Mental Health Case: Patient Examination and Therapeutic Care Plan
VerifiedAdded on 2023/06/13
|14
|2876
|284
Case Study
AI Summary
This case study presents a mental health assessment of a young Asian male experiencing auditory hallucinations and related challenges. The mental status examination covers appearance, behavior, affect, mood, speech, thought form and content, perception, cognition, and insight. Key risk factors identified include cognitive, affective, and psychomotor factors, potential sleeping disorders, and frustration related to learning disabilities. The comprehensive care plan addresses clinical issues such as hearing voices, impaired cognitive function, impaired social interaction, non-adherence to medications, and learning disabilities. Interventions include monitoring behavior, improving nutrition, social rhythm therapy, structured solitary activities, and cognitive therapies. The study also reflects on positive nurse-patient interactions and the importance of open-ended questions and non-verbal communication. The goal is to improve the patient's quality of life through therapeutic management and family support. Desklib provides a platform for students to access such solved assignments and past papers for academic assistance.

Running head: MENTAL HEALTH
MENTAL HEALTH
Name of the Student
Name of the university
Author’s note
MENTAL HEALTH
Name of the Student
Name of the university
Author’s note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1MENTAL HEALTH
Mental state examination
APPEARANCE: Young Asian black haired man. He is wearing glasses. His clothing is
appropriate for his age. Has a slim figure. He was dressed in cargo pants with red and
black flannel shirt along with glasses. Appeared disengage as his head was hung down,
arms crossed and restrictive posture. His Grooming is adequate and he was
cooperative about the examination.
BEHAVIOUR: The patient is avoiding eye contact, probably due to the sense of
insecurity or fear. He was Looking different direction, fidgeting with his fingers and
appeared uncomfortable while answering the questions, but became comfortable after
sometimes. He had a poor concentration. His eyes sometimes become fixated in the
opposite wall.
AFFECT: His affect was labile, response was stable and within the context.
MOOD: He reports that it is scary to hear the voices sometimes and he feels extremely
uncomfortable. He sometimes became distracted by the voices, while conversing with
the nurse. The curtains distracted him.
SPEECH: clients pitch was very low and not within a normal pace throughout the
conversation. Client sometimes becomes distracted with the voices and doesn’t answer
the nurse.
THOUGHT FORM: He was talking abstract in the beginning, but as the conversation
went on, his response seems logical.
Mental state examination
APPEARANCE: Young Asian black haired man. He is wearing glasses. His clothing is
appropriate for his age. Has a slim figure. He was dressed in cargo pants with red and
black flannel shirt along with glasses. Appeared disengage as his head was hung down,
arms crossed and restrictive posture. His Grooming is adequate and he was
cooperative about the examination.
BEHAVIOUR: The patient is avoiding eye contact, probably due to the sense of
insecurity or fear. He was Looking different direction, fidgeting with his fingers and
appeared uncomfortable while answering the questions, but became comfortable after
sometimes. He had a poor concentration. His eyes sometimes become fixated in the
opposite wall.
AFFECT: His affect was labile, response was stable and within the context.
MOOD: He reports that it is scary to hear the voices sometimes and he feels extremely
uncomfortable. He sometimes became distracted by the voices, while conversing with
the nurse. The curtains distracted him.
SPEECH: clients pitch was very low and not within a normal pace throughout the
conversation. Client sometimes becomes distracted with the voices and doesn’t answer
the nurse.
THOUGHT FORM: He was talking abstract in the beginning, but as the conversation
went on, his response seems logical.
2MENTAL HEALTH
THOUGHT CONTENT: He has friends but goes out on movies by himself, he has
expressed interest on calling her mom.
PERCEPTION: The boy was having auditory hallucinations and can hear voices. He
reported that the voices in the background often make fun of him for being weak in math
and criticize him. He sometimes gets distracted by the voices. He has reported he was
also suffering from sleeping disorders due to the voices as they often wake him up from
sleep.
COGNITION & INTELLECTUAL FUNCTIONING: He is alert and orientated. He knows
he is in a clinical mental health unit and knows the date, year and knows why he is in
that particular unit. Client appeared unfocused as he said that he is getting distracted by
the voices. The client confesses that he might have poor cognitive skills as he feels that
he cannot do math.
