Management Plan for a Patient with Personality Disorder and Drug Overdose
VerifiedAdded on 2023/06/07
|5
|1609
|206
AI Summary
This article presents a proposed management plan for a patient with personality disorder and drug overdose. It includes nursing diagnoses, goals, proposed interventions, and supporting evidence. The plan involves administering antidepressants, mood stabilizers, and anti-anxiety medication to lower the patient's aggressive level and improve her mental health status. The plan also includes working with the patient to improve her coping skills and social life. The rationale for the treatment recommendations is supported by evidence from various studies.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
ni er itU v s y:
AMN E :
t dentS u ID:
COURSE CODE
AMCOURSE N E
A M TSSIGN EN
AMN E :
t dentS u ID:
COURSE CODE
AMCOURSE N E
A M TSSIGN EN
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Description of the case
The case involves patient Theresa admitted for drug overdose inflicted on self. She is a victim
of stressful life events starting with traumatic childhood and intake of drugs. She undertook drug
overdose after disagreements with his boyfriend on the care given to the children. Her community
nurse is away on leave and she feels ashamed of his act and ready to mend fences and correct his
habits for the sake of his children
Demographic information
The patient is a 28 years old mother of two children aged 2 and 4 years. She has had a traumatic
past occasioned with intake of drugs, abuse. She has disagreed with her boyfriend on the issue of
children as the boyfriend doesn’t treat the children well.
The setting of treatment –
Inpatient – The patient has been admitted to the health facility emergency ward and
currently receives care.
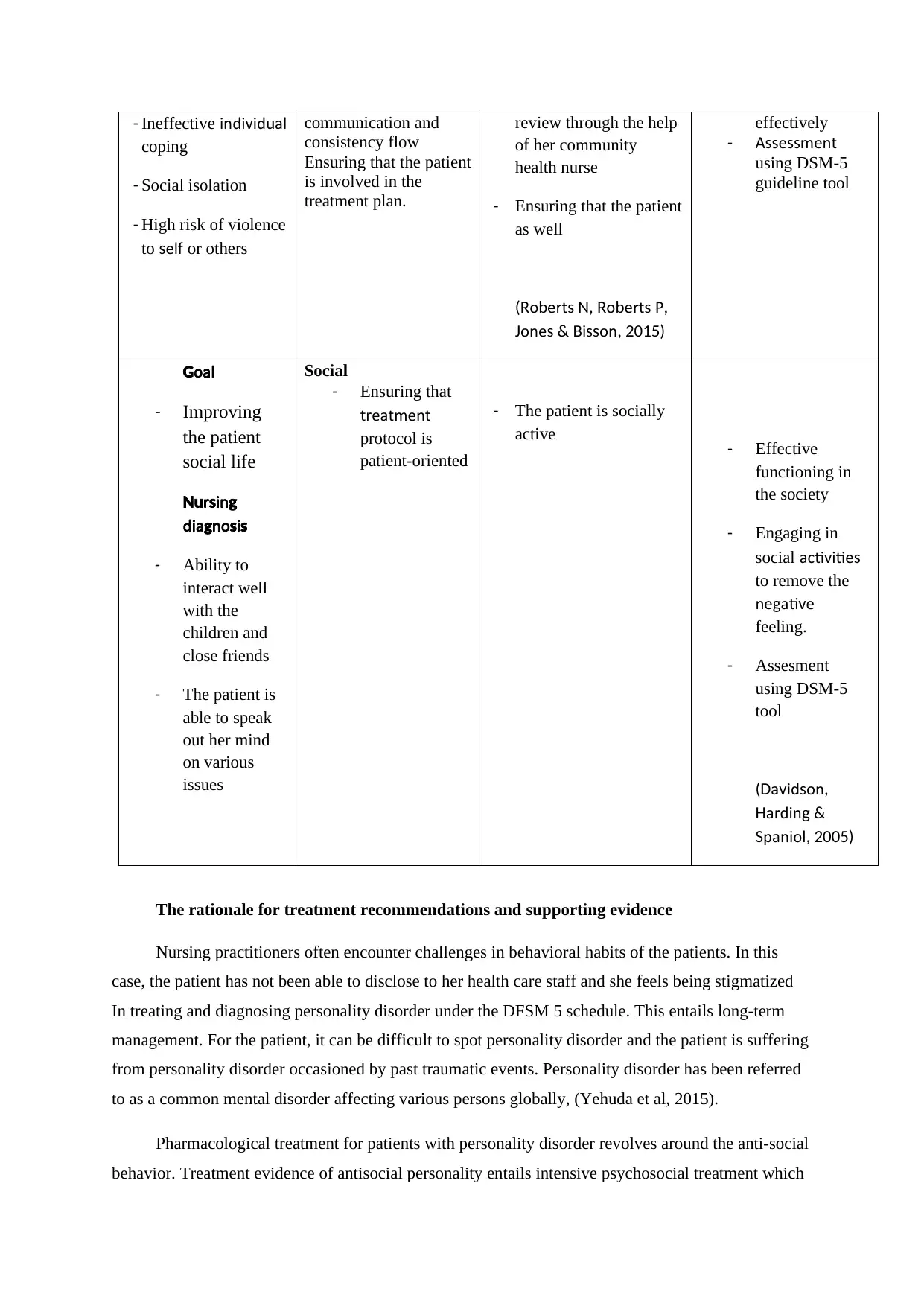
Template for the proposed management plan
Nursing Diagnoses
(provide at least
three)
Proposed intervention
for each diagnosis or
issue identified
Goals identified by the
nurse for the next 3
months
Evaluation tools and
expected outcome
Goal
- Lowering the
aggressive
level of the
patient
Nursing
diagnosis
- Administration of
antidepressants
- Mood stabilizers
administration
- Anti-anxiety
disorder
medication
Biological
Administering
antidepressants for the
patient is key in
enabling anti-depressive
mood
Mood stabilizers ensure
that the patient is well
and has a good mood
always
Anti-anxiety medication
for the patient is crucial
in ensuring agitation and
insomnia is regulated.
(Rauch et al, 2015)
-Regular intake of medicines
