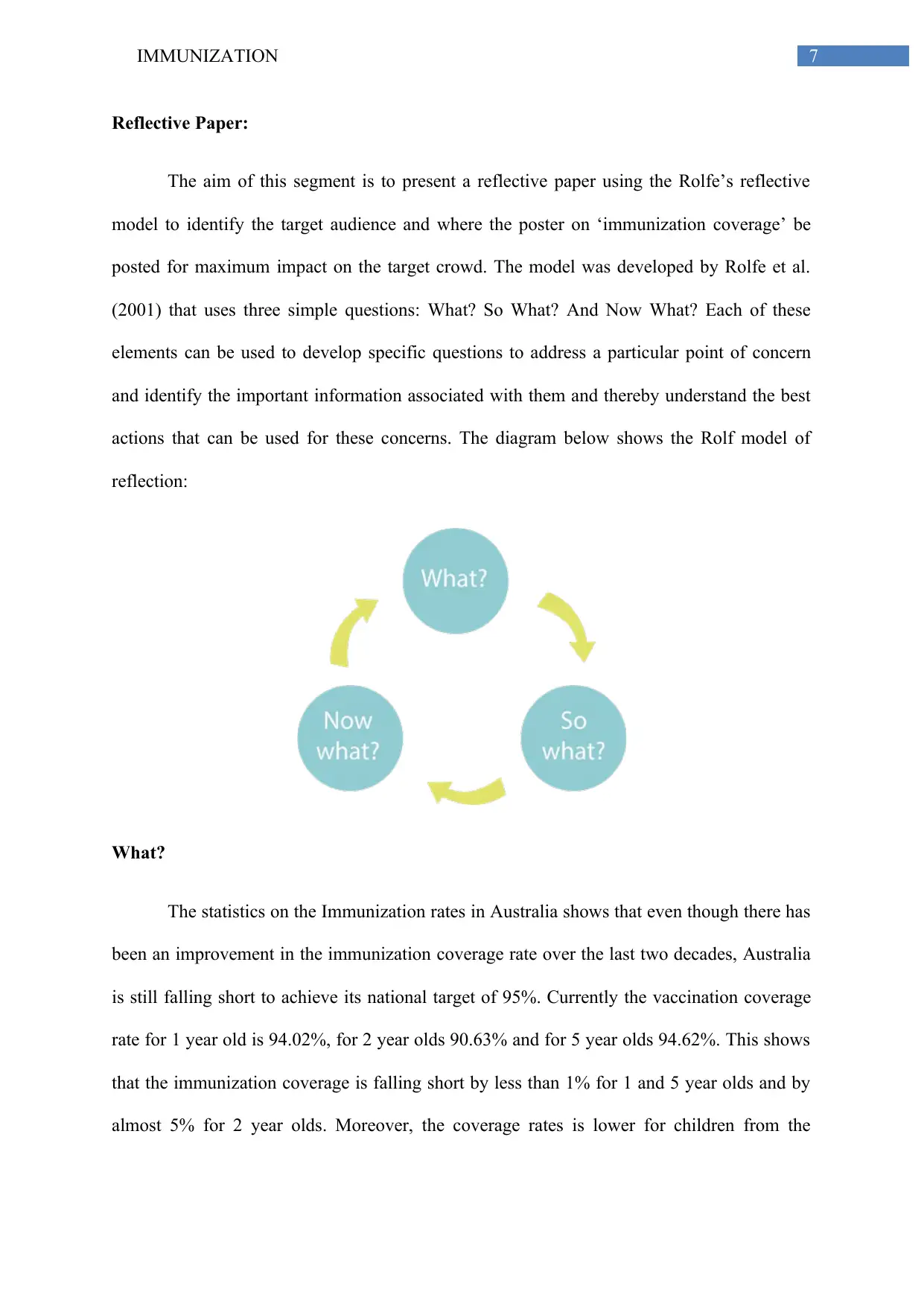
According to the Australian Institute of Health and Welfare (AIHW), the
immunization rate for one year old children have shown an increase between 1999 to 2001
after which it stayed relatively stable until 2012. A slight fall in immunization rates between
2013 and 2014 was because of the addition of new vaccines within the national vaccination
schedule. From 2014 to 2017 there was an increase in the immunization rates to reach 94%.
