Nur720: Literature Review on Dementia Palliative Care Challenges
VerifiedAdded on 2022/08/30
|30
|6463
|26
Literature Review
AI Summary
This literature review examines the challenges in providing palliative care to individuals with dementia, particularly within residential care settings. The review highlights that patients with dementia often experience inadequate pain control and end-of-life care due to communication difficulties, under-recognition of pain, and challenges in prognosis. The review explores the barriers to effective pain management, including cognitive impairment and the inability to self-report pain. The author conducted a search of online databases such as CINAHL, Pub Med and Google Scholar and analyzed multiple research papers, including those from Corbett et al. (2016), Duncan et al. (2011), Husebo et al. (2012), and Sampson et al. (2015), to identify key issues and potential solutions. The review emphasizes the need for comprehensive and palliative care approaches and offers recommendations to improve patient outcomes. The study also focuses on the importance of effective communication, staff training, and the implementation of evidence-based pain management strategies to enhance the quality of life for dementia patients during their final stages of life.

Running head: LITERATURE REVIEW
LITERATURE REVIEW
Name of the student
Name of the university
Author’s name
LITERATURE REVIEW
Name of the student
Name of the university
Author’s name
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

LITERATURE REVIEW
Abstract:
In recent times, substantial progress has been made in developing end-of-life healthcare, but
individuals suffering from dementia still die with inadequate pain control, feed tubes in place
and hospice care. Individuals of neurological conditions like dementia are vulnerable classes of
people in which the discomfort is often under recognized, misunderstood and undertreated. A
major barrier to effective treatment is the failure to effectively express pain in moderate-severe
dementia, and several observational studies have shown that pain is being undertreated in
elderly people with cognitive issues. Neuropsychiatric dementia signs such as anxiety, assault
and mood disturbance, as well as issues with sleep have associated discomfort. Successful pain
management has been shown to be effective to mediate or relieve these effects. This review thus
focuses on exploring the barriers to pain management in these patients and also provides
recommendation to improve care and treatment plan for these patients and improve their overall
health outcome.
Abstract:
In recent times, substantial progress has been made in developing end-of-life healthcare, but
individuals suffering from dementia still die with inadequate pain control, feed tubes in place
and hospice care. Individuals of neurological conditions like dementia are vulnerable classes of
people in which the discomfort is often under recognized, misunderstood and undertreated. A
major barrier to effective treatment is the failure to effectively express pain in moderate-severe
dementia, and several observational studies have shown that pain is being undertreated in
elderly people with cognitive issues. Neuropsychiatric dementia signs such as anxiety, assault
and mood disturbance, as well as issues with sleep have associated discomfort. Successful pain
management has been shown to be effective to mediate or relieve these effects. This review thus
focuses on exploring the barriers to pain management in these patients and also provides
recommendation to improve care and treatment plan for these patients and improve their overall
health outcome.

LITERATURE REVIEW
Introduction:
Patient suffering from dementia are at a high risk of experiencing pain as they are unable
to express or communicate about their problems as a result of their cognitive impairment.
Therefore, this population group is more susceptible to pain because of their inability to self-
report. Their pain is often left undertreated and under assessed and therefore, for these patients, a
comprehensive and palliative care is needed by addressing and accessing their health concerns.
Studies show that self-reporting is an important factor to manage as well as assess the pain, and
incapacity to communicate is a significant barrier in effective pain management in older patients
with dementia. Dementia belongs to a group of diseases characterised with a gradual and
progressive and in certain cases an irreversible deterioration in mental functioning. It is mainly
characterised by a reduced cognitive abilities due to damage in the neurons in some areas of the
brain complemented by a deteriorated emotional control, motivation and social behaviour which
over time intensifies and increases. In Ireland, it has been reported that the prevalence of
dementia is exponentially increasing with age and are almost doubling every five years. Females
are found to be more prevalent to suffer fromdementia in their old age. It has been reported that
about 35 million people worldwide, are affected by dementia. The increasing rate of older people
suffering from dementia, pressurizes the healthcare providers and healthcare services to meet the
need for treatment and care for these people since pain management is a significant challenge in
patients with dementia.
Search strategy:
For conducting this literature review several online databases such as CINAHL, Pub Med
and Google Scholar were searched to find the appropriate articles relevant to the research area. A
Introduction:
Patient suffering from dementia are at a high risk of experiencing pain as they are unable
to express or communicate about their problems as a result of their cognitive impairment.
Therefore, this population group is more susceptible to pain because of their inability to self-
report. Their pain is often left undertreated and under assessed and therefore, for these patients, a
comprehensive and palliative care is needed by addressing and accessing their health concerns.
Studies show that self-reporting is an important factor to manage as well as assess the pain, and
incapacity to communicate is a significant barrier in effective pain management in older patients
with dementia. Dementia belongs to a group of diseases characterised with a gradual and
progressive and in certain cases an irreversible deterioration in mental functioning. It is mainly
characterised by a reduced cognitive abilities due to damage in the neurons in some areas of the
brain complemented by a deteriorated emotional control, motivation and social behaviour which
over time intensifies and increases. In Ireland, it has been reported that the prevalence of
dementia is exponentially increasing with age and are almost doubling every five years. Females
are found to be more prevalent to suffer fromdementia in their old age. It has been reported that
about 35 million people worldwide, are affected by dementia. The increasing rate of older people
suffering from dementia, pressurizes the healthcare providers and healthcare services to meet the
need for treatment and care for these people since pain management is a significant challenge in
patients with dementia.
Search strategy:
For conducting this literature review several online databases such as CINAHL, Pub Med
and Google Scholar were searched to find the appropriate articles relevant to the research area. A
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
LITERATURE REVIEW
total of 25 articles were found to be relevant to the topic, however, out of those 25 articles, only
10 articles were found to be matching with the inclusion criteria. All the papers which did not
have conclusive research findings and lack proper analysis and supporting studies were
excluded. The articles extracted or filtered based on the information they have which could be
accessed by skimming through the abstract of the articles. Each articles were analysed based on
the criteria of including and the articles that did not match the criteria were excluded from the
study. Certain keywords like “Dementia”, “Dementia and pain”, “Pain management in older
patients”, “Barriers to pain management in older dementia patients:’ “causes of pain in dementia
patients”, “Chronic pain in older patients with dementia”, “barriers to pain management”, “older
patients and dementia” were searched. The studies that were included in the review were
conducted from 2010-19 to get the current findings on this topic.
