University Report: Multidisciplinary Approach to Childhood Obesity
VerifiedAdded on 2023/01/23
|9
|1115
|88
Report
AI Summary
This report, prepared for a Community Health and Disease Prevention course, examines the global issue of childhood obesity, citing statistics from the World Health Organization and the Australian Institute of Health and Welfare. It explores the health risks associated with childhood obesity, such as cardiovascular diseases, and emphasizes the need for effective intervention strategies. The report proposes a multidisciplinary approach, detailing primary, secondary, and tertiary prevention levels. These levels involve behavioral changes, weight management techniques, structured dietary changes, and physical activity promotion. The report references studies supporting this approach and outlines specific actions for each prevention level, targeting vulnerable age groups and involving family participation. The report also includes a comprehensive list of references that support the research and recommendations presented.
Running head: Medical 1
Medical
by
Course:
Tutor:
University:
Department:
Date:
Medical
by
Course:
Tutor:
University:
Department:
Date:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Medical 2
A multidisciplinary approach
According to the World Health Organization (WHO), there are over 42 million children who are
overweight and are aged five years (World Health Organization, 2016). The Australian Institute
of Health and Welfare (2018) report that 1 out of 4 children in Australian aged between 2 and 17
years are obese. Moreover, 5% of the Australian burden of disease was attributed to obesity in
2011. Childhood obesity has been associated with other health risks such as high blood pressure
and high cholesterol, all of which results in the increasing prevalence of childhood obesity.
Childhood obesity has been found to increase the risk of cardiovascular diseases (Pulgaron,
2013). Due to the multiple health risks that are associated with childhood obesity, several
interventions have been proposed such as changes in diet, increased exercise (Saavedra, García-
Hermoso, Escalante, & Domínguez, 2014) among others. However, these interventions seem to
be ineffective because childhood obesity is caused by multiple factors thus necessitating the need
for an effective intervention strategy that will comprehensively address the major causes of
childhood obesity.
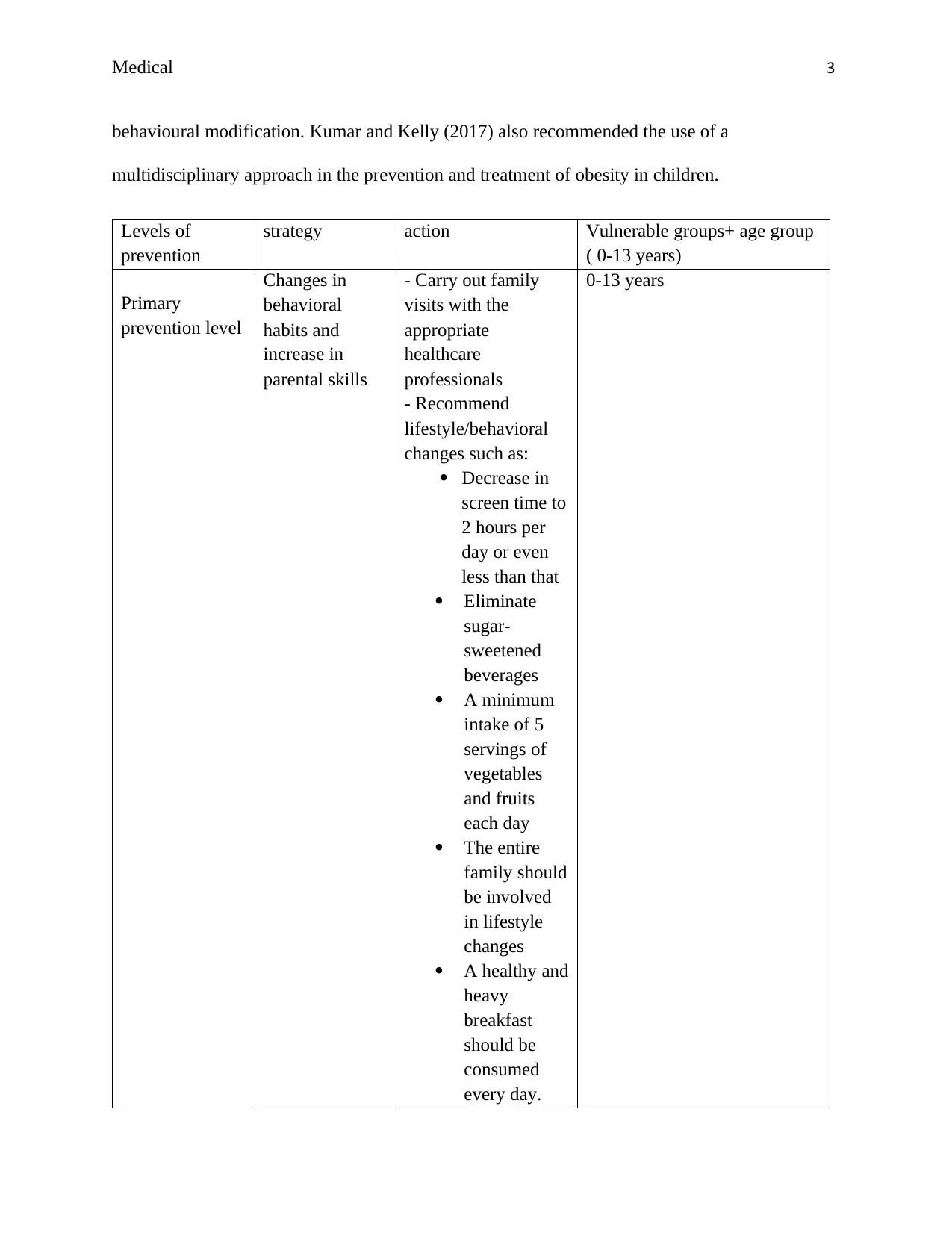
The multidisciplinary approach is an intervention strategy used in the prevention and treatement
of obesity in children. The strategy three fundamental intervention levels namely primary level
(prevention plus), secondary level (structured weight management) and tertiary levels
