Hydroxyurea Treatment for Sickle Cell Anemia: Efficacy and Impact
VerifiedAdded on 2020/12/09
|15
|3028
|149
Report
AI Summary
This report provides a comprehensive literature review on the use of hydroxyurea in treating sickle cell anemia (SCA). It begins with an introduction to SCA, detailing the disease's impact on red blood cells and the resulting complications, such as vaso-occlusive crises. The review then explores the efficacy of hydroxyurea in managing SCA, including its mechanism of action in increasing fetal hemoglobin (HbF) levels and reducing pain crises. It discusses the drug's advantages, such as ease of administration and clinical effectiveness, while also addressing the limitations, particularly regarding its use in children and the potential for long-term side effects like skin hyperpigmentation and potential risks of carcinogenicity and mutagenicity. The report examines the impact of hydroxyurea on various clinical parameters, such as white blood cell counts and hemoglobin levels, and reviews the drug's impact on organ function and overall health outcomes. The report also highlights the importance of monitoring drug dosage and adherence to treatment to maximize benefits and minimize risks, concluding that while hydroxyurea offers significant benefits in SCA management, careful consideration of potential side effects and long-term impacts is crucial.
Evidence Based Medicine
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Table of Contents
INTRODUCTION...........................................................................................................................1
LITERATURE REVIEW ...............................................................................................................1
Sickle Cell Anemia (SCA)...........................................................................................................1
Hydroxyurea treatment for sickle cell .........................................................................................2
Treatment efficacy and effectiveness ..........................................................................................3
Impact of prolong usage of hydroxyurea treatment and associated limitations ..........................5
CONCLUSION ...............................................................................................................................6
REFERENCES ...............................................................................................................................8
INTRODUCTION...........................................................................................................................1
LITERATURE REVIEW ...............................................................................................................1
Sickle Cell Anemia (SCA)...........................................................................................................1
Hydroxyurea treatment for sickle cell .........................................................................................2
Treatment efficacy and effectiveness ..........................................................................................3
Impact of prolong usage of hydroxyurea treatment and associated limitations ..........................5
CONCLUSION ...............................................................................................................................6
REFERENCES ...............................................................................................................................8
INTRODUCTION
Sickle cell anemia (SCA) is known as the blood disorder which causes shape deformation
of the red blood cells. The deformation of blood cells in the shape of sickle makes them fragile
and it clogs the blood vessels. Due to the blockage oxygen transportation through blood becomes
difficult and tissue damage cause severe pain. The pain events are called vaso-occlusive
incidence or pain crises (Jones, Howard and Nevitt, 2017). Usually these are treated with pain
relief medications, blood transfusion and vigorous hydration. However, Hydroxyurea is the best
known drug for the treatment of these SCA generated pain killers. This report will provide a
literature review on the efficacy of the hydroxyurea treatment in SCA.
LITERATURE REVIEW
Sickle Cell Anemia (SCA)
According to Ware and et.al., (2017) SCA is hemoglobin disorder and can be inherited
through genes. Its major symptoms results in the abnormal shape of red blood cells (RBC) which
hinders the easy and regular flow of blood through blood vessels. Hemoglobin is the protein
pigment present in the RBC which is responsible for carrying oxygen. The sickle shaped RBC as
the result of SCA are highly vulnerable to rupture due to their increase fragility. The rupture of
blood cells leads to significant reduction in the number of RBCs and thus anemia is resulted. The
irregular sickle shaped blood cells also cause extreme pain and break down of the tissues.
As per the view of Schumacker, (2018), vulnerability of SCA also depends upon
ethnicity. Like the disease is more common among Asian and African communities as compare
to the western regions. In healthy individuals RBC are round and flexible which allows them to
easily move through blood vessels. However due to SCA these cells becomes sticky and rigid
which hinders their free movement. Piel, Steinberg and Rees, (2017) stated that the most
common symptoms of this disorder are Anemia, severe pain episodes called pain crises, frequent
infections, visionary issues and painful swelling in foot and hands. Since the sickle cells can
easily break down the deficiency of RBC also causes fatigue or even death.
The intensity of the pain crises is also severe and can cause damage to joints or bones and
ulcers if not treated properly on time. In the same context Tshilolo and et.al., (2018) argued that
the genetic mutation is the only cause for SCA thus there are no effective treatment methods for
the disorder. However recent developments such as hydroxyurea have proven to be very
1
Sickle cell anemia (SCA) is known as the blood disorder which causes shape deformation
of the red blood cells. The deformation of blood cells in the shape of sickle makes them fragile
and it clogs the blood vessels. Due to the blockage oxygen transportation through blood becomes
difficult and tissue damage cause severe pain. The pain events are called vaso-occlusive
incidence or pain crises (Jones, Howard and Nevitt, 2017). Usually these are treated with pain
relief medications, blood transfusion and vigorous hydration. However, Hydroxyurea is the best
known drug for the treatment of these SCA generated pain killers. This report will provide a
literature review on the efficacy of the hydroxyurea treatment in SCA.
LITERATURE REVIEW
Sickle Cell Anemia (SCA)
According to Ware and et.al., (2017) SCA is hemoglobin disorder and can be inherited
through genes. Its major symptoms results in the abnormal shape of red blood cells (RBC) which
hinders the easy and regular flow of blood through blood vessels. Hemoglobin is the protein
pigment present in the RBC which is responsible for carrying oxygen. The sickle shaped RBC as
the result of SCA are highly vulnerable to rupture due to their increase fragility. The rupture of
blood cells leads to significant reduction in the number of RBCs and thus anemia is resulted. The
irregular sickle shaped blood cells also cause extreme pain and break down of the tissues.
