HLTENN007 Administer and Monitor Medicines and Intravenous Therapy Written Assessment
VerifiedAdded on 2023/05/31
|26
|10323
|168
AI Summary
This written assessment covers the topic of administering and monitoring medicines and intravenous therapy for HLT54115 Diploma of Nursing course. It discusses the legal and regulatory frameworks that enrolled nurses need to comply with, the rights of medication administration, and the influence of risk management on prevention and control for Standard 3.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
HLT54115 Diploma of Nursing
HLTENN007 - Administer and monitor medicines and intravenous therapy
Written Assessment Student Copy
1
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
HLTENN007 - Administer and monitor medicines and intravenous therapy
Written Assessment Student Copy
1
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Instructions to Students
Welcome to the written assessment. To successfully complete the assessment requirements,
you need to follow the following instructions.
Step 1
Read the study guide and the related resources.
Step 2
Read this assessment to gain an understanding of what you need to do to complete the unit.
Talk to your trainer or supervisor and ask for help if you need to.
Step 3
Complete all questions in this assessment. Please write clearly in pen (not pencil). You may
attach printed answers. Do not remove any pages from this assessment.
Step 4
Complete the cover sheet and attach to this assessment. We recommend you make and keep
a copy of your assessments.
Step 5
Submit for assessment.
2
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
Welcome to the written assessment. To successfully complete the assessment requirements,
you need to follow the following instructions.
Step 1
Read the study guide and the related resources.
Step 2
Read this assessment to gain an understanding of what you need to do to complete the unit.
Talk to your trainer or supervisor and ask for help if you need to.
Step 3
Complete all questions in this assessment. Please write clearly in pen (not pencil). You may
attach printed answers. Do not remove any pages from this assessment.
Step 4
Complete the cover sheet and attach to this assessment. We recommend you make and keep
a copy of your assessments.
Step 5
Submit for assessment.
2
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
Part A
Question 1
The following website may assist with this question
http://www.nursingmidwiferyboard.gov.au/Codes-Guidelines-Statements/FAQ/Enrolled-nurses-
and-medicine-administration.aspx
The Enrolled Nurse practices with and under the direction and supervision of the Registered
Nurse, and assists in the provision of nursing care. At all times the Enrolled Nurse retains
responsibility for his/her own actions and remains accountable to the Registered Nurse for all
delegated functions. Enrolled Nurses will be required to function only within the limits of their
education and competence.
What is meant by supervision?
Answer:
In the field of healthcare, supervision is used in psychotherapy, counselling and other disciplines
of mental health. Even in somatic disciplines supervision is used on practitioners on their
preparatory work for the patients and also their bond with the patients. Instead of being a formal
backdated investigation, supervision is rather a replacement. Supervision contains the meeting
of the practitioner with another professional on a regular basis, one who usually possesses
training in supervision skills and is not necessarily a senior (Butterworth and Faugier, 2013).
Such meetings are done for the discussion of professional issues and caseworks in a structured
manner. It is sometimes known as counselling or clinical supervision. The primary purpose of
supervision is helping the practitioners for learning from his progress and experience in
expertise and also for ensuring better quality services to the patients and the clients
(Butterworth and Faugier, 2013). The learnings of the practitioner would be applied to the
planning, diagnostic as well as therapeutic work. In the British National Health Service, several
disciplines have the usage of clinical supervision. It is now mandatory for having regular and
proper clinical supervision for the federal and registered health professionals like
physiotherapists, occupational therapists, dieticians, drama, music and art therapists. The
supervision skills that are focused on the solution are used in clinical super work as counselling
others. There is a compulsion of having supervision for a minimum of 1.5 hours a month’s time
period for the British Association of Counselling and Psychotherapy’s practicing members.
Supervision is a formal procedure of professional learning and support that helps in allowing
midwifes(supervisee) and nurses for developing the significant competence, knowledge and the
responsibility for their practices and enhancing public safety and protection as well (Butterworth
and Faugier, 2013). Supervision can be direct or indirect in accordance with the context’s nature
under which the supervision of practice takes place. In the practice plan of a supervision’s
context, a supervisor is responsible for providing reports to the territory board, state or the
committee of registration at intended intervals. A written agreement between the supervisee and
the supervisor which is submitted to the significant Nursing and Midwifery Board of Australia’s
(NMBA’s) registration committee, territory board or the state is known as the agreement of
Supervision. Such an agreement helps in identifying the supervisee and the supervisor, the two
party’s agreed responsibilities and the place of practice. A supervision report is a formal
document which is submitted in a format that is approved by NMBA and is given during the
relevant intervals and is agreed in the practiced plan of the supervision (Severinsson and Sand,
2010). The report details and shows the progress of the practice plan of the supervision. An
additional report of supervision might be submitted by a supervisor during any point of time.
Such a report is prepared when there is any mandatory requirement or proposal of changes to
the practice plan of the supervision or in case of the supervisee’s concerns.
3
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
Question 1
The following website may assist with this question
http://www.nursingmidwiferyboard.gov.au/Codes-Guidelines-Statements/FAQ/Enrolled-nurses-
and-medicine-administration.aspx
The Enrolled Nurse practices with and under the direction and supervision of the Registered
Nurse, and assists in the provision of nursing care. At all times the Enrolled Nurse retains
responsibility for his/her own actions and remains accountable to the Registered Nurse for all
delegated functions. Enrolled Nurses will be required to function only within the limits of their
education and competence.
What is meant by supervision?
Answer:
In the field of healthcare, supervision is used in psychotherapy, counselling and other disciplines
of mental health. Even in somatic disciplines supervision is used on practitioners on their
preparatory work for the patients and also their bond with the patients. Instead of being a formal
backdated investigation, supervision is rather a replacement. Supervision contains the meeting
of the practitioner with another professional on a regular basis, one who usually possesses
training in supervision skills and is not necessarily a senior (Butterworth and Faugier, 2013).
Such meetings are done for the discussion of professional issues and caseworks in a structured
manner. It is sometimes known as counselling or clinical supervision. The primary purpose of
supervision is helping the practitioners for learning from his progress and experience in
expertise and also for ensuring better quality services to the patients and the clients
(Butterworth and Faugier, 2013). The learnings of the practitioner would be applied to the
planning, diagnostic as well as therapeutic work. In the British National Health Service, several
disciplines have the usage of clinical supervision. It is now mandatory for having regular and
proper clinical supervision for the federal and registered health professionals like
physiotherapists, occupational therapists, dieticians, drama, music and art therapists. The
supervision skills that are focused on the solution are used in clinical super work as counselling
others. There is a compulsion of having supervision for a minimum of 1.5 hours a month’s time
period for the British Association of Counselling and Psychotherapy’s practicing members.
Supervision is a formal procedure of professional learning and support that helps in allowing
midwifes(supervisee) and nurses for developing the significant competence, knowledge and the
responsibility for their practices and enhancing public safety and protection as well (Butterworth
and Faugier, 2013). Supervision can be direct or indirect in accordance with the context’s nature
under which the supervision of practice takes place. In the practice plan of a supervision’s
context, a supervisor is responsible for providing reports to the territory board, state or the
committee of registration at intended intervals. A written agreement between the supervisee and
the supervisor which is submitted to the significant Nursing and Midwifery Board of Australia’s
(NMBA’s) registration committee, territory board or the state is known as the agreement of
Supervision. Such an agreement helps in identifying the supervisee and the supervisor, the two
party’s agreed responsibilities and the place of practice. A supervision report is a formal
document which is submitted in a format that is approved by NMBA and is given during the
relevant intervals and is agreed in the practiced plan of the supervision (Severinsson and Sand,
2010). The report details and shows the progress of the practice plan of the supervision. An
additional report of supervision might be submitted by a supervisor during any point of time.
Such a report is prepared when there is any mandatory requirement or proposal of changes to
the practice plan of the supervision or in case of the supervisee’s concerns.
3
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
A Supervisor is a properly experienced and qualified registered or enrolled nurse or/and midwife
who is responsible for supervising an individual who undertakes a supervision practice period
that is approves by the NMBA (Severinsson and Sand, 2010). The supervisor is responsible for
assessing, monitoring, providing significant feedback and reporting to the necessary territory
board, state or committee of registration of the NMBA regarding the nurse’s or midwife’s
performance under the supervision. An ideal supervisor should have more than two years of
experience as a midwife or nurse and should have completed a course of a supervisor or
preceptorship. A nurse or midwife who holds registration with undertakings or conditions or a
provisional registration, or enters into a supervision requiring undertaking is known as a
Supervisee (Severinsson and Sand, 2010). They practice under the guidance, direction and
oversight of a supervisor for meeting their objectives and goals of a supervised plan of practice.
Question 2
The following websites may assist with this question
http://www.health.nsw.gov.au/pharmaceutical/pages/legislation.aspx
http://www.safetyandquality.gov.au/wp-content/uploads/2011/09/NSQHS-Standards-Sept-
2012.pdf
The Registered Nurse retains overall accountability and responsibility for the nursing care
provided to his/her allocated consumers whether performed directly, in collaboration with, or
delegated to an Enrolled Nurse.
The Enrolled Nurse working in conjunction with and under the supervision of the Registered
Nurse will assist in the planning, the implementation and delivery of nursing care to consumers.
The Enrolled Nurse will implement medical/treatment orders under the direction and as
delegated by the Registered Nurse with reference to the Enrolled Nurses scope of education
and practice The Enrolled Nurse will practice in accordance with organisational policy within
their level of training and legal obligations. Discuss the legal and regulatory frameworks that
Enrolled nurses need to comply with.
Answer:
An enrolled nurse has several responsibilities and liabilities, and need to comply with certain
legal and regulatory frameworks. An enrolled nurse needs to demonstrate the in-depth
understanding and knowledge the state and territory legislation, commonwealth and the
common law that is relevant to the nursing practice (Eagar, Cowin, Gregory and Firtko, 2010).
During the undertaking of the enrolled nurse’s practice, they need to fulfill all the duties of care.
It is their duty to manifest and exhibit the thorough knowledge and implications of all the
standards, work policies, procedures and codes and guidelines of the Nursing and Midwifery
Board of Australia (NMBA) which are applicable on the nursing practice. In accordance with the
agreed care plan, policies of the workplace, guidelines of the procedures and the professional
standards, the enrolled nurse should provide nursing care. It is a must for them to identify and
clarify their own responsibilities for the particulars of entrusted care in order to work in
collaboration with the registered nurse and the healthcare team. The enrolled nurse should
recognize and identify their own limitations and liabilities in the competence and practice and
should seek supervision from the registered nurse and assist them as and when needed (Eagar,
Cowin, Gregory and Firtko, 2010). They are required to withhold from undertaking any acts
where there is no significant education, experience, training and demonstration regarding
competence or has not been undertaken. During any sorts of occurrence of incidents related to
unsafe practice, the enrolled nurse should immediately report to the registered nurse and other
individuals in authority or people in-charge, and should explores ways of preventing such
4
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
who is responsible for supervising an individual who undertakes a supervision practice period
that is approves by the NMBA (Severinsson and Sand, 2010). The supervisor is responsible for
assessing, monitoring, providing significant feedback and reporting to the necessary territory
board, state or committee of registration of the NMBA regarding the nurse’s or midwife’s
performance under the supervision. An ideal supervisor should have more than two years of
experience as a midwife or nurse and should have completed a course of a supervisor or
preceptorship. A nurse or midwife who holds registration with undertakings or conditions or a
provisional registration, or enters into a supervision requiring undertaking is known as a
Supervisee (Severinsson and Sand, 2010). They practice under the guidance, direction and
oversight of a supervisor for meeting their objectives and goals of a supervised plan of practice.
Question 2
The following websites may assist with this question
http://www.health.nsw.gov.au/pharmaceutical/pages/legislation.aspx
http://www.safetyandquality.gov.au/wp-content/uploads/2011/09/NSQHS-Standards-Sept-
2012.pdf
The Registered Nurse retains overall accountability and responsibility for the nursing care
provided to his/her allocated consumers whether performed directly, in collaboration with, or
delegated to an Enrolled Nurse.
The Enrolled Nurse working in conjunction with and under the supervision of the Registered
Nurse will assist in the planning, the implementation and delivery of nursing care to consumers.
The Enrolled Nurse will implement medical/treatment orders under the direction and as
delegated by the Registered Nurse with reference to the Enrolled Nurses scope of education
and practice The Enrolled Nurse will practice in accordance with organisational policy within
their level of training and legal obligations. Discuss the legal and regulatory frameworks that
Enrolled nurses need to comply with.
Answer:
An enrolled nurse has several responsibilities and liabilities, and need to comply with certain
legal and regulatory frameworks. An enrolled nurse needs to demonstrate the in-depth
understanding and knowledge the state and territory legislation, commonwealth and the
common law that is relevant to the nursing practice (Eagar, Cowin, Gregory and Firtko, 2010).
During the undertaking of the enrolled nurse’s practice, they need to fulfill all the duties of care.