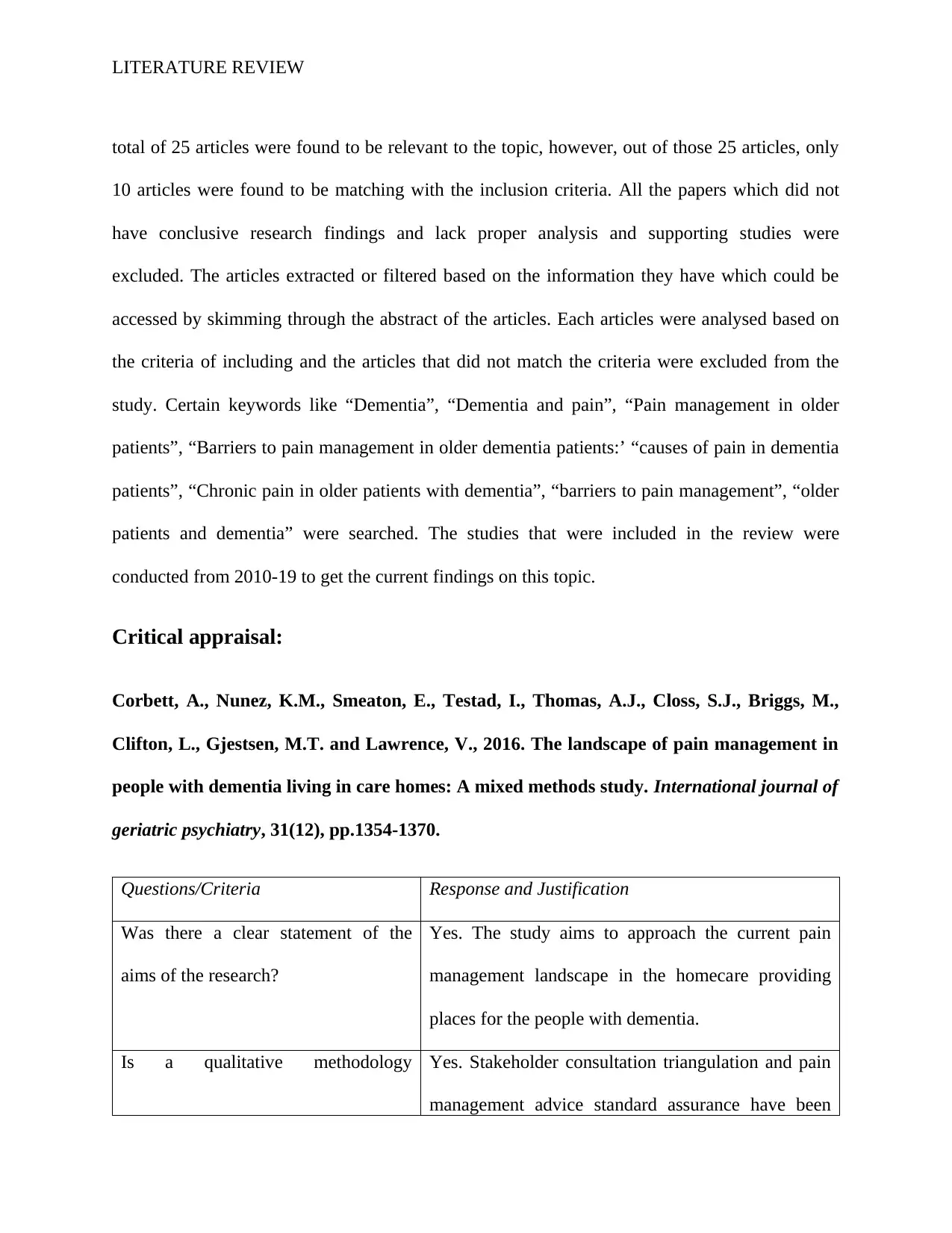
Critical appraisal:
Corbett, A., Nunez, K.M., Smeaton, E., Testad, I., Thomas, A.J., Closs, S.J., Briggs, M.,
Clifton, L., Gjestsen, M.T. and Lawrence, V., 2016. The landscape of pain management in
people with dementia living in care homes: A mixed methods study. International journal of
geriatric psychiatry, 31(12), pp.1354-1370.
Questions/Criteria Response and Justification
Was there a clear statement of the
aims of the research?
Yes. The study aims to approach the current pain
management landscape in the homecare providing
places for the people with dementia.
Is a qualitative methodology Yes. Stakeholder consultation triangulation and pain
management advice standard assurance have been
total of 25 articles were found to be relevant to the topic, however, out of those 25 articles, only
10 articles were found to be matching with the inclusion criteria. All the papers which did not
have conclusive research findings and lack proper analysis and supporting studies were
excluded. The articles extracted or filtered based on the information they have which could be
accessed by skimming through the abstract of the articles. Each articles were analysed based on
the criteria of including and the articles that did not match the criteria were excluded from the
study. Certain keywords like “Dementia”, “Dementia and pain”, “Pain management in older
patients”, “Barriers to pain management in older dementia patients:’ “causes of pain in dementia
patients”, “Chronic pain in older patients with dementia”, “barriers to pain management”, “older
patients and dementia” were searched. The studies that were included in the review were
conducted from 2010-19 to get the current findings on this topic.
Critical appraisal:
Corbett, A., Nunez, K.M., Smeaton, E., Testad, I., Thomas, A.J., Closs, S.J., Briggs, M.,
Clifton, L., Gjestsen, M.T. and Lawrence, V., 2016. The landscape of pain management in
people with dementia living in care homes: A mixed methods study. International journal of
geriatric psychiatry, 31(12), pp.1354-1370.
Questions/Criteria Response and Justification
Was there a clear statement of the
aims of the research?
Yes. The study aims to approach the current pain
management landscape in the homecare providing
places for the people with dementia.
