Implementation of a Practice Development Tool
VerifiedAdded on 2023/01/20
|11
|2504
|92
AI Summary
This article discusses the implementation of a practice development tool in healthcare settings to enhance collaboration and communication among healthcare professionals. It explores the use of the SCARF practice development tool and its impact on patient care. The article also provides an action plan and timeline for implementing the tool.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: IMPLEMENTATION OF A PRACTICE DEVELOPMENT TOOL
IMPLEMENTATION OF A PRACTICE DEVELOPMENT TOOL
Name of Student
Name of University
Author note
IMPLEMENTATION OF A PRACTICE DEVELOPMENT TOOL
Name of Student
Name of University
Author note
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1IMPLEMENTATION OF PRACTICE DEVELOPMENT TOOL
In an ideal healthcare setup, different healthcare disciplines comes together to impart
an experiential treatment to each of its clients (patients) through an excellent functional
collaboration of various teams. In the literal, day to day practice – the scenario is completely
different though and does not always lives up to the best practice norms. Claims, concerns
and issues is a crucial form of medical management best practice (Waring et al., 2016) which
helps in procuring positive and negative statements from the practitioners involved in a
typical patient- care process like handover or in-hospital medical diagnoses. These feedbacks
from everyone regarding the on-going medical process can enhance the practice ethics and
practice environment in a high paced patient care scenario. Critically ill patients are often
prescribed with a lot of neuro –imaging, radiological and cardiovascular procedures, very
much within the short span of time. The attending nurse has to take the unstable patient on
the stretcher to many diagnostic departments in the same day. Communication gap (Huston et
al., 2018) , high patient pressure, long cue and even a ‘patient knowledge’ gap between the
attending nurse who probably knows the best about the concerned patient and the technicians
or doctors who is about to diagnose the patient, who knows very less. Knowledge gap(Malik,
McKenna & Plummer, 2015) between the doctors and nurse is another roadblock to practice.
‘Knowledge transfer’ during the ‘handover’ process is often done vaguely and sketchily
because of a time issue or communication gap between the healthcare disciplines. The
medical technologists and technicians are often very myopic about their practice for the bias
developed towards repetitive cases but this can be potentially dangerous to a patient with
certain severe complications which needs to be managed. Here, the SCARF practice
development tool can come handy to better the treatment environment, communication and
situation. SCARF stands for Status, Certainty, Autonomy, relatedness and Fairness and it
becomes a highly important tool to be applied to the above mentioned practice issue (Jager et
al., 2017). Autonomy (Putturaj & Prashanth, 2017) is the first thing control phenomena that
In an ideal healthcare setup, different healthcare disciplines comes together to impart
an experiential treatment to each of its clients (patients) through an excellent functional
collaboration of various teams. In the literal, day to day practice – the scenario is completely
different though and does not always lives up to the best practice norms. Claims, concerns
and issues is a crucial form of medical management best practice (Waring et al., 2016) which
helps in procuring positive and negative statements from the practitioners involved in a
typical patient- care process like handover or in-hospital medical diagnoses. These feedbacks
from everyone regarding the on-going medical process can enhance the practice ethics and
practice environment in a high paced patient care scenario. Critically ill patients are often
prescribed with a lot of neuro –imaging, radiological and cardiovascular procedures, very
much within the short span of time. The attending nurse has to take the unstable patient on
the stretcher to many diagnostic departments in the same day. Communication gap (Huston et
al., 2018) , high patient pressure, long cue and even a ‘patient knowledge’ gap between the
attending nurse who probably knows the best about the concerned patient and the technicians
or doctors who is about to diagnose the patient, who knows very less. Knowledge gap(Malik,
McKenna & Plummer, 2015) between the doctors and nurse is another roadblock to practice.
‘Knowledge transfer’ during the ‘handover’ process is often done vaguely and sketchily
because of a time issue or communication gap between the healthcare disciplines. The
medical technologists and technicians are often very myopic about their practice for the bias
developed towards repetitive cases but this can be potentially dangerous to a patient with
certain severe complications which needs to be managed. Here, the SCARF practice
development tool can come handy to better the treatment environment, communication and
situation. SCARF stands for Status, Certainty, Autonomy, relatedness and Fairness and it
becomes a highly important tool to be applied to the above mentioned practice issue (Jager et
al., 2017). Autonomy (Putturaj & Prashanth, 2017) is the first thing control phenomena that
2IMPLEMENTATION OF PRACTICE DEVELOPMENT TOOL
comes from the individual and is a vital ‘sub-tool’ of SCARF which lays the first managerial
control over the co-practitioners, the nurse is working with – doctors, allied health
practitioners like medical therapists, medical technologists , other nurses. It is to be noted that
not always needs to be hierarchical but it can also mean great communication and self-
management skills directed to a collaborative patient centered care with a high functionality
ratio. The SCARF response is based on reward or threat response (Weinberg et al., 2016)
within a collaborative medical care and in this case, the social equation of the attending nurse
with other healthcare professionals somewhere affects the care given her patient by other
professionals. This is where ‘relatedness’ and ‘fairness’ (Freedman, 2019) of the SCARF
practice tool comes to play. Relatedness is dependent on approach- avoidance psychology
(Ferris et al., 2016) which is a factorial of perception, judgment and experiences – it is a form
of behavior that can form or break a potential interpersonal relationship. This very collective
behavioral mechanism is critical which incorporating relatedness (based on interpersonal
similarity or differences) and fairness (judgment) in a practice environment. In medical
practices, a general hierarchy is prevalent everywhere which brings in the ‘status’ factor into
play which modifies and affects a conversation during handover in a great way. It is to be
understood that the nurse’s interpersonal social skills and management would affect the
patient care directly. Certainty (of SCARF practice tool) focusses on the patterning and
predicting a successful outcome while planning for a practice development.
