Fall Risk Factors in Community-Dwelling Elderly Depending on Their Physical Function, Cognitive Status and Symptoms of Depression
VerifiedAdded on 2022/10/04
|11
|6513
|465
AI Summary
The study analyzes fall risk factors in community-dwelling elderly depending on their physical function, cognitive status and symptoms of depression. The incidence of falls may significantly increase in people with a lower functional status, which may be related to cognitive process disturbances and lower affective functioning. A comprehensive geriatric assessment, related to all aspects of advanced-age patients’ efficiency, is recommended.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
Int. J. Environ. Res. Public Health 2015, 12, 3406-3416; doi:10.3390/ijerph120403406
International Journal of
Environmental Research and
Public Health
ISSN 1660-4601
www.mdpi.com/journal/ijerph
Article
Fall Risk Factors in Community-Dwelling Elderly Depending
on Their Physical Function, Cognitive Status and Symptoms
of Depression
Magdalena Sylwia Kamińska 1,*, Jacek Brodowski 1 and Beata Karakiewicz 2
1 Department of Primary Health Care, Faculty of Health Sciences, Pomeranian Medical University in
Szczecin, 48 Żołnierska St., 71-210 Szczecin, Poland; E-Mail: jabrod@wp.pl
2 Public Health Department, Faculty of Health Sciences, Pomeranian Medical University in Szczecin,
48 Żołnierska St., 71-210 Szczecin, Poland; E-Mail: karabea@pum.edu.pl
* Author to whom correspondence should be addressed; E-Mail: magdalena.kaminska@pum.edu.pl;
Tel.: +48-91-00-920.
Academic Editor: Paul B. Tchounwou
Received: 3 November 2014 / Accepted: 11 March 2015 / Published: 24 March 2015
Abstract: Falls are the leading cause of unintentional injuries and injury-related disability,
morbidity and mortality in the geriatric population. Therefore, they may also lower quality
of life. The aim of this study was to analyze the fall risk factors in the community-dwelling
elderly depending on their physical function, cognitive status and symptoms of depression.
The study involved 304 individuals aged 65–100 years with a mean age of 78.6 ± 7.4.
This survey-based study was conducted using the Geriatric Environmental Inquiry,
the Barthel Scale (BS), the Abbreviated Mental Test Score (AMTS), the Geriatric Depression
Scale (GDS) and the Tinetti Test (TT). There was a statistically significant correlation
between the BS, the TT and the incidence of falls (p < 0.05). The number of falls
correlated significantly with the results of the BS (R = −0.39), the GDS (R = 0.18),
and the TT (R = −0.40). A statistically significant correlation was also noted between the
TT results and the results of the BS (R = 0.77), the AMTS (R = 0.40) and the GDS
(R = −0.37). The incidence of falls may significantly increase in people with a lower
functional status, which may be related to cognitive process disturbances and lower
affective functioning. A comprehensive geriatric assessment, related to all aspects of
OPEN ACCESS
International Journal of
Environmental Research and
Public Health
ISSN 1660-4601
www.mdpi.com/journal/ijerph
Article
Fall Risk Factors in Community-Dwelling Elderly Depending
on Their Physical Function, Cognitive Status and Symptoms
of Depression
Magdalena Sylwia Kamińska 1,*, Jacek Brodowski 1 and Beata Karakiewicz 2
1 Department of Primary Health Care, Faculty of Health Sciences, Pomeranian Medical University in
Szczecin, 48 Żołnierska St., 71-210 Szczecin, Poland; E-Mail: jabrod@wp.pl
2 Public Health Department, Faculty of Health Sciences, Pomeranian Medical University in Szczecin,
48 Żołnierska St., 71-210 Szczecin, Poland; E-Mail: karabea@pum.edu.pl
* Author to whom correspondence should be addressed; E-Mail: magdalena.kaminska@pum.edu.pl;
Tel.: +48-91-00-920.
Academic Editor: Paul B. Tchounwou
Received: 3 November 2014 / Accepted: 11 March 2015 / Published: 24 March 2015
Abstract: Falls are the leading cause of unintentional injuries and injury-related disability,
morbidity and mortality in the geriatric population. Therefore, they may also lower quality
of life. The aim of this study was to analyze the fall risk factors in the community-dwelling
elderly depending on their physical function, cognitive status and symptoms of depression.
The study involved 304 individuals aged 65–100 years with a mean age of 78.6 ± 7.4.
This survey-based study was conducted using the Geriatric Environmental Inquiry,
the Barthel Scale (BS), the Abbreviated Mental Test Score (AMTS), the Geriatric Depression
Scale (GDS) and the Tinetti Test (TT). There was a statistically significant correlation
between the BS, the TT and the incidence of falls (p < 0.05). The number of falls
correlated significantly with the results of the BS (R = −0.39), the GDS (R = 0.18),
and the TT (R = −0.40). A statistically significant correlation was also noted between the
TT results and the results of the BS (R = 0.77), the AMTS (R = 0.40) and the GDS
(R = −0.37). The incidence of falls may significantly increase in people with a lower
functional status, which may be related to cognitive process disturbances and lower
affective functioning. A comprehensive geriatric assessment, related to all aspects of
OPEN ACCESS
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Int. J. Environ. Res. Public Health 2015, 12 3407
advanced-age patients’ efficiency, is recommended. Fall prevention strategies should
include actions undertaken to evaluate and treat depression and cognitive disturbances.
Keywords: elderly falls; functional state; cognitive function; depression
1. Introduction
According to the definition accepted for the purpose of epidemiological research, a fall is an event
which results in a person coming to rest inadvertently on the ground or floor or other lower level [1].
Epidemiological statistics indicate that every year falls happen to about 30% of adults aged over 65
and living in their own homes. However, about 50% of them don’t talk about their falls either to their
caregivers or medical staff. What is more, elderly people staying in residential homes experience falls
more often than those living in their own homes. Every year, falls happen to about 45% of people
provided with long-term care, out of whom 40% experience multiple falls [1–3].
Among older adults, falls are the leading cause of both fatal and nonfatal injuries. The consequences of
fall-related injuries among over 65-year-olds include: long-lasting disability, loss of autonomy,
lower quality of life, and problems with organizing professional and non-professional care for this
group of patients. Falls are the main cause of injury-related disability, morbidity and mortality in
geriatric people [1–6].
In member countries of the European Union, the problem of injuries affects about 105,000 people.
Furthermore, nearly 40,000 elderly people are pronounced dead due to falls. The rate of fall-related
fatal injuries among those aged 60 or older is 36.8 per 100,000 in the United States, whereas in Canada
it is 9.4 per 10,000 in the same age group [1].
In 2013, over 2,000,000 non-fatal injuries were treated in emergency departments, and more than
700,000 of them required hospitalization [4]. The hospital admission rate for injuries caused by falls
among people over 60 and older in Australia, Canada, the United Kingdom of Great Britain and
Northern Ireland is 1.6–3.0 per 10,000 citizens. In Western Australia and Great Britain, it is as high as
5.5–8.9 per 10,000 people. The most common fall-related causes of admission to hospital are hip joint
fractures, traumatic brain injuries, and injuries to the upper extremities. It is also worth emphasizing
that, in the case of the elderly, the period of hospitalization due to falls is considerably longer than
hospitalization for other reasons [1].
Moreover, fall-related injuries among over 65-year-olds generate high costs for the health care and
welfare sectors. In 2012, the direct medical costs of injuries caused by falls among people over 65 years
of age, adjusted for inflation, was 30 billion dollars [1–7].
The incidence of falls rises with age and the worsening of general fitness. Regardless of the reasons,
falls in advanced age have serious physical, mental, and socio-economic consequences. Falls usually
result from the interaction and interference of factors categorized in four domains: biological,
behavioral, environmental, and socio-economic [1].
Biological fall risk factors include fixed factors, such as age, gender, and race, and are closely related to
involution changes and morbidity, which impair the functioning of the “postural control system” defined
as internal causes of falls. External causes include behavioral, environmental, and socioeconomic
advanced-age patients’ efficiency, is recommended. Fall prevention strategies should
include actions undertaken to evaluate and treat depression and cognitive disturbances.
Keywords: elderly falls; functional state; cognitive function; depression
1. Introduction
According to the definition accepted for the purpose of epidemiological research, a fall is an event
which results in a person coming to rest inadvertently on the ground or floor or other lower level [1].
Epidemiological statistics indicate that every year falls happen to about 30% of adults aged over 65
and living in their own homes. However, about 50% of them don’t talk about their falls either to their
caregivers or medical staff. What is more, elderly people staying in residential homes experience falls
more often than those living in their own homes. Every year, falls happen to about 45% of people
provided with long-term care, out of whom 40% experience multiple falls [1–3].
Among older adults, falls are the leading cause of both fatal and nonfatal injuries. The consequences of
fall-related injuries among over 65-year-olds include: long-lasting disability, loss of autonomy,
lower quality of life, and problems with organizing professional and non-professional care for this
group of patients. Falls are the main cause of injury-related disability, morbidity and mortality in
geriatric people [1–6].
In member countries of the European Union, the problem of injuries affects about 105,000 people.
Furthermore, nearly 40,000 elderly people are pronounced dead due to falls. The rate of fall-related
fatal injuries among those aged 60 or older is 36.8 per 100,000 in the United States, whereas in Canada
it is 9.4 per 10,000 in the same age group [1].
In 2013, over 2,000,000 non-fatal injuries were treated in emergency departments, and more than
700,000 of them required hospitalization [4]. The hospital admission rate for injuries caused by falls
among people over 60 and older in Australia, Canada, the United Kingdom of Great Britain and
Northern Ireland is 1.6–3.0 per 10,000 citizens. In Western Australia and Great Britain, it is as high as
5.5–8.9 per 10,000 people. The most common fall-related causes of admission to hospital are hip joint
fractures, traumatic brain injuries, and injuries to the upper extremities. It is also worth emphasizing
that, in the case of the elderly, the period of hospitalization due to falls is considerably longer than
hospitalization for other reasons [1].
