Master of Hospital Management Field Practicum Course: ATTITUDES AND BARRIERS FOR OPTIMAL HAND HYGIENE AMONG HEALTH CARE PROVIDERS in ZAYED MILITARY hospital AL BATAYEH, SHARJAH
VerifiedAdded on 2022/10/14
|22
|7086
|339
AI Summary
Master of Hospital Management Field Practicum Course (Summer 2019) AUDIT PROJECT: ATTITUDES AND BARRIERS FOR OPTIMAL HAND HYGIENE AMONG HEALTH CARE PROVIDERS in ZAYED MILITARY hospital AL BATAYEH, SHARJAH Submitted By: Amna Schmitz Aladwani 200104787 Submitted to: Prof. The practice is considered to be in the front line in prevention of health care associated infections (HCAI) and Nosocomial Infections/Hospital Acquire
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

0
Master of Hospital Management
Field Practicum Course (Summer 2019)
AUDIT PROJECT:
ATTITUDES AND BARRIERS FOR OPTIMAL HAND HYGIENE AMONG HEALTH CARE
PROVIDERS IN ZAYED MILITARY HOSPITAL AL BATAYEH, SHARJAH
Submitted By: Amna Aladwani 200104787
Submitted to: Prof. Awoniyi Awofeso
Date: 28/July/2019
Word Count: 2705 words
Abstract
Master of Hospital Management
Field Practicum Course (Summer 2019)
AUDIT PROJECT:
ATTITUDES AND BARRIERS FOR OPTIMAL HAND HYGIENE AMONG HEALTH CARE
PROVIDERS IN ZAYED MILITARY HOSPITAL AL BATAYEH, SHARJAH
Submitted By: Amna Aladwani 200104787
Submitted to: Prof. Awoniyi Awofeso
Date: 28/July/2019
Word Count: 2705 words
Abstract
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1
Introduction: “Prevention is better than cure”. Therefore, proper hands hygiene practice stands
out to be one of the measures of reducing transmission of disease to patients and to health care
providers. The practice is considered to be in the front line in prevention of health care
associated infections (HCAI) and Nosocomial Infections/Hospital Acquired Infections (Kumar,
Gupta, Kapil, Vij & Singh, 2014). Washing hands is taking a second position from hand rub to
meet the recommended standards with optimum time considered to be between 30 seconds and
one minute. The alcohol antiseptics are recommended worldwide due to their broad-spectrum
antimicrobial effects, the application process is easy and they are tolerable to many people skins
(Zayed Military Hospital - Al Batayeh, 2016). The scope of hand hygiene includes hand
washing, use of antiseptics to wash hands or rub and surgical hand antisepsis. Health care
associated infection (HCAI) is one of the most significant, and current phenomena for
discussions in health care industry. Hand hygiene was thought to be a key factor in reducing
hospital acquired infection during the initial development of healthcare system (Ducell, Fabry &
Nicoll, 2002). The present study aimed to determine hand hygiene compliance, attitude and
barriers among health care workers (HCWs).
Material & Methods: A cross sectional observational survey was conducted in 100 health care
providers from different out-patient departments at Zayed Military Hospital Al Batayeh,
Sharjah Convenience consecutive sampling technique was used to enroll HCPs. Modified hand
hygiene checklist, interview for identification of barriers was used to ascertain compliance,
attitude and barriers. Appropriate descriptive statistics was applied to compute the results.
Results: Results shows higher adherence (10%) to hand hygiene practices among faculty
followed by consultants (7.14%) and specialists (6.71%). However, the partial adherence to
hand hygiene practices was surprisingly high (63.04%) among HCWs. There was significant
difference in attitude towards hand hygiene practices among medical and nursing professionals.
Further, findings revealed that inconvenient placement of hand hygiene facility was prime
reported (85.21%) barrier for poor adherence to hand hygiene practices followed by over
burden of patient (80.87%), understaffing/overcrowding (81.73%) and hand hygiene is time
consuming activity (80.86%) HCWs.
Introduction: “Prevention is better than cure”. Therefore, proper hands hygiene practice stands
out to be one of the measures of reducing transmission of disease to patients and to health care
providers. The practice is considered to be in the front line in prevention of health care
associated infections (HCAI) and Nosocomial Infections/Hospital Acquired Infections (Kumar,
Gupta, Kapil, Vij & Singh, 2014). Washing hands is taking a second position from hand rub to
meet the recommended standards with optimum time considered to be between 30 seconds and
one minute. The alcohol antiseptics are recommended worldwide due to their broad-spectrum
antimicrobial effects, the application process is easy and they are tolerable to many people skins
(Zayed Military Hospital - Al Batayeh, 2016). The scope of hand hygiene includes hand
washing, use of antiseptics to wash hands or rub and surgical hand antisepsis. Health care
associated infection (HCAI) is one of the most significant, and current phenomena for
discussions in health care industry. Hand hygiene was thought to be a key factor in reducing
hospital acquired infection during the initial development of healthcare system (Ducell, Fabry &
Nicoll, 2002). The present study aimed to determine hand hygiene compliance, attitude and
barriers among health care workers (HCWs).
Material & Methods: A cross sectional observational survey was conducted in 100 health care
providers from different out-patient departments at Zayed Military Hospital Al Batayeh,
Sharjah Convenience consecutive sampling technique was used to enroll HCPs. Modified hand
hygiene checklist, interview for identification of barriers was used to ascertain compliance,
attitude and barriers. Appropriate descriptive statistics was applied to compute the results.
Results: Results shows higher adherence (10%) to hand hygiene practices among faculty
followed by consultants (7.14%) and specialists (6.71%). However, the partial adherence to
hand hygiene practices was surprisingly high (63.04%) among HCWs. There was significant
difference in attitude towards hand hygiene practices among medical and nursing professionals.
Further, findings revealed that inconvenient placement of hand hygiene facility was prime
reported (85.21%) barrier for poor adherence to hand hygiene practices followed by over
burden of patient (80.87%), understaffing/overcrowding (81.73%) and hand hygiene is time
consuming activity (80.86%) HCWs.
2
Conclusion & recommendation: The study concluded poor hand hygiene compliance among
HCWs. Study findings recommend improvement in existing facilities for hand hygiene and
make them readily accessible for HCWs at their respective departments to enable them to
engage in good practices which will be beneficial for them and patients.
Introduction
The Health Care Associated Infections (HCAI) trigger the main challenges to the health care
provision. This is because of the burden put on the people, families as well as health services.
HCAI is described as the infection acquired by both patients and healthcare providers while
seeking and providing treatment in the healthcare facilities respectively. HCAIs are caused by a
range of microbes like parasites, fungi, viruses and remains readily associated with bacteria. The
routes for transmission include via endogenous or exogenous infection agents. The former agents
are the infections triggered by microorganisms present in the body of patients that spread from
one to another area often via the hands of the HCWs by touching the area infected. The latter
agents sources further act as the reservoir of infections and encompass nose, skin, mouth, vagina
and gastrointestinal tract (Kurtz, 2017).
HCWs with poor HH adherence who never wash their hands in between indirect or direct with
patients might rapidly transmit potential antimicrobial resistant bacteria to the rest of the patients.
HCWs hands slowly get exposed as well as colonized by the germs and feasibly microbes as they
tend to patients. Thus, there is a surged risk of HCAI acquisition from the HCW with augmented
amount of hand contamination specifically in the Hospital lacking HH (Schwartz, Schmitz,
Safdar & Pop-Vicas, 2018).
Exogenous infections get spread because of external sources often through direct contact with
infected patients or via the surrounding. Exogenous infections sources include HCWs, patient
care equipment, visitors, as well as medical devices. Thus, HCWs hands alongside patients
remain the major trigger for HCAI spread both exogenously and endogenously to fellow patients
and HCW and visitors. It is, thus, imperative to examine the HH behavior of health care workers
in the Hospital faced with the provision of quality health care as well as patient safety
irrespective of scarce health system facilities or systems.
Conclusion & recommendation: The study concluded poor hand hygiene compliance among
HCWs. Study findings recommend improvement in existing facilities for hand hygiene and
make them readily accessible for HCWs at their respective departments to enable them to
engage in good practices which will be beneficial for them and patients.
Introduction
The Health Care Associated Infections (HCAI) trigger the main challenges to the health care
provision. This is because of the burden put on the people, families as well as health services.
HCAI is described as the infection acquired by both patients and healthcare providers while
seeking and providing treatment in the healthcare facilities respectively. HCAIs are caused by a
range of microbes like parasites, fungi, viruses and remains readily associated with bacteria. The
routes for transmission include via endogenous or exogenous infection agents. The former agents
are the infections triggered by microorganisms present in the body of patients that spread from
one to another area often via the hands of the HCWs by touching the area infected. The latter
agents sources further act as the reservoir of infections and encompass nose, skin, mouth, vagina
and gastrointestinal tract (Kurtz, 2017).
HCWs with poor HH adherence who never wash their hands in between indirect or direct with
patients might rapidly transmit potential antimicrobial resistant bacteria to the rest of the patients.
HCWs hands slowly get exposed as well as colonized by the germs and feasibly microbes as they
tend to patients. Thus, there is a surged risk of HCAI acquisition from the HCW with augmented
amount of hand contamination specifically in the Hospital lacking HH (Schwartz, Schmitz,
Safdar & Pop-Vicas, 2018).
Exogenous infections get spread because of external sources often through direct contact with
infected patients or via the surrounding. Exogenous infections sources include HCWs, patient
care equipment, visitors, as well as medical devices. Thus, HCWs hands alongside patients
remain the major trigger for HCAI spread both exogenously and endogenously to fellow patients
and HCW and visitors. It is, thus, imperative to examine the HH behavior of health care workers
in the Hospital faced with the provision of quality health care as well as patient safety
irrespective of scarce health system facilities or systems.
