Understanding Borderline Personality Disorder
VerifiedAdded on 2020/04/01
|13
|3263
|137
AI Summary
The assignment delves into the intricate nature of Borderline Personality Disorder (BPD), specifically examining its influence on emotional dysregulation. It analyzes research articles that shed light on various aspects of BPD, including cultural safety considerations within healthcare settings and the implementation of recovery-oriented mental health practices. Additionally, it investigates psychological treatment options for BPD and highlights the significance of therapeutic relationships in managing this complex disorder.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running Head: MANAGEMENT OF BIPOLAR PERSONALITY DISORDER (BPD)
Management of Bipolar Personality Disorder (BPD)
Name:
Institution and Affiliations:
Instructor:
Date:
Management of Bipolar Personality Disorder (BPD)
Name:
Institution and Affiliations:
Instructor:
Date:
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
MANAGEMENT OF BIPOLAR PERSONALITY DISORDER (BPD)
PART 1 Holistic assessment and planning
1.1 Introduction
Colleen is a 24 years old woman and mother of three from Mackay with a history of early
sexual assault, street life and trauma related to separation from her family 4 years of age. She has
been diagnosed with borderline personality disorder which she is under care for. She suffers
from chronic low self-esteem and a feeling of being unsafe. Her most dangerous symptoms
include self-mutilation and suicidal ideations. This presentation includes an assessment of the
patient’s mental status and a clinical formulation both of which inform decision making on
specific patient nursing plans. The nursing care plan targets the reduction of self-harm, assurance
of safety and encouraging development of self-esteem. These plans are in line with culturally
safe care principles of social justice, accountability, transparency and negotiated partnership. The
plan also incorporates the recovery philosophy principles which guide care provision. A clinic
handover description is also provided to ensure that other nurses other the one assigned to care
for the patients can assist her with necessary care when the earlier is not present.
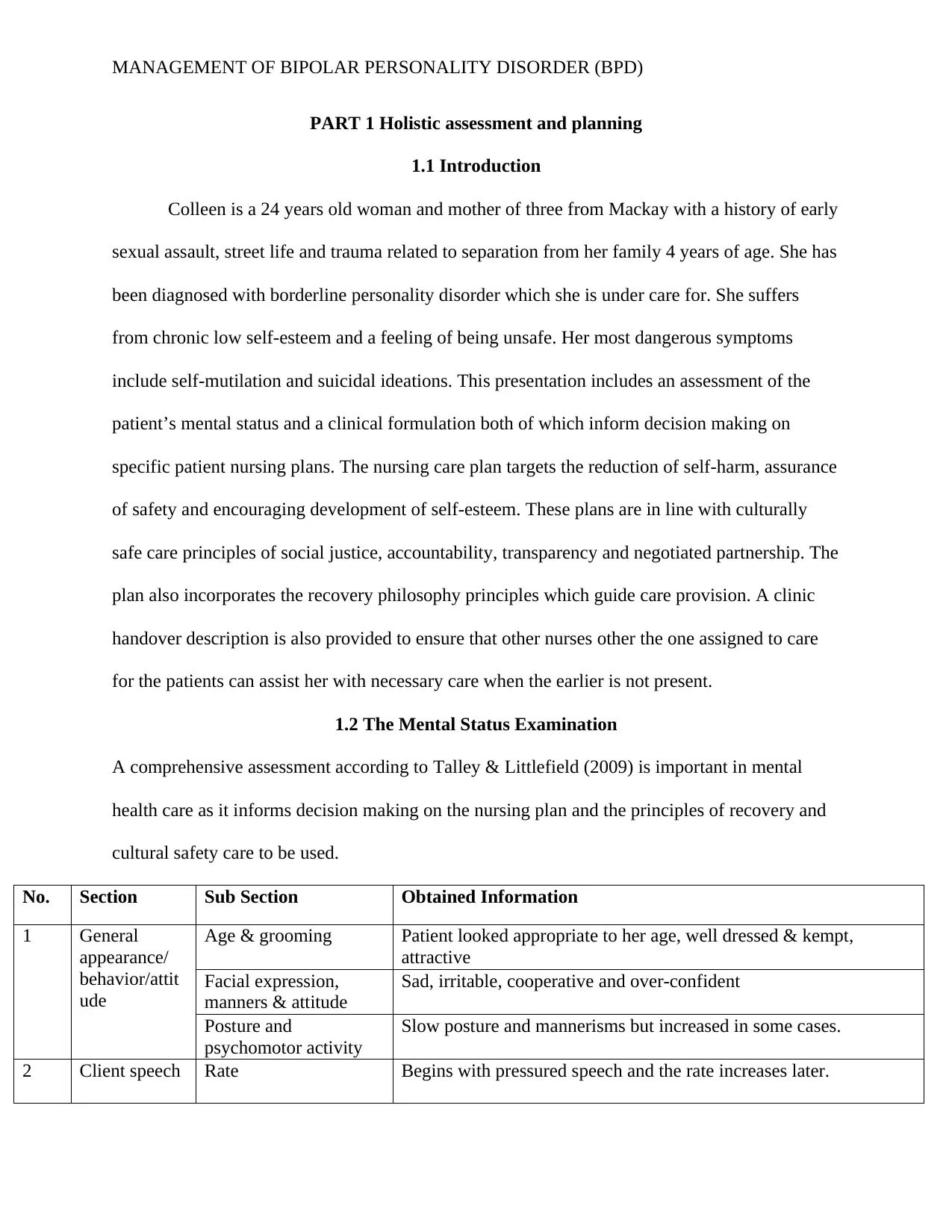
1.2 The Mental Status Examination
A comprehensive assessment according to Talley & Littlefield (2009) is important in mental
health care as it informs decision making on the nursing plan and the principles of recovery and
cultural safety care to be used.
No. Section Sub Section Obtained Information
1 General
appearance/
behavior/attit
ude
Age & grooming Patient looked appropriate to her age, well dressed & kempt,
attractive
Facial expression,
manners & attitude
Sad, irritable, cooperative and over-confident
Posture and
psychomotor activity
Slow posture and mannerisms but increased in some cases.
