The Effects of Exercise on Falls in Older People with Dementia
VerifiedAdded on 2022/08/23
|9
|9665
|32
Report
AI Summary
This report presents the findings of the Umeå Dementia and Exercise Study (UMDEX), a cluster-randomized controlled trial conducted in 16 nursing homes in Sweden. The study investigated the impact of a high-intensity functional exercise program on fall rates and fall-related injuries in older people with dementia. Participants were randomized to either the exercise intervention or an attention control activity. The results indicated that the exercise program did not significantly reduce the fall rate compared to the control group. However, participants in the exercise group were less likely to sustain moderate/serious fall-related injuries. The study concludes that while the exercise program alone did not prevent falls, it may have a positive effect on injury prevention, suggesting the need for a multifactorial fall-prevention approach in this high-risk population. The research highlights the importance of considering factors like multimorbidity and polypharmacy in fall prevention strategies for older people with dementia in nursing homes.
Original Study
The Effects of Exercise on Falls in Older People With Dementia Living
in Nursing Homes: A Randomized Controlled Trial
Annika Toots PhDa, b, *, Robert Wiklund PTa, b
, Håkan Littbrand PhDa, b
,
Ellinor Nordin PhDa
, Peter Nordström PhDb
, Lillemor Lundin-Olsson PhDa
,
Yngve Gustafson PhDb
, Erik Rosendahl PhDa, b
a Department of Community Medicine and Rehabilitation,Physiotherapy,Umeå University,Umeå,Sweden
b Department of Community Medicine and Rehabilitation,Geriatric Medicine,Umeå University,Umeå,Sweden
Keywords:
Falls
dementia
Alzheimer disease
exercise
residential facilities
fractures
a b s t r a c t
Objectives: To investigate exercise effects on falls in people with dementia living in nursing homes,and
whether effects were dependent on sex, dementia type, or improvement in balance. A further aim was to
describe the occurrence of fall-related injuries.
Design: A cluster-randomized controlled trial.
Setting and Participants: The Umeå Dementia and Exercise study was set in 16 nursing homes in Umeå,
Sweden and included 141 women and 45 men,a mean age of 85 years,and with a mean Mini-Mental
State Examination score of 15.
Intervention: Participants were randomized to the high-intensity functional exercise program or a seated
attention control activity; each conducted 2-3 times per week for 4 months.
Measures: Falls and fall-related injuries were followed for 12 months (after intervention completion) by
blinded review of medical records.Injuries were classified according to severity.
Results: During follow-up, 118 (67%) of the participants fell 473 times in total.At the interim 6-month
follow-up, the incidence rate was 2.7 and 2.8 falls per person-year in exercise and controlgroup,
respectively, and at 12-month follow-up 3.0 and 3.2 falls per person-year, respectively. Negative binomia
regression analyses indicated no difference in fall rate between groups at 6 or 12 months (incidence rate
ratio 0.9, 95% confidence interval(CI) 0.5e1.7,P ¼ .838 and incidence rate ratio 0.9,95% CI0.5e1.6,
P ¼ .782,respectively). No differences in exercise effects were found according to sex,dementia type,or
improvement in balance.Participants in the exercise group were less likely to sustain moderate/serious
fall-related injuries at 12-month follow-up (odds ratio 0.31,95% CI 0.10e0.94,P ¼ .039).
Conclusions/Implications: In older people with dementia living in nursing homes,a high-intensity func-
tional exercise program alone did not prevent falls when compared with an attention control group.In
high-risk populations,in which multimorbidity and polypharmacy are common,a multifactorialfall-
prevention approach may be required.Encouraging effectson fall-related injuries were observed,
which merits future investigations.
Ó 2018 AMDA e The Society for Post-Acute and Long-Term Care Medicine.This is an open access article
under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
This work was supported by the Swedish Research Council(grant numbers
K2009-69P-21298-01-4,K2009-69X-21299-01-1,K2009-69P-21298-04-4,K2014-
99X-22610-01-6); Forte e Swedish Research Councilfor Health,Working Life and
Welfare (formerly FAS e Swedish Council for Working Life and Social Research); the
Vårdal Foundation; the Swedish Dementia Association; the Promobilia Foundation;
the Swedish Society ofMedicine; the Swedish Alzheimer Foundation;the King
Gustav V and Queen Victoria’s Foundation ofFreemasons;the European Union
Bothnia-Atlantica Program; the County Council of Västerbotten,the Umeå Univer-
sity Foundation for MedicalResearch;the Ragnhild and Einar Lundström’s Me-
morial Foundation; and the Erik and Anne-Marie Detlof’s Foundation.
Littbrand developed and has received royalties on the weighted belt used in the
exercise program.
The study sponsors’had no role in the design,methods,subject recruitment,
data collection,analysis,or preparation of the article.
The authors declare no conflicts of interest.
* Address correspondence to Annika Toots,PhD, Departmentof Community
Medicine and Rehabilitation, Physiotherapy,Umeå University, 901 87 Umeå,
Sweden.
E-mail address: annika.toots@umu.se (A.Toots).
https://doi.org/10.1016/j.jamda.2018.10.009
1525-8610/Ó 2018 AMDA e The Society for Post-Acute and Long-Term Care Medicine. This is an open access article under the CC BY-NC-ND license (http://creativecom
org/licenses/by-nc-nd/4.0/).
JAMDA
j o u r n a lhomepage: www.jamda.com
JAMDA 20 (2019) 835e842
The Effects of Exercise on Falls in Older People With Dementia Living
in Nursing Homes: A Randomized Controlled Trial
Annika Toots PhDa, b, *, Robert Wiklund PTa, b
, Håkan Littbrand PhDa, b
,
Ellinor Nordin PhDa
, Peter Nordström PhDb
, Lillemor Lundin-Olsson PhDa
,
Yngve Gustafson PhDb
, Erik Rosendahl PhDa, b
a Department of Community Medicine and Rehabilitation,Physiotherapy,Umeå University,Umeå,Sweden
b Department of Community Medicine and Rehabilitation,Geriatric Medicine,Umeå University,Umeå,Sweden
Keywords:
Falls
dementia
Alzheimer disease
exercise
residential facilities
fractures
a b s t r a c t
Objectives: To investigate exercise effects on falls in people with dementia living in nursing homes,and
whether effects were dependent on sex, dementia type, or improvement in balance. A further aim was to
describe the occurrence of fall-related injuries.
Design: A cluster-randomized controlled trial.
Setting and Participants: The Umeå Dementia and Exercise study was set in 16 nursing homes in Umeå,
Sweden and included 141 women and 45 men,a mean age of 85 years,and with a mean Mini-Mental
State Examination score of 15.
Intervention: Participants were randomized to the high-intensity functional exercise program or a seated
attention control activity; each conducted 2-3 times per week for 4 months.
Measures: Falls and fall-related injuries were followed for 12 months (after intervention completion) by
blinded review of medical records.Injuries were classified according to severity.
Results: During follow-up, 118 (67%) of the participants fell 473 times in total.At the interim 6-month
follow-up, the incidence rate was 2.7 and 2.8 falls per person-year in exercise and controlgroup,
respectively, and at 12-month follow-up 3.0 and 3.2 falls per person-year, respectively. Negative binomia
regression analyses indicated no difference in fall rate between groups at 6 or 12 months (incidence rate
ratio 0.9, 95% confidence interval(CI) 0.5e1.7,P ¼ .838 and incidence rate ratio 0.9,95% CI0.5e1.6,
P ¼ .782,respectively). No differences in exercise effects were found according to sex,dementia type,or
improvement in balance.Participants in the exercise group were less likely to sustain moderate/serious
fall-related injuries at 12-month follow-up (odds ratio 0.31,95% CI 0.10e0.94,P ¼ .039).
Conclusions/Implications: In older people with dementia living in nursing homes,a high-intensity func-
tional exercise program alone did not prevent falls when compared with an attention control group.In
high-risk populations,in which multimorbidity and polypharmacy are common,a multifactorialfall-
prevention approach may be required.Encouraging effectson fall-related injuries were observed,
which merits future investigations.
Ó 2018 AMDA e The Society for Post-Acute and Long-Term Care Medicine.This is an open access article
under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
This work was supported by the Swedish Research Council(grant numbers
K2009-69P-21298-01-4,K2009-69X-21299-01-1,K2009-69P-21298-04-4,K2014-
99X-22610-01-6); Forte e Swedish Research Councilfor Health,Working Life and
Welfare (formerly FAS e Swedish Council for Working Life and Social Research); the
Vårdal Foundation; the Swedish Dementia Association; the Promobilia Foundation;
the Swedish Society ofMedicine; the Swedish Alzheimer Foundation;the King
Gustav V and Queen Victoria’s Foundation ofFreemasons;the European Union
Bothnia-Atlantica Program; the County Council of Västerbotten,the Umeå Univer-
sity Foundation for MedicalResearch;the Ragnhild and Einar Lundström’s Me-
morial Foundation; and the Erik and Anne-Marie Detlof’s Foundation.
Littbrand developed and has received royalties on the weighted belt used in the
exercise program.
The study sponsors’had no role in the design,methods,subject recruitment,
data collection,analysis,or preparation of the article.
The authors declare no conflicts of interest.
* Address correspondence to Annika Toots,PhD, Departmentof Community
Medicine and Rehabilitation, Physiotherapy,Umeå University, 901 87 Umeå,
Sweden.
E-mail address: annika.toots@umu.se (A.Toots).
https://doi.org/10.1016/j.jamda.2018.10.009
1525-8610/Ó 2018 AMDA e The Society for Post-Acute and Long-Term Care Medicine. This is an open access article under the CC BY-NC-ND license (http://creativecom
org/licenses/by-nc-nd/4.0/).
JAMDA
j o u r n a lhomepage: www.jamda.com
JAMDA 20 (2019) 835e842
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Older people with dementia have a higher risk of falls and fall-
related injuries compared with older people in general.1e3 The
increased risk can be attributed to symptoms such as cognitive and
physicalimpairment.1,3,4Furthermore,people with non-Alzheimer’s
types of dementia (non- Alzheimer’s disease), for example, Lewy body
dementia and vascular dementia,seem to have a higher fall risk
compared with Alzheimer’s disease.1,5 Consequences of falls (eg,hip
fractures) can have a detrimental influence on functional ability and
survival in older persons,6 let alone persons with dementia,who,
following a hip fracture,appear to have even worse prognosis than
those without dementia.2,7,8 The number of older people with de-
mentia is projected to increase in the near future,and falls and fall-
related injuries not only contribute to the burden of illness,but will
also challenge public health resources worldwide.
In community-dwelling older populations,there is evidence that
physical exercise,as a single intervention,can prevent falls.9,10Exer-
cise programs involving a high challenge to balance and performed at
least 3 times a week seem to have the greatest fall preventative ef-
fect.10 Also, in older people with cognitive impairment,promising
evidence of the effect of exercise on falls prevention is emerging.10,11
However,studies in people with dementia are comparatively few,
and most are set in the community.12e14 In nursing homes,where a
large proportion of the residents have dementia,there is limited ev-
idence of beneficialeffects of exercise.10,15Furthermore,improved
ability to ambulate independently may pose a higher risk of falls and
fall-related injuries through an increased exposure to high-risk
situations.15e17
Beneficial effects on balance of a high-intensity functional exercise
program in people with dementia living in nursing homes have been
found previously.The program appeared to particularly benefit par-
ticipants with non-Alzheimer’s disease compared with people with
Alzheimer’s disease,18 while no effects were observed on cognition.19
In addition, in older people with and without dementia living in
nursing homes,exercise programs have been shown to prevent falls
when balance was improved.20 The aim of this study was, therefore, to
investigate the effects of a high-intensity functional exercise program
on fall rate in people with dementia living in nursing homes,and if
effects were associated with sex,dementia type,or improvement in
balance.A further aim was to describe the occurrence of fall-related
injuries.
Methods
This study was part of the Umeå Dementia and Exercise Study
(UMDEX), a cluster-randomized controlled trial,set in 16 nursing
homes in Umeå, Sweden.18,19,21
The study protocol (ISRCTN31767087)
is published on the ISRCTN registry.
Participants
The UMDEX study included nursing home residents who had a
Mini-Mental State Examination (MMSE) score of at least 10,22 a de-
mentia diagnosis,23 were aged 65 years or over,dependent on assis-
tance in at least 1 personal activities of daily living (ADL) according to
the Katz Index,24 had the ability to stand up from a chair with armrests
with assistance from no more than 1 person, physician’s approval, and
ability to hear and understand spoken Swedish sufficiently to partic-
ipate in assessments.All participants gave informed oralconsent,
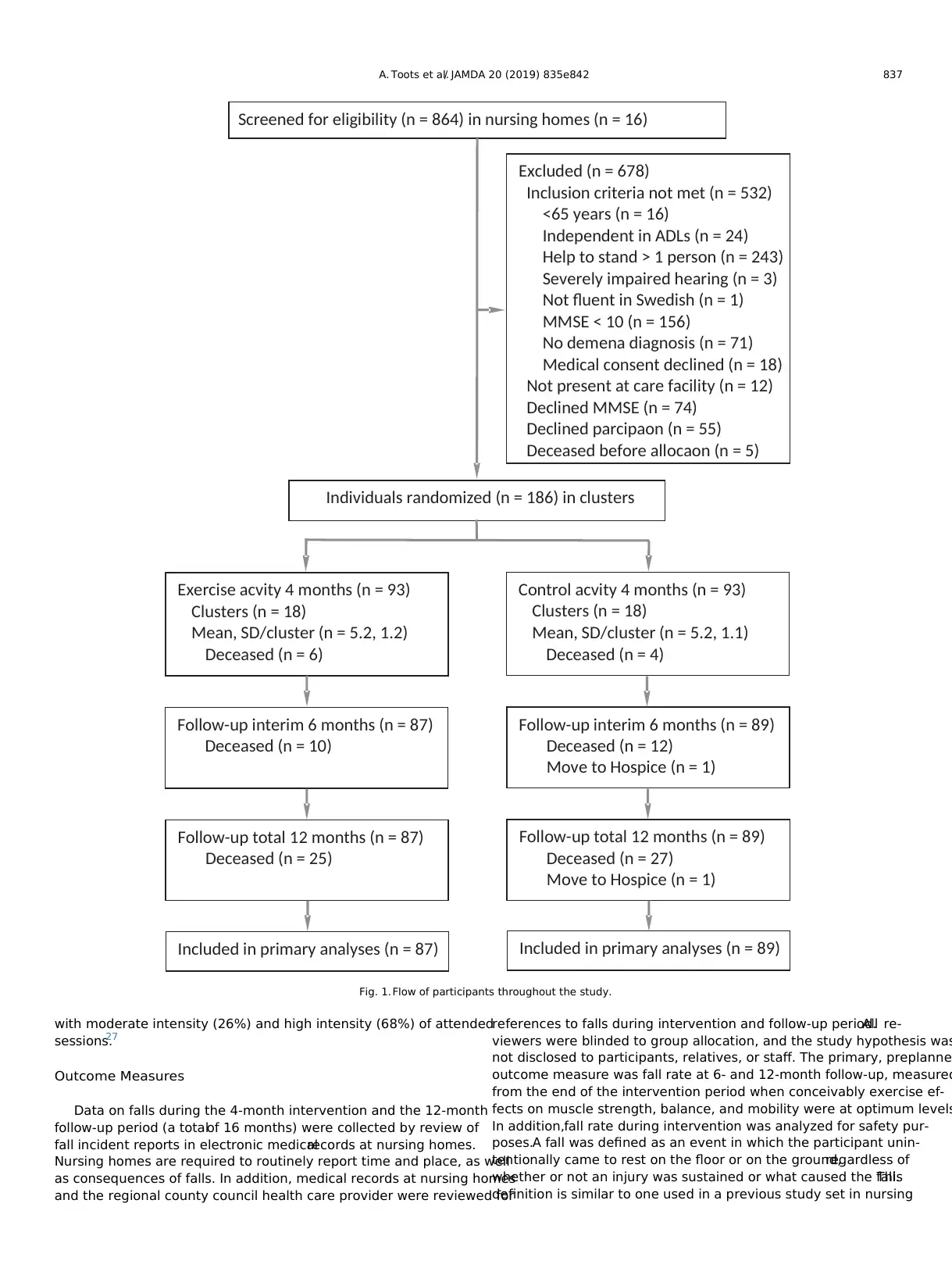
which was also confirmed by their next of kin.In the 864 nursing
home residents screened in total,age (P ¼ .189) and MMSE score
(P ¼ .713) did not differ between participants included and those who
declined participation (n ¼ 55; Figure 1).A larger proportion of men
than women declined participation (34% vs 18%; P ¼ .008).