The plan of action should be extensive and targeted profoundly to a collaborative
process between nurses and technologists chiefly and this collaboration should be directed
towards an all-important critical patient care. The issue ‘handover’ is to be managed and the
practice change can be bought by good means of interdisciplinary qualitative communication
(Stubbe, 2017), ‘information’ or ‘patient knowledge transfer’, planning, autonomy,
situational analysis (Amini et al., 2016) and clinical judgment (Ignatavicius & Workman,
comes from the individual and is a vital ‘sub-tool’ of SCARF which lays the first managerial
control over the co-practitioners, the nurse is working with – doctors, allied health
practitioners like medical therapists, medical technologists , other nurses. It is to be noted that
not always needs to be hierarchical but it can also mean great communication and self-
management skills directed to a collaborative patient centered care with a high functionality
ratio. The SCARF response is based on reward or threat response (Weinberg et al., 2016)
within a collaborative medical care and in this case, the social equation of the attending nurse
with other healthcare professionals somewhere affects the care given her patient by other
professionals. This is where ‘relatedness’ and ‘fairness’ (Freedman, 2019) of the SCARF
practice tool comes to play. Relatedness is dependent on approach- avoidance psychology
(Ferris et al., 2016) which is a factorial of perception, judgment and experiences – it is a form
of behavior that can form or break a potential interpersonal relationship. This very collective
behavioral mechanism is critical which incorporating relatedness (based on interpersonal
similarity or differences) and fairness (judgment) in a practice environment. In medical
practices, a general hierarchy is prevalent everywhere which brings in the ‘status’ factor into
play which modifies and affects a conversation during handover in a great way. It is to be
understood that the nurse’s interpersonal social skills and management would affect the
patient care directly. Certainty (of SCARF practice tool) focusses on the patterning and
predicting a successful outcome while planning for a practice development.
The plan of action should be extensive and targeted profoundly to a collaborative
process between nurses and technologists chiefly and this collaboration should be directed
towards an all-important critical patient care. The issue ‘handover’ is to be managed and the
practice change can be bought by good means of interdisciplinary qualitative communication
(Stubbe, 2017), ‘information’ or ‘patient knowledge transfer’, planning, autonomy,
situational analysis (Amini et al., 2016) and clinical judgment (Ignatavicius & Workman,
3IMPLEMENTATION OF PRACTICE DEVELOPMENT TOOL
2015). Hence, the SCARF model is to be incorporated with a pre implementation check with
PRAXIS evaluation. Based on the findings and feedbacks, the SCARF tool needs to be
designed according to a treatment and precisely, patient need. Once the mentioned practice
development tool is in the system, the PRAXIS can be used again to measure the
functionality of the model and what changes needs to be made. Specificity to a patient and
the bio –medical care required for the case requires is important to quality and alter the
practice environments for a hassle free ‘handover’ process. Carrying the important
information (patient files) with the patient is vital for supporting the verbal patient
information transferred during patient handover. The practice development tool should be
bought to practice by a joint consensus of all the multi- disciplinary specialists, participating
in the practice of it. A shared decision making with the patient and a collaborative decision
making with members of other disciplines is vital to develop a patient centered ‘handover’
process and patient centered care. The application of the above mentioned practice tool
should qualify the parameters of specificity, measurable, achievable, reasonable (logical) and
time – in a given special care health environment. The patient feedback (Greenhalgh et al.,
2017) from the care received in each department, the feedback of the caregivers in relation to
each other and the overall treatment process of each patient is crucial to the development of a
practice development. Empathy, active listening, heuristic and procedural problem solving
coupled with effective shared decision making is very important to adhere to patient centric
collaborative care. Principle 9 of practice development recommends inclusivity, active
participation of healthcare specialists and collaboration of trans-disciplinary practitioners
which is exactly to be followed by nurses, technologists and supervisory doctors to better the
‘patient handover’ practice. The short term goal of SCARF practice development tool in the
given scenario can be development of better, efficient, timely communication during patient
transfer. The other short term goals is to eliminate personal differences between practitioners
2015). Hence, the SCARF model is to be incorporated with a pre implementation check with
PRAXIS evaluation. Based on the findings and feedbacks, the SCARF tool needs to be
designed according to a treatment and precisely, patient need. Once the mentioned practice
development tool is in the system, the PRAXIS can be used again to measure the
functionality of the model and what changes needs to be made. Specificity to a patient and
the bio –medical care required for the case requires is important to quality and alter the
practice environments for a hassle free ‘handover’ process. Carrying the important
information (patient files) with the patient is vital for supporting the verbal patient
information transferred during patient handover. The practice development tool should be
bought to practice by a joint consensus of all the multi- disciplinary specialists, participating
in the practice of it. A shared decision making with the patient and a collaborative decision
making with members of other disciplines is vital to develop a patient centered ‘handover’
process and patient centered care. The application of the above mentioned practice tool
should qualify the parameters of specificity, measurable, achievable, reasonable (logical) and
time – in a given special care health environment. The patient feedback (Greenhalgh et al.,
2017) from the care received in each department, the feedback of the caregivers in relation to
each other and the overall treatment process of each patient is crucial to the development of a
practice development. Empathy, active listening, heuristic and procedural problem solving
coupled with effective shared decision making is very important to adhere to patient centric
collaborative care. Principle 9 of practice development recommends inclusivity, active
participation of healthcare specialists and collaboration of trans-disciplinary practitioners
which is exactly to be followed by nurses, technologists and supervisory doctors to better the
‘patient handover’ practice. The short term goal of SCARF practice development tool in the
given scenario can be development of better, efficient, timely communication during patient
transfer. The other short term goals is to eliminate personal differences between practitioners
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4IMPLEMENTATION OF PRACTICE DEVELOPMENT TOOL
to prevail a systematic operational flow while treating the patient. Short term goals should
also include fast head turning time, swift but right decision making, transfer of the ‘useful’
and ‘right’ patient knowledge should be implemented along with a practice development
protocol. The long term goal of the practice development project is to develop harmony and
develop concrete positive behavioral protocols between the members of a collaborative care
team for an advanced patient centered approach.
