Medication Safety: Impact on Child and Family Nursing Practice
VerifiedAdded on 2023/01/09
|12
|3179
|28
AI Summary
This article discusses the impact of complex medication issues on child and family nursing practice. It explores the various factors that contribute to medication errors and provides effective solutions. The importance of medication safety in improving patient outcomes is also emphasized.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
Medication safety 1
Medication Safety
Medication Safety
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Medication safety 2
Overview
Medications are provided by health services throughout the world. There are various ways
through which the drug administration can go wrong such as wrong patient, wrong time, wrong
drug, wrong dose and failure to administer. Along with that there are involvements of some key
issues that outline some circumstances relevant to medication errors in primary care such as
injection use, paediatrics and care homes. In the context of providing medication to the family
and children, it is necessary for nursing practices to take care of medication step in a sophisticate
manner as it can lead patient into critical health situation (Hayes, Jackson, Davidson & Power,
2015).
Clinical question
1- Do complex issues of medication impact child and family nursing practice?
2- Does transformation in practices of medication bring changes in the safety for
medication?
Literature review
Medication is referred as a common treatment interventions used in healthcare around the world.
They contribute to noteworthy developments in the health and well being of patients. According
to Letourneau et. al., (2012), there is five “R’s” that need to be followed by the hospital in the
context of paying attention to the medication safety. These are the right patient, the right drug,
the right dose, the right route, and the right time.
Complex issues impacting child and family nursing practice and propose effective solutions
Overview
Medications are provided by health services throughout the world. There are various ways
through which the drug administration can go wrong such as wrong patient, wrong time, wrong
drug, wrong dose and failure to administer. Along with that there are involvements of some key
issues that outline some circumstances relevant to medication errors in primary care such as
injection use, paediatrics and care homes. In the context of providing medication to the family
and children, it is necessary for nursing practices to take care of medication step in a sophisticate
manner as it can lead patient into critical health situation (Hayes, Jackson, Davidson & Power,
2015).
Clinical question
1- Do complex issues of medication impact child and family nursing practice?
2- Does transformation in practices of medication bring changes in the safety for
medication?
Literature review
Medication is referred as a common treatment interventions used in healthcare around the world.
They contribute to noteworthy developments in the health and well being of patients. According
to Letourneau et. al., (2012), there is five “R’s” that need to be followed by the hospital in the
context of paying attention to the medication safety. These are the right patient, the right drug,
the right dose, the right route, and the right time.
Complex issues impacting child and family nursing practice and propose effective solutions
Medication safety 3
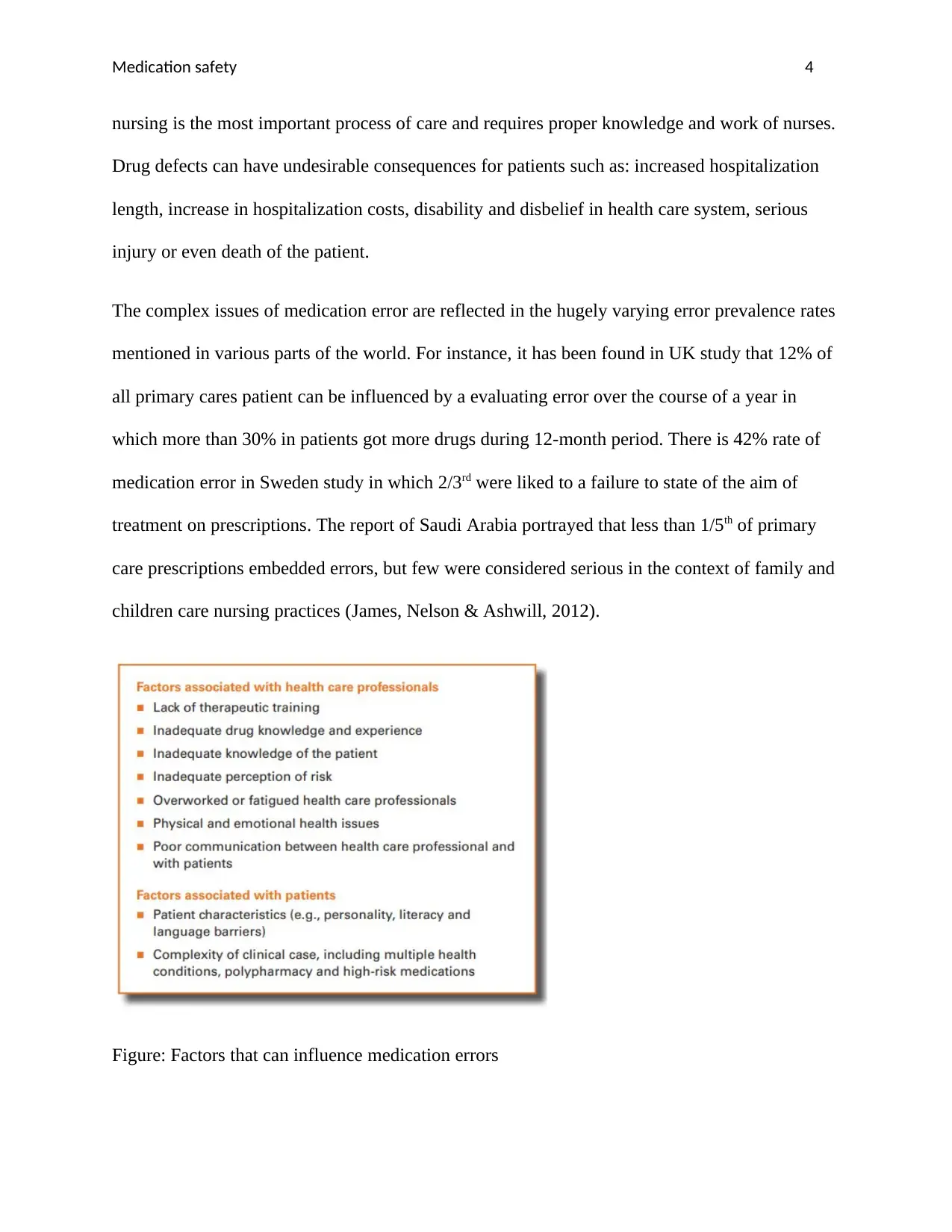
There are certain issues in medication safety which need to be considered by the healthcare
services in the context of child and family nursing practices. It has been found that Drug-drug
interaction (DDI) is portrayed as consolidation of at least two drugs so that the strength or
effectiveness of a drug is essentially replaced by the proximity of the other (Gadow, et. al.,
2016). DDI has 30% share of all unfriendly medicines and may extend the occurrence of ME. In
