MDR Resistance Drug Treatment: Identification of Resistant Genes
VerifiedAdded on 2022/12/01
|14
|3014
|402
Report
AI Summary
This report provides a comprehensive analysis of Multidrug-Resistant Tuberculosis (MDR TB), focusing on the identification of resistant genes and effective treatment strategies. The study investigates the use of qualitative PCR and molecular beacon assays for identifying mutant genes in Mycobacterium tuberculosis. It also examines the efficacy of the drug bedaquiline, including its target site within the bacteria and its impact on antibiotic resistance. Furthermore, the paper proposes targeting biofilm formation as a key strategy to prevent drug resistance. The report includes detailed procedures, results, and a discussion of the challenges and potential solutions for managing MDR TB, with references to relevant research and guidelines. The study highlights the importance of understanding resistance mechanisms and developing innovative approaches to combat this significant global health threat.

Running Head: MDR RESISTANCE DRUG TREATMENT
MDR RESISTANCE DRUG TREATMENT
Name of the Student
Name of the University
Author Note
MDR RESISTANCE DRUG TREATMENT
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1MDR RESISTANCE DRUG TREATMENT
Abstract
The MDR TB represents the multi-drug resistance tuberculosis in which the bacteria
Mycobacterium tuberculosis shows resistance to a large number of antibiotics and thus, this
paper will focus on the different methods that can be used for the identification of the
resistant or mutant gene present in the bacterium. This methods will include the qualitative
PCR as well as the molecular beacon assay that will help in the identification of the mutant
gene and the differentiation from the wild type respectively. The paper also focuses on the
drug bedaquiline and tests for its target site in order to validate the antibiotic pumping system
that will help in the better analysis of the drug and the target site within the bacteria. Finally,
the paper also proposes certain changes in the development of the drug by targeting the
biofilm formation in the bacteria. If a drug can prevent the formation of the drug in the
bacteria then it will be able to prevent the resistance as the biofilm acts as a sanitizer for the
antibiotics, thus, helping the antibiotics.
Abstract
The MDR TB represents the multi-drug resistance tuberculosis in which the bacteria
Mycobacterium tuberculosis shows resistance to a large number of antibiotics and thus, this
paper will focus on the different methods that can be used for the identification of the
resistant or mutant gene present in the bacterium. This methods will include the qualitative
PCR as well as the molecular beacon assay that will help in the identification of the mutant
gene and the differentiation from the wild type respectively. The paper also focuses on the
drug bedaquiline and tests for its target site in order to validate the antibiotic pumping system
that will help in the better analysis of the drug and the target site within the bacteria. Finally,
the paper also proposes certain changes in the development of the drug by targeting the
biofilm formation in the bacteria. If a drug can prevent the formation of the drug in the
bacteria then it will be able to prevent the resistance as the biofilm acts as a sanitizer for the
antibiotics, thus, helping the antibiotics.
2MDR RESISTANCE DRUG TREATMENT
Table of Contents
Introduction....................................................................................................................3
Procedure........................................................................................................................4
Results............................................................................................................................6
Discussion......................................................................................................................7
Conclusion......................................................................................................................8
References......................................................................................................................9
Table of Contents
Introduction....................................................................................................................3
Procedure........................................................................................................................4
Results............................................................................................................................6
Discussion......................................................................................................................7
Conclusion......................................................................................................................8
References......................................................................................................................9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3MDR RESISTANCE DRUG TREATMENT
Introduction
When a single bacteria is resistant to a number of antibiotic it is called to be multidrug
resistant bacteria or MDR bacteria. This property of resistance can be either due to the
presence of a resistance gene in the bacteria which can accumulate through the small DNA
pieces called plasmids that can be transferred between two bacteria in a single event. The
other way is the presence of a single resistance mechanism that can provide resistance to
more than one type of antibiotic in a bacteria. For instance, efflux or pumping out of
antibiotic is one strategy that is being used by the bacteria to pump out variety of antibiotics
out of the cell. This pumping mechanism is able to identify a large number of small-sized
molecule and thus, can pump out different antibiotics. This way the bacteria automatically
develops a power of resistance against a number of bacteria (Migliori et al., 2013).