Moreover, fall-related injuries among over 65-year-olds generate high costs for the health care and
welfare sectors. In 2012, the direct medical costs of injuries caused by falls among people over 65 years
of age, adjusted for inflation, was 30 billion dollars [1–7].
The incidence of falls rises with age and the worsening of general fitness. Regardless of the reasons,
falls in advanced age have serious physical, mental, and socio-economic consequences. Falls usually
result from the interaction and interference of factors categorized in four domains: biological,
behavioral, environmental, and socio-economic [1].
Biological fall risk factors include fixed factors, such as age, gender, and race, and are closely related to
involution changes and morbidity, which impair the functioning of the “postural control system” defined
as internal causes of falls. External causes include behavioral, environmental, and socioeconomic
Int. J. Environ. Res. Public Health 2015, 12 3408
factors. Behavioral fall risk factors are potentially modifiable, and include such issues as alcohol
abuse, using inappropriate shoes, as well as physical inactivity. Behavioral factors also include
polypharmacotherapy, and not taking into account the differences in drug pharmacokinetics and
pharmacodynamics in the organism of an old person. Environmental factors refer to the development of
private and public spaces (uneven terrain, architectural obstacles, and problems with transport).
Socio-economic issues are: low income, low standard of living, limited access to health and
social services, and the lack of social support [1].
Identification of the main fall risk factors may contribute to the implementation of preventive
actions reducing the incidence of falls. These actions should form a part of an interdisciplinary process
aiming at compensation of deficits in all spheres of human functioning. The specificity of geriatrics
necessitates the provision of an overall solution to the problems of advanced-age patients. Therefore,
the therapeutic and nursing management in the case of the elderly should be based on a comprehensive
geriatric assessment (CGA). The literature describes a number of functional tests used to assess the
risk of falls in people of advanced age. Their availability, the short time required for their execution,
and the possibility of using them in any conditions, mean that they can be also applied on an outpatient
basis [8]. The aim of this study was to analyze the fall risk factors in the community-dwelling elderly
depending on their physical function, cognitive status and symptoms of depression.
2. Materials and Methods
2.1. Ethics Statement
All subjects gave their informed consent for inclusion before they participated in the study.
The study was conducted in accordance with the Declaration of Helsinki, and the protocol was
approved by the Ethics Committee of the Pomeranian Medical University in Szczecin, Poland
(KB-0080/141/09).
2.2. Sample Size
The study involved 304 people aged 65–100 years, using outpatient health services provided by
The Regional Centre of Occupational Medicine - West Pomeranian Prevention and Therapy Centre
in Szczecin, North West Poland. Women constituted 77.3% of those analyzed, men −22.7%. The mean
age was 78.6 ± 7.4.
2.3. Participants and Recruitment
Principal criteria for the selection of participants were: the availability of the patients at the moment
of carrying out the study, no symptoms of the exacerbation of the co-existing diseases or other health
problems, the mental condition of the patients making them able to cooperate during the study and
understand the orders of the researcher, the ability of the surveyed to move without assistance,
as well as conscious and voluntary consent to participate in the research. All subjects who met the
above mentioned criteria were included in the study. All patients were acquainted with the nature,
goals, and course of the study, and informed that their participation in the study was voluntary and
they were free to resign at any stage. The examination time per patient was approximately 90–120 min
factors. Behavioral fall risk factors are potentially modifiable, and include such issues as alcohol
abuse, using inappropriate shoes, as well as physical inactivity. Behavioral factors also include
polypharmacotherapy, and not taking into account the differences in drug pharmacokinetics and
pharmacodynamics in the organism of an old person. Environmental factors refer to the development of
private and public spaces (uneven terrain, architectural obstacles, and problems with transport).
Socio-economic issues are: low income, low standard of living, limited access to health and
social services, and the lack of social support [1].
Identification of the main fall risk factors may contribute to the implementation of preventive
actions reducing the incidence of falls. These actions should form a part of an interdisciplinary process
aiming at compensation of deficits in all spheres of human functioning. The specificity of geriatrics
necessitates the provision of an overall solution to the problems of advanced-age patients. Therefore,
the therapeutic and nursing management in the case of the elderly should be based on a comprehensive
geriatric assessment (CGA). The literature describes a number of functional tests used to assess the
risk of falls in people of advanced age. Their availability, the short time required for their execution,
and the possibility of using them in any conditions, mean that they can be also applied on an outpatient
basis [8]. The aim of this study was to analyze the fall risk factors in the community-dwelling elderly
depending on their physical function, cognitive status and symptoms of depression.
2. Materials and Methods
2.1. Ethics Statement
All subjects gave their informed consent for inclusion before they participated in the study.
The study was conducted in accordance with the Declaration of Helsinki, and the protocol was
approved by the Ethics Committee of the Pomeranian Medical University in Szczecin, Poland
(KB-0080/141/09).
2.2. Sample Size
The study involved 304 people aged 65–100 years, using outpatient health services provided by
The Regional Centre of Occupational Medicine - West Pomeranian Prevention and Therapy Centre
in Szczecin, North West Poland. Women constituted 77.3% of those analyzed, men −22.7%. The mean
age was 78.6 ± 7.4.
2.3. Participants and Recruitment
Principal criteria for the selection of participants were: the availability of the patients at the moment
of carrying out the study, no symptoms of the exacerbation of the co-existing diseases or other health
problems, the mental condition of the patients making them able to cooperate during the study and
understand the orders of the researcher, the ability of the surveyed to move without assistance,
as well as conscious and voluntary consent to participate in the research. All subjects who met the
above mentioned criteria were included in the study. All patients were acquainted with the nature,
goals, and course of the study, and informed that their participation in the study was voluntary and
they were free to resign at any stage. The examination time per patient was approximately 90–120 min
Int. J. Environ. Res. Public Health 2015, 12 3409
and was adjusted to the individual needs of the patient. During the study the researchers applied the
principles of effective interpersonal communication.
2.4. Data Collection
The study was conducted in conditions which guaranteed the accuracy of the measurement and
elimination of interfering factors. The specificity of the research situation, as well as the characteristics
of the participants and their health status were taken into account. The place where the participants
were examined was suitable for people of advanced age. The study was conducted with respect for the
patients’ dignity, intimacy, comfort and feelings of safety.
The study was based on a diagnostics survey, conducted using the technique of an oral, open,
individual categorized interview. The interview was conducted directly with the patients or indirectly
with their professional or non-professional caregivers. Instruments employed in the study included the
original Geriatric Environmental Inquiry. The questionnaire concerned the general assessment of
socio-environmental and economic situation, as well as the health evaluation and circumstances of falls
in the past. Additionally, observations were conducted using a non-standard, occasional, direct and
spontaneous technique as a supplementary method. Another instrument used in the study was the
Barthel Scale (BS) for measuring the ability to perform activities of daily living. This test enables the
identification of three groups of patients depending on their self-reliance level. Individuals with scores
of 0–20, 21–85, 86–100 points were classified as “very dependent”, “moderately dependent”,
and “independent”, respectively. The Abbreviated Mental Test Score (AMTS) was applied to assess
cognitive functions. This test enables the identification of three groups of patients: a group with
seriously disturbed cognitive function (0–3 points), a group with moderate disability (4–6 points),
and a group with normal mental efficiency (>6 points). The short version of the Geriatric Depression
Scale (GDS) was used to assess the severity of depressive symptoms. Individuals with scores of
11–15 points are regarded as having severe depressive disorders, patients with scores of 6–10—moderate
depression, and those with the score of 0–5 - no depressive symptoms. The Tinetti Test (TT) was
employed to evaluate patients’ ability to walk and maintain balance. The TT enables the division of
patients into three groups depending on the level of their dependence and the risk of falls. The group at
the highest risk obtains the lowest scores ( ≤18). The group at moderate risk consists of people with
scores of 19–23 points, which reflects moderate dependence and fall risk. The group at minimal risk is
the one with scores of ≥24 points.
The last stage of the study involved the analysis of the documentation. The authors analyzed medical
documents filled in by those taking care of a given patient (family doctor, family nurse, doctors of different
specialties, physiotherapists) in order to verify information about health and nursing problems obtained
during medical interview. The study was performed using a standard technique. The research instruments
of choice were: the history of disease, the documentation of the nursing process, the results of consultation
and diagnostic tests and hospital treatment information charts.
2.5. Data Analysis
The research material was verified in terms of its completeness, reliability, and the correctness of
its collection. Then, a statistical grouping was conducted in order to organize and systematize
and was adjusted to the individual needs of the patient. During the study the researchers applied the
principles of effective interpersonal communication.
2.4. Data Collection
The study was conducted in conditions which guaranteed the accuracy of the measurement and
elimination of interfering factors. The specificity of the research situation, as well as the characteristics
of the participants and their health status were taken into account. The place where the participants
were examined was suitable for people of advanced age. The study was conducted with respect for the
patients’ dignity, intimacy, comfort and feelings of safety.