Sample and Randomization
Sample size (n ¼ 186) for the UMDEX study was calculated based
on the main outcome,the Barthel ADL Index.18 In addition,a power
simulation was undertaken using data on participants with dementia
from a previous trialinvestigating exercise effects on falls,20 which
assumed a dispersion parameter of 2.0, a control group fall rate of 5.0
falls/person-year,and a 30% difference in fall rate between groups.A
sample size of 135 participants was required to have a 80% chance of
detecting such reduction in fall rate significant at the 5% level.
Participants were randomized after completion of enrolment
process and baseline assessmentto ensure concealed allocation.
Clusters (n ¼ 36) of 3 to 8 participants each (who lived in the same
wing, unit, or floor) were formed to reduce contamination. The
randomization was stratified in all nursing homes except one that had
only a single cluster; the object being to have participants in both
exercise and attention controlgroups living in each nursing home,
which reduces the risk of site-specific factors influencing the outcome.
Two researchers not involved in the study performed randomiza-
tion by drawing lots using sealed opaque envelopes.The Regional
Ethics Review Board in Umeå approved the study (2011-205-31M).
Intervention
Physiotherapists (PT) led the exercise activities,and occupational
therapists (OT) or an OT assistant led the attention controlactivity.
Following exercise recommendations for generalolder populations,
the intervention consisted of 5 sessions per fortnight for the duration
of 4 months (40 sessions in total),with each session lasting approxi-
mately 45 minutes. Whenever possible, supervised individual sessions
were offered when participants were unable to attend a group session.
No activities were provided after the 4-month intervention.Partici-
pation in activities other than those provided by the study was not
restricted at any time.
The exercise intervention was based on the high-intensity func-
tional exercise program (HIFE),which includes a model for exercise
selection and a definition ofexercise intensity (available online at
https://www.hifeprogram.se/en).18,25,26In brief, the HIFE comprises
39 functional exercises for improved lower limb strength,balance,
and mobility to be performed with high intensity and in weight-
bearing positions similar to daily activities. High-intensity in
strength exercise is defined as 8e12 repetition maximum and in
balance exercise when posturalstability is fully challenged.25,26 Ex-
ercises were tailored based on participants’functionaldeficits.Par-
ticipants were supervised individually to promote the highest possible
exercise intensity, and adapted accordingly through progressive
adjustment of load and base of support, while also taking into account
participants’symptoms and changes in health and functional status.
For safety,participants wore belts with handles so that PTs could
provide support if needed when posturalstability was fully chal-
lenged,thereby preventing falls. Unnecessary support was avoided.
The attention controlgroup participated in structured activities
that were developed by the OTs/OT assistant that led the activities. The
activities were structured around topics believed to be interesting for
older people,including localwild life, seasons,and holidays.While
seated in a group,participants conversed,sang,listened to music or
readings,and/or looked at pictures and objects.
At the end of each session, leaders completed a structured protocol
for each participant pertaining to adverse events,and in the exercise
group,intensity achieved in muscle strength and balance exercises,
which was estimated separately as high, moderate, or low according to
the predefined scale.25 All adverse events recorded during exercise
sessions were minor or temporary.27 In the exercise group,partici-
pants performed strength exercises with moderate intensity (40%)
and at high intensity (49%) of attended sessions, and balance exercises
A. Toots et al./ JAMDA 20 (2019) 835e842836
related injuries compared with older people in general.1e3 The
increased risk can be attributed to symptoms such as cognitive and
physicalimpairment.1,3,4Furthermore,people with non-Alzheimer’s
types of dementia (non- Alzheimer’s disease), for example, Lewy body
dementia and vascular dementia,seem to have a higher fall risk
compared with Alzheimer’s disease.1,5 Consequences of falls (eg,hip
fractures) can have a detrimental influence on functional ability and
survival in older persons,6 let alone persons with dementia,who,
following a hip fracture,appear to have even worse prognosis than
those without dementia.2,7,8 The number of older people with de-
mentia is projected to increase in the near future,and falls and fall-
related injuries not only contribute to the burden of illness,but will
also challenge public health resources worldwide.
In community-dwelling older populations,there is evidence that
physical exercise,as a single intervention,can prevent falls.9,10Exer-
cise programs involving a high challenge to balance and performed at
least 3 times a week seem to have the greatest fall preventative ef-
fect.10 Also, in older people with cognitive impairment,promising
evidence of the effect of exercise on falls prevention is emerging.10,11
However,studies in people with dementia are comparatively few,
and most are set in the community.12e14 In nursing homes,where a
large proportion of the residents have dementia,there is limited ev-
idence of beneficialeffects of exercise.10,15Furthermore,improved
ability to ambulate independently may pose a higher risk of falls and
fall-related injuries through an increased exposure to high-risk
situations.15e17
Beneficial effects on balance of a high-intensity functional exercise
program in people with dementia living in nursing homes have been
found previously.The program appeared to particularly benefit par-
ticipants with non-Alzheimer’s disease compared with people with
Alzheimer’s disease,18 while no effects were observed on cognition.19
In addition, in older people with and without dementia living in
nursing homes,exercise programs have been shown to prevent falls
when balance was improved.20 The aim of this study was, therefore, to
investigate the effects of a high-intensity functional exercise program
on fall rate in people with dementia living in nursing homes,and if
effects were associated with sex,dementia type,or improvement in
balance.A further aim was to describe the occurrence of fall-related
injuries.
Methods
This study was part of the Umeå Dementia and Exercise Study
(UMDEX), a cluster-randomized controlled trial,set in 16 nursing
homes in Umeå, Sweden.18,19,21
The study protocol (ISRCTN31767087)
is published on the ISRCTN registry.
Participants
The UMDEX study included nursing home residents who had a
Mini-Mental State Examination (MMSE) score of at least 10,22 a de-
mentia diagnosis,23 were aged 65 years or over,dependent on assis-
tance in at least 1 personal activities of daily living (ADL) according to
the Katz Index,24 had the ability to stand up from a chair with armrests
with assistance from no more than 1 person, physician’s approval, and
ability to hear and understand spoken Swedish sufficiently to partic-
ipate in assessments.All participants gave informed oralconsent,
which was also confirmed by their next of kin.In the 864 nursing
home residents screened in total,age (P ¼ .189) and MMSE score
(P ¼ .713) did not differ between participants included and those who
declined participation (n ¼ 55; Figure 1).A larger proportion of men
than women declined participation (34% vs 18%; P ¼ .008).
Sample and Randomization
Sample size (n ¼ 186) for the UMDEX study was calculated based
on the main outcome,the Barthel ADL Index.18 In addition,a power
simulation was undertaken using data on participants with dementia
from a previous trialinvestigating exercise effects on falls,20 which
assumed a dispersion parameter of 2.0, a control group fall rate of 5.0
falls/person-year,and a 30% difference in fall rate between groups.A
sample size of 135 participants was required to have a 80% chance of
detecting such reduction in fall rate significant at the 5% level.
Participants were randomized after completion of enrolment
process and baseline assessmentto ensure concealed allocation.
Clusters (n ¼ 36) of 3 to 8 participants each (who lived in the same
wing, unit, or floor) were formed to reduce contamination. The
randomization was stratified in all nursing homes except one that had
only a single cluster; the object being to have participants in both
exercise and attention controlgroups living in each nursing home,
which reduces the risk of site-specific factors influencing the outcome.
Two researchers not involved in the study performed randomiza-
tion by drawing lots using sealed opaque envelopes.The Regional
Ethics Review Board in Umeå approved the study (2011-205-31M).
Intervention
Physiotherapists (PT) led the exercise activities,and occupational
therapists (OT) or an OT assistant led the attention controlactivity.
Following exercise recommendations for generalolder populations,
the intervention consisted of 5 sessions per fortnight for the duration
of 4 months (40 sessions in total),with each session lasting approxi-
mately 45 minutes. Whenever possible, supervised individual sessions
were offered when participants were unable to attend a group session.
No activities were provided after the 4-month intervention.Partici-
pation in activities other than those provided by the study was not
restricted at any time.
The exercise intervention was based on the high-intensity func-
tional exercise program (HIFE),which includes a model for exercise
selection and a definition ofexercise intensity (available online at
https://www.hifeprogram.se/en).18,25,26In brief, the HIFE comprises
39 functional exercises for improved lower limb strength,balance,
and mobility to be performed with high intensity and in weight-
bearing positions similar to daily activities. High-intensity in
strength exercise is defined as 8e12 repetition maximum and in
balance exercise when posturalstability is fully challenged.25,26 Ex-
ercises were tailored based on participants’functionaldeficits.Par-
ticipants were supervised individually to promote the highest possible
exercise intensity, and adapted accordingly through progressive
adjustment of load and base of support, while also taking into account
participants’symptoms and changes in health and functional status.
For safety,participants wore belts with handles so that PTs could
provide support if needed when posturalstability was fully chal-
lenged,thereby preventing falls. Unnecessary support was avoided.
The attention controlgroup participated in structured activities
that were developed by the OTs/OT assistant that led the activities. The
activities were structured around topics believed to be interesting for
older people,including localwild life, seasons,and holidays.While
seated in a group,participants conversed,sang,listened to music or
readings,and/or looked at pictures and objects.
At the end of each session, leaders completed a structured protocol
for each participant pertaining to adverse events,and in the exercise
group,intensity achieved in muscle strength and balance exercises,
which was estimated separately as high, moderate, or low according to
the predefined scale.25 All adverse events recorded during exercise
sessions were minor or temporary.27 In the exercise group,partici-
pants performed strength exercises with moderate intensity (40%)
and at high intensity (49%) of attended sessions, and balance exercises
A. Toots et al./ JAMDA 20 (2019) 835e842836
with moderate intensity (26%) and high intensity (68%) of attended
sessions.27
Outcome Measures
Data on falls during the 4-month intervention and the 12-month
follow-up period (a totalof 16 months) were collected by review of
fall incident reports in electronic medicalrecords at nursing homes.
Nursing homes are required to routinely report time and place, as well
as consequences of falls. In addition, medical records at nursing homes
and the regional county council health care provider were reviewed for
references to falls during intervention and follow-up period.All re-
viewers were blinded to group allocation, and the study hypothesis was
not disclosed to participants, relatives, or staff. The primary, preplanne
outcome measure was fall rate at 6- and 12-month follow-up, measured
from the end of the intervention period when conceivably exercise ef-
fects on muscle strength, balance, and mobility were at optimum levels
In addition,fall rate during intervention was analyzed for safety pur-
poses.A fall was defined as an event in which the participant unin-
tentionally came to rest on the floor or on the ground,regardless of
whether or not an injury was sustained or what caused the fall.This
definition is similar to one used in a previous study set in nursing
Screened for eligibility (n = 864) in nursing homes (n = 16)
Excluded (n = 678)
Inclusion criteria not met (n = 532)
<65 years (n = 16)
Independent in ADLs (n = 24)
Help to stand > 1 person (n = 243)
Severely impaired hearing (n = 3)
Not fluent in Swedish (n = 1)
MMSE < 10 (n = 156)
No demena diagnosis (n = 71)
Medical consent declined (n = 18)
Not present at care facility (n = 12)
Declined MMSE (n = 74)
Declined parcipaon (n = 55)
Deceased before allocaon (n = 5)
Individuals randomized (n = 186) in clusters
Exercise acvity 4 months (n = 93)
Clusters (n = 18)
Mean, SD/cluster (n = 5.2, 1.2)
Deceased (n = 6)
Control acvity 4 months (n = 93)
Clusters (n = 18)
Mean, SD/cluster (n = 5.2, 1.1)
Deceased (n = 4)
Follow-up interim 6 months (n = 87)
Deceased (n = 10)
Follow-up interim 6 months (n = 89)
Deceased (n = 12)
Move to Hospice (n = 1)
Follow-up total 12 months (n = 87)
Deceased (n = 25)
Follow-up total 12 months (n = 89)
Deceased (n = 27)
Move to Hospice (n = 1)
Included in primary analyses (n = 87) Included in primary analyses (n = 89)
Fig. 1. Flow of participants throughout the study.
A. Toots et al./ JAMDA 20 (2019) 835e842 837
sessions.27
Outcome Measures
Data on falls during the 4-month intervention and the 12-month
follow-up period (a totalof 16 months) were collected by review of
fall incident reports in electronic medicalrecords at nursing homes.
Nursing homes are required to routinely report time and place, as well
as consequences of falls. In addition, medical records at nursing homes
and the regional county council health care provider were reviewed for
references to falls during intervention and follow-up period.All re-
viewers were blinded to group allocation, and the study hypothesis was
not disclosed to participants, relatives, or staff. The primary, preplanne
outcome measure was fall rate at 6- and 12-month follow-up, measured
from the end of the intervention period when conceivably exercise ef-
fects on muscle strength, balance, and mobility were at optimum levels
In addition,fall rate during intervention was analyzed for safety pur-
poses.A fall was defined as an event in which the participant unin-
tentionally came to rest on the floor or on the ground,regardless of
whether or not an injury was sustained or what caused the fall.This
definition is similar to one used in a previous study set in nursing
Screened for eligibility (n = 864) in nursing homes (n = 16)
Excluded (n = 678)
Inclusion criteria not met (n = 532)
<65 years (n = 16)
Independent in ADLs (n = 24)
Help to stand > 1 person (n = 243)
Severely impaired hearing (n = 3)
Not fluent in Swedish (n = 1)
MMSE < 10 (n = 156)
No demena diagnosis (n = 71)
Medical consent declined (n = 18)
Not present at care facility (n = 12)
Declined MMSE (n = 74)
Declined parcipaon (n = 55)
Deceased before allocaon (n = 5)
Individuals randomized (n = 186) in clusters
Exercise acvity 4 months (n = 93)
Clusters (n = 18)
Mean, SD/cluster (n = 5.2, 1.2)
Deceased (n = 6)
Control acvity 4 months (n = 93)
Clusters (n = 18)
Mean, SD/cluster (n = 5.2, 1.1)
Deceased (n = 4)
Follow-up interim 6 months (n = 87)
Deceased (n = 10)
Follow-up interim 6 months (n = 89)
Deceased (n = 12)
Move to Hospice (n = 1)
Follow-up total 12 months (n = 87)
Deceased (n = 25)
Follow-up total 12 months (n = 89)
Deceased (n = 27)
Move to Hospice (n = 1)
Included in primary analyses (n = 87) Included in primary analyses (n = 89)
Fig. 1. Flow of participants throughout the study.