-Patient having a positive mood always
-Relaxed anxiety levels for
the patient
- Physical examination
of the patient through
in-depth discussion
and questions asked.
- Conducting a
psychiatric evaluation
which assesses
thoughts, behavior,
and feelings which is
crucial in pinpointing
the diagnosis
- Assessment can be
done using Diagnostic
criteria using the DS,
-5 c ed les h u s to assess
the level of treatment
for the patient.
Goal
Improving mental
health status
Nursing diagnosis
Psychological
Working with the client
in order to improve the
coping skills and to also
enable identification of
coping skills
Keeping clear
- Ensuring that the patient
is active and willing to
conclude to t eh
treatment plan.
- Conducting bi-monthly
It is expected
that that the
patient will have
peace of mind
and able to
control her
emotions
The case involves patient Theresa admitted for drug overdose inflicted on self. She is a victim
of stressful life events starting with traumatic childhood and intake of drugs. She undertook drug
overdose after disagreements with his boyfriend on the care given to the children. Her community
nurse is away on leave and she feels ashamed of his act and ready to mend fences and correct his
habits for the sake of his children
Demographic information
The patient is a 28 years old mother of two children aged 2 and 4 years. She has had a traumatic
past occasioned with intake of drugs, abuse. She has disagreed with her boyfriend on the issue of
children as the boyfriend doesn’t treat the children well.
The setting of treatment –
Inpatient – The patient has been admitted to the health facility emergency ward and
currently receives care.
Template for the proposed management plan
Nursing Diagnoses
(provide at least
three)
Proposed intervention
for each diagnosis or
issue identified
Goals identified by the
nurse for the next 3
months
Evaluation tools and
expected outcome
Goal
- Lowering the
aggressive
level of the
patient
Nursing
diagnosis
- Administration of
antidepressants
- Mood stabilizers
administration
- Anti-anxiety
disorder
medication
Biological
Administering
antidepressants for the
patient is key in
enabling anti-depressive
mood
Mood stabilizers ensure
that the patient is well
and has a good mood
always
Anti-anxiety medication
for the patient is crucial
in ensuring agitation and
insomnia is regulated.
(Rauch et al, 2015)
-Regular intake of medicines
-Patient having a positive mood always
-Relaxed anxiety levels for
the patient
- Physical examination
of the patient through
in-depth discussion
and questions asked.