For two year old children, the immunization rates had a significant increase between 1999 to
2004 (increasing from 74% to 92%) and remained stable between 2004 to 2013, rising by
only 1% (to reach 93%). However by 2015, the coverage rates fell to 89% and by 2016 it rose
again to 91% and by 2017 it again fell to 90%. These variations have been due to the addition
of the new vaccines in the national schedule. For five year olds, the rates of immunization
steadily increased since 2005, from 74% to 94% (as of 2017). It is also reported that the rates
For five year olds, the coverage rates for immunization have been the highest in
Capital Territory, Tasmania and Victoria with a national average of 94.63%, close to the
national target. This has been shown in the diagram below:
(Figure 4: coverage rate for five year olds. source: health.gov.au 2018b)
According to the Australian Institute of Health and Welfare (AIHW), the
immunization rate for one year old children have shown an increase between 1999 to 2001
after which it stayed relatively stable until 2012. A slight fall in immunization rates between
2013 and 2014 was because of the addition of new vaccines within the national vaccination
schedule. From 2014 to 2017 there was an increase in the immunization rates to reach 94%.
For two year old children, the immunization rates had a significant increase between 1999 to
2004 (increasing from 74% to 92%) and remained stable between 2004 to 2013, rising by
only 1% (to reach 93%). However by 2015, the coverage rates fell to 89% and by 2016 it rose
again to 91% and by 2017 it again fell to 90%. These variations have been due to the addition
of the new vaccines in the national schedule. For five year olds, the rates of immunization
steadily increased since 2005, from 74% to 94% (as of 2017). It is also reported that the rates
5IMMUNIZATION
of immunization among the indigenous children in Australia was lower than the
immunization rates of the non-indigenous Australian children of the same age at 92% for 1
year olds, 88% for two year olds, while for five year olds, the immunization rates was higher
for the indigenous children at 96% (aihw.gov.au 2018; National Centre for Immunisation
Research and Surveillance 2017). Such statistics shows that the discrepancies in the
immunization rates still exists between the indigenous and non indigenous children of
Australia, thereby supporting the health gap between the two populations. The diagram
below shows the AIHW statistics:
(Figure 5 Immunization rates for vaccines in the national schedule. Source: aihw.gov.au
2018)
of immunization among the indigenous children in Australia was lower than the
immunization rates of the non-indigenous Australian children of the same age at 92% for 1
year olds, 88% for two year olds, while for five year olds, the immunization rates was higher
for the indigenous children at 96% (aihw.gov.au 2018; National Centre for Immunisation
Research and Surveillance 2017). Such statistics shows that the discrepancies in the
immunization rates still exists between the indigenous and non indigenous children of
Australia, thereby supporting the health gap between the two populations. The diagram
below shows the AIHW statistics:
(Figure 5 Immunization rates for vaccines in the national schedule. Source: aihw.gov.au
2018)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6IMMUNIZATION
Thus from the above data it can be concluded that the immunization rates have
improved in Australia over the last two decades, especially for children of 1 year age.
However, the immunization rates is still lagging behind the national target of 95% which
implies that further improvements are required to reach the target. Additionally, the rates of
immunization have been found to be lower among the Indigenous Australian Children of 1
and 2 years age compared to Non Indigenous children of the same age in Australia which
implies that the immunization in the Indigenous communities needs further improvement.
Thus from the above data it can be concluded that the immunization rates have
improved in Australia over the last two decades, especially for children of 1 year age.
However, the immunization rates is still lagging behind the national target of 95% which
implies that further improvements are required to reach the target. Additionally, the rates of
immunization have been found to be lower among the Indigenous Australian Children of 1
and 2 years age compared to Non Indigenous children of the same age in Australia which
implies that the immunization in the Indigenous communities needs further improvement.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7IMMUNIZATION
Reflective Paper:
The aim of this segment is to present a reflective paper using the Rolfe’s reflective
model to identify the target audience and where the poster on ‘immunization coverage’ be
posted for maximum impact on the target crowd. The model was developed by Rolfe et al.
(2001) that uses three simple questions: What? So What? And Now What? Each of these
elements can be used to develop specific questions to address a particular point of concern
and identify the important information associated with them and thereby understand the best
actions that can be used for these concerns. The diagram below shows the Rolf model of
reflection:
What?