3
Hand Hygiene (HH) actions or practices remain cost-effective mechanisms towards the reduction
of the spread of HCAIs and have since proven extremely effective in the prevention of
transmission of microbes during the care for patients. It has since been verified that HCAIs hands
remain the major routes of HCAIs transmission. Despite this knowledge, HH remains overlooked
frequently among the HCWs specifically in the Hospitals with restricted resources. This current
study, hence, explores the HH knowledge and behaviors of private and public HCWs with focus
on the health belief model to understand the barriers and attitudes of the HCWs for optimal hand
hygiene in the Zayed Military Hospital.
The needed information or data was collected from the HCWs form the health care facility using
the structured questionnaires based on the WHO evaluation tool kit and the literature review on
the previous articles on the topic. HH knowledge of HCWs corresponded with their respective
HH behaviors and practices. Insufficient HH performance was observed in various HCWs
alongside limited HH resources availabilities from the Hospital. Private healthcare facilities
availed better HH opportunities for their HCWs, however, neither public nor private facilities
provided sufficient HH training alongside feedback on HH performance to their HCWs.
Problem Statement: HCAI remains a severe challenge which is presently faced by all Hospitals
globally irrespective of the economic state. Not solely does HCAI encompasses patient safety,
but also that of the health care workers. It remains in all HCWs interest to tackle this problem
and guarantee improved safety of patients alongside establishing suitable work surrounding for
all workers. Most specifically, since the adverse effects of HCAIs encompasses extra costs for
patients, surged resistance to the antimicrobials alongside a higher burden (financial) for the
society at large. Many HCWs in this Zayed Military Hospital are faced by the combination of
various determinants triggering a higher risk of HCAIs transmission. As noted above, such might
encompass understaffing, ineffective infrastructure with missing hygiene besides sanitation
conditions, shortage or lack of basic equipment, overcrowding of patients; all of which might be
connected to scarce financial resources.
Surveillance on health care workers HH actions and practices plays a key role towards
accomplishing safer alongside higher quality care for patients. Globally, campaigns have been
created to support prevention and control programs for infections including initiatives for HH.
Hand Hygiene (HH) actions or practices remain cost-effective mechanisms towards the reduction
of the spread of HCAIs and have since proven extremely effective in the prevention of
transmission of microbes during the care for patients. It has since been verified that HCAIs hands
remain the major routes of HCAIs transmission. Despite this knowledge, HH remains overlooked
frequently among the HCWs specifically in the Hospitals with restricted resources. This current
study, hence, explores the HH knowledge and behaviors of private and public HCWs with focus
on the health belief model to understand the barriers and attitudes of the HCWs for optimal hand
hygiene in the Zayed Military Hospital.
The needed information or data was collected from the HCWs form the health care facility using
the structured questionnaires based on the WHO evaluation tool kit and the literature review on
the previous articles on the topic. HH knowledge of HCWs corresponded with their respective
HH behaviors and practices. Insufficient HH performance was observed in various HCWs
alongside limited HH resources availabilities from the Hospital. Private healthcare facilities
availed better HH opportunities for their HCWs, however, neither public nor private facilities
provided sufficient HH training alongside feedback on HH performance to their HCWs.
Problem Statement: HCAI remains a severe challenge which is presently faced by all Hospitals
globally irrespective of the economic state. Not solely does HCAI encompasses patient safety,
but also that of the health care workers. It remains in all HCWs interest to tackle this problem
and guarantee improved safety of patients alongside establishing suitable work surrounding for
all workers. Most specifically, since the adverse effects of HCAIs encompasses extra costs for
patients, surged resistance to the antimicrobials alongside a higher burden (financial) for the
society at large. Many HCWs in this Zayed Military Hospital are faced by the combination of
various determinants triggering a higher risk of HCAIs transmission. As noted above, such might
encompass understaffing, ineffective infrastructure with missing hygiene besides sanitation
conditions, shortage or lack of basic equipment, overcrowding of patients; all of which might be
connected to scarce financial resources.
Surveillance on health care workers HH actions and practices plays a key role towards
accomplishing safer alongside higher quality care for patients. Globally, campaigns have been
created to support prevention and control programs for infections including initiatives for HH.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4
Nonetheless, solely a few hospitals manage to offer functional evaluation alongside monitoring
systems. Likely rationale for this remain the demanding alongside intensive requirements of the
national surveillance system associated with scarce resource allocation towards HCAI in these
hospitals where additional emerging health concerns and illness are accorded preference
(Kingston, Slevin, O'Connell & Dunne, 2017).
This study will emphasize on HH adherence for HCWs in Zayed Military Hospital where the
lack of enough HH resources is dominant and also marred with various HH barriers and negative
attitude of HCWs to proper HH practices.
Literature review
The provision of healthcare worldwide is always associated with a potential range of safety
problems. Yet, despite advances in healthcare systems, patients remain vulnerable to
unintentional harm in hospitals. Health care associated infection (HCAI) is the most frequent
adverse event in health care delivery system worldwide. The overall prevalence of HCAI in
developed countries varies from 5.1% to 11.6% and in developing countries it is around 15.6%
(World Health Organization, 2001). Hand hygiene is an important healthcare issue globally and
is a single most cost-effective and practical measure to reduce the incidence of HCAI and the
spread of antimicrobial resistance across all settings-from advanced health care systems to
primary healthcare centers.
Adequate hand hygiene among hospital personal could prevent an estimated 15 to 30% of the
HCAI despite the relative simplicity of this procedure, compliance to hand hygiene practices
among health care providers is as low as 40% (Kumar, Gupta, Kapil, Vij & Singh, 2014).
However, there are certain factors which predispose poor compliance to hand hygiene among
health care providers. Some of these factors are present regardless of the resources available like
prolonged and inappropriate use of invasive devices and antibiotics, high risk and sophisticated
procedures, insufficient application of standard and isolation precautions, immuno-suppression
and other severe underlying patient conditions (Ducell, Fabry & Nicoll, 2002).
Nonetheless, solely a few hospitals manage to offer functional evaluation alongside monitoring
systems. Likely rationale for this remain the demanding alongside intensive requirements of the
national surveillance system associated with scarce resource allocation towards HCAI in these
hospitals where additional emerging health concerns and illness are accorded preference
(Kingston, Slevin, O'Connell & Dunne, 2017).
This study will emphasize on HH adherence for HCWs in Zayed Military Hospital where the
lack of enough HH resources is dominant and also marred with various HH barriers and negative
attitude of HCWs to proper HH practices.
Literature review
The provision of healthcare worldwide is always associated with a potential range of safety
problems. Yet, despite advances in healthcare systems, patients remain vulnerable to
unintentional harm in hospitals. Health care associated infection (HCAI) is the most frequent
adverse event in health care delivery system worldwide. The overall prevalence of HCAI in
developed countries varies from 5.1% to 11.6% and in developing countries it is around 15.6%
(World Health Organization, 2001). Hand hygiene is an important healthcare issue globally and
is a single most cost-effective and practical measure to reduce the incidence of HCAI and the
spread of antimicrobial resistance across all settings-from advanced health care systems to
primary healthcare centers.
Adequate hand hygiene among hospital personal could prevent an estimated 15 to 30% of the
HCAI despite the relative simplicity of this procedure, compliance to hand hygiene practices
among health care providers is as low as 40% (Kumar, Gupta, Kapil, Vij & Singh, 2014).
However, there are certain factors which predispose poor compliance to hand hygiene among
health care providers. Some of these factors are present regardless of the resources available like
prolonged and inappropriate use of invasive devices and antibiotics, high risk and sophisticated
procedures, insufficient application of standard and isolation precautions, immuno-suppression
and other severe underlying patient conditions (Ducell, Fabry & Nicoll, 2002).
5
Some of the guidelines provided by CDC in 2000 are in line with those released by WHO in
2009 and recommends that visible dirt is supposed to be washed with soap or antiseptic and
water since hand rubs do not clean soiled hands and rinsing is important in this case, routine
hand washing require a minimum of 60 seconds with antiseptics and water, those working in
health sectors are supposed to use hand cream to reduce skin damages since skin that is
destroyed inhabit many pathogens and microorganisms, health care workers should use cold
water to clean their hands since hot water leads to a drying effect that spoil the skin, after
alcohol- based hand rubs are applied, the hands should be rubbed together for complete drying,
paper towel should be used for drying of hands or single use towel, multiple use or hang roll
towel should not be used and Alcohol –based hand rubs should be applied in five moments of
hand wash and not on contaminated hands that have dirt that is visible. Also, before wearing
and after removing of sterile and non-sterile gloves (Zayed Military Hospital - Al Batayeh,
2019).
Several studies have shown there is reduction of healthcare acquired infections with hand
hygiene compliance. In 1847, Semmelwels demonstrated that decontaminating hands with
chlorine prior to delivering a baby would reduce child death from 11.4% to 3.05%. Backman,
Zoutman, and Marck reviewed 31 studies 18 of all the reviewed studies showed that intervention
on hand hygiene compliance lead to reduction of hospital acquired infections. Other studies that
showed reduction had a range between 0.37% in rotavirus to 57% in MRSA bacteria (Allegranzi
& Pittet, 2009).
Despite the evidence that complying with hand hygiene reduces hospital acquired infections,
CDC report shows that health care workers have only showed 40% compliance. Recent studies
in USA have shown even more dismal performance with a record of 26% in intensive care unit
and 36% in non–intensive care unit ("Hand Hygiene in Healthcare Settings | CDC", 2019).
Despite the much effort that has been put on finding out the factors that leads to poor hand
hygiene practice and the interventions put forward little seems to be happening. This study
sought to assess if the undergraduate medical student had knowledge on hand hygiene and what
were their attitude and barriers on the practice which has received minimal attention yet could be
Some of the guidelines provided by CDC in 2000 are in line with those released by WHO in
2009 and recommends that visible dirt is supposed to be washed with soap or antiseptic and
water since hand rubs do not clean soiled hands and rinsing is important in this case, routine
hand washing require a minimum of 60 seconds with antiseptics and water, those working in
health sectors are supposed to use hand cream to reduce skin damages since skin that is
destroyed inhabit many pathogens and microorganisms, health care workers should use cold
water to clean their hands since hot water leads to a drying effect that spoil the skin, after
alcohol- based hand rubs are applied, the hands should be rubbed together for complete drying,
paper towel should be used for drying of hands or single use towel, multiple use or hang roll
towel should not be used and Alcohol –based hand rubs should be applied in five moments of
hand wash and not on contaminated hands that have dirt that is visible. Also, before wearing
and after removing of sterile and non-sterile gloves (Zayed Military Hospital - Al Batayeh,
2019).