2 Client speech Rate Begins with pressured speech and the rate increases later.
PART 1 Holistic assessment and planning
1.1 Introduction
Colleen is a 24 years old woman and mother of three from Mackay with a history of early
sexual assault, street life and trauma related to separation from her family 4 years of age. She has
been diagnosed with borderline personality disorder which she is under care for. She suffers
from chronic low self-esteem and a feeling of being unsafe. Her most dangerous symptoms
include self-mutilation and suicidal ideations. This presentation includes an assessment of the
patient’s mental status and a clinical formulation both of which inform decision making on
specific patient nursing plans. The nursing care plan targets the reduction of self-harm, assurance
of safety and encouraging development of self-esteem. These plans are in line with culturally
safe care principles of social justice, accountability, transparency and negotiated partnership. The
plan also incorporates the recovery philosophy principles which guide care provision. A clinic
handover description is also provided to ensure that other nurses other the one assigned to care
for the patients can assist her with necessary care when the earlier is not present.
1.2 The Mental Status Examination
A comprehensive assessment according to Talley & Littlefield (2009) is important in mental
health care as it informs decision making on the nursing plan and the principles of recovery and
cultural safety care to be used.
No. Section Sub Section Obtained Information
1 General
appearance/
behavior/attit
ude
Age & grooming Patient looked appropriate to her age, well dressed & kempt,
attractive
Facial expression,
manners & attitude
Sad, irritable, cooperative and over-confident
Posture and
psychomotor activity
Slow posture and mannerisms but increased in some cases.
2 Client speech Rate Begins with pressured speech and the rate increases later.
MANAGEMENT OF BIPOLAR PERSONALITY DISORDER (BPD)
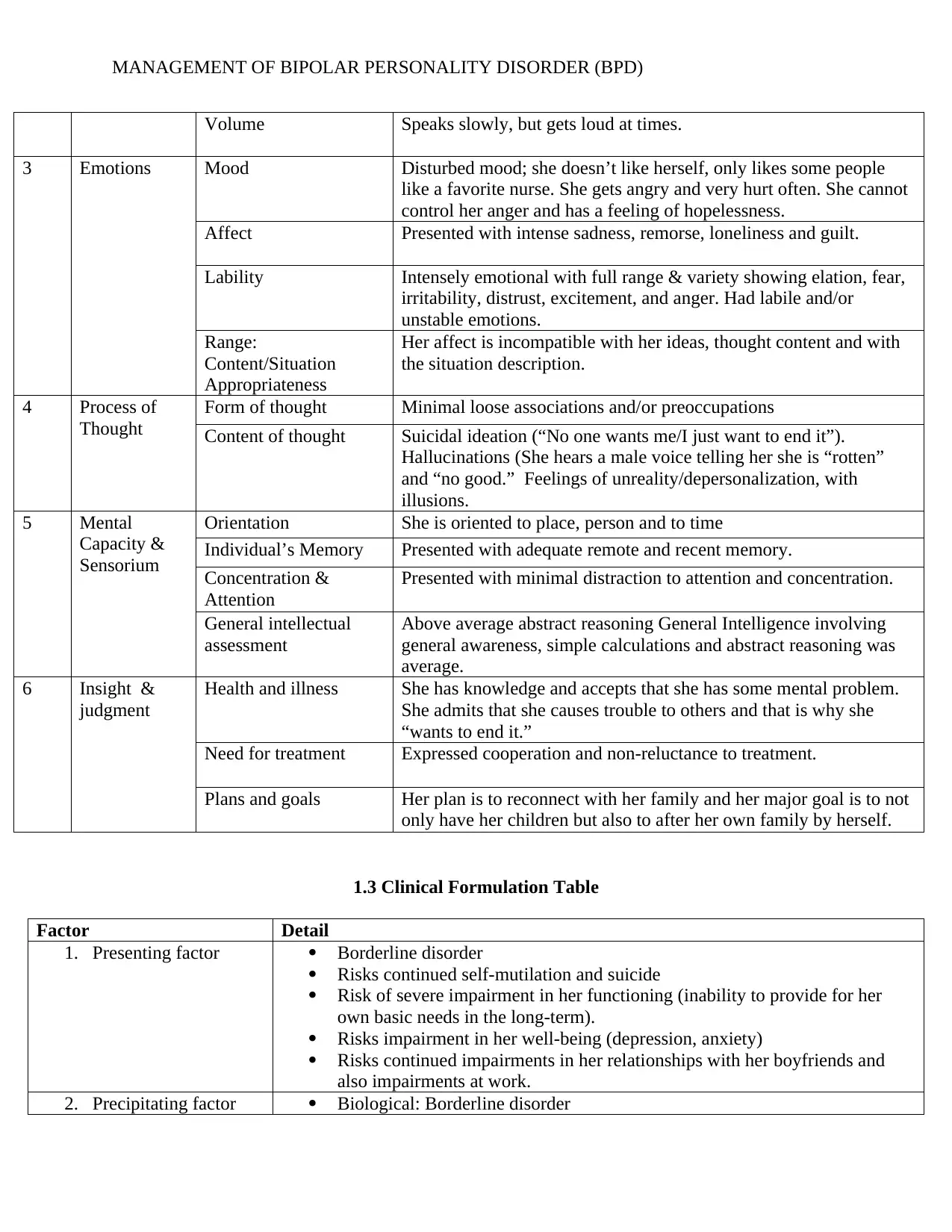
Volume Speaks slowly, but gets loud at times.
3 Emotions Mood Disturbed mood; she doesn’t like herself, only likes some people
like a favorite nurse. She gets angry and very hurt often. She cannot
control her anger and has a feeling of hopelessness.
Affect Presented with intense sadness, remorse, loneliness and guilt.
Lability Intensely emotional with full range & variety showing elation, fear,
irritability, distrust, excitement, and anger. Had labile and/or
unstable emotions.
Range:
Content/Situation
Appropriateness
Her affect is incompatible with her ideas, thought content and with
the situation description.
4 Process of
Thought
Form of thought Minimal loose associations and/or preoccupations
Content of thought Suicidal ideation (“No one wants me/I just want to end it”).
Hallucinations (She hears a male voice telling her she is “rotten”
and “no good.” Feelings of unreality/depersonalization, with
illusions.