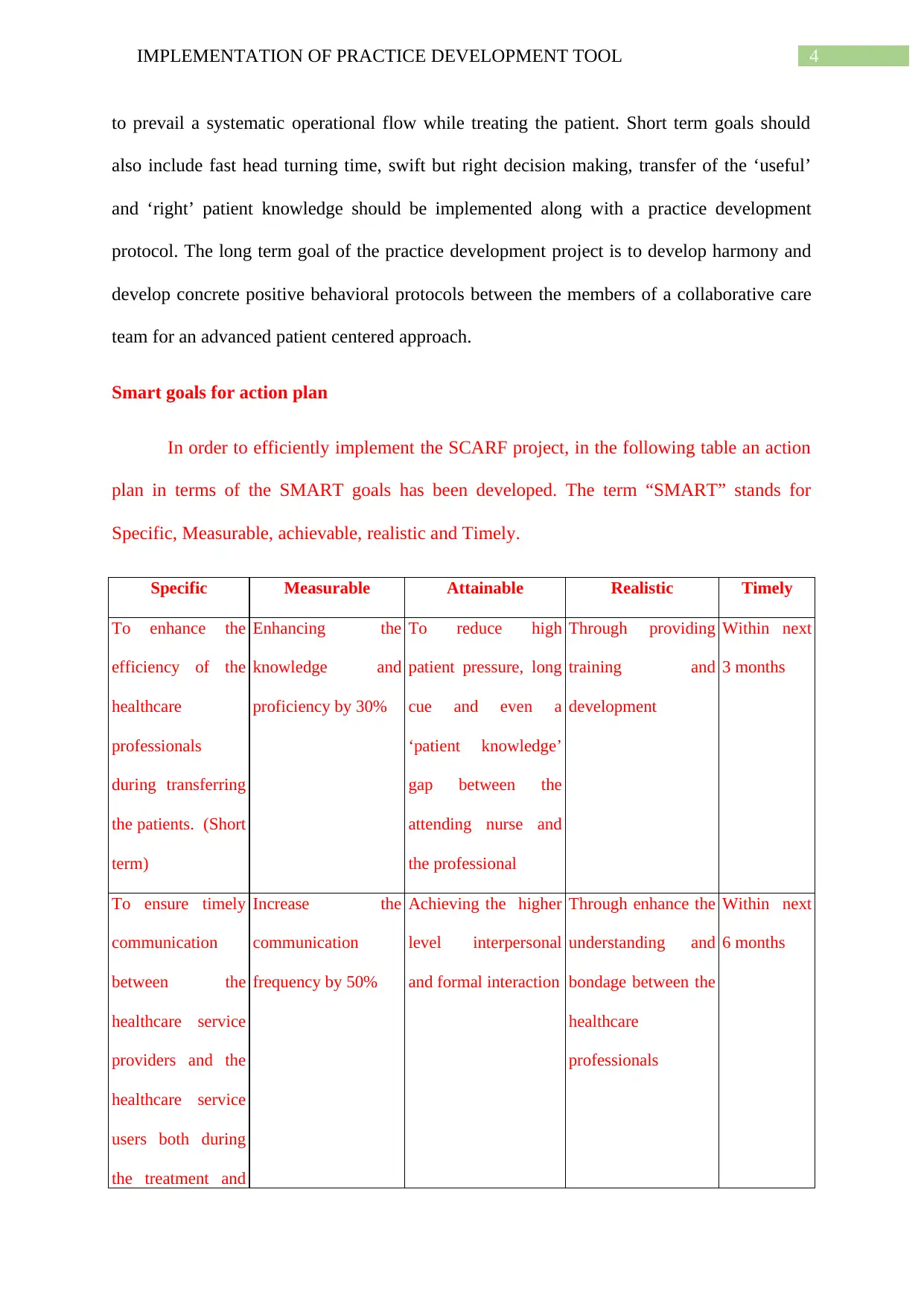
Smart goals for action plan
In order to efficiently implement the SCARF project, in the following table an action
plan in terms of the SMART goals has been developed. The term “SMART” stands for
Specific, Measurable, achievable, realistic and Timely.
