Medical Error: A Report on Causes, Interventions, and Safety Concerns
VerifiedAdded on 2022/10/01
|11
|2551
|25
Report
AI Summary
This report delves into the critical issue of medical errors, defining them as preventable events causing patient harm, with a focus on the Australian context where a significant percentage of hospital admissions are attributed to such errors. The study explores the causes of these errors, including incorrect medication, human factors, and unsafe medication practices, and emphasizes the importance of monitoring and evaluation to identify and prevent them. The research employs a PICO question to investigate whether computerized physician order entry systems reduce medical errors compared to paper-based systems. The report highlights the contribution of nursing knowledge in identifying and addressing errors. A SWOT analysis is used to determine the strengths, weaknesses, opportunities, and threats. The methodology includes studying an outpatient microsystem, implementing standardized work guidelines, and using a computerized system for medication reconciliation. The report reviews relevant literature, presents expected results, acknowledges limitations, and concludes that computerized systems, education, and standardized procedures are essential in reducing medical errors. The analysis suggests that a computer system, training, and guides are essential to avoid medical errors. The report underscores the importance of continued evaluation and improvement in healthcare practices.
Medical error1
MEDICAL ERROR
By (Name)
Course
Professor (Tutor)
The Name of the School
The City and State where it is located
The Date
MEDICAL ERROR
By (Name)
Course
Professor (Tutor)
The Name of the School
The City and State where it is located
The Date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Medical error2
Introduction
National Medication Error Reporting and Prevention council define medical error as
event that is preventable and can cause harm to a patient while under control of a medical
specialist. An “event that is preventable” means that error is avoidable. Medical error is a
national challenge and accounts for two or three percent of hospital admissions. This show that
230,000 of all hospital admission in Australia are caused by medical faults (Robertson, and
Long, 2018). Essentially, it is brought by patient taking wrong medicine, taking less or too much
of medicine which is estimated to have a yearly cost of $1.2 billion. Moreover, it occurs due to
human factors and other aspects that affect how drugs are administered, dispensed or prescribed.
Unsafe medication practices are a major cause of death, injury, and admission (Hines, Kynoch,
and Khalil, 2018). Therefore, avoiding them would improve the quality of health care system and
should and thus enhancing medical safety is a critical domain for the Australian Commission on
Safety and Quality in Health Care.
Monitor and evaluation is carried to identify medical errors related to marketed drug
products. This includes, generics, prescription, and over-the-counter (OTC) drugs. Voluntarily
reporting of errors is available but manufacturer, consumers, patients, and healthcare providers
are encouraged to report. Both confusing information and container labels that may lead or cause
medical errors. Regulatory action may be taken depending on roots cause, safety risk,
contributing factors and type of error to prevent further problems from occurring. In some cases,
propriety name may be changed to grapple safety concerns resulting from name confusion. Also,
tools to support safety in healthcare amenities include specialist medical charts, standardized
inpatient medication chart which reduces the chances of medical names being misread. This
Introduction
National Medication Error Reporting and Prevention council define medical error as
event that is preventable and can cause harm to a patient while under control of a medical
specialist. An “event that is preventable” means that error is avoidable. Medical error is a
national challenge and accounts for two or three percent of hospital admissions. This show that
230,000 of all hospital admission in Australia are caused by medical faults (Robertson, and
Long, 2018). Essentially, it is brought by patient taking wrong medicine, taking less or too much
of medicine which is estimated to have a yearly cost of $1.2 billion. Moreover, it occurs due to
human factors and other aspects that affect how drugs are administered, dispensed or prescribed.
Unsafe medication practices are a major cause of death, injury, and admission (Hines, Kynoch,
and Khalil, 2018). Therefore, avoiding them would improve the quality of health care system and
should and thus enhancing medical safety is a critical domain for the Australian Commission on
Safety and Quality in Health Care.
