Report on Indian Health System Meeting Global SDGs Targets
VerifiedAdded on 2023/04/08
|13
|2611
|149
Report
AI Summary
This report provides a comprehensive assessment of the Indian healthcare system's progress in meeting the Sustainable Development Goals (SDGs). It examines key health indicators, including health outcomes, healthcare utilization, nutrition, and determinants of health, within the context of India's socio-economic and political landscape. The report highlights the challenges posed by inadequate funding, infrastructure deficits, and disparities in access to healthcare services, particularly in rural areas. It also discusses the impact of global health initiatives and national health policies on the Indian healthcare system. While acknowledging the progress made in certain areas, such as the elimination of specific diseases, the report emphasizes the need for increased government expenditure on healthcare and improved resource allocation to achieve the SDGs and improve the overall health status of the Indian population. Desklib offers a range of resources including similar reports and solved assignments for students.

Running head: INDIAN HEALTH CARE SYSTEM AND SDGs 1
Report on the Status of Indian Health System in meeting the Global Sustainable Development
Goals (SDGs)
Name
Institution
Report on the Status of Indian Health System in meeting the Global Sustainable Development
Goals (SDGs)
Name
Institution
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
INDIAN HEALTH CARE SYSTEM AND SDGs 2
Report on the Status of Indian Health System in meeting the Global Sustainable
Development Goals (SDGs)
Background
Health policies and health systems in a country play a vital duty in the determination of
how health services are delivered, used, and the results realized. According to Selvaraj and
Karan (2009), the Indian population stands at 1.2 billion people which makes her the second
highest most populous country in the world after China. Economically, India is the 3rd largest
economy when considered in terms of Gross National Income (GNI) as well as the Purchasing
Power Parity (PPP), with the capacity and capability to develop quickly enough to become a
build country. In spite of the stable economic outlook and growth, India's healthcare system fails
to ride along these excellent credentials. The country is composed of 7 union territories and made
up of 29 states which are sub-divided into districts and blocks. Considering a large number of
people, providing adequate health care services becomes a challenge. Since the country gained
independence, the government has been struggling to offer holistic health care services due to the
elaborate measures and resources required to achieve this goal. Providing efficient health care
services requires proper management and resource planning.
Additionally, strong policies need to be made and implemented by government units in
collaboration with the private sector health care providers. This report has reviewed India's
health indicators and how they relate and meet with the Sustainable Development Goals (SDGs).
The signs analyzed are the health outcomes, the utilization of health care services, nutrition,
determinants of health as well as health care institutions.
Report on the Status of Indian Health System in meeting the Global Sustainable
Development Goals (SDGs)
Background
Health policies and health systems in a country play a vital duty in the determination of
how health services are delivered, used, and the results realized. According to Selvaraj and
Karan (2009), the Indian population stands at 1.2 billion people which makes her the second
highest most populous country in the world after China. Economically, India is the 3rd largest
economy when considered in terms of Gross National Income (GNI) as well as the Purchasing
Power Parity (PPP), with the capacity and capability to develop quickly enough to become a
build country. In spite of the stable economic outlook and growth, India's healthcare system fails
to ride along these excellent credentials. The country is composed of 7 union territories and made
up of 29 states which are sub-divided into districts and blocks. Considering a large number of
people, providing adequate health care services becomes a challenge. Since the country gained
independence, the government has been struggling to offer holistic health care services due to the
elaborate measures and resources required to achieve this goal. Providing efficient health care
services requires proper management and resource planning.
Additionally, strong policies need to be made and implemented by government units in
collaboration with the private sector health care providers. This report has reviewed India's
health indicators and how they relate and meet with the Sustainable Development Goals (SDGs).
The signs analyzed are the health outcomes, the utilization of health care services, nutrition,
determinants of health as well as health care institutions.
INDIAN HEALTH CARE SYSTEM AND SDGs 3
The endeavor by India to achieve the SDGs in a proper and timely fashion is vital not just
for the country's economic development but also for the entire world. This is significant because
of India's high population size as well as the enormous inequalities in the demographic and
socio-economic parameters all over the nation. Although it is one of the largest and fastest
growing economies in the world, the country's human development index is lower when
compared to those of other developing countries like China, Brazil, South Africa, and Russia.
India is the most significant contributor to the world under five deaths for the last four decades
recording over 1.2 million under-five deaths in 2015 which is over six times more than China. To
add to this, India is among the top five countries in the world with over 60% of its population
living in extreme poverty. As at the 2011 census, the ratio of poverty head in India was 22%
which has significantly been caused by the widespread hunger based on research done by
Ramani and Mavalankar (2006).