The statistics on the Immunization rates in Australia shows that even though there has
been an improvement in the immunization coverage rate over the last two decades, Australia
is still falling short to achieve its national target of 95%. Currently the vaccination coverage
rate for 1 year old is 94.02%, for 2 year olds 90.63% and for 5 year olds 94.62%. This shows
that the immunization coverage is falling short by less than 1% for 1 and 5 year olds and by
almost 5% for 2 year olds. Moreover, the coverage rates is lower for children from the
Reflective Paper:
The aim of this segment is to present a reflective paper using the Rolfe’s reflective
model to identify the target audience and where the poster on ‘immunization coverage’ be
posted for maximum impact on the target crowd. The model was developed by Rolfe et al.
(2001) that uses three simple questions: What? So What? And Now What? Each of these
elements can be used to develop specific questions to address a particular point of concern
and identify the important information associated with them and thereby understand the best
actions that can be used for these concerns. The diagram below shows the Rolf model of
reflection:
What?
The statistics on the Immunization rates in Australia shows that even though there has
been an improvement in the immunization coverage rate over the last two decades, Australia
is still falling short to achieve its national target of 95%. Currently the vaccination coverage
rate for 1 year old is 94.02%, for 2 year olds 90.63% and for 5 year olds 94.62%. This shows
that the immunization coverage is falling short by less than 1% for 1 and 5 year olds and by
almost 5% for 2 year olds. Moreover, the coverage rates is lower for children from the
8IMMUNIZATION
Indigenous communities in Australia for 1 year (92%) and 2 years old children (88%)
showing an even lower coverage in these communities.
Conducting the study, I was able to understand that the immunization coverage is still
lagging behind, especially within the Indigenous Australian communities. However, for 5
year olds, the immunization rates in the Indigenous have been higher than the national
average and for Non Indigenous Communities it has almost reached the national average. It is
important therefore that the gap in vaccination among the one and two year olds be addressed
soon, both in the indigenous as well as the non indigenous communities so that the coverage
rates for vaccination can reach the national target.
It has been suggested by Taddio et al. (2015) that educating the parents on the
importance of vaccination on the increase of vaccination rates among children as well as for
the management of pain. According to the author, when the parents are informed about the
importance of immunization and how to manage pain experienced by their infants while
vaccination can help them to be more proactive in immunizing their children against the
diseases. Kepka et al. (2015) also pointed out that a lack of understanding about vaccines
(such as the Human Pappiloma Virus) by the parents can lead to a low vaccination for HPV
and therefore increase the risks of these diseases in the community.
So What?
It can be suggested that the poster be targeted for the parents to inform them about the
current vaccination coverage in Australia, the vaccination program. This can impress upon
the parents about the current national trends in vaccination for diseases. Moreover, informing
about the national Vaccination program can improve their knowledge about the various
vaccines needed for their children and therefore adhere to the program in a better manner.
Indigenous communities in Australia for 1 year (92%) and 2 years old children (88%)
showing an even lower coverage in these communities.
Conducting the study, I was able to understand that the immunization coverage is still
lagging behind, especially within the Indigenous Australian communities. However, for 5
year olds, the immunization rates in the Indigenous have been higher than the national
average and for Non Indigenous Communities it has almost reached the national average. It is
important therefore that the gap in vaccination among the one and two year olds be addressed
soon, both in the indigenous as well as the non indigenous communities so that the coverage
rates for vaccination can reach the national target.
It has been suggested by Taddio et al. (2015) that educating the parents on the
importance of vaccination on the increase of vaccination rates among children as well as for
the management of pain. According to the author, when the parents are informed about the
importance of immunization and how to manage pain experienced by their infants while
vaccination can help them to be more proactive in immunizing their children against the
diseases. Kepka et al. (2015) also pointed out that a lack of understanding about vaccines
(such as the Human Pappiloma Virus) by the parents can lead to a low vaccination for HPV
and therefore increase the risks of these diseases in the community.
So What?