- Conducting a
psychiatric evaluation
which assesses
thoughts, behavior,
and feelings which is
crucial in pinpointing
the diagnosis
- Assessment can be
done using Diagnostic
criteria using the DS,
-5 c ed les h u s to assess
the level of treatment
for the patient.
Goal
Improving mental
health status
Nursing diagnosis
Psychological
Working with the client
in order to improve the
coping skills and to also
enable identification of
coping skills
Keeping clear
- Ensuring that the patient
is active and willing to
conclude to t eh
treatment plan.
- Conducting bi-monthly
It is expected
that that the
patient will have
peace of mind
and able to
control her
emotions
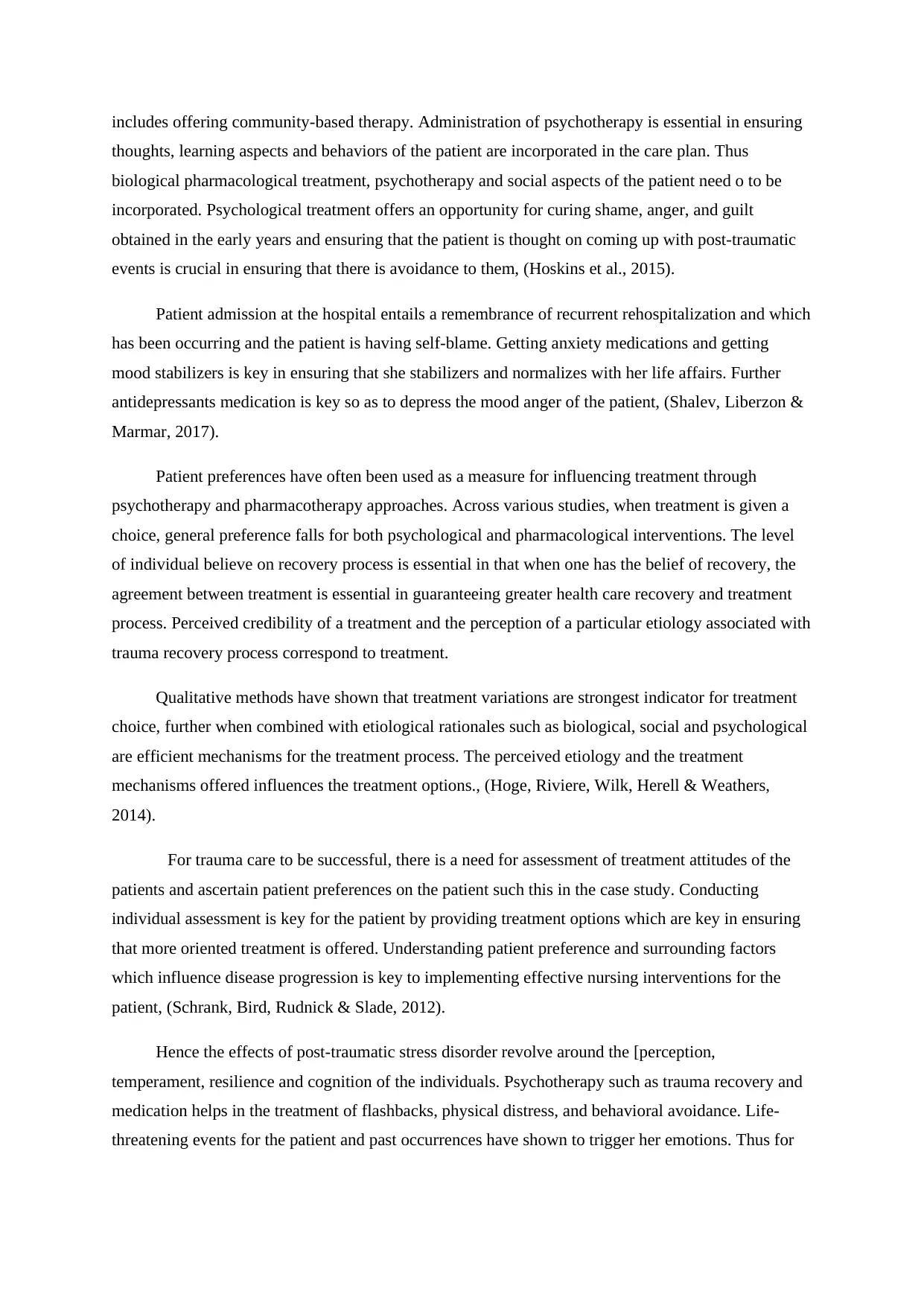
- Ineffective indi id alv u
coping
- Social isolation
- High risk of violence
to els f or others
communication and
consistency flow
Ensuring that the patient
is involved in the
treatment plan.
