Integrative Review: Mental Health Service Users' Experiences of Care
VerifiedAdded on 2022/09/07
|12
|10914
|81
Report
AI Summary
This integrative literature review, published in the Journal of Psychiatric and Mental Health Nursing, examines the experiences of mental health service users. The review, conducted by researchers at the University of Limerick, analyzed 34 studies published between 2008 and 2012, focusing on adults aged 18-65. The research explored service users' perspectives on accessing care, building relationships with providers, and the continuity of care within mental health services. Key themes emerged, including the importance of acknowledging mental health problems, fostering relationships, and ensuring continuity of care. The review highlights issues with stigma, poor communication, and the need for a shift in the provider-service user relationship to facilitate genuine engagement and empowerment, particularly in relation to the recovery model. The review emphasizes the critical role of relationships in mental health care and suggests implications for mental health nursing practices.
Mental health service users’ experiences of mental
health care: an integrative literature review
D . N E W M A N 1 M S c B Sc ( H o n s ) R P N,
P . O ’ R E I L LY 2 P h D M A ( Ed ) B Sc ( H o n s ) R G N R N I D ,
S . H . L E E3 P h D M P H E B Sc ( H o n s ) C e r t . E d . R N R M &
C . K E N N E D Y4 P h D B A ( H o n s ) D N R N T R N
1PhD Student,2Head of Department,3Post-Doctoral Research Fellow, and4Professor of Nursing and Midwifery,
Department of Nursing and Midwifery, University of Limerick, Limerick, Ireland
Keywords:communication, experience,
mental health, mental health service user
and relationships, service providers
Correspondence:
D. Newman
Department Nursing and Midwifery
University of Limerick
Health Science Building
Northbank Campus
Limerick
Ireland
E-mail: daniel.newman@ul.ie
Accepted for publication: 7 January
2015
doi: 10.1111/jpm.12202
Accessible summary
• A number of studies have highlighted issues around the relationship between
service users and providers. The recovery model is predominant in mental heal
as is the recognition of the importance of person-centred practice.The authors
completed an in-depth search of the literature to answer the question: What are
service users’ experiences of the mental health service?
• Three key themes emerged: acknowledging a mental health problem and seeki
help;building relationships through participation in care;and working towards
continuity of care.
• The review adds to the current body of knowledge by providing greater detail in
the importance of relationships between service users and providers and how th
may impact on the delivery of care in the mental health service. The overarchin
theme that emerged was the importance of the relationship between the servic
user and provider as a basis for interaction and support.
• This review has specific implications for mental health nursing. Despite the reco
nition made in policy documents for change, issues with stigma, poor attitudes
communication persist. There is a need for a fundamental shift in the provider–
service user relationship to facilitate true service-user engagement in their care
Abstract
The aim of this integrative literature review was to identify mentalhealth service
users’ experiences of services. The rationale for this review was based on the grow
emphasis and requirements for health services to deliver care and support,which
recognizes the preferences of individuals. Contemporary models of mental health c
strive to promote inclusion and empowerment.This review seeks to add to our
current understanding of how service users experience care and support in order t
determine to what extent the principles of contemporary models of mental health
are embedded in practice. A robust search of Web of Science, the Cochrane Datab
Science Direct, EBSCO host (Academic Search Complete, MEDLINE, CINAHL Plus
Full-Text),PsycINFO, PsycARTICLES, Social SciencesFull Text and the United
Kingdom and Ireland Reference Centre for data published between 1 January 2008
and 31 December 2012 was completed. The initial search retrieved 272 609 paper
The authors used a staged approach and the application of predetermined inclusio
exclusion criteria, thus the numbers of papers for inclusion were reduced to 34. Da
extraction, quality assessment and thematic analysis were completed for the inclu
Journal of Psychiatric and Mental Health Nursing, 2015, 22, 171–182
©2015 John Wiley & Sons Ltd 171
health care: an integrative literature review
D . N E W M A N 1 M S c B Sc ( H o n s ) R P N,
P . O ’ R E I L LY 2 P h D M A ( Ed ) B Sc ( H o n s ) R G N R N I D ,
S . H . L E E3 P h D M P H E B Sc ( H o n s ) C e r t . E d . R N R M &
C . K E N N E D Y4 P h D B A ( H o n s ) D N R N T R N
1PhD Student,2Head of Department,3Post-Doctoral Research Fellow, and4Professor of Nursing and Midwifery,
Department of Nursing and Midwifery, University of Limerick, Limerick, Ireland
Keywords:communication, experience,
mental health, mental health service user
and relationships, service providers
Correspondence:
D. Newman
Department Nursing and Midwifery
University of Limerick
Health Science Building
Northbank Campus
Limerick
Ireland
E-mail: daniel.newman@ul.ie
Accepted for publication: 7 January
2015
doi: 10.1111/jpm.12202
Accessible summary
• A number of studies have highlighted issues around the relationship between
service users and providers. The recovery model is predominant in mental heal
as is the recognition of the importance of person-centred practice.The authors
completed an in-depth search of the literature to answer the question: What are
service users’ experiences of the mental health service?
• Three key themes emerged: acknowledging a mental health problem and seeki
help;building relationships through participation in care;and working towards
continuity of care.
• The review adds to the current body of knowledge by providing greater detail in
the importance of relationships between service users and providers and how th
may impact on the delivery of care in the mental health service. The overarchin
theme that emerged was the importance of the relationship between the servic
user and provider as a basis for interaction and support.
• This review has specific implications for mental health nursing. Despite the reco
nition made in policy documents for change, issues with stigma, poor attitudes
communication persist. There is a need for a fundamental shift in the provider–
service user relationship to facilitate true service-user engagement in their care
Abstract
The aim of this integrative literature review was to identify mentalhealth service
users’ experiences of services. The rationale for this review was based on the grow
emphasis and requirements for health services to deliver care and support,which
recognizes the preferences of individuals. Contemporary models of mental health c
strive to promote inclusion and empowerment.This review seeks to add to our
current understanding of how service users experience care and support in order t
determine to what extent the principles of contemporary models of mental health
are embedded in practice. A robust search of Web of Science, the Cochrane Datab
Science Direct, EBSCO host (Academic Search Complete, MEDLINE, CINAHL Plus
Full-Text),PsycINFO, PsycARTICLES, Social SciencesFull Text and the United
Kingdom and Ireland Reference Centre for data published between 1 January 2008
and 31 December 2012 was completed. The initial search retrieved 272 609 paper
The authors used a staged approach and the application of predetermined inclusio
exclusion criteria, thus the numbers of papers for inclusion were reduced to 34. Da
extraction, quality assessment and thematic analysis were completed for the inclu
Journal of Psychiatric and Mental Health Nursing, 2015, 22, 171–182
©2015 John Wiley & Sons Ltd 171
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
studies. Satisfaction with the mental health service was moderately good. However
accessing services could be difficult because of a lack of knowledge and the stigma
surrounding mentalhealth.Large surveys document moderate satisfaction ratings;
however,feelings of fear regarding how services function and the lack of treatment
choice remain.The main finding from thisreview is while people may express
satisfaction with mentalhealth services,there are stillissuesaround three main
themes: acknowledging a mental health problem and seeking help; building relation
ship through participation and care;and working towards continuity of care.
Elements of the recovery model appear to be lacking in relation to user involvemen
empowerment and decision making.There is a need for a fundamentalshift in the
contextof the provider–service userrelationship to fully facilitate service users’
engagement in their care.
Introduction
A predominant focus in mental health policy and practice
over the last 20 years has been greater efforts to involve
people in their care planning.Historically,service users’
involvementin their mentalhealth serviceswas limited
(Campbell 2005, Dunne 2006). Understanding the views of
the service user remains essential in contemporary mental
health in order to identify the extent to which a service is
achieving its aims and purpose. The aim of this integrative
review wasto establish whatevidence existsas to the
experiences service users have of mental health services.
Legislationsprotecting service users’rights has been
introduced and implemented in the United Kingdom and
Ireland (Mental Health Act 2007, House of Parliament and
Mental Health Act 2001 Houses of the Oireachtas).
Furthermore, new models or approaches to care have been
advocated including the recovery modelwhich has been
promoted internationally [e.g. MHC (NZ) 1998;
Departmentof Health 2001;MHC (Ireland) 2008].The
main elements of the recovery modelare greater service-
user involvement,modernizing the mentalhealth work-
force, viewing the person beyond the illness,increased
personalization,facilitating choice of treatmentsand
changesto education programmes.The recovery model
seeks to invertthe role ofthe service user from being a
follower to one where they are able to lead,change and
direct their own care (Sainsbury Centre for Mental Health
2008). The prominence and importance of patient-centred
care,also identified by Epstein & Street (2011),aimed to
ensure service users’ needs and preferences are respected. A
key aim of patient-centred care is to help service users make
and contribute to, informed decisions about their care.
Research in the early 2000sidentified severalissues
around the relationship between service users and provid-
ers. For example,Dunne (2006)highlighted thatservice
userscontinued to experience poorcommunication and
lack of continuity of care.A preliminary literature search
did not identify a recent review that addressed experiences
acrossmentalhealth services.Therefore,as the debate
regarding theautonomy and rightsof serviceusersin
mentalhealth continues,it is timely to identify whatis
known aboutmentalhealth service users’experiences of
mental health services.
Aim and methods of the review
The aim of this integrative literature review was to identify
how service users experiencemental health services.
Mental health service users are not a homogeneous group
with similar experiences,so the focus ofthis integrative
review was the experiences of adults (18–65 years old) who
accessed and used a mental health service. Reports relating
to specialist services such as homeless services, the utiliza-
tion of mental health laws, detention or involuntary admis-
sion, clinical treatments or reports that outline changes in
work practices in specific areas were excluded as outlined
fully in Table 1. The focus of this review was on database
searchesin order to extract evidencefrom systematic
reviews and primary empirical qualitative and quantitative
studies (Table 1).
An integrative review was undertaken to address the aim
of the review. This approach is increasingly recognized as
appropriate to inform evidence-based practice.The inte-
grative review synthesize findings from a diverse range of
primary experimentaland non-experimentalresearch
methods in order to provide a breadth of perspectives and
a more comprehensive understanding of a healthcare issue
(Whittemore & Knafl 2005). Given the aim was to evaluate
services users’ experiences, an integrative review was con-
sidered to be the appropriatemethod.The approach
reported here reflects key aspects of the systematic review
methodsadvocated by the Cochrane Collaboration and
the Scottish IntercollegiateGuideline Network (SIGN
D Newman et al.
172 ©2015 John Wiley & Sons Ltd
accessing services could be difficult because of a lack of knowledge and the stigma
surrounding mentalhealth.Large surveys document moderate satisfaction ratings;
however,feelings of fear regarding how services function and the lack of treatment
choice remain.The main finding from thisreview is while people may express
satisfaction with mentalhealth services,there are stillissuesaround three main
themes: acknowledging a mental health problem and seeking help; building relation
ship through participation and care;and working towards continuity of care.
Elements of the recovery model appear to be lacking in relation to user involvemen
empowerment and decision making.There is a need for a fundamentalshift in the
contextof the provider–service userrelationship to fully facilitate service users’
engagement in their care.
Introduction
A predominant focus in mental health policy and practice
over the last 20 years has been greater efforts to involve
people in their care planning.Historically,service users’
involvementin their mentalhealth serviceswas limited
(Campbell 2005, Dunne 2006). Understanding the views of
the service user remains essential in contemporary mental
health in order to identify the extent to which a service is
achieving its aims and purpose. The aim of this integrative
review wasto establish whatevidence existsas to the
experiences service users have of mental health services.
Legislationsprotecting service users’rights has been
introduced and implemented in the United Kingdom and
Ireland (Mental Health Act 2007, House of Parliament and
Mental Health Act 2001 Houses of the Oireachtas).
Furthermore, new models or approaches to care have been
advocated including the recovery modelwhich has been
promoted internationally [e.g. MHC (NZ) 1998;
Departmentof Health 2001;MHC (Ireland) 2008].The
main elements of the recovery modelare greater service-
user involvement,modernizing the mentalhealth work-
force, viewing the person beyond the illness,increased
personalization,facilitating choice of treatmentsand
changesto education programmes.The recovery model
seeks to invertthe role ofthe service user from being a
follower to one where they are able to lead,change and
direct their own care (Sainsbury Centre for Mental Health
2008). The prominence and importance of patient-centred
care,also identified by Epstein & Street (2011),aimed to
ensure service users’ needs and preferences are respected. A
key aim of patient-centred care is to help service users make
and contribute to, informed decisions about their care.
Research in the early 2000sidentified severalissues
around the relationship between service users and provid-
ers. For example,Dunne (2006)highlighted thatservice
userscontinued to experience poorcommunication and
lack of continuity of care.A preliminary literature search
did not identify a recent review that addressed experiences
acrossmentalhealth services.Therefore,as the debate
regarding theautonomy and rightsof serviceusersin
mentalhealth continues,it is timely to identify whatis
known aboutmentalhealth service users’experiences of
mental health services.
Aim and methods of the review
The aim of this integrative literature review was to identify
how service users experiencemental health services.
Mental health service users are not a homogeneous group
with similar experiences,so the focus ofthis integrative
review was the experiences of adults (18–65 years old) who
accessed and used a mental health service. Reports relating
to specialist services such as homeless services, the utiliza-
tion of mental health laws, detention or involuntary admis-
sion, clinical treatments or reports that outline changes in
work practices in specific areas were excluded as outlined
fully in Table 1. The focus of this review was on database
searchesin order to extract evidencefrom systematic
reviews and primary empirical qualitative and quantitative
studies (Table 1).
An integrative review was undertaken to address the aim
of the review. This approach is increasingly recognized as
appropriate to inform evidence-based practice.The inte-
grative review synthesize findings from a diverse range of
primary experimentaland non-experimentalresearch
methods in order to provide a breadth of perspectives and
a more comprehensive understanding of a healthcare issue
(Whittemore & Knafl 2005). Given the aim was to evaluate
services users’ experiences, an integrative review was con-
sidered to be the appropriatemethod.The approach
reported here reflects key aspects of the systematic review
methodsadvocated by the Cochrane Collaboration and
the Scottish IntercollegiateGuideline Network (SIGN
D Newman et al.
172 ©2015 John Wiley & Sons Ltd
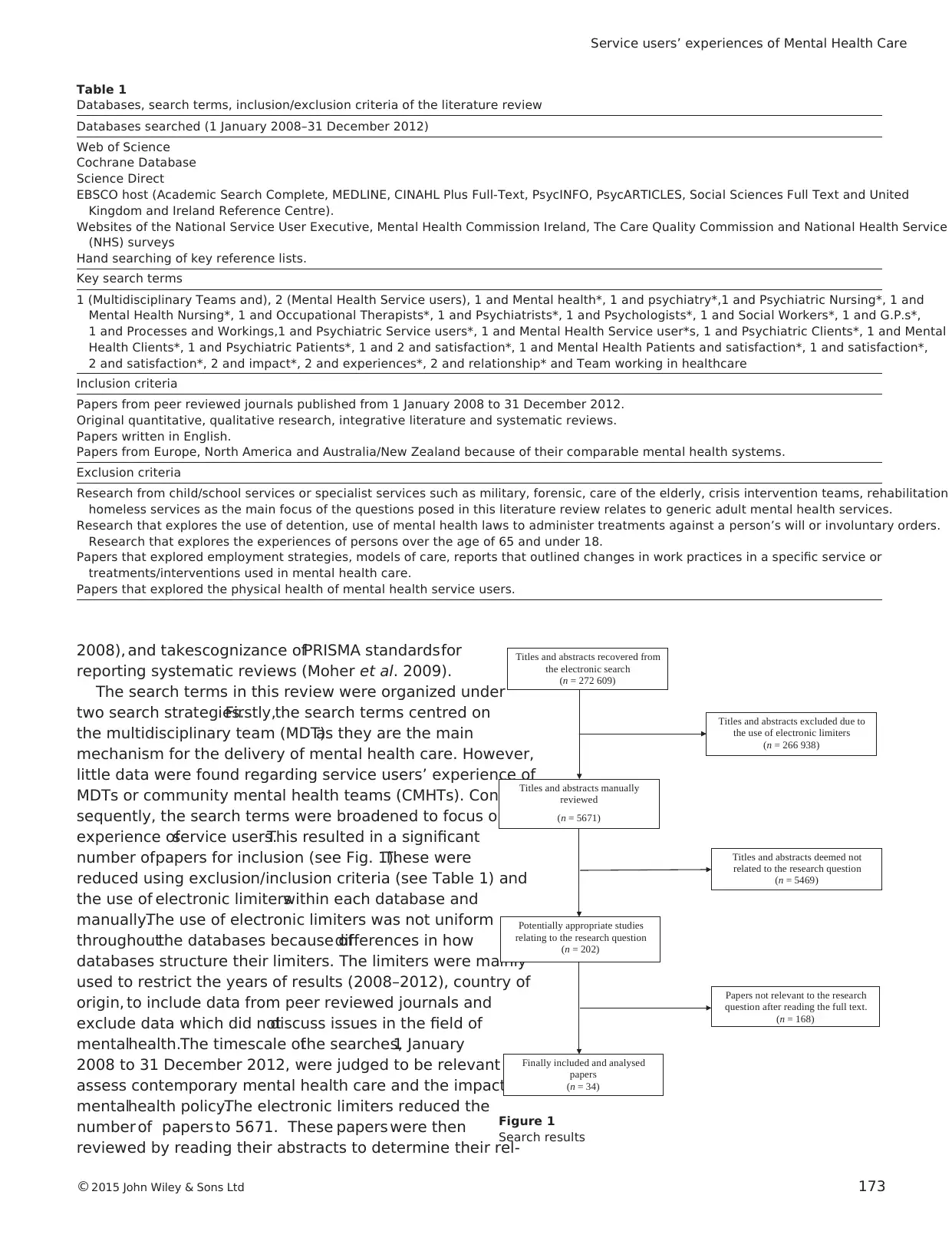
2008), and takescognizance ofPRISMA standardsfor
reporting systematic reviews (Moher et al. 2009).