Specific Measurable Attainable Realistic Timely
To enhance the
efficiency of the
healthcare
professionals
during transferring
the patients. (Short
term)
Enhancing the
knowledge and
proficiency by 30%
To reduce high
patient pressure, long
cue and even a
‘patient knowledge’
gap between the
attending nurse and
the professional
Through providing
training and
development
Within next
3 months
To ensure timely
communication
between the
healthcare service
providers and the
healthcare service
users both during
the treatment and
Increase the
communication
frequency by 50%
Achieving the higher
level interpersonal
and formal interaction
Through enhance the
understanding and
bondage between the
healthcare
professionals
Within next
6 months
to prevail a systematic operational flow while treating the patient. Short term goals should
also include fast head turning time, swift but right decision making, transfer of the ‘useful’
and ‘right’ patient knowledge should be implemented along with a practice development
protocol. The long term goal of the practice development project is to develop harmony and
develop concrete positive behavioral protocols between the members of a collaborative care
team for an advanced patient centered approach.
Smart goals for action plan
In order to efficiently implement the SCARF project, in the following table an action
plan in terms of the SMART goals has been developed. The term “SMART” stands for
Specific, Measurable, achievable, realistic and Timely.
Specific Measurable Attainable Realistic Timely
To enhance the
efficiency of the
healthcare
professionals
during transferring
the patients. (Short
term)
Enhancing the
knowledge and
proficiency by 30%
To reduce high
patient pressure, long
cue and even a
‘patient knowledge’
gap between the
attending nurse and
the professional
Through providing
training and
development
Within next
3 months
To ensure timely
communication
between the
healthcare service
providers and the
healthcare service
users both during
the treatment and
Increase the
communication
frequency by 50%
Achieving the higher
level interpersonal
and formal interaction
Through enhance the
understanding and
bondage between the
healthcare
professionals
Within next
6 months
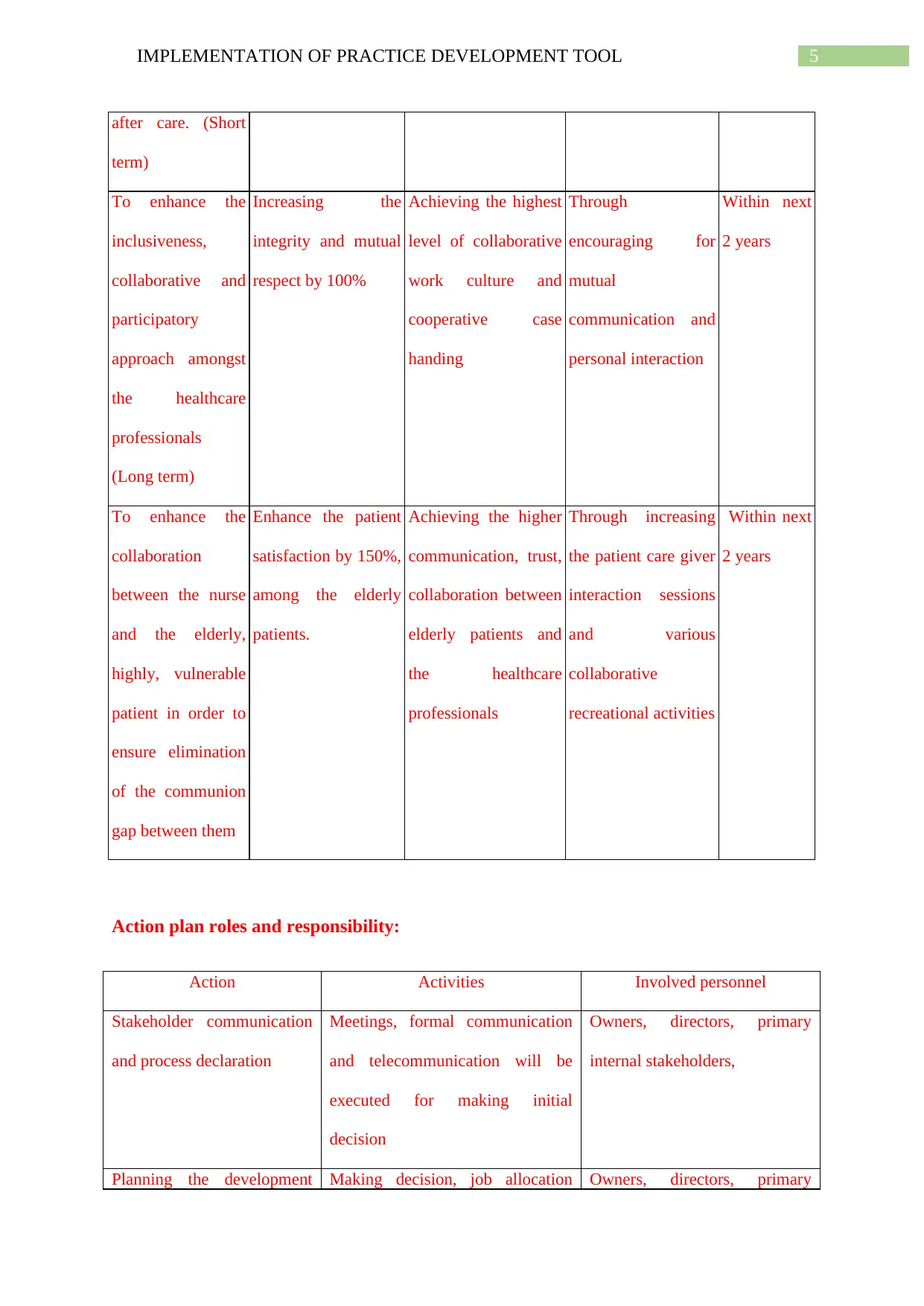
5IMPLEMENTATION OF PRACTICE DEVELOPMENT TOOL
after care. (Short
term)
To enhance the
inclusiveness,
collaborative and
participatory
approach amongst
the healthcare
professionals
(Long term)
Increasing the
integrity and mutual
respect by 100%
Achieving the highest
level of collaborative
work culture and
cooperative case
handing
Through
encouraging for
mutual
communication and
personal interaction
Within next
2 years
To enhance the
collaboration
between the nurse
and the elderly,
highly, vulnerable
patient in order to
ensure elimination
of the communion
gap between them
Enhance the patient
satisfaction by 150%,
among the elderly
patients.