System of Governance, Policies and Impacts on the Health Care System
The federal nature of India's system of government has devolved the management,
governance, and operations of the country's health system between the union and the state
governments. In India, there is a mixed system of health care which includes the public and
private service sector providers. The health care system is categorized into primary, secondary
and tertiary levels. Most of the urban areas are served by the private health care providers who
cater to the secondary and tertiary needs. On the other hand, the rural areas are mainly served by
the public health care providers who are developed in the three-tier system by the norms of the
population. An ideal health care system is composed of four main components (Chatterjee,
Kakkar and Chaturvedi, 2016). They are universal access, equitable distribution of financial
The endeavor by India to achieve the SDGs in a proper and timely fashion is vital not just
for the country's economic development but also for the entire world. This is significant because
of India's high population size as well as the enormous inequalities in the demographic and
socio-economic parameters all over the nation. Although it is one of the largest and fastest
growing economies in the world, the country's human development index is lower when
compared to those of other developing countries like China, Brazil, South Africa, and Russia.
India is the most significant contributor to the world under five deaths for the last four decades
recording over 1.2 million under-five deaths in 2015 which is over six times more than China. To
add to this, India is among the top five countries in the world with over 60% of its population
living in extreme poverty. As at the 2011 census, the ratio of poverty head in India was 22%
which has significantly been caused by the widespread hunger based on research done by
Ramani and Mavalankar (2006).
System of Governance, Policies and Impacts on the Health Care System
The federal nature of India's system of government has devolved the management,
governance, and operations of the country's health system between the union and the state
governments. In India, there is a mixed system of health care which includes the public and
private service sector providers. The health care system is categorized into primary, secondary