Several studies have shown there is reduction of healthcare acquired infections with hand
hygiene compliance. In 1847, Semmelwels demonstrated that decontaminating hands with
chlorine prior to delivering a baby would reduce child death from 11.4% to 3.05%. Backman,
Zoutman, and Marck reviewed 31 studies 18 of all the reviewed studies showed that intervention
on hand hygiene compliance lead to reduction of hospital acquired infections. Other studies that
showed reduction had a range between 0.37% in rotavirus to 57% in MRSA bacteria (Allegranzi
& Pittet, 2009).
Despite the evidence that complying with hand hygiene reduces hospital acquired infections,
CDC report shows that health care workers have only showed 40% compliance. Recent studies
in USA have shown even more dismal performance with a record of 26% in intensive care unit
and 36% in non–intensive care unit ("Hand Hygiene in Healthcare Settings | CDC", 2019).
Despite the much effort that has been put on finding out the factors that leads to poor hand
hygiene practice and the interventions put forward little seems to be happening. This study
sought to assess if the undergraduate medical student had knowledge on hand hygiene and what
were their attitude and barriers on the practice which has received minimal attention yet could be

6
a root cause of poor hand hygiene compliance in the healthcare settings (Basurrah & Madani,
2006).
Objectives
The aims and objectives of this project were to determine:
The prevalence of healthcare staff compliance in hand hygiene.
The attitude, factors and barriers affecting hand hygiene.
The knowledge of healthcare staff regarding optimal hand hygiene.
The suggested recommendations to improve the healthcare staff compliance. Excellent
outline and approach.
Methodology
A cross sectional observation was conducted among different kind of 100 HWPs working and
undergoing training at Zayed Military Hospital Al Batayeh, Sharjah. Convenience consecutive
sampling technique was adopted to enroll subjects over a period of 15 days. Data was collected
through a socio- demographic data sheet, Modified Hand hygiene performance from Zayed
Military Hospital, structured questionnaire and interview which is prepared with help of HICC
and approved by ethical committee. A group of trained nursing staffs observed hand hygiene
practices in respective area and questioned information on attitude and barriers. The detail of
instruments are given below:
Part A: Socio-demographic Profile Sheet:
This encompasses gender, age, level of education, religion, working experience year, kind
of educational institute finished, in-service training/education on hand-hygiene practices
exposure, and intern students’’ course. The tool’s validity was sought from the experts in
the general surgery, nursing, medicine and microbiology fields.
Part B: Hand Hygiene Observation Proforma in Zayed Military Hospital:
This is comprehensive proforma based on World Health Organization’s checklist for
hand hygiene from hospital and modified with the aid of professionals in infection control
and prevention department of Zayed Military Hospital Al Batayeh, Sharjah. It
a root cause of poor hand hygiene compliance in the healthcare settings (Basurrah & Madani,
2006).
Objectives
The aims and objectives of this project were to determine:
The prevalence of healthcare staff compliance in hand hygiene.
The attitude, factors and barriers affecting hand hygiene.
The knowledge of healthcare staff regarding optimal hand hygiene.
The suggested recommendations to improve the healthcare staff compliance. Excellent
outline and approach.
Methodology
A cross sectional observation was conducted among different kind of 100 HWPs working and
undergoing training at Zayed Military Hospital Al Batayeh, Sharjah. Convenience consecutive
sampling technique was adopted to enroll subjects over a period of 15 days. Data was collected
through a socio- demographic data sheet, Modified Hand hygiene performance from Zayed
Military Hospital, structured questionnaire and interview which is prepared with help of HICC
and approved by ethical committee. A group of trained nursing staffs observed hand hygiene
practices in respective area and questioned information on attitude and barriers. The detail of
instruments are given below:
Part A: Socio-demographic Profile Sheet:
This encompasses gender, age, level of education, religion, working experience year, kind
of educational institute finished, in-service training/education on hand-hygiene practices
exposure, and intern students’’ course. The tool’s validity was sought from the experts in
the general surgery, nursing, medicine and microbiology fields.
Part B: Hand Hygiene Observation Proforma in Zayed Military Hospital:
This is comprehensive proforma based on World Health Organization’s checklist for
hand hygiene from hospital and modified with the aid of professionals in infection control
and prevention department of Zayed Military Hospital Al Batayeh, Sharjah. It
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
encompasses information regarding the type of health care providers, number of
opportunities for hand hygiene faced in defined time, and hand hygiene practices (hand
wash and hand rub) etc. The tool validity was verified after submitting the tools to experts
in the field of nursing, surgery, medicine & Hospital Infection Control Committee
(HICC).
Part C: Attitude Scale: It is a self-develop five-point Likert Scale comprising eleven items
linked to the attitude towards the practices of hand-hygiene. Every item got measured on
five-point rating scale with Strongly Agree given 5; to Strong disagree given 1. The tool’s
reliability got conformed using the Cronbach‘s alpha and it stood at 0.830 for this present
study. The scale for attitude was discovered valid as well as reliable for this current study.
Part D- Structured Questionnaire:
It comprised of the factors hindering hand hygiene compliance among health care providers i.e.
availability of time, sink, soap and water which is prepared by the help of supervision from
HICC, on-site Supervisor and lack of knowledge of guidelines/ protocols etc. Validity of tool
was confirmed after submitting the tools to experts in the field of nursing, surgery, medicine &
HICC.
In addition, interview method also used like 10 selected open-ended questions approved by
hospital administration, ethical committee and HICC (appendix 2) to assess the staff knowledge,
factors, barriers and attitude in hand hygiene.
Ethical Consideration: The current study got the approval by the Institutional Ethical
Committee and information confidentiality as well as subjects’ anonymity stood
guaranteed both after and during the collection of data period. Such an ethical approval
wave-off requirement for consent for observation to eliminate bias and ensure best
outcomes regarding the compliance with hand-hygiene guidelines. Analysis of data was
through SPSS version twenty and both inferential and descriptive statistics were utilized.
encompasses information regarding the type of health care providers, number of
opportunities for hand hygiene faced in defined time, and hand hygiene practices (hand
wash and hand rub) etc. The tool validity was verified after submitting the tools to experts
in the field of nursing, surgery, medicine & Hospital Infection Control Committee
(HICC).
Part C: Attitude Scale: It is a self-develop five-point Likert Scale comprising eleven items
linked to the attitude towards the practices of hand-hygiene. Every item got measured on
five-point rating scale with Strongly Agree given 5; to Strong disagree given 1. The tool’s
reliability got conformed using the Cronbach‘s alpha and it stood at 0.830 for this present
study. The scale for attitude was discovered valid as well as reliable for this current study.
Part D- Structured Questionnaire:
It comprised of the factors hindering hand hygiene compliance among health care providers i.e.
availability of time, sink, soap and water which is prepared by the help of supervision from
HICC, on-site Supervisor and lack of knowledge of guidelines/ protocols etc. Validity of tool
was confirmed after submitting the tools to experts in the field of nursing, surgery, medicine &
HICC.
In addition, interview method also used like 10 selected open-ended questions approved by
hospital administration, ethical committee and HICC (appendix 2) to assess the staff knowledge,
factors, barriers and attitude in hand hygiene.
Ethical Consideration: The current study got the approval by the Institutional Ethical
Committee and information confidentiality as well as subjects’ anonymity stood
guaranteed both after and during the collection of data period. Such an ethical approval
wave-off requirement for consent for observation to eliminate bias and ensure best
outcomes regarding the compliance with hand-hygiene guidelines. Analysis of data was
through SPSS version twenty and both inferential and descriptive statistics were utilized.
