ACU BIOL122 Human Biological Science 2: Asthma Vodcast Presentation
VerifiedAdded on 2022/10/04
|7
|1485
|18
Presentation
AI Summary
This assignment is a vodcast presentation created for an Australian Catholic University BIOL122 Human Biological Science 2 course, focusing on asthma. The presentation details two major pathological changes during an asthma attack: bronchial smooth muscle contraction and increased mucus pr...
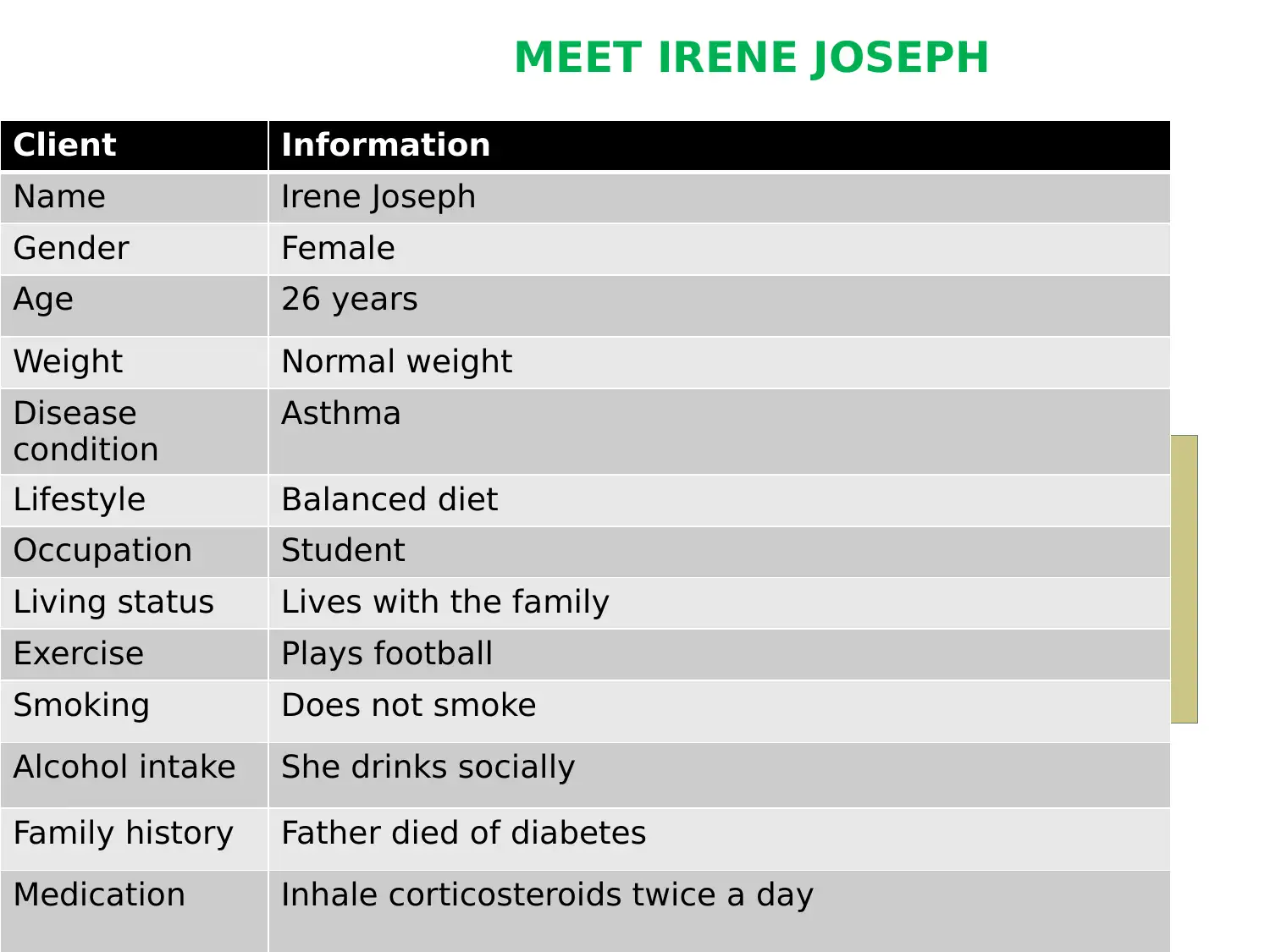
MEET IRENE JOSEPH
Client Information
Name Irene Joseph
Gender Female
Age 26 years
Weight Normal weight
Disease
condition
Asthma
Lifestyle Balanced diet
Occupation Student
Living status Lives with the family
Exercise Plays football
Smoking Does not smoke
Alcohol intake She drinks socially