Monitor and evaluation is carried to identify medical errors related to marketed drug
products. This includes, generics, prescription, and over-the-counter (OTC) drugs. Voluntarily
reporting of errors is available but manufacturer, consumers, patients, and healthcare providers
are encouraged to report. Both confusing information and container labels that may lead or cause
medical errors. Regulatory action may be taken depending on roots cause, safety risk,
contributing factors and type of error to prevent further problems from occurring. In some cases,
propriety name may be changed to grapple safety concerns resulting from name confusion. Also,
tools to support safety in healthcare amenities include specialist medical charts, standardized
inpatient medication chart which reduces the chances of medical names being misread. This
Medical error3
research purpose to find cause of medical error, effective intervention and handle safety concerns
that lead to medical errors.
PICO Question
Our research is “Does medical error reduce by using computerized physician order entry
system than using the paper system?” This is an important question for population who are at
risk for medication error. Nurses are normally last resort of protecting individual from effect of
error as they are in charge of monitoring, administrating and dispensing medication. In hospital,
computerized system is utilized to facilitate effective dissemination information between
healthcare specialists. When computer is used, physician can record prescription, therefore,
reducing error that would be encountered by misspelling, bad while interpreting handwriting. As
such, computer system minimizes errors at very early stage. Also, it gives opportunity for nurses
to countercheck if the dosage prescribed to patient is as required or if there error at any level of
prescription. Patient safety is overarching goal of all medical practitioners and stopping medical
error at first stage is valuable step to minimize harm to society. Therefore, using computer will
be able to reduce medical error by ensuring counterchecking and order completeness.
P: population: what disease? - Outpatients in alpha hospital I
I: intervention: accurate medical record including the purpose of medication
C: Comparison: standard/alternative treatment.
research purpose to find cause of medical error, effective intervention and handle safety concerns
that lead to medical errors.
PICO Question
Our research is “Does medical error reduce by using computerized physician order entry
system than using the paper system?” This is an important question for population who are at
risk for medication error. Nurses are normally last resort of protecting individual from effect of
error as they are in charge of monitoring, administrating and dispensing medication. In hospital,
computerized system is utilized to facilitate effective dissemination information between
healthcare specialists. When computer is used, physician can record prescription, therefore,
reducing error that would be encountered by misspelling, bad while interpreting handwriting. As
such, computer system minimizes errors at very early stage. Also, it gives opportunity for nurses
to countercheck if the dosage prescribed to patient is as required or if there error at any level of
prescription. Patient safety is overarching goal of all medical practitioners and stopping medical
error at first stage is valuable step to minimize harm to society. Therefore, using computer will
be able to reduce medical error by ensuring counterchecking and order completeness.
P: population: what disease? - Outpatients in alpha hospital I
I: intervention: accurate medical record including the purpose of medication
C: Comparison: standard/alternative treatment.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Medical error4
0: Outcome: Results you are trying to bring, measure and impact. Reducing medication
reconciliation error at admission so as to enhance quality of patient safety. This enables the
patient to receive correct medication throughout medication period.
Timeless: duration taken
Problem statement
A significant proportion of medical error results in serious harm to patient because of
unclear prescriptions, drug omission, wrong doses, and delayed medication. When this problem
occurs, the inconsistency goes through the system bring potential harm to consumers.
Contribution to nursing knowledge
The nursing function has evolved from helping physician to become independent and
autonomous healthcare providers who advocate for safety of the patients. It is seen that nurses
are responsible for identifying error in the system by analyzing and counterchecking errors to
hone patient safety. Also, it is clear that there is no standard setting for medication reconciliation.
Therefore, by introducing advanced technology into hospital settings, satisfaction level of nurses
will improve. As satisfaction increases, their outcome thus increasing quality of care within
hospital setting.