The search terms in this review were organized under
two search strategies.Firstly,the search terms centred on
the multidisciplinary team (MDT)as they are the main
mechanism for the delivery of mental health care. However,
little data were found regarding service users’ experience of
MDTs or community mental health teams (CMHTs). Con-
sequently, the search terms were broadened to focus on the
experience ofservice users.This resulted in a significant
number ofpapers for inclusion (see Fig. 1).These were
reduced using exclusion/inclusion criteria (see Table 1) and
the use of electronic limiterswithin each database and
manually.The use of electronic limiters was not uniform
throughoutthe databases because ofdifferences in how
databases structure their limiters. The limiters were mainly
used to restrict the years of results (2008–2012), country of
origin, to include data from peer reviewed journals and
exclude data which did notdiscuss issues in the field of
mentalhealth.The timescale ofthe searches,1 January
2008 to 31 December 2012, were judged to be relevant to
assess contemporary mental health care and the impact of
mentalhealth policy.The electronic limiters reduced the
number of papers to 5671. These papers were then
reviewed by reading their abstracts to determine their rel-
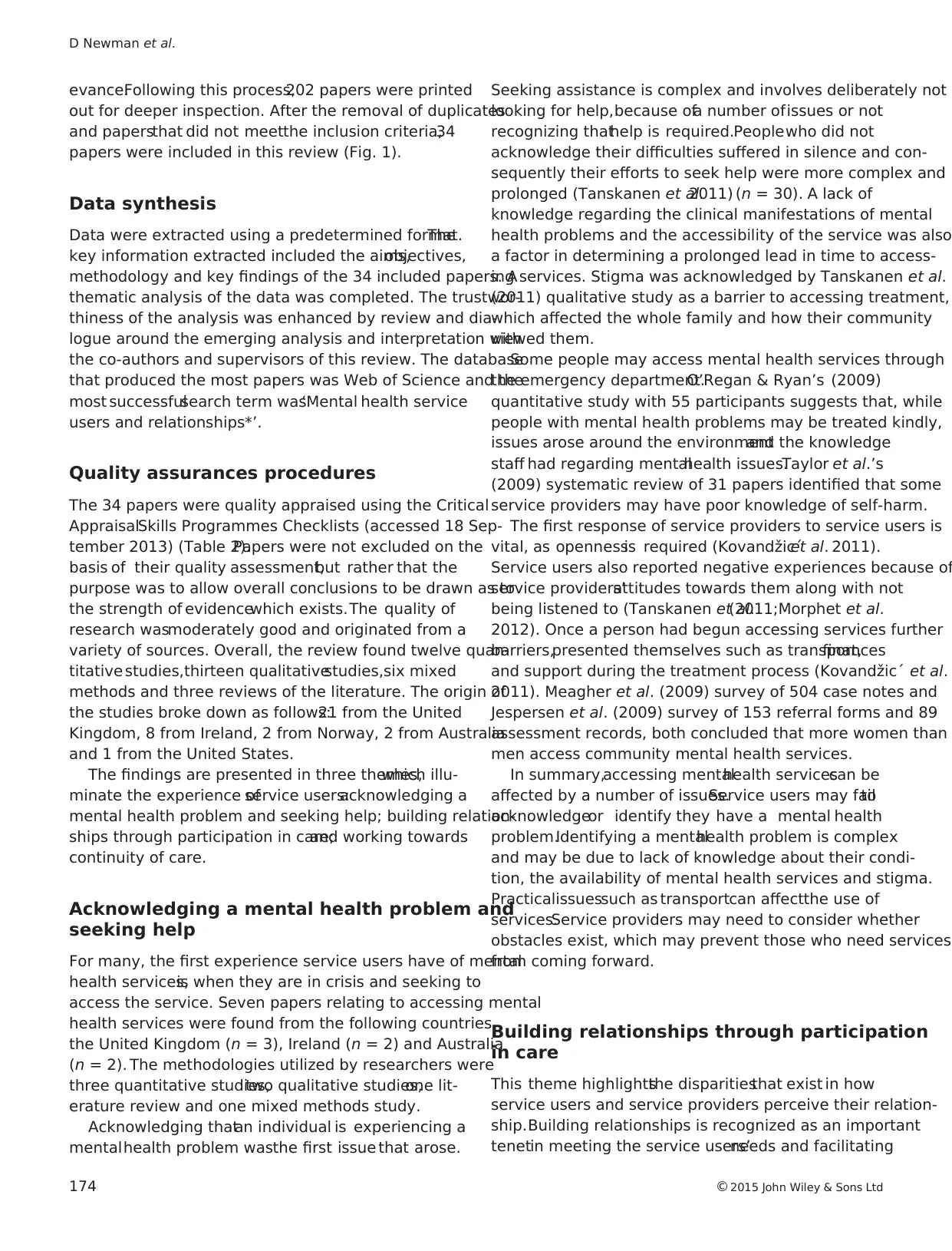
Table 1
Databases, search terms, inclusion/exclusion criteria of the literature review
Databases searched (1 January 2008–31 December 2012)
Web of Science
Cochrane Database
Science Direct
EBSCO host (Academic Search Complete, MEDLINE, CINAHL Plus Full-Text, PsycINFO, PsycARTICLES, Social Sciences Full Text and United
Kingdom and Ireland Reference Centre).
Websites of the National Service User Executive, Mental Health Commission Ireland, The Care Quality Commission and National Health Service
(NHS) surveys
Hand searching of key reference lists.
Key search terms
1 (Multidisciplinary Teams and), 2 (Mental Health Service users), 1 and Mental health*, 1 and psychiatry*,1 and Psychiatric Nursing*, 1 and
Mental Health Nursing*, 1 and Occupational Therapists*, 1 and Psychiatrists*, 1 and Psychologists*, 1 and Social Workers*, 1 and G.P.s*,
1 and Processes and Workings,1 and Psychiatric Service users*, 1 and Mental Health Service user*s, 1 and Psychiatric Clients*, 1 and Mental
Health Clients*, 1 and Psychiatric Patients*, 1 and 2 and satisfaction*, 1 and Mental Health Patients and satisfaction*, 1 and satisfaction*,
2 and satisfaction*, 2 and impact*, 2 and experiences*, 2 and relationship* and Team working in healthcare
Inclusion criteria
Papers from peer reviewed journals published from 1 January 2008 to 31 December 2012.
Original quantitative, qualitative research, integrative literature and systematic reviews.
Papers written in English.
Papers from Europe, North America and Australia/New Zealand because of their comparable mental health systems.
Exclusion criteria
Research from child/school services or specialist services such as military, forensic, care of the elderly, crisis intervention teams, rehabilitation
homeless services as the main focus of the questions posed in this literature review relates to generic adult mental health services.
Research that explores the use of detention, use of mental health laws to administer treatments against a person’s will or involuntary orders.
Research that explores the experiences of persons over the age of 65 and under 18.
Papers that explored employment strategies, models of care, reports that outlined changes in work practices in a specific service or
treatments/interventions used in mental health care.
Papers that explored the physical health of mental health service users.
Titles and abstracts recovered from
the electronic search
(n = 272 609)
Titles and abstracts excluded due to
the use of electronic limiters
(n = 266 938)
Titles and abstracts manually
reviewed
(n = 5671)
Titles and abstracts deemed not
related to the research question
(n = 5469)
Potentially appropriate studies
relating to the research question
(n = 202)
Papers not relevant to the research
question after reading the full text.
(n = 168)
Finally included and analysed
papers
(n = 34)
Figure 1
Search results
Service users’ experiences of Mental Health Care
©2015 John Wiley & Sons Ltd 173
reporting systematic reviews (Moher et al. 2009).
The search terms in this review were organized under
two search strategies.Firstly,the search terms centred on
the multidisciplinary team (MDT)as they are the main
mechanism for the delivery of mental health care. However,
little data were found regarding service users’ experience of
MDTs or community mental health teams (CMHTs). Con-
sequently, the search terms were broadened to focus on the
experience ofservice users.This resulted in a significant
number ofpapers for inclusion (see Fig. 1).These were
reduced using exclusion/inclusion criteria (see Table 1) and
the use of electronic limiterswithin each database and
manually.The use of electronic limiters was not uniform
throughoutthe databases because ofdifferences in how
databases structure their limiters. The limiters were mainly
used to restrict the years of results (2008–2012), country of
origin, to include data from peer reviewed journals and
exclude data which did notdiscuss issues in the field of
mentalhealth.The timescale ofthe searches,1 January
2008 to 31 December 2012, were judged to be relevant to
assess contemporary mental health care and the impact of
mentalhealth policy.The electronic limiters reduced the
number of papers to 5671. These papers were then
reviewed by reading their abstracts to determine their rel-
Table 1
Databases, search terms, inclusion/exclusion criteria of the literature review
Databases searched (1 January 2008–31 December 2012)
Web of Science
Cochrane Database
Science Direct
EBSCO host (Academic Search Complete, MEDLINE, CINAHL Plus Full-Text, PsycINFO, PsycARTICLES, Social Sciences Full Text and United
Kingdom and Ireland Reference Centre).
Websites of the National Service User Executive, Mental Health Commission Ireland, The Care Quality Commission and National Health Service
(NHS) surveys
Hand searching of key reference lists.
Key search terms
1 (Multidisciplinary Teams and), 2 (Mental Health Service users), 1 and Mental health*, 1 and psychiatry*,1 and Psychiatric Nursing*, 1 and
Mental Health Nursing*, 1 and Occupational Therapists*, 1 and Psychiatrists*, 1 and Psychologists*, 1 and Social Workers*, 1 and G.P.s*,
1 and Processes and Workings,1 and Psychiatric Service users*, 1 and Mental Health Service user*s, 1 and Psychiatric Clients*, 1 and Mental
Health Clients*, 1 and Psychiatric Patients*, 1 and 2 and satisfaction*, 1 and Mental Health Patients and satisfaction*, 1 and satisfaction*,
2 and satisfaction*, 2 and impact*, 2 and experiences*, 2 and relationship* and Team working in healthcare
Inclusion criteria
Papers from peer reviewed journals published from 1 January 2008 to 31 December 2012.
Original quantitative, qualitative research, integrative literature and systematic reviews.
Papers written in English.
Papers from Europe, North America and Australia/New Zealand because of their comparable mental health systems.
Exclusion criteria
Research from child/school services or specialist services such as military, forensic, care of the elderly, crisis intervention teams, rehabilitation
homeless services as the main focus of the questions posed in this literature review relates to generic adult mental health services.
Research that explores the use of detention, use of mental health laws to administer treatments against a person’s will or involuntary orders.
Research that explores the experiences of persons over the age of 65 and under 18.
Papers that explored employment strategies, models of care, reports that outlined changes in work practices in a specific service or
treatments/interventions used in mental health care.
Papers that explored the physical health of mental health service users.
Titles and abstracts recovered from
the electronic search
(n = 272 609)
Titles and abstracts excluded due to
the use of electronic limiters
(n = 266 938)
Titles and abstracts manually
reviewed
(n = 5671)
Titles and abstracts deemed not
related to the research question
(n = 5469)
Potentially appropriate studies
relating to the research question
(n = 202)
Papers not relevant to the research
question after reading the full text.
(n = 168)
Finally included and analysed
papers
(n = 34)
Figure 1
Search results
Service users’ experiences of Mental Health Care
©2015 John Wiley & Sons Ltd 173
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
evance.Following this process,202 papers were printed
out for deeper inspection. After the removal of duplicates
and papersthat did not meetthe inclusion criteria,34
papers were included in this review (Fig. 1).
Data synthesis
Data were extracted using a predetermined format.The
key information extracted included the aims,objectives,
methodology and key findings of the 34 included papers. A
thematic analysis of the data was completed. The trustwor-
thiness of the analysis was enhanced by review and dia-
logue around the emerging analysis and interpretation with
the co-authors and supervisors of this review. The database
that produced the most papers was Web of Science and the
most successfulsearch term was‘Mental health service
users and relationships*’.
Quality assurances procedures
The 34 papers were quality appraised using the Critical
AppraisalSkills Programmes Checklists (accessed 18 Sep-
tember 2013) (Table 2).Papers were not excluded on the
basis of their quality assessment,but rather that the
purpose was to allow overall conclusions to be drawn as to
the strength of evidencewhich exists.The quality of
research wasmoderately good and originated from a
variety of sources. Overall, the review found twelve quan-
titative studies,thirteen qualitativestudies,six mixed
methods and three reviews of the literature. The origin of
the studies broke down as follows:21 from the United
Kingdom, 8 from Ireland, 2 from Norway, 2 from Australia
and 1 from the United States.
The findings are presented in three themes,which illu-
minate the experience ofservice users:acknowledging a
mental health problem and seeking help; building relation-
ships through participation in care;and working towards
continuity of care.
Acknowledging a mental health problem and
seeking help
For many, the first experience service users have of mental
health services,is when they are in crisis and seeking to
access the service. Seven papers relating to accessing mental
health services were found from the following countries,
the United Kingdom (n = 3), Ireland (n = 2) and Australia
(n = 2). The methodologies utilized by researchers were
three quantitative studies,two qualitative studies,one lit-
erature review and one mixed methods study.
Acknowledging thatan individual is experiencing a
mentalhealth problem wasthe first issue that arose.
Seeking assistance is complex and involves deliberately not
looking for help,because ofa number ofissues or not
recognizing thathelp is required.Peoplewho did not
acknowledge their difficulties suffered in silence and con-
sequently their efforts to seek help were more complex and
prolonged (Tanskanen et al.2011) (n = 30). A lack of
knowledge regarding the clinical manifestations of mental
health problems and the accessibility of the service was also
a factor in determining a prolonged lead in time to access-
ing services. Stigma was acknowledged by Tanskanen et al.
(2011) qualitative study as a barrier to accessing treatment,
which affected the whole family and how their community
viewed them.
Some people may access mental health services through
the emergency department.O’Regan & Ryan’s (2009)
quantitative study with 55 participants suggests that, while
people with mental health problems may be treated kindly,
issues arose around the environmentand the knowledge
staff had regarding mentalhealth issues.Taylor et al.’s
(2009) systematic review of 31 papers identified that some
service providers may have poor knowledge of self-harm.
The first response of service providers to service users is
vital, as opennessis required (Kovandžic´et al. 2011).
Service users also reported negative experiences because of
service providers’attitudes towards them along with not
being listened to (Tanskanen et al.(2011;Morphet et al.
2012). Once a person had begun accessing services further
barriers,presented themselves such as transport,finances
and support during the treatment process (Kovandžic´ et al.
2011). Meagher et al. (2009) survey of 504 case notes and
Jespersen et al. (2009) survey of 153 referral forms and 89
assessment records, both concluded that more women than
men access community mental health services.
In summary,accessing mentalhealth servicescan be
affected by a number of issues.Service users may failto
acknowledgeor identify they have a mental health
problem.Identifying a mentalhealth problem is complex
and may be due to lack of knowledge about their condi-
tion, the availability of mental health services and stigma.
Practicalissuessuch as transportcan affectthe use of
services.Service providers may need to consider whether
obstacles exist, which may prevent those who need services
from coming forward.
Building relationships through participation
in care
This theme highlightsthe disparitiesthat exist in how
service users and service providers perceive their relation-
ship.Building relationships is recognized as an important
tenetin meeting the service users’needs and facilitating
D Newman et al.
174 ©2015 John Wiley & Sons Ltd
out for deeper inspection. After the removal of duplicates
and papersthat did not meetthe inclusion criteria,34
papers were included in this review (Fig. 1).