8
Results and Recommended Improvements
Hand Hygiene Compliance
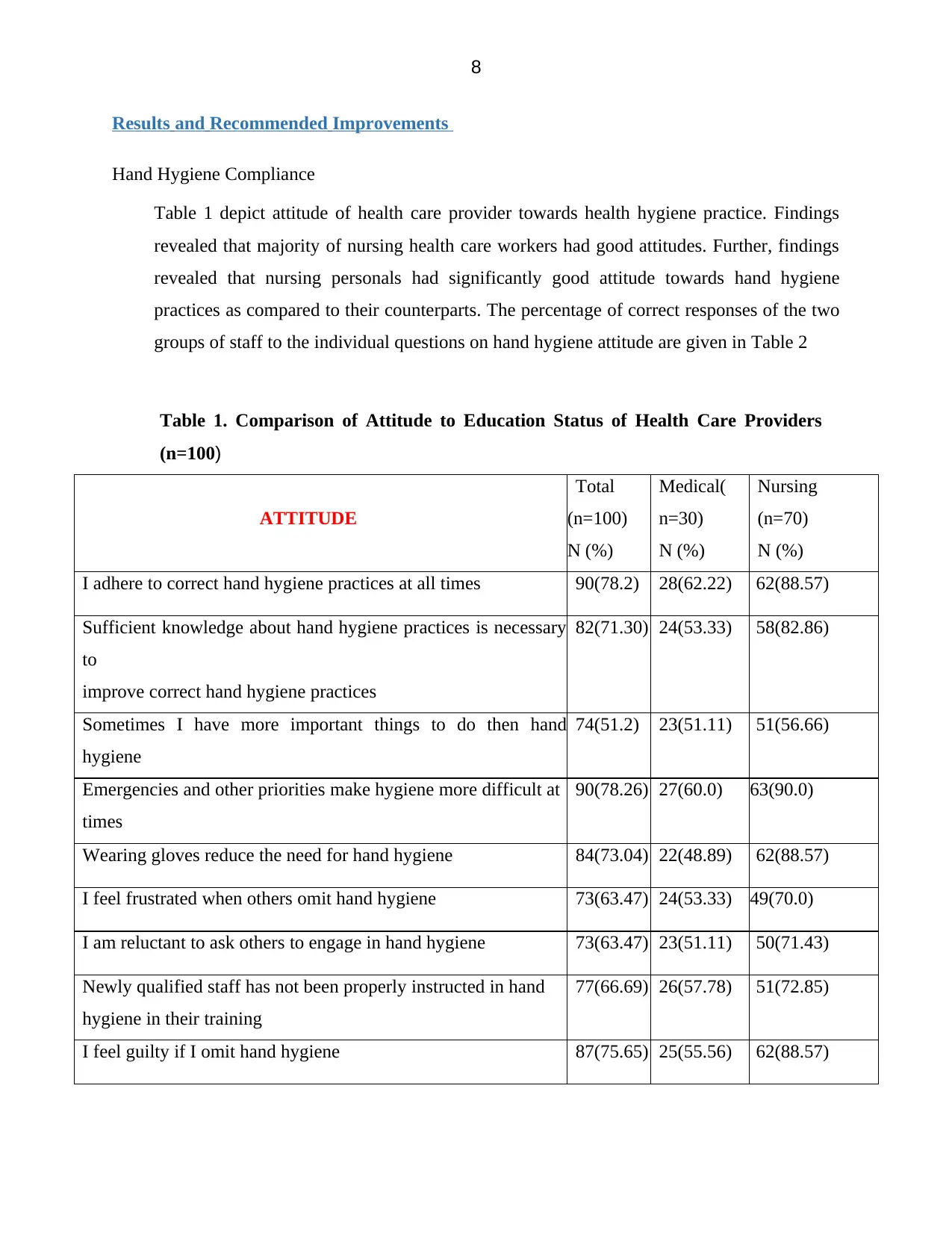
Table 1 depict attitude of health care provider towards health hygiene practice. Findings
revealed that majority of nursing health care workers had good attitudes. Further, findings
revealed that nursing personals had significantly good attitude towards hand hygiene
practices as compared to their counterparts. The percentage of correct responses of the two
groups of staff to the individual questions on hand hygiene attitude are given in Table 2
Table 1. Comparison of Attitude to Education Status of Health Care Providers
(n=100)
ATTITUDE
Total
(n=100)
N (%)
Medical(
n=30)
N (%)
Nursing
(n=70)
N (%)
I adhere to correct hand hygiene practices at all times 90(78.2) 28(62.22) 62(88.57)
Sufficient knowledge about hand hygiene practices is necessary
to
improve correct hand hygiene practices
82(71.30) 24(53.33) 58(82.86)
Sometimes I have more important things to do then hand
hygiene
74(51.2) 23(51.11) 51(56.66)
Emergencies and other priorities make hygiene more difficult at
times
90(78.26) 27(60.0) 63(90.0)
Wearing gloves reduce the need for hand hygiene 84(73.04) 22(48.89) 62(88.57)
I feel frustrated when others omit hand hygiene 73(63.47) 24(53.33) 49(70.0)
I am reluctant to ask others to engage in hand hygiene 73(63.47) 23(51.11) 50(71.43)
Newly qualified staff has not been properly instructed in hand
hygiene in their training
77(66.69) 26(57.78) 51(72.85)
I feel guilty if I omit hand hygiene 87(75.65) 25(55.56) 62(88.57)
Results and Recommended Improvements
Hand Hygiene Compliance
Table 1 depict attitude of health care provider towards health hygiene practice. Findings
revealed that majority of nursing health care workers had good attitudes. Further, findings
revealed that nursing personals had significantly good attitude towards hand hygiene
practices as compared to their counterparts. The percentage of correct responses of the two
groups of staff to the individual questions on hand hygiene attitude are given in Table 2
Table 1. Comparison of Attitude to Education Status of Health Care Providers
(n=100)
ATTITUDE
Total
(n=100)
N (%)
Medical(
n=30)
N (%)
Nursing
(n=70)
N (%)
I adhere to correct hand hygiene practices at all times 90(78.2) 28(62.22) 62(88.57)
Sufficient knowledge about hand hygiene practices is necessary
to
improve correct hand hygiene practices
82(71.30) 24(53.33) 58(82.86)
Sometimes I have more important things to do then hand
hygiene
74(51.2) 23(51.11) 51(56.66)
Emergencies and other priorities make hygiene more difficult at
times
90(78.26) 27(60.0) 63(90.0)
Wearing gloves reduce the need for hand hygiene 84(73.04) 22(48.89) 62(88.57)
I feel frustrated when others omit hand hygiene 73(63.47) 24(53.33) 49(70.0)
I am reluctant to ask others to engage in hand hygiene 73(63.47) 23(51.11) 50(71.43)
Newly qualified staff has not been properly instructed in hand
hygiene in their training
77(66.69) 26(57.78) 51(72.85)
I feel guilty if I omit hand hygiene 87(75.65) 25(55.56) 62(88.57)
9
Adhering to hand hygiene practices is easy in the current setup 91(79.13) 27(60.0) 64(91.42)
Health care personnel should act as a role model for others 79(68.70) 28(62.22) 51(72.86)
Table 2. Comparison of Factors Among Medical & Nursing HCPs (n=100)
FACTORS
Total
(n=100)
n (%)
Medical
(n=30)
N (%)
Nursing
(n=70)
N (%)
Hand hygiene facility are not conveniently placed 97(84.34) 34(75.55) 64(91.43)
Overburden of patient care not allow hand hygiene 93(80.87) 31(68.89) 62(88.57)
Understaffing/overcrowding or insufficient time 94(81.73) 33(73.33) 61(87.14)
Hand hygiene takes too much time 93(80.86) 31(68.89) 62(88.57)
Not thinking about hand hygiene or forgetfulness 88(76.52) 29(64.44) 59(84.29)
Sore hands/abrasions on hands stop me hand hygiene 80(69.57) 30(66.67) 50(71.43)
Hand hygiene unnecessary when gloves are worn 85(73.91) 31(68.89) 54(77.14)
Belief of low risk of acquiring infection from patients 62(53.91) 28(62.22) 34(48.57)
Hand hygiene damage skin and cause irritation 89(77.39) 31(68.89) 58(82.85)
Hand hygiene between patient is unnecessary 92(80.0) 32(71.11) 60(85.71)
Hand hygiene affects the clinical outcome 86(74.78) 32(71.11) 54(77.14)
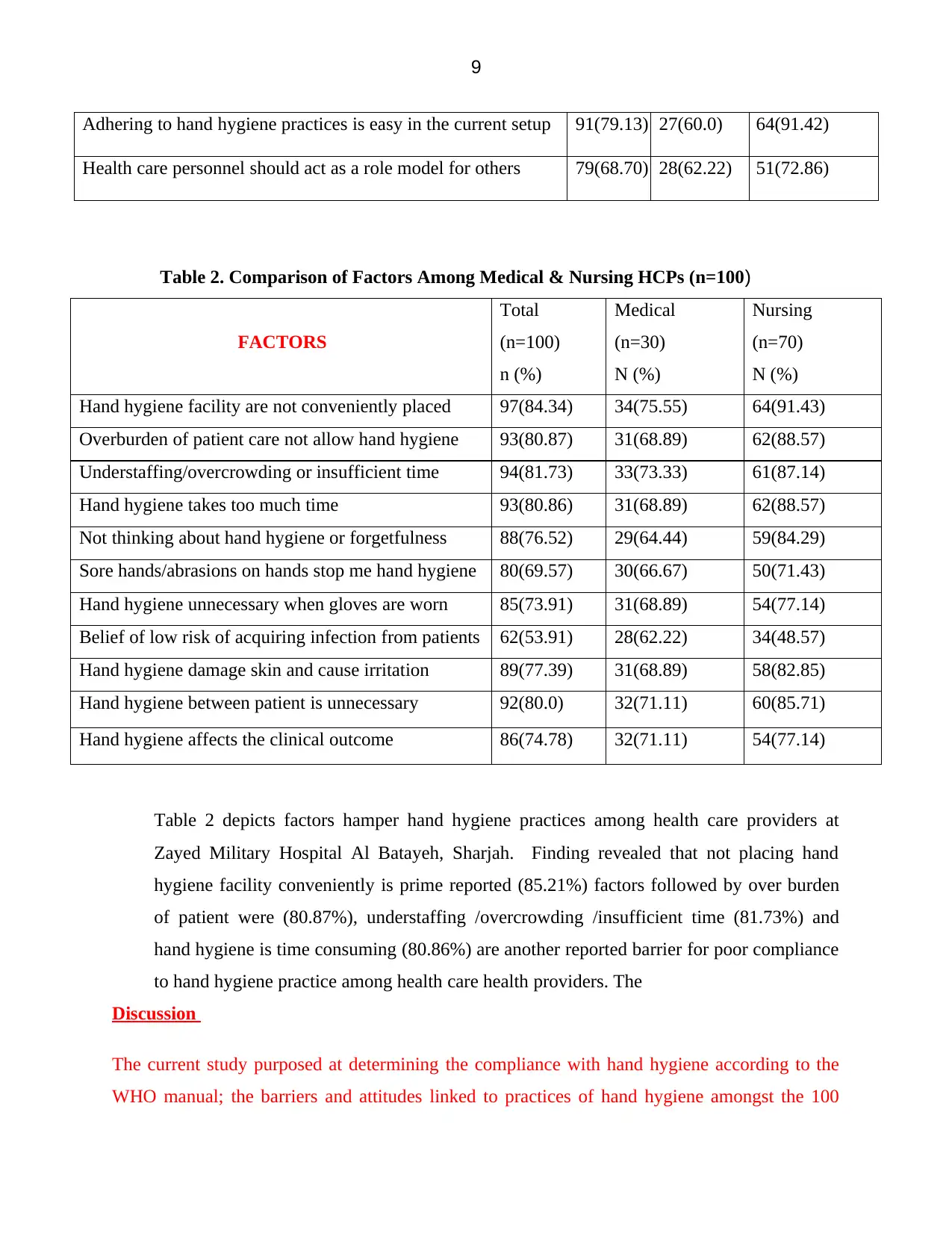
Table 2 depicts factors hamper hand hygiene practices among health care providers at
Zayed Military Hospital Al Batayeh, Sharjah. Finding revealed that not placing hand
hygiene facility conveniently is prime reported (85.21%) factors followed by over burden
of patient were (80.87%), understaffing /overcrowding /insufficient time (81.73%) and
hand hygiene is time consuming (80.86%) are another reported barrier for poor compliance
to hand hygiene practice among health care health providers. The
Discussion
The current study purposed at determining the compliance with hand hygiene according to the
WHO manual; the barriers and attitudes linked to practices of hand hygiene amongst the 100
Adhering to hand hygiene practices is easy in the current setup 91(79.13) 27(60.0) 64(91.42)
Health care personnel should act as a role model for others 79(68.70) 28(62.22) 51(72.86)
Table 2. Comparison of Factors Among Medical & Nursing HCPs (n=100)
FACTORS
Total
(n=100)
n (%)
Medical
(n=30)
N (%)
Nursing
(n=70)
N (%)
Hand hygiene facility are not conveniently placed 97(84.34) 34(75.55) 64(91.43)
Overburden of patient care not allow hand hygiene 93(80.87) 31(68.89) 62(88.57)
Understaffing/overcrowding or insufficient time 94(81.73) 33(73.33) 61(87.14)
Hand hygiene takes too much time 93(80.86) 31(68.89) 62(88.57)
Not thinking about hand hygiene or forgetfulness 88(76.52) 29(64.44) 59(84.29)
Sore hands/abrasions on hands stop me hand hygiene 80(69.57) 30(66.67) 50(71.43)
Hand hygiene unnecessary when gloves are worn 85(73.91) 31(68.89) 54(77.14)
Belief of low risk of acquiring infection from patients 62(53.91) 28(62.22) 34(48.57)
Hand hygiene damage skin and cause irritation 89(77.39) 31(68.89) 58(82.85)
Hand hygiene between patient is unnecessary 92(80.0) 32(71.11) 60(85.71)
Hand hygiene affects the clinical outcome 86(74.78) 32(71.11) 54(77.14)
Table 2 depicts factors hamper hand hygiene practices among health care providers at
Zayed Military Hospital Al Batayeh, Sharjah. Finding revealed that not placing hand
hygiene facility conveniently is prime reported (85.21%) factors followed by over burden
of patient were (80.87%), understaffing /overcrowding /insufficient time (81.73%) and
hand hygiene is time consuming (80.86%) are another reported barrier for poor compliance
to hand hygiene practice among health care health providers. The
Discussion
The current study purposed at determining the compliance with hand hygiene according to the
WHO manual; the barriers and attitudes linked to practices of hand hygiene amongst the 100
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10
healthcare providers at the Zayed Military Hospital. The present study outcomes unearthed that
faculty showcases higher compliance at ten percent to practise of hand hygiene followed by the
senior residents at 7.140 percent and the nursing and medical interns coming third at 6.71 percent
while the junior resident recording the least adherence at 1.03 percent. Among the HCWs, partial
compliance stood surprisingly high at 63.04 percent (Ataiyero, Dyson & Graham, 2018).
The current study outcomes remain in parallel to the research performed by Abdella MN at al. on
four hundred and sixty five heath care providers that showcased 16.5 percent full compliance
with hand hygiene requirements and practices. Nonetheless, in the research performed by Kumar
et al., a contradictory outcome stood unravelled since there remained a higher full adherence
levels at 76 percent to hand hygiene practices amongst the care providers working at the private
sector and the general compliance with practices of hand hygiene stood at 80.5 percent.
The study carried out by Shanu et al similarly discovered that observed adherence rates stood
