Intra-Professional Dynamics in Translational Health Research
VerifiedAdded on 2023/06/10
|8
|9631
|411
Report
AI Summary
This assignment delves into the intra-professional dynamics within translational health research, specifically focusing on the interactions between health services researchers and organization scientists. It uses the context of Collaborations for Leadership in Applied Health Research and Care (CLAHRCs) in England to highlight the contestation within social science, where health services researchers seek to elevate their position by emphasizing the practical impact of their research compared to the theory-oriented approach of organization scientists. The study explores how these dynamics influence resource allocation and professional standing within the translational health research domain, addressing the need for understanding how different scientific communities perceive and judge one another. The research questions address the basis of interaction between health services researchers and organization scientists, and how better interactions can be supported to improve disciplinary collaboration.
Intra-professional dynamics in translational health research:
The perspective of social scientists
Graeme Currie*
, Nellie El Enany,Andy Lockett
Warwick Business School,The University of Warwick,Coventry CV4 7AL,United Kingdom
a r t i c l e i n f o
Article history:
Received 23 May 2013
Received in revised form
18 April 2014
Accepted 27 May 2014
Available online 27 May 2014
Keywords:
Translational health research
Epistemic communities
Social scientists
Professional dynamics
CLAHRC
England
a b s t r a c t
In contrast to previous studies,which focus upon the professionaldynamics of translationalhealth
research between clinician scientists and socialscientists (inter-professionalcontestation),we focus
upon contestation within social science (intra-professionalcontestation).Drawing on the empirical
context of Collaborations for Leadership in Applied Health Research and Care (CLAHRCs) in England,we
highlight that although social scientists accept subordination to clinician scientists,health services re-
searchers attempt to enhance their position in translationalhealth research vis-a-vis organisation sci-
entists,whom they perceive as relative newcomers to the research domain.Health services researchers
do so through privileging the practicalimpact of their research,compared to organisation scientists'
orientation towards development of theory,which health services researchers argue is decoupled from
any concern with healthcare improvement.The concern of health services researchers lies with main-
taining existing patterns of resource allocation to support their research endeavours,working alongside
clinician scientists,in translationalhealth research.The response of organisation scientists is one that
might be considered ambivalent,since,unlike health services researchers, they do not rely upon a close
relationship with clinician scientists to carry out research,or more generally,garner resource.
© 2014 Elsevier Ltd.All rights reserved.
1. Introduction
In this paper we draw on the sociology of professions literature
(Abbott, 1988; Freidson, 1984) to explore the extent to which it is
possible for different epistemic communities within social science
to integrate into,and thrive in the domain of,translational health
research,within which the experimental paradigm occupiesa
hegemonic position.Extant studies have focused on interactions
across epistemic communities ofclinician scientists and social
scientists in translational health research (Albert et al., 2008; Albert
et al.,2009; Wilson-Kovacs and Hauskeller,2012).In contrast,we
view the challenge of translational health research from the
perspective of social scientists, a neglected focus of empirical study
(Albert et al.,2008; Wilson-Kovacs and Hauskeller,2012).Further,
we treat social scientists as a variegated,epistemic community
(Becher and Trowler,2001), and disaggregate those involved in
translational health research into two distinct epistemic commu-
nities: health services researchersand organisation scientists.
Finally,rather than focussing on the interaction between clinician
scientists and socialscientists (inter-professionaldynamics),we
focus upon interaction between health services researchers and
organisation scientists (intra-professionaldynamics).In so doing,
we adopt a relational perspective across and within epistemic
communities,which enables us to explore the discordance be-
tween social scientists involved in translationalhealth research
about the value of others'research (Albert et al.,2009).
In exploring the discordance between social scientists in
translationalresearch we address the callfor research to under-
stand how different epistemic scientific communities perceive and
judge one another,through consideration of the professionaldy-
namics of the translational health research domain (Albert et al.,
2008,2009; Wilson-Kovacs and Hauskeller,2012).As Albert et al.
(2009: 174) state: “in the current move towards inter-disciplinary
research,it is vital to understand how scientists from different
backgrounds and with different degrees of scientific authority
perceive and judge one another”,since this shapes not only their
attitudes towards collaboration,but has material resource conse-
quences.In particular,researchers are asked to consider how sci-
entific epistemic communities attempt to establish a distinct field
of expertise,maintain professional jurisdiction,and consolidate or
enhance status and collective standing as leaders of translational
health research (Wilson-Kovacs and Hauskeller,2012).
* Corresponding author.
E-mail address: Graeme.currie@wbs.ac.uk (G.Currie).
Contents lists available at ScienceDirect
Social Science & Medicine
j o u r n a lhomepage: w w w . e l s e v i e r . c o m / l o c a t e / s o c s c i m e d
http://dx.doi.org/10.1016/j.socscimed.2014.05.045
0277-9536/© 2014 Elsevier Ltd.All rights reserved.
Social Science & Medicine 114 (2014) 81e88
The perspective of social scientists
Graeme Currie*
, Nellie El Enany,Andy Lockett
Warwick Business School,The University of Warwick,Coventry CV4 7AL,United Kingdom
a r t i c l e i n f o
Article history:
Received 23 May 2013
Received in revised form
18 April 2014
Accepted 27 May 2014
Available online 27 May 2014
Keywords:
Translational health research
Epistemic communities
Social scientists
Professional dynamics
CLAHRC
England
a b s t r a c t
In contrast to previous studies,which focus upon the professionaldynamics of translationalhealth
research between clinician scientists and socialscientists (inter-professionalcontestation),we focus
upon contestation within social science (intra-professionalcontestation).Drawing on the empirical
context of Collaborations for Leadership in Applied Health Research and Care (CLAHRCs) in England,we
highlight that although social scientists accept subordination to clinician scientists,health services re-
searchers attempt to enhance their position in translationalhealth research vis-a-vis organisation sci-
entists,whom they perceive as relative newcomers to the research domain.Health services researchers
do so through privileging the practicalimpact of their research,compared to organisation scientists'
orientation towards development of theory,which health services researchers argue is decoupled from
any concern with healthcare improvement.The concern of health services researchers lies with main-
taining existing patterns of resource allocation to support their research endeavours,working alongside
clinician scientists,in translationalhealth research.The response of organisation scientists is one that
might be considered ambivalent,since,unlike health services researchers, they do not rely upon a close
relationship with clinician scientists to carry out research,or more generally,garner resource.
© 2014 Elsevier Ltd.All rights reserved.
1. Introduction
In this paper we draw on the sociology of professions literature
(Abbott, 1988; Freidson, 1984) to explore the extent to which it is
possible for different epistemic communities within social science
to integrate into,and thrive in the domain of,translational health
research,within which the experimental paradigm occupiesa
hegemonic position.Extant studies have focused on interactions
across epistemic communities ofclinician scientists and social
scientists in translational health research (Albert et al., 2008; Albert
et al.,2009; Wilson-Kovacs and Hauskeller,2012).In contrast,we
view the challenge of translational health research from the
perspective of social scientists, a neglected focus of empirical study
(Albert et al.,2008; Wilson-Kovacs and Hauskeller,2012).Further,
we treat social scientists as a variegated,epistemic community
(Becher and Trowler,2001), and disaggregate those involved in
translational health research into two distinct epistemic commu-
nities: health services researchersand organisation scientists.
Finally,rather than focussing on the interaction between clinician
scientists and socialscientists (inter-professionaldynamics),we
focus upon interaction between health services researchers and
organisation scientists (intra-professionaldynamics).In so doing,
we adopt a relational perspective across and within epistemic
communities,which enables us to explore the discordance be-
tween social scientists involved in translationalhealth research
about the value of others'research (Albert et al.,2009).
In exploring the discordance between social scientists in
translationalresearch we address the callfor research to under-
stand how different epistemic scientific communities perceive and
judge one another,through consideration of the professionaldy-
namics of the translational health research domain (Albert et al.,
2008,2009; Wilson-Kovacs and Hauskeller,2012).As Albert et al.
(2009: 174) state: “in the current move towards inter-disciplinary
research,it is vital to understand how scientists from different
backgrounds and with different degrees of scientific authority
perceive and judge one another”,since this shapes not only their
attitudes towards collaboration,but has material resource conse-
quences.In particular,researchers are asked to consider how sci-
entific epistemic communities attempt to establish a distinct field
of expertise,maintain professional jurisdiction,and consolidate or
enhance status and collective standing as leaders of translational
health research (Wilson-Kovacs and Hauskeller,2012).
* Corresponding author.
E-mail address: Graeme.currie@wbs.ac.uk (G.Currie).
Contents lists available at ScienceDirect
Social Science & Medicine
j o u r n a lhomepage: w w w . e l s e v i e r . c o m / l o c a t e / s o c s c i m e d
http://dx.doi.org/10.1016/j.socscimed.2014.05.045
0277-9536/© 2014 Elsevier Ltd.All rights reserved.
Social Science & Medicine 114 (2014) 81e88
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

In the remainder of the paper,and based on the above,we
address the following research questions: (i) on what basis,and
with what effect,do health services researchers and organisation
scientists interact (or not) in translational health research? And, (ii)
assuming policymakers are justified in their investment in trans-
lational health research, embedded within which disciplinary
collaboration is necessary,how might better interactions between
health services researchers and organisation scientists be
supported?
2. Conceptual framework
Our study conceives disciplinary and scientific practices as social
institutions (Albert et al., 2009), which are manifested as ‘epistemic
communities’ (Knorr-Cetina, 1999) or ‘academic tribes’ (Becher and
Trowler, 2001). Epistemic communities constitute, “taken-for-
granted ways of thinking about and doing science; e.g.shared as-
sumptions about what ‘good’ science is,what method is best to
generate valid results,how data should be collected and inter-
preted, and what constitutes productive science” (Albertet al.,
2009: 173).
In considering the interaction of epistemic communities within
translationalhealth research,scholars have highlighted that the
experimentalmethod is privileged (Albert et al., 2008, 2009;
Wilson-Kovacs and Hauskeller,2012),which positions biomed-
ical scientists and clinician scientists at the top of the hierarchy of
epistemic communities involved in translationalhealth research.
The process through which hierarchy is derived is one whereby
certain procedural assessment criteria are applied to evaluate the
science of an epistemic community.Albert et al. (2008, 2009)
describe how the interaction of biomedicalor clinician scientists
and socialscientists is framed by epistemic culture and position
(dominant or subordinate),and differential power to set out what
constituteslegitimate science.The current dominant scientific
criteria in translational health research are primarily atheoretical,
quantitative and hypothesis-driven, whereas social science is more
theoretical,qualitative and interpretive (Albert et al.,2008).The
effect of proceduralassessment criteria about value of science is
one that privileges the epistemic community of clinician scientists,
and renders subordinate the epistemic community ofsocial sci-
entists.Thus,Albert et al.(2008,2009) anticipate that the growth
of social sciences will continue to meet obstacles, derived from the
dominant position of the episteme of biomedicaland clinician
scientists,within the health research field.Reflecting the pessi-
mism of Albert et al.(2008,2009),other academic commentators
report that current attempts to integrate social scientists into the
translational health research domain are encountering significant
difficulties and resistance from clinician scientists (Bernier,2005;
De Villiers, 2005; Grol, 1997; Kislov et al., 2011; Rowley et al.,
2012).
The aforementioned studies focus upon interactions between
biomedical or clinician scientists and social scientists (a matter of
inter-disciplinary contestation),but treat social science as a
monolithic epistemic community.We suggest,however,that in-
teractions within the epistemic community of social scientists are
likely to be rather more dynamic than recognised in extant litera-
ture. In recognition of a gap within social science,as applied to
healthcare,Currie et al.(2012) edited a collection of studies pro-
duced by organisation scientists to draw to the attention of medical
sociologists and health policy academics the value of their work. In
reflecting upon why such integration ofepistemic communities
within social science has been slow to realise,we suggestthat
attention should be focused on the procedural assessment criteria
in framing the intra-disciplinary relations between organisation
scientists and health services researchers in translationalhealth
research.We suggest that the sociology ofprofessions literature
might provide insight into this issue.
The sociology of professions literature suggests thatthe dy-
namics of professional organisation relate to stratification and hi-
erarchy designed to protect or extend jurisdiction through expert
claims about exclusivity of knowledge, in a way that simultaneously
enhances professional status (Abbott, 1988; Freidson, 1984). Those
in privileged positions in the professional hierarchy (in the case of
translational health research,clinician scientists),may accommo-
date substitution of their labour where they are not competing for
resource. Simply stated, abundance or scarcity of resource is likely
to shape professional dynamics. Competition for resource has been
noted as a significant issue in contestation between scientific
epistemic communities in translationalhealth research (Albert
et al.,2008,2009).The incentive for social scientists to engage in
translationalhealth research is to gain higher status in the field,
exert more influence on health policy,and perhaps most impor-
tantly,to access more resources (Albert et al.,2008).Even where
resource constraints are less significant,however,powerful pro-
fessions may seek to controlthat labour with which it has been
substituted; i.e.a delegation tactic,which renders the substitute
labour subordinate to the powerful profession (Martin et al., 2009).
