Nursing Mental Health: Consumer Assessment and Intervention Report
VerifiedAdded on 2023/06/04
|6
|1384
|331
Report
AI Summary
This document presents a mental health consumer assessment report focusing on an 18-year-old male named Harry. The report details Harry's mental state examination, noting observations about his appearance, behavior, speech, mood, thought processes, and perceptions, including delusions and hallucinations. It outlines suggested nursing interventions for thought disorders, insomnia, and anxiety, emphasizing the importance of tailored care and coping mechanisms. Furthermore, the report provides a nursing summary, highlighting key symptoms, potential risks, and strategies for managing Harry's condition, underscoring the need for close monitoring and patient education. The document concludes with a list of references used in the assessment and proposed interventions. Desklib provides access to this and similar solved assignments.
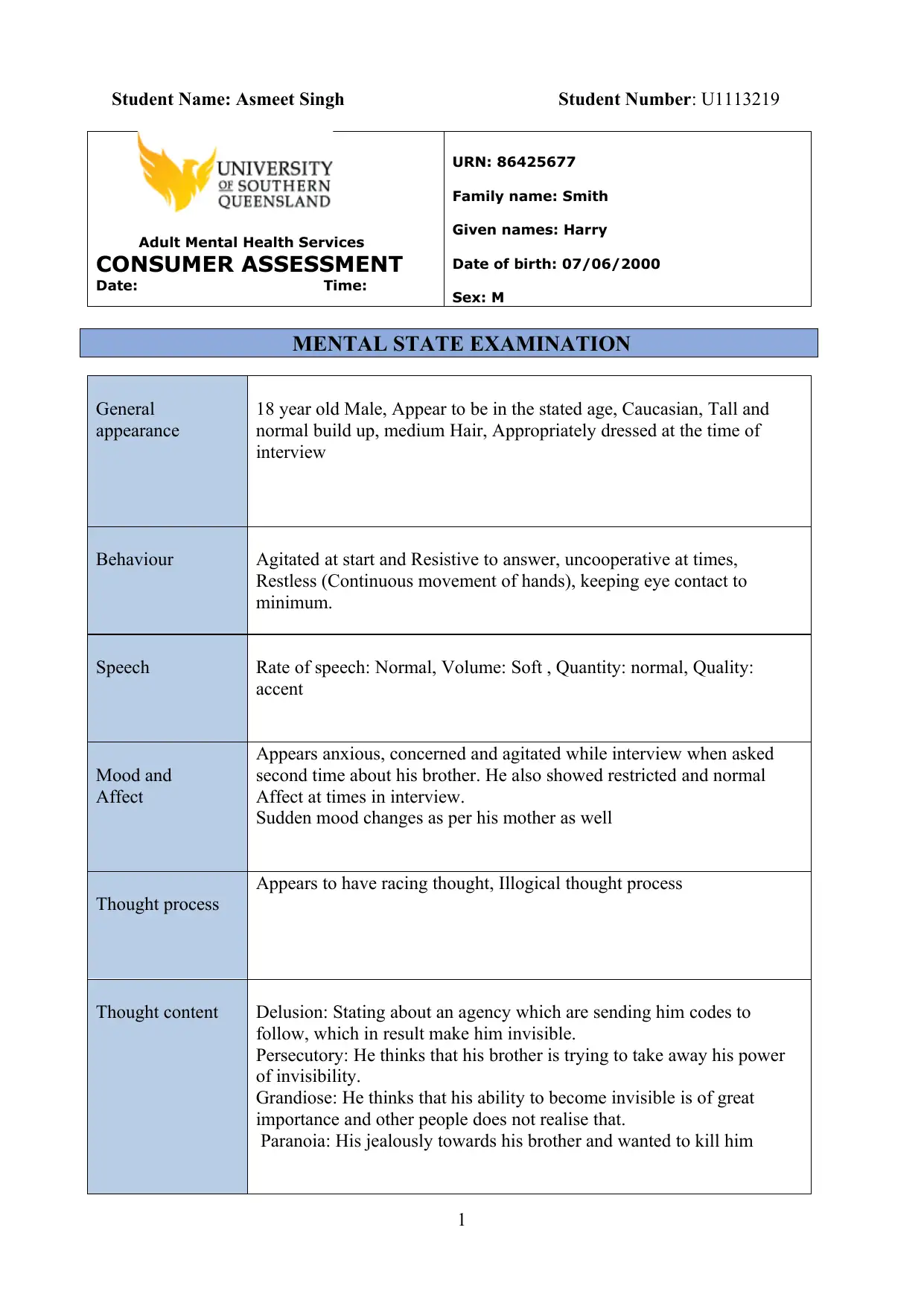
Student Name: Asmeet Singh Student Number: U1113219
Adult Mental Health Services
CONSUMER ASSESSMENT
Date: Time:
URN: 86425677
Family name: Smith
Given names: Harry
Date of birth: 07/06/2000
Sex: M
MENTAL STATE EXAMINATION
General
appearance
18 year old Male, Appear to be in the stated age, Caucasian, Tall and
normal build up, medium Hair, Appropriately dressed at the time of
interview
Behaviour Agitated at start and Resistive to answer, uncooperative at times,
Restless (Continuous movement of hands), keeping eye contact to
minimum.