(multidisciplinary intervention). The primary prevention level emphasizes on elementary healthy
lifestyle, the secondary prevention level focuses on approaches geared towards weight
management such as a planned diet and supervised activity etc. tertiary prevention level involves
pharmacologic, very restrictive diets and the likelihood of weight control surgery. The study by
Ross, Kolbash, Cohen and Skelton (2010) assessed a multidisciplinary treatment of pediatric
obesity and found out that it was most effective because incorporated nutritional evaluation and
A multidisciplinary approach
According to the World Health Organization (WHO), there are over 42 million children who are
overweight and are aged five years (World Health Organization, 2016). The Australian Institute
of Health and Welfare (2018) report that 1 out of 4 children in Australian aged between 2 and 17
years are obese. Moreover, 5% of the Australian burden of disease was attributed to obesity in
2011. Childhood obesity has been associated with other health risks such as high blood pressure
and high cholesterol, all of which results in the increasing prevalence of childhood obesity.
Childhood obesity has been found to increase the risk of cardiovascular diseases (Pulgaron,
2013). Due to the multiple health risks that are associated with childhood obesity, several
interventions have been proposed such as changes in diet, increased exercise (Saavedra, García-
Hermoso, Escalante, & Domínguez, 2014) among others. However, these interventions seem to
be ineffective because childhood obesity is caused by multiple factors thus necessitating the need
for an effective intervention strategy that will comprehensively address the major causes of
childhood obesity.
The multidisciplinary approach is an intervention strategy used in the prevention and treatement
of obesity in children. The strategy three fundamental intervention levels namely primary level
(prevention plus), secondary level (structured weight management) and tertiary levels
(multidisciplinary intervention). The primary prevention level emphasizes on elementary healthy
lifestyle, the secondary prevention level focuses on approaches geared towards weight
management such as a planned diet and supervised activity etc. tertiary prevention level involves
pharmacologic, very restrictive diets and the likelihood of weight control surgery. The study by
Ross, Kolbash, Cohen and Skelton (2010) assessed a multidisciplinary treatment of pediatric
obesity and found out that it was most effective because incorporated nutritional evaluation and
Medical 3
behavioural modification. Kumar and Kelly (2017) also recommended the use of a
multidisciplinary approach in the prevention and treatment of obesity in children.