Family history Father died of diabetes
Medication Inhale corticosteroids twice a day
Client Information
Name Irene Joseph
Gender Female
Age 26 years
Weight Normal weight
Disease
condition
Asthma
Lifestyle Balanced diet
Occupation Student
Living status Lives with the family
Exercise Plays football
Smoking Does not smoke
Alcohol intake She drinks socially
Family history Father died of diabetes
Medication Inhale corticosteroids twice a day
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
TWO MAJOR PATHOLOGICAL CHANGES THAT
OCCUR IN THE RESPIRATORY TRACT DURING
AN ASTHMA ATTACK ARE:
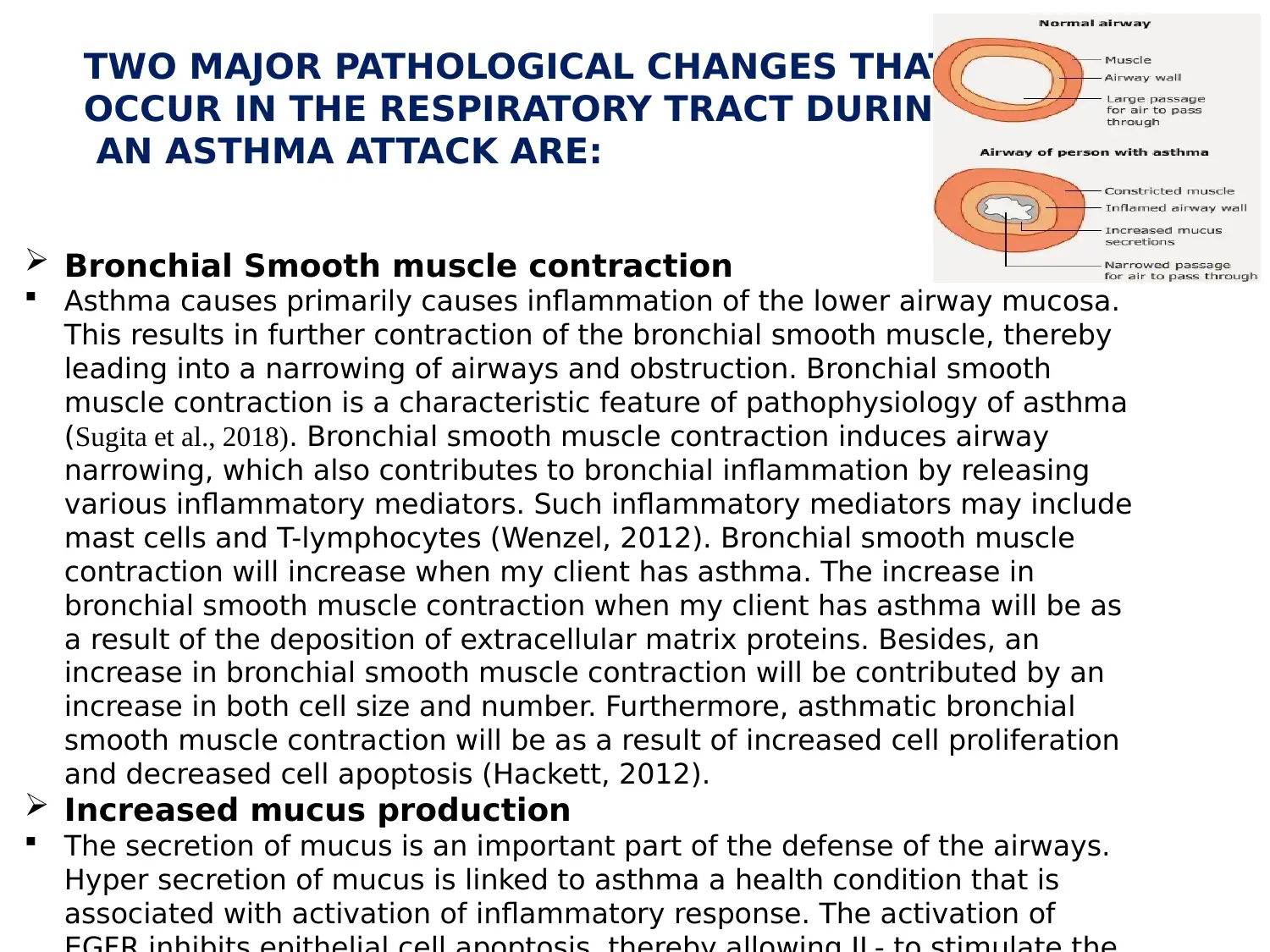
Bronchial Smooth muscle contraction
Asthma causes primarily causes inflammation of the lower airway mucosa.