and tertiary levels. Most of the urban areas are served by the private health care providers who
cater to the secondary and tertiary needs. On the other hand, the rural areas are mainly served by
the public health care providers who are developed in the three-tier system by the norms of the
population. An ideal health care system is composed of four main components (Chatterjee,
Kakkar and Chaturvedi, 2016). They are universal access, equitable distribution of financial
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
INDIAN HEALTH CARE SYSTEM AND SDGs 4
expenses, competent service providers and also special attention to vulnerable groups like
women, the aged, children, and people with disabilities.
Most of the Indian people are found in the rural areas where they live in poverty and
hence lack enough resources to take care of their health expenses. The state of the public sector
health care facilities is reduced and as such not able to provide proper health services. This is
mainly because the public sector is underfinanced and underdeveloped by the government
thereby leaving the private sector providing services to most of the people in the country.
According to Nabyonga-Orem (2017) data collected shows that the patients usually bear most of
the health care expenses and costs in the country.
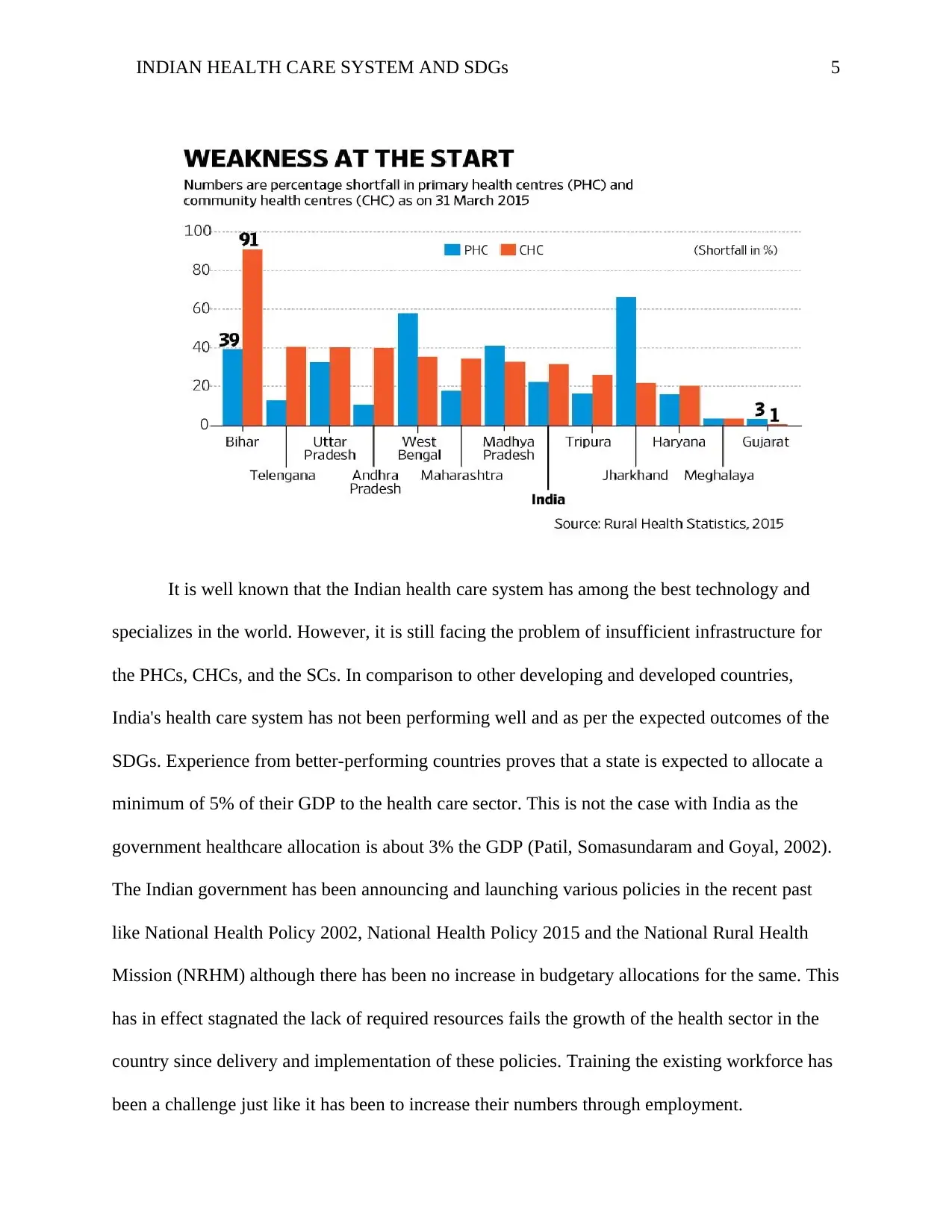
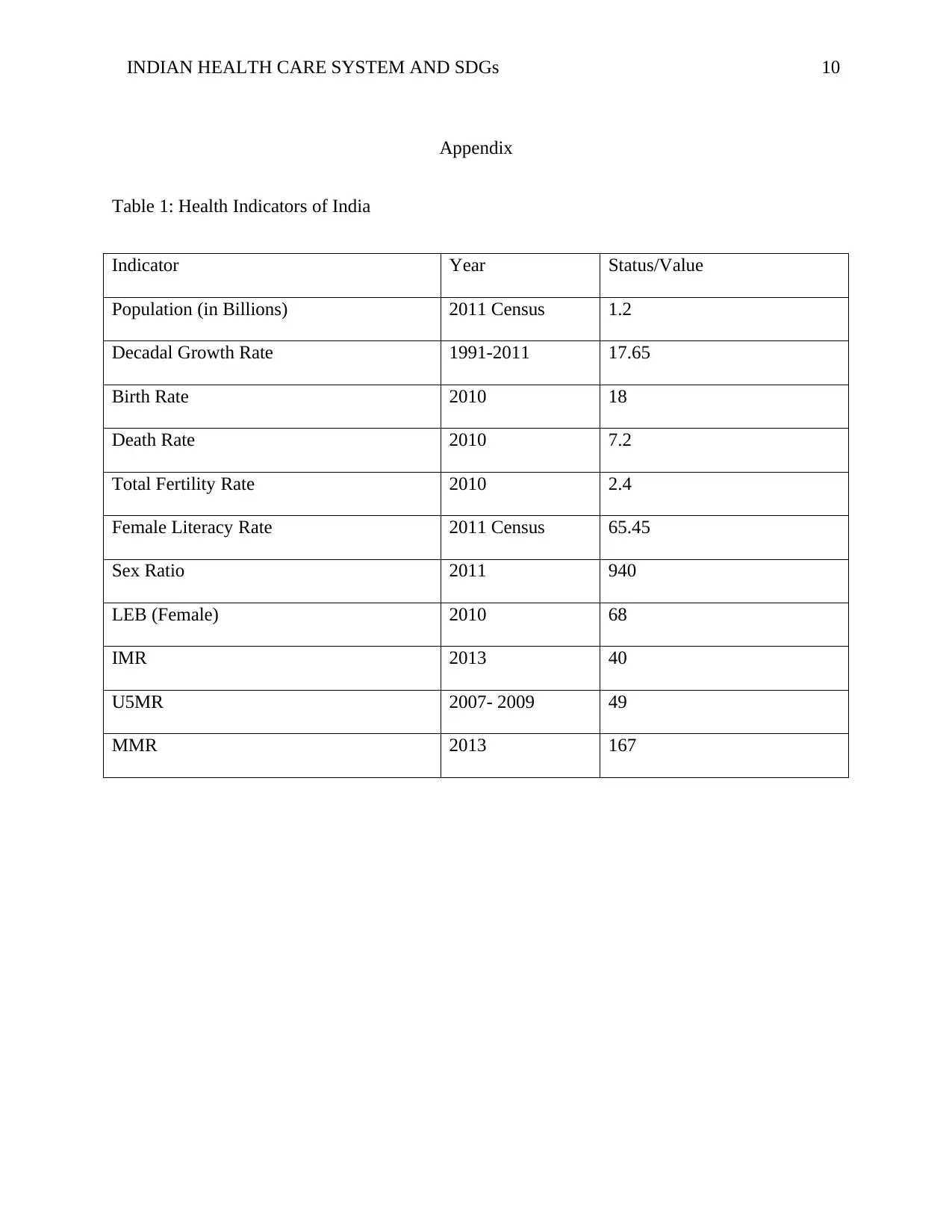
Data from NFHS-3 states that the Indian private health care sector is the primary provider
of health services for over 70% of the households nationally. This is further worsened by the fact
that over 40% of Indian children are malnourished with both maternal and child mortality rates
higher than other developing countries. This data is summarized in table 1. The reasons behind
the poor quality of health care services provided by the public health care providers because of
the distance and inaccessibility of primary health centers (PHCs), community health centers
(CHCs), and sub-centers (SCs). The above data is summarized through the graph below from
Rural Health Statistics 2015 with the overall national percentage falling to 21% for PHCs and
32% for CHCs (Reddy 2016).
expenses, competent service providers and also special attention to vulnerable groups like
women, the aged, children, and people with disabilities.