Is a qualitative methodology Yes. Stakeholder consultation triangulation and pain
management advice standard assurance have been
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
LITERATURE REVIEW
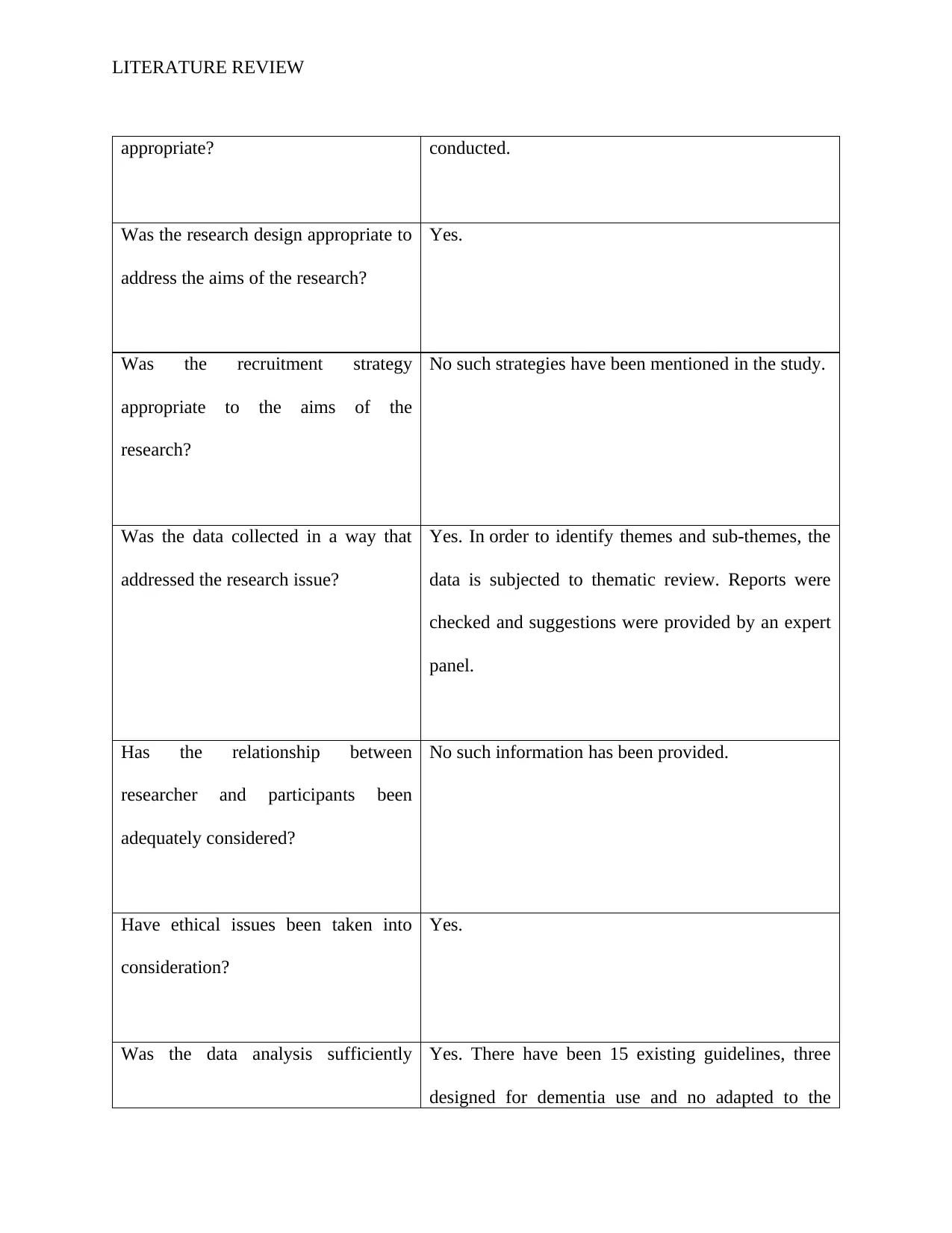
appropriate? conducted.
Was the research design appropriate to
address the aims of the research?
Yes.
Was the recruitment strategy
appropriate to the aims of the
research?
No such strategies have been mentioned in the study.
Was the data collected in a way that
addressed the research issue?
Yes. In order to identify themes and sub-themes, the
data is subjected to thematic review. Reports were
checked and suggestions were provided by an expert
panel.
Has the relationship between
researcher and participants been
adequately considered?
No such information has been provided.
Have ethical issues been taken into
consideration?
Yes.
Was the data analysis sufficiently Yes. There have been 15 existing guidelines, three
designed for dementia use and no adapted to the
appropriate? conducted.
Was the research design appropriate to
address the aims of the research?
Yes.
Was the recruitment strategy
appropriate to the aims of the
research?
No such strategies have been mentioned in the study.
Was the data collected in a way that
addressed the research issue?
Yes. In order to identify themes and sub-themes, the
data is subjected to thematic review. Reports were
checked and suggestions were provided by an expert
panel.
Has the relationship between
researcher and participants been
adequately considered?
No such information has been provided.
Have ethical issues been taken into
consideration?
Yes.
Was the data analysis sufficiently Yes. There have been 15 existing guidelines, three
designed for dementia use and no adapted to the
LITERATURE REVIEW
rigorous? home setting. Six main trends of pain management in
dementia were observed in the area of thematic
analysis: significance of personal centering, current
pain sensitivity of staff empathy as a central element,
difference of staffing accountability and confidence,
need for consistent treatment and the lack of training
for workers currently in progress. The expert panel
identified promising candidates for pharmacological
therapy in relation to the medical requirements that
require clinical evaluation.
Is there a clear statement of findings? Yes. The findings of this study clearly explain the
need for a pain management system based on
evidence for nursing homes that is centered on
stakeholder feedback and on a conceptual framework
for this purpose.
How valuable is the research? The aim of this study is to explore the present pain
management landscape in people living in health care
facilities with dementia. In this patient group, pain is
very common, but health professionals are guided by
very little.
rigorous? home setting. Six main trends of pain management in
dementia were observed in the area of thematic
analysis: significance of personal centering, current
pain sensitivity of staff empathy as a central element,
difference of staffing accountability and confidence,
need for consistent treatment and the lack of training
for workers currently in progress. The expert panel
identified promising candidates for pharmacological
therapy in relation to the medical requirements that
require clinical evaluation.
Is there a clear statement of findings? Yes. The findings of this study clearly explain the
need for a pain management system based on
evidence for nursing homes that is centered on
stakeholder feedback and on a conceptual framework
for this purpose.
How valuable is the research? The aim of this study is to explore the present pain
management landscape in people living in health care
facilities with dementia. In this patient group, pain is
very common, but health professionals are guided by
very little.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
LITERATURE REVIEW
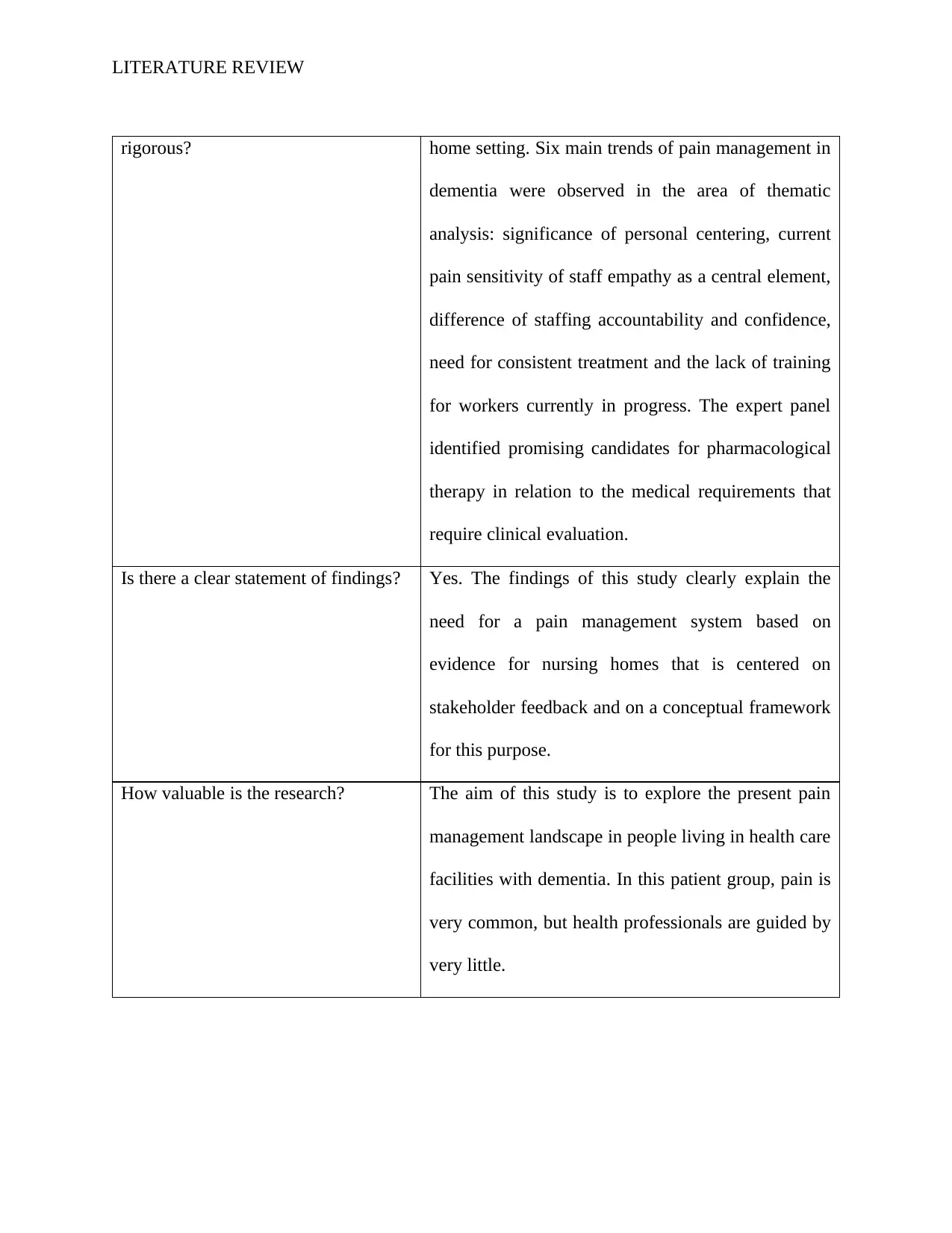
Duncan, R., Francis, R.M., Collerton, J., Davies, K., Jagger, C., Kingston, A., Kirkwood,
T., Robinson, L. and Birrell, F., 2011. Prevalence of arthritis and joint pain in the oldest
old: findings from the Newcastle 85+ study. Age and ageing, 40(6), pp.752-755.
