NCCCR: Improving Patient Flow in Oncology and Haematology
VerifiedAdded on 2023/01/06
|17
|4618
|58
Report
AI Summary
This report presents a business case for improving patient flow within the Oncology and Haematology departments at the National Centre for Cancer Care and Research (NCCCR). It begins by analyzing the current system, highlighting issues such as admission exceeding discharge rates and lengthy discharge processes. The rationale for improvement focuses on implementing a safe and holistic environment for individualized patient management, and the report outlines drivers like standardized staffing plans and patient education. A stakeholder analysis identifies key individuals and their influence on the project. Risk analysis identifies potential challenges and mitigation strategies. The expected benefits include reduced discharge times, improved patient care, and enhanced communication. The PDCA cycle is proposed as the primary methodology. An evaluation plan is also included to assess the project's effectiveness. The report aims to improve the overall efficiency and quality of care within the NCCCR's oncology and haematology departments.
Improve Oncology
Haematology and Palliative
Patients Flow
In National Centre for Cancer Care and Research (NCCCR)
Haematology and Palliative
Patients Flow
In National Centre for Cancer Care and Research (NCCCR)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Table of Contents
MAIN BODY..................................................................................................................................1
Current understanding of system/process....................................................................................1
Rationale and drivers for the improvement.................................................................................1
Stakeholder analysis and engagement plan.................................................................................2
Risk analysis................................................................................................................................3
Expected benefits.........................................................................................................................5
Methods to be used-.....................................................................................................................5
Evaluation plan............................................................................................................................6
REFERENCES................................................................................................................................8
MAIN BODY..................................................................................................................................1
Current understanding of system/process....................................................................................1
Rationale and drivers for the improvement.................................................................................1
Stakeholder analysis and engagement plan.................................................................................2
Risk analysis................................................................................................................................3
Expected benefits.........................................................................................................................5
Methods to be used-.....................................................................................................................5
Evaluation plan............................................................................................................................6
REFERENCES................................................................................................................................8
MAIN BODY
Current understanding of system/process
Present situation describes services and care of Oncology and Haematology department
which are resulting in enhancing quality and wellbeing of patients by making use of multi-
disciplinary approach (El-Jawahri et.al., 2016). From the data provided it can be summarised that
83 patients were admitted to oncology department in local Hospital of Qatar and out of these
only 72 people were timely discharged (Finlay, Rabow & Buss, 2018). It has also been analysed
that there are two admission discharge teams working in hospital i.e. team A and B. provided
figure has given the detail in comparison to admission, there were less patients who were
discharged. This is because discharge procedure includes lots of documentation because of
which it takes time (Tashkandi et.al., 2020).
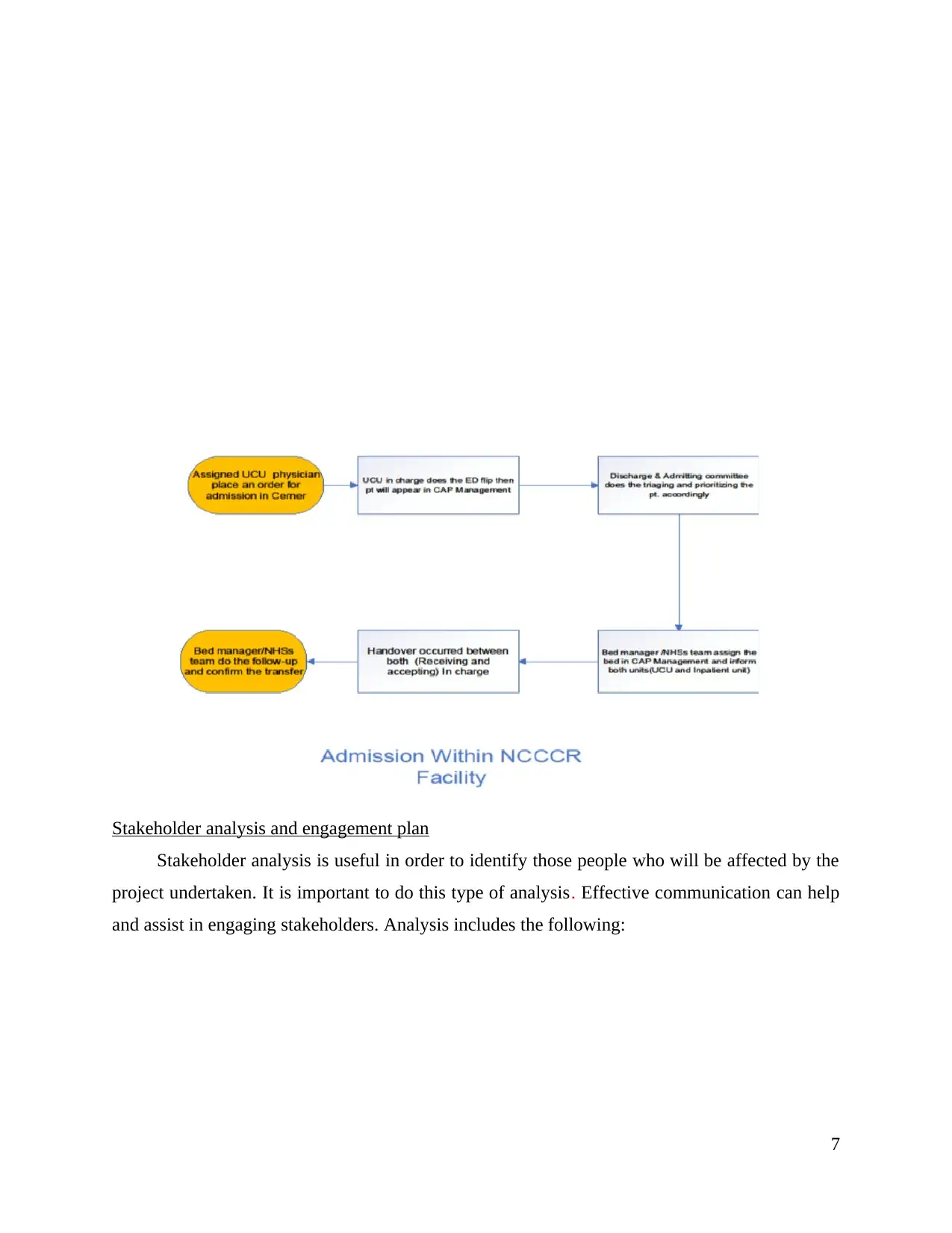
Discharged Patients need close observation, weekly follow up for blood work. The process
followed by hospital care unit should be enhanced in order to meet out the social, psychological
and spiritual needs of the patient and their families. It has also been analysed from the data
provided that admission is more than discharge on the same day (Silva & Paiva, 2019). There is
a long process followed even when patients are admitted. Impatient work flow has provided the
details that there is an elective admission of patient, Admission within NCCCR units, Admission
from other facility, Admission from abroad. In order to enhance quality of care provided by
oncology and haematology department, they need to be involved in making a staffing plan
(Nicosia et.al., 2018). A staffing plan for the Chemotherapy Day Care Unit is formulated to
identify staffing numbers needed and budgeted for the unit. The department is also trying to
discharge patients before 11 am but because of the long process, they are unable to manage and
handle work so most of the patients are discharged after 2 PM.