addition, there is an expansion of redundant prescribing in self-medication, poor correspondence
between the prescriber and the patient, and even the patient's interest for the drug for every
disclosure, the promotion and promotion of dishonest medicine. It increases the number of
medicines per prescription that can be ME and DDI. Therefore, DDI monitoring and rationality
plus ME would be an essential element of high quality of medical care (James, Nelson &
Ashwill, 2012).
Medication error is one of the most common medical errors. In addition, medication disturbances
mean an illusion in the treatment process, which is in the form of potential or actual delusional
risk for the patient. Nowadays, the complications of the prescription attract more attention given
the disadvantages of higher mortality and well-care costs. In the United States, there is a high
degree of fraud related to drug migration with car accidents, breast cancer and human
immunodeficiency virus/acquired immune deficiency syndrome (Letourneau et. al., 2012). The
reasons for drug errors in three categories of personal, relevant and knowledge-based factors
include personal factors, stress, fatigue, confusion, doctor prescription, errors in order
implementation, inadequate attention to details, lack of job satisfaction that decrease in the
feeling of unpleasant workplace, commitment and career discretion and so on. As per Goldspiel
et. al., (2015), Medical errors include determining the wrong medication at any stage of the
treatment process, which is preventive. Medication is one of the most important, complexes, yet
There are certain issues in medication safety which need to be considered by the healthcare
services in the context of child and family nursing practices. It has been found that Drug-drug
interaction (DDI) is portrayed as consolidation of at least two drugs so that the strength or
effectiveness of a drug is essentially replaced by the proximity of the other (Gadow, et. al.,
2016). DDI has 30% share of all unfriendly medicines and may extend the occurrence of ME. In
addition, there is an expansion of redundant prescribing in self-medication, poor correspondence
between the prescriber and the patient, and even the patient's interest for the drug for every
disclosure, the promotion and promotion of dishonest medicine. It increases the number of
medicines per prescription that can be ME and DDI. Therefore, DDI monitoring and rationality
plus ME would be an essential element of high quality of medical care (James, Nelson &
Ashwill, 2012).
Medication error is one of the most common medical errors. In addition, medication disturbances
mean an illusion in the treatment process, which is in the form of potential or actual delusional
risk for the patient. Nowadays, the complications of the prescription attract more attention given
the disadvantages of higher mortality and well-care costs. In the United States, there is a high
degree of fraud related to drug migration with car accidents, breast cancer and human
immunodeficiency virus/acquired immune deficiency syndrome (Letourneau et. al., 2012). The
reasons for drug errors in three categories of personal, relevant and knowledge-based factors
include personal factors, stress, fatigue, confusion, doctor prescription, errors in order
implementation, inadequate attention to details, lack of job satisfaction that decrease in the
feeling of unpleasant workplace, commitment and career discretion and so on. As per Goldspiel
et. al., (2015), Medical errors include determining the wrong medication at any stage of the
treatment process, which is preventive. Medication is one of the most important, complexes, yet
Medication safety 4
nursing is the most important process of care and requires proper knowledge and work of nurses.
Drug defects can have undesirable consequences for patients such as: increased hospitalization
length, increase in hospitalization costs, disability and disbelief in health care system, serious
injury or even death of the patient.