The MDR bacteria are thus, posing a great problem now as it becomes difficult to
treat the infections with the multidrug resistant bacteria. In certain cases, the clinicians advice
the patients with some drugs that are much more toxic for the patient than to the bacteria. The
MDR. The drug resistance also causes the spread of more and more antibiotic resistance
(Kuaban et al., 2015). The recent rise in the list of MDR bacteria are the Mycobacterium
tuberculosis that causes tuberculosis or TB. Thus, the treatment to TB has become a lot more
difficult and requires the use of a consortium of drugs in order to treat the bacterial disease
(Falzon et al., 2013).
The earlier treatment regime included the four effective drugs namely isoniazid,
rifampicin, etambutol and pyraniazid (Abubakar et al., 2013). However, TB continues to
cause a lot of morbidity and mortality among the patients that raised the need to develop
another set of therapy that is less invasive and more helpful in the treatment procedure
(Zumla, Payam & Col, 2013).
Introduction
When a single bacteria is resistant to a number of antibiotic it is called to be multidrug
resistant bacteria or MDR bacteria. This property of resistance can be either due to the
presence of a resistance gene in the bacteria which can accumulate through the small DNA
pieces called plasmids that can be transferred between two bacteria in a single event. The
other way is the presence of a single resistance mechanism that can provide resistance to
more than one type of antibiotic in a bacteria. For instance, efflux or pumping out of
antibiotic is one strategy that is being used by the bacteria to pump out variety of antibiotics
out of the cell. This pumping mechanism is able to identify a large number of small-sized
molecule and thus, can pump out different antibiotics. This way the bacteria automatically
develops a power of resistance against a number of bacteria (Migliori et al., 2013).
The MDR bacteria are thus, posing a great problem now as it becomes difficult to
treat the infections with the multidrug resistant bacteria. In certain cases, the clinicians advice
the patients with some drugs that are much more toxic for the patient than to the bacteria. The
MDR. The drug resistance also causes the spread of more and more antibiotic resistance
(Kuaban et al., 2015). The recent rise in the list of MDR bacteria are the Mycobacterium
tuberculosis that causes tuberculosis or TB. Thus, the treatment to TB has become a lot more
difficult and requires the use of a consortium of drugs in order to treat the bacterial disease
(Falzon et al., 2013).
The earlier treatment regime included the four effective drugs namely isoniazid,
rifampicin, etambutol and pyraniazid (Abubakar et al., 2013). However, TB continues to
cause a lot of morbidity and mortality among the patients that raised the need to develop
another set of therapy that is less invasive and more helpful in the treatment procedure
(Zumla, Payam & Col, 2013).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4MDR RESISTANCE DRUG TREATMENT
Procedure
The identification of new drugs for the treatment of the disease will include the meta-
analysis of the patients suffering from the disease. This will help in giving a complete review
about the condition of the disease in different patients who belong to different categories like
age, gender or even their location like whether the patients are located in the rural areas or the
urban areas (Migliori et al., 2013). Then there will be collection of blood samples from the
different participants for the study that will give a broad idea about the presence or absence of
bacteria. Then the blood samples with the identified bacterial group will be used for the
further analysis that will include qualitative PCR as well as the real time PCR with the
identifiable bacterial primer that will give a quantified amount of the bacterial DNA. This
bacterial DNA will be stored at -80ºC that will prevent it from thawing and the DNA will not
be destroyed (Prabowo et al., 2013). The qualitative PCR was done in order to check and
quantify the amount of hetero-resistance in MDR Tb. Hetero-resistance develops when
certain subpopulations of bacteria attain resistance in the presence of antibiotic thus, giving
rise to complete resistance (Pholwat et al., 2013). This method can be detected by the culture-
based methods or by sequencing the gene using the PCR-based technologies. This method
will be helpful in order to identify the desired gene of interest that is giving the bacteria
resistance against such a broad spectrum of antibiotics. Molecular Beacon assay can be done
to identify the mutant targets of the gene that is being mixed with the wild type DNA. These
methods rely on the fact that the position of the amplification curve with respect to the cycle-
axis is a measure for the initial quantity of the sample (Banu et al., 2014). The process
involves the use of the mycobacterial strain Mycobacterium tuberculosis and an extremely
resistant drug resistant strain of the bacteria. The isolates were cultured on the LB media for
about two weeks at 37ºC and then the cell suspensions were prepared. After that the DNA
Procedure
The identification of new drugs for the treatment of the disease will include the meta-
analysis of the patients suffering from the disease. This will help in giving a complete review
about the condition of the disease in different patients who belong to different categories like