Description of tenets
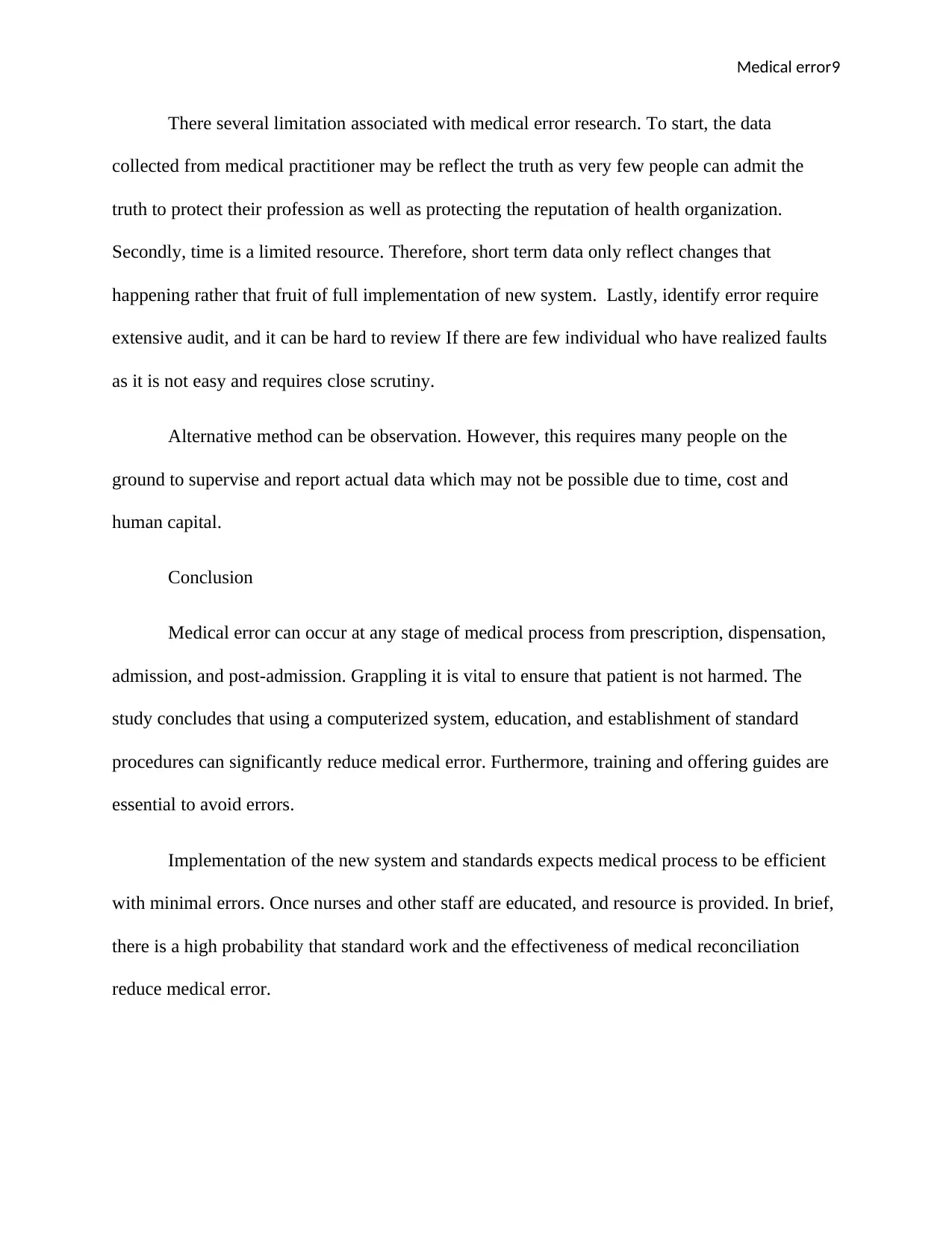
When I began analyzing issues related to medical error to hospital I was attached. I found
that numerous aspect causes this problem. Some staff raised the issue and relevant parties were
willing to address it to underpin medical safety and I volunteered to be a member of medical
administration team. We conducted the unit audit and discovered that only 40% of medical
administration was at per. Also there were discrepancies on free text notes in dosage were
0: Outcome: Results you are trying to bring, measure and impact. Reducing medication
reconciliation error at admission so as to enhance quality of patient safety. This enables the
patient to receive correct medication throughout medication period.
Timeless: duration taken
Problem statement
A significant proportion of medical error results in serious harm to patient because of
unclear prescriptions, drug omission, wrong doses, and delayed medication. When this problem
occurs, the inconsistency goes through the system bring potential harm to consumers.