Achieving the higher
communication, trust,
collaboration between
elderly patients and
the healthcare
professionals
Through increasing
the patient care giver
interaction sessions
and various
collaborative
recreational activities
Within next
2 years
Action plan roles and responsibility:
Action Activities Involved personnel
Stakeholder communication
and process declaration
Meetings, formal communication
and telecommunication will be
executed for making initial
decision
Owners, directors, primary
internal stakeholders,
Planning the development Making decision, job allocation Owners, directors, primary
after care. (Short
term)
To enhance the
inclusiveness,
collaborative and
participatory
approach amongst
the healthcare
professionals
(Long term)
Increasing the
integrity and mutual
respect by 100%
Achieving the highest
level of collaborative
work culture and
cooperative case
handing
Through
encouraging for
mutual
communication and
personal interaction
Within next
2 years
To enhance the
collaboration
between the nurse
and the elderly,
highly, vulnerable
patient in order to
ensure elimination
of the communion
gap between them
Enhance the patient
satisfaction by 150%,
among the elderly
patients.
Achieving the higher
communication, trust,
collaboration between
elderly patients and
the healthcare
professionals
Through increasing
the patient care giver
interaction sessions
and various
collaborative
recreational activities
Within next
2 years
Action plan roles and responsibility:
Action Activities Involved personnel
Stakeholder communication
and process declaration
Meetings, formal communication
and telecommunication will be
executed for making initial
decision
Owners, directors, primary
internal stakeholders,
Planning the development Making decision, job allocation Owners, directors, primary
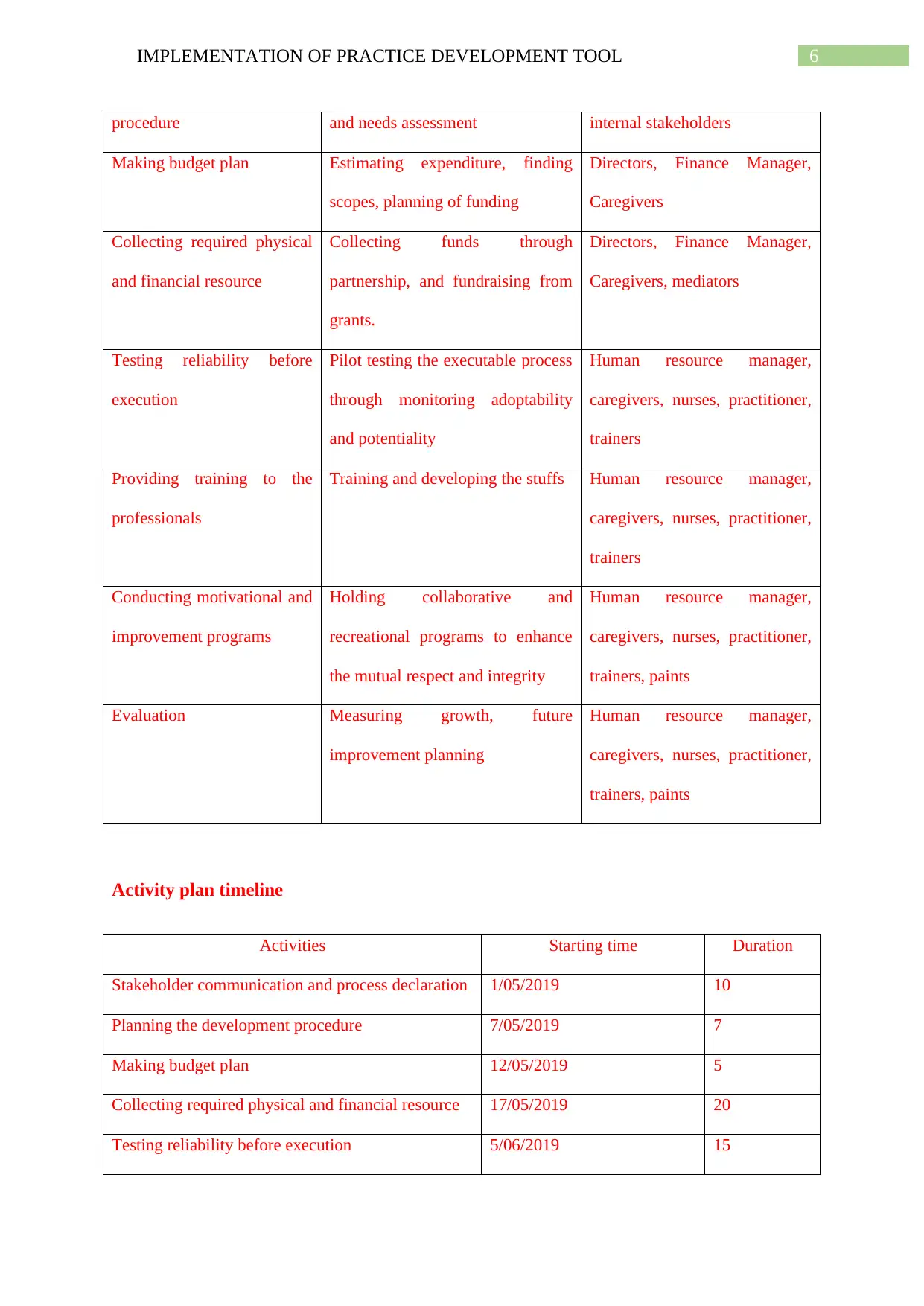
6IMPLEMENTATION OF PRACTICE DEVELOPMENT TOOL
procedure and needs assessment internal stakeholders
Making budget plan Estimating expenditure, finding
scopes, planning of funding
Directors, Finance Manager,
Caregivers
Collecting required physical
and financial resource
Collecting funds through
partnership, and fundraising from
grants.
Directors, Finance Manager,
Caregivers, mediators
Testing reliability before
execution
Pilot testing the executable process
through monitoring adoptability