age, gender or even their location like whether the patients are located in the rural areas or the
urban areas (Migliori et al., 2013). Then there will be collection of blood samples from the
different participants for the study that will give a broad idea about the presence or absence of
bacteria. Then the blood samples with the identified bacterial group will be used for the
further analysis that will include qualitative PCR as well as the real time PCR with the
identifiable bacterial primer that will give a quantified amount of the bacterial DNA. This
bacterial DNA will be stored at -80ºC that will prevent it from thawing and the DNA will not
be destroyed (Prabowo et al., 2013). The qualitative PCR was done in order to check and
quantify the amount of hetero-resistance in MDR Tb. Hetero-resistance develops when
certain subpopulations of bacteria attain resistance in the presence of antibiotic thus, giving
rise to complete resistance (Pholwat et al., 2013). This method can be detected by the culture-
based methods or by sequencing the gene using the PCR-based technologies. This method
will be helpful in order to identify the desired gene of interest that is giving the bacteria
resistance against such a broad spectrum of antibiotics. Molecular Beacon assay can be done
to identify the mutant targets of the gene that is being mixed with the wild type DNA. These
methods rely on the fact that the position of the amplification curve with respect to the cycle-
axis is a measure for the initial quantity of the sample (Banu et al., 2014). The process
involves the use of the mycobacterial strain Mycobacterium tuberculosis and an extremely
resistant drug resistant strain of the bacteria. The isolates were cultured on the LB media for
about two weeks at 37ºC and then the cell suspensions were prepared. After that the DNA
5MDR RESISTANCE DRUG TREATMENT
was extracted from each suspension and the template was stored at -20ºC (Colman et al.,
2016; Ruitjer et al., 2013).
After that the next step will include the application of the drug Bedaquiline that is
approved by the FDA as the only drug which can treat the resistant tuberculosis. The effect of
bedaquiline is that it will have the anti-mycobacterial activity derived from the inhibition of
the proton pump of mycobacterial ATP synthase (Mahajan, 2013). The drug binds to the
oligomeric and proteolipic subunit of mycobacterial ATP synthase. This was tested by the
patient’s sputum so that it becomes free of Mycobacterium tuberculosis (Cohen, 2013). The
development of the FDA approved drug was done after several testing on the bacteria. The
test was performed on the sputum in which bedaquiline was administered that increased the
sputum culture conversion that showed the effective reduction in the time for the treatment
period. Along with that it also showed reduced adverse effects that were associated with
some of the second-line anti-TB drug (Tiberi et al., 2014). In order to know the proper dosage
of the drug 160 random participants were assigned to use 400 mg of the drug once daily for
about 2 weeks followed by the 200 mg of the drug three times in a week for 22 weeks and
some participants were asked to take both the dosage in combination. The results were
measured with the help of primary sputum conversion in liquid broth (Diacon et al., 2014).
The identification of MDR strain over culture plates is an important step in the
analysis of the drug for the treatment of the disease as then it will be easier for the
identification of the culturable and non-culturable bacterial strain. This was done by the
application of the antibiotic spectrinomycin plates in order to know the range or group of
antibiotics to which these bacteria show resistant (Wang et al., 2013). Another important part
of mycobacterium is the formation of the biofilm in mycobacterium that has bactericidal
property against both the resistant as well as drug susceptible Mtb and also helps in the
sterilization of the bacteria. This was done after the appearance of the strain on the culture
was extracted from each suspension and the template was stored at -20ºC (Colman et al.,
2016; Ruitjer et al., 2013).
After that the next step will include the application of the drug Bedaquiline that is
approved by the FDA as the only drug which can treat the resistant tuberculosis. The effect of
bedaquiline is that it will have the anti-mycobacterial activity derived from the inhibition of
the proton pump of mycobacterial ATP synthase (Mahajan, 2013). The drug binds to the
oligomeric and proteolipic subunit of mycobacterial ATP synthase. This was tested by the
patient’s sputum so that it becomes free of Mycobacterium tuberculosis (Cohen, 2013). The
development of the FDA approved drug was done after several testing on the bacteria. The
test was performed on the sputum in which bedaquiline was administered that increased the
sputum culture conversion that showed the effective reduction in the time for the treatment
period. Along with that it also showed reduced adverse effects that were associated with
some of the second-line anti-TB drug (Tiberi et al., 2014). In order to know the proper dosage
of the drug 160 random participants were assigned to use 400 mg of the drug once daily for
about 2 weeks followed by the 200 mg of the drug three times in a week for 22 weeks and
some participants were asked to take both the dosage in combination. The results were
measured with the help of primary sputum conversion in liquid broth (Diacon et al., 2014).
