A Case Study on Diagnosis and Treatment of Intestinal Lymphoma
VerifiedAdded on 2023/06/05
|11
|2088
|273
Case Study
AI Summary
This case study presents a rare instance of intestinal lymphoma in a 21-year-old male with a history of gastrointestinal issues. The patient presented with ileac lesions and blood in the stool, exacerbated by alcohol and seafood consumption. Diagnosed after multiple examinations including gastroscopy, colonoscopy, and enteroscopy, the patient underwent several surgeries to address ileac ulcers and intestinal haemorrhage. The case highlights the challenges in diagnosing and treating this uncommon form of non-Hodgkin lymphoma, emphasizing the importance of early detection and comprehensive medical intervention. Ultimately, the patient recovered and was discharged with recommendations for rest, nutrition, and post-operative care. Desklib provides students access to similar case studies and solved assignments.

Running Head: INTESTINAL LYMPHOMA
Intestinal Lymphoma
Name
Institutional Affiliation
Course Title
Instructor’s Name
Date
Intestinal Lymphoma
Name
Institutional Affiliation
Course Title
Instructor’s Name
Date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2
INTESTINAL LYMPHOMA
Abstract
According to Ferreri, Zinzani, Govi, & Pileri, (2011) gastrointestinal tract lymphomas are
very rare menacing disordesr that accounts for only 1-5% of the total gastrointestinal tract
malignancies. The most common type is lymphoma of B –cell origin but, there are rare cases
of the peripheral T- cell lymphomas of the ileum that has been reported so far (Carrasco et
al., 2015). Gastrointestinal lymphoma is the most prevalent to attack from non- Hodgkin’s
lymphoma. Colon and rectum are not commonly involved when compared with stomach and
very small bowel (Hoshikawa, Takagi, Koike, Maeda, & Tadokoro, 2004).
Introduction
The digestive track lymphoma of the bowel is not common as compared with
adenocarcinoma, signet ring lymphoma is very rare variant of non- Hodgkin’s lymphoma
(Elli, Contiero, Tagliabue, Tomba, & Bardella, 2012)). The disease is characterised by the
occurrence of the presence of clear cytoplasm that instead they replace the nucleus to the cell
periphery thus, giving the cell an appearance of signet ring. Primary intestinal lymphoma is
not very common and comprises of 0.2% -0.65% of the all known colic malignancies (Kiupel
et al., 2011).
Basir, Bickle, Telisinghe, Abdullah & Chong, ((2012) explains most of these tumours
are composed of b-cells, but study has also shown that t- cell lymphoma of the small intestine
is secondary to a celiac condition. Intestinal lymphomas are divided into various entropathy,
T-cell lymphoma (EATCL), EATCL lymphoma that don’t have enteropathy and the non-
EATCL (Vaidy et al., 2013).
EATCL manifests itself as multifocal with circumferential ulcers that is located near
the jejunum. This type of lymphoma is always associated with history celiac disease and
INTESTINAL LYMPHOMA
Abstract
According to Ferreri, Zinzani, Govi, & Pileri, (2011) gastrointestinal tract lymphomas are
very rare menacing disordesr that accounts for only 1-5% of the total gastrointestinal tract
malignancies. The most common type is lymphoma of B –cell origin but, there are rare cases
of the peripheral T- cell lymphomas of the ileum that has been reported so far (Carrasco et
al., 2015). Gastrointestinal lymphoma is the most prevalent to attack from non- Hodgkin’s
lymphoma. Colon and rectum are not commonly involved when compared with stomach and
very small bowel (Hoshikawa, Takagi, Koike, Maeda, & Tadokoro, 2004).
Introduction
The digestive track lymphoma of the bowel is not common as compared with
adenocarcinoma, signet ring lymphoma is very rare variant of non- Hodgkin’s lymphoma
(Elli, Contiero, Tagliabue, Tomba, & Bardella, 2012)). The disease is characterised by the
occurrence of the presence of clear cytoplasm that instead they replace the nucleus to the cell
periphery thus, giving the cell an appearance of signet ring. Primary intestinal lymphoma is
not very common and comprises of 0.2% -0.65% of the all known colic malignancies (Kiupel
et al., 2011).
Basir, Bickle, Telisinghe, Abdullah & Chong, ((2012) explains most of these tumours
are composed of b-cells, but study has also shown that t- cell lymphoma of the small intestine
is secondary to a celiac condition. Intestinal lymphomas are divided into various entropathy,
T-cell lymphoma (EATCL), EATCL lymphoma that don’t have enteropathy and the non-
EATCL (Vaidy et al., 2013).
EATCL manifests itself as multifocal with circumferential ulcers that is located near
the jejunum. This type of lymphoma is always associated with history celiac disease and
3
INTESTINAL LYMPHOMA
shows tumours cells that are CD4-, CD5-, and CD7+,CD8-/+,CD3+and CD103+7. It has also
been confirmed that all ATLL that is associated with retrovirus has not been documented
(Gou, Zang, Jiang, Yang, Cao & Chen, 2012).
Case study
A 21yearold male was presented having ileac lesions for more than 9 months and
currently found blood in stool after drinking alcohol and eating sea food for about 1800g, and
had transient black sputum for several seconds no syncope and loss of consciousness. For the
past the family said that he had a history of blood in the stool at age of one year which
improved after no special treatment. The symptoms were detected after taking alcohol and
eating sea food.
Physical examination revealed that the young man is clear minded and self-subjected.
The general conditions were not high temperature (36.1o), stable blood pressure (140/90
mmHg), weight 73kg, height 170 cm and acceptable sleep. He had no distortion of the thorax,
no tenderness in the sternum, the heart rhythm regular with heart beats being 101 beats /min.
he had no significant change in the body weight, normal bowel movement, no touch under
the liver and spleen, murphy’s sign(-).
INTESTINAL LYMPHOMA
shows tumours cells that are CD4-, CD5-, and CD7+,CD8-/+,CD3+and CD103+7. It has also
been confirmed that all ATLL that is associated with retrovirus has not been documented
(Gou, Zang, Jiang, Yang, Cao & Chen, 2012).
Case study
A 21yearold male was presented having ileac lesions for more than 9 months and
currently found blood in stool after drinking alcohol and eating sea food for about 1800g, and
had transient black sputum for several seconds no syncope and loss of consciousness. For the
past the family said that he had a history of blood in the stool at age of one year which
improved after no special treatment. The symptoms were detected after taking alcohol and
eating sea food.