This results in further contraction of the bronchial smooth muscle, thereby
leading into a narrowing of airways and obstruction. Bronchial smooth
muscle contraction is a characteristic feature of pathophysiology of asthma
(Sugita et al., 2018). Bronchial smooth muscle contraction induces airway
narrowing, which also contributes to bronchial inflammation by releasing
various inflammatory mediators. Such inflammatory mediators may include
mast cells and T-lymphocytes (Wenzel, 2012). Bronchial smooth muscle
contraction will increase when my client has asthma. The increase in
bronchial smooth muscle contraction when my client has asthma will be as
a result of the deposition of extracellular matrix proteins. Besides, an
increase in bronchial smooth muscle contraction will be contributed by an
increase in both cell size and number. Furthermore, asthmatic bronchial
smooth muscle contraction will be as a result of increased cell proliferation
and decreased cell apoptosis (Hackett, 2012).
Increased mucus production
The secretion of mucus is an important part of the defense of the airways.
Hyper secretion of mucus is linked to asthma a health condition that is
associated with activation of inflammatory response. The activation of
OCCUR IN THE RESPIRATORY TRACT DURING
AN ASTHMA ATTACK ARE:
Bronchial Smooth muscle contraction
Asthma causes primarily causes inflammation of the lower airway mucosa.
This results in further contraction of the bronchial smooth muscle, thereby
leading into a narrowing of airways and obstruction. Bronchial smooth
muscle contraction is a characteristic feature of pathophysiology of asthma
(Sugita et al., 2018). Bronchial smooth muscle contraction induces airway
narrowing, which also contributes to bronchial inflammation by releasing
various inflammatory mediators. Such inflammatory mediators may include
mast cells and T-lymphocytes (Wenzel, 2012). Bronchial smooth muscle
contraction will increase when my client has asthma. The increase in
bronchial smooth muscle contraction when my client has asthma will be as
a result of the deposition of extracellular matrix proteins. Besides, an
increase in bronchial smooth muscle contraction will be contributed by an
increase in both cell size and number. Furthermore, asthmatic bronchial
smooth muscle contraction will be as a result of increased cell proliferation
and decreased cell apoptosis (Hackett, 2012).
Increased mucus production
The secretion of mucus is an important part of the defense of the airways.
Hyper secretion of mucus is linked to asthma a health condition that is