Thus, perhaps unsurprisingly,when engaging in translational
health research,social scientists are positioned as subordinate to
clinician scientists,meaning that they only have access to limited
financial resource (Albert et al.,2008,2009).How such processes
play out between organisation scientists and health services re-
searchers within the socialscience epistemic community is not
clear,but similar dynamics around knowledge claims and stratifi-
cation are likely to be evident.
3. Data and method
3.1.The empirical case
Our empirical case is CLAHRC,a translationalresearch inter-
vention in the English National Health Service (NHS) (Dzau et al.,
2010),which is one of many such translationalhealth research
interventions evident globally.For example,in the United States,
Veterans'Health Administration's Integrated Health and Research
System (Graham and Tetroe,2009), American Quality Enhance-
ment Research Initiative (www.queri.research.va.gov), and Clinical
Translational Science Centres (Butler,2008); in Canada,the Cana-
dian Health Services Research Foundation (Dussault et al.,2007);
and in the Netherlands,the Dutch Academic Collaborative Centres
for Public Health (Wehrens et al.,2012).
Nine pilot CLAHRCs were established in 2008,funded £100
million by the National Institute of Health Research (NIHR) forfive
years, with a similar amount of matched funding from participating
universities and healthcare organisations. Recently, further funding
of £120million,again with a similar amount of matched funding
from participating universities and healthcare organisations,was
awarded for 13 CLAHRCs, encompassing continuation of funding for
the earlier pilots,for a further five years from 2014.
The intention of the CLAHRC initiative was promote trans-
lational research to move beyond linear models of translating ac-
ademic evidence into practice (Nutley et al., 2007). In doing so the
nine CLAHRCs were tasked with three key interlocking functions:
(i) conducting high quality applied health research;(ii) imple-
menting the findings from research in clinicalpractice; and (iii)
increasing the capacity of NHS organisations to engage with and
apply research. The nine CLAHRCs are regionally focused, with their
agendas being determined by the partnering organisations and
tailored to healthcare needs in their respective geographical areas.
Whilst mandated by policy, CLAHRCs were regarded by the NIHR as
G. Currie et al./ Social Science & Medicine 114 (2014) 81e8882
address the following research questions: (i) on what basis,and
with what effect,do health services researchers and organisation
scientists interact (or not) in translational health research? And, (ii)
assuming policymakers are justified in their investment in trans-
lational health research, embedded within which disciplinary
collaboration is necessary,how might better interactions between
health services researchers and organisation scientists be
supported?
2. Conceptual framework
Our study conceives disciplinary and scientific practices as social
institutions (Albert et al., 2009), which are manifested as ‘epistemic
communities’ (Knorr-Cetina, 1999) or ‘academic tribes’ (Becher and
Trowler, 2001). Epistemic communities constitute, “taken-for-
granted ways of thinking about and doing science; e.g.shared as-
sumptions about what ‘good’ science is,what method is best to
generate valid results,how data should be collected and inter-
preted, and what constitutes productive science” (Albertet al.,
2009: 173).
In considering the interaction of epistemic communities within
translationalhealth research,scholars have highlighted that the
experimentalmethod is privileged (Albert et al., 2008, 2009;
Wilson-Kovacs and Hauskeller,2012),which positions biomed-
ical scientists and clinician scientists at the top of the hierarchy of
epistemic communities involved in translationalhealth research.
The process through which hierarchy is derived is one whereby
certain procedural assessment criteria are applied to evaluate the
science of an epistemic community.Albert et al. (2008, 2009)
describe how the interaction of biomedicalor clinician scientists
and socialscientists is framed by epistemic culture and position
(dominant or subordinate),and differential power to set out what
constituteslegitimate science.The current dominant scientific
criteria in translational health research are primarily atheoretical,
quantitative and hypothesis-driven, whereas social science is more
theoretical,qualitative and interpretive (Albert et al.,2008).The
effect of proceduralassessment criteria about value of science is
one that privileges the epistemic community of clinician scientists,
and renders subordinate the epistemic community ofsocial sci-
entists.Thus,Albert et al.(2008,2009) anticipate that the growth
of social sciences will continue to meet obstacles, derived from the
dominant position of the episteme of biomedicaland clinician
scientists,within the health research field.Reflecting the pessi-
mism of Albert et al.(2008,2009),other academic commentators
report that current attempts to integrate social scientists into the
translational health research domain are encountering significant
difficulties and resistance from clinician scientists (Bernier,2005;
De Villiers, 2005; Grol, 1997; Kislov et al., 2011; Rowley et al.,
2012).
The aforementioned studies focus upon interactions between
biomedical or clinician scientists and social scientists (a matter of
inter-disciplinary contestation),but treat social science as a
monolithic epistemic community.We suggest,however,that in-
teractions within the epistemic community of social scientists are
likely to be rather more dynamic than recognised in extant litera-
ture. In recognition of a gap within social science,as applied to
healthcare,Currie et al.(2012) edited a collection of studies pro-
duced by organisation scientists to draw to the attention of medical
sociologists and health policy academics the value of their work. In
reflecting upon why such integration ofepistemic communities
within social science has been slow to realise,we suggestthat
attention should be focused on the procedural assessment criteria
in framing the intra-disciplinary relations between organisation
scientists and health services researchers in translationalhealth
research.We suggest that the sociology ofprofessions literature
might provide insight into this issue.
The sociology of professions literature suggests thatthe dy-
namics of professional organisation relate to stratification and hi-
erarchy designed to protect or extend jurisdiction through expert
claims about exclusivity of knowledge, in a way that simultaneously
enhances professional status (Abbott, 1988; Freidson, 1984). Those
in privileged positions in the professional hierarchy (in the case of
translational health research,clinician scientists),may accommo-
date substitution of their labour where they are not competing for
resource. Simply stated, abundance or scarcity of resource is likely
to shape professional dynamics. Competition for resource has been
noted as a significant issue in contestation between scientific
epistemic communities in translationalhealth research (Albert
et al.,2008,2009).The incentive for social scientists to engage in
translationalhealth research is to gain higher status in the field,
exert more influence on health policy,and perhaps most impor-
tantly,to access more resources (Albert et al.,2008).Even where
resource constraints are less significant,however,powerful pro-
fessions may seek to controlthat labour with which it has been
substituted; i.e.a delegation tactic,which renders the substitute
labour subordinate to the powerful profession (Martin et al., 2009).
Thus, perhaps unsurprisingly,when engaging in translational
health research,social scientists are positioned as subordinate to
clinician scientists,meaning that they only have access to limited
financial resource (Albert et al.,2008,2009).How such processes
play out between organisation scientists and health services re-
searchers within the socialscience epistemic community is not
clear,but similar dynamics around knowledge claims and stratifi-
cation are likely to be evident.
3. Data and method
3.1.The empirical case
Our empirical case is CLAHRC,a translationalresearch inter-
vention in the English National Health Service (NHS) (Dzau et al.,
2010),which is one of many such translationalhealth research
interventions evident globally.For example,in the United States,
Veterans'Health Administration's Integrated Health and Research
System (Graham and Tetroe,2009), American Quality Enhance-
ment Research Initiative (www.queri.research.va.gov), and Clinical
Translational Science Centres (Butler,2008); in Canada,the Cana-
dian Health Services Research Foundation (Dussault et al.,2007);
and in the Netherlands,the Dutch Academic Collaborative Centres
for Public Health (Wehrens et al.,2012).
Nine pilot CLAHRCs were established in 2008,funded £100
million by the National Institute of Health Research (NIHR) forfive
years, with a similar amount of matched funding from participating
universities and healthcare organisations. Recently, further funding
of £120million,again with a similar amount of matched funding
from participating universities and healthcare organisations,was
awarded for 13 CLAHRCs, encompassing continuation of funding for
the earlier pilots,for a further five years from 2014.
The intention of the CLAHRC initiative was promote trans-
lational research to move beyond linear models of translating ac-
ademic evidence into practice (Nutley et al., 2007). In doing so the
nine CLAHRCs were tasked with three key interlocking functions:
(i) conducting high quality applied health research;(ii) imple-
menting the findings from research in clinicalpractice; and (iii)
increasing the capacity of NHS organisations to engage with and
apply research. The nine CLAHRCs are regionally focused, with their
agendas being determined by the partnering organisations and
tailored to healthcare needs in their respective geographical areas.
Whilst mandated by policy, CLAHRCs were regarded by the NIHR as
G. Currie et al./ Social Science & Medicine 114 (2014) 81e8882
experimentalin nature during their inception,with considerable
variation allowed for their structures and processes. Social sciences
were variably integrated into CLAHRC plans,with some involving
input from health services researchers located in or near to medical
schools,and others involving input from organisation scientists in
business schools;academic research and clinicalpractice were
blended in different ways; and there were differences in the disease
emphasis ofCLAHRCs,although all nine CLAHRCs focused upon
translational health research around long-term conditions.
Regarding the constituent epistemic communities upon whom
we focus within CLAHRC,we asked our respondents to self-define
themselvesas clinician scientists,1 health services researchers,
organisation scientists,NHS managers,and clinical practitioners.
We corroborated their self-definitions with our own assessment of
which epistemic community towards which they orientate (in all
cases,we agreed with the self-definition). We recognise,however,
that our categorisation is rather crude,and operates as a heuristic
device to aid theoretical analysis. Some academics, as discussed in
our empirical presentation,are not easily categorised and present
themselves as ‘hybrid’academics thatcross the boundaries of
epistemic communities.
Regarding the authors'own position, we are located in the
category oforganisation scientists,located in a business school
(although at least one of us might characterise himself/herself as
‘hybrid').We remained reflexive in our analysis to mediate any
partiality in analysis; e.g.analysis was presented to CLAHRC Di-
rectors (clinician scientists), other audiences where health services
researchers and clinician scientists were present. In support of our
impartial stance,we highlight analysis within the manuscript is
somewhat critical of our own community; e.g. as theoretically
driven with little concern for practical impact, as just chasing
research funding wherever its source and focus.
3.2. Data collection and analysis
We employed a longitudinal research strategy over a period of
three years to analyse interactions between constituent epistemic
communities of CLAHRC.Ethics approvalwas sought and gained
prior to commencing research (Research Ethics Committee refer-
ence: 10/H0402/6 Leicestershire,Northamptonshire and Rutland
Research Ethics Committee 2).CLAHRC Data presented in this
article is mainly drawn from 174 qualitative interviews carried out
between 2009 and 2012,encompassing a first,exploratory phase
across all 9 CLAHRCs (104 interviews), followed by a second phase
of data collection across four in-depth comparative cases (Cases B,
C, D, G: 70 interviews). Details of the interviewees are presented in
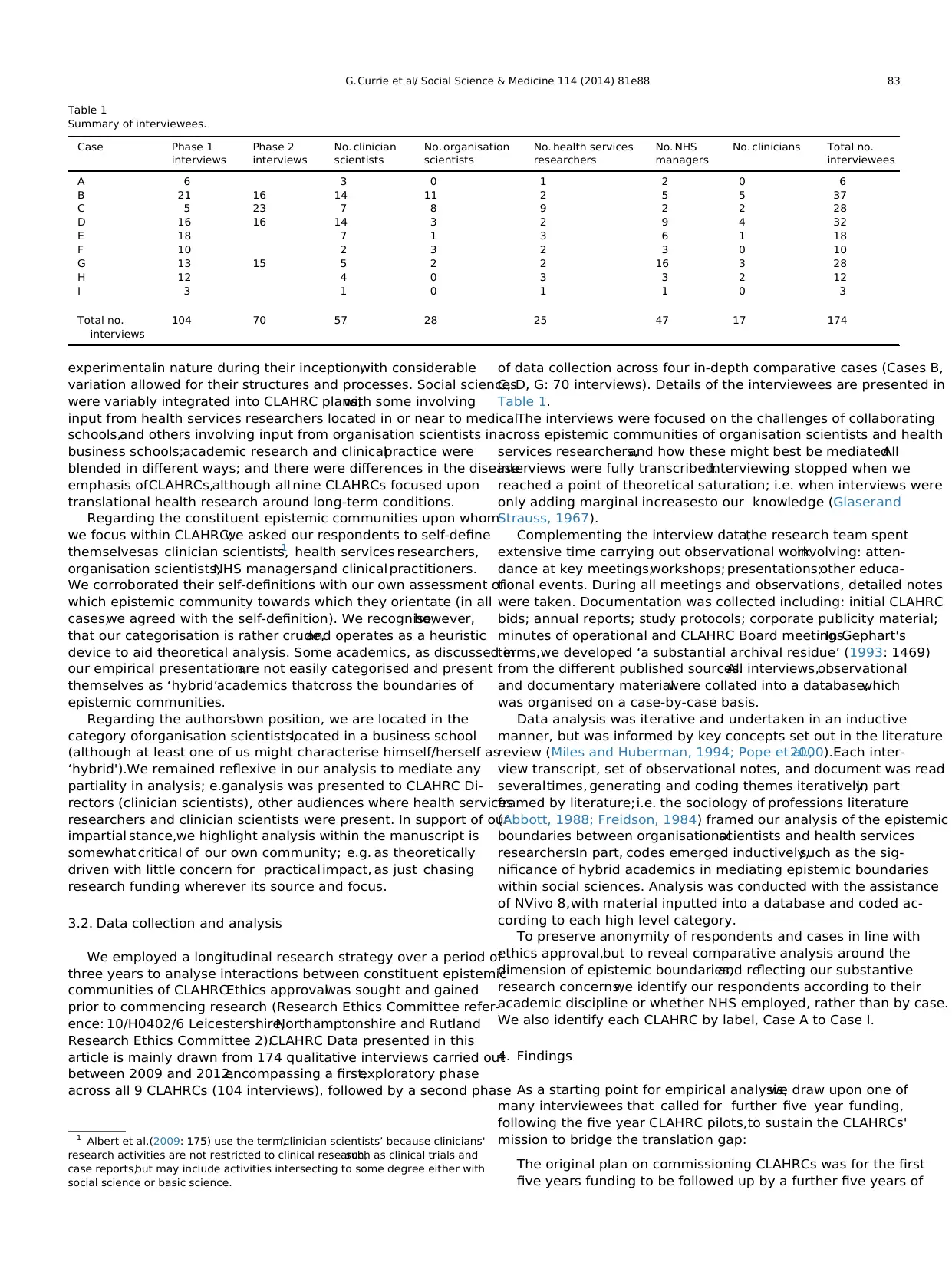
Table 1.
