Role of Luteinizing Hormone in Human Reproduction
Added on 2023-01-11
6 Pages2369 Words59 Views
Introduction
The hormones which come under the category gonadotropins are Luteinizing Hormone (LH) and
Follicle Stimulating Hormones. The hormones are released from the particular cells in the
anterior pituitary called the gonadotrophs. These hormones are large glycoproteins which are
made of alpha and beta parts 1. These gonadotropins play an essential part in the process of
reproduction. The physiological impact of these hormones is recognized in the gonads that is
ovaries and testes for female and male, respectively. Both the hormones together regulate several
facets of reproduction in both males and females 2. This essay will particularly focus on the
different features and aspect of LH in the process of human reproduction. LH initiates sex
steroids secretion from the gonads in males as well as females. In the male gonad, LH attaches to
the receptors on Leydig cells which leads to stimulation of production and secretion of
testosterone 3. In the ovary, theca cells react to the stimulation of LH by secreting testosterone,
which is changed into estrogen by nearby granulosa cells.
Discussion
Hormones are considered as the important elements of human body. They control the
reproductive system of the human body. Luteinizing hormone is a type of hormone which has
different roles in the male and female bodies. The production of LH takes place in the pituitary
gland. The primary function of this hormone is to control the ovaries in the female and testis in
the men which are known as gonads. In female, the particular hormone play the role of
sustaining the pregnancy. This hormone activates the ovaries to release oestradiol. After two- or
three-weeks LH releases an egg ovulation and in men leads to the production of testosterone.
Progesterone is a vital requirement for maintaining pregnancy efficiently and LH is needed for
consistent formation and functioning of corpora lutea.
It is essential to understand that folliculogenesis and oocyte maturation are complex processes
which involve a range of correlated cellular and endocrine pathways and mechanisms. Majority
of the germ cell maturation in fact, takes place within the intrauterine development. In the second
month of gestation, primordial germ cells move from the entoderm of the yolk sac to the genital
ridge and multiply at a rapid pace. In the genital ridge, the germ cells which are called oogonia at
this stage, go through mitosis and reach their highest number (6-7 million) by middle of the
The hormones which come under the category gonadotropins are Luteinizing Hormone (LH) and
Follicle Stimulating Hormones. The hormones are released from the particular cells in the
anterior pituitary called the gonadotrophs. These hormones are large glycoproteins which are
made of alpha and beta parts 1. These gonadotropins play an essential part in the process of
reproduction. The physiological impact of these hormones is recognized in the gonads that is
ovaries and testes for female and male, respectively. Both the hormones together regulate several
facets of reproduction in both males and females 2. This essay will particularly focus on the
different features and aspect of LH in the process of human reproduction. LH initiates sex
steroids secretion from the gonads in males as well as females. In the male gonad, LH attaches to
the receptors on Leydig cells which leads to stimulation of production and secretion of
testosterone 3. In the ovary, theca cells react to the stimulation of LH by secreting testosterone,
which is changed into estrogen by nearby granulosa cells.
Discussion
Hormones are considered as the important elements of human body. They control the
reproductive system of the human body. Luteinizing hormone is a type of hormone which has
different roles in the male and female bodies. The production of LH takes place in the pituitary
gland. The primary function of this hormone is to control the ovaries in the female and testis in
the men which are known as gonads. In female, the particular hormone play the role of
sustaining the pregnancy. This hormone activates the ovaries to release oestradiol. After two- or
three-weeks LH releases an egg ovulation and in men leads to the production of testosterone.
Progesterone is a vital requirement for maintaining pregnancy efficiently and LH is needed for
consistent formation and functioning of corpora lutea.
It is essential to understand that folliculogenesis and oocyte maturation are complex processes
which involve a range of correlated cellular and endocrine pathways and mechanisms. Majority
of the germ cell maturation in fact, takes place within the intrauterine development. In the second
month of gestation, primordial germ cells move from the entoderm of the yolk sac to the genital
ridge and multiply at a rapid pace. In the genital ridge, the germ cells which are called oogonia at
this stage, go through mitosis and reach their highest number (6-7 million) by middle of the

gestation 4. Subsequently, due to the beginning of meiosis and follicular atresia, female germ
cells number lower significantly, so that only nearly 300,000 oocytes remain during puberty.