associated with activation of inflammatory response. The activation of
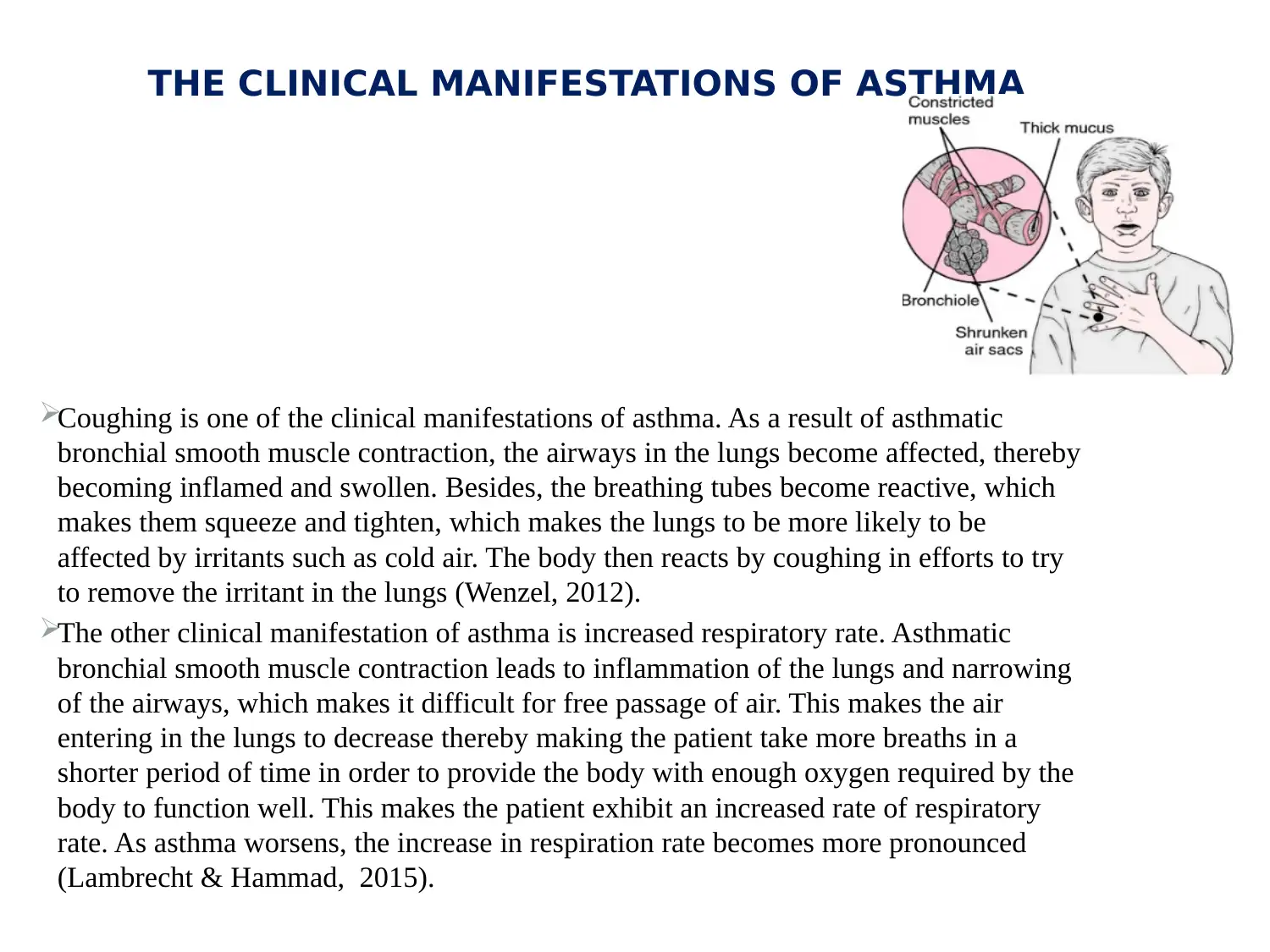
THE CLINICAL MANIFESTATIONS OF ASTHMA
Coughing is one of the clinical manifestations of asthma. As a result of asthmatic
bronchial smooth muscle contraction, the airways in the lungs become affected, thereby
becoming inflamed and swollen. Besides, the breathing tubes become reactive, which
makes them squeeze and tighten, which makes the lungs to be more likely to be
affected by irritants such as cold air. The body then reacts by coughing in efforts to try
to remove the irritant in the lungs (Wenzel, 2012).
The other clinical manifestation of asthma is increased respiratory rate. Asthmatic
bronchial smooth muscle contraction leads to inflammation of the lungs and narrowing
of the airways, which makes it difficult for free passage of air. This makes the air
entering in the lungs to decrease thereby making the patient take more breaths in a
shorter period of time in order to provide the body with enough oxygen required by the
body to function well. This makes the patient exhibit an increased rate of respiratory
rate. As asthma worsens, the increase in respiration rate becomes more pronounced
(Lambrecht & Hammad, 2015).
Coughing is one of the clinical manifestations of asthma. As a result of asthmatic
bronchial smooth muscle contraction, the airways in the lungs become affected, thereby
becoming inflamed and swollen. Besides, the breathing tubes become reactive, which
makes them squeeze and tighten, which makes the lungs to be more likely to be
affected by irritants such as cold air. The body then reacts by coughing in efforts to try
to remove the irritant in the lungs (Wenzel, 2012).
The other clinical manifestation of asthma is increased respiratory rate. Asthmatic
bronchial smooth muscle contraction leads to inflammation of the lungs and narrowing
of the airways, which makes it difficult for free passage of air. This makes the air
entering in the lungs to decrease thereby making the patient take more breaths in a
shorter period of time in order to provide the body with enough oxygen required by the
body to function well. This makes the patient exhibit an increased rate of respiratory
rate. As asthma worsens, the increase in respiration rate becomes more pronounced
(Lambrecht & Hammad, 2015).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Inhaled corticosteroid medication will be appropriate for the patient. The medication
is considered to be the most effective drug in controlling asthma when regularly used.