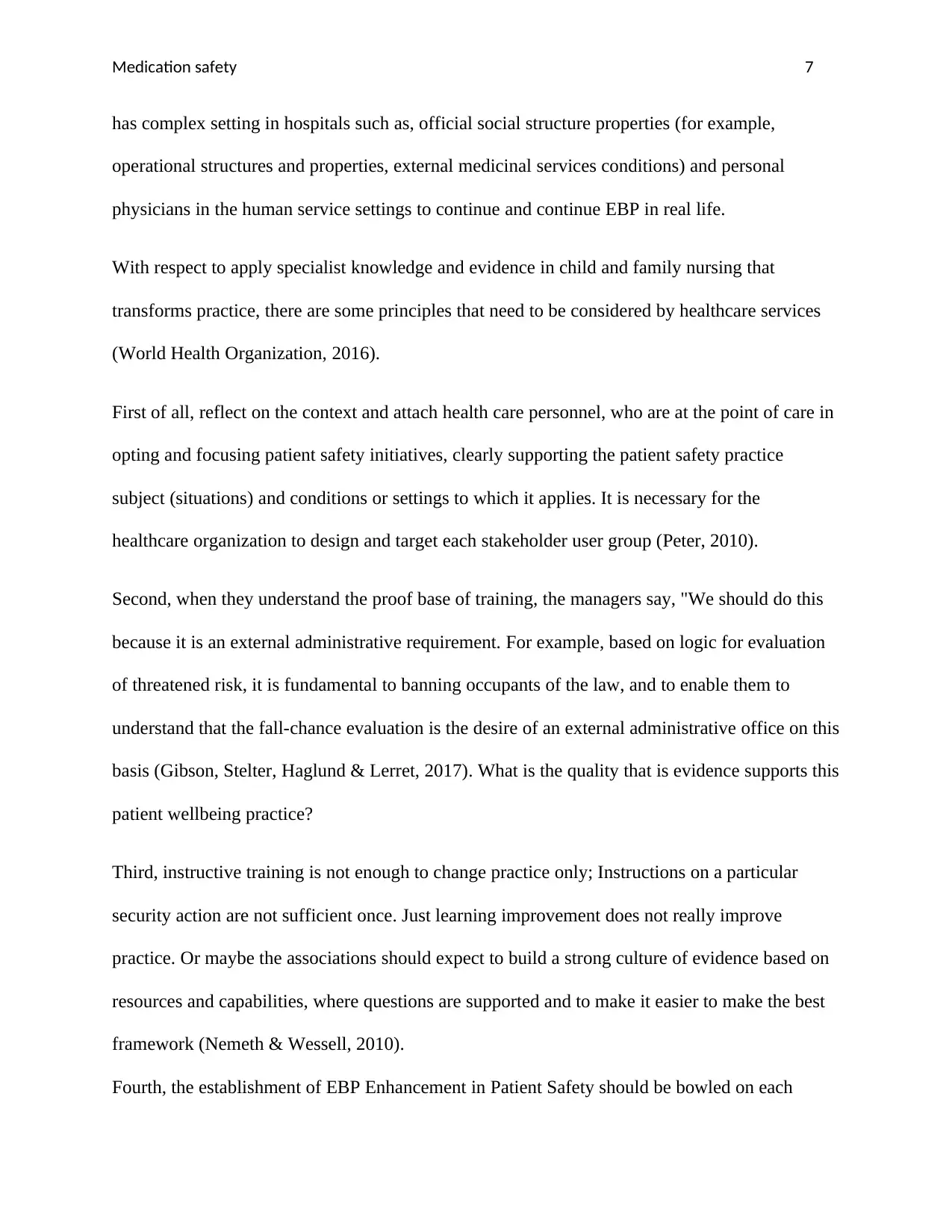
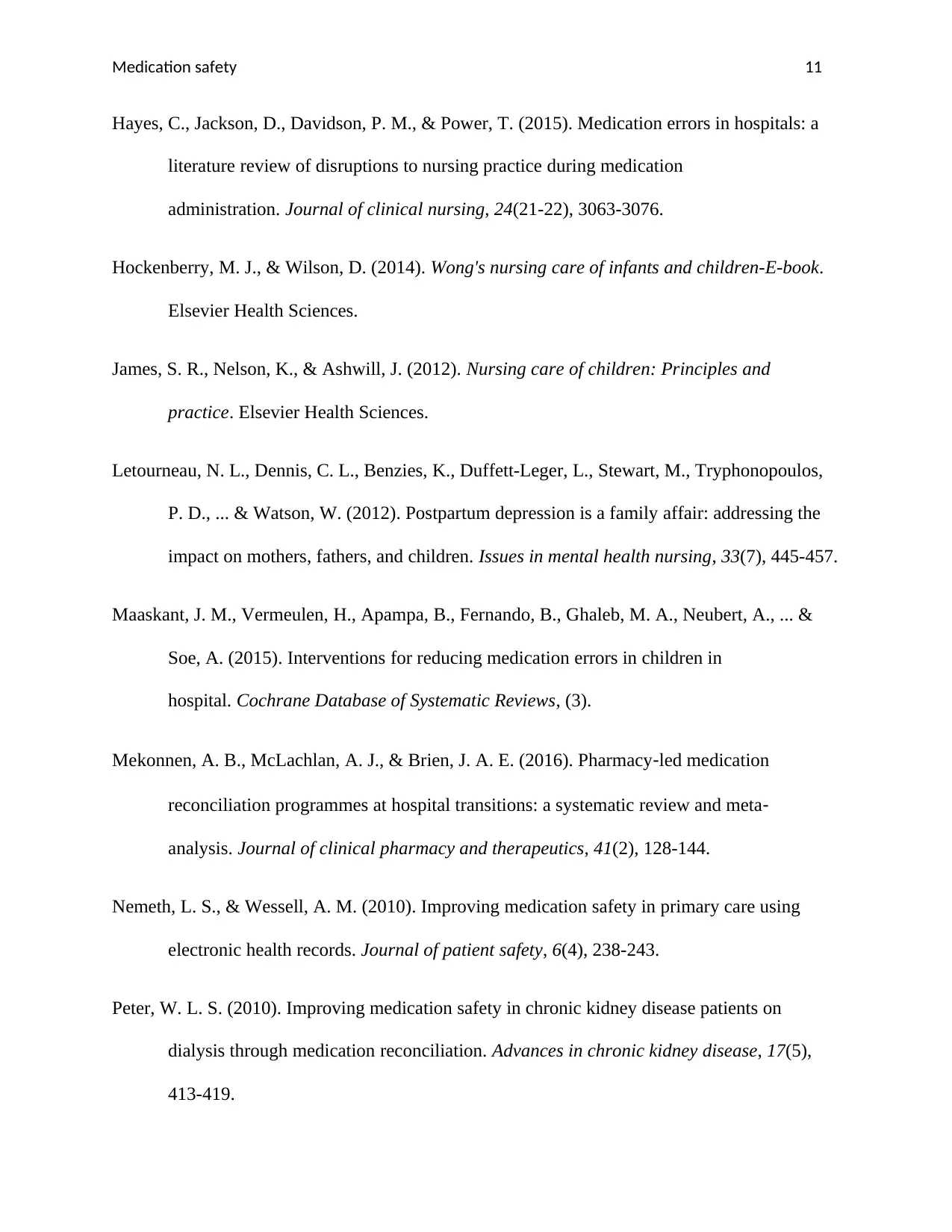
The complex issues of medication error are reflected in the hugely varying error prevalence rates
mentioned in various parts of the world. For instance, it has been found in UK study that 12% of
all primary cares patient can be influenced by a evaluating error over the course of a year in
which more than 30% in patients got more drugs during 12-month period. There is 42% rate of
medication error in Sweden study in which 2/3rd were liked to a failure to state of the aim of
treatment on prescriptions. The report of Saudi Arabia portrayed that less than 1/5th of primary
care prescriptions embedded errors, but few were considered serious in the context of family and
children care nursing practices (James, Nelson & Ashwill, 2012).
Figure: Factors that can influence medication errors
nursing is the most important process of care and requires proper knowledge and work of nurses.
Drug defects can have undesirable consequences for patients such as: increased hospitalization
length, increase in hospitalization costs, disability and disbelief in health care system, serious
injury or even death of the patient.
The complex issues of medication error are reflected in the hugely varying error prevalence rates
mentioned in various parts of the world. For instance, it has been found in UK study that 12% of
all primary cares patient can be influenced by a evaluating error over the course of a year in
which more than 30% in patients got more drugs during 12-month period. There is 42% rate of
medication error in Sweden study in which 2/3rd were liked to a failure to state of the aim of
treatment on prescriptions. The report of Saudi Arabia portrayed that less than 1/5th of primary