The study was based on a diagnostics survey, conducted using the technique of an oral, open,
individual categorized interview. The interview was conducted directly with the patients or indirectly
with their professional or non-professional caregivers. Instruments employed in the study included the
original Geriatric Environmental Inquiry. The questionnaire concerned the general assessment of
socio-environmental and economic situation, as well as the health evaluation and circumstances of falls
in the past. Additionally, observations were conducted using a non-standard, occasional, direct and
spontaneous technique as a supplementary method. Another instrument used in the study was the
Barthel Scale (BS) for measuring the ability to perform activities of daily living. This test enables the
identification of three groups of patients depending on their self-reliance level. Individuals with scores
of 0–20, 21–85, 86–100 points were classified as “very dependent”, “moderately dependent”,
and “independent”, respectively. The Abbreviated Mental Test Score (AMTS) was applied to assess
cognitive functions. This test enables the identification of three groups of patients: a group with
seriously disturbed cognitive function (0–3 points), a group with moderate disability (4–6 points),
and a group with normal mental efficiency (>6 points). The short version of the Geriatric Depression
Scale (GDS) was used to assess the severity of depressive symptoms. Individuals with scores of
11–15 points are regarded as having severe depressive disorders, patients with scores of 6–10—moderate
depression, and those with the score of 0–5 - no depressive symptoms. The Tinetti Test (TT) was
employed to evaluate patients’ ability to walk and maintain balance. The TT enables the division of
patients into three groups depending on the level of their dependence and the risk of falls. The group at
the highest risk obtains the lowest scores ( ≤18). The group at moderate risk consists of people with
scores of 19–23 points, which reflects moderate dependence and fall risk. The group at minimal risk is
the one with scores of ≥24 points.
The last stage of the study involved the analysis of the documentation. The authors analyzed medical
documents filled in by those taking care of a given patient (family doctor, family nurse, doctors of different
specialties, physiotherapists) in order to verify information about health and nursing problems obtained
during medical interview. The study was performed using a standard technique. The research instruments
of choice were: the history of disease, the documentation of the nursing process, the results of consultation
and diagnostic tests and hospital treatment information charts.
2.5. Data Analysis
The research material was verified in terms of its completeness, reliability, and the correctness of
its collection. Then, a statistical grouping was conducted in order to organize and systematize
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Int. J. Environ. Res. Public Health 2015, 12 3410
the material according to criteria determined by research problems and the aims of the study.
The next stage was the codification of the research material, due to the complexity of the planned
statistical procedures. The empirical material was processed using the calculation sheet MS EXCEL 2007.
Statistical calculations were performed with the software “Statistica 10.0” (StatSoft Poland Inc.,
Krakow, Poland). The significance of differences between qualitative variables was assessed using the
t-student test, and the Kolmogorov-Smirnov non-parametric test. The significance of differences between
quantitative variables was assessed using the Spearman’s rank correlation coefficient or the Pearson
correlation coefficient. The accepted level of statistical significance was α = 0.05. The authors also
conducted the multifactor analysis of falls (>1), using the logistic regression model (Quasi-Newton
estimation). The accepted level of statistical significance was α = 0.05.
2.6. Limitation of the Study
The limitation of this study was a relatively small study group, as well as the fact that this sample
was not representative of the population of the center where the study was performed.
3. Results
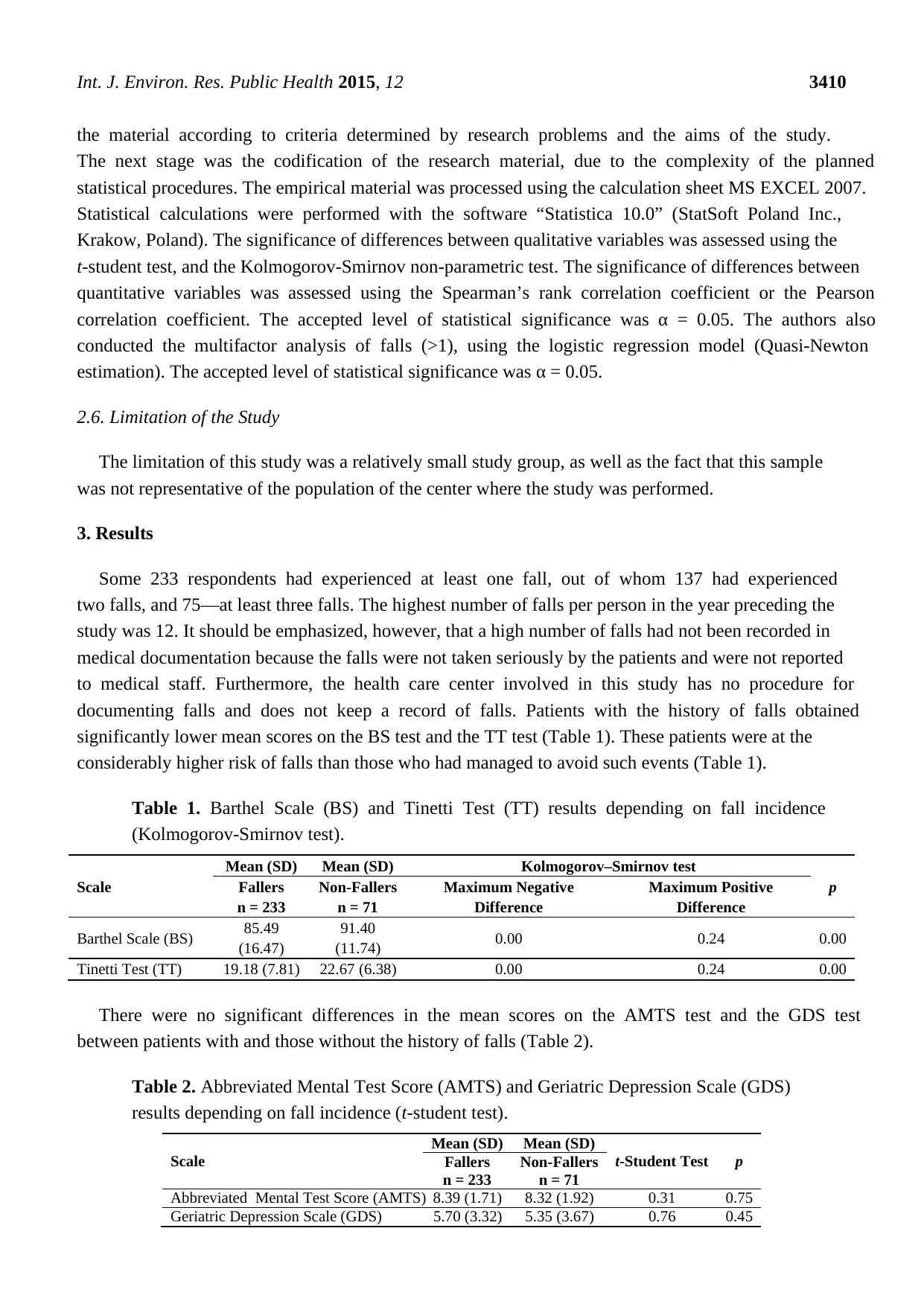
Some 233 respondents had experienced at least one fall, out of whom 137 had experienced
two falls, and 75—at least three falls. The highest number of falls per person in the year preceding the
study was 12. It should be emphasized, however, that a high number of falls had not been recorded in
medical documentation because the falls were not taken seriously by the patients and were not reported
to medical staff. Furthermore, the health care center involved in this study has no procedure for
documenting falls and does not keep a record of falls. Patients with the history of falls obtained
significantly lower mean scores on the BS test and the TT test (Table 1). These patients were at the
considerably higher risk of falls than those who had managed to avoid such events (Table 1).
Table 1. Barthel Scale (BS) and Tinetti Test (TT) results depending on fall incidence
(Kolmogorov-Smirnov test).
Scale
Mean (SD) Mean (SD) Kolmogorov–Smirnov test
pFallers
n = 233
Non-Fallers
n = 71
Maximum Negative
Difference
Maximum Positive
Difference
Barthel Scale (BS) 85.49
(16.47)
91.40
(11.74) 0.00 0.24 0.00
Tinetti Test (TT) 19.18 (7.81) 22.67 (6.38) 0.00 0.24 0.00
There were no significant differences in the mean scores on the AMTS test and the GDS test
between patients with and those without the history of falls (Table 2).
Table 2. Abbreviated Mental Test Score (AMTS) and Geriatric Depression Scale (GDS)
results depending on fall incidence (t-student test).
Scale
Mean (SD) Mean (SD)
t-Student Test pFallers
n = 233
Non-Fallers
n = 71
Abbreviated Mental Test Score (AMTS) 8.39 (1.71) 8.32 (1.92) 0.31 0.75
Geriatric Depression Scale (GDS) 5.70 (3.32) 5.35 (3.67) 0.76 0.45
the material according to criteria determined by research problems and the aims of the study.
The next stage was the codification of the research material, due to the complexity of the planned
statistical procedures. The empirical material was processed using the calculation sheet MS EXCEL 2007.
Statistical calculations were performed with the software “Statistica 10.0” (StatSoft Poland Inc.,
Krakow, Poland). The significance of differences between qualitative variables was assessed using the
t-student test, and the Kolmogorov-Smirnov non-parametric test. The significance of differences between
quantitative variables was assessed using the Spearman’s rank correlation coefficient or the Pearson
correlation coefficient. The accepted level of statistical significance was α = 0.05. The authors also
conducted the multifactor analysis of falls (>1), using the logistic regression model (Quasi-Newton
estimation). The accepted level of statistical significance was α = 0.05.
2.6. Limitation of the Study
The limitation of this study was a relatively small study group, as well as the fact that this sample
was not representative of the population of the center where the study was performed.
3. Results
Some 233 respondents had experienced at least one fall, out of whom 137 had experienced
two falls, and 75—at least three falls. The highest number of falls per person in the year preceding the
study was 12. It should be emphasized, however, that a high number of falls had not been recorded in
medical documentation because the falls were not taken seriously by the patients and were not reported
to medical staff. Furthermore, the health care center involved in this study has no procedure for
documenting falls and does not keep a record of falls. Patients with the history of falls obtained
significantly lower mean scores on the BS test and the TT test (Table 1). These patients were at the
considerably higher risk of falls than those who had managed to avoid such events (Table 1).