Speech Rate of speech: Normal, Volume: Soft , Quantity: normal, Quality:
accent
Mood and
Affect
Appears anxious, concerned and agitated while interview when asked
second time about his brother. He also showed restricted and normal
Affect at times in interview.
Sudden mood changes as per his mother as well
Thought process
Appears to have racing thought, Illogical thought process
Thought content Delusion: Stating about an agency which are sending him codes to
follow, which in result make him invisible.
Persecutory: He thinks that his brother is trying to take away his power
of invisibility.
Grandiose: He thinks that his ability to become invisible is of great
importance and other people does not realise that.
Paranoia: His jealously towards his brother and wanted to kill him
1
Adult Mental Health Services
CONSUMER ASSESSMENT
Date: Time:
URN: 86425677
Family name: Smith
Given names: Harry
Date of birth: 07/06/2000
Sex: M
MENTAL STATE EXAMINATION
General
appearance
18 year old Male, Appear to be in the stated age, Caucasian, Tall and
normal build up, medium Hair, Appropriately dressed at the time of
interview
Behaviour Agitated at start and Resistive to answer, uncooperative at times,
Restless (Continuous movement of hands), keeping eye contact to
minimum.
Speech Rate of speech: Normal, Volume: Soft , Quantity: normal, Quality:
accent
Mood and
Affect
Appears anxious, concerned and agitated while interview when asked
second time about his brother. He also showed restricted and normal
Affect at times in interview.
Sudden mood changes as per his mother as well
Thought process
Appears to have racing thought, Illogical thought process
Thought content Delusion: Stating about an agency which are sending him codes to
follow, which in result make him invisible.