The interviews were focused on the challenges of collaborating
across epistemic communities of organisation scientists and health
services researchers,and how these might best be mediated.All
interviews were fully transcribed.Interviewing stopped when we
reached a point of theoretical saturation; i.e. when interviews were
only adding marginal increasesto our knowledge (Glaserand
Strauss, 1967).
Complementing the interview data,the research team spent
extensive time carrying out observational work,involving: atten-
dance at key meetings;workshops; presentations;other educa-
tional events. During all meetings and observations, detailed notes
were taken. Documentation was collected including: initial CLAHRC
bids; annual reports; study protocols; corporate publicity material;
minutes of operational and CLAHRC Board meetings.In Gephart's
terms,we developed ‘a substantial archival residue’ (1993: 1469)
from the different published sources.All interviews,observational
and documentary materialwere collated into a database,which
was organised on a case-by-case basis.
Data analysis was iterative and undertaken in an inductive
manner, but was informed by key concepts set out in the literature
review (Miles and Huberman, 1994; Pope et al.,2000).Each inter-
view transcript, set of observational notes, and document was read
severaltimes, generating and coding themes iteratively,in part
framed by literature;i.e. the sociology of professions literature
(Abbott, 1988; Freidson, 1984) framed our analysis of the epistemic
boundaries between organisationalscientists and health services
researchers.In part, codes emerged inductively,such as the sig-
nificance of hybrid academics in mediating epistemic boundaries
within social sciences. Analysis was conducted with the assistance
of NVivo 8,with material inputted into a database and coded ac-
cording to each high level category.
To preserve anonymity of respondents and cases in line with
ethics approval,but to reveal comparative analysis around the
dimension of epistemic boundaries,and reflecting our substantive
research concerns,we identify our respondents according to their
academic discipline or whether NHS employed, rather than by case.
We also identify each CLAHRC by label, Case A to Case I.
4. Findings
As a starting point for empirical analysis,we draw upon one of
many interviewees that called for further five year funding,
following the five year CLAHRC pilots,to sustain the CLAHRCs'
mission to bridge the translation gap:
The original plan on commissioning CLAHRCs was for the first
five years funding to be followed up by a further five years of
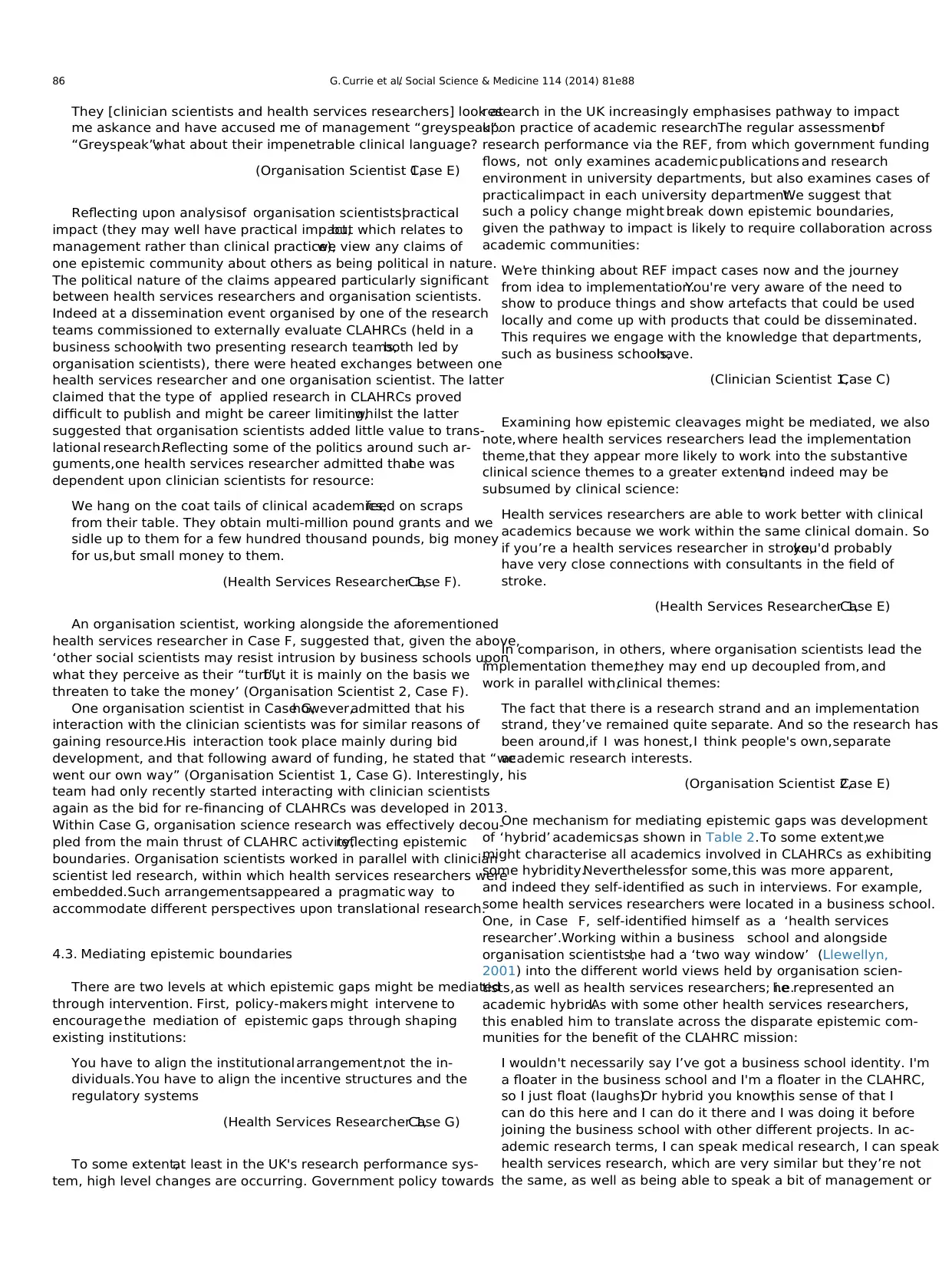
Table 1
Summary of interviewees.
Case Phase 1
interviews
Phase 2
interviews
No. clinician
scientists
No. organisation
scientists
No. health services
researchers
No. NHS
managers
No. clinicians Total no.
interviewees
A 6 3 0 1 2 0 6
B 21 16 14 11 2 5 5 37
C 5 23 7 8 9 2 2 28
D 16 16 14 3 2 9 4 32
E 18 7 1 3 6 1 18
F 10 2 3 2 3 0 10
G 13 15 5 2 2 16 3 28
H 12 4 0 3 3 2 12
I 3 1 0 1 1 0 3
Total no.
interviews
104 70 57 28 25 47 17 174
1 Albert et al.(2009: 175) use the term,‘clinician scientists’ because clinicians'
research activities are not restricted to clinical research,such as clinical trials and
case reports,but may include activities intersecting to some degree either with
social science or basic science.
G. Currie et al./ Social Science & Medicine 114 (2014) 81e88 83
variation allowed for their structures and processes. Social sciences
were variably integrated into CLAHRC plans,with some involving
input from health services researchers located in or near to medical
schools,and others involving input from organisation scientists in
business schools;academic research and clinicalpractice were
blended in different ways; and there were differences in the disease
emphasis ofCLAHRCs,although all nine CLAHRCs focused upon
translational health research around long-term conditions.
Regarding the constituent epistemic communities upon whom
we focus within CLAHRC,we asked our respondents to self-define
themselvesas clinician scientists,1 health services researchers,
organisation scientists,NHS managers,and clinical practitioners.
We corroborated their self-definitions with our own assessment of
which epistemic community towards which they orientate (in all
cases,we agreed with the self-definition). We recognise,however,
that our categorisation is rather crude,and operates as a heuristic
device to aid theoretical analysis. Some academics, as discussed in
our empirical presentation,are not easily categorised and present
themselves as ‘hybrid’academics thatcross the boundaries of
epistemic communities.
Regarding the authors'own position, we are located in the
category oforganisation scientists,located in a business school
(although at least one of us might characterise himself/herself as
‘hybrid').We remained reflexive in our analysis to mediate any
partiality in analysis; e.g.analysis was presented to CLAHRC Di-
rectors (clinician scientists), other audiences where health services
researchers and clinician scientists were present. In support of our
impartial stance,we highlight analysis within the manuscript is
somewhat critical of our own community; e.g. as theoretically
driven with little concern for practical impact, as just chasing
research funding wherever its source and focus.
3.2. Data collection and analysis
We employed a longitudinal research strategy over a period of
three years to analyse interactions between constituent epistemic
communities of CLAHRC.Ethics approvalwas sought and gained
prior to commencing research (Research Ethics Committee refer-
ence: 10/H0402/6 Leicestershire,Northamptonshire and Rutland
Research Ethics Committee 2).CLAHRC Data presented in this
article is mainly drawn from 174 qualitative interviews carried out
between 2009 and 2012,encompassing a first,exploratory phase
across all 9 CLAHRCs (104 interviews), followed by a second phase
of data collection across four in-depth comparative cases (Cases B,
C, D, G: 70 interviews). Details of the interviewees are presented in
Table 1.
The interviews were focused on the challenges of collaborating
across epistemic communities of organisation scientists and health
services researchers,and how these might best be mediated.All
interviews were fully transcribed.Interviewing stopped when we
reached a point of theoretical saturation; i.e. when interviews were
only adding marginal increasesto our knowledge (Glaserand
Strauss, 1967).
Complementing the interview data,the research team spent
extensive time carrying out observational work,involving: atten-
dance at key meetings;workshops; presentations;other educa-
tional events. During all meetings and observations, detailed notes
were taken. Documentation was collected including: initial CLAHRC
bids; annual reports; study protocols; corporate publicity material;
minutes of operational and CLAHRC Board meetings.In Gephart's
terms,we developed ‘a substantial archival residue’ (1993: 1469)
from the different published sources.All interviews,observational
and documentary materialwere collated into a database,which
was organised on a case-by-case basis.
Data analysis was iterative and undertaken in an inductive
manner, but was informed by key concepts set out in the literature
review (Miles and Huberman, 1994; Pope et al.,2000).Each inter-
view transcript, set of observational notes, and document was read
severaltimes, generating and coding themes iteratively,in part
framed by literature;i.e. the sociology of professions literature
(Abbott, 1988; Freidson, 1984) framed our analysis of the epistemic
boundaries between organisationalscientists and health services
researchers.In part, codes emerged inductively,such as the sig-
nificance of hybrid academics in mediating epistemic boundaries
within social sciences. Analysis was conducted with the assistance
of NVivo 8,with material inputted into a database and coded ac-
cording to each high level category.