Questions/Criteria Response and Justification
Did the study address a clearly
focused issue?
Yes. They present longitudinal findings from an unelected
sample of 1,029 individuals born in 1921 about the
incidence of arthritis and joint pain from the Newcastle 85
+ study.
Was the cohort recruited in an
acceptable way?
Yes.
Was the exposure accurately
measured to minimize bias?
No bias has been introduced in the study.
Was the outcome accurately
measured to minimise bias?
No bias has been introduced in the study.
Have the authors identified all
important confounding factors?
Yes. Using a single year of age cohort, a complete picture
of the health spectrum within this age group, unfounded by
age differences and secular trends, was obtained.
Duncan, R., Francis, R.M., Collerton, J., Davies, K., Jagger, C., Kingston, A., Kirkwood,
T., Robinson, L. and Birrell, F., 2011. Prevalence of arthritis and joint pain in the oldest
old: findings from the Newcastle 85+ study. Age and ageing, 40(6), pp.752-755.
Questions/Criteria Response and Justification
Did the study address a clearly
focused issue?
Yes. They present longitudinal findings from an unelected
sample of 1,029 individuals born in 1921 about the
incidence of arthritis and joint pain from the Newcastle 85
+ study.
Was the cohort recruited in an
acceptable way?
Yes.
Was the exposure accurately
measured to minimize bias?
No bias has been introduced in the study.
Was the outcome accurately
measured to minimise bias?
No bias has been introduced in the study.
Have the authors identified all
important confounding factors?
Yes. Using a single year of age cohort, a complete picture
of the health spectrum within this age group, unfounded by
age differences and secular trends, was obtained.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
LITERATURE REVIEW
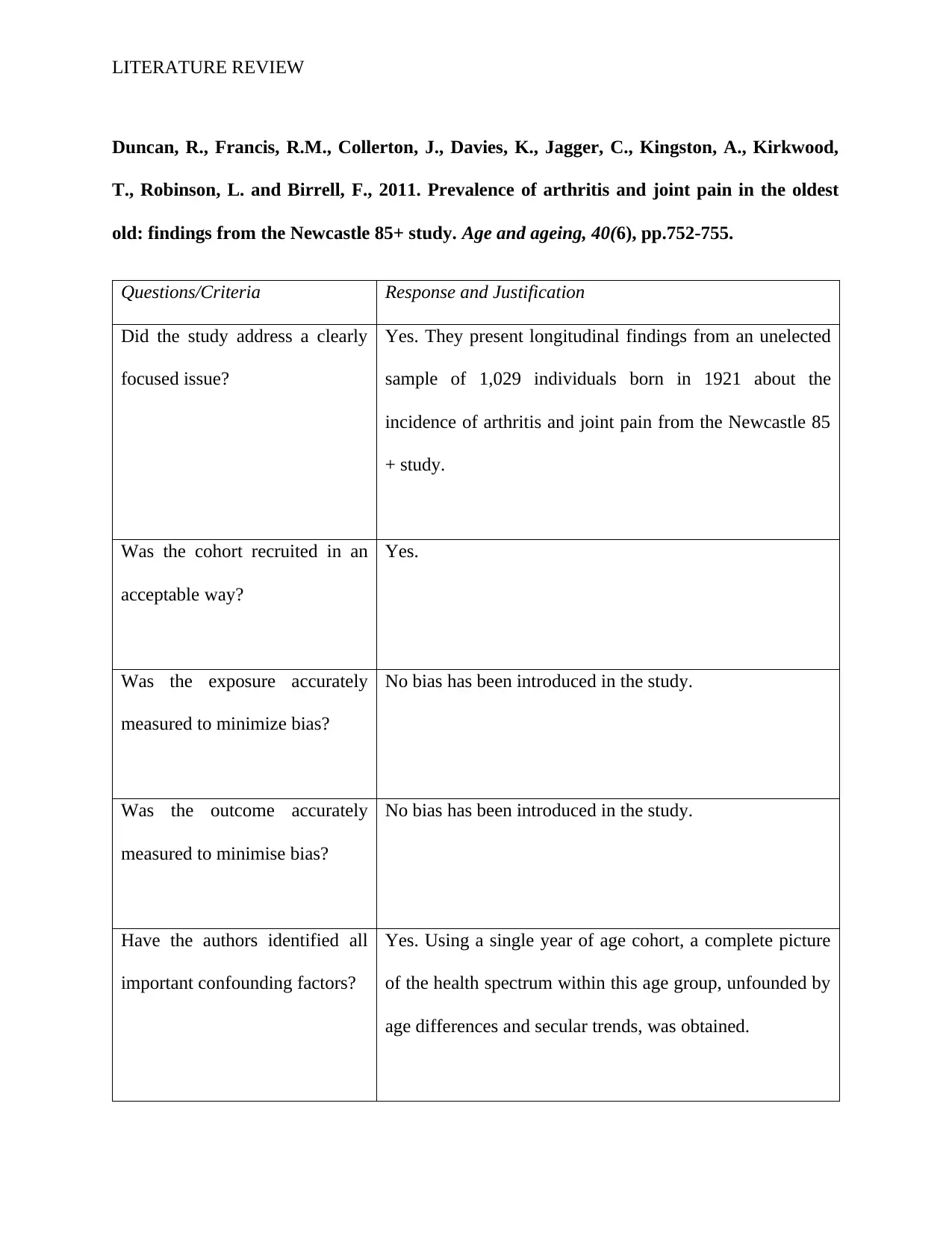
