Management of Raised Intracranial Pressure: PICU Protocols, AIIMS
VerifiedAdded on 2023/05/23
|8
|5719
|482
Report
AI Summary
This report, originating from the Indian Journal of Pediatrics, details the management of raised intracranial pressure (ICP) in a Pediatric Intensive Care Unit (PICU) setting, based on protocols established at the All India Institute of Medical Sciences (AIIMS). It begins with an overview of ICP dynamics, including the Monroe-Kellie hypothesis and the importance of cerebral perfusion pressure (CPP). The report outlines causes of raised ICP, the initial assessment procedures, including neurological and neuroimaging evaluations, and the role of invasive ICP monitoring. Key management strategies discussed encompass airway, breathing, and circulatory support (ABCs), positioning, hyperventilation, and osmotherapy with mannitol. The report also covers the avoidance of aggravating factors and the consideration of advanced interventions like barbiturate coma, hypothermia, and decompressive craniectomy for refractory intracranial hypertension. It emphasizes the need for prompt treatment, the importance of identifying underlying causes, and the use of specific medications and interventions to reduce ICP and improve patient outcomes.
SYMPOSIUM ON PICU PROTOCOLS OF AIIMS
Management of Raised Intracranial Pressure
Naveen Sankhyan&K. N. Vykunta Raju&
Suvasini Sharma&Sheffali Gulati
Received: 3 August 2010 / Accepted: 18 August 2010 / Published online: 7 September 2010
# Dr.K C Chaudhuri Foundation 2010
AbstractAppropriate managementof raised intracranial
pressurebeginswith stabilizationof the patientand
simultaneous assessment of the level of sensorium and the
causeof raisedintracranialpressure.Stabilizationis
initiated with securing the airway,ventilation and circula-
tory function.The identification ofsurgically remediable
conditions is a priority. Emergent use of external ventricular
drain orventriculo-peritonealshuntmay be lifesaving in
selected patients.In children with severe coma,signs of
herniation oracutely elevated intracranialpressure,treat-
mentshould bestartedprior to imagingor invasive
monitoring. Emergent use of hyperventilation and mannitol
are life saving in such situations.Medicalmanagement
involves careful use of head elevation, osmotic agents, and
avoiding hypotonic fluids.Appropriate care also includes
avoidance of aggravating factors. For refractory intracranial
hypertension,barbiturate coma,hypothermia,or decom-
pressive craniectomy should be considered.
Keywords Coma. Critically ill child. Intracranial
hypertension. Traumatic brain injury
Introduction
Raised intracranialpressure (ICP) is a common neurolog-
ical complication in critically ill children. The cause may be
either an increase in brain volume,cerebralblood flow,or
cerebrospinalfluid (CSF) volume.Despite itshigh inci-
dence,there are few systematically evaluated treatments o
intracranialhypertension.Mostmanagementrecommenda-
tions are based on clinical experience and research done i
patients with traumatic brain injury.
Intracranial Pressure: Normal Values
Intracranialpressure isthe totalpressure exerted by the
brain, blood and CSF in the intracranial vault. The Monroe-
Kellie hypothesis states the sum of the intracranial volume
of brain (≈80%), blood(≈10%), and CSF(≈10%) is constan
and thatan increase in any one of these mustbe offset by
an equal decrease in another, or else pressure increases. T
ICP varies with age and normative values for children are
not well established.Normalvaluesare lessthan 10 to
15 mm Hg for adults and older children, 3 to 7 mm Hg for
young children,and 1.5 to 6 mm Hg for term infants [1].
ICP values greater than 20 to 25 mm Hg require treatmen
in most circumstances. Sustained ICP values of greater tha
40 mm Hg indicatesevere,life-threatening intracranial
hypertension [2].
Cerebral Pressure Dynamics
Cerebralperfusion pressure (CPP)is a majorfactorthat
affects cerebral blood flow to the brain.CPP measurement
is expressed in millimeters of mercury and is determined b
measuring the difference between the mean arterial press
(MAP) and ICP (CPP = MAP – ICP).It is apparentfrom
the formula that,CPP can reduce as a resultof reduced
MAP or raised ICP,or a combination ofthese two.CPP
N. Sankhyan:K. N. Vykunta Raju:S. Sharma:S. Gulati (*)
Child Neurology Division,Department of Pediatrics,All India
Institute of Medical Sciences,
New Delhi 110029,India
e-mail: sheffaligulati@gmail.com
Indian J Pediatr (2010) 77:1409–1416
DOI 10.1007/s12098-010-0190-2
Management of Raised Intracranial Pressure
Naveen Sankhyan&K. N. Vykunta Raju&
Suvasini Sharma&Sheffali Gulati
Received: 3 August 2010 / Accepted: 18 August 2010 / Published online: 7 September 2010
# Dr.K C Chaudhuri Foundation 2010
AbstractAppropriate managementof raised intracranial
pressurebeginswith stabilizationof the patientand
simultaneous assessment of the level of sensorium and the
causeof raisedintracranialpressure.Stabilizationis
initiated with securing the airway,ventilation and circula-
tory function.The identification ofsurgically remediable
conditions is a priority. Emergent use of external ventricular
drain orventriculo-peritonealshuntmay be lifesaving in
selected patients.In children with severe coma,signs of
herniation oracutely elevated intracranialpressure,treat-
mentshould bestartedprior to imagingor invasive
monitoring. Emergent use of hyperventilation and mannitol
are life saving in such situations.Medicalmanagement
involves careful use of head elevation, osmotic agents, and
avoiding hypotonic fluids.Appropriate care also includes
avoidance of aggravating factors. For refractory intracranial
hypertension,barbiturate coma,hypothermia,or decom-
pressive craniectomy should be considered.
Keywords Coma. Critically ill child. Intracranial
hypertension. Traumatic brain injury
Introduction
Raised intracranialpressure (ICP) is a common neurolog-
ical complication in critically ill children. The cause may be
either an increase in brain volume,cerebralblood flow,or
cerebrospinalfluid (CSF) volume.Despite itshigh inci-
dence,there are few systematically evaluated treatments o
intracranialhypertension.Mostmanagementrecommenda-
tions are based on clinical experience and research done i
patients with traumatic brain injury.
Intracranial Pressure: Normal Values
Intracranialpressure isthe totalpressure exerted by the
brain, blood and CSF in the intracranial vault. The Monroe-
Kellie hypothesis states the sum of the intracranial volume
of brain (≈80%), blood(≈10%), and CSF(≈10%) is constan
and thatan increase in any one of these mustbe offset by
an equal decrease in another, or else pressure increases. T
ICP varies with age and normative values for children are
not well established.Normalvaluesare lessthan 10 to
15 mm Hg for adults and older children, 3 to 7 mm Hg for
young children,and 1.5 to 6 mm Hg for term infants [1].
ICP values greater than 20 to 25 mm Hg require treatmen
in most circumstances. Sustained ICP values of greater tha
40 mm Hg indicatesevere,life-threatening intracranial
hypertension [2].
Cerebral Pressure Dynamics
Cerebralperfusion pressure (CPP)is a majorfactorthat
affects cerebral blood flow to the brain.CPP measurement
is expressed in millimeters of mercury and is determined b
measuring the difference between the mean arterial press
(MAP) and ICP (CPP = MAP – ICP).It is apparentfrom
the formula that,CPP can reduce as a resultof reduced
MAP or raised ICP,or a combination ofthese two.CPP
N. Sankhyan:K. N. Vykunta Raju:S. Sharma:S. Gulati (*)
Child Neurology Division,Department of Pediatrics,All India
Institute of Medical Sciences,
New Delhi 110029,India
e-mail: sheffaligulati@gmail.com
Indian J Pediatr (2010) 77:1409–1416
DOI 10.1007/s12098-010-0190-2
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
measurementsaid in determining theamountof blood
volume presentin the intracranialspace.It is used as an
importantclinicalindicatorof cerebralblood flow and
henceadequateoxygenation.Normal CPP values for
children arenot clearly established,but the following
valuesare generally accepted asthe minimalpressure
necessary to preventischemia:adultsCPP>70 mm Hg;
children CPP>50–60 mm Hg;infants/toddlers CPP> 40–
50 mm Hg [3].
Causes of Raised ICP
The variouscausesof raised ICP (Table1) can occur
individually orin variouscombinations.Based on the
Monroe-Kelliehypothesis,raised ICP can resultfrom
increase in volume of brain,blood,or CSF.Frequently it is
a combination of these factors that result in raised ICP.The
causes ofraised ICP can also be divided into primary or
secondary depending on the primary pathology.In primary
causes of increased ICP,normalization of ICP depends on
rapidly addressing the underlying brain disorder.In second-
ary causesof raisedICP the underlyingsystemicor
extracranial cause has to be managed.
Assessment and Monitoring
Identify children atrisk for raised ICP (Table 1).Those at
greaterrisk are children with head trauma,suspected
neuroinfections,or suspected intracranialmasslesions.
Raised pressure usually manifests as headache,vomiting,
irritability,squint,tonic posturing or worsening sensorium.
Howeverthe symptomsdepend on the age,cause,and
evolution of the raised ICP.
Initial Assessment
As with any sick child,one begins with assessmentand
maintenance of the airway, breathing and circulatory func
An immediate priority is to look for potentially life threaten
signs of herniation (Table 2).If these signs are presentthen
measures to decrease intracranial pressure should be rapi
instituted.Cushing’striad (bradycardia,hypertension and
irregular breathing) is a late sign of herniation.
Neurological Assessment
After the initialstabilization,a thorough history and clinical
examination is performed to determine the possible etiolo
and further course of management. Pupillary abnormalitie
abnormalities in ocular movements as determined by spon
neous, dolls eye or cold caloric testing are important clues
localization ofbrainstem dysfunction.The examination of
fundus is focused on detection of papilledema, keeping in
that its absence does not rule out raised ICP. The motor sy
examination focuses on identifying posturing or flaccidity
to raised ICP or focal deficits. Findings on the general phys
and systemic examination may provide clues to the under
cause for raised ICP (e.g.jaundice/hepatomegaly in hepatic
encephalopathy, rash in viral encephalitis etc.).
Neuroimaging
The imaging study ofchoice forthe patientwith raised
intracranial pressure presenting to the emergency room is
computed tomography (CT)scan.A contraststudy is
helpfulto identify featuresof infection (meningealen-
hancement,brain abscess etc.)and tumors.If CT scan is
normal,and the patienthas clinicalfeatures of raised ICP,
then an MRI with MR venogram must be obtained once the
patient is stabilized.MRI can pick up early stroke,venous
thromboses,posteriorfossa tumorsand demyelinating
lesions which might be missed on CT.