As per the view of Schumacker, (2018), vulnerability of SCA also depends upon
ethnicity. Like the disease is more common among Asian and African communities as compare
to the western regions. In healthy individuals RBC are round and flexible which allows them to
easily move through blood vessels. However due to SCA these cells becomes sticky and rigid
which hinders their free movement. Piel, Steinberg and Rees, (2017) stated that the most
common symptoms of this disorder are Anemia, severe pain episodes called pain crises, frequent
infections, visionary issues and painful swelling in foot and hands. Since the sickle cells can
easily break down the deficiency of RBC also causes fatigue or even death.
The intensity of the pain crises is also severe and can cause damage to joints or bones and
ulcers if not treated properly on time. In the same context Tshilolo and et.al., (2018) argued that
the genetic mutation is the only cause for SCA thus there are no effective treatment methods for
the disorder. However recent developments such as hydroxyurea have proven to be very
1
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
effective in managing pain and SCA associated complications like stroke, cardiovascular issues,
leg ulcers and organ damage.
The most common treatment strategies for SCA and its complications are regular intake
of pain medications, blood transfusions, medications for preventing infections and folic acid and
bone marrow transplant. McGann and Ware, (2015)elucidated that since the bone marrow
transplant depends upon the availability of the donor the most common treatment intervention is
use of hydroxyurea in which medications are given to minimise the frequency of acute chest
syndrome and pain crises. It also reduces the frequent blood transfusion needs. However, there
has been several discussions regarding long term impact of hydroxyurea which must be
evaluated for the better health outcomes.
Hydroxyurea treatment for sickle cell
According to Ware, (2015) hydroxyurea therapy enhances the production of fetal
hemoglobin (HbF) which ameliorate the intensity and severity of SCA. Thus, the dosage of
hydroxyurea influences the yield of HbF and provides good response by reducing painful crises
(Savage and et.al., 2015). As compare to the other agents for the treatment of SCA hydroxyurea
has several advantages such as easy oral administration, prevention of vaso-occlusive events,
modest toxicity profile and clinical efficacy. It can also prevent from the organ dysfunction.
However, despite having several advantages the treatment is not preferably used for the younger
people especially for children. McGann and et.al., (2016) stated that even when hydroxyurea
treatment is available the health care professionals used to avoid its use for the children due to
unexplained long term impact of therapy on individuals.
2
leg ulcers and organ damage.
The most common treatment strategies for SCA and its complications are regular intake
of pain medications, blood transfusions, medications for preventing infections and folic acid and
bone marrow transplant. McGann and Ware, (2015)elucidated that since the bone marrow
transplant depends upon the availability of the donor the most common treatment intervention is
use of hydroxyurea in which medications are given to minimise the frequency of acute chest
syndrome and pain crises. It also reduces the frequent blood transfusion needs. However, there
has been several discussions regarding long term impact of hydroxyurea which must be
evaluated for the better health outcomes.
Hydroxyurea treatment for sickle cell
According to Ware, (2015) hydroxyurea therapy enhances the production of fetal
hemoglobin (HbF) which ameliorate the intensity and severity of SCA. Thus, the dosage of
hydroxyurea influences the yield of HbF and provides good response by reducing painful crises
(Savage and et.al., 2015). As compare to the other agents for the treatment of SCA hydroxyurea
has several advantages such as easy oral administration, prevention of vaso-occlusive events,
modest toxicity profile and clinical efficacy. It can also prevent from the organ dysfunction.
However, despite having several advantages the treatment is not preferably used for the younger
people especially for children. McGann and et.al., (2016) stated that even when hydroxyurea
treatment is available the health care professionals used to avoid its use for the children due to
unexplained long term impact of therapy on individuals.
