Postgraduate Medical Education: Clinical Leadership Development Review
VerifiedAdded on 2023/03/20
|14
|13638
|30
Report
AI Summary
This report, drawn from the Journal of Healthcare Leadership, focuses on clinical leadership development within postgraduate medical education and training in the UK National Health Service (NHS). It explores the significance of clinical leadership in improving healthcare quality and efficiency, particularly emphasizing the role of junior doctors as a crucial resource for initiating and championing improvements. The paper reviews various leadership theories and interventions, including competency frameworks and shared learning approaches, highlighting the shift from developing individual leaders to fostering a more inclusive, 'leader-ful' organizational model. It examines the historical context of postgraduate medical training, including the evolution of curricula and the impact of working time regulations. The report underscores the importance of engaging junior doctors in healthcare provision and the need for leadership development to ensure the future generation of healthcare professionals are well-equipped to drive system improvements. The study also considers the challenges and dynamics within healthcare organizations, emphasizing the need for cooperation and support from clinicians at all levels to facilitate meaningful change. The document highlights the evolution of postgraduate medical training and the shift towards emphasizing non-technical skills and generic competencies, including leadership, research, and education.
© 2015 Aggarwal and Swanwick. This work is published by Dove Medical Press Limited, and licensed under Creativ
License. The full terms of the License are available at http://creativecommons.org/licenses/by-nc/3.0/. Non-commer
permission from Dove Medical Press Limited, provided the work is properly attributed. Permissions beyond the scope of the Licen
how to request permission may be found at: http://www.dovepress.com/permissions.php
Journal of Healthcare Leadership 2015:7 109–122
Journal of Healthcare Leadership Dovepress
submit your manuscript | www.dovepress.com
Dovepress
109
R e v i e w
open access to scientific and medical research
Open Access Full Text Article
http://dx.doi.org/10.2147/JHL.S69330
Clinical leadership development in postgradu
medical education and training: policy, strate
and delivery in the UK National Health Servic
Reena Aggarwal1,2
Tim Swanwick2
1women’s Health, whittington Health,
London, UK;2Health education
england, North Central and east
London, London, UK
Correspondence: Reena Aggarwal
women’s Health, whittington Health,
Magdala Avenue, London N19 5NF, UK
Tel +44 7799 664 215
email raggarwal73@doctors.org.uk
Abstract:Achieving high quality health care against a background of continual change,
increasing demand, and shrinking financial resource is a major challenge. However, there is
significant international evidence that when clinicians use their voices and values to engage
with system delivery, operational efficiency and care outcomes are improved. In the UK
National Health Service, the traditional divide between doctors and managers is being bridged,
as clinical leadership is now foregrounded as an important organizational priority. There are
60,000 doctors in postgraduate training (junior doctors) in the UK who provide the majority
of front-line patient care and form an “operating core” of most health care organizations. This
group of doctors is therefore seen as an important resource in initiating, championing, and
delivering improvement in the quality of patient care. This paper provides a brief overview
of leadership theories and constructs that have been used to develop a raft of interventions to
develop leadership capability among junior doctors. We explore some of the approaches used,
including competency frameworks, talent management, shared learning, clinical fellowships,
and quality improvement. A new paradigm is identified as necessary to make a difference at a
local level, which moves learning and leadership away from developing “leaders”, to a more
inclusive model of developing relationships between individuals within organizations. This
shifts the emphasis from the development of a “heroic” individual leader to a more distributed
model, where organizations are “leader-ful” and not just “well led” and leadership is centered
on a shared vision owned by whole teams working on the frontline.
Keywords:National Health Service, junior doctors, quality improvement, management, health
care, leadership, fellowships, mentoring
Introduction
Health care has both scientific and social dimensions and is also the source of immense
political concern. Vast sums of gross domestic product are spent on health,1 the orga-
nization of complex systems of health care provision is difficult, and governments are
increasingly judged on their ability to deliver high value services.2 In the UK, a National
Health Service (NHS) employs over 1.5 million people with a budget of around £115
billion under the supervision of its departments of health. Notwithstanding its size,
the NHS appears to be an effective system. In 2014, a Commonwealth Fund report
concluded that in comparison with the health care systems of ten other countries
(Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden,
Switzerland, and USA), the NHS was the most impressive overall, although lagging
behind on health outcomes.3 By comparison, the USA has the most expensive health
care system, yet ranked last in measures of health outcomes, quality, and efficiency.
Journal of Healthcare Leadership downloaded from https://www.dovepress.com/ by 193.93.195.147 on 25-Aug-2018
For personal use only.
Powered by TCPDF (www.tcpdf.org)
License. The full terms of the License are available at http://creativecommons.org/licenses/by-nc/3.0/. Non-commer
permission from Dove Medical Press Limited, provided the work is properly attributed. Permissions beyond the scope of the Licen
how to request permission may be found at: http://www.dovepress.com/permissions.php
Journal of Healthcare Leadership 2015:7 109–122
Journal of Healthcare Leadership Dovepress
submit your manuscript | www.dovepress.com
Dovepress
109
R e v i e w
open access to scientific and medical research
Open Access Full Text Article
http://dx.doi.org/10.2147/JHL.S69330
Clinical leadership development in postgradu
medical education and training: policy, strate
and delivery in the UK National Health Servic
Reena Aggarwal1,2
Tim Swanwick2
1women’s Health, whittington Health,
London, UK;2Health education
england, North Central and east
London, London, UK
Correspondence: Reena Aggarwal
women’s Health, whittington Health,
Magdala Avenue, London N19 5NF, UK
Tel +44 7799 664 215
email raggarwal73@doctors.org.uk
Abstract:Achieving high quality health care against a background of continual change,
increasing demand, and shrinking financial resource is a major challenge. However, there is
significant international evidence that when clinicians use their voices and values to engage
with system delivery, operational efficiency and care outcomes are improved. In the UK
National Health Service, the traditional divide between doctors and managers is being bridged,
as clinical leadership is now foregrounded as an important organizational priority. There are
60,000 doctors in postgraduate training (junior doctors) in the UK who provide the majority
of front-line patient care and form an “operating core” of most health care organizations. This
group of doctors is therefore seen as an important resource in initiating, championing, and
delivering improvement in the quality of patient care. This paper provides a brief overview
of leadership theories and constructs that have been used to develop a raft of interventions to
develop leadership capability among junior doctors. We explore some of the approaches used,
including competency frameworks, talent management, shared learning, clinical fellowships,
and quality improvement. A new paradigm is identified as necessary to make a difference at a
local level, which moves learning and leadership away from developing “leaders”, to a more
inclusive model of developing relationships between individuals within organizations. This
shifts the emphasis from the development of a “heroic” individual leader to a more distributed
model, where organizations are “leader-ful” and not just “well led” and leadership is centered
on a shared vision owned by whole teams working on the frontline.
Keywords:National Health Service, junior doctors, quality improvement, management, health
care, leadership, fellowships, mentoring
Introduction
Health care has both scientific and social dimensions and is also the source of immense
political concern. Vast sums of gross domestic product are spent on health,1 the orga-
nization of complex systems of health care provision is difficult, and governments are
increasingly judged on their ability to deliver high value services.2 In the UK, a National
Health Service (NHS) employs over 1.5 million people with a budget of around £115
billion under the supervision of its departments of health. Notwithstanding its size,
the NHS appears to be an effective system. In 2014, a Commonwealth Fund report
concluded that in comparison with the health care systems of ten other countries
(Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden,
Switzerland, and USA), the NHS was the most impressive overall, although lagging
behind on health outcomes.3 By comparison, the USA has the most expensive health
care system, yet ranked last in measures of health outcomes, quality, and efficiency.
Journal of Healthcare Leadership downloaded from https://www.dovepress.com/ by 193.93.195.147 on 25-Aug-2018
For personal use only.
Powered by TCPDF (www.tcpdf.org)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Journal of Healthcare Leadership 2015:7submit your manuscript | www.dovepress.com
Dovepress
Dovepress
110
Aggarwal and Swanwick
Despite the UK’s high-ranking, significant shortcomings
exist in the quality and availability of care, as highlighted by
a recent public inquiry by Sir Robert Francis. The “Francis
Report” detailed catastrophic failings in patient care occur-
ring over a number of years in one particular NHS trust. Sig-
nificantly, the report also identified a “learned helplessness”
among medical and nursing staff, resulting in disengagement
of health care professionals from management.4 Subsequent
reviews of other NHS provider organizations have unearthed
similar problems with a focus on targets and efficiency sav-
ings dominating board agendas and organizations losing sight
of the patient. This has been viewed widely as something
that needs fixing, and a significant element in the solution
has been to invite clinicians to engage with system delivery,
to use their voices and values in improving quality and
productivity, while simultaneously controlling the costs of
service provision.4–6
Clinicians, doctors in particular, have considerable influ-
ence in relation to health care expenditure, occupy the moral
high ground of patient advocacy, and have a large measure
of autonomy by virtue of their training and professional
knowledge. Drawing upon the organizational theories of
Mintzberg, health care organizations function as “profes-
sional bureaucracies” in which the continually evolving
expertise of skilled and knowledgeable workers exercises
a high degree of degree of control over the delivery of
services.7 In a professional organization, workers’ autonomy
is regulated by external professional bodies, contrasting
with a “machine bureaucracy”, where the organization itself
designs and enforces standards through strong line manage-
ment structures. Professional bureaucracies create an inverted
power structure, where frontline staff have greater influence
over daily decision-making than those who, through formal
positions of authority, are responsible for managing the ser-
vice.5,8 In such a system, the ability of managers to influence
clinical decision-making is constrained since clinical profes-
sionals form the “operating core” of health organizations,
thereby controlling the means of production.9
According to Ham and Dickenson,10 this has three signifi-
cant implications for health care organizations: key leader-
ship roles are played by professionals; leadership is dispersed
or distributed among staff and not limited to individuals in
formal managerial roles, and the system requires collective
leadership, ie, teams that bring together leaders at different
levels. In understanding the relationships and power dynam-
ics within health care organizations, it becomes evident that
significant clinical change is impossible without the coop-
eration and support of clinicians at all levels. The operating
core of most health care organizations consists of a large
body of doctors in postgraduate training, resolutely engaged
at the front line of patient care. “Junior” doctors, then, are
the perfect tool for initiating, championing, and delivering
change and improvement in the quality of care.
Postgraduate medical training in
the UK
There are around 60,000 junior doctors (In the UK, the term
“junior doctor” is used to describe a qualified doctor who has
yet to be placed on the General Medical Council’s special-
ist or general practice register. Junior doctors are normally
“trainees” enrolled in a postgraduate training program and
work under the supervision of “seniors”, usually registered
consultant specialists or general practitioners) in postgradu-
ate training programs in the UK, with multiple agencies
responsible for different aspects of the training. Setting and
monitoring professional standards is primarily a role of the
General Medical Council and Royal Colleges, funding is
controlled centrally from the relevant Department of Health
and dispersed via various bodies such as Health Education
England or NHS Education for Scotland, and those delivering
the training are situated in a variety of a community, inte-
grated, and hospital settings. Unlike undergraduate students,
postgraduate trainees do not have a university structure to
manage their placements, programs, or the progression of
individuals. Historically therefore, a “deanery” has sat as
“an organization in the middle”, providing an umbrella for
postgraduate medical education and training, controlling the
funding flows, ensuring training is delivered to curricular
specifications, and that quality standards are monitored and
maintained.
There is broad agreement that the prime purpose of
postgraduate medical training is “… to ensure that special-
ized doctors competently address the medical needs of the
community” (p 3),11 an aim reiterated in a recent report on
the future of postgraduate medical education and training,
The Shape of Training. 12 Indeed, training structures in the
UK have been in evolution since the publication, in the
1990s, of the Calman report.13 Predominantly concerned with
improving specialist hospital training, this report resulted
in the introduction of specialist registrar posts with explicit
curricula, regular assessments of progress, and time-limited
specialist training. Alongside this development was the
implementation of European Working Time Directive –
later, European Working Time Regulations – restricting
junior doctors to a maximum of 58 hours per week by 2004,
with a further reduction to 48 hours by 2009. Many doctors
Journal of Healthcare Leadership downloaded from https://www.dovepress.com/ by 193.93.195.147 on 25-Aug-2018
For personal use only.
Powered by TCPDF (www.tcpdf.org)
Dovepress
Dovepress
110
Aggarwal and Swanwick
Despite the UK’s high-ranking, significant shortcomings
exist in the quality and availability of care, as highlighted by
a recent public inquiry by Sir Robert Francis. The “Francis
Report” detailed catastrophic failings in patient care occur-
ring over a number of years in one particular NHS trust. Sig-
nificantly, the report also identified a “learned helplessness”
among medical and nursing staff, resulting in disengagement
of health care professionals from management.4 Subsequent
reviews of other NHS provider organizations have unearthed
similar problems with a focus on targets and efficiency sav-
ings dominating board agendas and organizations losing sight
of the patient. This has been viewed widely as something
that needs fixing, and a significant element in the solution
has been to invite clinicians to engage with system delivery,
to use their voices and values in improving quality and
productivity, while simultaneously controlling the costs of
service provision.4–6
Clinicians, doctors in particular, have considerable influ-
ence in relation to health care expenditure, occupy the moral
high ground of patient advocacy, and have a large measure
of autonomy by virtue of their training and professional
knowledge. Drawing upon the organizational theories of
Mintzberg, health care organizations function as “profes-
sional bureaucracies” in which the continually evolving
expertise of skilled and knowledgeable workers exercises
a high degree of degree of control over the delivery of
services.7 In a professional organization, workers’ autonomy
is regulated by external professional bodies, contrasting
with a “machine bureaucracy”, where the organization itself
designs and enforces standards through strong line manage-
ment structures. Professional bureaucracies create an inverted
power structure, where frontline staff have greater influence
over daily decision-making than those who, through formal
positions of authority, are responsible for managing the ser-
vice.5,8 In such a system, the ability of managers to influence
clinical decision-making is constrained since clinical profes-
sionals form the “operating core” of health organizations,
thereby controlling the means of production.9
According to Ham and Dickenson,10 this has three signifi-
cant implications for health care organizations: key leader-
ship roles are played by professionals; leadership is dispersed
or distributed among staff and not limited to individuals in
formal managerial roles, and the system requires collective
leadership, ie, teams that bring together leaders at different
levels. In understanding the relationships and power dynam-
ics within health care organizations, it becomes evident that
significant clinical change is impossible without the coop-
eration and support of clinicians at all levels. The operating
core of most health care organizations consists of a large
body of doctors in postgraduate training, resolutely engaged
at the front line of patient care. “Junior” doctors, then, are
the perfect tool for initiating, championing, and delivering
change and improvement in the quality of care.
