PG Program: Inter, Intra, and Transprofessional Practice in Profession
VerifiedAdded on 2023/06/10
|7
|6404
|485
Essay
AI Summary
This essay critically evaluates the main themes in professional practice literature, including interprofessional, intraprofessional, and transprofessional practice, and discusses how these concepts apply to the author's professional practice. It also explores a challenging aspect of their professional practice and considers potential solutions to enhance it. The essay references a seven-phase procedure outlined by Jabareen [14], with specific procedures modified according to the nature and requirements of the current study [14]. The author reflects on interprofessional collaboration (IPC) which is a complex and multidimensional process in which different professionals work together to positively impact health care. The work raises some interesting points for discussion, and some personal reflections. However, the essay consists mostly of a collection of abstract generalised statements in need of supporting evidence and referencing in many places. Evidence could be in the form of supporting materials from the course and/or real examples from your practice.

http://informahealthcare.com/dre
ISSN 0963-8288 print/ISSN 1464-5165 online
DisabilRehabil,Early Online:1–7
! 2014 Informa UK Ltd.DOI:10.3109/09638288.2014.918193
EDUCATION AND TRAINING
Interprofessionalcollaboration:development of a tool to enhance
knowledge translation
Emmanuelle Careau1,2
, Nathalie Brie`re3, Nathalie Houle2, Serge Dumont3,4
, Claude Vincent1,2
, and Bonnie Swaine5,6
1Center for Interdisciplinary Research in Rehabilitation and SocialIntegration (CIRRIS),Quebec City,Quebec,Canada,2Faculty of Medicine,
Universite´ Laval, Quebec City, Quebec, Canada,3Centre de Sante´ et Services Sociaux de la Vieille-Capitale, Quebec City, Quebec, Canada,4School of
SocialWork,Universite´ Laval,Quebec City,Quebec,Canada,5Schoolof Rehabilitation,Universite´ de Montre´al, Montre´al, Quebec,Canada,and
6Centre for Interdisciplinary Research in Rehabilitation of Greater Montreal(CRIR),Quebec City,Quebec,Canada
Abstract
Purpose:Interprofessionalcollaboration (IPC)is a complex and multidimensionalprocess in
which differentprofessionalswork togetherto positively impacthealth care.In order to
enhance the knowledge translation and improve rehabilitation practitioners’knowledge and
skills toward IPC, it is essential to develop a comprehensive tool that illustrates how IPC should
be operationalized in clinicalsettings.Thus,this study aims atdeveloping,validating and
assessing the usefulnessof a comprehensive framework illustrating how the interactional
factors should be operationalized in clinicalsettings to promote good collaboration.Methods:
This article presents a mixed-method approach used to involve rehabilitation stakeholders
(n ¼ 20)in the developmentand validation ofan IPC framework according to a systematic
seven-phase procedure.Results:The final framework shows five types of practices according to
four components:the situation of the client and family, the intention underlying the
collaboration,the interaction between practitioners,and the combining of disciplinary
knowledge.Conclusion:The framework integrates the current scientific knowledge and clinical
experience regarding the conceptualization of IPC.It is considered as a relevant and useful KT
tool to enhance IPC knowledge for various stakeholders,especially in the rehabilitation field.
This comprehensive and contextualized framework could be used in undergraduate and
continuing education initiatives.
ä Implications for Rehabilitation
The framework developed integrates the current scientific knowledge and clinical experience
regarding the conceptualization of interprofessional collaboration (IPC) that is relevant to the
rehabilitation field.
It could be used in undergraduate and continuing education initiatives to help learners
understand the multidimensionaland dynamic nature of IPC.
It could be useful to support practitioners and managers from the rehabilitation field in their
efforts to optimize collaborative practice within their organization.
Keywords
Interprofessionalcollaboration,
interprofessionalrelations,
knowledge translation
History
Received 26 August 2013
Revised 15 April2014
Accepted 22 April2014
Published online 14 May 2014
Introduction
According to a recentreportof the World Health Organization
(WHO) (2010),the developmentof a ‘‘collaborative practice-
ready health workforce’’ is the main determinantof successful
interprofessionalcollaboration (IPC).A ‘‘collaborative practice-
ready health worker’’ is a practitioner ‘‘who has learned how to
work in an interprofessional team and who is competent to do so
(p. 7)’’ [1]. However, consulting the scientific literature, in itself,
does notnecessarily help practitioners understand clearly how
they should interactwith each otherto achieve optimalIPC
practices in a rehabilitation context.Indeed,Reeves et al.(2010)
report on the limited theory about IPC in the literature and writ
that,although all researchers generally accept that IPC improve
health and social care, few have focused on developing underly
empirically-based theory [2].Researchersoften conceptualize
IPC using a three-stage‘‘input–process–output’’architecture
derived from organizationalliteratureon team effectiveness,
mostly emphasizing inputs (determinants) and outputs (results
but ignoringthe system’sconstitution.This ‘‘black box’’
approach may be sufficientfor a simple phenomenon,butIPC
is recognized as complex,multidimensionaland evolving [3,4].
Thus,it is essentialthatrehabilitation practitioners understand
clearly whathappens ‘‘inside the box’’,i.e.how IPC should be
operationalized within different settings and with various client
Address for correspondence:Dr. Emmanuelle Careau,PhD, Center for
InterdisciplinaryResearchin Rehabilitationand Social Integration
(CIRRIS), Quebec City,Quebec,Canada.E-mail:emmanuelle.careau@
rea.ulaval.ca
Disabil Rehabil Downloaded from informahealthcare.com by Karolinska Institutet University Library on 06/02/14
For personal use only.
ISSN 0963-8288 print/ISSN 1464-5165 online
DisabilRehabil,Early Online:1–7
! 2014 Informa UK Ltd.DOI:10.3109/09638288.2014.918193
EDUCATION AND TRAINING
Interprofessionalcollaboration:development of a tool to enhance
knowledge translation
Emmanuelle Careau1,2
, Nathalie Brie`re3, Nathalie Houle2, Serge Dumont3,4
, Claude Vincent1,2
, and Bonnie Swaine5,6
1Center for Interdisciplinary Research in Rehabilitation and SocialIntegration (CIRRIS),Quebec City,Quebec,Canada,2Faculty of Medicine,
Universite´ Laval, Quebec City, Quebec, Canada,3Centre de Sante´ et Services Sociaux de la Vieille-Capitale, Quebec City, Quebec, Canada,4School of
SocialWork,Universite´ Laval,Quebec City,Quebec,Canada,5Schoolof Rehabilitation,Universite´ de Montre´al, Montre´al, Quebec,Canada,and
6Centre for Interdisciplinary Research in Rehabilitation of Greater Montreal(CRIR),Quebec City,Quebec,Canada
Abstract
Purpose:Interprofessionalcollaboration (IPC)is a complex and multidimensionalprocess in
which differentprofessionalswork togetherto positively impacthealth care.In order to
enhance the knowledge translation and improve rehabilitation practitioners’knowledge and
skills toward IPC, it is essential to develop a comprehensive tool that illustrates how IPC should
be operationalized in clinicalsettings.Thus,this study aims atdeveloping,validating and
assessing the usefulnessof a comprehensive framework illustrating how the interactional
factors should be operationalized in clinicalsettings to promote good collaboration.Methods:
This article presents a mixed-method approach used to involve rehabilitation stakeholders
(n ¼ 20)in the developmentand validation ofan IPC framework according to a systematic
seven-phase procedure.Results:The final framework shows five types of practices according to
four components:the situation of the client and family, the intention underlying the
collaboration,the interaction between practitioners,and the combining of disciplinary
knowledge.Conclusion:The framework integrates the current scientific knowledge and clinical
experience regarding the conceptualization of IPC.It is considered as a relevant and useful KT
tool to enhance IPC knowledge for various stakeholders,especially in the rehabilitation field.
This comprehensive and contextualized framework could be used in undergraduate and
continuing education initiatives.
ä Implications for Rehabilitation
The framework developed integrates the current scientific knowledge and clinical experience
regarding the conceptualization of interprofessional collaboration (IPC) that is relevant to the
rehabilitation field.
It could be used in undergraduate and continuing education initiatives to help learners
understand the multidimensionaland dynamic nature of IPC.
It could be useful to support practitioners and managers from the rehabilitation field in their
efforts to optimize collaborative practice within their organization.
Keywords
Interprofessionalcollaboration,
interprofessionalrelations,
knowledge translation
History
Received 26 August 2013
Revised 15 April2014
Accepted 22 April2014
Published online 14 May 2014
Introduction
According to a recentreportof the World Health Organization
(WHO) (2010),the developmentof a ‘‘collaborative practice-
ready health workforce’’ is the main determinantof successful
interprofessionalcollaboration (IPC).A ‘‘collaborative practice-
ready health worker’’ is a practitioner ‘‘who has learned how to
work in an interprofessional team and who is competent to do so
(p. 7)’’ [1]. However, consulting the scientific literature, in itself,
does notnecessarily help practitioners understand clearly how
they should interactwith each otherto achieve optimalIPC
practices in a rehabilitation context.Indeed,Reeves et al.(2010)
report on the limited theory about IPC in the literature and writ
that,although all researchers generally accept that IPC improve
health and social care, few have focused on developing underly
empirically-based theory [2].Researchersoften conceptualize
IPC using a three-stage‘‘input–process–output’’architecture
derived from organizationalliteratureon team effectiveness,
mostly emphasizing inputs (determinants) and outputs (results
but ignoringthe system’sconstitution.This ‘‘black box’’
approach may be sufficientfor a simple phenomenon,butIPC
is recognized as complex,multidimensionaland evolving [3,4].
Thus,it is essentialthatrehabilitation practitioners understand
clearly whathappens ‘‘inside the box’’,i.e.how IPC should be
operationalized within different settings and with various client
Address for correspondence:Dr. Emmanuelle Careau,PhD, Center for
InterdisciplinaryResearchin Rehabilitationand Social Integration
(CIRRIS), Quebec City,Quebec,Canada.E-mail:emmanuelle.careau@
rea.ulaval.ca
Disabil Rehabil Downloaded from informahealthcare.com by Karolinska Institutet University Library on 06/02/14
For personal use only.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
The term IPC is often defined as‘‘the processin which
differentprofessionalgroups work together to positively impact
healthcare. IPC involves a negotiatedagreementbetween
professionals which values the expertise and contributions that
various healthcare professionals bring to patientcare’’ [5,p. 2].