Most of the Indian people are found in the rural areas where they live in poverty and
hence lack enough resources to take care of their health expenses. The state of the public sector
health care facilities is reduced and as such not able to provide proper health services. This is
mainly because the public sector is underfinanced and underdeveloped by the government
thereby leaving the private sector providing services to most of the people in the country.
According to Nabyonga-Orem (2017) data collected shows that the patients usually bear most of
the health care expenses and costs in the country.
Data from NFHS-3 states that the Indian private health care sector is the primary provider
of health services for over 70% of the households nationally. This is further worsened by the fact
that over 40% of Indian children are malnourished with both maternal and child mortality rates
higher than other developing countries. This data is summarized in table 1. The reasons behind
the poor quality of health care services provided by the public health care providers because of
the distance and inaccessibility of primary health centers (PHCs), community health centers
(CHCs), and sub-centers (SCs). The above data is summarized through the graph below from
Rural Health Statistics 2015 with the overall national percentage falling to 21% for PHCs and
32% for CHCs (Reddy 2016).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
INDIAN HEALTH CARE SYSTEM AND SDGs 5
It is well known that the Indian health care system has among the best technology and
specializes in the world. However, it is still facing the problem of insufficient infrastructure for
the PHCs, CHCs, and the SCs. In comparison to other developing and developed countries,
India's health care system has not been performing well and as per the expected outcomes of the
SDGs. Experience from better-performing countries proves that a state is expected to allocate a
minimum of 5% of their GDP to the health care sector. This is not the case with India as the
government healthcare allocation is about 3% the GDP (Patil, Somasundaram and Goyal, 2002).
The Indian government has been announcing and launching various policies in the recent past
like National Health Policy 2002, National Health Policy 2015 and the National Rural Health
Mission (NRHM) although there has been no increase in budgetary allocations for the same. This
has in effect stagnated the lack of required resources fails the growth of the health sector in the
country since delivery and implementation of these policies. Training the existing workforce has
been a challenge just like it has been to increase their numbers through employment.
It is well known that the Indian health care system has among the best technology and
specializes in the world. However, it is still facing the problem of insufficient infrastructure for
the PHCs, CHCs, and the SCs. In comparison to other developing and developed countries,
India's health care system has not been performing well and as per the expected outcomes of the
SDGs. Experience from better-performing countries proves that a state is expected to allocate a