It cures asthma by continuously reducing the swelling and inflammation of the
airways. With the use of inhaling corticosteroids, it will only take a week to reduce the
inflammation in airways. Corticosteroids are highly considered as it can better manage
asthma besides relieving some of the symptoms of asthma (Ernst & Suissa, 2012).
Its mechanism involves suppressing the airway inflammation and bronchial smooth
muscle contraction. The medication exerts its effects on the airway vasculature via
genomic and nongenomic processes. The genomic mechanism involves controlling the
target genes and inhibiting most of the vascular components of inflammation as well
as angiogenesis that are found in the airway. Also, nongenomic action involves the
mediation by rapid cellular processes and induction of the transient vasoconstriction in
the airway, which leads to the reversing of hyper inflammatory perfusion (Gelb,
Christenson & Nadel, 2016).
INHALED CORTICOSTEROIDS IN TREATMENT OF ASTHMA
is considered to be the most effective drug in controlling asthma when regularly used.
It cures asthma by continuously reducing the swelling and inflammation of the
airways. With the use of inhaling corticosteroids, it will only take a week to reduce the
inflammation in airways. Corticosteroids are highly considered as it can better manage
asthma besides relieving some of the symptoms of asthma (Ernst & Suissa, 2012).
Its mechanism involves suppressing the airway inflammation and bronchial smooth
muscle contraction. The medication exerts its effects on the airway vasculature via
genomic and nongenomic processes. The genomic mechanism involves controlling the
target genes and inhibiting most of the vascular components of inflammation as well
as angiogenesis that are found in the airway. Also, nongenomic action involves the
mediation by rapid cellular processes and induction of the transient vasoconstriction in
the airway, which leads to the reversing of hyper inflammatory perfusion (Gelb,
Christenson & Nadel, 2016).
INHALED CORTICOSTEROIDS IN TREATMENT OF ASTHMA
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