care prescriptions embedded errors, but few were considered serious in the context of family and
children care nursing practices (James, Nelson & Ashwill, 2012).
Figure: Factors that can influence medication errors
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Medication safety 5
Source: https://apps.who.int/iris/bitstream/handle/10665/252274/9789241511643-
eng.pdf;jsessionid=2C989A5F3DB74DE7C2FD9722F7B48965?sequence=1
In the course of the fact that, a serious lack in the nursing employees in Iran's emergency clinic
might accumulate the choice of prescription blunders event, it tends to be without a doubt that it
is not the main explanation behind the medication mistakes. It should be in the way, explored to
discover which elements may prompt. Since, the errors in medication made by healthcare team
involving nurses as well as physicians can affect the result and quality of health care, moreover
to the fact the nursing personnel and more included in medication administration activities in
comparison of health care workers, recognizing the aspects that contribute to medication errors
occurrence from the perception of nurses will facilitate in reducing the medication errors to a
minimum of nursing services (Hockenberry & Wilson, 2014).
The use of medication for children shows some extra confronts. The off-label use of medicines
can increase the issue of less care towards medication to the family and children nursing
practices. On the other hand, primary care providers do not have time to check proper
medications for family and children, which is matter to amendment over time, has the
opportunity to lead to improper prescriptions being dispensed (World Health Organizations,
2016).