Physical examination revealed that the young man is clear minded and self-subjected.
The general conditions were not high temperature (36.1o), stable blood pressure (140/90
mmHg), weight 73kg, height 170 cm and acceptable sleep. He had no distortion of the thorax,
no tenderness in the sternum, the heart rhythm regular with heart beats being 101 beats /min.
he had no significant change in the body weight, normal bowel movement, no touch under
the liver and spleen, murphy’s sign(-).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
4
INTESTINAL LYMPHOMA
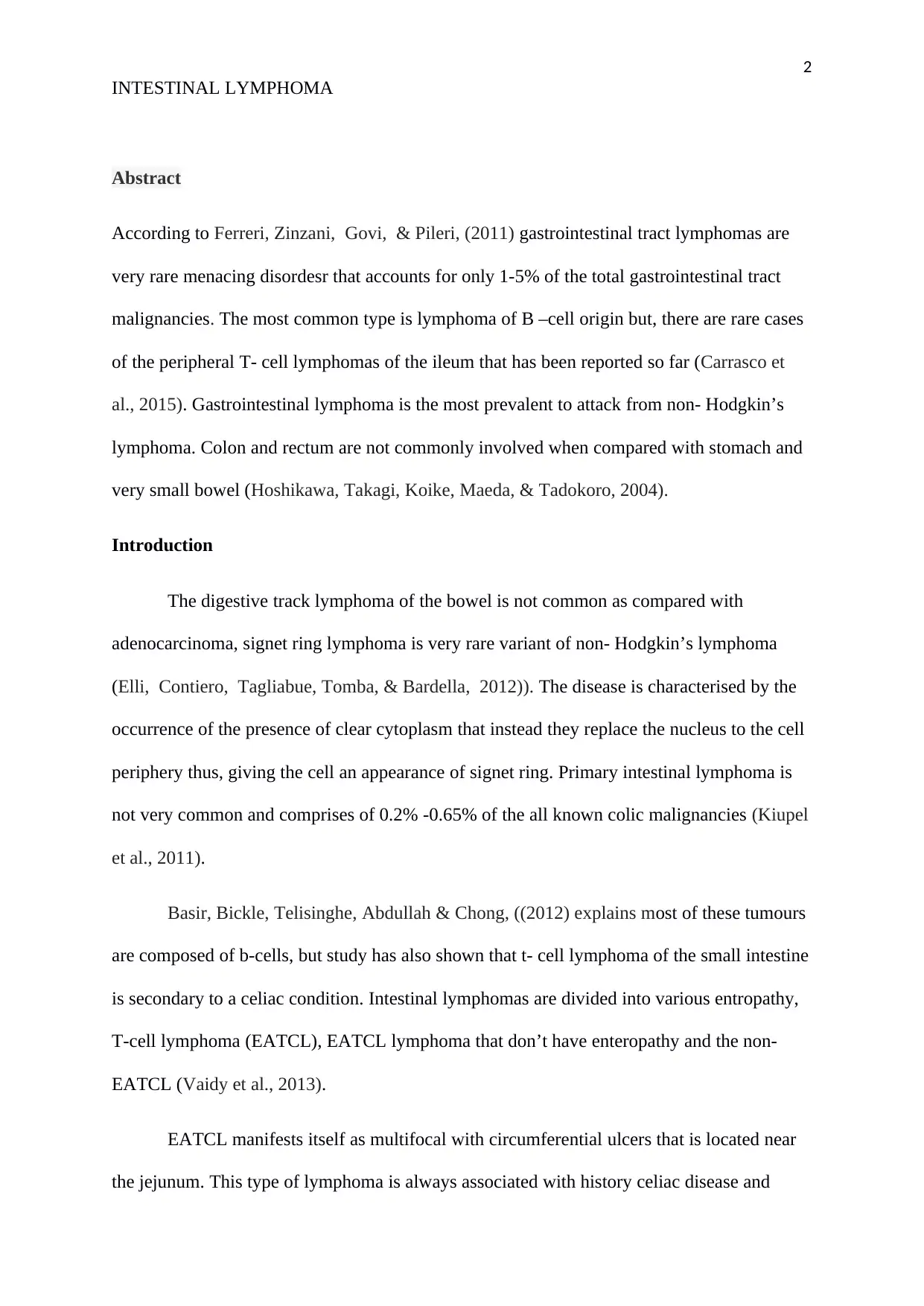
Figure 1 Auxiliary examination 2017-4-17 gastroscopy showing: chronic non-collapse
gastritis, pathological results showed: (gastric biopsy) mucosal chronic active inflammation
with erosion. (Shandong Provincial Hospital) 2017-5-25 colonoscopy).
The bowel sounds were normal and had no lower extremity edema, gastroscopy was
carried out and showed chronic non –atrophic gastritis, and pathological showed that mucosal
chronic active inflammation with erosion (gastric biopsy) from Shandong provincial hospital.
Auxiliary examination showed no significant abnormalities in the colorectal and capsule
endoscopy showed there was no obvious ulcer occupying and there was active bleeding in the
lower part of small intestine from Qianfoshan hospital.
INTESTINAL LYMPHOMA
Figure 1 Auxiliary examination 2017-4-17 gastroscopy showing: chronic non-collapse
gastritis, pathological results showed: (gastric biopsy) mucosal chronic active inflammation
with erosion. (Shandong Provincial Hospital) 2017-5-25 colonoscopy).
The bowel sounds were normal and had no lower extremity edema, gastroscopy was
carried out and showed chronic non –atrophic gastritis, and pathological showed that mucosal
chronic active inflammation with erosion (gastric biopsy) from Shandong provincial hospital.