Invasive ICP Monitoring
ICP monitoring is used mainly to guide therapy,such as
in determiningwhen to drain CSF or administer
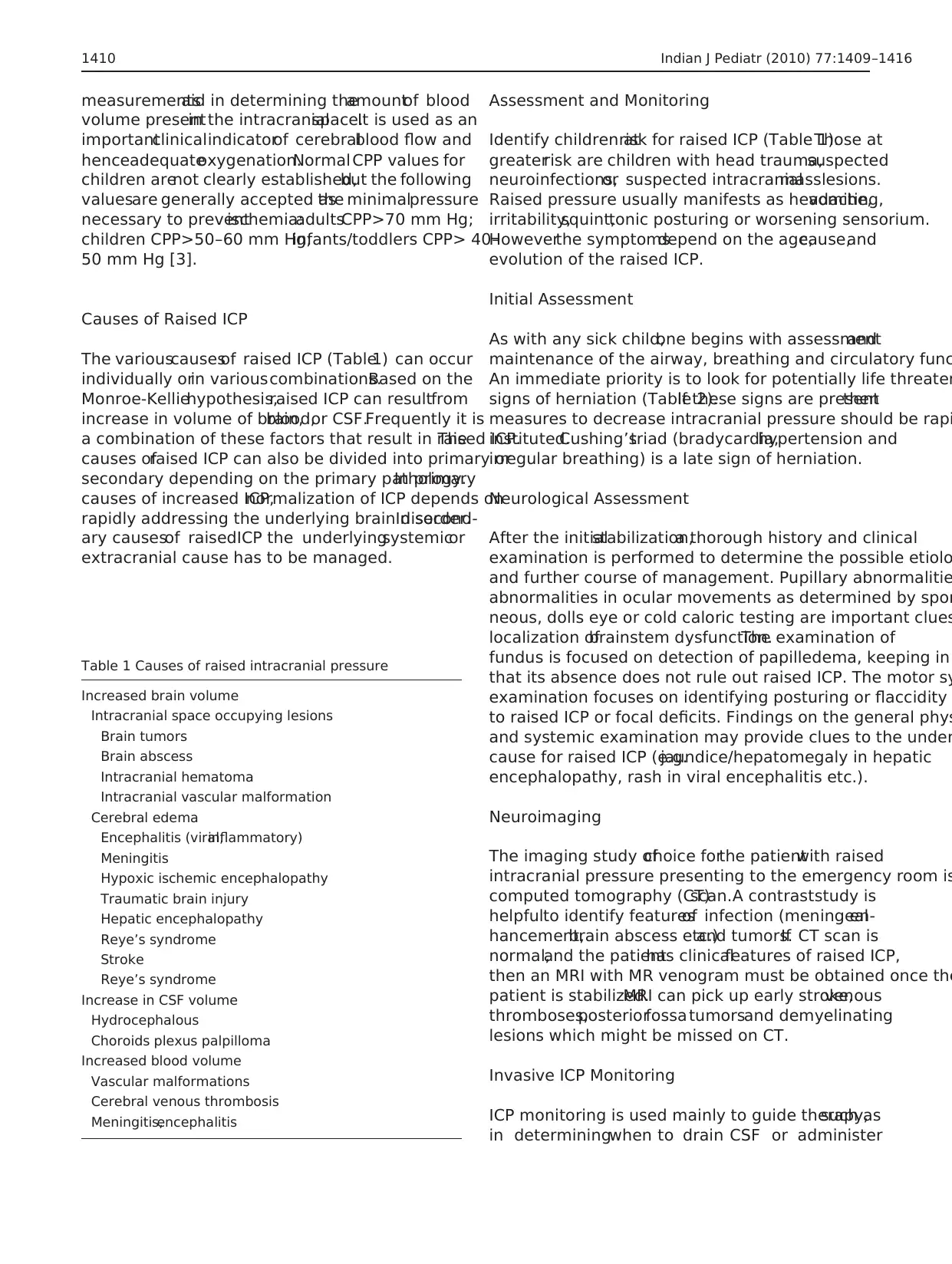
Table 1 Causes of raised intracranial pressure
Increased brain volume
Intracranial space occupying lesions
Brain tumors
Brain abscess
Intracranial hematoma
Intracranial vascular malformation
Cerebral edema
Encephalitis (viral,inflammatory)
Meningitis
Hypoxic ischemic encephalopathy
Traumatic brain injury
Hepatic encephalopathy
Reye’s syndrome
Stroke
Reye’s syndrome
Increase in CSF volume
Hydrocephalous
Choroids plexus palpilloma
Increased blood volume
Vascular malformations
Cerebral venous thrombosis
Meningitis,encephalitis
1410 Indian J Pediatr (2010) 77:1409–1416
volume presentin the intracranialspace.It is used as an
importantclinicalindicatorof cerebralblood flow and
henceadequateoxygenation.Normal CPP values for
children arenot clearly established,but the following
valuesare generally accepted asthe minimalpressure
necessary to preventischemia:adultsCPP>70 mm Hg;
children CPP>50–60 mm Hg;infants/toddlers CPP> 40–
50 mm Hg [3].
Causes of Raised ICP
The variouscausesof raised ICP (Table1) can occur
individually orin variouscombinations.Based on the
Monroe-Kelliehypothesis,raised ICP can resultfrom
increase in volume of brain,blood,or CSF.Frequently it is
a combination of these factors that result in raised ICP.The
causes ofraised ICP can also be divided into primary or
secondary depending on the primary pathology.In primary
causes of increased ICP,normalization of ICP depends on
rapidly addressing the underlying brain disorder.In second-
ary causesof raisedICP the underlyingsystemicor
extracranial cause has to be managed.
Assessment and Monitoring
Identify children atrisk for raised ICP (Table 1).Those at
greaterrisk are children with head trauma,suspected
neuroinfections,or suspected intracranialmasslesions.
Raised pressure usually manifests as headache,vomiting,
irritability,squint,tonic posturing or worsening sensorium.
Howeverthe symptomsdepend on the age,cause,and
evolution of the raised ICP.
Initial Assessment
As with any sick child,one begins with assessmentand
maintenance of the airway, breathing and circulatory func
An immediate priority is to look for potentially life threaten
signs of herniation (Table 2).If these signs are presentthen
measures to decrease intracranial pressure should be rapi
instituted.Cushing’striad (bradycardia,hypertension and
irregular breathing) is a late sign of herniation.
Neurological Assessment
After the initialstabilization,a thorough history and clinical
examination is performed to determine the possible etiolo
and further course of management. Pupillary abnormalitie
abnormalities in ocular movements as determined by spon
neous, dolls eye or cold caloric testing are important clues
localization ofbrainstem dysfunction.The examination of
fundus is focused on detection of papilledema, keeping in
that its absence does not rule out raised ICP. The motor sy
examination focuses on identifying posturing or flaccidity
to raised ICP or focal deficits. Findings on the general phys
and systemic examination may provide clues to the under
cause for raised ICP (e.g.jaundice/hepatomegaly in hepatic
encephalopathy, rash in viral encephalitis etc.).
Neuroimaging
The imaging study ofchoice forthe patientwith raised
intracranial pressure presenting to the emergency room is
computed tomography (CT)scan.A contraststudy is
helpfulto identify featuresof infection (meningealen-
hancement,brain abscess etc.)and tumors.If CT scan is
normal,and the patienthas clinicalfeatures of raised ICP,
then an MRI with MR venogram must be obtained once the
patient is stabilized.MRI can pick up early stroke,venous
thromboses,posteriorfossa tumorsand demyelinating
lesions which might be missed on CT.
Invasive ICP Monitoring
ICP monitoring is used mainly to guide therapy,such as
in determiningwhen to drain CSF or administer
Table 1 Causes of raised intracranial pressure
Increased brain volume
Intracranial space occupying lesions
Brain tumors
Brain abscess
Intracranial hematoma
Intracranial vascular malformation
Cerebral edema
Encephalitis (viral,inflammatory)
Meningitis
Hypoxic ischemic encephalopathy
Traumatic brain injury
Hepatic encephalopathy
Reye’s syndrome
Stroke
Reye’s syndrome
Increase in CSF volume
Hydrocephalous
Choroids plexus palpilloma
Increased blood volume
Vascular malformations
Cerebral venous thrombosis
Meningitis,encephalitis
1410 Indian J Pediatr (2010) 77:1409–1416
mannitolor sedation.In addition,invasive monitoring
allows forobservation ofthe shape,height,and trends
of individualand consecutive ICP waveforms thatmay
reflectintracranialcompliance,cerebrovascularstatus
and cerebralperfusion.Guidelinesfor ICP monitoring
are available for traumaticbrain injury [4]. ICP
monitoring is indicated for a patient with Glasgow Coma
Scale (GCS) score of 3–8 (after resuscitation) with either
an abnormaladmission head CT or motor posturing and
hypotension [4].The role and benefitof ICP monitoring
in other conditionssuch assubarachnoid hemorrhage,
hydrocephalus,intracranialinfections,and Reyessyn-
dromeremainsunclear.Also, the availability ofthis
modality is limited.In other brain injuries,such as
hypoxic and ischemic injuries,monitoring ICP has not
been shown to improve outcome [5].
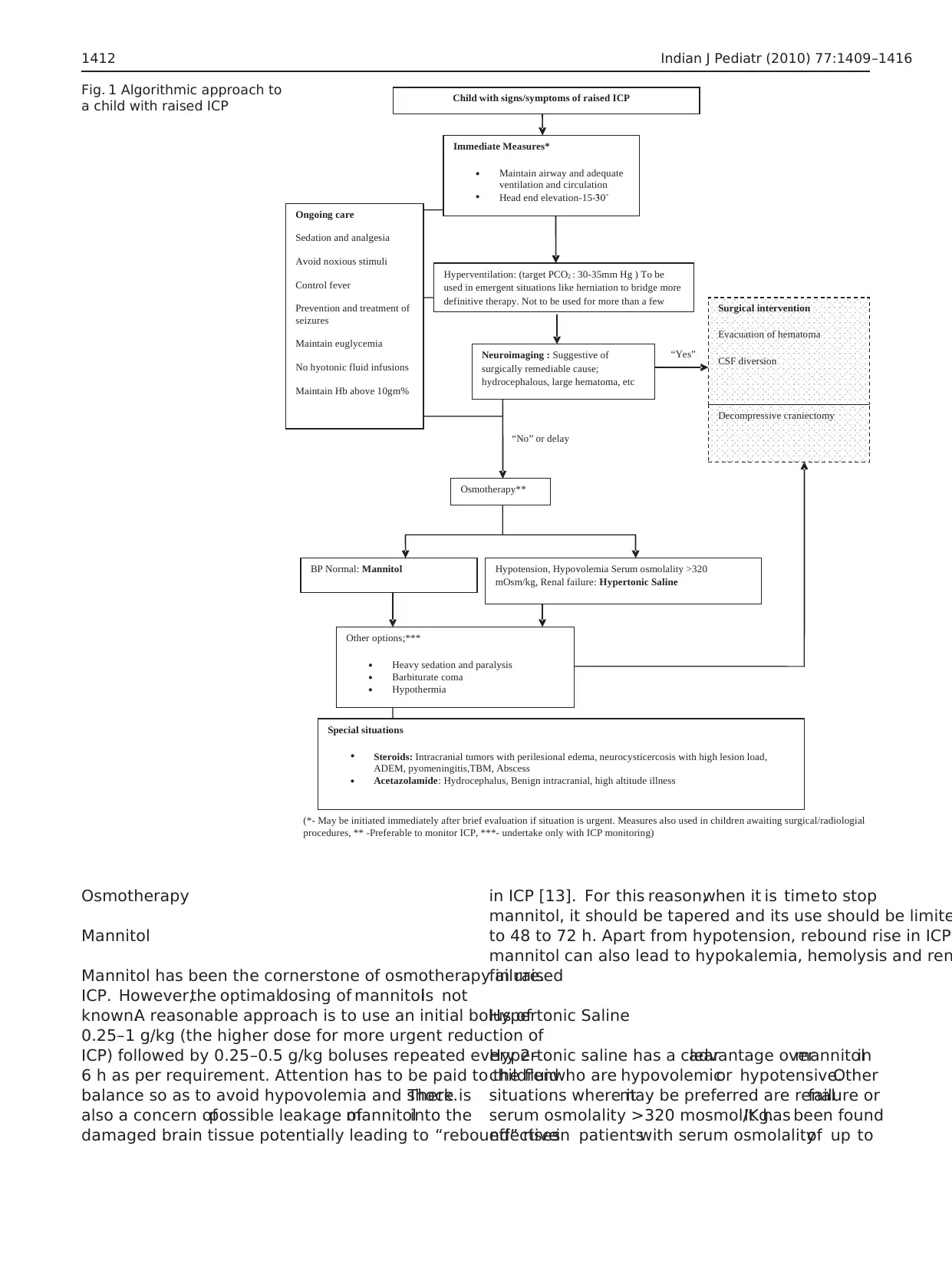
Management of Intracranial Hypertension
The goal for patients presenting with raised ICP is to identify
and addressthe underlying cause along with measuresto
reduce ICP (Fig.1, Table 3).It is importantnotto delay
treatment, in situations where identifying the underlying cause
will take time.When elevated ICP is clinically evident,the
situation is urgentand requires immediate reduction in ICP.