However,the IPC literature yieldsmany surrogate orrelated
concepts.Surrogate concepts include allthe terms thatdefine
the phenomenon,while related concepts include most,butnot
all, of the defining attributes of IPC (i.e.the concept’s essential
characteristics)[6]. Petri (2010) identifiedinterdisciplinary
collaboration,interprofessionalcollaboration,interdisciplinary
team,multidisciplinarycollaboration,interdisciplinaryteam-
work, interdisciplinarypracticeand teamworkas surrogate
concepts for IPC thatare often used interchangeably by authors
[7].Related concepts include team,integrated team,cooperative
work,cooperation,jointpractice,working group [7],teamwork
[8], cooperation,competition,compromise,avoidance,accom-
modation and conflictresolution [9].The problem is thatvery
few authors carefully define these terms,and when definitions
are provided,they are often contradictory.Nevertheless,in the
literature there are severalframeworks thatattemptto identify
the relationsbetweentheseconcepts,and thesegenerally
illustrateIPC processesalong a continuum.Some authors
depictan evolution of professionalautonomy,with autonomous
and parallelpractices atone end and a more integrated practice
at the other. Here, concept-based prefixes as defined by Leathard
[10] (e.g. uni-, multi-, inter-,trans-)are often used.Other
authorsfocuson putting in sequence process-based keywords
such as consultation,coordinationand cooperation[11].
However,theseframeworksare eitherincompleteor do not
adequately reflectthe currentstateof knowledge.Moreover,
becausethey havenot beendevelopedin order to ensure
effectiveknowledgetranslation(KT) betweenscholarsand
practitioners,it is difficult to use them for an educational
purpose.KT is defined as a dynamic and iterative process that
includes synthesis,dissemination,exchange and ethically-sound
application of knowledge [12].To develop effective educational
strategiesaiming at improvingpractitioners’knowledgeand
skills toward IPC,it is essentialto contextualize the body of
knowledge and tailorthe message and medium to the audience
[13].In this article,we describe a mixed-method approach used
to involve rehabilitationstakeholdersin the development,
validationand usefulnessassessmentof a comprehensive
framework illustrating how IPC should be operationalized in
clinicalsettings to promote good collaboration.
Methods
This initiative was partof a research projectapproved by the
ethicscommittee ofthe Institutde re´adaptation en de´ficience
physique de Que´bec (project #2008-145). To develop and validate
this new KT tool on IPC, we followed a seven-phase
procedure outlined by Jabareen [14],with specific procedures
modified according to the nature and requirements of the current
study [14].
Phase 1:Mapping the selected data sources
The first phase in developing a comprehensive framework is
to map the literatureregardingthe phenomenonbeing
studied [14].Our data sourcesconsisted ofgovernmentaland
institutionalreports, websitesof organizationsdedicated
to interprofessionaleducation/collaborativepractice(IPECP),
and journal articles retrievedfrom the Medline and
CINAHL databases with a search strategy using the keywords
‘‘interprofessionalrelations[MESH]’’; ‘‘interprofessional*’’,
multiprofessional*’’,‘‘transprofessional*’’,‘‘interdisciplinary*’’,
‘‘multidisciplinary*’’,‘‘transdisciplinar*’’1 AND ‘‘concept*’’,
‘‘model*’’, ‘‘theor*’’ ‘‘framework’’, ‘‘continuum’’, ‘‘spectrum’’.
In total,we consulted 60 journal articles,20 reports,20 clinical
guidelines,as wellas severalbooks and theses on IPECP [15].
Three of the authors(E.C., N.H., and N.B.) also attended
internationaland nationalIPECP conferencesoverthe past5
years and engagedin informaldiscussionswith attending
practitioners and scholars to better understand the phenomeno
Phase 2:Extensive reading and categorizing of the
selected data
After examining the data,E.C., N.H., and N.B.discussed their
understanding of the texts and shared information obtained du
the conferences,workshopsand informaldiscussions.They
categorized data according to theirsource (scientific literature,
clinicalguidelines,politicalreports,editorial)and theiruse of
keywords (concept-based,process-based or agency-based) [10].
Phase 3:Identifying and naming concepts
The aim in this phase is ‘‘to read and reread’’ the selected data
orderto ‘‘discover’’concepts[14]. Conceptsrelated to IPC
characteristics were identified in discussion sessions among the
authors.
Phase 4:Deconstructing and categorizing the concepts
Jabareen[14] suggestscreatinga table to ‘‘identify[each
concept’s]main attributes,characteristics,assumptions,and
role’’ (p.54).Then,we categorized the concepts and character-
istics according to ‘‘inputs’’,‘‘process’’ and ‘‘outputs’’,in order
to conserve only those related to processes for our framework.
Phase 5:Integrating concepts and Phase 6:Synthesis,
resynthesis,and making it all make sense
According to Jabareen [14],the aim of the fifth and sixth phase
‘‘is to integrate and group together concepts that have similari
to one new concept’’(p. 54) and to synthesize the remaining
concepts into a comprehensive framework.To do so, the first
author synthesized the results thus far and presented the synth
to the others. This theorization process was iterative and includ
severalcycles of synthesis,discussion and data consultation to
produce an initial framework.
Phase 7:Validating the conceptual framework
Jabareen [14] suggests seeking validation among stakeholders
presenting the framework ata conference,a seminar,or some
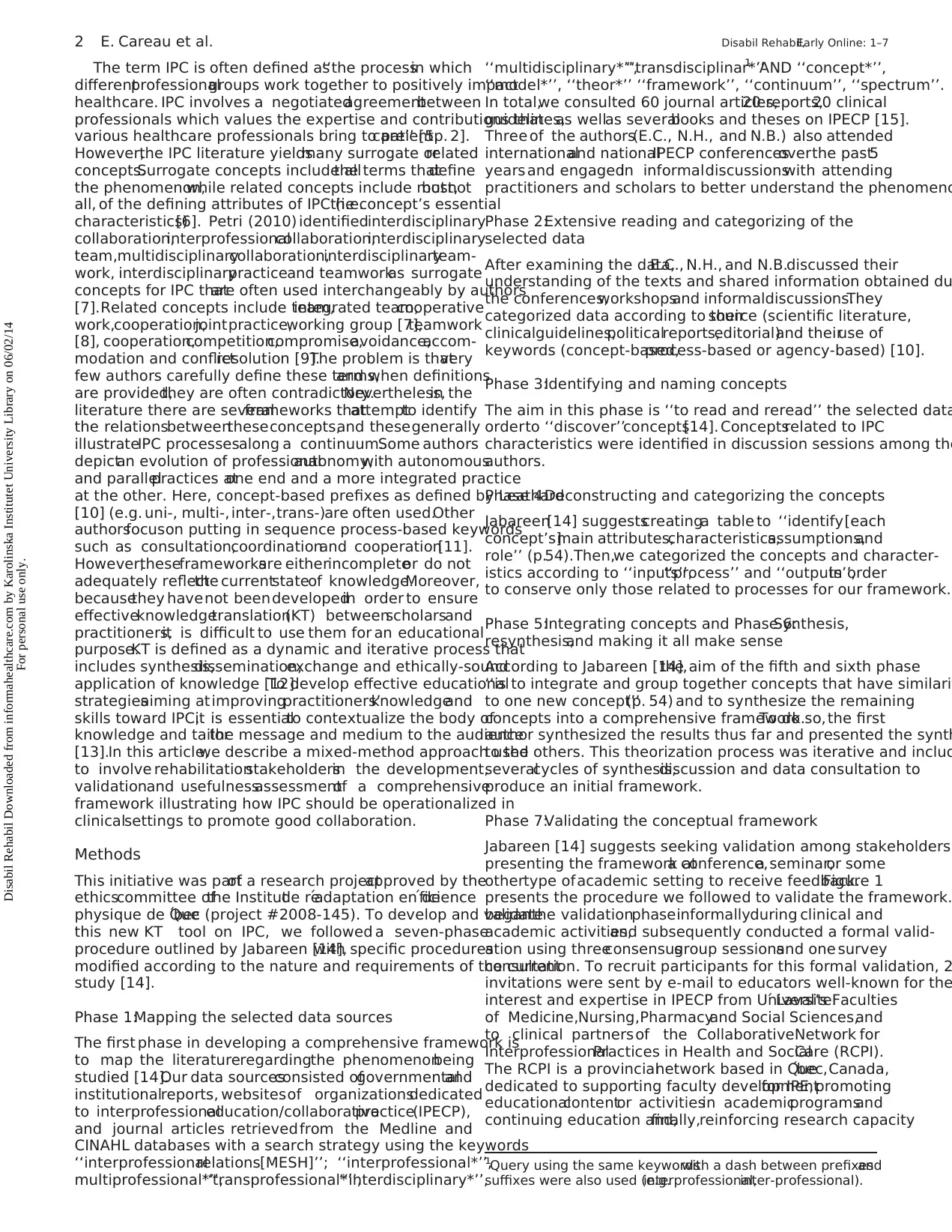
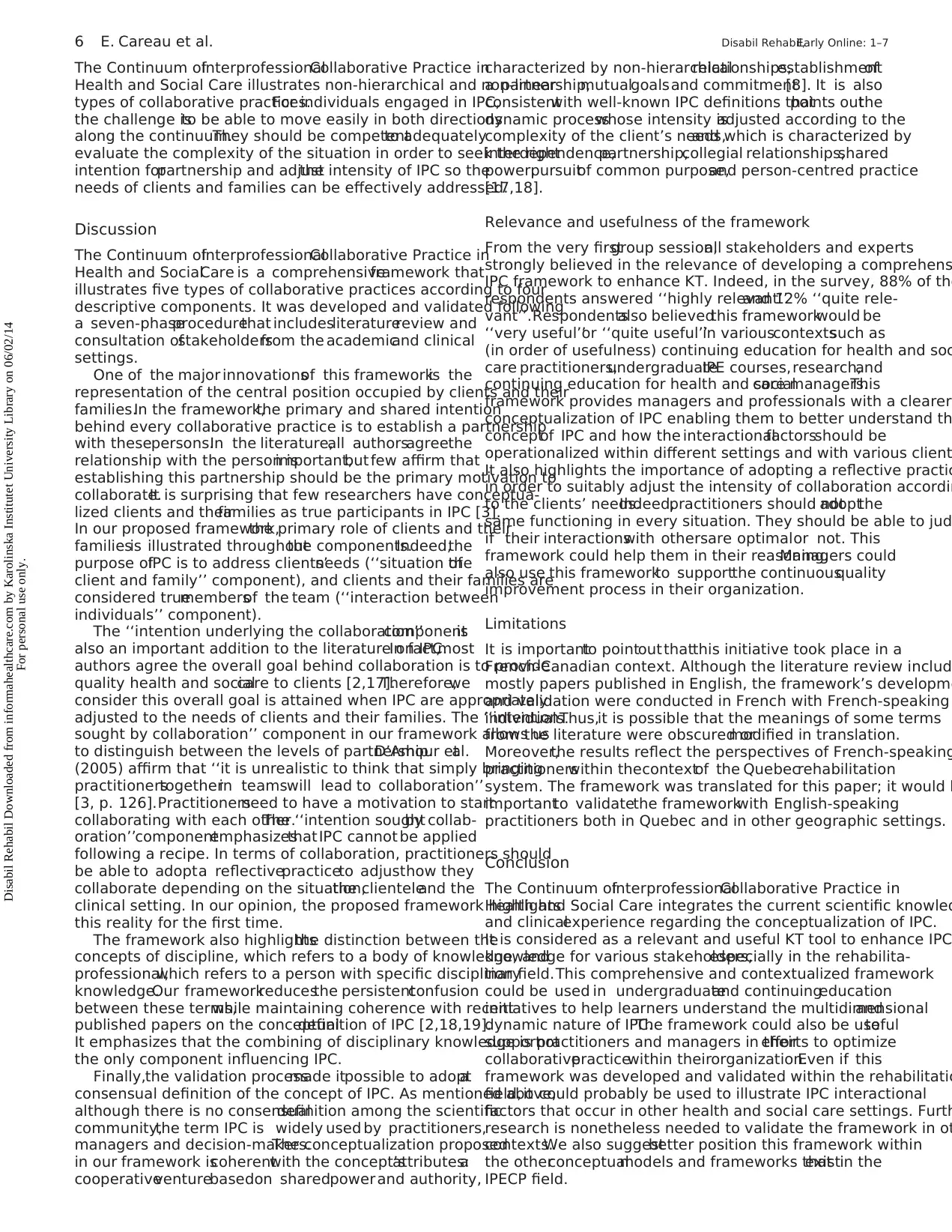
othertype ofacademic setting to receive feedback.Figure 1
presents the procedure we followed to validate the framework.
beganthe validationphaseinformallyduring clinical and
academic activities,and subsequently conducted a formal valid-
ation using threeconsensusgroup sessionsand one survey
consultation. To recruit participants for this formal validation, 2
invitations were sent by e-mail to educators well-known for the
interest and expertise in IPECP from Universite´ Laval’s Faculties
of Medicine,Nursing,Pharmacyand Social Sciences,and
to clinical partners of the CollaborativeNetwork for
InterprofessionalPractices in Health and SocialCare (RCPI).