Auxiliary examination showed no significant abnormalities in the colorectal and capsule
endoscopy showed there was no obvious ulcer occupying and there was active bleeding in the
lower part of small intestine from Qianfoshan hospital.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
5
INTESTINAL LYMPHOMA
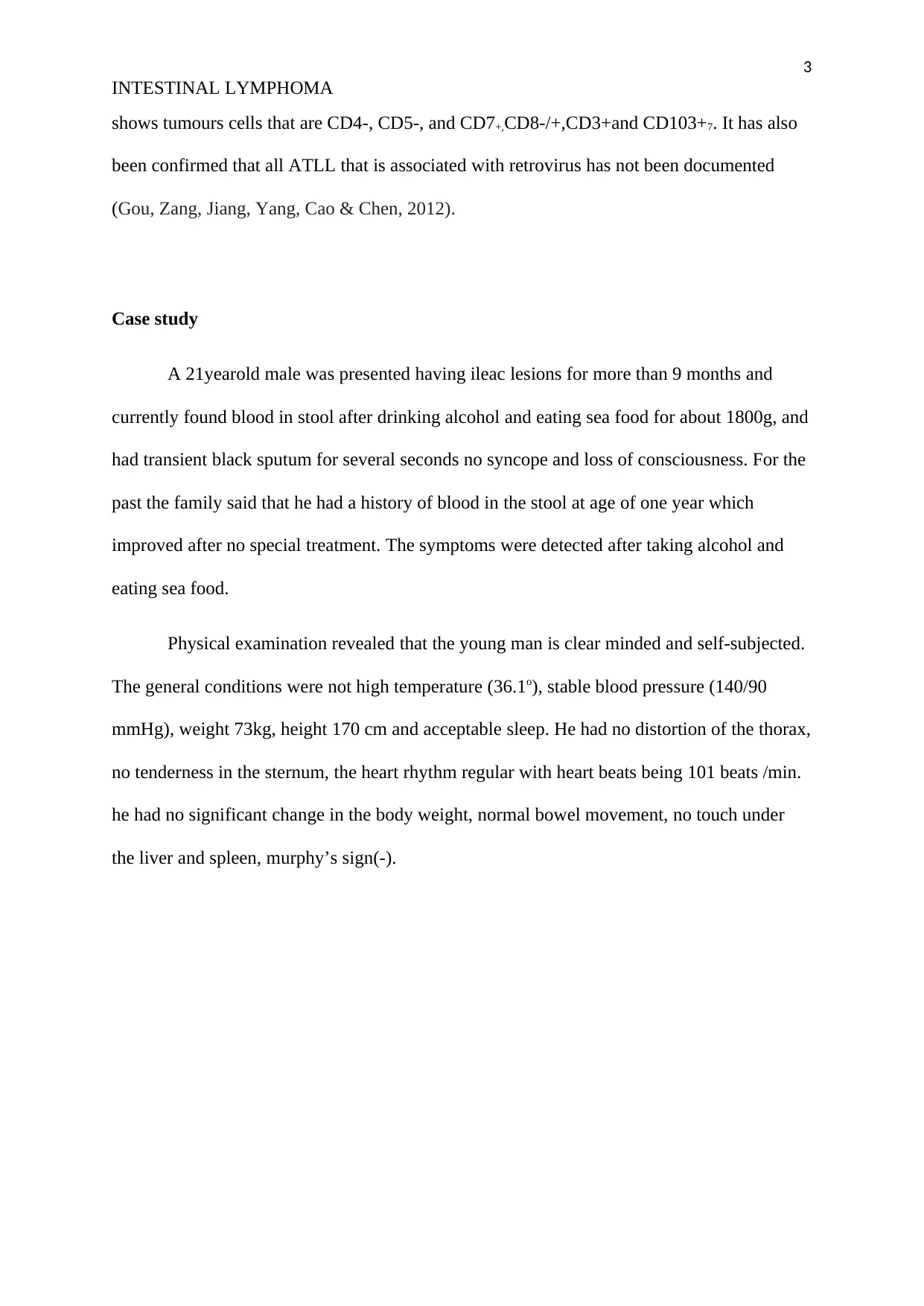
Figure2
Laparoscopic small intestine Mecke 1 diverticulum resection located on the walls of the
small intestine.
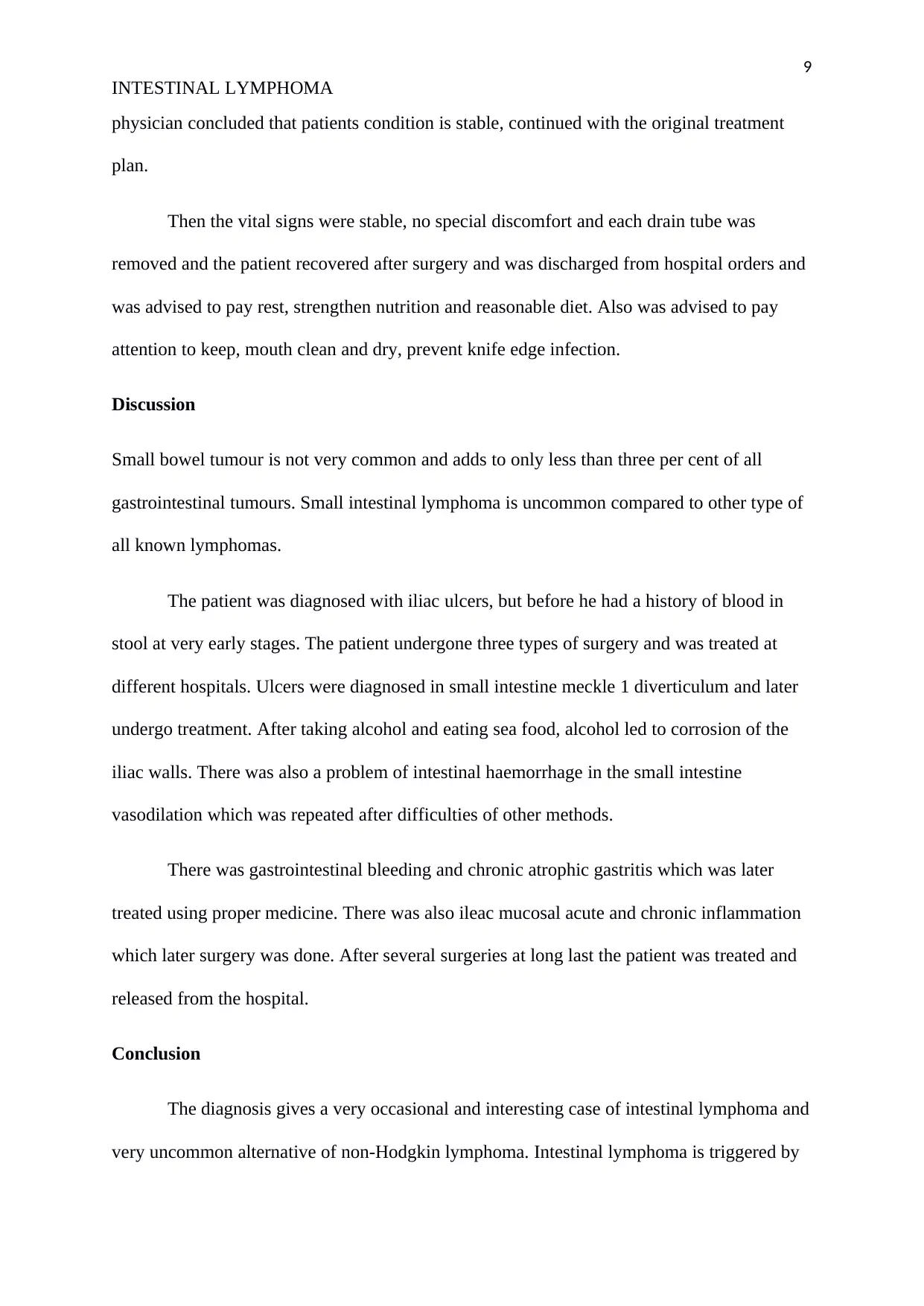
Intestonaloscopy showed that ileum was 70 cm away from ileocecal valve and the
spherical mucosal bulge. The surface was congested and edema and mucosal erosion was
visible. Pathological results showed ileac mucosal acute and chronic inflammation,
Eosinophils and small number glandular dysplasia from Shandong University Qilu Hospital.
