Report: Mental Health Staff Attitudes Impact on BPD Patients
VerifiedAdded on 2022/11/26
|28
|7409
|250
Report
AI Summary
This report investigates the impact of mental health staff attitudes on patients diagnosed with Borderline Personality Disorder (BPD). It begins with a comprehensive literature review, defining BPD, exploring its history, characteristics, and prevalence, including a focus on the UK and international contexts. The review examines stigmatization within diagnoses, implications for treatment, and the feelings of mental health professionals towards BPD patients, including gender bias. The methodology section details a systematic review of secondary data, justifying the approach and outlining the planning, execution, and data reporting processes, including search criteria and outcome tables. Data analysis utilizes thematic and content methods. The findings section presents key themes derived from the literature, addressing the research question. The discussion section links findings to relevant theories, particularly Labelling Theory, and explores implications for policy and practice. The report aims to provide a thorough understanding of the complex relationship between staff attitudes and patient outcomes in BPD, offering valuable insights for mental health professionals and researchers.

Impacts of Mental Health Staff Attitudes Towards Patients with BPD 1
IMPACTS OF MENTAL HEALTH STAFF ATTITUDES TOWARDS PATIENTS WITH
BPD
By (Student’s Name)
Professor’s Name
College
Course
Date
IMPACTS OF MENTAL HEALTH STAFF ATTITUDES TOWARDS PATIENTS WITH
BPD
By (Student’s Name)
Professor’s Name
College
Course
Date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Impacts of Mental Health Staff Attitudes Towards Patients with BPD 2
Research question- What impact mental health staff attitudes towards patients with BPD has
on the patients?
Chapter 2: Literature Review
2.1 BDP
2.1.1 Definition
BDP is a mental disorder which impacts the manner in which a person thinks and
feels regarding himself and other people, triggering problems functioning in daily life. BDP
encompasses impulsiveness, distorted self-image, wobbly intense relationship, and extreme
emotions (Day et al. 2018). With BDP, an individual has a strong instability or abandonment
fear, and he might have challenges tolerating loneliness. However, inappropriate anger, often
mood swings and impulsiveness might push other people away, though the person wants to
have lasting and loving relationships. BDP often starts by early adulthood and appears to get
worse in young adulthood as well as might slowly become better as one ages.
2.1.2 History
The phrase “borderline” was initially introduced in the US in the year 1938. It was a
phrase utilized by ancient psychiatrists when describing individuals thought to be on the
“border” between diagnoses, mainly psychosis and neurosis. Then, individuals with neurosis
stood believed to remain treatable, while individuals with psychoses were believed
untreatable. In the 1970s, in-depth comprehension of BDD started to arise. Individuals with
BPD stood described as being extremely emotional, difficult, needy, at high suicidal risk, and
to have a general unstable functioning level. Soon, the symptoms patterns started to surface
describing the people with BPD. The symptoms encompassed rapid swifts from period of
confidence to full despair, unstable self-image, quickly alternating mood swings, fear of
abandonment, firm tendency for both suicidal- and self-harm thought (Dean et al. 2018).
Research question- What impact mental health staff attitudes towards patients with BPD has
on the patients?
Chapter 2: Literature Review
2.1 BDP
2.1.1 Definition
BDP is a mental disorder which impacts the manner in which a person thinks and
feels regarding himself and other people, triggering problems functioning in daily life. BDP
encompasses impulsiveness, distorted self-image, wobbly intense relationship, and extreme
emotions (Day et al. 2018). With BDP, an individual has a strong instability or abandonment
fear, and he might have challenges tolerating loneliness. However, inappropriate anger, often
mood swings and impulsiveness might push other people away, though the person wants to
have lasting and loving relationships. BDP often starts by early adulthood and appears to get
worse in young adulthood as well as might slowly become better as one ages.
2.1.2 History
The phrase “borderline” was initially introduced in the US in the year 1938. It was a
phrase utilized by ancient psychiatrists when describing individuals thought to be on the
“border” between diagnoses, mainly psychosis and neurosis. Then, individuals with neurosis
stood believed to remain treatable, while individuals with psychoses were believed
untreatable. In the 1970s, in-depth comprehension of BDD started to arise. Individuals with
BPD stood described as being extremely emotional, difficult, needy, at high suicidal risk, and
to have a general unstable functioning level. Soon, the symptoms patterns started to surface
describing the people with BPD. The symptoms encompassed rapid swifts from period of
confidence to full despair, unstable self-image, quickly alternating mood swings, fear of
abandonment, firm tendency for both suicidal- and self-harm thought (Dean et al. 2018).
Impacts of Mental Health Staff Attitudes Towards Patients with BPD 3
In 1980s, BPD emerged as official personality disorder in DSM-III. Today, much is
known regarding the condition. The phrase “neurosis” is not utilized in diagnostic system,
while BPD is not thought to be psychotic condition. Presently, BPD is acknowledged as a
disorder featuring intense emotional experiences alongside instability in relationships with
the behavior which starts in early adulthood and displays itself in various settings. Experts
have further recognized a firm genetic constituent to BPD- implying it can run in families
(Dickens, Hallett and Lamont 2016).
2.1.3 Characteristics of BDP
There are nine commonly known characteristics of BDP. The first characteristics is
frantic efforts of the person to evade imagined or real abandonment. Another characteristic is
a trend of unstable as well as intense interpersonal relationship featuring alternating extremes
of devaluation and idealization (Dickens, Lamont and Gray 2016). BDG is also characterized
by identity disturbance with remarkably as well as persistently unstable sense of self or self-
image. It is also featuring impulsivity in at minimum 2 areas which stay possibly self-
damaging, for instance binge eating, irresponsible driving, and sex, expenditure and drug
abuse. Recurrent suicidal gestures, behavior, threats as well as self-mutilating behavior
(SMB) is also common (Dickens et al. 2019). Another feature is affective instability because
of a marked mood reactivity like intense episodic irritability, anxiety, or dysphonia often
taking some hours and seldom beyond 5 days. BPD is also characterized by chronic
emptiness feeling and inappropriate, difficulty controlling anger or penetrating anger plus
recurrent manifestation of temper, recurring physical fights or constant anger. Another
feature of BPD is momentary, stress-linked distrustful ideation or even serious dissociative
symptoms.