To preserve anonymity of respondents and cases in line with
ethics approval,but to reveal comparative analysis around the
dimension of epistemic boundaries,and reflecting our substantive
research concerns,we identify our respondents according to their
academic discipline or whether NHS employed, rather than by case.
We also identify each CLAHRC by label, Case A to Case I.
4. Findings
As a starting point for empirical analysis,we draw upon one of
many interviewees that called for further five year funding,
following the five year CLAHRC pilots,to sustain the CLAHRCs'
mission to bridge the translation gap:
The original plan on commissioning CLAHRCs was for the first
five years funding to be followed up by a further five years of
Table 1
Summary of interviewees.
Case Phase 1
interviews
Phase 2
interviews
No. clinician
scientists
No. organisation
scientists
No. health services
researchers
No. NHS
managers
No. clinicians Total no.
interviewees
A 6 3 0 1 2 0 6
B 21 16 14 11 2 5 5 37
C 5 23 7 8 9 2 2 28
D 16 16 14 3 2 9 4 32
E 18 7 1 3 6 1 18
F 10 2 3 2 3 0 10
G 13 15 5 2 2 16 3 28
H 12 4 0 3 3 2 12
I 3 1 0 1 1 0 3
Total no.
interviews
104 70 57 28 25 47 17 174
1 Albert et al.(2009: 175) use the term,‘clinician scientists’ because clinicians'
research activities are not restricted to clinical research,such as clinical trials and
case reports,but may include activities intersecting to some degree either with
social science or basic science.
G. Currie et al./ Social Science & Medicine 114 (2014) 81e88 83
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
funding. In all honesty, we need that. We took a long time to get
going and the CLAHRC journey needs to continue,not just for
capacity building purposes,but because success has been vari-
able.For every clinicalstudy that has bridged the translation
gap, another has failed. In large part the academic side has failed
to get their act together around improvement science.
(NHS Manager 1, Case B)
Regarding our theoreticalconcerns,the last sentence in the
quote above is particularly interesting in highlighting the ‘failure’
within the academic community itselfto cohere around trans-
lational health research. Following such assertions, we examine the
epistemic gap within the academic community itself,between
organisation scientistsand health services researchers,and in
which clinician scientists are implicated.
Before presenting analysis,within Table 2, set out below,we
summarise features of our comparative CLAHRC cases,which are
relevant for our theoretical analysis.
Within Table 2, first, we provide an assessmentof research
reputation of each case,based upon the research ranking ofthe
constituentmedical schools within each CLAHRC as three-way
categorisation:(i) high (top ten per cent of medical schools as
measured by UK's Research Excellence Framework (REF),which
represents a nationalaudit of a university department's research
environment,activity and output); (ii) mid (medicalschools be-
tween the halfway point and upper decile in league tables gener-
ated by REF); and (iii) low (below the halfway point). The REF
criterion was applied a priori to select the second phase cases. Two
high ranking cases (B and G), and two medium ranking cases (C and
D), were selected. Second,we categorised the involvementof
organisation scientists from business schools in each CLAHRC as
follows: (i) no involvement; (ii) limited involvement (very limited
number of organisation scientists outside an institutional CLAHRC
partnership with a business school); and (iii) significant involve-
ment (larger number of organisation scientists encompassed
within an institutional CLAHRC partnership with a business
school). We also applied the business school involvement criterion
to select second phase cases,with Cases C and G exhibiting sig-
nificant involvement of organisation scientists,and Cases B and D,
exhibiting limited involvementof organisation scientists.Third,
induced from our data analysis, we identify the presence of hybrid
academics at the senior level of each CLAHRC.By hybrid academic
we mean those academics that have worked across,and under-
stand through,a ‘two way window’ (Llewellyn,2001) on our two
focal epistemic communities oforganisation science and health
services research. Finally, within Table 2, in terms of outcomes, we
make a qualitative judgement about whether the research carried
out by organisation scientists is either decoupled (runs in parallel)
or more integrated in translational health research,focused upon
the same health service domain within each CLAHRC. So, for
example,in Case G organisation scientists ran a study, which
focused on overall CLAHRC strategy over the five years, but did not
inform the substantive health research studies within which
clinician scientists and health services researchers collaborated.In
contrast,in case D, organisation scientists and their researchers
worked within the substantive health research studies alongside
clinician scientists and health services researchers (see later a quote
detailing this point). We note, and as evidenced in Table 2, the latter
situation,in part, may have been due to presence of hybrid aca-
demics at the senior level of the CLAHRC (Cases D,E and F).The
phenomenon of hybrid academic is subjected to more detailed
discussion in the empirical sections that follow.
Following on from Table 2, we detail the perceptions each
epistemic community has of others, and their interactions with one
another,in the three empirical sections that follow: (i) procedural
assessment criteria for translationalhealth research;(ii) perfor-
mance and resource pressures; and (iii) mediating epistemic
boundaries.
4.1.Procedural assessment criteria for translational health research
The interaction oforganisation scientists and health services
researchers is one in which the proceduralassessmentcriteria
privileged by clinician scientists are implicated. Clinician scientists
not only privilege the experimental methods, but value that
research which has practical impact upon the frontline of clinical
care. On this basis, clinician scientists disparage organisation
science:
I don't feelthe people that are in the implementation theme
from the business schoolcan possibly understand about psy-
chologicaltreatment for patients,but unless you understand
that,can you really understand the barriers and the problems
properly?
(Clinician Scientist 1,Case F)
Some clinician scientists viewed organisation scientists as
engaging in the CLAHRC initiative from a purely self-interested
position:
I think one of the issues that we have probably had has been
trying to get the researchers closer and more supportive to the
groups, rather than just seeing them as experiments. However, I
think the business schoolhere has adopted a position that is
very much ‘we are doing the research and we will let you know
when there is stuff to know’,whereas we want more regular
feedback.We want feedback so that if they have got learning
that we need to know,but we are not learning later when we
can do nothing about it.
(Clinician Scientist 1,Case G)
Table 2
Comparative cases.
Case Research
ranking
Collaboration with
organisation scientists
Involvement of senior
level academic hybrid
Interaction between organisation scientists & health services researchers
A Mid None No Not applicable
B High Significant No Decoupled
C Mid Limited No Decoupled
D Mid Limited Yes Organisation scientists embedded in health services research
E Mid Limited Yes Organisation scientists embedded in health services research
F Mid Significant Yes Initially decoupled but over time organisation scientists embedded in
health services research
G High Significant No Decoupled
H Mid None No Not applicable
I Low None No Not applicable
G. Currie et al./ Social Science & Medicine 114 (2014) 81e8884
going and the CLAHRC journey needs to continue,not just for
capacity building purposes,but because success has been vari-
able.For every clinicalstudy that has bridged the translation
gap, another has failed. In large part the academic side has failed
to get their act together around improvement science.
(NHS Manager 1, Case B)
Regarding our theoreticalconcerns,the last sentence in the
quote above is particularly interesting in highlighting the ‘failure’
within the academic community itselfto cohere around trans-
lational health research. Following such assertions, we examine the
epistemic gap within the academic community itself,between
organisation scientistsand health services researchers,and in
which clinician scientists are implicated.
Before presenting analysis,within Table 2, set out below,we
summarise features of our comparative CLAHRC cases,which are
relevant for our theoretical analysis.
Within Table 2, first, we provide an assessmentof research
reputation of each case,based upon the research ranking ofthe
constituentmedical schools within each CLAHRC as three-way
categorisation:(i) high (top ten per cent of medical schools as
measured by UK's Research Excellence Framework (REF),which
represents a nationalaudit of a university department's research
environment,activity and output); (ii) mid (medicalschools be-
tween the halfway point and upper decile in league tables gener-
ated by REF); and (iii) low (below the halfway point). The REF
criterion was applied a priori to select the second phase cases. Two
high ranking cases (B and G), and two medium ranking cases (C and
D), were selected. Second,we categorised the involvementof
organisation scientists from business schools in each CLAHRC as
follows: (i) no involvement; (ii) limited involvement (very limited
number of organisation scientists outside an institutional CLAHRC
partnership with a business school); and (iii) significant involve-
ment (larger number of organisation scientists encompassed
within an institutional CLAHRC partnership with a business
school). We also applied the business school involvement criterion
to select second phase cases,with Cases C and G exhibiting sig-
nificant involvement of organisation scientists,and Cases B and D,
exhibiting limited involvementof organisation scientists.Third,
induced from our data analysis, we identify the presence of hybrid
academics at the senior level of each CLAHRC.By hybrid academic
we mean those academics that have worked across,and under-
stand through,a ‘two way window’ (Llewellyn,2001) on our two
focal epistemic communities oforganisation science and health
services research. Finally, within Table 2, in terms of outcomes, we
make a qualitative judgement about whether the research carried
out by organisation scientists is either decoupled (runs in parallel)
or more integrated in translational health research,focused upon
the same health service domain within each CLAHRC. So, for
example,in Case G organisation scientists ran a study, which
focused on overall CLAHRC strategy over the five years, but did not
inform the substantive health research studies within which
clinician scientists and health services researchers collaborated.In
contrast,in case D, organisation scientists and their researchers
worked within the substantive health research studies alongside
clinician scientists and health services researchers (see later a quote
detailing this point). We note, and as evidenced in Table 2, the latter
situation,in part, may have been due to presence of hybrid aca-
demics at the senior level of the CLAHRC (Cases D,E and F).The
phenomenon of hybrid academic is subjected to more detailed
discussion in the empirical sections that follow.
Following on from Table 2, we detail the perceptions each
epistemic community has of others, and their interactions with one
another,in the three empirical sections that follow: (i) procedural
assessment criteria for translationalhealth research;(ii) perfor-
mance and resource pressures; and (iii) mediating epistemic
boundaries.
4.1.Procedural assessment criteria for translational health research
The interaction oforganisation scientists and health services
researchers is one in which the proceduralassessmentcriteria
privileged by clinician scientists are implicated. Clinician scientists
not only privilege the experimental methods, but value that
research which has practical impact upon the frontline of clinical
care. On this basis, clinician scientists disparage organisation
science:
I don't feelthe people that are in the implementation theme
from the business schoolcan possibly understand about psy-
chologicaltreatment for patients,but unless you understand
that,can you really understand the barriers and the problems
properly?
(Clinician Scientist 1,Case F)
Some clinician scientists viewed organisation scientists as
engaging in the CLAHRC initiative from a purely self-interested
position:
I think one of the issues that we have probably had has been
trying to get the researchers closer and more supportive to the
groups, rather than just seeing them as experiments. However, I
think the business schoolhere has adopted a position that is
very much ‘we are doing the research and we will let you know
when there is stuff to know’,whereas we want more regular
feedback.We want feedback so that if they have got learning
that we need to know,but we are not learning later when we
can do nothing about it.
(Clinician Scientist 1,Case G)
Table 2
Comparative cases.
Case Research
ranking
Collaboration with
organisation scientists
Involvement of senior
level academic hybrid
Interaction between organisation scientists & health services researchers
A Mid None No Not applicable
B High Significant No Decoupled
C Mid Limited No Decoupled
D Mid Limited Yes Organisation scientists embedded in health services research
E Mid Limited Yes Organisation scientists embedded in health services research
F Mid Significant Yes Initially decoupled but over time organisation scientists embedded in
health services research
G High Significant No Decoupled
H Mid None No Not applicable
I Low None No Not applicable
G. Currie et al./ Social Science & Medicine 114 (2014) 81e8884
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
The response of organisation scientists is ambivalent towards
criticism by clinician scientists.Indeed they might be seen to dis-
tance themselves from the research endeavours of clinician scien-
tists through orientating towards a distinct procedural assessment
criteria,which privileges more theoretical research:
I think they (clinician scientists)expected thatthe business
school might facilitate their work,rather than come up with
work of their own. However, we want to understand the
organisational processes around knowledge sharing, not
necessarily to push along their research […] they don't under-
stand this area of scholarship […] I really don't feel understood
by the clinical community.What we want to do is to concep-
tualise and generate theory,rather than tell them how they
should do it.
(Organisation Scientist 1,Case B)
At the same time,organisation scientists criticise those experi-
mental methods privileged by clinician scientists,with the latter
seeking to defend their expertise:
It does annoy me how [the respondent is focussing upon orga-
nisation scientists at this point in the interview], social sciences
come along and criticise randomised controltrials, which is
something they don't know a lot about. So they come along and
say blah,blah,blah,about randomised control trials and I just
know they are talking rubbish.They don't understand what
randomised controltrials do. I feel that the current sway of
those (social) sciences is undervaluing clinicalscience and is
likely, if we continue to do that it is likely to drive away and
offend an awful lot of clinical researchers.