Initial diagnoses were lower gastrointestinal bleeding, ileum lesions and chronic non
atrophic gastritis and treatment: admission to the hospital to improve relevant examination,
exclusion of contraindications after enteroscopy, under the microscope under intravenous
anaesthesia. Intestinal haemorrhage was classified as unexplained gastrointestinal bleeding,
INTESTINAL LYMPHOMA
Figure2
Laparoscopic small intestine Mecke 1 diverticulum resection located on the walls of the
small intestine.
Intestonaloscopy showed that ileum was 70 cm away from ileocecal valve and the
spherical mucosal bulge. The surface was congested and edema and mucosal erosion was
visible. Pathological results showed ileac mucosal acute and chronic inflammation,
Eosinophils and small number glandular dysplasia from Shandong University Qilu Hospital.
Initial diagnoses were lower gastrointestinal bleeding, ileum lesions and chronic non
atrophic gastritis and treatment: admission to the hospital to improve relevant examination,
exclusion of contraindications after enteroscopy, under the microscope under intravenous
anaesthesia. Intestinal haemorrhage was classified as unexplained gastrointestinal bleeding,
6
INTESTINAL LYMPHOMA
dominant or occult gastrointestinal bleeding if the upper digestive tract and lower digestive
tract endoscopy was normal.
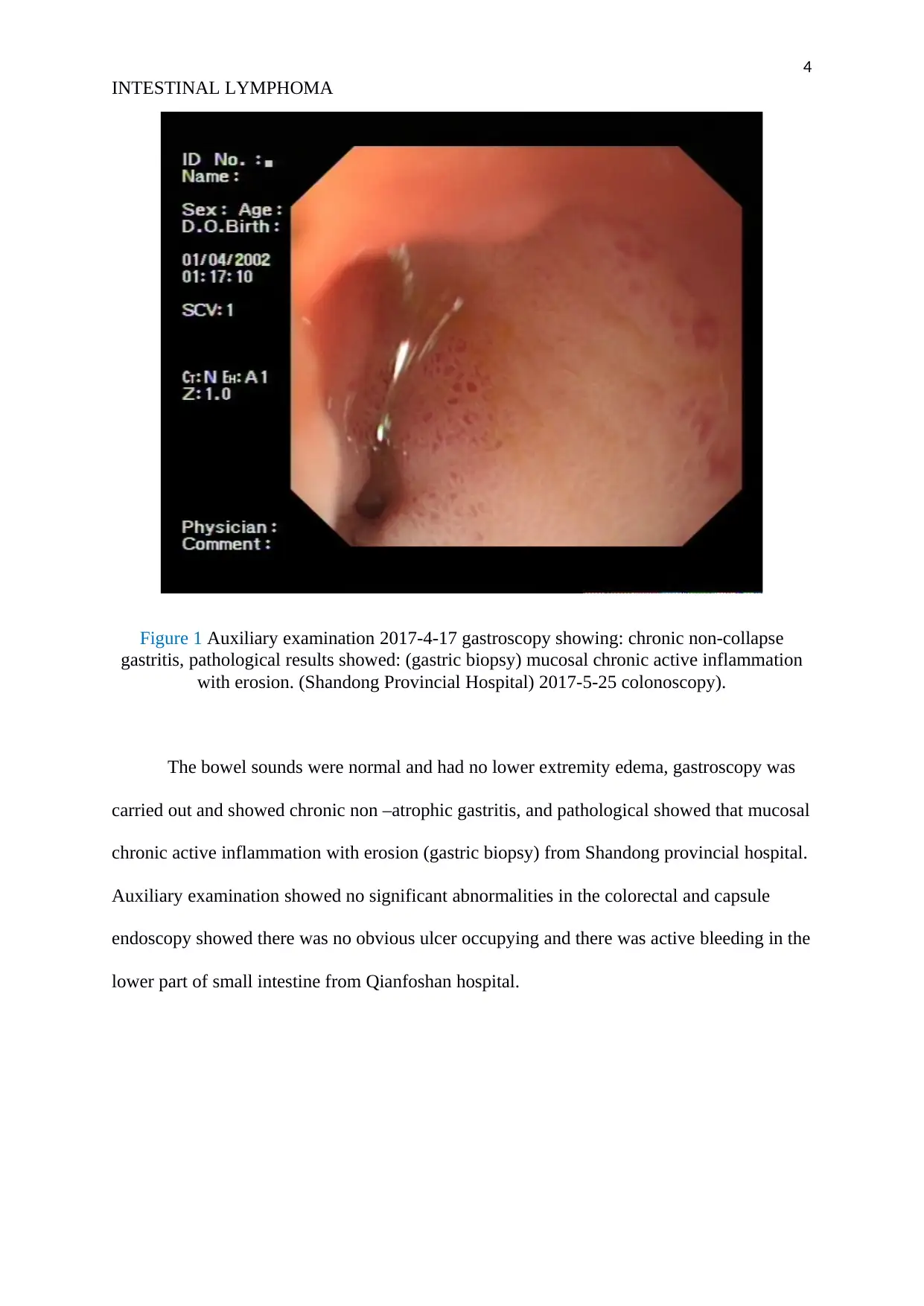
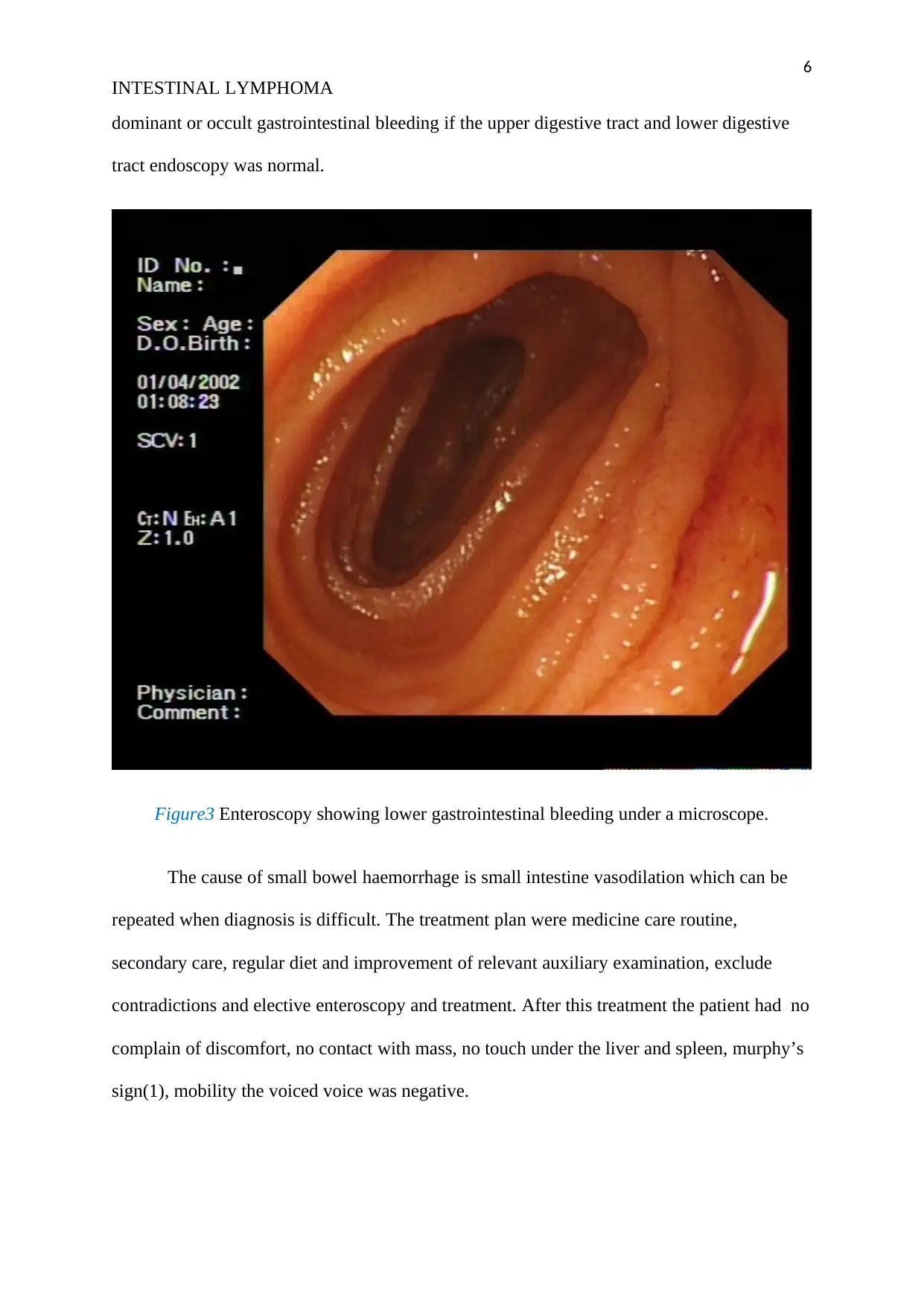
Figure3 Enteroscopy showing lower gastrointestinal bleeding under a microscope.
The cause of small bowel haemorrhage is small intestine vasodilation which can be
repeated when diagnosis is difficult. The treatment plan were medicine care routine,
secondary care, regular diet and improvement of relevant auxiliary examination, exclude
contradictions and elective enteroscopy and treatment. After this treatment the patient had no