It is their duty to manifest and exhibit the thorough knowledge and implications of all the
standards, work policies, procedures and codes and guidelines of the Nursing and Midwifery
Board of Australia (NMBA) which are applicable on the nursing practice. In accordance with the
agreed care plan, policies of the workplace, guidelines of the procedures and the professional
standards, the enrolled nurse should provide nursing care. It is a must for them to identify and
clarify their own responsibilities for the particulars of entrusted care in order to work in
collaboration with the registered nurse and the healthcare team. The enrolled nurse should
recognize and identify their own limitations and liabilities in the competence and practice and
should seek supervision from the registered nurse and assist them as and when needed (Eagar,
Cowin, Gregory and Firtko, 2010). They are required to withhold from undertaking any acts
where there is no significant education, experience, training and demonstration regarding
competence or has not been undertaken. During any sorts of occurrence of incidents related to
unsafe practice, the enrolled nurse should immediately report to the registered nurse and other
individuals in authority or people in-charge, and should explores ways of preventing such
4
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
incidents from taking place again in the future. The registered nurse should also negotiate and
cooperate with the all the appropriate personnel as well as the registered nurse for ensuring the
rights and needs of people and patients in care receipt are upheld and addressed.
The nurses should have significant knowledge about certain legal acts and frameworks. these
include the Poison and Therapeutic Goods Regulation Act 2008, the NSW Poisons List,
Standard for the Uniform Scheduling of Medicines and Poisons (SUSMP), the Trafficking and
Drug Misuse Act and Regulations, Dangerous Goods legislation, NSW and Commonwealth
Food regulations, National Industrial Chemicals Notification and Assessment Scheme
(NICNAS), Commonwealth Therapeutic Goods Act, Competition and Consumer legislation,
SafeWork Australia national code for labelling workplace substances, import and exports
regulations that are customs prohibited, Therapeutic Goods Administration (TGA), Australian
Pesticides and Veterinary Medicines Authority (APVMA) etc.
Question 3
The following website may assist with this question
http://www.safetyandquality.gov.au/wp-content/uploads/2012/10/
Standard3_Oct_2012_WEB.pdf
The Australian Commission on Safety and Quality in Health Care developed the National Safety
and Quality Health Service (NSQHS) Standards to improve the quality of health service
provision in Australia. The NSQHS Standards provide a nationally consistent statement of the
level of care consumers should be able to expect from health service organisations. How does
risk management influence prevention and control for Standard 3?
Answer:
For the Standard 3, risk management is related to the risk of transmission or acquisition of an
infectious agent or an infection for patients, visitors and the workforce within a healthcare
organization. The implementation and the usage of an approach of risk management helps in
allowing the healthcare provider to determine the specific areas where there is low or high risk
and focus on how it should be responded to accordingly. The senior managers of a healthcare
organization and clinical leaders implement certain systems for preventing and managing the
healthcare related infections and convey the same to the staff or the workforce for the
achievement of significant results. The clinicians and other representatives of the organization’s
workplace use and implement the systems for control and prevention of the healthcare related
infections. These infections are very common difficulties that affect the patients of a hospital. In
Australia, every year, patients contract with nearly 200,000 healthcare infections (NHMRC,
2010). Almost half of these healthcare infections can be prevented. In order to control infections
successfully and for minimizing the transmission risks, a certain range of strategies is required
across all the levels of the system of healthcare. It also requires a collective approach for the
implementation to be successful. Such a standard’s objective is the prevention of the patients
from acquiring the healthcare related infections that are preventable and management of the
infections effectively as and when they occur by using strategies which are based on evidences.
There are certain requirements of the Standard 3. Effective management and governance
systems should be implemented and maintained for the healthcare related infections.
Appropriate strategies should be developed, used and maintained for controlling and preventing
these healthcare related infections. Patients that are brought into the hospital carrying an
infection or colonialization, or acquire the same during the period of care should be taken proper
care of, their complications should be determined promptly and should receive the appropriate
treatment and management. A strategic aim of the system of clinical governance is the
significant and safe prescription of antimicrobials. The environment of the healthcare and the
5
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
cooperate with the all the appropriate personnel as well as the registered nurse for ensuring the
rights and needs of people and patients in care receipt are upheld and addressed.
The nurses should have significant knowledge about certain legal acts and frameworks. these
include the Poison and Therapeutic Goods Regulation Act 2008, the NSW Poisons List,
Standard for the Uniform Scheduling of Medicines and Poisons (SUSMP), the Trafficking and
Drug Misuse Act and Regulations, Dangerous Goods legislation, NSW and Commonwealth
Food regulations, National Industrial Chemicals Notification and Assessment Scheme
(NICNAS), Commonwealth Therapeutic Goods Act, Competition and Consumer legislation,
SafeWork Australia national code for labelling workplace substances, import and exports
regulations that are customs prohibited, Therapeutic Goods Administration (TGA), Australian
Pesticides and Veterinary Medicines Authority (APVMA) etc.
Question 3
The following website may assist with this question
http://www.safetyandquality.gov.au/wp-content/uploads/2012/10/
Standard3_Oct_2012_WEB.pdf
The Australian Commission on Safety and Quality in Health Care developed the National Safety
and Quality Health Service (NSQHS) Standards to improve the quality of health service
provision in Australia. The NSQHS Standards provide a nationally consistent statement of the
level of care consumers should be able to expect from health service organisations. How does
risk management influence prevention and control for Standard 3?
Answer:
For the Standard 3, risk management is related to the risk of transmission or acquisition of an
infectious agent or an infection for patients, visitors and the workforce within a healthcare
organization. The implementation and the usage of an approach of risk management helps in
allowing the healthcare provider to determine the specific areas where there is low or high risk
and focus on how it should be responded to accordingly. The senior managers of a healthcare
organization and clinical leaders implement certain systems for preventing and managing the
healthcare related infections and convey the same to the staff or the workforce for the
achievement of significant results. The clinicians and other representatives of the organization’s
workplace use and implement the systems for control and prevention of the healthcare related
infections. These infections are very common difficulties that affect the patients of a hospital. In
Australia, every year, patients contract with nearly 200,000 healthcare infections (NHMRC,
2010). Almost half of these healthcare infections can be prevented. In order to control infections
successfully and for minimizing the transmission risks, a certain range of strategies is required
across all the levels of the system of healthcare. It also requires a collective approach for the
implementation to be successful. Such a standard’s objective is the prevention of the patients
from acquiring the healthcare related infections that are preventable and management of the
infections effectively as and when they occur by using strategies which are based on evidences.
There are certain requirements of the Standard 3. Effective management and governance
systems should be implemented and maintained for the healthcare related infections.
Appropriate strategies should be developed, used and maintained for controlling and preventing
these healthcare related infections. Patients that are brought into the hospital carrying an
infection or colonialization, or acquire the same during the period of care should be taken proper
care of, their complications should be determined promptly and should receive the appropriate
treatment and management. A strategic aim of the system of clinical governance is the
significant and safe prescription of antimicrobials. The environment of the healthcare and the
5
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
related facilities should be hygienic and clean. The reprocessing of the instrumentation and
equipment helps in meeting the guidelines of practice that are the best. The patients,
caretakers, service providers and the consumers are provided with relevant information and
knowledge on healthcare related infections.
Question 4
The following website may assist with this question
http://www.newhealthadvisor.com/10-Rights-of-Medication-Administration.html
Discuss the rights of medication administration.
Answer:
Whether it is a nurse providing medications or a patient receiving the same, it is very crucial to
understand the medication administration rights. While consuming medication by oneself, or
while giving it to a family member, safety should be considered at the very first place. There are
always chances and risk of wrong medications or improper dose or the medications of the wrong
person being provided. Such incidents can result in bringing dangerous, harmful and even life-
taking consequences. It is very critical for everyone to have prior knowledge and understanding
of rules of safety for medications even though protocol for the medications have always been
there. The various medication administration rights are as follows.
Right Patient
It should be ensured that the right medications are being given to the right patient (Elliott and
Liu, 2010). If a person is at home and is providing medication to their family member, the bottle
of medication should be checked and it should be ensured that it is being given to the right
person in accordance with the appropriate prescription.
Right Medication
When certain medication is prescribed by a doctor, the medication container would include a
prescription label. Often, mistakes and blunders are made by pharmacies and clinicians as well.
The medication should be checked against the prescription label and a person should be aware of
the names of medications that sound alike.
Right Dosage
One of the most vital administration rights is the right dosage. One should always be careful
about the appropriate proportion of dosage of the medicine to be given to a patient (Elliott and
Liu, 2010). Until and unless surety is obtained regarding the dosage amount, the medications
should not be given to a patient. Different dosages such as pediatric, adult, pregnant, elderly, etc.
should be kept in mind.
Right Route
The right route of medication is important to be considered as well. If a patient is unable to
swallow a pill form medicine, he should be given liquid form of the same. Appropriateness of
medications should be focused on such as whether they can be given by suppositories, cream or
lotions form, syrup form or in form of pills (Macdonald, 2010).
Right Time
The appropriate timing of taking a medication should be given prior consideration to. Whether
the medicines should be given to the patient during the daytime, in the morning or before bed,
before or after meals, all are crucial to be considered (Macdonald, 2010).
The other five rights of medication administration are the Right Documentation, Right Client
Education, Right to Refuse, Right Assessment and the Right Evaluation (Elliott and Liu, 2010).
6
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
equipment helps in meeting the guidelines of practice that are the best. The patients,
caretakers, service providers and the consumers are provided with relevant information and
knowledge on healthcare related infections.
Question 4
The following website may assist with this question
http://www.newhealthadvisor.com/10-Rights-of-Medication-Administration.html
Discuss the rights of medication administration.
Answer:
Whether it is a nurse providing medications or a patient receiving the same, it is very crucial to
understand the medication administration rights. While consuming medication by oneself, or
while giving it to a family member, safety should be considered at the very first place. There are
always chances and risk of wrong medications or improper dose or the medications of the wrong
person being provided. Such incidents can result in bringing dangerous, harmful and even life-
taking consequences. It is very critical for everyone to have prior knowledge and understanding
of rules of safety for medications even though protocol for the medications have always been
there. The various medication administration rights are as follows.
Right Patient
It should be ensured that the right medications are being given to the right patient (Elliott and
Liu, 2010). If a person is at home and is providing medication to their family member, the bottle
of medication should be checked and it should be ensured that it is being given to the right
person in accordance with the appropriate prescription.
Right Medication
When certain medication is prescribed by a doctor, the medication container would include a
prescription label. Often, mistakes and blunders are made by pharmacies and clinicians as well.
The medication should be checked against the prescription label and a person should be aware of
the names of medications that sound alike.
Right Dosage
One of the most vital administration rights is the right dosage. One should always be careful
about the appropriate proportion of dosage of the medicine to be given to a patient (Elliott and
Liu, 2010). Until and unless surety is obtained regarding the dosage amount, the medications
should not be given to a patient. Different dosages such as pediatric, adult, pregnant, elderly, etc.
should be kept in mind.
Right Route
The right route of medication is important to be considered as well. If a patient is unable to
swallow a pill form medicine, he should be given liquid form of the same. Appropriateness of
medications should be focused on such as whether they can be given by suppositories, cream or
lotions form, syrup form or in form of pills (Macdonald, 2010).
Right Time
The appropriate timing of taking a medication should be given prior consideration to. Whether
the medicines should be given to the patient during the daytime, in the morning or before bed,
before or after meals, all are crucial to be considered (Macdonald, 2010).
The other five rights of medication administration are the Right Documentation, Right Client
Education, Right to Refuse, Right Assessment and the Right Evaluation (Elliott and Liu, 2010).
6
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd

Question 5
The following website may assist with this question
http://www.safetyandquality.gov.au/our-work/medication-safety/medication-chart/
Medication charts are legal documents and must be completed accurately and unambiguously
in order to ensure that clients receive safe and optimal drug therapy. What constitutes a legal
medication order?
Answer:
An order for any kind of medication, compound or nutritional agent of a policy which is defined
by the institutional policy during an order requirement from a prescriber. A legal medication
order is constituted by the policy purposes, scope of policy and the various policy statements.
The policy purpose is related with providing a base for safe communication of nutritional and
medication orders. Hence, they reduce the possibility of preventable adverse events or errors
and also establish the continuity of prescriptions. Its foundation is related to a set of common
guidelines of practice that are developed for the health authorities and are applied on the
ambulatory, residential and impatient services. There are various policy statements which
compose the legal medication order. These are namely, Medication order writing, Medication
order legibility, Medication order forms, Core Medication order components, Verbal (Medication)
orders, Telephone (Medication) orders, Medication order dosage format, Medication order
dosage formula, Medication order disallowed, Suggested Medication orders, Standing
Medication orders, Safety validation of Medication orders: Practitioner responsibilities,
Prescriber or practitioner compliance reviews.
Question 6
The following website may assist with this question
http://medical-dictionary.thefreedictionary.com/
The nurse is responsible for ensuring that they have the knowledge to ensure the correct
administration of drugs. This includes pharmacology, anatomy and physiology, and legal issues.
Another responsibility of the nurse is to monitor the effect of the drugs that are administered to a
client, i.e.
- whether the drug had the required effect
- little or no effect or
- if any adverse reactions occurred.
7
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
The following website may assist with this question
http://www.safetyandquality.gov.au/our-work/medication-safety/medication-chart/
Medication charts are legal documents and must be completed accurately and unambiguously
in order to ensure that clients receive safe and optimal drug therapy. What constitutes a legal
medication order?
Answer:
An order for any kind of medication, compound or nutritional agent of a policy which is defined
by the institutional policy during an order requirement from a prescriber. A legal medication
order is constituted by the policy purposes, scope of policy and the various policy statements.