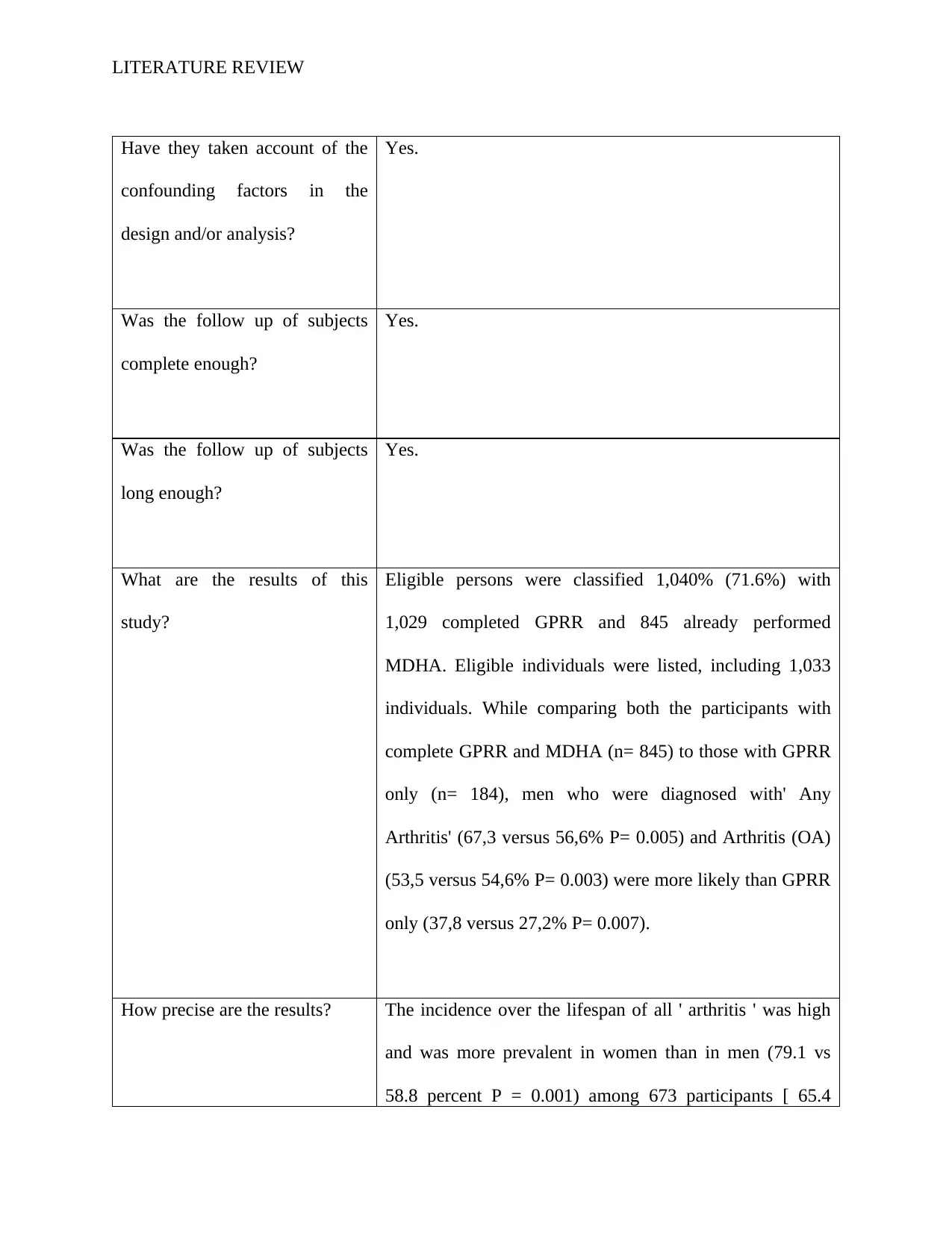
Have they taken account of the
confounding factors in the
design and/or analysis?
Yes.
Was the follow up of subjects
complete enough?
Yes.
Was the follow up of subjects
long enough?
Yes.
What are the results of this
study?
Eligible persons were classified 1,040% (71.6%) with
1,029 completed GPRR and 845 already performed
MDHA. Eligible individuals were listed, including 1,033
individuals. While comparing both the participants with
complete GPRR and MDHA (n= 845) to those with GPRR
only (n= 184), men who were diagnosed with' Any
Arthritis' (67,3 versus 56,6% P= 0.005) and Arthritis (OA)
(53,5 versus 54,6% P= 0.003) were more likely than GPRR
only (37,8 versus 27,2% P= 0.007).
How precise are the results? The incidence over the lifespan of all ' arthritis ' was high
and was more prevalent in women than in men (79.1 vs
58.8 percent P = 0.001) among 673 participants [ 65.4
Have they taken account of the
confounding factors in the
design and/or analysis?
Yes.
Was the follow up of subjects
complete enough?
Yes.
Was the follow up of subjects
long enough?
Yes.
What are the results of this
study?
Eligible persons were classified 1,040% (71.6%) with
1,029 completed GPRR and 845 already performed
MDHA. Eligible individuals were listed, including 1,033
individuals. While comparing both the participants with
complete GPRR and MDHA (n= 845) to those with GPRR
only (n= 184), men who were diagnosed with' Any
Arthritis' (67,3 versus 56,6% P= 0.005) and Arthritis (OA)
(53,5 versus 54,6% P= 0.003) were more likely than GPRR
only (37,8 versus 27,2% P= 0.007).
How precise are the results? The incidence over the lifespan of all ' arthritis ' was high
and was more prevalent in women than in men (79.1 vs
58.8 percent P = 0.001) among 673 participants [ 65.4
LITERATURE REVIEW
percent (95% CI: 62.5–68.3) ].