Avoidance of factors aggravating or precipitating raised ICP is
an importantgoalfor allchildren with intracranialhyperten-
sion.The availability ofICP monitors is notuniversaland
should not come in the way of emergent therapy.
ABCs
The assessment and management of the airway,breathing
and circulation (ABCs) is the beginning point of manage-
ment.Early endotracheal intubation should be considered
for those children with GCS <8,evidence ofherniation,
apneaor haveinability to maintain airway.Intubation
should proceed with administration of medications to blun
the ICP during the procedure.Suggested medications are
lidocaine,thiopentaland a short-acting non depolarizing
neuromuscularblockadeagent(e.g.vecuronium,atracu-
rium) [6].Appropriate oxygenation should be ensured.If
there is evidence of circulatory failure,fluid bolus should
be given.Samples should be drawn for investigations as
suggested by history.
Positioning
Mild head elevation of 15–30° has been shown to reduce
ICP with no significantdetrimentaleffectson CPP or
CBF [7]. The child’s head is positioned midline with the
head end ofthe bed elevated to 15–30°to encourage
jugular venous drainage [7].Sharp head angulations and
tight neck garments or taping should be avoided [8].One
has to ensure that the child is euvolemic and not in shock
prior to placing in this position [6].
Hyperventilation
Decreasing the PaCO2 to the range of 30–35 mm of Hg, is
an effectiveand rapid meansto reduceICP [6, 9].
Hyperventilation actsby constriction ofcerebralblood
vessels and lowering of CBF.This vasoconstrictive effect
on cerebral arterioles lasts only 11 to 20 h because the pH
of the CSF rapidly equilibrates to the new PaCO2 level.
Moreover,aggressivehyperventilation can dramatically
decreases the CBF,causing or aggravating cerebral ische-
mia [10,11].Hence,the mosteffective use of hyperven-
tilation is foracute,sharp increases in ICP orsigns of
impending herniation [12].
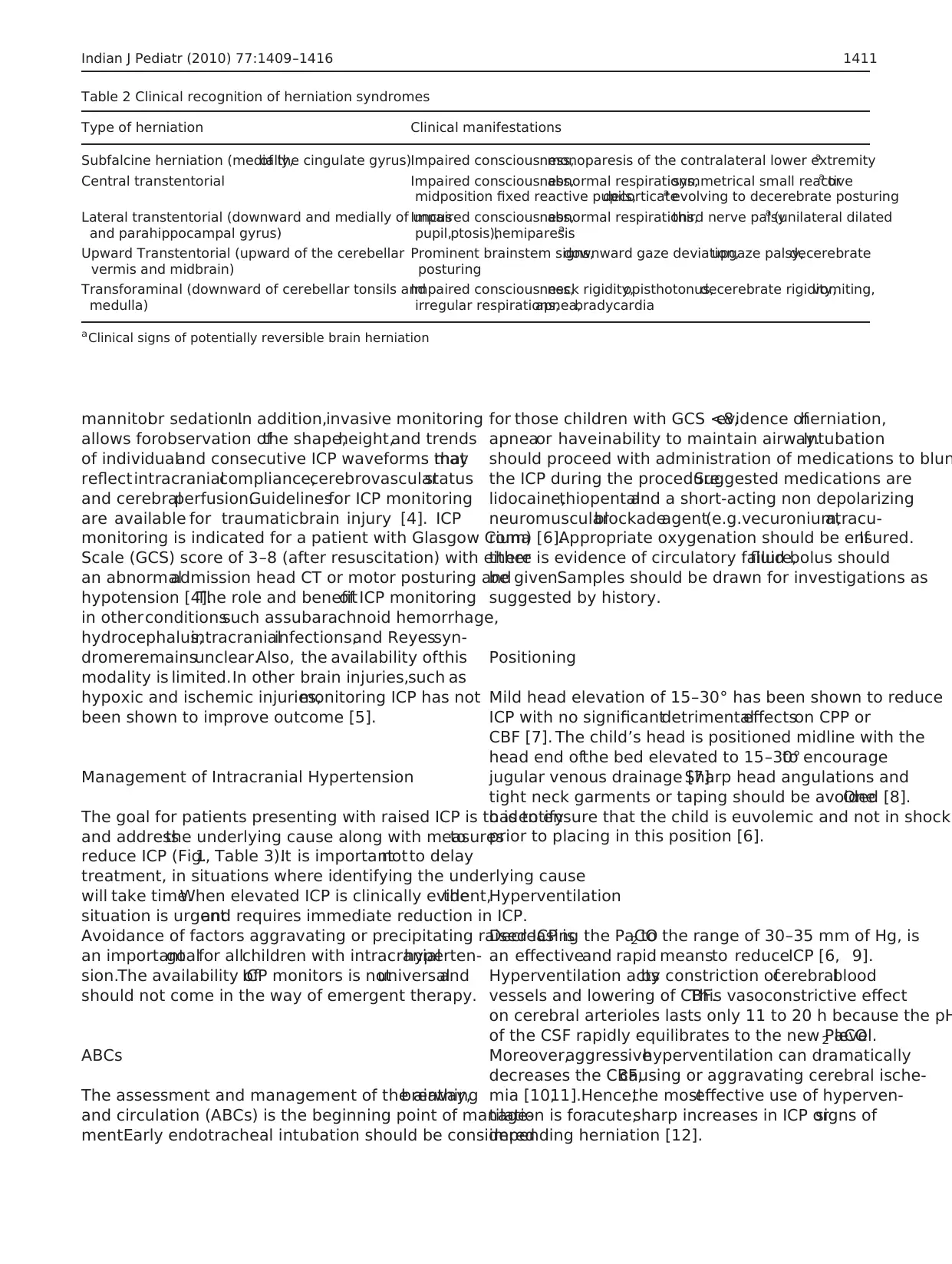
Table 2 Clinical recognition of herniation syndromes
Type of herniation Clinical manifestations
Subfalcine herniation (medially,of the cingulate gyrus)Impaired consciousness,monoparesis of the contralateral lower extremitya
Central transtentorial Impaired consciousness,abnormal respirations,symmetrical small reactivea or
midposition fixed reactive pupils,decorticatea evolving to decerebrate posturing
Lateral transtentorial (downward and medially of uncus
and parahippocampal gyrus)
Impaired consciousness,abnormal respirations,third nerve palsya (unilateral dilated
pupil,ptosis),hemiparesisa
Upward Transtentorial (upward of the cerebellar
vermis and midbrain)
Prominent brainstem signs,downward gaze deviation,upgaze palsy,decerebrate
posturing
Transforaminal (downward of cerebellar tonsils and
medulla)
Impaired consciousness,neck rigidity,opisthotonus,decerebrate rigidity,vomiting,
irregular respirations,apnea,bradycardia
aClinical signs of potentially reversible brain herniation
Indian J Pediatr (2010) 77:1409–1416 1411
allows forobservation ofthe shape,height,and trends
of individualand consecutive ICP waveforms thatmay
reflectintracranialcompliance,cerebrovascularstatus
and cerebralperfusion.Guidelinesfor ICP monitoring
are available for traumaticbrain injury [4]. ICP
monitoring is indicated for a patient with Glasgow Coma
Scale (GCS) score of 3–8 (after resuscitation) with either
an abnormaladmission head CT or motor posturing and
hypotension [4].The role and benefitof ICP monitoring
in other conditionssuch assubarachnoid hemorrhage,
hydrocephalus,intracranialinfections,and Reyessyn-
dromeremainsunclear.Also, the availability ofthis
modality is limited.In other brain injuries,such as
hypoxic and ischemic injuries,monitoring ICP has not
been shown to improve outcome [5].
Management of Intracranial Hypertension
The goal for patients presenting with raised ICP is to identify
and addressthe underlying cause along with measuresto
reduce ICP (Fig.1, Table 3).It is importantnotto delay
treatment, in situations where identifying the underlying cause
will take time.When elevated ICP is clinically evident,the
situation is urgentand requires immediate reduction in ICP.
Avoidance of factors aggravating or precipitating raised ICP is
an importantgoalfor allchildren with intracranialhyperten-
sion.The availability ofICP monitors is notuniversaland
should not come in the way of emergent therapy.
ABCs
The assessment and management of the airway,breathing
and circulation (ABCs) is the beginning point of manage-
ment.Early endotracheal intubation should be considered
for those children with GCS <8,evidence ofherniation,
apneaor haveinability to maintain airway.Intubation
should proceed with administration of medications to blun
the ICP during the procedure.Suggested medications are
lidocaine,thiopentaland a short-acting non depolarizing
neuromuscularblockadeagent(e.g.vecuronium,atracu-
rium) [6].Appropriate oxygenation should be ensured.If
there is evidence of circulatory failure,fluid bolus should
be given.Samples should be drawn for investigations as
suggested by history.
Positioning
Mild head elevation of 15–30° has been shown to reduce
ICP with no significantdetrimentaleffectson CPP or
CBF [7]. The child’s head is positioned midline with the
head end ofthe bed elevated to 15–30°to encourage
jugular venous drainage [7].Sharp head angulations and
tight neck garments or taping should be avoided [8].One
has to ensure that the child is euvolemic and not in shock
prior to placing in this position [6].