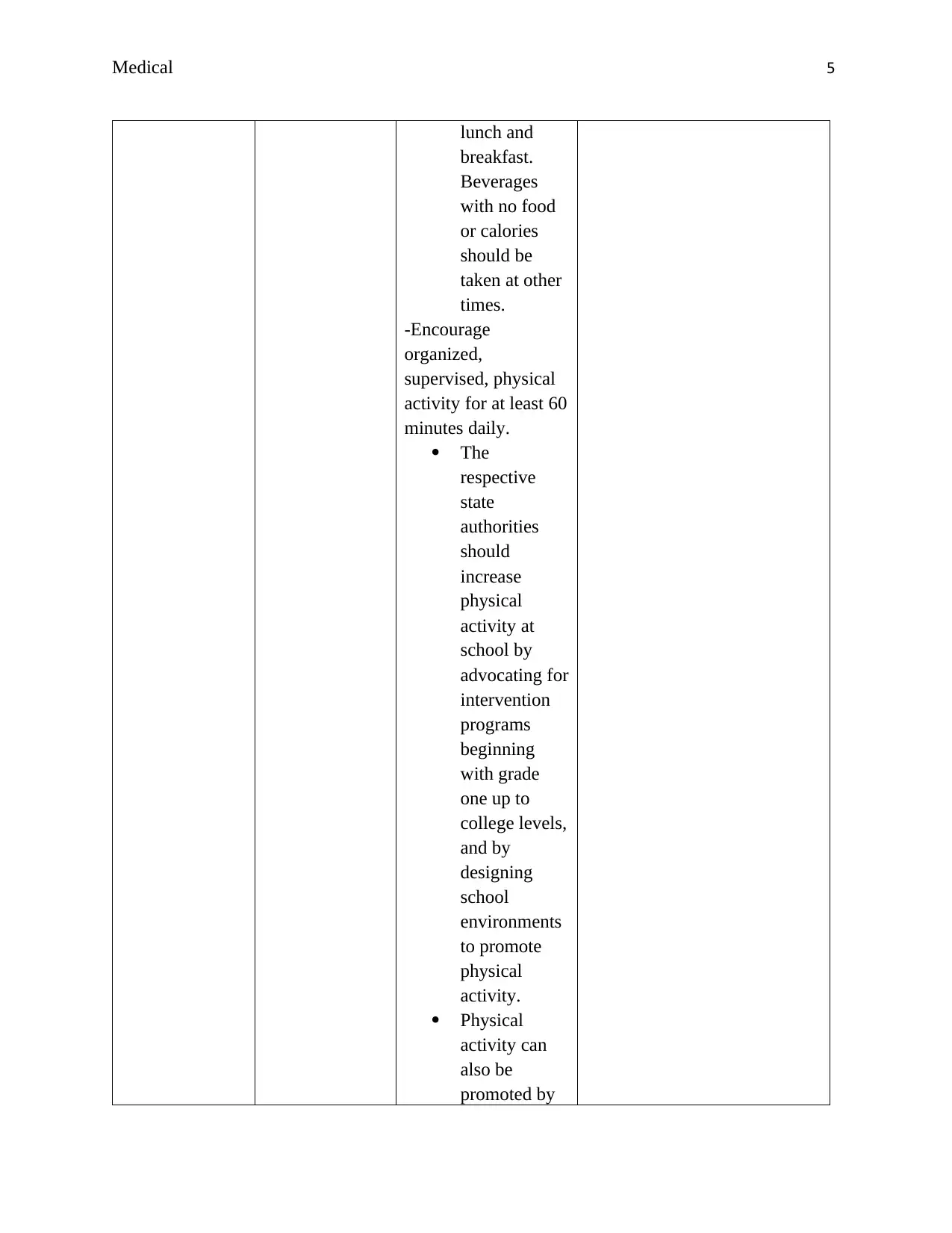
Levels of
prevention
strategy action Vulnerable groups+ age group
( 0-13 years)
Primary
prevention level
Changes in
behavioral
habits and
increase in
parental skills
- Carry out family
visits with the
appropriate
healthcare
professionals
- Recommend
lifestyle/behavioral
changes such as:
Decrease in
screen time to
2 hours per
day or even
less than that
Eliminate
sugar-
sweetened
beverages
A minimum
intake of 5
servings of
vegetables
and fruits
each day
The entire
family should
be involved
in lifestyle
changes
A healthy and
heavy
breakfast
should be
consumed
every day.