2.2 Patients with BDP in the UK
In 1980s, BPD emerged as official personality disorder in DSM-III. Today, much is
known regarding the condition. The phrase “neurosis” is not utilized in diagnostic system,
while BPD is not thought to be psychotic condition. Presently, BPD is acknowledged as a
disorder featuring intense emotional experiences alongside instability in relationships with
the behavior which starts in early adulthood and displays itself in various settings. Experts
have further recognized a firm genetic constituent to BPD- implying it can run in families
(Dickens, Hallett and Lamont 2016).
2.1.3 Characteristics of BDP
There are nine commonly known characteristics of BDP. The first characteristics is
frantic efforts of the person to evade imagined or real abandonment. Another characteristic is
a trend of unstable as well as intense interpersonal relationship featuring alternating extremes
of devaluation and idealization (Dickens, Lamont and Gray 2016). BDG is also characterized
by identity disturbance with remarkably as well as persistently unstable sense of self or self-
image. It is also featuring impulsivity in at minimum 2 areas which stay possibly self-
damaging, for instance binge eating, irresponsible driving, and sex, expenditure and drug
abuse. Recurrent suicidal gestures, behavior, threats as well as self-mutilating behavior
(SMB) is also common (Dickens et al. 2019). Another feature is affective instability because
of a marked mood reactivity like intense episodic irritability, anxiety, or dysphonia often
taking some hours and seldom beyond 5 days. BPD is also characterized by chronic
emptiness feeling and inappropriate, difficulty controlling anger or penetrating anger plus
recurrent manifestation of temper, recurring physical fights or constant anger. Another
feature of BPD is momentary, stress-linked distrustful ideation or even serious dissociative
symptoms.
2.2 Patients with BDP in the UK
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Impacts of Mental Health Staff Attitudes Towards Patients with BPD 4
BPD affects a great number of people in the UK. It is common amongst the adulthood
especially the young adults.
2.3 Patients with BDP in the rest of the word – Example of USA/Italia/New Zealand
BPD is common in both general population alongside clinical contexts. The ratio of
females to make with BPD stays greater in clinical population than it is in general population
in the US. Nonetheless, lifetime BPD prevalence does not significantly differ in the US
between males and females. In the United States, latest study has indicated that 1.60 percent
of population suffer from BPD. Women stay far more probable to be diagnosed with BPD as
opposed to me with nearly 75 percent of individuals diagnosed being women (3:1) (Ebrahim
et al. 2016).
2.4 Stigmatization attitudes in Mental Health (MH) staff towards patients with BDP
2.4.1 Stigma within the diagnoses
There is a stigma within diagnoses in regards to BPD. It is common that BPD stigma
is gender-bias within diagnosis. Literature shows that BPD remains significantly in women
with ratio of 7:1 woman to man ratio in people with BPD. The DSM-IV-TR (2000) states that
75% percent of persons diagnosed with BPD remain females (Haynos et al. 2016).
2.4.2 Implication of the BDP diagnostics in treatment
Besides the stigma linked to BPD diagnosis, implications linked to such a diagnostic
label for treatment alongside engagement within systems exist. It is discovered that females
diagnosed with BPD remain usually regarded within communal systems as unstable
emotionally and extra probable than the people undiagnosed with it to become
institutionalized hence forcing treatment, losing potential rights as well as never considered
credible witness in instances engaging sexual abuse. BPD biased diagnosis has implications
on treatment type resulting to the clinical context and attitudes have towards patients based
on every diagnosis (Jones and Wright 2017).
BPD affects a great number of people in the UK. It is common amongst the adulthood
especially the young adults.
2.3 Patients with BDP in the rest of the word – Example of USA/Italia/New Zealand
BPD is common in both general population alongside clinical contexts. The ratio of
females to make with BPD stays greater in clinical population than it is in general population
in the US. Nonetheless, lifetime BPD prevalence does not significantly differ in the US
between males and females. In the United States, latest study has indicated that 1.60 percent
of population suffer from BPD. Women stay far more probable to be diagnosed with BPD as
opposed to me with nearly 75 percent of individuals diagnosed being women (3:1) (Ebrahim
et al. 2016).
2.4 Stigmatization attitudes in Mental Health (MH) staff towards patients with BDP
2.4.1 Stigma within the diagnoses
There is a stigma within diagnoses in regards to BPD. It is common that BPD stigma
is gender-bias within diagnosis. Literature shows that BPD remains significantly in women
with ratio of 7:1 woman to man ratio in people with BPD. The DSM-IV-TR (2000) states that
75% percent of persons diagnosed with BPD remain females (Haynos et al. 2016).
2.4.2 Implication of the BDP diagnostics in treatment
Besides the stigma linked to BPD diagnosis, implications linked to such a diagnostic
label for treatment alongside engagement within systems exist. It is discovered that females
diagnosed with BPD remain usually regarded within communal systems as unstable
emotionally and extra probable than the people undiagnosed with it to become
institutionalized hence forcing treatment, losing potential rights as well as never considered
credible witness in instances engaging sexual abuse. BPD biased diagnosis has implications
on treatment type resulting to the clinical context and attitudes have towards patients based
on every diagnosis (Jones and Wright 2017).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Impacts of Mental Health Staff Attitudes Towards Patients with BPD 5
2.4.3 Mental health professional feelings towards patients
Researchers have examined attitudes held by professionals towards BPD patients and
discovered that 89 percent of nurses surveyed perceived BPD patients as manipulative, 38 %
viewing them as nuisance and 32 percent make them angry. Other studies have shown that
nurses view BPD patients as responsible for their individual suicidal actions (Keuroghlian et
al. 2016.).