complain of discomfort, no contact with mass, no touch under the liver and spleen, murphy’s
sign(1), mobility the voiced voice was negative.
INTESTINAL LYMPHOMA
dominant or occult gastrointestinal bleeding if the upper digestive tract and lower digestive
tract endoscopy was normal.
Figure3 Enteroscopy showing lower gastrointestinal bleeding under a microscope.
The cause of small bowel haemorrhage is small intestine vasodilation which can be
repeated when diagnosis is difficult. The treatment plan were medicine care routine,
secondary care, regular diet and improvement of relevant auxiliary examination, exclude
contradictions and elective enteroscopy and treatment. After this treatment the patient had no
complain of discomfort, no contact with mass, no touch under the liver and spleen, murphy’s
sign(1), mobility the voiced voice was negative.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
7
INTESTINAL LYMPHOMA
Microscopic diagnosis showed small intestine meckle 1 diverticulum and ulcers and
was to undergo surgery. Preoperative diagnosis showed small intestine meckle 1 diverticulum
and ulcers and chronic non atrophic gastritis and the treatment plan was surgical approach
and laparoscopic small bowel disease resection anaesthesia was carried out: laparoscopic
small bowel disease in the case of lesion resection.
The degree of mouth opening and cervical vertebra activity were normal, and the
ASA grade was graded without obvious anaesthesia contraindications. The anaesthesia
method: static inhalation combined with general anaesthesia. After anaesthesia was carried
out the patients data was checked, Sp02, NBP, ECG was monitored. Oral injection was
induced into laryngeal mask, controlled ventilation (IPPV), and inhalation combined surgery.