Persecutory: He thinks that his brother is trying to take away his power
of invisibility.
Grandiose: He thinks that his ability to become invisible is of great
importance and other people does not realise that.
Paranoia: His jealously towards his brother and wanted to kill him
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
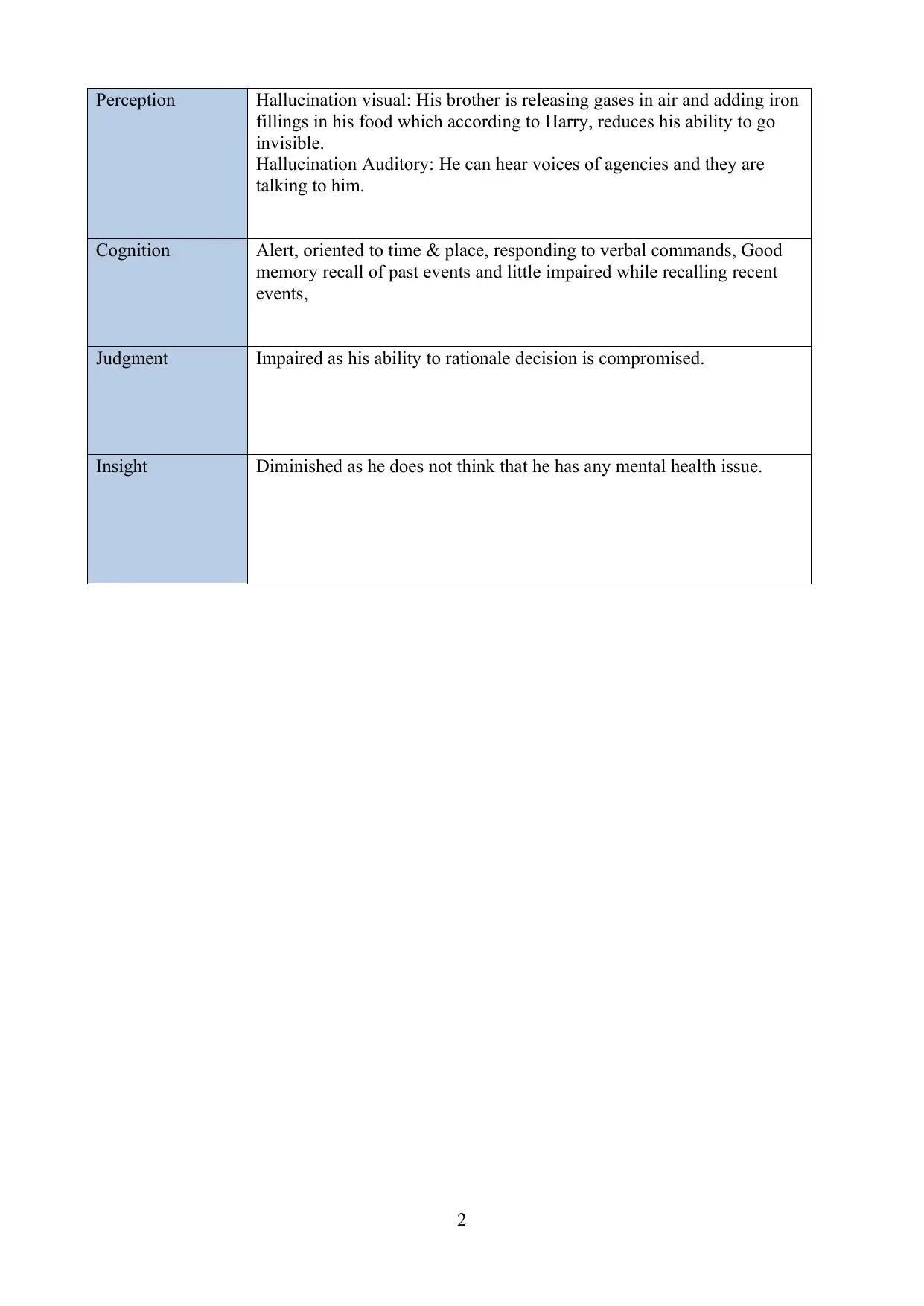
Perception Hallucination visual: His brother is releasing gases in air and adding iron
fillings in his food which according to Harry, reduces his ability to go
invisible.
Hallucination Auditory: He can hear voices of agencies and they are
talking to him.
Cognition Alert, oriented to time & place, responding to verbal commands, Good
memory recall of past events and little impaired while recalling recent
events,
Judgment Impaired as his ability to rationale decision is compromised.
Insight Diminished as he does not think that he has any mental health issue.
2
fillings in his food which according to Harry, reduces his ability to go
invisible.
Hallucination Auditory: He can hear voices of agencies and they are
talking to him.
Cognition Alert, oriented to time & place, responding to verbal commands, Good
memory recall of past events and little impaired while recalling recent
events,
Judgment Impaired as his ability to rationale decision is compromised.
Insight Diminished as he does not think that he has any mental health issue.
2
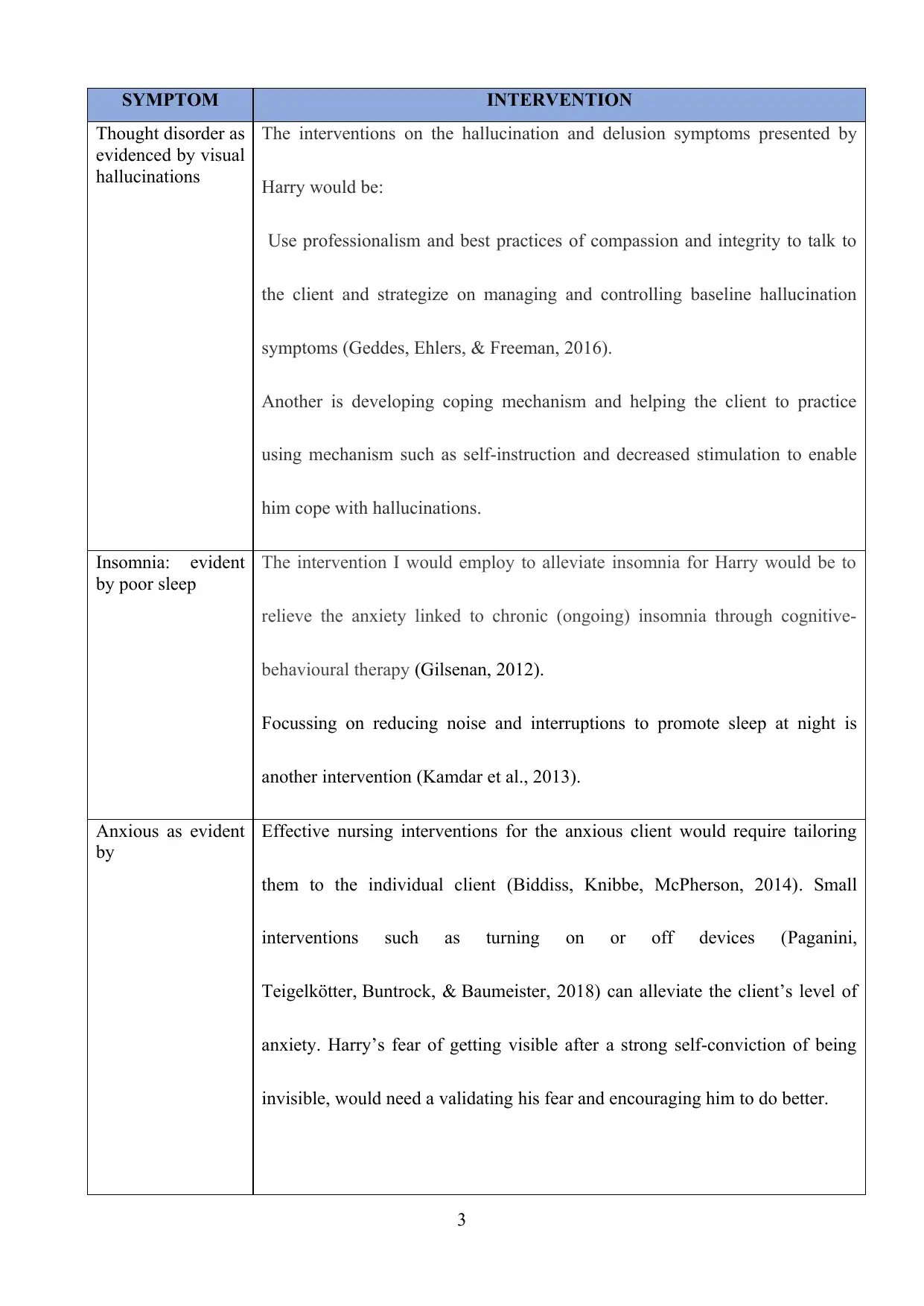
SYMPTOM INTERVENTION
Thought disorder as
evidenced by visual
hallucinations
The interventions on the hallucination and delusion symptoms presented by
Harry would be:
Use professionalism and best practices of compassion and integrity to talk to
the client and strategize on managing and controlling baseline hallucination