2.4.4 Gender Bias in the diagnosis of BPD
Studies show a biased diagnosis of BPD with females being diagnosed more than
males. However, some studies have shown no significant differences in gender diagnosis
(Knaak, Mantler and Szeto 2017).
2.5 Conclusion
The review of literature has demonstrated existence of negative attitude towards the
people with BPD which not only affects the diagnosis, but also treatment of people with BPD
(Walthall 2013).
Chapter 3: Methodology
3.1 Justification
The systematic review of secondary data is the research method used in this study.
The rationale is that secondary data is gathered without the need for fieldwork. It allows for
collection of both quantitative and qualitative information already gathered in previous
studies on this topic (Johnston 2017). This systematic review has the greatest advantage of
cost-effective and time-saving. The information published in the initial studies can be quickly
and freely be retrieved from the internet and credible databases. The data is clean, reliable,
valid and accessible in several formats including electronic thus the retriever and reviewer
can easily gather useful information (Johnson 2017).
2.4.3 Mental health professional feelings towards patients
Researchers have examined attitudes held by professionals towards BPD patients and
discovered that 89 percent of nurses surveyed perceived BPD patients as manipulative, 38 %
viewing them as nuisance and 32 percent make them angry. Other studies have shown that
nurses view BPD patients as responsible for their individual suicidal actions (Keuroghlian et
al. 2016.).
2.4.4 Gender Bias in the diagnosis of BPD
Studies show a biased diagnosis of BPD with females being diagnosed more than
males. However, some studies have shown no significant differences in gender diagnosis