Contribution to nursing knowledge
The nursing function has evolved from helping physician to become independent and
autonomous healthcare providers who advocate for safety of the patients. It is seen that nurses
are responsible for identifying error in the system by analyzing and counterchecking errors to
hone patient safety. Also, it is clear that there is no standard setting for medication reconciliation.
Therefore, by introducing advanced technology into hospital settings, satisfaction level of nurses
will improve. As satisfaction increases, their outcome thus increasing quality of care within
hospital setting.
Description of tenets
When I began analyzing issues related to medical error to hospital I was attached. I found
that numerous aspect causes this problem. Some staff raised the issue and relevant parties were
willing to address it to underpin medical safety and I volunteered to be a member of medical
administration team. We conducted the unit audit and discovered that only 40% of medical
administration was at per. Also there were discrepancies on free text notes in dosage were
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Medical error5
different from what was listed (Hines, Kynoch, and Khalil, 2018). The existence of incorrect
medical reconciliation decreases patient safety, delays care and decrease satisfaction of the
nurses. While using SWOT analysis to identify strengths of nurses, nurses had required
experience in both outpatient and inpatient setting which give them diverse skills needed in the
department. Nurses all further provided compassionate care. However, there some delays and
resistance within the unit. The threats included new standardized work and expectation is likely
to increase time for completing medical administration tasks. Therefore, data will be able to be
analyzed using electronic health records which even makes it easy for monitoring to be
conducted. Hence computerized system is established be an astute system.
When using cost-benefit analysis, a lot of expense and time is used for medication
administration meetings, pharmacy consultation and finding best practices used in magnet
institution. Approximately $9240 cost and 120 hours are used. The cost is inclusive of staff
education regarding workflow.
The benefits consisted of enhanced customer safety by increasing medical reconciliation
accuracy during the administration process, increasing nursing efficacy, and creating standardize
workflow which guarantees proper medical administration. E-prescribing tends to reduce
medical error by approximately 85% hence saving cost resulting from incorrect medication.
Methodology
The studying of microsystem of outpatient for post and pre patient which receives about
40 to 50 individuals during the night and has also a unit for overnight observation. As explained
different from what was listed (Hines, Kynoch, and Khalil, 2018). The existence of incorrect
medical reconciliation decreases patient safety, delays care and decrease satisfaction of the
nurses. While using SWOT analysis to identify strengths of nurses, nurses had required
experience in both outpatient and inpatient setting which give them diverse skills needed in the
department. Nurses all further provided compassionate care. However, there some delays and
resistance within the unit. The threats included new standardized work and expectation is likely
to increase time for completing medical administration tasks. Therefore, data will be able to be
analyzed using electronic health records which even makes it easy for monitoring to be
conducted. Hence computerized system is established be an astute system.
When using cost-benefit analysis, a lot of expense and time is used for medication
administration meetings, pharmacy consultation and finding best practices used in magnet
institution. Approximately $9240 cost and 120 hours are used. The cost is inclusive of staff
education regarding workflow.
The benefits consisted of enhanced customer safety by increasing medical reconciliation
accuracy during the administration process, increasing nursing efficacy, and creating standardize
workflow which guarantees proper medical administration. E-prescribing tends to reduce
medical error by approximately 85% hence saving cost resulting from incorrect medication.