The RCPI is a provincialnetwork based in Que´bec,Canada,
dedicated to supporting faculty developmentfor IPE,promoting
educationalcontentor activitiesin academicprogramsand
continuing education and,finally,reinforcing research capacity
1Query using the same keywordswith a dash between prefixesand
suffixes were also used (e.g.interprofessional,inter-professional).
2 E. Careau et al. Disabil Rehabil,Early Online: 1–7
Disabil Rehabil Downloaded from informahealthcare.com by Karolinska Institutet University Library on 06/02/14
For personal use only.
differentprofessionalgroups work together to positively impact
healthcare. IPC involves a negotiatedagreementbetween
professionals which values the expertise and contributions that
various healthcare professionals bring to patientcare’’ [5,p. 2].
However,the IPC literature yieldsmany surrogate orrelated
concepts.Surrogate concepts include allthe terms thatdefine
the phenomenon,while related concepts include most,butnot
all, of the defining attributes of IPC (i.e.the concept’s essential
characteristics)[6]. Petri (2010) identifiedinterdisciplinary
collaboration,interprofessionalcollaboration,interdisciplinary
team,multidisciplinarycollaboration,interdisciplinaryteam-
work, interdisciplinarypracticeand teamworkas surrogate
concepts for IPC thatare often used interchangeably by authors
[7].Related concepts include team,integrated team,cooperative
work,cooperation,jointpractice,working group [7],teamwork
[8], cooperation,competition,compromise,avoidance,accom-
modation and conflictresolution [9].The problem is thatvery
few authors carefully define these terms,and when definitions
are provided,they are often contradictory.Nevertheless,in the
literature there are severalframeworks thatattemptto identify
the relationsbetweentheseconcepts,and thesegenerally
illustrateIPC processesalong a continuum.Some authors
depictan evolution of professionalautonomy,with autonomous
and parallelpractices atone end and a more integrated practice
at the other. Here, concept-based prefixes as defined by Leathard
[10] (e.g. uni-, multi-, inter-,trans-)are often used.Other
authorsfocuson putting in sequence process-based keywords
such as consultation,coordinationand cooperation[11].
However,theseframeworksare eitherincompleteor do not
adequately reflectthe currentstateof knowledge.Moreover,
becausethey havenot beendevelopedin order to ensure
effectiveknowledgetranslation(KT) betweenscholarsand
practitioners,it is difficult to use them for an educational
purpose.KT is defined as a dynamic and iterative process that
includes synthesis,dissemination,exchange and ethically-sound
application of knowledge [12].To develop effective educational
strategiesaiming at improvingpractitioners’knowledgeand
skills toward IPC,it is essentialto contextualize the body of
knowledge and tailorthe message and medium to the audience
[13].In this article,we describe a mixed-method approach used
to involve rehabilitationstakeholdersin the development,
validationand usefulnessassessmentof a comprehensive
framework illustrating how IPC should be operationalized in
clinicalsettings to promote good collaboration.
Methods
This initiative was partof a research projectapproved by the
ethicscommittee ofthe Institutde re´adaptation en de´ficience
physique de Que´bec (project #2008-145). To develop and validate
this new KT tool on IPC, we followed a seven-phase
procedure outlined by Jabareen [14],with specific procedures
modified according to the nature and requirements of the current
study [14].
Phase 1:Mapping the selected data sources
The first phase in developing a comprehensive framework is
to map the literatureregardingthe phenomenonbeing
studied [14].Our data sourcesconsisted ofgovernmentaland
institutionalreports, websitesof organizationsdedicated
to interprofessionaleducation/collaborativepractice(IPECP),
and journal articles retrievedfrom the Medline and
CINAHL databases with a search strategy using the keywords
‘‘interprofessionalrelations[MESH]’’; ‘‘interprofessional*’’,
multiprofessional*’’,‘‘transprofessional*’’,‘‘interdisciplinary*’’,
‘‘multidisciplinary*’’,‘‘transdisciplinar*’’1 AND ‘‘concept*’’,
‘‘model*’’, ‘‘theor*’’ ‘‘framework’’, ‘‘continuum’’, ‘‘spectrum’’.
In total,we consulted 60 journal articles,20 reports,20 clinical
guidelines,as wellas severalbooks and theses on IPECP [15].
Three of the authors(E.C., N.H., and N.B.) also attended
internationaland nationalIPECP conferencesoverthe past5
years and engagedin informaldiscussionswith attending
practitioners and scholars to better understand the phenomeno
Phase 2:Extensive reading and categorizing of the
selected data
After examining the data,E.C., N.H., and N.B.discussed their
understanding of the texts and shared information obtained du
the conferences,workshopsand informaldiscussions.They
categorized data according to theirsource (scientific literature,
clinicalguidelines,politicalreports,editorial)and theiruse of
keywords (concept-based,process-based or agency-based) [10].
Phase 3:Identifying and naming concepts
The aim in this phase is ‘‘to read and reread’’ the selected data
orderto ‘‘discover’’concepts[14]. Conceptsrelated to IPC
characteristics were identified in discussion sessions among the
authors.
Phase 4:Deconstructing and categorizing the concepts
Jabareen[14] suggestscreatinga table to ‘‘identify[each
concept’s]main attributes,characteristics,assumptions,and
role’’ (p.54).Then,we categorized the concepts and character-
istics according to ‘‘inputs’’,‘‘process’’ and ‘‘outputs’’,in order
to conserve only those related to processes for our framework.
Phase 5:Integrating concepts and Phase 6:Synthesis,
resynthesis,and making it all make sense
According to Jabareen [14],the aim of the fifth and sixth phase
‘‘is to integrate and group together concepts that have similari
to one new concept’’(p. 54) and to synthesize the remaining
concepts into a comprehensive framework.To do so, the first
author synthesized the results thus far and presented the synth
to the others. This theorization process was iterative and includ
severalcycles of synthesis,discussion and data consultation to
produce an initial framework.
Phase 7:Validating the conceptual framework
Jabareen [14] suggests seeking validation among stakeholders
presenting the framework ata conference,a seminar,or some
othertype ofacademic setting to receive feedback.Figure 1
presents the procedure we followed to validate the framework.
beganthe validationphaseinformallyduring clinical and
academic activities,and subsequently conducted a formal valid-
ation using threeconsensusgroup sessionsand one survey
consultation. To recruit participants for this formal validation, 2
invitations were sent by e-mail to educators well-known for the
interest and expertise in IPECP from Universite´ Laval’s Faculties
of Medicine,Nursing,Pharmacyand Social Sciences,and
to clinical partners of the CollaborativeNetwork for
InterprofessionalPractices in Health and SocialCare (RCPI).
The RCPI is a provincialnetwork based in Que´bec,Canada,
dedicated to supporting faculty developmentfor IPE,promoting
educationalcontentor activitiesin academicprogramsand
continuing education and,finally,reinforcing research capacity
1Query using the same keywordswith a dash between prefixesand
suffixes were also used (e.g.interprofessional,inter-professional).
2 E. Careau et al. Disabil Rehabil,Early Online: 1–7
Disabil Rehabil Downloaded from informahealthcare.com by Karolinska Institutet University Library on 06/02/14
For personal use only.
and KT on IPECP. Targeted experts and stakeholders had either a
scientificknowledgeof IPC or expertisein how IPC is
experienceddaily in clinical settings.At eachstep of the
validation process, invitations were sent to all the targeted experts
and stakeholders, but the number who were able to attend differed
at each step.Experts’ and stakeholders’ occupations and discip-
linary backgrounds are provided in Table 1.