(Knaak, Mantler and Szeto 2017).
2.5 Conclusion
The review of literature has demonstrated existence of negative attitude towards the
people with BPD which not only affects the diagnosis, but also treatment of people with BPD
(Walthall 2013).
Chapter 3: Methodology
3.1 Justification
The systematic review of secondary data is the research method used in this study.
The rationale is that secondary data is gathered without the need for fieldwork. It allows for
collection of both quantitative and qualitative information already gathered in previous
studies on this topic (Johnston 2017). This systematic review has the greatest advantage of
cost-effective and time-saving. The information published in the initial studies can be quickly
and freely be retrieved from the internet and credible databases. The data is clean, reliable,
valid and accessible in several formats including electronic thus the retriever and reviewer
can easily gather useful information (Johnson 2017).
Impacts of Mental Health Staff Attitudes Towards Patients with BPD 6
Systematic review of secondary data is also advantageous since it has follows high
level of professional and expertise. The sources are peer-reviewed journals and this makes
them credible, valid and reliable sources of information (Walthall 2013). The data is retrieved
only from credible databases including public database which allows the researcher to access
an array of statistical records from essential organizations. Academic researchers or scholars
have spent enough time, energy and funds working on these resources thereby making
credible information (Johnston 2017).
The data is also viable, reliable, and valid since they have undergone re-examination
by external reviewers before being published. However, the researcher will only include up-