The policy purpose is related with providing a base for safe communication of nutritional and
medication orders. Hence, they reduce the possibility of preventable adverse events or errors
and also establish the continuity of prescriptions. Its foundation is related to a set of common
guidelines of practice that are developed for the health authorities and are applied on the
ambulatory, residential and impatient services. There are various policy statements which
compose the legal medication order. These are namely, Medication order writing, Medication
order legibility, Medication order forms, Core Medication order components, Verbal (Medication)
orders, Telephone (Medication) orders, Medication order dosage format, Medication order
dosage formula, Medication order disallowed, Suggested Medication orders, Standing
Medication orders, Safety validation of Medication orders: Practitioner responsibilities,
Prescriber or practitioner compliance reviews.
Question 6
The following website may assist with this question
http://medical-dictionary.thefreedictionary.com/
The nurse is responsible for ensuring that they have the knowledge to ensure the correct
administration of drugs. This includes pharmacology, anatomy and physiology, and legal issues.
Another responsibility of the nurse is to monitor the effect of the drugs that are administered to a
client, i.e.
- whether the drug had the required effect
- little or no effect or
- if any adverse reactions occurred.
7
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
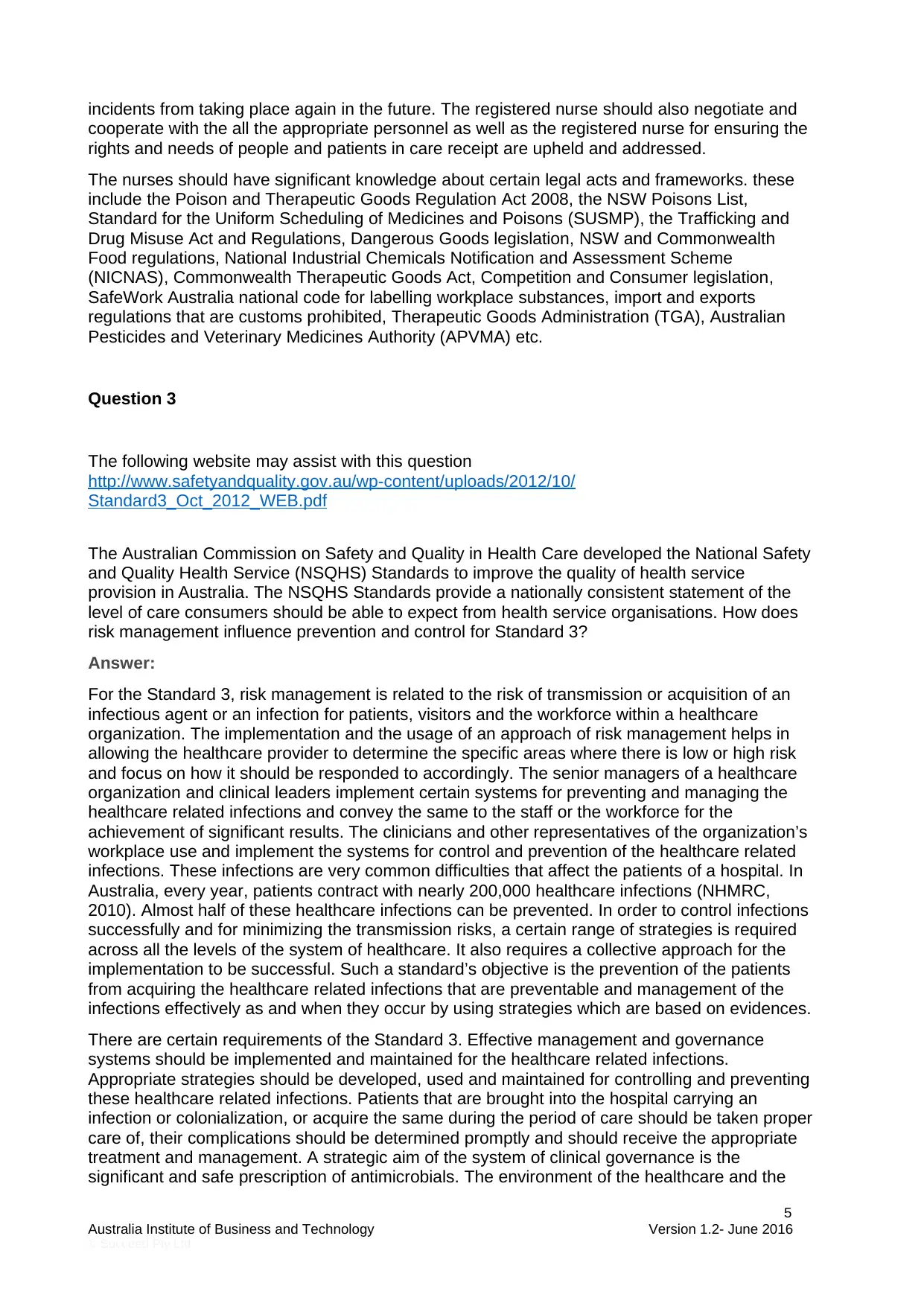
Complete the following table.
Define pharmacology The science which deals with the nature,
origin, effects, chemistry and the usage of
drugs and medications is known as
Pharmacology (Lesko, Zineh and Huang,
2010). It also includes
the science that deals with the origin, nature, c
hemistry, effects, and uses of drugs; it includes
pharmacokinetics, pharmacognosy, toxicology,
pharmacotherapeutics and
pharmacodynamics.
Define pharmacodynamics. It is the study of the physiological and
biochemical effects of medicines and their
action mechanisms, including their actions’
correlation effects with the chemical
composition of the drugs (van der Graaf and
Benson, 2011).
Define pharmacokinetics. It is the study which is related to the
movements of medicines and drugs inside the
human body, including the different processes
of
the study of the movement of drugs in the body
, including the processes of distribution,
absorption, biotransformation, tissue
localization and excretion (Bergen, et. al.,
2012).
8
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
Define pharmacology The science which deals with the nature,
origin, effects, chemistry and the usage of
drugs and medications is known as
Pharmacology (Lesko, Zineh and Huang,
2010). It also includes
the science that deals with the origin, nature, c
hemistry, effects, and uses of drugs; it includes
pharmacokinetics, pharmacognosy, toxicology,
pharmacotherapeutics and
pharmacodynamics.
Define pharmacodynamics. It is the study of the physiological and
biochemical effects of medicines and their
action mechanisms, including their actions’
correlation effects with the chemical
composition of the drugs (van der Graaf and
Benson, 2011).
Define pharmacokinetics. It is the study which is related to the
movements of medicines and drugs inside the
human body, including the different processes
of
the study of the movement of drugs in the body
, including the processes of distribution,
absorption, biotransformation, tissue
localization and excretion (Bergen, et. al.,
2012).
8
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
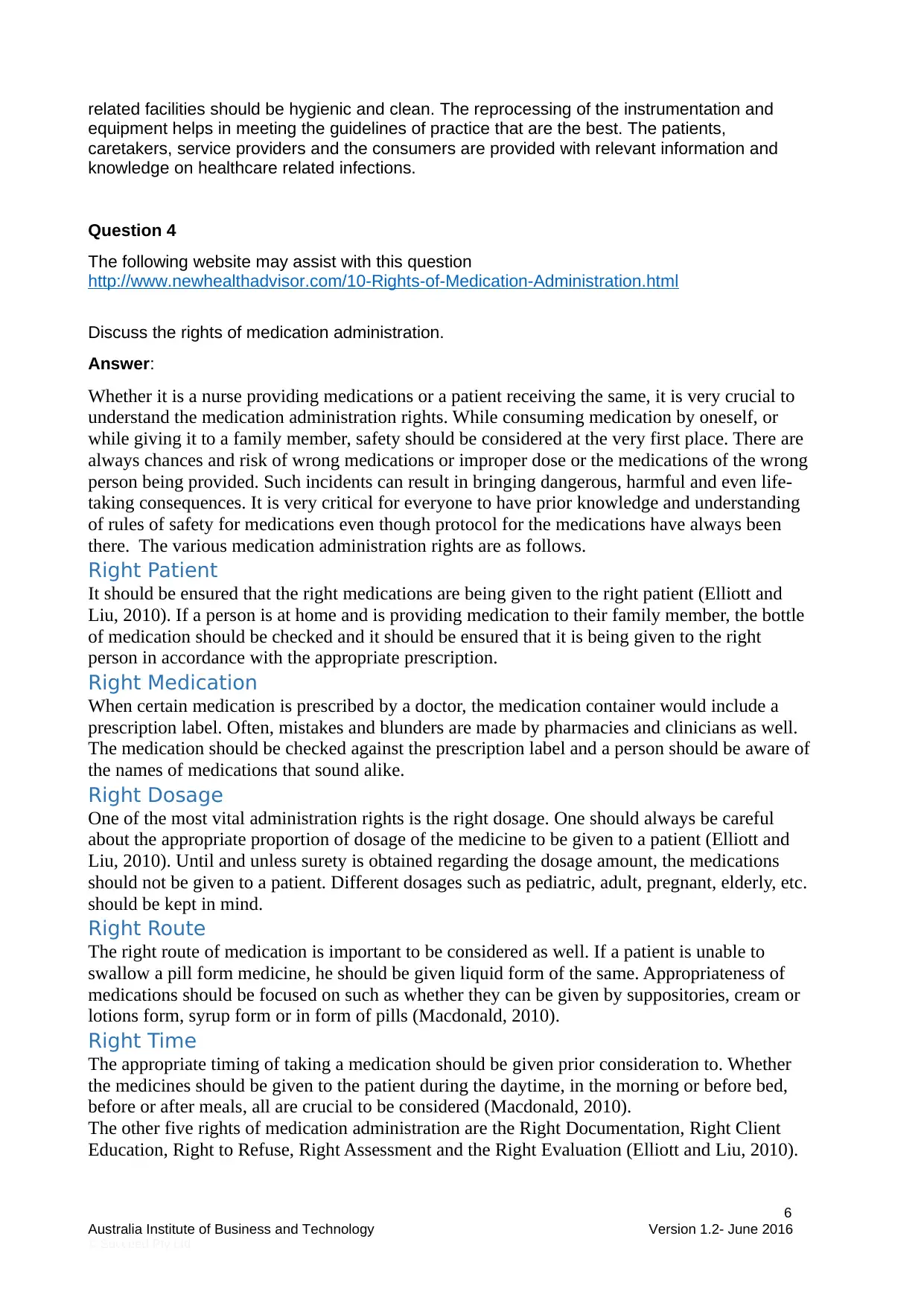
Define pharmacotherapeutics. It is the study of medical science that deals
with the therapeutic effects and usage of
medicines and drugs. It identifies the adverse
and beneficial effects of medicines.
Define toxicology. Toxicology is basically the study or science of
poisons (Elsaesser and Howard, 2012).
Developmental toxicology is another popular
and close related terms which is related to the
study of the toxin effects that are caused on
the development of embryos.
Define adverse reactions The serious and unexpected symptoms with
coincide with a drug’s or medicine’s
administration are known as adverse reactions.
In other words, they are the unfavorable
reactions which are caused due to the usage
of local anesthetic. The factors that are
responsible include the concentration of drug,
its usage and usage route.
What are contraindications? The indication of inadvisability of a medical
treatment is known as contraindication (Ryoo,
et. al., 2013).
9
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
with the therapeutic effects and usage of
medicines and drugs. It identifies the adverse
and beneficial effects of medicines.
Define toxicology. Toxicology is basically the study or science of
poisons (Elsaesser and Howard, 2012).
Developmental toxicology is another popular
and close related terms which is related to the
study of the toxin effects that are caused on
the development of embryos.
Define adverse reactions The serious and unexpected symptoms with
coincide with a drug’s or medicine’s
administration are known as adverse reactions.
In other words, they are the unfavorable
reactions which are caused due to the usage
of local anesthetic. The factors that are
responsible include the concentration of drug,
its usage and usage route.
What are contraindications? The indication of inadvisability of a medical
treatment is known as contraindication (Ryoo,
et. al., 2013).