1
Current understanding of system/process
Present situation describes services and care of Oncology and Haematology department
which are resulting in enhancing quality and wellbeing of patients by making use of multi-
disciplinary approach (El-Jawahri et.al., 2016). From the data provided it can be summarised that
83 patients were admitted to oncology department in local Hospital of Qatar and out of these
only 72 people were timely discharged (Finlay, Rabow & Buss, 2018). It has also been analysed
that there are two admission discharge teams working in hospital i.e. team A and B. provided
figure has given the detail in comparison to admission, there were less patients who were
discharged. This is because discharge procedure includes lots of documentation because of
which it takes time (Tashkandi et.al., 2020).
Discharged Patients need close observation, weekly follow up for blood work. The process
followed by hospital care unit should be enhanced in order to meet out the social, psychological
and spiritual needs of the patient and their families. It has also been analysed from the data
provided that admission is more than discharge on the same day (Silva & Paiva, 2019). There is
a long process followed even when patients are admitted. Impatient work flow has provided the
details that there is an elective admission of patient, Admission within NCCCR units, Admission
from other facility, Admission from abroad. In order to enhance quality of care provided by
oncology and haematology department, they need to be involved in making a staffing plan
(Nicosia et.al., 2018). A staffing plan for the Chemotherapy Day Care Unit is formulated to
identify staffing numbers needed and budgeted for the unit. The department is also trying to
discharge patients before 11 am but because of the long process, they are unable to manage and
handle work so most of the patients are discharged after 2 PM.
1
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
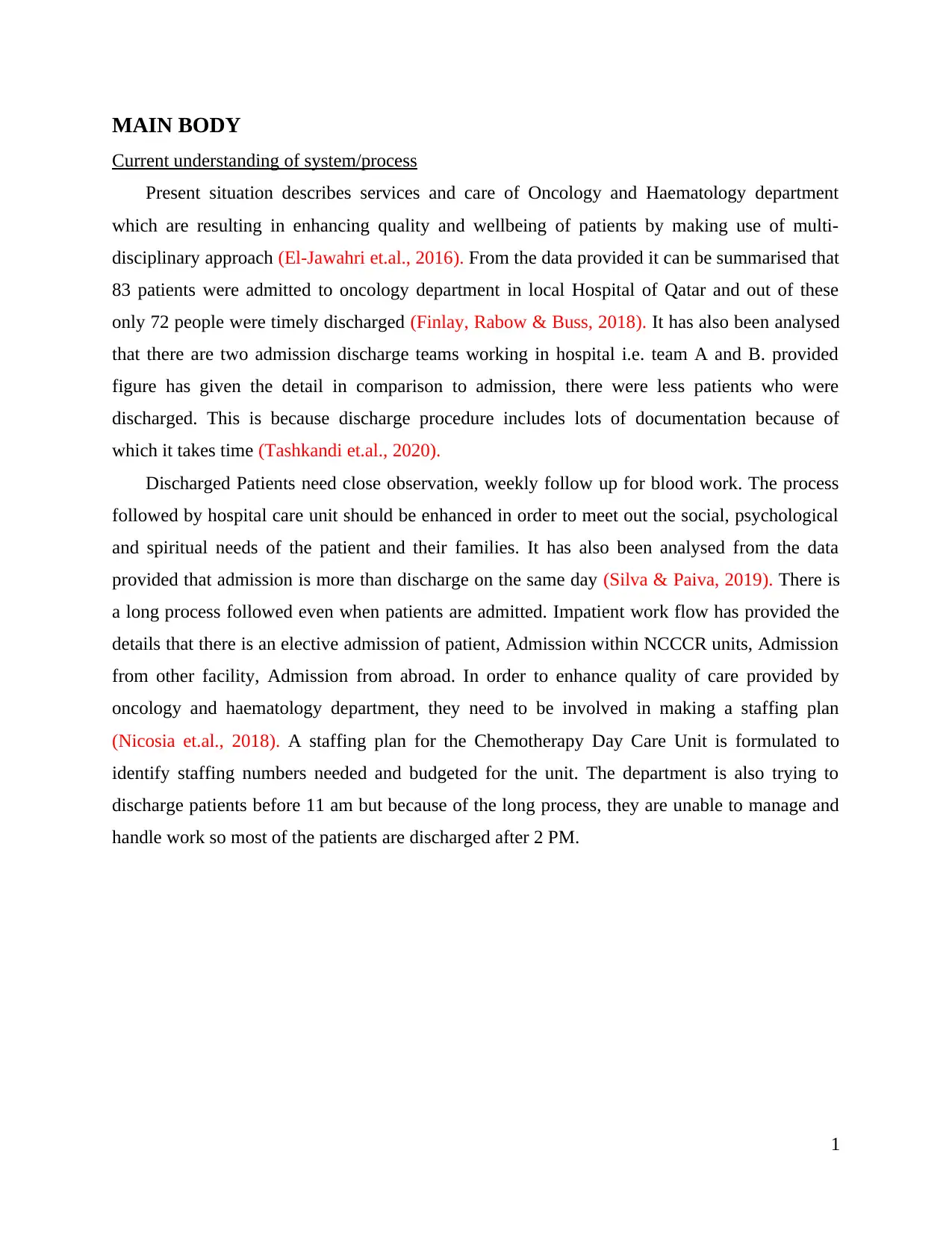
Rationale and drivers for the improvement
2
Supplier
s
Input Process Outcome Customers
Beds
Resources
Medication
Transportation
Sponsor
Work flow
Finance
Preference
Language
related
issues
Staff issues
Shortage of
staff
Readiness of
patients/ family
problems
Incorrect
entry
No shortage
of bed
Early
admission
Improve
healthcare
outcome
Nurses
Physcisans
Patients
Families
SIPOC:
Decrease
cost
2
Supplier
s
Input Process Outcome Customers
Beds
Resources
Medication
Transportation
Sponsor
Work flow
Finance
Preference
Language
related
issues
Staff issues
Shortage of
staff
Readiness of
patients/ family
problems
Incorrect
entry
No shortage
of bed
Early
admission
Improve
healthcare