higher at 67.08 percent as opposed to self-reported adherence at 90 percent among the
practitioners. In the past study performed in Saudi Arabia, sub-optimal adherence to practices of
hand hygiene was noted at 70, 18.8 as well as 9.10 percent among the students, nurses alongside
senior medical practitioners in that order. Such differences between the current and past studies
might be as a result of utilization of distinct methodologies, contexts/setting alongside use of
different instruments.
Additionally, 78.30 percent HCWs indicated the need for adherence with hand hygiene
requirements while 71.30 care providers held that full knowledge linked to practices of hand
hygiene remains the most significant to undertake hand-hygiene practices. Nonetheless, 78.260
percent of the HCWs held that these practices become challenging during the emergencies and
other priorities.
Nair et al. reported the similar outcomes in their study whereby 35.30 and 74.40 percent medical
alongside nursing students had assumed that they had better knowledge regarding practices of
hand hygiene in that order. An Indian study also discovered similar findings on staff nurses as
well as residents. Moreover, it was highlighted that solely 21.40 percent of medical students
alongside 61.80 percent of nursing students indicated adherence to correct practices of hand
healthcare providers at the Zayed Military Hospital. The present study outcomes unearthed that
faculty showcases higher compliance at ten percent to practise of hand hygiene followed by the
senior residents at 7.140 percent and the nursing and medical interns coming third at 6.71 percent
while the junior resident recording the least adherence at 1.03 percent. Among the HCWs, partial
compliance stood surprisingly high at 63.04 percent (Ataiyero, Dyson & Graham, 2018).
The current study outcomes remain in parallel to the research performed by Abdella MN at al. on
four hundred and sixty five heath care providers that showcased 16.5 percent full compliance
with hand hygiene requirements and practices. Nonetheless, in the research performed by Kumar
et al., a contradictory outcome stood unravelled since there remained a higher full adherence
levels at 76 percent to hand hygiene practices amongst the care providers working at the private
sector and the general compliance with practices of hand hygiene stood at 80.5 percent.
The study carried out by Shanu et al similarly discovered that observed adherence rates stood
higher at 67.08 percent as opposed to self-reported adherence at 90 percent among the
practitioners. In the past study performed in Saudi Arabia, sub-optimal adherence to practices of
hand hygiene was noted at 70, 18.8 as well as 9.10 percent among the students, nurses alongside
senior medical practitioners in that order. Such differences between the current and past studies
might be as a result of utilization of distinct methodologies, contexts/setting alongside use of
different instruments.
Additionally, 78.30 percent HCWs indicated the need for adherence with hand hygiene
requirements while 71.30 care providers held that full knowledge linked to practices of hand
hygiene remains the most significant to undertake hand-hygiene practices. Nonetheless, 78.260
percent of the HCWs held that these practices become challenging during the emergencies and
other priorities.
Nair et al. reported the similar outcomes in their study whereby 35.30 and 74.40 percent medical
alongside nursing students had assumed that they had better knowledge regarding practices of
hand hygiene in that order. An Indian study also discovered similar findings on staff nurses as
well as residents. Moreover, it was highlighted that solely 21.40 percent of medical students
alongside 61.80 percent of nursing students indicated adherence to correct practices of hand
11
hygiene at all points. Also, the past studies have indicated that staff nurses negate hand hygiene
because of fear of frightened skin challenges like dermatitis.
Additionally, in the current research, 85.210 percent of the HCWs held that facilities of hand
hygiene are never conveniently situated and 80.870 percent of the care workers indicated that
due to overburden of caring for patients, practices of hand hygiene are never adhered to
effectively. It is further unravelled that 81.730 percent of HCWs were either understaffed or
overcrowded or insufficient time, all of which culminate in poor compliance with these practices
of hand hygiene.
The current study outcomes remain aligned to the previous research performed by Segum et al.
which showed that 66.80 percent of HCWs were convinced that insufficient facilities for hand
hygiene existed. Similarly, nearly 35.70 percent of HCWs indicated that that time limitation was
a key obstacle to full adherence to hand hygiene practices. In the same manner, 14.30 percent of
HCWs felt that heavy patient workload or overburden as another key deterrence to full
adherence. The existing literature further indicate that hand rub solutions’ availability at patient
bedside makes the patients to increase their compliance to practices for hand hygiene.
Conclusion and Recommendation
Present study revealed a very poor adherence to hand hygiene practices among health care
providers at a tertiary care teaching hospital. However, study findings recommended a hand on
training or periodic in-service education programme to sensitize HCPs. Findings also suggest to
make it mandatory to undergo a training programme for newly joined HCPs to develop
understanding about the importance of hand hygiene practices.
Action Plan
There are two action plans for this study project. The first action plan is to perform a training
program for the healthcare providers in Zayed Military Hospital Al Batayeh by the infection
control department. The training program will consist of a lecture about the importance of hand
hygiene, types, technique, complication of the non-compliance of the hand hygiene in addition to
the hand hygiene practice. The training program will be conducted in Zayed Military Hospital
AL Batayeh, 4th floor, and lecture hall on Wednesday 31/Jul/2019.
hygiene at all points. Also, the past studies have indicated that staff nurses negate hand hygiene
because of fear of frightened skin challenges like dermatitis.
Additionally, in the current research, 85.210 percent of the HCWs held that facilities of hand
hygiene are never conveniently situated and 80.870 percent of the care workers indicated that
due to overburden of caring for patients, practices of hand hygiene are never adhered to
effectively. It is further unravelled that 81.730 percent of HCWs were either understaffed or
overcrowded or insufficient time, all of which culminate in poor compliance with these practices
of hand hygiene.
The current study outcomes remain aligned to the previous research performed by Segum et al.
which showed that 66.80 percent of HCWs were convinced that insufficient facilities for hand
hygiene existed. Similarly, nearly 35.70 percent of HCWs indicated that that time limitation was
a key obstacle to full adherence to hand hygiene practices. In the same manner, 14.30 percent of
HCWs felt that heavy patient workload or overburden as another key deterrence to full
adherence. The existing literature further indicate that hand rub solutions’ availability at patient
bedside makes the patients to increase their compliance to practices for hand hygiene.
Conclusion and Recommendation
Present study revealed a very poor adherence to hand hygiene practices among health care
providers at a tertiary care teaching hospital. However, study findings recommended a hand on
training or periodic in-service education programme to sensitize HCPs. Findings also suggest to
make it mandatory to undergo a training programme for newly joined HCPs to develop
understanding about the importance of hand hygiene practices.