2
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
(Source: Green and Barral, 2014)
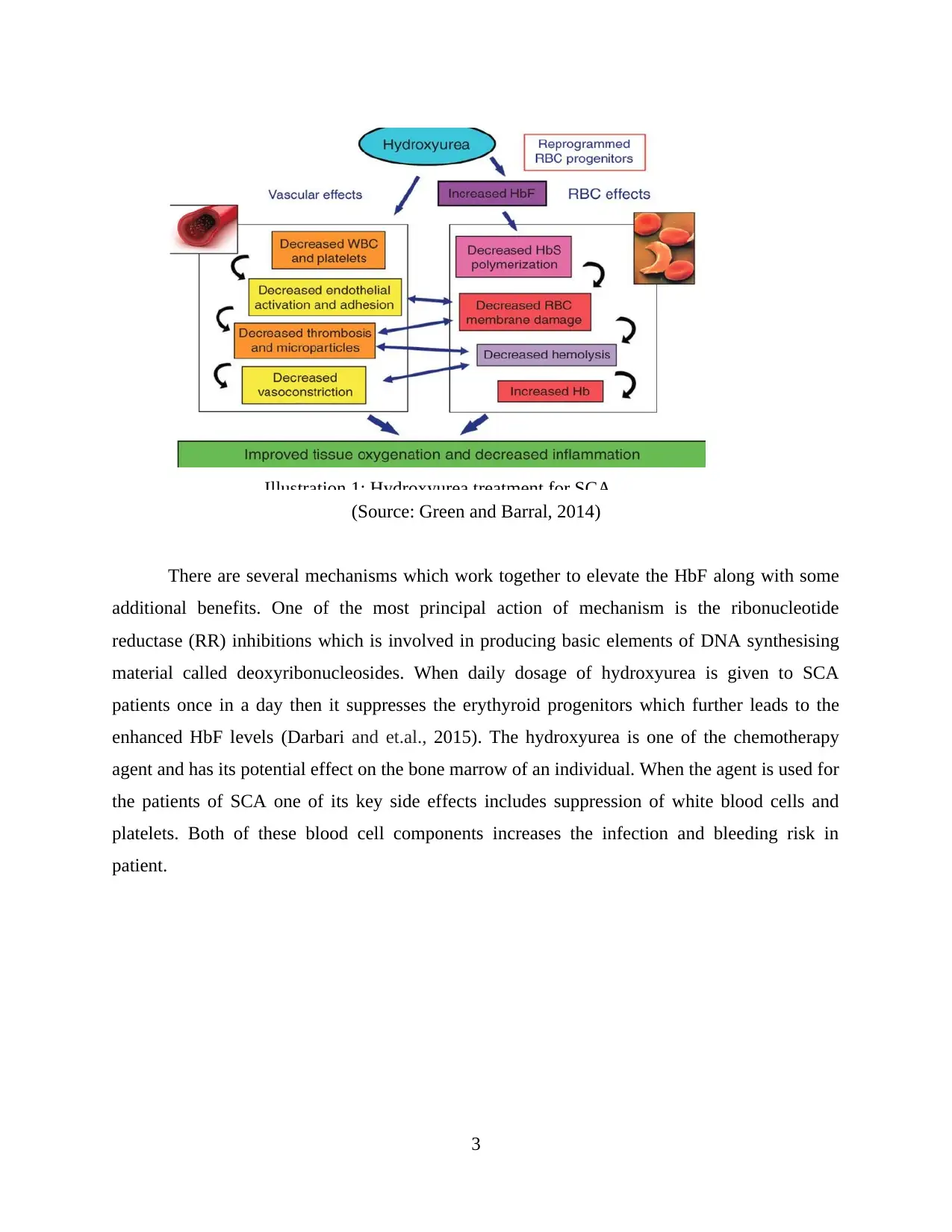
There are several mechanisms which work together to elevate the HbF along with some
additional benefits. One of the most principal action of mechanism is the ribonucleotide
reductase (RR) inhibitions which is involved in producing basic elements of DNA synthesising
material called deoxyribonucleosides. When daily dosage of hydroxyurea is given to SCA
patients once in a day then it suppresses the erythyroid progenitors which further leads to the
enhanced HbF levels (Darbari and et.al., 2015). The hydroxyurea is one of the chemotherapy
agent and has its potential effect on the bone marrow of an individual. When the agent is used for
the patients of SCA one of its key side effects includes suppression of white blood cells and
platelets. Both of these blood cell components increases the infection and bleeding risk in
patient.
3
Illustration 1: Hydroxyurea treatment for SCA
There are several mechanisms which work together to elevate the HbF along with some
additional benefits. One of the most principal action of mechanism is the ribonucleotide
reductase (RR) inhibitions which is involved in producing basic elements of DNA synthesising
material called deoxyribonucleosides. When daily dosage of hydroxyurea is given to SCA
patients once in a day then it suppresses the erythyroid progenitors which further leads to the
enhanced HbF levels (Darbari and et.al., 2015). The hydroxyurea is one of the chemotherapy
agent and has its potential effect on the bone marrow of an individual. When the agent is used for
the patients of SCA one of its key side effects includes suppression of white blood cells and
platelets. Both of these blood cell components increases the infection and bleeding risk in
patient.
3
Illustration 1: Hydroxyurea treatment for SCA
(Source: Reaching Children With Sickle Cell Anemia in Sub-Saharan Africa, 2019)
Treatment efficacy and effectiveness
The primary issue with the use of hydroxyureas is its usage in children. The drug is
advisable and prfered for only young people above 18 years of age. As per Nagalla and Ballas,
(2016) most of the research studies suggests that the drug can have possible side effect on the
development and growth phase. The hydroxyurea blocks the cell division and thus their use
among children can influence their growth stage (Tshilolo and et.al., 2018). The parameters such
as dose escalation, initiating dose, trial period and the limiting effects can influence the overall
health impact of the drug. The hydroxyurea is assumed to be effective for SCA patients due to its
multiple benefits.