Hyperventilation
Decreasing the PaCO2 to the range of 30–35 mm of Hg, is
an effectiveand rapid meansto reduceICP [6, 9].
Hyperventilation actsby constriction ofcerebralblood
vessels and lowering of CBF.This vasoconstrictive effect
on cerebral arterioles lasts only 11 to 20 h because the pH
of the CSF rapidly equilibrates to the new PaCO2 level.
Moreover,aggressivehyperventilation can dramatically
decreases the CBF,causing or aggravating cerebral ische-
mia [10,11].Hence,the mosteffective use of hyperven-
tilation is foracute,sharp increases in ICP orsigns of
impending herniation [12].
Table 2 Clinical recognition of herniation syndromes
Type of herniation Clinical manifestations
Subfalcine herniation (medially,of the cingulate gyrus)Impaired consciousness,monoparesis of the contralateral lower extremitya
Central transtentorial Impaired consciousness,abnormal respirations,symmetrical small reactivea or
midposition fixed reactive pupils,decorticatea evolving to decerebrate posturing
Lateral transtentorial (downward and medially of uncus
and parahippocampal gyrus)
Impaired consciousness,abnormal respirations,third nerve palsya (unilateral dilated
pupil,ptosis),hemiparesisa
Upward Transtentorial (upward of the cerebellar
vermis and midbrain)
Prominent brainstem signs,downward gaze deviation,upgaze palsy,decerebrate
posturing
Transforaminal (downward of cerebellar tonsils and
medulla)
Impaired consciousness,neck rigidity,opisthotonus,decerebrate rigidity,vomiting,
irregular respirations,apnea,bradycardia
aClinical signs of potentially reversible brain herniation
Indian J Pediatr (2010) 77:1409–1416 1411
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Osmotherapy
Mannitol
Mannitol has been the cornerstone of osmotherapy in raised
ICP. However,the optimaldosing of mannitolis not
known.A reasonable approach is to use an initial bolus of
0.25–1 g/kg (the higher dose for more urgent reduction of
ICP) followed by 0.25–0.5 g/kg boluses repeated every 2–
6 h as per requirement. Attention has to be paid to the fluid
balance so as to avoid hypovolemia and shock.There is
also a concern ofpossible leakage ofmannitolinto the
damaged brain tissue potentially leading to “rebound” rises
in ICP [13]. For this reason,when it is timeto stop
mannitol, it should be tapered and its use should be limite
to 48 to 72 h. Apart from hypotension, rebound rise in ICP,
mannitol can also lead to hypokalemia, hemolysis and ren
failure.
Hypertonic Saline
Hypertonic saline has a clearadvantage overmannitolin
childrenwho are hypovolemicor hypotensive.Other
situations where itmay be preferred are renalfailure or
serum osmolality >320 mosmol/Kg.It has been found
effectivein patientswith serum osmolalityof up to
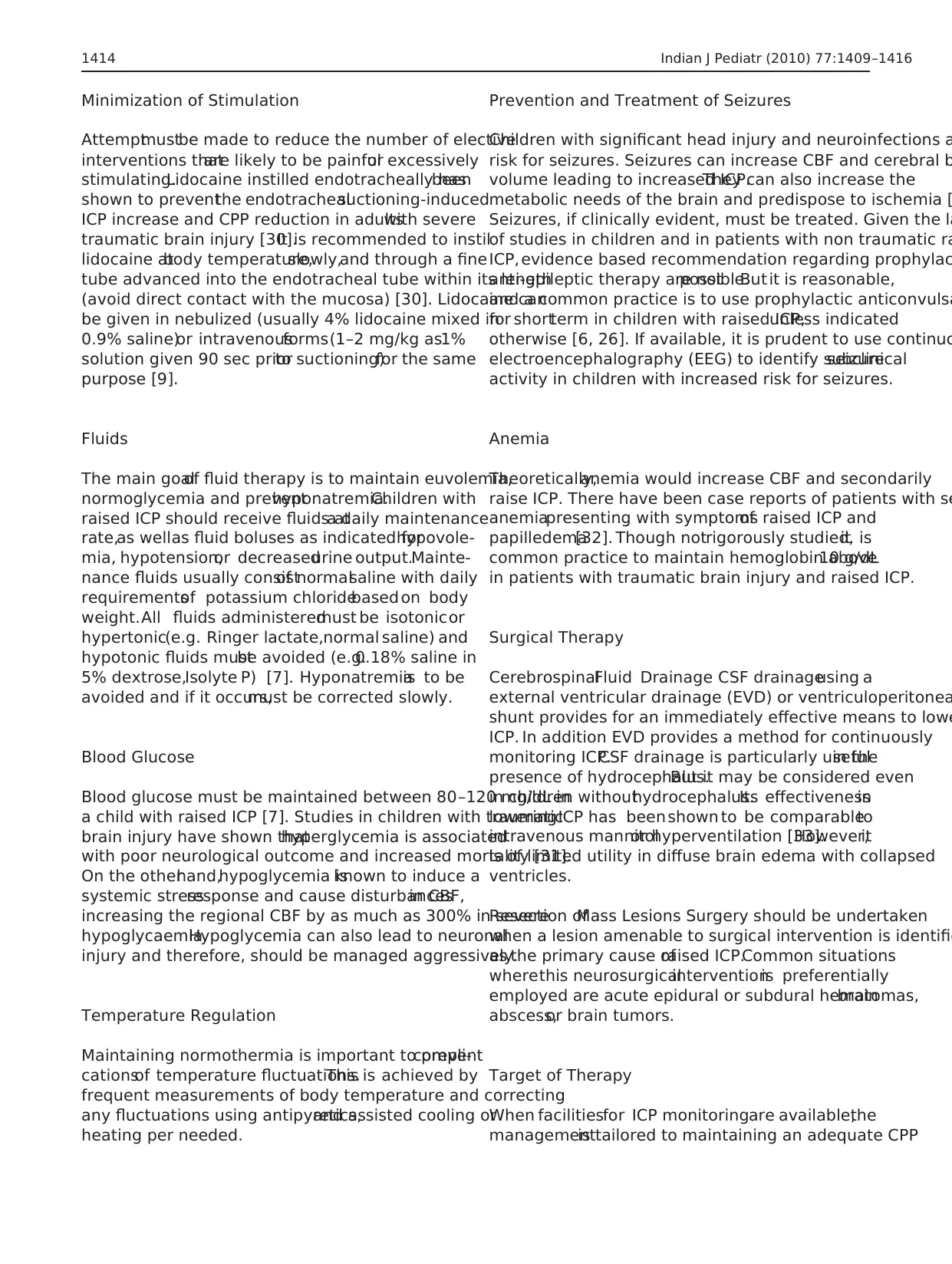
Surgical intervention
Evacuation of hematoma
CSF diversion
Neuroimaging : Suggestive of
surgically remediable cause;
hydrocephalous, large hematoma, etc
“Yes”
“No” or delay
Immediate Measures*
Maintain airway and adequate
ventilation and circulation
Head end elevation-15-
Hyperventilation: (target PCO2 : 30-35mm Hg ) To be
used in emergent situations like herniation to bridge more
definitive therapy. Not to be used for more than a few
Osmotherapy**
Child with signs/symptoms of raised ICP
Decompressive craniectomy
BP Normal: Mannitol Hypotension, Hypovolemia Serum osmolality >320
mOsm/kg, Renal failure: Hypertonic Saline
Other options;***
Heavy sedation and paralysis
Barbiturate coma
Hypothermia
Special situations
Steroids: Intracranial tumors with perilesional edema, neurocysticercosis with high lesion load,
ADEM, pyomeningitis,TBM, Abscess
Acetazolamide: Hydrocephalus, Benign intracranial, high altitude illness
Ongoing care
Sedation and analgesia
Avoid noxious stimuli
Control fever
Prevention and treatment of
seizures
Maintain euglycemia
No hyotonic fluid infusions
Maintain Hb above 10gm%
.
.
.
.
.
.
.
(*- May be initiated immediately after brief evaluation if situation is urgent. Measures also used in children awaiting surgical/radiologial
procedures, ** -Preferable to monitor ICP, ***- undertake only with ICP monitoring)
Fig. 1 Algorithmic approach to
a child with raised ICP
1412 Indian J Pediatr (2010) 77:1409–1416
Mannitol
Mannitol has been the cornerstone of osmotherapy in raised
ICP. However,the optimaldosing of mannitolis not
known.A reasonable approach is to use an initial bolus of
0.25–1 g/kg (the higher dose for more urgent reduction of
ICP) followed by 0.25–0.5 g/kg boluses repeated every 2–
6 h as per requirement. Attention has to be paid to the fluid
balance so as to avoid hypovolemia and shock.There is
also a concern ofpossible leakage ofmannitolinto the
damaged brain tissue potentially leading to “rebound” rises
in ICP [13]. For this reason,when it is timeto stop
mannitol, it should be tapered and its use should be limite
to 48 to 72 h. Apart from hypotension, rebound rise in ICP,
mannitol can also lead to hypokalemia, hemolysis and ren
failure.
Hypertonic Saline
Hypertonic saline has a clearadvantage overmannitolin
childrenwho are hypovolemicor hypotensive.Other
situations where itmay be preferred are renalfailure or
serum osmolality >320 mosmol/Kg.It has been found
effectivein patientswith serum osmolalityof up to
Surgical intervention
Evacuation of hematoma
CSF diversion
Neuroimaging : Suggestive of
surgically remediable cause;
hydrocephalous, large hematoma, etc
“Yes”
“No” or delay
Immediate Measures*
Maintain airway and adequate
ventilation and circulation
Head end elevation-15-
Hyperventilation: (target PCO2 : 30-35mm Hg ) To be
used in emergent situations like herniation to bridge more
definitive therapy. Not to be used for more than a few
Osmotherapy**
Child with signs/symptoms of raised ICP
Decompressive craniectomy
BP Normal: Mannitol Hypotension, Hypovolemia Serum osmolality >320
mOsm/kg, Renal failure: Hypertonic Saline
Other options;***
Heavy sedation and paralysis
Barbiturate coma
Hypothermia
Special situations
Steroids: Intracranial tumors with perilesional edema, neurocysticercosis with high lesion load,
ADEM, pyomeningitis,TBM, Abscess
Acetazolamide: Hydrocephalus, Benign intracranial, high altitude illness
Ongoing care
Sedation and analgesia
Avoid noxious stimuli
Control fever
Prevention and treatment of
seizures
Maintain euglycemia
No hyotonic fluid infusions
Maintain Hb above 10gm%
.
.
.
.
.
.
.
(*- May be initiated immediately after brief evaluation if situation is urgent. Measures also used in children awaiting surgical/radiologial
procedures, ** -Preferable to monitor ICP, ***- undertake only with ICP monitoring)
Fig. 1 Algorithmic approach to
a child with raised ICP
1412 Indian J Pediatr (2010) 77:1409–1416
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
360 mosmol/Kg [14].Concerns with its use are bleeding,
rebound risein ICP, hypokalemia,and hyperchloremic
acidosis,centralpontine myelinolysis,acute volume over-
load, renal failure, cardiac failure or pulmonary edema [15–
17].Despite these concerns,current evidence suggests that
hypertonic saline as currently used is safe and does not
result in major adverse effects [18].In different studies the
concentration ofhypertonic saline used hasvaried from
1.7% to 30% [18].The method of administration has also
varied and hence,evidence based recommendationsare
difficult.It would be reasonable to administerhypertonic
saline as a continuous infusion at0.1 to 1.0 mL/kg/hr,to
targeta serum sodium levelof 145–155 meq/L [19,20].