Surgery was carried out and Jiawei returned to the ward and ECG monitoring showed
that vital signs were stable. Rehydration and analgesia were given and other treatments.one
day after the surgery the vital signs were stable, no fever, self-reported knife pain, the bowel
sounds were not detected and the peristalsis did not recover. The drainage tubes were
smoothly circulated and nature of the drainage fluid and drainage volume was not
significantly abnormal. The knife dressing was clean and dry without oozing and seepage.
INTESTINAL LYMPHOMA
Microscopic diagnosis showed small intestine meckle 1 diverticulum and ulcers and
was to undergo surgery. Preoperative diagnosis showed small intestine meckle 1 diverticulum
and ulcers and chronic non atrophic gastritis and the treatment plan was surgical approach
and laparoscopic small bowel disease resection anaesthesia was carried out: laparoscopic
small bowel disease in the case of lesion resection.
The degree of mouth opening and cervical vertebra activity were normal, and the
ASA grade was graded without obvious anaesthesia contraindications. The anaesthesia
method: static inhalation combined with general anaesthesia. After anaesthesia was carried
out the patients data was checked, Sp02, NBP, ECG was monitored. Oral injection was
induced into laryngeal mask, controlled ventilation (IPPV), and inhalation combined surgery.
Surgery was carried out and Jiawei returned to the ward and ECG monitoring showed
that vital signs were stable. Rehydration and analgesia were given and other treatments.one
day after the surgery the vital signs were stable, no fever, self-reported knife pain, the bowel
sounds were not detected and the peristalsis did not recover. The drainage tubes were
smoothly circulated and nature of the drainage fluid and drainage volume was not
significantly abnormal. The knife dressing was clean and dry without oozing and seepage.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
8
INTESTINAL LYMPHOMA
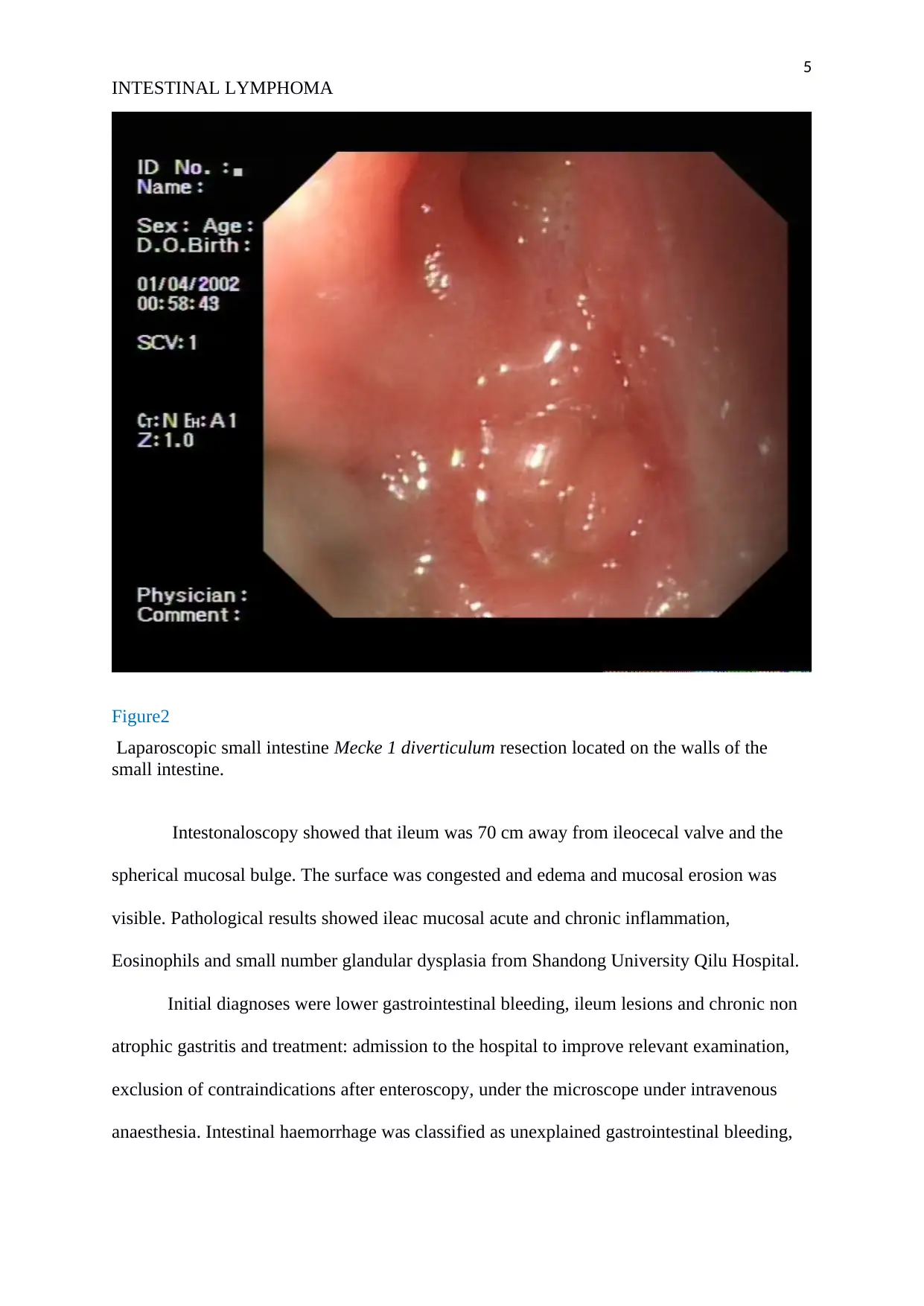
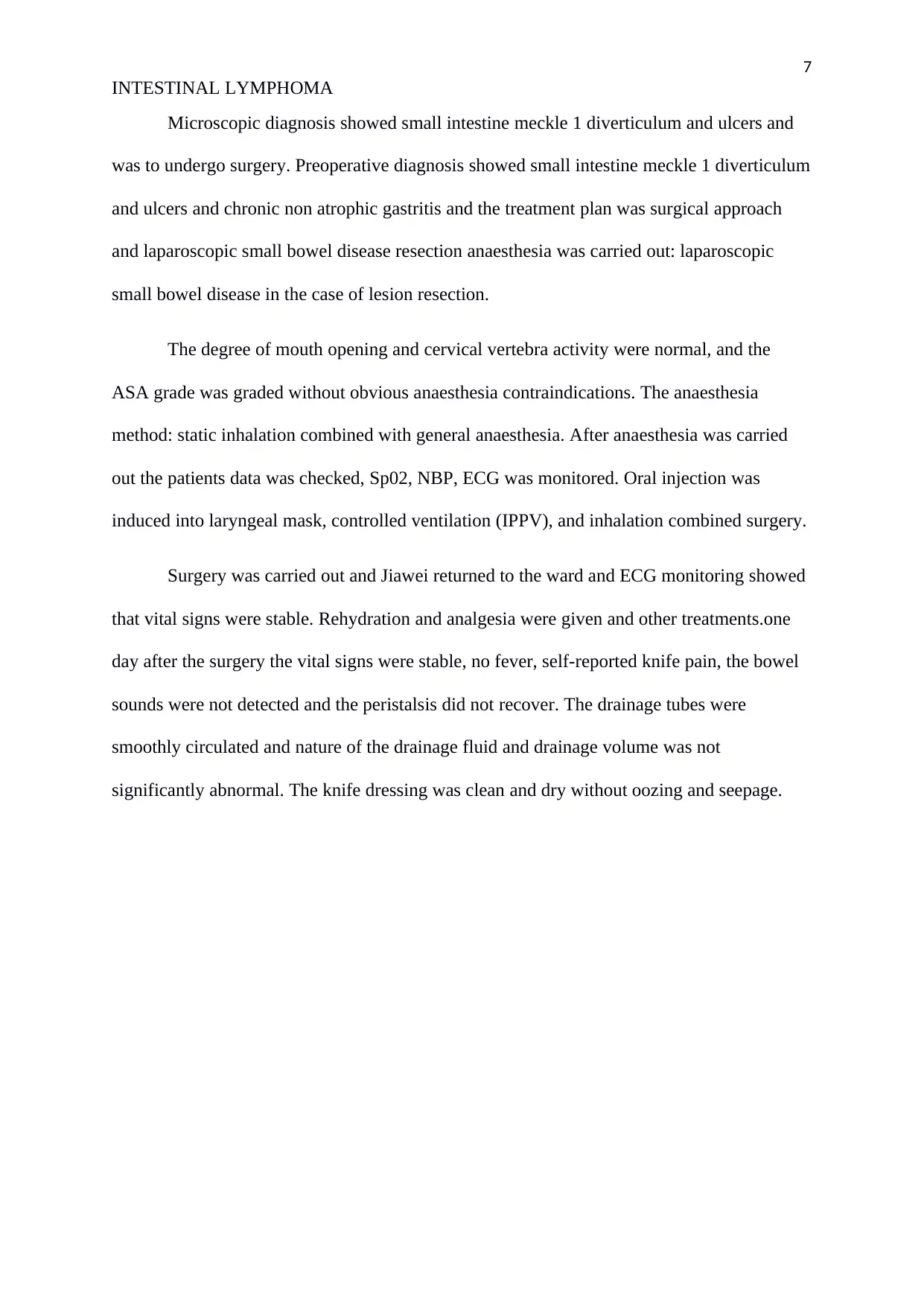
Figure 4 Sagittal CT reconstruction showing a small bowel mass in the lower abdomen.
The second day after surgery: the temperature was normal, no abdominal pains,
bloating, no nausea and vomiting, no deflation. Pain was relieved, body sounds were weak
and bowel movement was not restored. Drainage tubes were smoothly circulated, and the
nature of the drainage fluid and volume was not significantly abnormal. The knife mouth
healed well, no redness and exudation. This did show that the patient was recovering well and
can enter the fluid diet, continue current treatment, observed the changes in condition and
follow the implementation.
The third day after surgery the vital signs were stable, no fever, knife pain was