Postgraduate medical training in
the UK
There are around 60,000 junior doctors (In the UK, the term
“junior doctor” is used to describe a qualified doctor who has
yet to be placed on the General Medical Council’s special-
ist or general practice register. Junior doctors are normally
“trainees” enrolled in a postgraduate training program and
work under the supervision of “seniors”, usually registered
consultant specialists or general practitioners) in postgradu-
ate training programs in the UK, with multiple agencies
responsible for different aspects of the training. Setting and
monitoring professional standards is primarily a role of the
General Medical Council and Royal Colleges, funding is
controlled centrally from the relevant Department of Health
and dispersed via various bodies such as Health Education
England or NHS Education for Scotland, and those delivering
the training are situated in a variety of a community, inte-
grated, and hospital settings. Unlike undergraduate students,
postgraduate trainees do not have a university structure to
manage their placements, programs, or the progression of
individuals. Historically therefore, a “deanery” has sat as
“an organization in the middle”, providing an umbrella for
postgraduate medical education and training, controlling the
funding flows, ensuring training is delivered to curricular
specifications, and that quality standards are monitored and
maintained.
There is broad agreement that the prime purpose of
postgraduate medical training is “… to ensure that special-
ized doctors competently address the medical needs of the
community” (p 3),11 an aim reiterated in a recent report on
the future of postgraduate medical education and training,
The Shape of Training. 12 Indeed, training structures in the
UK have been in evolution since the publication, in the
1990s, of the Calman report.13 Predominantly concerned with
improving specialist hospital training, this report resulted
in the introduction of specialist registrar posts with explicit
curricula, regular assessments of progress, and time-limited
specialist training. Alongside this development was the
implementation of European Working Time Directive –
later, European Working Time Regulations – restricting
junior doctors to a maximum of 58 hours per week by 2004,
with a further reduction to 48 hours by 2009. Many doctors
Journal of Healthcare Leadership downloaded from https://www.dovepress.com/ by 193.93.195.147 on 25-Aug-2018
For personal use only.
Powered by TCPDF (www.tcpdf.org)

Journal of Healthcare Leadership 2015:7 submit your manuscript | www.dovepress.com
Dovepress
Dovepress
111
Leadership development in postgraduate medical education and trainin
traditionally worked much longer hours, and these changes
reduced the degree to which the NHS could rely on doc-
tors in training for service delivery and, correspondingly,
decreased the amount of time doctors would have available
for training.
In order to address these issues, postgraduate training was
further reformed – under the banner of “Modernising Medical
Careers” – predominantly to accelerate the production of
competent specialists. “Modernising Medical Careers” led to
the creation of a 2-year foundation program, followed by basic
specialist training in a broad specialty grouping (eg, core med-
ical training), and then higher specialist training in a specific
specialty (eg, neurology).14 The aim was to provide doctors
with wide initial breadth of training, which would ultimately
be shorter by virtue of a more structured program later on.15
Explicit curricula for each specialty (there are 67 in the UK
with 35 subspecialties) were introduced alongside a wholesale
revision of training standards and accountabilities.
Since then, there has been a gradual shift in curricula
emphases, from the dominance of technocratic expertise to the
foregrounding of “nontechnical skills”.16,17 A range of generic
competencies have found their way into postgraduate medical
education and training, particularly in the areas of leadership,
research, and education. This recognition that doctors are an
integral part of a health care system, rather than isolated and
autonomous clinical professionals, is further underscored by
an increasing focus on quality improvement and population
health, and most recently a rediscovery of the patient at the
heart of care, with attention turning to issues such as coproduc-
tion, patient engagement, and supported self-management.18
With these changes has come the recognition that the
potential of the trainee body (junior doctors), a large sector
of the NHS workforce, is largely untapped. 19 Furthermore,
there is a risk that this future generation of influential health
care professionals may not be adequately engaged with the
“business” of health care provision, with the consequence
that our professional bureaucracy continues to normalize
around professional rather than system drivers.
Why engage junior doctors?
At the heart of postgraduate medical education is a managed
tension between service and training, with the learner also
as employee.20 Junior doctors rotate frequently between dif-
ferent service providers as part of their training in order to
achieve their competency-based curricula, but also represent
the front line of clinical service delivering, for example,
80% of ward-based activity.21 Due to their transient nature
within organizations, junior doctors are often disconnected
from their employers and viewed as a temporary work-
force providing service. However, this peripatetic group is
exposed to a myriad of different working practices within
a wide range of service providers and have the potential
to disseminate good practice as well the ability to identify
areas for change.22,23
With recognition that today’s junior doctors will be tomor-
row’s clinical leaders, the importance of the development of
management and leadership has been highlighted in many
policy documents, including an independent inquiry into
“Modernising Medical Careers”,
[…] the doctor’s frequent role as the head of the healthcare
team and commander of considerable resources requires
that greater attention is paid to managerial and leadership
skills irrespective of specialism (p 90).21
Many commentators have expressed concern that the
ability of doctors in training to influence change is not
being harnessed and are an underused resource, which if
mobilized could significantly improve quality and safety of
patient care.10,14,19,24 A recent survey of over 1,500 doctors in
training found that 91% had ideas for workplace improve-
ment, but only 11% had been able to implement these. 22,25
This is a waste. Leadership development of this group of
youthful energetic junior doctors should be an essential part
of “improving health, reducing its variation and doing so in
an affordable way” (p 466).26
What is clinical leadership?
As understood in Anglo–American contexts,27 the terms “lead-
ership” and “management” are sometimes used interchange-
ably,28 but within the health care literature they tend to describe
different approaches to how change can be achieved.
Management is sometimes viewed as a pejorative term,
particularly in the public sector, and the discourse of leader-
ship provides a more attractive narrative for professionals,
enabling policymakers to engage professionals into activi-
ties they desire, such as service reform. 29–31 While this may
be seen as a cynical tactic to co-opt professionals into the
organizational arena in order to control their activity,32 it
may also reflect a genuine recognition that to address the
“wicked” problems faced by health and social care organi-
zations, the particular knowledge and insight professionals
bring are crucial for effective negotiation, influence, and
persuasion with a variety of stakeholders in an increasingly
complex system.33
Definitions of leadership are many and contested, but
most commentators agree that leaders motivate, inspire, and
Journal of Healthcare Leadership downloaded from https://www.dovepress.com/ by 193.93.195.147 on 25-Aug-2018
For personal use only.
Powered by TCPDF (www.tcpdf.org)
Dovepress
Dovepress
111
Leadership development in postgraduate medical education and trainin
traditionally worked much longer hours, and these changes
reduced the degree to which the NHS could rely on doc-
tors in training for service delivery and, correspondingly,
decreased the amount of time doctors would have available
for training.
In order to address these issues, postgraduate training was
further reformed – under the banner of “Modernising Medical
Careers” – predominantly to accelerate the production of
competent specialists. “Modernising Medical Careers” led to
the creation of a 2-year foundation program, followed by basic
specialist training in a broad specialty grouping (eg, core med-
ical training), and then higher specialist training in a specific
specialty (eg, neurology).14 The aim was to provide doctors
with wide initial breadth of training, which would ultimately
be shorter by virtue of a more structured program later on.15
Explicit curricula for each specialty (there are 67 in the UK
with 35 subspecialties) were introduced alongside a wholesale
revision of training standards and accountabilities.
Since then, there has been a gradual shift in curricula
emphases, from the dominance of technocratic expertise to the
foregrounding of “nontechnical skills”.16,17 A range of generic
competencies have found their way into postgraduate medical
education and training, particularly in the areas of leadership,
research, and education. This recognition that doctors are an
integral part of a health care system, rather than isolated and
autonomous clinical professionals, is further underscored by
an increasing focus on quality improvement and population
health, and most recently a rediscovery of the patient at the
heart of care, with attention turning to issues such as coproduc-
tion, patient engagement, and supported self-management.18
With these changes has come the recognition that the
potential of the trainee body (junior doctors), a large sector
of the NHS workforce, is largely untapped. 19 Furthermore,
there is a risk that this future generation of influential health
care professionals may not be adequately engaged with the
“business” of health care provision, with the consequence
that our professional bureaucracy continues to normalize
around professional rather than system drivers.
Why engage junior doctors?
At the heart of postgraduate medical education is a managed
tension between service and training, with the learner also
as employee.20 Junior doctors rotate frequently between dif-
ferent service providers as part of their training in order to
achieve their competency-based curricula, but also represent
the front line of clinical service delivering, for example,
80% of ward-based activity.21 Due to their transient nature
within organizations, junior doctors are often disconnected
from their employers and viewed as a temporary work-
force providing service. However, this peripatetic group is
exposed to a myriad of different working practices within
a wide range of service providers and have the potential
to disseminate good practice as well the ability to identify
areas for change.22,23
With recognition that today’s junior doctors will be tomor-
row’s clinical leaders, the importance of the development of
management and leadership has been highlighted in many
policy documents, including an independent inquiry into
“Modernising Medical Careers”,
[…] the doctor’s frequent role as the head of the healthcare
team and commander of considerable resources requires
that greater attention is paid to managerial and leadership
skills irrespective of specialism (p 90).21
Many commentators have expressed concern that the
ability of doctors in training to influence change is not
being harnessed and are an underused resource, which if
mobilized could significantly improve quality and safety of
patient care.10,14,19,24 A recent survey of over 1,500 doctors in
training found that 91% had ideas for workplace improve-
ment, but only 11% had been able to implement these. 22,25
This is a waste. Leadership development of this group of
youthful energetic junior doctors should be an essential part
of “improving health, reducing its variation and doing so in
an affordable way” (p 466).26
What is clinical leadership?
As understood in Anglo–American contexts,27 the terms “lead-
ership” and “management” are sometimes used interchange-
ably,28 but within the health care literature they tend to describe
different approaches to how change can be achieved.
Management is sometimes viewed as a pejorative term,
particularly in the public sector, and the discourse of leader-
ship provides a more attractive narrative for professionals,
enabling policymakers to engage professionals into activi-
ties they desire, such as service reform. 29–31 While this may
be seen as a cynical tactic to co-opt professionals into the
organizational arena in order to control their activity,32 it
may also reflect a genuine recognition that to address the
“wicked” problems faced by health and social care organi-
zations, the particular knowledge and insight professionals
bring are crucial for effective negotiation, influence, and
persuasion with a variety of stakeholders in an increasingly
complex system.33
Definitions of leadership are many and contested, but
most commentators agree that leaders motivate, inspire, and
Journal of Healthcare Leadership downloaded from https://www.dovepress.com/ by 193.93.195.147 on 25-Aug-2018
For personal use only.
Powered by TCPDF (www.tcpdf.org)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Journal of Healthcare Leadership 2015:7submit your manuscript | www.dovepress.com
Dovepress
Dovepress
112
Aggarwal and Swanwick
align strategy to establish direction for individuals and the
systems in which they work, while managers are process
driven and use problem solving to direct individuals and
resources to achieve goals already established by leader-
ship.1,34,35 As described in an influential report from the
King’s Fund, leadership, management, and administration
are interdependent since … without leadership there can be
no effective management – because the organization will not
know what it is meant to be doing – and without good admin-
istration management can be rendered ineffective (p 1).36
If we accept Mintzberg’s theory that health care organi-
zations exhibit an inverted power structure, a new leadership
paradigm emerges. Those providing front-line service have
significant influence over the operational activities, result-
ing in a range of patient- and population-related outcomes
compared to those who occupy hierarchical positions of
authority. Hence, clinical leadership becomes an inclusive
endeavor. By engaging champions of health care quality
at service-level, behaviors and attitudes on the front line
can be aligned with organizational vision, ensuring that the
needs of the patient are central in the organization’s aims
and delivery. This view of clinical leadership appeals to
clinicians as it frames health care management around the
leadership of change and improvement for the safety and
quality of patient care. It is a discourse that also replaces the
previous one of professionals as the cause of problems in
public service organizations and, crucially, begins to view
them as part of the solution.
Leadership models, trends,
and contexts
Swanwick and McKimm35 frame leadership as a social
construct, influenced by the preoccupations, sociopoliti-
cal system, and cultural values of the time. The leadership
theories and models espoused will influence the discourses
adopted and reflect societal views of how systems are or
should be organized. This is clearly crucial when we consider
leadership development, as how leadership is conceptualized
will profoundly influence approaches taken in the name of
its development. In the following sections, we summarize
some of the previous century’s most influential leadership
models and consider what might be needed for a 21st century
health service.
Trait theory
In the first half of the 20th Century, “trait” theories emerged
around the ideal of the “Great Man” proposing that great
leaders (usually men, reflecting the position women had in
society at that time) had a defined collection of personal
attributes, including ability, sociability, motivation, and
dominance. This theory is attractive to doctors given the
weight placed on key personal characteristics in their selec-
tion process, but as Willcocks37 maintains, while many doc-
tors may possess leadership qualities, these are not equally
distributed and some doctors may be able to employ these
in a clinical encounter, but not necessarily in the dynamic
group context of leadership. Literature reviews in the 1970s
failed to consistently identify the personality traits that
distinguish leaders from nonleaders, although one more
recent review has identified a weak positive correlation
between successful leaders and three of the “big five” per-
sonality factors – extroversion, openness to new experience,
and conscientiousness. 38 Additionally, leaders had a weak
negative correlation with neuroticism, but interestingly, no
relationship was found to the extent to which the leader is
agreeable. Another review in the context of school leader-
ship found less emphasis or correlation on these “innate
qualities” with successful leadership. 39
Leadership styles
From the 1950, greater emphasis began to be placed
on leadership styles and behaviors rather than personal
characteristics. In part, this was a reaction to the deficiencies
of the trait approach and its failure to recognize the context
in which leadership occurred. The shift in theory focused
on two aspects – how leaders made decisions and on what
they were focused. Many taxonomies for decision-making
styles developed, but the most famous is perhaps that of
Tannenbaum and Schmidt 40 who describe a continuum of
leadership behavior from autocratic (“do as I say”) to abdi-
catory (“do what you like”). Other styles embraced team
management, where leadership is focused on results or the
people in the organization,41,42 or an authoritative manner
which mobilizes empathetically toward a vision.43 These
styles are attractive for clinicians in leadership roles as they
embrace balancing the needs of patients and team members
within an environment where resources are constrained and
management targets need to be met.