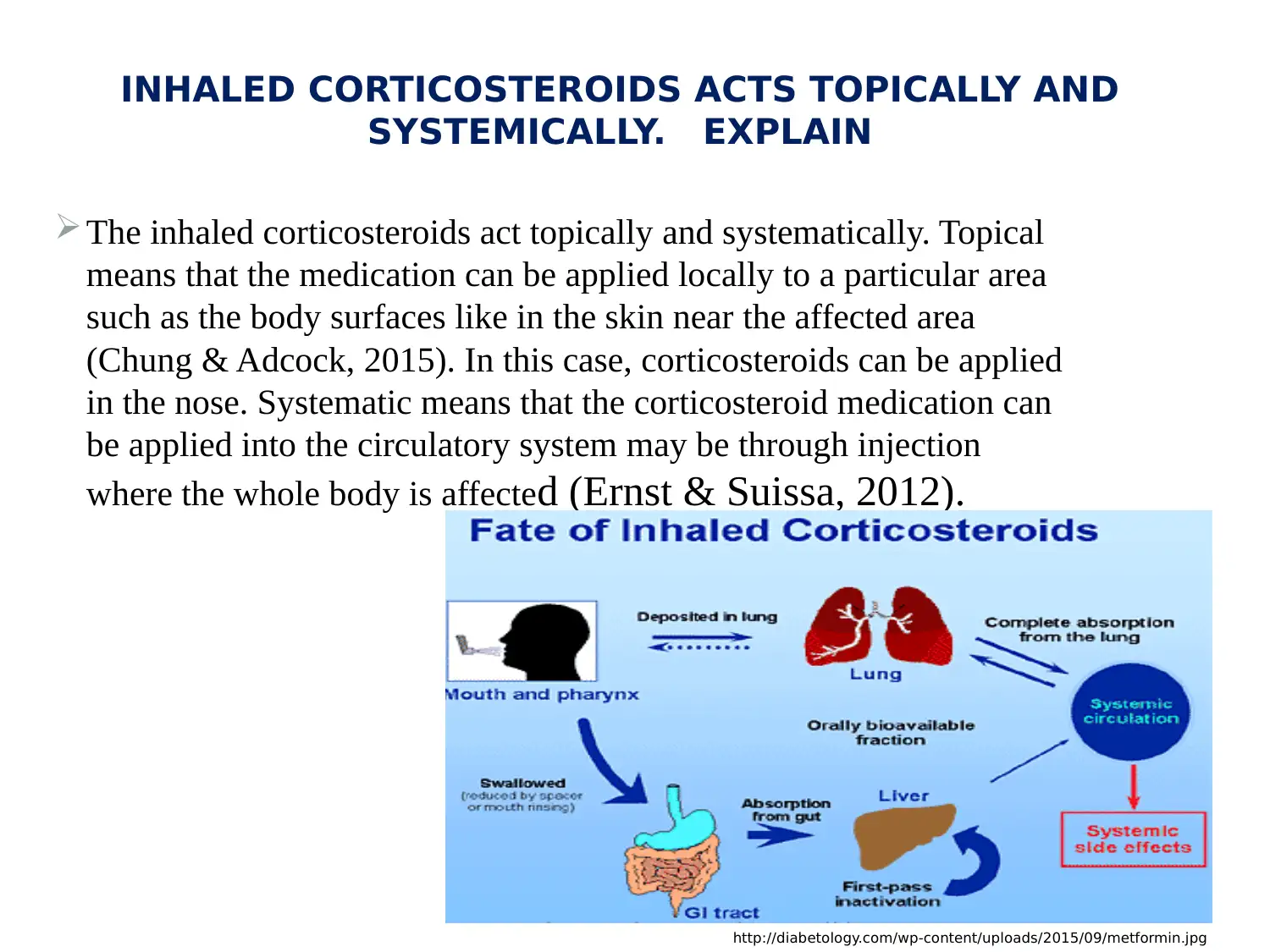
INHALED CORTICOSTEROIDS ACTS TOPICALLY AND
SYSTEMICALLY. EXPLAIN
The inhaled corticosteroids act topically and systematically. Topical
means that the medication can be applied locally to a particular area
such as the body surfaces like in the skin near the affected area
(Chung & Adcock, 2015). In this case, corticosteroids can be applied
in the nose. Systematic means that the corticosteroid medication can
be applied into the circulatory system may be through injection
where the whole body is affected (Ernst & Suissa, 2012).
http://diabetology.com/wp-content/uploads/2015/09/metformin.jpg
SYSTEMICALLY. EXPLAIN
The inhaled corticosteroids act topically and systematically. Topical
means that the medication can be applied locally to a particular area
such as the body surfaces like in the skin near the affected area
(Chung & Adcock, 2015). In this case, corticosteroids can be applied
in the nose. Systematic means that the corticosteroid medication can
be applied into the circulatory system may be through injection
where the whole body is affected (Ernst & Suissa, 2012).
http://diabetology.com/wp-content/uploads/2015/09/metformin.jpg
EDUCATIONAL ON ADMINISTRATION OF
CORTICOSTEROIDS
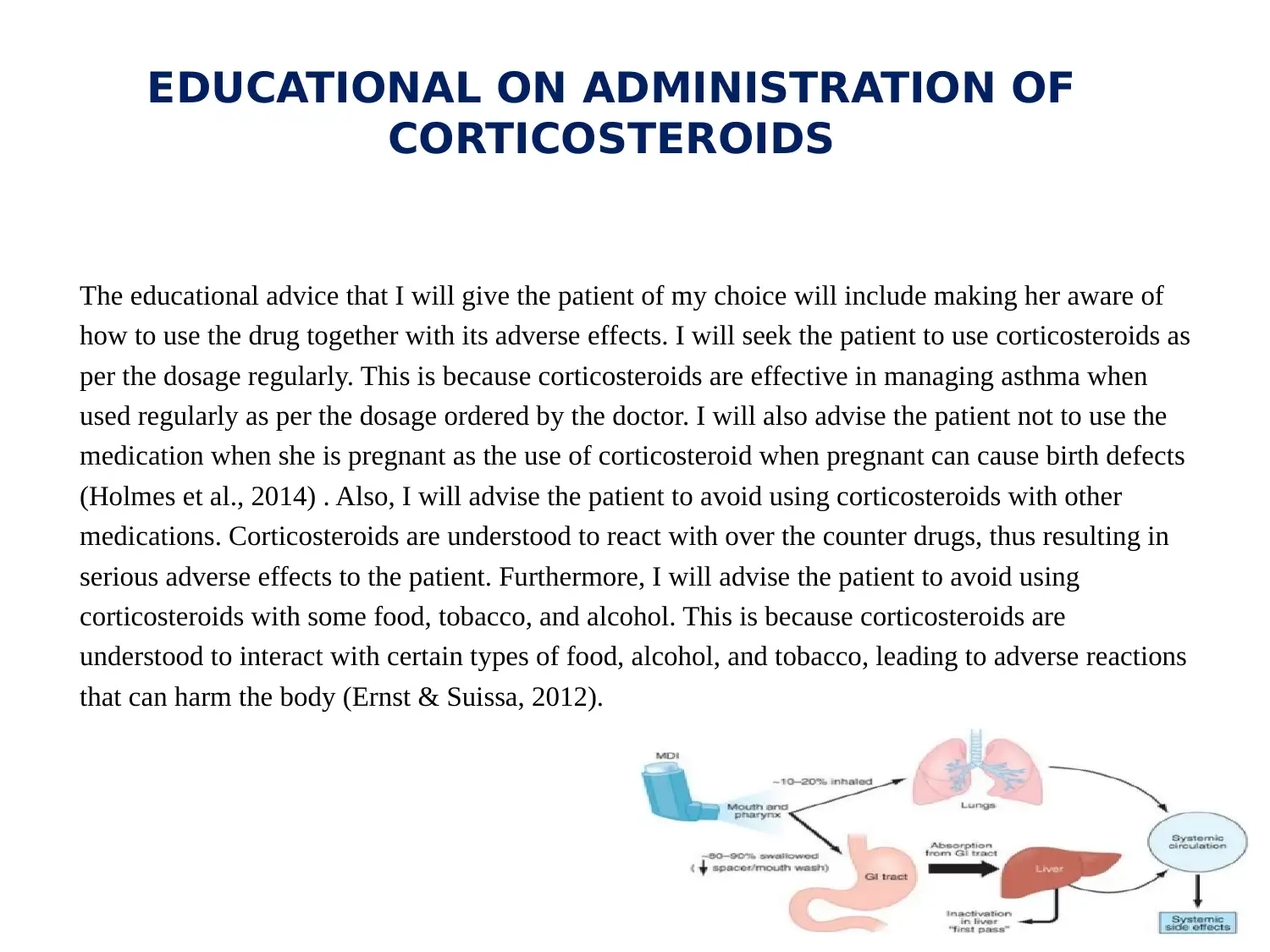
The educational advice that I will give the patient of my choice will include making her aware of
how to use the drug together with its adverse effects. I will seek the patient to use corticosteroids as
per the dosage regularly. This is because corticosteroids are effective in managing asthma when
used regularly as per the dosage ordered by the doctor. I will also advise the patient not to use the
medication when she is pregnant as the use of corticosteroid when pregnant can cause birth defects
(Holmes et al., 2014) . Also, I will advise the patient to avoid using corticosteroids with other
medications. Corticosteroids are understood to react with over the counter drugs, thus resulting in
serious adverse effects to the patient. Furthermore, I will advise the patient to avoid using