A. Toots et al./ JAMDA 20 (2019) 835e842 837
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
homes,20 and includes falls resulting from, for instance, acute disease or
an epileptic seizure.In community-dwelling populations,the recom-
mended definition of falls also includes falls coming to rest on a “lower
level,”28 for example, the uncontrolled sitting down from loss of balance
during rising from a chair. This part was omitted because it would likely
not be reported as a fall in our population.
Descriptive Assessments
Trained research staff(PTs and physicians),blinded to activity
allocation,performed all measurements.Dependence in ADLs was
measured using Barthel ADL Index (0e20).29 Gait speed was measured
over 4.0 m.30 Global cognition was measured using the MMSE
(0e30)22,31and the Verbal fluency test was used to measure executive
function.32 Nutritional status was assessed using the Mini-Nutritional
Assessment (0e30).33 Vision was considered impaired when unable to
read a word printed in 5-mm capital letters, with or without glasses, at
normal reading distance.Hearing was considered impaired when
unable to hear a conversation held at usualspeaking voice from a
distance of 1 m, with or without hearing aids. Self-reported health was
evaluated using the firstquestion from the Short-Form-36 Health
Survey.34 Nurses performed blood tests,which were analyzed by
standardized methodsat the (the University Hospital of Umeå).
Behavioral and psychological symptoms in dementia were measured
using the Neuropsychiatric Inventory (0e144).35 Symptoms of
depression were assessed using the 15-item Geriatric Depression Scale
(0e15).36 Electronic records of past medical history,which included
brain imaging in most cases,current pharmaceutical treatment,and
assessment results,were used to record dementia type,depressive
disorders,and delirium diagnoses.A specialist in geriatric medicine
reviewed and confirmed these diagnoses according to DSM-IV-TR
criteria.23 Balance was measured using the Berg Balance Scale (BBS,
0e56)37 at baseline,and on intervention completion.Data on fall-
related injuries was collected in conjunction with falls over
16 months in total. All injuries related to falls were classified according
to maximum severity using the abbreviated injury scale38: injuries
limited to superficial wounds and bruises as minor;intermediate-
level injuries, such as head injuries,vertebral,wrist or ankle frac-
tures as moderate; and major fractures, such as hip fractures and other
femoral fractures as serious.
Data Analysis
Baseline characteristics were summarized as means (standard de-
viation) or frequencies (percentages).An a priori strategy for the se-
lection of adjusting variables was adhered to.Comparisons between
exercise and attention control groups were conducted for all variables
in Table 1 (preselected as possible confounders) using Student t-test or
Pearsonc2 test,in addition to associations (r 0.3) with fall rate at 6
and 12 months using Pearson correlation coefficient.No variables
differed significantly between groups at baseline bar antidepressant use
(P ¼ .04), which was adjusted for in analyses. No variable was found to
associate with change in outcome measures above predefined levels.
In an intention-to-treat approach, all available data for participants
were analyzed according to original allocation and regardless of level
of attendance. Incidence rates (IRs) for falls were calculated in relation
to person-year using number ofobservation days,deducting 9107
(16%) days absent in cases of relocation or death.Negative binomial
regression was used to analyze the IR ratio (IRR) of falls between ex-
ercise and attention control groups for the different time periods, with
observation days as exposure term and adjusted for age,sex,antide-
pressants,and cluster.Negative binomialregression analysis is rec-
ommended when fitting models for count data that has a Poisson
distribution and are also over-dispersed (the variance exceeds the
mean).39
Subgroup comparisons according to type of dementia, longitudinal
change in balance,and sex were conducted.Differences in effects on
fall rate in subgroups were analyzed by adding an interaction term to
adjusted models.Dementia type was dichotomized into Alzheimer’s
disease vs all other (non-Alzheimer’s disease) types of dementias18
; in
part to aid comparison of results with studies that include participants
with Alzheimer’s disease only,and also because previous studies
indicate that relevant differences between these 2 dementia sub-
groups may exist.5,18Change in functional balance was based on the
median difference in the BBS (post- minus preintervention) in the
total sample, and defined as a BBS score of 2.20
In additional analyses, logistic regression was used to compare fall-
related risk of moderate/serious vs no/minor injuries, adjusted for age,
sex, and antidepressants, between exercise and control groups.
All analyses were performed using IBM SPSS statistics for Macin-
tosh v 23.0 (IBM Corp.Armonk, NY.) and StataCorp.2013.Stata Sta-
tistical Software for Macintosh: Release 13.1.(StataCorp LP,College
Station, TX). All statistical tests were 2 tailed and a P value of < .05 was
considered to be statistically significant.
Results
In total, 141 women and 45 men, with mean standard deviation
(SD) age of 85.1 7.1 years and a MMSE score of 14.9 3.5 were
included (Table 1).Sixty-seven (36.0%) participants had Alzheimer’s
disease and 119 (64%)had non-Alzheimer’s disease;of which 77
participants had vascular dementia, 15 mixed Alzheimer’s disease and
vascular dementia,and 27 had other types of dementia.Over the
4-month intervention period,adherence in the exercise group was
73% and in the attention control group, 70%.
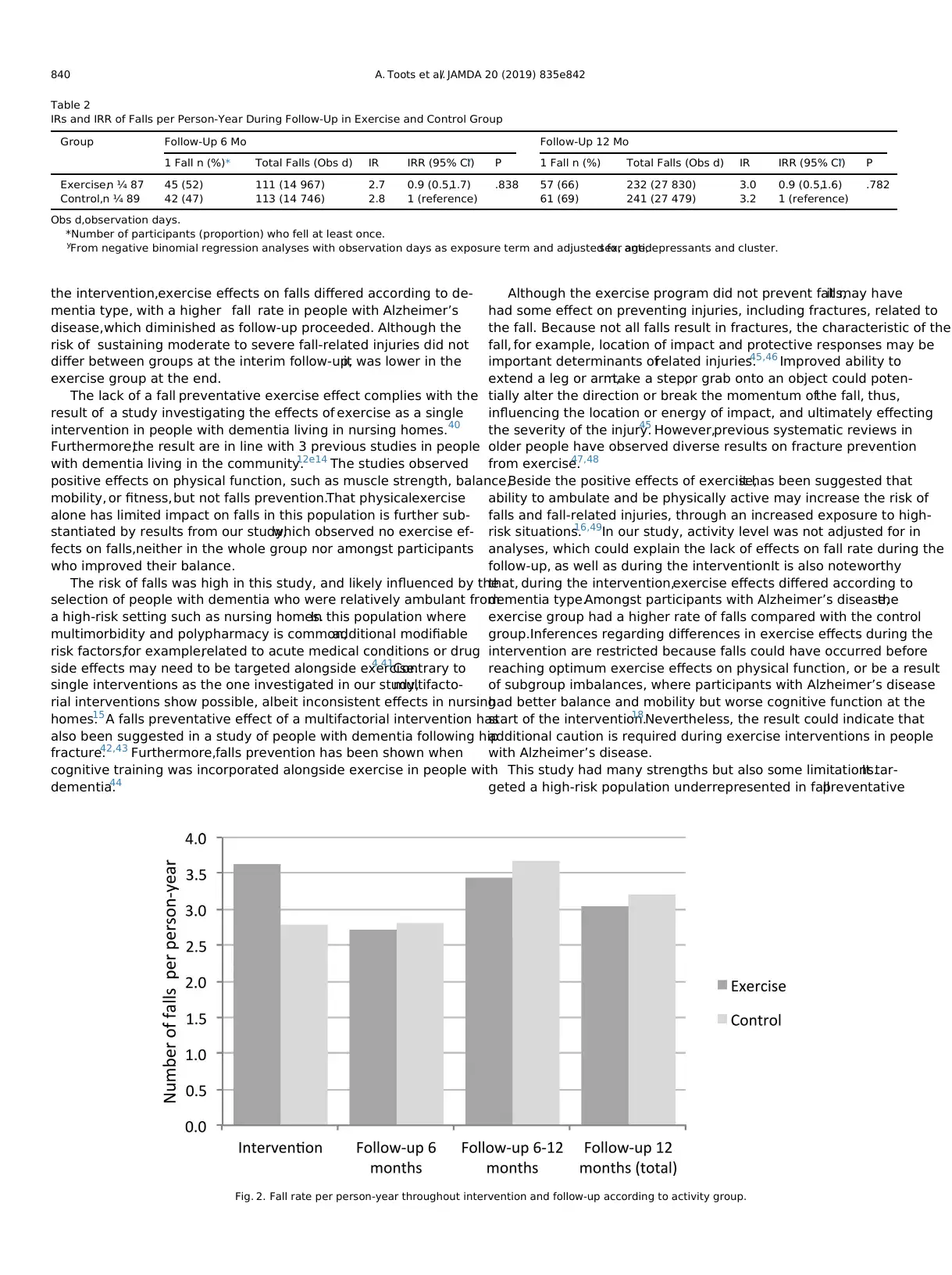
Data on falls during follow-up is summarized in Table 2.In total
during the 12-month follow-up, 34 (19%) of the participants fell once
and 84 (48%) fell at least twice. The number of falls per person ranged
from 0 to 28.There was no difference in fall rate (IRR) between ex-
ercise and control group at either 6- or 12-month follow-up [IRR 0.9,
95% confidence interval(CI) 0.5e1.7,P ¼ .838 and IRR 0.9,95% CI
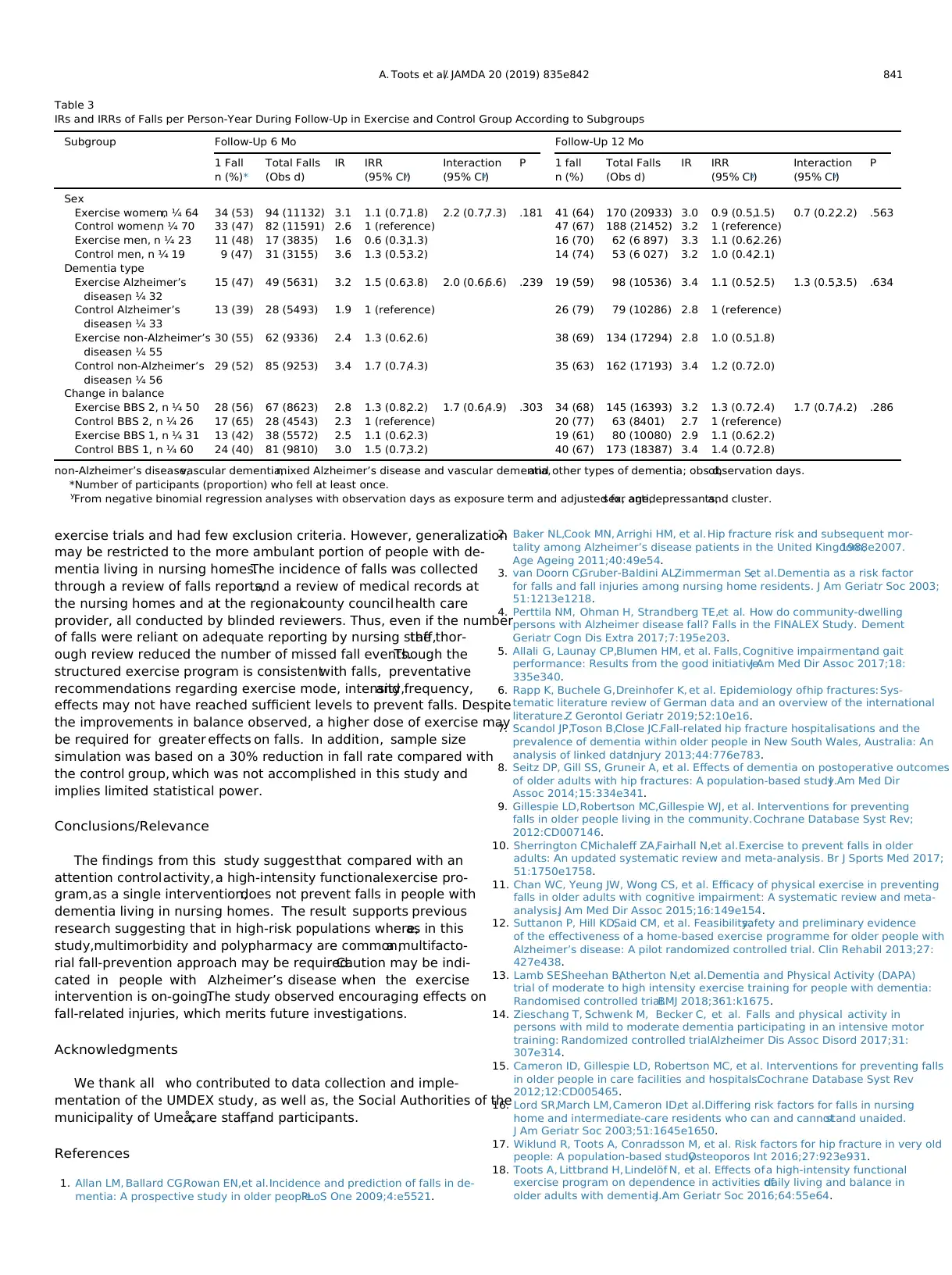
0.5e1.6,P ¼ .782,respectively; Table 2,Figure 2].No differences in
exercise effects on falls were found according to sex, dementia type, or
change in balance (Table 3). Of 473 falls, 271 (57%) resulted in no injury
(128 and 143 in exercise and controlgroup, respectively) and 173
(37%)in minor injury (92 and 81 in exercise and control group,
respectively).In 10 (2%) of the falls (7 and 3 in exercise and control
group, respectively), a differentiation between no or mild injury could
not be determined because of insufficient documentation. Eleven (2%)
of the falls resulted in moderate injury; 1 injury in the exercise group
(patella fracture) vs 10 injuries in the control group (3 pelvic fractures,
1 patella fracture,2 ribcage fractures,1 elbow fracture,1 vertebral
compression fracture, and 2 humerus fractures). Eight (2%) of the falls
resulted in serious injury (4 hip fractures in exercise and control
groups each).Of the 19 participants with moderate to serious inju-
rious falls, 18 required a visit or admission to a hospital (5 in the ex-
ercise group and 13 in the control group).