Table 1. Barthel Scale (BS) and Tinetti Test (TT) results depending on fall incidence
(Kolmogorov-Smirnov test).
Scale
Mean (SD) Mean (SD) Kolmogorov–Smirnov test
pFallers
n = 233
Non-Fallers
n = 71
Maximum Negative
Difference
Maximum Positive
Difference
Barthel Scale (BS) 85.49
(16.47)
91.40
(11.74) 0.00 0.24 0.00
Tinetti Test (TT) 19.18 (7.81) 22.67 (6.38) 0.00 0.24 0.00
There were no significant differences in the mean scores on the AMTS test and the GDS test
between patients with and those without the history of falls (Table 2).
Table 2. Abbreviated Mental Test Score (AMTS) and Geriatric Depression Scale (GDS)
results depending on fall incidence (t-student test).
Scale
Mean (SD) Mean (SD)
t-Student Test pFallers
n = 233
Non-Fallers
n = 71
Abbreviated Mental Test Score (AMTS) 8.39 (1.71) 8.32 (1.92) 0.31 0.75
Geriatric Depression Scale (GDS) 5.70 (3.32) 5.35 (3.67) 0.76 0.45
Int. J. Environ. Res. Public Health 2015, 12 3411
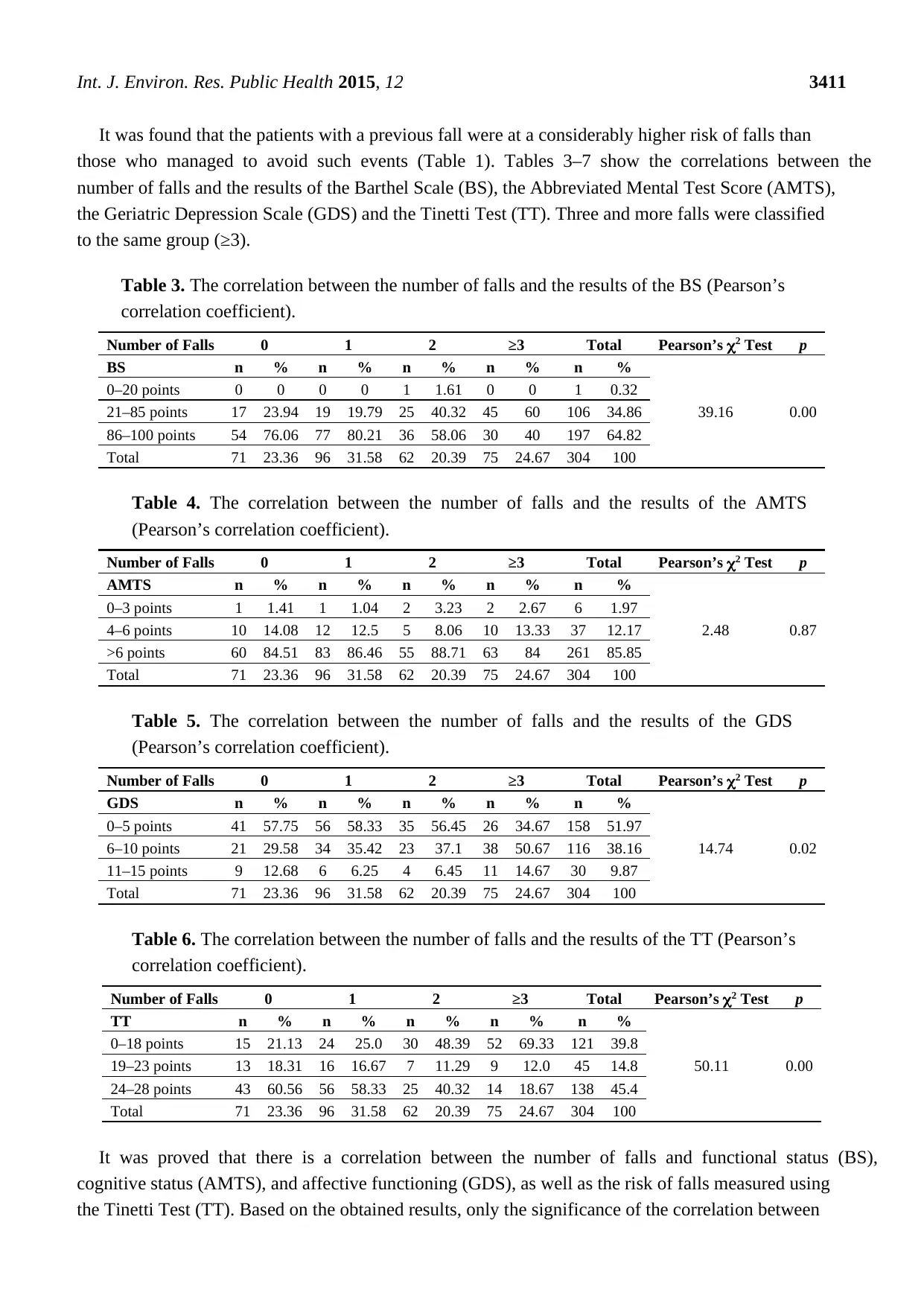
It was found that the patients with a previous fall were at a considerably higher risk of falls than
those who managed to avoid such events (Table 1). Tables 3–7 show the correlations between the
number of falls and the results of the Barthel Scale (BS), the Abbreviated Mental Test Score (AMTS),
the Geriatric Depression Scale (GDS) and the Tinetti Test (TT). Three and more falls were classified
to the same group (≥3).
Table 3. The correlation between the number of falls and the results of the BS (Pearson’s
correlation coefficient).
Number of Falls 0 1 2 ≥3 Total Pearson’s χ2 Test p
BS n % n % n % n % n %
39.16 0.00
0–20 points 0 0 0 0 1 1.61 0 0 1 0.32
21–85 points 17 23.94 19 19.79 25 40.32 45 60 106 34.86
86–100 points 54 76.06 77 80.21 36 58.06 30 40 197 64.82
Total 71 23.36 96 31.58 62 20.39 75 24.67 304 100
Table 4. The correlation between the number of falls and the results of the AMTS
(Pearson’s correlation coefficient).
Number of Falls 0 1 2 ≥3 Total Pearson’s χ2 Test p
AMTS n % n % n % n % n %
2.48 0.87
0–3 points 1 1.41 1 1.04 2 3.23 2 2.67 6 1.97
4–6 points 10 14.08 12 12.5 5 8.06 10 13.33 37 12.17
>6 points 60 84.51 83 86.46 55 88.71 63 84 261 85.85
Total 71 23.36 96 31.58 62 20.39 75 24.67 304 100
Table 5. The correlation between the number of falls and the results of the GDS
(Pearson’s correlation coefficient).
Number of Falls 0 1 2 ≥3 Total Pearson’s χ2 Test p
GDS n % n % n % n % n %
14.74 0.02
0–5 points 41 57.75 56 58.33 35 56.45 26 34.67 158 51.97
6–10 points 21 29.58 34 35.42 23 37.1 38 50.67 116 38.16
11–15 points 9 12.68 6 6.25 4 6.45 11 14.67 30 9.87
Total 71 23.36 96 31.58 62 20.39 75 24.67 304 100
Table 6. The correlation between the number of falls and the results of the TT (Pearson’s
correlation coefficient).
Number of Falls 0 1 2 ≥3 Total Pearson’s χ2 Test p
TT n % n % n % n % n %
50.11 0.00
0–18 points 15 21.13 24 25.0 30 48.39 52 69.33 121 39.8
19–23 points 13 18.31 16 16.67 7 11.29 9 12.0 45 14.8
24–28 points 43 60.56 56 58.33 25 40.32 14 18.67 138 45.4
Total 71 23.36 96 31.58 62 20.39 75 24.67 304 100
It was proved that there is a correlation between the number of falls and functional status (BS),
cognitive status (AMTS), and affective functioning (GDS), as well as the risk of falls measured using
the Tinetti Test (TT). Based on the obtained results, only the significance of the correlation between
It was found that the patients with a previous fall were at a considerably higher risk of falls than
those who managed to avoid such events (Table 1). Tables 3–7 show the correlations between the
number of falls and the results of the Barthel Scale (BS), the Abbreviated Mental Test Score (AMTS),
the Geriatric Depression Scale (GDS) and the Tinetti Test (TT). Three and more falls were classified
to the same group (≥3).
Table 3. The correlation between the number of falls and the results of the BS (Pearson’s
correlation coefficient).
Number of Falls 0 1 2 ≥3 Total Pearson’s χ2 Test p
BS n % n % n % n % n %
39.16 0.00
0–20 points 0 0 0 0 1 1.61 0 0 1 0.32
21–85 points 17 23.94 19 19.79 25 40.32 45 60 106 34.86
86–100 points 54 76.06 77 80.21 36 58.06 30 40 197 64.82
Total 71 23.36 96 31.58 62 20.39 75 24.67 304 100
Table 4. The correlation between the number of falls and the results of the AMTS
(Pearson’s correlation coefficient).
Number of Falls 0 1 2 ≥3 Total Pearson’s χ2 Test p
AMTS n % n % n % n % n %
2.48 0.87
0–3 points 1 1.41 1 1.04 2 3.23 2 2.67 6 1.97
4–6 points 10 14.08 12 12.5 5 8.06 10 13.33 37 12.17
>6 points 60 84.51 83 86.46 55 88.71 63 84 261 85.85
Total 71 23.36 96 31.58 62 20.39 75 24.67 304 100
Table 5. The correlation between the number of falls and the results of the GDS
(Pearson’s correlation coefficient).