5 Mental
Capacity &
Sensorium
Orientation She is oriented to place, person and to time
Individual’s Memory Presented with adequate remote and recent memory.
Concentration &
Attention
Presented with minimal distraction to attention and concentration.
General intellectual
assessment
Above average abstract reasoning General Intelligence involving
general awareness, simple calculations and abstract reasoning was
average.
6 Insight &
judgment
Health and illness She has knowledge and accepts that she has some mental problem.
She admits that she causes trouble to others and that is why she
“wants to end it.”
Need for treatment Expressed cooperation and non-reluctance to treatment.
Plans and goals Her plan is to reconnect with her family and her major goal is to not
only have her children but also to after her own family by herself.
1.3 Clinical Formulation Table
Factor Detail
1. Presenting factor Borderline disorder
Risks continued self-mutilation and suicide
Risk of severe impairment in her functioning (inability to provide for her
own basic needs in the long-term).
Risks impairment in her well-being (depression, anxiety)
Risks continued impairments in her relationships with her boyfriends and
also impairments at work.
2. Precipitating factor Biological: Borderline disorder
Volume Speaks slowly, but gets loud at times.
3 Emotions Mood Disturbed mood; she doesn’t like herself, only likes some people
like a favorite nurse. She gets angry and very hurt often. She cannot
control her anger and has a feeling of hopelessness.
Affect Presented with intense sadness, remorse, loneliness and guilt.
Lability Intensely emotional with full range & variety showing elation, fear,
irritability, distrust, excitement, and anger. Had labile and/or
unstable emotions.
Range:
Content/Situation
Appropriateness
Her affect is incompatible with her ideas, thought content and with
the situation description.
4 Process of
Thought
Form of thought Minimal loose associations and/or preoccupations
Content of thought Suicidal ideation (“No one wants me/I just want to end it”).
Hallucinations (She hears a male voice telling her she is “rotten”
and “no good.” Feelings of unreality/depersonalization, with
illusions.
5 Mental
Capacity &
Sensorium
Orientation She is oriented to place, person and to time
Individual’s Memory Presented with adequate remote and recent memory.
Concentration &
Attention
Presented with minimal distraction to attention and concentration.
General intellectual
assessment
Above average abstract reasoning General Intelligence involving
general awareness, simple calculations and abstract reasoning was
average.
6 Insight &
judgment
Health and illness She has knowledge and accepts that she has some mental problem.
She admits that she causes trouble to others and that is why she
“wants to end it.”
Need for treatment Expressed cooperation and non-reluctance to treatment.
Plans and goals Her plan is to reconnect with her family and her major goal is to not
only have her children but also to after her own family by herself.
1.3 Clinical Formulation Table
Factor Detail
1. Presenting factor Borderline disorder
Risks continued self-mutilation and suicide
Risk of severe impairment in her functioning (inability to provide for her
own basic needs in the long-term).
Risks impairment in her well-being (depression, anxiety)
Risks continued impairments in her relationships with her boyfriends and
also impairments at work.
2. Precipitating factor Biological: Borderline disorder
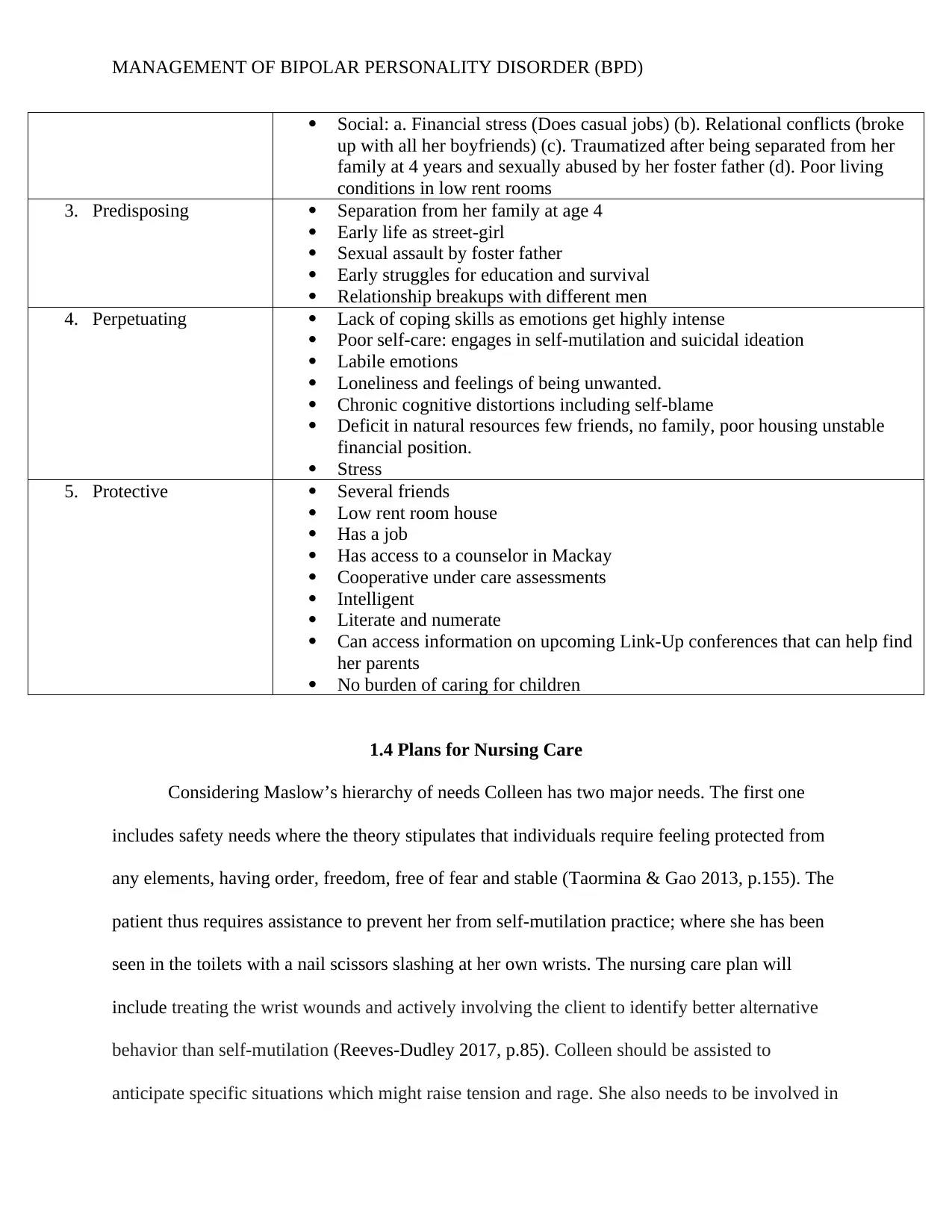
MANAGEMENT OF BIPOLAR PERSONALITY DISORDER (BPD)
Social: a. Financial stress (Does casual jobs) (b). Relational conflicts (broke
up with all her boyfriends) (c). Traumatized after being separated from her
family at 4 years and sexually abused by her foster father (d). Poor living
conditions in low rent rooms
3. Predisposing Separation from her family at age 4
Early life as street-girl
Sexual assault by foster father
Early struggles for education and survival
Relationship breakups with different men
4. Perpetuating Lack of coping skills as emotions get highly intense
Poor self-care: engages in self-mutilation and suicidal ideation
Labile emotions
Loneliness and feelings of being unwanted.