During the intervention, no difference in fall rate between exercise
and controlgroup was observed (IRR 1.2,95% CI 0.8e2.0,P ¼ .398;
SupplementalTable 1, Figure 2). No falls occurred during activity
sessions. Interaction analyses indicated a difference in falls according
to dementia type during the intervention (IRR 2.6,95% CI1.0e6.7,
P ¼ .048), where participants with Alzheimer’s disease in the exercise
group fell more than the controlgroup (SupplementalTable 1).No
difference in exercise effects on falls according to sex was found
(Supplemental Table 1).Of the 190 falls that occurred in the exercise
and control group,87 (46%) resulted in no injury (52 and 35 in the
respective groups)and 92 (48%) in minor injury (50 and 42 in
respective groups).In 2 (1%) of the falls (1 in exercise and control
groups each), a differentiation between no or mild injury could not be
A. Toots et al./ JAMDA 20 (2019) 835e842838
an epileptic seizure.In community-dwelling populations,the recom-
mended definition of falls also includes falls coming to rest on a “lower
level,”28 for example, the uncontrolled sitting down from loss of balance
during rising from a chair. This part was omitted because it would likely
not be reported as a fall in our population.
Descriptive Assessments
Trained research staff(PTs and physicians),blinded to activity
allocation,performed all measurements.Dependence in ADLs was
measured using Barthel ADL Index (0e20).29 Gait speed was measured
over 4.0 m.30 Global cognition was measured using the MMSE
(0e30)22,31and the Verbal fluency test was used to measure executive
function.32 Nutritional status was assessed using the Mini-Nutritional
Assessment (0e30).33 Vision was considered impaired when unable to
read a word printed in 5-mm capital letters, with or without glasses, at
normal reading distance.Hearing was considered impaired when
unable to hear a conversation held at usualspeaking voice from a
distance of 1 m, with or without hearing aids. Self-reported health was
evaluated using the firstquestion from the Short-Form-36 Health
Survey.34 Nurses performed blood tests,which were analyzed by
standardized methodsat the (the University Hospital of Umeå).
Behavioral and psychological symptoms in dementia were measured
using the Neuropsychiatric Inventory (0e144).35 Symptoms of
depression were assessed using the 15-item Geriatric Depression Scale
(0e15).36 Electronic records of past medical history,which included
brain imaging in most cases,current pharmaceutical treatment,and
assessment results,were used to record dementia type,depressive
disorders,and delirium diagnoses.A specialist in geriatric medicine
reviewed and confirmed these diagnoses according to DSM-IV-TR
criteria.23 Balance was measured using the Berg Balance Scale (BBS,
0e56)37 at baseline,and on intervention completion.Data on fall-
related injuries was collected in conjunction with falls over
16 months in total. All injuries related to falls were classified according
to maximum severity using the abbreviated injury scale38: injuries
limited to superficial wounds and bruises as minor;intermediate-
level injuries, such as head injuries,vertebral,wrist or ankle frac-
tures as moderate; and major fractures, such as hip fractures and other
femoral fractures as serious.
Data Analysis
Baseline characteristics were summarized as means (standard de-
viation) or frequencies (percentages).An a priori strategy for the se-
lection of adjusting variables was adhered to.Comparisons between
exercise and attention control groups were conducted for all variables
in Table 1 (preselected as possible confounders) using Student t-test or
Pearsonc2 test,in addition to associations (r 0.3) with fall rate at 6
and 12 months using Pearson correlation coefficient.No variables
differed significantly between groups at baseline bar antidepressant use
(P ¼ .04), which was adjusted for in analyses. No variable was found to
associate with change in outcome measures above predefined levels.
In an intention-to-treat approach, all available data for participants
were analyzed according to original allocation and regardless of level
of attendance. Incidence rates (IRs) for falls were calculated in relation
to person-year using number ofobservation days,deducting 9107
(16%) days absent in cases of relocation or death.Negative binomial
regression was used to analyze the IR ratio (IRR) of falls between ex-
ercise and attention control groups for the different time periods, with
observation days as exposure term and adjusted for age,sex,antide-
pressants,and cluster.Negative binomialregression analysis is rec-
ommended when fitting models for count data that has a Poisson
distribution and are also over-dispersed (the variance exceeds the
mean).39
Subgroup comparisons according to type of dementia, longitudinal
change in balance,and sex were conducted.Differences in effects on
fall rate in subgroups were analyzed by adding an interaction term to
adjusted models.Dementia type was dichotomized into Alzheimer’s
disease vs all other (non-Alzheimer’s disease) types of dementias18
; in
part to aid comparison of results with studies that include participants
with Alzheimer’s disease only,and also because previous studies
indicate that relevant differences between these 2 dementia sub-
groups may exist.5,18Change in functional balance was based on the
median difference in the BBS (post- minus preintervention) in the
total sample, and defined as a BBS score of 2.20
In additional analyses, logistic regression was used to compare fall-
related risk of moderate/serious vs no/minor injuries, adjusted for age,
sex, and antidepressants, between exercise and control groups.
All analyses were performed using IBM SPSS statistics for Macin-
tosh v 23.0 (IBM Corp.Armonk, NY.) and StataCorp.2013.Stata Sta-
tistical Software for Macintosh: Release 13.1.(StataCorp LP,College
Station, TX). All statistical tests were 2 tailed and a P value of < .05 was
considered to be statistically significant.
Results
In total, 141 women and 45 men, with mean standard deviation
(SD) age of 85.1 7.1 years and a MMSE score of 14.9 3.5 were
included (Table 1).Sixty-seven (36.0%) participants had Alzheimer’s
disease and 119 (64%)had non-Alzheimer’s disease;of which 77
participants had vascular dementia, 15 mixed Alzheimer’s disease and
vascular dementia,and 27 had other types of dementia.Over the
4-month intervention period,adherence in the exercise group was
73% and in the attention control group, 70%.
Data on falls during follow-up is summarized in Table 2.In total
during the 12-month follow-up, 34 (19%) of the participants fell once
and 84 (48%) fell at least twice. The number of falls per person ranged
from 0 to 28.There was no difference in fall rate (IRR) between ex-
ercise and control group at either 6- or 12-month follow-up [IRR 0.9,
95% confidence interval(CI) 0.5e1.7,P ¼ .838 and IRR 0.9,95% CI
0.5e1.6,P ¼ .782,respectively; Table 2,Figure 2].No differences in
exercise effects on falls were found according to sex, dementia type, or
change in balance (Table 3). Of 473 falls, 271 (57%) resulted in no injury
(128 and 143 in exercise and controlgroup, respectively) and 173
(37%)in minor injury (92 and 81 in exercise and control group,
respectively).In 10 (2%) of the falls (7 and 3 in exercise and control
group, respectively), a differentiation between no or mild injury could
not be determined because of insufficient documentation. Eleven (2%)
of the falls resulted in moderate injury; 1 injury in the exercise group
(patella fracture) vs 10 injuries in the control group (3 pelvic fractures,
1 patella fracture,2 ribcage fractures,1 elbow fracture,1 vertebral
compression fracture, and 2 humerus fractures). Eight (2%) of the falls
resulted in serious injury (4 hip fractures in exercise and control
groups each).Of the 19 participants with moderate to serious inju-
rious falls, 18 required a visit or admission to a hospital (5 in the ex-
ercise group and 13 in the control group).
During the intervention, no difference in fall rate between exercise
and controlgroup was observed (IRR 1.2,95% CI 0.8e2.0,P ¼ .398;
SupplementalTable 1, Figure 2). No falls occurred during activity
sessions. Interaction analyses indicated a difference in falls according
to dementia type during the intervention (IRR 2.6,95% CI1.0e6.7,
P ¼ .048), where participants with Alzheimer’s disease in the exercise
group fell more than the controlgroup (SupplementalTable 1).No
difference in exercise effects on falls according to sex was found
(Supplemental Table 1).Of the 190 falls that occurred in the exercise
and control group,87 (46%) resulted in no injury (52 and 35 in the
respective groups)and 92 (48%) in minor injury (50 and 42 in
respective groups).In 2 (1%) of the falls (1 in exercise and control
groups each), a differentiation between no or mild injury could not be
A. Toots et al./ JAMDA 20 (2019) 835e842838
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
determined because of insufficient documentation. Six (3%) of the falls
resulted in moderate injury (3 each in exercise and control groups).
Three (2%) of the falls resulted in serious injury (1 hip fracture in the
exercise and 2 in the control group).
Participants in the exercise group were less likely to sustain
moderate or serious injuries as a result of falls during the 12-month
follow-up [odds ratio (OR) 0.31, 95%CI 0.10e0.94, P ¼ .039;
Supplemental Table 2]. No differences between groups were observed
at the 6-month follow-up (OR 0.98,95% CI0.19e5.18,P ¼ .980) or
during the intervention (OR 0.23, 95% CI 0.23e4.02, P ¼ .946).
Discussion
This study of people with dementia living in nursing homes
observed no exercise effects on fallrate compared with a control
activity,independent of sex or change in balance.However,during
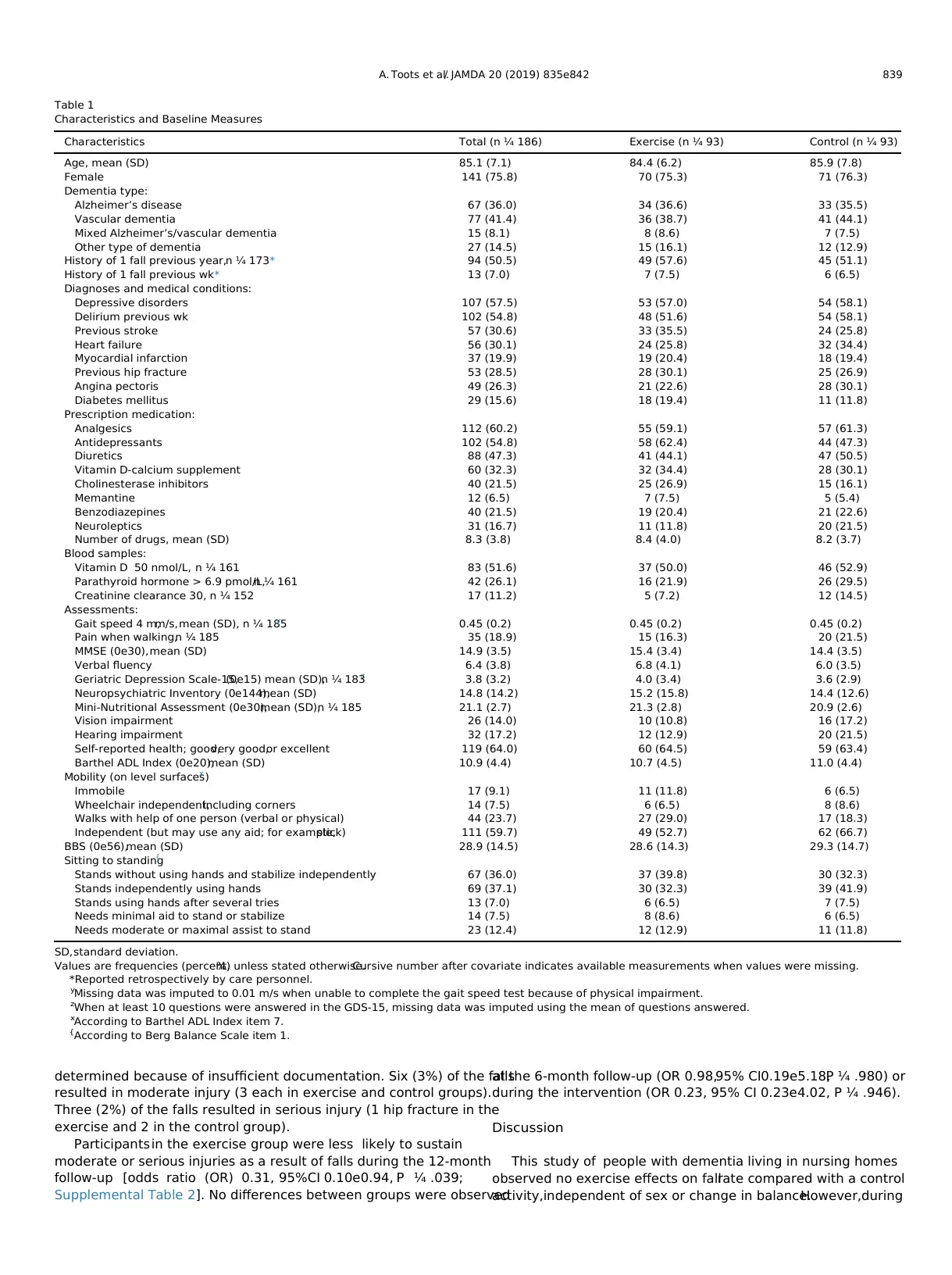
Table 1
Characteristics and Baseline Measures
Characteristics Total (n ¼ 186) Exercise (n ¼ 93) Control (n ¼ 93)
Age, mean (SD) 85.1 (7.1) 84.4 (6.2) 85.9 (7.8)
Female 141 (75.8) 70 (75.3) 71 (76.3)
Dementia type:
Alzheimer’s disease 67 (36.0) 34 (36.6) 33 (35.5)
Vascular dementia 77 (41.4) 36 (38.7) 41 (44.1)
Mixed Alzheimer’s/vascular dementia 15 (8.1) 8 (8.6) 7 (7.5)
Other type of dementia 27 (14.5) 15 (16.1) 12 (12.9)
History of 1 fall previous year,n ¼ 173* 94 (50.5) 49 (57.6) 45 (51.1)
History of 1 fall previous wk* 13 (7.0) 7 (7.5) 6 (6.5)
Diagnoses and medical conditions:
Depressive disorders 107 (57.5) 53 (57.0) 54 (58.1)
Delirium previous wk 102 (54.8) 48 (51.6) 54 (58.1)
Previous stroke 57 (30.6) 33 (35.5) 24 (25.8)
Heart failure 56 (30.1) 24 (25.8) 32 (34.4)
Myocardial infarction 37 (19.9) 19 (20.4) 18 (19.4)
Previous hip fracture 53 (28.5) 28 (30.1) 25 (26.9)
Angina pectoris 49 (26.3) 21 (22.6) 28 (30.1)
Diabetes mellitus 29 (15.6) 18 (19.4) 11 (11.8)
Prescription medication:
Analgesics 112 (60.2) 55 (59.1) 57 (61.3)
Antidepressants 102 (54.8) 58 (62.4) 44 (47.3)
Diuretics 88 (47.3) 41 (44.1) 47 (50.5)
Vitamin D-calcium supplement 60 (32.3) 32 (34.4) 28 (30.1)
Cholinesterase inhibitors 40 (21.5) 25 (26.9) 15 (16.1)
Memantine 12 (6.5) 7 (7.5) 5 (5.4)
Benzodiazepines 40 (21.5) 19 (20.4) 21 (22.6)
Neuroleptics 31 (16.7) 11 (11.8) 20 (21.5)
Number of drugs, mean (SD) 8.3 (3.8) 8.4 (4.0) 8.2 (3.7)
Blood samples:
Vitamin D 50 nmol/L, n ¼ 161 83 (51.6) 37 (50.0) 46 (52.9)
Parathyroid hormone > 6.9 pmol/L,n ¼ 161 42 (26.1) 16 (21.9) 26 (29.5)
Creatinine clearance 30, n ¼ 152 17 (11.2) 5 (7.2) 12 (14.5)
Assessments:
Gait speed 4 m,m/s,mean (SD), n ¼ 185y 0.45 (0.2) 0.45 (0.2) 0.45 (0.2)
Pain when walking,n ¼ 185 35 (18.9) 15 (16.3) 20 (21.5)
MMSE (0e30),mean (SD) 14.9 (3.5) 15.4 (3.4) 14.4 (3.5)
Verbal fluency 6.4 (3.8) 6.8 (4.1) 6.0 (3.5)
Geriatric Depression Scale-15,(0e15) mean (SD),n ¼ 183z 3.8 (3.2) 4.0 (3.4) 3.6 (2.9)
Neuropsychiatric Inventory (0e144),mean (SD) 14.8 (14.2) 15.2 (15.8) 14.4 (12.6)
Mini-Nutritional Assessment (0e30),mean (SD),n ¼ 185 21.1 (2.7) 21.3 (2.8) 20.9 (2.6)
Vision impairment 26 (14.0) 10 (10.8) 16 (17.2)
Hearing impairment 32 (17.2) 12 (12.9) 20 (21.5)
Self-reported health; good,very good,or excellent 119 (64.0) 60 (64.5) 59 (63.4)
Barthel ADL Index (0e20),mean (SD) 10.9 (4.4) 10.7 (4.5) 11.0 (4.4)
Mobility (on level surfaces)x
Immobile 17 (9.1) 11 (11.8) 6 (6.5)
Wheelchair independent,including corners 14 (7.5) 6 (6.5) 8 (8.6)
Walks with help of one person (verbal or physical) 44 (23.7) 27 (29.0) 17 (18.3)
Independent (but may use any aid; for example,stick) 111 (59.7) 49 (52.7) 62 (66.7)
BBS (0e56),mean (SD) 28.9 (14.5) 28.6 (14.3) 29.3 (14.7)
Sitting to standing{
Stands without using hands and stabilize independently 67 (36.0) 37 (39.8) 30 (32.3)
Stands independently using hands 69 (37.1) 30 (32.3) 39 (41.9)
Stands using hands after several tries 13 (7.0) 6 (6.5) 7 (7.5)
Needs minimal aid to stand or stabilize 14 (7.5) 8 (8.6) 6 (6.5)
Needs moderate or maximal assist to stand 23 (12.4) 12 (12.9) 11 (11.8)
SD,standard deviation.