to-date sources, especially those published between 2015 and 2019 to avoid the risk of using
obsolete information. The data will only be included when it is peer-reviewed and the
credibility of the authors are ascertained. Moreover, the data will only be drawn from credible
databases. All these inclusion and exclusion criteria will help filter the data to guarantee
credibility, validity, reliability, and trustworthiness.
Systematic review of secondary data is also advantageous since it has follows high
level of professional and expertise. The sources are peer-reviewed journals and this makes
them credible, valid and reliable sources of information (Walthall 2013). The data is retrieved
only from credible databases including public database which allows the researcher to access
an array of statistical records from essential organizations. Academic researchers or scholars
have spent enough time, energy and funds working on these resources thereby making
credible information (Johnston 2017).
The data is also viable, reliable, and valid since they have undergone re-examination
by external reviewers before being published. However, the researcher will only include up-
to-date sources, especially those published between 2015 and 2019 to avoid the risk of using
obsolete information. The data will only be included when it is peer-reviewed and the
credibility of the authors are ascertained. Moreover, the data will only be drawn from credible
databases. All these inclusion and exclusion criteria will help filter the data to guarantee
credibility, validity, reliability, and trustworthiness.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Impacts of Mental Health Staff Attitudes Towards Patients with BPD 7
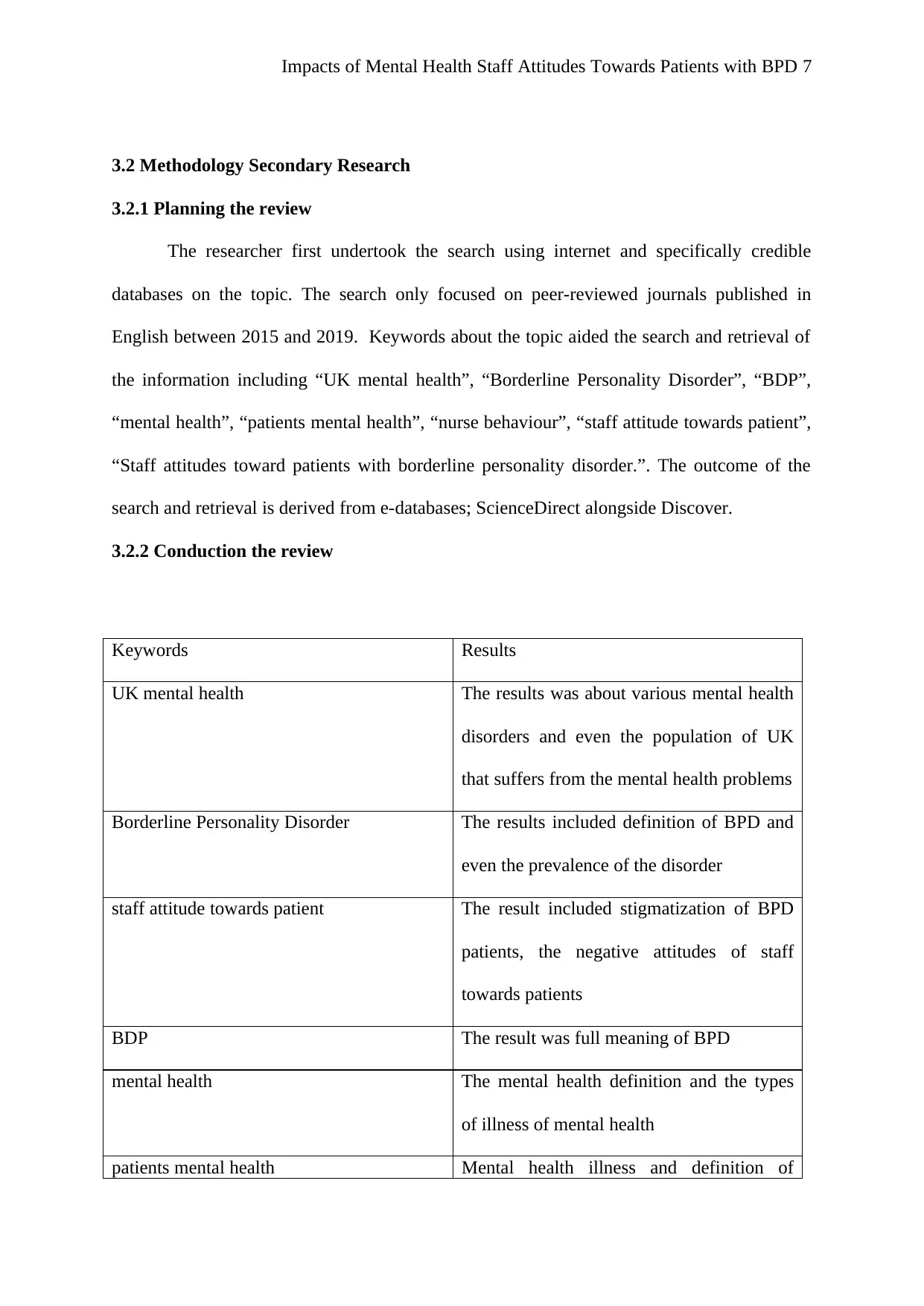