Data synthesis
Data were extracted using a predetermined format.The
key information extracted included the aims,objectives,
methodology and key findings of the 34 included papers. A
thematic analysis of the data was completed. The trustwor-
thiness of the analysis was enhanced by review and dia-
logue around the emerging analysis and interpretation with
the co-authors and supervisors of this review. The database
that produced the most papers was Web of Science and the
most successfulsearch term was‘Mental health service
users and relationships*’.
Quality assurances procedures
The 34 papers were quality appraised using the Critical
AppraisalSkills Programmes Checklists (accessed 18 Sep-
tember 2013) (Table 2).Papers were not excluded on the
basis of their quality assessment,but rather that the
purpose was to allow overall conclusions to be drawn as to
the strength of evidencewhich exists.The quality of
research wasmoderately good and originated from a
variety of sources. Overall, the review found twelve quan-
titative studies,thirteen qualitativestudies,six mixed
methods and three reviews of the literature. The origin of
the studies broke down as follows:21 from the United
Kingdom, 8 from Ireland, 2 from Norway, 2 from Australia
and 1 from the United States.
The findings are presented in three themes,which illu-
minate the experience ofservice users:acknowledging a
mental health problem and seeking help; building relation-
ships through participation in care;and working towards
continuity of care.
Acknowledging a mental health problem and
seeking help
For many, the first experience service users have of mental
health services,is when they are in crisis and seeking to
access the service. Seven papers relating to accessing mental
health services were found from the following countries,
the United Kingdom (n = 3), Ireland (n = 2) and Australia
(n = 2). The methodologies utilized by researchers were
three quantitative studies,two qualitative studies,one lit-
erature review and one mixed methods study.
Acknowledging thatan individual is experiencing a
mentalhealth problem wasthe first issue that arose.
Seeking assistance is complex and involves deliberately not
looking for help,because ofa number ofissues or not
recognizing thathelp is required.Peoplewho did not
acknowledge their difficulties suffered in silence and con-
sequently their efforts to seek help were more complex and
prolonged (Tanskanen et al.2011) (n = 30). A lack of
knowledge regarding the clinical manifestations of mental
health problems and the accessibility of the service was also
a factor in determining a prolonged lead in time to access-
ing services. Stigma was acknowledged by Tanskanen et al.
(2011) qualitative study as a barrier to accessing treatment,
which affected the whole family and how their community
viewed them.
Some people may access mental health services through
the emergency department.O’Regan & Ryan’s (2009)
quantitative study with 55 participants suggests that, while
people with mental health problems may be treated kindly,
issues arose around the environmentand the knowledge
staff had regarding mentalhealth issues.Taylor et al.’s
(2009) systematic review of 31 papers identified that some
service providers may have poor knowledge of self-harm.
The first response of service providers to service users is
vital, as opennessis required (Kovandžic´et al. 2011).
Service users also reported negative experiences because of
service providers’attitudes towards them along with not
being listened to (Tanskanen et al.(2011;Morphet et al.
2012). Once a person had begun accessing services further
barriers,presented themselves such as transport,finances
and support during the treatment process (Kovandžic´ et al.
2011). Meagher et al. (2009) survey of 504 case notes and
Jespersen et al. (2009) survey of 153 referral forms and 89
assessment records, both concluded that more women than
men access community mental health services.
In summary,accessing mentalhealth servicescan be
affected by a number of issues.Service users may failto
acknowledgeor identify they have a mental health
problem.Identifying a mentalhealth problem is complex
and may be due to lack of knowledge about their condi-
tion, the availability of mental health services and stigma.
Practicalissuessuch as transportcan affectthe use of
services.Service providers may need to consider whether
obstacles exist, which may prevent those who need services
from coming forward.
Building relationships through participation
in care
This theme highlightsthe disparitiesthat exist in how
service users and service providers perceive their relation-
ship.Building relationships is recognized as an important
tenetin meeting the service users’needs and facilitating
D Newman et al.
174 ©2015 John Wiley & Sons Ltd
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
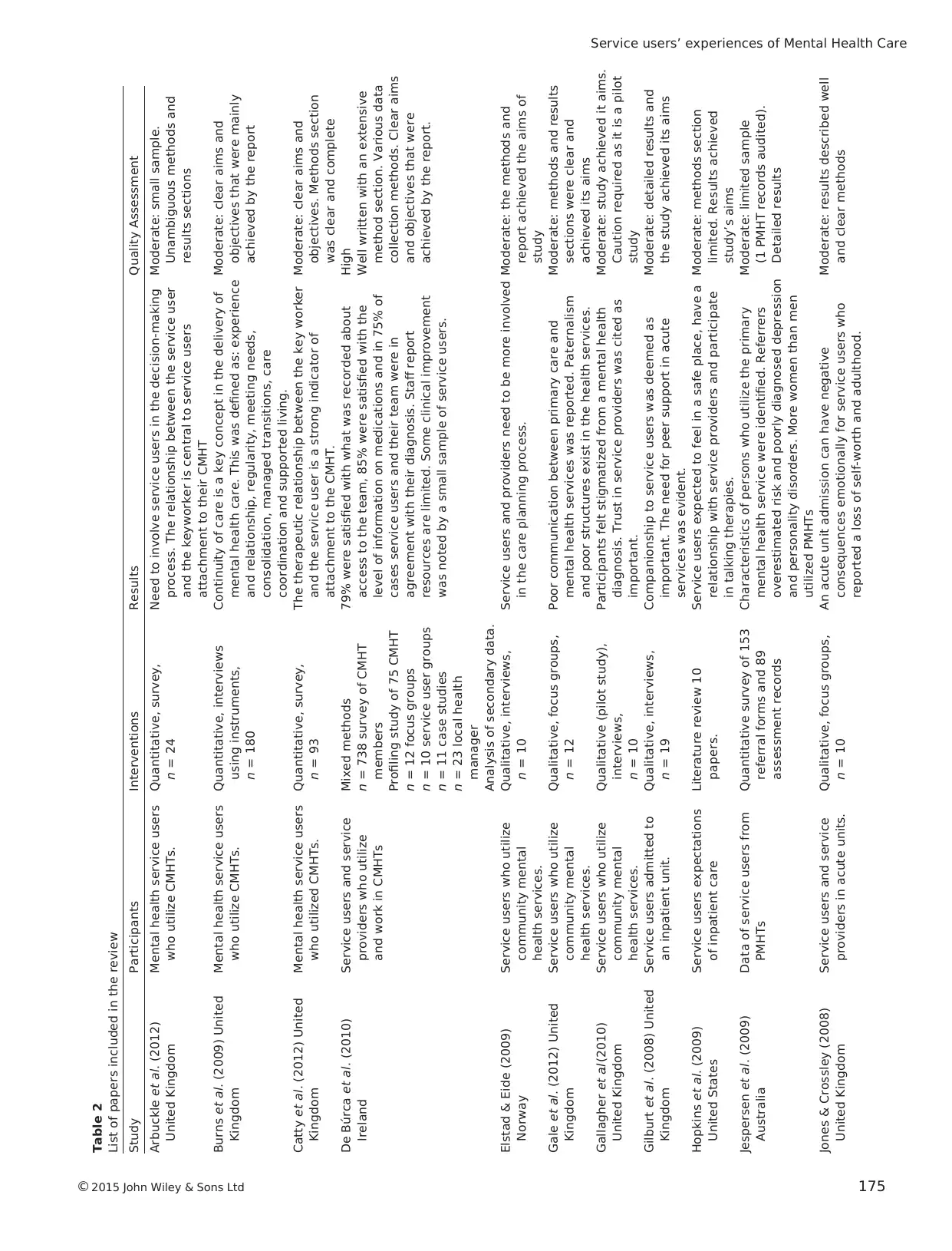
Table 2
List of papers included in the review
Study Participants Interventions Results Quality Assessment
Arbuckle et al. (2012)
United Kingdom
Mental health service users
who utilize CMHTs.
Quantitative, survey,
n = 24
Need to involve service users in the decision-making
process. The relationship between the service user
and the keyworker is central to service users
attachment to their CMHT
Moderate: small sample.
Unambiguous methods and
results sections
Burns et al. (2009) United
Kingdom
Mental health service users
who utilize CMHTs.
Quantitative, interviews
using instruments,
n = 180
Continuity of care is a key concept in the delivery of
mental health care. This was defined as: experience
and relationship, regularity, meeting needs,
consolidation, managed transitions, care
coordination and supported living.
Moderate: clear aims and
objectives that were mainly
achieved by the report
Catty et al. (2012) United
Kingdom
Mental health service users
who utilized CMHTs.
Quantitative, survey,
n = 93
The therapeutic relationship between the key worker
and the service user is a strong indicator of
attachment to the CMHT.
Moderate: clear aims and
objectives. Methods section
was clear and complete
De Búrca et al. (2010)
Ireland
Service users and service
providers who utilize
and work in CMHTs
Mixed methods
n = 738 survey of CMHT
members
Profiling study of 75 CMHT
n = 12 focus groups
n = 10 service user groups
n = 11 case studies
n = 23 local health
manager
Analysis of secondary data.
79% were satisfied with what was recorded about
access to the team, 85% were satisfied with the
level of information on medications and in 75% of
cases service users and their team were in
agreement with their diagnosis. Staff report
resources are limited. Some clinical improvement
was noted by a small sample of service users.
High
Well written with an extensive
method section. Various data
collection methods. Clear aims
and objectives that were
achieved by the report.
Elstad & Eide (2009)
Norway
Service users who utilize
community mental
health services.
Qualitative, interviews,
n = 10
Service users and providers need to be more involved
in the care planning process.
Moderate: the methods and
report achieved the aims of
study
Gale et al. (2012) United
Kingdom
Service users who utilize
community mental
health services.
Qualitative, focus groups,
n = 12
Poor communication between primary care and
mental health services was reported. Paternalism
and poor structures exist in the health services.
Moderate: methods and results
sections were clear and
achieved its aims
Gallagher et al. (2010)
United Kingdom
Service users who utilize
community mental
health services.
Qualitative (pilot study),
interviews,
n = 10
Participants felt stigmatized from a mental health
diagnosis. Trust in service providers was cited as
important.
Moderate: study achieved it aims.
Caution required as it is a pilot
study
Gilburt et al. (2008) United
Kingdom
Service users admitted to
an inpatient unit.
Qualitative, interviews,
n = 19
Companionship to service users was deemed as
important. The need for peer support in acute
services was evident.
Moderate: detailed results and
the study achieved its aims
Hopkins et al. (2009)
United States
Service users expectations
of inpatient care
Literature review 10
papers.
Service users expected to feel in a safe place, have a
relationship with service providers and participate
in talking therapies.
Moderate: methods section
limited. Results achieved
study’s aims
Jespersen et al. (2009)
Australia
Data of service users from
PMHTs
Quantitative survey of 153
referral forms and 89
assessment records
Characteristics of persons who utilize the primary
mental health service were identified. Referrers
overestimated risk and poorly diagnosed depression
and personality disorders. More women than men
utilized PMHTs
Moderate: limited sample
(1 PMHT records audited).
Detailed results
Jones & Crossley (2008)
United Kingdom
Service users and service
providers in acute units.
Qualitative, focus groups,
n = 10
An acute unit admission can have negative
consequences emotionally for service users who
reported a loss of self-worth and adulthood.
Moderate: results described well
and clear methods
Service users’ experiences of Mental Health Care
©2015 John Wiley & Sons Ltd 175
List of papers included in the review
Study Participants Interventions Results Quality Assessment
Arbuckle et al. (2012)
United Kingdom
Mental health service users
who utilize CMHTs.
Quantitative, survey,
n = 24
Need to involve service users in the decision-making
process. The relationship between the service user
and the keyworker is central to service users
attachment to their CMHT
Moderate: small sample.
Unambiguous methods and
results sections
Burns et al. (2009) United
Kingdom
Mental health service users
who utilize CMHTs.
Quantitative, interviews
using instruments,
n = 180
Continuity of care is a key concept in the delivery of
mental health care. This was defined as: experience
and relationship, regularity, meeting needs,
consolidation, managed transitions, care
coordination and supported living.
Moderate: clear aims and
objectives that were mainly
achieved by the report
Catty et al. (2012) United
Kingdom
Mental health service users
who utilized CMHTs.
Quantitative, survey,
n = 93
The therapeutic relationship between the key worker
and the service user is a strong indicator of
attachment to the CMHT.
Moderate: clear aims and
objectives. Methods section
was clear and complete
De Búrca et al. (2010)
Ireland
Service users and service
providers who utilize
and work in CMHTs
Mixed methods
n = 738 survey of CMHT
members
Profiling study of 75 CMHT
n = 12 focus groups
n = 10 service user groups
n = 11 case studies
n = 23 local health
manager
Analysis of secondary data.
79% were satisfied with what was recorded about
access to the team, 85% were satisfied with the
level of information on medications and in 75% of
cases service users and their team were in
agreement with their diagnosis. Staff report
resources are limited. Some clinical improvement
was noted by a small sample of service users.
High
Well written with an extensive
method section. Various data
collection methods. Clear aims
and objectives that were
achieved by the report.
Elstad & Eide (2009)
Norway
Service users who utilize
community mental
health services.
Qualitative, interviews,
n = 10
Service users and providers need to be more involved
in the care planning process.
Moderate: the methods and
report achieved the aims of
study
Gale et al. (2012) United
Kingdom
Service users who utilize
community mental
health services.
Qualitative, focus groups,
n = 12
Poor communication between primary care and
mental health services was reported. Paternalism
and poor structures exist in the health services.
Moderate: methods and results
sections were clear and
achieved its aims
Gallagher et al. (2010)
United Kingdom
Service users who utilize
community mental
health services.
Qualitative (pilot study),
interviews,
n = 10
Participants felt stigmatized from a mental health
diagnosis. Trust in service providers was cited as
important.
Moderate: study achieved it aims.
Caution required as it is a pilot
study
Gilburt et al. (2008) United
Kingdom
Service users admitted to
an inpatient unit.
Qualitative, interviews,
n = 19
Companionship to service users was deemed as
important. The need for peer support in acute
services was evident.
Moderate: detailed results and
the study achieved its aims
Hopkins et al. (2009)
United States
Service users expectations
of inpatient care
Literature review 10
papers.
Service users expected to feel in a safe place, have a
relationship with service providers and participate
in talking therapies.
Moderate: methods section
limited. Results achieved
study’s aims
Jespersen et al. (2009)
Australia
Data of service users from
PMHTs
Quantitative survey of 153
referral forms and 89
assessment records
Characteristics of persons who utilize the primary
mental health service were identified. Referrers
overestimated risk and poorly diagnosed depression
and personality disorders. More women than men
utilized PMHTs
Moderate: limited sample
(1 PMHT records audited).
Detailed results
Jones & Crossley (2008)
United Kingdom
Service users and service
providers in acute units.
Qualitative, focus groups,
n = 10
An acute unit admission can have negative
consequences emotionally for service users who
reported a loss of self-worth and adulthood.