outcome
Nurses
Physcisans
Patients
Families
SIPOC:
Decrease
cost
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
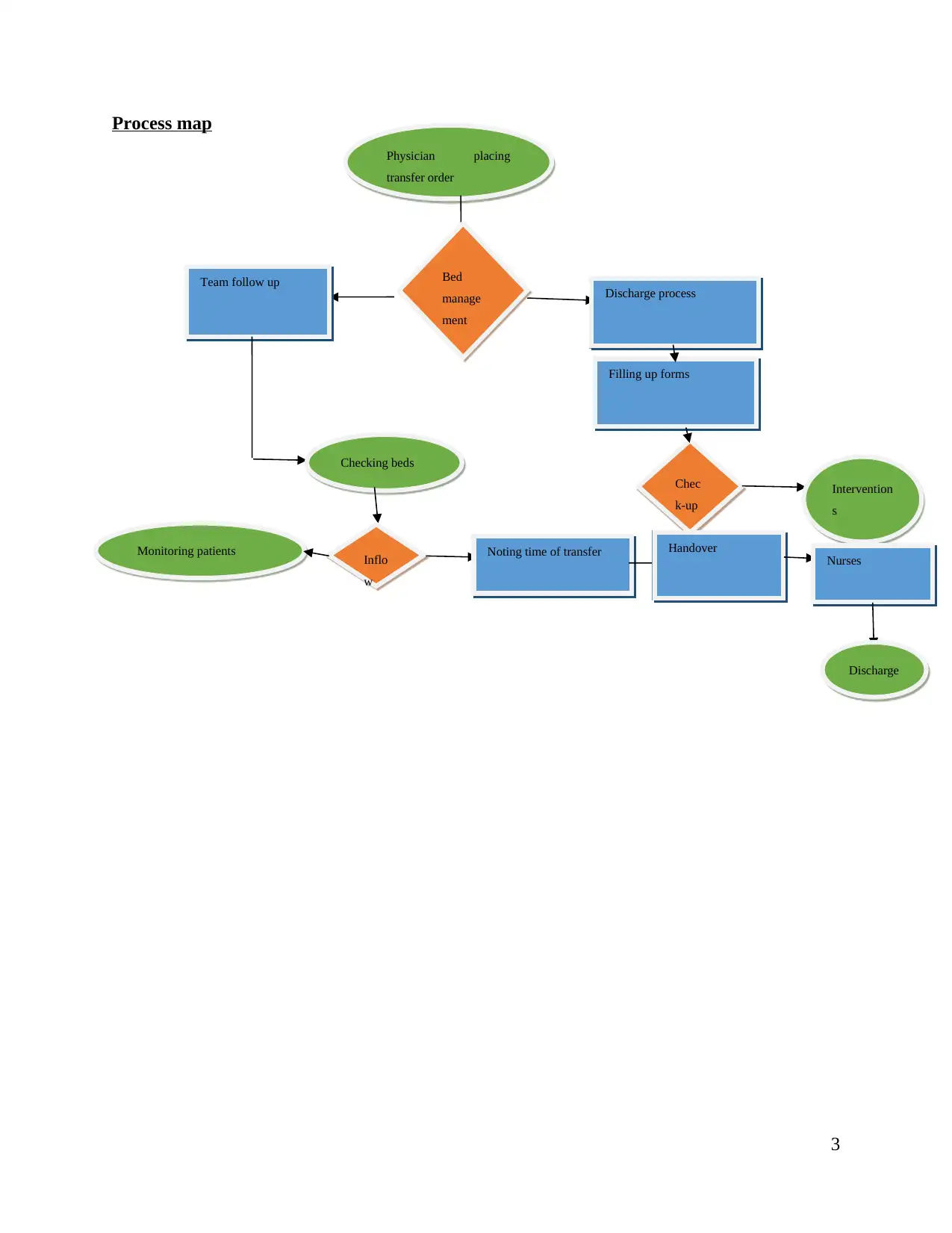
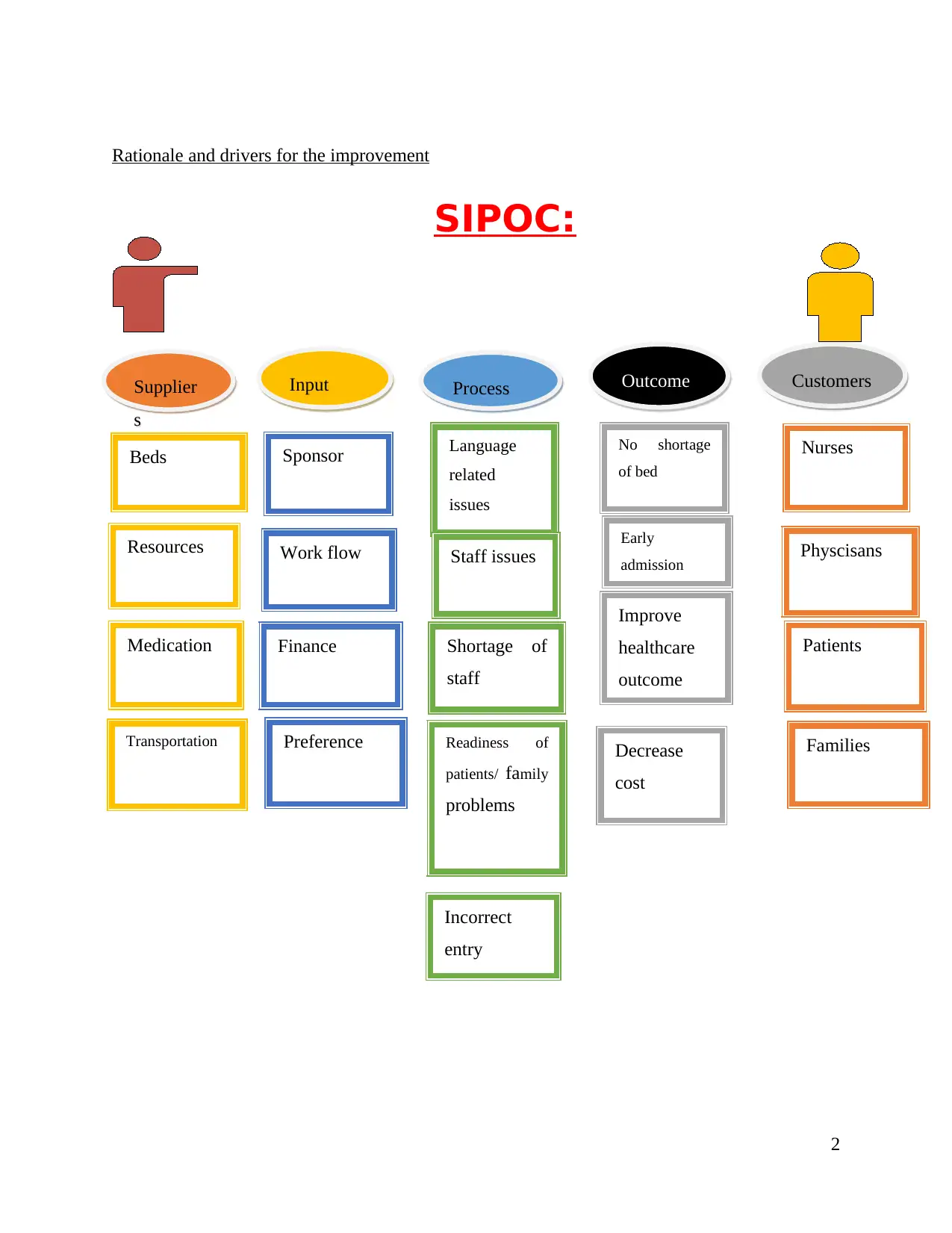
Process map
3
Physician placing
transfer order
Bed
manage
ment
Discharge process
Team follow up
Checking beds
Filling up forms
Chec
k-up
Intervention
s
Monitoring patients Inflo
w
Noting time of transfer Handover
Nurses
Discharge
3
Physician placing
transfer order
Bed
manage
ment
Discharge process
Team follow up
Checking beds
Filling up forms
Chec
k-up
Intervention
s
Monitoring patients Inflo
w
Noting time of transfer Handover
Nurses
Discharge
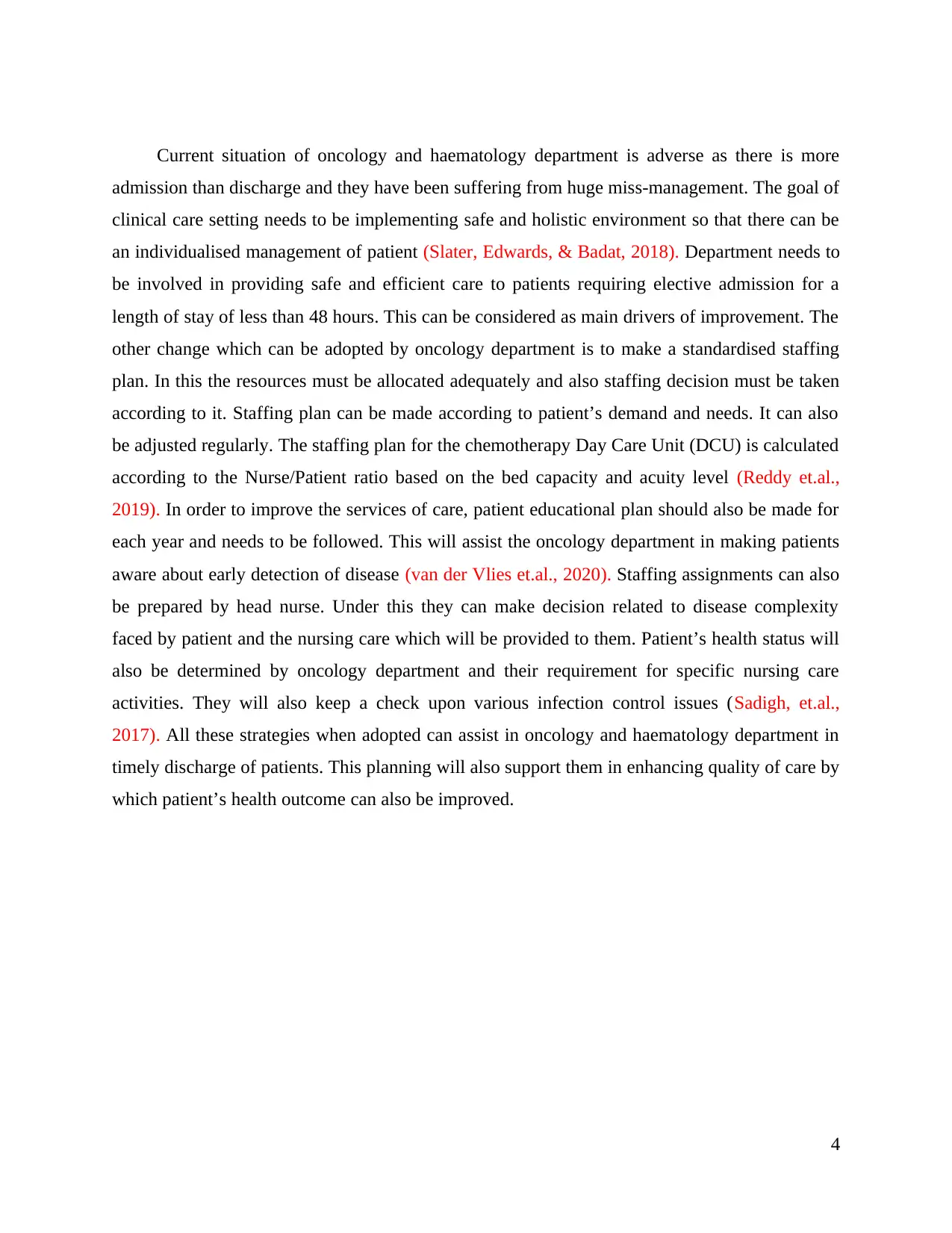
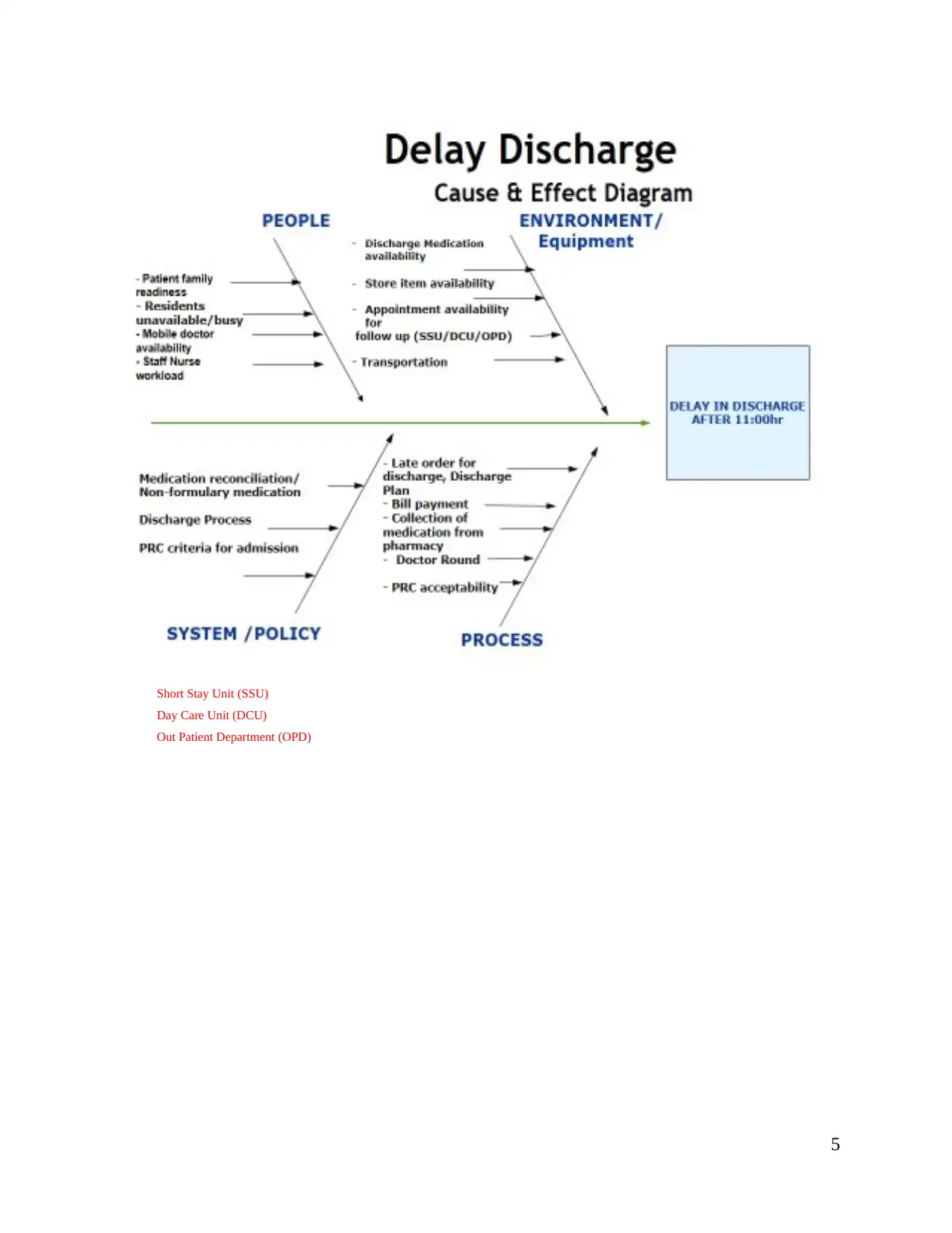
Current situation of oncology and haematology department is adverse as there is more
admission than discharge and they have been suffering from huge miss-management. The goal of
clinical care setting needs to be implementing safe and holistic environment so that there can be
an individualised management of patient (Slater, Edwards, & Badat, 2018). Department needs to
be involved in providing safe and efficient care to patients requiring elective admission for a
length of stay of less than 48 hours. This can be considered as main drivers of improvement. The
other change which can be adopted by oncology department is to make a standardised staffing
plan. In this the resources must be allocated adequately and also staffing decision must be taken
according to it. Staffing plan can be made according to patient’s demand and needs. It can also
be adjusted regularly. The staffing plan for the chemotherapy Day Care Unit (DCU) is calculated
according to the Nurse/Patient ratio based on the bed capacity and acuity level (Reddy et.al.,
2019). In order to improve the services of care, patient educational plan should also be made for
each year and needs to be followed. This will assist the oncology department in making patients
aware about early detection of disease (van der Vlies et.al., 2020). Staffing assignments can also
be prepared by head nurse. Under this they can make decision related to disease complexity
faced by patient and the nursing care which will be provided to them. Patient’s health status will
also be determined by oncology department and their requirement for specific nursing care
activities. They will also keep a check upon various infection control issues (Sadigh, et.al.,
2017). All these strategies when adopted can assist in oncology and haematology department in
timely discharge of patients. This planning will also support them in enhancing quality of care by
which patient’s health outcome can also be improved.