corticosteroids with some food, tobacco, and alcohol. This is because corticosteroids are
understood to interact with certain types of food, alcohol, and tobacco, leading to adverse reactions
that can harm the body (Ernst & Suissa, 2012).
CORTICOSTEROIDS
The educational advice that I will give the patient of my choice will include making her aware of
how to use the drug together with its adverse effects. I will seek the patient to use corticosteroids as
per the dosage regularly. This is because corticosteroids are effective in managing asthma when
used regularly as per the dosage ordered by the doctor. I will also advise the patient not to use the
medication when she is pregnant as the use of corticosteroid when pregnant can cause birth defects
(Holmes et al., 2014) . Also, I will advise the patient to avoid using corticosteroids with other
medications. Corticosteroids are understood to react with over the counter drugs, thus resulting in
serious adverse effects to the patient. Furthermore, I will advise the patient to avoid using
corticosteroids with some food, tobacco, and alcohol. This is because corticosteroids are
understood to interact with certain types of food, alcohol, and tobacco, leading to adverse reactions
that can harm the body (Ernst & Suissa, 2012).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
ANNOTATED BIBLIOGRAPHY
• Chung, K. F., & Adcock, I. M. (2015). Clinical phenotypes of asthma should link up with disease mechanisms. Current opinion in
allergy and clinical immunology, 15(1), 56-62.
(I used this article to determine the pathophysiology of asthma. It is a reliable source as it is peer reviewed).
• Ernst, P., & Suissa, S. (2012). Systemic effects of inhaled corticosteroids. Current opinion in pulmonary medicine, 18(1), 85-89.
(I used this article to determine the systemic effects of inhaled corticosteroids. It is a reliable source as it is peer reviewed).
Gelb, A. F., Christenson, S. A., & Nadel, J. A. (2016). Understanding the pathophysiology of the asthma–chronic obstructive
pulmonary disease overlap syndrome. Current opinion in pulmonary medicine, 22(2), 100-105.