Number of Falls 0 1 2 ≥3 Total Pearson’s χ2 Test p
GDS n % n % n % n % n %
14.74 0.02
0–5 points 41 57.75 56 58.33 35 56.45 26 34.67 158 51.97
6–10 points 21 29.58 34 35.42 23 37.1 38 50.67 116 38.16
11–15 points 9 12.68 6 6.25 4 6.45 11 14.67 30 9.87
Total 71 23.36 96 31.58 62 20.39 75 24.67 304 100
Table 6. The correlation between the number of falls and the results of the TT (Pearson’s
correlation coefficient).
Number of Falls 0 1 2 ≥3 Total Pearson’s χ2 Test p
TT n % n % n % n % n %
50.11 0.00
0–18 points 15 21.13 24 25.0 30 48.39 52 69.33 121 39.8
19–23 points 13 18.31 16 16.67 7 11.29 9 12.0 45 14.8
24–28 points 43 60.56 56 58.33 25 40.32 14 18.67 138 45.4
Total 71 23.36 96 31.58 62 20.39 75 24.67 304 100
It was proved that there is a correlation between the number of falls and functional status (BS),
cognitive status (AMTS), and affective functioning (GDS), as well as the risk of falls measured using
the Tinetti Test (TT). Based on the obtained results, only the significance of the correlation between
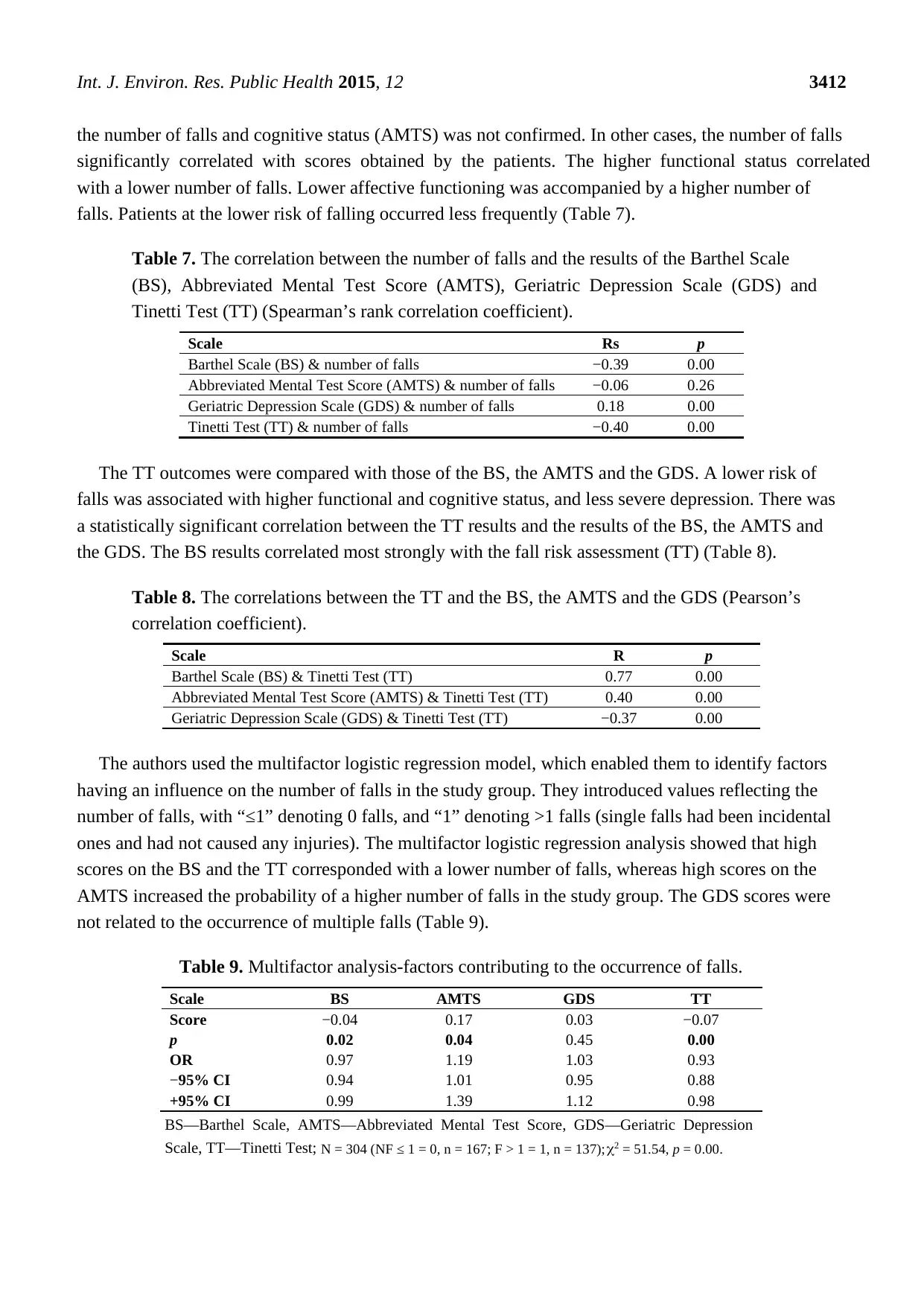
Int. J. Environ. Res. Public Health 2015, 12 3412
the number of falls and cognitive status (AMTS) was not confirmed. In other cases, the number of falls
significantly correlated with scores obtained by the patients. The higher functional status correlated
with a lower number of falls. Lower affective functioning was accompanied by a higher number of
falls. Patients at the lower risk of falling occurred less frequently (Table 7).
Table 7. The correlation between the number of falls and the results of the Barthel Scale
(BS), Abbreviated Mental Test Score (AMTS), Geriatric Depression Scale (GDS) and
Tinetti Test (TT) (Spearman’s rank correlation coefficient).
Scale Rs p
Barthel Scale (BS) & number of falls −0.39 0.00
Abbreviated Mental Test Score (AMTS) & number of falls −0.06 0.26
Geriatric Depression Scale (GDS) & number of falls 0.18 0.00
Tinetti Test (TT) & number of falls −0.40 0.00
The TT outcomes were compared with those of the BS, the AMTS and the GDS. A lower risk of
falls was associated with higher functional and cognitive status, and less severe depression. There was
a statistically significant correlation between the TT results and the results of the BS, the AMTS and
the GDS. The BS results correlated most strongly with the fall risk assessment (TT) (Table 8).
Table 8. The correlations between the TT and the BS, the AMTS and the GDS (Pearson’s
correlation coefficient).
Scale R p
Barthel Scale (BS) & Tinetti Test (TT) 0.77 0.00
Abbreviated Mental Test Score (AMTS) & Tinetti Test (TT) 0.40 0.00
Geriatric Depression Scale (GDS) & Tinetti Test (TT) −0.37 0.00
The authors used the multifactor logistic regression model, which enabled them to identify factors
having an influence on the number of falls in the study group. They introduced values reflecting the
number of falls, with “≤1” denoting 0 falls, and “1” denoting >1 falls (single falls had been incidental
ones and had not caused any injuries). The multifactor logistic regression analysis showed that high
scores on the BS and the TT corresponded with a lower number of falls, whereas high scores on the
AMTS increased the probability of a higher number of falls in the study group. The GDS scores were
not related to the occurrence of multiple falls (Table 9).
Table 9. Multifactor analysis-factors contributing to the occurrence of falls.
Scale BS AMTS GDS TT
Score −0.04 0.17 0.03 −0.07
p 0.02 0.04 0.45 0.00
OR 0.97 1.19 1.03 0.93
−95% CI 0.94 1.01 0.95 0.88
+95% CI 0.99 1.39 1.12 0.98
BS—Barthel Scale, AMTS—Abbreviated Mental Test Score, GDS—Geriatric Depression
Scale, TT—Tinetti Test; N = 304 (NF ≤ 1 = 0, n = 167; F > 1 = 1, n = 137); χ2 = 51.54, p = 0.00.
the number of falls and cognitive status (AMTS) was not confirmed. In other cases, the number of falls
significantly correlated with scores obtained by the patients. The higher functional status correlated
with a lower number of falls. Lower affective functioning was accompanied by a higher number of
falls. Patients at the lower risk of falling occurred less frequently (Table 7).
Table 7. The correlation between the number of falls and the results of the Barthel Scale
(BS), Abbreviated Mental Test Score (AMTS), Geriatric Depression Scale (GDS) and
Tinetti Test (TT) (Spearman’s rank correlation coefficient).
Scale Rs p
Barthel Scale (BS) & number of falls −0.39 0.00
Abbreviated Mental Test Score (AMTS) & number of falls −0.06 0.26
Geriatric Depression Scale (GDS) & number of falls 0.18 0.00
Tinetti Test (TT) & number of falls −0.40 0.00
The TT outcomes were compared with those of the BS, the AMTS and the GDS. A lower risk of
falls was associated with higher functional and cognitive status, and less severe depression. There was
a statistically significant correlation between the TT results and the results of the BS, the AMTS and
the GDS. The BS results correlated most strongly with the fall risk assessment (TT) (Table 8).
Table 8. The correlations between the TT and the BS, the AMTS and the GDS (Pearson’s
correlation coefficient).
Scale R p
Barthel Scale (BS) & Tinetti Test (TT) 0.77 0.00
Abbreviated Mental Test Score (AMTS) & Tinetti Test (TT) 0.40 0.00
Geriatric Depression Scale (GDS) & Tinetti Test (TT) −0.37 0.00
The authors used the multifactor logistic regression model, which enabled them to identify factors
having an influence on the number of falls in the study group. They introduced values reflecting the
number of falls, with “≤1” denoting 0 falls, and “1” denoting >1 falls (single falls had been incidental
ones and had not caused any injuries). The multifactor logistic regression analysis showed that high
scores on the BS and the TT corresponded with a lower number of falls, whereas high scores on the
AMTS increased the probability of a higher number of falls in the study group. The GDS scores were
not related to the occurrence of multiple falls (Table 9).
Table 9. Multifactor analysis-factors contributing to the occurrence of falls.