Contingency theories
In order to recognize the complexity and context of different
situations, contingency theories became popular in the 1960s,
the concept being that leaders should adapt their style to the
competence and commitment of followers, using a range of
interventions, such as directing, coaching, supporting, and
delegating. Such an approach requires not only awareness of
Journal of Healthcare Leadership downloaded from https://www.dovepress.com/ by 193.93.195.147 on 25-Aug-2018
For personal use only.
Powered by TCPDF (www.tcpdf.org)
Dovepress
Dovepress
112
Aggarwal and Swanwick
align strategy to establish direction for individuals and the
systems in which they work, while managers are process
driven and use problem solving to direct individuals and
resources to achieve goals already established by leader-
ship.1,34,35 As described in an influential report from the
King’s Fund, leadership, management, and administration
are interdependent since … without leadership there can be
no effective management – because the organization will not
know what it is meant to be doing – and without good admin-
istration management can be rendered ineffective (p 1).36
If we accept Mintzberg’s theory that health care organi-
zations exhibit an inverted power structure, a new leadership
paradigm emerges. Those providing front-line service have
significant influence over the operational activities, result-
ing in a range of patient- and population-related outcomes
compared to those who occupy hierarchical positions of
authority. Hence, clinical leadership becomes an inclusive
endeavor. By engaging champions of health care quality
at service-level, behaviors and attitudes on the front line
can be aligned with organizational vision, ensuring that the
needs of the patient are central in the organization’s aims
and delivery. This view of clinical leadership appeals to
clinicians as it frames health care management around the
leadership of change and improvement for the safety and
quality of patient care. It is a discourse that also replaces the
previous one of professionals as the cause of problems in
public service organizations and, crucially, begins to view
them as part of the solution.
Leadership models, trends,
and contexts
Swanwick and McKimm35 frame leadership as a social
construct, influenced by the preoccupations, sociopoliti-
cal system, and cultural values of the time. The leadership
theories and models espoused will influence the discourses
adopted and reflect societal views of how systems are or
should be organized. This is clearly crucial when we consider
leadership development, as how leadership is conceptualized
will profoundly influence approaches taken in the name of
its development. In the following sections, we summarize
some of the previous century’s most influential leadership
models and consider what might be needed for a 21st century
health service.
Trait theory
In the first half of the 20th Century, “trait” theories emerged
around the ideal of the “Great Man” proposing that great
leaders (usually men, reflecting the position women had in
society at that time) had a defined collection of personal
attributes, including ability, sociability, motivation, and
dominance. This theory is attractive to doctors given the
weight placed on key personal characteristics in their selec-
tion process, but as Willcocks37 maintains, while many doc-
tors may possess leadership qualities, these are not equally
distributed and some doctors may be able to employ these
in a clinical encounter, but not necessarily in the dynamic
group context of leadership. Literature reviews in the 1970s
failed to consistently identify the personality traits that
distinguish leaders from nonleaders, although one more
recent review has identified a weak positive correlation
between successful leaders and three of the “big five” per-
sonality factors – extroversion, openness to new experience,
and conscientiousness. 38 Additionally, leaders had a weak
negative correlation with neuroticism, but interestingly, no
relationship was found to the extent to which the leader is
agreeable. Another review in the context of school leader-
ship found less emphasis or correlation on these “innate
qualities” with successful leadership. 39
Leadership styles
From the 1950, greater emphasis began to be placed
on leadership styles and behaviors rather than personal
characteristics. In part, this was a reaction to the deficiencies
of the trait approach and its failure to recognize the context
in which leadership occurred. The shift in theory focused
on two aspects – how leaders made decisions and on what
they were focused. Many taxonomies for decision-making
styles developed, but the most famous is perhaps that of
Tannenbaum and Schmidt 40 who describe a continuum of
leadership behavior from autocratic (“do as I say”) to abdi-
catory (“do what you like”). Other styles embraced team
management, where leadership is focused on results or the
people in the organization,41,42 or an authoritative manner
which mobilizes empathetically toward a vision.43 These
styles are attractive for clinicians in leadership roles as they
embrace balancing the needs of patients and team members
within an environment where resources are constrained and
management targets need to be met.
Contingency theories
In order to recognize the complexity and context of different
situations, contingency theories became popular in the 1960s,
the concept being that leaders should adapt their style to the
competence and commitment of followers, using a range of
interventions, such as directing, coaching, supporting, and
delegating. Such an approach requires not only awareness of
Journal of Healthcare Leadership downloaded from https://www.dovepress.com/ by 193.93.195.147 on 25-Aug-2018
For personal use only.
Powered by TCPDF (www.tcpdf.org)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Journal of Healthcare Leadership 2015:7 submit your manuscript | www.dovepress.com
Dovepress
Dovepress
113
Leadership development in postgraduate medical education and trainin
these styles of leadership, but also the recognition of when a
particular approach is required with appropriate enactment.
A criticism of contingency theories is that they are highly
dependent upon who defines the situation in question.44
Transformational leadership
In the 1980s, a new paradigm of transformational leadership
emerged, arising in part from the recognition that previous
leadership approaches failed to account for the fact that envi-
ronments are subject to continual change.45 Existing models
tended to be transactional and managerial in nature, which
were useful to plan and organize at times of stability, but inad-
equate when describing how to lead people or organizations
through periods of significant change. In the transformational
model, leaders release human potential through empower-
ment and development of followers. Leaders articulate the
values and direction of an organization, work of individuals
within the organization is aligned to the achievement of these
long-term goals, and followers are nurtured thereby strength-
ening organizational culture and engendering a commitment
to move toward a shared envisioned future.
One of the problems with a transformational leadership
approach is the tendency toward the veneration of indi-
vidual leaders as “tsars”. This led in the 1990s to a wave
of charismatic individuals sweeping into “turnaround”
failing organizations using their dominant personality and
self-confidence to influence others, while exhibiting strong
role modeling, extolling high expectations, and articulat-
ing ideological goals. As a complete antithesis, servant
leadership offers a quieter stewardship approach where
leaders facilitate growth and development, and serve the
needs of the community by persuasion rather than coercion
with empathetic listening and encouragement to collective
action.46 Nevertheless, “heroic” transformational leadership
has proven to be an enduring model, being incorporated into
many public sector frameworks including the UK’s NHS
Healthcare Leadership Model. 47
Distributed leadership
This “post heroic” model considers leadership not to
reside in one individual but instead the focus is on “…
organisational relations, connectedness, interventions into
the organization system, changing organization practices
and processes” (p 6). 48 Boundaries to leadership are open,
encompassing multiple individuals whose expertise is dis-
tributed across professional and organizational boundaries,
building upon social capital for innovation, collaboration, and
improved outcomes.49,50 Leadership shifts from the focus on
individual qualities of a leader at the top of an organization
to the process of leadership within an organization. It offers
the exciting opportunity where leadership development is not
about creating more leaders, but systems where leadership
is everyone’s responsibility and enabled by a diverse range
of groups and individuals. 23 Distributed leadership moves
beyond the lonely model of heroic leadership to a shared,
adaptive, and collaborative approach that forces leaders to
focus on systems of care and not just organizational delivery
of results through followership.
So what is it then about the clinical context that influ-
ences the way we might think about “clinical leadership”,
and medical leadership specifically. As we have discussed,
health systems are complex. They have range of aims
and objectives (not simple profit/loss) controlled through
professional networks often with an absence of direct line
management or contractual control, with colleagues who
may have completely different sets of accountabilities and
who often are situated in completely different organizations.
Health and social care systems in the UK are also incredibly
diverse in terms of the culture, ethnicity, sex, and educational
background of its workforce.
Evidence from a study of 13 organizations shows that
a team structure working on a basis of trust will create
“a mutually reinforcing circle of benefits” (p 370). 51 This
supports the view that a top-down approach of leadership is
doomed to fail in a complex and uncertain environment. The
distributed leadership model enables local decision-making
by individuals, who guided by organizational vision, values,
and strategic intent do not then need excessive hierarchical
structures. This approach shifts away from a focus on indi-
vidual leadership characteristics or styles to a process of
“engagement”, where the mobilization, commitment, and
alignment of front line staff create a culture of leadership
within an organization.36,50
But is this enough? Health care is increasingly deliv-
ered by organizations working together, across the tradi-
tional boundaries of health and social care toward a set of
shared objectives. This requires leadership that not only is
distributed vertically within individual organizations, but
horizontally across whole health care systems, where the
leadership, at any one moment, might be taken by anyone,
from anywhere. This requires an even more sophisticated
approach and in a series of review publications by the
Kings Fund, a consensus is building that such a chal-
lenging environment requires leadership that is not only
distributed, but also collective, collaborative, and, above
all, compassionate. 52
Journal of Healthcare Leadership downloaded from https://www.dovepress.com/ by 193.93.195.147 on 25-Aug-2018
For personal use only.
Powered by TCPDF (www.tcpdf.org)
Dovepress
Dovepress
113
Leadership development in postgraduate medical education and trainin
these styles of leadership, but also the recognition of when a
particular approach is required with appropriate enactment.
A criticism of contingency theories is that they are highly
dependent upon who defines the situation in question.44
Transformational leadership
In the 1980s, a new paradigm of transformational leadership
emerged, arising in part from the recognition that previous
leadership approaches failed to account for the fact that envi-
ronments are subject to continual change.45 Existing models
tended to be transactional and managerial in nature, which
were useful to plan and organize at times of stability, but inad-
equate when describing how to lead people or organizations
through periods of significant change. In the transformational
model, leaders release human potential through empower-
ment and development of followers. Leaders articulate the
values and direction of an organization, work of individuals
within the organization is aligned to the achievement of these
long-term goals, and followers are nurtured thereby strength-
ening organizational culture and engendering a commitment
to move toward a shared envisioned future.
One of the problems with a transformational leadership
approach is the tendency toward the veneration of indi-
vidual leaders as “tsars”. This led in the 1990s to a wave
of charismatic individuals sweeping into “turnaround”
failing organizations using their dominant personality and
self-confidence to influence others, while exhibiting strong
role modeling, extolling high expectations, and articulat-
ing ideological goals. As a complete antithesis, servant
leadership offers a quieter stewardship approach where
leaders facilitate growth and development, and serve the
needs of the community by persuasion rather than coercion
with empathetic listening and encouragement to collective
action.46 Nevertheless, “heroic” transformational leadership
has proven to be an enduring model, being incorporated into
many public sector frameworks including the UK’s NHS
Healthcare Leadership Model. 47
Distributed leadership
This “post heroic” model considers leadership not to
reside in one individual but instead the focus is on “…
organisational relations, connectedness, interventions into
the organization system, changing organization practices
and processes” (p 6). 48 Boundaries to leadership are open,
encompassing multiple individuals whose expertise is dis-
tributed across professional and organizational boundaries,
building upon social capital for innovation, collaboration, and
improved outcomes.49,50 Leadership shifts from the focus on
individual qualities of a leader at the top of an organization
to the process of leadership within an organization. It offers
the exciting opportunity where leadership development is not
about creating more leaders, but systems where leadership
is everyone’s responsibility and enabled by a diverse range
of groups and individuals. 23 Distributed leadership moves
beyond the lonely model of heroic leadership to a shared,
adaptive, and collaborative approach that forces leaders to
focus on systems of care and not just organizational delivery
of results through followership.
So what is it then about the clinical context that influ-
ences the way we might think about “clinical leadership”,
and medical leadership specifically. As we have discussed,
health systems are complex. They have range of aims
and objectives (not simple profit/loss) controlled through
professional networks often with an absence of direct line
management or contractual control, with colleagues who
may have completely different sets of accountabilities and
who often are situated in completely different organizations.
Health and social care systems in the UK are also incredibly
diverse in terms of the culture, ethnicity, sex, and educational
background of its workforce.
Evidence from a study of 13 organizations shows that
a team structure working on a basis of trust will create
“a mutually reinforcing circle of benefits” (p 370). 51 This
supports the view that a top-down approach of leadership is
doomed to fail in a complex and uncertain environment. The
distributed leadership model enables local decision-making
by individuals, who guided by organizational vision, values,
and strategic intent do not then need excessive hierarchical
structures. This approach shifts away from a focus on indi-
vidual leadership characteristics or styles to a process of
“engagement”, where the mobilization, commitment, and
alignment of front line staff create a culture of leadership
within an organization.36,50
But is this enough? Health care is increasingly deliv-
ered by organizations working together, across the tradi-
tional boundaries of health and social care toward a set of
shared objectives. This requires leadership that not only is
distributed vertically within individual organizations, but
horizontally across whole health care systems, where the
leadership, at any one moment, might be taken by anyone,
from anywhere. This requires an even more sophisticated
approach and in a series of review publications by the
Kings Fund, a consensus is building that such a chal-
lenging environment requires leadership that is not only
distributed, but also collective, collaborative, and, above
all, compassionate. 52
Journal of Healthcare Leadership downloaded from https://www.dovepress.com/ by 193.93.195.147 on 25-Aug-2018
For personal use only.
Powered by TCPDF (www.tcpdf.org)

Journal of Healthcare Leadership 2015:7submit your manuscript | www.dovepress.com
Dovepress
Dovepress
114
Aggarwal and Swanwick
Does clinical leadership make a
difference?