9
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
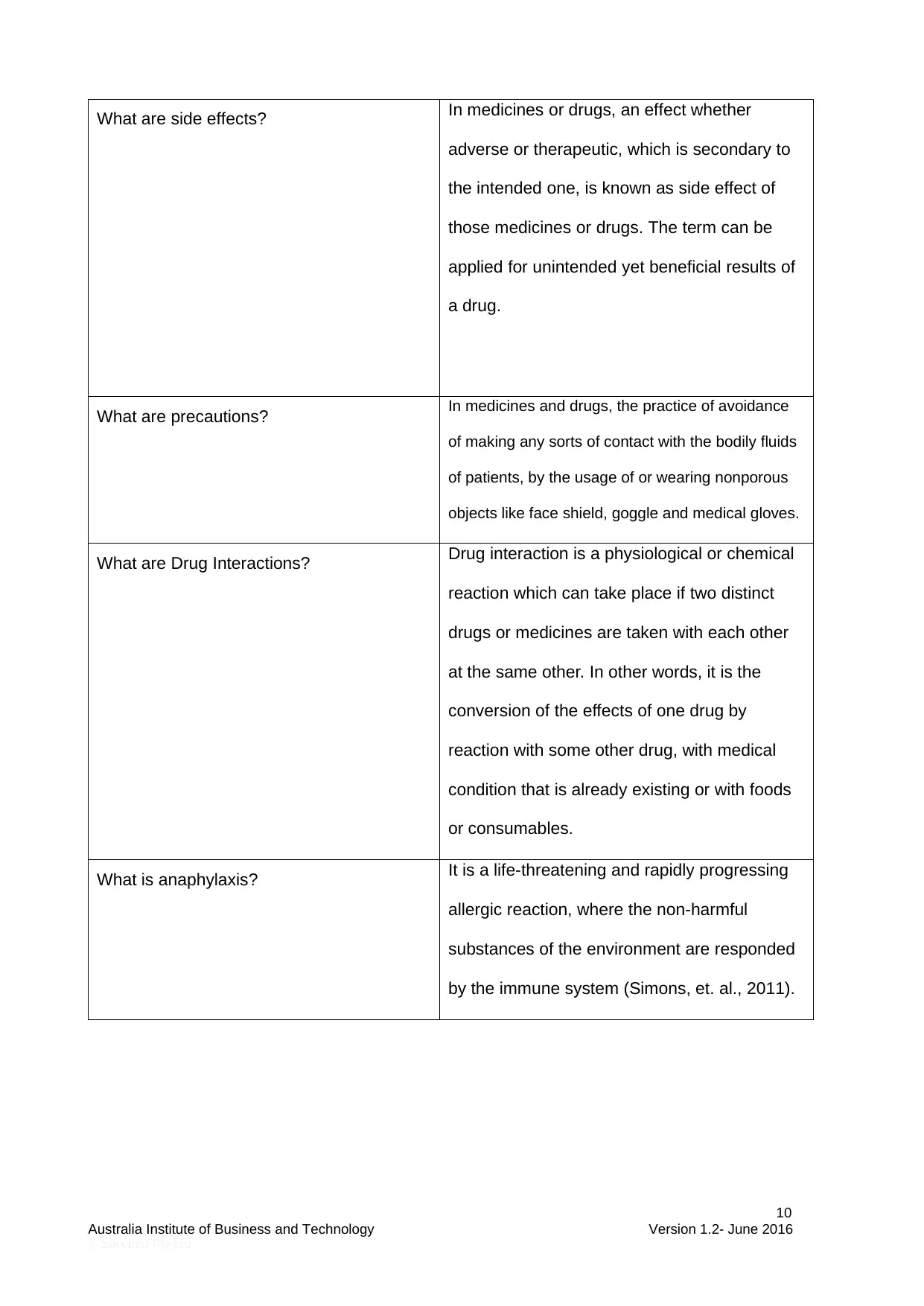
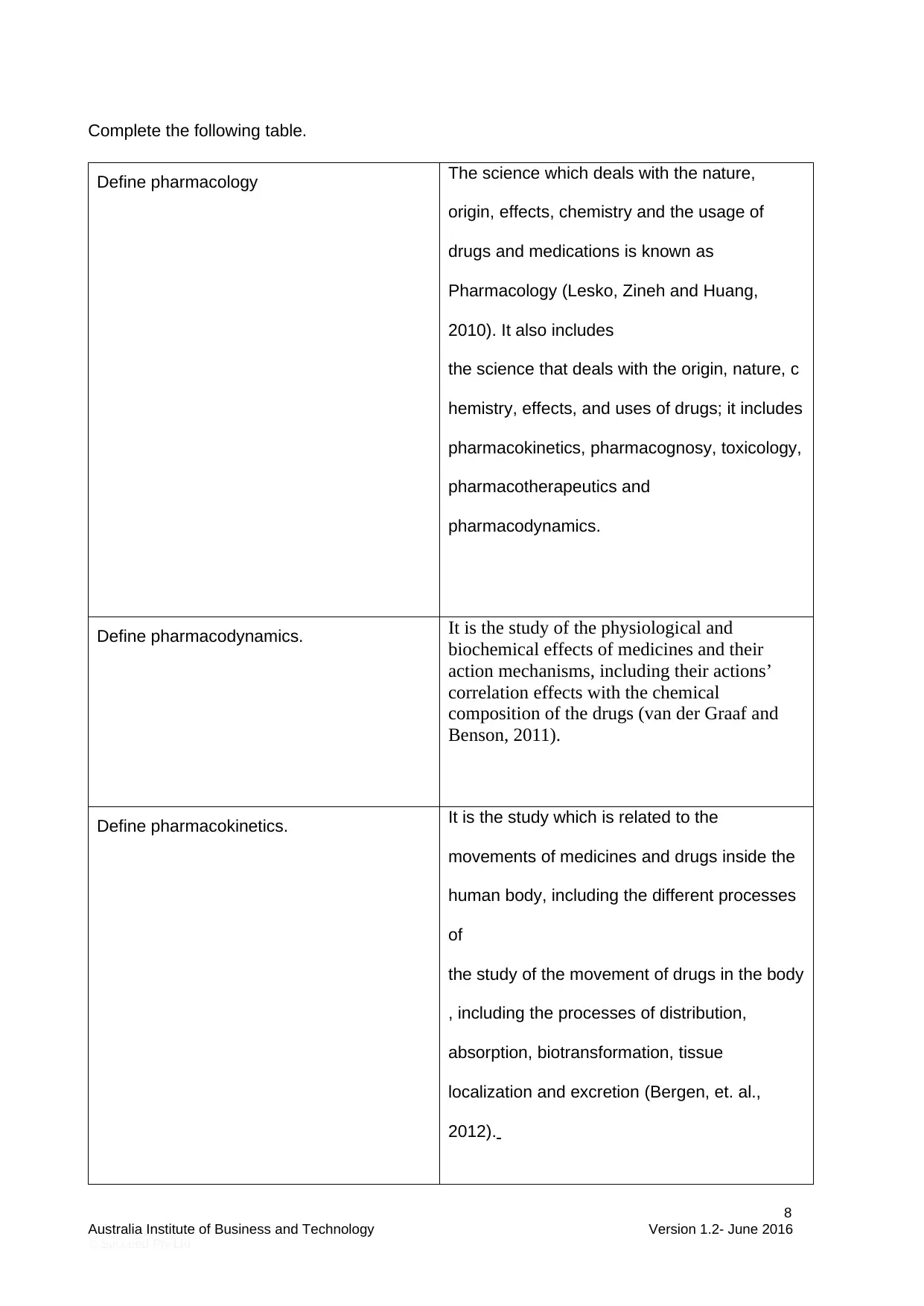
What are side effects? In medicines or drugs, an effect whether
adverse or therapeutic, which is secondary to
the intended one, is known as side effect of
those medicines or drugs. The term can be
applied for unintended yet beneficial results of
a drug.
What are precautions? In medicines and drugs, the practice of avoidance
of making any sorts of contact with the bodily fluids
of patients, by the usage of or wearing nonporous
objects like face shield, goggle and medical gloves.
What are Drug Interactions? Drug interaction is a physiological or chemical
reaction which can take place if two distinct
drugs or medicines are taken with each other
at the same other. In other words, it is the
conversion of the effects of one drug by
reaction with some other drug, with medical
condition that is already existing or with foods
or consumables.
What is anaphylaxis? It is a life-threatening and rapidly progressing
allergic reaction, where the non-harmful
substances of the environment are responded
by the immune system (Simons, et. al., 2011).
10
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
adverse or therapeutic, which is secondary to
the intended one, is known as side effect of
those medicines or drugs. The term can be
applied for unintended yet beneficial results of
a drug.
What are precautions? In medicines and drugs, the practice of avoidance
of making any sorts of contact with the bodily fluids
of patients, by the usage of or wearing nonporous
objects like face shield, goggle and medical gloves.
What are Drug Interactions? Drug interaction is a physiological or chemical
reaction which can take place if two distinct
drugs or medicines are taken with each other
at the same other. In other words, it is the
conversion of the effects of one drug by
reaction with some other drug, with medical
condition that is already existing or with foods
or consumables.
What is anaphylaxis? It is a life-threatening and rapidly progressing
allergic reaction, where the non-harmful
substances of the environment are responded
by the immune system (Simons, et. al., 2011).
10
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Question 7
The following websites my assist with this question
http://nursing.flinders.edu.au/students/studyaids/drugcalculations/page.php?id=1
http://www.safetyandquality.gov.au/wp-content/uploads/2014/02/Literature-Review-Medication-
Safety-in-Australia-2013.pdf
https://www.nursingcenter.com/ncblog/may-2011/8-rights-of-medication-administration
Part A
Administration of medications is a major component of the enrolled nurse’s role within clinical
settings. Medication administration is a high risk activity which requires a consistently accurate
approach by the enrolled nurse in any workplace. List the factors you need to consider when
calculating medication dosages.
Answer:
The factors that should be considered for calculating the medication dosages are age, weight,
sex, race, genetic make-up, occupation, habitual use, administration time and frequency.
Part B
Paediatric medication calculations have high risks due to
- Immature organ function to metabolise drugs
- Mg/kg doses require calculations
- Small doses required: a small change may make a big difference clinically
- Dosage forms are usually in adult sizes
- Liquid formulations need to be measured and/or diluted
Emily is a 4 year old girl who has Cystic Fibrosis. Emily has been admitted into hospital for the
treatment of a chest infection. Emily has been ordered IV antibiotics. What factors do you need
to consider when calculating her medication?
Answer:
The factors that are needed to be considered while calculating Emily’s medication are her
Weight, Formula of calculation, Dosage calculation, Flow rate drops per minute, Flow rate
milliliters per hour.
Part C
Prescribing for older patients presents unique challenges. Many medications need to be used
with special caution because of age-related changes in pharmacokinetics (ie, absorption,
distribution, metabolism, and excretion) and pharmacodynamics (the physiologic effects of the
drug).
Particular care must be taken in determining drug dosages when prescribing for older adults. An
increased volume of distribution may result from the proportional increase in body fat relative to
skeletal muscle with aging. Decreased drug clearance may result from the natural decline in
renal function with age, even in the absence of renal disease. Larger drug storage reservoirs
and decreased clearance prolong drug half-lives and lead to increased plasma drug
concentrations in older people.
11
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
The following websites my assist with this question
http://nursing.flinders.edu.au/students/studyaids/drugcalculations/page.php?id=1
http://www.safetyandquality.gov.au/wp-content/uploads/2014/02/Literature-Review-Medication-
Safety-in-Australia-2013.pdf
https://www.nursingcenter.com/ncblog/may-2011/8-rights-of-medication-administration
Part A
Administration of medications is a major component of the enrolled nurse’s role within clinical
settings. Medication administration is a high risk activity which requires a consistently accurate
approach by the enrolled nurse in any workplace. List the factors you need to consider when
calculating medication dosages.
Answer:
The factors that should be considered for calculating the medication dosages are age, weight,
sex, race, genetic make-up, occupation, habitual use, administration time and frequency.
Part B
Paediatric medication calculations have high risks due to
- Immature organ function to metabolise drugs
- Mg/kg doses require calculations
- Small doses required: a small change may make a big difference clinically
- Dosage forms are usually in adult sizes
- Liquid formulations need to be measured and/or diluted
Emily is a 4 year old girl who has Cystic Fibrosis. Emily has been admitted into hospital for the
treatment of a chest infection. Emily has been ordered IV antibiotics. What factors do you need
to consider when calculating her medication?
Answer:
The factors that are needed to be considered while calculating Emily’s medication are her
Weight, Formula of calculation, Dosage calculation, Flow rate drops per minute, Flow rate
milliliters per hour.
Part C
Prescribing for older patients presents unique challenges. Many medications need to be used
with special caution because of age-related changes in pharmacokinetics (ie, absorption,
distribution, metabolism, and excretion) and pharmacodynamics (the physiologic effects of the
drug).
Particular care must be taken in determining drug dosages when prescribing for older adults. An
increased volume of distribution may result from the proportional increase in body fat relative to
skeletal muscle with aging. Decreased drug clearance may result from the natural decline in
renal function with age, even in the absence of renal disease. Larger drug storage reservoirs
and decreased clearance prolong drug half-lives and lead to increased plasma drug
concentrations in older people.
11
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
Mr Howard King, 93 year old frail man, has been prescribed paracetamol prn. Discuss safe
paracetamol use in the elderly.
Answer:
For the usage of paracetamol in elderly people, calculations of geriatric dosage should be taken
into consideration, the body weight of the person should be considered, along with the surface
area and his age.
Part D
Mr Howard King has been admitted to hospital. He has a dose administration aid that he has
brought with him, however, he is not sure of the contents. What would you do in this
circumstance? How would you explain to Mr King how medication is administered in the hospital
if you are to use hospital stock?
Answer:
An explanation to Mr. King would be that the administration of medication in hospitals and the
usage of the hospital stocks would require the policies and procedures of the organization to be
followed and proper and significant reporting and documenting of the medications would be
needed.
Question 8
The following website may assist with this question
http://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/
Peripheral_Intravenous_IV_Device_Management/
https://www2.health.vic.gov.au/about/publications/policiesandguidelines/Intravenous%20therapy
(Download Intravenous therapy PDF)
While medical staff are responsible for IV fluid orders, you need to be aware of the indications,
techniques and problems associated with IV fluid administration
Part A
List six indications for IV fluid therapy
The major indications for IV fluid therapy are:
1. Dehydration: This refers to the fluid which is lost from the interstitial space. This is either
due to intake of less fluid in diet or due to the loss of excess fluid through vomiting,
polyuria, diarrhoea, etc.
2. Hypovolemia: In this case the fluid is lost from intravascular space. This is also caused
due to intake of less amount of fluids in the daily diet or from haemorrhage. This is also
caused by loss of fluid from the body during vomiting, diarrhoea, etc.
3. Distributive shock: This can be caused due to transfusion reactions which are severe,
tissue hypoxia, tissue perfusion reduction, vasodilation, etc (Hoste, et.al, 2014).