relieved, no defecation. The bowel sounds were normal and the bowel movement was
restored. The knife dressing is clean and dry without oozing and seepage thus deputy chief
INTESTINAL LYMPHOMA
Figure 4 Sagittal CT reconstruction showing a small bowel mass in the lower abdomen.
The second day after surgery: the temperature was normal, no abdominal pains,
bloating, no nausea and vomiting, no deflation. Pain was relieved, body sounds were weak
and bowel movement was not restored. Drainage tubes were smoothly circulated, and the
nature of the drainage fluid and volume was not significantly abnormal. The knife mouth
healed well, no redness and exudation. This did show that the patient was recovering well and
can enter the fluid diet, continue current treatment, observed the changes in condition and
follow the implementation.
The third day after surgery the vital signs were stable, no fever, knife pain was
relieved, no defecation. The bowel sounds were normal and the bowel movement was
restored. The knife dressing is clean and dry without oozing and seepage thus deputy chief
9
INTESTINAL LYMPHOMA
physician concluded that patients condition is stable, continued with the original treatment
plan.
Then the vital signs were stable, no special discomfort and each drain tube was
removed and the patient recovered after surgery and was discharged from hospital orders and
was advised to pay rest, strengthen nutrition and reasonable diet. Also was advised to pay
attention to keep, mouth clean and dry, prevent knife edge infection.
Discussion
Small bowel tumour is not very common and adds to only less than three per cent of all
gastrointestinal tumours. Small intestinal lymphoma is uncommon compared to other type of
all known lymphomas.
The patient was diagnosed with iliac ulcers, but before he had a history of blood in
stool at very early stages. The patient undergone three types of surgery and was treated at
different hospitals. Ulcers were diagnosed in small intestine meckle 1 diverticulum and later
undergo treatment. After taking alcohol and eating sea food, alcohol led to corrosion of the
iliac walls. There was also a problem of intestinal haemorrhage in the small intestine
vasodilation which was repeated after difficulties of other methods.
There was gastrointestinal bleeding and chronic atrophic gastritis which was later
treated using proper medicine. There was also ileac mucosal acute and chronic inflammation
which later surgery was done. After several surgeries at long last the patient was treated and
released from the hospital.
Conclusion
The diagnosis gives a very occasional and interesting case of intestinal lymphoma and
very uncommon alternative of non-Hodgkin lymphoma. Intestinal lymphoma is triggered by
INTESTINAL LYMPHOMA
physician concluded that patients condition is stable, continued with the original treatment
plan.