Values are frequencies (percent,%) unless stated otherwise.Cursive number after covariate indicates available measurements when values were missing.
*Reported retrospectively by care personnel.
y
Missing data was imputed to 0.01 m/s when unable to complete the gait speed test because of physical impairment.
z
When at least 10 questions were answered in the GDS-15, missing data was imputed using the mean of questions answered.
x
According to Barthel ADL Index item 7.
{
According to Berg Balance Scale item 1.
A. Toots et al./ JAMDA 20 (2019) 835e842 839
resulted in moderate injury (3 each in exercise and control groups).
Three (2%) of the falls resulted in serious injury (1 hip fracture in the
exercise and 2 in the control group).
Participants in the exercise group were less likely to sustain
moderate or serious injuries as a result of falls during the 12-month
follow-up [odds ratio (OR) 0.31, 95%CI 0.10e0.94, P ¼ .039;
Supplemental Table 2]. No differences between groups were observed
at the 6-month follow-up (OR 0.98,95% CI0.19e5.18,P ¼ .980) or
during the intervention (OR 0.23, 95% CI 0.23e4.02, P ¼ .946).
Discussion
This study of people with dementia living in nursing homes
observed no exercise effects on fallrate compared with a control
activity,independent of sex or change in balance.However,during
Table 1
Characteristics and Baseline Measures
Characteristics Total (n ¼ 186) Exercise (n ¼ 93) Control (n ¼ 93)
Age, mean (SD) 85.1 (7.1) 84.4 (6.2) 85.9 (7.8)
Female 141 (75.8) 70 (75.3) 71 (76.3)
Dementia type:
Alzheimer’s disease 67 (36.0) 34 (36.6) 33 (35.5)
Vascular dementia 77 (41.4) 36 (38.7) 41 (44.1)
Mixed Alzheimer’s/vascular dementia 15 (8.1) 8 (8.6) 7 (7.5)
Other type of dementia 27 (14.5) 15 (16.1) 12 (12.9)
History of 1 fall previous year,n ¼ 173* 94 (50.5) 49 (57.6) 45 (51.1)
History of 1 fall previous wk* 13 (7.0) 7 (7.5) 6 (6.5)
Diagnoses and medical conditions:
Depressive disorders 107 (57.5) 53 (57.0) 54 (58.1)
Delirium previous wk 102 (54.8) 48 (51.6) 54 (58.1)
Previous stroke 57 (30.6) 33 (35.5) 24 (25.8)
Heart failure 56 (30.1) 24 (25.8) 32 (34.4)
Myocardial infarction 37 (19.9) 19 (20.4) 18 (19.4)
Previous hip fracture 53 (28.5) 28 (30.1) 25 (26.9)
Angina pectoris 49 (26.3) 21 (22.6) 28 (30.1)
Diabetes mellitus 29 (15.6) 18 (19.4) 11 (11.8)
Prescription medication:
Analgesics 112 (60.2) 55 (59.1) 57 (61.3)
Antidepressants 102 (54.8) 58 (62.4) 44 (47.3)
Diuretics 88 (47.3) 41 (44.1) 47 (50.5)
Vitamin D-calcium supplement 60 (32.3) 32 (34.4) 28 (30.1)
Cholinesterase inhibitors 40 (21.5) 25 (26.9) 15 (16.1)
Memantine 12 (6.5) 7 (7.5) 5 (5.4)
Benzodiazepines 40 (21.5) 19 (20.4) 21 (22.6)
Neuroleptics 31 (16.7) 11 (11.8) 20 (21.5)
Number of drugs, mean (SD) 8.3 (3.8) 8.4 (4.0) 8.2 (3.7)
Blood samples:
Vitamin D 50 nmol/L, n ¼ 161 83 (51.6) 37 (50.0) 46 (52.9)
Parathyroid hormone > 6.9 pmol/L,n ¼ 161 42 (26.1) 16 (21.9) 26 (29.5)
Creatinine clearance 30, n ¼ 152 17 (11.2) 5 (7.2) 12 (14.5)
Assessments:
Gait speed 4 m,m/s,mean (SD), n ¼ 185y 0.45 (0.2) 0.45 (0.2) 0.45 (0.2)
Pain when walking,n ¼ 185 35 (18.9) 15 (16.3) 20 (21.5)
MMSE (0e30),mean (SD) 14.9 (3.5) 15.4 (3.4) 14.4 (3.5)
Verbal fluency 6.4 (3.8) 6.8 (4.1) 6.0 (3.5)
Geriatric Depression Scale-15,(0e15) mean (SD),n ¼ 183z 3.8 (3.2) 4.0 (3.4) 3.6 (2.9)
Neuropsychiatric Inventory (0e144),mean (SD) 14.8 (14.2) 15.2 (15.8) 14.4 (12.6)
Mini-Nutritional Assessment (0e30),mean (SD),n ¼ 185 21.1 (2.7) 21.3 (2.8) 20.9 (2.6)
Vision impairment 26 (14.0) 10 (10.8) 16 (17.2)
Hearing impairment 32 (17.2) 12 (12.9) 20 (21.5)
Self-reported health; good,very good,or excellent 119 (64.0) 60 (64.5) 59 (63.4)
Barthel ADL Index (0e20),mean (SD) 10.9 (4.4) 10.7 (4.5) 11.0 (4.4)
Mobility (on level surfaces)x
Immobile 17 (9.1) 11 (11.8) 6 (6.5)
Wheelchair independent,including corners 14 (7.5) 6 (6.5) 8 (8.6)
Walks with help of one person (verbal or physical) 44 (23.7) 27 (29.0) 17 (18.3)
Independent (but may use any aid; for example,stick) 111 (59.7) 49 (52.7) 62 (66.7)
BBS (0e56),mean (SD) 28.9 (14.5) 28.6 (14.3) 29.3 (14.7)
Sitting to standing{
Stands without using hands and stabilize independently 67 (36.0) 37 (39.8) 30 (32.3)
Stands independently using hands 69 (37.1) 30 (32.3) 39 (41.9)
Stands using hands after several tries 13 (7.0) 6 (6.5) 7 (7.5)
Needs minimal aid to stand or stabilize 14 (7.5) 8 (8.6) 6 (6.5)
Needs moderate or maximal assist to stand 23 (12.4) 12 (12.9) 11 (11.8)
SD,standard deviation.
Values are frequencies (percent,%) unless stated otherwise.Cursive number after covariate indicates available measurements when values were missing.
*Reported retrospectively by care personnel.
y
Missing data was imputed to 0.01 m/s when unable to complete the gait speed test because of physical impairment.
z
When at least 10 questions were answered in the GDS-15, missing data was imputed using the mean of questions answered.
x
According to Barthel ADL Index item 7.
{
According to Berg Balance Scale item 1.
A. Toots et al./ JAMDA 20 (2019) 835e842 839
the intervention,exercise effects on falls differed according to de-
mentia type, with a higher fall rate in people with Alzheimer’s
disease,which diminished as follow-up proceeded. Although the
risk of sustaining moderate to severe fall-related injuries did not
differ between groups at the interim follow-up,it was lower in the
exercise group at the end.
The lack of a fall preventative exercise effect complies with the
result of a study investigating the effects of exercise as a single
intervention in people with dementia living in nursing homes.40
Furthermore,the result are in line with 3 previous studies in people
with dementia living in the community.12e14 The studies observed
positive effects on physical function, such as muscle strength, balance,
mobility, or fitness,but not falls prevention.That physicalexercise
alone has limited impact on falls in this population is further sub-
stantiated by results from our study,which observed no exercise ef-
fects on falls,neither in the whole group nor amongst participants
who improved their balance.
The risk of falls was high in this study, and likely influenced by the
selection of people with dementia who were relatively ambulant from
a high-risk setting such as nursing homes.In this population where
multimorbidity and polypharmacy is common,additional modifiable
risk factors,for example,related to acute medical conditions or drug
side effects may need to be targeted alongside exercise.4,41Contrary to
single interventions as the one investigated in our study,multifacto-
rial interventions show possible, albeit inconsistent effects in nursing
homes.15A falls preventative effect of a multifactorial intervention has
also been suggested in a study of people with dementia following hip
fracture.42,43 Furthermore,falls prevention has been shown when
cognitive training was incorporated alongside exercise in people with
dementia.44
Although the exercise program did not prevent falls,it may have
had some effect on preventing injuries, including fractures, related to
the fall. Because not all falls result in fractures, the characteristic of the
fall, for example, location of impact and protective responses may be
important determinants ofrelated injuries.45,46 Improved ability to
extend a leg or arm,take a step,or grab onto an object could poten-
tially alter the direction or break the momentum ofthe fall, thus,
influencing the location or energy of impact, and ultimately effecting
the severity of the injury.45 However,previous systematic reviews in
older people have observed diverse results on fracture prevention
from exercise.47,48
Beside the positive effects of exercise,it has been suggested that
ability to ambulate and be physically active may increase the risk of
falls and fall-related injuries, through an increased exposure to high-
risk situations.16,49In our study, activity level was not adjusted for in
analyses, which could explain the lack of effects on fall rate during the
follow-up, as well as during the intervention.It is also noteworthy
that, during the intervention,exercise effects differed according to
dementia type.Amongst participants with Alzheimer’s disease,the
exercise group had a higher rate of falls compared with the control
group.Inferences regarding differences in exercise effects during the
intervention are restricted because falls could have occurred before
reaching optimum exercise effects on physical function, or be a result
of subgroup imbalances, where participants with Alzheimer’s disease
had better balance and mobility but worse cognitive function at the
start of the intervention.18 Nevertheless, the result could indicate that
additional caution is required during exercise interventions in people
with Alzheimer’s disease.
This study had many strengths but also some limitations.It tar-
geted a high-risk population underrepresented in fallpreventative
Fig. 2. Fall rate per person-year throughout intervention and follow-up according to activity group.
Table 2
IRs and IRR of Falls per Person-Year During Follow-Up in Exercise and Control Group
Group Follow-Up 6 Mo Follow-Up 12 Mo
1 Fall n (%)* Total Falls (Obs d) IR IRR (95% CI)y P 1 Fall n (%) Total Falls (Obs d) IR IRR (95% CI)y P
Exercise,n ¼ 87 45 (52) 111 (14 967) 2.7 0.9 (0.5,1.7) .838 57 (66) 232 (27 830) 3.0 0.9 (0.5,1.6) .782
Control,n ¼ 89 42 (47) 113 (14 746) 2.8 1 (reference) 61 (69) 241 (27 479) 3.2 1 (reference)
Obs d,observation days.
*Number of participants (proportion) who fell at least once.
y
From negative binomial regression analyses with observation days as exposure term and adjusted for age,sex, antidepressants and cluster.
A. Toots et al./ JAMDA 20 (2019) 835e842840
mentia type, with a higher fall rate in people with Alzheimer’s
disease,which diminished as follow-up proceeded. Although the
risk of sustaining moderate to severe fall-related injuries did not
differ between groups at the interim follow-up,it was lower in the
exercise group at the end.
The lack of a fall preventative exercise effect complies with the
result of a study investigating the effects of exercise as a single
intervention in people with dementia living in nursing homes.40
Furthermore,the result are in line with 3 previous studies in people
with dementia living in the community.12e14 The studies observed
positive effects on physical function, such as muscle strength, balance,
mobility, or fitness,but not falls prevention.That physicalexercise
alone has limited impact on falls in this population is further sub-
stantiated by results from our study,which observed no exercise ef-
fects on falls,neither in the whole group nor amongst participants
who improved their balance.