Scale BS AMTS GDS TT
Score −0.04 0.17 0.03 −0.07
p 0.02 0.04 0.45 0.00
OR 0.97 1.19 1.03 0.93
−95% CI 0.94 1.01 0.95 0.88
+95% CI 0.99 1.39 1.12 0.98
BS—Barthel Scale, AMTS—Abbreviated Mental Test Score, GDS—Geriatric Depression
Scale, TT—Tinetti Test; N = 304 (NF ≤ 1 = 0, n = 167; F > 1 = 1, n = 137); χ2 = 51.54, p = 0.00.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Int. J. Environ. Res. Public Health 2015, 12 3413
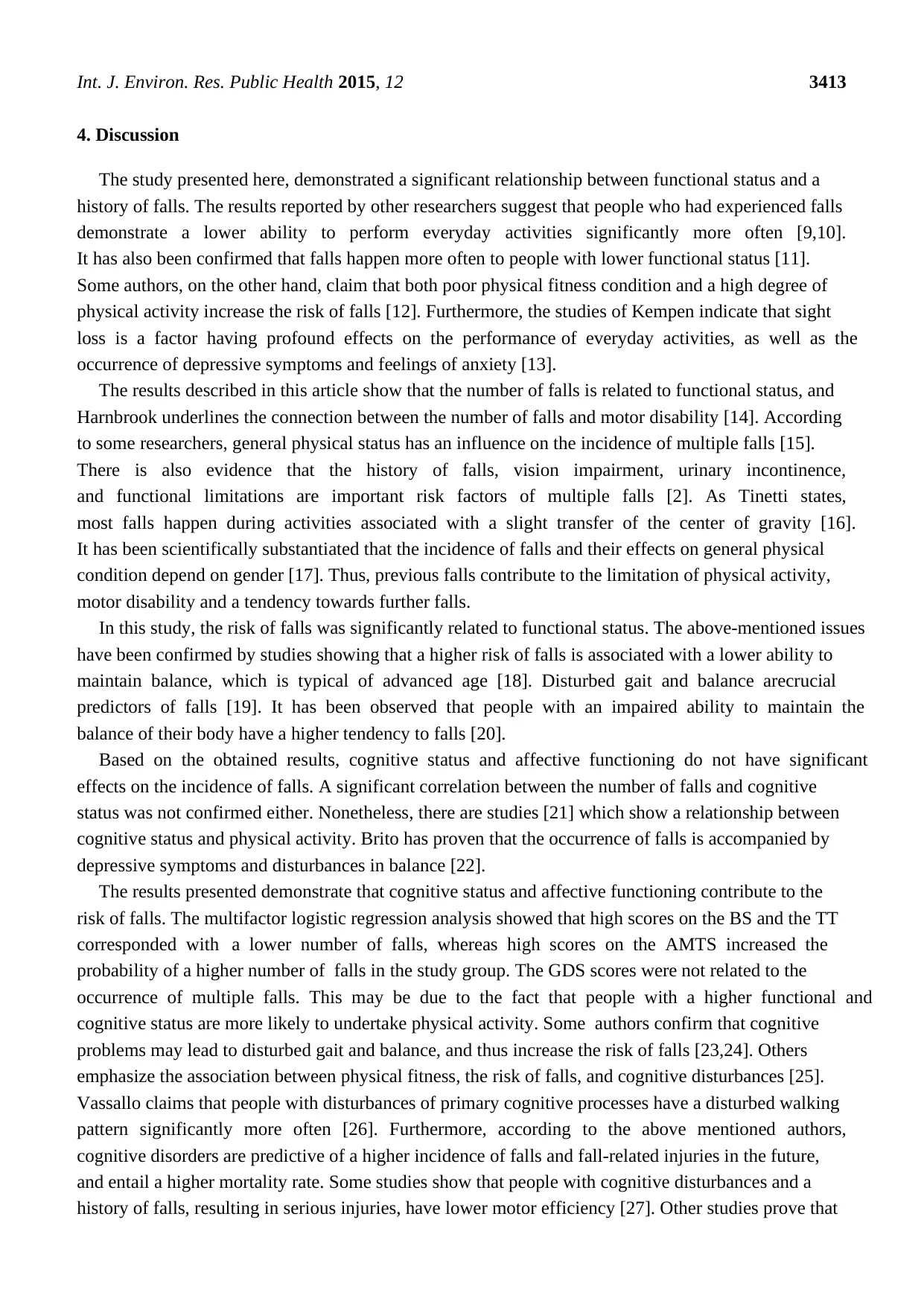
4. Discussion
The study presented here, demonstrated a significant relationship between functional status and a
history of falls. The results reported by other researchers suggest that people who had experienced falls
demonstrate a lower ability to perform everyday activities significantly more often [9,10].
It has also been confirmed that falls happen more often to people with lower functional status [11].
Some authors, on the other hand, claim that both poor physical fitness condition and a high degree of
physical activity increase the risk of falls [12]. Furthermore, the studies of Kempen indicate that sight
loss is a factor having profound effects on the performance of everyday activities, as well as the
occurrence of depressive symptoms and feelings of anxiety [13].
The results described in this article show that the number of falls is related to functional status, and
Harnbrook underlines the connection between the number of falls and motor disability [14]. According
to some researchers, general physical status has an influence on the incidence of multiple falls [15].
There is also evidence that the history of falls, vision impairment, urinary incontinence,
and functional limitations are important risk factors of multiple falls [2]. As Tinetti states,
most falls happen during activities associated with a slight transfer of the center of gravity [16].
It has been scientifically substantiated that the incidence of falls and their effects on general physical
condition depend on gender [17]. Thus, previous falls contribute to the limitation of physical activity,
motor disability and a tendency towards further falls.
In this study, the risk of falls was significantly related to functional status. The above-mentioned issues
have been confirmed by studies showing that a higher risk of falls is associated with a lower ability to
maintain balance, which is typical of advanced age [18]. Disturbed gait and balance arecrucial
predictors of falls [19]. It has been observed that people with an impaired ability to maintain the
balance of their body have a higher tendency to falls [20].
Based on the obtained results, cognitive status and affective functioning do not have significant
effects on the incidence of falls. A significant correlation between the number of falls and cognitive
status was not confirmed either. Nonetheless, there are studies [21] which show a relationship between
cognitive status and physical activity. Brito has proven that the occurrence of falls is accompanied by
depressive symptoms and disturbances in balance [22].
The results presented demonstrate that cognitive status and affective functioning contribute to the
risk of falls. The multifactor logistic regression analysis showed that high scores on the BS and the TT
corresponded with a lower number of falls, whereas high scores on the AMTS increased the
probability of a higher number of falls in the study group. The GDS scores were not related to the
occurrence of multiple falls. This may be due to the fact that people with a higher functional and
cognitive status are more likely to undertake physical activity. Some authors confirm that cognitive
problems may lead to disturbed gait and balance, and thus increase the risk of falls [23,24]. Others
emphasize the association between physical fitness, the risk of falls, and cognitive disturbances [25].
Vassallo claims that people with disturbances of primary cognitive processes have a disturbed walking
pattern significantly more often [26]. Furthermore, according to the above mentioned authors,
cognitive disorders are predictive of a higher incidence of falls and fall-related injuries in the future,
and entail a higher mortality rate. Some studies show that people with cognitive disturbances and a
history of falls, resulting in serious injuries, have lower motor efficiency [27]. Other studies prove that
4. Discussion
The study presented here, demonstrated a significant relationship between functional status and a
history of falls. The results reported by other researchers suggest that people who had experienced falls
demonstrate a lower ability to perform everyday activities significantly more often [9,10].
It has also been confirmed that falls happen more often to people with lower functional status [11].
Some authors, on the other hand, claim that both poor physical fitness condition and a high degree of
physical activity increase the risk of falls [12]. Furthermore, the studies of Kempen indicate that sight
loss is a factor having profound effects on the performance of everyday activities, as well as the
occurrence of depressive symptoms and feelings of anxiety [13].
The results described in this article show that the number of falls is related to functional status, and
Harnbrook underlines the connection between the number of falls and motor disability [14]. According
to some researchers, general physical status has an influence on the incidence of multiple falls [15].
There is also evidence that the history of falls, vision impairment, urinary incontinence,
and functional limitations are important risk factors of multiple falls [2]. As Tinetti states,
most falls happen during activities associated with a slight transfer of the center of gravity [16].
It has been scientifically substantiated that the incidence of falls and their effects on general physical
condition depend on gender [17]. Thus, previous falls contribute to the limitation of physical activity,
motor disability and a tendency towards further falls.
In this study, the risk of falls was significantly related to functional status. The above-mentioned issues
have been confirmed by studies showing that a higher risk of falls is associated with a lower ability to
maintain balance, which is typical of advanced age [18]. Disturbed gait and balance arecrucial
predictors of falls [19]. It has been observed that people with an impaired ability to maintain the
balance of their body have a higher tendency to falls [20].
Based on the obtained results, cognitive status and affective functioning do not have significant
effects on the incidence of falls. A significant correlation between the number of falls and cognitive
status was not confirmed either. Nonetheless, there are studies [21] which show a relationship between
cognitive status and physical activity. Brito has proven that the occurrence of falls is accompanied by
depressive symptoms and disturbances in balance [22].
The results presented demonstrate that cognitive status and affective functioning contribute to the
risk of falls. The multifactor logistic regression analysis showed that high scores on the BS and the TT
corresponded with a lower number of falls, whereas high scores on the AMTS increased the
probability of a higher number of falls in the study group. The GDS scores were not related to the
occurrence of multiple falls. This may be due to the fact that people with a higher functional and
cognitive status are more likely to undertake physical activity. Some authors confirm that cognitive
problems may lead to disturbed gait and balance, and thus increase the risk of falls [23,24]. Others
emphasize the association between physical fitness, the risk of falls, and cognitive disturbances [25].