4. Kidney failure: The patients who suffer from kidney failure are those who face from
isotonic crystalloid fluids administration.
12
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
paracetamol use in the elderly.
Answer:
For the usage of paracetamol in elderly people, calculations of geriatric dosage should be taken
into consideration, the body weight of the person should be considered, along with the surface
area and his age.
Part D
Mr Howard King has been admitted to hospital. He has a dose administration aid that he has
brought with him, however, he is not sure of the contents. What would you do in this
circumstance? How would you explain to Mr King how medication is administered in the hospital
if you are to use hospital stock?
Answer:
An explanation to Mr. King would be that the administration of medication in hospitals and the
usage of the hospital stocks would require the policies and procedures of the organization to be
followed and proper and significant reporting and documenting of the medications would be
needed.
Question 8
The following website may assist with this question
http://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/
Peripheral_Intravenous_IV_Device_Management/
https://www2.health.vic.gov.au/about/publications/policiesandguidelines/Intravenous%20therapy
(Download Intravenous therapy PDF)
While medical staff are responsible for IV fluid orders, you need to be aware of the indications,
techniques and problems associated with IV fluid administration
Part A
List six indications for IV fluid therapy
The major indications for IV fluid therapy are:
1. Dehydration: This refers to the fluid which is lost from the interstitial space. This is either
due to intake of less fluid in diet or due to the loss of excess fluid through vomiting,
polyuria, diarrhoea, etc.
2. Hypovolemia: In this case the fluid is lost from intravascular space. This is also caused
due to intake of less amount of fluids in the daily diet or from haemorrhage. This is also
caused by loss of fluid from the body during vomiting, diarrhoea, etc.
3. Distributive shock: This can be caused due to transfusion reactions which are severe,
tissue hypoxia, tissue perfusion reduction, vasodilation, etc (Hoste, et.al, 2014).
4. Kidney failure: The patients who suffer from kidney failure are those who face from
isotonic crystalloid fluids administration.
12
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
5. Certain toxicities: There are many toxins which are being excreted through the kidneys.
This elimination of the toxics can be enhanced by the fluid therapy.
6. Palpitations: The person might have palpitations, fast breathing and chest pain of the
patient.
Part B
Discuss the infusion equipment that is required for IV infusion.
The most effective and widely used infusion therapy equipment is the infusion pump. These
medical devices are used quite often for IV fusion. The availability of the infusion pumps is not
very easy all the time when there is a prompt need. When there is an increased inflow of
patients there is a need for more infusion pumps for carrying out the IV infusion therapy. There
are many products of infusion which are given on rental basis. These include the syringe,
feeding pumps, volumetric, PCA, IV poles, etc. There are many more equipment needed for the
administration of the infusion therapy. The equipment accessories are needed so that the IV
infusion can take place accurately with adequate precision.
Part C
Discuss the complications of IV fluid therapy.
There are many types of complications which can arise due to the IV infusion therapy. These
include hematoma, infiltration, phlebitis, air embolism, intraarterial injection, extravascular drug
administration, etc. The infusion complications are quite complex and they are threatening
though much rare in their occurrence. In case of infiltration, the soft tissue area around the
intravascular space is either infused by the fluid or medication (Peng,et.al, 2014). When the
needle is put in a wrong way outside the lumen in a human body infiltration takes place.
Hematoma is caused by the blood leakage into the soft tissue area and its surroundings.
Through the IV administration set when large amounts of air enters the veins of the patients, air
embolism is caused. There are many other complications which are caused due to different
aspects of IV infusion therapy.
Question 9
The following website may assist with this question
http://www.vipscore.net/wp-content/uploads/2012/04/002-IV3000-A4-score-and-vein-card.pdf
Part A
Using the Visual Infusion Phlebitis Score, discuss the symptoms and signs of transfusion
reactions.
There are many signs and symptoms of transfusion reactions. The most commonly observed
signs of transfusion reactions are chills, fever, urticaria, itching, hives, etc (Klein and Anstee,
2014). There are some symptoms which when observed one can go for light medication and get
cured of it easily. In fact there are some symptoms which do not even need any kind of
treatment and get resolved on their own. However there are certain complicated symptoms as
well which need serious medical help for getting resolved. These complex diseases include
hypotension, red urine known as hemoglobinuria, low blood pressure, high fever, respiratory
distress, etc. These can result in very serious kinds of reactions.
Part B
13
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
This elimination of the toxics can be enhanced by the fluid therapy.
6. Palpitations: The person might have palpitations, fast breathing and chest pain of the
patient.
Part B
Discuss the infusion equipment that is required for IV infusion.
The most effective and widely used infusion therapy equipment is the infusion pump. These
medical devices are used quite often for IV fusion. The availability of the infusion pumps is not
very easy all the time when there is a prompt need. When there is an increased inflow of
patients there is a need for more infusion pumps for carrying out the IV infusion therapy. There
are many products of infusion which are given on rental basis. These include the syringe,
feeding pumps, volumetric, PCA, IV poles, etc. There are many more equipment needed for the
administration of the infusion therapy. The equipment accessories are needed so that the IV
infusion can take place accurately with adequate precision.
Part C
Discuss the complications of IV fluid therapy.
There are many types of complications which can arise due to the IV infusion therapy. These
include hematoma, infiltration, phlebitis, air embolism, intraarterial injection, extravascular drug
administration, etc. The infusion complications are quite complex and they are threatening
though much rare in their occurrence. In case of infiltration, the soft tissue area around the
intravascular space is either infused by the fluid or medication (Peng,et.al, 2014). When the
needle is put in a wrong way outside the lumen in a human body infiltration takes place.
Hematoma is caused by the blood leakage into the soft tissue area and its surroundings.
Through the IV administration set when large amounts of air enters the veins of the patients, air
embolism is caused. There are many other complications which are caused due to different
aspects of IV infusion therapy.
Question 9
The following website may assist with this question
http://www.vipscore.net/wp-content/uploads/2012/04/002-IV3000-A4-score-and-vein-card.pdf
Part A
Using the Visual Infusion Phlebitis Score, discuss the symptoms and signs of transfusion
reactions.
There are many signs and symptoms of transfusion reactions. The most commonly observed
signs of transfusion reactions are chills, fever, urticaria, itching, hives, etc (Klein and Anstee,
2014). There are some symptoms which when observed one can go for light medication and get
cured of it easily. In fact there are some symptoms which do not even need any kind of
treatment and get resolved on their own. However there are certain complicated symptoms as
well which need serious medical help for getting resolved. These complex diseases include
hypotension, red urine known as hemoglobinuria, low blood pressure, high fever, respiratory
distress, etc. These can result in very serious kinds of reactions.
Part B
13
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Mrs Jones has an IV cannula insitu. Mrs Jones has been complaining of slight pain and you
note that there is slight redness near the IV site. Using the Visual Infusion Phlebitis Score, what
score is this IV cannula site and, following the Visual Infusion Phlebitis policy statement, what
would be your actions.
After the stage or score of 0 when the cannula site is healthy comes the score of 1 when there
is cannula site accompanied by slight pain near to the IV site and some redness also observed
near the same area (Higgingson, 2015). Thus Mrs. Jones is in score 1 of the IV cannula site.
Now the actions which are good for practice after this cannula site of score 1 include observing
the cannula on a daily basis. There is a need for intravenous dressing in order to secure the
cannula. The contaminated and loose dressing must be removed. Whenever it is possible the
cannula must be kept far from the joints. The technique of aseptic need to be followed. The
cannula needs to be resisted following the position of the policy. The care must be planned and
documented so that it can be continued and sustained. The cannula which is being used must
be apt for the patient and their need. Thus the smallest gauge must be used. When the Visual
Infusion Phlebitis Score is 2 during stage 2, the cannula must be replaced at that very first
infusion phlebitis indication.
Part C
Mrs White has been receiving IV saline with 20mmol KCL. Mrs White has been complaining of
- Fatigue or weakness
- A feeling of numbness or tingling
- Nausea and vomiting
- Shortness of breath
- Chest pain and palpitations
a) What would you do in this situation?
When the intravenous sodium chloride (KCL) is being pushed in 20mmol, this IV fluid saline
is having certain side effects on the patients. These side effects include the problems which
Mrs, White is complaining of like nausea, vomiting, fatigue and weakness of the body, The
shortness of breath and the palpitations or even the chest pain is an impact of the KCL which
is pushed into the body of the patient. By increasing the intake of the fluids, providing proper
medication, preventing all the loss of fluid from the body, etc. can be the actions which can
improve or resolve the problems which Mrs. White is facing.
b) Discuss how IV KCL is monitored in the health setting.
In the health care setting it is monitored by the medical board and officials that the patients
do not receive any form of overdose of the IV fluids. The dosage that has been allowed for
the patients for potassium is 40 mEq/h. However, the medical professionals and the board
prevent the dosage of more than 20 mEq/h of IV fluid to be given to any patient. There could
be many deleterious impacts potentially arising from over dose. Therefore, this can be
14
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
note that there is slight redness near the IV site. Using the Visual Infusion Phlebitis Score, what
score is this IV cannula site and, following the Visual Infusion Phlebitis policy statement, what
would be your actions.
After the stage or score of 0 when the cannula site is healthy comes the score of 1 when there
is cannula site accompanied by slight pain near to the IV site and some redness also observed
near the same area (Higgingson, 2015). Thus Mrs. Jones is in score 1 of the IV cannula site.
Now the actions which are good for practice after this cannula site of score 1 include observing
the cannula on a daily basis. There is a need for intravenous dressing in order to secure the
cannula. The contaminated and loose dressing must be removed. Whenever it is possible the
cannula must be kept far from the joints. The technique of aseptic need to be followed. The
cannula needs to be resisted following the position of the policy. The care must be planned and
documented so that it can be continued and sustained. The cannula which is being used must
be apt for the patient and their need. Thus the smallest gauge must be used. When the Visual
Infusion Phlebitis Score is 2 during stage 2, the cannula must be replaced at that very first
infusion phlebitis indication.
Part C
Mrs White has been receiving IV saline with 20mmol KCL. Mrs White has been complaining of
- Fatigue or weakness
- A feeling of numbness or tingling
- Nausea and vomiting
- Shortness of breath
- Chest pain and palpitations
a) What would you do in this situation?
When the intravenous sodium chloride (KCL) is being pushed in 20mmol, this IV fluid saline
is having certain side effects on the patients. These side effects include the problems which
Mrs, White is complaining of like nausea, vomiting, fatigue and weakness of the body, The
shortness of breath and the palpitations or even the chest pain is an impact of the KCL which
is pushed into the body of the patient. By increasing the intake of the fluids, providing proper
medication, preventing all the loss of fluid from the body, etc. can be the actions which can
improve or resolve the problems which Mrs. White is facing.
b) Discuss how IV KCL is monitored in the health setting.
In the health care setting it is monitored by the medical board and officials that the patients
do not receive any form of overdose of the IV fluids. The dosage that has been allowed for
the patients for potassium is 40 mEq/h. However, the medical professionals and the board
prevent the dosage of more than 20 mEq/h of IV fluid to be given to any patient. There could
be many deleterious impacts potentially arising from over dose. Therefore, this can be
14
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
prevented. The adverse effect on the system of cardiac conduction can be prevented by
minimising the dosage. The intravenous pushing of the potassium solutions must be
prevented at all times. The potassium solution needs to be given in the form of dilute
solutions.
c) From the listed signs and symptoms, what would you be concerned about?
Among all the symptoms and the signs which have been observed, the sign or the symptom
about which I am most concerned is the chest pain and the palpitations which Mrs. White is
experiencing. My concern for this is because the patient facing chest pain may eventually
have a heart attack if not provided timely and proper medication.
Part D
Mrs White is ordered bd paracetamol. Mrs White states that paracetamol “doesn’t work” and
refuses the paracetamol. What are your actions?
When the patient refuses to intake the paracetamol or any other medicine which is suggested to
the patient as a part of the medication process, the duty of the nurse or the doctor in the first
place is to talk about the problem and make the patient agree to take the required medicines.
However, there could be situations under which the nurse or the doctor might just have to push
in the right dosage of the bd paracetamol which was suggested to the patient for his/ her intake
considering the medical condition of the patient.
Question 10
The following website may assist with this question
http://www.safetyandquality.gov.au/wp-content/uploads/2012/10/Standard7_Oct_2012_WEB.pdf
Part A
The aim of Standard 7 of the NSQHS Standards is to ensure safe, appropriate, effective and
efficient blood management systems. Discuss the four key accreditation criteria under the
National Blood and Blood Products Standard.
Answer:
The four key accreditation criteria under the National Blood and Blood Products Standard are:
1. A system or governance followed for the prescription of the blood or related products for
clinical usage. Thus the duty of the health care settings and units is to see that the blood
is being prescribed and used at the clinics in a safe and prescribed manner.
2. There is a need for proper documentation of the information regarding the patients. The
staff involved in the work at the clinics need to ensure that all the information regarding
the patients is noted, kept as a record for future reference. All the history regarding the
blood products used for the patient, their blood transfusion details, etc. need to be
maintained.
15
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
minimising the dosage. The intravenous pushing of the potassium solutions must be
prevented at all times. The potassium solution needs to be given in the form of dilute
solutions.
c) From the listed signs and symptoms, what would you be concerned about?
Among all the symptoms and the signs which have been observed, the sign or the symptom
about which I am most concerned is the chest pain and the palpitations which Mrs. White is
experiencing. My concern for this is because the patient facing chest pain may eventually
have a heart attack if not provided timely and proper medication.