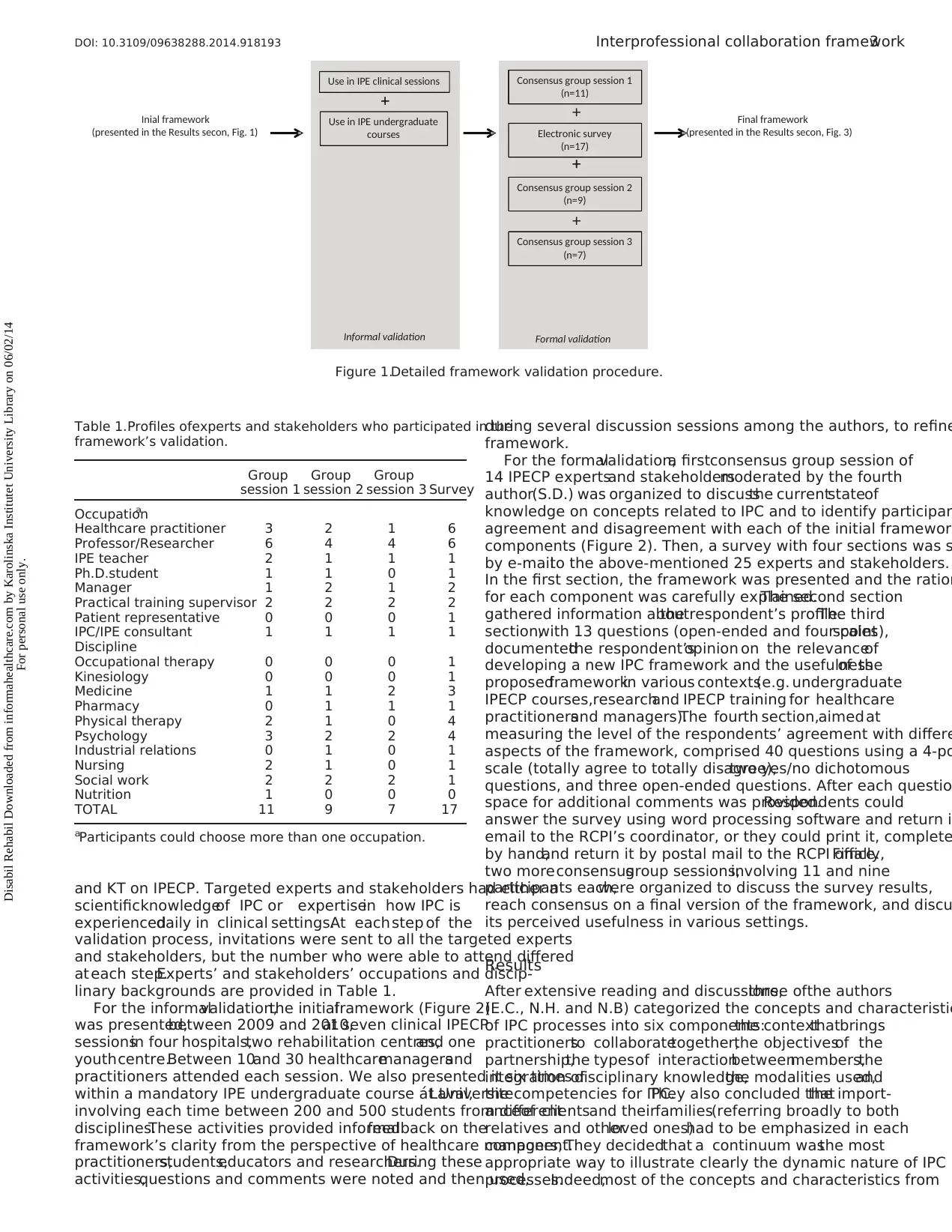
For the informalvalidation,the initialframework (Figure 2)
was presented,between 2009 and 2010,at seven clinical IPECP
sessionsin four hospitals,two rehabilitation centres,and one
youthcentre.Between 10and 30 healthcaremanagersand
practitioners attended each session. We also presented it six times
within a mandatory IPE undergraduate course at Universite´ Laval,
involving each time between 200 and 500 students from different
disciplines.These activities provided informalfeedback on the
framework’s clarity from the perspective of healthcare managers,
practitioners,students,educators and researchers.During these
activities,questions and comments were noted and then used,
during several discussion sessions among the authors, to refine
framework.
For the formalvalidation,a firstconsensus group session of
14 IPECP expertsand stakeholdersmoderated by the fourth
author(S.D.) was organized to discussthe currentstateof
knowledge on concepts related to IPC and to identify participan
agreement and disagreement with each of the initial framework
components (Figure 2). Then, a survey with four sections was s
by e-mailto the above-mentioned 25 experts and stakeholders.
In the first section, the framework was presented and the ration
for each component was carefully explained.The second section
gathered information aboutthe respondent’s profile.The third
section,with 13 questions (open-ended and four-pointscales),
documentedthe respondent’sopinion on the relevanceof
developing a new IPC framework and the usefulnessof the
proposedframeworkin various contexts(e.g. undergraduate
IPECP courses,researchand IPECP training for healthcare
practitionersand managers).The fourth section,aimed at
measuring the level of the respondents’ agreement with differe
aspects of the framework, comprised 40 questions using a 4-po
scale (totally agree to totally disagree),two yes/no dichotomous
questions, and three open-ended questions. After each questio
space for additional comments was provided.Respondents could
answer the survey using word processing software and return i
email to the RCPI’s coordinator, or they could print it, complete
by hand,and return it by postal mail to the RCPI office.Finally,
two moreconsensusgroup sessions,involving 11 and nine
participants each,were organized to discuss the survey results,
reach consensus on a final version of the framework, and discu
its perceived usefulness in various settings.
Results
After extensive reading and discussions,three ofthe authors
(E.C., N.H. and N.B) categorized the concepts and characteristic
of IPC processes into six components:the contextthatbrings
practitionersto collaboratetogether,the objectivesof the
partnership,the typesof interactionbetweenmembers,the
integration ofdisciplinary knowledge,the modalities used,and
the competencies for IPC.They also concluded thatthe import-
anceof clientsand theirfamilies(referring broadly to both
relatives and otherloved ones)had to be emphasized in each
component.They decidedthat a continuum wasthe most
appropriate way to illustrate clearly the dynamic nature of IPC
processes.Indeed,most of the concepts and characteristics from
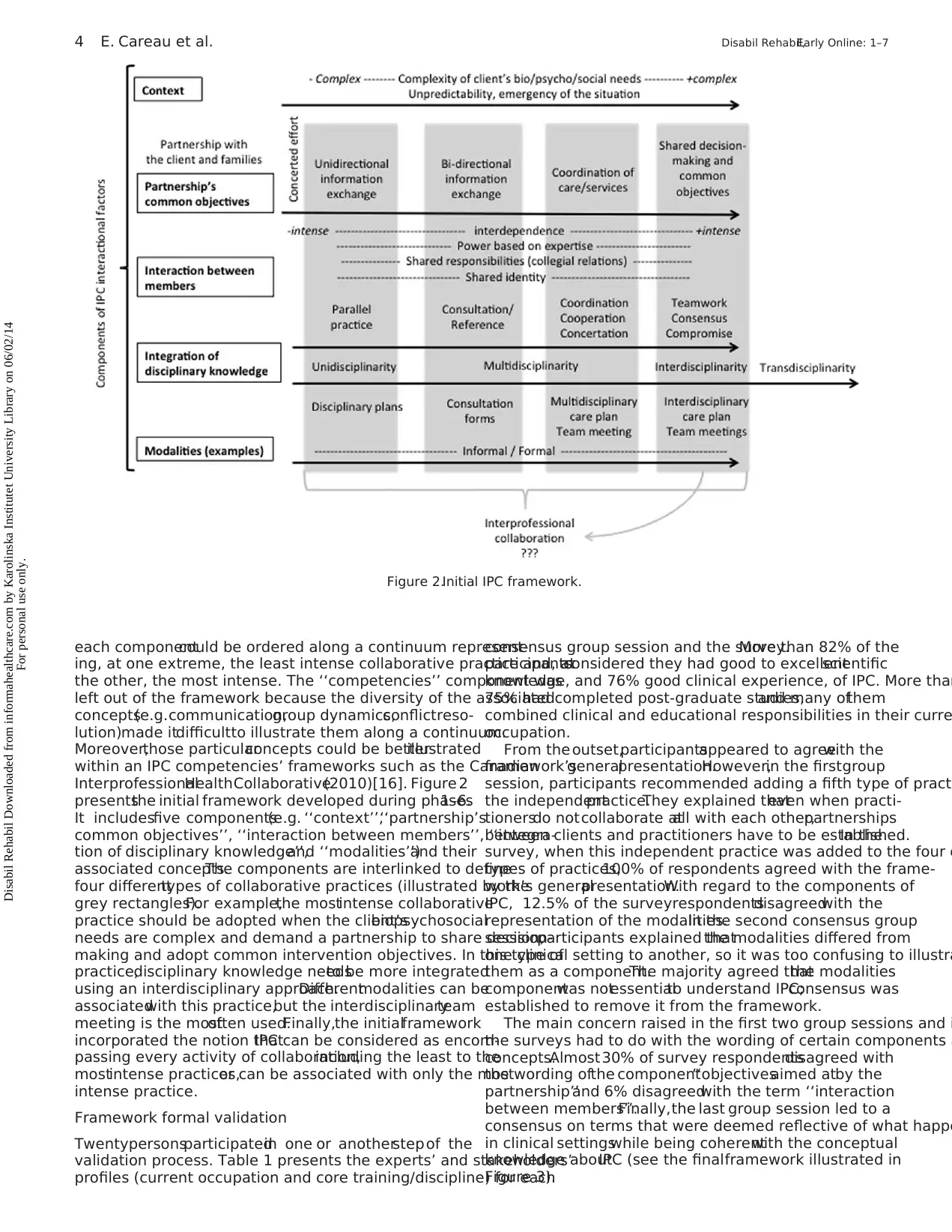
Table 1.Profiles ofexperts and stakeholders who participated in the
framework’s validation.
Group
session 1
Group
session 2
Group
session 3 Survey
Occupationa
Healthcare practitioner 3 2 1 6
Professor/Researcher 6 4 4 6
IPE teacher 2 1 1 1
Ph.D.student 1 1 0 1
Manager 1 2 1 2
Practical training supervisor 2 2 2 2
Patient representative 0 0 0 1
IPC/IPE consultant 1 1 1 1
Discipline
Occupational therapy 0 0 0 1
Kinesiology 0 0 0 1
Medicine 1 1 2 3
Pharmacy 0 1 1 1
Physical therapy 2 1 0 4
Psychology 3 2 2 4
Industrial relations 0 1 0 1
Nursing 2 1 0 1
Social work 2 2 2 1
Nutrition 1 0 0 0
TOTAL 11 9 7 17
aParticipants could choose more than one occupation.
Use in IPE clinical sessions
+
Consensus group session 1
(n=11)
Inial framework
(presented in the Results secon, Fig. 1)
Final framework
(presented in the Results secon, Fig. 3)
Use in IPE undergraduate
courses
+
Electronic survey
(n=17)
+
+
Consensus group session 2
(n=9)
+
+
Consensus group session 3
(n=7)
Informal validation Formal validation
Figure 1.Detailed framework validation procedure.
DOI: 10.3109/09638288.2014.918193 Interprofessional collaboration framework3
Disabil Rehabil Downloaded from informahealthcare.com by Karolinska Institutet University Library on 06/02/14
For personal use only.
scientificknowledgeof IPC or expertisein how IPC is
experienceddaily in clinical settings.At eachstep of the
validation process, invitations were sent to all the targeted experts
and stakeholders, but the number who were able to attend differed
at each step.Experts’ and stakeholders’ occupations and discip-
linary backgrounds are provided in Table 1.
For the informalvalidation,the initialframework (Figure 2)
was presented,between 2009 and 2010,at seven clinical IPECP
sessionsin four hospitals,two rehabilitation centres,and one
youthcentre.Between 10and 30 healthcaremanagersand
practitioners attended each session. We also presented it six times
within a mandatory IPE undergraduate course at Universite´ Laval,
involving each time between 200 and 500 students from different
disciplines.These activities provided informalfeedback on the
framework’s clarity from the perspective of healthcare managers,
practitioners,students,educators and researchers.During these
activities,questions and comments were noted and then used,
during several discussion sessions among the authors, to refine
framework.
For the formalvalidation,a firstconsensus group session of
14 IPECP expertsand stakeholdersmoderated by the fourth
author(S.D.) was organized to discussthe currentstateof
knowledge on concepts related to IPC and to identify participan
agreement and disagreement with each of the initial framework
components (Figure 2). Then, a survey with four sections was s
by e-mailto the above-mentioned 25 experts and stakeholders.