Moderate: results described well
and clear methods
Service users’ experiences of Mental Health Care
©2015 John Wiley & Sons Ltd 175
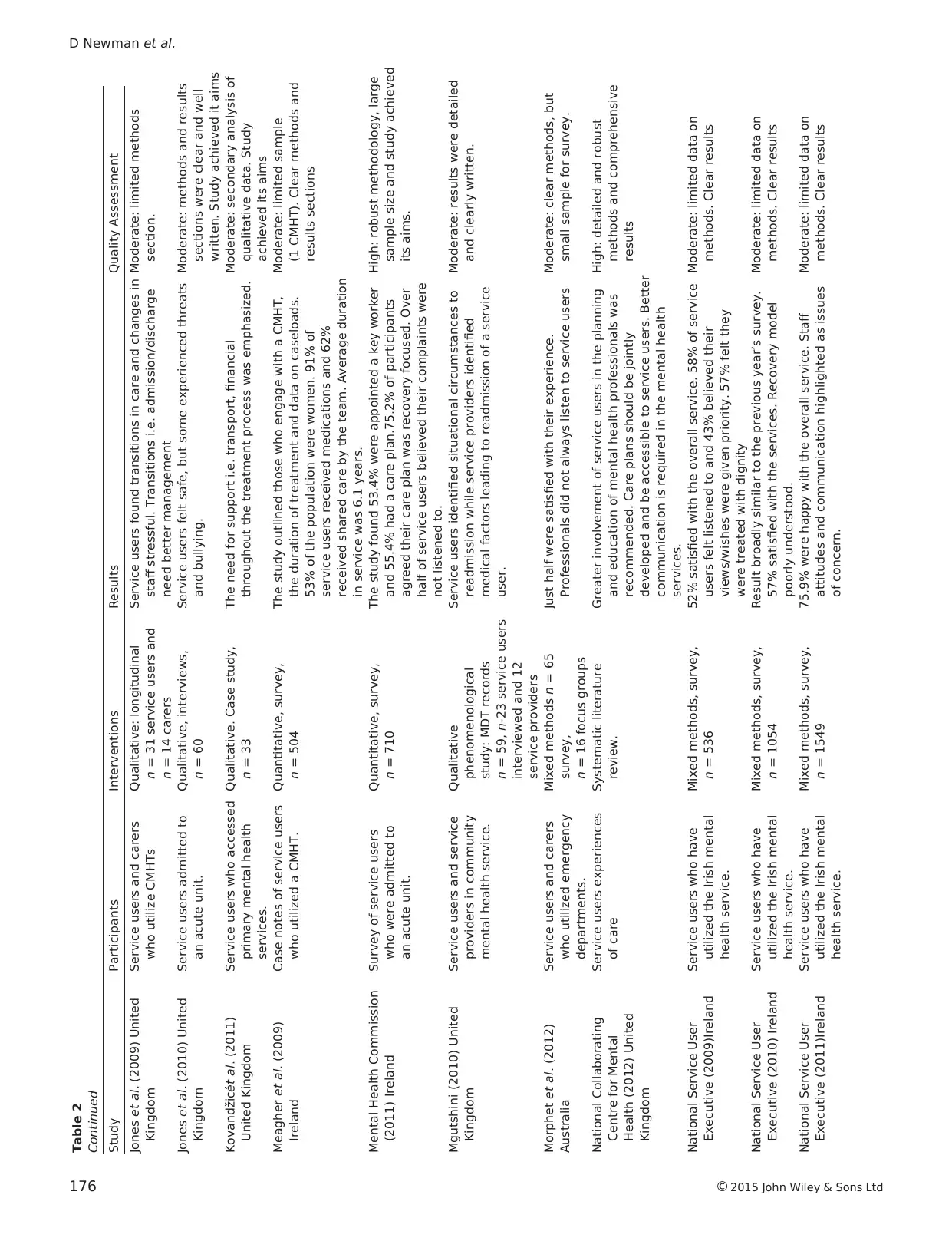
Table 2
Continued
Study Participants Interventions Results Quality Assessment
Jones et al. (2009) United
Kingdom
Service users and carers
who utilize CMHTs
Qualitative: longitudinal
n = 31 service users and
n = 14 carers
Service users found transitions in care and changes in
staff stressful. Transitions i.e. admission/discharge
need better management
Moderate: limited methods
section.
Jones et al. (2010) United
Kingdom
Service users admitted to
an acute unit.
Qualitative, interviews,
n = 60
Service users felt safe, but some experienced threats
and bullying.
Moderate: methods and results
sections were clear and well
written. Study achieved it aims
Kovandžic´et al. (2011)
United Kingdom
Service users who accessed
primary mental health
services.
Qualitative. Case study,
n = 33
The need for support i.e. transport, financial
throughout the treatment process was emphasized.
Moderate: secondary analysis of
qualitative data. Study
achieved its aims
Meagher et al. (2009)
Ireland
Case notes of service users
who utilized a CMHT.
Quantitative, survey,
n = 504
The study outlined those who engage with a CMHT,
the duration of treatment and data on caseloads.
53% of the population were women. 91% of
service users received medications and 62%
received shared care by the team. Average duration
in service was 6.1 years.
Moderate: limited sample
(1 CMHT). Clear methods and
results sections
Mental Health Commission
(2011) Ireland
Survey of service users
who were admitted to
an acute unit.
Quantitative, survey,
n = 710
The study found 53.4% were appointed a key worker
and 55.4% had a care plan.75.2% of participants
agreed their care plan was recovery focused. Over
half of service users believed their complaints were
not listened to.
High: robust methodology, large
sample size and study achieved
its aims.
Mgutshini (2010) United
Kingdom
Service users and service
providers in community
mental health service.
Qualitative
phenomenological
study: MDT records
n = 59, n-23 service users
interviewed and 12
service providers
Service users identified situational circumstances to
readmission while service providers identified
medical factors leading to readmission of a service
user.
Moderate: results were detailed
and clearly written.
Morphet et al. (2012)
Australia
Service users and carers
who utilized emergency
departments.
Mixed methods n = 65
survey,
n = 16 focus groups
Just half were satisfied with their experience.
Professionals did not always listen to service users
Moderate: clear methods, but
small sample for survey.
National Collaborating
Centre for Mental
Health (2012) United
Kingdom
Service users experiences
of care
Systematic literature
review.
Greater involvement of service users in the planning
and education of mental health professionals was
recommended. Care plans should be jointly
developed and be accessible to service users. Better
communication is required in the mental health
services.
High: detailed and robust
methods and comprehensive
results
National Service User
Executive (2009)Ireland
Service users who have
utilized the Irish mental
health service.
Mixed methods, survey,
n = 536
52% satisfied with the overall service. 58% of service
users felt listened to and 43% believed their
views/wishes were given priority. 57% felt they
were treated with dignity
Moderate: limited data on
methods. Clear results
National Service User
Executive (2010) Ireland
Service users who have
utilized the Irish mental
health service.
Mixed methods, survey,
n = 1054
Result broadly similar to the previous year’s survey.
57% satisfied with the services. Recovery model
poorly understood.
Moderate: limited data on
methods. Clear results
National Service User
Executive (2011)Ireland
Service users who have
utilized the Irish mental
health service.
Mixed methods, survey,
n = 1549
75.9% were happy with the overall service. Staff
attitudes and communication highlighted as issues
of concern.
Moderate: limited data on
methods. Clear results
D Newman et al.
176 ©2015 John Wiley & Sons Ltd
Continued
Study Participants Interventions Results Quality Assessment
Jones et al. (2009) United
Kingdom
Service users and carers
who utilize CMHTs
Qualitative: longitudinal
n = 31 service users and
n = 14 carers
Service users found transitions in care and changes in
staff stressful. Transitions i.e. admission/discharge
need better management
Moderate: limited methods
section.
Jones et al. (2010) United
Kingdom
Service users admitted to
an acute unit.
Qualitative, interviews,
n = 60
Service users felt safe, but some experienced threats
and bullying.
Moderate: methods and results
sections were clear and well
written. Study achieved it aims
Kovandžic´et al. (2011)
United Kingdom
Service users who accessed
primary mental health
services.
Qualitative. Case study,
n = 33
The need for support i.e. transport, financial
throughout the treatment process was emphasized.
Moderate: secondary analysis of
qualitative data. Study
achieved its aims
Meagher et al. (2009)
Ireland
Case notes of service users
who utilized a CMHT.
Quantitative, survey,
n = 504
The study outlined those who engage with a CMHT,
the duration of treatment and data on caseloads.
53% of the population were women. 91% of
service users received medications and 62%
received shared care by the team. Average duration
in service was 6.1 years.
Moderate: limited sample
(1 CMHT). Clear methods and
results sections
Mental Health Commission
(2011) Ireland
Survey of service users
who were admitted to
an acute unit.
Quantitative, survey,
n = 710
The study found 53.4% were appointed a key worker
and 55.4% had a care plan.75.2% of participants
agreed their care plan was recovery focused. Over
half of service users believed their complaints were
not listened to.
High: robust methodology, large
sample size and study achieved
its aims.
Mgutshini (2010) United
Kingdom
Service users and service
providers in community
mental health service.
Qualitative
phenomenological
study: MDT records
n = 59, n-23 service users
interviewed and 12
service providers
Service users identified situational circumstances to
readmission while service providers identified
medical factors leading to readmission of a service
user.
Moderate: results were detailed
and clearly written.
Morphet et al. (2012)
Australia
Service users and carers
who utilized emergency
departments.
Mixed methods n = 65
survey,
n = 16 focus groups
Just half were satisfied with their experience.
Professionals did not always listen to service users
Moderate: clear methods, but
small sample for survey.
National Collaborating
Centre for Mental
Health (2012) United
Kingdom
Service users experiences
of care
Systematic literature
review.
Greater involvement of service users in the planning
and education of mental health professionals was
recommended. Care plans should be jointly
developed and be accessible to service users. Better
communication is required in the mental health
services.
High: detailed and robust
methods and comprehensive
results
National Service User
Executive (2009)Ireland
Service users who have
utilized the Irish mental
health service.
Mixed methods, survey,
n = 536
52% satisfied with the overall service. 58% of service
users felt listened to and 43% believed their
views/wishes were given priority. 57% felt they
were treated with dignity
Moderate: limited data on
methods. Clear results
National Service User
Executive (2010) Ireland
Service users who have
utilized the Irish mental
health service.
Mixed methods, survey,
n = 1054
Result broadly similar to the previous year’s survey.
57% satisfied with the services. Recovery model
poorly understood.
Moderate: limited data on
methods. Clear results
National Service User
Executive (2011)Ireland
Service users who have
utilized the Irish mental
health service.
Mixed methods, survey,
n = 1549
75.9% were happy with the overall service. Staff
attitudes and communication highlighted as issues
of concern.
Moderate: limited data on
methods. Clear results
D Newman et al.
176 ©2015 John Wiley & Sons Ltd
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
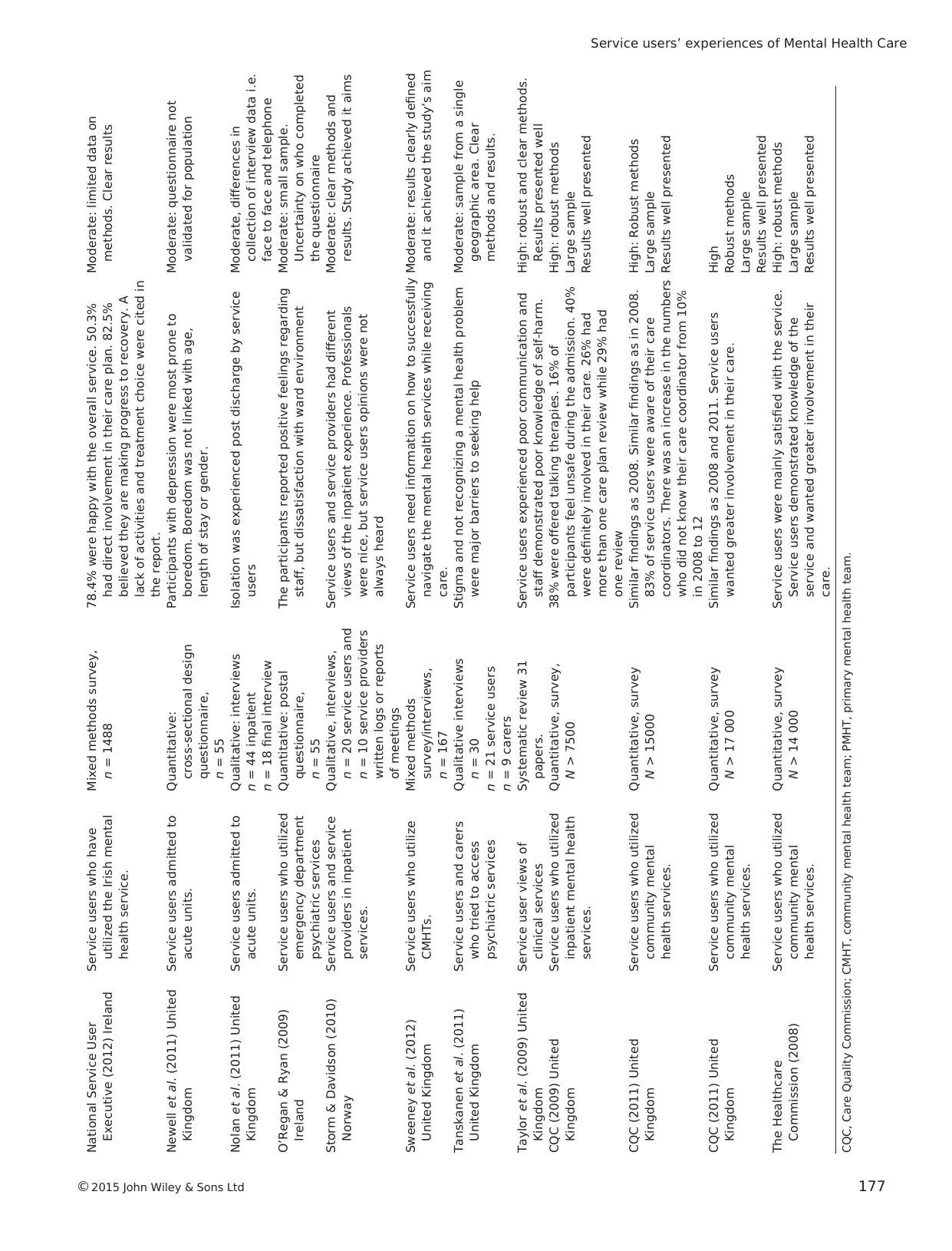
National Service User
Executive (2012) Ireland
Service users who have
utilized the Irish mental
health service.
Mixed methods survey,
n = 1488
78.4% were happy with the overall service. 50.3%
had direct involvement in their care plan. 82.5%
believed they are making progress to recovery. A
lack of activities and treatment choice were cited in
the report.
Moderate: limited data on
methods. Clear results
Newell et al. (2011) United
Kingdom
Service users admitted to
acute units.
Quantitative:
cross-sectional design
questionnaire,
n = 55
Participants with depression were most prone to
boredom. Boredom was not linked with age,
length of stay or gender.
Moderate: questionnaire not
validated for population
Nolan et al. (2011) United
Kingdom
Service users admitted to
acute units.
Qualitative: interviews
n = 44 inpatient
n = 18 final interview
Isolation was experienced post discharge by service
users
Moderate, differences in
collection of interview data i.e.
face to face and telephone
O’Regan & Ryan (2009)
Ireland
Service users who utilized
emergency department
psychiatric services
Quantitative: postal
questionnaire,
n = 55
The participants reported positive feelings regarding
staff, but dissatisfaction with ward environment
Moderate: small sample.
Uncertainty on who completed
the questionnaire
Storm & Davidson (2010)
Norway
Service users and service
providers in inpatient
services.
Qualitative, interviews,
n = 20 service users and
n = 10 service providers
written logs or reports
of meetings
Service users and service providers had different
views of the inpatient experience. Professionals
were nice, but service users opinions were not
always heard
Moderate: clear methods and
results. Study achieved it aims
Sweeney et al. (2012)
United Kingdom
Service users who utilize
CMHTs.
Mixed methods
survey/interviews,
n = 167
Service users need information on how to successfully
navigate the mental health services while receiving
care.
Moderate: results clearly defined
and it achieved the study’s aim
Tanskanen et al. (2011)
United Kingdom
Service users and carers
who tried to access
psychiatric services
Qualitative interviews
n = 30
n = 21 service users
n = 9 carers
Stigma and not recognizing a mental health problem
were major barriers to seeking help
Moderate: sample from a single
geographic area. Clear
methods and results.
Taylor et al. (2009) United
Kingdom
Service user views of
clinical services
Systematic review 31
papers.
Service users experienced poor communication and
staff demonstrated poor knowledge of self-harm.
High: robust and clear methods.
Results presented well
CQC (2009) United
Kingdom
Service users who utilized
inpatient mental health
services.
Quantitative, survey,
N > 7500
38% were offered talking therapies. 16% of
participants feel unsafe during the admission. 40%
were definitely involved in their care. 26% had
more than one care plan review while 29% had
one review
High: robust methods
Large sample
Results well presented
CQC (2011) United
Kingdom
Service users who utilized
community mental
health services.
Quantitative, survey
N > 15000
Similar findings as 2008. Similar findings as in 2008.
83% of service users were aware of their care
coordinators. There was an increase in the numbers
who did not know their care coordinator from 10%
in 2008 to 12
High: Robust methods
Large sample
Results well presented
CQC (2011) United
Kingdom
Service users who utilized
community mental
health services.
Quantitative, survey
N > 17 000
Similar findings as 2008 and 2011. Service users
wanted greater involvement in their care.
High
Robust methods
Large sample
Results well presented
The Healthcare
Commission (2008)
Service users who utilized
community mental
health services.
Quantitative, survey
N > 14 000
Service users were mainly satisfied with the service.
Service users demonstrated knowledge of the
service and wanted greater involvement in their
care.
High: robust methods
Large sample
Results well presented
CQC, Care Quality Commission; CMHT, community mental health team; PMHT, primary mental health team.
Service users’ experiences of Mental Health Care
©2015 John Wiley & Sons Ltd 177
Executive (2012) Ireland
Service users who have
utilized the Irish mental
health service.
Mixed methods survey,
n = 1488
78.4% were happy with the overall service. 50.3%
had direct involvement in their care plan. 82.5%
believed they are making progress to recovery. A
lack of activities and treatment choice were cited in
the report.
Moderate: limited data on
methods. Clear results
Newell et al. (2011) United
Kingdom
Service users admitted to
acute units.
Quantitative:
cross-sectional design
questionnaire,
n = 55
Participants with depression were most prone to
boredom. Boredom was not linked with age,
length of stay or gender.