Action Plan
There are two action plans for this study project. The first action plan is to perform a training
program for the healthcare providers in Zayed Military Hospital Al Batayeh by the infection
control department. The training program will consist of a lecture about the importance of hand
hygiene, types, technique, complication of the non-compliance of the hand hygiene in addition to
the hand hygiene practice. The training program will be conducted in Zayed Military Hospital
AL Batayeh, 4th floor, and lecture hall on Wednesday 31/Jul/2019.
12
This training will be effective since it will help underpin the importance of using effective
hand hygiene methods and impart the knowledge amongst the HCWs on the best methods
to use when dealing with the patients to control the infections. The training will focus on
the significant of hand hygiene and its need for promotion as it will lead to the prevention
of the spread of the microbes contact alongside fecal-oral transmission. As has been seen in
the literature and the current study outcomes, there is a glaring proof which support the
positive health impacts of clean hands. The interventions studies like training the HCWs
have demonstrated decreased infections and mortality rates in hospitals that ensure
complete adherence to hand hygiene practices. For example, when the women at the labor
wards are attended to by the HCW who has washed her hands with the antiseptic agents,
there has been a reduced rates of mortality. Thus, this training will be effective when it
focuses on the ensuring hand hygiene methods since this will prove the protective impacts
of hand hygiene against the HCAIs when the antiseptic agents are used instead of regular
bar soaps. Thus the HCWs will be urged to use these antiseptic agents and this will
improve both health and safety of not only patients but also the HCWs. Moreover, this
training will further help promote the necessary moves or actions towards prosperous
epidemiologically-inspired infection control intervention in the Hospital known as
“Recognize-Explain Act.”
The training will further help the HCWs appreciate the significance of complying with
hand hygiene practices which has since been the most imperative within the healthcare
context. Moreover, the training will ensure that HCWs have clear understanding of their
mandate of performing hand hygiene practices at a time of care for the safety of the
patients (White et al., 2015). They will be vast with the range of ways to keep hands free
from any potentially harmful microbes as well as safe for all the patient care. Moreover,
this training will be effective as it will additionally show the HCWs different ways of
keeping hands safe through washing hands with soaps alongside water or via application of
the alcohol-oriented hand-rub. They will further be told that, the proper hand hygiene
actions effective, nonetheless, relies on the combination of many variables like suitable type
as well as amount of hand hygiene agents application; adequate duration of hand hygiene
This training will be effective since it will help underpin the importance of using effective
hand hygiene methods and impart the knowledge amongst the HCWs on the best methods
to use when dealing with the patients to control the infections. The training will focus on
the significant of hand hygiene and its need for promotion as it will lead to the prevention
of the spread of the microbes contact alongside fecal-oral transmission. As has been seen in
the literature and the current study outcomes, there is a glaring proof which support the
positive health impacts of clean hands. The interventions studies like training the HCWs
have demonstrated decreased infections and mortality rates in hospitals that ensure
complete adherence to hand hygiene practices. For example, when the women at the labor
wards are attended to by the HCW who has washed her hands with the antiseptic agents,
there has been a reduced rates of mortality. Thus, this training will be effective when it
focuses on the ensuring hand hygiene methods since this will prove the protective impacts
of hand hygiene against the HCAIs when the antiseptic agents are used instead of regular
bar soaps. Thus the HCWs will be urged to use these antiseptic agents and this will
improve both health and safety of not only patients but also the HCWs. Moreover, this
training will further help promote the necessary moves or actions towards prosperous
epidemiologically-inspired infection control intervention in the Hospital known as
“Recognize-Explain Act.”
The training will further help the HCWs appreciate the significance of complying with
hand hygiene practices which has since been the most imperative within the healthcare
context. Moreover, the training will ensure that HCWs have clear understanding of their
mandate of performing hand hygiene practices at a time of care for the safety of the
patients (White et al., 2015). They will be vast with the range of ways to keep hands free
from any potentially harmful microbes as well as safe for all the patient care. Moreover,
this training will be effective as it will additionally show the HCWs different ways of
keeping hands safe through washing hands with soaps alongside water or via application of
the alcohol-oriented hand-rub. They will further be told that, the proper hand hygiene
actions effective, nonetheless, relies on the combination of many variables like suitable type
as well as amount of hand hygiene agents application; adequate duration of hand hygiene
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
13
actions., proper hand drying methods as well as satisfactory coverage of all surfaces of
hand. Such information will ensure that HCWs have the correct information and
knowledge of keeping their hands safe from the potential microbes which will help them
not only reduce the spread of infections amongst patients, but also amongst the HCWs
themselves (Anderson & Weese, 2016).
The training will also be important since it will focus on showing the HCWs the situations
that require proper hand washing. They will be shown that they need to wash their hands
when faced with such situations as visibly dirty hands which are soiled with body fluids or
blood, exposure to spore-forming organism and following the use of restrooms. This
information will ensure that HCWs known all the situations that should require hand
washing and hence increased safety amongst the patients through a reduction in infections.
The training will further ensure that the HCWs become aware of the alcohol-based hand
rub which remains the ideal method for hand hygiene (Zellmer, Blakney, Van Hoof &
Safdar, 2015). Thus, this will help solve the problem of lack of facility for hand hygiene
while at the same time ensuring that patients are safe. The training will also be a beneficial
to the Hospital since it will ensure that they make the alcohol-based hand rub always
available and this will ensure hand hygiene via the elimination of majority of the viruses
and germs, cutting down on the duration of period spent on hand hygiene. Moreover, it will
also be readily available at care points hence excluding the need for additional resources
like clean water availability for hand washing alongside with functioning hand-wash basins
with soap and correct hand-drying materials. Lastly, alcohol-based hand rubs have better
skin tolerability because many of them entail humectants alongside skin-conditioning
agents that effectively combat the alcohol drying effects.
As highlighted overhead, this training will be important by imparting the knowledge of
ensuring proper hand hygiene undertaking, regardless of whether via hand washing or
even alcohol-oriented hand rub. This is because it will help explain the range of variables
that determine facilitate hand hygiene for increased HCWs and patient safety as they
introduce interventions. The training will further help the HCWs know the barriers to
effective hand hygiene by stressing on the barriers identification before introducing the
actions., proper hand drying methods as well as satisfactory coverage of all surfaces of
hand. Such information will ensure that HCWs have the correct information and
knowledge of keeping their hands safe from the potential microbes which will help them
not only reduce the spread of infections amongst patients, but also amongst the HCWs
themselves (Anderson & Weese, 2016).
The training will also be important since it will focus on showing the HCWs the situations
that require proper hand washing. They will be shown that they need to wash their hands
when faced with such situations as visibly dirty hands which are soiled with body fluids or
blood, exposure to spore-forming organism and following the use of restrooms. This
information will ensure that HCWs known all the situations that should require hand
washing and hence increased safety amongst the patients through a reduction in infections.
The training will further ensure that the HCWs become aware of the alcohol-based hand
rub which remains the ideal method for hand hygiene (Zellmer, Blakney, Van Hoof &
Safdar, 2015). Thus, this will help solve the problem of lack of facility for hand hygiene
while at the same time ensuring that patients are safe. The training will also be a beneficial
to the Hospital since it will ensure that they make the alcohol-based hand rub always
available and this will ensure hand hygiene via the elimination of majority of the viruses
and germs, cutting down on the duration of period spent on hand hygiene. Moreover, it will
also be readily available at care points hence excluding the need for additional resources
like clean water availability for hand washing alongside with functioning hand-wash basins
with soap and correct hand-drying materials. Lastly, alcohol-based hand rubs have better
skin tolerability because many of them entail humectants alongside skin-conditioning
agents that effectively combat the alcohol drying effects.
As highlighted overhead, this training will be important by imparting the knowledge of
ensuring proper hand hygiene undertaking, regardless of whether via hand washing or
even alcohol-oriented hand rub. This is because it will help explain the range of variables
that determine facilitate hand hygiene for increased HCWs and patient safety as they
introduce interventions. The training will further help the HCWs know the barriers to
effective hand hygiene by stressing on the barriers identification before introducing the
14
theory-based interventions. Thus, this training will help combine both HCWs education
with performance feedback to be undertaken via randomized controlled trials. This will
help ensure that HCWs appreciate that solely using alcohol-based handrub as a single
intervention never enhances hand hygiene adherence in a sustainable way. Thus, the
HCWs will advocate for the combination of various interventions that target their
behaviors including ongoing feedback, motivation practise and education.
The training will further be effective since it will focus on the identification of the moments of
hand hygiene. It will show that health initiatives within the Hospital remain anchored on both
indirect and direct contact with patients from all health experts except the administrative staff.
Thus, by focusing this training on explaining to the HCWs the critical moments of hand hygiene,
it will greatly enhance hand hygiene practices. This is because, it will help impart the knowledge
amongst the HCWs that different health activities often vary in degrees of the transmission of
microbes. The issue for focus of the training is that Hospital will standardize hand hygiene
routines for particular health activities and hence helping the HCWs to effectively enhance safe
and clean hands. Moreover, this training will help override the challenge in predetermining
contexts and individuals at higher risk of contact with transmission irrespective of health
activities to be undertaken. Thus, thus training will help emphasize that all the HCWs who are
involved in the provision of healthcare are subject to the performance of proper hand hygiene
irrespective of whether undertaking indirect or direct patient contact indicates risk of transmitting
microbes (Carter et al., 2016).
Thus, the training will show the HCWs the specific time or situation to undertake the hand
hygiene actions as a means of facilitating hand hygiene promotion for the health care workers.
Specifically, the HCWs will know that they need to perform hand hygiene actions in such
moments as before touching any patient; before clean or aseptic procedures; following exposure
to body fluids, after touching the patient; and after touching the surroundings of the patient
(Mearkle, Houghton, Bwonya & Lindfield, 2016).