It can be suggested that the poster be targeted for the parents to inform them about the
current vaccination coverage in Australia, the vaccination program. This can impress upon
the parents about the current national trends in vaccination for diseases. Moreover, informing
about the national Vaccination program can improve their knowledge about the various
vaccines needed for their children and therefore adhere to the program in a better manner.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9IMMUNIZATION
According to Khan et al. (2015), the knowledge, perceptions and attitudes of the
parents towards vaccines played a significant role in the immunization of children against
polio virus. A misconception among the parents that polio immunization can adversely
impact the health of their children as well as a lack of trust on the healthcare industry have
resulted in lower immunization against polio in Pakistan. This shows how the misconceptions
held by the parents can negatively impact the immunization coverage within the country.
From such study it can be assumed that by improving the understanding of vaccination and
immunization program among the parents can help them overcome such misconceptions and
therefore facilitate the improvement of the immunization coverage. The parents can also be
educated about the consequences of not immunizing the child against the preventable
diseases, and how it can impact the health and wellbeing of the children as well as that of the
community if the vaccines are not given on time. Involvement of the health educators is also
important to facilitate the education of the parents and to help them understand how the
vaccines would safeguard their children against various preventable diseases.
Based on such aspects, I believe that by targeting the parents in the poster, it is
possible to help them understand the importance of the national immunization program, and
how by achieving the national immunization target they can help to protect the health and
wellbeing of not only their children but also other children as well. To ensure best access to
the parents, the posters can be placed on the school notice boards, public places, and school
gates as well as through handouts from the school.
Now What?
In order to further reinforce the success of the immunization coverage, it is also
essential to address the misconceptions and myths about the vaccinations as well as improve
the vaccination rates among the indigenous communities. According to Schmidt (2018)
According to Khan et al. (2015), the knowledge, perceptions and attitudes of the
parents towards vaccines played a significant role in the immunization of children against
polio virus. A misconception among the parents that polio immunization can adversely
impact the health of their children as well as a lack of trust on the healthcare industry have
resulted in lower immunization against polio in Pakistan. This shows how the misconceptions
held by the parents can negatively impact the immunization coverage within the country.
From such study it can be assumed that by improving the understanding of vaccination and
immunization program among the parents can help them overcome such misconceptions and
therefore facilitate the improvement of the immunization coverage. The parents can also be
educated about the consequences of not immunizing the child against the preventable
diseases, and how it can impact the health and wellbeing of the children as well as that of the
community if the vaccines are not given on time. Involvement of the health educators is also
important to facilitate the education of the parents and to help them understand how the
vaccines would safeguard their children against various preventable diseases.
Based on such aspects, I believe that by targeting the parents in the poster, it is
possible to help them understand the importance of the national immunization program, and
how by achieving the national immunization target they can help to protect the health and
wellbeing of not only their children but also other children as well. To ensure best access to
the parents, the posters can be placed on the school notice boards, public places, and school
gates as well as through handouts from the school.
Now What?
In order to further reinforce the success of the immunization coverage, it is also
essential to address the misconceptions and myths about the vaccinations as well as improve
the vaccination rates among the indigenous communities. According to Schmidt (2018)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10IMMUNIZATION
debunking the myths and misconceptions about vaccinations is essential strategy to facilitate
the success of a vaccination program. The World Health Organization have outlined six
common misconceptions about vaccinations such as 1) better sanitation and hygiene have
helped to reduce the incidence of diseases before vaccines were developed and therefore they
are adequate measures to prevent diseases, 2) people who get vaccinated still can get sick and
therefore vaccines are not really effective, 3) there are several vaccines that have caused
adverse health effects and even death, therefore parents do not want their children to be
immunized with those vaccines, 4) vaccines can have several harmful side effects (short term
and long term), 5) rates of vaccine preventable diseases have been drastically reduced in
many countries and therefore such vaccines are not really required, 6) giving multiple
vaccinations for different types of diseases at the same time can greatly increase the risks of
side effects and therefore multiple vaccines are not good (who.int 2018).