(Clinician Scientist 1,Case D)
In contrast,unlike organisation scientists,whilst they may not
enact experimental methods, health services researchers take their
cue from clinician scientists in privileging impact upon the front-
line of clinical delivery, something they claim their own research is
set up to realise:
I see the NHS as a place to do research. For me personally I see it
as a place to make a difference to patient care and I think that
does come from my roots you know, that I actually want to be in
there doing it and the research is part and parcel of that. I don't
just want to go in and do it at a distance you know,observe or
contribute at a distance,develop new theoreticalinsights but
then don't have a commitment to then apply what they know in
a very practical way to make a difference.
(Health Services Researcher 1,Case E)
But, health services researchers claim that organisation scien-
tists are not set up to realise such practical impact. Health services
researchers commented upon opportunistic behaviourof some
organisation scientists working in business schools:
They don't engage with the health service audience because
they’re engaged in developing esoteric theory first and fore-
most, for academic business and managementjournals. The
health service is just a case study,whereas for me, I guess
traditionally I would have been the opposite because I'm trying
to fix healthcare problems. If all the funding for health services
research dried up,business and managementwouldn't care,
they'd move on to wherever the next funding would be.
(Health Services Researcher 1,Case I)
However,our study suggests the practical impact of organisa-
tion scientists may lie less in the domain of clinical delivery,and
more in the domain of healthcare management.The practice
epistemic community to which organisation scientists relate is that
of NHS managers. Indeed, organisation scientistsperceived a
greater receptivity towards their translational research from NHS
managers, as compared to other scientific epistemic communities:
When I go along to present leadership or knowledge manage-
ment at one of our healthcare partners, I am guaranteed a much
more favourable reception from their managers than from my
clinical science collaborators.
(Organisation Scientist 2,Case F)
Notwithstanding those organisation scientists more orientated
towards theory generation,some were concerned to draw health-
care practitioners into their research,and consider the organisa-
tional and managerialimplications associated with translational
health research:
I think the words should be knowledge exchange,not knowl-
edge transfer.I am being rather pedantic because knowledge
transfer infers that we,the clever people in the university who
are doing research,know the answers and you the silly practi-
tioners who are out there doing it need to learn from us and I
don't accept that. I think what I would say is we are not driven
by the practitioners,but we are engaging the practitioners.
(Organisation Scientist 2,Case C)
In the next empirical section, we consider further why tensions
exist between organisation scientists and health services
researchers.
4.2. Performance and resource pressures
Decoupling of,rather than collaborative,research across the
epistemic communities of organisationalscientists and health
services researcherswas, in part, a consequenceof coercive
pressures:
We serve the REF.And even if you have clinical academics and
social science academics, we serve different REF panels, so that
pushes us in certain directions towards peer-reviewed
publications.
(Health Services Researcher 1,Case F)
Being pushed in a particular publication trajectory appeared
very significant for organisation scientists:
We are bound by an institutionalised list of journals, developed
by Association of Business Schools. These are graded from high,
four star, to low quality, no or one star. In this respect, we are a
bit more constrained than others.I could publish in the top
clinical journal and it wouldn't count in a business school.
Health services researchers,meanwhile,seem more able to
publish in clinical journals,but these seem the lower quality
ones as judged by clinical academics
(Organisation Scientist 1,Case B).
The more coercive influences that caused epistemic commu-
nities to diverge were buttressed by normative forces. Each
epistemic community viewed the language of the others as opaque:
G. Currie et al./ Social Science & Medicine 114 (2014) 81e88 85
criticism by clinician scientists.Indeed they might be seen to dis-
tance themselves from the research endeavours of clinician scien-
tists through orientating towards a distinct procedural assessment
criteria,which privileges more theoretical research:
I think they (clinician scientists)expected thatthe business
school might facilitate their work,rather than come up with
work of their own. However, we want to understand the
organisational processes around knowledge sharing, not
necessarily to push along their research […] they don't under-
stand this area of scholarship […] I really don't feel understood
by the clinical community.What we want to do is to concep-
tualise and generate theory,rather than tell them how they
should do it.
(Organisation Scientist 1,Case B)
At the same time,organisation scientists criticise those experi-
mental methods privileged by clinician scientists,with the latter
seeking to defend their expertise:
It does annoy me how [the respondent is focussing upon orga-
nisation scientists at this point in the interview], social sciences
come along and criticise randomised controltrials, which is
something they don't know a lot about. So they come along and
say blah,blah,blah,about randomised control trials and I just
know they are talking rubbish.They don't understand what
randomised controltrials do. I feel that the current sway of
those (social) sciences is undervaluing clinicalscience and is
likely, if we continue to do that it is likely to drive away and
offend an awful lot of clinical researchers.
(Clinician Scientist 1,Case D)
In contrast,unlike organisation scientists,whilst they may not
enact experimental methods, health services researchers take their
cue from clinician scientists in privileging impact upon the front-
line of clinical delivery, something they claim their own research is
set up to realise:
I see the NHS as a place to do research. For me personally I see it
as a place to make a difference to patient care and I think that
does come from my roots you know, that I actually want to be in
there doing it and the research is part and parcel of that. I don't
just want to go in and do it at a distance you know,observe or
contribute at a distance,develop new theoreticalinsights but
then don't have a commitment to then apply what they know in
a very practical way to make a difference.
(Health Services Researcher 1,Case E)
But, health services researchers claim that organisation scien-
tists are not set up to realise such practical impact. Health services
researchers commented upon opportunistic behaviourof some
organisation scientists working in business schools:
They don't engage with the health service audience because
they’re engaged in developing esoteric theory first and fore-
most, for academic business and managementjournals. The
health service is just a case study,whereas for me, I guess
traditionally I would have been the opposite because I'm trying
to fix healthcare problems. If all the funding for health services
research dried up,business and managementwouldn't care,
they'd move on to wherever the next funding would be.
(Health Services Researcher 1,Case I)
However,our study suggests the practical impact of organisa-
tion scientists may lie less in the domain of clinical delivery,and
more in the domain of healthcare management.The practice
epistemic community to which organisation scientists relate is that
of NHS managers. Indeed, organisation scientistsperceived a
greater receptivity towards their translational research from NHS
managers, as compared to other scientific epistemic communities:
When I go along to present leadership or knowledge manage-
ment at one of our healthcare partners, I am guaranteed a much
more favourable reception from their managers than from my
clinical science collaborators.
(Organisation Scientist 2,Case F)
Notwithstanding those organisation scientists more orientated
towards theory generation,some were concerned to draw health-
care practitioners into their research,and consider the organisa-
tional and managerialimplications associated with translational
health research:
I think the words should be knowledge exchange,not knowl-
edge transfer.I am being rather pedantic because knowledge
transfer infers that we,the clever people in the university who
are doing research,know the answers and you the silly practi-
tioners who are out there doing it need to learn from us and I
don't accept that. I think what I would say is we are not driven
by the practitioners,but we are engaging the practitioners.
(Organisation Scientist 2,Case C)
In the next empirical section, we consider further why tensions
exist between organisation scientists and health services
researchers.
4.2. Performance and resource pressures
Decoupling of,rather than collaborative,research across the
epistemic communities of organisationalscientists and health
services researcherswas, in part, a consequenceof coercive
pressures:
We serve the REF.And even if you have clinical academics and
social science academics, we serve different REF panels, so that
pushes us in certain directions towards peer-reviewed
publications.
(Health Services Researcher 1,Case F)
Being pushed in a particular publication trajectory appeared
very significant for organisation scientists:
We are bound by an institutionalised list of journals, developed
by Association of Business Schools. These are graded from high,
four star, to low quality, no or one star. In this respect, we are a
bit more constrained than others.I could publish in the top
clinical journal and it wouldn't count in a business school.
Health services researchers,meanwhile,seem more able to
publish in clinical journals,but these seem the lower quality
ones as judged by clinical academics
(Organisation Scientist 1,Case B).
The more coercive influences that caused epistemic commu-
nities to diverge were buttressed by normative forces. Each
epistemic community viewed the language of the others as opaque:
G. Currie et al./ Social Science & Medicine 114 (2014) 81e88 85
They [clinician scientists and health services researchers] look at
me askance and have accused me of management “greyspeak”.
“Greyspeak”,what about their impenetrable clinical language?
(Organisation Scientist 1,Case E)
Reflecting upon analysisof organisation scientists'practical
impact (they may well have practical impact,but which relates to
management rather than clinical practice),we view any claims of
one epistemic community about others as being political in nature.
The political nature of the claims appeared particularly significant
between health services researchers and organisation scientists.
Indeed at a dissemination event organised by one of the research
teams commissioned to externally evaluate CLAHRCs (held in a
business school,with two presenting research teams,both led by
organisation scientists), there were heated exchanges between one
health services researcher and one organisation scientist. The latter
claimed that the type of applied research in CLAHRCs proved
difficult to publish and might be career limiting,whilst the latter
suggested that organisation scientists added little value to trans-
lational research.Reflecting some of the politics around such ar-
guments,one health services researcher admitted thathe was
dependent upon clinician scientists for resource:
We hang on the coat tails of clinical academics,feed on scraps
from their table. They obtain multi-million pound grants and we
sidle up to them for a few hundred thousand pounds, big money
for us,but small money to them.
(Health Services Researcher 1,Case F).
An organisation scientist, working alongside the aforementioned
health services researcher in Case F, suggested that, given the above,
‘other social scientists may resist intrusion by business schools upon
what they perceive as their “turf”,but it is mainly on the basis we
threaten to take the money’ (Organisation Scientist 2, Case F).
One organisation scientist in Case G,however,admitted that his
interaction with the clinician scientists was for similar reasons of
gaining resource.His interaction took place mainly during bid
development, and that following award of funding, he stated that “we
went our own way” (Organisation Scientist 1, Case G). Interestingly, his
team had only recently started interacting with clinician scientists
again as the bid for re-financing of CLAHRCs was developed in 2013.
Within Case G, organisation science research was effectively decou-
pled from the main thrust of CLAHRC activity,reflecting epistemic
boundaries. Organisation scientists worked in parallel with clinician
scientist led research, within which health services researchers were
embedded.Such arrangementsappeared a pragmatic way to
accommodate different perspectives upon translational research.
4.3. Mediating epistemic boundaries
There are two levels at which epistemic gaps might be mediated
through intervention. First, policy-makers might intervene to
encourage the mediation of epistemic gaps through shaping
existing institutions:
You have to align the institutional arrangement,not the in-
dividuals.You have to align the incentive structures and the
regulatory systems
(Health Services Researcher 1,Case G)
To some extent,at least in the UK's research performance sys-
tem, high level changes are occurring. Government policy towards
research in the UK increasingly emphasises pathway to impact
upon practice of academic research.The regular assessmentof
research performance via the REF, from which government funding
flows, not only examines academicpublications and research
environment in university departments, but also examines cases of
practicalimpact in each university department.We suggest that
such a policy change might break down epistemic boundaries,
given the pathway to impact is likely to require collaboration across
academic communities:
We're thinking about REF impact cases now and the journey
from idea to implementation.You're very aware of the need to
show to produce things and show artefacts that could be used
locally and come up with products that could be disseminated.
This requires we engage with the knowledge that departments,
such as business schools,have.
(Clinician Scientist 1,Case C)
Examining how epistemic cleavages might be mediated, we also
note,where health services researchers lead the implementation
theme,that they appear more likely to work into the substantive
clinical science themes to a greater extent,and indeed may be
subsumed by clinical science:
Health services researchers are able to work better with clinical
academics because we work within the same clinical domain. So
if you’re a health services researcher in stroke,you'd probably
have very close connections with consultants in the field of
stroke.
(Health Services Researcher 1,Case E)
In comparison, in others, where organisation scientists lead the
implementation theme,they may end up decoupled from,and
work in parallel with,clinical themes:
The fact that there is a research strand and an implementation
strand, they’ve remained quite separate. And so the research has
been around,if I was honest,I think people's own,separate
academic research interests.
(Organisation Scientist 2,Case E)
One mechanism for mediating epistemic gaps was development
of ‘hybrid’ academics,as shown in Table 2.To some extent,we
might characterise all academics involved in CLAHRCs as exhibiting
some hybridity.Nevertheless,for some,this was more apparent,
and indeed they self-identified as such in interviews. For example,
some health services researchers were located in a business school.