Moderate: questionnaire not
validated for population
Nolan et al. (2011) United
Kingdom
Service users admitted to
acute units.
Qualitative: interviews
n = 44 inpatient
n = 18 final interview
Isolation was experienced post discharge by service
users
Moderate, differences in
collection of interview data i.e.
face to face and telephone
O’Regan & Ryan (2009)
Ireland
Service users who utilized
emergency department
psychiatric services
Quantitative: postal
questionnaire,
n = 55
The participants reported positive feelings regarding
staff, but dissatisfaction with ward environment
Moderate: small sample.
Uncertainty on who completed
the questionnaire
Storm & Davidson (2010)
Norway
Service users and service
providers in inpatient
services.
Qualitative, interviews,
n = 20 service users and
n = 10 service providers
written logs or reports
of meetings
Service users and service providers had different
views of the inpatient experience. Professionals
were nice, but service users opinions were not
always heard
Moderate: clear methods and
results. Study achieved it aims
Sweeney et al. (2012)
United Kingdom
Service users who utilize
CMHTs.
Mixed methods
survey/interviews,
n = 167
Service users need information on how to successfully
navigate the mental health services while receiving
care.
Moderate: results clearly defined
and it achieved the study’s aim
Tanskanen et al. (2011)
United Kingdom
Service users and carers
who tried to access
psychiatric services
Qualitative interviews
n = 30
n = 21 service users
n = 9 carers
Stigma and not recognizing a mental health problem
were major barriers to seeking help
Moderate: sample from a single
geographic area. Clear
methods and results.
Taylor et al. (2009) United
Kingdom
Service user views of
clinical services
Systematic review 31
papers.
Service users experienced poor communication and
staff demonstrated poor knowledge of self-harm.
High: robust and clear methods.
Results presented well
CQC (2009) United
Kingdom
Service users who utilized
inpatient mental health
services.
Quantitative, survey,
N > 7500
38% were offered talking therapies. 16% of
participants feel unsafe during the admission. 40%
were definitely involved in their care. 26% had
more than one care plan review while 29% had
one review
High: robust methods
Large sample
Results well presented
CQC (2011) United
Kingdom
Service users who utilized
community mental
health services.
Quantitative, survey
N > 15000
Similar findings as 2008. Similar findings as in 2008.
83% of service users were aware of their care
coordinators. There was an increase in the numbers
who did not know their care coordinator from 10%
in 2008 to 12
High: Robust methods
Large sample
Results well presented
CQC (2011) United
Kingdom
Service users who utilized
community mental
health services.
Quantitative, survey
N > 17 000
Similar findings as 2008 and 2011. Service users
wanted greater involvement in their care.
High
Robust methods
Large sample
Results well presented
The Healthcare
Commission (2008)
Service users who utilized
community mental
health services.
Quantitative, survey
N > 14 000
Service users were mainly satisfied with the service.
Service users demonstrated knowledge of the
service and wanted greater involvement in their
care.
High: robust methods
Large sample
Results well presented
CQC, Care Quality Commission; CMHT, community mental health team; PMHT, primary mental health team.
Service users’ experiences of Mental Health Care
©2015 John Wiley & Sons Ltd 177
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

participation in their care. Furthermore, the theme illumi-
nates the difficulties and barriers in facilitating this process.
Twenty-one studies from a range of countries identified
issuesaround relationshipsbetween serviceusers and
service providers (United Kingdom n = 12,Ireland n = 6,
United States n = 1, and Norway n = 2). Of the 21 studies,
8 were quantitative, 6 qualitative, 5 mixed methods and 2
were literature reviews.
Commonly,studiesreported on the importanceof
building relationshipsbetween service usersand service
providers in order to meet service users’ needs
and expectations (Arbuckle et al. 2012 n = 24, Catty et al.
2012 n = 93, Gale et al. 2012 n = 12, National
Collaborating Centre for MentalHealth 2012).Hopkins
et al. (2009),in their review of 10 studies,found that
therapeutic relationships were notalways evidentwithin
mental health settings. Being valued and connected to staff
and peerswas an importantcomponentof the service
users treatmentprogramme(Hopkins et al. 2009). In
addition,Arbuckle et al.(2012)and Catty et al.(2012)
found that the relationship between a service user and a
key worker was centralto service users’connection with
their CMHT.
Service users expressed difficulties in building relation-
ships with service providers,and this can be limiting to
their participation in theircare. The difficultiesranged
from unsupported attitudes ofservice providers to inad-
equatecommunication abouttheir treatment(National
Service User Executive 2009,2010,2011,2012).Within
the inpatient settings,relationships between service users
and service providers were driven by power and lack of
choice.In a study conducted in the United Kingdom,
Gilburt et al.(2008)interviewed patients (n = 19)who
highlighted thatsome staff may use coercion.Service
users reported that fear was an element of their relation-
ship with staff.Other concerns expressed by the patients
were limited information on medication, lack of choice of
treatment,restricted freedom and violence on the ward.
Threats and coercion were cited as influenceswhich
inhibited the service users’role in the decision-making
process (Storm & Davidson 2010).In another qualitative
study, participants expressed the need to trust service pro-
viderswhen providing new information such asa new
mentalhealth diagnosis (Gallagher et al.2010).
Nevertheless, a majority of participants (57%) felt their
psychiatrist listened to them, while 48% of participants felt
that nurses always listened to them according to the Care
Quality Commission (CQC)inpatientquantitative study
(CQC 2009). Engagement can be difficult as service users
and service providers can have differing viewpoints.An
example of this disparity was demonstrated in Mgutshini’s
(2010) qualitative study. From the service providers’ view-
point,rehospitalization was centred on medicalproblems
such as non-concordanceto medication,while service
users’concerns were focused on the psychosocialfactors
that they experienced prior to readmission.
However,some service users reported positive experi-
ences. For example, half of the respondents in the National
Service User Executive (2012) survey felt that service pro-
viders’ attitudes were changing. Of those, 60% felt that staff
attitudes were changing for the better while 36% stated the
shift in attitudes was a mix of positive and negative. Service
users have become more aware of the structure of commu-
nity services and are increasingly engaging with them, for
example in 2008, the CQC reported that 74% of respond-
ents knew their Care Coordinator, while 85% were aware
of their Care Coordinator in 2012. MHC (Ireland) (2011)
reported that 81% of participants had access to a member
of staff at all times, and 87% of participants reported that
they trusted their healthcare team.
The CQC and the HealthcareCommission annual
surveys ofCMHTs on inpatient services showed greater
serviceuser involvementin the care planning process.
These surveyshad substantialnumbersof participants
(2008 N > 14 000, 2009 N = 7500, 2011 N > 15 000, 2012
N > 17 000). CQC (2009) inpatient survey found that 34%
of participants stated they were involved in the decisions
about their care, while 40% reported they were involved to
some extentin the decision-making processand 27%
responded ‘no’to the question.In addition,CQC (2012)
CMHT survey found that54% of service users believed
their views were taken into account during their treatment,
and 43% of service users acknowledged their goals were
included in theircare plan.In contrast,participantsin
Storm & Davidson’s (2010) Norwegian qualitative study
reported their input in the decision-making process were
not taken into consideration although the service providers
showed kindness in their care.In the Irish context,De
Búrca et al.(2010) reported 64% of service users under-
stood and were satisfied with their care plan while 75% of
service users were aware oftheir treatmentreview.The
qualitative study by Elstad & Eide (2009) with 10 partici-
pants outlined the need for service users to be fully involved
in the care planning process.
Activitiesas part of the treatmentprogramme were
sometimes limited. Newell et al. (2011) quantitative study
(n = 55),found thatboredom in acute psychiatric units
plays a significant part of the inpatient experience. Partici-
pants questioned how therapeutic the activities were, while
others described an obligation to join in ward-based activ-
ities (Storm & Davidson 2010).Additionally,the CQC’s
inpatient survey (CQC 2009) identified that 24% of par-
ticipantsbelieved there were enough activitiesavailable
during weekdays;however,thesewere reduced during
D Newman et al.
178 ©2015 John Wiley & Sons Ltd
nates the difficulties and barriers in facilitating this process.
Twenty-one studies from a range of countries identified
issuesaround relationshipsbetween serviceusers and
service providers (United Kingdom n = 12,Ireland n = 6,
United States n = 1, and Norway n = 2). Of the 21 studies,
8 were quantitative, 6 qualitative, 5 mixed methods and 2
were literature reviews.
Commonly,studiesreported on the importanceof
building relationshipsbetween service usersand service
providers in order to meet service users’ needs
and expectations (Arbuckle et al. 2012 n = 24, Catty et al.
2012 n = 93, Gale et al. 2012 n = 12, National
Collaborating Centre for MentalHealth 2012).Hopkins
et al. (2009),in their review of 10 studies,found that
therapeutic relationships were notalways evidentwithin
mental health settings. Being valued and connected to staff
and peerswas an importantcomponentof the service
users treatmentprogramme(Hopkins et al. 2009). In
addition,Arbuckle et al.(2012)and Catty et al.(2012)
found that the relationship between a service user and a
key worker was centralto service users’connection with
their CMHT.
Service users expressed difficulties in building relation-
ships with service providers,and this can be limiting to
their participation in theircare. The difficultiesranged
from unsupported attitudes ofservice providers to inad-
equatecommunication abouttheir treatment(National
Service User Executive 2009,2010,2011,2012).Within
the inpatient settings,relationships between service users
and service providers were driven by power and lack of
choice.In a study conducted in the United Kingdom,
Gilburt et al.(2008)interviewed patients (n = 19)who
highlighted thatsome staff may use coercion.Service
users reported that fear was an element of their relation-
ship with staff.Other concerns expressed by the patients
were limited information on medication, lack of choice of
treatment,restricted freedom and violence on the ward.
Threats and coercion were cited as influenceswhich
inhibited the service users’role in the decision-making
process (Storm & Davidson 2010).In another qualitative
study, participants expressed the need to trust service pro-
viderswhen providing new information such asa new
mentalhealth diagnosis (Gallagher et al.2010).
Nevertheless, a majority of participants (57%) felt their
psychiatrist listened to them, while 48% of participants felt
that nurses always listened to them according to the Care
Quality Commission (CQC)inpatientquantitative study
(CQC 2009). Engagement can be difficult as service users
and service providers can have differing viewpoints.An
example of this disparity was demonstrated in Mgutshini’s
(2010) qualitative study. From the service providers’ view-
point,rehospitalization was centred on medicalproblems
such as non-concordanceto medication,while service
users’concerns were focused on the psychosocialfactors
that they experienced prior to readmission.
However,some service users reported positive experi-
ences. For example, half of the respondents in the National
Service User Executive (2012) survey felt that service pro-
viders’ attitudes were changing. Of those, 60% felt that staff
attitudes were changing for the better while 36% stated the
shift in attitudes was a mix of positive and negative. Service
users have become more aware of the structure of commu-
nity services and are increasingly engaging with them, for
example in 2008, the CQC reported that 74% of respond-
ents knew their Care Coordinator, while 85% were aware
of their Care Coordinator in 2012. MHC (Ireland) (2011)
reported that 81% of participants had access to a member
of staff at all times, and 87% of participants reported that
they trusted their healthcare team.
The CQC and the HealthcareCommission annual
surveys ofCMHTs on inpatient services showed greater
serviceuser involvementin the care planning process.
These surveyshad substantialnumbersof participants
(2008 N > 14 000, 2009 N = 7500, 2011 N > 15 000, 2012
N > 17 000). CQC (2009) inpatient survey found that 34%
of participants stated they were involved in the decisions
about their care, while 40% reported they were involved to
some extentin the decision-making processand 27%
responded ‘no’to the question.In addition,CQC (2012)
CMHT survey found that54% of service users believed
their views were taken into account during their treatment,
and 43% of service users acknowledged their goals were
included in theircare plan.In contrast,participantsin
Storm & Davidson’s (2010) Norwegian qualitative study
reported their input in the decision-making process were
not taken into consideration although the service providers
showed kindness in their care.In the Irish context,De
Búrca et al.(2010) reported 64% of service users under-
stood and were satisfied with their care plan while 75% of
service users were aware oftheir treatmentreview.The
qualitative study by Elstad & Eide (2009) with 10 partici-
pants outlined the need for service users to be fully involved
in the care planning process.
Activitiesas part of the treatmentprogramme were
sometimes limited. Newell et al. (2011) quantitative study
(n = 55),found thatboredom in acute psychiatric units
plays a significant part of the inpatient experience. Partici-
pants questioned how therapeutic the activities were, while
others described an obligation to join in ward-based activ-
ities (Storm & Davidson 2010).Additionally,the CQC’s
inpatient survey (CQC 2009) identified that 24% of par-
ticipantsbelieved there were enough activitiesavailable
during weekdays;however,thesewere reduced during
D Newman et al.
178 ©2015 John Wiley & Sons Ltd
weekends. The level and choice of activities are important
issues for services providers to consider.
In summary,building relationshipsis an important
element in the service users’ treatment programme. Service
users expect and want to have good interpersonal relation-
ships with service providers. Relationships are the basis on
which participation in care may be realized. The relation-
ship between both parties can be attimes unequalwith
limited opportunitiesfor service usersto feel that their
concerns are taken into account. The relationship between
service users and providers remain ambiguous as existing
data do not suggest how these relationships are or should
be constructed in practice.
Working towards continuity of care
This theme illustrates the challenges faced by services users
as they navigate the services during their mental healthcare
journey.Continuity of care is a key componentin the
delivery of mental health care.
Twelve papersdiscussed continuity ofcare and its
impact on service users.However,six of the papers were
also referred to in the previous themes [MHC (Ireland)
2011; De Búrca et al.2010; Storm & Davidson 2010;
National Service User Executive 2012;CQC 2012; The
Healthcare Commission 2008].The papers in this theme
included five qualitative, four quantitative and three mixed
methods studies and were from the United Kingdom (n =
8), Ireland (n = 3) and Norway (n = 1).
Sweeney et al.(2012) mixed methods study (n = 167)
outlined the preconditions to continuity of care in CMHTs.
These were: easy access, the availability of the services and
adequateinformation about the service.Furthermore,
Burns et al.’s (2009) quantitative study with mental health
service users (n = 180),defined the conceptin terms of
experiences, relationships, regularity of meetings, address-
ing needs,consolidating care,managing transitions,coor-
dinating care and supported living. A lack of continuity in
care leads to feelings of loneliness, isolation and less oppor-
tunities for service users to contribute to their care plan
(Nolan et al. 2011). Jones et al. (2009) stressed that service
users experienced social vulnerability when they were not
supported in navigating socialservicessuch asbenefits,
housing and employment.This had a negative impact on
how service users perceived continuity of care.
The system of care, which aims to provide seamless care
to service users has been assessed by various researchers.
According to MHC’s (Ireland) (2011) survey, over half of
the study’s population were assigned a key worker (53.4%),
with 55.4% having had a care plan completed.Less than
30% of service users (29.9%) could not remember a care
plan being drawn up for them during their inpatient stay. In
addition, 52% of complaints made by service users were no
satisfactorily dealt with from a service user’s perspective.
Serviceusers were dissatisfied with thecare planning
process (Storm & Davidson 2010,Nolan et al.2011).A
new process in which service users participate in their care
plan is being introduced to enhance service user participa-
tion in their care. CQC (2012) found that 33% of service
users were involved in more than one care plan review in
2012 compared with 26% in 2008. The numbers of service
users who had no care plan review meeting dropped from
45% in 2008 to 38% in 2012. Despite this improvement,
the number of service users who did not understand their
care plan increased from 8% in 2008 to 9% in 2012.
The consequences of becoming a mentalhealth service
user may not be seen as a positive for some. Some service
users experienced shame and a loss ofadulthood when
admitted to an acute ward (Jones & Crossley 2008). Never-
theless,satisfactions with the services were atmoderate
levels. MHC (Ireland) (2011) reported that just over 84%
of participants were satisfied with the inpatient service and
73% reported some improvementin their health status.
Over 75% agreed their care was recovery focused while
82.5% believed their length of stay in hospital was appro-
priate. The majority of participantsin the qualitative
reports by Jones et al. (2010) and Nolan et al. (2011) felt
stressed and isolated upon discharge from the acute setting
De Búrca et al.’s (2010) mixed methods study found 79%
of service userswere satisfied with theiraccessto the
CMHT; 67% of service users were content with the level of
information provided during their first meeting and 85%
were satisfied with the length of appointments. In relation
to perceived clinicalimprovements,77% of service users
perceived improvements in family relationships, while 56%
experiencedimproved social functioning, and 70%
reported increased self-confidence.The results regarding
perceived improvements must be treated with caution as
only 91 service users were involved in this aspect of the
study. Finally, the National Service User Executive (2012)
mixed methods study found that 78% of service users were
generally satisfied with their service.