The HCWs will know that they need to undertake HH action before being in contact with patient
and before aseptic or clean procedure to minimize the risk of transmitting microbes to their
theory-based interventions. Thus, this training will help combine both HCWs education
with performance feedback to be undertaken via randomized controlled trials. This will
help ensure that HCWs appreciate that solely using alcohol-based handrub as a single
intervention never enhances hand hygiene adherence in a sustainable way. Thus, the
HCWs will advocate for the combination of various interventions that target their
behaviors including ongoing feedback, motivation practise and education.
The training will further be effective since it will focus on the identification of the moments of
hand hygiene. It will show that health initiatives within the Hospital remain anchored on both
indirect and direct contact with patients from all health experts except the administrative staff.
Thus, by focusing this training on explaining to the HCWs the critical moments of hand hygiene,
it will greatly enhance hand hygiene practices. This is because, it will help impart the knowledge
amongst the HCWs that different health activities often vary in degrees of the transmission of
microbes. The issue for focus of the training is that Hospital will standardize hand hygiene
routines for particular health activities and hence helping the HCWs to effectively enhance safe
and clean hands. Moreover, this training will help override the challenge in predetermining
contexts and individuals at higher risk of contact with transmission irrespective of health
activities to be undertaken. Thus, thus training will help emphasize that all the HCWs who are
involved in the provision of healthcare are subject to the performance of proper hand hygiene
irrespective of whether undertaking indirect or direct patient contact indicates risk of transmitting
microbes (Carter et al., 2016).
Thus, the training will show the HCWs the specific time or situation to undertake the hand
hygiene actions as a means of facilitating hand hygiene promotion for the health care workers.
Specifically, the HCWs will know that they need to perform hand hygiene actions in such
moments as before touching any patient; before clean or aseptic procedures; following exposure
to body fluids, after touching the patient; and after touching the surroundings of the patient
(Mearkle, Houghton, Bwonya & Lindfield, 2016).
The HCWs will know that they need to undertake HH action before being in contact with patient
and before aseptic or clean procedure to minimize the risk of transmitting microbes to their
15
patients. They will also be told that the rest of the moments occur following the patient contact
and exposure to body fluids which are good safeguard against transferring microbes to the
HCWs from the patents and hence to the surroundings within the Hospital. A range of health
care activities remain often undertaken in a shared manner during the provision of healthcare.
Therefore, this training will help show the HCWs that it might be adequate to solely undertake
one hand hygiene action per time (Sadule-Rios & Aguilera, 2017). Thus, where various health
activities are involved, the HH action choice must be anchored on individual assessment of each
patient. Therefore, to prevent the HCAI transmission, this training will help emphasise that
HCWs must comprehend as well acknowledge all the above five moments of hand hygiene to
execute relevant actions for HH when a specific scenario calls for it.
The second action plan is the relocation on the hand sanitizers in Zayed Military Hospital Al
Batayeh since the height percentage of the reason of the non-compliance is Hand hygiene facility
are not conveniently placed with 85.21%. Thus, my action is to contact the infection control
department and the maintenance department to put a plan for the relocation of certain hand
sanitizer dispensers in the departments that complains about the barrier of performing the hand
hygiene is because of the accessibility of the hand sanitizers, the plan of the relocation will take
one-week period after the taking the approval of all the infection control committee and the
chairman. The process of the relocation takes two weeks period and we will allow them time to
get used of the new nearest location of the hand sanitizers. Accordingly, after approximately 5
weeks at 01/Sep/2019 which is the monthly audit of august the re-audit will be conducted though
using the monthly hand hygiene observation form, by me and the infection control in charge (the
on-site supervisor) or someone on his behalf from the infection control department.
Plan the re-audit
1st of September/2019 is the time of the re-audit after performing two action plans which are the
training program and the relocation of the hand sanitizers in certain departments. The re-audit
will be done mainly in the departments where the hand sanitizers were relocated. The re-audit
will be done through the infection control monthly audit for hand hygiene by using monthly hand
hygiene observation form in addition to specific questionnaire and interview that will be
reviewed by infection control department and approved by the ethical committee.
patients. They will also be told that the rest of the moments occur following the patient contact
and exposure to body fluids which are good safeguard against transferring microbes to the
HCWs from the patents and hence to the surroundings within the Hospital. A range of health
care activities remain often undertaken in a shared manner during the provision of healthcare.
Therefore, this training will help show the HCWs that it might be adequate to solely undertake
one hand hygiene action per time (Sadule-Rios & Aguilera, 2017). Thus, where various health
activities are involved, the HH action choice must be anchored on individual assessment of each
patient. Therefore, to prevent the HCAI transmission, this training will help emphasise that
HCWs must comprehend as well acknowledge all the above five moments of hand hygiene to
execute relevant actions for HH when a specific scenario calls for it.
The second action plan is the relocation on the hand sanitizers in Zayed Military Hospital Al
Batayeh since the height percentage of the reason of the non-compliance is Hand hygiene facility
are not conveniently placed with 85.21%. Thus, my action is to contact the infection control
department and the maintenance department to put a plan for the relocation of certain hand
sanitizer dispensers in the departments that complains about the barrier of performing the hand
hygiene is because of the accessibility of the hand sanitizers, the plan of the relocation will take
one-week period after the taking the approval of all the infection control committee and the
chairman. The process of the relocation takes two weeks period and we will allow them time to
get used of the new nearest location of the hand sanitizers. Accordingly, after approximately 5
weeks at 01/Sep/2019 which is the monthly audit of august the re-audit will be conducted though
using the monthly hand hygiene observation form, by me and the infection control in charge (the
on-site supervisor) or someone on his behalf from the infection control department.
Plan the re-audit
1st of September/2019 is the time of the re-audit after performing two action plans which are the
training program and the relocation of the hand sanitizers in certain departments. The re-audit
will be done mainly in the departments where the hand sanitizers were relocated. The re-audit
will be done through the infection control monthly audit for hand hygiene by using monthly hand
hygiene observation form in addition to specific questionnaire and interview that will be
reviewed by infection control department and approved by the ethical committee.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
16
Limitations
The present study was modest attempt to put forward evidence-based findings on hand hygiene
compliance and associated factors among HCPs. However, small sample size, non-probability
sampling technique and inclusive selection of HCPs from in-patient departments may impede
the generalization of the findings.
Ethical Committee permission: Obtained from Hospital Infection Control Committee (HICC) -
Zayed Military Hospital Al Batayeh, Sharjah.
References
Allegranzi, B., & Pittet, D. (2009). Role of hand hygiene in healthcare-associated
infection prevention. Journal Of Hospital Infection, 73(4), 305-315. doi:
10.1016/j.jhin.2009.04.019
Anderson, M. E., & Weese, J. S. (2016). Self-reported hand hygiene perceptions and
barriers among companion animal veterinary clinic personnel in Ontario,
Canada. The Canadian Veterinary Journal, 57(3), 282.
Ataiyero, Y., Dyson, J., & Graham, M. (2018). Barriers to hand hygiene practices among
health care workers in sub-Saharan African countries: A narrative
review. American journal of infection control.
Basurrah, M., & Madani, T. (2006). Handwashing and gloving practice among health
care workers in medical and surgical wards in a tertiary care centre in Riyadh,
Saudi Arabia. Scandinavian Journal Of Infectious Diseases, 38(8), 620-624. doi:
Limitations
The present study was modest attempt to put forward evidence-based findings on hand hygiene
compliance and associated factors among HCPs. However, small sample size, non-probability
sampling technique and inclusive selection of HCPs from in-patient departments may impede
the generalization of the findings.
Ethical Committee permission: Obtained from Hospital Infection Control Committee (HICC) -
Zayed Military Hospital Al Batayeh, Sharjah.
References
Allegranzi, B., & Pittet, D. (2009). Role of hand hygiene in healthcare-associated
infection prevention. Journal Of Hospital Infection, 73(4), 305-315. doi:
10.1016/j.jhin.2009.04.019
Anderson, M. E., & Weese, J. S. (2016). Self-reported hand hygiene perceptions and
barriers among companion animal veterinary clinic personnel in Ontario,
Canada. The Canadian Veterinary Journal, 57(3), 282.
Ataiyero, Y., Dyson, J., & Graham, M. (2018). Barriers to hand hygiene practices among
health care workers in sub-Saharan African countries: A narrative
review. American journal of infection control.
Basurrah, M., & Madani, T. (2006). Handwashing and gloving practice among health
care workers in medical and surgical wards in a tertiary care centre in Riyadh,
Saudi Arabia. Scandinavian Journal Of Infectious Diseases, 38(8), 620-624. doi:
17
10.1080/00365540600617025
Carter, E. J., Wyer, P., Giglio, J., Jia, H., Nelson, G., Kauari, V. E., & Larson, E. L.
(2016). Environmental factors and their association with emergency department
hand hygiene compliance: an observational study. BMJ Qual Saf, 25(5), 372-378.
Ducell, G., Fabry, J., & Nicoll, L. (2002). Prevention of hospital acquired infections. A
practical guide [PDF] (3rd ed.). World Health Organization.
Hand Hygiene in Healthcare Settings | CDC. (2019). Retrieved 24 July 2019, from
https://www.cdc.gov/handhygiene/
Kingston, L. M., Slevin, B. L., O'Connell, N. H., & Dunne, C. P. (2017). Attitudes and
practices of Irish hospital-based physicians towards hand hygiene and hand
rubbing using alcohol-based hand rub: a comparison between 2007 and
2015. Journal of Hospital Infection, 97(1), 17-25.
Kumar, P., Gupta, S., Kapil, A., Vij, A., & Singh, I. (2014). A Comparative Study of
Hand Hygiene Practices in Operation Theaters in Tertiary Level Hospitals in
Delhi, India. International Journal Of Research Foundation Of Hospital And
Health Care Administration, 2, 87-93. doi: 10.5005/jp-journals-10035-1021
Kurtz, S. L. (2017). Identification of low, high, and super gelers and barriers to hand
hygiene among intensive care unit nurses. American journal of infection
control, 45(8), 839-843.
Mearkle, R., Houghton, R., Bwonya, D., & Lindfield, R. (2016). Barriers to hand
hygiene in ophthalmic outpatients in Uganda: a mixed methods
approach. Journal of ophthalmic inflammation and infection, 6(1), 11.