Serum sodium and neurologicalstatus needs to be closely
monitored during therapy.When thehypertonicsaline
therapy isno longerrequired,serum sodium should be
slowly corrected to normal values (hourly decline in serum
sodium of not more than 0.5 meq/L) to avoid complications
associated with fluid shifts[6]. Monitoring of serum
sodium and serum osmolality should be done every 2–4 h
till targetlevelis reached and then followed up with 12
hourly estimations.Undercarefulmonitoring,hypertonic
saline has been used for up to 7 days [21].
Other Agents
Acetazolamide (20–100 mg/kg/day, in 3 divided doses, ma
2 g/day) is a carbonic anhydrase inhibitor thatreduces the
production of CSF.It is particularly usefulin patients with
hydrocephalous, high altitude illness and benign intracran
hypertension.Furosemide (1 mg/kg/day,q8hrly),a loop
diuretic has sometimes been administered either alone or
combination with mannitol,with variable success [22,23].
Glycerol is another alternative osmotic agent for treatmen
raised ICP.It is used in the oral (1.5 g/kg/day,q4–6hrly) or
intravenous forms. Given intravenously, it reduces ICP with
effect lasting for about 70 min without any prolonged effe
on serum osmolality [24]. Glycerol readily moves across th
blood brain barrier into the brain. Though not proven,there
is concern of rebound rise in ICP with its use.
Steroids
Glucocorticoidsare very effectivein ameliorating the
vasogenic edema thataccompanies tumors,inflammatory
conditions,infections and otherdisorders associated with
increased permeability ofblood brain barrier,including
surgical manipulation [25]. Dexamethasone is the preferre
agent due to its very low mineralocorticoid activity (Dose:
0.4–1.5 mg/kg/day, q 6 hrly) [26]. Steroids are not routinel
indicated in individuals with traumatic brain injury [27].
Steroidshave notbeen found to be usefuland may be
detrimentalin ischemiclesions,cerebralmalariaand
intracranial hemorrhage [26,28,29].
Sedation and Analgesia
Raised ICP is worsened due to agitation, pain, and patient-
ventilator asynchrony [8]. Adequate analgesia, sedation a
occasionally neuromuscular blockade are useful adjuvant
the managementof raised ICP.Appropriate Analgesia and
sedation is usually preferred over neuromuscular blockade
as it is quickly reversibleand allowsfor neurological
monitoring.For sedation it is preferable to use agents with
minimal effect on blood pressure. Short acting benzodiaze
pines (e.g. midazolam) are useful for sedation in children.
the sedatives are notcompletely effective,then a neuro-
muscularblocking agent(e.g.Pancuronium,atracurium,
vecuronium) may be required.
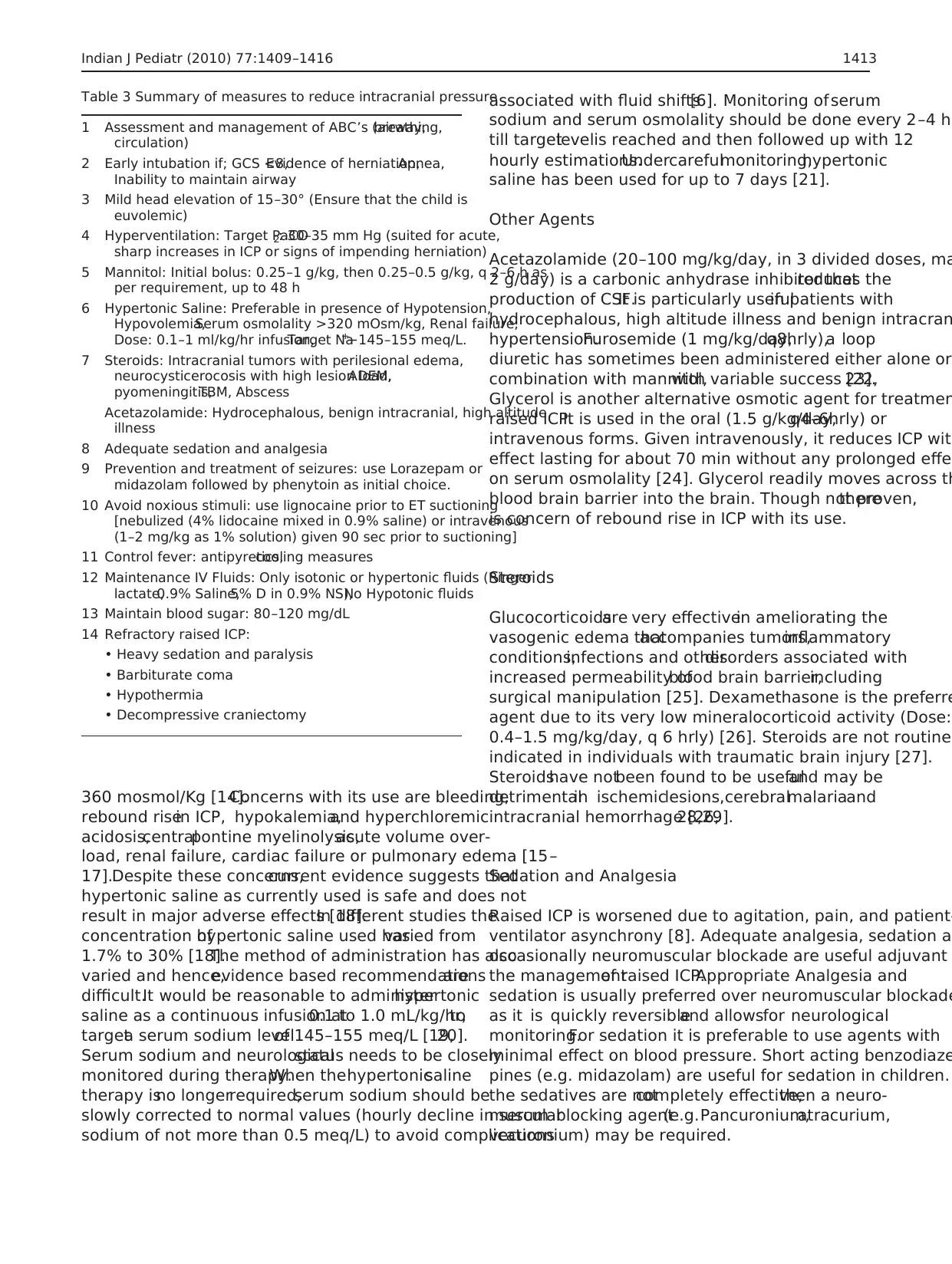
Table 3 Summary of measures to reduce intracranial pressure
1 Assessment and management of ABC’s (airway,breathing,
circulation)
2 Early intubation if; GCS <8,Evidence of herniation,Apnea,
Inability to maintain airway
3 Mild head elevation of 15–30° (Ensure that the child is
euvolemic)
4 Hyperventilation: Target PaCO2: 30–35 mm Hg (suited for acute,
sharp increases in ICP or signs of impending herniation)
5 Mannitol: Initial bolus: 0.25–1 g/kg, then 0.25–0.5 g/kg, q 2–6 h as
per requirement, up to 48 h
6 Hypertonic Saline: Preferable in presence of Hypotension,
Hypovolemia,Serum osmolality >320 mOsm/kg, Renal failure,
Dose: 0.1–1 ml/kg/hr infusion,Target Na+
−145–155 meq/L.
7 Steroids: Intracranial tumors with perilesional edema,
neurocysticerocosis with high lesion load,ADEM,
pyomeningitis,TBM, Abscess
Acetazolamide: Hydrocephalous, benign intracranial, high altitude
illness
8 Adequate sedation and analgesia
9 Prevention and treatment of seizures: use Lorazepam or
midazolam followed by phenytoin as initial choice.
10 Avoid noxious stimuli: use lignocaine prior to ET suctioning
[nebulized (4% lidocaine mixed in 0.9% saline) or intravenous
(1–2 mg/kg as 1% solution) given 90 sec prior to suctioning]
11 Control fever: antipyretics,cooling measures
12 Maintenance IV Fluids: Only isotonic or hypertonic fluids (Ringer
lactate,0.9% Saline,5% D in 0.9% NS),No Hypotonic fluids
13 Maintain blood sugar: 80–120 mg/dL
14 Refractory raised ICP:
• Heavy sedation and paralysis
• Barbiturate coma
• Hypothermia
• Decompressive craniectomy
Indian J Pediatr (2010) 77:1409–1416 1413
rebound risein ICP, hypokalemia,and hyperchloremic
acidosis,centralpontine myelinolysis,acute volume over-
load, renal failure, cardiac failure or pulmonary edema [15–
17].Despite these concerns,current evidence suggests that
hypertonic saline as currently used is safe and does not
result in major adverse effects [18].In different studies the
concentration ofhypertonic saline used hasvaried from
1.7% to 30% [18].The method of administration has also
varied and hence,evidence based recommendationsare
difficult.It would be reasonable to administerhypertonic
saline as a continuous infusion at0.1 to 1.0 mL/kg/hr,to
targeta serum sodium levelof 145–155 meq/L [19,20].
Serum sodium and neurologicalstatus needs to be closely
monitored during therapy.When thehypertonicsaline
therapy isno longerrequired,serum sodium should be
slowly corrected to normal values (hourly decline in serum
sodium of not more than 0.5 meq/L) to avoid complications
associated with fluid shifts[6]. Monitoring of serum
sodium and serum osmolality should be done every 2–4 h
till targetlevelis reached and then followed up with 12
hourly estimations.Undercarefulmonitoring,hypertonic
saline has been used for up to 7 days [21].
Other Agents
Acetazolamide (20–100 mg/kg/day, in 3 divided doses, ma
2 g/day) is a carbonic anhydrase inhibitor thatreduces the
production of CSF.It is particularly usefulin patients with
hydrocephalous, high altitude illness and benign intracran
hypertension.Furosemide (1 mg/kg/day,q8hrly),a loop
diuretic has sometimes been administered either alone or
combination with mannitol,with variable success [22,23].
Glycerol is another alternative osmotic agent for treatmen
raised ICP.It is used in the oral (1.5 g/kg/day,q4–6hrly) or
intravenous forms. Given intravenously, it reduces ICP with
effect lasting for about 70 min without any prolonged effe
on serum osmolality [24]. Glycerol readily moves across th
blood brain barrier into the brain. Though not proven,there
is concern of rebound rise in ICP with its use.
Steroids
Glucocorticoidsare very effectivein ameliorating the
vasogenic edema thataccompanies tumors,inflammatory
conditions,infections and otherdisorders associated with
increased permeability ofblood brain barrier,including
surgical manipulation [25]. Dexamethasone is the preferre
agent due to its very low mineralocorticoid activity (Dose:
0.4–1.5 mg/kg/day, q 6 hrly) [26]. Steroids are not routinel
indicated in individuals with traumatic brain injury [27].