In summary,continuity in careis recognized asan
importantgoal; however,these findings suggestthat the
reality falls short of expectations in this regard. Continuity
in care covers both health and social issues for many people
with mentalhealth problems.The limited number of key
workers and completed care plans suggests the concept of
continuity of care remains a goal yet to be achieved.
Discussion
This integrative review hasanalysed the findingsof 34
papers and has identified three key areas that impact on
Service users’ experiences of Mental Health Care
©2015 John Wiley & Sons Ltd 179
issues for services providers to consider.
In summary,building relationshipsis an important
element in the service users’ treatment programme. Service
users expect and want to have good interpersonal relation-
ships with service providers. Relationships are the basis on
which participation in care may be realized. The relation-
ship between both parties can be attimes unequalwith
limited opportunitiesfor service usersto feel that their
concerns are taken into account. The relationship between
service users and providers remain ambiguous as existing
data do not suggest how these relationships are or should
be constructed in practice.
Working towards continuity of care
This theme illustrates the challenges faced by services users
as they navigate the services during their mental healthcare
journey.Continuity of care is a key componentin the
delivery of mental health care.
Twelve papersdiscussed continuity ofcare and its
impact on service users.However,six of the papers were
also referred to in the previous themes [MHC (Ireland)
2011; De Búrca et al.2010; Storm & Davidson 2010;
National Service User Executive 2012;CQC 2012; The
Healthcare Commission 2008].The papers in this theme
included five qualitative, four quantitative and three mixed
methods studies and were from the United Kingdom (n =
8), Ireland (n = 3) and Norway (n = 1).
Sweeney et al.(2012) mixed methods study (n = 167)
outlined the preconditions to continuity of care in CMHTs.
These were: easy access, the availability of the services and
adequateinformation about the service.Furthermore,
Burns et al.’s (2009) quantitative study with mental health
service users (n = 180),defined the conceptin terms of
experiences, relationships, regularity of meetings, address-
ing needs,consolidating care,managing transitions,coor-
dinating care and supported living. A lack of continuity in
care leads to feelings of loneliness, isolation and less oppor-
tunities for service users to contribute to their care plan
(Nolan et al. 2011). Jones et al. (2009) stressed that service
users experienced social vulnerability when they were not
supported in navigating socialservicessuch asbenefits,
housing and employment.This had a negative impact on
how service users perceived continuity of care.
The system of care, which aims to provide seamless care
to service users has been assessed by various researchers.
According to MHC’s (Ireland) (2011) survey, over half of
the study’s population were assigned a key worker (53.4%),
with 55.4% having had a care plan completed.Less than
30% of service users (29.9%) could not remember a care
plan being drawn up for them during their inpatient stay. In
addition, 52% of complaints made by service users were no
satisfactorily dealt with from a service user’s perspective.
Serviceusers were dissatisfied with thecare planning
process (Storm & Davidson 2010,Nolan et al.2011).A
new process in which service users participate in their care
plan is being introduced to enhance service user participa-
tion in their care. CQC (2012) found that 33% of service
users were involved in more than one care plan review in
2012 compared with 26% in 2008. The numbers of service
users who had no care plan review meeting dropped from
45% in 2008 to 38% in 2012. Despite this improvement,
the number of service users who did not understand their
care plan increased from 8% in 2008 to 9% in 2012.
The consequences of becoming a mentalhealth service
user may not be seen as a positive for some. Some service
users experienced shame and a loss ofadulthood when
admitted to an acute ward (Jones & Crossley 2008). Never-
theless,satisfactions with the services were atmoderate
levels. MHC (Ireland) (2011) reported that just over 84%
of participants were satisfied with the inpatient service and
73% reported some improvementin their health status.
Over 75% agreed their care was recovery focused while
82.5% believed their length of stay in hospital was appro-
priate. The majority of participantsin the qualitative
reports by Jones et al. (2010) and Nolan et al. (2011) felt
stressed and isolated upon discharge from the acute setting
De Búrca et al.’s (2010) mixed methods study found 79%
of service userswere satisfied with theiraccessto the
CMHT; 67% of service users were content with the level of
information provided during their first meeting and 85%
were satisfied with the length of appointments. In relation
to perceived clinicalimprovements,77% of service users
perceived improvements in family relationships, while 56%
experiencedimproved social functioning, and 70%
reported increased self-confidence.The results regarding
perceived improvements must be treated with caution as
only 91 service users were involved in this aspect of the
study. Finally, the National Service User Executive (2012)
mixed methods study found that 78% of service users were
generally satisfied with their service.
In summary,continuity in careis recognized asan
importantgoal; however,these findings suggestthat the
reality falls short of expectations in this regard. Continuity
in care covers both health and social issues for many people
with mentalhealth problems.The limited number of key
workers and completed care plans suggests the concept of
continuity of care remains a goal yet to be achieved.
Discussion
This integrative review hasanalysed the findingsof 34
papers and has identified three key areas that impact on
Service users’ experiences of Mental Health Care
©2015 John Wiley & Sons Ltd 179
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
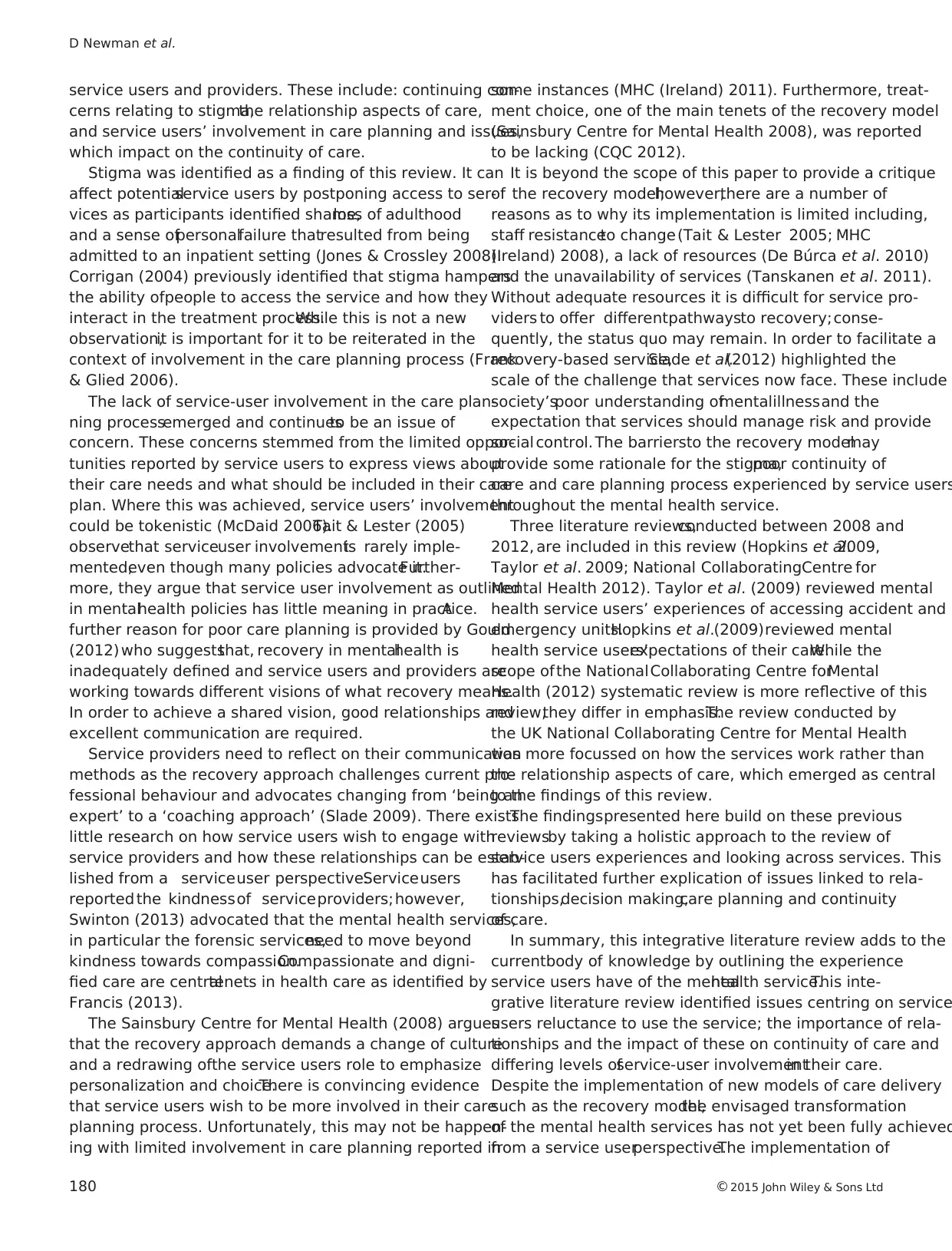
service users and providers. These include: continuing con-
cerns relating to stigma,the relationship aspects of care,
and service users’ involvement in care planning and issues,
which impact on the continuity of care.
Stigma was identified as a finding of this review. It can
affect potentialservice users by postponing access to ser-
vices as participants identified shame,loss of adulthood
and a sense ofpersonalfailure thatresulted from being
admitted to an inpatient setting (Jones & Crossley 2008).
Corrigan (2004) previously identified that stigma hampers
the ability ofpeople to access the service and how they
interact in the treatment process.While this is not a new
observation,it is important for it to be reiterated in the
context of involvement in the care planning process (Frank
& Glied 2006).
The lack of service-user involvement in the care plan-
ning processemerged and continuesto be an issue of
concern. These concerns stemmed from the limited oppor-
tunities reported by service users to express views about
their care needs and what should be included in their care
plan. Where this was achieved, service users’ involvement
could be tokenistic (McDaid 2006).Tait & Lester (2005)
observethat serviceuser involvementis rarely imple-
mented,even though many policies advocate it.Further-
more, they argue that service user involvement as outlined
in mentalhealth policies has little meaning in practice.A
further reason for poor care planning is provided by Gould
(2012) who suggeststhat, recovery in mentalhealth is
inadequately defined and service users and providers are
working towards different visions of what recovery means.
In order to achieve a shared vision, good relationships and
excellent communication are required.
Service providers need to reflect on their communication
methods as the recovery approach challenges current pro-
fessional behaviour and advocates changing from ‘being an
expert’ to a ‘coaching approach’ (Slade 2009). There exists
little research on how service users wish to engage with
service providers and how these relationships can be estab-
lished from a serviceuser perspective.Serviceusers
reported the kindnessof serviceproviders;however,
Swinton (2013) advocated that the mental health services,
in particular the forensic services,need to move beyond
kindness towards compassion.Compassionate and digni-
fied care are centraltenets in health care as identified by
Francis (2013).
The Sainsbury Centre for Mental Health (2008) argues
that the recovery approach demands a change of culture
and a redrawing ofthe service users role to emphasize
personalization and choice.There is convincing evidence
that service users wish to be more involved in their care
planning process. Unfortunately, this may not be happen-
ing with limited involvement in care planning reported in
some instances (MHC (Ireland) 2011). Furthermore, treat-
ment choice, one of the main tenets of the recovery model
(Sainsbury Centre for Mental Health 2008), was reported
to be lacking (CQC 2012).
It is beyond the scope of this paper to provide a critique
of the recovery model;however,there are a number of
reasons as to why its implementation is limited including,
staff resistanceto change(Tait & Lester 2005; MHC
(Ireland) 2008), a lack of resources (De Búrca et al. 2010)
and the unavailability of services (Tanskanen et al. 2011).
Without adequate resources it is difficult for service pro-
viders to offer differentpathwaysto recovery;conse-
quently, the status quo may remain. In order to facilitate a
recovery-based service,Slade et al.(2012) highlighted the
scale of the challenge that services now face. These include
society’spoor understanding ofmentalillnessand the
expectation that services should manage risk and provide
social control. The barriersto the recovery modelmay
provide some rationale for the stigma,poor continuity of
care and care planning process experienced by service users
throughout the mental health service.
Three literature reviews,conducted between 2008 and
2012, are included in this review (Hopkins et al.2009,
Taylor et al. 2009; National CollaboratingCentre for
Mental Health 2012). Taylor et al. (2009) reviewed mental
health service users’ experiences of accessing accident and
emergency units.Hopkins et al.(2009)reviewed mental
health service users’expectations of their care.While the
scope ofthe NationalCollaborating Centre forMental
Health (2012) systematic review is more reflective of this
review,they differ in emphasis.The review conducted by
the UK National Collaborating Centre for Mental Health
was more focussed on how the services work rather than
the relationship aspects of care, which emerged as central
to the findings of this review.
The findingspresented here build on these previous
reviewsby taking a holistic approach to the review of
service users experiences and looking across services. This
has facilitated further explication of issues linked to rela-
tionships,decision making,care planning and continuity
of care.
In summary, this integrative literature review adds to the
currentbody of knowledge by outlining the experience
service users have of the mentalhealth service.This inte-
grative literature review identified issues centring on service
users reluctance to use the service; the importance of rela-
tionships and the impact of these on continuity of care and
differing levels ofservice-user involvementin their care.
Despite the implementation of new models of care delivery
such as the recovery model,the envisaged transformation
of the mental health services has not yet been fully achieved
from a service userperspective.The implementation of
D Newman et al.
180 ©2015 John Wiley & Sons Ltd
cerns relating to stigma,the relationship aspects of care,
and service users’ involvement in care planning and issues,
which impact on the continuity of care.
Stigma was identified as a finding of this review. It can
affect potentialservice users by postponing access to ser-
vices as participants identified shame,loss of adulthood
and a sense ofpersonalfailure thatresulted from being
admitted to an inpatient setting (Jones & Crossley 2008).
Corrigan (2004) previously identified that stigma hampers
the ability ofpeople to access the service and how they
interact in the treatment process.While this is not a new
observation,it is important for it to be reiterated in the
context of involvement in the care planning process (Frank
& Glied 2006).
The lack of service-user involvement in the care plan-
ning processemerged and continuesto be an issue of
concern. These concerns stemmed from the limited oppor-
tunities reported by service users to express views about
their care needs and what should be included in their care
plan. Where this was achieved, service users’ involvement
could be tokenistic (McDaid 2006).Tait & Lester (2005)
observethat serviceuser involvementis rarely imple-
mented,even though many policies advocate it.Further-
more, they argue that service user involvement as outlined
in mentalhealth policies has little meaning in practice.A
further reason for poor care planning is provided by Gould
(2012) who suggeststhat, recovery in mentalhealth is
inadequately defined and service users and providers are
working towards different visions of what recovery means.
In order to achieve a shared vision, good relationships and
excellent communication are required.
Service providers need to reflect on their communication
methods as the recovery approach challenges current pro-
fessional behaviour and advocates changing from ‘being an
expert’ to a ‘coaching approach’ (Slade 2009). There exists
little research on how service users wish to engage with
service providers and how these relationships can be estab-
lished from a serviceuser perspective.Serviceusers
reported the kindnessof serviceproviders;however,
Swinton (2013) advocated that the mental health services,
in particular the forensic services,need to move beyond
kindness towards compassion.Compassionate and digni-
fied care are centraltenets in health care as identified by
Francis (2013).
The Sainsbury Centre for Mental Health (2008) argues
that the recovery approach demands a change of culture
and a redrawing ofthe service users role to emphasize
personalization and choice.There is convincing evidence
that service users wish to be more involved in their care
planning process. Unfortunately, this may not be happen-
ing with limited involvement in care planning reported in
some instances (MHC (Ireland) 2011). Furthermore, treat-
ment choice, one of the main tenets of the recovery model
(Sainsbury Centre for Mental Health 2008), was reported
to be lacking (CQC 2012).
It is beyond the scope of this paper to provide a critique
of the recovery model;however,there are a number of
reasons as to why its implementation is limited including,
staff resistanceto change(Tait & Lester 2005; MHC
(Ireland) 2008), a lack of resources (De Búrca et al. 2010)
and the unavailability of services (Tanskanen et al. 2011).
Without adequate resources it is difficult for service pro-
viders to offer differentpathwaysto recovery;conse-
quently, the status quo may remain. In order to facilitate a
recovery-based service,Slade et al.(2012) highlighted the
scale of the challenge that services now face. These include
society’spoor understanding ofmentalillnessand the
expectation that services should manage risk and provide
social control. The barriersto the recovery modelmay
provide some rationale for the stigma,poor continuity of
care and care planning process experienced by service users
throughout the mental health service.
Three literature reviews,conducted between 2008 and
2012, are included in this review (Hopkins et al.2009,
Taylor et al. 2009; National CollaboratingCentre for
Mental Health 2012). Taylor et al. (2009) reviewed mental
health service users’ experiences of accessing accident and
emergency units.Hopkins et al.(2009)reviewed mental
health service users’expectations of their care.While the
scope ofthe NationalCollaborating Centre forMental
Health (2012) systematic review is more reflective of this
review,they differ in emphasis.The review conducted by
the UK National Collaborating Centre for Mental Health
was more focussed on how the services work rather than
the relationship aspects of care, which emerged as central
to the findings of this review.