Chronic cognitive distortions including self-blame
Deficit in natural resources few friends, no family, poor housing unstable
financial position.
Stress
5. Protective Several friends
Low rent room house
Has a job
Has access to a counselor in Mackay
Cooperative under care assessments
Intelligent
Literate and numerate
Can access information on upcoming Link-Up conferences that can help find
her parents
No burden of caring for children
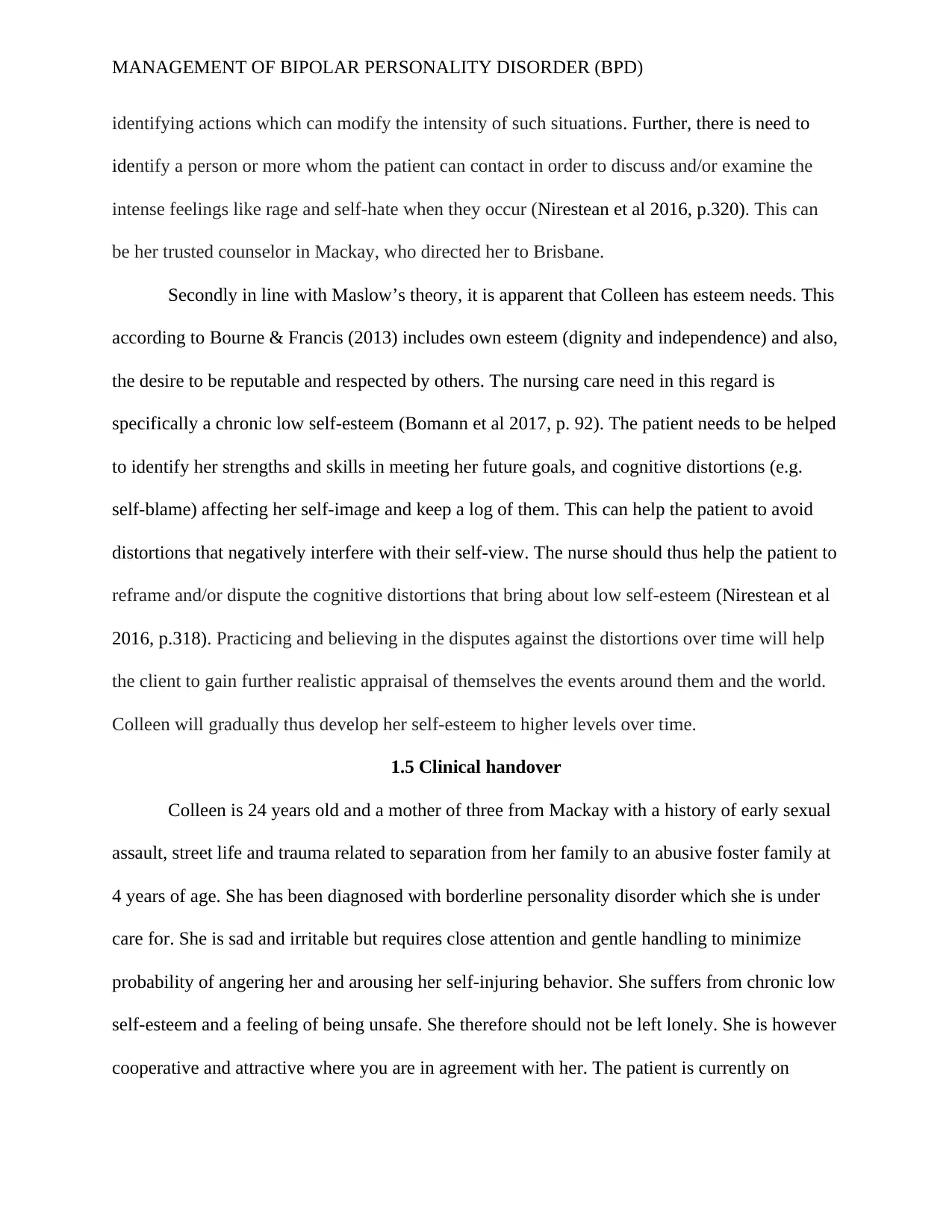
1.4 Plans for Nursing Care
Considering Maslow’s hierarchy of needs Colleen has two major needs. The first one
includes safety needs where the theory stipulates that individuals require feeling protected from
any elements, having order, freedom, free of fear and stable (Taormina & Gao 2013, p.155). The
patient thus requires assistance to prevent her from self-mutilation practice; where she has been
seen in the toilets with a nail scissors slashing at her own wrists. The nursing care plan will
include treating the wrist wounds and actively involving the client to identify better alternative
behavior than self-mutilation (Reeves-Dudley 2017, p.85). Colleen should be assisted to
anticipate specific situations which might raise tension and rage. She also needs to be involved in
Social: a. Financial stress (Does casual jobs) (b). Relational conflicts (broke
up with all her boyfriends) (c). Traumatized after being separated from her
family at 4 years and sexually abused by her foster father (d). Poor living
conditions in low rent rooms
3. Predisposing Separation from her family at age 4
Early life as street-girl
Sexual assault by foster father
Early struggles for education and survival
Relationship breakups with different men
4. Perpetuating Lack of coping skills as emotions get highly intense
Poor self-care: engages in self-mutilation and suicidal ideation
Labile emotions
Loneliness and feelings of being unwanted.