Then the vital signs were stable, no special discomfort and each drain tube was
removed and the patient recovered after surgery and was discharged from hospital orders and
was advised to pay rest, strengthen nutrition and reasonable diet. Also was advised to pay
attention to keep, mouth clean and dry, prevent knife edge infection.
Discussion
Small bowel tumour is not very common and adds to only less than three per cent of all
gastrointestinal tumours. Small intestinal lymphoma is uncommon compared to other type of
all known lymphomas.
The patient was diagnosed with iliac ulcers, but before he had a history of blood in
stool at very early stages. The patient undergone three types of surgery and was treated at
different hospitals. Ulcers were diagnosed in small intestine meckle 1 diverticulum and later
undergo treatment. After taking alcohol and eating sea food, alcohol led to corrosion of the
iliac walls. There was also a problem of intestinal haemorrhage in the small intestine
vasodilation which was repeated after difficulties of other methods.
There was gastrointestinal bleeding and chronic atrophic gastritis which was later
treated using proper medicine. There was also ileac mucosal acute and chronic inflammation
which later surgery was done. After several surgeries at long last the patient was treated and
released from the hospital.
Conclusion
The diagnosis gives a very occasional and interesting case of intestinal lymphoma and
very uncommon alternative of non-Hodgkin lymphoma. Intestinal lymphoma is triggered by
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
10
INTESTINAL LYMPHOMA
drinking alcohol and eating sea food. It’s evidence seen from the patient. The condition
should be checked as early as possible to reduce the fatal incidence at adult stages.
References
Basir, N., Bickle, I. C., Telisinghe, P. U., Abdullah, M. S., & Chong, V. H. (2012). Signet
ring cell lymphoma of the small bowel: a case report. Oman medical journal, 27(6),
491.
Carrasco, V., Rodriguez-Bertos, A., Rodríguez-Franco, F., Wise, A. G., Maes, R., Mullaney,
T., & Kiupel, M. (2015). Distinguishing intestinal lymphoma from inflammatory
bowel disease in canine duodenal endoscopic biopsy samples. Veterinary
pathology, 52(4), 668-675.
INTESTINAL LYMPHOMA
drinking alcohol and eating sea food. It’s evidence seen from the patient. The condition
should be checked as early as possible to reduce the fatal incidence at adult stages.
References
Basir, N., Bickle, I. C., Telisinghe, P. U., Abdullah, M. S., & Chong, V. H. (2012). Signet
ring cell lymphoma of the small bowel: a case report. Oman medical journal, 27(6),
491.
Carrasco, V., Rodriguez-Bertos, A., Rodríguez-Franco, F., Wise, A. G., Maes, R., Mullaney,
T., & Kiupel, M. (2015). Distinguishing intestinal lymphoma from inflammatory
bowel disease in canine duodenal endoscopic biopsy samples. Veterinary
pathology, 52(4), 668-675.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
11
INTESTINAL LYMPHOMA
Gou, H. F., Zang, J., Jiang, M., Yang, Y., Cao, D., & Chen, X. C. (2012). Clinical prognostic
analysis of 116 patients with primary intestinal non-Hodgkin lymphoma. Medical
Oncology, 29(1), 227-234..
Elli, L., Contiero, P., Tagliabue, G., Tomba, C., & Bardella, M. T. (2012). Risk of intestinal
lymphoma in undiagnosed coeliac disease: results from a registered population with
different coeliac disease prevalence. Digestive and Liver Disease, 44(9), 743-747.
Ferreri, A. J., Zinzani, P. L., Govi, S., & Pileri, S. A. (2011). Enteropathy-associated T-cell
lymphoma. Critical reviews in oncology/hematology, 79(1), 84-90.
Hoshikawa, M., Takagi, M., Abe, M., Koike, J., Maeda, I., & Tadokoro, M. (2004). A case of
intestinal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue
(MALT Lymphoma) with signet-ring cell morphology. St. Marianna Med J, 32, 569-
576.
Kiupel, M., Smedley, R. C., Pfent, C., Xie, Y., Xue, Y., Wise, A. G., ... & Maes, R. K.
(2011). Diagnostic algorithm to differentiate lymphoma from inflammation in feline
small intestinal biopsy samples. Veterinary Pathology, 48(1), 212-222.
Vaidya, R., Habermann, T. M., Donohue, J. H., Ristow, K. M., Maurer, M. J., Macon, W.
R., ... & Micallef, I. N. (2013). Bowel perforation in intestinal lymphoma: incidence
and clinical features. Annals of oncology, 24(9), 2439-2443.
INTESTINAL LYMPHOMA
Gou, H. F., Zang, J., Jiang, M., Yang, Y., Cao, D., & Chen, X. C. (2012). Clinical prognostic
analysis of 116 patients with primary intestinal non-Hodgkin lymphoma. Medical
Oncology, 29(1), 227-234..
Elli, L., Contiero, P., Tagliabue, G., Tomba, C., & Bardella, M. T. (2012). Risk of intestinal
lymphoma in undiagnosed coeliac disease: results from a registered population with
different coeliac disease prevalence. Digestive and Liver Disease, 44(9), 743-747.
Ferreri, A. J., Zinzani, P. L., Govi, S., & Pileri, S. A. (2011). Enteropathy-associated T-cell
lymphoma. Critical reviews in oncology/hematology, 79(1), 84-90.
Hoshikawa, M., Takagi, M., Abe, M., Koike, J., Maeda, I., & Tadokoro, M. (2004). A case of
intestinal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue
(MALT Lymphoma) with signet-ring cell morphology. St. Marianna Med J, 32, 569-
576.
Kiupel, M., Smedley, R. C., Pfent, C., Xie, Y., Xue, Y., Wise, A. G., ... & Maes, R. K.
(2011). Diagnostic algorithm to differentiate lymphoma from inflammation in feline
small intestinal biopsy samples. Veterinary Pathology, 48(1), 212-222.
Vaidya, R., Habermann, T. M., Donohue, J. H., Ristow, K. M., Maurer, M. J., Macon, W.
R., ... & Micallef, I. N. (2013). Bowel perforation in intestinal lymphoma: incidence
and clinical features. Annals of oncology, 24(9), 2439-2443.
1 out of 11
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.