0-13 years
behavioural modification. Kumar and Kelly (2017) also recommended the use of a
multidisciplinary approach in the prevention and treatment of obesity in children.
Levels of
prevention
strategy action Vulnerable groups+ age group
( 0-13 years)
Primary
prevention level
Changes in
behavioral
habits and
increase in
parental skills
- Carry out family
visits with the
appropriate
healthcare
professionals
- Recommend
lifestyle/behavioral
changes such as:
Decrease in
screen time to
2 hours per
day or even
less than that
Eliminate
sugar-
sweetened
beverages
A minimum
intake of 5
servings of
vegetables
and fruits
each day
The entire
family should
be involved
in lifestyle
changes
A healthy and
heavy
breakfast
should be
consumed
every day.
0-13 years
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Medical 4
The family
should ensure
that more
meals are
prepared at
home than
buying fast
foods.
-Carryout
motivational
interviewing with an
objective of
negotiating for
change.
N/B. If there is no
significant
improvement after 3-
6 months, then move
to secondary
prevention level
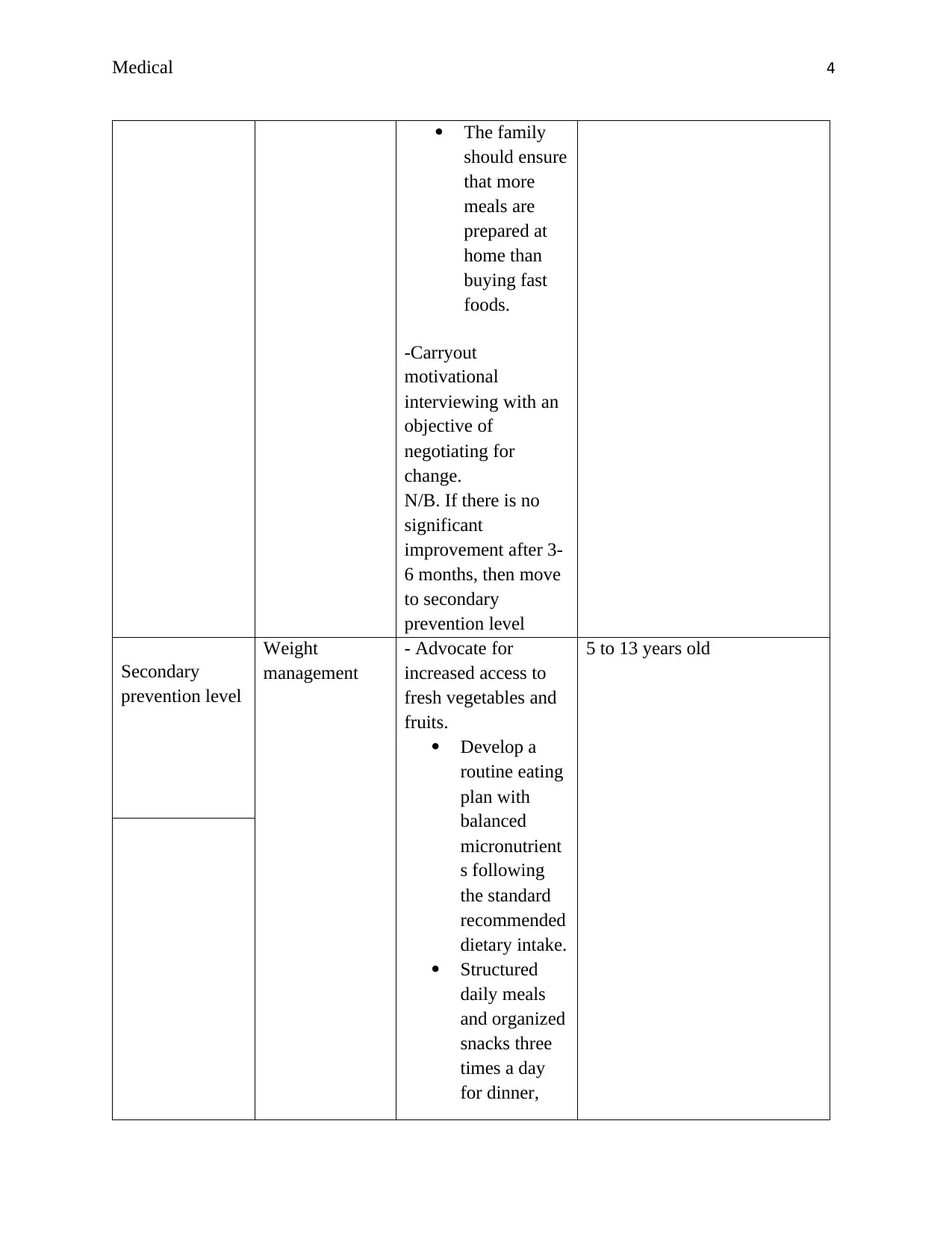
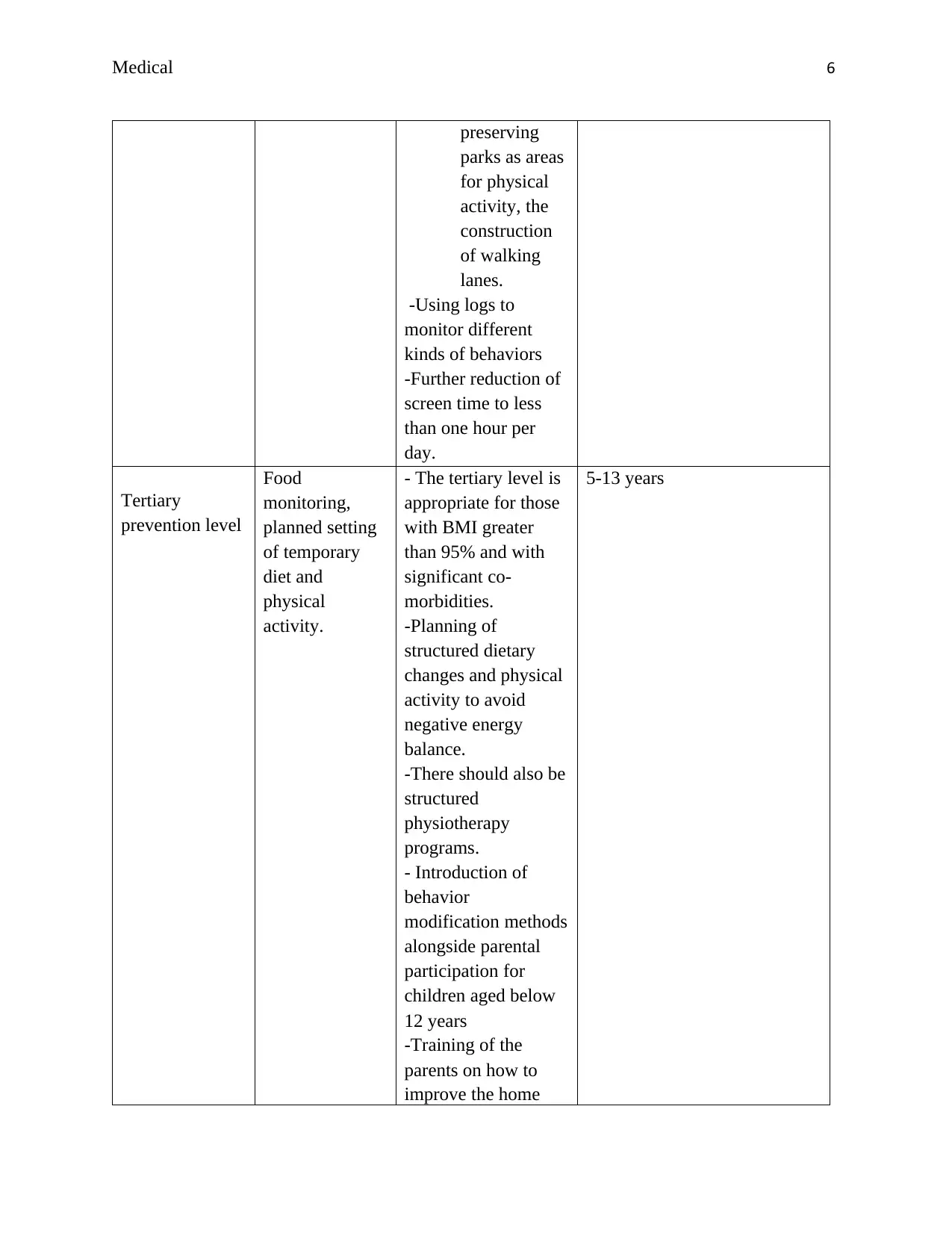
Secondary
prevention level
Weight
management
- Advocate for
increased access to
fresh vegetables and
fruits.
Develop a
routine eating
plan with
balanced
micronutrient
s following
the standard
recommended
dietary intake.
Structured
daily meals
and organized