One, in Case F, self-identified himself as a ‘health services
researcher’.Working within a business school and alongside
organisation scientists,he had a ‘two way window’ (Llewellyn,
2001) into the different world views held by organisation scien-
tists,as well as health services researchers; i.e.he represented an
academic hybrid.As with some other health services researchers,
this enabled him to translate across the disparate epistemic com-
munities for the benefit of the CLAHRC mission:
I wouldn't necessarily say I’ve got a business school identity. I'm
a floater in the business school and I'm a floater in the CLAHRC,
so I just float (laughs).Or hybrid you know,this sense of that I
can do this here and I can do it there and I was doing it before
joining the business school with other different projects. In ac-
ademic research terms, I can speak medical research, I can speak
health services research, which are very similar but they’re not
the same, as well as being able to speak a bit of management or
G. Currie et al./ Social Science & Medicine 114 (2014) 81e8886
me askance and have accused me of management “greyspeak”.
“Greyspeak”,what about their impenetrable clinical language?
(Organisation Scientist 1,Case E)
Reflecting upon analysisof organisation scientists'practical
impact (they may well have practical impact,but which relates to
management rather than clinical practice),we view any claims of
one epistemic community about others as being political in nature.
The political nature of the claims appeared particularly significant
between health services researchers and organisation scientists.
Indeed at a dissemination event organised by one of the research
teams commissioned to externally evaluate CLAHRCs (held in a
business school,with two presenting research teams,both led by
organisation scientists), there were heated exchanges between one
health services researcher and one organisation scientist. The latter
claimed that the type of applied research in CLAHRCs proved
difficult to publish and might be career limiting,whilst the latter
suggested that organisation scientists added little value to trans-
lational research.Reflecting some of the politics around such ar-
guments,one health services researcher admitted thathe was
dependent upon clinician scientists for resource:
We hang on the coat tails of clinical academics,feed on scraps
from their table. They obtain multi-million pound grants and we
sidle up to them for a few hundred thousand pounds, big money
for us,but small money to them.
(Health Services Researcher 1,Case F).
An organisation scientist, working alongside the aforementioned
health services researcher in Case F, suggested that, given the above,
‘other social scientists may resist intrusion by business schools upon
what they perceive as their “turf”,but it is mainly on the basis we
threaten to take the money’ (Organisation Scientist 2, Case F).
One organisation scientist in Case G,however,admitted that his
interaction with the clinician scientists was for similar reasons of
gaining resource.His interaction took place mainly during bid
development, and that following award of funding, he stated that “we
went our own way” (Organisation Scientist 1, Case G). Interestingly, his
team had only recently started interacting with clinician scientists
again as the bid for re-financing of CLAHRCs was developed in 2013.
Within Case G, organisation science research was effectively decou-
pled from the main thrust of CLAHRC activity,reflecting epistemic
boundaries. Organisation scientists worked in parallel with clinician
scientist led research, within which health services researchers were
embedded.Such arrangementsappeared a pragmatic way to
accommodate different perspectives upon translational research.
4.3. Mediating epistemic boundaries
There are two levels at which epistemic gaps might be mediated
through intervention. First, policy-makers might intervene to
encourage the mediation of epistemic gaps through shaping
existing institutions:
You have to align the institutional arrangement,not the in-
dividuals.You have to align the incentive structures and the
regulatory systems
(Health Services Researcher 1,Case G)
To some extent,at least in the UK's research performance sys-
tem, high level changes are occurring. Government policy towards
research in the UK increasingly emphasises pathway to impact
upon practice of academic research.The regular assessmentof
research performance via the REF, from which government funding
flows, not only examines academicpublications and research
environment in university departments, but also examines cases of
practicalimpact in each university department.We suggest that
such a policy change might break down epistemic boundaries,
given the pathway to impact is likely to require collaboration across
academic communities:
We're thinking about REF impact cases now and the journey
from idea to implementation.You're very aware of the need to
show to produce things and show artefacts that could be used
locally and come up with products that could be disseminated.
This requires we engage with the knowledge that departments,
such as business schools,have.
(Clinician Scientist 1,Case C)
Examining how epistemic cleavages might be mediated, we also
note,where health services researchers lead the implementation
theme,that they appear more likely to work into the substantive
clinical science themes to a greater extent,and indeed may be
subsumed by clinical science:
Health services researchers are able to work better with clinical
academics because we work within the same clinical domain. So
if you’re a health services researcher in stroke,you'd probably
have very close connections with consultants in the field of
stroke.
(Health Services Researcher 1,Case E)
In comparison, in others, where organisation scientists lead the
implementation theme,they may end up decoupled from,and
work in parallel with,clinical themes:
The fact that there is a research strand and an implementation
strand, they’ve remained quite separate. And so the research has
been around,if I was honest,I think people's own,separate
academic research interests.
(Organisation Scientist 2,Case E)
One mechanism for mediating epistemic gaps was development
of ‘hybrid’ academics,as shown in Table 2.To some extent,we
might characterise all academics involved in CLAHRCs as exhibiting
some hybridity.Nevertheless,for some,this was more apparent,
and indeed they self-identified as such in interviews. For example,
some health services researchers were located in a business school.
One, in Case F, self-identified himself as a ‘health services
researcher’.Working within a business school and alongside
organisation scientists,he had a ‘two way window’ (Llewellyn,
2001) into the different world views held by organisation scien-
tists,as well as health services researchers; i.e.he represented an
academic hybrid.As with some other health services researchers,
this enabled him to translate across the disparate epistemic com-
munities for the benefit of the CLAHRC mission:
I wouldn't necessarily say I’ve got a business school identity. I'm
a floater in the business school and I'm a floater in the CLAHRC,
so I just float (laughs).Or hybrid you know,this sense of that I
can do this here and I can do it there and I was doing it before
joining the business school with other different projects. In ac-
ademic research terms, I can speak medical research, I can speak
health services research, which are very similar but they’re not
the same, as well as being able to speak a bit of management or
G. Currie et al./ Social Science & Medicine 114 (2014) 81e8886
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
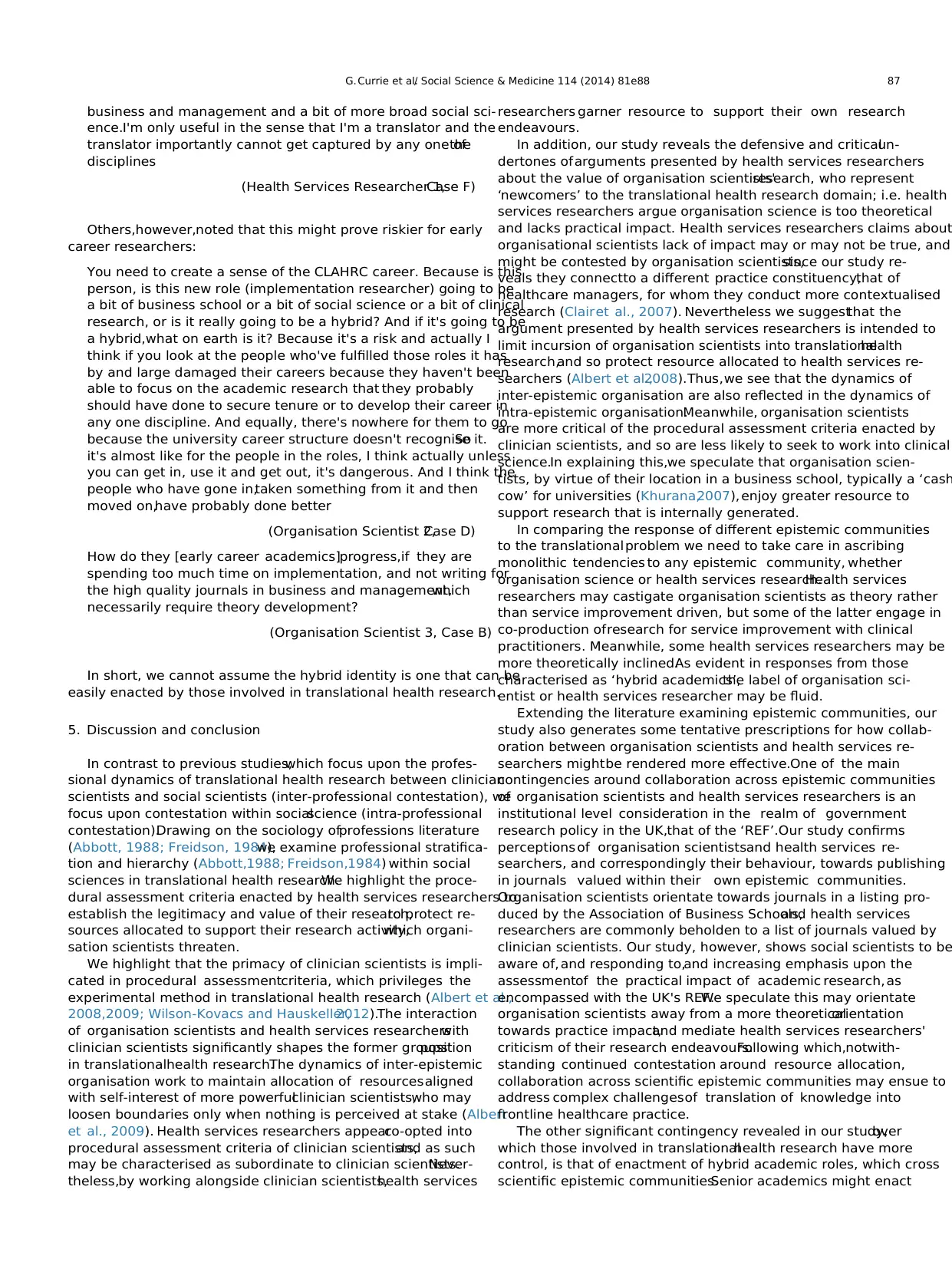
business and management and a bit of more broad social sci-
ence.I'm only useful in the sense that I'm a translator and the
translator importantly cannot get captured by any one ofthe
disciplines
(Health Services Researcher 1,Case F)
Others,however,noted that this might prove riskier for early
career researchers:
You need to create a sense of the CLAHRC career. Because is this
person, is this new role (implementation researcher) going to be
a bit of business school or a bit of social science or a bit of clinical
research, or is it really going to be a hybrid? And if it's going to be
a hybrid,what on earth is it? Because it's a risk and actually I
think if you look at the people who've fulfilled those roles it has
by and large damaged their careers because they haven't been
able to focus on the academic research that they probably
should have done to secure tenure or to develop their career in
any one discipline. And equally, there's nowhere for them to go
because the university career structure doesn't recognise it.So
it's almost like for the people in the roles, I think actually unless
you can get in, use it and get out, it's dangerous. And I think the
people who have gone in,taken something from it and then
moved on,have probably done better
(Organisation Scientist 2,Case D)
How do they [early career academics]progress,if they are
spending too much time on implementation, and not writing for
the high quality journals in business and management,which
necessarily require theory development?
(Organisation Scientist 3, Case B)
In short, we cannot assume the hybrid identity is one that can be
easily enacted by those involved in translational health research.
5. Discussion and conclusion
In contrast to previous studies,which focus upon the profes-
sional dynamics of translational health research between clinician
scientists and social scientists (inter-professional contestation), we
focus upon contestation within socialscience (intra-professional
contestation).Drawing on the sociology ofprofessions literature
(Abbott, 1988; Freidson, 1984),we examine professional stratifica-
tion and hierarchy (Abbott,1988; Freidson,1984) within social
sciences in translational health research.We highlight the proce-
dural assessment criteria enacted by health services researchers to
establish the legitimacy and value of their research,to protect re-
sources allocated to support their research activity,which organi-
sation scientists threaten.
We highlight that the primacy of clinician scientists is impli-
cated in procedural assessmentcriteria, which privileges the
experimental method in translational health research (Albert et al.,
2008,2009; Wilson-Kovacs and Hauskeller,2012).The interaction
of organisation scientists and health services researcherswith
clinician scientists significantly shapes the former groups'position
in translationalhealth research.The dynamics of inter-epistemic
organisation work to maintain allocation of resourcesaligned
with self-interest of more powerfulclinician scientists,who may
loosen boundaries only when nothing is perceived at stake (Albert
et al., 2009). Health services researchers appearco-opted into
procedural assessment criteria of clinician scientists,and as such
may be characterised as subordinate to clinician scientists.Never-
theless,by working alongside clinician scientists,health services
researchers garner resource to support their own research
endeavours.
In addition, our study reveals the defensive and criticalun-
dertones ofarguments presented by health services researchers
about the value of organisation scientists'research, who represent
‘newcomers’ to the translational health research domain; i.e. health
services researchers argue organisation science is too theoretical
and lacks practical impact. Health services researchers claims about
organisational scientists lack of impact may or may not be true, and
might be contested by organisation scientists,since our study re-
veals they connectto a different practice constituency,that of
healthcare managers, for whom they conduct more contextualised
research (Clairet al., 2007). Nevertheless we suggestthat the
argument presented by health services researchers is intended to
limit incursion of organisation scientists into translationalhealth
research,and so protect resource allocated to health services re-
searchers (Albert et al.,2008).Thus,we see that the dynamics of
inter-epistemic organisation are also reflected in the dynamics of
intra-epistemic organisation.Meanwhile, organisation scientists
are more critical of the procedural assessment criteria enacted by
clinician scientists, and so are less likely to seek to work into clinical
science.In explaining this,we speculate that organisation scien-
tists, by virtue of their location in a business school, typically a ‘cash
cow’ for universities (Khurana,2007), enjoy greater resource to
support research that is internally generated.