Effective leadership is an important component of success-
ful health care organizations,53,54 whereas lack of leadership
can be associated with organizational failure.4,55 Veronesi
et al56 suggest clinical leaders influence health care system
outcomes since they have the expert knowledge of the core
business of health services and a deeper awareness of what
patient care involves … [to] make better informed decisions
regarding service design and resource allocation.
Forbes et al57 describe “role design” for clinician manag-
ers, who, instead of replicating the role of hospital managers,
use their unique voice to focus on clinical priorities.
There is a growing literature on the benefit of clinicians
in management and evidence that high-performing medical
groups build relationships with managers, with an emphasis
on clinical quality.58,59 Clinicians in senior management roles
tend to enhance operational outcomes for hospitals and orga-
nizations perform significantly better than those with lower
levels of clinician participation.60–63 A review conducted by
the Academy of Royal Medical Colleges in the UK concluded
that chief executive officers from high-performing institutions
engaged clinicians in dialogue and joint problem solving.64
Goodall65 demonstrates that hospital quality scores are 25%
higher in physician-headed hospitals compared to those with
chief executive officers from nonmedical backgrounds. More
recently, research undertaken by Veronesi et al56 in the UK
tentatively suggested that the “share of doctors” on the board
made most difference, and this relationship became less robust
when other health professionals were involved at board level.
This chimes with Dorgan et al 6 who investigated organiza-
tions across seven countries and suggested that having higher
proportions of medically qualified managers results in more
effective management practices.
It can be difficult to quantify the exact impact of clini-
cal leadership on service quality; however, studies do exist
which suggest improvements in various domains. A study
of hospitals in Michigan found that by using bed occupancy
rates and market share as performance measures and by
excluding clinical leaders from strategic decisions resulted
in lower hospital performance.66 Keroack et al67 ranked
health care institutions using a composite index of qual-
ity and safety that was developed to incorporate domains
identified as attributes of an ideal health care system. High
performance scores for organizations were associated with
organizational leadership that prioritized patients, focused
on quality and safety, used clear systems of accountability,
sought continual improvement as evidenced by results, and
emphasized collaboration between different staff groups
to make use of their varied expertise. Commissioned by
the King’s Fund to inform the leadership commission,
Baker68 used case studies to identify factors accounting
for success in high-performing systems; again, clinical
leadership that prioritized patients, quality and safety,
and that promoted collaborative working between differ-
ent professional groups was consistently present in all of
these institutions.
Barriers to clinical leadership
development
It becomes increasingly clear that clinical leadership is a cen-
tral ingredient to improve the quality of health care.36,69 It is
an essential component to align process redesign for business
operations and quality assurance, with clinical agendas per-
taining to patient care, service development, and professional
development for high quality services. Yet, despite the wealth
of evidence concerning the importance of clinical leadership
in health care organizations, it remains a variable constituent
of health systems. Darzi70 concluded in the NHS Next Stage
Review that “leadership has been the neglected element of the
[health service] reforms of recent years” (p 66). A report by
the King’s Fund again highlighted the failure of the NHS to
engage doctors in management and leadership and that “man-
agement and leadership needs to be shared between managers
and clinicians and equally valued by both” (p xi).36
The evidence for this lack of engagement highlights three
factors that prevent clinical leadership from being embraced:
reluctance of doctors to enter into management, weak incen-
tives for leadership activities, and the lack of provision of
training or nurturing mechanisms for young clinicians wish-
ing to engage with this aspect of health care provision.
Ham8 recognizes that change is incremental, slow, and
painstaking work, which can be at odds with policymakers
and taxpayers who want to see quick results. There is a mis-
match between those introducing the bottom-up incremental
changes for effective and enduring service improvement
compared to the expectations of policymakers who want “big
bang reforms” (p 2).8 Clinicians are used to the immediacy
of delivering patient care and are reticent to shift their focus
to leadership, where rewards are longer term and often not
easily defined.71 Among doctors, the emphasis through-
out training is on “individual action and accountability”
(p 483), and they often cannot conceive how leadership can
be relevant to patient care.72 Doctors also face consider-
able pressure to meet clinical targets, and a recent British
Medical Association review found a consistent barrier for
Journal of Healthcare Leadership downloaded from https://www.dovepress.com/ by 193.93.195.147 on 25-Aug-2018
For personal use only.
Powered by TCPDF (www.tcpdf.org)
Dovepress
Dovepress
114
Aggarwal and Swanwick
Does clinical leadership make a
difference?
Effective leadership is an important component of success-
ful health care organizations,53,54 whereas lack of leadership
can be associated with organizational failure.4,55 Veronesi
et al56 suggest clinical leaders influence health care system
outcomes since they have the expert knowledge of the core
business of health services and a deeper awareness of what
patient care involves … [to] make better informed decisions
regarding service design and resource allocation.
Forbes et al57 describe “role design” for clinician manag-
ers, who, instead of replicating the role of hospital managers,
use their unique voice to focus on clinical priorities.
There is a growing literature on the benefit of clinicians
in management and evidence that high-performing medical
groups build relationships with managers, with an emphasis
on clinical quality.58,59 Clinicians in senior management roles
tend to enhance operational outcomes for hospitals and orga-
nizations perform significantly better than those with lower
levels of clinician participation.60–63 A review conducted by
the Academy of Royal Medical Colleges in the UK concluded
that chief executive officers from high-performing institutions
engaged clinicians in dialogue and joint problem solving.64
Goodall65 demonstrates that hospital quality scores are 25%
higher in physician-headed hospitals compared to those with
chief executive officers from nonmedical backgrounds. More
recently, research undertaken by Veronesi et al56 in the UK
tentatively suggested that the “share of doctors” on the board
made most difference, and this relationship became less robust
when other health professionals were involved at board level.
This chimes with Dorgan et al 6 who investigated organiza-
tions across seven countries and suggested that having higher
proportions of medically qualified managers results in more
effective management practices.
It can be difficult to quantify the exact impact of clini-
cal leadership on service quality; however, studies do exist
which suggest improvements in various domains. A study
of hospitals in Michigan found that by using bed occupancy
rates and market share as performance measures and by
excluding clinical leaders from strategic decisions resulted
in lower hospital performance.66 Keroack et al67 ranked
health care institutions using a composite index of qual-
ity and safety that was developed to incorporate domains
identified as attributes of an ideal health care system. High
performance scores for organizations were associated with
organizational leadership that prioritized patients, focused
on quality and safety, used clear systems of accountability,
sought continual improvement as evidenced by results, and
emphasized collaboration between different staff groups
to make use of their varied expertise. Commissioned by
the King’s Fund to inform the leadership commission,
Baker68 used case studies to identify factors accounting
for success in high-performing systems; again, clinical
leadership that prioritized patients, quality and safety,
and that promoted collaborative working between differ-
ent professional groups was consistently present in all of
these institutions.
Barriers to clinical leadership
development
It becomes increasingly clear that clinical leadership is a cen-
tral ingredient to improve the quality of health care.36,69 It is
an essential component to align process redesign for business
operations and quality assurance, with clinical agendas per-
taining to patient care, service development, and professional
development for high quality services. Yet, despite the wealth
of evidence concerning the importance of clinical leadership
in health care organizations, it remains a variable constituent
of health systems. Darzi70 concluded in the NHS Next Stage
Review that “leadership has been the neglected element of the
[health service] reforms of recent years” (p 66). A report by
the King’s Fund again highlighted the failure of the NHS to
engage doctors in management and leadership and that “man-
agement and leadership needs to be shared between managers
and clinicians and equally valued by both” (p xi).36
The evidence for this lack of engagement highlights three
factors that prevent clinical leadership from being embraced:
reluctance of doctors to enter into management, weak incen-
tives for leadership activities, and the lack of provision of
training or nurturing mechanisms for young clinicians wish-
ing to engage with this aspect of health care provision.
Ham8 recognizes that change is incremental, slow, and
painstaking work, which can be at odds with policymakers
and taxpayers who want to see quick results. There is a mis-
match between those introducing the bottom-up incremental
changes for effective and enduring service improvement
compared to the expectations of policymakers who want “big
bang reforms” (p 2).8 Clinicians are used to the immediacy
of delivering patient care and are reticent to shift their focus
to leadership, where rewards are longer term and often not
easily defined.71 Among doctors, the emphasis through-
out training is on “individual action and accountability”
(p 483), and they often cannot conceive how leadership can
be relevant to patient care.72 Doctors also face consider-
able pressure to meet clinical targets, and a recent British
Medical Association review found a consistent barrier for
Journal of Healthcare Leadership downloaded from https://www.dovepress.com/ by 193.93.195.147 on 25-Aug-2018
For personal use only.
Powered by TCPDF (www.tcpdf.org)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

Journal of Healthcare Leadership 2015:7 submit your manuscript | www.dovepress.com
Dovepress
Dovepress
115
Leadership development in postgraduate medical education and trainin
engagement in leadership to be a lack of time and resources
to meet clinical priorities.73 So, time away from patient care
to concentrate on management and leadership is perceived
as a distraction unless doctors have robust evidence for the
value of such activities.
Despite the recent foregrounding of clinicians in manage-
ment and the emergence of a new definition of the medical
professional, tribalism and an ingrained distrust of doctors
entering the management sphere persists. Clinicians function
in an era of evidence-based practice and can have entrenched
views about the credibility and value of leadership. Degeling
et al74 accept that clinical leaders are well placed to take
forward NHS reforms, but find reluctance among medical
managers to question the perceived dominance of medicine in
clinical settings, thus making collective working difficult. On
the other side, a culture of “antimanagerialism” exists where
clinical leader colleagues are described as having gone “over
to the dark side”.71,75,76
Mintzberg77 (p 199) believes that clinicians and clinical
leaders fail to understand the role of professional manag-
ers, perceiving them as servants in the system as opposed
to powerful allies, seated at “the locus of uncertainty” and
able to influence the power afforded to clinicians within the
organization. Edmonstone78 is brutal in chastising clinicians
for working in uniprofessional silos, which he claims prevents
effective and safe delivery of health care. He offers an alter-
native where effective organizations have models of service
delivery based upon supportive team structures, learning
from mistakes, and instigation of service change.
Alongside these issues, incentives for entering into such
activities are weak. There is no predefined career structure
for service leadership, with promotion and remuneration
linked to clinical activities as opposed to participation in
management. Measurement of quality of care is imperfect
and rudimentary; therefore, it is not possible to reward those
who build the best services unlike those who receive financial
accolades for clinical or research activity. Moreover, tradi-
tional role models for clinicians are individuals who excel in
the practice of their profession and not organizational leaders.
Leadership is not viewed as equivalent to research, where
participation in the latter results in career advancement,
prestige, influence, promotion, and financial reward.2
For learners in the health care professions, there has been
little provision for clinical leadership development in the
past, with training and education in this area being largely
absent from core curricula. However, this is changing. The
undergraduate curricula developed by the Nursing and
Midwifery Council (2010) and the General Medical Council
(2009) have started to reflect the need for clinical leadership
development in the preregistration workforce, and all post-
graduate curricula now contain intended learning outcomes
in the area of leadership and management. But embedding a
leadership competency framework into professional curricula
is merely a start.79
The bulk of the professional workforce are already active
in the NHS and often represent the front line of service,
whom Swanwick19 states “have the capability, energy, and
enthusiasm to transform the NHS” (p 117). In Denmark, an
explicit aim to increase the number of doctors stepping into
leadership roles has shifted the culture to not only impact
medical behavior and curricula, but also form the basis of
appointment criteria.80 Danish postgraduate doctors receive
mandatory leadership training based upon the CanMEDS
roles framework,81 and after consultant appointment, they
are expected to participate in leadership development
programs.10 A similar robust program of systematic leader-
ship development utilizing CanMEDS is also evident in the
Netherlands.10
In their extensive review of theoretical and empirical
literature of leadership and leadership development, Day
et al82 conclude that while leadership is something that all
organizations value, they are much less interested in which
theory or model is the “right” approach, instead they want to
know how to develop leaders and leadership as effectively and
efficiently as possible. In the next section of this paper, we
provide a review of some of the leadership interventions for
junior doctors that have been utilized in the UK and attempt
to identify the hallmarks of effective leadership development
in this context.
Leadership development of junior
doctors in the UK
Against this backdrop of evidence for the impact of clinical
leadership and the significant issues surrounding its prac-
tice, a raft of interventions has been deployed in an effort to
engage young clinicians in leadership activities. Leadership
development interventions in common use range from one-
day workshops, short courses, experiential programs to
postgraduate masters and doctoral awards. A number of these
approaches are now explored in more depth.
Competency frameworks
In early 2000, the NHS in England commissioned Hay Group
management consultancy to identify a core set of leader-
ship qualities associated with success at chief executive and
executive director levels, which lead to the production of
Journal of Healthcare Leadership downloaded from https://www.dovepress.com/ by 193.93.195.147 on 25-Aug-2018
For personal use only.
Powered by TCPDF (www.tcpdf.org)
Dovepress
Dovepress
115
Leadership development in postgraduate medical education and trainin
engagement in leadership to be a lack of time and resources
to meet clinical priorities.73 So, time away from patient care
to concentrate on management and leadership is perceived
as a distraction unless doctors have robust evidence for the
value of such activities.
Despite the recent foregrounding of clinicians in manage-
ment and the emergence of a new definition of the medical
professional, tribalism and an ingrained distrust of doctors
entering the management sphere persists. Clinicians function
in an era of evidence-based practice and can have entrenched
views about the credibility and value of leadership. Degeling
et al74 accept that clinical leaders are well placed to take
forward NHS reforms, but find reluctance among medical
managers to question the perceived dominance of medicine in
clinical settings, thus making collective working difficult. On
the other side, a culture of “antimanagerialism” exists where
clinical leader colleagues are described as having gone “over
to the dark side”.71,75,76
Mintzberg77 (p 199) believes that clinicians and clinical
leaders fail to understand the role of professional manag-
ers, perceiving them as servants in the system as opposed
to powerful allies, seated at “the locus of uncertainty” and
able to influence the power afforded to clinicians within the
organization. Edmonstone78 is brutal in chastising clinicians
for working in uniprofessional silos, which he claims prevents
effective and safe delivery of health care. He offers an alter-
native where effective organizations have models of service
delivery based upon supportive team structures, learning
from mistakes, and instigation of service change.