review through the help
of her community
health nurse
- Ensuring that the patient
as well
o ert o ert P(R b s N, R b s ,
one i onJ s & B ss , 2015)
effectively
- A e mentss ss
using DSM-5
guideline tool
oalG
- Improving
the patient
social life
r inNu s g
dia no ig s s
- Ability to
interact well
with the
children and
close friends
- The patient is
able to speak
out her mind
on various
issues
Social
- Ensuring that
treatment
protocol is
patient-oriented
- The patient is socially
active - Effective
functioning in
the society
- Engaging in
social acti itiev s
to remove the
ne ati eg v
feeling.
- Assesment
using DSM-5
tool
a id on(D v s ,
ardinH g &
paniolS , 2005)
The rationale for treatment recommendations and supporting evidence
Nursing practitioners often encounter challenges in behavioral habits of the patients. In this
case, the patient has not been able to disclose to her health care staff and she feels being stigmatized
In treating and diagnosing personality disorder under the DFSM 5 schedule. This entails long-term
management. For the patient, it can be difficult to spot personality disorder and the patient is suffering
from personality disorder occasioned by past traumatic events. Personality disorder has been referred
to as a common mental disorder affecting various persons globally, (Yehuda et al, 2015).
Pharmacological treatment for patients with personality disorder revolves around the anti-social
behavior. Treatment evidence of antisocial personality entails intensive psychosocial treatment which
coping
- Social isolation
- High risk of violence
to els f or others
communication and
consistency flow
Ensuring that the patient
is involved in the
treatment plan.
review through the help
of her community
health nurse
- Ensuring that the patient
as well
o ert o ert P(R b s N, R b s ,
one i onJ s & B ss , 2015)
effectively
- A e mentss ss
using DSM-5
guideline tool
oalG
- Improving
the patient
social life
r inNu s g
dia no ig s s
- Ability to
interact well
with the
children and
close friends
- The patient is
able to speak
out her mind
on various
issues
Social
- Ensuring that
treatment
protocol is
patient-oriented
- The patient is socially
active - Effective
functioning in
the society
- Engaging in
social acti itiev s
to remove the
ne ati eg v
feeling.
- Assesment
using DSM-5
tool
a id on(D v s ,
ardinH g &
paniolS , 2005)
The rationale for treatment recommendations and supporting evidence
Nursing practitioners often encounter challenges in behavioral habits of the patients. In this
case, the patient has not been able to disclose to her health care staff and she feels being stigmatized
In treating and diagnosing personality disorder under the DFSM 5 schedule. This entails long-term
management. For the patient, it can be difficult to spot personality disorder and the patient is suffering
from personality disorder occasioned by past traumatic events. Personality disorder has been referred
to as a common mental disorder affecting various persons globally, (Yehuda et al, 2015).
Pharmacological treatment for patients with personality disorder revolves around the anti-social
behavior. Treatment evidence of antisocial personality entails intensive psychosocial treatment which
includes offering community-based therapy. Administration of psychotherapy is essential in ensuring
thoughts, learning aspects and behaviors of the patient are incorporated in the care plan. Thus
biological pharmacological treatment, psychotherapy and social aspects of the patient need o to be
incorporated. Psychological treatment offers an opportunity for curing shame, anger, and guilt
obtained in the early years and ensuring that the patient is thought on coming up with post-traumatic
events is crucial in ensuring that there is avoidance to them, (Hoskins et al., 2015).
Patient admission at the hospital entails a remembrance of recurrent rehospitalization and which
has been occurring and the patient is having self-blame. Getting anxiety medications and getting
mood stabilizers is key in ensuring that she stabilizers and normalizes with her life affairs. Further
antidepressants medication is key so as to depress the mood anger of the patient, (Shalev, Liberzon &
Marmar, 2017).