These myths reduces the propensity of the parents to immunization their children
against various diseases out of fear for any possible side effects or harmful effects from the
vaccines. It is therefore vital that such myths be debunked in any educational medium
targeted for the parents for them to understand that such information is not correct and to
understand the importance of the vaccines.
debunking the myths and misconceptions about vaccinations is essential strategy to facilitate
the success of a vaccination program. The World Health Organization have outlined six
common misconceptions about vaccinations such as 1) better sanitation and hygiene have
helped to reduce the incidence of diseases before vaccines were developed and therefore they
are adequate measures to prevent diseases, 2) people who get vaccinated still can get sick and
therefore vaccines are not really effective, 3) there are several vaccines that have caused
adverse health effects and even death, therefore parents do not want their children to be
immunized with those vaccines, 4) vaccines can have several harmful side effects (short term
and long term), 5) rates of vaccine preventable diseases have been drastically reduced in
many countries and therefore such vaccines are not really required, 6) giving multiple
vaccinations for different types of diseases at the same time can greatly increase the risks of
side effects and therefore multiple vaccines are not good (who.int 2018).
These myths reduces the propensity of the parents to immunization their children
against various diseases out of fear for any possible side effects or harmful effects from the
vaccines. It is therefore vital that such myths be debunked in any educational medium
targeted for the parents for them to understand that such information is not correct and to
understand the importance of the vaccines.
11IMMUNIZATION
References:
aihw.gov.au (2018). Australia's health 2018, Immunisation rates for vaccines in the national
schedule (children) - Australian Institute of Health and Welfare. [online] Australian Institute
of Health and Welfare. Available at:
https://www.aihw.gov.au/reports/australias-health/australias-health-2018/contents/indicators-
of-australias-health/immunisation-rates-for-vaccines-in-the-national-schedule-children
[Accessed 4 Dec. 2018].
Bordon, Y., 2017. Antibodies: Herd immunity. Nature Reviews Immunology, 17(9), p.530.
Gibson, D.G., Kagucia, E.W., Ochieng, B., Hariharan, N., Obor, D., Moulton, L.H., Winch,
P.J., Levine, O.S., Odhiambo, F., O'Brien, K.L. and Feikin, D.R., 2016. The Mobile Solutions
for Immunization (M-SIMU) Trial: a protocol for a cluster randomized controlled trial that
assesses the impact of mobile phone delivered reminders and travel subsidies to improve
childhood immunization coverage rates and timeliness in western Kenya. JMIR research
protocols, 5(2).
health.gov.au (2018a). Childhood immunisation coverage | Australian Government
Department of Health. [online] Australian Government Department of Health. Available at:
https://beta.health.gov.au/health-topics/immunisation/childhood-immunisation-coverage
[Accessed 4 Dec. 2018].
health.gov.au (2018b). Immunisation coverage rates for all children | Australian Government
Department of Health. [online] Australian Government Department of Health. Available at:
https://beta.health.gov.au/health-topics/immunisation/childhood-immunisation-coverage/
immunisation-coverage-rates-for-all-children [Accessed 4 Dec. 2018].
References:
aihw.gov.au (2018). Australia's health 2018, Immunisation rates for vaccines in the national
schedule (children) - Australian Institute of Health and Welfare. [online] Australian Institute
of Health and Welfare. Available at:
https://www.aihw.gov.au/reports/australias-health/australias-health-2018/contents/indicators-
of-australias-health/immunisation-rates-for-vaccines-in-the-national-schedule-children
[Accessed 4 Dec. 2018].
Bordon, Y., 2017. Antibodies: Herd immunity. Nature Reviews Immunology, 17(9), p.530.
Gibson, D.G., Kagucia, E.W., Ochieng, B., Hariharan, N., Obor, D., Moulton, L.H., Winch,
P.J., Levine, O.S., Odhiambo, F., O'Brien, K.L. and Feikin, D.R., 2016. The Mobile Solutions
for Immunization (M-SIMU) Trial: a protocol for a cluster randomized controlled trial that
assesses the impact of mobile phone delivered reminders and travel subsidies to improve
childhood immunization coverage rates and timeliness in western Kenya. JMIR research
protocols, 5(2).
health.gov.au (2018a). Childhood immunisation coverage | Australian Government
Department of Health. [online] Australian Government Department of Health. Available at:
https://beta.health.gov.au/health-topics/immunisation/childhood-immunisation-coverage
[Accessed 4 Dec. 2018].
health.gov.au (2018b). Immunisation coverage rates for all children | Australian Government
Department of Health. [online] Australian Government Department of Health. Available at:
https://beta.health.gov.au/health-topics/immunisation/childhood-immunisation-coverage/
immunisation-coverage-rates-for-all-children [Accessed 4 Dec. 2018].
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