minimum of 5% of their GDP to the health care sector. This is not the case with India as the
government healthcare allocation is about 3% the GDP (Patil, Somasundaram and Goyal, 2002).
The Indian government has been announcing and launching various policies in the recent past
like National Health Policy 2002, National Health Policy 2015 and the National Rural Health
Mission (NRHM) although there has been no increase in budgetary allocations for the same. This
has in effect stagnated the lack of required resources fails the growth of the health sector in the
country since delivery and implementation of these policies. Training the existing workforce has
been a challenge just like it has been to increase their numbers through employment.
INDIAN HEALTH CARE SYSTEM AND SDGs 6
Government Expenditure on Health Care
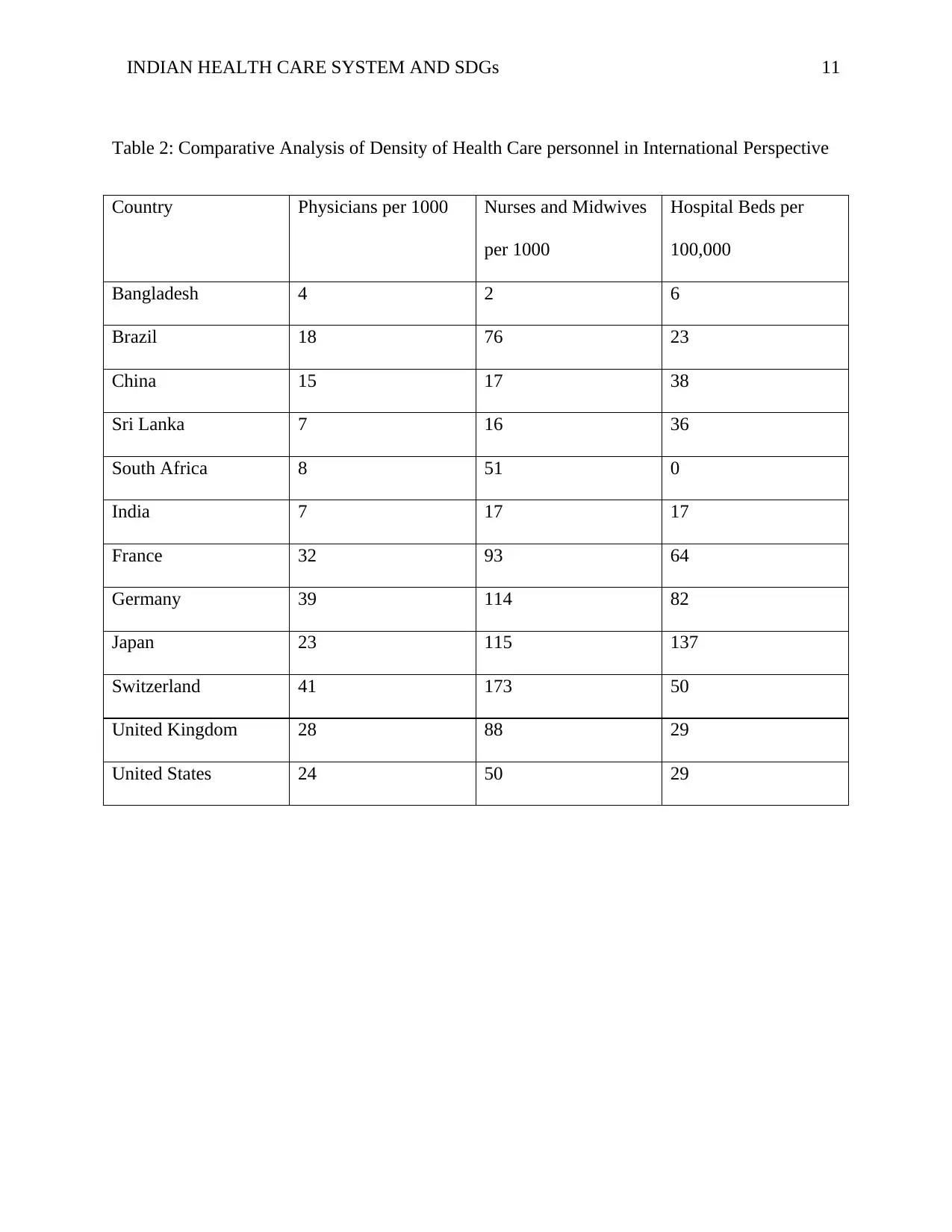
In comparison with the BRIC nations, India is outperformed by Brazil, China, and Russia
in terms of universal health coverage with all these nations spending over 6% of their GDPs on
healthcare. When compared to the developed nations and some developing countries, India is
lagging in the sector of health status, the per capita health expenditures and public health
expenditures. Additionally, the infrastructure is outdated and worn out. The outpatient numbers
compared to the doctors and facilities is very high (Balarajan, Selvaraj and Subramanian, 2011).
This comparison can be found as a summary in table 2 of the appendix.
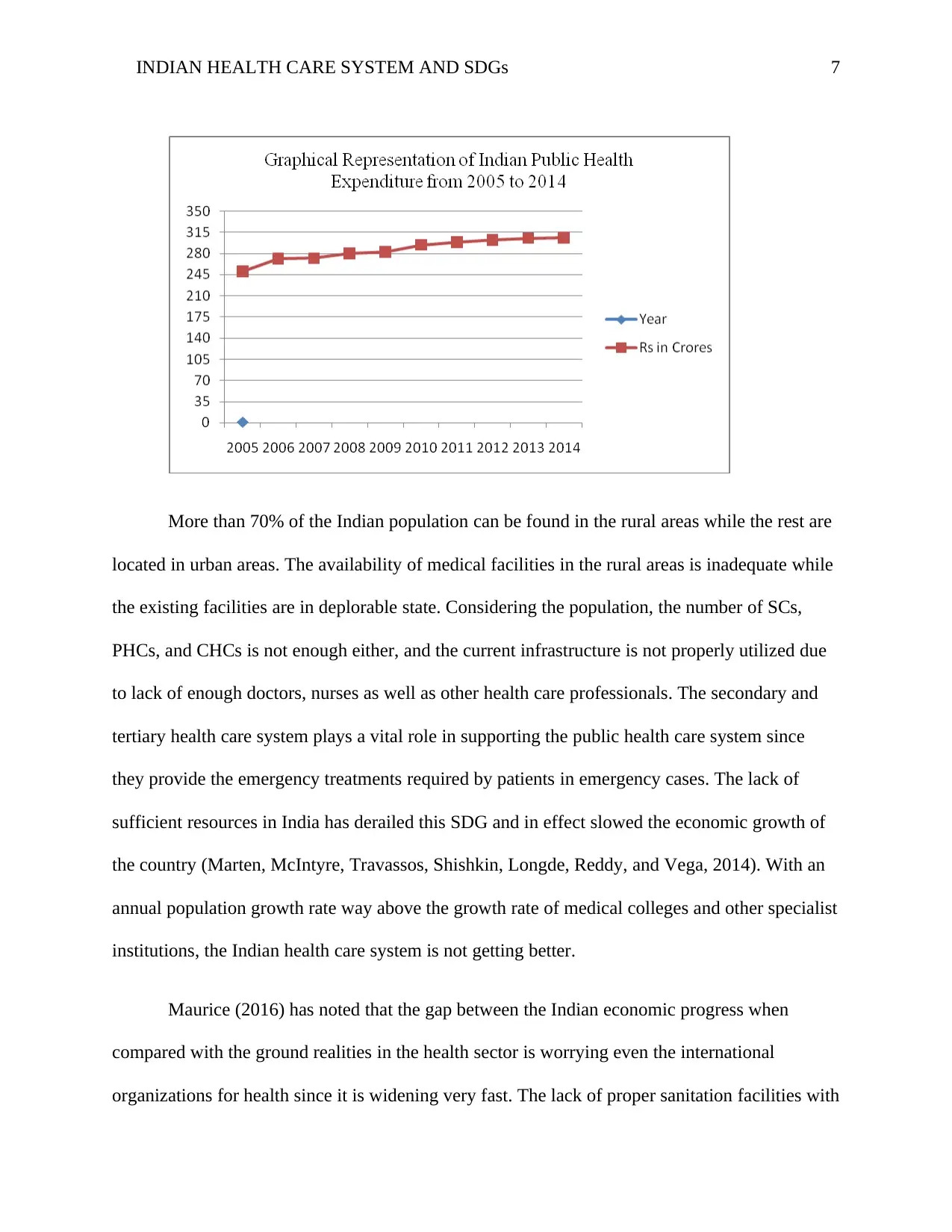
India lacks referral transport services and the laboratory services are not enough shown in
the NRHM, Second Common Review Mission Report of 2009. Therefore, there is an urgent
demand to improve on the number of public health expenditure to cater to all these underlying
issues. The graph below is a summary of the Indian expenditure on public health over a 10 year
period sourced from the Journal of health organization and management by Ramani and
Mavalankar (2006). The expenditure has been increasing at a very low margin which is why
there has been very minimal progress in the country's health sector.
Government Expenditure on Health Care
In comparison with the BRIC nations, India is outperformed by Brazil, China, and Russia
in terms of universal health coverage with all these nations spending over 6% of their GDPs on
healthcare. When compared to the developed nations and some developing countries, India is
lagging in the sector of health status, the per capita health expenditures and public health
expenditures. Additionally, the infrastructure is outdated and worn out. The outpatient numbers
compared to the doctors and facilities is very high (Balarajan, Selvaraj and Subramanian, 2011).
This comparison can be found as a summary in table 2 of the appendix.
India lacks referral transport services and the laboratory services are not enough shown in
the NRHM, Second Common Review Mission Report of 2009. Therefore, there is an urgent
demand to improve on the number of public health expenditure to cater to all these underlying
issues. The graph below is a summary of the Indian expenditure on public health over a 10 year