The identification of MDR strain over culture plates is an important step in the
analysis of the drug for the treatment of the disease as then it will be easier for the
identification of the culturable and non-culturable bacterial strain. This was done by the
application of the antibiotic spectrinomycin plates in order to know the range or group of
antibiotics to which these bacteria show resistant (Wang et al., 2013). Another important part
of mycobacterium is the formation of the biofilm in mycobacterium that has bactericidal
property against both the resistant as well as drug susceptible Mtb and also helps in the
sterilization of the bacteria. This was done after the appearance of the strain on the culture
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6MDR RESISTANCE DRUG TREATMENT
plate by the transcriptional assay which revealed that there are certain small molecules whose
down-regulation can cause the resistance in TB and thus, to target the biofilm formation
should be the next step in the development of new drug (Ramon et al., 2011).
Results
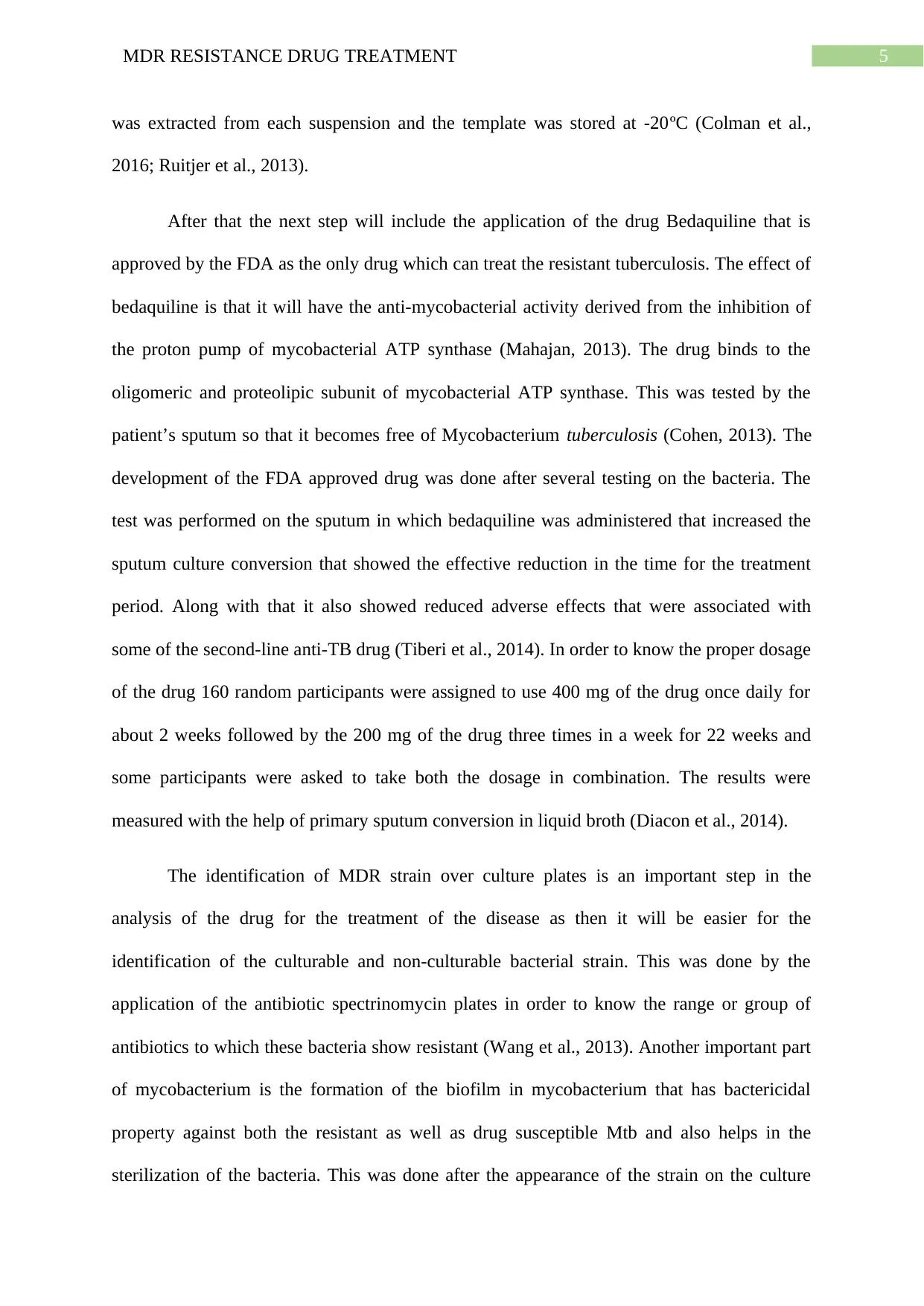
The results highlight the presence of the mutant gene in the bacteria as well as the
target site for the action of the drug bedaquiline. The results of the qualitative PCR clearly
tell the site for the mutant gene that shows the difference between the wild type and the
mutant gene in the strains of the Mycobacterium tuberculosis. The results showing the
normal gene as well as the mutant gene (Rocha, Santos & Pacheco, 2015; Udikovic-Kolic et
al., 2014)
plate by the transcriptional assay which revealed that there are certain small molecules whose
down-regulation can cause the resistance in TB and thus, to target the biofilm formation
should be the next step in the development of new drug (Ramon et al., 2011).