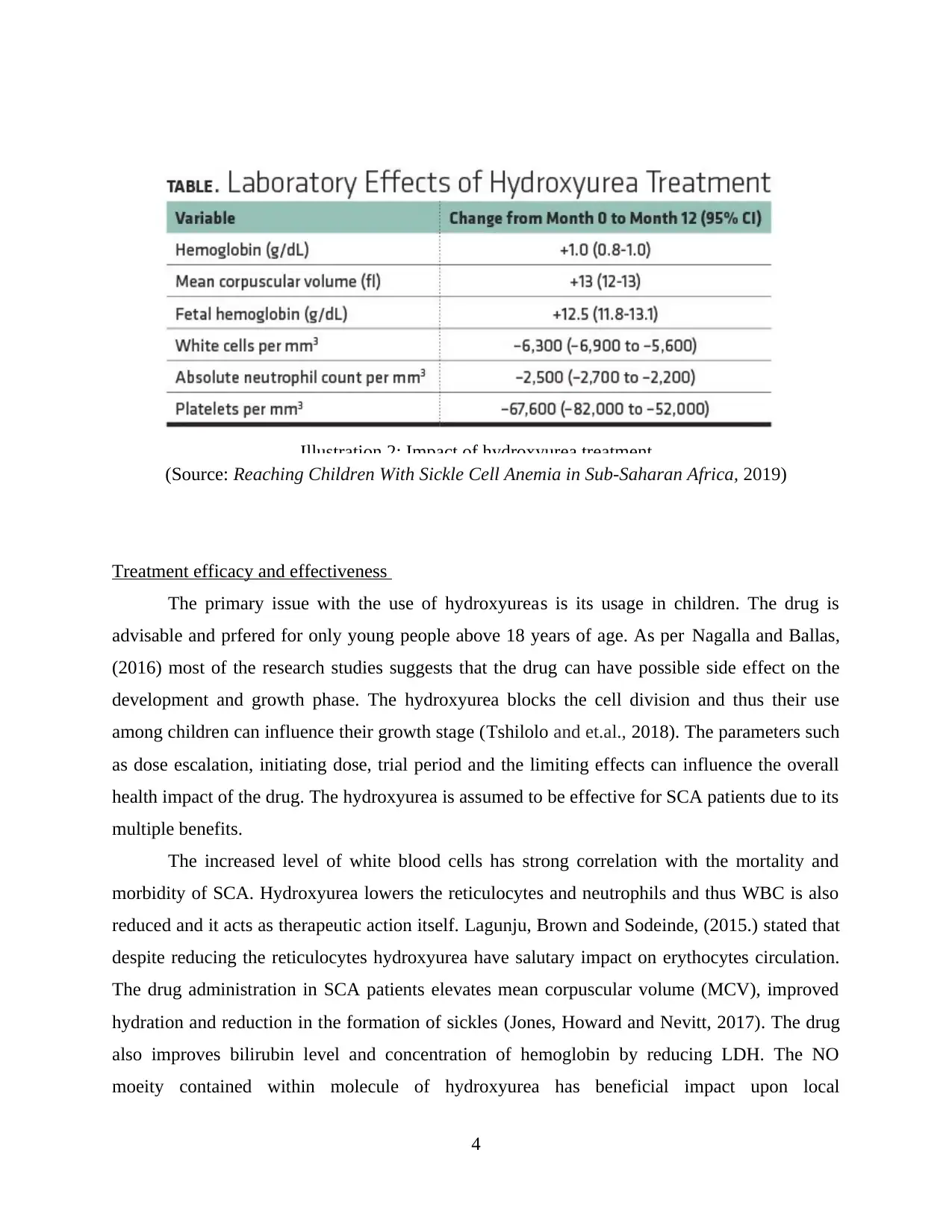
The increased level of white blood cells has strong correlation with the mortality and
morbidity of SCA. Hydroxyurea lowers the reticulocytes and neutrophils and thus WBC is also
reduced and it acts as therapeutic action itself. Lagunju, Brown and Sodeinde, (2015.) stated that
despite reducing the reticulocytes hydroxyurea have salutary impact on erythocytes circulation.
The drug administration in SCA patients elevates mean corpuscular volume (MCV), improved
hydration and reduction in the formation of sickles (Jones, Howard and Nevitt, 2017). The drug
also improves bilirubin level and concentration of hemoglobin by reducing LDH. The NO
moeity contained within molecule of hydroxyurea has beneficial impact upon local
4
Illustration 2: Impact of hydroxyurea treatment
Treatment efficacy and effectiveness
The primary issue with the use of hydroxyureas is its usage in children. The drug is
advisable and prfered for only young people above 18 years of age. As per Nagalla and Ballas,
(2016) most of the research studies suggests that the drug can have possible side effect on the
development and growth phase. The hydroxyurea blocks the cell division and thus their use
among children can influence their growth stage (Tshilolo and et.al., 2018). The parameters such
as dose escalation, initiating dose, trial period and the limiting effects can influence the overall
health impact of the drug. The hydroxyurea is assumed to be effective for SCA patients due to its
multiple benefits.
The increased level of white blood cells has strong correlation with the mortality and
morbidity of SCA. Hydroxyurea lowers the reticulocytes and neutrophils and thus WBC is also
reduced and it acts as therapeutic action itself. Lagunju, Brown and Sodeinde, (2015.) stated that
despite reducing the reticulocytes hydroxyurea have salutary impact on erythocytes circulation.