symptoms (Geddes, Ehlers, & Freeman, 2016).
Another is developing coping mechanism and helping the client to practice
using mechanism such as self-instruction and decreased stimulation to enable
him cope with hallucinations.
Insomnia: evident
by poor sleep
The intervention I would employ to alleviate insomnia for Harry would be to
relieve the anxiety linked to chronic (ongoing) insomnia through cognitive-
behavioural therapy (Gilsenan, 2012).
Focussing on reducing noise and interruptions to promote sleep at night is
another intervention (Kamdar et al., 2013).
Anxious as evident
by
Effective nursing interventions for the anxious client would require tailoring
them to the individual client (Biddiss, Knibbe, McPherson, 2014). Small
interventions such as turning on or off devices (Paganini,
Teigelkötter, Buntrock, & Baumeister, 2018) can alleviate the client’s level of
anxiety. Harry’s fear of getting visible after a strong self-conviction of being
invisible, would need a validating his fear and encouraging him to do better.
3
Thought disorder as
evidenced by visual
hallucinations
The interventions on the hallucination and delusion symptoms presented by
Harry would be:
Use professionalism and best practices of compassion and integrity to talk to
the client and strategize on managing and controlling baseline hallucination
symptoms (Geddes, Ehlers, & Freeman, 2016).
Another is developing coping mechanism and helping the client to practice
using mechanism such as self-instruction and decreased stimulation to enable
him cope with hallucinations.
Insomnia: evident
by poor sleep
The intervention I would employ to alleviate insomnia for Harry would be to
relieve the anxiety linked to chronic (ongoing) insomnia through cognitive-
behavioural therapy (Gilsenan, 2012).