3.2 Methodology Secondary Research
3.2.1 Planning the review
The researcher first undertook the search using internet and specifically credible
databases on the topic. The search only focused on peer-reviewed journals published in
English between 2015 and 2019. Keywords about the topic aided the search and retrieval of
the information including “UK mental health”, “Borderline Personality Disorder”, “BDP”,
“mental health”, “patients mental health”, “nurse behaviour”, “staff attitude towards patient”,
“Staff attitudes toward patients with borderline personality disorder.”. The outcome of the
search and retrieval is derived from e-databases; ScienceDirect alongside Discover.
3.2.2 Conduction the review
Keywords Results
UK mental health The results was about various mental health
disorders and even the population of UK
that suffers from the mental health problems
Borderline Personality Disorder The results included definition of BPD and
even the prevalence of the disorder
staff attitude towards patient The result included stigmatization of BPD
patients, the negative attitudes of staff
towards patients
BDP The result was full meaning of BPD
mental health The mental health definition and the types
of illness of mental health
patients mental health Mental health illness and definition of
3.2 Methodology Secondary Research
3.2.1 Planning the review
The researcher first undertook the search using internet and specifically credible
databases on the topic. The search only focused on peer-reviewed journals published in
English between 2015 and 2019. Keywords about the topic aided the search and retrieval of
the information including “UK mental health”, “Borderline Personality Disorder”, “BDP”,
“mental health”, “patients mental health”, “nurse behaviour”, “staff attitude towards patient”,