Steroidshave notbeen found to be usefuland may be
detrimentalin ischemiclesions,cerebralmalariaand
intracranial hemorrhage [26,28,29].
Sedation and Analgesia
Raised ICP is worsened due to agitation, pain, and patient-
ventilator asynchrony [8]. Adequate analgesia, sedation a
occasionally neuromuscular blockade are useful adjuvant
the managementof raised ICP.Appropriate Analgesia and
sedation is usually preferred over neuromuscular blockade
as it is quickly reversibleand allowsfor neurological
monitoring.For sedation it is preferable to use agents with
minimal effect on blood pressure. Short acting benzodiaze
pines (e.g. midazolam) are useful for sedation in children.
the sedatives are notcompletely effective,then a neuro-
muscularblocking agent(e.g.Pancuronium,atracurium,
vecuronium) may be required.
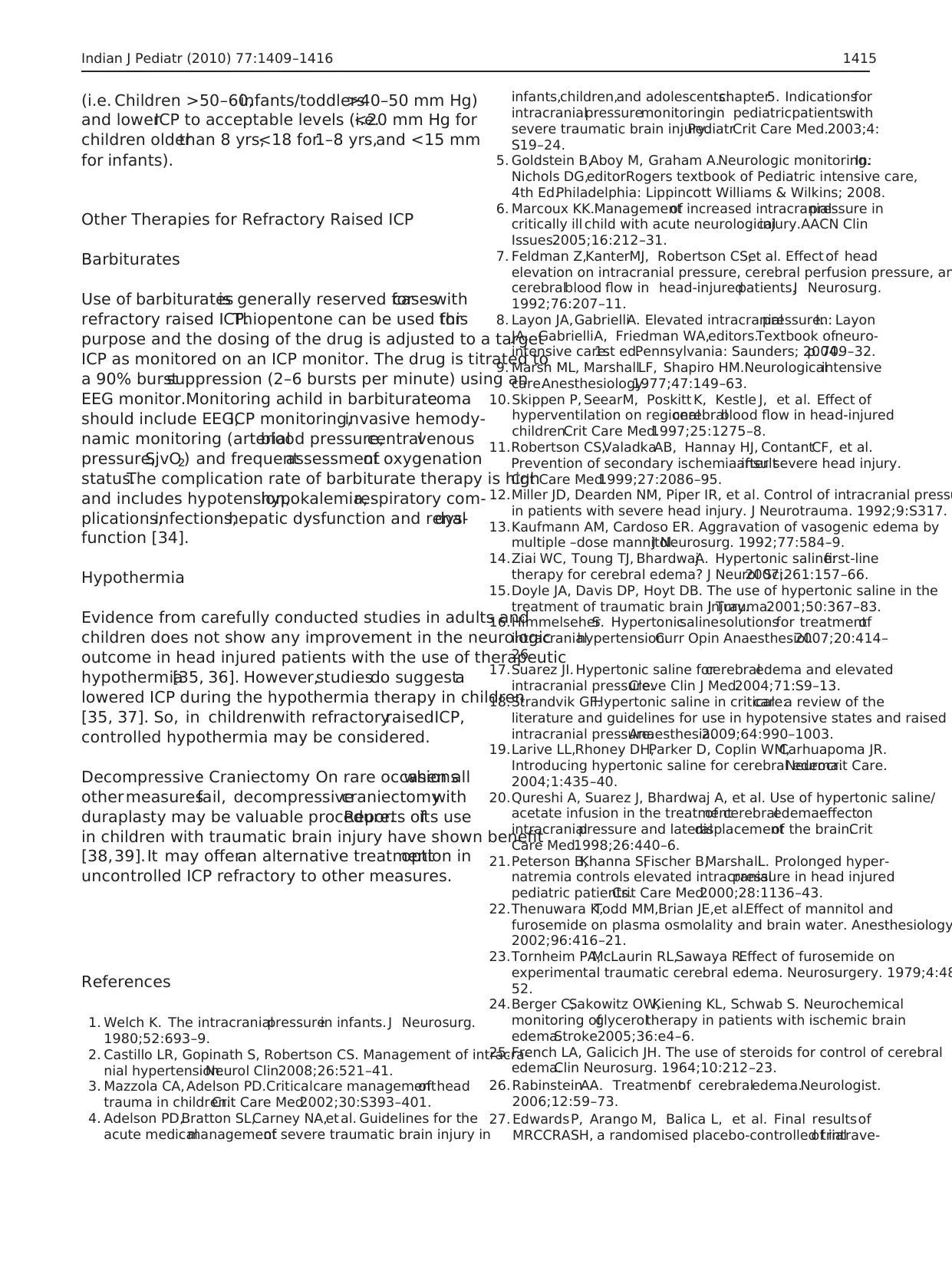
Table 3 Summary of measures to reduce intracranial pressure
1 Assessment and management of ABC’s (airway,breathing,
circulation)
2 Early intubation if; GCS <8,Evidence of herniation,Apnea,
Inability to maintain airway
3 Mild head elevation of 15–30° (Ensure that the child is
euvolemic)
4 Hyperventilation: Target PaCO2: 30–35 mm Hg (suited for acute,
sharp increases in ICP or signs of impending herniation)
5 Mannitol: Initial bolus: 0.25–1 g/kg, then 0.25–0.5 g/kg, q 2–6 h as
per requirement, up to 48 h
6 Hypertonic Saline: Preferable in presence of Hypotension,
Hypovolemia,Serum osmolality >320 mOsm/kg, Renal failure,
Dose: 0.1–1 ml/kg/hr infusion,Target Na+
−145–155 meq/L.
7 Steroids: Intracranial tumors with perilesional edema,
neurocysticerocosis with high lesion load,ADEM,
pyomeningitis,TBM, Abscess
Acetazolamide: Hydrocephalous, benign intracranial, high altitude
illness
8 Adequate sedation and analgesia
9 Prevention and treatment of seizures: use Lorazepam or
midazolam followed by phenytoin as initial choice.
10 Avoid noxious stimuli: use lignocaine prior to ET suctioning
[nebulized (4% lidocaine mixed in 0.9% saline) or intravenous
(1–2 mg/kg as 1% solution) given 90 sec prior to suctioning]
11 Control fever: antipyretics,cooling measures
12 Maintenance IV Fluids: Only isotonic or hypertonic fluids (Ringer
lactate,0.9% Saline,5% D in 0.9% NS),No Hypotonic fluids
13 Maintain blood sugar: 80–120 mg/dL
14 Refractory raised ICP:
• Heavy sedation and paralysis
• Barbiturate coma
• Hypothermia
• Decompressive craniectomy
Indian J Pediatr (2010) 77:1409–1416 1413
Minimization of Stimulation
Attemptmustbe made to reduce the number of elective
interventions thatare likely to be painfulor excessively
stimulating.Lidocaine instilled endotracheally hasbeen
shown to preventthe endotrachealsuctioning-induced
ICP increase and CPP reduction in adultswith severe
traumatic brain injury [30].It is recommended to instil
lidocaine atbody temperature,slowly,and through a fine
tube advanced into the endotracheal tube within its length
(avoid direct contact with the mucosa) [30]. Lidocaine can
be given in nebulized (usually 4% lidocaine mixed in
0.9% saline)or intravenousforms(1–2 mg/kg as1%
solution given 90 sec priorto suctioning)for the same
purpose [9].
Fluids
The main goalof fluid therapy is to maintain euvolemia,
normoglycemia and preventhyponatremia.Children with
raised ICP should receive fluids ata daily maintenance
rate,as wellas fluid boluses as indicated forhypovole-
mia, hypotension,or decreasedurine output.Mainte-
nance fluids usually consistof normalsaline with daily
requirementsof potassium chloridebased on body
weight.All fluids administeredmust be isotonicor
hypertonic(e.g. Ringer lactate,normal saline) and
hypotonic fluids mustbe avoided (e.g.0.18% saline in
5% dextrose,Isolyte P) [7]. Hyponatremiais to be
avoided and if it occurs,must be corrected slowly.
Blood Glucose
Blood glucose must be maintained between 80–120 mg/dL in
a child with raised ICP [7]. Studies in children with traumatic
brain injury have shown thathyperglycemia is associated
with poor neurological outcome and increased mortality [31].
On the otherhand,hypoglycemia isknown to induce a
systemic stressresponse and cause disturbancesin CBF,
increasing the regional CBF by as much as 300% in severe
hypoglycaemia.Hypoglycemia can also lead to neuronal
injury and therefore, should be managed aggressively.
Temperature Regulation
Maintaining normothermia is important to preventcompli-
cationsof temperature fluctuations.This is achieved by
frequent measurements of body temperature and correcting
any fluctuations using antipyretics,and assisted cooling or
heating per needed.
Prevention and Treatment of Seizures
Children with significant head injury and neuroinfections a
risk for seizures. Seizures can increase CBF and cerebral b
volume leading to increased ICP.They can also increase the
metabolic needs of the brain and predispose to ischemia [
Seizures, if clinically evident, must be treated. Given the la
of studies in children and in patients with non traumatic ra
ICP, evidence based recommendation regarding prophylac
anti-epileptic therapy are notpossible.But it is reasonable,
and a common practice is to use prophylactic anticonvulsa
for shortterm in children with raised ICP,unless indicated
otherwise [6, 26]. If available, it is prudent to use continuo
electroencephalography (EEG) to identify subclinicalseizure
activity in children with increased risk for seizures.
Anemia
Theoretically,anemia would increase CBF and secondarily
raise ICP. There have been case reports of patients with se
anemiapresenting with symptomsof raised ICP and
papilledema[32]. Though notrigorously studied,it is
common practice to maintain hemoglobin above10 g/dL
in patients with traumatic brain injury and raised ICP.
Surgical Therapy
CerebrospinalFluid Drainage CSF drainageusing a
external ventricular drainage (EVD) or ventriculoperitonea
shunt provides for an immediately effective means to lowe
ICP. In addition EVD provides a method for continuously
monitoring ICP.CSF drainage is particularly usefulin the
presence of hydrocephalus.But it may be considered even
in children withouthydrocephalus.Its effectivenessin
loweringICP has been shown to be comparableto
intravenous mannitolor hyperventilation [33].However,it
is of limited utility in diffuse brain edema with collapsed
ventricles.
Resection ofMass Lesions Surgery should be undertaken
when a lesion amenable to surgical intervention is identifie
as the primary cause ofraised ICP.Common situations
wherethis neurosurgicalinterventionis preferentially
employed are acute epidural or subdural hematomas,brain
abscess,or brain tumors.