Alongside these issues, incentives for entering into such
activities are weak. There is no predefined career structure
for service leadership, with promotion and remuneration
linked to clinical activities as opposed to participation in
management. Measurement of quality of care is imperfect
and rudimentary; therefore, it is not possible to reward those
who build the best services unlike those who receive financial
accolades for clinical or research activity. Moreover, tradi-
tional role models for clinicians are individuals who excel in
the practice of their profession and not organizational leaders.
Leadership is not viewed as equivalent to research, where
participation in the latter results in career advancement,
prestige, influence, promotion, and financial reward.2
For learners in the health care professions, there has been
little provision for clinical leadership development in the
past, with training and education in this area being largely
absent from core curricula. However, this is changing. The
undergraduate curricula developed by the Nursing and
Midwifery Council (2010) and the General Medical Council
(2009) have started to reflect the need for clinical leadership
development in the preregistration workforce, and all post-
graduate curricula now contain intended learning outcomes
in the area of leadership and management. But embedding a
leadership competency framework into professional curricula
is merely a start.79
The bulk of the professional workforce are already active
in the NHS and often represent the front line of service,
whom Swanwick19 states “have the capability, energy, and
enthusiasm to transform the NHS” (p 117). In Denmark, an
explicit aim to increase the number of doctors stepping into
leadership roles has shifted the culture to not only impact
medical behavior and curricula, but also form the basis of
appointment criteria.80 Danish postgraduate doctors receive
mandatory leadership training based upon the CanMEDS
roles framework,81 and after consultant appointment, they
are expected to participate in leadership development
programs.10 A similar robust program of systematic leader-
ship development utilizing CanMEDS is also evident in the
Netherlands.10
In their extensive review of theoretical and empirical
literature of leadership and leadership development, Day
et al82 conclude that while leadership is something that all
organizations value, they are much less interested in which
theory or model is the “right” approach, instead they want to
know how to develop leaders and leadership as effectively and
efficiently as possible. In the next section of this paper, we
provide a review of some of the leadership interventions for
junior doctors that have been utilized in the UK and attempt
to identify the hallmarks of effective leadership development
in this context.
Leadership development of junior
doctors in the UK
Against this backdrop of evidence for the impact of clinical
leadership and the significant issues surrounding its prac-
tice, a raft of interventions has been deployed in an effort to
engage young clinicians in leadership activities. Leadership
development interventions in common use range from one-
day workshops, short courses, experiential programs to
postgraduate masters and doctoral awards. A number of these
approaches are now explored in more depth.
Competency frameworks
In early 2000, the NHS in England commissioned Hay Group
management consultancy to identify a core set of leader-
ship qualities associated with success at chief executive and
executive director levels, which lead to the production of
Journal of Healthcare Leadership downloaded from https://www.dovepress.com/ by 193.93.195.147 on 25-Aug-2018
For personal use only.
Powered by TCPDF (www.tcpdf.org)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Journal of Healthcare Leadership 2015:7submit your manuscript | www.dovepress.com
Dovepress
Dovepress
116
Aggarwal and Swanwick
the Leadership Qualities Framework published in 2002 and
further reviewed in 2006.83 This identified 15 personal, cogni-
tive, and social qualities essential for successful leadership
across health services. These qualities are clustered into
three broader domains: personal qualities, setting direction,
and delivering the service. This led to the development of the
Medical Leadership Competency Framework (MLCF) by the
Academy of Royal Medical Colleges. The MLCF codifies
20 elements essential for effective medical leadership that
are divided into five leadership competency domains needed
to plan, deliver, and transform health services. A perceived
advantage of the MLCF is its continuous nature being pur-
posefully designed for championing leadership on the front
line commencing from medical school and crucially to make
this a “normal part of their roles as doctors” (p 110). 68 It
embeds acquisition of leadership and management skills as a
core function as opposed to an extracurricular activity. While
these competency domains may be necessary for clinical lead-
ership, they are by no means sufficient to build up the social
capital required for collaborative and supportive change.84
In relation to the wider NHS in England, an NHS Leader-
ship Academy was set up in 2012 as an umbrella organization
to bring together all national activity supporting leadership
development in health and NHS funded services. In 2013, it
launched an array of national programs that it described as
“the most far-reaching and comprehensive leadership devel-
opment portfolio the NHS has ever developed”, designed to
support staff from a diverse range of clinical and nonclinical
backgrounds to create “a more capable and compassion-
ate” health care system. 85 The programs range from online
introductions through master-level courses to action learning
orientated offerings for senior leaders. In parallel, the Acad-
emy has developed a new framework to underpin its work,
the Healthcare Leadership Model.86
Opponents of competency frameworks contend it is a
reductionist approach,87 steering learners toward a tick box
attitude and neglecting the emotional intelligence needed for
leadership.88 Edmonstone89 suggests that leadership needs to
move beyond explicit knowledge embodying competence
(solving “tame” issues which are clear and unambiguous
problems), but neglects tacit knowledge, which is learned
through experience and creates capability to tackle “wicked”
problems. McKimm and Swanwick90 agree that the compe-
tency approach can reinforce particular conceptions of leader-
ship, such as a trait-based approach, but are more conciliatory
and suggest that frameworks like the MLCF serve to raise
the profile of leadership and provide a common language to
use in interrogating its nature.
Talent management
Forbes et al57 identified two roles generally taken by clinicians
engaged in management – investors pursuing management
as an alternative to clinical medicine and reluctants assum-
ing management roles as protective custodians for their
specialty from others. The authors identified that neither
the reluctants nor investors had sufficient understanding
or contact with management prior to taking on their roles,
and therefore advocate earlier preparation of clinicians to
develop a “managerial self ” and a process of “management
talent”, whereby clinicians interested in management are
identified at an earlier point in their careers and supported
to develop these skills. Spehar et al91 found path dependency
and social pressure to influence clinicians’ decisions to enter
into management positions, and they also suggest formalized
pathways to attract and retain early stage clinicians into man-
agement. Talent management systems and whole organization
approaches to leadership development are now widespread
in the NHS, but because of the transient nature of the junior
doctor population, they tend to eschew this large section of
the clinical workforce.
Shared learning
In deconstructing the physical and conceptual barriers
between managers and clinicians, programs have been devel-
oped with a shadowing approach where seemingly opposite
sides of the leadership divide, meet and understand, and
appreciate and collaborate for enhanced delivery of care.
In 2008, NHS London set up ‘Prepare to Lead’ - a leadership
development mentoring scheme, which ran complementary
to clinical training. This scheme matched selected high
potential registrars or newly qualified general practitioners
into mentoring relationships with senior health care leaders
from the NHS or the private sector.92 The year-long pro-
gram involved action learning sets and mentoring by senior
clinical leaders to equip these clinicians with the ability to
progress to strategic organizational level responsibilities in
their future careers.
Other examples include pairing of a management trainee
with a foundation level junior doctor who work together over
a period of 6–9 months to enhance patient care. 93 Hawken
et al97 argue that this experience allowed doctors and manag-
ers to obtain shared learning and understanding of “… areas
of practice and expertise at an early stage of their careers
and to begin developing leadership skills”, which they hope
would normalize this “integration at a much earlier point of
a medical career”. This approach has been further developed
in schemes where registrars were paired with middle level
Journal of Healthcare Leadership downloaded from https://www.dovepress.com/ by 193.93.195.147 on 25-Aug-2018
For personal use only.
Powered by TCPDF (www.tcpdf.org)
Dovepress
Dovepress
116
Aggarwal and Swanwick
the Leadership Qualities Framework published in 2002 and
further reviewed in 2006.83 This identified 15 personal, cogni-
tive, and social qualities essential for successful leadership
across health services. These qualities are clustered into
three broader domains: personal qualities, setting direction,
and delivering the service. This led to the development of the
Medical Leadership Competency Framework (MLCF) by the
Academy of Royal Medical Colleges. The MLCF codifies
20 elements essential for effective medical leadership that
are divided into five leadership competency domains needed
to plan, deliver, and transform health services. A perceived
advantage of the MLCF is its continuous nature being pur-
posefully designed for championing leadership on the front
line commencing from medical school and crucially to make
this a “normal part of their roles as doctors” (p 110). 68 It
embeds acquisition of leadership and management skills as a
core function as opposed to an extracurricular activity. While
these competency domains may be necessary for clinical lead-
ership, they are by no means sufficient to build up the social
capital required for collaborative and supportive change.84
In relation to the wider NHS in England, an NHS Leader-
ship Academy was set up in 2012 as an umbrella organization
to bring together all national activity supporting leadership
development in health and NHS funded services. In 2013, it
launched an array of national programs that it described as
“the most far-reaching and comprehensive leadership devel-
opment portfolio the NHS has ever developed”, designed to
support staff from a diverse range of clinical and nonclinical
backgrounds to create “a more capable and compassion-
ate” health care system. 85 The programs range from online
introductions through master-level courses to action learning
orientated offerings for senior leaders. In parallel, the Acad-
emy has developed a new framework to underpin its work,
the Healthcare Leadership Model.86
Opponents of competency frameworks contend it is a
reductionist approach,87 steering learners toward a tick box
attitude and neglecting the emotional intelligence needed for
leadership.88 Edmonstone89 suggests that leadership needs to
move beyond explicit knowledge embodying competence
(solving “tame” issues which are clear and unambiguous
problems), but neglects tacit knowledge, which is learned
through experience and creates capability to tackle “wicked”
problems. McKimm and Swanwick90 agree that the compe-
tency approach can reinforce particular conceptions of leader-
ship, such as a trait-based approach, but are more conciliatory
and suggest that frameworks like the MLCF serve to raise
the profile of leadership and provide a common language to
use in interrogating its nature.
Talent management
Forbes et al57 identified two roles generally taken by clinicians
engaged in management – investors pursuing management
as an alternative to clinical medicine and reluctants assum-
ing management roles as protective custodians for their
specialty from others. The authors identified that neither
the reluctants nor investors had sufficient understanding
or contact with management prior to taking on their roles,
and therefore advocate earlier preparation of clinicians to
develop a “managerial self ” and a process of “management
talent”, whereby clinicians interested in management are
identified at an earlier point in their careers and supported
to develop these skills. Spehar et al91 found path dependency
and social pressure to influence clinicians’ decisions to enter
into management positions, and they also suggest formalized
pathways to attract and retain early stage clinicians into man-
agement. Talent management systems and whole organization
approaches to leadership development are now widespread
in the NHS, but because of the transient nature of the junior
doctor population, they tend to eschew this large section of
the clinical workforce.
Shared learning
In deconstructing the physical and conceptual barriers
between managers and clinicians, programs have been devel-
oped with a shadowing approach where seemingly opposite
sides of the leadership divide, meet and understand, and
appreciate and collaborate for enhanced delivery of care.
In 2008, NHS London set up ‘Prepare to Lead’ - a leadership
development mentoring scheme, which ran complementary
to clinical training. This scheme matched selected high
potential registrars or newly qualified general practitioners
into mentoring relationships with senior health care leaders
from the NHS or the private sector.92 The year-long pro-
gram involved action learning sets and mentoring by senior
clinical leaders to equip these clinicians with the ability to
progress to strategic organizational level responsibilities in
their future careers.
Other examples include pairing of a management trainee
with a foundation level junior doctor who work together over
a period of 6–9 months to enhance patient care. 93 Hawken
et al97 argue that this experience allowed doctors and manag-
ers to obtain shared learning and understanding of “… areas
of practice and expertise at an early stage of their careers
and to begin developing leadership skills”, which they hope
would normalize this “integration at a much earlier point of
a medical career”. This approach has been further developed
in schemes where registrars were paired with middle level
Journal of Healthcare Leadership downloaded from https://www.dovepress.com/ by 193.93.195.147 on 25-Aug-2018
For personal use only.
Powered by TCPDF (www.tcpdf.org)
Journal of Healthcare Leadership 2015:7 submit your manuscript | www.dovepress.com
Dovepress
Dovepress
117
Leadership development in postgraduate medical education and trainin
managers within organizations to provide practical leadership
experience and education.94,95 These programs used a combi-
nation of informal conversation, shadowing, workshops, and
improvement skills to enable participants to better understand
each other’s perspectives and to drive learning. According to
Klaber and Lee,94 short-term gains have included demonstra-
ble changes in quality of patient care and greater efficiency;
however, more exciting is the longer term gain of cultural
change between managers and junior doctors, allowing for
more collaborative working in the future.
Secondments and clinical
fellowships
In recent years, secondments and clinical fellowships have
become a popular way for junior doctors to “dip a toe” into
a different world and experience clinical leadership, policy
making, and strategic decision-making outside of the clinical
training environment. There are a number of national and
international fellowships that have been developed to enable
identification of future leaders and provide a mixture of train-
ing, mentoring, and leadership experience.96
The National Medical Director’s Clinical Fellow Scheme
provides doctors in training with the unique opportunity to
spend 1 year in a national healthcare-affiliated organization
to develop their skills in leadership, management, strategy,
project management, and health policy.97
This scheme has grown from a pilot scheme in 2008 and
affords junior doctors the opportunity to work as clinical
advisors to senior medical directors within organizations as
diverse as NHS England, Bupa, National Institute of Clinical
Excellence, and the Royal Colleges. The scheme is a mixture
of day-to-day experiences within the organization, learning
sets, and personal development sessions, which can focus
on public speaking, publication, or networking. Advantages
of this scheme include the opportunity for junior doctors to
understand organizational function, decision-making, and
policy implementation within health systems.98 It has helped
shape personal careers for previous incumbents and offers an
insight into theory and practice of leadership.