INSIGHT & JUDGEMENT (Insight- He was aware he has a problem and needs
medication as he knows that his symptoms remain in control as long as he is under
medications, But becomes anxious with the thought of going to the hospital, insight to a
degree – denial; judgment = on the self-defense question he wouldn’t harm anyone
understanding of consequences of their behaviors, hence he says that the voice does
not tell him to cause harm to others). He likes writing. He is worried about his mother.
He remembers that he in under medications.
THOUGHT CONTENT: He has friends but goes out on movies by himself, he has
expressed interest on calling her mom.
PERCEPTION: The boy was having auditory hallucinations and can hear voices. He
reported that the voices in the background often make fun of him for being weak in math
and criticize him. He sometimes gets distracted by the voices. He has reported he was
also suffering from sleeping disorders due to the voices as they often wake him up from
sleep.
COGNITION & INTELLECTUAL FUNCTIONING: He is alert and orientated. He knows
he is in a clinical mental health unit and knows the date, year and knows why he is in
that particular unit. Client appeared unfocused as he said that he is getting distracted by
the voices. The client confesses that he might have poor cognitive skills as he feels that
he cannot do math.
INSIGHT & JUDGEMENT (Insight- He was aware he has a problem and needs
medication as he knows that his symptoms remain in control as long as he is under
medications, But becomes anxious with the thought of going to the hospital, insight to a
degree – denial; judgment = on the self-defense question he wouldn’t harm anyone
understanding of consequences of their behaviors, hence he says that the voice does
not tell him to cause harm to others). He likes writing. He is worried about his mother.
He remembers that he in under medications.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3MENTAL HEALTH
Risk factors
The risk factors are the cognitive, affective and the psychomotor factors.
The voices wake him up sometimes from his sleeps that can also lead to
sleeping disorders.
Another risk factor is that the hearing voices may arise suicidal tendencies on
him as he had already told that he cannot concentrate on his studies as the
voices constantly distracts him (Hepworth et al., 2012).
Another risk factor is that the patient is weak in math and hence has developed a
sense of frustration. He has also stated that the voices do not let him to do math.
Hence the boy may also get into depression for not being able to do his studies
and he feared that he might be humiliated by his classmates. Furthermore he is
also concerned that his mother will become anxious if he comes to know
regarding his problems.
Risk factors
The risk factors are the cognitive, affective and the psychomotor factors.
The voices wake him up sometimes from his sleeps that can also lead to
sleeping disorders.
Another risk factor is that the hearing voices may arise suicidal tendencies on
him as he had already told that he cannot concentrate on his studies as the
voices constantly distracts him (Hepworth et al., 2012).
Another risk factor is that the patient is weak in math and hence has developed a
sense of frustration. He has also stated that the voices do not let him to do math.
Hence the boy may also get into depression for not being able to do his studies
and he feared that he might be humiliated by his classmates. Furthermore he is
also concerned that his mother will become anxious if he comes to know
regarding his problems.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4MENTAL HEALTH
CARE PLAN
1. CLINICAL ISSUE: Hearing voices.
RATIONALE FOR CHOSEN ISSUE: Hearing voices is a clinical issue as it is a common
type of auditory hallucination faced by the people of with psychotic disorders. The
sounds can be unusual sounds, familiar sounds and even human voices. A proper plan
of care is needed as the sounds can be extremely disturbing, pleasant or threatening.
GOAL/S: The goal is to provide a healthy life style to the patient; patient would stop
hearing voices and would be able to concentrate on his life
INTERVENTIONS -
1. To monitor the behavioral
pattern of the patient.
2. To check whether there the
voices are accompanied by the
blue coloration of the skin or
cold and clammy skin.
3. To check whether the patient
have shown any suicidal
tendencies.
RATIONALES
1. This would help the health care
professionals to evaluate the predisposing
factors behind the behavior (Thomas et
al., 2014).
2. This is because such symptoms are
often caused by the seizures and serious
brain injury (Shinn et al., 2012).
3. Auditory hallucinations can be deadly
as patients at some pint might have the
thought to finish himself for avoiding this
unnatural and strange feeling of
CARE PLAN
1. CLINICAL ISSUE: Hearing voices.
RATIONALE FOR CHOSEN ISSUE: Hearing voices is a clinical issue as it is a common
type of auditory hallucination faced by the people of with psychotic disorders. The
sounds can be unusual sounds, familiar sounds and even human voices. A proper plan
of care is needed as the sounds can be extremely disturbing, pleasant or threatening.