Results
The results highlight the presence of the mutant gene in the bacteria as well as the
target site for the action of the drug bedaquiline. The results of the qualitative PCR clearly
tell the site for the mutant gene that shows the difference between the wild type and the
mutant gene in the strains of the Mycobacterium tuberculosis. The results showing the
normal gene as well as the mutant gene (Rocha, Santos & Pacheco, 2015; Udikovic-Kolic et
al., 2014)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7MDR RESISTANCE DRUG TREATMENT
Fig-1 Normal gene expression (Onsnetwork.org, 2010)
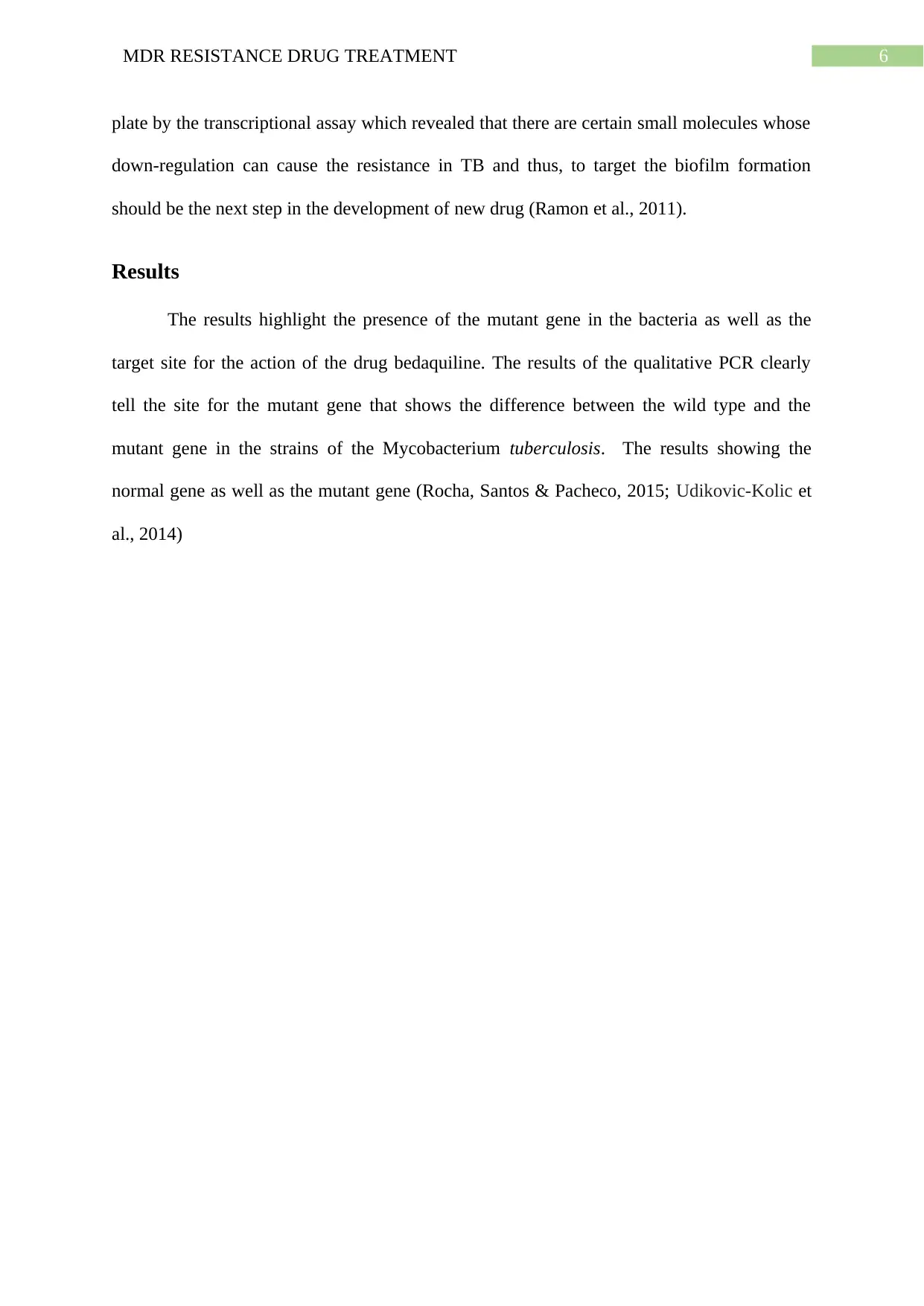
The use of the drug bedaquiline in the patients with TB is seen and the results with sputum
conversion are presented below.