In London, a highly successful 12-month “out of program”
experience for a cohort of junior doctors was designed to
develop the organizational and leadership capability for future
roles as clinical leaders.99 Now in its 7th year, the scheme has
expanded to not only include doctors in training, but also other
health care professionals in their early careers, all of whom work
for a medical or clinical director of an NHS organization.100
Participants undertake a bespoke development program, while
actively leading a change management project. The scheme
also has an academic component with participants completing
an accredited postgraduate certificate as well as a personal
development focus incorporating workshops, coaching, men-
toring, and action learning sets.24
International schemes include the Harkness Fellowships
in Health Policy run by the Commonwealth Fund in USA.101
These fellowships in Health Care Policy and Practice pro-
vide a unique opportunity for mid-career health services
researchers and practitioners from Australia, Canada,
France, Germany, the Netherlands, New Zealand, Norway,
Sweden, and the UK to spend up to 12 months in the
USA, conducting original research and working with leading
US health policy experts. A stipend is provided, and fellows
divide their time between research under the mentorship of
a host organization in the USA and learning about health
policy as a group.
There is no doubt that the fellowships described above
offer junior doctors an invaluable opportunity to expand their
clinical training to develop an appreciation of managerial,
leadership, and policy concerns. As a junior doctor, much
of this can seem opaque, and these opportunities may help
to illuminate these important areas. Most fellowships ensure
leadership development is rooted in project-orientated work-
based activities. However, Nicol96 suggests there may be
lack of clarity as to the ultimate aim of fellowships which
may develop the “hero” clinical leader, but may also disen-
gage others when faced with lack of clinical credibility or
authority. Additionally, is the learning that arises from such
fellowships harnessed and disseminated when the fellows
return to their clinical roles after their period of secondment?
Stoll et al99 recognize that such fellowships are a healthy start
as they begin to “spawn[ing] clinical leadership development
throughout the wider health care system” (p 284), but whole-
system engagement of doctors in training requires more
than a fellowship that is available only to a small number
of self-selected, highly motivated individuals.
Quality improvement
As the emphasis moves away from the “hero” clinical leader
and more toward a culture of learning throughout and within
the organizations, quality improvement has become the
tool with which to instill distributed leadership. Bohmer 72
described this form of leadership as leadership with a small
“L” which is exercised at the level of team, ward, unit, and
department, and the goal is to oversee the local system of
care in which patients receive care. All members of the
health care team, including junior doctors, are part of this
leadership; it does not require doctors to step out of clinical
Journal of Healthcare Leadership downloaded from https://www.dovepress.com/ by 193.93.195.147 on 25-Aug-2018
For personal use only.
Powered by TCPDF (www.tcpdf.org)
Dovepress
Dovepress
117
Leadership development in postgraduate medical education and trainin
managers within organizations to provide practical leadership
experience and education.94,95 These programs used a combi-
nation of informal conversation, shadowing, workshops, and
improvement skills to enable participants to better understand
each other’s perspectives and to drive learning. According to
Klaber and Lee,94 short-term gains have included demonstra-
ble changes in quality of patient care and greater efficiency;
however, more exciting is the longer term gain of cultural
change between managers and junior doctors, allowing for
more collaborative working in the future.
Secondments and clinical
fellowships
In recent years, secondments and clinical fellowships have
become a popular way for junior doctors to “dip a toe” into
a different world and experience clinical leadership, policy
making, and strategic decision-making outside of the clinical
training environment. There are a number of national and
international fellowships that have been developed to enable
identification of future leaders and provide a mixture of train-
ing, mentoring, and leadership experience.96
The National Medical Director’s Clinical Fellow Scheme
provides doctors in training with the unique opportunity to
spend 1 year in a national healthcare-affiliated organization
to develop their skills in leadership, management, strategy,
project management, and health policy.97
This scheme has grown from a pilot scheme in 2008 and
affords junior doctors the opportunity to work as clinical
advisors to senior medical directors within organizations as
diverse as NHS England, Bupa, National Institute of Clinical
Excellence, and the Royal Colleges. The scheme is a mixture
of day-to-day experiences within the organization, learning
sets, and personal development sessions, which can focus
on public speaking, publication, or networking. Advantages
of this scheme include the opportunity for junior doctors to
understand organizational function, decision-making, and
policy implementation within health systems.98 It has helped
shape personal careers for previous incumbents and offers an
insight into theory and practice of leadership.
In London, a highly successful 12-month “out of program”
experience for a cohort of junior doctors was designed to
develop the organizational and leadership capability for future
roles as clinical leaders.99 Now in its 7th year, the scheme has
expanded to not only include doctors in training, but also other
health care professionals in their early careers, all of whom work
for a medical or clinical director of an NHS organization.100
Participants undertake a bespoke development program, while
actively leading a change management project. The scheme
also has an academic component with participants completing
an accredited postgraduate certificate as well as a personal
development focus incorporating workshops, coaching, men-
toring, and action learning sets.24
International schemes include the Harkness Fellowships
in Health Policy run by the Commonwealth Fund in USA.101
These fellowships in Health Care Policy and Practice pro-
vide a unique opportunity for mid-career health services
researchers and practitioners from Australia, Canada,
France, Germany, the Netherlands, New Zealand, Norway,
Sweden, and the UK to spend up to 12 months in the
USA, conducting original research and working with leading
US health policy experts. A stipend is provided, and fellows
divide their time between research under the mentorship of
a host organization in the USA and learning about health
policy as a group.
There is no doubt that the fellowships described above
offer junior doctors an invaluable opportunity to expand their
clinical training to develop an appreciation of managerial,
leadership, and policy concerns. As a junior doctor, much
of this can seem opaque, and these opportunities may help
to illuminate these important areas. Most fellowships ensure
leadership development is rooted in project-orientated work-
based activities. However, Nicol96 suggests there may be
lack of clarity as to the ultimate aim of fellowships which
may develop the “hero” clinical leader, but may also disen-
gage others when faced with lack of clinical credibility or
authority. Additionally, is the learning that arises from such
fellowships harnessed and disseminated when the fellows
return to their clinical roles after their period of secondment?
Stoll et al99 recognize that such fellowships are a healthy start
as they begin to “spawn[ing] clinical leadership development
throughout the wider health care system” (p 284), but whole-
system engagement of doctors in training requires more
than a fellowship that is available only to a small number
of self-selected, highly motivated individuals.
Quality improvement
As the emphasis moves away from the “hero” clinical leader
and more toward a culture of learning throughout and within
the organizations, quality improvement has become the
tool with which to instill distributed leadership. Bohmer 72
described this form of leadership as leadership with a small
“L” which is exercised at the level of team, ward, unit, and
department, and the goal is to oversee the local system of
care in which patients receive care. All members of the
health care team, including junior doctors, are part of this
leadership; it does not require doctors to step out of clinical
Journal of Healthcare Leadership downloaded from https://www.dovepress.com/ by 193.93.195.147 on 25-Aug-2018
For personal use only.
Powered by TCPDF (www.tcpdf.org)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
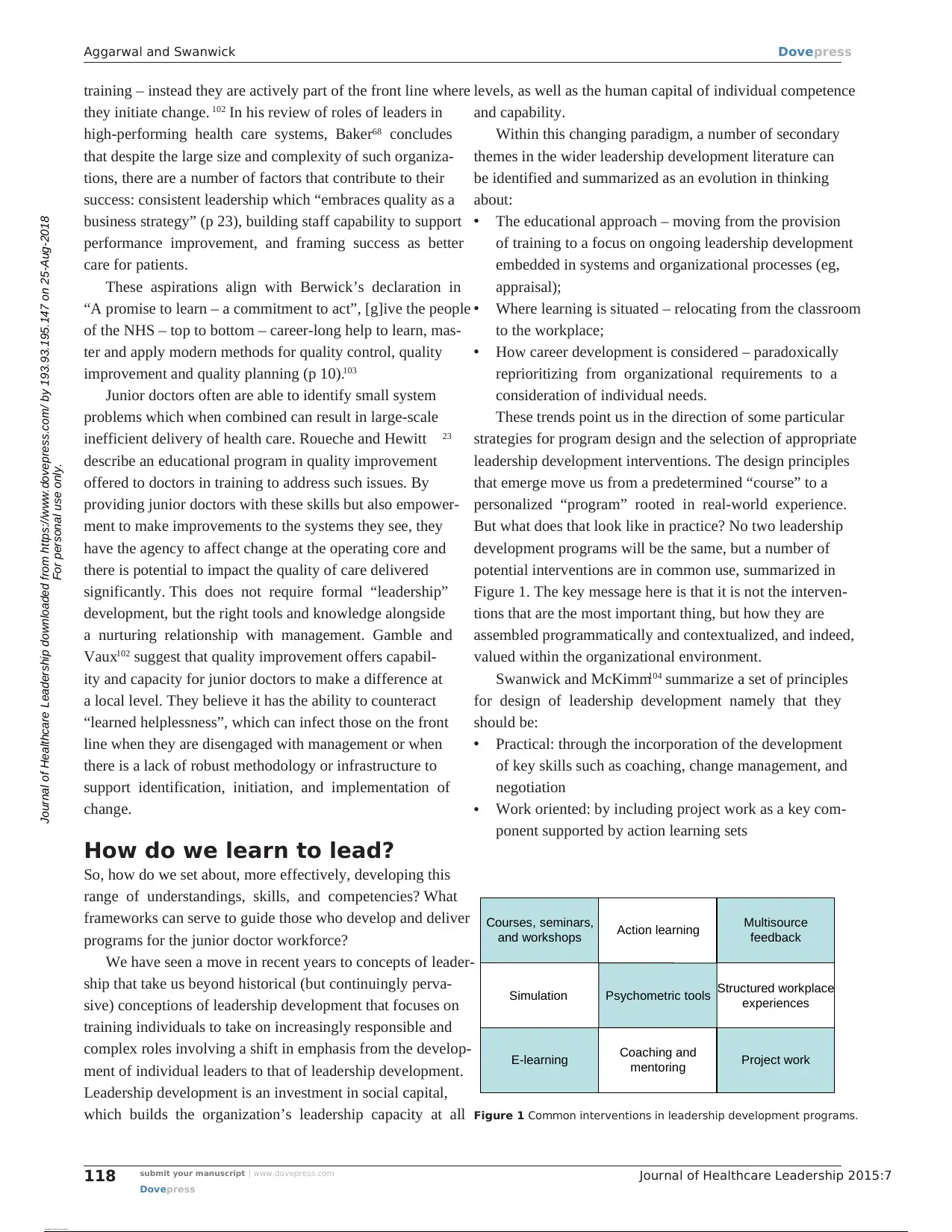
Journal of Healthcare Leadership 2015:7submit your manuscript | www.dovepress.com
Dovepress
Dovepress
118
Aggarwal and Swanwick
training – instead they are actively part of the front line where
they initiate change. 102 In his review of roles of leaders in
high-performing health care systems, Baker68 concludes
that despite the large size and complexity of such organiza-
tions, there are a number of factors that contribute to their
success: consistent leadership which “embraces quality as a
business strategy” (p 23), building staff capability to support
performance improvement, and framing success as better
care for patients.
These aspirations align with Berwick’s declaration in
“A promise to learn – a commitment to act”, [g]ive the people
of the NHS – top to bottom – career-long help to learn, mas-
ter and apply modern methods for quality control, quality
improvement and quality planning (p 10).103
Junior doctors often are able to identify small system
problems which when combined can result in large-scale
inefficient delivery of health care. Roueche and Hewitt 23
describe an educational program in quality improvement
offered to doctors in training to address such issues. By
providing junior doctors with these skills but also empower-
ment to make improvements to the systems they see, they
have the agency to affect change at the operating core and
there is potential to impact the quality of care delivered
significantly. This does not require formal “leadership”
development, but the right tools and knowledge alongside
a nurturing relationship with management. Gamble and
Vaux102 suggest that quality improvement offers capabil-
ity and capacity for junior doctors to make a difference at
a local level. They believe it has the ability to counteract
“learned helplessness”, which can infect those on the front
line when they are disengaged with management or when
there is a lack of robust methodology or infrastructure to
support identification, initiation, and implementation of
change.
How do we learn to lead?
So, how do we set about, more effectively, developing this
range of understandings, skills, and competencies? What
frameworks can serve to guide those who develop and deliver
programs for the junior doctor workforce?
We have seen a move in recent years to concepts of leader-
ship that take us beyond historical (but continuingly perva-
sive) conceptions of leadership development that focuses on
training individuals to take on increasingly responsible and
complex roles involving a shift in emphasis from the develop-
ment of individual leaders to that of leadership development.
Leadership development is an investment in social capital,
which builds the organization’s leadership capacity at all
levels, as well as the human capital of individual competence
and capability.
Within this changing paradigm, a number of secondary
themes in the wider leadership development literature can
be identified and summarized as an evolution in thinking
about:
• The educational approach – moving from the provision
of training to a focus on ongoing leadership development
embedded in systems and organizational processes (eg,
appraisal);
• Where learning is situated – relocating from the classroom
to the workplace;
• How career development is considered – paradoxically
reprioritizing from organizational requirements to a
consideration of individual needs.
These trends point us in the direction of some particular
strategies for program design and the selection of appropriate
leadership development interventions. The design principles
that emerge move us from a predetermined “course” to a
personalized “program” rooted in real-world experience.
But what does that look like in practice? No two leadership
development programs will be the same, but a number of
potential interventions are in common use, summarized in
Figure 1. The key message here is that it is not the interven-
tions that are the most important thing, but how they are
assembled programmatically and contextualized, and indeed,
valued within the organizational environment.
Swanwick and McKimm104 summarize a set of principles
for design of leadership development namely that they
should be:
• Practical: through the incorporation of the development
of key skills such as coaching, change management, and
negotiation
• Work oriented: by including project work as a key com-
ponent supported by action learning sets
Courses, seminars,
and workshops
Simulation
E-learning
Action learning
Psychometric tools
Coaching and
mentoring
Multisource
feedback
Structured workplace
experiences
Project work
Figure 1 Common interventions in leadership development programs.
Journal of Healthcare Leadership downloaded from https://www.dovepress.com/ by 193.93.195.147 on 25-Aug-2018
For personal use only.
Powered by TCPDF (www.tcpdf.org)
Dovepress
Dovepress
118
Aggarwal and Swanwick
training – instead they are actively part of the front line where
they initiate change. 102 In his review of roles of leaders in
high-performing health care systems, Baker68 concludes
that despite the large size and complexity of such organiza-
tions, there are a number of factors that contribute to their
success: consistent leadership which “embraces quality as a
business strategy” (p 23), building staff capability to support
performance improvement, and framing success as better
care for patients.