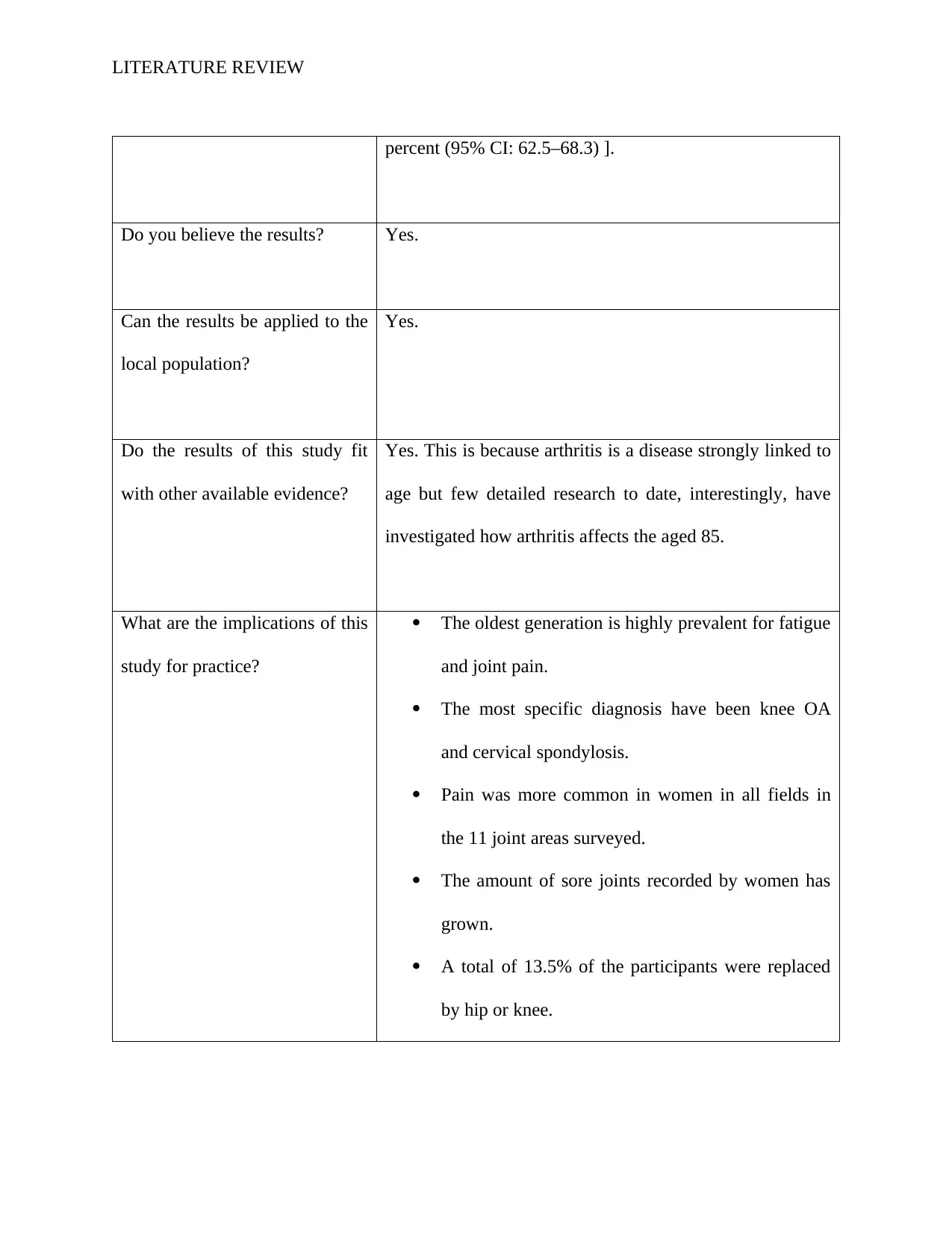
Do you believe the results? Yes.
Can the results be applied to the
local population?
Yes.
Do the results of this study fit
with other available evidence?
Yes. This is because arthritis is a disease strongly linked to
age but few detailed research to date, interestingly, have
investigated how arthritis affects the aged 85.
What are the implications of this
study for practice?
The oldest generation is highly prevalent for fatigue
and joint pain.
The most specific diagnosis have been knee OA
and cervical spondylosis.
Pain was more common in women in all fields in
the 11 joint areas surveyed.
The amount of sore joints recorded by women has
grown.
A total of 13.5% of the participants were replaced
by hip or knee.
percent (95% CI: 62.5–68.3) ].
Do you believe the results? Yes.
Can the results be applied to the
local population?
Yes.
Do the results of this study fit
with other available evidence?
Yes. This is because arthritis is a disease strongly linked to
age but few detailed research to date, interestingly, have
investigated how arthritis affects the aged 85.
What are the implications of this
study for practice?
The oldest generation is highly prevalent for fatigue
and joint pain.
The most specific diagnosis have been knee OA
and cervical spondylosis.
Pain was more common in women in all fields in
the 11 joint areas surveyed.
The amount of sore joints recorded by women has
grown.
A total of 13.5% of the participants were replaced
by hip or knee.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
LITERATURE REVIEW
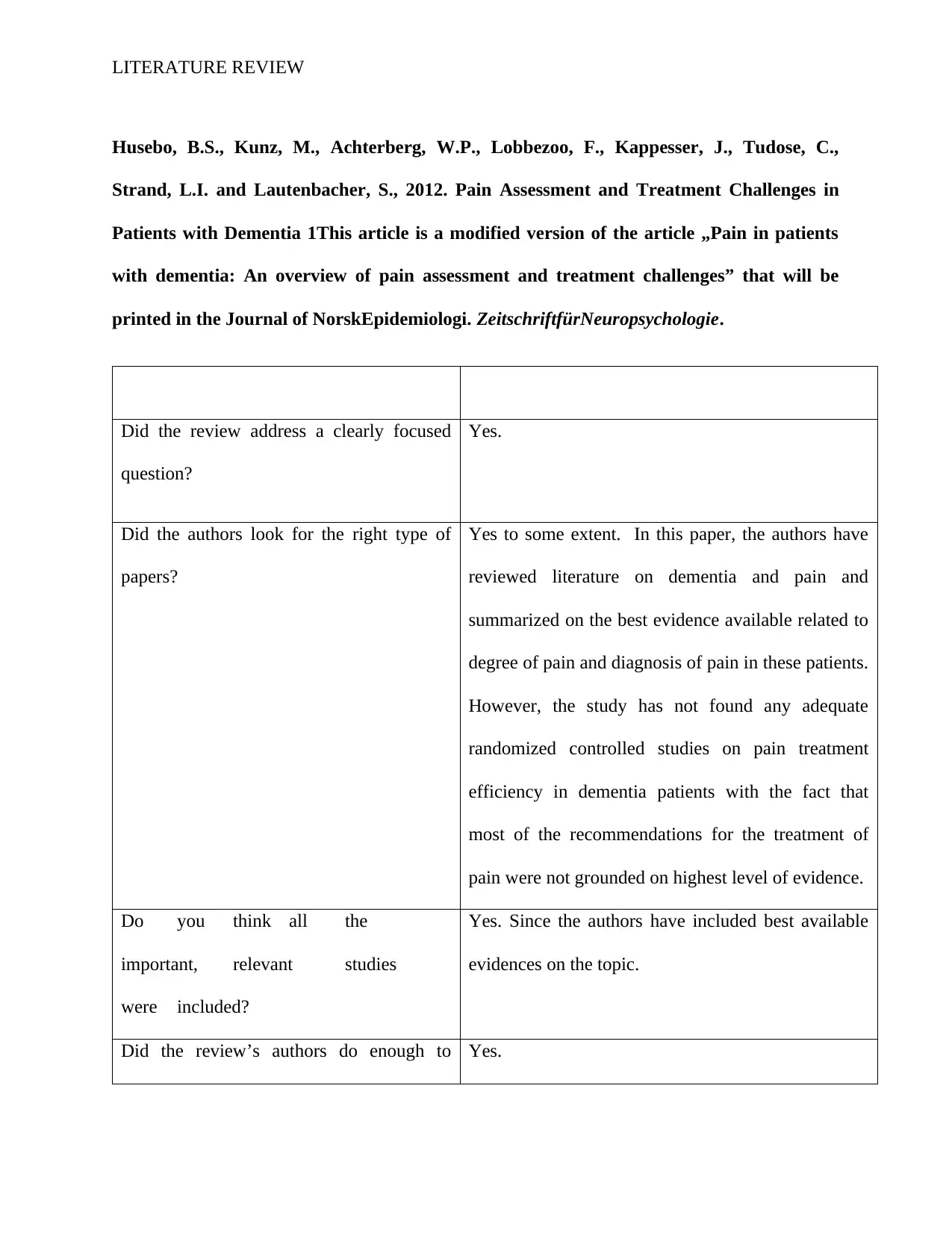
Husebo, B.S., Kunz, M., Achterberg, W.P., Lobbezoo, F., Kappesser, J., Tudose, C.,
Strand, L.I. and Lautenbacher, S., 2012. Pain Assessment and Treatment Challenges in
Patients with Dementia 1This article is a modified version of the article „Pain in patients
with dementia: An overview of pain assessment and treatment challenges” that will be
printed in the Journal of NorskEpidemiologi. ZeitschriftfürNeuropsychologie.