Target of Therapy
When facilitiesfor ICP monitoringare available,the
managementis tailored to maintaining an adequate CPP
1414 Indian J Pediatr (2010) 77:1409–1416
Attemptmustbe made to reduce the number of elective
interventions thatare likely to be painfulor excessively
stimulating.Lidocaine instilled endotracheally hasbeen
shown to preventthe endotrachealsuctioning-induced
ICP increase and CPP reduction in adultswith severe
traumatic brain injury [30].It is recommended to instil
lidocaine atbody temperature,slowly,and through a fine
tube advanced into the endotracheal tube within its length
(avoid direct contact with the mucosa) [30]. Lidocaine can
be given in nebulized (usually 4% lidocaine mixed in
0.9% saline)or intravenousforms(1–2 mg/kg as1%
solution given 90 sec priorto suctioning)for the same
purpose [9].
Fluids
The main goalof fluid therapy is to maintain euvolemia,
normoglycemia and preventhyponatremia.Children with
raised ICP should receive fluids ata daily maintenance
rate,as wellas fluid boluses as indicated forhypovole-
mia, hypotension,or decreasedurine output.Mainte-
nance fluids usually consistof normalsaline with daily
requirementsof potassium chloridebased on body
weight.All fluids administeredmust be isotonicor
hypertonic(e.g. Ringer lactate,normal saline) and
hypotonic fluids mustbe avoided (e.g.0.18% saline in
5% dextrose,Isolyte P) [7]. Hyponatremiais to be
avoided and if it occurs,must be corrected slowly.
Blood Glucose
Blood glucose must be maintained between 80–120 mg/dL in
a child with raised ICP [7]. Studies in children with traumatic
brain injury have shown thathyperglycemia is associated
with poor neurological outcome and increased mortality [31].
On the otherhand,hypoglycemia isknown to induce a
systemic stressresponse and cause disturbancesin CBF,
increasing the regional CBF by as much as 300% in severe
hypoglycaemia.Hypoglycemia can also lead to neuronal
injury and therefore, should be managed aggressively.
Temperature Regulation
Maintaining normothermia is important to preventcompli-
cationsof temperature fluctuations.This is achieved by
frequent measurements of body temperature and correcting
any fluctuations using antipyretics,and assisted cooling or
heating per needed.
Prevention and Treatment of Seizures
Children with significant head injury and neuroinfections a
risk for seizures. Seizures can increase CBF and cerebral b
volume leading to increased ICP.They can also increase the
metabolic needs of the brain and predispose to ischemia [
Seizures, if clinically evident, must be treated. Given the la
of studies in children and in patients with non traumatic ra
ICP, evidence based recommendation regarding prophylac
anti-epileptic therapy are notpossible.But it is reasonable,
and a common practice is to use prophylactic anticonvulsa
for shortterm in children with raised ICP,unless indicated
otherwise [6, 26]. If available, it is prudent to use continuo
electroencephalography (EEG) to identify subclinicalseizure
activity in children with increased risk for seizures.
Anemia
Theoretically,anemia would increase CBF and secondarily
raise ICP. There have been case reports of patients with se
anemiapresenting with symptomsof raised ICP and
papilledema[32]. Though notrigorously studied,it is
common practice to maintain hemoglobin above10 g/dL
in patients with traumatic brain injury and raised ICP.
Surgical Therapy
CerebrospinalFluid Drainage CSF drainageusing a
external ventricular drainage (EVD) or ventriculoperitonea
shunt provides for an immediately effective means to lowe
ICP. In addition EVD provides a method for continuously
monitoring ICP.CSF drainage is particularly usefulin the
presence of hydrocephalus.But it may be considered even
in children withouthydrocephalus.Its effectivenessin
loweringICP has been shown to be comparableto
intravenous mannitolor hyperventilation [33].However,it
is of limited utility in diffuse brain edema with collapsed
ventricles.
Resection ofMass Lesions Surgery should be undertaken
when a lesion amenable to surgical intervention is identifie
as the primary cause ofraised ICP.Common situations
wherethis neurosurgicalinterventionis preferentially
employed are acute epidural or subdural hematomas,brain
abscess,or brain tumors.
Target of Therapy
When facilitiesfor ICP monitoringare available,the
managementis tailored to maintaining an adequate CPP
1414 Indian J Pediatr (2010) 77:1409–1416
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
(i.e. Children >50–60,infants/toddlers>40–50 mm Hg)
and lowerICP to acceptable levels (i.e.<20 mm Hg for
children olderthan 8 yrs,<18 for1–8 yrs,and <15 mm
for infants).
Other Therapies for Refractory Raised ICP
Barbiturates
Use of barbituratesis generally reserved forcaseswith
refractory raised ICP.Thiopentone can be used forthis
purpose and the dosing of the drug is adjusted to a target
ICP as monitored on an ICP monitor. The drug is titrated to
a 90% burstsuppression (2–6 bursts per minute) using an
EEG monitor.Monitoring achild in barbituratecoma
should include EEG,ICP monitoring,invasive hemody-
namic monitoring (arterialblood pressure,centralvenous
pressure,SjvO2) and frequentassessmentof oxygenation
status.The complication rate of barbiturate therapy is high
and includes hypotension,hypokalemia,respiratory com-
plications,infections,hepatic dysfunction and renaldys-
function [34].
Hypothermia
Evidence from carefully conducted studies in adults and
children does not show any improvement in the neurologic
outcome in head injured patients with the use of therapeutic
hypothermia[35, 36]. However,studiesdo suggesta
lowered ICP during the hypothermia therapy in children
[35, 37]. So, in childrenwith refractoryraisedICP,
controlled hypothermia may be considered.
Decompressive Craniectomy On rare occasionswhen all
other measuresfail, decompressivecraniectomywith
duraplasty may be valuable procedure.Reports ofits use
in children with traumatic brain injury have shown benefit
[38,39].It may offeran alternative treatmentoption in
uncontrolled ICP refractory to other measures.
References
1. Welch K. The intracranialpressurein infants. J Neurosurg.
1980;52:693–9.
2. Castillo LR, Gopinath S, Robertson CS. Management of intracra-
nial hypertension.Neurol Clin.2008;26:521–41.
3. Mazzola CA, Adelson PD.Criticalcare managementof head
trauma in children.Crit Care Med.2002;30:S393–401.
4. Adelson PD,Bratton SL,Carney NA,et al. Guidelines for the
acute medicalmanagementof severe traumatic brain injury in
infants,children,and adolescents:chapter5. Indicationsfor
intracranialpressuremonitoringin pediatricpatientswith
severe traumatic brain injury.PediatrCrit Care Med.2003;4:
S19–24.
5. Goldstein B,Aboy M, Graham A.Neurologic monitoring.In:
Nichols DG,editor.Rogers textbook of Pediatric intensive care,
4th Ed.Philadelphia: Lippincott Williams & Wilkins; 2008.
6. Marcoux KK.Managementof increased intracranialpressure in
critically ill child with acute neurologicalinjury.AACN Clin
Issues.2005;16:212–31.
7. Feldman Z,KanterMJ, Robertson CS,et al. Effect of head
elevation on intracranial pressure, cerebral perfusion pressure, an
cerebralblood flow in head-injuredpatients.J Neurosurg.
1992;76:207–11.
8. Layon JA,GabrielliA. Elevated intracranialpressure.In: Layon
JA, GabrielliA, Friedman WA,editors.Textbook ofneuro-
intensive care.1st ed.Pennsylvania: Saunders; 2004.p. 709–32.
9. Marsh ML, MarshallLF, Shapiro HM.Neurologicalintensive
care.Anesthesiology.1977;47:149–63.
10.Skippen P, SeearM, Poskitt K, Kestle J, et al. Effect of
hyperventilation on regionalcerebralblood flow in head-injured
children.Crit Care Med.1997;25:1275–8.
11.Robertson CS,ValadkaAB, Hannay HJ, ContantCF, et al.
Prevention of secondary ischemia insultafter severe head injury.
Crit Care Med.1999;27:2086–95.
12.Miller JD, Dearden NM, Piper IR, et al. Control of intracranial pressu
in patients with severe head injury. J Neurotrauma. 1992;9:S317.
13.Kaufmann AM, Cardoso ER. Aggravation of vasogenic edema by
multiple –dose mannitol.J Neurosurg. 1992;77:584–9.
14.Ziai WC, Toung TJ, BhardwajA. Hypertonic saline:first-line
therapy for cerebral edema? J Neurol Sci.2007;261:157–66.
15.Doyle JA, Davis DP, Hoyt DB. The use of hypertonic saline in the
treatment of traumatic brain injury.J Trauma.2001;50:367–83.
16.HimmelseherS. Hypertonicsalinesolutionsfor treatmentof
intracranialhypertension.Curr Opin Anaesthesiol.2007;20:414–
26.
17.Suarez JI. Hypertonic saline forcerebraledema and elevated
intracranial pressure.Cleve Clin J Med.2004;71:S9–13.
18.Strandvik GF.Hypertonic saline in criticalcare:a review of the
literature and guidelines for use in hypotensive states and raised
intracranial pressure.Anaesthesia.2009;64:990–1003.
19.Larive LL,Rhoney DH,Parker D, Coplin WM,Carhuapoma JR.
Introducing hypertonic saline for cerebral edema.Neurocrit Care.
2004;1:435–40.
20.Qureshi A, Suarez J, Bhardwaj A, et al. Use of hypertonic saline/
acetate infusion in the treatmentof cerebraledema:effecton
intracranialpressure and lateraldisplacementof the brain.Crit
Care Med.1998;26:440–6.
21.Peterson B,Khanna S,Fischer B,MarshallL. Prolonged hyper-
natremia controls elevated intracranialpressure in head injured
pediatric patients.Crit Care Med.2000;28:1136–43.
22.Thenuwara K,Todd MM,Brian JE,et al.Effect of mannitol and
furosemide on plasma osmolality and brain water. Anesthesiology
2002;96:416–21.
23.Tornheim PA,McLaurin RL,Sawaya R.Effect of furosemide on
experimental traumatic cerebral edema. Neurosurgery. 1979;4:48
52.
24.Berger C,Sakowitz OW,Kiening KL, Schwab S. Neurochemical
monitoring ofglyceroltherapy in patients with ischemic brain
edema.Stroke.2005;36:e4–6.
25.French LA, Galicich JH. The use of steroids for control of cerebral
edema.Clin Neurosurg. 1964;10:212–23.
26. RabinsteinAA. Treatmentof cerebraledema.Neurologist.
2006;12:59–73.
27. Edwards P, Arango M, Balica L, et al. Final resultsof
MRCCRASH, a randomised placebo-controlled trialof intrave-
Indian J Pediatr (2010) 77:1409–1416 1415
and lowerICP to acceptable levels (i.e.<20 mm Hg for
children olderthan 8 yrs,<18 for1–8 yrs,and <15 mm
for infants).
Other Therapies for Refractory Raised ICP
Barbiturates
Use of barbituratesis generally reserved forcaseswith
refractory raised ICP.Thiopentone can be used forthis
purpose and the dosing of the drug is adjusted to a target
ICP as monitored on an ICP monitor. The drug is titrated to
a 90% burstsuppression (2–6 bursts per minute) using an
EEG monitor.Monitoring achild in barbituratecoma
should include EEG,ICP monitoring,invasive hemody-
namic monitoring (arterialblood pressure,centralvenous
pressure,SjvO2) and frequentassessmentof oxygenation
status.The complication rate of barbiturate therapy is high
and includes hypotension,hypokalemia,respiratory com-
plications,infections,hepatic dysfunction and renaldys-
function [34].