4
admission than discharge and they have been suffering from huge miss-management. The goal of
clinical care setting needs to be implementing safe and holistic environment so that there can be
an individualised management of patient (Slater, Edwards, & Badat, 2018). Department needs to
be involved in providing safe and efficient care to patients requiring elective admission for a
length of stay of less than 48 hours. This can be considered as main drivers of improvement. The
other change which can be adopted by oncology department is to make a standardised staffing
plan. In this the resources must be allocated adequately and also staffing decision must be taken
according to it. Staffing plan can be made according to patient’s demand and needs. It can also
be adjusted regularly. The staffing plan for the chemotherapy Day Care Unit (DCU) is calculated
according to the Nurse/Patient ratio based on the bed capacity and acuity level (Reddy et.al.,
2019). In order to improve the services of care, patient educational plan should also be made for
each year and needs to be followed. This will assist the oncology department in making patients
aware about early detection of disease (van der Vlies et.al., 2020). Staffing assignments can also
be prepared by head nurse. Under this they can make decision related to disease complexity
faced by patient and the nursing care which will be provided to them. Patient’s health status will
also be determined by oncology department and their requirement for specific nursing care
activities. They will also keep a check upon various infection control issues (Sadigh, et.al.,
2017). All these strategies when adopted can assist in oncology and haematology department in
timely discharge of patients. This planning will also support them in enhancing quality of care by
which patient’s health outcome can also be improved.
4
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Short Stay Unit (SSU)
Day Care Unit (DCU)
Out Patient Department (OPD)
5
Day Care Unit (DCU)
Out Patient Department (OPD)
5
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
6
Stakeholder analysis and engagement plan
Stakeholder analysis is useful in order to identify those people who will be affected by the
project undertaken. It is important to do this type of analysis. Effective communication can help
and assist in engaging stakeholders. Analysis includes the following:
7
Stakeholder analysis is useful in order to identify those people who will be affected by the
project undertaken. It is important to do this type of analysis. Effective communication can help
and assist in engaging stakeholders. Analysis includes the following:
7
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
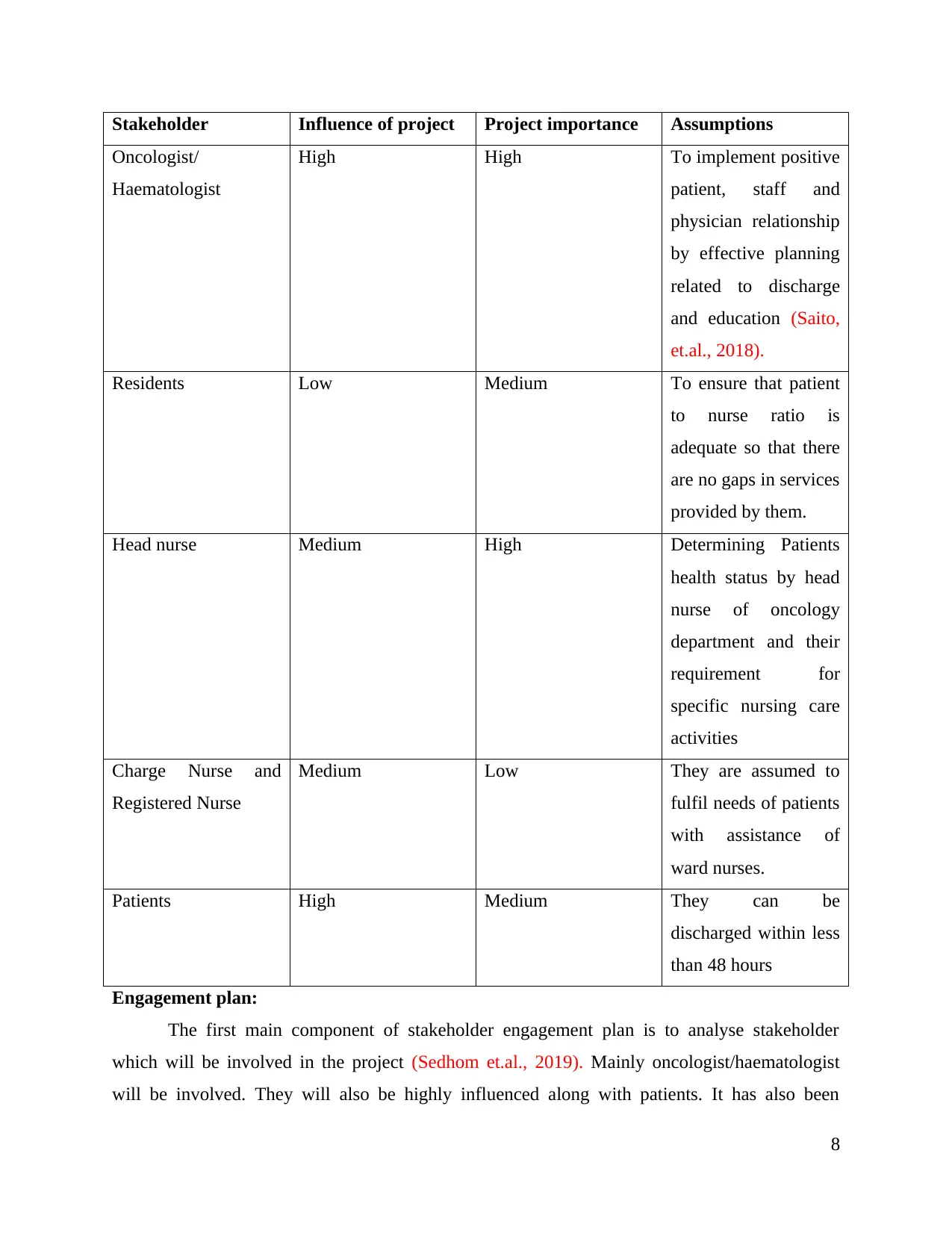
Stakeholder Influence of project Project importance Assumptions
Oncologist/
Haematologist
High High To implement positive
patient, staff and
physician relationship
by effective planning
related to discharge
and education (Saito,
et.al., 2018).