“Staff attitudes toward patients with borderline personality disorder.”. The outcome of the
search and retrieval is derived from e-databases; ScienceDirect alongside Discover.
3.2.2 Conduction the review
Keywords Results
UK mental health The results was about various mental health
disorders and even the population of UK
that suffers from the mental health problems
Borderline Personality Disorder The results included definition of BPD and
even the prevalence of the disorder
staff attitude towards patient The result included stigmatization of BPD
patients, the negative attitudes of staff
towards patients
BDP The result was full meaning of BPD
mental health The mental health definition and the types
of illness of mental health
patients mental health Mental health illness and definition of
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Impacts of Mental Health Staff Attitudes Towards Patients with BPD 8
mental health
nurse behaviour Definition of nurse behavior
staff attitude towards patient Staff attitudes patients; negative and
positive attitudes of staff
Staff attitudes toward patients with
borderline personality disorder
Stigmatization, effects of staff attitudes,
negative and positive attitudes
Table 1: Search criteria outcome in staff attitudes toward patients with BPD
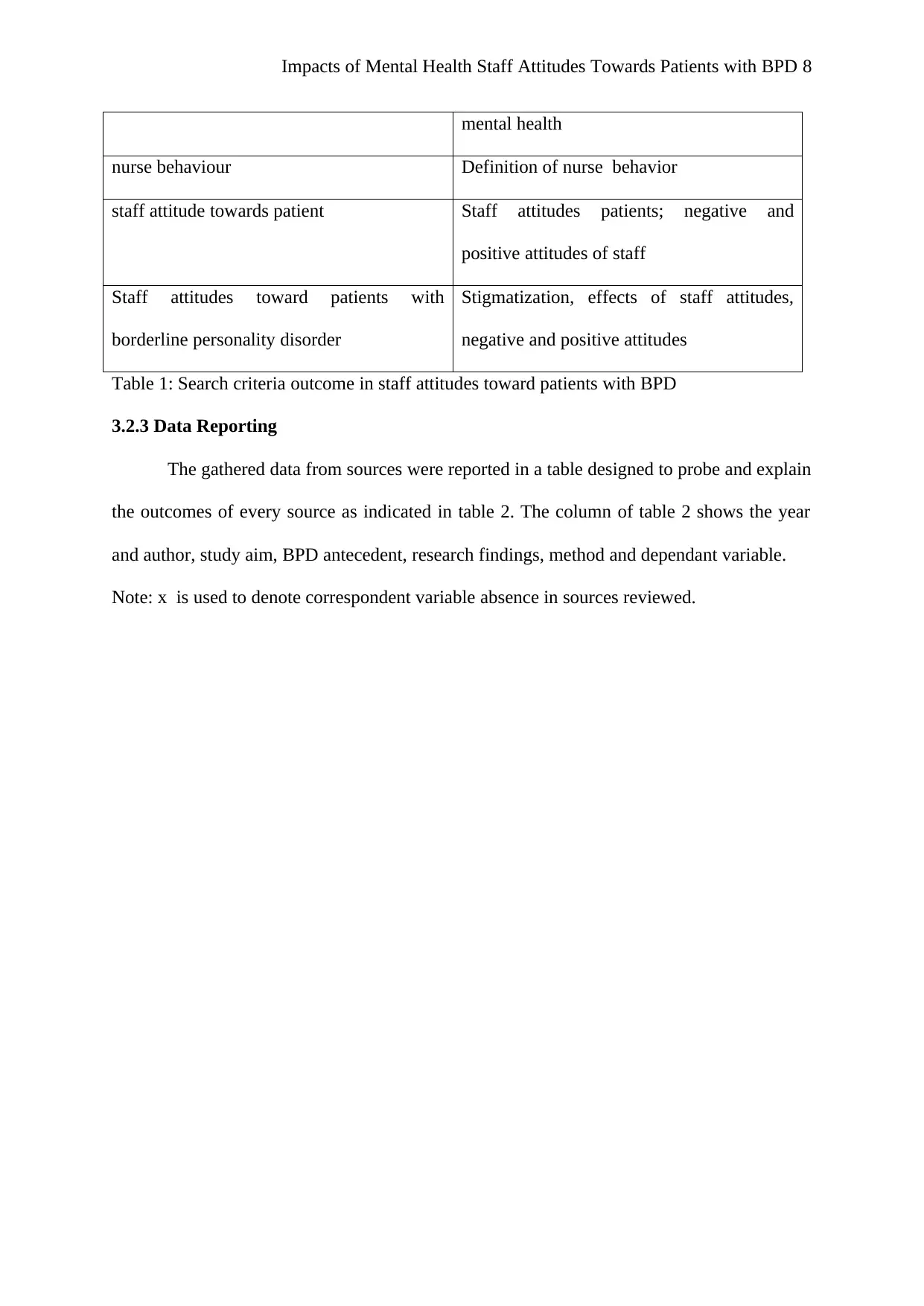
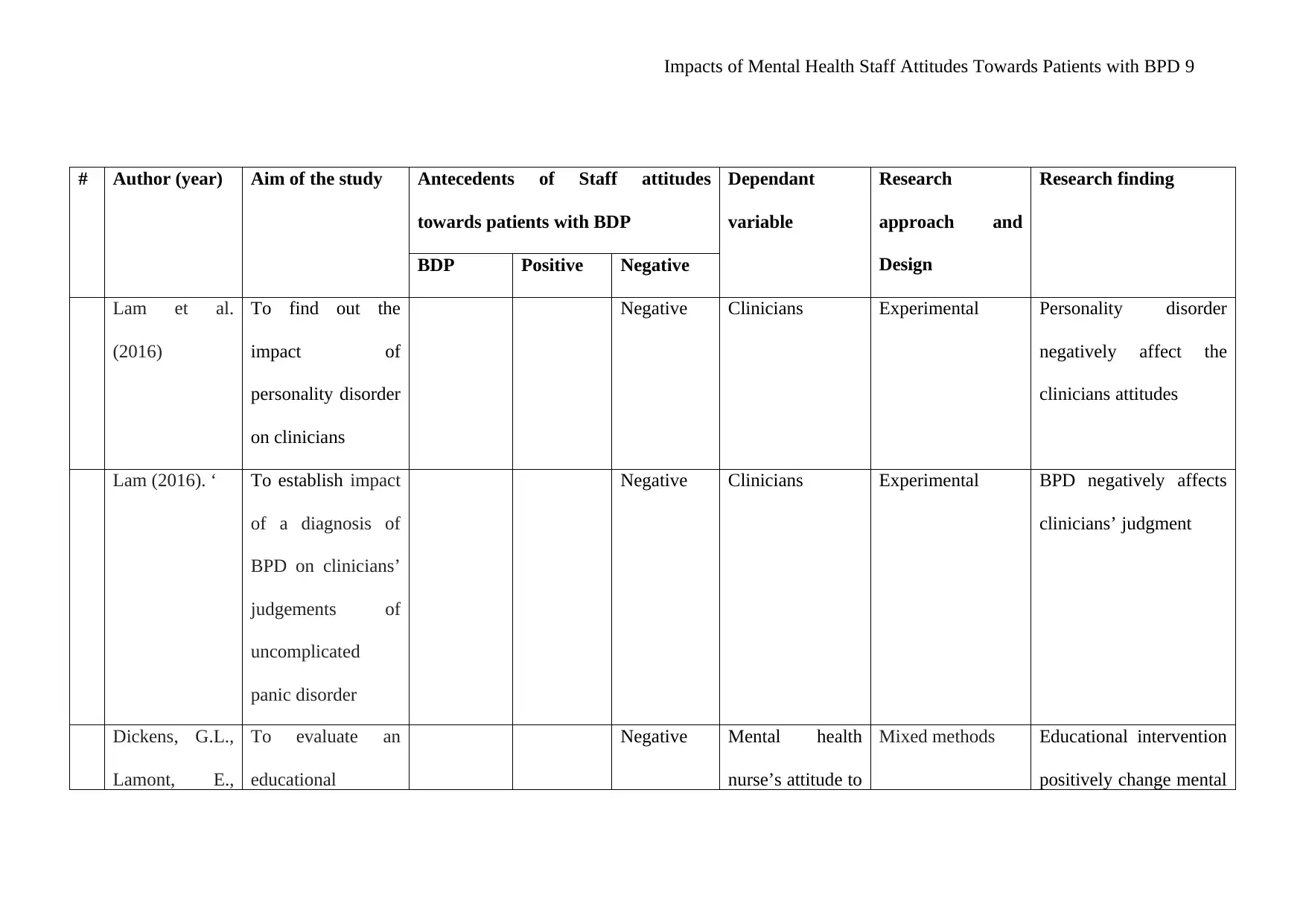
3.2.3 Data Reporting
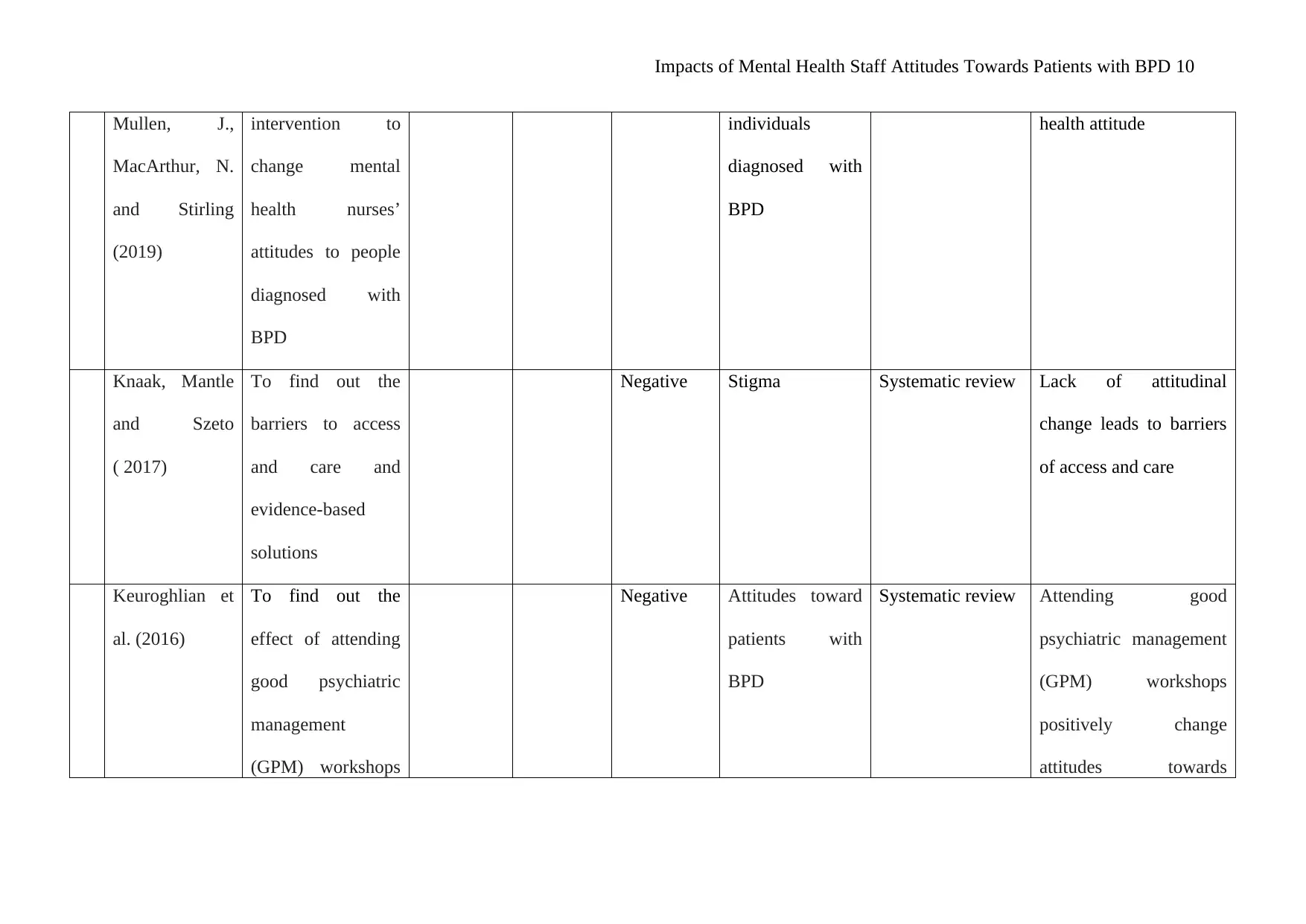
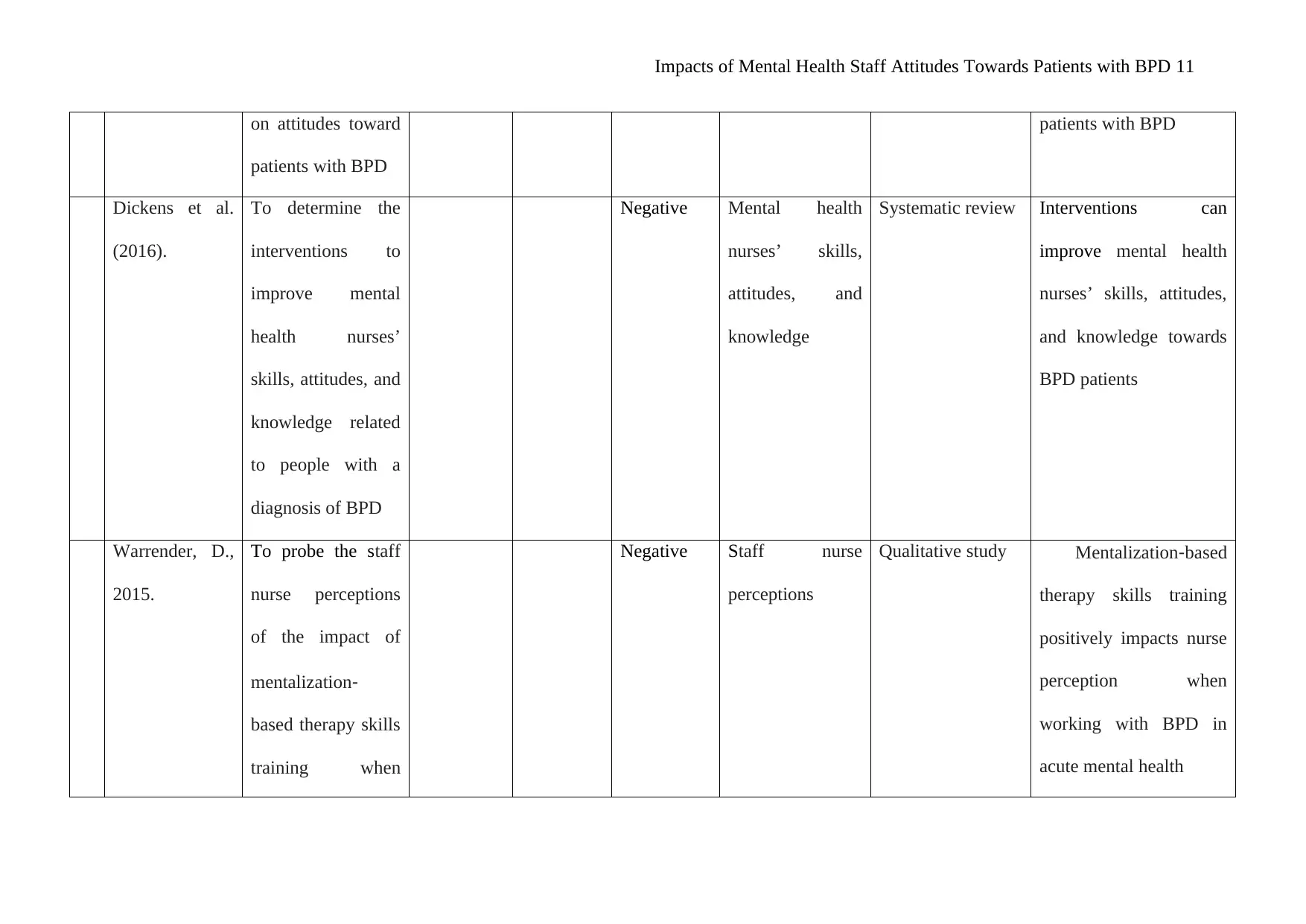
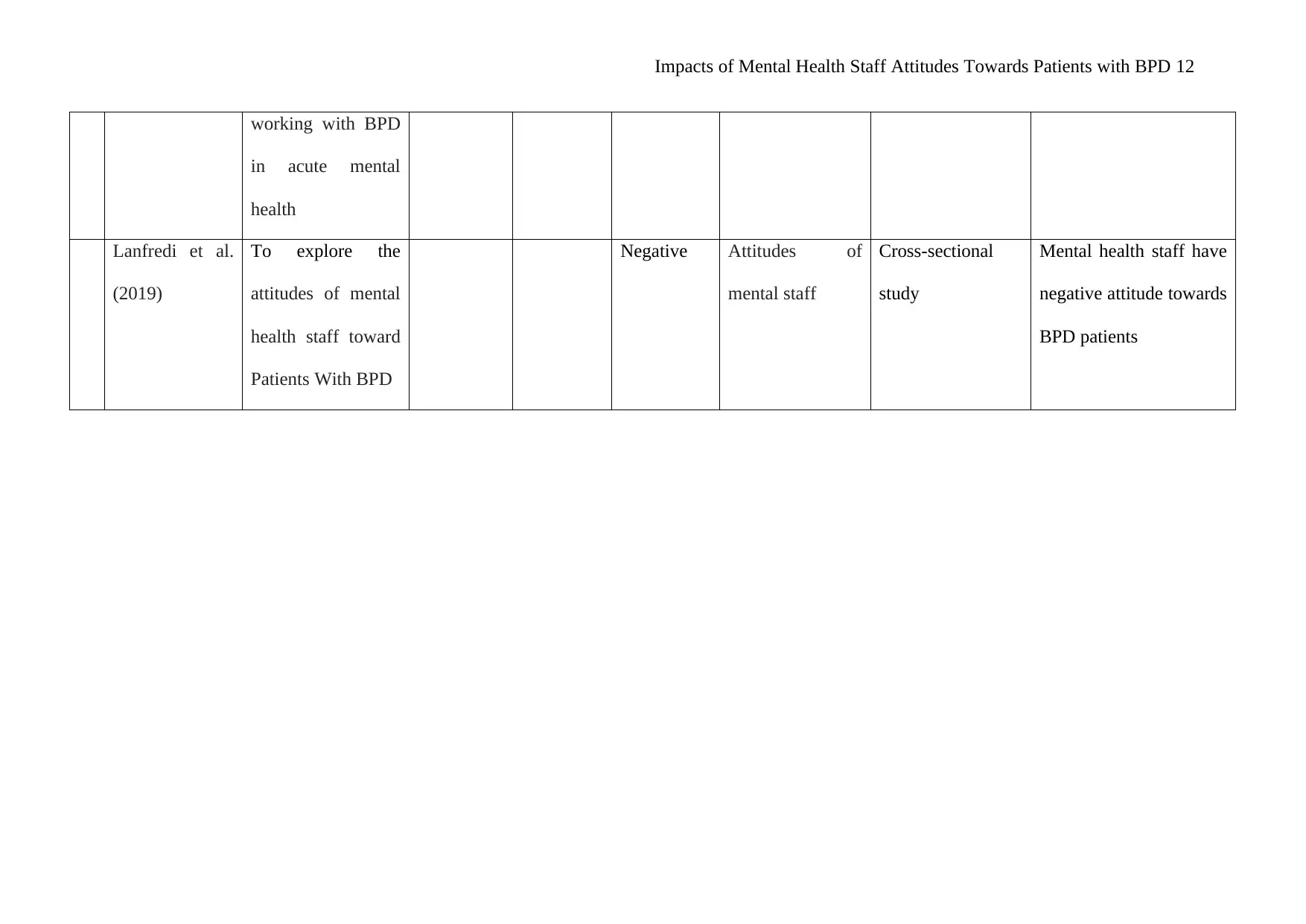
The gathered data from sources were reported in a table designed to probe and explain
the outcomes of every source as indicated in table 2. The column of table 2 shows the year
and author, study aim, BPD antecedent, research findings, method and dependant variable.