and potentiality
Human resource manager,
caregivers, nurses, practitioner,
trainers
Providing training to the
professionals
Training and developing the stuffs Human resource manager,
caregivers, nurses, practitioner,
trainers
Conducting motivational and
improvement programs
Holding collaborative and
recreational programs to enhance
the mutual respect and integrity
Human resource manager,
caregivers, nurses, practitioner,
trainers, paints
Evaluation Measuring growth, future
improvement planning
Human resource manager,
caregivers, nurses, practitioner,
trainers, paints
Activity plan timeline
Activities Starting time Duration
Stakeholder communication and process declaration 1/05/2019 10
Planning the development procedure 7/05/2019 7
Making budget plan 12/05/2019 5
Collecting required physical and financial resource 17/05/2019 20
Testing reliability before execution 5/06/2019 15
procedure and needs assessment internal stakeholders
Making budget plan Estimating expenditure, finding
scopes, planning of funding
Directors, Finance Manager,
Caregivers
Collecting required physical
and financial resource
Collecting funds through
partnership, and fundraising from
grants.
Directors, Finance Manager,
Caregivers, mediators
Testing reliability before
execution
Pilot testing the executable process
through monitoring adoptability
and potentiality
Human resource manager,
caregivers, nurses, practitioner,
trainers
Providing training to the
professionals
Training and developing the stuffs Human resource manager,
caregivers, nurses, practitioner,
trainers
Conducting motivational and
improvement programs
Holding collaborative and
recreational programs to enhance
the mutual respect and integrity
Human resource manager,
caregivers, nurses, practitioner,
trainers, paints
Evaluation Measuring growth, future
improvement planning
Human resource manager,
caregivers, nurses, practitioner,
trainers, paints
Activity plan timeline
Activities Starting time Duration
Stakeholder communication and process declaration 1/05/2019 10
Planning the development procedure 7/05/2019 7
Making budget plan 12/05/2019 5
Collecting required physical and financial resource 17/05/2019 20
Testing reliability before execution 5/06/2019 15
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
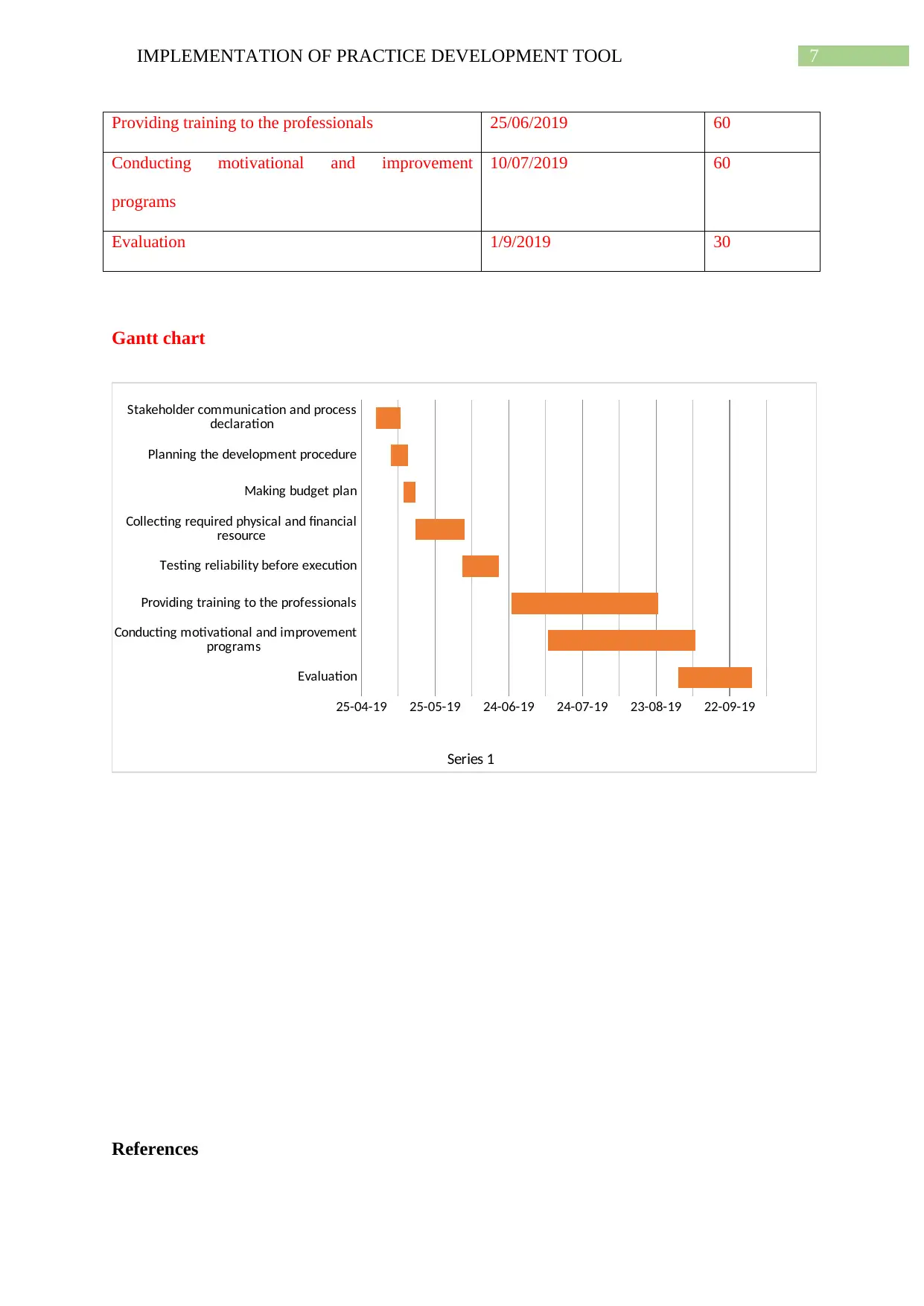