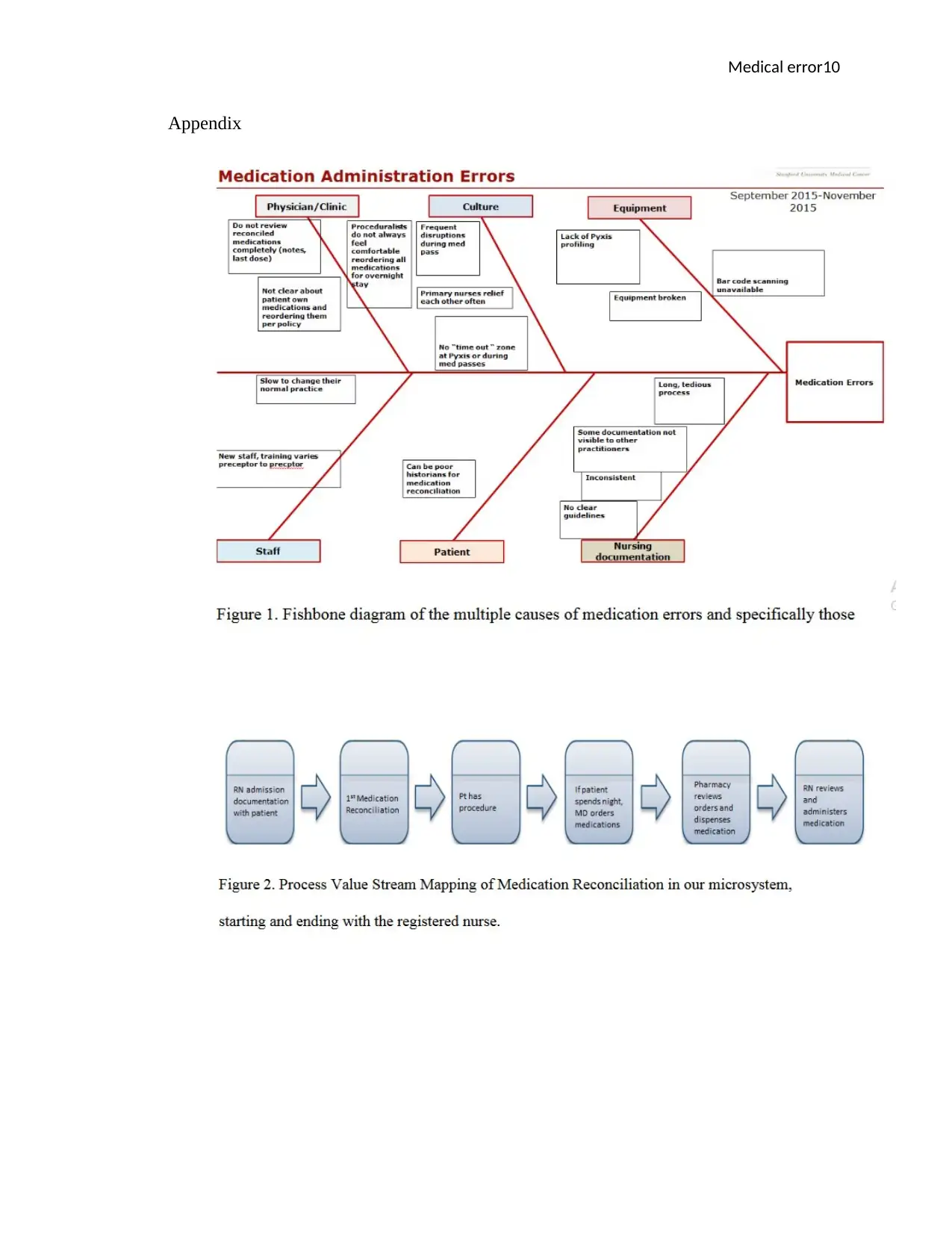
Methodology
The studying of microsystem of outpatient for post and pre patient which receives about
40 to 50 individuals during the night and has also a unit for overnight observation. As explained
Medical error6
above, the hospital faces medical administration errors and inconsistencies if illustrating medical
purposes. Moreover, medical documentation was a challenge. Hence, upon admission, we will
do medical reconciliation. Since there is electrical record system documentation, it will be
seamless to truck nurses while explaining medication verbally. It has valuable effect as it impacts
the whole patient stat. I have to work together with IT, pharmacy and nurses staff. It looks like
medication reconciliation is element that institution is aspiring to standardize. A standard work
guideline to follow by RNs who finish medical reconciliation will be established. We will run
report on computerized framework to confirm if all nurse is able complete medication
reconciliation. To identify improvements, we will closely work with pharmacy to see if there are
fewer errors being experienced and incorrect reconciliation with using computerized system. If
the system is effective, we will be able to see if we can reach and maintain 80% accuracy level of
all medications,
The project team has been working with the health records team and pharmacy in order
to develop short term success for major challenges. The process is low as the issue has many
later, and its small progress is recognized, staff will be motivated to continue engaging in the
process. In effect, it demonstrates interpersonal relations, effective communication and
collaboration among health delivery team. Upon completion of the project, we will continue to
evaluate the progress inconsistent with PDCA cycle and align our self-consistent with the cycle.