snacks three
times a day
for dinner,
5 to 13 years old
The family
should ensure
that more
meals are
prepared at
home than
buying fast
foods.
-Carryout
motivational
interviewing with an
objective of
negotiating for
change.
N/B. If there is no
significant
improvement after 3-
6 months, then move
to secondary
prevention level
Secondary
prevention level
Weight
management
- Advocate for
increased access to
fresh vegetables and
fruits.
Develop a
routine eating
plan with
balanced
micronutrient
s following
the standard
recommended
dietary intake.
Structured
daily meals
and organized
snacks three
times a day
for dinner,
5 to 13 years old
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Medical 5
lunch and
breakfast.
Beverages
with no food
or calories
should be
taken at other
times.
-Encourage
organized,
supervised, physical
activity for at least 60
minutes daily.
The
respective
state
authorities
should
increase
physical
activity at
school by
advocating for
intervention
programs
beginning
with grade
one up to
college levels,
and by
designing
school
environments
to promote
physical
activity.
Physical
activity can
also be
promoted by
lunch and
breakfast.
Beverages
with no food
or calories
should be
taken at other
times.
-Encourage
organized,
supervised, physical
activity for at least 60
minutes daily.
The
respective
state
authorities
should
increase
physical
activity at
school by
advocating for
intervention