In the first section, the framework was presented and the ration
for each component was carefully explained.The second section
gathered information aboutthe respondent’s profile.The third
section,with 13 questions (open-ended and four-pointscales),
documentedthe respondent’sopinion on the relevanceof
developing a new IPC framework and the usefulnessof the
proposedframeworkin various contexts(e.g. undergraduate
IPECP courses,researchand IPECP training for healthcare
practitionersand managers).The fourth section,aimed at
measuring the level of the respondents’ agreement with differe
aspects of the framework, comprised 40 questions using a 4-po
scale (totally agree to totally disagree),two yes/no dichotomous
questions, and three open-ended questions. After each questio
space for additional comments was provided.Respondents could
answer the survey using word processing software and return i
email to the RCPI’s coordinator, or they could print it, complete
by hand,and return it by postal mail to the RCPI office.Finally,
two moreconsensusgroup sessions,involving 11 and nine
participants each,were organized to discuss the survey results,
reach consensus on a final version of the framework, and discu
its perceived usefulness in various settings.
Results
After extensive reading and discussions,three ofthe authors
(E.C., N.H. and N.B) categorized the concepts and characteristic
of IPC processes into six components:the contextthatbrings
practitionersto collaboratetogether,the objectivesof the
partnership,the typesof interactionbetweenmembers,the
integration ofdisciplinary knowledge,the modalities used,and
the competencies for IPC.They also concluded thatthe import-
anceof clientsand theirfamilies(referring broadly to both
relatives and otherloved ones)had to be emphasized in each
component.They decidedthat a continuum wasthe most
appropriate way to illustrate clearly the dynamic nature of IPC
processes.Indeed,most of the concepts and characteristics from
Table 1.Profiles ofexperts and stakeholders who participated in the
framework’s validation.
Group
session 1
Group
session 2
Group
session 3 Survey
Occupationa
Healthcare practitioner 3 2 1 6
Professor/Researcher 6 4 4 6
IPE teacher 2 1 1 1
Ph.D.student 1 1 0 1
Manager 1 2 1 2
Practical training supervisor 2 2 2 2
Patient representative 0 0 0 1
IPC/IPE consultant 1 1 1 1
Discipline
Occupational therapy 0 0 0 1
Kinesiology 0 0 0 1
Medicine 1 1 2 3
Pharmacy 0 1 1 1
Physical therapy 2 1 0 4
Psychology 3 2 2 4
Industrial relations 0 1 0 1
Nursing 2 1 0 1
Social work 2 2 2 1
Nutrition 1 0 0 0
TOTAL 11 9 7 17
aParticipants could choose more than one occupation.
Use in IPE clinical sessions
+
Consensus group session 1
(n=11)
Inial framework
(presented in the Results secon, Fig. 1)
Final framework
(presented in the Results secon, Fig. 3)
Use in IPE undergraduate
courses
+
Electronic survey
(n=17)
+
+
Consensus group session 2
(n=9)
+
+
Consensus group session 3
(n=7)
Informal validation Formal validation
Figure 1.Detailed framework validation procedure.
DOI: 10.3109/09638288.2014.918193 Interprofessional collaboration framework3
Disabil Rehabil Downloaded from informahealthcare.com by Karolinska Institutet University Library on 06/02/14
For personal use only.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
each componentcould be ordered along a continuum represent-
ing, at one extreme, the least intense collaborative practice and, at
the other, the most intense. The ‘‘competencies’’ component was
left out of the framework because the diversity of the associated
concepts(e.g.communication,group dynamics,conflictreso-
lution)made itdifficultto illustrate them along a continuum.
Moreover,those particularconcepts could be betterillustrated
within an IPC competencies’ frameworks such as the Canadian
InterprofessionalHealthCollaborative(2010)[16]. Figure 2
presentsthe initial framework developed during phases1–6.
It includesfive components(e.g. ‘‘context’’,‘‘partnership’s
common objectives’’, ‘‘interaction between members’’, ‘‘integra-
tion of disciplinary knowledge’’,and ‘‘modalities’’)and their
associated concepts.The components are interlinked to define
four differenttypes of collaborative practices (illustrated by the
grey rectangles).For example,the mostintense collaborative
practice should be adopted when the client’sbiopsychosocial
needs are complex and demand a partnership to share decision-
making and adopt common intervention objectives. In this type of
practice,disciplinary knowledge needsto be more integrated
using an interdisciplinary approach.Differentmodalities can be
associatedwith this practice,but the interdisciplinaryteam
meeting is the mostoften used.Finally,the initialframework
incorporated the notion thatIPC can be considered as encom-
passing every activity of collaboration,including the least to the
mostintense practices,or can be associated with only the most
intense practice.
Framework formal validation
Twentypersonsparticipatedin one or anotherstep of the
validation process. Table 1 presents the experts’ and stakeholders’
profiles (current occupation and core training/discipline) for each
consensus group session and the survey.More than 82% of the
participantsconsidered they had good to excellentscientific
knowledge, and 76% good clinical experience, of IPC. More than
75% had completed post-graduate studies,and many ofthem
combined clinical and educational responsibilities in their curre
occupation.
From the outset,participantsappeared to agreewith the
framework’sgeneralpresentation.However,in the firstgroup
session, participants recommended adding a fifth type of pract
the independentpractice.They explained thateven when practi-
tionersdo notcollaborate atall with each other,partnerships
between clients and practitioners have to be established.In the
survey, when this independent practice was added to the four o
types of practices,100% of respondents agreed with the frame-
work’s generalpresentation.With regard to the components of
IPC, 12.5% of the surveyrespondentsdisagreedwith the
representation of the modalities.In the second consensus group
session,participants explained thatthe modalities differed from
one clinical setting to another, so it was too confusing to illustra
them as a component.The majority agreed thatthe modalities
componentwas notessentialto understand IPC;consensus was
established to remove it from the framework.
The main concern raised in the first two group sessions and i
the surveys had to do with the wording of certain components a
concepts.Almost30% of survey respondentsdisagreed with
the wording ofthe component‘‘objectivesaimed atby the
partnership’’and 6% disagreedwith the term ‘‘interaction
between members’’.Finally,the last group session led to a
consensus on terms that were deemed reflective of what happe
in clinical settingswhile being coherentwith the conceptual
knowledge aboutIPC (see the finalframework illustrated in
Figure 3).
Figure 2.Initial IPC framework.
4 E. Careau et al. Disabil Rehabil,Early Online: 1–7
Disabil Rehabil Downloaded from informahealthcare.com by Karolinska Institutet University Library on 06/02/14
For personal use only.
ing, at one extreme, the least intense collaborative practice and, at
the other, the most intense. The ‘‘competencies’’ component was
left out of the framework because the diversity of the associated
concepts(e.g.communication,group dynamics,conflictreso-
lution)made itdifficultto illustrate them along a continuum.
Moreover,those particularconcepts could be betterillustrated
within an IPC competencies’ frameworks such as the Canadian
InterprofessionalHealthCollaborative(2010)[16]. Figure 2
presentsthe initial framework developed during phases1–6.
It includesfive components(e.g. ‘‘context’’,‘‘partnership’s
common objectives’’, ‘‘interaction between members’’, ‘‘integra-
tion of disciplinary knowledge’’,and ‘‘modalities’’)and their
associated concepts.The components are interlinked to define
four differenttypes of collaborative practices (illustrated by the
grey rectangles).For example,the mostintense collaborative
practice should be adopted when the client’sbiopsychosocial
needs are complex and demand a partnership to share decision-
making and adopt common intervention objectives. In this type of
practice,disciplinary knowledge needsto be more integrated
using an interdisciplinary approach.Differentmodalities can be
associatedwith this practice,but the interdisciplinaryteam
meeting is the mostoften used.Finally,the initialframework
incorporated the notion thatIPC can be considered as encom-
passing every activity of collaboration,including the least to the
mostintense practices,or can be associated with only the most
intense practice.
Framework formal validation
Twentypersonsparticipatedin one or anotherstep of the
validation process. Table 1 presents the experts’ and stakeholders’
profiles (current occupation and core training/discipline) for each
consensus group session and the survey.More than 82% of the
participantsconsidered they had good to excellentscientific
knowledge, and 76% good clinical experience, of IPC. More than
75% had completed post-graduate studies,and many ofthem
combined clinical and educational responsibilities in their curre
occupation.
From the outset,participantsappeared to agreewith the
framework’sgeneralpresentation.However,in the firstgroup
session, participants recommended adding a fifth type of pract
the independentpractice.They explained thateven when practi-
tionersdo notcollaborate atall with each other,partnerships
between clients and practitioners have to be established.In the
survey, when this independent practice was added to the four o
types of practices,100% of respondents agreed with the frame-
work’s generalpresentation.With regard to the components of
IPC, 12.5% of the surveyrespondentsdisagreedwith the
representation of the modalities.In the second consensus group
session,participants explained thatthe modalities differed from
one clinical setting to another, so it was too confusing to illustra
them as a component.The majority agreed thatthe modalities
componentwas notessentialto understand IPC;consensus was
established to remove it from the framework.
The main concern raised in the first two group sessions and i
the surveys had to do with the wording of certain components a
concepts.Almost30% of survey respondentsdisagreed with
the wording ofthe component‘‘objectivesaimed atby the
partnership’’and 6% disagreedwith the term ‘‘interaction
between members’’.Finally,the last group session led to a
consensus on terms that were deemed reflective of what happe
in clinical settingswhile being coherentwith the conceptual
knowledge aboutIPC (see the finalframework illustrated in
Figure 3).
Figure 2.Initial IPC framework.
4 E. Careau et al. Disabil Rehabil,Early Online: 1–7
Disabil Rehabil Downloaded from informahealthcare.com by Karolinska Institutet University Library on 06/02/14
For personal use only.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Anothermajorconcern was the theorization ofthe concept
‘‘interprofessionalcollaboration’’.In the survey,88.2% of
respondents said they were familiar with this term,butthey all
had differentdefinitionsof the concept.We observed in the
subsequentgroup sessions thatthe definitions used were clearly
influenced by the culture of the participant’s discipline and work
place. After discussing the different points of view and comparing
them to definitions found in the literature, participants agreed that
the common goal of practitioners getting involved in IPC was to
provide quality health and socialcare.To do this,practitioners
adopt different types of IPC, so that the intensity of the interaction
between clients,families and practitioners is adjusted depending
on the complexity of the situation.