Focussing on reducing noise and interruptions to promote sleep at night is
another intervention (Kamdar et al., 2013).
Anxious as evident
by
Effective nursing interventions for the anxious client would require tailoring
them to the individual client (Biddiss, Knibbe, McPherson, 2014). Small
interventions such as turning on or off devices (Paganini,
Teigelkötter, Buntrock, & Baumeister, 2018) can alleviate the client’s level of
anxiety. Harry’s fear of getting visible after a strong self-conviction of being
invisible, would need a validating his fear and encouraging him to do better.
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

NURSING REPORT
A nurse report for Harry will ensuring flow of information to other care team responsible for
the client when my shift ends .Safe report in mental health case client ensures patient safety
as inadequate reporting lead to medication errors .The synthesized report for the case would
be as follow: Harry is 18 years old male whose symptoms on admission are delusion,
hallucination and presents anxiety. He has a racing thought with illogical thought process.
He is anxious and agitated moods with some restricted affect. He is biologically vulnerable to
his mother’s mood changes. He is paranoiac and persecutory hence need close monitoring as
he poses risk of harm to others notably his brother. He seems isolated and spiteful. Insomnia
and loss of appetite has been reported thus monitoring his sleep patterns and eating habits
will help alleviate the problem. He has diminished insight of his own mental state with
impaired judgement. His physical health is good with history of low adherence to medication.
His protective strategy is being alert as he think of his brother harming and rendering him
invisible hence will kill him. His coping strategies are good physical health and good level of
consciousness. He speaks well hence can be talked to validate his fear of being visible. He
has illogical reasoning hence the client can be educated can be alleviated the incorrect
thoughts through educating the client on the mental health disorder he is experiencing and the
appropriate care process required to empower him to be actively involved in his care.
4
A nurse report for Harry will ensuring flow of information to other care team responsible for
the client when my shift ends .Safe report in mental health case client ensures patient safety
as inadequate reporting lead to medication errors .The synthesized report for the case would
be as follow: Harry is 18 years old male whose symptoms on admission are delusion,
hallucination and presents anxiety. He has a racing thought with illogical thought process.
He is anxious and agitated moods with some restricted affect. He is biologically vulnerable to
his mother’s mood changes. He is paranoiac and persecutory hence need close monitoring as
he poses risk of harm to others notably his brother. He seems isolated and spiteful. Insomnia
and loss of appetite has been reported thus monitoring his sleep patterns and eating habits
will help alleviate the problem. He has diminished insight of his own mental state with
impaired judgement. His physical health is good with history of low adherence to medication.
His protective strategy is being alert as he think of his brother harming and rendering him
invisible hence will kill him. His coping strategies are good physical health and good level of
consciousness. He speaks well hence can be talked to validate his fear of being visible. He
has illogical reasoning hence the client can be educated can be alleviated the incorrect
thoughts through educating the client on the mental health disorder he is experiencing and the
appropriate care process required to empower him to be actively involved in his care.
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
References
Biddiss,E., Knibbe, T.J., McPherson, A.(2014) .The effectiveness of interventions aimed at
reducing anxiety in health care waiting spaces: a systematic review of randomized and
nonrandomized trials. Anesth Analg, 119(2), 433-48. doi:
10.1213/ANE.0000000000000294.
Geddes, G., Ehlers, A., & Freeman, D. (2016). Hallucinations in the months after a trauma:
An investigation of the role of cognitive processing of a physical assault in the
occurrence of hallucinatory experiences. Psychiatry Research, 246, 601–605.
http://doi.org/10.1016/j.psychres.2016.10.081
Gilsenan, I. (2012) .Nursing interventions to alleviate insomnia.
Nurse Older People, 24(4), 8-14.
Jason, W., Siefferman, Emerald, L., Jeffrey, S.F., (2012).Patient Safety at Handoff in
Rehabilitation Medicine.PubMed, 23(2), 241-257.doi:10.1016/j.pmr.2012.02.003
Publishers, LLC, 2010.
Kamdar, B.B., Yang, J., King, L. M., Neufeld, K. J., Bienvenu, O. J., Rowden, A. M.,
Brower, R. G., Collop, N. A., Needham, D. M. (2013). Developing, implementing,
and evaluating a multifaceted quality improvement intervention to promote sleep in
an icu. American Journal of Medical Quality, 29(6),546-554.
doi:10.1177/1062860613509684
Lie, J. D., Tu, K. N., Shen, D. D., & Wong, B. M. (2015). Pharmacological Treatment of
Insomnia. Pharmacy and Therapeutics, 40(11), 759–771.