programs
beginning
with grade
one up to
college levels,
and by
designing
school
environments
to promote
physical
activity.
Physical
activity can
also be
promoted by
Medical 6
preserving
parks as areas
for physical
activity, the
construction
of walking
lanes.
-Using logs to
monitor different
kinds of behaviors
-Further reduction of
screen time to less
than one hour per
day.
Tertiary
prevention level
Food
monitoring,
planned setting
of temporary
diet and
physical
activity.
- The tertiary level is
appropriate for those
with BMI greater
than 95% and with
significant co-
morbidities.
-Planning of
structured dietary
changes and physical
activity to avoid
negative energy
balance.
-There should also be
structured
physiotherapy
programs.
- Introduction of
behavior
modification methods
alongside parental
participation for
children aged below
12 years
-Training of the
parents on how to
improve the home
5-13 years
preserving
parks as areas
for physical
activity, the
construction
of walking
lanes.
-Using logs to
monitor different
kinds of behaviors
-Further reduction of
screen time to less
than one hour per
day.
Tertiary
prevention level
Food
monitoring,
planned setting
of temporary
diet and
physical
activity.
- The tertiary level is
appropriate for those
with BMI greater
than 95% and with
significant co-
morbidities.
-Planning of
structured dietary
changes and physical
activity to avoid
negative energy
balance.