GOAL/S: The goal is to provide a healthy life style to the patient; patient would stop
hearing voices and would be able to concentrate on his life
INTERVENTIONS -
1. To monitor the behavioral
pattern of the patient.
2. To check whether there the
voices are accompanied by the
blue coloration of the skin or
cold and clammy skin.
3. To check whether the patient
have shown any suicidal
tendencies.
RATIONALES
1. This would help the health care
professionals to evaluate the predisposing
factors behind the behavior (Thomas et
al., 2014).
2. This is because such symptoms are
often caused by the seizures and serious
brain injury (Shinn et al., 2012).
3. Auditory hallucinations can be deadly
as patients at some pint might have the
thought to finish himself for avoiding this
unnatural and strange feeling of
5MENTAL HEALTH
background voices (Thomas et al., 2014).
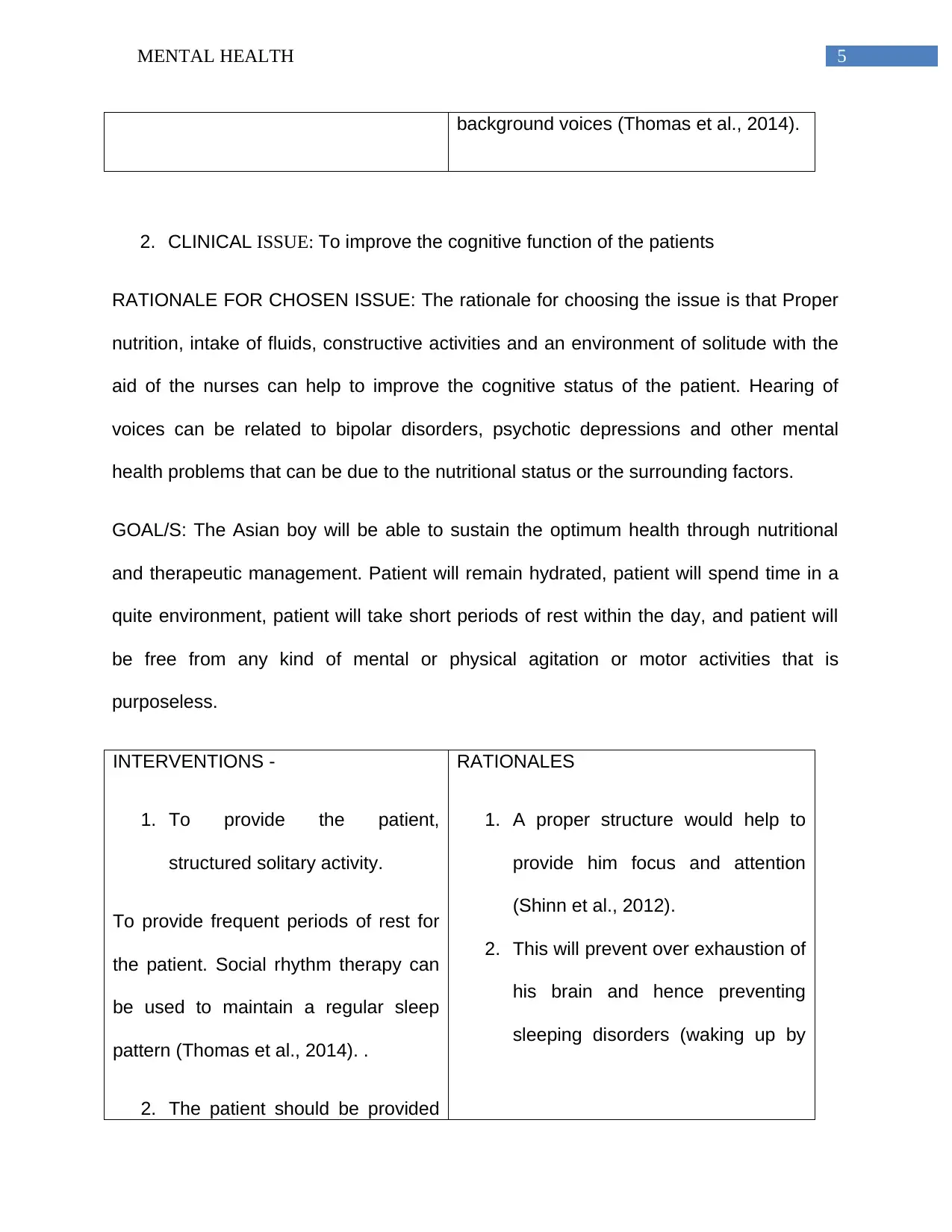
2. CLINICAL ISSUE: To improve the cognitive function of the patients
RATIONALE FOR CHOSEN ISSUE: The rationale for choosing the issue is that Proper
nutrition, intake of fluids, constructive activities and an environment of solitude with the
aid of the nurses can help to improve the cognitive status of the patient. Hearing of
voices can be related to bipolar disorders, psychotic depressions and other mental
health problems that can be due to the nutritional status or the surrounding factors.