Oogonia are converted into primary oocytes during the early stages of meiosis and stay in
prophase of the first meiotic division till just prior to ovulation. At this stage, meiosis is
completed, and primary oocytes are transformed into secondary oocytes 5. Germ cells maturation
at the time of intrauterine development and after birth is corresponded with conversion of the
adjacent follicle. Granulosa cells enhance in thickness and stratify, and theca cells are needed 6.
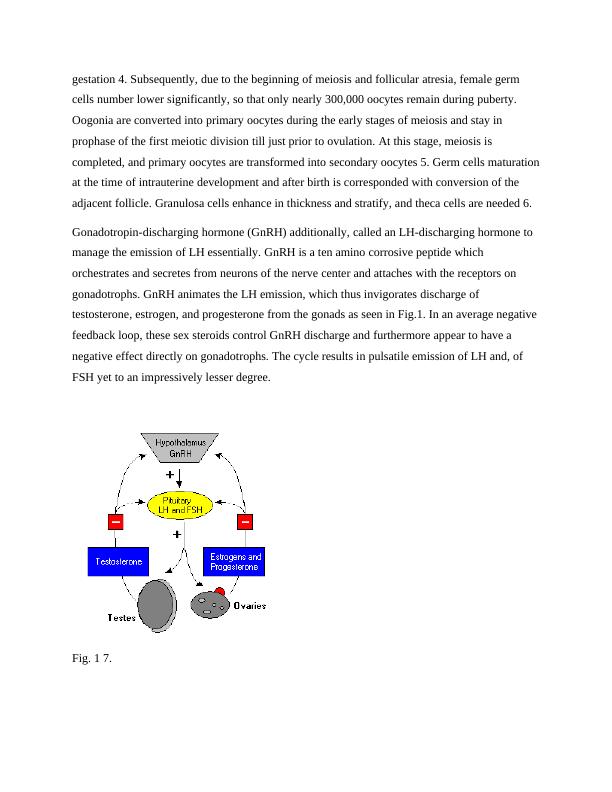
Gonadotropin-discharging hormone (GnRH) additionally, called an LH-discharging hormone to
manage the emission of LH essentially. GnRH is a ten amino corrosive peptide which
orchestrates and secretes from neurons of the nerve center and attaches with the receptors on
gonadotrophs. GnRH animates the LH emission, which thus invigorates discharge of
testosterone, estrogen, and progesterone from the gonads as seen in Fig.1. In an average negative
feedback loop, these sex steroids control GnRH discharge and furthermore appear to have a
negative effect directly on gonadotrophs. The cycle results in pulsatile emission of LH and, of
FSH yet to an impressively lesser degree.
Fig. 1 7.
cells number lower significantly, so that only nearly 300,000 oocytes remain during puberty.
Oogonia are converted into primary oocytes during the early stages of meiosis and stay in
prophase of the first meiotic division till just prior to ovulation. At this stage, meiosis is
completed, and primary oocytes are transformed into secondary oocytes 5. Germ cells maturation
at the time of intrauterine development and after birth is corresponded with conversion of the
adjacent follicle. Granulosa cells enhance in thickness and stratify, and theca cells are needed 6.
Gonadotropin-discharging hormone (GnRH) additionally, called an LH-discharging hormone to
manage the emission of LH essentially. GnRH is a ten amino corrosive peptide which
orchestrates and secretes from neurons of the nerve center and attaches with the receptors on
gonadotrophs. GnRH animates the LH emission, which thus invigorates discharge of
testosterone, estrogen, and progesterone from the gonads as seen in Fig.1. In an average negative
feedback loop, these sex steroids control GnRH discharge and furthermore appear to have a
negative effect directly on gonadotrophs. The cycle results in pulsatile emission of LH and, of
FSH yet to an impressively lesser degree.
Fig. 1 7.
The high level of LH is the major cause of infertility because it directly impacts the reproductive
system. In females, LH causes a syndrome which disturbs the testis system of the men.