-There should also be
structured
physiotherapy
programs.
- Introduction of
behavior
modification methods
alongside parental
participation for
children aged below
12 years
-Training of the
parents on how to
improve the home
5-13 years
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Medical 7
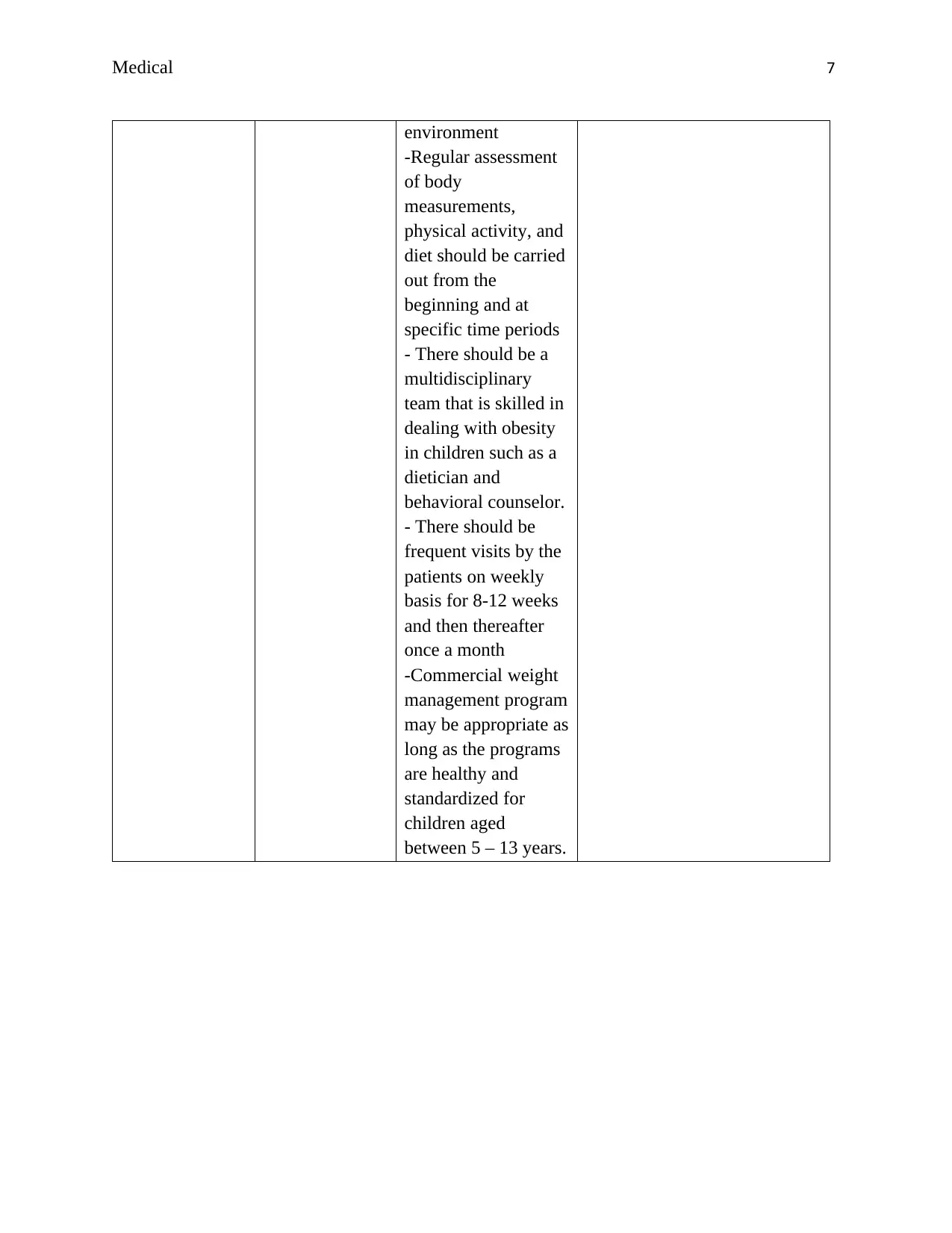
environment
-Regular assessment
of body
measurements,
physical activity, and
diet should be carried
out from the
beginning and at
specific time periods
- There should be a
multidisciplinary
team that is skilled in
dealing with obesity
in children such as a
dietician and
behavioral counselor.