period sourced from the Journal of health organization and management by Ramani and
Mavalankar (2006). The expenditure has been increasing at a very low margin which is why
there has been very minimal progress in the country's health sector.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
INDIAN HEALTH CARE SYSTEM AND SDGs 7
More than 70% of the Indian population can be found in the rural areas while the rest are
located in urban areas. The availability of medical facilities in the rural areas is inadequate while
the existing facilities are in deplorable state. Considering the population, the number of SCs,
PHCs, and CHCs is not enough either, and the current infrastructure is not properly utilized due
to lack of enough doctors, nurses as well as other health care professionals. The secondary and
tertiary health care system plays a vital role in supporting the public health care system since
they provide the emergency treatments required by patients in emergency cases. The lack of
sufficient resources in India has derailed this SDG and in effect slowed the economic growth of
the country (Marten, McIntyre, Travassos, Shishkin, Longde, Reddy, and Vega, 2014). With an
annual population growth rate way above the growth rate of medical colleges and other specialist
institutions, the Indian health care system is not getting better.
Maurice (2016) has noted that the gap between the Indian economic progress when
compared with the ground realities in the health sector is worrying even the international
organizations for health since it is widening very fast. The lack of proper sanitation facilities with
More than 70% of the Indian population can be found in the rural areas while the rest are
located in urban areas. The availability of medical facilities in the rural areas is inadequate while
the existing facilities are in deplorable state. Considering the population, the number of SCs,
PHCs, and CHCs is not enough either, and the current infrastructure is not properly utilized due
to lack of enough doctors, nurses as well as other health care professionals. The secondary and
tertiary health care system plays a vital role in supporting the public health care system since
they provide the emergency treatments required by patients in emergency cases. The lack of
sufficient resources in India has derailed this SDG and in effect slowed the economic growth of
the country (Marten, McIntyre, Travassos, Shishkin, Longde, Reddy, and Vega, 2014). With an
annual population growth rate way above the growth rate of medical colleges and other specialist
institutions, the Indian health care system is not getting better.
Maurice (2016) has noted that the gap between the Indian economic progress when
compared with the ground realities in the health sector is worrying even the international
organizations for health since it is widening very fast. The lack of proper sanitation facilities with
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
INDIAN HEALTH CARE SYSTEM AND SDGs 8
over 60% of Indians lacking access to toilets and over 250 million people living without
electricity further proves the worse case of the healthcare system.