When revision is done, employee approved and examined tested standard work, we can utilize it
successfully, and it has to add task or tie to staff work.
Data source
above, the hospital faces medical administration errors and inconsistencies if illustrating medical
purposes. Moreover, medical documentation was a challenge. Hence, upon admission, we will
do medical reconciliation. Since there is electrical record system documentation, it will be
seamless to truck nurses while explaining medication verbally. It has valuable effect as it impacts
the whole patient stat. I have to work together with IT, pharmacy and nurses staff. It looks like
medication reconciliation is element that institution is aspiring to standardize. A standard work
guideline to follow by RNs who finish medical reconciliation will be established. We will run
report on computerized framework to confirm if all nurse is able complete medication
reconciliation. To identify improvements, we will closely work with pharmacy to see if there are
fewer errors being experienced and incorrect reconciliation with using computerized system. If
the system is effective, we will be able to see if we can reach and maintain 80% accuracy level of
all medications,
The project team has been working with the health records team and pharmacy in order
to develop short term success for major challenges. The process is low as the issue has many
later, and its small progress is recognized, staff will be motivated to continue engaging in the
process. In effect, it demonstrates interpersonal relations, effective communication and
collaboration among health delivery team. Upon completion of the project, we will continue to
evaluate the progress inconsistent with PDCA cycle and align our self-consistent with the cycle.
When revision is done, employee approved and examined tested standard work, we can utilize it
successfully, and it has to add task or tie to staff work.
Data source
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Medical error7
The study focuses on unit information assessment, the patient's satisfactory story
associated with medical error and staff have driven audits. It is critical for us to consider daily
medication reconciliation frequency due to high number of patients in Alpha Hospital.
Additionally, for me to reach medication safety as per National patient safety goals, PICOT was
utilized for search of research questions.
I used Key words in the library, PubMed, google scholar to search keywords like patient
safety, medical error, and medication reconciliation to find article, and readouts relevant to area
of study.
Literature review
This section discusses previous studies regarding topic under study. Summarizing past
studies helps to know the depth which the subject has been analyzed. Prospective pilot research
by Belda-Rustarazo et al. (2015) on “Medical reconciliation at discharge and admission: an
examination of prevalence and associated risk:” establish that medication error is the main cause
of morbidity. Thus, medical reconciliation is key strategy to prevent error at any level of care
process. This study involved 814 patient and drug omission was most occurring error.
The article about “financial and clinical of Pharmacist Involvement in Discharge
Medication Reconciliation at an Academic Medical Center” authored by Sebaaly et al., 2015
insinuate that implementing medical reconciliation is very challenging task. The research
findings indicate that pharmacy involvement and medical evaluation upon discharge reduced
medical error substantially. Examination of 77 patients and 33 health attendants indicate that
The study focuses on unit information assessment, the patient's satisfactory story
associated with medical error and staff have driven audits. It is critical for us to consider daily
medication reconciliation frequency due to high number of patients in Alpha Hospital.
Additionally, for me to reach medication safety as per National patient safety goals, PICOT was
utilized for search of research questions.
I used Key words in the library, PubMed, google scholar to search keywords like patient
safety, medical error, and medication reconciliation to find article, and readouts relevant to area
of study.
Literature review
This section discusses previous studies regarding topic under study. Summarizing past
studies helps to know the depth which the subject has been analyzed. Prospective pilot research
by Belda-Rustarazo et al. (2015) on “Medical reconciliation at discharge and admission: an
examination of prevalence and associated risk:” establish that medication error is the main cause
of morbidity. Thus, medical reconciliation is key strategy to prevent error at any level of care
process. This study involved 814 patient and drug omission was most occurring error.