- There should be
frequent visits by the
patients on weekly
basis for 8-12 weeks
and then thereafter
once a month
-Commercial weight
management program
may be appropriate as
long as the programs
are healthy and
standardized for
children aged
between 5 – 13 years.
environment
-Regular assessment
of body
measurements,
physical activity, and
diet should be carried
out from the
beginning and at
specific time periods
- There should be a
multidisciplinary
team that is skilled in
dealing with obesity
in children such as a
dietician and
behavioral counselor.
- There should be
frequent visits by the
patients on weekly
basis for 8-12 weeks
and then thereafter
once a month
-Commercial weight
management program
may be appropriate as
long as the programs
are healthy and
standardized for
children aged
between 5 – 13 years.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Medical 8
References
Australian Institute of Health and Welfare. (2018). Overweight and Obesity. Retrieved from
https://www.aihw.gov.au/reports-data/behaviours-risk-factors/overweight-obesity/
overview
Kumar, S., & Kelly, A. S. (2017, February). Review of childhood obesity: from epidemiology,
etiology, and comorbidities to clinical assessment and treatment. In Mayo Clinic
Proceedings, 92 (2), 251-265.
Pulgaron, E. R. (2013). Childhood obesity: a review of increased risk for physical and
psychological comorbidities. Clinical therapeutics, 35(1), A18-A32.
Ross, M. M., Kolbash, S., Cohen, G. M., & Skelton, J. A. (2010). Multidisciplinary treatment of
pediatric obesity: nutrition evaluation and management. Nutrition in clinical practice :
official publication of the American Society for Parenteral and Enteral Nutrition, 25(4),
327–334. doi:10.1177/0884533610373771
Saavedra, J. M., García-Hermoso, A., Escalante, Y., & Domínguez, A. M. (2014). Self-
determined motivation, physical exercise and diet in obese children: A three-year follow-
up study. International Journal of Clinical and Health Psychology, 14(3), 195-201.
World Health Organization. (2016). Report of the Commission on Ending Childhood Obesity.
Retrieved from
https://apps.who.int/iris/bitstream/handle/10665/204176/9789241510066_eng.pdf;jsessio
nid=D92C72E6BADC6E061AF15E195A3F34CA?sequence=1
References
Australian Institute of Health and Welfare. (2018). Overweight and Obesity. Retrieved from
https://www.aihw.gov.au/reports-data/behaviours-risk-factors/overweight-obesity/
overview
Kumar, S., & Kelly, A. S. (2017, February). Review of childhood obesity: from epidemiology,
etiology, and comorbidities to clinical assessment and treatment. In Mayo Clinic
Proceedings, 92 (2), 251-265.
Pulgaron, E. R. (2013). Childhood obesity: a review of increased risk for physical and
psychological comorbidities. Clinical therapeutics, 35(1), A18-A32.
Ross, M. M., Kolbash, S., Cohen, G. M., & Skelton, J. A. (2010). Multidisciplinary treatment of
pediatric obesity: nutrition evaluation and management. Nutrition in clinical practice :
official publication of the American Society for Parenteral and Enteral Nutrition, 25(4),
327–334. doi:10.1177/0884533610373771
Saavedra, J. M., García-Hermoso, A., Escalante, Y., & Domínguez, A. M. (2014). Self-
determined motivation, physical exercise and diet in obese children: A three-year follow-
up study. International Journal of Clinical and Health Psychology, 14(3), 195-201.
World Health Organization. (2016). Report of the Commission on Ending Childhood Obesity.
Retrieved from
https://apps.who.int/iris/bitstream/handle/10665/204176/9789241510066_eng.pdf;jsessio
nid=D92C72E6BADC6E061AF15E195A3F34CA?sequence=1

Medical 9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