The risk of falls was high in this study, and likely influenced by the
selection of people with dementia who were relatively ambulant from
a high-risk setting such as nursing homes.In this population where
multimorbidity and polypharmacy is common,additional modifiable
risk factors,for example,related to acute medical conditions or drug
side effects may need to be targeted alongside exercise.4,41Contrary to
single interventions as the one investigated in our study,multifacto-
rial interventions show possible, albeit inconsistent effects in nursing
homes.15A falls preventative effect of a multifactorial intervention has
also been suggested in a study of people with dementia following hip
fracture.42,43 Furthermore,falls prevention has been shown when
cognitive training was incorporated alongside exercise in people with
dementia.44
Although the exercise program did not prevent falls,it may have
had some effect on preventing injuries, including fractures, related to
the fall. Because not all falls result in fractures, the characteristic of the
fall, for example, location of impact and protective responses may be
important determinants ofrelated injuries.45,46 Improved ability to
extend a leg or arm,take a step,or grab onto an object could poten-
tially alter the direction or break the momentum ofthe fall, thus,
influencing the location or energy of impact, and ultimately effecting
the severity of the injury.45 However,previous systematic reviews in
older people have observed diverse results on fracture prevention
from exercise.47,48
Beside the positive effects of exercise,it has been suggested that
ability to ambulate and be physically active may increase the risk of
falls and fall-related injuries, through an increased exposure to high-
risk situations.16,49In our study, activity level was not adjusted for in
analyses, which could explain the lack of effects on fall rate during the
follow-up, as well as during the intervention.It is also noteworthy
that, during the intervention,exercise effects differed according to
dementia type.Amongst participants with Alzheimer’s disease,the
exercise group had a higher rate of falls compared with the control
group.Inferences regarding differences in exercise effects during the
intervention are restricted because falls could have occurred before
reaching optimum exercise effects on physical function, or be a result
of subgroup imbalances, where participants with Alzheimer’s disease
had better balance and mobility but worse cognitive function at the
start of the intervention.18 Nevertheless, the result could indicate that
additional caution is required during exercise interventions in people
with Alzheimer’s disease.
This study had many strengths but also some limitations.It tar-
geted a high-risk population underrepresented in fallpreventative
Fig. 2. Fall rate per person-year throughout intervention and follow-up according to activity group.
Table 2
IRs and IRR of Falls per Person-Year During Follow-Up in Exercise and Control Group
Group Follow-Up 6 Mo Follow-Up 12 Mo
1 Fall n (%)* Total Falls (Obs d) IR IRR (95% CI)y P 1 Fall n (%) Total Falls (Obs d) IR IRR (95% CI)y P
Exercise,n ¼ 87 45 (52) 111 (14 967) 2.7 0.9 (0.5,1.7) .838 57 (66) 232 (27 830) 3.0 0.9 (0.5,1.6) .782
Control,n ¼ 89 42 (47) 113 (14 746) 2.8 1 (reference) 61 (69) 241 (27 479) 3.2 1 (reference)
Obs d,observation days.
*Number of participants (proportion) who fell at least once.
y
From negative binomial regression analyses with observation days as exposure term and adjusted for age,sex, antidepressants and cluster.
A. Toots et al./ JAMDA 20 (2019) 835e842840
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
exercise trials and had few exclusion criteria. However, generalization
may be restricted to the more ambulant portion of people with de-
mentia living in nursing homes.The incidence of falls was collected
through a review of falls reports,and a review of medical records at
the nursing homes and at the regionalcounty councilhealth care
provider, all conducted by blinded reviewers. Thus, even if the number
of falls were reliant on adequate reporting by nursing staff,the thor-
ough review reduced the number of missed fall events.Though the
structured exercise program is consistentwith falls, preventative
recommendations regarding exercise mode, intensity,and frequency,
effects may not have reached sufficient levels to prevent falls. Despite
the improvements in balance observed, a higher dose of exercise may
be required for greater effects on falls. In addition, sample size
simulation was based on a 30% reduction in fall rate compared with
the control group, which was not accomplished in this study and
implies limited statistical power.
Conclusions/Relevance
The findings from this study suggestthat compared with an
attention controlactivity,a high-intensity functionalexercise pro-
gram,as a single intervention,does not prevent falls in people with
dementia living in nursing homes. The result supports previous
research suggesting that in high-risk populations where,as in this
study,multimorbidity and polypharmacy are common,a multifacto-
rial fall-prevention approach may be required.Caution may be indi-
cated in people with Alzheimer’s disease when the exercise
intervention is on-going.The study observed encouraging effects on
fall-related injuries, which merits future investigations.
Acknowledgments
We thank all who contributed to data collection and imple-
mentation of the UMDEX study, as well as, the Social Authorities of the
municipality of Umeå,care staff,and participants.
References
1. Allan LM, Ballard CG,Rowan EN,et al.Incidence and prediction of falls in de-
mentia: A prospective study in older people.PLoS One 2009;4:e5521.
2. Baker NL,Cook MN, Arrighi HM, et al. Hip fracture risk and subsequent mor-
tality among Alzheimer’s disease patients in the United Kingdom,1988e2007.
Age Ageing 2011;40:49e54.
3. van Doorn C,Gruber-Baldini AL,Zimmerman S,et al.Dementia as a risk factor
for falls and fall injuries among nursing home residents. J Am Geriatr Soc 2003;
51:1213e1218.
4. Perttila NM, Ohman H, Strandberg TE,et al. How do community-dwelling
persons with Alzheimer disease fall? Falls in the FINALEX Study. Dement
Geriatr Cogn Dis Extra 2017;7:195e203.
5. Allali G, Launay CP,Blumen HM, et al. Falls, Cognitive impairment,and gait
performance: Results from the good initiative.J Am Med Dir Assoc 2017;18:
335e340.
6. Rapp K, Buchele G,Dreinhofer K, et al. Epidemiology ofhip fractures: Sys-
tematic literature review of German data and an overview of the international
literature.Z Gerontol Geriatr 2019;52:10e16.
7. Scandol JP,Toson B,Close JC.Fall-related hip fracture hospitalisations and the
prevalence of dementia within older people in New South Wales, Australia: An
analysis of linked data.Injury 2013;44:776e783.
8. Seitz DP, Gill SS, Gruneir A, et al. Effects of dementia on postoperative outcomes
of older adults with hip fractures: A population-based study.J Am Med Dir
Assoc 2014;15:334e341.
9. Gillespie LD,Robertson MC,Gillespie WJ, et al. Interventions for preventing
falls in older people living in the community.Cochrane Database Syst Rev;
2012:CD007146.
10. Sherrington C,Michaleff ZA,Fairhall N,et al.Exercise to prevent falls in older
adults: An updated systematic review and meta-analysis. Br J Sports Med 2017;
51:1750e1758.
11. Chan WC, Yeung JW, Wong CS, et al. Efficacy of physical exercise in preventing
falls in older adults with cognitive impairment: A systematic review and meta-
analysis.J Am Med Dir Assoc 2015;16:149e154.
12. Suttanon P, Hill KD,Said CM, et al. Feasibility,safety and preliminary evidence
of the effectiveness of a home-based exercise programme for older people with
Alzheimer’s disease: A pilot randomized controlled trial. Clin Rehabil 2013;27:
427e438.
13. Lamb SE,Sheehan B,Atherton N,et al.Dementia and Physical Activity (DAPA)
trial of moderate to high intensity exercise training for people with dementia:
Randomised controlled trial.BMJ 2018;361:k1675.
14. Zieschang T, Schwenk M, Becker C, et al. Falls and physical activity in
persons with mild to moderate dementia participating in an intensive motor
training: Randomized controlled trial.Alzheimer Dis Assoc Disord 2017;31:
307e314.
15. Cameron ID, Gillespie LD, Robertson MC, et al. Interventions for preventing falls
in older people in care facilities and hospitals.Cochrane Database Syst Rev
2012;12:CD005465.
16. Lord SR,March LM,Cameron ID,et al.Differing risk factors for falls in nursing
home and intermediate-care residents who can and cannotstand unaided.
J Am Geriatr Soc 2003;51:1645e1650.
17. Wiklund R, Toots A, Conradsson M, et al. Risk factors for hip fracture in very old
people: A population-based study.Osteoporos Int 2016;27:923e931.
18. Toots A, Littbrand H, Lindelöf N, et al. Effects ofa high-intensity functional
exercise program on dependence in activities ofdaily living and balance in
older adults with dementia.J Am Geriatr Soc 2016;64:55e64.
Table 3
IRs and IRRs of Falls per Person-Year During Follow-Up in Exercise and Control Group According to Subgroups
Subgroup Follow-Up 6 Mo Follow-Up 12 Mo
1 Fall
n (%)*
Total Falls
(Obs d)
IR IRR
(95% CI)y
Interaction
(95% CI)y
P 1 fall
n (%)
Total Falls
(Obs d)
IR IRR
(95% CI)y
Interaction
(95% CI)y
P
Sex
Exercise women,n ¼ 64 34 (53) 94 (11132) 3.1 1.1 (0.7,1.8) 2.2 (0.7,7.3) .181 41 (64) 170 (20933) 3.0 0.9 (0.5,1.5) 0.7 (0.2,2.2) .563
Control women,n ¼ 70 33 (47) 82 (11591) 2.6 1 (reference) 47 (67) 188 (21452) 3.2 1 (reference)
Exercise men, n ¼ 23 11 (48) 17 (3835) 1.6 0.6 (0.3,1.3) 16 (70) 62 (6 897) 3.3 1.1 (0.6,2.26)
Control men, n ¼ 19 9 (47) 31 (3155) 3.6 1.3 (0.5,3.2) 14 (74) 53 (6 027) 3.2 1.0 (0.4,2.1)
Dementia type
Exercise Alzheimer’s
disease,n ¼ 32
15 (47) 49 (5631) 3.2 1.5 (0.6,3.8) 2.0 (0.6,6.6) .239 19 (59) 98 (10536) 3.4 1.1 (0.5,2.5) 1.3 (0.5,3.5) .634
Control Alzheimer’s
disease,n ¼ 33
13 (39) 28 (5493) 1.9 1 (reference) 26 (79) 79 (10286) 2.8 1 (reference)
Exercise non-Alzheimer’s
disease,n ¼ 55
30 (55) 62 (9336) 2.4 1.3 (0.6,2.6) 38 (69) 134 (17294) 2.8 1.0 (0.5,1.8)
Control non-Alzheimer’s
disease,n ¼ 56
29 (52) 85 (9253) 3.4 1.7 (0.7,4.3) 35 (63) 162 (17193) 3.4 1.2 (0.7,2.0)
Change in balance
Exercise BBS 2, n ¼ 50 28 (56) 67 (8623) 2.8 1.3 (0.8,2.2) 1.7 (0.6,4.9) .303 34 (68) 145 (16393) 3.2 1.3 (0.7,2.4) 1.7 (0.7,4.2) .286
Control BBS 2, n ¼ 26 17 (65) 28 (4543) 2.3 1 (reference) 20 (77) 63 (8401) 2.7 1 (reference)
Exercise BBS 1, n ¼ 31 13 (42) 38 (5572) 2.5 1.1 (0.6,2.3) 19 (61) 80 (10080) 2.9 1.1 (0.6,2.2)
Control BBS 1, n ¼ 60 24 (40) 81 (9810) 3.0 1.5 (0.7,3.2) 40 (67) 173 (18387) 3.4 1.4 (0.7,2.8)
non-Alzheimer’s disease,vascular dementia,mixed Alzheimer’s disease and vascular dementia,and other types of dementia; obs d,observation days.
*Number of participants (proportion) who fell at least once.
y
From negative binomial regression analyses with observation days as exposure term and adjusted for age,sex, antidepressants,and cluster.
A. Toots et al./ JAMDA 20 (2019) 835e842 841
may be restricted to the more ambulant portion of people with de-
mentia living in nursing homes.The incidence of falls was collected
through a review of falls reports,and a review of medical records at
the nursing homes and at the regionalcounty councilhealth care
provider, all conducted by blinded reviewers. Thus, even if the number
of falls were reliant on adequate reporting by nursing staff,the thor-
ough review reduced the number of missed fall events.Though the
structured exercise program is consistentwith falls, preventative
recommendations regarding exercise mode, intensity,and frequency,
effects may not have reached sufficient levels to prevent falls. Despite
the improvements in balance observed, a higher dose of exercise may
be required for greater effects on falls. In addition, sample size
simulation was based on a 30% reduction in fall rate compared with
the control group, which was not accomplished in this study and
implies limited statistical power.
Conclusions/Relevance
The findings from this study suggestthat compared with an
attention controlactivity,a high-intensity functionalexercise pro-
gram,as a single intervention,does not prevent falls in people with
dementia living in nursing homes. The result supports previous
research suggesting that in high-risk populations where,as in this
study,multimorbidity and polypharmacy are common,a multifacto-
rial fall-prevention approach may be required.Caution may be indi-
cated in people with Alzheimer’s disease when the exercise
intervention is on-going.The study observed encouraging effects on
fall-related injuries, which merits future investigations.
Acknowledgments
We thank all who contributed to data collection and imple-
mentation of the UMDEX study, as well as, the Social Authorities of the
municipality of Umeå,care staff,and participants.
References
1. Allan LM, Ballard CG,Rowan EN,et al.Incidence and prediction of falls in de-
mentia: A prospective study in older people.PLoS One 2009;4:e5521.
2. Baker NL,Cook MN, Arrighi HM, et al. Hip fracture risk and subsequent mor-
tality among Alzheimer’s disease patients in the United Kingdom,1988e2007.
Age Ageing 2011;40:49e54.
3. van Doorn C,Gruber-Baldini AL,Zimmerman S,et al.Dementia as a risk factor
for falls and fall injuries among nursing home residents. J Am Geriatr Soc 2003;
51:1213e1218.
4. Perttila NM, Ohman H, Strandberg TE,et al. How do community-dwelling
persons with Alzheimer disease fall? Falls in the FINALEX Study. Dement
Geriatr Cogn Dis Extra 2017;7:195e203.
5. Allali G, Launay CP,Blumen HM, et al. Falls, Cognitive impairment,and gait
performance: Results from the good initiative.J Am Med Dir Assoc 2017;18:
335e340.
6. Rapp K, Buchele G,Dreinhofer K, et al. Epidemiology ofhip fractures: Sys-
tematic literature review of German data and an overview of the international
literature.Z Gerontol Geriatr 2019;52:10e16.
7. Scandol JP,Toson B,Close JC.Fall-related hip fracture hospitalisations and the
prevalence of dementia within older people in New South Wales, Australia: An
analysis of linked data.Injury 2013;44:776e783.
8. Seitz DP, Gill SS, Gruneir A, et al. Effects of dementia on postoperative outcomes
of older adults with hip fractures: A population-based study.J Am Med Dir
Assoc 2014;15:334e341.
9. Gillespie LD,Robertson MC,Gillespie WJ, et al. Interventions for preventing
falls in older people living in the community.Cochrane Database Syst Rev;
2012:CD007146.
10. Sherrington C,Michaleff ZA,Fairhall N,et al.Exercise to prevent falls in older
adults: An updated systematic review and meta-analysis. Br J Sports Med 2017;
51:1750e1758.
11. Chan WC, Yeung JW, Wong CS, et al. Efficacy of physical exercise in preventing
falls in older adults with cognitive impairment: A systematic review and meta-
analysis.J Am Med Dir Assoc 2015;16:149e154.
12. Suttanon P, Hill KD,Said CM, et al. Feasibility,safety and preliminary evidence
of the effectiveness of a home-based exercise programme for older people with
Alzheimer’s disease: A pilot randomized controlled trial. Clin Rehabil 2013;27:
427e438.