Part D
Mrs White is ordered bd paracetamol. Mrs White states that paracetamol “doesn’t work” and
refuses the paracetamol. What are your actions?
When the patient refuses to intake the paracetamol or any other medicine which is suggested to
the patient as a part of the medication process, the duty of the nurse or the doctor in the first
place is to talk about the problem and make the patient agree to take the required medicines.
However, there could be situations under which the nurse or the doctor might just have to push
in the right dosage of the bd paracetamol which was suggested to the patient for his/ her intake
considering the medical condition of the patient.
Question 10
The following website may assist with this question
http://www.safetyandquality.gov.au/wp-content/uploads/2012/10/Standard7_Oct_2012_WEB.pdf
Part A
The aim of Standard 7 of the NSQHS Standards is to ensure safe, appropriate, effective and
efficient blood management systems. Discuss the four key accreditation criteria under the
National Blood and Blood Products Standard.
Answer:
The four key accreditation criteria under the National Blood and Blood Products Standard are:
1. A system or governance followed for the prescription of the blood or related products for
clinical usage. Thus the duty of the health care settings and units is to see that the blood
is being prescribed and used at the clinics in a safe and prescribed manner.
2. There is a need for proper documentation of the information regarding the patients. The
staff involved in the work at the clinics need to ensure that all the information regarding
the patients is noted, kept as a record for future reference. All the history regarding the
blood products used for the patient, their blood transfusion details, etc. need to be
maintained.
15
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
3. The blood as well as the related blood products is maintained in a safe manner. The
receipt, storage, transportation and the usage of the blood products is done in a very
safe manner so that the products which are very crucial for the patients at times of need
are not misused.
4. A strong communication is established between the caregivers and the patients. There
are many pros and cons associated with the treatment process. These risks and other
subsequent benefits need to be communicated to the caregivers and their patients so
that the treatment plan is well understood.
Part B
All blood donations are processed into a number of blood components with specific indications.
Complete the following
Red cells are used
Red cells are used for carrying the oxygen from the lungs to the various tissues in the body
and carrying the carbon dioxide from the body to the lungs. Haemoglobin is the protein which is
present in the red blood cells and does this work of carrying oxygen and carbon dioxide in and
out of the lungs respectively.
Platelets are used
Platelets are used to stop the bleeding after any cut. The blood is able to get clot and blood
flow is stopped after an injury due to the presence of platelets.
Plasma contains
Plasma contains fibrinogen, albumin and globulins. The albumin is the main constituent of the
protein. The fibrinogen is the present in the blood and helps in clotting. The antibodies are
formed by the globulins. The work of the plasma is to maintain the blood pressure in the body,
supply proteins enabling clotting of blood and increasing or maintaining the immunity level.
Part C
The basic principle of client care during transfusion is to ensure the client’s safety. The client
receiving a transfusion must be actively monitored for a possible transfusion reaction as serious
reactions can occur within a few minutes of the transfusion commencing. Any suspected
problems must be dealt with promptly and followed through appropriately.
It is also important that the effectiveness of the transfusion is evaluated and documented.
Each blood pack transfused carries the risk of an acute or delayed adverse effect. So that these
are recognised and managed promptly, the client must be observed and their vital signs (TPR,
BP) measured and recorded.
Additional vital sign measurements, including oxygen saturation are at the discretion of each
clinical area/hospital policy.
Discuss the adverse reactions that you need to be aware of.
Answer:
The possible reactions of suspected transfusion reactions are fever, hypotension, chills, back
and chest pain, acute distress of the respiratory system, bleeding, dark urine, urticaria, oozing,
etc.
16
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
receipt, storage, transportation and the usage of the blood products is done in a very
safe manner so that the products which are very crucial for the patients at times of need
are not misused.
4. A strong communication is established between the caregivers and the patients. There
are many pros and cons associated with the treatment process. These risks and other
subsequent benefits need to be communicated to the caregivers and their patients so
that the treatment plan is well understood.
Part B
All blood donations are processed into a number of blood components with specific indications.
Complete the following
Red cells are used
Red cells are used for carrying the oxygen from the lungs to the various tissues in the body
and carrying the carbon dioxide from the body to the lungs. Haemoglobin is the protein which is
present in the red blood cells and does this work of carrying oxygen and carbon dioxide in and
out of the lungs respectively.
Platelets are used
Platelets are used to stop the bleeding after any cut. The blood is able to get clot and blood
flow is stopped after an injury due to the presence of platelets.
Plasma contains
Plasma contains fibrinogen, albumin and globulins. The albumin is the main constituent of the
protein. The fibrinogen is the present in the blood and helps in clotting. The antibodies are
formed by the globulins. The work of the plasma is to maintain the blood pressure in the body,
supply proteins enabling clotting of blood and increasing or maintaining the immunity level.
Part C
The basic principle of client care during transfusion is to ensure the client’s safety. The client
receiving a transfusion must be actively monitored for a possible transfusion reaction as serious
reactions can occur within a few minutes of the transfusion commencing. Any suspected
problems must be dealt with promptly and followed through appropriately.
It is also important that the effectiveness of the transfusion is evaluated and documented.
Each blood pack transfused carries the risk of an acute or delayed adverse effect. So that these
are recognised and managed promptly, the client must be observed and their vital signs (TPR,
BP) measured and recorded.
Additional vital sign measurements, including oxygen saturation are at the discretion of each
clinical area/hospital policy.
Discuss the adverse reactions that you need to be aware of.
Answer:
The possible reactions of suspected transfusion reactions are fever, hypotension, chills, back
and chest pain, acute distress of the respiratory system, bleeding, dark urine, urticaria, oozing,
etc.
16
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Part D
Outline your actions In the event of a suspected blood transfusion reaction.
The patient in each of a suspected blood transfusion reaction needs immediate medical care.
The pack of the blood used for transfusion must be disconnected immediately. A proper
documented report of the transfusion reaction is to be submitted to the medical board.
Part E
A record of the administration of blood components must be kept in the client’s medical record.
What would you include in your documentation?
Answer:
The client’s medical record has to be maintained very effectively by the health care unit. The
following components need to be included while maintaining a document for a single patient.
1. Every blood transfusion history regarding the patient has to be recorded.
2. All the blood products which were transfused will be documented.
3. All the suspected transfusion reactions of the past must be noted.
4. All the indications pertaining to the blood use need to be noted.
Part F
Blood transfusion involves a chain of decisions and actions by health professionals. Every link in
this chain is vital to the safety of the patient, and every person along that chain is capable of
making an error. These mistakes can be fatal.
Human blood is fragile and in order to prevent damage and deterioration, including bacterial
growth that can be fatal, blood must always be stored under appropriate conditions. For red
cells this is a designated, temperature-monitored blood fridge that may be located within the
transfusion provider's laboratory or within the hospital. If for some reason blood is required to be
stored or transported for longer than 30 minutes outside a blood fridge, a validated transport
container and packing procedure must be used to ensure appropriate temperature control
complies with the current Australian Standard Contact the transfusion provider for more
information.
When should blood be picked-up from the laboratory of blood fridge? How do you correctly
identify the correct client for the blood?
Answer:
The blood should not be preserved and stored in any local or domestic refrigerators. The blood
must be picked-up from the laboratory of blood fridge one unit at one time. This must not be
done from before. Just when there are 30 minutes left before the blood transfusion, the blood
must be taken out of the fridge (Hess, 2014). Thus the blood bank or laboratory fridge will store
the blood until it is needed for immediate use.
Question 11
Every medication must have a drug profile included in the package of the medication. The
following information is included:
(1) Drug Name---includes generic name and trade name
(2) Classification---determined based on its effect on the patient and its mechanism of
action
(3) Mechanism of Action--describes how the medication causes the intended effect
17
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
Outline your actions In the event of a suspected blood transfusion reaction.
The patient in each of a suspected blood transfusion reaction needs immediate medical care.
The pack of the blood used for transfusion must be disconnected immediately. A proper
documented report of the transfusion reaction is to be submitted to the medical board.
Part E
A record of the administration of blood components must be kept in the client’s medical record.
What would you include in your documentation?
Answer:
The client’s medical record has to be maintained very effectively by the health care unit. The
following components need to be included while maintaining a document for a single patient.
1. Every blood transfusion history regarding the patient has to be recorded.
2. All the blood products which were transfused will be documented.
3. All the suspected transfusion reactions of the past must be noted.
4. All the indications pertaining to the blood use need to be noted.
Part F
Blood transfusion involves a chain of decisions and actions by health professionals. Every link in
this chain is vital to the safety of the patient, and every person along that chain is capable of
making an error. These mistakes can be fatal.
Human blood is fragile and in order to prevent damage and deterioration, including bacterial
growth that can be fatal, blood must always be stored under appropriate conditions. For red
cells this is a designated, temperature-monitored blood fridge that may be located within the
transfusion provider's laboratory or within the hospital. If for some reason blood is required to be
stored or transported for longer than 30 minutes outside a blood fridge, a validated transport
container and packing procedure must be used to ensure appropriate temperature control
complies with the current Australian Standard Contact the transfusion provider for more
information.
When should blood be picked-up from the laboratory of blood fridge? How do you correctly
identify the correct client for the blood?
Answer:
The blood should not be preserved and stored in any local or domestic refrigerators. The blood
must be picked-up from the laboratory of blood fridge one unit at one time. This must not be
done from before. Just when there are 30 minutes left before the blood transfusion, the blood
must be taken out of the fridge (Hess, 2014). Thus the blood bank or laboratory fridge will store
the blood until it is needed for immediate use.
Question 11
Every medication must have a drug profile included in the package of the medication. The
following information is included:
(1) Drug Name---includes generic name and trade name
(2) Classification---determined based on its effect on the patient and its mechanism of
action
(3) Mechanism of Action--describes how the medication causes the intended effect
17
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
(4) Indications---Reasons or conditions why the medication is given
(5) Pharmacokinetics---Describes how the medication is absorbed, distributed, and
eliminated from the body
(6) Side and adverse effects---lists the undesired effects that are found during the
development of the drug
(7) Routes of administration---lists the route of administration for that drug
(8) Drug forms---lists available forms and their concentrations
(9) Doses-----amount of medication that should be administered for a particular condition
(10) Contraindications--Conditions under which it is inappropriate to administer the
medication
(11) Special Considerations--Information necessary to administer the medication to
pediatrics, pregnant, or geriatric patients, and any other special groups defined for the drug.
Select one medication from the following list and complete the drug profile information:
Digoxin
Warfarin
Morphine
Glyceryl Trinitrate
Prednisolone
Diabex
Captopril
Drug Profile
Research a drug of your choice including:
1) Generic/trade name of drug
2) Schedule and
3) Class of drug
4) Available forms/usual dosage (lifespan)/timing of dose
5) Indications for use
6) Administration considerations
7) Factors affecting absorption, metabolism, and excretion of the drug
8) Mode of Action of the drug
9) Interactions/side effects/toxic effects
10) Monitoring requirements e.g. nursing observation/ reporting and documentation
11) Education requirements for clients to self-administer medication
Storage of Medications
- Discuss how the drug is stored in the workplace
Answer:
Drug Profile
Morphine
1) Generic name: Morphine Sulfate
2) Schedule: Schedule 8
3) Class of drug: Opioid (Narcotic) Analgesics
4) Available forms/usual dosage (lifespan)/timing of dose: Different forms of Morphine
are Tablet, Extended Release, Capsule, Extended Release, 24 HR, Solution,
Capsule, Extended Release and Tablet.
5) Indications for use: Morphine should be used only when the other options for
treatment become ineffective on the patients like opioid combination products, non-
opioid analgesics, etc.
6) Administration considerations: The Schedule 8 Morphine Drug needs same
administration like any poison.
7) Factors affecting absorption, metabolism, and excretion of the drug: Metabolism of
Morphine is between MG3 – MG6. The role of kidney and the renal function is
18
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
(5) Pharmacokinetics---Describes how the medication is absorbed, distributed, and
eliminated from the body
(6) Side and adverse effects---lists the undesired effects that are found during the
development of the drug
(7) Routes of administration---lists the route of administration for that drug
(8) Drug forms---lists available forms and their concentrations
(9) Doses-----amount of medication that should be administered for a particular condition
(10) Contraindications--Conditions under which it is inappropriate to administer the
medication
(11) Special Considerations--Information necessary to administer the medication to
pediatrics, pregnant, or geriatric patients, and any other special groups defined for the drug.
Select one medication from the following list and complete the drug profile information:
Digoxin
Warfarin
Morphine
Glyceryl Trinitrate
Prednisolone
Diabex
Captopril
Drug Profile
Research a drug of your choice including:
1) Generic/trade name of drug
2) Schedule and
3) Class of drug
4) Available forms/usual dosage (lifespan)/timing of dose
5) Indications for use
6) Administration considerations
7) Factors affecting absorption, metabolism, and excretion of the drug
8) Mode of Action of the drug
9) Interactions/side effects/toxic effects
10) Monitoring requirements e.g. nursing observation/ reporting and documentation
11) Education requirements for clients to self-administer medication
Storage of Medications
- Discuss how the drug is stored in the workplace
Answer:
Drug Profile
Morphine
1) Generic name: Morphine Sulfate
2) Schedule: Schedule 8
3) Class of drug: Opioid (Narcotic) Analgesics
4) Available forms/usual dosage (lifespan)/timing of dose: Different forms of Morphine
are Tablet, Extended Release, Capsule, Extended Release, 24 HR, Solution,
Capsule, Extended Release and Tablet.