Vassallo claims that people with disturbances of primary cognitive processes have a disturbed walking
pattern significantly more often [26]. Furthermore, according to the above mentioned authors,
cognitive disorders are predictive of a higher incidence of falls and fall-related injuries in the future,
and entail a higher mortality rate. Some studies show that people with cognitive disturbances and a
history of falls, resulting in serious injuries, have lower motor efficiency [27]. Other studies prove that
Int. J. Environ. Res. Public Health 2015, 12 3414
disturbed posture-balance, and especially such parameters as walking speed, standing balance and
changes in the sitting-standing position, are related to a disturbed cognitive process [28]. Nevertheless,
there are also reports suggesting that a program of exercises improving balance and the leg strength, in
a group of patients with Parkinson’s disease, can contribute to a reduction in the incidence of falls,
but only among patients at a mild stage of the disease [29]. Tinetti observed a significant correlation
between the risk of falls and the incidence of depression [16]. However, other researchers suggest that
a factor significantly increasing the risk of falls is not depression itself, but rather the administration of
thymoanaleptiques [30]. Issues mentioned as important fall risk factors are also: a history of falls,
visual disturbances, urinary incontinence, and using benzodiazepines [2].
5. Conclusions
The incidence of falls may significantly increase in people with lower functional status, which may be
related to cognitive process disturbances and lower affective functioning. Since there was a relationship
between the risk of falls and the lower functional status, cognitive status, and affective functioning in the
analyzed group, a comprehensive geriatric assessment, related to all aspects of advanced-age patients’
efficiency, is recommended. Apart from improving the general health, fall prevention strategies should
include actions undertaken to evaluate and treat depression and cognitive disturbances.
Acknowledgments
The research was funded by the Pomeranian Medical University in Szczecin, Poland.
Author Contributions
Magdalena Sylwia Kamińska: responsibility for the integrity of the work as a whole, conception
and design; performing the experiment, acquisition of data; analysis and interpretation of data and
preparing the paper. Jacek Brodowski: responsibility for analysis and interpretation of data.
Beata Karakiewicz: drafting the article and revising it critically for important intellectual content;
final approval of the version to be published.
Conflict of Interests
The authors declare no conflict of interest.
References
1. WHO Global Report on Falls Prevention in Older Age; World Health Organization: Geneva,
Switzerland, 2007.
2. Tromp, A.M.; Pluijm, S.M.F.; Smit, J.H.; Deeg, D.J.H.; Bouter, L.M.; Lips, P. Fall-risk screening test:
A prospective study on predictors for falls in community-dwelling elderly. J. Clin. Epidemiol. 2001,
54, 837–844.
3. Stevens, J.A.; Ballesteros, M.F.; Mack, K.A.; Rudd, R.A.; DeCaro, E.; Adler, G. Gender differences
in seeking care for falls in the aged Medicare Population. Amer. J. Prev. Med. 2012, 43, 59–62.
disturbed posture-balance, and especially such parameters as walking speed, standing balance and
changes in the sitting-standing position, are related to a disturbed cognitive process [28]. Nevertheless,
there are also reports suggesting that a program of exercises improving balance and the leg strength, in
a group of patients with Parkinson’s disease, can contribute to a reduction in the incidence of falls,
but only among patients at a mild stage of the disease [29]. Tinetti observed a significant correlation
between the risk of falls and the incidence of depression [16]. However, other researchers suggest that
a factor significantly increasing the risk of falls is not depression itself, but rather the administration of
thymoanaleptiques [30]. Issues mentioned as important fall risk factors are also: a history of falls,
visual disturbances, urinary incontinence, and using benzodiazepines [2].
5. Conclusions
The incidence of falls may significantly increase in people with lower functional status, which may be
related to cognitive process disturbances and lower affective functioning. Since there was a relationship
between the risk of falls and the lower functional status, cognitive status, and affective functioning in the
analyzed group, a comprehensive geriatric assessment, related to all aspects of advanced-age patients’
efficiency, is recommended. Apart from improving the general health, fall prevention strategies should
include actions undertaken to evaluate and treat depression and cognitive disturbances.
Acknowledgments
The research was funded by the Pomeranian Medical University in Szczecin, Poland.
Author Contributions
Magdalena Sylwia Kamińska: responsibility for the integrity of the work as a whole, conception
and design; performing the experiment, acquisition of data; analysis and interpretation of data and
preparing the paper. Jacek Brodowski: responsibility for analysis and interpretation of data.
Beata Karakiewicz: drafting the article and revising it critically for important intellectual content;
final approval of the version to be published.
Conflict of Interests
The authors declare no conflict of interest.
References
1. WHO Global Report on Falls Prevention in Older Age; World Health Organization: Geneva,
Switzerland, 2007.
2. Tromp, A.M.; Pluijm, S.M.F.; Smit, J.H.; Deeg, D.J.H.; Bouter, L.M.; Lips, P. Fall-risk screening test:
A prospective study on predictors for falls in community-dwelling elderly. J. Clin. Epidemiol. 2001,
54, 837–844.
3. Stevens, J.A.; Ballesteros, M.F.; Mack, K.A.; Rudd, R.A.; DeCaro, E.; Adler, G. Gender differences
in seeking care for falls in the aged Medicare Population. Amer. J. Prev. Med. 2012, 43, 59–62.
Int. J. Environ. Res. Public Health 2015, 12 3415
4. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Injury
Prevention & Control: Data & Statistics (WISQARSTM). Available online: http://www.cdc.gov/
injury/wisqars/ (accessed on 15 August 2013).
5. Petridou, E.; Kyllekidis, S.; Jeffrey, S.; Chishti, P.; Dessypris, N.; Stone, D.H. Unintentional injury
mortality in the European Union: How many more lives could be saved? Scand. J. Public Health
2007, 35, 278–287.
6. Spaniolas, K.; Cheng, J.D.; Gestring, M.L.; Sangosanya, A.; Stassen, N.A.; Bankey, P.E.
Ground level falls are associated with significant mortality in elderly patients. J. Trauma 2010,
69, 821–825.
7. Stevens, J.A.; Corso, P.S.; Finkelstein, E.A.; Miller, T.R. The costs of fatal and nonfatal falls
among older adults. Inj. Prev. 2006, 12, 290–295.
8. Persad, C.C.; Cook, S.; Giordani, B. Assessing falls in the elderly: Should we use simple screening
tests or a comprehensive fall risk evaluation? Eur. J. Phys. Rehabil. Med. 2010, 46, 457–460.
9. Shin, K.R.; Kang, Y.; Hwang, E.H.; Jung, D. The prevalence, characteristics and correlates of
falls in Korean community-dwelling older adults. Int. Nurs. Rev. 2009, 56, 387–392.
10. Van der Meulen, E.; Zijlstra, G.A.; Ambergen, T.; Kempem, G.I. Effect of fall-related concerns
on physical, mental, and social function in community-dwelling older adults: A prospective cohort
study. J. Amer. Geriatr. Soc. 2014, 62, 2333–2338.
11. Van Bemmel, T.; Vandenbroucke, J.P.; Westendorp, R.G.; Gussekloo, J. In an observational study
elderly patients had an increased risk of falling due to home hazards. J. Clin. Epidemiol. 2005, 58,
63–67.
12. Chan, B.K.S.; Marshall, L.M.; Winters, K.M.; Faulkner, K.A.; Schwartz, A.V.; Orwoll, E.S.
Incident fall risk and physical activity and physical performance among older men. Amer. J.
Epidemiol. 2007, 165, 696–703.
13. Kempen, G.I.; Ballemans, J.; Ranchor, A.V.; van Rens, G.H.; Zijlstra, G.A. The impact of low vision
on activities of daily living, symptoms of depression, feelings of anxiety and social support in
community-living older adults seeking vision rehabilitation services. Qual. Life Res. 2012, 21,
1405–1411.
14. Harnbrook, M.C.; Stevens, V.J.; Wingfield, D.J.; Hollis, J.F.; Greenlick, M.R.; Ory, M.G.
Preventing falls among community—Dwelling older persons: Results from a randomized trial.
Gerontologist 1994, 34, 16–23.
15. Melzer, I.; Kurz, I. Self-reported function and disability in late life: A comparison between
recurrent fallers and non-fallers. Disabil. Rehabil. 2009, 31, 791–798.
16. Tinetti, M.E.; Baker, D.I.; Mc Vay, G. A multifactorial intervention to reduce the risk of falling
among elderly people living in the community. N. Engl. J. Med. 1994, 331, 821–827.
17. Stahl, S.T.; Albert, S.M. Gender differences in physical activity patterns among older adults
who fall. Prev. Med. 2014, doi:10.1016/j.ypmed.2014.12.0.
18. Lajoie, Y.; Gallagher, S.P. Predicting falls within the elderly community: comparison of postural
sway, reaction time, the Berg Balance Scale and the Activities-specific Balance Confidence
(ABC) scale for comparing fallers and non-fallers. Arch. Gerontol. Geriatr. 2004, 38, 11–26.
19. Bergland, A.; Pettersen, A.M.; Laake, K. Functional status among elderly Norwegian fallers
living at home. Physiother. Res. Int. 2000, 5, 33–45.
4. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Injury
Prevention & Control: Data & Statistics (WISQARSTM). Available online: http://www.cdc.gov/
injury/wisqars/ (accessed on 15 August 2013).
5. Petridou, E.; Kyllekidis, S.; Jeffrey, S.; Chishti, P.; Dessypris, N.; Stone, D.H. Unintentional injury
mortality in the European Union: How many more lives could be saved? Scand. J. Public Health
2007, 35, 278–287.