Did the review address a clearly focused
question?
Yes.
Did the authors look for the right type of
papers?
Yes to some extent. In this paper, the authors have
reviewed literature on dementia and pain and
summarized on the best evidence available related to
degree of pain and diagnosis of pain in these patients.
However, the study has not found any adequate
randomized controlled studies on pain treatment
efficiency in dementia patients with the fact that
most of the recommendations for the treatment of
pain were not grounded on highest level of evidence.
Do you think all the
important, relevant studies
were included?
Yes. Since the authors have included best available
evidences on the topic.
Did the review’s authors do enough to Yes.
Husebo, B.S., Kunz, M., Achterberg, W.P., Lobbezoo, F., Kappesser, J., Tudose, C.,
Strand, L.I. and Lautenbacher, S., 2012. Pain Assessment and Treatment Challenges in
Patients with Dementia 1This article is a modified version of the article „Pain in patients
with dementia: An overview of pain assessment and treatment challenges” that will be
printed in the Journal of NorskEpidemiologi. ZeitschriftfürNeuropsychologie.
Did the review address a clearly focused
question?
Yes.
Did the authors look for the right type of
papers?
Yes to some extent. In this paper, the authors have
reviewed literature on dementia and pain and
summarized on the best evidence available related to
degree of pain and diagnosis of pain in these patients.
However, the study has not found any adequate
randomized controlled studies on pain treatment
efficiency in dementia patients with the fact that
most of the recommendations for the treatment of
pain were not grounded on highest level of evidence.
Do you think all the
important, relevant studies
were included?
Yes. Since the authors have included best available
evidences on the topic.
Did the review’s authors do enough to Yes.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
LITERATURE REVIEW
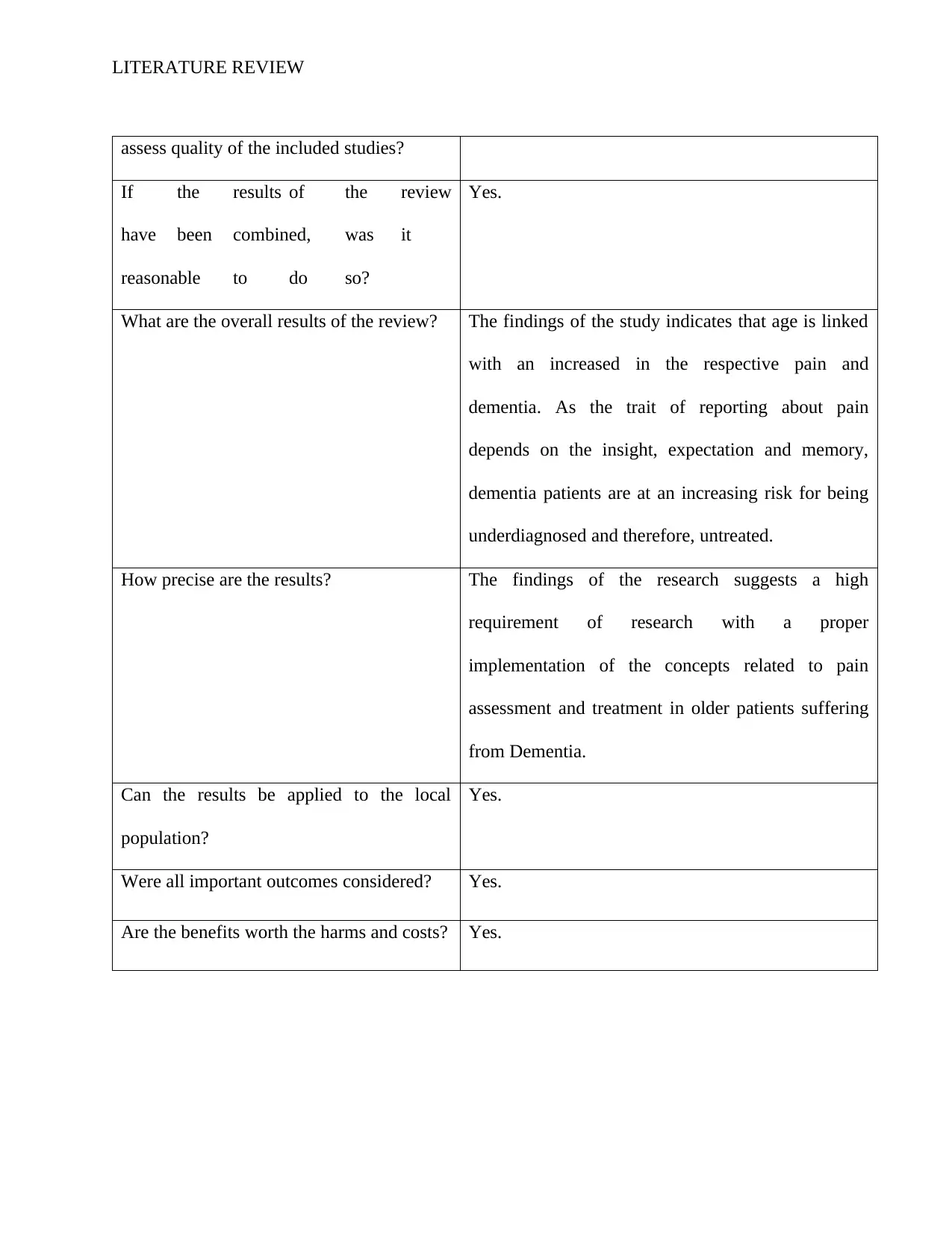
assess quality of the included studies?
If the results of the review
have been combined, was it
reasonable to do so?
Yes.
What are the overall results of the review? The findings of the study indicates that age is linked
with an increased in the respective pain and
dementia. As the trait of reporting about pain
depends on the insight, expectation and memory,
dementia patients are at an increasing risk for being
underdiagnosed and therefore, untreated.
How precise are the results? The findings of the research suggests a high
requirement of research with a proper
implementation of the concepts related to pain
assessment and treatment in older patients suffering
from Dementia.