5) Indications for use: Morphine should be used only when the other options for
treatment become ineffective on the patients like opioid combination products, non-
opioid analgesics, etc.
6) Administration considerations: The Schedule 8 Morphine Drug needs same
administration like any poison.
7) Factors affecting absorption, metabolism, and excretion of the drug: Metabolism of
Morphine is between MG3 – MG6. The role of kidney and the renal function is
18
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
important in case of excretion of the morphine drug.
8) Mode of Action of the drug: The drug has a strong effect on the central nervous
system of the body and the smooth muscles.
9) Interactions/side effects/toxic effects: Vomiting, nausea, constipation, dizziness,
sweating, dry mouth, etc.
10) Monitoring requirements e.g. nursing observation/ reporting and documentation: The
nurse cannot use the morphine drug unless prescribed or permitted by a medical
officer or authority during an emergency situation.
11) Education requirements for clients to self-administer medication: The medical
practitioner must know how the drug can be used and in which situations exactly.
Storage of Medications
Morphine must be stored in a place exposed to room temperature. This should be kept
away from the reach of the small children. The drug must be kept away from direct sunlight.
This drug should not be disposed of with any other domestic waste.
Assessment Criteria Comments
Presentation and structure, - 1
Appropriate sequencing of information - 1
Expression of information - 1
Identification and description
- Generic/trade name of drug -1
- Schedule and class of drug -2
- Available forms / usual dosage (lifespan) /
timing of dose -2
Administration considerations - 2
Factors affecting absorption, metabolism, and
excretion of drug - 4
Interactions / allergic reactions/ side effects /
toxic effects - 3
Mode of Action of drugs -2
Indications for use - 2
Monitoring of effects /nursing observation/
reporting
and documentation -4
Education requirements for clients to self-
administer
medication - 3
Question 12
Joseph is a 45 year old male who works as a roofer for a building contractor. He fell from a third
floor roof, suffering from multiple fractures and a severe head injury. He has been in a comatose
state ever since. Unable to take foods orally, a nasogastric tube was inserted for feeding. Full
strength Ensure at 50 cc/hour was ordered initially, and then advanced to 75 cc/hr after the first
24 hours. Joseph had mild diarrhoea when the tube feeding was first initiated, but this resolved
after 2 days. At the time of admission, Joseph was 5'8" tall and weighed 82 kg, his usual body
weight.
19
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
8) Mode of Action of the drug: The drug has a strong effect on the central nervous
system of the body and the smooth muscles.
9) Interactions/side effects/toxic effects: Vomiting, nausea, constipation, dizziness,
sweating, dry mouth, etc.
10) Monitoring requirements e.g. nursing observation/ reporting and documentation: The
nurse cannot use the morphine drug unless prescribed or permitted by a medical
officer or authority during an emergency situation.
11) Education requirements for clients to self-administer medication: The medical
practitioner must know how the drug can be used and in which situations exactly.
Storage of Medications
Morphine must be stored in a place exposed to room temperature. This should be kept
away from the reach of the small children. The drug must be kept away from direct sunlight.
This drug should not be disposed of with any other domestic waste.
Assessment Criteria Comments
Presentation and structure, - 1
Appropriate sequencing of information - 1
Expression of information - 1
Identification and description
- Generic/trade name of drug -1
- Schedule and class of drug -2
- Available forms / usual dosage (lifespan) /
timing of dose -2
Administration considerations - 2
Factors affecting absorption, metabolism, and
excretion of drug - 4
Interactions / allergic reactions/ side effects /
toxic effects - 3
Mode of Action of drugs -2
Indications for use - 2
Monitoring of effects /nursing observation/
reporting
and documentation -4
Education requirements for clients to self-
administer
medication - 3
Question 12
Joseph is a 45 year old male who works as a roofer for a building contractor. He fell from a third
floor roof, suffering from multiple fractures and a severe head injury. He has been in a comatose
state ever since. Unable to take foods orally, a nasogastric tube was inserted for feeding. Full
strength Ensure at 50 cc/hour was ordered initially, and then advanced to 75 cc/hr after the first
24 hours. Joseph had mild diarrhoea when the tube feeding was first initiated, but this resolved
after 2 days. At the time of admission, Joseph was 5'8" tall and weighed 82 kg, his usual body
weight.
19
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
One month later, Joseph, who has no gag reflex=x, was transferred to an extended care facility.
By this time he weighed 71kg. A PEG line was inserted and full strength Ensure Plus was begun
at 65cc/hr with the goal of anabolism (weight gain). The formula was tolerated well. However,
after several weeks constipation developed. The formula was changed to Jevity at 75cc/hr. The
protocol was also changed from a continuous drip to bolus feedings to equal the amount
provided by the continuous drip.
Part A
What does the abbreviation PEG stand for?
Answer:
The full form of PEG is Percutaneous Endoscopic Gastronomy.
Part B
Jevity comes in a ba of 500ml. How many hours will this bag take to run through?
Answer:
When the medicine Jevity is given in a 500ml measurement, it would take 8 hours for this
measurement to run through.
Part C
Give two reasons why a PEG tube would be used
Answer:
The Percutaneous Endoscopic Gastronomy is mainly used for the victims who are unable to
consume food orally. It is used for providing food and nutrition to the victims who cannot eat,
chew or swallow food. Another use of the PEG tube is to make a way for feeding enterally,
providing the medication and hydrating the victim’s abdominal wall who has been handicapped
since many years (Vanis et al., 2012).
Part D
Give two complications of a PEG. List two signs and symptoms for each complication.
Answer:
The severe complications of using PEG tube is that it can cause peristomal wound infections.
The sign and indication of such a complication include difficulties in transmission of food in the
stomach, the patient’s skin getting inflamed and fall in the food intake level of the patient.
Another complication of the PEG tube is acute bleeding. The signs and indications include the
clogging and bursting of blood vessels due to pressure, reddening of the skin etc.
Part E
Joseph is complaining of abdominal pain 8/10 with not effect from Panadol Morphine elixier
5gm is ordered stat. Morphine strength is 10mgs in 10mls.
What schedule drug is morphine?
20
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
By this time he weighed 71kg. A PEG line was inserted and full strength Ensure Plus was begun
at 65cc/hr with the goal of anabolism (weight gain). The formula was tolerated well. However,
after several weeks constipation developed. The formula was changed to Jevity at 75cc/hr. The
protocol was also changed from a continuous drip to bolus feedings to equal the amount
provided by the continuous drip.
Part A
What does the abbreviation PEG stand for?
Answer:
The full form of PEG is Percutaneous Endoscopic Gastronomy.
Part B
Jevity comes in a ba of 500ml. How many hours will this bag take to run through?
Answer:
When the medicine Jevity is given in a 500ml measurement, it would take 8 hours for this
measurement to run through.
Part C
Give two reasons why a PEG tube would be used
Answer:
The Percutaneous Endoscopic Gastronomy is mainly used for the victims who are unable to
consume food orally. It is used for providing food and nutrition to the victims who cannot eat,
chew or swallow food. Another use of the PEG tube is to make a way for feeding enterally,
providing the medication and hydrating the victim’s abdominal wall who has been handicapped
since many years (Vanis et al., 2012).
Part D
Give two complications of a PEG. List two signs and symptoms for each complication.
Answer:
The severe complications of using PEG tube is that it can cause peristomal wound infections.
The sign and indication of such a complication include difficulties in transmission of food in the
stomach, the patient’s skin getting inflamed and fall in the food intake level of the patient.
Another complication of the PEG tube is acute bleeding. The signs and indications include the
clogging and bursting of blood vessels due to pressure, reddening of the skin etc.
Part E
Joseph is complaining of abdominal pain 8/10 with not effect from Panadol Morphine elixier
5gm is ordered stat. Morphine strength is 10mgs in 10mls.
What schedule drug is morphine?
20
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
Answer:
Morphine drug is included under the Schedule II drugs. They are used for medical purposes for
curing chronic diseases.
How many mls would you give?
Answer:
The morphine drug can be given through the veins within the range of 2.5 to 10 ml. While giving
morphine to the patient through muscles or subcutaneously, the range should be within 5 to 20
ml.
Part F
Erythromycin suspension 500mg is ordered 4/24.
What is the schedule of Erythromycin?
Answer:
Erythromycin belongs to schedule IV. It is commonly called Macrolide Antibiotic. This aids in the
ceasing of development of bacteria.
In stock is Erythromycin 250mg in 5mls. Joseph is ordered 500mg. How many mls is required
every four hours?
Answer:
In this case, Joseph is ordered with 500mg of erythromycin. Around 10ml of erythromycin is
required to be given to the patient during every hour.
Part G
What procedures are required before and after administration of drugs via a PEG. Include
infection control measures.
Answer:
The putting of a PEG tube can be fulfilled by two people. One is an Endoscopist and another is
the skin person who would look into the non-endoscopic mechanisms. Before the tube is put, it
has to be placed in accordance with the position o the abdominal wall of the patient. After it is is
laced, the food should be started to ensure its proper working. Complete sterilization is required
for prohibition of infection. Anti-infection drugs can also be given to the patient.
Part H
10 minutes post administration of erythromycin Joseph looks pale and clammy, RR increases to
40 and he suddenly collapses. What steps would you do in this medical emergency?
Answer:
21
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
Morphine drug is included under the Schedule II drugs. They are used for medical purposes for
curing chronic diseases.
How many mls would you give?
Answer:
The morphine drug can be given through the veins within the range of 2.5 to 10 ml. While giving
morphine to the patient through muscles or subcutaneously, the range should be within 5 to 20
ml.
Part F
Erythromycin suspension 500mg is ordered 4/24.
What is the schedule of Erythromycin?
Answer:
Erythromycin belongs to schedule IV. It is commonly called Macrolide Antibiotic. This aids in the
ceasing of development of bacteria.
In stock is Erythromycin 250mg in 5mls. Joseph is ordered 500mg. How many mls is required
every four hours?
Answer:
In this case, Joseph is ordered with 500mg of erythromycin. Around 10ml of erythromycin is
required to be given to the patient during every hour.
Part G
What procedures are required before and after administration of drugs via a PEG. Include
infection control measures.
Answer:
The putting of a PEG tube can be fulfilled by two people. One is an Endoscopist and another is
the skin person who would look into the non-endoscopic mechanisms. Before the tube is put, it
has to be placed in accordance with the position o the abdominal wall of the patient. After it is is
laced, the food should be started to ensure its proper working. Complete sterilization is required
for prohibition of infection. Anti-infection drugs can also be given to the patient.
Part H
10 minutes post administration of erythromycin Joseph looks pale and clammy, RR increases to
40 and he suddenly collapses. What steps would you do in this medical emergency?
Answer:
21
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
After 10 minutes, when Joseph turns pale, the dose of erythromycin has to be stopped
immediately. The paleness is the outcome of over dosage of erythromycin. The rehydration of
the patient is essential followed by some food and other essential fluids.
Question 13
The following website may assist with this question
http://www.asthmahandbook.org.au/uploads/555143d72c3e3.pdf
Shelly is 30 year old female patient presents to the clinic with an asthma attack. Clinical records
show that she has been admitted to hospital on several occasions and once to ICU within the
past 12 months. On assessment she was finding it difficult to complete full sentences and had a
48-hour history of an upper respiratory illness with increasing shortness of breath and wheezing
for the past six hours. Her prescribed asthma medication was a twice-daily inhaled
corticosteroid in combination with a long-acting beta-2 agonist and inhaled salbutamol. She
normally used salbutamol once or twice a day but over the past two days her use had increased
to eight to 10 times per day and she could not sleep because of her breathlessness and
wheeze. Her vital signs are temperature 37° C, blood pressure 190/88 mm Hg, pulse 122
beats/minute, and respiratory rate 32 breaths/minute, oxygen saturation (O2 sat) is 88%.
Part A
What are your nursing actions?
Answer:
Shelly has entered into a pre stroke stage and it becomes essential to give her medication for
reduction the systolic blood pressure to a minimum of 150/80. The heart rate would decrease
automatically. Providing her 10 liters of oxygen would be feasible. This would lower her tension
and breathing trouble. In this way, her oxygen level in the body would increase and she would
switch to a comfortable position (To et al., 2012).
22
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
immediately. The paleness is the outcome of over dosage of erythromycin. The rehydration of
the patient is essential followed by some food and other essential fluids.
Question 13
The following website may assist with this question
http://www.asthmahandbook.org.au/uploads/555143d72c3e3.pdf
Shelly is 30 year old female patient presents to the clinic with an asthma attack. Clinical records
show that she has been admitted to hospital on several occasions and once to ICU within the
past 12 months. On assessment she was finding it difficult to complete full sentences and had a
48-hour history of an upper respiratory illness with increasing shortness of breath and wheezing
for the past six hours. Her prescribed asthma medication was a twice-daily inhaled
corticosteroid in combination with a long-acting beta-2 agonist and inhaled salbutamol. She
normally used salbutamol once or twice a day but over the past two days her use had increased
to eight to 10 times per day and she could not sleep because of her breathlessness and
wheeze. Her vital signs are temperature 37° C, blood pressure 190/88 mm Hg, pulse 122
beats/minute, and respiratory rate 32 breaths/minute, oxygen saturation (O2 sat) is 88%.
Part A
What are your nursing actions?