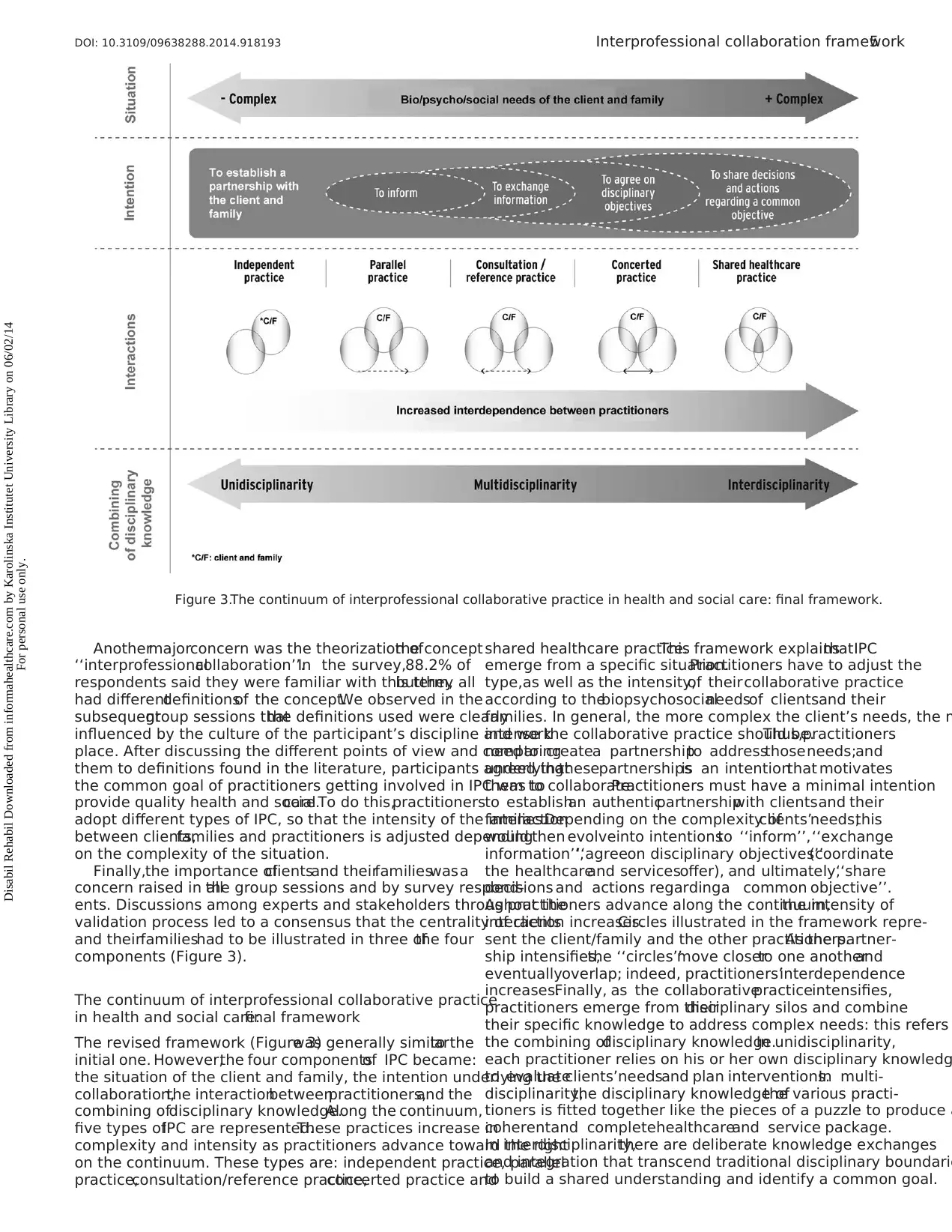
Finally,the importance ofclientsand theirfamilieswasa
concern raised in allthe group sessions and by survey respond-
ents. Discussions among experts and stakeholders throughout the
validation process led to a consensus that the centrality of clients
and theirfamilieshad to be illustrated in three ofthe four
components (Figure 3).
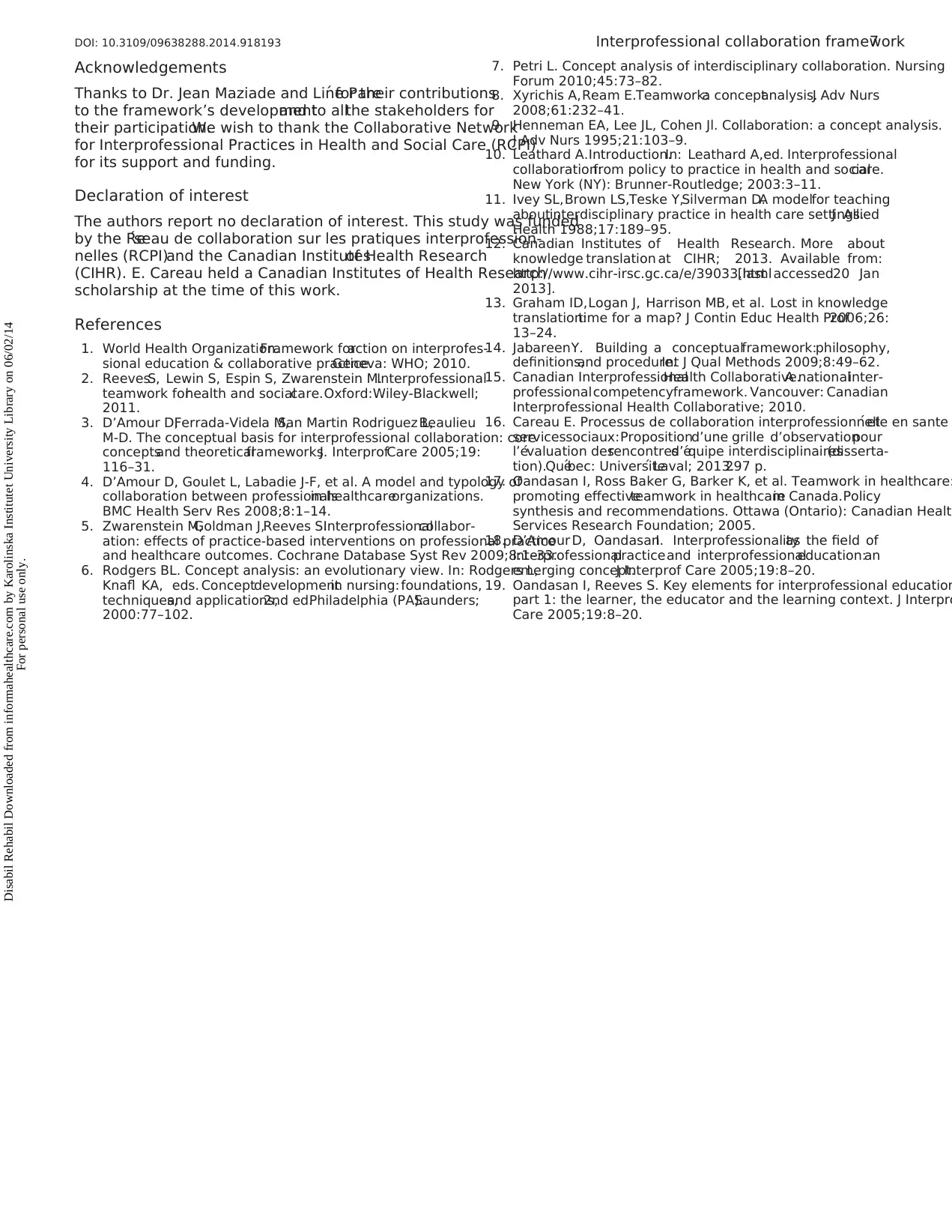
The continuum of interprofessional collaborative practice
in health and social care:final framework
The revised framework (Figure 3)was generally similarto the
initial one. However,the four componentsof IPC became:
the situation of the client and family, the intention underlying the
collaboration,the interactionbetweenpractitioners,and the
combining ofdisciplinary knowledge.Along the continuum,
five types ofIPC are represented.These practices increase in
complexity and intensity as practitioners advance toward the right
on the continuum. These types are: independent practice, parallel
practice,consultation/reference practice,concerted practice and
shared healthcare practice.This framework explainsthatIPC
emerge from a specific situation.Practitioners have to adjust the
type,as well as the intensity,of theircollaborative practice
according to thebiopsychosocialneedsof clientsand their
families. In general, the more complex the client’s needs, the m
intense the collaborative practice should be.Thus,practitioners
need to createa partnershipto addressthoseneeds;and
underlyingthesepartnershipsis an intentionthat motivates
them to collaborate.Practitioners must have a minimal intention
to establishan authenticpartnershipwith clientsand their
families.Depending on the complexity ofclients’needs,this
would then evolveinto intentionsto ‘‘inform’’,‘‘exchange
information’’,‘‘agreeon disciplinary objectives’’(coordinate
the healthcareand servicesoffer), and ultimately,‘‘share
decisions and actions regardinga common objective’’.
As practitioners advance along the continuum,the intensity of
interaction increases.Circles illustrated in the framework repre-
sent the client/family and the other practitioners.As the partner-
ship intensifies,the ‘‘circles’’move closerto one anotherand
eventuallyoverlap; indeed, practitioners’interdependence
increases.Finally, as the collaborativepracticeintensifies,
practitioners emerge from theirdisciplinary silos and combine
their specific knowledge to address complex needs: this refers
the combining ofdisciplinary knowledge.In unidisciplinarity,
each practitioner relies on his or her own disciplinary knowledg
to evaluateclients’needsand plan interventions.In multi-
disciplinarity,the disciplinary knowledge ofthe various practi-
tioners is fitted together like the pieces of a puzzle to produce a
coherentand completehealthcareand service package.
In interdisciplinarity,there are deliberate knowledge exchanges
and integration that transcend traditional disciplinary boundarie
to build a shared understanding and identify a common goal.
Figure 3.The continuum of interprofessional collaborative practice in health and social care: final framework.
DOI: 10.3109/09638288.2014.918193 Interprofessional collaboration framework5
Disabil Rehabil Downloaded from informahealthcare.com by Karolinska Institutet University Library on 06/02/14
For personal use only.
‘‘interprofessionalcollaboration’’.In the survey,88.2% of
respondents said they were familiar with this term,butthey all
had differentdefinitionsof the concept.We observed in the
subsequentgroup sessions thatthe definitions used were clearly
influenced by the culture of the participant’s discipline and work
place. After discussing the different points of view and comparing
them to definitions found in the literature, participants agreed that
the common goal of practitioners getting involved in IPC was to
provide quality health and socialcare.To do this,practitioners
adopt different types of IPC, so that the intensity of the interaction
between clients,families and practitioners is adjusted depending
on the complexity of the situation.
Finally,the importance ofclientsand theirfamilieswasa
concern raised in allthe group sessions and by survey respond-
ents. Discussions among experts and stakeholders throughout the
validation process led to a consensus that the centrality of clients
and theirfamilieshad to be illustrated in three ofthe four
components (Figure 3).
The continuum of interprofessional collaborative practice
in health and social care:final framework
The revised framework (Figure 3)was generally similarto the
initial one. However,the four componentsof IPC became:
the situation of the client and family, the intention underlying the
collaboration,the interactionbetweenpractitioners,and the
combining ofdisciplinary knowledge.Along the continuum,
five types ofIPC are represented.These practices increase in
complexity and intensity as practitioners advance toward the right
on the continuum. These types are: independent practice, parallel
practice,consultation/reference practice,concerted practice and
shared healthcare practice.This framework explainsthatIPC
emerge from a specific situation.Practitioners have to adjust the
type,as well as the intensity,of theircollaborative practice
according to thebiopsychosocialneedsof clientsand their
families. In general, the more complex the client’s needs, the m
intense the collaborative practice should be.Thus,practitioners
need to createa partnershipto addressthoseneeds;and
underlyingthesepartnershipsis an intentionthat motivates
them to collaborate.Practitioners must have a minimal intention
to establishan authenticpartnershipwith clientsand their
families.Depending on the complexity ofclients’needs,this
would then evolveinto intentionsto ‘‘inform’’,‘‘exchange
information’’,‘‘agreeon disciplinary objectives’’(coordinate
the healthcareand servicesoffer), and ultimately,‘‘share
decisions and actions regardinga common objective’’.