Can the results be applied to the local
population?
Yes.
Were all important outcomes considered? Yes.
Are the benefits worth the harms and costs? Yes.
assess quality of the included studies?
If the results of the review
have been combined, was it
reasonable to do so?
Yes.
What are the overall results of the review? The findings of the study indicates that age is linked
with an increased in the respective pain and
dementia. As the trait of reporting about pain
depends on the insight, expectation and memory,
dementia patients are at an increasing risk for being
underdiagnosed and therefore, untreated.
How precise are the results? The findings of the research suggests a high
requirement of research with a proper
implementation of the concepts related to pain
assessment and treatment in older patients suffering
from Dementia.
Can the results be applied to the local
population?
Yes.
Were all important outcomes considered? Yes.
Are the benefits worth the harms and costs? Yes.
LITERATURE REVIEW
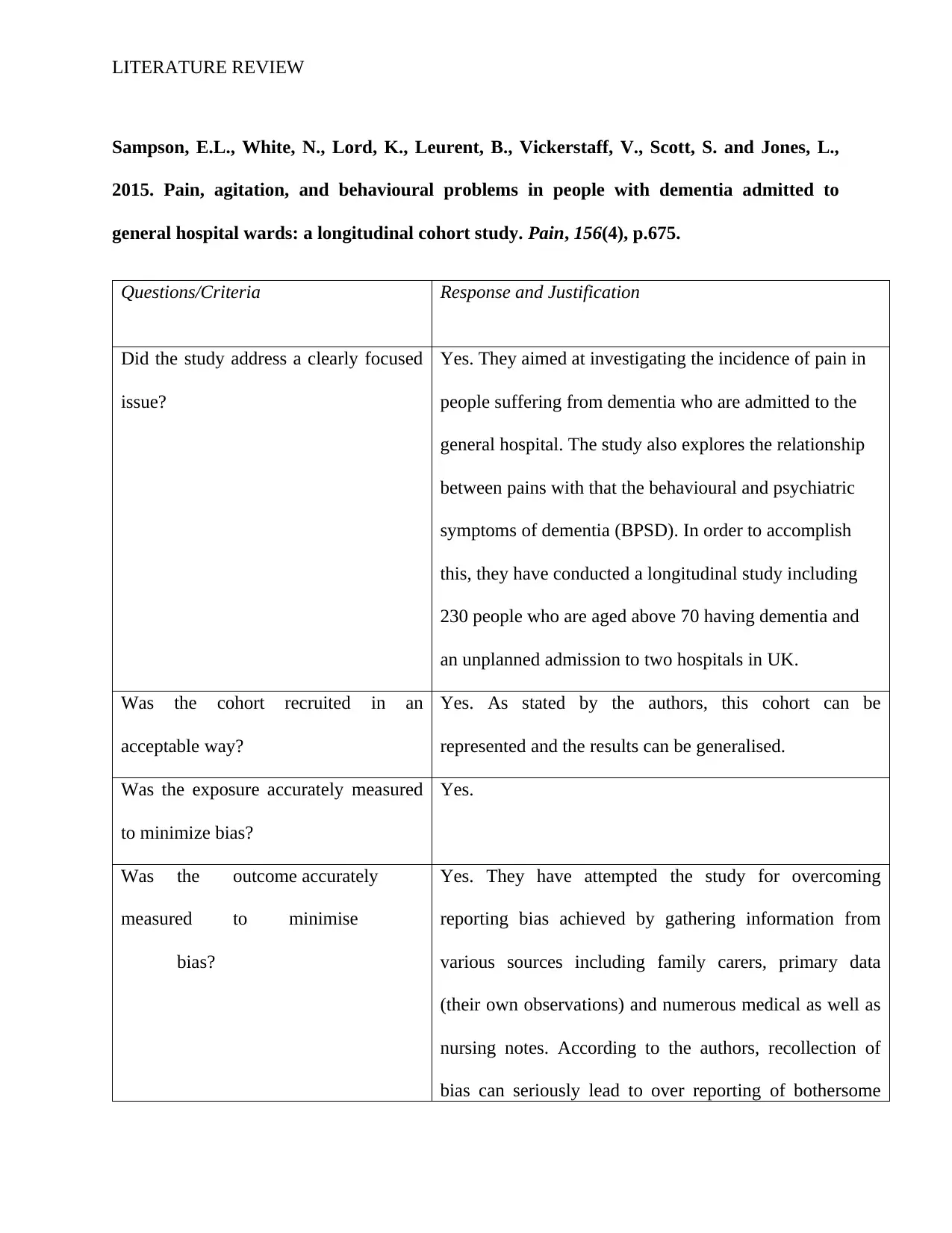
Sampson, E.L., White, N., Lord, K., Leurent, B., Vickerstaff, V., Scott, S. and Jones, L.,
2015. Pain, agitation, and behavioural problems in people with dementia admitted to
general hospital wards: a longitudinal cohort study. Pain, 156(4), p.675.
Questions/Criteria Response and Justification
Did the study address a clearly focused
issue?
Yes. They aimed at investigating the incidence of pain in
people suffering from dementia who are admitted to the
general hospital. The study also explores the relationship
between pains with that the behavioural and psychiatric
symptoms of dementia (BPSD). In order to accomplish
this, they have conducted a longitudinal study including
230 people who are aged above 70 having dementia and
an unplanned admission to two hospitals in UK.
Was the cohort recruited in an
acceptable way?
Yes. As stated by the authors, this cohort can be
represented and the results can be generalised.
Was the exposure accurately measured
to minimize bias?
Yes.
Was the outcome accurately
measured to minimise
bias?
Yes. They have attempted the study for overcoming
reporting bias achieved by gathering information from
various sources including family carers, primary data
(their own observations) and numerous medical as well as
nursing notes. According to the authors, recollection of
bias can seriously lead to over reporting of bothersome
Sampson, E.L., White, N., Lord, K., Leurent, B., Vickerstaff, V., Scott, S. and Jones, L.,
2015. Pain, agitation, and behavioural problems in people with dementia admitted to
general hospital wards: a longitudinal cohort study. Pain, 156(4), p.675.
Questions/Criteria Response and Justification
Did the study address a clearly focused
issue?
Yes. They aimed at investigating the incidence of pain in
people suffering from dementia who are admitted to the
general hospital. The study also explores the relationship
between pains with that the behavioural and psychiatric
symptoms of dementia (BPSD). In order to accomplish
this, they have conducted a longitudinal study including
230 people who are aged above 70 having dementia and
an unplanned admission to two hospitals in UK.
Was the cohort recruited in an
acceptable way?
Yes. As stated by the authors, this cohort can be
represented and the results can be generalised.
Was the exposure accurately measured
to minimize bias?
Yes.
Was the outcome accurately
measured to minimise
bias?
Yes. They have attempted the study for overcoming
reporting bias achieved by gathering information from
various sources including family carers, primary data
(their own observations) and numerous medical as well as
nursing notes. According to the authors, recollection of
bias can seriously lead to over reporting of bothersome
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 30
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