Note: x is used to denote correspondent variable absence in sources reviewed.
mental health
nurse behaviour Definition of nurse behavior
staff attitude towards patient Staff attitudes patients; negative and
positive attitudes of staff
Staff attitudes toward patients with
borderline personality disorder
Stigmatization, effects of staff attitudes,
negative and positive attitudes
Table 1: Search criteria outcome in staff attitudes toward patients with BPD
3.2.3 Data Reporting
The gathered data from sources were reported in a table designed to probe and explain
the outcomes of every source as indicated in table 2. The column of table 2 shows the year
and author, study aim, BPD antecedent, research findings, method and dependant variable.
Note: x is used to denote correspondent variable absence in sources reviewed.
Impacts of Mental Health Staff Attitudes Towards Patients with BPD 9
# Author (year) Aim of the study Antecedents of Staff attitudes
towards patients with BDP
Dependant
variable
Research
approach and
Design
Research finding
BDP Positive Negative
Lam et al.
(2016)
To find out the
impact of
personality disorder
on clinicians
Negative Clinicians Experimental Personality disorder
negatively affect the
clinicians attitudes
Lam (2016). ‘ To establish impact
of a diagnosis of
BPD on clinicians’
judgements of
uncomplicated
panic disorder
Negative Clinicians Experimental BPD negatively affects
clinicians’ judgment
Dickens, G.L.,
Lamont, E.,
To evaluate an
educational
Negative Mental health
nurse’s attitude to
Mixed methods Educational intervention
positively change mental
# Author (year) Aim of the study Antecedents of Staff attitudes
towards patients with BDP
Dependant
variable
Research
approach and
Design
Research finding
BDP Positive Negative
Lam et al.
(2016)
To find out the
impact of
personality disorder
on clinicians
Negative Clinicians Experimental Personality disorder
negatively affect the
clinicians attitudes
Lam (2016). ‘ To establish impact
of a diagnosis of
BPD on clinicians’
judgements of
uncomplicated
panic disorder
Negative Clinicians Experimental BPD negatively affects
clinicians’ judgment
Dickens, G.L.,
Lamont, E.,
To evaluate an
educational
Negative Mental health
nurse’s attitude to
Mixed methods Educational intervention
positively change mental
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Impacts of Mental Health Staff Attitudes Towards Patients with BPD 10
Mullen, J.,
MacArthur, N.
and Stirling
(2019)
intervention to
change mental
health nurses’
attitudes to people
diagnosed with
BPD
individuals
diagnosed with
BPD
health attitude
Knaak, Mantle
and Szeto
( 2017)
To find out the
barriers to access
and care and
evidence-based
solutions
Negative Stigma Systematic review Lack of attitudinal
change leads to barriers
of access and care
Keuroghlian et
al. (2016)
To find out the
effect of attending
good psychiatric
management
(GPM) workshops
Negative Attitudes toward
patients with
BPD
Systematic review Attending good
psychiatric management
(GPM) workshops
positively change
attitudes towards
Mullen, J.,
MacArthur, N.
and Stirling
(2019)
intervention to
change mental
health nurses’
attitudes to people
diagnosed with
BPD
individuals
diagnosed with
BPD
health attitude
Knaak, Mantle
and Szeto
( 2017)
To find out the
barriers to access
and care and
evidence-based
solutions
Negative Stigma Systematic review Lack of attitudinal
change leads to barriers
of access and care
Keuroghlian et
al. (2016)
To find out the
effect of attending
good psychiatric
management
(GPM) workshops
Negative Attitudes toward
patients with
BPD
Systematic review Attending good
psychiatric management
(GPM) workshops
positively change
attitudes towards
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Impacts of Mental Health Staff Attitudes Towards Patients with BPD 11
on attitudes toward
patients with BPD
patients with BPD
Dickens et al.
(2016).
To determine the
interventions to
improve mental
health nurses’
skills, attitudes, and
knowledge related
to people with a
diagnosis of BPD
Negative Mental health
nurses’ skills,
attitudes, and
knowledge
Systematic review Interventions can
improve mental health
nurses’ skills, attitudes,
and knowledge towards
BPD patients
Warrender, D.,
2015.
To probe the staff
nurse perceptions
of the impact of
mentalization‐
based therapy skills
training when
Negative Staff nurse
perceptions
Qualitative study Mentalization‐based
therapy skills training
positively impacts nurse
perception when
working with BPD in
acute mental health
on attitudes toward
patients with BPD
patients with BPD
Dickens et al.
(2016).
To determine the
interventions to
improve mental
health nurses’
skills, attitudes, and
knowledge related
to people with a
diagnosis of BPD
Negative Mental health
nurses’ skills,
attitudes, and
knowledge
Systematic review Interventions can
improve mental health
nurses’ skills, attitudes,
and knowledge towards
BPD patients
Warrender, D.,
2015.
To probe the staff
nurse perceptions
of the impact of
mentalization‐
based therapy skills
training when
Negative Staff nurse
perceptions
Qualitative study Mentalization‐based
therapy skills training
positively impacts nurse
perception when
working with BPD in
acute mental health
Impacts of Mental Health Staff Attitudes Towards Patients with BPD 12
working with BPD
in acute mental
health
Lanfredi et al.
(2019)
To explore the
attitudes of mental
health staff toward
Patients With BPD
Negative Attitudes of
mental staff
Cross-sectional
study
Mental health staff have
negative attitude towards
BPD patients
working with BPD
in acute mental
health
Lanfredi et al.
(2019)
To explore the
attitudes of mental
health staff toward
Patients With BPD
Negative Attitudes of
mental staff
Cross-sectional
study
Mental health staff have
negative attitude towards
BPD patients
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 28
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