In comparing the response of different epistemic communities
to the translationalproblem we need to take care in ascribing
monolithic tendencies to any epistemic community, whether
organisation science or health services research.Health services
researchers may castigate organisation scientists as theory rather
than service improvement driven, but some of the latter engage in
co-production ofresearch for service improvement with clinical
practitioners. Meanwhile, some health services researchers may be
more theoretically inclined.As evident in responses from those
characterised as ‘hybrid academics’,the label of organisation sci-
entist or health services researcher may be fluid.
Extending the literature examining epistemic communities, our
study also generates some tentative prescriptions for how collab-
oration between organisation scientists and health services re-
searchers mightbe rendered more effective.One of the main
contingencies around collaboration across epistemic communities
of organisation scientists and health services researchers is an
institutional level consideration in the realm of government
research policy in the UK,that of the ‘REF’.Our study confirms
perceptions of organisation scientistsand health services re-
searchers, and correspondingly their behaviour, towards publishing
in journals valued within their own epistemic communities.
Organisation scientists orientate towards journals in a listing pro-
duced by the Association of Business Schools,and health services
researchers are commonly beholden to a list of journals valued by
clinician scientists. Our study, however, shows social scientists to be
aware of, and responding to,and increasing emphasis upon the
assessmentof the practical impact of academic research, as
encompassed with the UK's REF.We speculate this may orientate
organisation scientists away from a more theoreticalorientation
towards practice impact,and mediate health services researchers'
criticism of their research endeavours.Following which,notwith-
standing continued contestation around resource allocation,
collaboration across scientific epistemic communities may ensue to
address complex challengesof translation of knowledge into
frontline healthcare practice.
The other significant contingency revealed in our study,over
which those involved in translationalhealth research have more
control, is that of enactment of hybrid academic roles, which cross
scientific epistemic communities.Senior academics might enact
G. Currie et al./ Social Science & Medicine 114 (2014) 81e88 87
ence.I'm only useful in the sense that I'm a translator and the
translator importantly cannot get captured by any one ofthe
disciplines
(Health Services Researcher 1,Case F)
Others,however,noted that this might prove riskier for early
career researchers:
You need to create a sense of the CLAHRC career. Because is this
person, is this new role (implementation researcher) going to be
a bit of business school or a bit of social science or a bit of clinical
research, or is it really going to be a hybrid? And if it's going to be
a hybrid,what on earth is it? Because it's a risk and actually I
think if you look at the people who've fulfilled those roles it has
by and large damaged their careers because they haven't been
able to focus on the academic research that they probably
should have done to secure tenure or to develop their career in
any one discipline. And equally, there's nowhere for them to go
because the university career structure doesn't recognise it.So
it's almost like for the people in the roles, I think actually unless
you can get in, use it and get out, it's dangerous. And I think the
people who have gone in,taken something from it and then
moved on,have probably done better
(Organisation Scientist 2,Case D)
How do they [early career academics]progress,if they are
spending too much time on implementation, and not writing for
the high quality journals in business and management,which
necessarily require theory development?
(Organisation Scientist 3, Case B)
In short, we cannot assume the hybrid identity is one that can be
easily enacted by those involved in translational health research.
5. Discussion and conclusion
In contrast to previous studies,which focus upon the profes-
sional dynamics of translational health research between clinician
scientists and social scientists (inter-professional contestation), we
focus upon contestation within socialscience (intra-professional
contestation).Drawing on the sociology ofprofessions literature
(Abbott, 1988; Freidson, 1984),we examine professional stratifica-
tion and hierarchy (Abbott,1988; Freidson,1984) within social
sciences in translational health research.We highlight the proce-
dural assessment criteria enacted by health services researchers to
establish the legitimacy and value of their research,to protect re-
sources allocated to support their research activity,which organi-
sation scientists threaten.
We highlight that the primacy of clinician scientists is impli-
cated in procedural assessmentcriteria, which privileges the
experimental method in translational health research (Albert et al.,
2008,2009; Wilson-Kovacs and Hauskeller,2012).The interaction
of organisation scientists and health services researcherswith
clinician scientists significantly shapes the former groups'position
in translationalhealth research.The dynamics of inter-epistemic
organisation work to maintain allocation of resourcesaligned
with self-interest of more powerfulclinician scientists,who may
loosen boundaries only when nothing is perceived at stake (Albert
et al., 2009). Health services researchers appearco-opted into
procedural assessment criteria of clinician scientists,and as such
may be characterised as subordinate to clinician scientists.Never-
theless,by working alongside clinician scientists,health services
researchers garner resource to support their own research
endeavours.
In addition, our study reveals the defensive and criticalun-
dertones ofarguments presented by health services researchers
about the value of organisation scientists'research, who represent
‘newcomers’ to the translational health research domain; i.e. health
services researchers argue organisation science is too theoretical
and lacks practical impact. Health services researchers claims about
organisational scientists lack of impact may or may not be true, and
might be contested by organisation scientists,since our study re-
veals they connectto a different practice constituency,that of
healthcare managers, for whom they conduct more contextualised
research (Clairet al., 2007). Nevertheless we suggestthat the
argument presented by health services researchers is intended to
limit incursion of organisation scientists into translationalhealth
research,and so protect resource allocated to health services re-
searchers (Albert et al.,2008).Thus,we see that the dynamics of
inter-epistemic organisation are also reflected in the dynamics of
intra-epistemic organisation.Meanwhile, organisation scientists
are more critical of the procedural assessment criteria enacted by
clinician scientists, and so are less likely to seek to work into clinical
science.In explaining this,we speculate that organisation scien-
tists, by virtue of their location in a business school, typically a ‘cash
cow’ for universities (Khurana,2007), enjoy greater resource to
support research that is internally generated.
In comparing the response of different epistemic communities
to the translationalproblem we need to take care in ascribing
monolithic tendencies to any epistemic community, whether
organisation science or health services research.Health services
researchers may castigate organisation scientists as theory rather
than service improvement driven, but some of the latter engage in
co-production ofresearch for service improvement with clinical
practitioners. Meanwhile, some health services researchers may be
more theoretically inclined.As evident in responses from those
characterised as ‘hybrid academics’,the label of organisation sci-
entist or health services researcher may be fluid.
Extending the literature examining epistemic communities, our
study also generates some tentative prescriptions for how collab-
oration between organisation scientists and health services re-
searchers mightbe rendered more effective.One of the main
contingencies around collaboration across epistemic communities
of organisation scientists and health services researchers is an
institutional level consideration in the realm of government
research policy in the UK,that of the ‘REF’.Our study confirms
perceptions of organisation scientistsand health services re-
searchers, and correspondingly their behaviour, towards publishing
in journals valued within their own epistemic communities.
Organisation scientists orientate towards journals in a listing pro-
duced by the Association of Business Schools,and health services
researchers are commonly beholden to a list of journals valued by
clinician scientists. Our study, however, shows social scientists to be
aware of, and responding to,and increasing emphasis upon the
assessmentof the practical impact of academic research, as
encompassed with the UK's REF.We speculate this may orientate
organisation scientists away from a more theoreticalorientation
towards practice impact,and mediate health services researchers'
criticism of their research endeavours.Following which,notwith-
standing continued contestation around resource allocation,
collaboration across scientific epistemic communities may ensue to
address complex challengesof translation of knowledge into
frontline healthcare practice.
The other significant contingency revealed in our study,over
which those involved in translationalhealth research have more
control, is that of enactment of hybrid academic roles, which cross
scientific epistemic communities.Senior academics might enact
G. Currie et al./ Social Science & Medicine 114 (2014) 81e88 87
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

hybrid roles within translational health research, being able to view
epistemic perspectives through the ‘two way window’ (Llewellyn,
2001) of health services research and organisation science.In do-
ing so, senior academics may be able to actas translators,or
‘knowledge brokers’, across different epistemic communities
(Lomas, 2007; Long et al., 2013). Such knowledge brokering is likely
to engender necessary understanding and appreciation of the value
of others'perspectives upon the translational problem. Within our
study, the presence of senior academics enacting hybrid roles,
across epistemic communities of organisation science and health
services research,appears to encourage greaterintegration of
organisation scientists into the translational health research
endeavour through enhancing the application of theory to practical
health services problems,whilst encouraging health services re-
searchers towards theoreticalgeneralisation.We note, however,
that this may take time and require support for sustained interac-
tion across epistemic communities (Gray,2008).Our respondents
also suggest it proves challenging for academics to develop a career
trajectory towards a hybrid role because of demands of epistemic
communities for a certain career profile; e.g. certain peer-reviewed
publications and a more practical or theoretical orientation towards
translational health research, which are valued by distinct
epistemic communities.
Finally,the question might be asked about whether epistemic
cleavages can be mediated by merely leaving organisation scientists
out of translational health research initiatives, such as CLAHRC. We
suggest that in doing so would overlook their expertise in inno-
vation and the organisational and system level problems that
pervade translation (Martin et al.,2011).In short,we argue trans-
lational initiatives need to remain pluralistin order that trans-
lational gaps can be effectively bridged, and this requires
collaboration across the scientific epistemic communities of orga-
nisation scientists and health services researchers.
Regarding further research,we suggest two ways in which our
analysis of collaboration across epistemic communities of organi-
sation scientists and health services researchers in translational
health research might be further progressed.Related to our first
contingency of research performance measurement,we recognise
our study examines translationalhealth research in a particular
national context.We encourage further research that investigates
transferability to other translational initiatives internationally.
Research needs to move beyond the English NHS and academic
context, recognising that a particularly parochial set of system level
incentives impacts the way that epistemic communities interact
within translationalhealth research (Atun,2012).Related to our
second contingency, further research might investigate how hybrid
roles are realised given the tendency for organisational scientists
and health services researchers to cohere around relatively narrow
proceduralassessmentcriteria, which might stymie career pro-
gression for those more pluralistminded members ofscientific
epistemic communities.Finally,we suggest that effective collabo-
ration is manifested in clinician scientists,health services re-
searchers,and organisation scientists working with each other
focused upon the same health service domain,rather than the
latter working in parallelwith the others.Such claims might be
subjected to greater analysis.
Acknowledgements
This paper presents independent research funded by the Na-
tional Institute for Health Research (NIHR) e NIHR HS&DR 09/1809/
1073. The views expressed are those of the authors and not
necessarily those of the NHS,NIHR or the Department of Health.
References
Abbott,A.D.,1988.The System of Professions: an Essay on the Division of Expert
Labor.University Of Chicago Press,Chicago.
Albert, M., Laberge,S., Hodges,B.D.,Regehr,G., Lingard,L., 2008.Biomedicalsci-
entists'perception of the socialsciences in health research.Soc.Sci. Med. 66
(12),2520e2531.
Albert,M., Laberge,S., Hodges,B.D.,2009.Boundary work in the health research
field: biomedical and clinician scientists'perceptions of social science research.
Minerva.Rev.Sci.Learn.Policy 47 (2), 171e194.
Atun, R., 2012. Health systems, systems thinking and innovation. Health Policy Plan.
27 (S4),iv4eiv8.
Becher,T., Trowler,P., 2001.Academic Tribes and Territories: IntellectualEnquiry
and the Culture of Disciplines.Open University Press/SHRE,Buckingham.
Bernier,N.F.,2005.Integrating politicalscience into health sciences.In: Canadian
Institutes of Health Research (Ed.),The Social Sciences and Humanities in
Health Research.CIHR,Ottawa,pp. 124e125.
Butler,D., 2008. Translationalresearch: crossing the valley ofdeath.Nature 453
(7197),84e842.
Clair,J.M., Clark,C.,Hinote,B.P.,Robinson,C.O.,Wasserman,J.A.,2007.Developing,
integrating and perpetuating new ways of applying sociology to health,med-
icine, policy,and everyday life.Soc.Sci.Med. 64 (1),248e258.
Currie, G., Dingwall, R., Kitchener,M., Waring, J., 2012. Let's dance:organiza-
tion studies, medical sociology and health policy. Soc. Sci. Med. 74 (3),
273e280.
De Villiers, J., 2005. Integrating the techniques of linguistic discourse into the health
sciences.In: Canadian Institutes of Health Research (Ed.),The SocialSciences
and Humanities in Health Research.CIHR,Ottawa,pp. 122e123.