(I used this article to examine the pathophysiology of asthma. It is a reliable source as it is peer reviewed).
• Hackett, T. L. (2012). Epithelial–mesenchymal transition in the pathophysiology of airway remodelling in asthma. Current
opinion in allergy and clinical immunology, 12(1), 53-59.
(I used this article to determine the pathophysiology of asthma. Epithelial–mesenchymal transition in the pathophysiology of airway
remodelling in asthma . It is a reliable source as it is peer reviewed).
Holmes, M. S., D'arcy, S., Costello, R. W., & Reilly, R. B. (2014). Acoustic analysis of inhaler sounds from community-dwelling
asthmatic patients for automatic assessment of adherence. IEEE journal of translational engineering in health and medicine, 2, 1-
10.
(I used this article to determine the mechanisms of inhaled corticosteroids in management of asthma)
• Lambrecht, B. N., & Hammad, H. (2015). The immunology of asthma. Nature immunology, 16(1), 45.
• (I used this article to determine the immunology of asthma. It is a reliable source as it is a peer reviewed)
Sugita, K., Steer, C. A., Martinez-Gonzalez, I., Altunbulakli, C., Morita, H., Castro-Giner, F., ... & Nakae, S. (2018). Type 2 innate
lymphoid cells disrupt bronchial epithelial barrier integrity by targeting tight junctions through IL-13 in asthmatic patients. Journal
of Allergy and Clinical Immunology, 141(1), 300-310.
• (I used this article to determine the pathophysiology of asthma. It is a reliable source as it is peer reviewe)d.
Wenzel, S. E. (2012). Asthma phenotypes: the evolution from clinical to molecular approaches. Nature medicine, 18(5), 716.
• I used this article to determine the clinical manifestation of asthma. It is a reliable source as it is peer reviewed.
• Chung, K. F., & Adcock, I. M. (2015). Clinical phenotypes of asthma should link up with disease mechanisms. Current opinion in
allergy and clinical immunology, 15(1), 56-62.
(I used this article to determine the pathophysiology of asthma. It is a reliable source as it is peer reviewed).
• Ernst, P., & Suissa, S. (2012). Systemic effects of inhaled corticosteroids. Current opinion in pulmonary medicine, 18(1), 85-89.
(I used this article to determine the systemic effects of inhaled corticosteroids. It is a reliable source as it is peer reviewed).
Gelb, A. F., Christenson, S. A., & Nadel, J. A. (2016). Understanding the pathophysiology of the asthma–chronic obstructive
pulmonary disease overlap syndrome. Current opinion in pulmonary medicine, 22(2), 100-105.
(I used this article to examine the pathophysiology of asthma. It is a reliable source as it is peer reviewed).
• Hackett, T. L. (2012). Epithelial–mesenchymal transition in the pathophysiology of airway remodelling in asthma. Current
opinion in allergy and clinical immunology, 12(1), 53-59.
(I used this article to determine the pathophysiology of asthma. Epithelial–mesenchymal transition in the pathophysiology of airway
remodelling in asthma . It is a reliable source as it is peer reviewed).
Holmes, M. S., D'arcy, S., Costello, R. W., & Reilly, R. B. (2014). Acoustic analysis of inhaler sounds from community-dwelling
asthmatic patients for automatic assessment of adherence. IEEE journal of translational engineering in health and medicine, 2, 1-
10.
(I used this article to determine the mechanisms of inhaled corticosteroids in management of asthma)
• Lambrecht, B. N., & Hammad, H. (2015). The immunology of asthma. Nature immunology, 16(1), 45.
• (I used this article to determine the immunology of asthma. It is a reliable source as it is a peer reviewed)
Sugita, K., Steer, C. A., Martinez-Gonzalez, I., Altunbulakli, C., Morita, H., Castro-Giner, F., ... & Nakae, S. (2018). Type 2 innate
lymphoid cells disrupt bronchial epithelial barrier integrity by targeting tight junctions through IL-13 in asthmatic patients. Journal
of Allergy and Clinical Immunology, 141(1), 300-310.
• (I used this article to determine the pathophysiology of asthma. It is a reliable source as it is peer reviewe)d.
Wenzel, S. E. (2012). Asthma phenotypes: the evolution from clinical to molecular approaches. Nature medicine, 18(5), 716.
• I used this article to determine the clinical manifestation of asthma. It is a reliable source as it is peer reviewed.
1 out of 7
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