13. Lamb SE,Sheehan B,Atherton N,et al.Dementia and Physical Activity (DAPA)
trial of moderate to high intensity exercise training for people with dementia:
Randomised controlled trial.BMJ 2018;361:k1675.
14. Zieschang T, Schwenk M, Becker C, et al. Falls and physical activity in
persons with mild to moderate dementia participating in an intensive motor
training: Randomized controlled trial.Alzheimer Dis Assoc Disord 2017;31:
307e314.
15. Cameron ID, Gillespie LD, Robertson MC, et al. Interventions for preventing falls
in older people in care facilities and hospitals.Cochrane Database Syst Rev
2012;12:CD005465.
16. Lord SR,March LM,Cameron ID,et al.Differing risk factors for falls in nursing
home and intermediate-care residents who can and cannotstand unaided.
J Am Geriatr Soc 2003;51:1645e1650.
17. Wiklund R, Toots A, Conradsson M, et al. Risk factors for hip fracture in very old
people: A population-based study.Osteoporos Int 2016;27:923e931.
18. Toots A, Littbrand H, Lindelöf N, et al. Effects ofa high-intensity functional
exercise program on dependence in activities ofdaily living and balance in
older adults with dementia.J Am Geriatr Soc 2016;64:55e64.
Table 3
IRs and IRRs of Falls per Person-Year During Follow-Up in Exercise and Control Group According to Subgroups
Subgroup Follow-Up 6 Mo Follow-Up 12 Mo
1 Fall
n (%)*
Total Falls
(Obs d)
IR IRR
(95% CI)y
Interaction
(95% CI)y
P 1 fall
n (%)
Total Falls
(Obs d)
IR IRR
(95% CI)y
Interaction
(95% CI)y
P
Sex
Exercise women,n ¼ 64 34 (53) 94 (11132) 3.1 1.1 (0.7,1.8) 2.2 (0.7,7.3) .181 41 (64) 170 (20933) 3.0 0.9 (0.5,1.5) 0.7 (0.2,2.2) .563
Control women,n ¼ 70 33 (47) 82 (11591) 2.6 1 (reference) 47 (67) 188 (21452) 3.2 1 (reference)
Exercise men, n ¼ 23 11 (48) 17 (3835) 1.6 0.6 (0.3,1.3) 16 (70) 62 (6 897) 3.3 1.1 (0.6,2.26)
Control men, n ¼ 19 9 (47) 31 (3155) 3.6 1.3 (0.5,3.2) 14 (74) 53 (6 027) 3.2 1.0 (0.4,2.1)
Dementia type
Exercise Alzheimer’s
disease,n ¼ 32
15 (47) 49 (5631) 3.2 1.5 (0.6,3.8) 2.0 (0.6,6.6) .239 19 (59) 98 (10536) 3.4 1.1 (0.5,2.5) 1.3 (0.5,3.5) .634
Control Alzheimer’s
disease,n ¼ 33
13 (39) 28 (5493) 1.9 1 (reference) 26 (79) 79 (10286) 2.8 1 (reference)
Exercise non-Alzheimer’s
disease,n ¼ 55
30 (55) 62 (9336) 2.4 1.3 (0.6,2.6) 38 (69) 134 (17294) 2.8 1.0 (0.5,1.8)
Control non-Alzheimer’s
disease,n ¼ 56
29 (52) 85 (9253) 3.4 1.7 (0.7,4.3) 35 (63) 162 (17193) 3.4 1.2 (0.7,2.0)
Change in balance
Exercise BBS 2, n ¼ 50 28 (56) 67 (8623) 2.8 1.3 (0.8,2.2) 1.7 (0.6,4.9) .303 34 (68) 145 (16393) 3.2 1.3 (0.7,2.4) 1.7 (0.7,4.2) .286
Control BBS 2, n ¼ 26 17 (65) 28 (4543) 2.3 1 (reference) 20 (77) 63 (8401) 2.7 1 (reference)
Exercise BBS 1, n ¼ 31 13 (42) 38 (5572) 2.5 1.1 (0.6,2.3) 19 (61) 80 (10080) 2.9 1.1 (0.6,2.2)
Control BBS 1, n ¼ 60 24 (40) 81 (9810) 3.0 1.5 (0.7,3.2) 40 (67) 173 (18387) 3.4 1.4 (0.7,2.8)
non-Alzheimer’s disease,vascular dementia,mixed Alzheimer’s disease and vascular dementia,and other types of dementia; obs d,observation days.
*Number of participants (proportion) who fell at least once.
y
From negative binomial regression analyses with observation days as exposure term and adjusted for age,sex, antidepressants,and cluster.
A. Toots et al./ JAMDA 20 (2019) 835e842 841
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
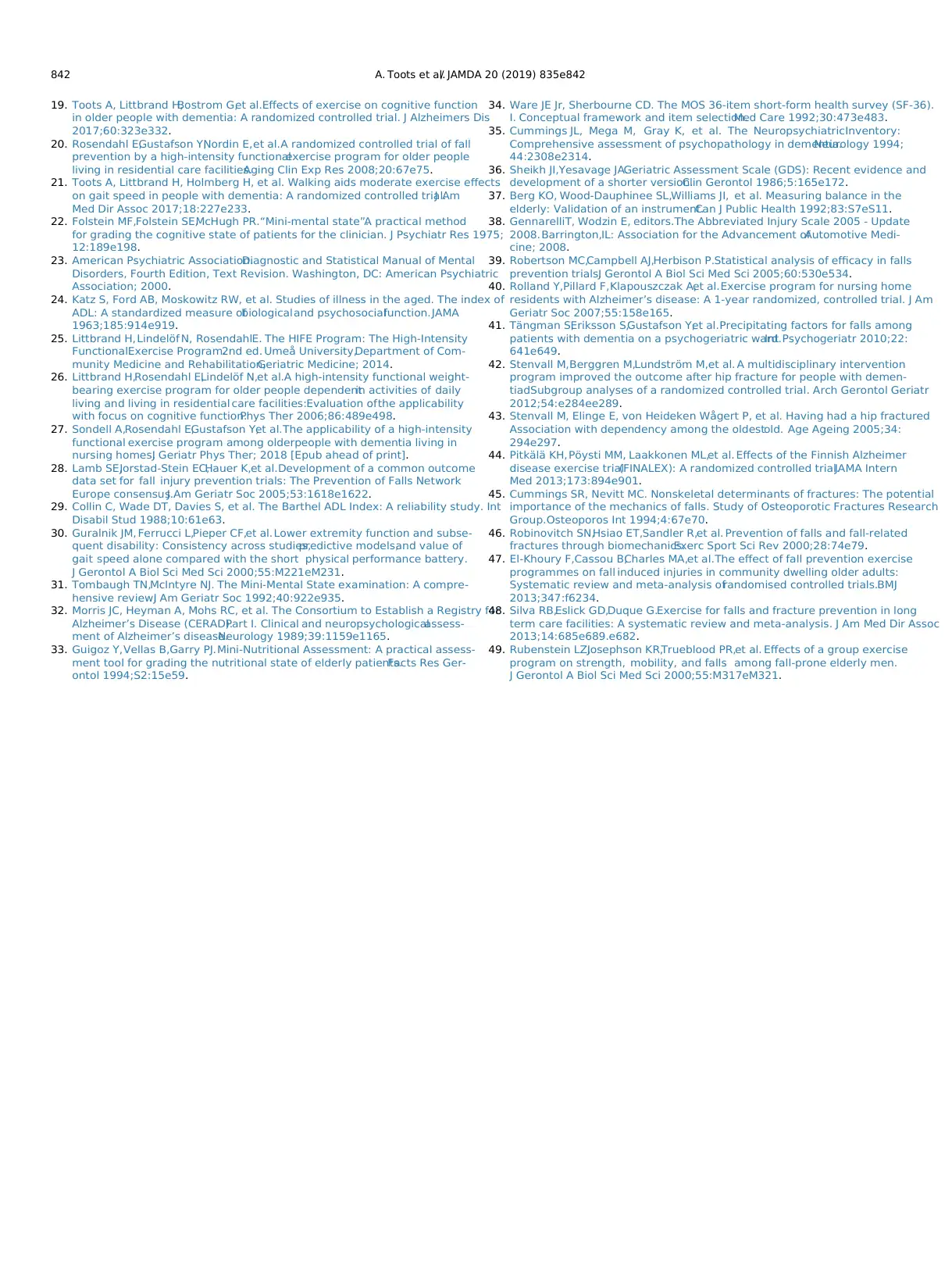
19. Toots A, Littbrand H,Bostrom G,et al.Effects of exercise on cognitive function
in older people with dementia: A randomized controlled trial. J Alzheimers Dis
2017;60:323e332.
20. Rosendahl E,Gustafson Y,Nordin E,et al.A randomized controlled trial of fall
prevention by a high-intensity functionalexercise program for older people
living in residential care facilities.Aging Clin Exp Res 2008;20:67e75.
21. Toots A, Littbrand H, Holmberg H, et al. Walking aids moderate exercise effects
on gait speed in people with dementia: A randomized controlled trial.J Am
Med Dir Assoc 2017;18:227e233.
22. Folstein MF,Folstein SE,McHugh PR.“Mini-mental state”.A practical method
for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;
12:189e198.
23. American Psychiatric Association.Diagnostic and Statistical Manual of Mental
Disorders, Fourth Edition, Text Revision. Washington, DC: American Psychiatric
Association; 2000.
24. Katz S, Ford AB, Moskowitz RW, et al. Studies of illness in the aged. The index of
ADL: A standardized measure ofbiologicaland psychosocialfunction.JAMA
1963;185:914e919.
25. Littbrand H,Lindelöf N, RosendahlE. The HIFE Program: The High-Intensity
FunctionalExercise Program.2nd ed. Umeå University,Department of Com-
munity Medicine and Rehabilitation,Geriatric Medicine; 2014.
26. Littbrand H,Rosendahl E,Lindelöf N,et al.A high-intensity functional weight-
bearing exercise program for older people dependentin activities of daily
living and living in residential care facilities:Evaluation ofthe applicability
with focus on cognitive function.Phys Ther 2006;86:489e498.
27. Sondell A,Rosendahl E,Gustafson Y,et al.The applicability of a high-intensity
functional exercise program among olderpeople with dementia living in
nursing homes.J Geriatr Phys Ther; 2018 [Epub ahead of print].
28. Lamb SE,Jorstad-Stein EC,Hauer K,et al.Development of a common outcome
data set for fall injury prevention trials: The Prevention of Falls Network
Europe consensus.J Am Geriatr Soc 2005;53:1618e1622.
29. Collin C, Wade DT, Davies S, et al. The Barthel ADL Index: A reliability study. Int
Disabil Stud 1988;10:61e63.
30. Guralnik JM, Ferrucci L,Pieper CF,et al.Lower extremity function and subse-
quent disability: Consistency across studies,predictive models,and value of
gait speed alone compared with the short physical performance battery.
J Gerontol A Biol Sci Med Sci 2000;55:M221eM231.
31. Tombaugh TN,McIntyre NJ. The Mini-Mental State examination: A compre-
hensive review.J Am Geriatr Soc 1992;40:922e935.
32. Morris JC, Heyman A, Mohs RC, et al. The Consortium to Establish a Registry for
Alzheimer’s Disease (CERAD).Part I. Clinical and neuropsychologicalassess-
ment of Alzheimer’s disease.Neurology 1989;39:1159e1165.
33. Guigoz Y,Vellas B,Garry PJ.Mini-Nutritional Assessment: A practical assess-
ment tool for grading the nutritional state of elderly patients.Facts Res Ger-
ontol 1994;S2:15e59.
34. Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36).
I. Conceptual framework and item selection.Med Care 1992;30:473e483.
35. Cummings JL, Mega M, Gray K, et al. The NeuropsychiatricInventory:
Comprehensive assessment of psychopathology in dementia.Neurology 1994;
44:2308e2314.
36. Sheikh JI,Yesavage JA.Geriatric Assessment Scale (GDS): Recent evidence and
development of a shorter version.Clin Gerontol 1986;5:165e172.
37. Berg KO, Wood-Dauphinee SL,Williams JI, et al. Measuring balance in the
elderly: Validation of an instrument.Can J Public Health 1992;83:S7eS11.
38. GennarelliT, Wodzin E, editors.The Abbreviated Injury Scale 2005 - Update
2008.Barrington,IL: Association for the Advancement ofAutomotive Medi-
cine; 2008.
39. Robertson MC,Campbell AJ,Herbison P.Statistical analysis of efficacy in falls
prevention trials.J Gerontol A Biol Sci Med Sci 2005;60:530e534.
40. Rolland Y,Pillard F,Klapouszczak A,et al.Exercise program for nursing home
residents with Alzheimer’s disease: A 1-year randomized, controlled trial. J Am
Geriatr Soc 2007;55:158e165.
41. Tängman S,Eriksson S,Gustafson Y,et al.Precipitating factors for falls among
patients with dementia on a psychogeriatric ward.Int Psychogeriatr 2010;22:
641e649.
42. Stenvall M,Berggren M,Lundström M,et al. A multidisciplinary intervention
program improved the outcome after hip fracture for people with demen-
tiadSubgroup analyses of a randomized controlled trial. Arch Gerontol Geriatr
2012;54:e284ee289.
43. Stenvall M, Elinge E, von Heideken Wågert P, et al. Having had a hip fractured
Association with dependency among the oldestold. Age Ageing 2005;34:
294e297.
44. Pitkälä KH, Pöysti MM, Laakkonen ML,et al. Effects of the Finnish Alzheimer
disease exercise trial(FINALEX): A randomized controlled trial.JAMA Intern
Med 2013;173:894e901.
45. Cummings SR, Nevitt MC. Nonskeletal determinants of fractures: The potential
importance of the mechanics of falls. Study of Osteoporotic Fractures Research
Group.Osteoporos Int 1994;4:67e70.
46. Robinovitch SN,Hsiao ET,Sandler R,et al. Prevention of falls and fall-related
fractures through biomechanics.Exerc Sport Sci Rev 2000;28:74e79.
47. El-Khoury F,Cassou B,Charles MA,et al.The effect of fall prevention exercise
programmes on fall induced injuries in community dwelling older adults:
Systematic review and meta-analysis ofrandomised controlled trials.BMJ
2013;347:f6234.
48. Silva RB,Eslick GD,Duque G.Exercise for falls and fracture prevention in long
term care facilities: A systematic review and meta-analysis. J Am Med Dir Assoc
2013;14:685e689.e682.
49. Rubenstein LZ,Josephson KR,Trueblood PR,et al. Effects of a group exercise
program on strength, mobility, and falls among fall-prone elderly men.
J Gerontol A Biol Sci Med Sci 2000;55:M317eM321.
A. Toots et al./ JAMDA 20 (2019) 835e842842
in older people with dementia: A randomized controlled trial. J Alzheimers Dis
2017;60:323e332.
20. Rosendahl E,Gustafson Y,Nordin E,et al.A randomized controlled trial of fall
prevention by a high-intensity functionalexercise program for older people
living in residential care facilities.Aging Clin Exp Res 2008;20:67e75.