GOAL/S: The Asian boy will be able to sustain the optimum health through nutritional
and therapeutic management. Patient will remain hydrated, patient will spend time in a
quite environment, patient will take short periods of rest within the day, and patient will
be free from any kind of mental or physical agitation or motor activities that is
purposeless.
INTERVENTIONS -
1. To provide the patient,
structured solitary activity.
To provide frequent periods of rest for
the patient. Social rhythm therapy can
be used to maintain a regular sleep
pattern (Thomas et al., 2014). .
2. The patient should be provided
RATIONALES
1. A proper structure would help to
provide him focus and attention
(Shinn et al., 2012).
2. This will prevent over exhaustion of
his brain and hence preventing
sleeping disorders (waking up by
background voices (Thomas et al., 2014).
2. CLINICAL ISSUE: To improve the cognitive function of the patients
RATIONALE FOR CHOSEN ISSUE: The rationale for choosing the issue is that Proper
nutrition, intake of fluids, constructive activities and an environment of solitude with the
aid of the nurses can help to improve the cognitive status of the patient. Hearing of
voices can be related to bipolar disorders, psychotic depressions and other mental
health problems that can be due to the nutritional status or the surrounding factors.
GOAL/S: The Asian boy will be able to sustain the optimum health through nutritional
and therapeutic management. Patient will remain hydrated, patient will spend time in a
quite environment, patient will take short periods of rest within the day, and patient will
be free from any kind of mental or physical agitation or motor activities that is
purposeless.
INTERVENTIONS -
1. To provide the patient,
structured solitary activity.
To provide frequent periods of rest for
the patient. Social rhythm therapy can
be used to maintain a regular sleep
pattern (Thomas et al., 2014). .
2. The patient should be provided
RATIONALES
1. A proper structure would help to
provide him focus and attention
(Shinn et al., 2012).
2. This will prevent over exhaustion of
his brain and hence preventing
sleeping disorders (waking up by