Fig-1 Normal gene expression (Onsnetwork.org, 2010)
The use of the drug bedaquiline in the patients with TB is seen and the results with sputum
conversion are presented below.
8MDR RESISTANCE DRUG TREATMENT
Fig-2: Gene expression in patients with TB taking Bedaquiline (Sigma-Aldrich, 2019)
Discussion
It becomes clear that MDR TB is a growing threat to the mankind as it there is no
proper treatment for the disease. As the bacteria are resistant to a number of antibiotics it
becomes highly important to know the mechanism of resistance as well the drug which can
stop the spread of the antibiotic resistance. According to the WHO guidelines (2016), there is
certain guideline that has to be followed in order to have a proper optimal approach towards
the regimen that has to be undertaken for TB. The guidelines also highlight that the effective
treatment therapy should have a shelf life of about 12 months. The guidelines also focus on
the effect of surgery for the people with MDR TB. There are also some long term and short
term recommendations for the disease.
The experiments clearly state that Mtb is highly resistant against the broad spectrum
of the antibiotics and it has a biofilm formation that helps in the sterilization of the bacterium
from the antibiotics, thus, the next target for the antibiotics will be the prevention of biofilm
formation (Ramon et al.,2011). The bacteria also have an efflux system for pumping out the
antibiotics out of its own system and thus, it helps the bacteria to develop resistance against a
number of antibiotics. Research reveals that the drug bedaquiline helps in hampering the
antibiotic pumping system and thus, the drug has been approved by FDA for use in the
treatment of MDR TB (Tiberi et al., 2014).
Conclusion
The conclusion that can be drawn from the paper is that MDR TB really needs some
special interventions so that the treatment becomes a lot easier for the patients. As the
bacteria are very much resistant to the broad spectrum of antibiotics, thus it is necessary to do
the quantitative PCR to identify the mutant gene that gives the resistance to the bacterium.
Fig-2: Gene expression in patients with TB taking Bedaquiline (Sigma-Aldrich, 2019)
Discussion
It becomes clear that MDR TB is a growing threat to the mankind as it there is no
proper treatment for the disease. As the bacteria are resistant to a number of antibiotics it
becomes highly important to know the mechanism of resistance as well the drug which can
stop the spread of the antibiotic resistance. According to the WHO guidelines (2016), there is
certain guideline that has to be followed in order to have a proper optimal approach towards
the regimen that has to be undertaken for TB. The guidelines also highlight that the effective
treatment therapy should have a shelf life of about 12 months. The guidelines also focus on
the effect of surgery for the people with MDR TB. There are also some long term and short
term recommendations for the disease.
The experiments clearly state that Mtb is highly resistant against the broad spectrum
of the antibiotics and it has a biofilm formation that helps in the sterilization of the bacterium
from the antibiotics, thus, the next target for the antibiotics will be the prevention of biofilm
formation (Ramon et al.,2011). The bacteria also have an efflux system for pumping out the
antibiotics out of its own system and thus, it helps the bacteria to develop resistance against a
number of antibiotics. Research reveals that the drug bedaquiline helps in hampering the
antibiotic pumping system and thus, the drug has been approved by FDA for use in the
treatment of MDR TB (Tiberi et al., 2014).