Apply specialist knowledge and evidence in child and family nursing that
transforms practice
Evidence-based health care practices are accessible for, asthma, heart disappointment, and
diabetes. Conventionally, the research of patient safety has concentrated on information
investigations to recognize patient safety issues and to portray that training will lead to enhanced
Source: https://apps.who.int/iris/bitstream/handle/10665/252274/9789241511643-
eng.pdf;jsessionid=2C989A5F3DB74DE7C2FD9722F7B48965?sequence=1
In the course of the fact that, a serious lack in the nursing employees in Iran's emergency clinic
might accumulate the choice of prescription blunders event, it tends to be without a doubt that it
is not the main explanation behind the medication mistakes. It should be in the way, explored to
discover which elements may prompt. Since, the errors in medication made by healthcare team
involving nurses as well as physicians can affect the result and quality of health care, moreover
to the fact the nursing personnel and more included in medication administration activities in
comparison of health care workers, recognizing the aspects that contribute to medication errors
occurrence from the perception of nurses will facilitate in reducing the medication errors to a
minimum of nursing services (Hockenberry & Wilson, 2014).
The use of medication for children shows some extra confronts. The off-label use of medicines
can increase the issue of less care towards medication to the family and children nursing
practices. On the other hand, primary care providers do not have time to check proper
medications for family and children, which is matter to amendment over time, has the
opportunity to lead to improper prescriptions being dispensed (World Health Organizations,
2016).
Apply specialist knowledge and evidence in child and family nursing that
transforms practice
Evidence-based health care practices are accessible for, asthma, heart disappointment, and
diabetes. Conventionally, the research of patient safety has concentrated on information
investigations to recognize patient safety issues and to portray that training will lead to enhanced
Medication safety 6
quality and patient safety. Much less research consideration has been paid to how to actualize
practices. However, just by putting into practice what is found out from research will be safer.
According to Titler & Moore (2010), there are some steps that need to focused by nurse and
individual practitioners in the context of implementing evidence based practices in healthcare
system in order to transform practices for child and family nursing. These are
Knowledge creation and distillation
It is fundamental that the sophisticated process of learning for research should be educated and
guided by the ultimate customers, so that the concept of communication can be improved in real
life. The criteria used in the information purification should be to include the approach of the
final customers.
Diffusion and dissemination
Dissemination partnerships connect researcher with delegates, who can work as experts and
representatives of the Medicinal Service Convention Associations and Connectors. Middle
people can be a skilled association, for example, the National Patient Safety Foundation or a
multidisciplinary information exchange group, for example, forcing them to spread research-
based malware programs (Smyth, 2011). In this model, the dissemination organization gives a
valid stamp of support for new information and helps identify motivational meetings and
networks that can be used to make an interest in the use of evidence for practical speaking.
End user adoption, implementation, and institutionalization
This stage gives the center to achieve associations, groups and people and use the evidence-
based research discoveries and development in general practice to the surrounding people. EBP
quality and patient safety. Much less research consideration has been paid to how to actualize
practices. However, just by putting into practice what is found out from research will be safer.
According to Titler & Moore (2010), there are some steps that need to focused by nurse and
individual practitioners in the context of implementing evidence based practices in healthcare
system in order to transform practices for child and family nursing. These are
Knowledge creation and distillation
It is fundamental that the sophisticated process of learning for research should be educated and
guided by the ultimate customers, so that the concept of communication can be improved in real
life. The criteria used in the information purification should be to include the approach of the
final customers.
Diffusion and dissemination
Dissemination partnerships connect researcher with delegates, who can work as experts and
representatives of the Medicinal Service Convention Associations and Connectors. Middle
people can be a skilled association, for example, the National Patient Safety Foundation or a
multidisciplinary information exchange group, for example, forcing them to spread research-
based malware programs (Smyth, 2011). In this model, the dissemination organization gives a
valid stamp of support for new information and helps identify motivational meetings and
networks that can be used to make an interest in the use of evidence for practical speaking.
End user adoption, implementation, and institutionalization
This stage gives the center to achieve associations, groups and people and use the evidence-
based research discoveries and development in general practice to the surrounding people. EBP
Medication safety 7
has complex setting in hospitals such as, official social structure properties (for example,
operational structures and properties, external medicinal services conditions) and personal
physicians in the human service settings to continue and continue EBP in real life.
With respect to apply specialist knowledge and evidence in child and family nursing that
transforms practice, there are some principles that need to be considered by healthcare services
(World Health Organization, 2016).
First of all, reflect on the context and attach health care personnel, who are at the point of care in
opting and focusing patient safety initiatives, clearly supporting the patient safety practice
subject (situations) and conditions or settings to which it applies. It is necessary for the
healthcare organization to design and target each stakeholder user group (Peter, 2010).
Second, when they understand the proof base of training, the managers say, "We should do this
because it is an external administrative requirement. For example, based on logic for evaluation
of threatened risk, it is fundamental to banning occupants of the law, and to enable them to
understand that the fall-chance evaluation is the desire of an external administrative office on this
basis (Gibson, Stelter, Haglund & Lerret, 2017). What is the quality that is evidence supports this
patient wellbeing practice?
Third, instructive training is not enough to change practice only; Instructions on a particular
security action are not sufficient once. Just learning improvement does not really improve
practice. Or maybe the associations should expect to build a strong culture of evidence based on
resources and capabilities, where questions are supported and to make it easier to make the best
framework (Nemeth & Wessell, 2010).