The findingspresented here build on these previous
reviewsby taking a holistic approach to the review of
service users experiences and looking across services. This
has facilitated further explication of issues linked to rela-
tionships,decision making,care planning and continuity
of care.
In summary, this integrative literature review adds to the
currentbody of knowledge by outlining the experience
service users have of the mentalhealth service.This inte-
grative literature review identified issues centring on service
users reluctance to use the service; the importance of rela-
tionships and the impact of these on continuity of care and
differing levels ofservice-user involvementin their care.
Despite the implementation of new models of care delivery
such as the recovery model,the envisaged transformation
of the mental health services has not yet been fully achieved
from a service userperspective.The implementation of
D Newman et al.
180 ©2015 John Wiley & Sons Ltd
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
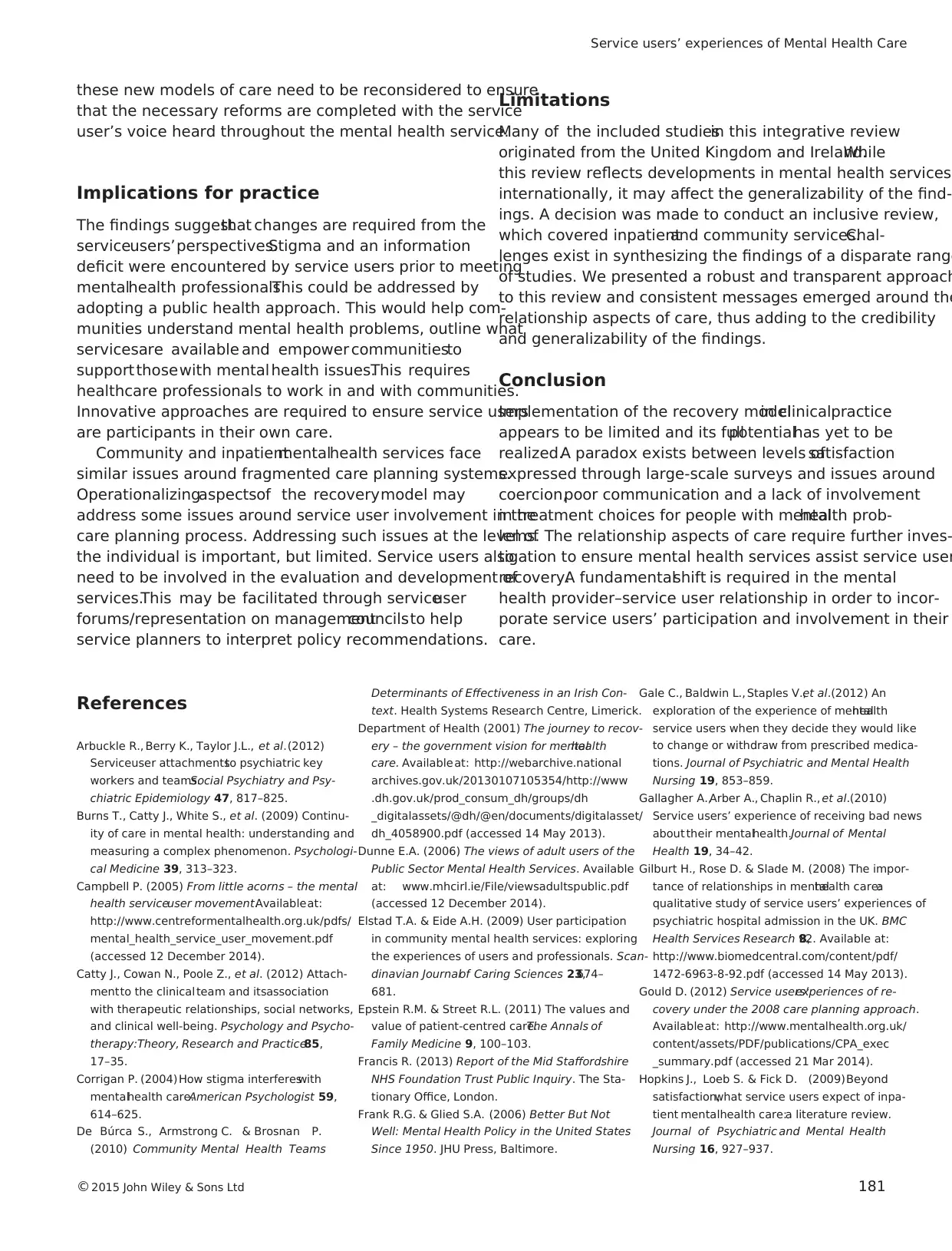
these new models of care need to be reconsidered to ensure
that the necessary reforms are completed with the service
user’s voice heard throughout the mental health service.
Implications for practice
The findings suggestthat changes are required from the
serviceusers’perspectives.Stigma and an information
deficit were encountered by service users prior to meeting
mentalhealth professionals.This could be addressed by
adopting a public health approach. This would help com-
munities understand mental health problems, outline what
servicesare available and empower communitiesto
support thosewith mental health issues.This requires
healthcare professionals to work in and with communities.
Innovative approaches are required to ensure service users
are participants in their own care.
Community and inpatientmentalhealth services face
similar issues around fragmented care planning systems.
Operationalizingaspectsof the recoverymodel may
address some issues around service user involvement in the
care planning process. Addressing such issues at the level of
the individual is important, but limited. Service users also
need to be involved in the evaluation and development of
services.This may be facilitated through serviceuser
forums/representation on managementcouncilsto help
service planners to interpret policy recommendations.
Limitations
Many of the included studiesin this integrative review
originated from the United Kingdom and Ireland.While
this review reflects developments in mental health services
internationally, it may affect the generalizability of the find-
ings. A decision was made to conduct an inclusive review,
which covered inpatientand community services.Chal-
lenges exist in synthesizing the findings of a disparate range
of studies. We presented a robust and transparent approach
to this review and consistent messages emerged around the
relationship aspects of care, thus adding to the credibility
and generalizability of the findings.
Conclusion
Implementation of the recovery modelin clinicalpractice
appears to be limited and its fullpotentialhas yet to be
realized.A paradox exists between levels ofsatisfaction
expressed through large-scale surveys and issues around
coercion,poor communication and a lack of involvement
in treatment choices for people with mentalhealth prob-
lems. The relationship aspects of care require further inves-
tigation to ensure mental health services assist service user
recovery.A fundamentalshift is required in the mental
health provider–service user relationship in order to incor-
porate service users’ participation and involvement in their
care.
References
Arbuckle R., Berry K., Taylor J.L., et al.(2012)
Serviceuser attachmentsto psychiatric key
workers and teams.Social Psychiatry and Psy-
chiatric Epidemiology 47, 817–825.
Burns T., Catty J., White S., et al. (2009) Continu-
ity of care in mental health: understanding and
measuring a complex phenomenon. Psychologi-
cal Medicine 39, 313–323.
Campbell P. (2005) From little acorns – the mental
health serviceuser movement.Availableat:
http://www.centreformentalhealth.org.uk/pdfs/
mental_health_service_user_movement.pdf
(accessed 12 December 2014).
Catty J., Cowan N., Poole Z., et al. (2012) Attach-
mentto the clinical team and itsassociation
with therapeutic relationships, social networks,
and clinical well-being. Psychology and Psycho-
therapy:Theory, Research and Practice85,
17–35.
Corrigan P. (2004) How stigma interfereswith
mentalhealth care.American Psychologist 59,
614–625.
De Búrca S., Armstrong C. & Brosnan P.
(2010) Community Mental Health Teams
Determinants of Effectiveness in an Irish Con-
text. Health Systems Research Centre, Limerick.
Department of Health (2001) The journey to recov-
ery – the government vision for mentalhealth
care. Availableat: http://webarchive.national
archives.gov.uk/20130107105354/http://www
.dh.gov.uk/prod_consum_dh/groups/dh
_digitalassets/@dh/@en/documents/digitalasset/
dh_4058900.pdf (accessed 14 May 2013).
Dunne E.A. (2006) The views of adult users of the
Public Sector Mental Health Services. Available
at: www.mhcirl.ie/File/viewsadultspublic.pdf
(accessed 12 December 2014).
Elstad T.A. & Eide A.H. (2009) User participation
in community mental health services: exploring
the experiences of users and professionals. Scan-
dinavian Journalof Caring Sciences 23,674–
681.
Epstein R.M. & Street R.L. (2011) The values and
value of patient-centred care.The Annals of
Family Medicine 9, 100–103.
Francis R. (2013) Report of the Mid Staffordshire
NHS Foundation Trust Public Inquiry. The Sta-
tionary Office, London.
Frank R.G. & Glied S.A. (2006) Better But Not
Well: Mental Health Policy in the United States
Since 1950. JHU Press, Baltimore.
Gale C., Baldwin L., Staples V.,et al.(2012) An
exploration of the experience of mentalhealth
service users when they decide they would like
to change or withdraw from prescribed medica-
tions. Journal of Psychiatric and Mental Health
Nursing 19, 853–859.
Gallagher A.,Arber A., Chaplin R., et al.(2010)
Service users’ experience of receiving bad news
about their mentalhealth.Journal of Mental
Health 19, 34–42.
Gilburt H., Rose D. & Slade M. (2008) The impor-
tance of relationships in mentalhealth care:a
qualitative study of service users’ experiences of
psychiatric hospital admission in the UK. BMC
Health Services Research 8,92. Available at:
http://www.biomedcentral.com/content/pdf/
1472-6963-8-92.pdf (accessed 14 May 2013).
Gould D. (2012) Service users’experiences of re-
covery under the 2008 care planning approach.
Availableat: http://www.mentalhealth.org.uk/
content/assets/PDF/publications/CPA_exec
_summary.pdf (accessed 21 Mar 2014).
Hopkins J., Loeb S. & Fick D. (2009)Beyond
satisfaction,what service users expect of inpa-
tient mentalhealth care:a literature review.
Journal of Psychiatric and Mental Health
Nursing 16, 927–937.
Service users’ experiences of Mental Health Care
©2015 John Wiley & Sons Ltd 181
that the necessary reforms are completed with the service
user’s voice heard throughout the mental health service.
Implications for practice
The findings suggestthat changes are required from the
serviceusers’perspectives.Stigma and an information
deficit were encountered by service users prior to meeting
mentalhealth professionals.This could be addressed by
adopting a public health approach. This would help com-
munities understand mental health problems, outline what
servicesare available and empower communitiesto
support thosewith mental health issues.This requires
healthcare professionals to work in and with communities.
Innovative approaches are required to ensure service users
are participants in their own care.
Community and inpatientmentalhealth services face
similar issues around fragmented care planning systems.
Operationalizingaspectsof the recoverymodel may
address some issues around service user involvement in the
care planning process. Addressing such issues at the level of
the individual is important, but limited. Service users also
need to be involved in the evaluation and development of
services.This may be facilitated through serviceuser
forums/representation on managementcouncilsto help
service planners to interpret policy recommendations.
Limitations
Many of the included studiesin this integrative review
originated from the United Kingdom and Ireland.While
this review reflects developments in mental health services
internationally, it may affect the generalizability of the find-
ings. A decision was made to conduct an inclusive review,
which covered inpatientand community services.Chal-
lenges exist in synthesizing the findings of a disparate range
of studies. We presented a robust and transparent approach
to this review and consistent messages emerged around the
relationship aspects of care, thus adding to the credibility
and generalizability of the findings.
Conclusion
Implementation of the recovery modelin clinicalpractice
appears to be limited and its fullpotentialhas yet to be
realized.A paradox exists between levels ofsatisfaction
expressed through large-scale surveys and issues around
coercion,poor communication and a lack of involvement
in treatment choices for people with mentalhealth prob-
lems. The relationship aspects of care require further inves-
tigation to ensure mental health services assist service user
recovery.A fundamentalshift is required in the mental
health provider–service user relationship in order to incor-
porate service users’ participation and involvement in their
care.
References
Arbuckle R., Berry K., Taylor J.L., et al.(2012)
Serviceuser attachmentsto psychiatric key
workers and teams.Social Psychiatry and Psy-
chiatric Epidemiology 47, 817–825.
Burns T., Catty J., White S., et al. (2009) Continu-
ity of care in mental health: understanding and
measuring a complex phenomenon. Psychologi-
cal Medicine 39, 313–323.
Campbell P. (2005) From little acorns – the mental
health serviceuser movement.Availableat:
http://www.centreformentalhealth.org.uk/pdfs/
mental_health_service_user_movement.pdf
(accessed 12 December 2014).
Catty J., Cowan N., Poole Z., et al. (2012) Attach-
mentto the clinical team and itsassociation
with therapeutic relationships, social networks,
and clinical well-being. Psychology and Psycho-
therapy:Theory, Research and Practice85,
17–35.
Corrigan P. (2004) How stigma interfereswith
mentalhealth care.American Psychologist 59,
614–625.
De Búrca S., Armstrong C. & Brosnan P.
(2010) Community Mental Health Teams
Determinants of Effectiveness in an Irish Con-
text. Health Systems Research Centre, Limerick.
Department of Health (2001) The journey to recov-
ery – the government vision for mentalhealth
care. Availableat: http://webarchive.national
archives.gov.uk/20130107105354/http://www
.dh.gov.uk/prod_consum_dh/groups/dh
_digitalassets/@dh/@en/documents/digitalasset/
dh_4058900.pdf (accessed 14 May 2013).
Dunne E.A. (2006) The views of adult users of the
Public Sector Mental Health Services. Available
at: www.mhcirl.ie/File/viewsadultspublic.pdf
(accessed 12 December 2014).
Elstad T.A. & Eide A.H. (2009) User participation
in community mental health services: exploring
the experiences of users and professionals. Scan-
dinavian Journalof Caring Sciences 23,674–
681.
Epstein R.M. & Street R.L. (2011) The values and
value of patient-centred care.The Annals of
Family Medicine 9, 100–103.
Francis R. (2013) Report of the Mid Staffordshire
NHS Foundation Trust Public Inquiry. The Sta-
tionary Office, London.
Frank R.G. & Glied S.A. (2006) Better But Not
Well: Mental Health Policy in the United States
Since 1950. JHU Press, Baltimore.
Gale C., Baldwin L., Staples V.,et al.(2012) An
exploration of the experience of mentalhealth
service users when they decide they would like
to change or withdraw from prescribed medica-
tions. Journal of Psychiatric and Mental Health
Nursing 19, 853–859.
Gallagher A.,Arber A., Chaplin R., et al.(2010)
Service users’ experience of receiving bad news
about their mentalhealth.Journal of Mental
Health 19, 34–42.
Gilburt H., Rose D. & Slade M. (2008) The impor-
tance of relationships in mentalhealth care:a
qualitative study of service users’ experiences of
psychiatric hospital admission in the UK. BMC
Health Services Research 8,92. Available at:
http://www.biomedcentral.com/content/pdf/
1472-6963-8-92.pdf (accessed 14 May 2013).
Gould D. (2012) Service users’experiences of re-
covery under the 2008 care planning approach.
Availableat: http://www.mentalhealth.org.uk/
content/assets/PDF/publications/CPA_exec
_summary.pdf (accessed 21 Mar 2014).
Hopkins J., Loeb S. & Fick D. (2009)Beyond
satisfaction,what service users expect of inpa-
tient mentalhealth care:a literature review.
Journal of Psychiatric and Mental Health
Nursing 16, 927–937.