Answer:
Shelly has entered into a pre stroke stage and it becomes essential to give her medication for
reduction the systolic blood pressure to a minimum of 150/80. The heart rate would decrease
automatically. Providing her 10 liters of oxygen would be feasible. This would lower her tension
and breathing trouble. In this way, her oxygen level in the body would increase and she would
switch to a comfortable position (To et al., 2012).
22
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Part B
What is a nebulisation?
Answer:
Nebulization is the process by which a nebulizer is used. A nebulizer is an instrument which aids
in breathing. It is used to treat lung disorders, respiratory issues and cystic fibrosis. The
medicine is inhaled through nebulization (Sharafkhaneh et al., 2013).
Part C
Discuss the policy and procedure for administering nebulisation in the nursing home.
Answer:
The policy of nebulization includes the process of using it as per the prescription of the doctor,
the using of the appropriate method is required to be done by the nurses.
The procedure includes setting up the instrument in a sterilized place. The medicenes should be
put inside the container of the nebulizer’s tube. The prescribed medicine along with 2cc of saline
water is to be mixed. The wires should be plugged in. the patient should wear the mask
attached to the instrument. When the instrument starts, the patient should inhale it.
Part D
Discuss the maintenance and cleaning of nebulisers as per the nursing homes policies and
procedures.
Answer:
The nursing homes should follow the detailed instructions of the brochure given in the nebulizer.
The filter should be changed and cleaned regularly to move the dust particles. The mask should
not be used for more than the time prescribed. The parts should be sterilized.
Part E
Shelly states that she sometimes suffers from anxiety and chest pain after an asthma attack.
Shelly states that she would prefer not to take medications for her anxiety and chest pain and is
refusing her analgesia. Discuss your actions and consider the complementary therapies that
you may suggest to Shelly.
Answer:
To relieve Shelly of anxiety and chest pain, the complementary therapies like aromatherapy,
Biofeedback, acupuncture, Chiropractic Hypnotherapy and the like can be offered by the
nursing staff.
Part F
Discuss how medications are stored in the nursing home. What are the enrolled nurses roles
and responsibilities in medication administration. Refer to the organisations policies and
procedures.
Answer:
23
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
What is a nebulisation?
Answer:
Nebulization is the process by which a nebulizer is used. A nebulizer is an instrument which aids
in breathing. It is used to treat lung disorders, respiratory issues and cystic fibrosis. The
medicine is inhaled through nebulization (Sharafkhaneh et al., 2013).
Part C
Discuss the policy and procedure for administering nebulisation in the nursing home.
Answer:
The policy of nebulization includes the process of using it as per the prescription of the doctor,
the using of the appropriate method is required to be done by the nurses.
The procedure includes setting up the instrument in a sterilized place. The medicenes should be
put inside the container of the nebulizer’s tube. The prescribed medicine along with 2cc of saline
water is to be mixed. The wires should be plugged in. the patient should wear the mask
attached to the instrument. When the instrument starts, the patient should inhale it.
Part D
Discuss the maintenance and cleaning of nebulisers as per the nursing homes policies and
procedures.
Answer:
The nursing homes should follow the detailed instructions of the brochure given in the nebulizer.
The filter should be changed and cleaned regularly to move the dust particles. The mask should
not be used for more than the time prescribed. The parts should be sterilized.
Part E
Shelly states that she sometimes suffers from anxiety and chest pain after an asthma attack.
Shelly states that she would prefer not to take medications for her anxiety and chest pain and is
refusing her analgesia. Discuss your actions and consider the complementary therapies that
you may suggest to Shelly.
Answer:
To relieve Shelly of anxiety and chest pain, the complementary therapies like aromatherapy,
Biofeedback, acupuncture, Chiropractic Hypnotherapy and the like can be offered by the
nursing staff.
Part F
Discuss how medications are stored in the nursing home. What are the enrolled nurses roles
and responsibilities in medication administration. Refer to the organisations policies and
procedures.
Answer:
23
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
The medications in a nursing home should be kept in cool, dark and a separate room. It should
be under lock and key. The room should be devoid of dirt and dust. The expired medicines
should be replaces immediately. Refrigeration should be provided to those which require it.
It is the duty of the nursing staff to maintain the medicine room. They should have a continuous
vigilance upon the medicenes and a record should be maintained with regard to the dates and
expiries. They also have the duty of preserving the stock to fulfill the needs of patients.
24
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
be under lock and key. The room should be devoid of dirt and dust. The expired medicines
should be replaces immediately. Refrigeration should be provided to those which require it.
It is the duty of the nursing staff to maintain the medicine room. They should have a continuous
vigilance upon the medicenes and a record should be maintained with regard to the dates and
expiries. They also have the duty of preserving the stock to fulfill the needs of patients.
24
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
Reference List
Bergen, P.J., Landersdorfer, C.B., Zhang, J., Zhao, M., Lee, H.J., Nation, R.L. and Li, J., 2012.
Pharmacokinetics and pharmacodynamics of ‘old’polymyxins: what is new? Diagnostic
microbiology and infectious disease, 74(3), pp.213-223.
Butterworth, T. and Faugier, J., 2013. Clinical supervision and mentorship in nursing. 6th ed.
New York: Springer.
Eagar, S.C., Cowin, L.S., Gregory, L. and Firtko, A., 2010. Scope of practice conflict in nursing:
A new war or just the same battle? Contemporary Nurse, 36(1-2), pp.86-95.
Elliott, M. and Liu, Y., 2010. The nine rights of medication administration: an overview. British
Journal of Nursing, 19(5), pp.300-305.
Elsaesser, A. and Howard, C.V., 2012. Toxicology of nanoparticles. Advanced drug delivery
reviews, 64(2), pp.129-137.
Hess, J.R., 2014. Measures of stored red blood cell quality. Vox sanguinis, 107(1), pp.1-9.
Higgingson, R., 2015. IV cannula securement: protecting the patient from infection. British
Journal of Nursing, 24(Sup8), pp.S23-S28.
Hoste, E.A., Maitland, K., Brudney, C.S., Mehta, R., Vincent, J.L., Yates, D., Kellum, J.A.,
Mythen, M.G. and Shaw, A.D., 2014. Four phases of intravenous fluid therapy: a conceptual
model. British journal of anaesthesia, 113(5), pp.740-747.
Klein, H.G. and Anstee, D.J., 2014. Mollison's blood transfusion in clinical medicine. 7th ed. New
Jersey: John Wiley & Sons.
Lesko, L.J., Zineh, I. and Huang, S.M., 2010. What is clinical utility and why should we
care? Clinical Pharmacology & Therapeutics, 88(6), pp.729-733.
Macdonald, M., 2010. Patient safety: examining the adequacy of the 5 rights of medication
administration. Clinical Nurse Specialist, 24(4), pp.196-201.
National Health and Medical Research Council (NHMRC), 2010. Australian Guidelines for the
Prevention and Control of Infection in Healthcare. 8th ed. Canberra: NHMRC.
Peng, K., Li, J., Cheng, H. and Ji, F.H., 2014. Goal-directed fluid therapy based on stroke
volume variations improves fluid management and gastrointestinal perfusion in patients
undergoing major orthopedic surgery. Medical Principles and Practice, 23(5), pp.413-420.
Ryoo, J.J., Ordin, D.L., Antonio, A.L.M., Oishi, S.M., Gould, M.K., Asch, S.M. and Malin, J.L.,
2013. Patient preference and contraindications in measuring quality of care: what do
administrative data miss? Journal of Clinical Oncology, 31(21), p.2716.
Severinsson, E. and Sand, Å., 2010. Evaluation of the clinical supervision and professional
development of student nurses. Journal of nursing management, 18(6), pp.669-677.
Sharafkhaneh, A., Wolf, R.A., Goodnight, S., Hanania, N.A., Make, B.J. and Tashkin, D.P., 2013.
Perceptions and attitudes toward the use of nebulized therapy for COPD: patient and caregiver
perspectives. COPD: Journal of Chronic Obstructive Pulmonary Disease, 10(4), pp.482-492.
Simons, F.E.R., Ardusso, L.R., Bilò, M.B., El-Gamal, Y.M., Ledford, D.K., Ring, J., Sanchez-
Borges, M., Senna, G.E., Sheikh, A. and Thong, B.Y., 2011. World Allergy Organization
anaphylaxis guidelines: summary. Journal of Allergy and Clinical Immunology, 127(3), pp.587-
593.
To, T., Stanojevic, S., Moores, G., Gershon, A.S., Bateman, E.D., Cruz, A.A. and Boulet, L.P.,
2012. Global asthma prevalence in adults: findings from the cross-sectional world health survey.
BMC public health, 12(1), p.204.
25
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
Bergen, P.J., Landersdorfer, C.B., Zhang, J., Zhao, M., Lee, H.J., Nation, R.L. and Li, J., 2012.
Pharmacokinetics and pharmacodynamics of ‘old’polymyxins: what is new? Diagnostic
microbiology and infectious disease, 74(3), pp.213-223.
Butterworth, T. and Faugier, J., 2013. Clinical supervision and mentorship in nursing. 6th ed.
New York: Springer.
Eagar, S.C., Cowin, L.S., Gregory, L. and Firtko, A., 2010. Scope of practice conflict in nursing:
A new war or just the same battle? Contemporary Nurse, 36(1-2), pp.86-95.
Elliott, M. and Liu, Y., 2010. The nine rights of medication administration: an overview. British
Journal of Nursing, 19(5), pp.300-305.
Elsaesser, A. and Howard, C.V., 2012. Toxicology of nanoparticles. Advanced drug delivery
reviews, 64(2), pp.129-137.
Hess, J.R., 2014. Measures of stored red blood cell quality. Vox sanguinis, 107(1), pp.1-9.
Higgingson, R., 2015. IV cannula securement: protecting the patient from infection. British
Journal of Nursing, 24(Sup8), pp.S23-S28.
Hoste, E.A., Maitland, K., Brudney, C.S., Mehta, R., Vincent, J.L., Yates, D., Kellum, J.A.,
Mythen, M.G. and Shaw, A.D., 2014. Four phases of intravenous fluid therapy: a conceptual
model. British journal of anaesthesia, 113(5), pp.740-747.
Klein, H.G. and Anstee, D.J., 2014. Mollison's blood transfusion in clinical medicine. 7th ed. New
Jersey: John Wiley & Sons.
Lesko, L.J., Zineh, I. and Huang, S.M., 2010. What is clinical utility and why should we
care? Clinical Pharmacology & Therapeutics, 88(6), pp.729-733.
Macdonald, M., 2010. Patient safety: examining the adequacy of the 5 rights of medication
administration. Clinical Nurse Specialist, 24(4), pp.196-201.
National Health and Medical Research Council (NHMRC), 2010. Australian Guidelines for the
Prevention and Control of Infection in Healthcare. 8th ed. Canberra: NHMRC.
Peng, K., Li, J., Cheng, H. and Ji, F.H., 2014. Goal-directed fluid therapy based on stroke
volume variations improves fluid management and gastrointestinal perfusion in patients
undergoing major orthopedic surgery. Medical Principles and Practice, 23(5), pp.413-420.
Ryoo, J.J., Ordin, D.L., Antonio, A.L.M., Oishi, S.M., Gould, M.K., Asch, S.M. and Malin, J.L.,
2013. Patient preference and contraindications in measuring quality of care: what do
administrative data miss? Journal of Clinical Oncology, 31(21), p.2716.
Severinsson, E. and Sand, Å., 2010. Evaluation of the clinical supervision and professional
development of student nurses. Journal of nursing management, 18(6), pp.669-677.
Sharafkhaneh, A., Wolf, R.A., Goodnight, S., Hanania, N.A., Make, B.J. and Tashkin, D.P., 2013.
Perceptions and attitudes toward the use of nebulized therapy for COPD: patient and caregiver
perspectives. COPD: Journal of Chronic Obstructive Pulmonary Disease, 10(4), pp.482-492.
Simons, F.E.R., Ardusso, L.R., Bilò, M.B., El-Gamal, Y.M., Ledford, D.K., Ring, J., Sanchez-
Borges, M., Senna, G.E., Sheikh, A. and Thong, B.Y., 2011. World Allergy Organization
anaphylaxis guidelines: summary. Journal of Allergy and Clinical Immunology, 127(3), pp.587-
593.
To, T., Stanojevic, S., Moores, G., Gershon, A.S., Bateman, E.D., Cruz, A.A. and Boulet, L.P.,
2012. Global asthma prevalence in adults: findings from the cross-sectional world health survey.
BMC public health, 12(1), p.204.
25
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

van der Graaf, P.H. and Benson, N., 2011. Systems pharmacology: bridging systems biology
and pharmacokinetics-pharmacodynamics (PKPD) in drug discovery and
development. Pharmaceutical research, 28(7), pp.1460-1464.
Vanis, N., Saray, A., Gornjakovic, S. and Mesihovic, R., 2012. Percutaneous endoscopic
gastrostomy (PEG): retrospective analysis of a 7-year clinical experience. Acta Informatica
Medica, 20(4), p.235.
26
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
and pharmacokinetics-pharmacodynamics (PKPD) in drug discovery and
development. Pharmaceutical research, 28(7), pp.1460-1464.
Vanis, N., Saray, A., Gornjakovic, S. and Mesihovic, R., 2012. Percutaneous endoscopic
gastrostomy (PEG): retrospective analysis of a 7-year clinical experience. Acta Informatica
Medica, 20(4), p.235.
26
Australia Institute of Business and Technology Version 1.2- June 2016
© Succeed Pty Ltd
1 out of 26
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.