Patient preferences have often been used as a measure for influencing treatment through
psychotherapy and pharmacotherapy approaches. Across various studies, when treatment is given a
choice, general preference falls for both psychological and pharmacological interventions. The level
of individual believe on recovery process is essential in that when one has the belief of recovery, the
agreement between treatment is essential in guaranteeing greater health care recovery and treatment
process. Perceived credibility of a treatment and the perception of a particular etiology associated with
trauma recovery process correspond to treatment.
Qualitative methods have shown that treatment variations are strongest indicator for treatment
choice, further when combined with etiological rationales such as biological, social and psychological
are efficient mechanisms for the treatment process. The perceived etiology and the treatment
mechanisms offered influences the treatment options., (Hoge, Riviere, Wilk, Herell & Weathers,
2014).
For trauma care to be successful, there is a need for assessment of treatment attitudes of the
patients and ascertain patient preferences on the patient such this in the case study. Conducting
individual assessment is key for the patient by providing treatment options which are key in ensuring
that more oriented treatment is offered. Understanding patient preference and surrounding factors
which influence disease progression is key to implementing effective nursing interventions for the
patient, (Schrank, Bird, Rudnick & Slade, 2012).
Hence the effects of post-traumatic stress disorder revolve around the [perception,
temperament, resilience and cognition of the individuals. Psychotherapy such as trauma recovery and
medication helps in the treatment of flashbacks, physical distress, and behavioral avoidance. Life-
threatening events for the patient and past occurrences have shown to trigger her emotions. Thus for
thoughts, learning aspects and behaviors of the patient are incorporated in the care plan. Thus
biological pharmacological treatment, psychotherapy and social aspects of the patient need o to be
incorporated. Psychological treatment offers an opportunity for curing shame, anger, and guilt
obtained in the early years and ensuring that the patient is thought on coming up with post-traumatic
events is crucial in ensuring that there is avoidance to them, (Hoskins et al., 2015).
Patient admission at the hospital entails a remembrance of recurrent rehospitalization and which
has been occurring and the patient is having self-blame. Getting anxiety medications and getting
mood stabilizers is key in ensuring that she stabilizers and normalizes with her life affairs. Further
antidepressants medication is key so as to depress the mood anger of the patient, (Shalev, Liberzon &
Marmar, 2017).
Patient preferences have often been used as a measure for influencing treatment through
psychotherapy and pharmacotherapy approaches. Across various studies, when treatment is given a
choice, general preference falls for both psychological and pharmacological interventions. The level
of individual believe on recovery process is essential in that when one has the belief of recovery, the
agreement between treatment is essential in guaranteeing greater health care recovery and treatment
process. Perceived credibility of a treatment and the perception of a particular etiology associated with
trauma recovery process correspond to treatment.
Qualitative methods have shown that treatment variations are strongest indicator for treatment
choice, further when combined with etiological rationales such as biological, social and psychological
are efficient mechanisms for the treatment process. The perceived etiology and the treatment
mechanisms offered influences the treatment options., (Hoge, Riviere, Wilk, Herell & Weathers,
2014).
For trauma care to be successful, there is a need for assessment of treatment attitudes of the
patients and ascertain patient preferences on the patient such this in the case study. Conducting
individual assessment is key for the patient by providing treatment options which are key in ensuring
that more oriented treatment is offered. Understanding patient preference and surrounding factors
which influence disease progression is key to implementing effective nursing interventions for the
patient, (Schrank, Bird, Rudnick & Slade, 2012).
Hence the effects of post-traumatic stress disorder revolve around the [perception,
temperament, resilience and cognition of the individuals. Psychotherapy such as trauma recovery and
medication helps in the treatment of flashbacks, physical distress, and behavioral avoidance. Life-
threatening events for the patient and past occurrences have shown to trigger her emotions. Thus for
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
her recovery plan, a detailed evaluation plan needs to entail plans which meet the uniqueness of the
portrayed trauma
References
Davidson, L. E., Harding, C. E., & Spaniol, L. E. (2005). Recovery from severe mental
illnesses: Research evidence and implications for practice, Vol 1. Center for Psychiatric
Rehabilitation/Boston U.