Service users’ experiences of Mental Health Care
©2015 John Wiley & Sons Ltd 181
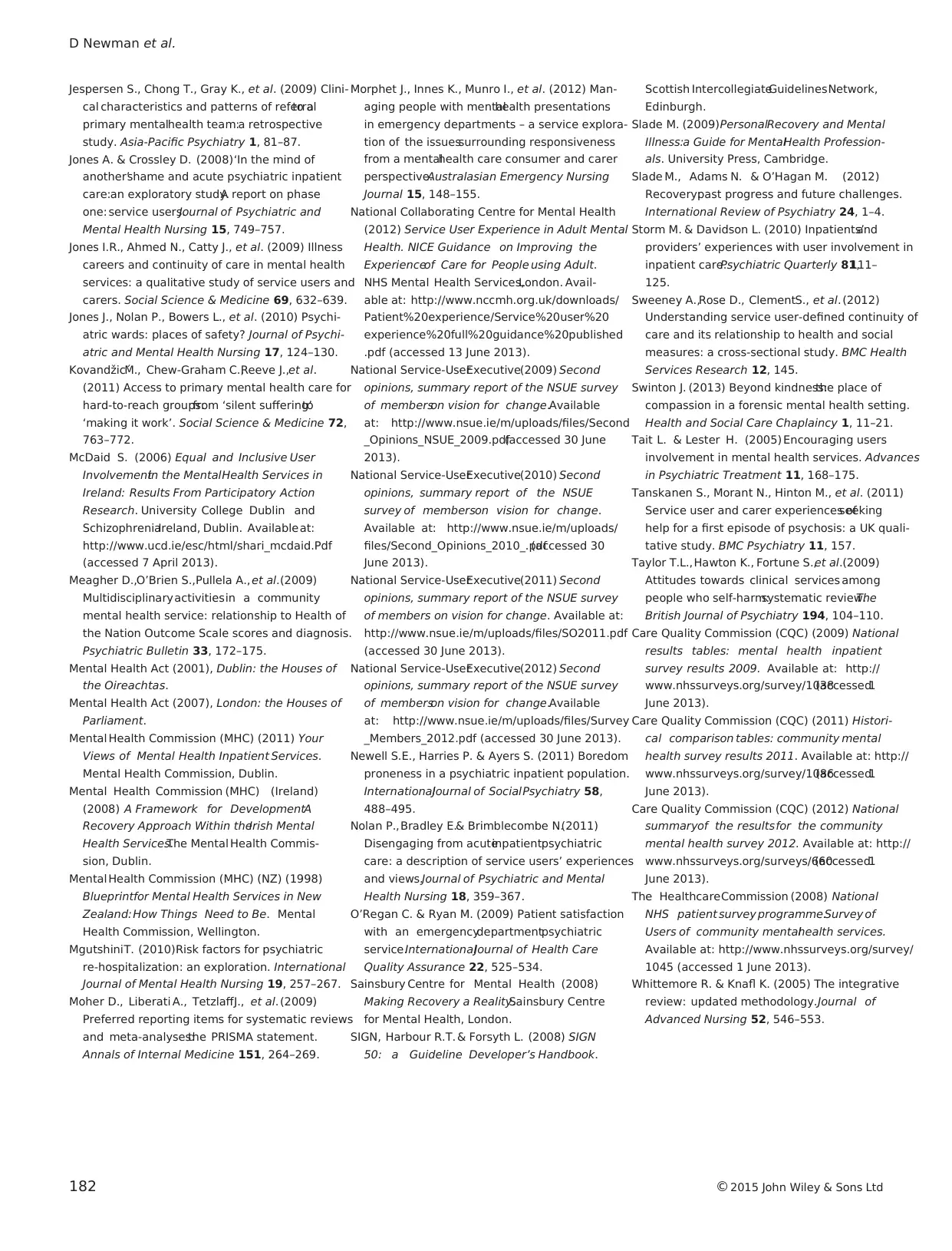
Jespersen S., Chong T., Gray K., et al. (2009) Clini-
cal characteristics and patterns of referralto a
primary mentalhealth team:a retrospective
study. Asia-Pacific Psychiatry 1, 81–87.
Jones A. & Crossley D. (2008)‘In the mind of
another’shame and acute psychiatric inpatient
care:an exploratory study.A report on phase
one: service users.Journal of Psychiatric and
Mental Health Nursing 15, 749–757.
Jones I.R., Ahmed N., Catty J., et al. (2009) Illness
careers and continuity of care in mental health
services: a qualitative study of service users and
carers. Social Science & Medicine 69, 632–639.
Jones J., Nolan P., Bowers L., et al. (2010) Psychi-
atric wards: places of safety? Journal of Psychi-
atric and Mental Health Nursing 17, 124–130.
Kovandžic´M., Chew-Graham C.,Reeve J.,et al.
(2011) Access to primary mental health care for
hard-to-reach groups:from ‘silent suffering’to
‘making it work’. Social Science & Medicine 72,
763–772.
McDaid S. (2006) Equal and Inclusive User
Involvementin the MentalHealth Services in
Ireland: Results From Participatory Action
Research. University College Dublin and
SchizophreniaIreland, Dublin. Availableat:
http://www.ucd.ie/esc/html/shari_mcdaid.Pdf
(accessed 7 April 2013).
Meagher D.,O’Brien S.,Pullela A., et al.(2009)
Multidisciplinaryactivitiesin a community
mental health service: relationship to Health of
the Nation Outcome Scale scores and diagnosis.
Psychiatric Bulletin 33, 172–175.
Mental Health Act (2001), Dublin: the Houses of
the Oireachtas.
Mental Health Act (2007), London: the Houses of
Parliament.
Mental Health Commission (MHC) (2011) Your
Views of Mental Health Inpatient Services.
Mental Health Commission, Dublin.
Mental Health Commission (MHC) (Ireland)
(2008) A Framework for DevelopmentA
Recovery Approach Within theIrish Mental
Health Services.The Mental Health Commis-
sion, Dublin.
Mental Health Commission (MHC) (NZ) (1998)
Blueprintfor Mental Health Services in New
Zealand:How Things Need to Be. Mental
Health Commission, Wellington.
MgutshiniT. (2010)Risk factors for psychiatric
re-hospitalization: an exploration. International
Journal of Mental Health Nursing 19, 257–267.
Moher D., Liberati A., TetzlaffJ., et al.(2009)
Preferred reporting items for systematic reviews
and meta-analyses:the PRISMA statement.
Annals of Internal Medicine 151, 264–269.
Morphet J., Innes K., Munro I., et al. (2012) Man-
aging people with mentalhealth presentations
in emergency departments – a service explora-
tion of the issuessurrounding responsiveness
from a mentalhealth care consumer and carer
perspective.Australasian Emergency Nursing
Journal 15, 148–155.
National Collaborating Centre for Mental Health
(2012) Service User Experience in Adult Mental
Health. NICE Guidance on Improving the
Experienceof Care for People using Adult.
NHS Mental Health Services,London. Avail-
able at: http://www.nccmh.org.uk/downloads/
Patient%20experience/Service%20user%20
experience%20full%20guidance%20published
.pdf (accessed 13 June 2013).
National Service-UserExecutive(2009) Second
opinions, summary report of the NSUE survey
of memberson vision for change.Available
at: http://www.nsue.ie/m/uploads/files/Second
_Opinions_NSUE_2009.pdf(accessed 30 June
2013).
National Service-UserExecutive(2010) Second
opinions, summary report of the NSUE
survey of memberson vision for change.
Available at: http://www.nsue.ie/m/uploads/
files/Second_Opinions_2010_.pdf(accessed 30
June 2013).
National Service-UserExecutive(2011) Second
opinions, summary report of the NSUE survey
of members on vision for change. Available at:
http://www.nsue.ie/m/uploads/files/SO2011.pdf
(accessed 30 June 2013).
National Service-UserExecutive(2012) Second
opinions, summary report of the NSUE survey
of memberson vision for change.Available
at: http://www.nsue.ie/m/uploads/files/Survey
_Members_2012.pdf (accessed 30 June 2013).
Newell S.E., Harries P. & Ayers S. (2011) Boredom
proneness in a psychiatric inpatient population.
InternationalJournal of SocialPsychiatry 58,
488–495.
Nolan P.,Bradley E.& Brimblecombe N.(2011)
Disengaging from acuteinpatientpsychiatric
care: a description of service users’ experiences
and views.Journal of Psychiatric and Mental
Health Nursing 18, 359–367.
O’Regan C. & Ryan M. (2009) Patient satisfaction
with an emergencydepartmentpsychiatric
service.InternationalJournal of Health Care
Quality Assurance 22, 525–534.
Sainsbury Centre for Mental Health (2008)
Making Recovery a Reality.Sainsbury Centre
for Mental Health, London.
SIGN, Harbour R.T. & Forsyth L. (2008) SIGN
50: a Guideline Developer’s Handbook.
Scottish IntercollegiateGuidelinesNetwork,
Edinburgh.
Slade M. (2009)PersonalRecovery and Mental
Illness:a Guide for MentalHealth Profession-
als. University Press, Cambridge.
Slade M., Adams N. & O’Hagan M. (2012)
Recovery:past progress and future challenges.
International Review of Psychiatry 24, 1–4.
Storm M. & Davidson L. (2010) Inpatients’and
providers’ experiences with user involvement in
inpatient care.Psychiatric Quarterly 81,111–
125.
Sweeney A.,Rose D., ClementS., et al. (2012)
Understanding service user-defined continuity of
care and its relationship to health and social
measures: a cross-sectional study. BMC Health
Services Research 12, 145.
Swinton J. (2013) Beyond kindness:the place of
compassion in a forensic mental health setting.
Health and Social Care Chaplaincy 1, 11–21.
Tait L. & Lester H. (2005) Encouraging users
involvement in mental health services. Advances
in Psychiatric Treatment 11, 168–175.
Tanskanen S., Morant N., Hinton M., et al. (2011)
Service user and carer experiences ofseeking
help for a first episode of psychosis: a UK quali-
tative study. BMC Psychiatry 11, 157.
Taylor T.L.,Hawton K., Fortune S.,et al.(2009)
Attitudes towards clinical services among
people who self-harm:systematic review.The
British Journal of Psychiatry 194, 104–110.
Care Quality Commission (CQC) (2009) National
results tables: mental health inpatient
survey results 2009. Available at: http://
www.nhssurveys.org/survey/1038(accessed1
June 2013).
Care Quality Commission (CQC) (2011) Histori-
cal comparison tables: community mental
health survey results 2011. Available at: http://
www.nhssurveys.org/survey/1086(accessed1
June 2013).
Care Quality Commission (CQC) (2012) National
summaryof the resultsfor the community
mental health survey 2012. Available at: http://
www.nhssurveys.org/surveys/660(accessed1
June 2013).
The HealthcareCommission (2008) National
NHS patient survey programme.Survey of
Users of community mentalhealth services.
Available at: http://www.nhssurveys.org/survey/
1045 (accessed 1 June 2013).
Whittemore R. & Knafl K. (2005) The integrative
review: updated methodology.Journal of
Advanced Nursing 52, 546–553.
D Newman et al.
182 ©2015 John Wiley & Sons Ltd
cal characteristics and patterns of referralto a
primary mentalhealth team:a retrospective
study. Asia-Pacific Psychiatry 1, 81–87.
Jones A. & Crossley D. (2008)‘In the mind of
another’shame and acute psychiatric inpatient
care:an exploratory study.A report on phase
one: service users.Journal of Psychiatric and
Mental Health Nursing 15, 749–757.
Jones I.R., Ahmed N., Catty J., et al. (2009) Illness
careers and continuity of care in mental health
services: a qualitative study of service users and
carers. Social Science & Medicine 69, 632–639.
Jones J., Nolan P., Bowers L., et al. (2010) Psychi-
atric wards: places of safety? Journal of Psychi-
atric and Mental Health Nursing 17, 124–130.
Kovandžic´M., Chew-Graham C.,Reeve J.,et al.
(2011) Access to primary mental health care for
hard-to-reach groups:from ‘silent suffering’to
‘making it work’. Social Science & Medicine 72,
763–772.
McDaid S. (2006) Equal and Inclusive User
Involvementin the MentalHealth Services in
Ireland: Results From Participatory Action
Research. University College Dublin and
SchizophreniaIreland, Dublin. Availableat:
http://www.ucd.ie/esc/html/shari_mcdaid.Pdf
(accessed 7 April 2013).
Meagher D.,O’Brien S.,Pullela A., et al.(2009)
Multidisciplinaryactivitiesin a community
mental health service: relationship to Health of
the Nation Outcome Scale scores and diagnosis.
Psychiatric Bulletin 33, 172–175.
Mental Health Act (2001), Dublin: the Houses of
the Oireachtas.
Mental Health Act (2007), London: the Houses of
Parliament.
Mental Health Commission (MHC) (2011) Your
Views of Mental Health Inpatient Services.
Mental Health Commission, Dublin.
Mental Health Commission (MHC) (Ireland)
(2008) A Framework for DevelopmentA
Recovery Approach Within theIrish Mental
Health Services.The Mental Health Commis-
sion, Dublin.
Mental Health Commission (MHC) (NZ) (1998)
Blueprintfor Mental Health Services in New
Zealand:How Things Need to Be. Mental
Health Commission, Wellington.
MgutshiniT. (2010)Risk factors for psychiatric
re-hospitalization: an exploration. International
Journal of Mental Health Nursing 19, 257–267.
Moher D., Liberati A., TetzlaffJ., et al.(2009)
Preferred reporting items for systematic reviews
and meta-analyses:the PRISMA statement.
Annals of Internal Medicine 151, 264–269.
Morphet J., Innes K., Munro I., et al. (2012) Man-
aging people with mentalhealth presentations
in emergency departments – a service explora-
tion of the issuessurrounding responsiveness
from a mentalhealth care consumer and carer
perspective.Australasian Emergency Nursing
Journal 15, 148–155.
National Collaborating Centre for Mental Health
(2012) Service User Experience in Adult Mental
Health. NICE Guidance on Improving the
Experienceof Care for People using Adult.
NHS Mental Health Services,London. Avail-
able at: http://www.nccmh.org.uk/downloads/
Patient%20experience/Service%20user%20
experience%20full%20guidance%20published
.pdf (accessed 13 June 2013).
National Service-UserExecutive(2009) Second
opinions, summary report of the NSUE survey
of memberson vision for change.Available
at: http://www.nsue.ie/m/uploads/files/Second
_Opinions_NSUE_2009.pdf(accessed 30 June
2013).
National Service-UserExecutive(2010) Second
opinions, summary report of the NSUE
survey of memberson vision for change.
Available at: http://www.nsue.ie/m/uploads/
files/Second_Opinions_2010_.pdf(accessed 30
June 2013).
National Service-UserExecutive(2011) Second
opinions, summary report of the NSUE survey
of members on vision for change. Available at:
http://www.nsue.ie/m/uploads/files/SO2011.pdf
(accessed 30 June 2013).
National Service-UserExecutive(2012) Second
opinions, summary report of the NSUE survey
of memberson vision for change.Available
at: http://www.nsue.ie/m/uploads/files/Survey
_Members_2012.pdf (accessed 30 June 2013).
Newell S.E., Harries P. & Ayers S. (2011) Boredom
proneness in a psychiatric inpatient population.
InternationalJournal of SocialPsychiatry 58,
488–495.
Nolan P.,Bradley E.& Brimblecombe N.(2011)
Disengaging from acuteinpatientpsychiatric
care: a description of service users’ experiences
and views.Journal of Psychiatric and Mental
Health Nursing 18, 359–367.
O’Regan C. & Ryan M. (2009) Patient satisfaction
with an emergencydepartmentpsychiatric
service.InternationalJournal of Health Care
Quality Assurance 22, 525–534.
Sainsbury Centre for Mental Health (2008)
Making Recovery a Reality.Sainsbury Centre
for Mental Health, London.
SIGN, Harbour R.T. & Forsyth L. (2008) SIGN
50: a Guideline Developer’s Handbook.
Scottish IntercollegiateGuidelinesNetwork,
Edinburgh.
Slade M. (2009)PersonalRecovery and Mental
Illness:a Guide for MentalHealth Profession-
als. University Press, Cambridge.
Slade M., Adams N. & O’Hagan M. (2012)
Recovery:past progress and future challenges.
International Review of Psychiatry 24, 1–4.
Storm M. & Davidson L. (2010) Inpatients’and
providers’ experiences with user involvement in
inpatient care.Psychiatric Quarterly 81,111–
125.
Sweeney A.,Rose D., ClementS., et al. (2012)
Understanding service user-defined continuity of
care and its relationship to health and social
measures: a cross-sectional study. BMC Health
Services Research 12, 145.
Swinton J. (2013) Beyond kindness:the place of
compassion in a forensic mental health setting.
Health and Social Care Chaplaincy 1, 11–21.
Tait L. & Lester H. (2005) Encouraging users
involvement in mental health services. Advances
in Psychiatric Treatment 11, 168–175.
Tanskanen S., Morant N., Hinton M., et al. (2011)
Service user and carer experiences ofseeking
help for a first episode of psychosis: a UK quali-
tative study. BMC Psychiatry 11, 157.
Taylor T.L.,Hawton K., Fortune S.,et al.(2009)
Attitudes towards clinical services among
people who self-harm:systematic review.The
British Journal of Psychiatry 194, 104–110.
Care Quality Commission (CQC) (2009) National
results tables: mental health inpatient
survey results 2009. Available at: http://
www.nhssurveys.org/survey/1038(accessed1
June 2013).
Care Quality Commission (CQC) (2011) Histori-
cal comparison tables: community mental
health survey results 2011. Available at: http://
www.nhssurveys.org/survey/1086(accessed1
June 2013).
Care Quality Commission (CQC) (2012) National
summaryof the resultsfor the community
mental health survey 2012. Available at: http://
www.nhssurveys.org/surveys/660(accessed1
June 2013).
The HealthcareCommission (2008) National
NHS patient survey programme.Survey of
Users of community mentalhealth services.
Available at: http://www.nhssurveys.org/survey/
1045 (accessed 1 June 2013).
Whittemore R. & Knafl K. (2005) The integrative
review: updated methodology.Journal of
Advanced Nursing 52, 546–553.
D Newman et al.
182 ©2015 John Wiley & Sons Ltd
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