The drug administration in SCA patients elevates mean corpuscular volume (MCV), improved
hydration and reduction in the formation of sickles (Jones, Howard and Nevitt, 2017). The drug
also improves bilirubin level and concentration of hemoglobin by reducing LDH. The NO
moeity contained within molecule of hydroxyurea has beneficial impact upon local
4
Illustration 2: Impact of hydroxyurea treatment
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
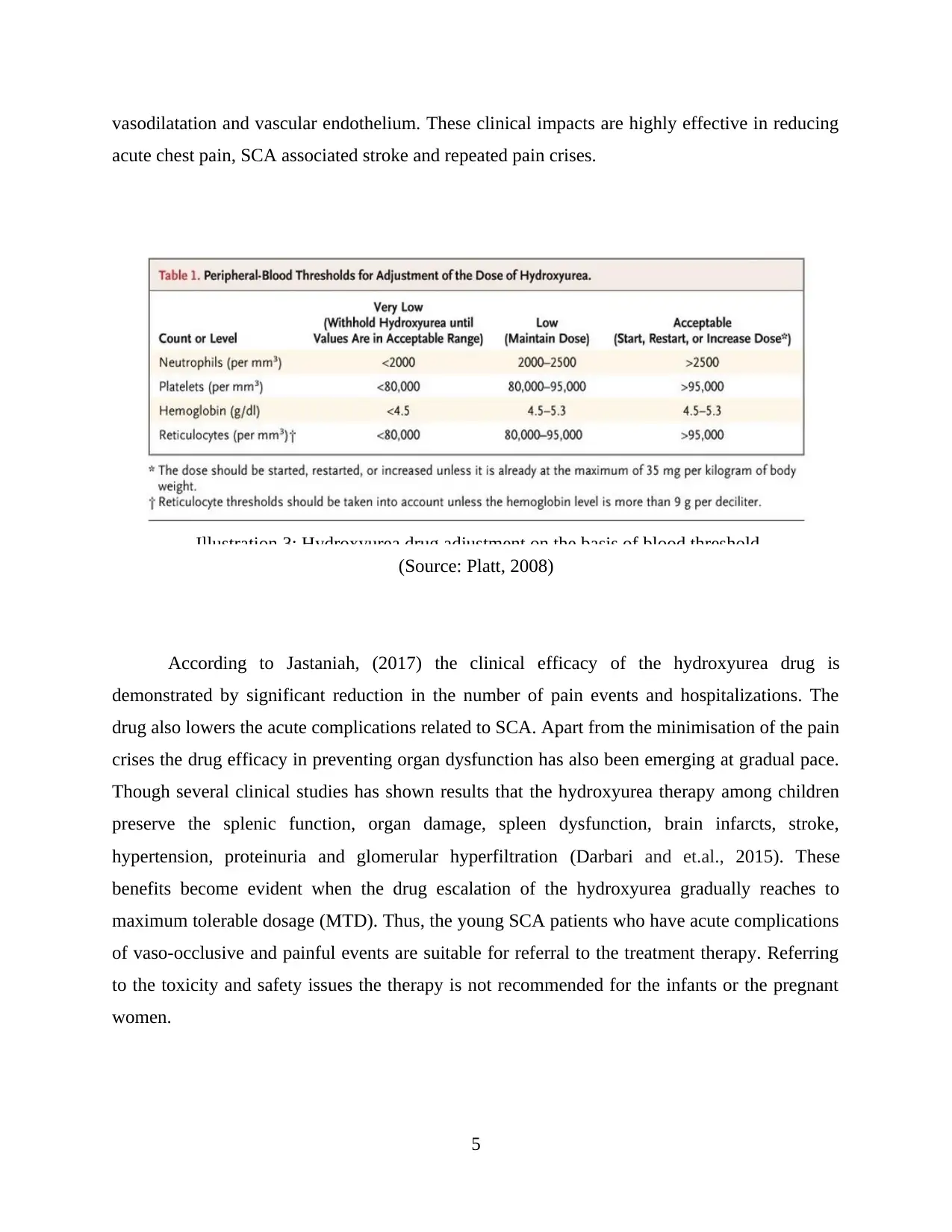
vasodilatation and vascular endothelium. These clinical impacts are highly effective in reducing
acute chest pain, SCA associated stroke and repeated pain crises.
(Source: Platt, 2008)
According to Jastaniah, (2017) the clinical efficacy of the hydroxyurea drug is
demonstrated by significant reduction in the number of pain events and hospitalizations. The
drug also lowers the acute complications related to SCA. Apart from the minimisation of the pain
crises the drug efficacy in preventing organ dysfunction has also been emerging at gradual pace.
Though several clinical studies has shown results that the hydroxyurea therapy among children
preserve the splenic function, organ damage, spleen dysfunction, brain infarcts, stroke,
hypertension, proteinuria and glomerular hyperfiltration (Darbari and et.al., 2015). These
benefits become evident when the drug escalation of the hydroxyurea gradually reaches to
maximum tolerable dosage (MTD). Thus, the young SCA patients who have acute complications
of vaso-occlusive and painful events are suitable for referral to the treatment therapy. Referring
to the toxicity and safety issues the therapy is not recommended for the infants or the pregnant
women.
5
Illustration 3: Hydroxyurea drug adjustment on the basis of blood threshold
acute chest pain, SCA associated stroke and repeated pain crises.
(Source: Platt, 2008)
According to Jastaniah, (2017) the clinical efficacy of the hydroxyurea drug is
demonstrated by significant reduction in the number of pain events and hospitalizations. The
drug also lowers the acute complications related to SCA. Apart from the minimisation of the pain
crises the drug efficacy in preventing organ dysfunction has also been emerging at gradual pace.
Though several clinical studies has shown results that the hydroxyurea therapy among children
preserve the splenic function, organ damage, spleen dysfunction, brain infarcts, stroke,
hypertension, proteinuria and glomerular hyperfiltration (Darbari and et.al., 2015). These
benefits become evident when the drug escalation of the hydroxyurea gradually reaches to
maximum tolerable dosage (MTD). Thus, the young SCA patients who have acute complications
of vaso-occlusive and painful events are suitable for referral to the treatment therapy. Referring
to the toxicity and safety issues the therapy is not recommended for the infants or the pregnant
women.