Fourth, the establishment of EBP Enhancement in Patient Safety should be bowled on each
has complex setting in hospitals such as, official social structure properties (for example,
operational structures and properties, external medicinal services conditions) and personal
physicians in the human service settings to continue and continue EBP in real life.
With respect to apply specialist knowledge and evidence in child and family nursing that
transforms practice, there are some principles that need to be considered by healthcare services
(World Health Organization, 2016).
First of all, reflect on the context and attach health care personnel, who are at the point of care in
opting and focusing patient safety initiatives, clearly supporting the patient safety practice
subject (situations) and conditions or settings to which it applies. It is necessary for the
healthcare organization to design and target each stakeholder user group (Peter, 2010).
Second, when they understand the proof base of training, the managers say, "We should do this
because it is an external administrative requirement. For example, based on logic for evaluation
of threatened risk, it is fundamental to banning occupants of the law, and to enable them to
understand that the fall-chance evaluation is the desire of an external administrative office on this
basis (Gibson, Stelter, Haglund & Lerret, 2017). What is the quality that is evidence supports this
patient wellbeing practice?
Third, instructive training is not enough to change practice only; Instructions on a particular
security action are not sufficient once. Just learning improvement does not really improve
practice. Or maybe the associations should expect to build a strong culture of evidence based on
resources and capabilities, where questions are supported and to make it easier to make the best
framework (Nemeth & Wessell, 2010).
Fourth, the establishment of EBP Enhancement in Patient Safety should be bowled on each
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Medication safety 8
progression of the use process; it is fundamental to guide adjustments to make decisions by
fitting between understanding the data and development well and establishing the idea
communication. There is no approach to the real situation, and what works in a single office may
require a change to fit the hierarchical culture of any other unique situation (Australian
Commission, 2010).
In the end, it is compulsory to assess the procedures and results of execution. Customers and
partners need to realize that attempts to improve the wellbeing affect the nature of the idea
positively. For example, if any other bar-coding structure is being used to control blood items,
then realize that the tools are being followed in the process (process marker) and that adjustment
is practically speaking Low blood item is bringing about the transfusion mistakes (result signal).
The review of the medication is the process of evaluation of patient’s medicines for the purpose
of improving the outcomes for the health and reduces the drug-related issues (Mekonnen,
McLachlan & Brien, 2016). In the article of Gardella, Cardwell & Nnadi, (2012), it has been
found that the systematic review of 38 studies of primary care interventions framed to decrease
medication linked adverse events searched that number of successful interventions involve a
medication review conducted by clinicians, which had a medication review through professional.
It has been analyzed that the evidence in the context of medication management education is
lacking. It has been found through review that the patient self-administration keeps significant
value in providing care than usual care following effective education and preparation (Grove,
Burns & Gray, 2012).
Supportive culture is required for developing safety in primary care. This depicts developing
setting where patient feel able to elaborate regarding safety in primary care. It means endorsing
where people want to convey message regarding risks and safety incidents for the purpose of
progression of the use process; it is fundamental to guide adjustments to make decisions by
fitting between understanding the data and development well and establishing the idea
communication. There is no approach to the real situation, and what works in a single office may
require a change to fit the hierarchical culture of any other unique situation (Australian
Commission, 2010).
In the end, it is compulsory to assess the procedures and results of execution. Customers and
partners need to realize that attempts to improve the wellbeing affect the nature of the idea
positively. For example, if any other bar-coding structure is being used to control blood items,
then realize that the tools are being followed in the process (process marker) and that adjustment
is practically speaking Low blood item is bringing about the transfusion mistakes (result signal).
The review of the medication is the process of evaluation of patient’s medicines for the purpose
of improving the outcomes for the health and reduces the drug-related issues (Mekonnen,
McLachlan & Brien, 2016). In the article of Gardella, Cardwell & Nnadi, (2012), it has been
found that the systematic review of 38 studies of primary care interventions framed to decrease
medication linked adverse events searched that number of successful interventions involve a
medication review conducted by clinicians, which had a medication review through professional.
It has been analyzed that the evidence in the context of medication management education is
lacking. It has been found through review that the patient self-administration keeps significant
value in providing care than usual care following effective education and preparation (Grove,
Burns & Gray, 2012).
Supportive culture is required for developing safety in primary care. This depicts developing
setting where patient feel able to elaborate regarding safety in primary care. It means endorsing
where people want to convey message regarding risks and safety incidents for the purpose of
Medication safety 9
learning from them and decrease their recurrence, and where incidents are observed as reasoned
largely by system failures instead of individuals (Maaskant, Vermeulen, Apampa, Fernando,
Ghaleb, Neubert & Soe, 2015). This involves the magnitude of having criticism in the term of
defining improvements that develop safety issues. It has been found that endorsing transparency
is major to developing a well-built safety culture. Various tools are ready elaborating approaches
to support the development (Polit & Beck, 2010). With respect to gap, it can be said that the
research can go beyond the selected topic in which primary research can be conducted by taking
consideration of staff of the hospitals, it would be helpful for the researcher to get relevant and
ongoing challenges faced by the patient as well as employees of the healthcare (Rees, et. al.,
2015).