Conclusion
The conclusion that can be drawn from the paper is that MDR TB really needs some
special interventions so that the treatment becomes a lot easier for the patients. As the
bacteria are very much resistant to the broad spectrum of antibiotics, thus it is necessary to do
the quantitative PCR to identify the mutant gene that gives the resistance to the bacterium.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9MDR RESISTANCE DRUG TREATMENT
The FDA approved drug was also tested in the experiment to identify the target to which
these drugs bind and can kill the resistance of the bacteria. The paper also focus that the drug
bedaquiline affects the antibiotic efflux system present inside the bacteria. The paper also
gives future recommendations for the drug target that is the prevention of the biofilm
formation in the bacteria that act as a sterilizer for the various antibiotics.
The FDA approved drug was also tested in the experiment to identify the target to which
these drugs bind and can kill the resistance of the bacteria. The paper also focus that the drug
bedaquiline affects the antibiotic efflux system present inside the bacteria. The paper also
gives future recommendations for the drug target that is the prevention of the biofilm
formation in the bacteria that act as a sterilizer for the various antibiotics.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10MDR RESISTANCE DRUG TREATMENT
References
Abubakar, I., Zignol, M., Falzon, D., Raviglione, M., Ditiu, L., Masham, S., ... & Marais, B.
J. (2013). Drug-resistant tuberculosis: time for visionary political leadership. The
Lancet infectious diseases, 13(6), 529-539.
Banu, S., Rahman, S. M., Khan, M. S. R., Ferdous, S. S., Ahmed, S., Gratz, J., ... & Houpt, E.
R. (2014). Discordance across several methods for drug susceptibility testing of drug-
resistant Mycobacterium tuberculosis isolates in a single laboratory. Journal of
clinical microbiology, 52(1), 156-163.
Cohen, J. (2013). Approval of novel TB drug celebrated—with restraint.
Colman, R. E., Anderson, J., Lemmer, D., Lehmkuhl, E., Georghiou, S. B., Heaton, H., ... &
Crudu, V. (2016). Rapid drug susceptibility testing of drug-resistant Mycobacterium
tuberculosis isolates directly from clinical samples by use of amplicon sequencing: a
proof-of-concept study. Journal of clinical microbiology, 54(8), 2058-2067.
Diacon, A. H., Pym, A., Grobusch, M. P., de Los Rios, J. M., Gotuzzo, E., Vasilyeva, I., ... &
Haxaire-Theeuwes, M. (2014). Multidrug-resistant tuberculosis and culture
conversion with bedaquiline. New England Journal of Medicine, 371(8), 723-732.
Falzon, D., Gandhi, N., Migliori, G. B., Sotgiu, G., Cox, H. S., Holtz, T. H., ... &
D'Ambrosio, L. (2013). Resistance to fluoroquinolones and second-line injectable
drugs: impact on multidrug-resistant TB outcomes. European Respiratory
Journal, 42(1), 156-168.
Kuaban, C., Noeske, J., Rieder, H. L., Ait-Khaled, N., Abena Foe, J. L., & Trébucq, A.
(2015). High effectiveness of a 12-month regimen for MDR-TB patients in
References
Abubakar, I., Zignol, M., Falzon, D., Raviglione, M., Ditiu, L., Masham, S., ... & Marais, B.
J. (2013). Drug-resistant tuberculosis: time for visionary political leadership. The
Lancet infectious diseases, 13(6), 529-539.
Banu, S., Rahman, S. M., Khan, M. S. R., Ferdous, S. S., Ahmed, S., Gratz, J., ... & Houpt, E.
R. (2014). Discordance across several methods for drug susceptibility testing of drug-
resistant Mycobacterium tuberculosis isolates in a single laboratory. Journal of
clinical microbiology, 52(1), 156-163.
Cohen, J. (2013). Approval of novel TB drug celebrated—with restraint.
Colman, R. E., Anderson, J., Lemmer, D., Lehmkuhl, E., Georghiou, S. B., Heaton, H., ... &
Crudu, V. (2016). Rapid drug susceptibility testing of drug-resistant Mycobacterium
tuberculosis isolates directly from clinical samples by use of amplicon sequencing: a
proof-of-concept study. Journal of clinical microbiology, 54(8), 2058-2067.