Residents Low Medium To ensure that patient
to nurse ratio is
adequate so that there
are no gaps in services
provided by them.
Head nurse Medium High Determining Patients
health status by head
nurse of oncology
department and their
requirement for
specific nursing care
activities
Charge Nurse and
Registered Nurse
Medium Low They are assumed to
fulfil needs of patients
with assistance of
ward nurses.
Patients High Medium They can be
discharged within less
than 48 hours
Engagement plan:
The first main component of stakeholder engagement plan is to analyse stakeholder
which will be involved in the project (Sedhom et.al., 2019). Mainly oncologist/haematologist
will be involved. They will also be highly influenced along with patients. It has also been
8
Oncologist/
Haematologist
High High To implement positive
patient, staff and
physician relationship
by effective planning
related to discharge
and education (Saito,
et.al., 2018).
Residents Low Medium To ensure that patient
to nurse ratio is
adequate so that there
are no gaps in services
provided by them.
Head nurse Medium High Determining Patients
health status by head
nurse of oncology
department and their
requirement for
specific nursing care
activities
Charge Nurse and
Registered Nurse
Medium Low They are assumed to
fulfil needs of patients
with assistance of
ward nurses.
Patients High Medium They can be
discharged within less
than 48 hours
Engagement plan:
The first main component of stakeholder engagement plan is to analyse stakeholder
which will be involved in the project (Sedhom et.al., 2019). Mainly oncologist/haematologist
will be involved. They will also be highly influenced along with patients. It has also been
8
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
analysed that the other step in planning can be related to power as each stakeholder as the ability
to change the aspects. In this case situation the high power is been given to oncologist and head
nurses.
Commitment, enrolment and compliance tool can also be used to engage stakeholders for
improvement in the project undertaken (Stavas et.al., 2017). It can be used in order to better
understand the requirements of stakeholders so that decisions can be accordingly taken. Apart
from the stakeholder mapping and analysis, this tool can be used. Team involved in improving
discharge situation can make use of this so that proper changes can be implemented (Sermet &
Demir, 2019).
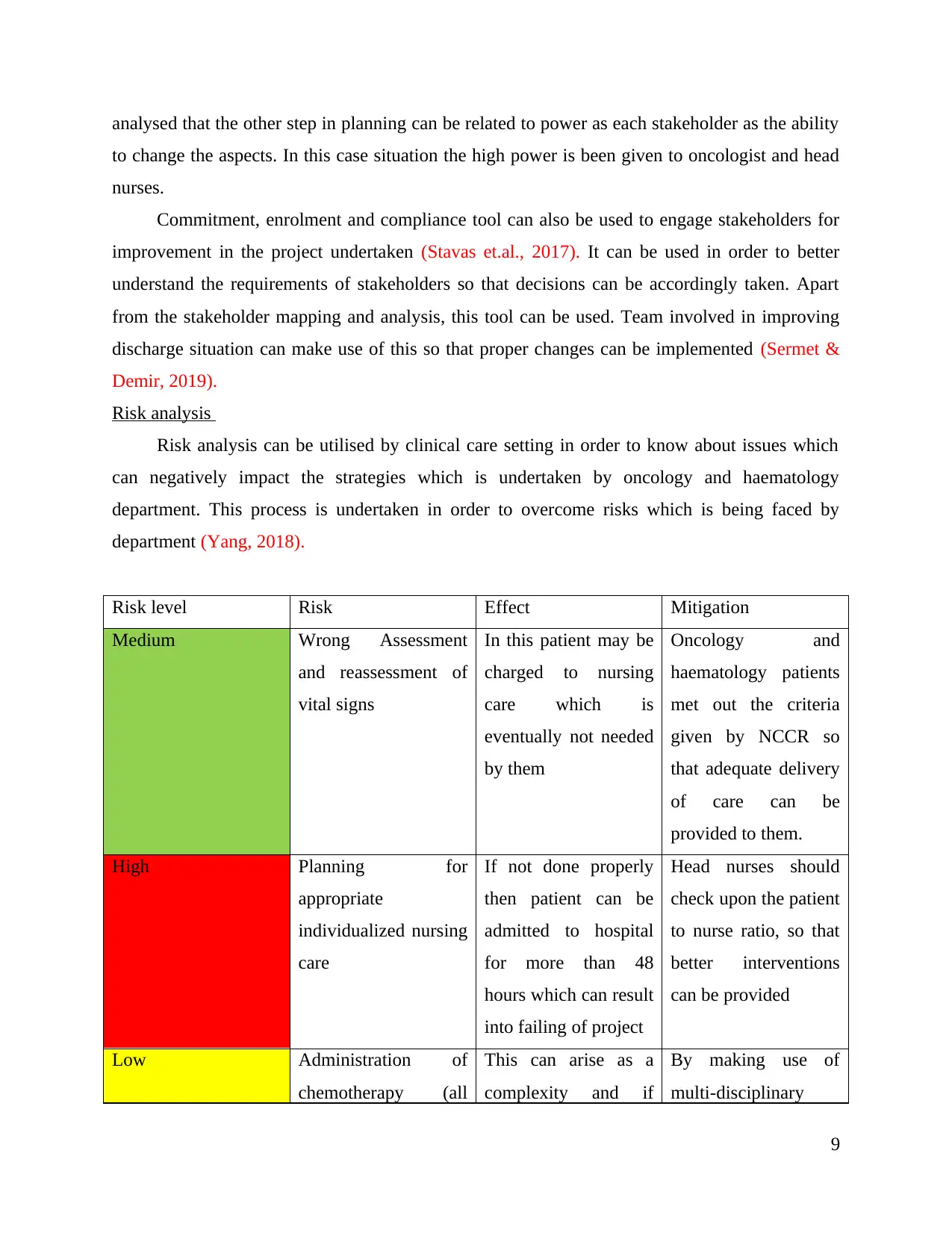
Risk analysis
Risk analysis can be utilised by clinical care setting in order to know about issues which
can negatively impact the strategies which is undertaken by oncology and haematology
department. This process is undertaken in order to overcome risks which is being faced by
department (Yang, 2018).