It can be concluded from above discussion that medications safety is necessary for not only
children but also for all patient. There are number of incidents occurred all over the world that
lead patients into adverse situation. Across the world, there are various systems that are not
designed to care for people with number of health conditions.
learning from them and decrease their recurrence, and where incidents are observed as reasoned
largely by system failures instead of individuals (Maaskant, Vermeulen, Apampa, Fernando,
Ghaleb, Neubert & Soe, 2015). This involves the magnitude of having criticism in the term of
defining improvements that develop safety issues. It has been found that endorsing transparency
is major to developing a well-built safety culture. Various tools are ready elaborating approaches
to support the development (Polit & Beck, 2010). With respect to gap, it can be said that the
research can go beyond the selected topic in which primary research can be conducted by taking
consideration of staff of the hospitals, it would be helpful for the researcher to get relevant and
ongoing challenges faced by the patient as well as employees of the healthcare (Rees, et. al.,
2015).
It can be concluded from above discussion that medications safety is necessary for not only
children but also for all patient. There are number of incidents occurred all over the world that
lead patients into adverse situation. Across the world, there are various systems that are not
designed to care for people with number of health conditions.
Medication safety 10
References
Australian Commission, (2010). Pathways for medication safety. Retrieved from:
https://www.safetyandquality.gov.au/wp-content/uploads/2012/08/1.1-Medication-
Safety.pdf
Gadow, K. D., Brown, N. V., Arnold, L. E., Buchan-Page, K. A., Bukstein, O. G., Butter, E., ...
& Rice Jr, R. R. (2016). Severely aggressive children receiving stimulant medication
versus stimulant and risperidone: 12-month follow-up of the TOSCA trial. Journal of the
American Academy of Child & Adolescent Psychiatry, 55(6), 469-478.
Gardella, J. E., Cardwell, T. B., & Nnadi, M. (2012). Improving medication safety with accurate
preadmission medication lists and postdischarge education. The Joint Commission
Journal on Quality and Patient Safety, 38(10), 452-458.
Gibson, C. A., Stelter, A. J., Haglund, K. A., & Lerret, S. M. (2017). Pediatric Nurses'
Perspectives on Medication Teaching in a Children's Hospital. Journal of pediatric
nursing, 36, 225-231.
Goldspiel, B., Hoffman, J. M., Griffith, N. L., Goodin, S., DeChristoforo, R., Montello, C. M., ...
& Patel, J. T. (2015). ASHP guidelines on preventing medication errors with
chemotherapy and biotherapy. American Journal of Health-System Pharmacy, 72(8), e6-
e35.
Grove, S. K., Burns, N., & Gray, J. (2012). The practice of nursing research: Appraisal,
synthesis, and generation of evidence. Elsevier Health Sciences.
References
Australian Commission, (2010). Pathways for medication safety. Retrieved from:
https://www.safetyandquality.gov.au/wp-content/uploads/2012/08/1.1-Medication-
Safety.pdf
Gadow, K. D., Brown, N. V., Arnold, L. E., Buchan-Page, K. A., Bukstein, O. G., Butter, E., ...
& Rice Jr, R. R. (2016). Severely aggressive children receiving stimulant medication
versus stimulant and risperidone: 12-month follow-up of the TOSCA trial. Journal of the
American Academy of Child & Adolescent Psychiatry, 55(6), 469-478.
Gardella, J. E., Cardwell, T. B., & Nnadi, M. (2012). Improving medication safety with accurate
preadmission medication lists and postdischarge education. The Joint Commission
Journal on Quality and Patient Safety, 38(10), 452-458.
Gibson, C. A., Stelter, A. J., Haglund, K. A., & Lerret, S. M. (2017). Pediatric Nurses'
Perspectives on Medication Teaching in a Children's Hospital. Journal of pediatric
nursing, 36, 225-231.
Goldspiel, B., Hoffman, J. M., Griffith, N. L., Goodin, S., DeChristoforo, R., Montello, C. M., ...
& Patel, J. T. (2015). ASHP guidelines on preventing medication errors with
chemotherapy and biotherapy. American Journal of Health-System Pharmacy, 72(8), e6-
e35.
Grove, S. K., Burns, N., & Gray, J. (2012). The practice of nursing research: Appraisal,
synthesis, and generation of evidence. Elsevier Health Sciences.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Medication safety 11
Hayes, C., Jackson, D., Davidson, P. M., & Power, T. (2015). Medication errors in hospitals: a
literature review of disruptions to nursing practice during medication
administration. Journal of clinical nursing, 24(21-22), 3063-3076.
Hockenberry, M. J., & Wilson, D. (2014). Wong's nursing care of infants and children-E-book.
Elsevier Health Sciences.
James, S. R., Nelson, K., & Ashwill, J. (2012). Nursing care of children: Principles and
practice. Elsevier Health Sciences.
Letourneau, N. L., Dennis, C. L., Benzies, K., Duffett-Leger, L., Stewart, M., Tryphonopoulos,
P. D., ... & Watson, W. (2012). Postpartum depression is a family affair: addressing the
impact on mothers, fathers, and children. Issues in mental health nursing, 33(7), 445-457.