As practitioners advance along the continuum,the intensity of
interaction increases.Circles illustrated in the framework repre-
sent the client/family and the other practitioners.As the partner-
ship intensifies,the ‘‘circles’’move closerto one anotherand
eventuallyoverlap; indeed, practitioners’interdependence
increases.Finally, as the collaborativepracticeintensifies,
practitioners emerge from theirdisciplinary silos and combine
their specific knowledge to address complex needs: this refers
the combining ofdisciplinary knowledge.In unidisciplinarity,
each practitioner relies on his or her own disciplinary knowledg
to evaluateclients’needsand plan interventions.In multi-
disciplinarity,the disciplinary knowledge ofthe various practi-
tioners is fitted together like the pieces of a puzzle to produce a
coherentand completehealthcareand service package.
In interdisciplinarity,there are deliberate knowledge exchanges
and integration that transcend traditional disciplinary boundarie
to build a shared understanding and identify a common goal.
Figure 3.The continuum of interprofessional collaborative practice in health and social care: final framework.
DOI: 10.3109/09638288.2014.918193 Interprofessional collaboration framework5
Disabil Rehabil Downloaded from informahealthcare.com by Karolinska Institutet University Library on 06/02/14
For personal use only.
The Continuum ofInterprofessionalCollaborative Practice in
Health and Social Care illustrates non-hierarchical and non-linear
types of collaborative practices.For individuals engaged in IPC,
the challenge isto be able to move easily in both directions
along the continuum.They should be competentto adequately
evaluate the complexity of the situation in order to seek the right
intention forpartnership and adjustthe intensity of IPC so the
needs of clients and families can be effectively addressed.
Discussion
The Continuum ofInterprofessionalCollaborative Practice in
Health and SocialCare is a comprehensiveframework that
illustrates five types of collaborative practices according to four
descriptive components. It was developed and validated following
a seven-phaseprocedurethat includesliteraturereview and
consultation ofstakeholdersfrom the academicand clinical
settings.
One of the major innovationsof this frameworkis the
representation of the central position occupied by clients and their
families.In the framework,the primary and shared intention
behind every collaborative practice is to establish a partnership
with thesepersons.In the literature,all authorsagreethe
relationship with the person isimportant,but few affirm that
establishing this partnership should be the primary motivation to
collaborate.It is surprising that few researchers have conceptua-
lized clients and theirfamilies as true participants in IPC [3].
In our proposed framework,the primary role of clients and their
familiesis illustrated throughoutthe components.Indeed,the
purpose ofIPC is to address clients’needs (‘‘situation ofthe
client and family’’ component), and clients and their families are
considered truemembersof the team (‘‘interaction between
individuals’’ component).
The ‘‘intention underlying the collaboration’’componentis
also an important addition to the literature on IPC.In fact,most
authors agree the overall goal behind collaboration is to provide
quality health and socialcare to clients [2,17].Therefore,we
consider this overall goal is attained when IPC are appropriately
adjusted to the needs of clients and their families. The ‘‘intention
sought by collaboration’’ component in our framework allows us
to distinguish between the levels of partnership.D’Amour etal.
(2005) affirm that ‘‘it is unrealistic to think that simply bringing
practitionerstogetherin teamswill lead to collaboration’’
[3, p. 126].Practitionersneed to have a motivation to start
collaborating with each other.The ‘‘intention soughtby collab-
oration’’componentemphasizesthatIPC cannot be applied
following a recipe. In terms of collaboration, practitioners should
be able to adopta reflectivepracticeto adjusthow they
collaborate depending on the situation,the clienteleand the
clinical setting. In our opinion, the proposed framework highlights
this reality for the first time.
The framework also highlightsthe distinction between the
concepts of discipline, which refers to a body of knowledge, and
professional,which refers to a person with specific disciplinary
knowledge.Our frameworkreducesthe persistentconfusion
between these terms,while maintaining coherence with recent
published papers on the conceptualdefinition of IPC [2,18,19].
It emphasizes that the combining of disciplinary knowledge is not
the only component influencing IPC.
Finally,the validation processmade itpossible to adopta
consensual definition of the concept of IPC. As mentioned above,
although there is no consensualdefinition among the scientific
community,the term IPC is widely used by practitioners,
managers and decision-makers.The conceptualization proposed
in our framework iscoherentwith the concept’sattributes:a
cooperativeventurebasedon sharedpower and authority,
characterized by non-hierarchicalrelationships,establishmentof
a partnership,mutualgoalsand commitment[8]. It is also
consistentwith well-known IPC definitions thatpoints outthe
dynamic processwhose intensity isadjusted according to the
complexity of the client’s needs,and which is characterized by
interdependence,partnership,collegial relationships,shared
power,pursuitof common purpose,and person-centred practice
[17,18].
Relevance and usefulness of the framework
From the very firstgroup session,all stakeholders and experts
strongly believed in the relevance of developing a comprehens
IPC framework to enhance KT. Indeed, in the survey, 88% of the
respondents answered ‘‘highly relevant’’and 12% ‘‘quite rele-
vant’’.Respondentsalso believedthis frameworkwould be
‘‘very useful’’or ‘‘quite useful’’in variouscontextssuch as
(in order of usefulness) continuing education for health and soc
care practitioners,undergraduateIPE courses,research,and
continuing education for health and socialcare managers.This
framework provides managers and professionals with a clearer
conceptualization of IPC enabling them to better understand th
conceptof IPC and how the interactionalfactorsshould be
operationalized within different settings and with various client
It also highlights the importance of adopting a reflective practic
in order to suitably adjust the intensity of collaboration accordin
to the clients’ needs.Indeed,practitioners should notadoptthe
same functioning in every situation. They should be able to jud
if their interactionswith othersare optimalor not. This
framework could help them in their reasoning.Managers could
also use this frameworkto supportthe continuousquality
improvement process in their organization.
Limitations
It is importantto pointout thatthis initiative took place in a
French-Canadian context. Although the literature review includ
mostly papers published in English, the framework’s developme
and validation were conducted in French with French-speaking
individuals.Thus,it is possible that the meanings of some terms
from the literature were obscured ormodified in translation.
Moreover,the results reflect the perspectives of French-speaking
practitionerswithin thecontextof the Quebecrehabilitation
system. The framework was translated for this paper; it would b
importantto validatethe frameworkwith English-speaking
practitioners both in Quebec and in other geographic settings.
Conclusion
The Continuum ofInterprofessionalCollaborative Practice in
Health and Social Care integrates the current scientific knowled
and clinicalexperience regarding the conceptualization of IPC.
It is considered as a relevant and useful KT tool to enhance IPC
knowledge for various stakeholders,especially in the rehabilita-
tion field.This comprehensive and contextualized framework
could be used in undergraduateand continuingeducation
initiatives to help learners understand the multidimensionaland
dynamic nature of IPC.The framework could also be usefulto
supportpractitioners and managers in theirefforts to optimize
collaborativepracticewithin theirorganization.Even if this
framework was developed and validated within the rehabilitatio
field, it could probably be used to illustrate IPC interactional
factors that occur in other health and social care settings. Furth
research is nonetheless needed to validate the framework in ot
contexts.We also suggestbetter position this framework within
the otherconceptualmodels and frameworks thatexistin the
IPECP field.
6 E. Careau et al. Disabil Rehabil,Early Online: 1–7
Disabil Rehabil Downloaded from informahealthcare.com by Karolinska Institutet University Library on 06/02/14
For personal use only.
Health and Social Care illustrates non-hierarchical and non-linear
types of collaborative practices.For individuals engaged in IPC,
the challenge isto be able to move easily in both directions
along the continuum.They should be competentto adequately
evaluate the complexity of the situation in order to seek the right
intention forpartnership and adjustthe intensity of IPC so the
needs of clients and families can be effectively addressed.
Discussion
The Continuum ofInterprofessionalCollaborative Practice in
Health and SocialCare is a comprehensiveframework that
illustrates five types of collaborative practices according to four
descriptive components. It was developed and validated following
a seven-phaseprocedurethat includesliteraturereview and
consultation ofstakeholdersfrom the academicand clinical
settings.
One of the major innovationsof this frameworkis the
representation of the central position occupied by clients and their
families.In the framework,the primary and shared intention
behind every collaborative practice is to establish a partnership
with thesepersons.In the literature,all authorsagreethe
relationship with the person isimportant,but few affirm that
establishing this partnership should be the primary motivation to
collaborate.It is surprising that few researchers have conceptua-
lized clients and theirfamilies as true participants in IPC [3].
In our proposed framework,the primary role of clients and their
familiesis illustrated throughoutthe components.Indeed,the
purpose ofIPC is to address clients’needs (‘‘situation ofthe
client and family’’ component), and clients and their families are
considered truemembersof the team (‘‘interaction between
individuals’’ component).
The ‘‘intention underlying the collaboration’’componentis
also an important addition to the literature on IPC.In fact,most
authors agree the overall goal behind collaboration is to provide
quality health and socialcare to clients [2,17].Therefore,we
consider this overall goal is attained when IPC are appropriately
adjusted to the needs of clients and their families. The ‘‘intention
sought by collaboration’’ component in our framework allows us
to distinguish between the levels of partnership.D’Amour etal.
(2005) affirm that ‘‘it is unrealistic to think that simply bringing
practitionerstogetherin teamswill lead to collaboration’’
[3, p. 126].Practitionersneed to have a motivation to start
collaborating with each other.The ‘‘intention soughtby collab-
oration’’componentemphasizesthatIPC cannot be applied
following a recipe. In terms of collaboration, practitioners should
be able to adopta reflectivepracticeto adjusthow they
collaborate depending on the situation,the clienteleand the
clinical setting. In our opinion, the proposed framework highlights
this reality for the first time.
The framework also highlightsthe distinction between the
concepts of discipline, which refers to a body of knowledge, and
professional,which refers to a person with specific disciplinary
knowledge.Our frameworkreducesthe persistentconfusion
between these terms,while maintaining coherence with recent
published papers on the conceptualdefinition of IPC [2,18,19].
It emphasizes that the combining of disciplinary knowledge is not
the only component influencing IPC.
Finally,the validation processmade itpossible to adopta
consensual definition of the concept of IPC. As mentioned above,
although there is no consensualdefinition among the scientific
community,the term IPC is widely used by practitioners,
managers and decision-makers.The conceptualization proposed
in our framework iscoherentwith the concept’sattributes:a
cooperativeventurebasedon sharedpower and authority,
characterized by non-hierarchicalrelationships,establishmentof
a partnership,mutualgoalsand commitment[8]. It is also
consistentwith well-known IPC definitions thatpoints outthe
dynamic processwhose intensity isadjusted according to the
complexity of the client’s needs,and which is characterized by
interdependence,partnership,collegial relationships,shared
power,pursuitof common purpose,and person-centred practice
[17,18].