The article about “financial and clinical of Pharmacist Involvement in Discharge
Medication Reconciliation at an Academic Medical Center” authored by Sebaaly et al., 2015
insinuate that implementing medical reconciliation is very challenging task. The research
findings indicate that pharmacy involvement and medical evaluation upon discharge reduced
medical error substantially. Examination of 77 patients and 33 health attendants indicate that
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Medical error8
Introduction of microsystem during discharge and medication education resulted in more
positive outcomes for both nurses and patients.
According to an article written by Ruggiero et al 2014 about innovative medical
reconciliation by nurses, researchers hold that there was at least one medical error for 71% of
hospital discharge (Palojoki, Pajunen, Saranto, and Lehtonen, 2016). The Pennsylvania hospital
nurse created a time out process used during discharge, an evidence-based practice. Before
implementation, there was 77% error upon discharge, but after implementation, the discrepancies
reduced to 21%. In this case, concept of standard work was used and discharge teaching was
regarded as important. In respect, teaching of nurses will be used to place standard procedures.
Results
Bring medical safety is immeasurable that can be brought by medical reconciliation that
is reached by using the computer system. The expected results are that upon installation of
effective computer system to facilitate medical reconciliation, medical error will reduce to more
than a half. With a month and compliance of 80% medical reconciliation, 21% incident of
medical error was eliminated.
From the evaluation of feedback, all employees who used the guided found it very useful.
The progress was pleasing and medical practitioners wished they would review the guide for a
longer period. As such, a standard work templet and advanced system is the right path to reduce
errors.
Limitation
Introduction of microsystem during discharge and medication education resulted in more
positive outcomes for both nurses and patients.
According to an article written by Ruggiero et al 2014 about innovative medical
reconciliation by nurses, researchers hold that there was at least one medical error for 71% of
hospital discharge (Palojoki, Pajunen, Saranto, and Lehtonen, 2016). The Pennsylvania hospital
nurse created a time out process used during discharge, an evidence-based practice. Before
implementation, there was 77% error upon discharge, but after implementation, the discrepancies
reduced to 21%. In this case, concept of standard work was used and discharge teaching was
regarded as important. In respect, teaching of nurses will be used to place standard procedures.
Results
Bring medical safety is immeasurable that can be brought by medical reconciliation that
is reached by using the computer system. The expected results are that upon installation of
effective computer system to facilitate medical reconciliation, medical error will reduce to more
than a half. With a month and compliance of 80% medical reconciliation, 21% incident of
medical error was eliminated.
From the evaluation of feedback, all employees who used the guided found it very useful.
The progress was pleasing and medical practitioners wished they would review the guide for a
longer period. As such, a standard work templet and advanced system is the right path to reduce
errors.
Limitation
Medical error9
There several limitation associated with medical error research. To start, the data
collected from medical practitioner may be reflect the truth as very few people can admit the
truth to protect their profession as well as protecting the reputation of health organization.
Secondly, time is a limited resource. Therefore, short term data only reflect changes that
happening rather that fruit of full implementation of new system. Lastly, identify error require
extensive audit, and it can be hard to review If there are few individual who have realized faults
as it is not easy and requires close scrutiny.
Alternative method can be observation. However, this requires many people on the
ground to supervise and report actual data which may not be possible due to time, cost and
human capital.
Conclusion
Medical error can occur at any stage of medical process from prescription, dispensation,
admission, and post-admission. Grappling it is vital to ensure that patient is not harmed. The
study concludes that using a computerized system, education, and establishment of standard
procedures can significantly reduce medical error. Furthermore, training and offering guides are
essential to avoid errors.
Implementation of the new system and standards expects medical process to be efficient
with minimal errors. Once nurses and other staff are educated, and resource is provided. In brief,
there is a high probability that standard work and the effectiveness of medical reconciliation
reduce medical error.
There several limitation associated with medical error research. To start, the data
collected from medical practitioner may be reflect the truth as very few people can admit the
truth to protect their profession as well as protecting the reputation of health organization.
Secondly, time is a limited resource. Therefore, short term data only reflect changes that
happening rather that fruit of full implementation of new system. Lastly, identify error require
extensive audit, and it can be hard to review If there are few individual who have realized faults
as it is not easy and requires close scrutiny.