Reddy (2016) and Selvaraj and Karan (2009) agree that all these scenarios can be
summed up and attributed to the fact that Indian government allocates less than 3% of its GDP to
the health care sector in their annual budget. This is many times below the global average of 6%
and the recommended proportion of 5-6%. As a result, India continues to lag in the global SDG
ranking in spite of being in one of the best position to be among the top. India has the potential to
perform better and achieve the SDGs if the health allocation and expenditure is increased by
1.2% annually until 2025. However, it is also good to note that India has made some
commendable progress and achievements in several areas. Such areas include the complete
elimination of kala-azar and filariasis in 2017, elimination of leprosy in 2018 as well as the
planned complete elimination of tuberculosis by 2025.
Impact of Global Health Initiatives
Indian health care system has benefitted from various global health initiatives. An
example is the Public Health Foundation of India which is a public-private initiative which is
composed of multiple institutions that collaborate and consult with numerous constituencies like
the Indian and international medical academics, state and central governments, multi and
bilateral agencies as well as civil society groups. The initiative is aimed at addressing the
challenges of institutional capacities in India by training the professionals, strengthening policy
development and research in the public health care sector (Marten, McIntyre, Travassos,
Shishkin, Longde, Reddy, and Vega, 2014).
over 60% of Indians lacking access to toilets and over 250 million people living without
electricity further proves the worse case of the healthcare system.
Reddy (2016) and Selvaraj and Karan (2009) agree that all these scenarios can be
summed up and attributed to the fact that Indian government allocates less than 3% of its GDP to
the health care sector in their annual budget. This is many times below the global average of 6%
and the recommended proportion of 5-6%. As a result, India continues to lag in the global SDG
ranking in spite of being in one of the best position to be among the top. India has the potential to
perform better and achieve the SDGs if the health allocation and expenditure is increased by
1.2% annually until 2025. However, it is also good to note that India has made some
commendable progress and achievements in several areas. Such areas include the complete
elimination of kala-azar and filariasis in 2017, elimination of leprosy in 2018 as well as the
planned complete elimination of tuberculosis by 2025.
Impact of Global Health Initiatives
Indian health care system has benefitted from various global health initiatives. An
example is the Public Health Foundation of India which is a public-private initiative which is
composed of multiple institutions that collaborate and consult with numerous constituencies like
the Indian and international medical academics, state and central governments, multi and
bilateral agencies as well as civil society groups. The initiative is aimed at addressing the
challenges of institutional capacities in India by training the professionals, strengthening policy
development and research in the public health care sector (Marten, McIntyre, Travassos,
Shishkin, Longde, Reddy, and Vega, 2014).
INDIAN HEALTH CARE SYSTEM AND SDGs 9
Another global health care initiative that has had substantial influence in India is the
Global Healthcare Information Network (GHI-net). This initiative aims at helping health care
professionals to deliver services more effectively and professionally through creating,
exchanging and using health care information. This group focuses on the health status in low and
middle earning nations and provides online forums for promoting communication and sharing of
knowledge. In a positive and encouraging move, the Indian health care system has shown an
increase in health and wellness facilities as a result of the shift in focus from primary health and
towards universal health coverage. With increased emphasis on preventive care, digital care, and
improved nutrition, this policy is expected to have long term positive implications. In 2013 there
was a merger between the National Urban Health Mission and the National Rural Health Mission
to form The National Health Mission (NHM) as a health initiative that was geared towards the
global communicable disease control, prevention, and surveillance and eradication (Marten,
McIntyre, Travassos, Shishkin, Longde, Reddy, and Vega, 2014).
Conclusion and Recommendations
It is the right time for the Indian government to adequately fund and fully implement the
various health policies already recommended and therefore make them beneficial to the people.
Every person has the right to health care, but lack of adequate and qualified nurses, doctors and
other health professionals coupled with inadequate health facilities as it is the case in India only
thwarts the availability to the people.
Another global health care initiative that has had substantial influence in India is the
Global Healthcare Information Network (GHI-net). This initiative aims at helping health care
professionals to deliver services more effectively and professionally through creating,
exchanging and using health care information. This group focuses on the health status in low and
middle earning nations and provides online forums for promoting communication and sharing of
knowledge. In a positive and encouraging move, the Indian health care system has shown an
increase in health and wellness facilities as a result of the shift in focus from primary health and
towards universal health coverage. With increased emphasis on preventive care, digital care, and
improved nutrition, this policy is expected to have long term positive implications. In 2013 there
was a merger between the National Urban Health Mission and the National Rural Health Mission
to form The National Health Mission (NHM) as a health initiative that was geared towards the
global communicable disease control, prevention, and surveillance and eradication (Marten,
McIntyre, Travassos, Shishkin, Longde, Reddy, and Vega, 2014).
Conclusion and Recommendations
It is the right time for the Indian government to adequately fund and fully implement the
various health policies already recommended and therefore make them beneficial to the people.