Diacon, A. H., Pym, A., Grobusch, M. P., de Los Rios, J. M., Gotuzzo, E., Vasilyeva, I., ... &
Haxaire-Theeuwes, M. (2014). Multidrug-resistant tuberculosis and culture
conversion with bedaquiline. New England Journal of Medicine, 371(8), 723-732.
Falzon, D., Gandhi, N., Migliori, G. B., Sotgiu, G., Cox, H. S., Holtz, T. H., ... &
D'Ambrosio, L. (2013). Resistance to fluoroquinolones and second-line injectable
drugs: impact on multidrug-resistant TB outcomes. European Respiratory
Journal, 42(1), 156-168.
Kuaban, C., Noeske, J., Rieder, H. L., Ait-Khaled, N., Abena Foe, J. L., & Trébucq, A.
(2015). High effectiveness of a 12-month regimen for MDR-TB patients in
11MDR RESISTANCE DRUG TREATMENT
Cameroon. The International Journal of Tuberculosis and Lung Disease, 19(5), 517-
524.
Mahajan, R. (2013). Bedaquiline: first FDA-approved tuberculosis drug in 40
years. International Journal of Applied and Basic Medical Research, 3(1), 1.
Migliori, G. B., Sotgiu, G., Gandhi, N. R., Falzon, D., DeRiemer, K., Centis, R., ... &
D'Ambrosio, L. (2013). Drug resistance beyond extensively drug-resistant
tuberculosis: individual patient data meta-analysis. European Respiratory
Journal, 42(1), 169-179.
Onsnetwork.org. (2010). qPCR - Hard Clam Primers on cDNA. Retrieved July 17, 2019,
from Sam’s Notebook website: http://onsnetwork.org/kubu4/2010/09/09/qpcr-hard-
clam-primers-on-cdna-from-yesterday/
Pholwat, S., Stroup, S., Foongladda, S., & Houpt, E. (2013). Digital PCR to detect and
quantify heteroresistance in drug resistant Mycobacterium tuberculosis. PloS
one, 8(2), e57238.
Prabowo, S. A., Gröschel, M. I., Schmidt, E. D., Skrahina, A., Mihaescu, T., Hastürk, S., ... &
Stanford, J. L. (2013). Targeting multidrug-resistant tuberculosis (MDR-TB) by
therapeutic vaccines. Medical microbiology and immunology, 202(2), 95-104.
Ramón-García, S., Ng, C., Anderson, H., Chao, J. D., Zheng, X., Pfeifer, T., ... & Thompson,
C. J. (2011). Synergistic drug combinations for tuberculosis therapy identified by a
novel high-throughput screen. Antimicrobial agents and chemotherapy, 55(8), 3861-
3869.
Cameroon. The International Journal of Tuberculosis and Lung Disease, 19(5), 517-
524.
Mahajan, R. (2013). Bedaquiline: first FDA-approved tuberculosis drug in 40
years. International Journal of Applied and Basic Medical Research, 3(1), 1.
Migliori, G. B., Sotgiu, G., Gandhi, N. R., Falzon, D., DeRiemer, K., Centis, R., ... &
D'Ambrosio, L. (2013). Drug resistance beyond extensively drug-resistant
tuberculosis: individual patient data meta-analysis. European Respiratory
Journal, 42(1), 169-179.
Onsnetwork.org. (2010). qPCR - Hard Clam Primers on cDNA. Retrieved July 17, 2019,
from Sam’s Notebook website: http://onsnetwork.org/kubu4/2010/09/09/qpcr-hard-
clam-primers-on-cdna-from-yesterday/
Pholwat, S., Stroup, S., Foongladda, S., & Houpt, E. (2013). Digital PCR to detect and
quantify heteroresistance in drug resistant Mycobacterium tuberculosis. PloS
one, 8(2), e57238.
Prabowo, S. A., Gröschel, M. I., Schmidt, E. D., Skrahina, A., Mihaescu, T., Hastürk, S., ... &
Stanford, J. L. (2013). Targeting multidrug-resistant tuberculosis (MDR-TB) by
therapeutic vaccines. Medical microbiology and immunology, 202(2), 95-104.
Ramón-García, S., Ng, C., Anderson, H., Chao, J. D., Zheng, X., Pfeifer, T., ... & Thompson,
C. J. (2011). Synergistic drug combinations for tuberculosis therapy identified by a
novel high-throughput screen. Antimicrobial agents and chemotherapy, 55(8), 3861-
3869.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