Alternative method can be observation. However, this requires many people on the
ground to supervise and report actual data which may not be possible due to time, cost and
human capital.
Conclusion
Medical error can occur at any stage of medical process from prescription, dispensation,
admission, and post-admission. Grappling it is vital to ensure that patient is not harmed. The
study concludes that using a computerized system, education, and establishment of standard
procedures can significantly reduce medical error. Furthermore, training and offering guides are
essential to avoid errors.
Implementation of the new system and standards expects medical process to be efficient
with minimal errors. Once nurses and other staff are educated, and resource is provided. In brief,
there is a high probability that standard work and the effectiveness of medical reconciliation
reduce medical error.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Medical error10
Appendix
Appendix
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Medical error11
Bibliography
Ruggiero, J., Smith, J., Copeland, J. and Boxer, B., 2015. Discharge time out: An innovative
nurse-driven protocol for medication reconciliation. MedSurg Nursing, 24(3), p.165.
Sebaaly, J., Parsons, L.B., Pilch, N.A., Bullington, W., Hayes, G.L. and Piasterling, H., 2015.
Clinical and financial impact of pharmacist involvement in discharge medication reconciliation
at an academic medical center: a prospective pilot study. Hospital pharmacy, 50(6), pp.505-513.
Burton, M.M., Hope, C., Murray, M.D., Hui, S. and Overhage, J.M., 2007, October. The cost of
adverse drug events in ambulatory care. In AMIA... Annual Symposium proceedings. AMIA
Symposium (pp. 90-93).
Robertson, J.J. and Long, B., 2018. Suffering in silence: medical error and its impact on health
care providers. The Journal of emergency medicine, 54(4), pp.402-409.
Delacroix, R., 2017. Exploring the experience of nurse practitioners who have committed
medical errors: A phenomenological approach. Journal of the American Association of Nurse
Practitioners, 29(7), pp.403-409.
Hines, S., Kynoch, K. and Khalil, H., 2018. Effectiveness of interventions to prevent medication
errors: an umbrella systematic review protocol. JBI database of systematic reviews and
implementation reports, 16(2), pp.291-296.
Palojoki, S., Pajunen, T., Saranto, K. and Lehtonen, L., 2016. Electronic health record-related
safety concerns: a cross-sectional survey of electronic health record users. JMIR medical
informatics, 4(2), p.e13.
Bibliography
Ruggiero, J., Smith, J., Copeland, J. and Boxer, B., 2015. Discharge time out: An innovative
nurse-driven protocol for medication reconciliation. MedSurg Nursing, 24(3), p.165.
Sebaaly, J., Parsons, L.B., Pilch, N.A., Bullington, W., Hayes, G.L. and Piasterling, H., 2015.
Clinical and financial impact of pharmacist involvement in discharge medication reconciliation
at an academic medical center: a prospective pilot study. Hospital pharmacy, 50(6), pp.505-513.
Burton, M.M., Hope, C., Murray, M.D., Hui, S. and Overhage, J.M., 2007, October. The cost of
adverse drug events in ambulatory care. In AMIA... Annual Symposium proceedings. AMIA
Symposium (pp. 90-93).
Robertson, J.J. and Long, B., 2018. Suffering in silence: medical error and its impact on health
care providers. The Journal of emergency medicine, 54(4), pp.402-409.
Delacroix, R., 2017. Exploring the experience of nurse practitioners who have committed
medical errors: A phenomenological approach. Journal of the American Association of Nurse
Practitioners, 29(7), pp.403-409.
Hines, S., Kynoch, K. and Khalil, H., 2018. Effectiveness of interventions to prevent medication
errors: an umbrella systematic review protocol. JBI database of systematic reviews and
implementation reports, 16(2), pp.291-296.
Palojoki, S., Pajunen, T., Saranto, K. and Lehtonen, L., 2016. Electronic health record-related
safety concerns: a cross-sectional survey of electronic health record users. JMIR medical
informatics, 4(2), p.e13.
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