5
Illustration 3: Hydroxyurea drug adjustment on the basis of blood threshold
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Impact of prolong usage of hydroxyurea treatment and associated limitations
The hydroxyurea is also used in the treatment of other bone marrow associated disorders
or in critical conditions such as polycythemia vera. Savage and et.al., (2015) argued that
although the drug is used in lower dosage with SCA patients but still some sort of cellular
growth suppression occur. These aspects limit the drug usage among children. For avoiding these
possibilities most of the health professionals in UK tend to follow the lower dosage of drug
without reaching to maximum tolerated dosage (MTD) so that the clinical benefits can be
achieved.
Apart from the uncertainty on side effects on growth among young children there are
several effects which can be considered as mild (Jones, Howard and Nevitt, 2017). The issues
such as headache, gastrointestinal symptoms, nausea and abdominal discomfort are quite
common. The long term usage of the hydroxyurea in younger patients can also cause skin
hyperpigmentation and melanonychia. These adverse effects do not depend upon the dosage
instead these are sporadic. For the adult patients the usage of this drug can have side effect such
as skin ulcers (Jones, Howard and Nevitt, 2017).
Though the possibility is very rare but it cannot be denied. The long term usage of the
drug among adults enhances life quality and is also associated with the reduced mortality.
Contrary to the above discussion on efficacy of hydroxyurea Lanzkron and et.al., (2018) stated
that the open label hydroxyurea treatment for school going children or the young SCA patients
also leads to good development and growth without any kind of delay in sexual maturation and
other growth aspects. Hydroxyurea inhibits the replication of DNA and thus it has harmful
impact on the pregnancy and fertility issues (Sinha and et.al., 2017). Though there has not been
any documentation of impact of the treatment on fertility aspects but it has been observed in
several clinical outcomes and research studies.
As per Taylor and et.al., (2019) one of the greatest risk associated with the hydroxyurea
usage among children for long term is that there are high possibilities of development of
carcinogenicity and mutagenicity. When used for the treatment of SCA the drug has its impact
on both DNA repair and DNA synthesis. Since the DNA cannot be repaired completely with the
presence of hydroxyurea as a consequence chromosomes can be damaged and somatic mutations
can be developed. Event the short term usage of the hydroxyurea therapy can influence the blood
6
The hydroxyurea is also used in the treatment of other bone marrow associated disorders
or in critical conditions such as polycythemia vera. Savage and et.al., (2015) argued that
although the drug is used in lower dosage with SCA patients but still some sort of cellular
growth suppression occur. These aspects limit the drug usage among children. For avoiding these
possibilities most of the health professionals in UK tend to follow the lower dosage of drug
without reaching to maximum tolerated dosage (MTD) so that the clinical benefits can be
achieved.
Apart from the uncertainty on side effects on growth among young children there are
several effects which can be considered as mild (Jones, Howard and Nevitt, 2017). The issues
such as headache, gastrointestinal symptoms, nausea and abdominal discomfort are quite
common. The long term usage of the hydroxyurea in younger patients can also cause skin
hyperpigmentation and melanonychia. These adverse effects do not depend upon the dosage
instead these are sporadic. For the adult patients the usage of this drug can have side effect such
as skin ulcers (Jones, Howard and Nevitt, 2017).
Though the possibility is very rare but it cannot be denied. The long term usage of the
drug among adults enhances life quality and is also associated with the reduced mortality.
Contrary to the above discussion on efficacy of hydroxyurea Lanzkron and et.al., (2018) stated
that the open label hydroxyurea treatment for school going children or the young SCA patients
also leads to good development and growth without any kind of delay in sexual maturation and
other growth aspects. Hydroxyurea inhibits the replication of DNA and thus it has harmful
impact on the pregnancy and fertility issues (Sinha and et.al., 2017). Though there has not been
any documentation of impact of the treatment on fertility aspects but it has been observed in
several clinical outcomes and research studies.
As per Taylor and et.al., (2019) one of the greatest risk associated with the hydroxyurea
usage among children for long term is that there are high possibilities of development of
carcinogenicity and mutagenicity. When used for the treatment of SCA the drug has its impact
on both DNA repair and DNA synthesis. Since the DNA cannot be repaired completely with the
presence of hydroxyurea as a consequence chromosomes can be damaged and somatic mutations
can be developed. Event the short term usage of the hydroxyurea therapy can influence the blood
6
count (WBC reduction). Thus, it is necessary that the dosage of drug must be reviewed
periodically, usually in the intervals of 4-8 weeks.
The health professionals must assure that rapid escalation in the drug dosage can cause
hematologic toxicity which may not be apparent initially. For the short term use of the drug also
the regular analysis of blood count is recommended so that their pattern can be identified and
understood. Badawy and et.al., (2017) stated that the dosage must be increased only when
adherence to the drug can be carefully addressed otherwise it will lead to toxicity. For the better
induction of HbF the higher dosage of hydroxyurea maintained at MTD are maintained. This
approach helps to sustain the maximum value of HbF without causing any toxicity or
hematologic.
There are several short term concerns associated with the drug. For instance the impact of
the discussed oral drug are very powerful and thus taking medications at same time every day
can be effective in promoting adherence. According to Colombatti and et.al., (2018) the
treatment duration of the drug can be as long as 15-20 years among children. Most of the
paediatric SCA patients have to suffer from the long term consequences of the therapy. The
treatment can contribute to the development of cancer anecdotes however prior exposing to the
hydroxyurea treatment in SCA patients can also cause malignancy and other SCA complexities.