7IMPLEMENTATION OF PRACTICE DEVELOPMENT TOOL
Providing training to the professionals 25/06/2019 60
Conducting motivational and improvement
programs
10/07/2019 60
Evaluation 1/9/2019 30
Gantt chart
Evaluation
Conducting motivational and improvement
programs
Providing training to the professionals
Testing reliability before execution
Collecting required physical and financial
resource
Making budget plan
Planning the development procedure
Stakeholder communication and process
declaration
25-04-19 25-05-19 24-06-19 24-07-19 23-08-19 22-09-19
Series 1
References
Providing training to the professionals 25/06/2019 60
Conducting motivational and improvement
programs
10/07/2019 60
Evaluation 1/9/2019 30
Gantt chart
Evaluation
Conducting motivational and improvement
programs
Providing training to the professionals
Testing reliability before execution
Collecting required physical and financial
resource
Making budget plan
Planning the development procedure
Stakeholder communication and process
declaration
25-04-19 25-05-19 24-06-19 24-07-19 23-08-19 22-09-19
Series 1
References
8IMPLEMENTATION OF PRACTICE DEVELOPMENT TOOL
Amini, H., Shakiba, A., Sharifi, V., Shirazi, M., Sadeghi, M., Abolhasani, F., & Hajebi, A.
(2016). Evaluation of the performance of general practitioners in a collaborative care
program by employing simulated patients. Social psychiatry and psychiatric
epidemiology, 51(9), 1311-1319., doi:10.1007/s00127-016-1226-3
Ferris, D. L., Yan, M., Lim, V. K., Chen, Y., & Fatimah, S. (2016). An approach–avoidance
framework of workplace aggression. Academy of Management Journal, 59(5), 1777-
1800. doi: 10.5465/amj.2014.0221
Freedman, B. D. (2019). Risk factors and causes of interpersonal conflict in nursing
workplaces: Understandings from neuroscience. Collegian. doi:
10.1016/j.colegn.2019.02.001
Greenhalgh, J., Dalkin, S., Gooding, K., Gibbons, E., Wright, J., Meads, D., ... & Pawson, R.
(2017). Functionality and feedback: a realist synthesis of the collation, interpretation
and utilisation of patient-reported outcome measures data to improve patient
care. Health Services and Delivery Research, 5(2), 1-280. doi: 10.3310/hsdr05020
Huston, C. L., Phillips, B., Jeffries, P., Todero, C., Rich, J., Knecht, P., ... & Lewis, M. P.
(2018, January). The academic‐practice gap: Strategies for an enduring problem.