Hoge, C. W., Riviere, L. A., Wilk, J. E., Herrell, R. K., & Weathers, F. W. (2014). The
prevalence of post-traumatic stress disorder (PTSD) in US combat soldiers: a head-to-
head comparison of DSM-5 versus DSM-IV-TR symptom criteria with the PTSD
checklist. The Lancet Psychiatry, 1(4), 269-277.
Hoskins, M., Pearce, J., Bethell, A., Dankova, L., Barbui, C., Tol, W. A., ... & Bisson, J. I.
(2015). Pharmacotherapy for post-traumatic stress disorder: systematic review and
meta-analysis. The British Journal of Psychiatry, 206(2), 93-100.
Rauch, S. A., King, A. P., Abelson, J., Tuerk, P. W., Smith, E., Rothbaum, B. O., ... &
Liberzon, I. (2015). Biological and symptom changes in posttraumatic stress disorder
treatment: a randomized clinical trial. Depression and anxiety, 32(3), 204-212.
Roberts, N. P., Roberts, P. A., Jones, N., & Bisson, J. I. (2015). Psychological interventions
for post-traumatic stress disorder and comorbid substance use disorder: A systematic
review and meta-analysis. Clinical psychology review, 38, 25-38.
Schrank, B., Bird, V., Rudnick, A., & Slade, M. (2012). Determinants, self-management
strategies, and interventions for hope in people with mental disorders: a systematic
search and narrative review. Social science & medicine, 74(4), 554-564.
Shalev, A., Liberzon, I., & Marmar, C. (2017). Post-traumatic stress disorder. New England
Journal of Medicine, 376(25), 2459-2469.
Yehuda, R., Hoge, C. W., McFarlane, A. C., Vermetten, E., Lanius, R. A., Nievergelt, C.
M., ... & Hyman, S. E. (2015). Post-traumatic stress disorder. Nature Reviews Disease
Primers, 1, 15057.
portrayed trauma
References
Davidson, L. E., Harding, C. E., & Spaniol, L. E. (2005). Recovery from severe mental
illnesses: Research evidence and implications for practice, Vol 1. Center for Psychiatric
Rehabilitation/Boston U.
Hoge, C. W., Riviere, L. A., Wilk, J. E., Herrell, R. K., & Weathers, F. W. (2014). The
prevalence of post-traumatic stress disorder (PTSD) in US combat soldiers: a head-to-
head comparison of DSM-5 versus DSM-IV-TR symptom criteria with the PTSD
checklist. The Lancet Psychiatry, 1(4), 269-277.
Hoskins, M., Pearce, J., Bethell, A., Dankova, L., Barbui, C., Tol, W. A., ... & Bisson, J. I.
(2015). Pharmacotherapy for post-traumatic stress disorder: systematic review and
meta-analysis. The British Journal of Psychiatry, 206(2), 93-100.
Rauch, S. A., King, A. P., Abelson, J., Tuerk, P. W., Smith, E., Rothbaum, B. O., ... &
Liberzon, I. (2015). Biological and symptom changes in posttraumatic stress disorder
treatment: a randomized clinical trial. Depression and anxiety, 32(3), 204-212.
Roberts, N. P., Roberts, P. A., Jones, N., & Bisson, J. I. (2015). Psychological interventions
for post-traumatic stress disorder and comorbid substance use disorder: A systematic
review and meta-analysis. Clinical psychology review, 38, 25-38.
Schrank, B., Bird, V., Rudnick, A., & Slade, M. (2012). Determinants, self-management
strategies, and interventions for hope in people with mental disorders: a systematic
search and narrative review. Social science & medicine, 74(4), 554-564.
Shalev, A., Liberzon, I., & Marmar, C. (2017). Post-traumatic stress disorder. New England
Journal of Medicine, 376(25), 2459-2469.
Yehuda, R., Hoge, C. W., McFarlane, A. C., Vermetten, E., Lanius, R. A., Nievergelt, C.
M., ... & Hyman, S. E. (2015). Post-traumatic stress disorder. Nature Reviews Disease
Primers, 1, 15057.
1 out of 5
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