Maaskant, J. M., Vermeulen, H., Apampa, B., Fernando, B., Ghaleb, M. A., Neubert, A., ... &
Soe, A. (2015). Interventions for reducing medication errors in children in
hospital. Cochrane Database of Systematic Reviews, (3).
Mekonnen, A. B., McLachlan, A. J., & Brien, J. A. E. (2016). Pharmacy‐led medication
reconciliation programmes at hospital transitions: a systematic review and meta‐
analysis. Journal of clinical pharmacy and therapeutics, 41(2), 128-144.
Nemeth, L. S., & Wessell, A. M. (2010). Improving medication safety in primary care using
electronic health records. Journal of patient safety, 6(4), 238-243.
Peter, W. L. S. (2010). Improving medication safety in chronic kidney disease patients on
dialysis through medication reconciliation. Advances in chronic kidney disease, 17(5),
413-419.
Hayes, C., Jackson, D., Davidson, P. M., & Power, T. (2015). Medication errors in hospitals: a
literature review of disruptions to nursing practice during medication
administration. Journal of clinical nursing, 24(21-22), 3063-3076.
Hockenberry, M. J., & Wilson, D. (2014). Wong's nursing care of infants and children-E-book.
Elsevier Health Sciences.
James, S. R., Nelson, K., & Ashwill, J. (2012). Nursing care of children: Principles and
practice. Elsevier Health Sciences.
Letourneau, N. L., Dennis, C. L., Benzies, K., Duffett-Leger, L., Stewart, M., Tryphonopoulos,
P. D., ... & Watson, W. (2012). Postpartum depression is a family affair: addressing the
impact on mothers, fathers, and children. Issues in mental health nursing, 33(7), 445-457.
Maaskant, J. M., Vermeulen, H., Apampa, B., Fernando, B., Ghaleb, M. A., Neubert, A., ... &
Soe, A. (2015). Interventions for reducing medication errors in children in
hospital. Cochrane Database of Systematic Reviews, (3).
Mekonnen, A. B., McLachlan, A. J., & Brien, J. A. E. (2016). Pharmacy‐led medication
reconciliation programmes at hospital transitions: a systematic review and meta‐
analysis. Journal of clinical pharmacy and therapeutics, 41(2), 128-144.
Nemeth, L. S., & Wessell, A. M. (2010). Improving medication safety in primary care using
electronic health records. Journal of patient safety, 6(4), 238-243.
Peter, W. L. S. (2010). Improving medication safety in chronic kidney disease patients on
dialysis through medication reconciliation. Advances in chronic kidney disease, 17(5),
413-419.
Medication safety 12
Polit, D. F., & Beck, C. T. (2010). Essentials of nursing research: Appraising evidence for
nursing practice. Lippincott Williams & Wilkins.
Rees, P., Edwards, A., Panesar, S., Powell, C., Carter, B., Williams, H., ... & Avery, A. (2015).
Safety incidents in the primary care office setting. Pediatrics, 135(6), 1027-1035.
Smyth, R. L. (2011). The Evidence-Based Practice Manual for Nurses: with Pageburst online
access. Elsevier Health Sciences.
Titler, M. G., & Moore, J. (2010). Evidence-based practice: a civilian perspective. Nursing
research, 59(1), S2-S6.
World Health Organization. (2016). Consultative meeting planning for the global patient safety
challenge: medication safety, 19-20 April 2016, WHO Headquarters Geneva,
Switzerland: meeting report (No. WHO/HIS/SDS/2016.20). World Health Organization.
World Health Organizations, (2016). Medication Errors. Retrieved from:
https://apps.who.int/iris/bitstream/handle/10665/252274/9789241511643-
eng.pdf;jsessionid=2C989A5F3DB74DE7C2FD9722F7B48965?sequence=1
Polit, D. F., & Beck, C. T. (2010). Essentials of nursing research: Appraising evidence for
nursing practice. Lippincott Williams & Wilkins.
Rees, P., Edwards, A., Panesar, S., Powell, C., Carter, B., Williams, H., ... & Avery, A. (2015).
Safety incidents in the primary care office setting. Pediatrics, 135(6), 1027-1035.
Smyth, R. L. (2011). The Evidence-Based Practice Manual for Nurses: with Pageburst online
access. Elsevier Health Sciences.
Titler, M. G., & Moore, J. (2010). Evidence-based practice: a civilian perspective. Nursing
research, 59(1), S2-S6.
World Health Organization. (2016). Consultative meeting planning for the global patient safety
challenge: medication safety, 19-20 April 2016, WHO Headquarters Geneva,
Switzerland: meeting report (No. WHO/HIS/SDS/2016.20). World Health Organization.
World Health Organizations, (2016). Medication Errors. Retrieved from:
https://apps.who.int/iris/bitstream/handle/10665/252274/9789241511643-
eng.pdf;jsessionid=2C989A5F3DB74DE7C2FD9722F7B48965?sequence=1
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