Chronic cognitive distortions including self-blame
Deficit in natural resources few friends, no family, poor housing unstable
financial position.
Stress
5. Protective Several friends
Low rent room house
Has a job
Has access to a counselor in Mackay
Cooperative under care assessments
Intelligent
Literate and numerate
Can access information on upcoming Link-Up conferences that can help find
her parents
No burden of caring for children
1.4 Plans for Nursing Care
Considering Maslow’s hierarchy of needs Colleen has two major needs. The first one
includes safety needs where the theory stipulates that individuals require feeling protected from
any elements, having order, freedom, free of fear and stable (Taormina & Gao 2013, p.155). The
patient thus requires assistance to prevent her from self-mutilation practice; where she has been
seen in the toilets with a nail scissors slashing at her own wrists. The nursing care plan will
include treating the wrist wounds and actively involving the client to identify better alternative
behavior than self-mutilation (Reeves-Dudley 2017, p.85). Colleen should be assisted to
anticipate specific situations which might raise tension and rage. She also needs to be involved in
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
MANAGEMENT OF BIPOLAR PERSONALITY DISORDER (BPD)
identifying actions which can modify the intensity of such situations. Further, there is need to
identify a person or more whom the patient can contact in order to discuss and/or examine the
intense feelings like rage and self-hate when they occur (Nirestean et al 2016, p.320). This can
be her trusted counselor in Mackay, who directed her to Brisbane.
Secondly in line with Maslow’s theory, it is apparent that Colleen has esteem needs. This
according to Bourne & Francis (2013) includes own esteem (dignity and independence) and also,
the desire to be reputable and respected by others. The nursing care need in this regard is
specifically a chronic low self-esteem (Bomann et al 2017, p. 92). The patient needs to be helped
to identify her strengths and skills in meeting her future goals, and cognitive distortions (e.g.
self-blame) affecting her self-image and keep a log of them. This can help the patient to avoid
distortions that negatively interfere with their self-view. The nurse should thus help the patient to
reframe and/or dispute the cognitive distortions that bring about low self-esteem (Nirestean et al
2016, p.318). Practicing and believing in the disputes against the distortions over time will help
the client to gain further realistic appraisal of themselves the events around them and the world.
Colleen will gradually thus develop her self-esteem to higher levels over time.
1.5 Clinical handover
Colleen is 24 years old and a mother of three from Mackay with a history of early sexual
assault, street life and trauma related to separation from her family to an abusive foster family at
4 years of age. She has been diagnosed with borderline personality disorder which she is under
care for. She is sad and irritable but requires close attention and gentle handling to minimize
probability of angering her and arousing her self-injuring behavior. She suffers from chronic low
self-esteem and a feeling of being unsafe. She therefore should not be left lonely. She is however
cooperative and attractive where you are in agreement with her. The patient is currently on
identifying actions which can modify the intensity of such situations. Further, there is need to
identify a person or more whom the patient can contact in order to discuss and/or examine the
intense feelings like rage and self-hate when they occur (Nirestean et al 2016, p.320). This can
be her trusted counselor in Mackay, who directed her to Brisbane.
Secondly in line with Maslow’s theory, it is apparent that Colleen has esteem needs. This
according to Bourne & Francis (2013) includes own esteem (dignity and independence) and also,
the desire to be reputable and respected by others. The nursing care need in this regard is
specifically a chronic low self-esteem (Bomann et al 2017, p. 92). The patient needs to be helped
to identify her strengths and skills in meeting her future goals, and cognitive distortions (e.g.
self-blame) affecting her self-image and keep a log of them. This can help the patient to avoid
distortions that negatively interfere with their self-view. The nurse should thus help the patient to
reframe and/or dispute the cognitive distortions that bring about low self-esteem (Nirestean et al
2016, p.318). Practicing and believing in the disputes against the distortions over time will help
the client to gain further realistic appraisal of themselves the events around them and the world.
Colleen will gradually thus develop her self-esteem to higher levels over time.
1.5 Clinical handover
Colleen is 24 years old and a mother of three from Mackay with a history of early sexual
assault, street life and trauma related to separation from her family to an abusive foster family at
4 years of age. She has been diagnosed with borderline personality disorder which she is under
care for. She is sad and irritable but requires close attention and gentle handling to minimize
probability of angering her and arousing her self-injuring behavior. She suffers from chronic low
self-esteem and a feeling of being unsafe. She therefore should not be left lonely. She is however
cooperative and attractive where you are in agreement with her. The patient is currently on
MANAGEMENT OF BIPOLAR PERSONALITY DISORDER (BPD)
dialectical behavior therapy to enable her minimize cognitive distortions that hinder her
motivation to be positive and appraise herself for her strengths. Any nurse handling her requires
establishing a well-thought out therapeutic relationship based on cultural safe care principles.
dialectical behavior therapy to enable her minimize cognitive distortions that hinder her
motivation to be positive and appraise herself for her strengths. Any nurse handling her requires
establishing a well-thought out therapeutic relationship based on cultural safe care principles.
MANAGEMENT OF BIPOLAR PERSONALITY DISORDER (BPD)
PART 2: Therapeutic Engagement & Clinical Interpretation
2.1 The Therapeutic Relationship
A therapeutic relationship will be created by first the nursing orientating herself with the
client to establish a trust-creating rapport (Wright, 2011, p.360). The nurse will encourage
Colleen to identify her problems and also be a collaborative partner to help herself. This is
followed by clarification of perceptions, setting of goals together, working to achieve goals one
by one, and the full resolution of the client’s problem (Klatkiewicz 2015, p. 24). Establishing a
therapeutic relationship is important in caring for patients with BPD. In this particular case, a
therapeutic relationship is important first, in order to create trust between the nurse and Colleen.