Risk level Risk Effect Mitigation
Medium Wrong Assessment
and reassessment of
vital signs
In this patient may be
charged to nursing
care which is
eventually not needed
by them
Oncology and
haematology patients
met out the criteria
given by NCCR so
that adequate delivery
of care can be
provided to them.
High Planning for
appropriate
individualized nursing
care
If not done properly
then patient can be
admitted to hospital
for more than 48
hours which can result
into failing of project
Head nurses should
check upon the patient
to nurse ratio, so that
better interventions
can be provided
Low Administration of
chemotherapy (all
This can arise as a
complexity and if
By making use of
multi-disciplinary
9
to change the aspects. In this case situation the high power is been given to oncologist and head
nurses.
Commitment, enrolment and compliance tool can also be used to engage stakeholders for
improvement in the project undertaken (Stavas et.al., 2017). It can be used in order to better
understand the requirements of stakeholders so that decisions can be accordingly taken. Apart
from the stakeholder mapping and analysis, this tool can be used. Team involved in improving
discharge situation can make use of this so that proper changes can be implemented (Sermet &
Demir, 2019).
Risk analysis
Risk analysis can be utilised by clinical care setting in order to know about issues which
can negatively impact the strategies which is undertaken by oncology and haematology
department. This process is undertaken in order to overcome risks which is being faced by
department (Yang, 2018).
Risk level Risk Effect Mitigation
Medium Wrong Assessment
and reassessment of
vital signs
In this patient may be
charged to nursing
care which is
eventually not needed
by them
Oncology and
haematology patients
met out the criteria
given by NCCR so
that adequate delivery
of care can be
provided to them.
High Planning for
appropriate
individualized nursing
care
If not done properly
then patient can be
admitted to hospital
for more than 48
hours which can result
into failing of project
Head nurses should
check upon the patient
to nurse ratio, so that
better interventions
can be provided
Low Administration of
chemotherapy (all
This can arise as a
complexity and if
By making use of
multi-disciplinary
9
routes) proper administration
is not being done then
patients have to
handle high
complexity (Sharma
et.al., 2019).
approach highest
quality of care can be
provided to patient.
If all these aspects are being faced by hospital care setting than there are chances that
project can be failed. For this the oncology department can be involved in doing proper planning
related to discharge (Sheikholeslami et.al., 2020). They need to ensure that effective
communication with staff members across settings take place. There should be a proper
alignment of services so that there is continuity of care. Proper discharge management plans are
being made. They can also be involved in analysing potential causes of delays in discharge
procedures. This will assist in making sure that project is huge success. There should also be
adequate involvement of patients and their families in procedures of discharge. Thus, reducing
chances of project failure.
Expected benefits
Before implementing system in oncology department, it is important to assess and find
out impact as well as benefit of it. this is because it gives insight about it. So, it has been
identified that there are several benefits which will be obtained through implementing discharge
process. moreover, there will be a positive impact as well of this process in oncology department
(Ambroggi et.al., 2018). So, it is found that main benefit will be reduction in discharge time and
offering high quality care to patient. Also, the process will fasten discharge process and will
provide support to patient in effective way. In addition, it has been evaluated that process will
benefit nurse and doctor as they will be able to communicate with one another and identify needs
of patient. Thus, it will improve their efficiency as they can engage with patient and ensure that
process discharge process is within less time (Prakash et.al., 2018).
Along with it, process will bring change in discharge time, duration, days, etc leading to
making it easier and effective. So, patient discharge count will be more as compared to
admission one. The process will also support staff of oncology department to focus on patient
palliative care and ensuring its quality. Moreover, discharge process will benefit in enhancing
10
is not being done then
patients have to
handle high
complexity (Sharma
et.al., 2019).
approach highest
quality of care can be
provided to patient.
If all these aspects are being faced by hospital care setting than there are chances that
project can be failed. For this the oncology department can be involved in doing proper planning
related to discharge (Sheikholeslami et.al., 2020). They need to ensure that effective
communication with staff members across settings take place. There should be a proper
alignment of services so that there is continuity of care. Proper discharge management plans are
being made. They can also be involved in analysing potential causes of delays in discharge
procedures. This will assist in making sure that project is huge success. There should also be
adequate involvement of patients and their families in procedures of discharge. Thus, reducing
chances of project failure.
Expected benefits
Before implementing system in oncology department, it is important to assess and find
out impact as well as benefit of it. this is because it gives insight about it. So, it has been
identified that there are several benefits which will be obtained through implementing discharge
process. moreover, there will be a positive impact as well of this process in oncology department
(Ambroggi et.al., 2018). So, it is found that main benefit will be reduction in discharge time and
offering high quality care to patient. Also, the process will fasten discharge process and will
provide support to patient in effective way. In addition, it has been evaluated that process will
benefit nurse and doctor as they will be able to communicate with one another and identify needs
of patient. Thus, it will improve their efficiency as they can engage with patient and ensure that
process discharge process is within less time (Prakash et.al., 2018).
Along with it, process will bring change in discharge time, duration, days, etc leading to
making it easier and effective. So, patient discharge count will be more as compared to
admission one. The process will also support staff of oncology department to focus on patient
palliative care and ensuring its quality. Moreover, discharge process will benefit in enhancing
10
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 17
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