Relevance and usefulness of the framework
From the very firstgroup session,all stakeholders and experts
strongly believed in the relevance of developing a comprehens
IPC framework to enhance KT. Indeed, in the survey, 88% of the
respondents answered ‘‘highly relevant’’and 12% ‘‘quite rele-
vant’’.Respondentsalso believedthis frameworkwould be
‘‘very useful’’or ‘‘quite useful’’in variouscontextssuch as
(in order of usefulness) continuing education for health and soc
care practitioners,undergraduateIPE courses,research,and
continuing education for health and socialcare managers.This
framework provides managers and professionals with a clearer
conceptualization of IPC enabling them to better understand th
conceptof IPC and how the interactionalfactorsshould be
operationalized within different settings and with various client
It also highlights the importance of adopting a reflective practic
in order to suitably adjust the intensity of collaboration accordin
to the clients’ needs.Indeed,practitioners should notadoptthe
same functioning in every situation. They should be able to jud
if their interactionswith othersare optimalor not. This
framework could help them in their reasoning.Managers could
also use this frameworkto supportthe continuousquality
improvement process in their organization.
Limitations
It is importantto pointout thatthis initiative took place in a
French-Canadian context. Although the literature review includ
mostly papers published in English, the framework’s developme
and validation were conducted in French with French-speaking
individuals.Thus,it is possible that the meanings of some terms
from the literature were obscured ormodified in translation.
Moreover,the results reflect the perspectives of French-speaking
practitionerswithin thecontextof the Quebecrehabilitation
system. The framework was translated for this paper; it would b
importantto validatethe frameworkwith English-speaking
practitioners both in Quebec and in other geographic settings.
Conclusion
The Continuum ofInterprofessionalCollaborative Practice in
Health and Social Care integrates the current scientific knowled
and clinicalexperience regarding the conceptualization of IPC.
It is considered as a relevant and useful KT tool to enhance IPC
knowledge for various stakeholders,especially in the rehabilita-
tion field.This comprehensive and contextualized framework
could be used in undergraduateand continuingeducation
initiatives to help learners understand the multidimensionaland
dynamic nature of IPC.The framework could also be usefulto
supportpractitioners and managers in theirefforts to optimize
collaborativepracticewithin theirorganization.Even if this
framework was developed and validated within the rehabilitatio
field, it could probably be used to illustrate IPC interactional
factors that occur in other health and social care settings. Furth
research is nonetheless needed to validate the framework in ot
contexts.We also suggestbetter position this framework within
the otherconceptualmodels and frameworks thatexistin the
IPECP field.
6 E. Careau et al. Disabil Rehabil,Early Online: 1–7
Disabil Rehabil Downloaded from informahealthcare.com by Karolinska Institutet University Library on 06/02/14
For personal use only.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Acknowledgements
Thanks to Dr. Jean Maziade and Line Pare´ for their contributions
to the framework’s developmentand to allthe stakeholders for
their participation.We wish to thank the Collaborative Network
for Interprofessional Practices in Health and Social Care (RCPI)
for its support and funding.
Declaration of interest
The authors report no declaration of interest. This study was funded
by the Re´seau de collaboration sur les pratiques interprofession-
nelles (RCPI)and the Canadian Institutesof Health Research
(CIHR). E. Careau held a Canadian Institutes of Health Research
scholarship at the time of this work.
References
1. World Health Organization.Framework foraction on interprofes-
sional education & collaborative practice.Geneva: WHO; 2010.
2. ReevesS, Lewin S, Espin S, Zwarenstein M.Interprofessional
teamwork forhealth and socialcare.Oxford:Wiley-Blackwell;
2011.
3. D’Amour D,Ferrada-Videla M,San Martin Rodriguez L,Beaulieu
M-D. The conceptual basis for interprofessional collaboration: core
conceptsand theoreticalframeworks.J InterprofCare 2005;19:
116–31.
4. D’Amour D, Goulet L, Labadie J-F, et al. A model and typology of
collaboration between professionalsin healthcareorganizations.
BMC Health Serv Res 2008;8:1–14.
5. Zwarenstein M,Goldman J,Reeves S.Interprofessionalcollabor-
ation: effects of practice-based interventions on professional practice
and healthcare outcomes. Cochrane Database Syst Rev 2009;8:1–33.
6. Rodgers BL. Concept analysis: an evolutionary view. In: Rodgers L,
Knafl KA, eds. Conceptdevelopmentin nursing: foundations,
techniques,and applications,2nd ed.Philadelphia (PA):Saunders;
2000:77–102.
7. Petri L. Concept analysis of interdisciplinary collaboration. Nursing
Forum 2010;45:73–82.
8. Xyrichis A,Ream E.Teamwork:a conceptanalysis.J Adv Nurs
2008;61:232–41.
9. Henneman EA, Lee JL, Cohen Jl. Collaboration: a concept analysis.
J Adv Nurs 1995;21:103–9.
10. Leathard A.Introduction.In: Leathard A,ed. Interprofessional
collaboration:from policy to practice in health and socialcare.
New York (NY): Brunner-Routledge; 2003:3–11.
11. Ivey SL,Brown LS,Teske Y,Silverman D.A modelfor teaching
aboutinterdisciplinary practice in health care settings.J Allied
Health 1988;17:189–95.
12. Canadian Institutes of Health Research. More about
knowledge translation at CIHR; 2013. Available from:
http://www.cihr-irsc.gc.ca/e/39033.html[last accessed20 Jan
2013].
13. Graham ID,Logan J, Harrison MB, et al. Lost in knowledge
translation:time for a map? J Contin Educ Health Prof2006;26:
13–24.
14. JabareenY. Building a conceptualframework:philosophy,
definitions,and procedure.Int J Qual Methods 2009;8:49–62.
15. Canadian InterprofessionalHealth Collaborative.A nationalinter-
professionalcompetencyframework. Vancouver: Canadian
Interprofessional Health Collaborative; 2010.
16. Careau E. Processus de collaboration interprofessionnelle en sante´ et
servicessociaux:Propositiond’une grille d’observationpour
l’e´valuation desrencontresd’e´quipe interdisciplinaires(disserta-
tion).Que´bec: Universite´ Laval; 2013.297 p.
17. Oandasan I, Ross Baker G, Barker K, et al. Teamwork in healthcare:
promoting effectiveteamwork in healthcarein Canada.Policy
synthesis and recommendations. Ottawa (Ontario): Canadian Healt
Services Research Foundation; 2005.
18. D’Amour D, OandasanI. Interprofessionalityas the field of
interprofessionalpracticeand interprofessionaleducation:an
emerging concept.J Interprof Care 2005;19:8–20.
19. Oandasan I, Reeves S. Key elements for interprofessional education
part 1: the learner, the educator and the learning context. J Interpro
Care 2005;19:8–20.
DOI: 10.3109/09638288.2014.918193 Interprofessional collaboration framework7
Disabil Rehabil Downloaded from informahealthcare.com by Karolinska Institutet University Library on 06/02/14
For personal use only.
Thanks to Dr. Jean Maziade and Line Pare´ for their contributions
to the framework’s developmentand to allthe stakeholders for
their participation.We wish to thank the Collaborative Network
for Interprofessional Practices in Health and Social Care (RCPI)
for its support and funding.
Declaration of interest
The authors report no declaration of interest. This study was funded
by the Re´seau de collaboration sur les pratiques interprofession-
nelles (RCPI)and the Canadian Institutesof Health Research
(CIHR). E. Careau held a Canadian Institutes of Health Research
scholarship at the time of this work.
References
1. World Health Organization.Framework foraction on interprofes-
sional education & collaborative practice.Geneva: WHO; 2010.
2. ReevesS, Lewin S, Espin S, Zwarenstein M.Interprofessional
teamwork forhealth and socialcare.Oxford:Wiley-Blackwell;
2011.
3. D’Amour D,Ferrada-Videla M,San Martin Rodriguez L,Beaulieu
M-D. The conceptual basis for interprofessional collaboration: core
conceptsand theoreticalframeworks.J InterprofCare 2005;19:
116–31.
4. D’Amour D, Goulet L, Labadie J-F, et al. A model and typology of
collaboration between professionalsin healthcareorganizations.
BMC Health Serv Res 2008;8:1–14.
5. Zwarenstein M,Goldman J,Reeves S.Interprofessionalcollabor-
ation: effects of practice-based interventions on professional practice
and healthcare outcomes. Cochrane Database Syst Rev 2009;8:1–33.
6. Rodgers BL. Concept analysis: an evolutionary view. In: Rodgers L,
Knafl KA, eds. Conceptdevelopmentin nursing: foundations,
techniques,and applications,2nd ed.Philadelphia (PA):Saunders;
2000:77–102.
7. Petri L. Concept analysis of interdisciplinary collaboration. Nursing
Forum 2010;45:73–82.
8. Xyrichis A,Ream E.Teamwork:a conceptanalysis.J Adv Nurs
2008;61:232–41.
9. Henneman EA, Lee JL, Cohen Jl. Collaboration: a concept analysis.
J Adv Nurs 1995;21:103–9.
10. Leathard A.Introduction.In: Leathard A,ed. Interprofessional
collaboration:from policy to practice in health and socialcare.
New York (NY): Brunner-Routledge; 2003:3–11.
11. Ivey SL,Brown LS,Teske Y,Silverman D.A modelfor teaching
aboutinterdisciplinary practice in health care settings.J Allied
Health 1988;17:189–95.
12. Canadian Institutes of Health Research. More about
knowledge translation at CIHR; 2013. Available from:
http://www.cihr-irsc.gc.ca/e/39033.html[last accessed20 Jan
2013].
13. Graham ID,Logan J, Harrison MB, et al. Lost in knowledge
translation:time for a map? J Contin Educ Health Prof2006;26:
13–24.
14. JabareenY. Building a conceptualframework:philosophy,
definitions,and procedure.Int J Qual Methods 2009;8:49–62.
15. Canadian InterprofessionalHealth Collaborative.A nationalinter-
professionalcompetencyframework. Vancouver: Canadian
Interprofessional Health Collaborative; 2010.
16. Careau E. Processus de collaboration interprofessionnelle en sante´ et
servicessociaux:Propositiond’une grille d’observationpour
l’e´valuation desrencontresd’e´quipe interdisciplinaires(disserta-
tion).Que´bec: Universite´ Laval; 2013.297 p.
17. Oandasan I, Ross Baker G, Barker K, et al. Teamwork in healthcare:
promoting effectiveteamwork in healthcarein Canada.Policy
synthesis and recommendations. Ottawa (Ontario): Canadian Healt
Services Research Foundation; 2005.
18. D’Amour D, OandasanI. Interprofessionalityas the field of
interprofessionalpracticeand interprofessionaleducation:an
emerging concept.J Interprof Care 2005;19:8–20.
19. Oandasan I, Reeves S. Key elements for interprofessional education
part 1: the learner, the educator and the learning context. J Interpro
Care 2005;19:8–20.
DOI: 10.3109/09638288.2014.918193 Interprofessional collaboration framework7
Disabil Rehabil Downloaded from informahealthcare.com by Karolinska Institutet University Library on 06/02/14
For personal use only.
1 out of 7
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.