Dussault,G., Davis, J., Gruman,J., Thorton, W., 2007.CHSRF at the Crossroads:
Capitalizing on Success e Report of the International Review Panel to the Board
of Trustees ofthe Canadian Health Services Research Foundation.Canadian
Institutes of Health Research,Ottowa,ON.
Dzau, V., Ackerly,D., Sutton-Wallace,P., Merson, M., Williams, R., Krishnan, K.,
Taber,R., Califf, R., 2010.The role of academic health science systems in the
transformation of medicine.Lancet 375 (9718),949e953.
Freidson, E., 1984. The changing nature of professional control. Annu. Rev. Sociol. 10,
1e20.
Gephart,R.P., 1993.The textual approach: risk and blame in disaster sensemaking.
Acad.Manag.J. 36 (6), 1465e1514.
Glaser,B.G.,Strauss,A.L.,1967.The Discovery of Grounded Theory: Strategies for
Qualitative Research.Aldine Publishing Company,Chicago,ILL.
Gray,B., 2008. Enhancing trans-disciplinary research through collaborative lead-
ership.Am. J. Prevent.Med. 35, S124eS132.
Graham, I., Tetroe, J., 2009. Learning from the U.S. Department of Veterans
Affairs Quality EnhancementResearch Initiative:QUERI Series.Implement.
Sci. 4 (1), 13.
Grol, R., 1997.Beliefs and evidence in changing clinicalpractice.Br. Med. J. 315,
418e421.
Khurana,R.,2007.From Higher Aims to Hired Hands: the Social Transformation of
American Business Schools and the Unfulfilled Promise of Management as a
Profession.Princeton University Press,Princeton and Oxford.
Kislov, R., Harvey,G., Walshe, K., 2011.Collaborations for Leadership in Applied
Health Research and Care: lessons from the theory of communities of practice.
Implement.Sci.6, 64.
Knorr-Cetina,K., 1999. Epistemic Cultures:How the Sciences Make Knowledge.
Harvard University Press,Cambridge,MA.
Llewellyn,S., 2001.‘Two-way windows’: clinicians as medicalmanagers.Organ.
Stud.22 (4),593e623.
Lomas,J., 2007.The in-between world of knowledge brokering.Br. Med. J. 334,
129e132.
Long, J., Cunningham,F.C.,Braithwaite,J., 2013.Bridges,brokers and boundary
spanners in collaborative networks: a systematic review. BMC Health Serv. Res.
13, 158.
Martin, G., Currie, G., Finn, R., 2009. Reconfiguring or reproducing intra-professional
boundaries? Specialist expertise, generalist knowledge and the ‘modernization’
of the medical workforce.Soc.Sci.Med. 68 (7), 1191e1198.
Martin, G., Currie, G.,Lockett, A., 2011. Prospects for knowledge exchange in health
policy and management: institutional and epistemic boundaries. J. Health Serv.
Res.Policy 16 (4),211e217.
Miles, M., Huberman, M., 1994. Qualitative Data Analysis: an Expanded Sourcebook.
Beverley Hills,London.
Nutley,S., Walter,I., Davies,H., 2007.Using Evidence: How Research Can Inform
Public Services.Policy Press,Bristol.
Pope,C.,Ziebland,S.,Mays,N., 2000.Qualitative research in health care: analysing
qualitative data.Br.Med. J. 320 (7227), 114e116.
Rowley, E., Morriss, R., Currie, G., Schneider,J., 2012. Research into practice:
Collaboration for Leadership in Applied Health Research and care (CLAHRC) for
Nottinghamshire,Derbyshire,Lincolnshire (NDL).Implement.Sci.7,40.
Wehrens,R., Bekker,M., Bal, R., 2012.Within The Netherlands,Dutch Academic
Collaborative Centres for Public Health: development through time e issues,
dilemmas and coping strategies.Evid. Policy 8 (2), 149e170.
Wilson-Kovacs,D., Hauskeller,C., 2012.The clinician-scientist:professionaldy-
namics in clinical stem cell research.Sociol.Health Illn.34 (4),497e512.
G. Currie et al./ Social Science & Medicine 114 (2014) 81e8888
epistemic perspectives through the ‘two way window’ (Llewellyn,
2001) of health services research and organisation science.In do-
ing so, senior academics may be able to actas translators,or
‘knowledge brokers’, across different epistemic communities
(Lomas, 2007; Long et al., 2013). Such knowledge brokering is likely
to engender necessary understanding and appreciation of the value
of others'perspectives upon the translational problem. Within our
study, the presence of senior academics enacting hybrid roles,
across epistemic communities of organisation science and health
services research,appears to encourage greaterintegration of
organisation scientists into the translational health research
endeavour through enhancing the application of theory to practical
health services problems,whilst encouraging health services re-
searchers towards theoreticalgeneralisation.We note, however,
that this may take time and require support for sustained interac-
tion across epistemic communities (Gray,2008).Our respondents
also suggest it proves challenging for academics to develop a career
trajectory towards a hybrid role because of demands of epistemic
communities for a certain career profile; e.g. certain peer-reviewed
publications and a more practical or theoretical orientation towards
translational health research, which are valued by distinct
epistemic communities.
Finally,the question might be asked about whether epistemic
cleavages can be mediated by merely leaving organisation scientists
out of translational health research initiatives, such as CLAHRC. We
suggest that in doing so would overlook their expertise in inno-
vation and the organisational and system level problems that
pervade translation (Martin et al.,2011).In short,we argue trans-
lational initiatives need to remain pluralistin order that trans-
lational gaps can be effectively bridged, and this requires
collaboration across the scientific epistemic communities of orga-
nisation scientists and health services researchers.
Regarding further research,we suggest two ways in which our
analysis of collaboration across epistemic communities of organi-
sation scientists and health services researchers in translational
health research might be further progressed.Related to our first
contingency of research performance measurement,we recognise
our study examines translationalhealth research in a particular
national context.We encourage further research that investigates
transferability to other translational initiatives internationally.
Research needs to move beyond the English NHS and academic
context, recognising that a particularly parochial set of system level
incentives impacts the way that epistemic communities interact
within translationalhealth research (Atun,2012).Related to our
second contingency, further research might investigate how hybrid
roles are realised given the tendency for organisational scientists
and health services researchers to cohere around relatively narrow
proceduralassessmentcriteria, which might stymie career pro-
gression for those more pluralistminded members ofscientific
epistemic communities.Finally,we suggest that effective collabo-
ration is manifested in clinician scientists,health services re-
searchers,and organisation scientists working with each other
focused upon the same health service domain,rather than the
latter working in parallelwith the others.Such claims might be
subjected to greater analysis.
Acknowledgements
This paper presents independent research funded by the Na-
tional Institute for Health Research (NIHR) e NIHR HS&DR 09/1809/
1073. The views expressed are those of the authors and not
necessarily those of the NHS,NIHR or the Department of Health.
References
Abbott,A.D.,1988.The System of Professions: an Essay on the Division of Expert
Labor.University Of Chicago Press,Chicago.
Albert, M., Laberge,S., Hodges,B.D.,Regehr,G., Lingard,L., 2008.Biomedicalsci-
entists'perception of the socialsciences in health research.Soc.Sci. Med. 66
(12),2520e2531.
Albert,M., Laberge,S., Hodges,B.D.,2009.Boundary work in the health research
field: biomedical and clinician scientists'perceptions of social science research.
Minerva.Rev.Sci.Learn.Policy 47 (2), 171e194.
Atun, R., 2012. Health systems, systems thinking and innovation. Health Policy Plan.
27 (S4),iv4eiv8.
Becher,T., Trowler,P., 2001.Academic Tribes and Territories: IntellectualEnquiry
and the Culture of Disciplines.Open University Press/SHRE,Buckingham.
Bernier,N.F.,2005.Integrating politicalscience into health sciences.In: Canadian
Institutes of Health Research (Ed.),The Social Sciences and Humanities in
Health Research.CIHR,Ottawa,pp. 124e125.
Butler,D., 2008. Translationalresearch: crossing the valley ofdeath.Nature 453
(7197),84e842.
Clair,J.M., Clark,C.,Hinote,B.P.,Robinson,C.O.,Wasserman,J.A.,2007.Developing,
integrating and perpetuating new ways of applying sociology to health,med-
icine, policy,and everyday life.Soc.Sci.Med. 64 (1),248e258.
Currie, G., Dingwall, R., Kitchener,M., Waring, J., 2012. Let's dance:organiza-
tion studies, medical sociology and health policy. Soc. Sci. Med. 74 (3),
273e280.
De Villiers, J., 2005. Integrating the techniques of linguistic discourse into the health
sciences.In: Canadian Institutes of Health Research (Ed.),The SocialSciences
and Humanities in Health Research.CIHR,Ottawa,pp. 122e123.
Dussault,G., Davis, J., Gruman,J., Thorton, W., 2007.CHSRF at the Crossroads:
Capitalizing on Success e Report of the International Review Panel to the Board
of Trustees ofthe Canadian Health Services Research Foundation.Canadian
Institutes of Health Research,Ottowa,ON.
Dzau, V., Ackerly,D., Sutton-Wallace,P., Merson, M., Williams, R., Krishnan, K.,
Taber,R., Califf, R., 2010.The role of academic health science systems in the
transformation of medicine.Lancet 375 (9718),949e953.
Freidson, E., 1984. The changing nature of professional control. Annu. Rev. Sociol. 10,
1e20.
Gephart,R.P., 1993.The textual approach: risk and blame in disaster sensemaking.
Acad.Manag.J. 36 (6), 1465e1514.
Glaser,B.G.,Strauss,A.L.,1967.The Discovery of Grounded Theory: Strategies for
Qualitative Research.Aldine Publishing Company,Chicago,ILL.
Gray,B., 2008. Enhancing trans-disciplinary research through collaborative lead-
ership.Am. J. Prevent.Med. 35, S124eS132.
Graham, I., Tetroe, J., 2009. Learning from the U.S. Department of Veterans
Affairs Quality EnhancementResearch Initiative:QUERI Series.Implement.
Sci. 4 (1), 13.
Grol, R., 1997.Beliefs and evidence in changing clinicalpractice.Br. Med. J. 315,
418e421.
Khurana,R.,2007.From Higher Aims to Hired Hands: the Social Transformation of
American Business Schools and the Unfulfilled Promise of Management as a
Profession.Princeton University Press,Princeton and Oxford.
Kislov, R., Harvey,G., Walshe, K., 2011.Collaborations for Leadership in Applied
Health Research and Care: lessons from the theory of communities of practice.
Implement.Sci.6, 64.
Knorr-Cetina,K., 1999. Epistemic Cultures:How the Sciences Make Knowledge.
Harvard University Press,Cambridge,MA.
Llewellyn,S., 2001.‘Two-way windows’: clinicians as medicalmanagers.Organ.
Stud.22 (4),593e623.
Lomas,J., 2007.The in-between world of knowledge brokering.Br. Med. J. 334,
129e132.
Long, J., Cunningham,F.C.,Braithwaite,J., 2013.Bridges,brokers and boundary
spanners in collaborative networks: a systematic review. BMC Health Serv. Res.
13, 158.
Martin, G., Currie, G., Finn, R., 2009. Reconfiguring or reproducing intra-professional
boundaries? Specialist expertise, generalist knowledge and the ‘modernization’
of the medical workforce.Soc.Sci.Med. 68 (7), 1191e1198.
Martin, G., Currie, G.,Lockett, A., 2011. Prospects for knowledge exchange in health
policy and management: institutional and epistemic boundaries. J. Health Serv.
Res.Policy 16 (4),211e217.
Miles, M., Huberman, M., 1994. Qualitative Data Analysis: an Expanded Sourcebook.
Beverley Hills,London.
Nutley,S., Walter,I., Davies,H., 2007.Using Evidence: How Research Can Inform
Public Services.Policy Press,Bristol.
Pope,C.,Ziebland,S.,Mays,N., 2000.Qualitative research in health care: analysing
qualitative data.Br.Med. J. 320 (7227), 114e116.
Rowley, E., Morriss, R., Currie, G., Schneider,J., 2012. Research into practice:
Collaboration for Leadership in Applied Health Research and care (CLAHRC) for
Nottinghamshire,Derbyshire,Lincolnshire (NDL).Implement.Sci.7,40.
Wehrens,R., Bekker,M., Bal, R., 2012.Within The Netherlands,Dutch Academic
Collaborative Centres for Public Health: development through time e issues,
dilemmas and coping strategies.Evid. Policy 8 (2), 149e170.
Wilson-Kovacs,D., Hauskeller,C., 2012.The clinician-scientist:professionaldy-
namics in clinical stem cell research.Sociol.Health Illn.34 (4),497e512.
G. Currie et al./ Social Science & Medicine 114 (2014) 81e8888
1 out of 8
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.