In Nursing forum (Vol. 53, No. 1, pp. 27-34). doi: 10.5465/amj.2014.0221
Ignatavicius, D. D., & Workman, M. L. (2015). Medical-Surgical Nursing-E-Book: Patient-
Centered Collaborative Care, Single Volume. Elsevier health sciences. doi:
10.5465/amj.2014.0221
Jager, A. J., Choudhry, S. A., Marsteller, J. A., Telford, R. P., & Wynia, M. K. (2017).
Development and initial validation of a new practice context assessment tool for
ambulatory practices engaged in quality improvement. American Journal of Medical
Quality, 32(4), 423-437. doi: 10.1177/1062860616659132
Amini, H., Shakiba, A., Sharifi, V., Shirazi, M., Sadeghi, M., Abolhasani, F., & Hajebi, A.
(2016). Evaluation of the performance of general practitioners in a collaborative care
program by employing simulated patients. Social psychiatry and psychiatric
epidemiology, 51(9), 1311-1319., doi:10.1007/s00127-016-1226-3
Ferris, D. L., Yan, M., Lim, V. K., Chen, Y., & Fatimah, S. (2016). An approach–avoidance
framework of workplace aggression. Academy of Management Journal, 59(5), 1777-
1800. doi: 10.5465/amj.2014.0221
Freedman, B. D. (2019). Risk factors and causes of interpersonal conflict in nursing
workplaces: Understandings from neuroscience. Collegian. doi:
10.1016/j.colegn.2019.02.001
Greenhalgh, J., Dalkin, S., Gooding, K., Gibbons, E., Wright, J., Meads, D., ... & Pawson, R.
(2017). Functionality and feedback: a realist synthesis of the collation, interpretation
and utilisation of patient-reported outcome measures data to improve patient
care. Health Services and Delivery Research, 5(2), 1-280. doi: 10.3310/hsdr05020
Huston, C. L., Phillips, B., Jeffries, P., Todero, C., Rich, J., Knecht, P., ... & Lewis, M. P.
(2018, January). The academic‐practice gap: Strategies for an enduring problem.
In Nursing forum (Vol. 53, No. 1, pp. 27-34). doi: 10.5465/amj.2014.0221
Ignatavicius, D. D., & Workman, M. L. (2015). Medical-Surgical Nursing-E-Book: Patient-
Centered Collaborative Care, Single Volume. Elsevier health sciences. doi:
10.5465/amj.2014.0221
Jager, A. J., Choudhry, S. A., Marsteller, J. A., Telford, R. P., & Wynia, M. K. (2017).
Development and initial validation of a new practice context assessment tool for
ambulatory practices engaged in quality improvement. American Journal of Medical
Quality, 32(4), 423-437. doi: 10.1177/1062860616659132
9IMPLEMENTATION OF PRACTICE DEVELOPMENT TOOL
Malik, G., McKenna, L., & Plummer, V. (2015). Perceived knowledge, skills, attitude and
contextual factors affecting evidence‐based practice among nurse educators, clinical
coaches and nurse specialists. International journal of nursing practice, 21, 46-57.,
doi: 10.1111/ijn.12366
Putturaj, M., & Prashanth, N. S. (2017). Enhancing the autonomy of Indian nurses. Indian
journal of medical ethics, 2(4). Retrieved from:
http://www.ijme.in/wp-content/uploads/2017/05/254com275_enhancing_the_autono
my.pdf
Stubbe, D. E. (2017). Competent Communication in Collaborative Care. FOCUS, 15(3), 298-
300. doi: 10.1111/1467-9566.12391
Waring, J., Allen, D., Braithwaite, J., & Sandall, J. (2016). Healthcare quality and safety: a
review of policy, practice and research. Sociology of Health & Illness, 38(2), 198-215.
doi: 10.5465/amj.2014.0221
Weinberg, A., Perlman, G., Kotov, R., & Hajcak, G. (2016). Depression and reduced neural
response to emotional images: Distinction from anxiety, and importance of symptom
dimensions and age of onset. Journal of abnormal psychology, 125(1), 26. doi:
10.1037/abn0000118
Malik, G., McKenna, L., & Plummer, V. (2015). Perceived knowledge, skills, attitude and
contextual factors affecting evidence‐based practice among nurse educators, clinical
coaches and nurse specialists. International journal of nursing practice, 21, 46-57.,
doi: 10.1111/ijn.12366
Putturaj, M., & Prashanth, N. S. (2017). Enhancing the autonomy of Indian nurses. Indian
journal of medical ethics, 2(4). Retrieved from:
http://www.ijme.in/wp-content/uploads/2017/05/254com275_enhancing_the_autono
my.pdf
Stubbe, D. E. (2017). Competent Communication in Collaborative Care. FOCUS, 15(3), 298-
300. doi: 10.1111/1467-9566.12391
Waring, J., Allen, D., Braithwaite, J., & Sandall, J. (2016). Healthcare quality and safety: a
review of policy, practice and research. Sociology of Health & Illness, 38(2), 198-215.
doi: 10.5465/amj.2014.0221
Weinberg, A., Perlman, G., Kotov, R., & Hajcak, G. (2016). Depression and reduced neural
response to emotional images: Distinction from anxiety, and importance of symptom
dimensions and age of onset. Journal of abnormal psychology, 125(1), 26. doi:
10.1037/abn0000118
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

10IMPLEMENTATION OF PRACTICE DEVELOPMENT TOOL
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