These aspirations align with Berwick’s declaration in
“A promise to learn – a commitment to act”, [g]ive the people
of the NHS – top to bottom – career-long help to learn, mas-
ter and apply modern methods for quality control, quality
improvement and quality planning (p 10).103
Junior doctors often are able to identify small system
problems which when combined can result in large-scale
inefficient delivery of health care. Roueche and Hewitt 23
describe an educational program in quality improvement
offered to doctors in training to address such issues. By
providing junior doctors with these skills but also empower-
ment to make improvements to the systems they see, they
have the agency to affect change at the operating core and
there is potential to impact the quality of care delivered
significantly. This does not require formal “leadership”
development, but the right tools and knowledge alongside
a nurturing relationship with management. Gamble and
Vaux102 suggest that quality improvement offers capabil-
ity and capacity for junior doctors to make a difference at
a local level. They believe it has the ability to counteract
“learned helplessness”, which can infect those on the front
line when they are disengaged with management or when
there is a lack of robust methodology or infrastructure to
support identification, initiation, and implementation of
change.
How do we learn to lead?
So, how do we set about, more effectively, developing this
range of understandings, skills, and competencies? What
frameworks can serve to guide those who develop and deliver
programs for the junior doctor workforce?
We have seen a move in recent years to concepts of leader-
ship that take us beyond historical (but continuingly perva-
sive) conceptions of leadership development that focuses on
training individuals to take on increasingly responsible and
complex roles involving a shift in emphasis from the develop-
ment of individual leaders to that of leadership development.
Leadership development is an investment in social capital,
which builds the organization’s leadership capacity at all
levels, as well as the human capital of individual competence
and capability.
Within this changing paradigm, a number of secondary
themes in the wider leadership development literature can
be identified and summarized as an evolution in thinking
about:
• The educational approach – moving from the provision
of training to a focus on ongoing leadership development
embedded in systems and organizational processes (eg,
appraisal);
• Where learning is situated – relocating from the classroom
to the workplace;
• How career development is considered – paradoxically
reprioritizing from organizational requirements to a
consideration of individual needs.
These trends point us in the direction of some particular
strategies for program design and the selection of appropriate
leadership development interventions. The design principles
that emerge move us from a predetermined “course” to a
personalized “program” rooted in real-world experience.
But what does that look like in practice? No two leadership
development programs will be the same, but a number of
potential interventions are in common use, summarized in
Figure 1. The key message here is that it is not the interven-
tions that are the most important thing, but how they are
assembled programmatically and contextualized, and indeed,
valued within the organizational environment.
Swanwick and McKimm104 summarize a set of principles
for design of leadership development namely that they
should be:
• Practical: through the incorporation of the development
of key skills such as coaching, change management, and
negotiation
• Work oriented: by including project work as a key com-
ponent supported by action learning sets
Courses, seminars,
and workshops
Simulation
E-learning
Action learning
Psychometric tools
Coaching and
mentoring
Multisource
feedback
Structured workplace
experiences
Project work
Figure 1 Common interventions in leadership development programs.
Journal of Healthcare Leadership downloaded from https://www.dovepress.com/ by 193.93.195.147 on 25-Aug-2018
For personal use only.
Powered by TCPDF (www.tcpdf.org)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Journal of Healthcare Leadership 2015:7 submit your manuscript | www.dovepress.com
Dovepress
Dovepress
119
Leadership development in postgraduate medical education and trainin
• Supportive of individual development: through 360°
feedback, coaching, and mentoring
• Link theory to practice: through the provision of selected
leadership and management literature, relevant to the
educational context
• Build networks: through action learning, coaching, and
social networking.
At the heart is a debate about whether leadership can be
learned, ie, is leadership a function of personality or a learned
set of behaviors. In reality, it is probably a mix of the two. So,
developing a sense of who you are and how you impact others is
every bit as important as the syllabic content. The implications
of this are then the need to shift from instructor-centered teach-
ing to learner-centered personal transformation.
Leaders or leadership?
As Bolden105 (p 7) explains if we do consider leadership to
be a “collective process”, then leadership development is not
about sending selected individuals to high-level courses and
encouraging others to “follow the leader”. The model of the
leader who will be the “superhero” is not fit for purpose in
the current health care environment (p 18). 36 By choosing
to develop “leaders” as opposed to relationships between
individuals, Edmonstone 106 contends that leadership can
become divorced from the context in which it occurs and fails
to harness the importance of teams and networks, making
leadership a “multi-professional and multi-agency concern”
(p 290). He is critical that most leadership activities in the
NHS have been based upon developing individual leaders
rather than that of “health care leadership”, which is much
more challenging and complex.
Successfully led organizations require empowered mul-
tiprofessional teams where any one member can step up to
the plate to lead. But West et al52 point out that our approach
to leader and leadership development in UK health care is
“distorted by a preoccupation with individual leader devel-
opment (important though it is), often provided by external
providers in remote locations” (p 4). The report reiterates the
view that successful organizations are “leader-ful” not just
“well led”, highlighting that in comparison with the literature
on leader development, “the development of the capacity
of groups and organizations for leadership as a shared and
collective process – is far less well explored and researched”
(p 3)52 and urge that we begin to look in that direction.
Conclusion
There is a growing body of international evidence that when
clinicians are involved in strategic decision-making at an
organizational level, they are able to add their voices to enact
change, which is not only resource friendly but enhances
clinical and operational outcomes. Clinical leadership has
become the “high profile” conduit to enable this to occur.
According to Baker and Denis,107 three elements are
required to develop medical leadership in health care orga-
nizations: encouragement to formal leadership roles; the
promulgation of a collective understanding of organizational
leadership, occurring in a coordinated manner at all levels;
and aligning development of leadership with clear quality
and safety improvement goals at strategic and operational
levels in the organization. Gilbert et al22 state that when doc-
tors in training attend leadership training, they have greater
desire and perceived ability to contribute to improvement
in the NHS.
An express wish of the Medical Director of NHS England
has been that clinicians should routinely be shortlisted senior
positions in health care.24 While this is a laudable aim, this
may continue to perpetuate the historic model of command
and control and a target-driven approach, when we should be
striving for a model of “engaging leadership”.108 This model
is not about being an extraordinary individual but the empha-
sis shifts to “… teamwork, collaboration, connectedness and
removing barriers to communication and original thinking”.109
Leadership then becomes the “cognitive catalyst” (p 8)
and is based upon a shared vision and has to encompass
those on the front line.108 Perhaps, we can take a lesson from
organizations such as Intermountain Healthcare or Kaiser
Permanente in the USA, which invest in formal leadership
development backed up with quality improvement skills that
support this work. In essence, clinicians become involved in
daily management of their institutions alongside long-term
improvement work, translating into enhanced organizational
performance and outcomes.
Bohmer74 states, leadership is not only about the big “L”
(senior leadership roles in organizations), but is also the
very important “leading of the micro-systems that have such
an effect on care outcomes” (p 483). Leadership in high-
performing organizations is not reliant on a charismatic leader;
instead it is distributed in nature, where senior leaders define
strategy, support execution of strategic initiatives, and engage
individuals within the organization to lead on improvement
activities. Ensuring that clinical leadership development has
an equal weight within postgraduate training programs as
clinical skill development is, therefore, essential, if we are to
build health organizations with the capability for continual
improvement in order that they might better meet the future
needs of our patients and local populations.
Journal of Healthcare Leadership downloaded from https://www.dovepress.com/ by 193.93.195.147 on 25-Aug-2018
For personal use only.
Powered by TCPDF (www.tcpdf.org)
Dovepress
Dovepress
119
Leadership development in postgraduate medical education and trainin
• Supportive of individual development: through 360°
feedback, coaching, and mentoring
• Link theory to practice: through the provision of selected
leadership and management literature, relevant to the
educational context
• Build networks: through action learning, coaching, and
social networking.
At the heart is a debate about whether leadership can be
learned, ie, is leadership a function of personality or a learned
set of behaviors. In reality, it is probably a mix of the two. So,
developing a sense of who you are and how you impact others is
every bit as important as the syllabic content. The implications
of this are then the need to shift from instructor-centered teach-
ing to learner-centered personal transformation.
Leaders or leadership?
As Bolden105 (p 7) explains if we do consider leadership to
be a “collective process”, then leadership development is not
about sending selected individuals to high-level courses and
encouraging others to “follow the leader”. The model of the
leader who will be the “superhero” is not fit for purpose in
the current health care environment (p 18). 36 By choosing
to develop “leaders” as opposed to relationships between
individuals, Edmonstone 106 contends that leadership can
become divorced from the context in which it occurs and fails
to harness the importance of teams and networks, making
leadership a “multi-professional and multi-agency concern”
(p 290). He is critical that most leadership activities in the
NHS have been based upon developing individual leaders
rather than that of “health care leadership”, which is much
more challenging and complex.
Successfully led organizations require empowered mul-
tiprofessional teams where any one member can step up to
the plate to lead. But West et al52 point out that our approach
to leader and leadership development in UK health care is
“distorted by a preoccupation with individual leader devel-
opment (important though it is), often provided by external
providers in remote locations” (p 4). The report reiterates the
view that successful organizations are “leader-ful” not just
“well led”, highlighting that in comparison with the literature
on leader development, “the development of the capacity
of groups and organizations for leadership as a shared and
collective process – is far less well explored and researched”
(p 3)52 and urge that we begin to look in that direction.
Conclusion
There is a growing body of international evidence that when
clinicians are involved in strategic decision-making at an
organizational level, they are able to add their voices to enact
change, which is not only resource friendly but enhances
clinical and operational outcomes. Clinical leadership has
become the “high profile” conduit to enable this to occur.
According to Baker and Denis,107 three elements are
required to develop medical leadership in health care orga-
nizations: encouragement to formal leadership roles; the
promulgation of a collective understanding of organizational
leadership, occurring in a coordinated manner at all levels;
and aligning development of leadership with clear quality
and safety improvement goals at strategic and operational
levels in the organization. Gilbert et al22 state that when doc-
tors in training attend leadership training, they have greater
desire and perceived ability to contribute to improvement
in the NHS.
An express wish of the Medical Director of NHS England
has been that clinicians should routinely be shortlisted senior
positions in health care.24 While this is a laudable aim, this
may continue to perpetuate the historic model of command
and control and a target-driven approach, when we should be
striving for a model of “engaging leadership”.108 This model
is not about being an extraordinary individual but the empha-
sis shifts to “… teamwork, collaboration, connectedness and
removing barriers to communication and original thinking”.109
Leadership then becomes the “cognitive catalyst” (p 8)
and is based upon a shared vision and has to encompass
those on the front line.108 Perhaps, we can take a lesson from
organizations such as Intermountain Healthcare or Kaiser
Permanente in the USA, which invest in formal leadership
development backed up with quality improvement skills that
support this work. In essence, clinicians become involved in
daily management of their institutions alongside long-term
improvement work, translating into enhanced organizational
performance and outcomes.
Bohmer74 states, leadership is not only about the big “L”
(senior leadership roles in organizations), but is also the
very important “leading of the micro-systems that have such
an effect on care outcomes” (p 483). Leadership in high-
performing organizations is not reliant on a charismatic leader;
instead it is distributed in nature, where senior leaders define
strategy, support execution of strategic initiatives, and engage
individuals within the organization to lead on improvement
activities. Ensuring that clinical leadership development has
an equal weight within postgraduate training programs as
clinical skill development is, therefore, essential, if we are to
build health organizations with the capability for continual
improvement in order that they might better meet the future
needs of our patients and local populations.
Journal of Healthcare Leadership downloaded from https://www.dovepress.com/ by 193.93.195.147 on 25-Aug-2018
For personal use only.
Powered by TCPDF (www.tcpdf.org)

Journal of Healthcare Leadership 2015:7submit your manuscript | www.dovepress.com
Dovepress
Dovepress
120
Aggarwal and Swanwick
Acknowledgment
Thanks to Genevieve Holt for discussions regarding leader-
ship development for junior doctors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. The World Bank. Available from: http://data.worldbank.org/indicator/
SH.XPD.TOTL.ZS. Accessed April 8, 2015.
2. Jonas S, McCay L, Keogh B. The importance of clinical leadership.
In: Swanwick T, McKimm J, editors. The ABC of Clinical Leadership.
Chichester, UK: Wiley-Blackwell, BMJ Books; 2011:1–7.
3. Davis K, Stremikis K, Squires D, et al. Mirror, Mirror on the Wall, 2014
Update: How the US Health Care System Compares Internationally.
New York, NY: The Commonwealth Fund; 2014. Available from:
http://www.commonwealthfund.org/publications/fund-reports/2014/
jun/mirror-mirror. Accessed April 9, 2015.
4. Francis R. Mid staffordshire NHS foundation trust public enquiry;
2013. Available from: http://www.midstaffspublicinquiry.com/report.
Accessed April 9, 2015.
5. Mountford J. Clinical leadership: bringing the strands together. In:
Stanton E, Lemer C, Mountford J, editors. Clinical Leadership, Bridging
the Divide. London, UK: Quay Books Division; 2010:159–166.
6. Dorgan S, Layton D, Bloom N, et al. Management in Healthcare: Why
Good Practice Really Matters. London, UK: Centre for Economic
Performance, LSE; 2010.
7. Mintzberg H. The Structuring of Organisations: A Synthesis of
Research. Englewood Cliffs, NJ: Prentice Hall; 1979.
8. Ham C. Improving the performance of health services: the role of
clinical leadership; 2003. Available from: http://image.thelancet.com/
extras/02art8342web.pdf. Accessed January 26, 2015.
9. Edmonstone J. Clinical leadership: the elephant in the room. Int J Health
Plann Manage. 2009;24(4):290–305.
10. Ham C, Dickenson H. Engaging Doctors in Leadership: What We
Can Learn from International Experience and Research Evidence?
Coventry, UK: NHS Institute for Innovation and Improvement;
2008.