Hypothermia
Evidence from carefully conducted studies in adults and
children does not show any improvement in the neurologic
outcome in head injured patients with the use of therapeutic
hypothermia[35, 36]. However,studiesdo suggesta
lowered ICP during the hypothermia therapy in children
[35, 37]. So, in childrenwith refractoryraisedICP,
controlled hypothermia may be considered.
Decompressive Craniectomy On rare occasionswhen all
other measuresfail, decompressivecraniectomywith
duraplasty may be valuable procedure.Reports ofits use
in children with traumatic brain injury have shown benefit
[38,39].It may offeran alternative treatmentoption in
uncontrolled ICP refractory to other measures.
References
1. Welch K. The intracranialpressurein infants. J Neurosurg.
1980;52:693–9.
2. Castillo LR, Gopinath S, Robertson CS. Management of intracra-
nial hypertension.Neurol Clin.2008;26:521–41.
3. Mazzola CA, Adelson PD.Criticalcare managementof head
trauma in children.Crit Care Med.2002;30:S393–401.
4. Adelson PD,Bratton SL,Carney NA,et al. Guidelines for the
acute medicalmanagementof severe traumatic brain injury in
infants,children,and adolescents:chapter5. Indicationsfor
intracranialpressuremonitoringin pediatricpatientswith
severe traumatic brain injury.PediatrCrit Care Med.2003;4:
S19–24.
5. Goldstein B,Aboy M, Graham A.Neurologic monitoring.In:
Nichols DG,editor.Rogers textbook of Pediatric intensive care,
4th Ed.Philadelphia: Lippincott Williams & Wilkins; 2008.
6. Marcoux KK.Managementof increased intracranialpressure in
critically ill child with acute neurologicalinjury.AACN Clin
Issues.2005;16:212–31.
7. Feldman Z,KanterMJ, Robertson CS,et al. Effect of head
elevation on intracranial pressure, cerebral perfusion pressure, an
cerebralblood flow in head-injuredpatients.J Neurosurg.
1992;76:207–11.
8. Layon JA,GabrielliA. Elevated intracranialpressure.In: Layon
JA, GabrielliA, Friedman WA,editors.Textbook ofneuro-
intensive care.1st ed.Pennsylvania: Saunders; 2004.p. 709–32.
9. Marsh ML, MarshallLF, Shapiro HM.Neurologicalintensive
care.Anesthesiology.1977;47:149–63.
10.Skippen P, SeearM, Poskitt K, Kestle J, et al. Effect of
hyperventilation on regionalcerebralblood flow in head-injured
children.Crit Care Med.1997;25:1275–8.
11.Robertson CS,ValadkaAB, Hannay HJ, ContantCF, et al.
Prevention of secondary ischemia insultafter severe head injury.
Crit Care Med.1999;27:2086–95.
12.Miller JD, Dearden NM, Piper IR, et al. Control of intracranial pressu
in patients with severe head injury. J Neurotrauma. 1992;9:S317.
13.Kaufmann AM, Cardoso ER. Aggravation of vasogenic edema by
multiple –dose mannitol.J Neurosurg. 1992;77:584–9.
14.Ziai WC, Toung TJ, BhardwajA. Hypertonic saline:first-line
therapy for cerebral edema? J Neurol Sci.2007;261:157–66.
15.Doyle JA, Davis DP, Hoyt DB. The use of hypertonic saline in the
treatment of traumatic brain injury.J Trauma.2001;50:367–83.
16.HimmelseherS. Hypertonicsalinesolutionsfor treatmentof
intracranialhypertension.Curr Opin Anaesthesiol.2007;20:414–
26.
17.Suarez JI. Hypertonic saline forcerebraledema and elevated
intracranial pressure.Cleve Clin J Med.2004;71:S9–13.
18.Strandvik GF.Hypertonic saline in criticalcare:a review of the
literature and guidelines for use in hypotensive states and raised
intracranial pressure.Anaesthesia.2009;64:990–1003.
19.Larive LL,Rhoney DH,Parker D, Coplin WM,Carhuapoma JR.
Introducing hypertonic saline for cerebral edema.Neurocrit Care.
2004;1:435–40.
20.Qureshi A, Suarez J, Bhardwaj A, et al. Use of hypertonic saline/
acetate infusion in the treatmentof cerebraledema:effecton
intracranialpressure and lateraldisplacementof the brain.Crit
Care Med.1998;26:440–6.
21.Peterson B,Khanna S,Fischer B,MarshallL. Prolonged hyper-
natremia controls elevated intracranialpressure in head injured
pediatric patients.Crit Care Med.2000;28:1136–43.
22.Thenuwara K,Todd MM,Brian JE,et al.Effect of mannitol and
furosemide on plasma osmolality and brain water. Anesthesiology
2002;96:416–21.
23.Tornheim PA,McLaurin RL,Sawaya R.Effect of furosemide on
experimental traumatic cerebral edema. Neurosurgery. 1979;4:48
52.
24.Berger C,Sakowitz OW,Kiening KL, Schwab S. Neurochemical
monitoring ofglyceroltherapy in patients with ischemic brain
edema.Stroke.2005;36:e4–6.
25.French LA, Galicich JH. The use of steroids for control of cerebral
edema.Clin Neurosurg. 1964;10:212–23.
26. RabinsteinAA. Treatmentof cerebraledema.Neurologist.
2006;12:59–73.
27. Edwards P, Arango M, Balica L, et al. Final resultsof
MRCCRASH, a randomised placebo-controlled trialof intrave-
Indian J Pediatr (2010) 77:1409–1416 1415
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
nouscorticosteroid in adultswith head injury outcomesat 6
months.Lancet.2005;365:1957–9.
28.Feigin VL, Anderson N, Rinkel GJ, Algra A, van Gijn J,
BennettDA. Corticosteroidsfor aneurysmalsubarachnoid
haemorrhage and primary intracerebralhaemorrhage.Cochrane
Database SystRev 2005;CD004583.
29.Hoffman SL, Rustama D, Punjabi NH, et al. High-dose dexameth-
asone in quinine-treated patients with cerebralmalaria:a double-
blind, placebo-controlled trial. J Infect Dis. 1988;158:325–31.
30.Bilitta F,Branca G,Lam A, Cuzzone V,Doronzio A,Rosa G.
Endotraceallidocainein preventingendotrachealsuctioning
induced changesin cerebralhemodynamicsin patientswith
severe head trauma.Neurocrit Care.2008;8:241–6.
31.Cochran A, Scaife ER, Hansen KW, Downey EC. Hyperglycemia
and outcomes from pediatric traumatic brain injury.J Trauma.
2003;55:1035–8.
32.Biousse V,Rucker JC,Vignal C,et al.Anemia and papilledema.
Am J Ophthalmol.2003;135:437–46.
33.Fortune JB,Feustal PJ,Graca L, et al.Effect of hyperventilation,
mannitol,and ventriculostomy drainage on cerebralblood flow
after head injury.J Trauma.1995;39:1091–9.
34.Schalen W,Sonesson B,MesseterK, et al. Clinical outcome
and cognitive impairmentin patients with severe head injuries
treatedwith barbituratecoma. Acta Neurochir (Wien).
1992;117:153–9.
35.Hutchison JS,Ward RE,Lacroix J,et al. Hypothermia therapy
after traumaticbrain injury in children. N Engl J Med.
2008;358:2447–56.
36.Clifton GL, Miller ER, Choi SC, Levin HS, et al. Lack of effect of
induction of hypothermia after acute brain injury.N Engl J Med.
2001;344:556–63.
37.Adelson PD,Ragheb J,Kanev P,et al. Phase II clinicaltrialof
moderatehypothermiaafterseveretraumaticbrain injury in
children.Neurosurgery.2005;56:740–54.
38.BergerS, Schwarz M,Huth R. Hypertonic saline solution and
decompressive craniectomy fortreatmentof intracranialhyper-
tension in pediatricseveretraumaticbrain injury.J Trauma.
2002;53:558–63.
39.Taylor A,ButtW, Rosenfeld J,etal. A randomized trialof very
early decompressive craniectomy in children with traumatic brain
injury and sustained intracranial hypertension.Child’s Nerv Syst.
2001;17:154–62.
1416 Indian J Pediatr (2010) 77:1409–1416
months.Lancet.2005;365:1957–9.
28.Feigin VL, Anderson N, Rinkel GJ, Algra A, van Gijn J,
BennettDA. Corticosteroidsfor aneurysmalsubarachnoid
haemorrhage and primary intracerebralhaemorrhage.Cochrane
Database SystRev 2005;CD004583.
29.Hoffman SL, Rustama D, Punjabi NH, et al. High-dose dexameth-
asone in quinine-treated patients with cerebralmalaria:a double-
blind, placebo-controlled trial. J Infect Dis. 1988;158:325–31.
30.Bilitta F,Branca G,Lam A, Cuzzone V,Doronzio A,Rosa G.
Endotraceallidocainein preventingendotrachealsuctioning
induced changesin cerebralhemodynamicsin patientswith
severe head trauma.Neurocrit Care.2008;8:241–6.
31.Cochran A, Scaife ER, Hansen KW, Downey EC. Hyperglycemia
and outcomes from pediatric traumatic brain injury.J Trauma.
2003;55:1035–8.
32.Biousse V,Rucker JC,Vignal C,et al.Anemia and papilledema.
Am J Ophthalmol.2003;135:437–46.
33.Fortune JB,Feustal PJ,Graca L, et al.Effect of hyperventilation,
mannitol,and ventriculostomy drainage on cerebralblood flow
after head injury.J Trauma.1995;39:1091–9.
34.Schalen W,Sonesson B,MesseterK, et al. Clinical outcome
and cognitive impairmentin patients with severe head injuries
treatedwith barbituratecoma. Acta Neurochir (Wien).
1992;117:153–9.
35.Hutchison JS,Ward RE,Lacroix J,et al. Hypothermia therapy
after traumaticbrain injury in children. N Engl J Med.
2008;358:2447–56.
36.Clifton GL, Miller ER, Choi SC, Levin HS, et al. Lack of effect of
induction of hypothermia after acute brain injury.N Engl J Med.
2001;344:556–63.
37.Adelson PD,Ragheb J,Kanev P,et al. Phase II clinicaltrialof
moderatehypothermiaafterseveretraumaticbrain injury in
children.Neurosurgery.2005;56:740–54.
38.BergerS, Schwarz M,Huth R. Hypertonic saline solution and
decompressive craniectomy fortreatmentof intracranialhyper-
tension in pediatricseveretraumaticbrain injury.J Trauma.
2002;53:558–63.
39.Taylor A,ButtW, Rosenfeld J,etal. A randomized trialof very
early decompressive craniectomy in children with traumatic brain
injury and sustained intracranial hypertension.Child’s Nerv Syst.
2001;17:154–62.
1416 Indian J Pediatr (2010) 77:1409–1416
1 out of 8
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.