Thus, it has been evaluated that in short term hydroxyurea does not have any benefit or losses in
short term their long term usage can be great in improving the anemia by reducing sickled
circulation and alteration in the morphology.
CONCLUSION
It can be concluded that the daily consumption of the hydroxyurea enhances the level of
MCV, HvF and Hb while the clinical parameters such as reticulocytes, WBC and neutrophils are
decreased. These effects are helpful in improving the health outcomes of the SCA patients. It has
been also analysed from the above literature analysis that the timings and dosage of hydroxyurea
plays significant role in overall health outcomes. Thus, it is required that their its administration
must be regulated and monitored on the basis of the age and health condition of the individual.
7
periodically, usually in the intervals of 4-8 weeks.
The health professionals must assure that rapid escalation in the drug dosage can cause
hematologic toxicity which may not be apparent initially. For the short term use of the drug also
the regular analysis of blood count is recommended so that their pattern can be identified and
understood. Badawy and et.al., (2017) stated that the dosage must be increased only when
adherence to the drug can be carefully addressed otherwise it will lead to toxicity. For the better
induction of HbF the higher dosage of hydroxyurea maintained at MTD are maintained. This
approach helps to sustain the maximum value of HbF without causing any toxicity or
hematologic.
There are several short term concerns associated with the drug. For instance the impact of
the discussed oral drug are very powerful and thus taking medications at same time every day
can be effective in promoting adherence. According to Colombatti and et.al., (2018) the
treatment duration of the drug can be as long as 15-20 years among children. Most of the
paediatric SCA patients have to suffer from the long term consequences of the therapy. The
treatment can contribute to the development of cancer anecdotes however prior exposing to the
hydroxyurea treatment in SCA patients can also cause malignancy and other SCA complexities.
Thus, it has been evaluated that in short term hydroxyurea does not have any benefit or losses in
short term their long term usage can be great in improving the anemia by reducing sickled
circulation and alteration in the morphology.
CONCLUSION
It can be concluded that the daily consumption of the hydroxyurea enhances the level of
MCV, HvF and Hb while the clinical parameters such as reticulocytes, WBC and neutrophils are
decreased. These effects are helpful in improving the health outcomes of the SCA patients. It has
been also analysed from the above literature analysis that the timings and dosage of hydroxyurea
plays significant role in overall health outcomes. Thus, it is required that their its administration
must be regulated and monitored on the basis of the age and health condition of the individual.
7
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
REFERENCES
Books and Journals
Badawy, S.M. and et.al., 2017. Barriers to hydroxyurea adherence and health‐related quality of
life in adolescents and young adults with sickle cell disease. European journal of
haematology. 98(6). pp.608-614.
Boulad, F. and et.al., 2018. Safety and efficacy of plerixafor dose escalation for the mobilization
of CD34+ hematopoietic progenitor cells in patients with sickle cell disease: interim
results. Haematologica. 103(5). pp.770-777.
Colombatti, R. and et.al., 2018. Hydroxyurea prescription, availability and use for children with
sickle cell disease in Italy: Results of a National Multicenter survey. Pediatric blood &
cancer. 65(2). p.e26774.
Darbari, D.S. and et.al., 2015. Frequency of hospitalizations for pain and association with altered
brain network connectivity in sickle cell disease. The Journal of Pain. 16(11). pp.1077-
1086.
Jastaniah, W., 2017. Challenges in the management of silent cerebral infarct in sickle cell
disease. PROCEEDINGS and ABSTRACT BOOK. 102(s1). pp.30-31.
Jones, A.P., Howard, J. and Nevitt, S.J., 2017. Hydroxyurea (hydroxycarbamide) for sickle cell
disease. The Cochrane Database of Systematic Reviews. 2017(4).
Lagunju, I., Brown, B.J. and Sodeinde, O., 2015. Hydroxyurea lowers transcranial Doppler flow
velocities in children with sickle cell anaemia in a Nigerian cohort. Pediatric blood &
cancer. 62(9). pp.1587-1591.
Lanzkron, S. and et.al., 2018. Increased acute care utilization in a prospective cohort of adults
with sickle cell disease. Blood advances. 2(18). pp.2412-2417.
McGann, P.T. and et.al., 2016. Hydroxyurea therapy for children with sickle cell anemia in sub‐
saharan africa: rationale and design of the REACH trial. Pediatric blood & cancer. 63(1).
pp.98-104.
McGann, P.T. and Ware, R.E., 2015. Hydroxyurea therapy for sickle cell anemia. Expert opinion
on drug safety. 14(11). pp.1749-1758.
Nagalla, S. and Ballas, S.K., 2016. Drugs for preventing red blood cell dehydration in people
with sickle cell disease. Cochrane Database of Systematic Reviews. (3).
Piel, F.B., Steinberg, M.H. and Rees, D.C., 2017. Sickle cell disease. New England Journal of
Medicine. 376(16). pp.1561-1573.
Savage, W.J. and et.al., 2015. Evidence gaps in the management of sickle cell disease: a
summary of needed research. American journal of hematology. 90(4). pp.273-275.
Schumacker, P.T., 2018. Rescuing Decrepit Soluble Guanylate Cyclase: A Therapy for Sickle
Cell Disease?.