Moreover, the higher level of hormones leads to the infertility. The follicular phase includes a
sequence of actions of hormones and autocrine–paracrine peptides on the follicle, directing the
follicle meant to ovulate through a period of early development from a primordial follicle over
the pre-antral, antral and preovulatory follicle stages. The two-cell, two-gonadotrophin theory is
a basic concept in ovarian physiology that ascertains the role of LH and FSH in production of
hormone 8. Formation of androgen and release during the process of folliculogenesis is based on
the stimulation of the theca cells in response to LH. Theca cells are present nearby the granulosa
cells which multiply at the time of follicular growth and are stimulated in response to FSH to
prompt the expression of the aromatase enzyme. Therefore, androgens synthesized by the theca
cells are later moved to the granulosa cells where they can be transformed into estradiol by the
action of aromatase. So, both the gonadotrophins, LH and FSH are included in the production of
estradiol during the process of folliculogenesis. The presence of LH receptors in granulosa cells
during the intermediate follicular phase indicates towards a supplementary role of LH in this
phase. Growth factors, like insulin growth factors I and II aid in promotion of follicular
maturation. These are expressed by granulosa as well as theca cells during the process of
folliculogenesis. It is indicated that action of LH on granulosa and theca cells contributes in
induction and maintenance of this paracrine system. So, as soon as granulosa cells provides
expression of adequate number of receptors for LH, the action of FSH is replaceable to
administration of LH alone. However, the exact time when in the follicular phase this action of
LH on granulosa cells starts is not evident, but the local production of factors is essential for
growth of granulosa cell and control of oocyte maturation 9.
In the period of follicular development, the choice of the foremost follicle is existent in spite of
decreasing FSH levels as the nominated follicle states FSH receptors with a inferior limit than
the not picked follicles. It is also explored that LH also shows a character in assisting in
deselection of these non-dominant follicles. At the same time, the LH flow at the indications to
interruption of succeeding granulosa cell mitosis as well as helps decisive oocyte development to
initiate in addition to luteinization of the cumulus-oophorus to take place in the instance.
Improved amounts of LH stop progressive expansion of the non-dominant follicles. This
particular knowledge leads to the construction of the ‘LH ceiling’ model in which every cavity
system. In females, LH causes a syndrome which disturbs the testis system of the men.
Moreover, the higher level of hormones leads to the infertility. The follicular phase includes a
sequence of actions of hormones and autocrine–paracrine peptides on the follicle, directing the
follicle meant to ovulate through a period of early development from a primordial follicle over
the pre-antral, antral and preovulatory follicle stages. The two-cell, two-gonadotrophin theory is
a basic concept in ovarian physiology that ascertains the role of LH and FSH in production of
hormone 8. Formation of androgen and release during the process of folliculogenesis is based on
the stimulation of the theca cells in response to LH. Theca cells are present nearby the granulosa
cells which multiply at the time of follicular growth and are stimulated in response to FSH to
prompt the expression of the aromatase enzyme. Therefore, androgens synthesized by the theca
cells are later moved to the granulosa cells where they can be transformed into estradiol by the
action of aromatase. So, both the gonadotrophins, LH and FSH are included in the production of
estradiol during the process of folliculogenesis. The presence of LH receptors in granulosa cells
during the intermediate follicular phase indicates towards a supplementary role of LH in this
phase. Growth factors, like insulin growth factors I and II aid in promotion of follicular
maturation. These are expressed by granulosa as well as theca cells during the process of
folliculogenesis. It is indicated that action of LH on granulosa and theca cells contributes in
induction and maintenance of this paracrine system. So, as soon as granulosa cells provides
expression of adequate number of receptors for LH, the action of FSH is replaceable to
administration of LH alone. However, the exact time when in the follicular phase this action of
LH on granulosa cells starts is not evident, but the local production of factors is essential for
growth of granulosa cell and control of oocyte maturation 9.
In the period of follicular development, the choice of the foremost follicle is existent in spite of
decreasing FSH levels as the nominated follicle states FSH receptors with a inferior limit than
the not picked follicles. It is also explored that LH also shows a character in assisting in
deselection of these non-dominant follicles. At the same time, the LH flow at the indications to
interruption of succeeding granulosa cell mitosis as well as helps decisive oocyte development to
initiate in addition to luteinization of the cumulus-oophorus to take place in the instance.
Improved amounts of LH stop progressive expansion of the non-dominant follicles. This
particular knowledge leads to the construction of the ‘LH ceiling’ model in which every cavity

End of preview
Want to access all the pages? Upload your documents or become a member.
Related Documents
Male and Female Reproductive Cycles and Hormonal Controllg...
|6
|835
|224
Human Regulation and Reproduction : Assignmentlg...
|6
|555
|111
Human Regulation and Reproduction (Biology) - Assignmentlg...
|6
|555
|75
Reproductive System: Male and Female Anatomy, Fertilization and Developmentlg...
|7
|845
|422
Endocrinology 1.lg...
|3
|431
|1
The Endocrine System: Functions of Hormones, Role of Blood, and Hormone Replacement Therapylg...
|6
|1651
|381