It is clear that she trusts her counselor in Mackay and this trust should also be created first in
order to explore her cognitive distortions that need to be changed. Secondly a therapeutic
relationship will help the patient to collaborate with the nurse in identifying her perceptions of
life and setting the goals of the intended therapy (Wright 2011, p. 360). Colleen is evidently
choosy and has favorite nurses. It is important that one of these favorite nurses be chosen to carry
out this process. Further, a therapeutic relationship will make the patient be committed to
psychotherapy process and the created relationship with the nurse. She will be able to participate
in own self-help, take responsibility and show some kind of independence (Kleindienst et al
2014, p.2). One appropriate strategy in creating a therapeutic relationship with Colleen as applied
in the nursing care interventions above include the use of dialectical behavior therapy. In this
regard, the nurse should ask the client (Colleen) to openly agree that she has dysfunctional
thoughts, behaviors and/or emotions right before starting her on active therapeutic change
process (Abdelhamid Gado 2016, p.48). The patient’s admission of this dysfunctional
functioning helps in reducing any perceived difficulty of the process of self-change. It will also
PART 2: Therapeutic Engagement & Clinical Interpretation
2.1 The Therapeutic Relationship
A therapeutic relationship will be created by first the nursing orientating herself with the
client to establish a trust-creating rapport (Wright, 2011, p.360). The nurse will encourage
Colleen to identify her problems and also be a collaborative partner to help herself. This is
followed by clarification of perceptions, setting of goals together, working to achieve goals one
by one, and the full resolution of the client’s problem (Klatkiewicz 2015, p. 24). Establishing a
therapeutic relationship is important in caring for patients with BPD. In this particular case, a
therapeutic relationship is important first, in order to create trust between the nurse and Colleen.
It is clear that she trusts her counselor in Mackay and this trust should also be created first in
order to explore her cognitive distortions that need to be changed. Secondly a therapeutic
relationship will help the patient to collaborate with the nurse in identifying her perceptions of
life and setting the goals of the intended therapy (Wright 2011, p. 360). Colleen is evidently
choosy and has favorite nurses. It is important that one of these favorite nurses be chosen to carry
out this process. Further, a therapeutic relationship will make the patient be committed to
psychotherapy process and the created relationship with the nurse. She will be able to participate
in own self-help, take responsibility and show some kind of independence (Kleindienst et al
2014, p.2). One appropriate strategy in creating a therapeutic relationship with Colleen as applied
in the nursing care interventions above include the use of dialectical behavior therapy. In this
regard, the nurse should ask the client (Colleen) to openly agree that she has dysfunctional
thoughts, behaviors and/or emotions right before starting her on active therapeutic change
process (Abdelhamid Gado 2016, p.48). The patient’s admission of this dysfunctional
functioning helps in reducing any perceived difficulty of the process of self-change. It will also
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
MANAGEMENT OF BIPOLAR PERSONALITY DISORDER (BPD)
reduce the frequency of self-mutilation behavior, minimization of suicidal thoughts, enhance
basic motivation to pursue positive change, and boost the ability to function appropriately while
under high-stress situations.
2.2 Cultural Safety
The first step to provide the patient with culturally safe care is to establish a negotiated
partnership which is paramount in developing a therapeutic relationship (Downing et al 2011,
p.247). Establishing a good rapport with the patient represents respect for her rights and
appreciation for her role in participating in her own care. One issue which might present while
working with Colleen includes her divided identity as one of the victims of the stolen generation.
Having lived with her foster family until she was 17 and her life on the streets is likely to have
drifted her concept of culture. It is likely that Colleen will prefer any care approach and not
necessarily be handled as an Aboriginal and/or Torres Strait Islander.
Several principles of culturally safe care were applied in designing and implementing the
nursing plan. The first one included the emphasis on negotiated partnership (Laverty et al 2017,
p.15). Negotiated partnership was essential in establishing a therapeutic relationship with
Colleen in that the patient willingly participates in her own care. Secondly, the nursing plan
incorporated transparency as a cultural safety principle (Downing et al 2011, p.251). This
ensures that care options are transparent and meant to help the patient to appropriately resume
normalcy and minimize extreme response to situations that aggravate her moods. A further
principle incorporated in the nursing plan includes the special emphasis on social and restorative
justice (Laverty et al 2017, p.16). Helping the patient to cope with stressors in her life, find
alternatives to cognitive distortions and to appreciate her strengths are all intended to restore her
reduce the frequency of self-mutilation behavior, minimization of suicidal thoughts, enhance
basic motivation to pursue positive change, and boost the ability to function appropriately while
under high-stress situations.
2.2 Cultural Safety
The first step to provide the patient with culturally safe care is to establish a negotiated
partnership which is paramount in developing a therapeutic relationship (Downing et al 2011,
p.247). Establishing a good rapport with the patient represents respect for her rights and
appreciation for her role in participating in her own care. One issue which might present while
working with Colleen includes her divided identity as one of the victims of the stolen generation.
Having lived with her foster family until she was 17 and her life on the streets is likely to have
drifted her concept of culture. It is likely that Colleen will prefer any care approach and not
necessarily be handled as an Aboriginal and/or Torres Strait Islander.
Several principles of culturally safe care were applied in designing and implementing the
nursing plan. The first one included the emphasis on negotiated partnership (Laverty et al 2017,
p.15). Negotiated partnership was essential in establishing a therapeutic relationship with
Colleen in that the patient willingly participates in her own care. Secondly, the nursing plan
incorporated transparency as a cultural safety principle (Downing et al 2011, p.251). This
ensures that care options are transparent and meant to help the patient to appropriately resume
normalcy and minimize extreme response to situations that aggravate her moods. A further
principle incorporated in the nursing plan includes the special emphasis on social and restorative
justice (Laverty et al 2017, p.16). Helping the patient to cope with stressors in her life, find
alternatives to cognitive distortions and to appreciate her strengths are all intended to restore her
MANAGEMENT OF BIPOLAR PERSONALITY DISORDER (BPD)
social self. The strategy will boost her interaction with people positively in the social sphere,
which is a natural psychotherapy approach.