Sadule-Rios, N., & Aguilera, G. (2017). Nurses’ perceptions of reasons for persistent low
rates in hand hygiene compliance. Intensive and critical care nursing, 42, 17-21.
Schwartz, X., Schmitz, M., Safdar, N., & Pop-Vicas, A. (2018). Adherence to surgical
hand antisepsis: Barriers and facilitators in a tertiary care hospital. American
journal of infection control, 46(6), 714-716.
White, K. M., Jimmieson, N. L., Obst, P. L., Graves, N., Barnett, A., Cockshaw, W., ...
& Martin, E. (2015). Using a theory of planned behaviour framework to explore
hand hygiene beliefs at the ‘5 critical moments’ among Australian hospital-based
nurses. BMC health services research, 15(1), 59.
10.1080/00365540600617025
Carter, E. J., Wyer, P., Giglio, J., Jia, H., Nelson, G., Kauari, V. E., & Larson, E. L.
(2016). Environmental factors and their association with emergency department
hand hygiene compliance: an observational study. BMJ Qual Saf, 25(5), 372-378.
Ducell, G., Fabry, J., & Nicoll, L. (2002). Prevention of hospital acquired infections. A
practical guide [PDF] (3rd ed.). World Health Organization.
Hand Hygiene in Healthcare Settings | CDC. (2019). Retrieved 24 July 2019, from
https://www.cdc.gov/handhygiene/
Kingston, L. M., Slevin, B. L., O'Connell, N. H., & Dunne, C. P. (2017). Attitudes and
practices of Irish hospital-based physicians towards hand hygiene and hand
rubbing using alcohol-based hand rub: a comparison between 2007 and
2015. Journal of Hospital Infection, 97(1), 17-25.
Kumar, P., Gupta, S., Kapil, A., Vij, A., & Singh, I. (2014). A Comparative Study of
Hand Hygiene Practices in Operation Theaters in Tertiary Level Hospitals in
Delhi, India. International Journal Of Research Foundation Of Hospital And
Health Care Administration, 2, 87-93. doi: 10.5005/jp-journals-10035-1021
Kurtz, S. L. (2017). Identification of low, high, and super gelers and barriers to hand
hygiene among intensive care unit nurses. American journal of infection
control, 45(8), 839-843.
Mearkle, R., Houghton, R., Bwonya, D., & Lindfield, R. (2016). Barriers to hand
hygiene in ophthalmic outpatients in Uganda: a mixed methods
approach. Journal of ophthalmic inflammation and infection, 6(1), 11.
Sadule-Rios, N., & Aguilera, G. (2017). Nurses’ perceptions of reasons for persistent low
rates in hand hygiene compliance. Intensive and critical care nursing, 42, 17-21.
Schwartz, X., Schmitz, M., Safdar, N., & Pop-Vicas, A. (2018). Adherence to surgical
hand antisepsis: Barriers and facilitators in a tertiary care hospital. American
journal of infection control, 46(6), 714-716.
White, K. M., Jimmieson, N. L., Obst, P. L., Graves, N., Barnett, A., Cockshaw, W., ...
& Martin, E. (2015). Using a theory of planned behaviour framework to explore
hand hygiene beliefs at the ‘5 critical moments’ among Australian hospital-based
nurses. BMC health services research, 15(1), 59.
18
World Health Organization. (2001). WHO Global Strategy for Containment of
Antimicrobial Resistance [PDF]. Retrieved from
https://www.who.int/drugresistance/WHO_Global_Strategy_English.pdf
Zayed Military Hospital - Al Batayeh. (2016). Infection control and prevention Manual.
version 1 Page no 142-148.
Zayed Military Hospital - Al Batayeh. (2019). Infection control and prevention policy
file. version 3, page no 32-38
Zellmer, C., Blakney, R., Van Hoof, S., & Safdar, N. (2015). Impact of sink location on
hand hygiene compliance for Clostridium difficile infection. American journal of
infection control, 43(4), 387-389.
World Health Organization. (2001). WHO Global Strategy for Containment of
Antimicrobial Resistance [PDF]. Retrieved from
https://www.who.int/drugresistance/WHO_Global_Strategy_English.pdf
Zayed Military Hospital - Al Batayeh. (2016). Infection control and prevention Manual.
version 1 Page no 142-148.
Zayed Military Hospital - Al Batayeh. (2019). Infection control and prevention policy
file. version 3, page no 32-38
Zellmer, C., Blakney, R., Van Hoof, S., & Safdar, N. (2015). Impact of sink location on
hand hygiene compliance for Clostridium difficile infection. American journal of
infection control, 43(4), 387-389.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
19
Appendix 1
HAND HYGIENE AUDIT FORM USING IN ZAYED MILITARY HOSPITAL
Appendix 1
HAND HYGIENE AUDIT FORM USING IN ZAYED MILITARY HOSPITAL
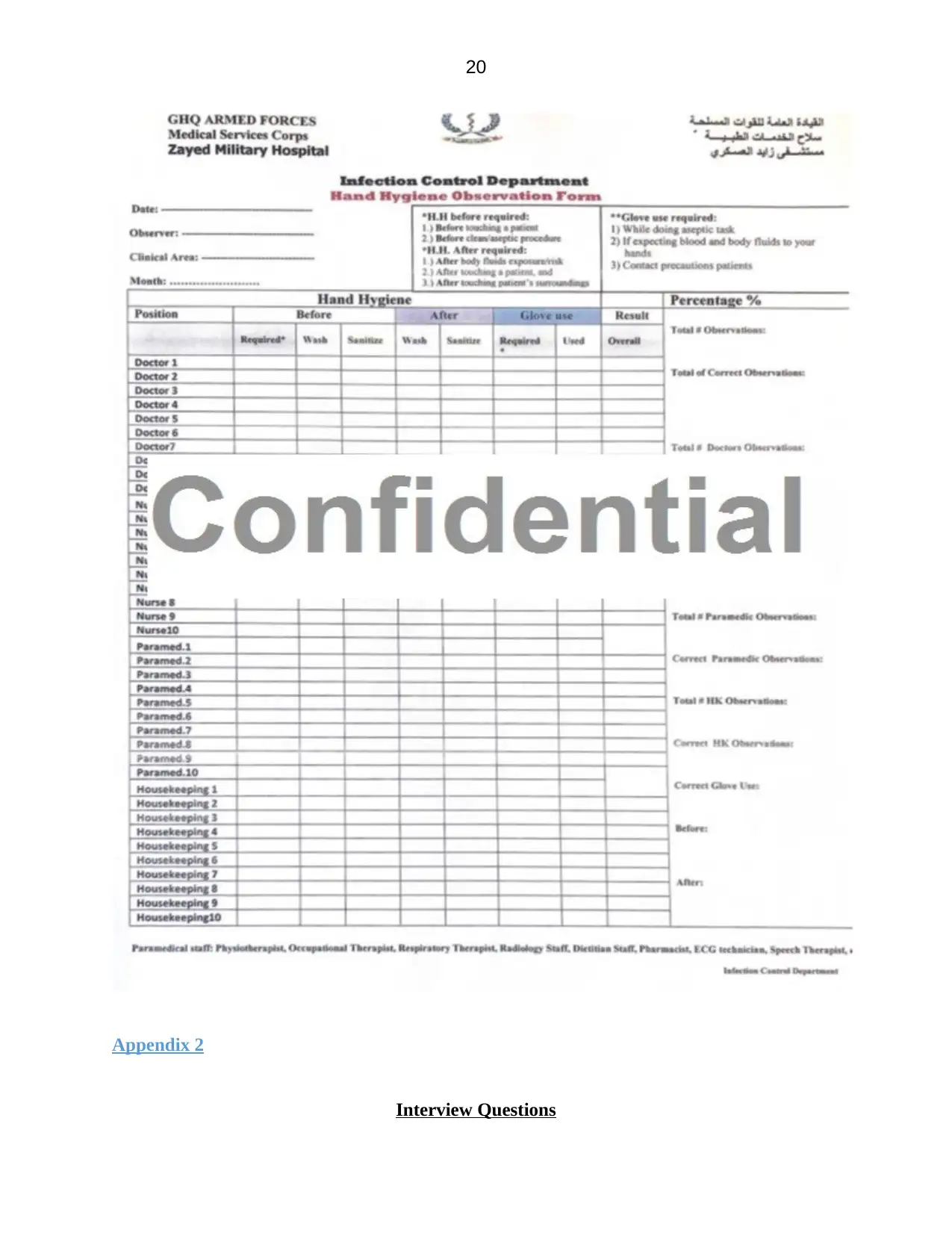
20
Appendix 2
Interview Questions
Appendix 2
Interview Questions
21
1. Does your facility provides you with adequate hand hygiene procedure?
2. What measures are needed to improve hand hygiene practice in your facility?
3. What is your major hurdles in following correct hand hygiene procedure in your facility?
4. Do you follow correct hand hygiene practice according to your facility approved policy?
5. What do you feel when your colleague omits hand hygiene?
6. Can you tell me your opinion in hand hygiene practice of newly joined HCP in your facility?
7. How do you feel about the current setup in providing adequate time to adhere to correct hand
hygiene?
8. How can the hand hygiene be made practical in other staffs?
9. Tell me about the factors makes hand hygiene difficult in your facility?
10. Do you follow correct hand hygiene procedure?
1. Does your facility provides you with adequate hand hygiene procedure?
2. What measures are needed to improve hand hygiene practice in your facility?
3. What is your major hurdles in following correct hand hygiene procedure in your facility?
4. Do you follow correct hand hygiene practice according to your facility approved policy?
5. What do you feel when your colleague omits hand hygiene?
6. Can you tell me your opinion in hand hygiene practice of newly joined HCP in your facility?
7. How do you feel about the current setup in providing adequate time to adhere to correct hand
hygiene?
8. How can the hand hygiene be made practical in other staffs?
9. Tell me about the factors makes hand hygiene difficult in your facility?
10. Do you follow correct hand hygiene procedure?
1 out of 22
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