Every person has the right to health care, but lack of adequate and qualified nurses, doctors and
other health professionals coupled with inadequate health facilities as it is the case in India only
thwarts the availability to the people.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
INDIAN HEALTH CARE SYSTEM AND SDGs 10
Appendix
Table 1: Health Indicators of India
Indicator Year Status/Value
Population (in Billions) 2011 Census 1.2
Decadal Growth Rate 1991-2011 17.65
Birth Rate 2010 18
Death Rate 2010 7.2
Total Fertility Rate 2010 2.4
Female Literacy Rate 2011 Census 65.45
Sex Ratio 2011 940
LEB (Female) 2010 68
IMR 2013 40
U5MR 2007- 2009 49
MMR 2013 167
Appendix
Table 1: Health Indicators of India
Indicator Year Status/Value
Population (in Billions) 2011 Census 1.2
Decadal Growth Rate 1991-2011 17.65
Birth Rate 2010 18
Death Rate 2010 7.2
Total Fertility Rate 2010 2.4
Female Literacy Rate 2011 Census 65.45
Sex Ratio 2011 940
LEB (Female) 2010 68
IMR 2013 40
U5MR 2007- 2009 49
MMR 2013 167
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
INDIAN HEALTH CARE SYSTEM AND SDGs 11
Table 2: Comparative Analysis of Density of Health Care personnel in International Perspective
Country Physicians per 1000 Nurses and Midwives
per 1000
Hospital Beds per
100,000
Bangladesh 4 2 6
Brazil 18 76 23
China 15 17 38
Sri Lanka 7 16 36
South Africa 8 51 0
India 7 17 17
France 32 93 64
Germany 39 114 82
Japan 23 115 137
Switzerland 41 173 50
United Kingdom 28 88 29
United States 24 50 29
Table 2: Comparative Analysis of Density of Health Care personnel in International Perspective
Country Physicians per 1000 Nurses and Midwives
per 1000
Hospital Beds per
100,000
Bangladesh 4 2 6
Brazil 18 76 23
China 15 17 38
Sri Lanka 7 16 36
South Africa 8 51 0
India 7 17 17
France 32 93 64
Germany 39 114 82
Japan 23 115 137
Switzerland 41 173 50
United Kingdom 28 88 29
United States 24 50 29
INDIAN HEALTH CARE SYSTEM AND SDGs 12
References
Balarajan, Y., Selvaraj, S., & Subramanian, S. V. (2011). Health care and equity in India. The
Lancet, 377(9764), 505-515.
Chatterjee, P., Kakkar, M., & Chaturvedi, S. (2016). Integrating one health in national health
policies of developing countries: India’s lost opportunities. Infectious diseases of poverty,
5(1), 87.
Clifford, K. L., & Zaman, M. H. (2016). Engineering, global health, and inclusive innovation:
focus on partnership, system strengthening, and local impact for SDGs. Global health
action, 9(1), 30175.
De Costa, A., & Diwan, V. (2007). ‘Where is the public health sector?’: Public and private sector
healthcare provision in Madhya Pradesh, India. Health Policy, 84(2-3), 269-276.
Malhotra, C., & Do, Y. K. (2012). Socio-economic disparities in health system responsiveness in
India. Health policy and planning, 28(2), 197-205.
Marten, R., McIntyre, D., Travassos, C., Shishkin, S., Longde, W., Reddy, S., & Vega, J. (2014).
An assessment of progress towards universal health coverage in Brazil, Russia, India,
China, and South Africa (BRICS). The Lancet, 384(9960), 2164-2171.
Maurice, J. (2016). Measuring progress towards the SDGs—a new vital science. The Lancet,
388(10053), 1455-1458.
Mukherjee, K. (2016). MDGs to SDGs: lessons for UHC for India. Global Journal of Medicine
and Public Health, 5(4), 1-3.
References
Balarajan, Y., Selvaraj, S., & Subramanian, S. V. (2011). Health care and equity in India. The
Lancet, 377(9764), 505-515.
Chatterjee, P., Kakkar, M., & Chaturvedi, S. (2016). Integrating one health in national health
policies of developing countries: India’s lost opportunities. Infectious diseases of poverty,
5(1), 87.
Clifford, K. L., & Zaman, M. H. (2016). Engineering, global health, and inclusive innovation:
focus on partnership, system strengthening, and local impact for SDGs. Global health
action, 9(1), 30175.
De Costa, A., & Diwan, V. (2007). ‘Where is the public health sector?’: Public and private sector
healthcare provision in Madhya Pradesh, India. Health Policy, 84(2-3), 269-276.
Malhotra, C., & Do, Y. K. (2012). Socio-economic disparities in health system responsiveness in
India. Health policy and planning, 28(2), 197-205.
Marten, R., McIntyre, D., Travassos, C., Shishkin, S., Longde, W., Reddy, S., & Vega, J. (2014).
An assessment of progress towards universal health coverage in Brazil, Russia, India,
China, and South Africa (BRICS). The Lancet, 384(9960), 2164-2171.
Maurice, J. (2016). Measuring progress towards the SDGs—a new vital science. The Lancet,
388(10053), 1455-1458.
Mukherjee, K. (2016). MDGs to SDGs: lessons for UHC for India. Global Journal of Medicine
and Public Health, 5(4), 1-3.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