2.3 Recovery-oriented Nursing Care
Among the principles of the recovery philosophy used in the nursing care plan includes
first, the need for dignity and respect (Vourakis 2016, p.64). The nursing plan for Colleen’s BPD
involves approaches that are respectful, honest and courteous to ensure in nature. The plan does
not indicate any discrimination of the patient and/or stigma which might hinder learning
behavioral changes. The second recovery principle includes the need for partnership and proper
communication (Parker et al 2017, p.87). The nursing plan involves a close sharing of
information between the nurse and the patient. In this regard, the plan acknowledges that the
patient is an expert on her own life and further that there is need for partnership to achieve
recovery. The nursing plan allows the patient to be part of his own care goal setting and follow-
up on change in order to speed up recovery (Vourakis 2016, p.64). Thirdly, the recovery
principle which focuses on individual attitudes and rights has been incorporated in the nursing
plan. The strategies in the plan can instill hope in the patient’s future and her ability to have a
meaningful life ahead. The principle stipulates that recovery oriented strategies in mental health
include listening keenly, learning from and/or on communications from the patient and the
therapist (McKenna 2017, p.90). This helps both parties to prioritize the most important issues to
each one of them. Another recovery philosophy principle entitled “Real choices” emphasizes that
recovery includes supporting the patient to build on her strengths and to take responsibility for
her life at any time. The nursing plan includes this principle as it emphasizes on helping the
patient to use her abilities to minimize stressors in life. The precipitating factors to BPD
including emotional complications can be resolved once the patient has resolved to use her
social self. The strategy will boost her interaction with people positively in the social sphere,
which is a natural psychotherapy approach.
2.3 Recovery-oriented Nursing Care
Among the principles of the recovery philosophy used in the nursing care plan includes
first, the need for dignity and respect (Vourakis 2016, p.64). The nursing plan for Colleen’s BPD
involves approaches that are respectful, honest and courteous to ensure in nature. The plan does
not indicate any discrimination of the patient and/or stigma which might hinder learning
behavioral changes. The second recovery principle includes the need for partnership and proper
communication (Parker et al 2017, p.87). The nursing plan involves a close sharing of
information between the nurse and the patient. In this regard, the plan acknowledges that the
patient is an expert on her own life and further that there is need for partnership to achieve
recovery. The nursing plan allows the patient to be part of his own care goal setting and follow-
up on change in order to speed up recovery (Vourakis 2016, p.64). Thirdly, the recovery
principle which focuses on individual attitudes and rights has been incorporated in the nursing
plan. The strategies in the plan can instill hope in the patient’s future and her ability to have a
meaningful life ahead. The principle stipulates that recovery oriented strategies in mental health
include listening keenly, learning from and/or on communications from the patient and the
therapist (McKenna 2017, p.90). This helps both parties to prioritize the most important issues to
each one of them. Another recovery philosophy principle entitled “Real choices” emphasizes that
recovery includes supporting the patient to build on her strengths and to take responsibility for
her life at any time. The nursing plan includes this principle as it emphasizes on helping the
patient to use her abilities to minimize stressors in life. The precipitating factors to BPD
including emotional complications can be resolved once the patient has resolved to use her

MANAGEMENT OF BIPOLAR PERSONALITY DISORDER (BPD)
abilities for countering stressing situations. Further, recovery for mental health problems should
involve recognition that interventions are not mainly meant to bring about cure. Instead as
implied in the nursing plan recovery will involve the patient being able to live a meaningful,
satisfactory, and purposeful life including being valued community member (Parker et al 2017,
p.88). The plan also in line with the last principle ensures that the patient remains at the center of
her care. She thus plays a major role in ensuring that her psychotherapy goals and plans are
achieved as agreed upon with the nurse.
abilities for countering stressing situations. Further, recovery for mental health problems should
involve recognition that interventions are not mainly meant to bring about cure. Instead as
implied in the nursing plan recovery will involve the patient being able to live a meaningful,
satisfactory, and purposeful life including being valued community member (Parker et al 2017,
p.88). The plan also in line with the last principle ensures that the patient remains at the center of
her care. She thus plays a major role in ensuring that her psychotherapy goals and plans are
achieved as agreed upon with the nurse.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
MANAGEMENT OF BIPOLAR PERSONALITY DISORDER (BPD)
References
Abdelhamid Gado, G. (2016). The Effectiveness of Dialectical Behavior Therapy on Reducing
Symptoms of Borderline Personality Disorder: Case Study. International Journal Of Social
Science And Humanity, 6(1), 47-51. http://dx.doi.org/10.7763/ijssh.2016.v6.616
Bomann, A., Jørgensen, M., Bo, S., Nielsen, M., Gede, L., Elfving, B., & Simonsen, E. (2017).
The neurobiology of social deficits in female patients with borderline personality disorder:
The importance of oxytocin. Personality And Mental Health, 11(2), 91-100.
http://dx.doi.org/10.1002/pmh.1369
Borderline personality disorder: management. (2014). Clinical Pharmacist.
http://dx.doi.org/10.1211/cp.2014.20066443
Bourne, P., & Francis, C. (2013). Wellbeing and correlates of wellbeing: Using Maslow's 5
Needs Hierarchy to evaluate wellbeing. Journal Of Behavioral Health, 2(3), 269.
http://dx.doi.org/10.5455/jbh.20130202125320
Downing, R., Kowal, E., & Paradies, Y. (2011). Indigenous cultural training for health workers
in Australia. International Journal For Quality In Health Care, 23(3), 247-257.
http://dx.doi.org/10.1093/intqhc/mzr008
Klatkiewicz, A. (2015). Therapeutic relationship in the therapy of patients with borderline
personality disorder. Psychoterapia, 173(2), 23-32. http://dx.doi.org/10.12740/pt/43653
Kleindienst, N., Priebe, K., Borgmann, E., Cornelisse, S., Krüger, A., Ebner-Priemer, U., &
Dyer, A. (2014). Body self-evaluation and physical scars in patients with borderline
personality disorder: an observational study. Borderline Personality Disorder And Emotion
Dysregulation, 1(1), 2. http://dx.doi.org/10.1186/2051-6673-1-2
References
Abdelhamid Gado, G. (2016). The Effectiveness of Dialectical Behavior Therapy on Reducing
Symptoms of Borderline Personality Disorder: Case Study. International Journal Of Social
Science And Humanity, 6(1), 47-51. http://dx.doi.org/10.7763/ijssh.2016.v6.616
Bomann, A., Jørgensen, M., Bo, S., Nielsen, M., Gede, L., Elfving, B., & Simonsen, E. (2017).