Sinha, C. and et.al., 2017. The Influence of the Age of Adults with Sickle Cell Disease on the
Uptake, Utilization and Efficacy of Hydroxyurea.
Taylor, C. and et.al., 2019. Combined hydroxyurea and ETA receptor blockade reduces renal
injury in the humanized sickle cell mouse. Acta Physiologica. 225(2). p.e13178.
Tshilolo, L. and et.al., 2018. Realizing Effectiveness across Continents with Hydroxyurea
(REACH): A Prospective Multi-National Trial of Hydroxyurea for Sickle Cell Anemia in
Sub-Saharan Africa.
Ware, R.E. and et.al., 2017. Sickle cell disease. The Lancet. 390(10091). pp.311-323.
Online
8
Books and Journals
Badawy, S.M. and et.al., 2017. Barriers to hydroxyurea adherence and health‐related quality of
life in adolescents and young adults with sickle cell disease. European journal of
haematology. 98(6). pp.608-614.
Boulad, F. and et.al., 2018. Safety and efficacy of plerixafor dose escalation for the mobilization
of CD34+ hematopoietic progenitor cells in patients with sickle cell disease: interim
results. Haematologica. 103(5). pp.770-777.
Colombatti, R. and et.al., 2018. Hydroxyurea prescription, availability and use for children with
sickle cell disease in Italy: Results of a National Multicenter survey. Pediatric blood &
cancer. 65(2). p.e26774.
Darbari, D.S. and et.al., 2015. Frequency of hospitalizations for pain and association with altered
brain network connectivity in sickle cell disease. The Journal of Pain. 16(11). pp.1077-
1086.
Jastaniah, W., 2017. Challenges in the management of silent cerebral infarct in sickle cell
disease. PROCEEDINGS and ABSTRACT BOOK. 102(s1). pp.30-31.
Jones, A.P., Howard, J. and Nevitt, S.J., 2017. Hydroxyurea (hydroxycarbamide) for sickle cell
disease. The Cochrane Database of Systematic Reviews. 2017(4).
Lagunju, I., Brown, B.J. and Sodeinde, O., 2015. Hydroxyurea lowers transcranial Doppler flow
velocities in children with sickle cell anaemia in a Nigerian cohort. Pediatric blood &
cancer. 62(9). pp.1587-1591.
Lanzkron, S. and et.al., 2018. Increased acute care utilization in a prospective cohort of adults
with sickle cell disease. Blood advances. 2(18). pp.2412-2417.
McGann, P.T. and et.al., 2016. Hydroxyurea therapy for children with sickle cell anemia in sub‐
saharan africa: rationale and design of the REACH trial. Pediatric blood & cancer. 63(1).
pp.98-104.
McGann, P.T. and Ware, R.E., 2015. Hydroxyurea therapy for sickle cell anemia. Expert opinion
on drug safety. 14(11). pp.1749-1758.
Nagalla, S. and Ballas, S.K., 2016. Drugs for preventing red blood cell dehydration in people
with sickle cell disease. Cochrane Database of Systematic Reviews. (3).
Piel, F.B., Steinberg, M.H. and Rees, D.C., 2017. Sickle cell disease. New England Journal of
Medicine. 376(16). pp.1561-1573.
Savage, W.J. and et.al., 2015. Evidence gaps in the management of sickle cell disease: a
summary of needed research. American journal of hematology. 90(4). pp.273-275.
Schumacker, P.T., 2018. Rescuing Decrepit Soluble Guanylate Cyclase: A Therapy for Sickle
Cell Disease?.
Sinha, C. and et.al., 2017. The Influence of the Age of Adults with Sickle Cell Disease on the
Uptake, Utilization and Efficacy of Hydroxyurea.
Taylor, C. and et.al., 2019. Combined hydroxyurea and ETA receptor blockade reduces renal
injury in the humanized sickle cell mouse. Acta Physiologica. 225(2). p.e13178.
Tshilolo, L. and et.al., 2018. Realizing Effectiveness across Continents with Hydroxyurea
(REACH): A Prospective Multi-National Trial of Hydroxyurea for Sickle Cell Anemia in
Sub-Saharan Africa.
Ware, R.E. and et.al., 2017. Sickle cell disease. The Lancet. 390(10091). pp.311-323.
Online
8
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Green, N.S., and Barral,. S., 2014. Emerging science of hydroxyurea therapy for pediatric sickle
cell disease. [Online]. Accessed through <https://www.nature.com/articles/pr2013227>
Platt, O.S., 2008. Hydroxyurea for the Treatment of Sickle Cell Anemia. [Online]. Accessed
through <https://www.nejm.org/doi/full/10.1056/NEJMct0708272>
Reaching Children With Sickle Cell Anemia in Sub-Saharan Africa. 2019. [Online]. Accessed
through <https://www.ashclinicalnews.org/on-location/reaching-children-sickle-cell-
anemia-sub-saharan-africa/>
9
cell disease. [Online]. Accessed through <https://www.nature.com/articles/pr2013227>
Platt, O.S., 2008. Hydroxyurea for the Treatment of Sickle Cell Anemia. [Online]. Accessed
through <https://www.nejm.org/doi/full/10.1056/NEJMct0708272>
Reaching Children With Sickle Cell Anemia in Sub-Saharan Africa. 2019. [Online]. Accessed
through <https://www.ashclinicalnews.org/on-location/reaching-children-sickle-cell-
anemia-sub-saharan-africa/>
9

10
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 15
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