21. Toots A, Littbrand H, Holmberg H, et al. Walking aids moderate exercise effects
on gait speed in people with dementia: A randomized controlled trial.J Am
Med Dir Assoc 2017;18:227e233.
22. Folstein MF,Folstein SE,McHugh PR.“Mini-mental state”.A practical method
for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;
12:189e198.
23. American Psychiatric Association.Diagnostic and Statistical Manual of Mental
Disorders, Fourth Edition, Text Revision. Washington, DC: American Psychiatric
Association; 2000.
24. Katz S, Ford AB, Moskowitz RW, et al. Studies of illness in the aged. The index of
ADL: A standardized measure ofbiologicaland psychosocialfunction.JAMA
1963;185:914e919.
25. Littbrand H,Lindelöf N, RosendahlE. The HIFE Program: The High-Intensity
FunctionalExercise Program.2nd ed. Umeå University,Department of Com-
munity Medicine and Rehabilitation,Geriatric Medicine; 2014.
26. Littbrand H,Rosendahl E,Lindelöf N,et al.A high-intensity functional weight-
bearing exercise program for older people dependentin activities of daily
living and living in residential care facilities:Evaluation ofthe applicability
with focus on cognitive function.Phys Ther 2006;86:489e498.
27. Sondell A,Rosendahl E,Gustafson Y,et al.The applicability of a high-intensity
functional exercise program among olderpeople with dementia living in
nursing homes.J Geriatr Phys Ther; 2018 [Epub ahead of print].
28. Lamb SE,Jorstad-Stein EC,Hauer K,et al.Development of a common outcome
data set for fall injury prevention trials: The Prevention of Falls Network
Europe consensus.J Am Geriatr Soc 2005;53:1618e1622.
29. Collin C, Wade DT, Davies S, et al. The Barthel ADL Index: A reliability study. Int
Disabil Stud 1988;10:61e63.
30. Guralnik JM, Ferrucci L,Pieper CF,et al.Lower extremity function and subse-
quent disability: Consistency across studies,predictive models,and value of
gait speed alone compared with the short physical performance battery.
J Gerontol A Biol Sci Med Sci 2000;55:M221eM231.
31. Tombaugh TN,McIntyre NJ. The Mini-Mental State examination: A compre-
hensive review.J Am Geriatr Soc 1992;40:922e935.
32. Morris JC, Heyman A, Mohs RC, et al. The Consortium to Establish a Registry for
Alzheimer’s Disease (CERAD).Part I. Clinical and neuropsychologicalassess-
ment of Alzheimer’s disease.Neurology 1989;39:1159e1165.
33. Guigoz Y,Vellas B,Garry PJ.Mini-Nutritional Assessment: A practical assess-
ment tool for grading the nutritional state of elderly patients.Facts Res Ger-
ontol 1994;S2:15e59.
34. Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36).
I. Conceptual framework and item selection.Med Care 1992;30:473e483.
35. Cummings JL, Mega M, Gray K, et al. The NeuropsychiatricInventory:
Comprehensive assessment of psychopathology in dementia.Neurology 1994;
44:2308e2314.
36. Sheikh JI,Yesavage JA.Geriatric Assessment Scale (GDS): Recent evidence and
development of a shorter version.Clin Gerontol 1986;5:165e172.
37. Berg KO, Wood-Dauphinee SL,Williams JI, et al. Measuring balance in the
elderly: Validation of an instrument.Can J Public Health 1992;83:S7eS11.
38. GennarelliT, Wodzin E, editors.The Abbreviated Injury Scale 2005 - Update
2008.Barrington,IL: Association for the Advancement ofAutomotive Medi-
cine; 2008.
39. Robertson MC,Campbell AJ,Herbison P.Statistical analysis of efficacy in falls
prevention trials.J Gerontol A Biol Sci Med Sci 2005;60:530e534.
40. Rolland Y,Pillard F,Klapouszczak A,et al.Exercise program for nursing home
residents with Alzheimer’s disease: A 1-year randomized, controlled trial. J Am
Geriatr Soc 2007;55:158e165.
41. Tängman S,Eriksson S,Gustafson Y,et al.Precipitating factors for falls among
patients with dementia on a psychogeriatric ward.Int Psychogeriatr 2010;22:
641e649.
42. Stenvall M,Berggren M,Lundström M,et al. A multidisciplinary intervention
program improved the outcome after hip fracture for people with demen-
tiadSubgroup analyses of a randomized controlled trial. Arch Gerontol Geriatr
2012;54:e284ee289.
43. Stenvall M, Elinge E, von Heideken Wågert P, et al. Having had a hip fractured
Association with dependency among the oldestold. Age Ageing 2005;34:
294e297.
44. Pitkälä KH, Pöysti MM, Laakkonen ML,et al. Effects of the Finnish Alzheimer
disease exercise trial(FINALEX): A randomized controlled trial.JAMA Intern
Med 2013;173:894e901.
45. Cummings SR, Nevitt MC. Nonskeletal determinants of fractures: The potential
importance of the mechanics of falls. Study of Osteoporotic Fractures Research
Group.Osteoporos Int 1994;4:67e70.
46. Robinovitch SN,Hsiao ET,Sandler R,et al. Prevention of falls and fall-related
fractures through biomechanics.Exerc Sport Sci Rev 2000;28:74e79.
47. El-Khoury F,Cassou B,Charles MA,et al.The effect of fall prevention exercise
programmes on fall induced injuries in community dwelling older adults:
Systematic review and meta-analysis ofrandomised controlled trials.BMJ
2013;347:f6234.
48. Silva RB,Eslick GD,Duque G.Exercise for falls and fracture prevention in long
term care facilities: A systematic review and meta-analysis. J Am Med Dir Assoc
2013;14:685e689.e682.
49. Rubenstein LZ,Josephson KR,Trueblood PR,et al. Effects of a group exercise
program on strength, mobility, and falls among fall-prone elderly men.
J Gerontol A Biol Sci Med Sci 2000;55:M317eM321.
A. Toots et al./ JAMDA 20 (2019) 835e842842
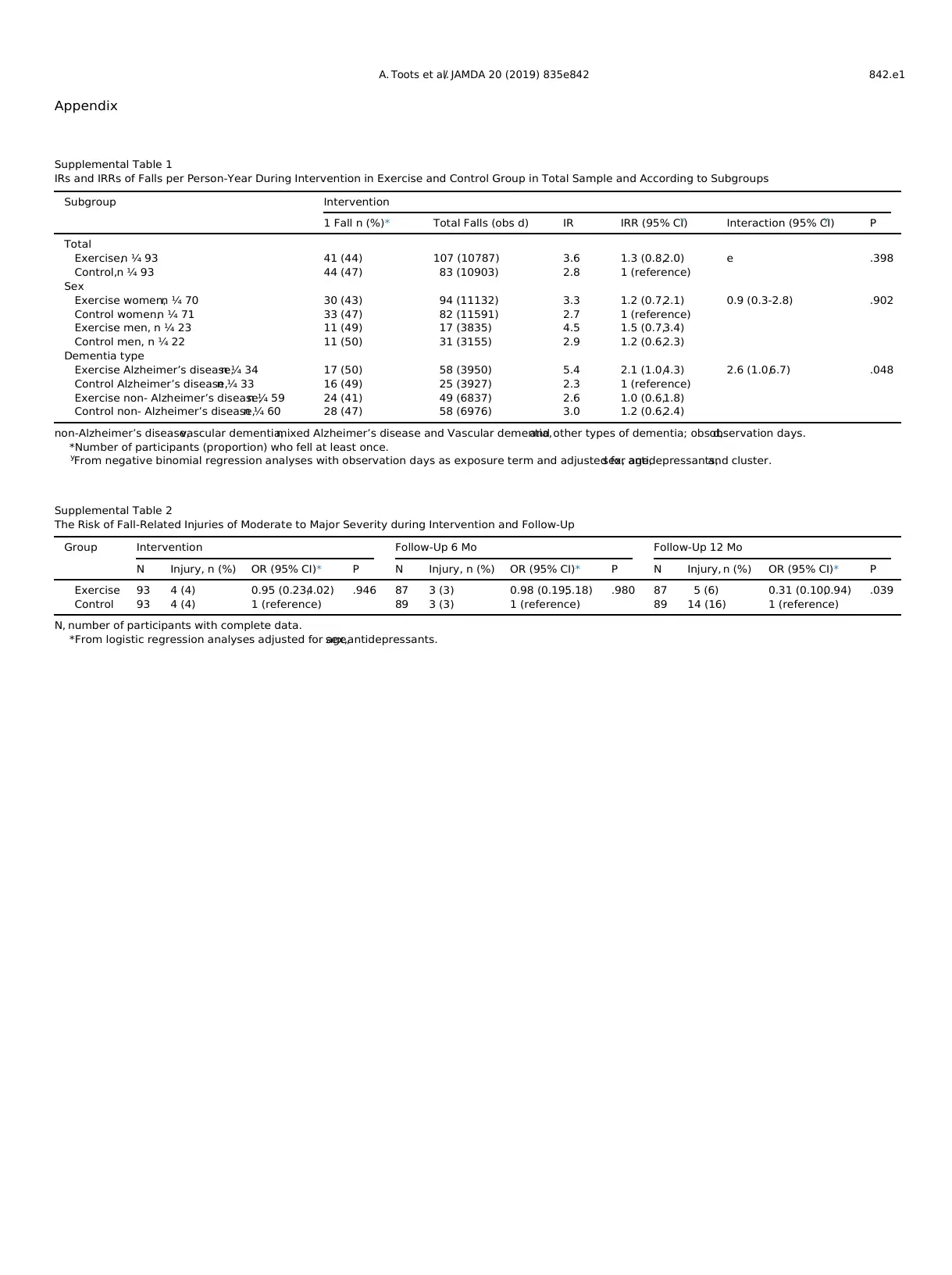
Appendix
Supplemental Table 2
The Risk of Fall-Related Injuries of Moderate to Major Severity during Intervention and Follow-Up
Group Intervention Follow-Up 6 Mo Follow-Up 12 Mo
N Injury, n (%) OR (95% CI)* P N Injury, n (%) OR (95% CI)* P N Injury, n (%) OR (95% CI)* P
Exercise 93 4 (4) 0.95 (0.23,4.02) .946 87 3 (3) 0.98 (0.19,5.18) .980 87 5 (6) 0.31 (0.10,0.94) .039
Control 93 4 (4) 1 (reference) 89 3 (3) 1 (reference) 89 14 (16) 1 (reference)
N, number of participants with complete data.
*From logistic regression analyses adjusted for age,sex,antidepressants.
Supplemental Table 1
IRs and IRRs of Falls per Person-Year During Intervention in Exercise and Control Group in Total Sample and According to Subgroups
Subgroup Intervention
1 Fall n (%)* Total Falls (obs d) IR IRR (95% CI)y Interaction (95% CI)y P
Total
Exercise,n ¼ 93 41 (44) 107 (10787) 3.6 1.3 (0.8,2.0) e .398
Control,n ¼ 93 44 (47) 83 (10903) 2.8 1 (reference)
Sex
Exercise women,n ¼ 70 30 (43) 94 (11132) 3.3 1.2 (0.7,2.1) 0.9 (0.3-2.8) .902
Control women,n ¼ 71 33 (47) 82 (11591) 2.7 1 (reference)
Exercise men, n ¼ 23 11 (49) 17 (3835) 4.5 1.5 (0.7,3.4)
Control men, n ¼ 22 11 (50) 31 (3155) 2.9 1.2 (0.6,2.3)
Dementia type
Exercise Alzheimer’s disease,n ¼ 34 17 (50) 58 (3950) 5.4 2.1 (1.0,4.3) 2.6 (1.0,6.7) .048
Control Alzheimer’s disease,n ¼ 33 16 (49) 25 (3927) 2.3 1 (reference)
Exercise non- Alzheimer’s disease,n ¼ 59 24 (41) 49 (6837) 2.6 1.0 (0.6,1.8)
Control non- Alzheimer’s disease,n ¼ 60 28 (47) 58 (6976) 3.0 1.2 (0.6,2.4)
non-Alzheimer’s disease,vascular dementia,mixed Alzheimer’s disease and Vascular dementia,and other types of dementia; obs d,observation days.
*Number of participants (proportion) who fell at least once.
y
From negative binomial regression analyses with observation days as exposure term and adjusted for age,sex, antidepressants,and cluster.
A. Toots et al./ JAMDA 20 (2019) 835e842 842.e1
Supplemental Table 2
The Risk of Fall-Related Injuries of Moderate to Major Severity during Intervention and Follow-Up
Group Intervention Follow-Up 6 Mo Follow-Up 12 Mo
N Injury, n (%) OR (95% CI)* P N Injury, n (%) OR (95% CI)* P N Injury, n (%) OR (95% CI)* P
Exercise 93 4 (4) 0.95 (0.23,4.02) .946 87 3 (3) 0.98 (0.19,5.18) .980 87 5 (6) 0.31 (0.10,0.94) .039
Control 93 4 (4) 1 (reference) 89 3 (3) 1 (reference) 89 14 (16) 1 (reference)
N, number of participants with complete data.
*From logistic regression analyses adjusted for age,sex,antidepressants.
Supplemental Table 1
IRs and IRRs of Falls per Person-Year During Intervention in Exercise and Control Group in Total Sample and According to Subgroups
Subgroup Intervention
1 Fall n (%)* Total Falls (obs d) IR IRR (95% CI)y Interaction (95% CI)y P
Total
Exercise,n ¼ 93 41 (44) 107 (10787) 3.6 1.3 (0.8,2.0) e .398
Control,n ¼ 93 44 (47) 83 (10903) 2.8 1 (reference)
Sex
Exercise women,n ¼ 70 30 (43) 94 (11132) 3.3 1.2 (0.7,2.1) 0.9 (0.3-2.8) .902
Control women,n ¼ 71 33 (47) 82 (11591) 2.7 1 (reference)
Exercise men, n ¼ 23 11 (49) 17 (3835) 4.5 1.5 (0.7,3.4)
Control men, n ¼ 22 11 (50) 31 (3155) 2.9 1.2 (0.6,2.3)
Dementia type
Exercise Alzheimer’s disease,n ¼ 34 17 (50) 58 (3950) 5.4 2.1 (1.0,4.3) 2.6 (1.0,6.7) .048
Control Alzheimer’s disease,n ¼ 33 16 (49) 25 (3927) 2.3 1 (reference)
Exercise non- Alzheimer’s disease,n ¼ 59 24 (41) 49 (6837) 2.6 1.0 (0.6,1.8)
Control non- Alzheimer’s disease,n ¼ 60 28 (47) 58 (6976) 3.0 1.2 (0.6,2.4)
non-Alzheimer’s disease,vascular dementia,mixed Alzheimer’s disease and Vascular dementia,and other types of dementia; obs d,observation days.
*Number of participants (proportion) who fell at least once.
y
From negative binomial regression analyses with observation days as exposure term and adjusted for age,sex, antidepressants,and cluster.
A. Toots et al./ JAMDA 20 (2019) 835e842 842.e1
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.