The neurobiology of social deficits in female patients with borderline personality disorder:
The importance of oxytocin. Personality And Mental Health, 11(2), 91-100.
http://dx.doi.org/10.1002/pmh.1369
Borderline personality disorder: management. (2014). Clinical Pharmacist.
http://dx.doi.org/10.1211/cp.2014.20066443
Bourne, P., & Francis, C. (2013). Wellbeing and correlates of wellbeing: Using Maslow's 5
Needs Hierarchy to evaluate wellbeing. Journal Of Behavioral Health, 2(3), 269.
http://dx.doi.org/10.5455/jbh.20130202125320
Downing, R., Kowal, E., & Paradies, Y. (2011). Indigenous cultural training for health workers
in Australia. International Journal For Quality In Health Care, 23(3), 247-257.
http://dx.doi.org/10.1093/intqhc/mzr008
Klatkiewicz, A. (2015). Therapeutic relationship in the therapy of patients with borderline
personality disorder. Psychoterapia, 173(2), 23-32. http://dx.doi.org/10.12740/pt/43653
Kleindienst, N., Priebe, K., Borgmann, E., Cornelisse, S., Krüger, A., Ebner-Priemer, U., &
Dyer, A. (2014). Body self-evaluation and physical scars in patients with borderline
personality disorder: an observational study. Borderline Personality Disorder And Emotion
Dysregulation, 1(1), 2. http://dx.doi.org/10.1186/2051-6673-1-2
MANAGEMENT OF BIPOLAR PERSONALITY DISORDER (BPD)
Laverty, M., McDermott, D., & Calma, T. (2017). Embedding cultural safety in Australia's main
health care standards. The Medical Journal Of Australia, 207(1), 15-16.
http://dx.doi.org/10.5694/mja17.00328
McKenna, B. (2017). Further Reflections on Recovery-Oriented Mental Health Practice in a
Community Care Unit. Journal Of Forensic Nursing, 13(2), 89-90.
http://dx.doi.org/10.1097/jfn.0000000000000149
Nirestean, T., Lukacs, E., Nirestean, A., & Gabos Grecu, I. (2016). Dependent personality
features in a complex case of borderline personality disorder. Personality And Mental
Health, 10(4), 317-322. http://dx.doi.org/10.1002/pmh.1360
Parker, S., Siskind, D., & Meurk, C. (2017). Further Reflections on Recovery-Oriented Mental
Health Practice in a Community Care Unit. Journal Of Forensic Nursing, 13(2), 87-88.
http://dx.doi.org/10.1097/jfn.0000000000000150
Reeves-Dudley, B. (2017). Borderline Personality Disorder Psychological Treatment: An
Integrative Review. Archives Of Psychiatric Nursing, 31(1), 83-87.
http://dx.doi.org/10.1016/j.apnu.2016.08.009
Talley, B., & Littlefield, J. (2009). Efficiently teaching mental status examination to medical
students. Medical Education, 43(11), 1100-1101. http://dx.doi.org/10.1111/j.1365-
2923.2009.03494.x
Taormina, & Gao. (2013). Maslow and the Motivation Hierarchy: Measuring Satisfaction of the
Needs. The American Journal Of Psychology, 126(2), 155.
http://dx.doi.org/10.5406/amerjpsyc.126.2.0155
Laverty, M., McDermott, D., & Calma, T. (2017). Embedding cultural safety in Australia's main
health care standards. The Medical Journal Of Australia, 207(1), 15-16.
http://dx.doi.org/10.5694/mja17.00328
McKenna, B. (2017). Further Reflections on Recovery-Oriented Mental Health Practice in a
Community Care Unit. Journal Of Forensic Nursing, 13(2), 89-90.
http://dx.doi.org/10.1097/jfn.0000000000000149
Nirestean, T., Lukacs, E., Nirestean, A., & Gabos Grecu, I. (2016). Dependent personality
features in a complex case of borderline personality disorder. Personality And Mental
Health, 10(4), 317-322. http://dx.doi.org/10.1002/pmh.1360
Parker, S., Siskind, D., & Meurk, C. (2017). Further Reflections on Recovery-Oriented Mental
Health Practice in a Community Care Unit. Journal Of Forensic Nursing, 13(2), 87-88.
http://dx.doi.org/10.1097/jfn.0000000000000150
Reeves-Dudley, B. (2017). Borderline Personality Disorder Psychological Treatment: An
Integrative Review. Archives Of Psychiatric Nursing, 31(1), 83-87.
http://dx.doi.org/10.1016/j.apnu.2016.08.009
Talley, B., & Littlefield, J. (2009). Efficiently teaching mental status examination to medical
students. Medical Education, 43(11), 1100-1101. http://dx.doi.org/10.1111/j.1365-
2923.2009.03494.x
Taormina, & Gao. (2013). Maslow and the Motivation Hierarchy: Measuring Satisfaction of the
Needs. The American Journal Of Psychology, 126(2), 155.
http://dx.doi.org/10.5406/amerjpsyc.126.2.0155
MANAGEMENT OF BIPOLAR PERSONALITY DISORDER (BPD)
Vourakis, C. (2016). Recovery Oriented Systems of Care (ROSC) and Recovery
Management. Journal Of Addictions Nursing, 27(2), 63-64.
http://dx.doi.org/10.1097/jan.0000000000000129
Wright, L. (2011). The Therapeutic Relationship and Borderline Personality
Disorder. International Journal Of Therapy And Rehabilitation, 18(7), 360-361.
http://dx.doi.org/10.12968/ijtr.2011.18.7.360
Vourakis, C. (2016). Recovery Oriented Systems of Care (ROSC) and Recovery
Management. Journal Of Addictions Nursing, 27(2), 63-64.
http://dx.doi.org/10.1097/jan.0000000000000129
Wright, L. (2011). The Therapeutic Relationship and Borderline Personality
Disorder. International Journal Of Therapy And Rehabilitation, 18(7), 360-361.
http://dx.doi.org/10.12968/ijtr.2011.18.7.360
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