6. Spaniolas, K.; Cheng, J.D.; Gestring, M.L.; Sangosanya, A.; Stassen, N.A.; Bankey, P.E.
Ground level falls are associated with significant mortality in elderly patients. J. Trauma 2010,
69, 821–825.
7. Stevens, J.A.; Corso, P.S.; Finkelstein, E.A.; Miller, T.R. The costs of fatal and nonfatal falls
among older adults. Inj. Prev. 2006, 12, 290–295.
8. Persad, C.C.; Cook, S.; Giordani, B. Assessing falls in the elderly: Should we use simple screening
tests or a comprehensive fall risk evaluation? Eur. J. Phys. Rehabil. Med. 2010, 46, 457–460.
9. Shin, K.R.; Kang, Y.; Hwang, E.H.; Jung, D. The prevalence, characteristics and correlates of
falls in Korean community-dwelling older adults. Int. Nurs. Rev. 2009, 56, 387–392.
10. Van der Meulen, E.; Zijlstra, G.A.; Ambergen, T.; Kempem, G.I. Effect of fall-related concerns
on physical, mental, and social function in community-dwelling older adults: A prospective cohort
study. J. Amer. Geriatr. Soc. 2014, 62, 2333–2338.
11. Van Bemmel, T.; Vandenbroucke, J.P.; Westendorp, R.G.; Gussekloo, J. In an observational study
elderly patients had an increased risk of falling due to home hazards. J. Clin. Epidemiol. 2005, 58,
63–67.
12. Chan, B.K.S.; Marshall, L.M.; Winters, K.M.; Faulkner, K.A.; Schwartz, A.V.; Orwoll, E.S.
Incident fall risk and physical activity and physical performance among older men. Amer. J.
Epidemiol. 2007, 165, 696–703.
13. Kempen, G.I.; Ballemans, J.; Ranchor, A.V.; van Rens, G.H.; Zijlstra, G.A. The impact of low vision
on activities of daily living, symptoms of depression, feelings of anxiety and social support in
community-living older adults seeking vision rehabilitation services. Qual. Life Res. 2012, 21,
1405–1411.
14. Harnbrook, M.C.; Stevens, V.J.; Wingfield, D.J.; Hollis, J.F.; Greenlick, M.R.; Ory, M.G.
Preventing falls among community—Dwelling older persons: Results from a randomized trial.
Gerontologist 1994, 34, 16–23.
15. Melzer, I.; Kurz, I. Self-reported function and disability in late life: A comparison between
recurrent fallers and non-fallers. Disabil. Rehabil. 2009, 31, 791–798.
16. Tinetti, M.E.; Baker, D.I.; Mc Vay, G. A multifactorial intervention to reduce the risk of falling
among elderly people living in the community. N. Engl. J. Med. 1994, 331, 821–827.
17. Stahl, S.T.; Albert, S.M. Gender differences in physical activity patterns among older adults
who fall. Prev. Med. 2014, doi:10.1016/j.ypmed.2014.12.0.
18. Lajoie, Y.; Gallagher, S.P. Predicting falls within the elderly community: comparison of postural
sway, reaction time, the Berg Balance Scale and the Activities-specific Balance Confidence
(ABC) scale for comparing fallers and non-fallers. Arch. Gerontol. Geriatr. 2004, 38, 11–26.
19. Bergland, A.; Pettersen, A.M.; Laake, K. Functional status among elderly Norwegian fallers
living at home. Physiother. Res. Int. 2000, 5, 33–45.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Int. J. Environ. Res. Public Health 2015, 12 3416
20. Sihvonen, S.; Kulmala, J.; Kallinen, M.; Alén, M.; Kiviranta, I.; Sipilä, S. Postural balance and
self-reported balance confidence in older adults with a hip fracture history. Gerontology 2009, 55,
630–636.
21. Nieto, M.L.; Albert, S.M.; Morrow, L.A.; Saxton, J. Cognitive status and physical function in
older African Americans. J. Amer. Geriatr. Soc. 2008, 56, 2014–2019.
22. Brito, T.A.; Coqueiro, R.S.; Fernandes, M.H.; de Jesus, C.S. Determinants of falls in
community-dwelling elderly: Hierarchical analysis. Public Health Nurs. 2014, 31, 290–297.
23. Tabbarah, M.; Crimmins, E.M.; Seeman, T.E. The relationship between cognitive and physical
performance: MacArthur studies of successful aging. J. Gerontol. Ser. A-Biol. Sci. Med. 2002, 51,
1259–1264.
24. Zanocchi, M.; Pilon, S.; Speme, S.; Nicola, E.; Corsinovi, L.; Ponte, E.; Cerrato, F.; Luppino, A.;
Martinelli, E.; Margolicci, A.; Molaschi, M. Falls in hospitalized elderly patients: Incidence and
risk factors. Recent. Prog. Med. 2004, 95, 570–574.
25. Kose, N.; Cuvalci, S.; Ekici, G.; Otman, A.S.; Karakaya, M.G. The risk factors of falls and their
correlation with balance, depression, cognitive impairment and mobility skills in elderly nursing
home residents. Saudi Med. J. 2005, 26, 978–981.
26. Vassallo, M.; Mallela, S.K.; Williams, A.; Kwan, J. Fall risk factors in elderly patients with
cognitive impairment on rehabilitation wards. Geriatr. Gerontol. Int. 2009, 9, 41–46.
27. Hauer, K.; Pfisterer, M.; Weber, C.; Wezler, N.; Kliegel, M.; Oster, P. Cognitive impairment
decreases postural control during dual tasks in geriatric patients with a history of severe falls.
J. Amer. Geriatr. Soc. 2003, 51, 1638–1644.
28. Rosano, C.; Simonsick, E.M.; Harris, T.B.; Rubin, S.; Kritchevsky, S.B.; Brach, J.; Wisser, M.;
Yaffe, K.; Newman, A.B. Association between physical and cognitive function in healthy elderly:
Health aging and body composition study. Neuroepidemiology 2005, 24, 8–14.
29. Canning, C.G.; Sherrington, C.; Lord, S.R.; Close, J.C.; Heritier, S.; Heller, G.Z.; Howard, K.;
Allen, N.E.; Latt, M.D.; Murray, S.M.; et al. Exercise for falls prevention in Parkinson disease:
A randomized controlled trial. Neurology 2014, 84, 304–312.
30. Kallin, K.; Lundin-Olsson, L.; Jensen, J.; Nyberg, L.; Gustafson, Y. Predisposing and precipitating
factors for falls among older people in residential care. Public Health 2002, 116, 163–271.
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article
distributed under the terms and conditions of the Creative Commons Attribution license
(http://creativecommons.org/licenses/by/4.0/).
20. Sihvonen, S.; Kulmala, J.; Kallinen, M.; Alén, M.; Kiviranta, I.; Sipilä, S. Postural balance and
self-reported balance confidence in older adults with a hip fracture history. Gerontology 2009, 55,
630–636.
21. Nieto, M.L.; Albert, S.M.; Morrow, L.A.; Saxton, J. Cognitive status and physical function in
older African Americans. J. Amer. Geriatr. Soc. 2008, 56, 2014–2019.
22. Brito, T.A.; Coqueiro, R.S.; Fernandes, M.H.; de Jesus, C.S. Determinants of falls in
community-dwelling elderly: Hierarchical analysis. Public Health Nurs. 2014, 31, 290–297.
23. Tabbarah, M.; Crimmins, E.M.; Seeman, T.E. The relationship between cognitive and physical
performance: MacArthur studies of successful aging. J. Gerontol. Ser. A-Biol. Sci. Med. 2002, 51,
1259–1264.
24. Zanocchi, M.; Pilon, S.; Speme, S.; Nicola, E.; Corsinovi, L.; Ponte, E.; Cerrato, F.; Luppino, A.;
Martinelli, E.; Margolicci, A.; Molaschi, M. Falls in hospitalized elderly patients: Incidence and
risk factors. Recent. Prog. Med. 2004, 95, 570–574.
25. Kose, N.; Cuvalci, S.; Ekici, G.; Otman, A.S.; Karakaya, M.G. The risk factors of falls and their
correlation with balance, depression, cognitive impairment and mobility skills in elderly nursing
home residents. Saudi Med. J. 2005, 26, 978–981.
26. Vassallo, M.; Mallela, S.K.; Williams, A.; Kwan, J. Fall risk factors in elderly patients with
cognitive impairment on rehabilitation wards. Geriatr. Gerontol. Int. 2009, 9, 41–46.
27. Hauer, K.; Pfisterer, M.; Weber, C.; Wezler, N.; Kliegel, M.; Oster, P. Cognitive impairment
decreases postural control during dual tasks in geriatric patients with a history of severe falls.
J. Amer. Geriatr. Soc. 2003, 51, 1638–1644.
28. Rosano, C.; Simonsick, E.M.; Harris, T.B.; Rubin, S.; Kritchevsky, S.B.; Brach, J.; Wisser, M.;
Yaffe, K.; Newman, A.B. Association between physical and cognitive function in healthy elderly:
Health aging and body composition study. Neuroepidemiology 2005, 24, 8–14.
29. Canning, C.G.; Sherrington, C.; Lord, S.R.; Close, J.C.; Heritier, S.; Heller, G.Z.; Howard, K.;
Allen, N.E.; Latt, M.D.; Murray, S.M.; et al. Exercise for falls prevention in Parkinson disease:
A randomized controlled trial. Neurology 2014, 84, 304–312.
30. Kallin, K.; Lundin-Olsson, L.; Jensen, J.; Nyberg, L.; Gustafson, Y. Predisposing and precipitating
factors for falls among older people in residential care. Public Health 2002, 116, 163–271.
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article
distributed under the terms and conditions of the Creative Commons Attribution license
(http://creativecommons.org/licenses/by/4.0/).
1 out of 11
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.