11. Borman E, O’Grady P. Postgraduate training. Policy paper prepared
by the subcommittee on postgraduate training: Permanent Work-
ing Group of European Junior Hospital Doctors. Med Educ. 1997;
31:3–8.
12. Greenaway D. Shape of training: securing the future of excellent
patient care. Final report of the independent review led by Profes-
sor David Greenaway. General Medical Council; 2013. Available
from: http://www.shapeoftraining.co.uk/static/documents/content/
Shape_of_training_FINAL_Report.pdf_53977887.pdf. Accessed
August 6, 2015.
13. Department of Health, Hospital doctors: training for the future. The
Report of the Working Group on Specialist Medical Training. London,
UK: Stationery Office; 1993.
14. Department of Health. Modernising Medical Careers: The Response
of the Four UK Health Ministers to the Consultation on Unfinished
Business: Proposals for Reform of the Senior House Officer Grade.
London, UK: Stationery Office; 2003.
15. Madden GB, Madden AP. Has Modernising Medical Careers lost its
way? Br Med J. 2007;335:426.
16. Fletcher G, Flin R, McGeorge P, et al. Anaesthetists’ non-technical
skills (ANTS): evaluation of a behavioural marker system. Br J Anaesth.
2003;90:580–588.
17. University of Aberdeen. Anaesthetic non-technical skills (ANTS)
system handbook; 2003. Available from: http://www.abdn.ac.uk/iprc/
documents/ants/ants_handbook_v1.0_electronic_access_version.pdf.
Accessed April 8, 2015.
18. NHS England, Public Health England, Health Education England, Moni-
tor, Care Quality Commission, NHS Trust Development Authority. Five
Year Forward View; 2014. Available from: http://www.england.nhs.uk/
wp-content/uploads/2014/10/5yfv-web.pdf. Accessed April 8, 2015.
19. Swanwick T. Junior doctors: the best kept secret in the NHS? Postgrad
Med J. 2011;88:1037.
20. Swanwick T. Postgraduate medical education: the same, but different.
Postgrad Med J. 2015;91(1074):179–181.
21. Tooke J. Aspiring to Excellence: Final Report of The Independent
Inquiry into Modernising Medical Careers. London, UK: MMC Inquiry;
2008. Available from: http://www.medschools.ac.uk/AboutUs/Projects/
Documents/Final%20MMC%20Inquiry%20Jan2008.pdf. Accessed
July 13, 2015.
22. Gilbert A, Hockey P, Vaithianathan R, et al. Perceptions of junior doc-
tors in the NHS about their training: results of a regional questionnaire.
BMJ Qual Saf. 2012;21:234–238. doi: 10.1136/bmjqs-2011-000611.
23. Roueche A, Hewitt J. ‘Wading through treacle’: quality improvement
lessons from the frontline. BMJ Qual Saf. 2012;21:179–183.
24. Malby R, Edmonstone J, Ross D, et al. Clinical leadership: the challenge
of making the most of doctors in management. Br J Hosp Manage.
2011;72(6):341–345.
25. Penlington C, Marshall P. Why Junior Doctors are Innovation Leaders
[homepage on the internet]. London, UK: Health Services Journal; 2013.
Available from: http://www.hsj.co.uk/leadership/why-junior-doctors-
are-innovation-leaders/5060206.article#.VT-QIUttfoA. Accessed
April 30, 2015.
26. Brook R, Medical leadership in an increasingly complex world. JAMA.
2010;304(4):465–466.
27. Grey C. ‘We are all managers now’; ‘We always were’: ‘on the devel-
opment and demise of management’. J Manage Stud. 1999;36(5):
561–585.
28. Griffiths D, Sheehan C, Debar S, et al. Clinical leadership – the what,
why and how. In: Stanton E, Lemer C, Mountford J, editors. Clinical
Leadership: Bridging the Divide. London, UK: Quay Books; 2010:
1–14.
29. O’Reilly D, Reed M. ‘Leadersism’: an evolution of managerialism in
UK public sector reform. Publ Admin. 2011;88(4):960–978.
30. Wallace M, Tomlinson M, O’Reilly D. The mediation of acculturation:
orchestrating school leadership development in England. Educ Manage
Admin Leader. 2011;39(3):261–282.
31. Thorpe R, Gold, G. 2010. Leadership and management development:
the current state. In: Gold G, Thorpe R, Mumford A, editors. The
Gower Handbook of Leadership and Management Development. 5th ed.
Farnham, UK: Gower; 2010;3–22.
32. Martin GP, Learmouth M. A critical account of the rise and spread
of ‘leadership’: the case of UK healthcare. Soc Sci Med. 2012;74:
281–288.
33. Head B, Alford J. Wicked problems: implications for public
policy and management. Admin Soc. 2015;47(6):711–739. doi:
10.1177/0095399713481601.
34. Kotter JP. Leading Change. Boston, MA: Harvard Business School
Press; 1996.
35. Swanwick T, McKimm J. What is clinical leadership … and why is it
important? Clin Teach. 2011;8:22–26.
36. King’s Fund. The Future of Leadership and Management in the NHS: No
More Heroes. London. UK: King’s Fund; 2011. Available from: http://
www.kingsfund.org.uk/sites/files/kf/future-of-leadership-and-manage-
ment-nhs-may-2011-kings-fund.pdf. Accessed January 30, 2015.
37. Willcocks S. Doctors and leadership in the UK National Health Service.
Clin Manage. 2005;13:11–21.
38. Judge TA, Bobo JE, Ilies R, et al. Personality and leadership: a qualita-
tive and quantitative review. J Appl Psychol. 2002;87(4):765–780.
39. Earley P, Weindling D. Understanding School Leadership. Thousand
Oaks, CA: Sage Publications; 2004.
40. Tannenbaum R, Schmidt W. How to choose a leadership pattern: should
a leader be democratic or autocratic or something in between? Harv
Bus Rev. 1958;36:95–101.
Journal of Healthcare Leadership downloaded from https://www.dovepress.com/ by 193.93.195.147 on 25-Aug-2018
For personal use only.
Powered by TCPDF (www.tcpdf.org)
Dovepress
Dovepress
120
Aggarwal and Swanwick
Acknowledgment
Thanks to Genevieve Holt for discussions regarding leader-
ship development for junior doctors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. The World Bank. Available from: http://data.worldbank.org/indicator/
SH.XPD.TOTL.ZS. Accessed April 8, 2015.
2. Jonas S, McCay L, Keogh B. The importance of clinical leadership.
In: Swanwick T, McKimm J, editors. The ABC of Clinical Leadership.
Chichester, UK: Wiley-Blackwell, BMJ Books; 2011:1–7.
3. Davis K, Stremikis K, Squires D, et al. Mirror, Mirror on the Wall, 2014
Update: How the US Health Care System Compares Internationally.
New York, NY: The Commonwealth Fund; 2014. Available from:
http://www.commonwealthfund.org/publications/fund-reports/2014/
jun/mirror-mirror. Accessed April 9, 2015.
4. Francis R. Mid staffordshire NHS foundation trust public enquiry;
2013. Available from: http://www.midstaffspublicinquiry.com/report.
Accessed April 9, 2015.
5. Mountford J. Clinical leadership: bringing the strands together. In:
Stanton E, Lemer C, Mountford J, editors. Clinical Leadership, Bridging
the Divide. London, UK: Quay Books Division; 2010:159–166.
6. Dorgan S, Layton D, Bloom N, et al. Management in Healthcare: Why
Good Practice Really Matters. London, UK: Centre for Economic
Performance, LSE; 2010.
7. Mintzberg H. The Structuring of Organisations: A Synthesis of
Research. Englewood Cliffs, NJ: Prentice Hall; 1979.
8. Ham C. Improving the performance of health services: the role of
clinical leadership; 2003. Available from: http://image.thelancet.com/
extras/02art8342web.pdf. Accessed January 26, 2015.
9. Edmonstone J. Clinical leadership: the elephant in the room. Int J Health
Plann Manage. 2009;24(4):290–305.
10. Ham C, Dickenson H. Engaging Doctors in Leadership: What We
Can Learn from International Experience and Research Evidence?
Coventry, UK: NHS Institute for Innovation and Improvement;
2008.
11. Borman E, O’Grady P. Postgraduate training. Policy paper prepared
by the subcommittee on postgraduate training: Permanent Work-
ing Group of European Junior Hospital Doctors. Med Educ. 1997;
31:3–8.
12. Greenaway D. Shape of training: securing the future of excellent
patient care. Final report of the independent review led by Profes-
sor David Greenaway. General Medical Council; 2013. Available
from: http://www.shapeoftraining.co.uk/static/documents/content/
Shape_of_training_FINAL_Report.pdf_53977887.pdf. Accessed
August 6, 2015.
13. Department of Health, Hospital doctors: training for the future. The
Report of the Working Group on Specialist Medical Training. London,
UK: Stationery Office; 1993.
14. Department of Health. Modernising Medical Careers: The Response
of the Four UK Health Ministers to the Consultation on Unfinished
Business: Proposals for Reform of the Senior House Officer Grade.
London, UK: Stationery Office; 2003.
15. Madden GB, Madden AP. Has Modernising Medical Careers lost its
way? Br Med J. 2007;335:426.
16. Fletcher G, Flin R, McGeorge P, et al. Anaesthetists’ non-technical
skills (ANTS): evaluation of a behavioural marker system. Br J Anaesth.
2003;90:580–588.
17. University of Aberdeen. Anaesthetic non-technical skills (ANTS)
system handbook; 2003. Available from: http://www.abdn.ac.uk/iprc/
documents/ants/ants_handbook_v1.0_electronic_access_version.pdf.
Accessed April 8, 2015.
18. NHS England, Public Health England, Health Education England, Moni-
tor, Care Quality Commission, NHS Trust Development Authority. Five
Year Forward View; 2014. Available from: http://www.england.nhs.uk/
wp-content/uploads/2014/10/5yfv-web.pdf. Accessed April 8, 2015.
19. Swanwick T. Junior doctors: the best kept secret in the NHS? Postgrad
Med J. 2011;88:1037.
20. Swanwick T. Postgraduate medical education: the same, but different.
Postgrad Med J. 2015;91(1074):179–181.
21. Tooke J. Aspiring to Excellence: Final Report of The Independent
Inquiry into Modernising Medical Careers. London, UK: MMC Inquiry;
2008. Available from: http://www.medschools.ac.uk/AboutUs/Projects/
Documents/Final%20MMC%20Inquiry%20Jan2008.pdf. Accessed
July 13, 2015.
22. Gilbert A, Hockey P, Vaithianathan R, et al. Perceptions of junior doc-
tors in the NHS about their training: results of a regional questionnaire.
BMJ Qual Saf. 2012;21:234–238. doi: 10.1136/bmjqs-2011-000611.
23. Roueche A, Hewitt J. ‘Wading through treacle’: quality improvement
lessons from the frontline. BMJ Qual Saf. 2012;21:179–183.
24. Malby R, Edmonstone J, Ross D, et al. Clinical leadership: the challenge
of making the most of doctors in management. Br J Hosp Manage.
2011;72(6):341–345.
25. Penlington C, Marshall P. Why Junior Doctors are Innovation Leaders
[homepage on the internet]. London, UK: Health Services Journal; 2013.
Available from: http://www.hsj.co.uk/leadership/why-junior-doctors-
are-innovation-leaders/5060206.article#.VT-QIUttfoA. Accessed
April 30, 2015.
26. Brook R, Medical leadership in an increasingly complex world. JAMA.
2010;304(4):465–466.
27. Grey C. ‘We are all managers now’; ‘We always were’: ‘on the devel-
opment and demise of management’. J Manage Stud. 1999;36(5):
561–585.
28. Griffiths D, Sheehan C, Debar S, et al. Clinical leadership – the what,
why and how. In: Stanton E, Lemer C, Mountford J, editors. Clinical
Leadership: Bridging the Divide. London, UK: Quay Books; 2010:
1–14.
29. O’Reilly D, Reed M. ‘Leadersism’: an evolution of managerialism in
UK public sector reform. Publ Admin. 2011;88(4):960–978.
30. Wallace M, Tomlinson M, O’Reilly D. The mediation of acculturation:
orchestrating school leadership development in England. Educ Manage
Admin Leader. 2011;39(3):261–282.
31. Thorpe R, Gold, G. 2010. Leadership and management development:
the current state. In: Gold G, Thorpe R, Mumford A, editors. The
Gower Handbook of Leadership and Management Development. 5th ed.
Farnham, UK: Gower; 2010;3–22.
32. Martin GP, Learmouth M. A critical account of the rise and spread
of ‘leadership’: the case of UK healthcare. Soc Sci Med. 2012;74:
281–288.
33. Head B, Alford J. Wicked problems: implications for public
policy and management. Admin Soc. 2015;47(6):711–739. doi:
10.1177/0095399713481601.
34. Kotter JP. Leading Change. Boston, MA: Harvard Business School
Press; 1996.
35. Swanwick T, McKimm J. What is clinical leadership … and why is it
important? Clin Teach. 2011;8:22–26.
36. King’s Fund. The Future of Leadership and Management in the NHS: No
More Heroes. London. UK: King’s Fund; 2011. Available from: http://
www.kingsfund.org.uk/sites/files/kf/future-of-leadership-and-manage-
ment-nhs-may-2011-kings-fund.pdf. Accessed January 30, 2015.
37. Willcocks S. Doctors and leadership in the UK National Health Service.
Clin Manage. 2005;13:11–21.
38. Judge TA, Bobo JE, Ilies R, et al. Personality and leadership: a qualita-
tive and quantitative review. J Appl Psychol. 2002;87(4):765–780.
39. Earley P, Weindling D. Understanding School Leadership. Thousand
Oaks, CA: Sage Publications; 2004.
40. Tannenbaum R, Schmidt W. How to choose a leadership pattern: should
a leader be democratic or autocratic or something in between? Harv
Bus Rev. 1958;36:95–101.
Journal of Healthcare Leadership downloaded from https://www.dovepress.com/ by 193.93.195.147 on 25-Aug-2018
For personal use only.
Powered by TCPDF (www.tcpdf.org)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 14
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.