5
Biddiss,E., Knibbe, T.J., McPherson, A.(2014) .The effectiveness of interventions aimed at
reducing anxiety in health care waiting spaces: a systematic review of randomized and
nonrandomized trials. Anesth Analg, 119(2), 433-48. doi:
10.1213/ANE.0000000000000294.
Geddes, G., Ehlers, A., & Freeman, D. (2016). Hallucinations in the months after a trauma:
An investigation of the role of cognitive processing of a physical assault in the
occurrence of hallucinatory experiences. Psychiatry Research, 246, 601–605.
http://doi.org/10.1016/j.psychres.2016.10.081
Gilsenan, I. (2012) .Nursing interventions to alleviate insomnia.
Nurse Older People, 24(4), 8-14.
Jason, W., Siefferman, Emerald, L., Jeffrey, S.F., (2012).Patient Safety at Handoff in
Rehabilitation Medicine.PubMed, 23(2), 241-257.doi:10.1016/j.pmr.2012.02.003
Publishers, LLC, 2010.
Kamdar, B.B., Yang, J., King, L. M., Neufeld, K. J., Bienvenu, O. J., Rowden, A. M.,
Brower, R. G., Collop, N. A., Needham, D. M. (2013). Developing, implementing,
and evaluating a multifaceted quality improvement intervention to promote sleep in
an icu. American Journal of Medical Quality, 29(6),546-554.
doi:10.1177/1062860613509684
Lie, J. D., Tu, K. N., Shen, D. D., & Wong, B. M. (2015). Pharmacological Treatment of
Insomnia. Pharmacy and Therapeutics, 40(11), 759–771.
5
Malla, A. (2015).Mental illness is like any other medical illness: A critical examination of the
statement and its impact on patients care and society. Journal of Psychiatry and
Neuroscience, 40(3), 147-150.doi:http://ispub.com/ljANP/1011/7218
Manias, E., Gerdtz, M., Williams, A., & Dooley, M. (2014). Complexities of medicines
safety: communicating about managing medicines at transition points of care across
emergency departments and medical wards. Journal of Clinical Nursing, 24, 69-80.
Paganini, S., Teigelkötter, W., Buntrock, C. & Baumeister,H.(2018). Economic evaluations
of internet- and mobile-based interventions for the treatment and prevention of
depression: A systematic review, Journal of Affective Disorders, 225,733-755.
Wang, P., & Si, T. (2013). Use of antipsychotics in the treatment of depressive
disorders. Shanghai Archives of Psychiatry, 25(3), 134–140.
http://doi.org/10.3969/j.issn.1002-0829.2013.03.002
Wilson, L., Crowe, M., Scott, A. and Lacey, C. (2018). Psychoeducation for bipolar
disorder: A discourse analysis. International Journal of Mental Health Nursing, 27,
349-357. doi:10.1111/inm.12328
Maren, S., & Holmes, A. (2016). Stress and Fear
Extinction. Neuropsychopharmacology, 41(1), 58–79.
http://doi.org/10.1038/npp.2015.180
6
statement and its impact on patients care and society. Journal of Psychiatry and
Neuroscience, 40(3), 147-150.doi:http://ispub.com/ljANP/1011/7218
Manias, E., Gerdtz, M., Williams, A., & Dooley, M. (2014). Complexities of medicines
safety: communicating about managing medicines at transition points of care across
emergency departments and medical wards. Journal of Clinical Nursing, 24, 69-80.
Paganini, S., Teigelkötter, W., Buntrock, C. & Baumeister,H.(2018). Economic evaluations
of internet- and mobile-based interventions for the treatment and prevention of
depression: A systematic review, Journal of Affective Disorders, 225,733-755.
Wang, P., & Si, T. (2013). Use of antipsychotics in the treatment of depressive
disorders. Shanghai Archives of Psychiatry, 25(3), 134–140.
http://doi.org/10.3969/j.issn.1002-0829.2013.03.002
Wilson, L., Crowe, M., Scott, A. and Lacey, C. (2018). Psychoeducation for bipolar
disorder: A discourse analysis. International Journal of Mental Health Nursing, 27,
349-357. doi:10.1111/inm.12328
Maren, S., & Holmes, A. (2016). Stress and Fear
Extinction. Neuropsychopharmacology, 41(1), 58–79.
http://doi.org/10.1038/npp.2015.180
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 6
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