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6MENTAL HEALTH
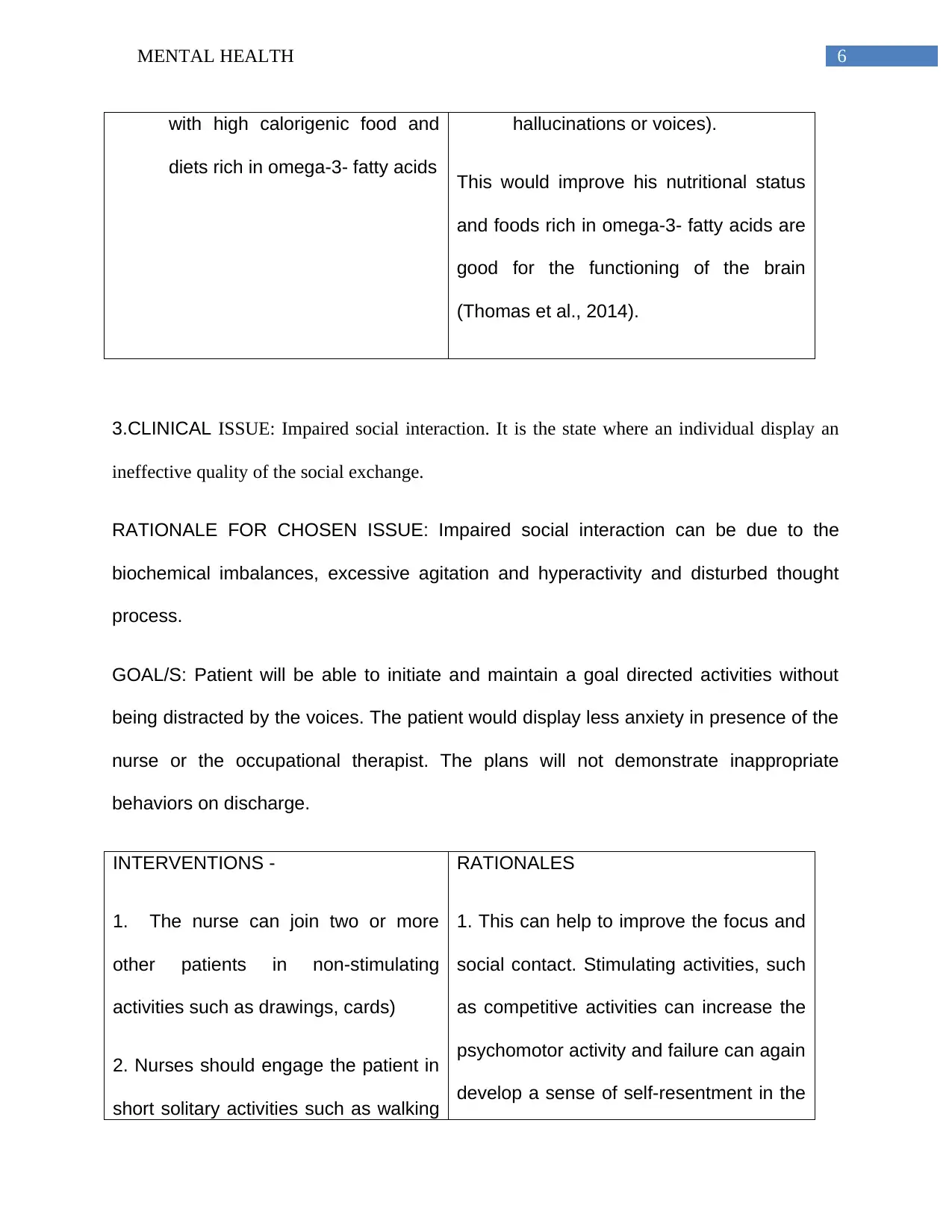
with high calorigenic food and
diets rich in omega-3- fatty acids
hallucinations or voices).
This would improve his nutritional status
and foods rich in omega-3- fatty acids are
good for the functioning of the brain
(Thomas et al., 2014).
3.CLINICAL ISSUE: Impaired social interaction. It is the state where an individual display an
ineffective quality of the social exchange.
RATIONALE FOR CHOSEN ISSUE: Impaired social interaction can be due to the
biochemical imbalances, excessive agitation and hyperactivity and disturbed thought
process.
GOAL/S: Patient will be able to initiate and maintain a goal directed activities without
being distracted by the voices. The patient would display less anxiety in presence of the
nurse or the occupational therapist. The plans will not demonstrate inappropriate
behaviors on discharge.
INTERVENTIONS -
1. The nurse can join two or more
other patients in non-stimulating
activities such as drawings, cards)
2. Nurses should engage the patient in
short solitary activities such as walking
RATIONALES
1. This can help to improve the focus and
social contact. Stimulating activities, such
as competitive activities can increase the
psychomotor activity and failure can again
develop a sense of self-resentment in the
with high calorigenic food and
diets rich in omega-3- fatty acids
hallucinations or voices).
This would improve his nutritional status
and foods rich in omega-3- fatty acids are
good for the functioning of the brain
(Thomas et al., 2014).
3.CLINICAL ISSUE: Impaired social interaction. It is the state where an individual display an
ineffective quality of the social exchange.
RATIONALE FOR CHOSEN ISSUE: Impaired social interaction can be due to the
biochemical imbalances, excessive agitation and hyperactivity and disturbed thought
process.
GOAL/S: Patient will be able to initiate and maintain a goal directed activities without
being distracted by the voices. The patient would display less anxiety in presence of the
nurse or the occupational therapist. The plans will not demonstrate inappropriate
behaviors on discharge.
INTERVENTIONS -
1. The nurse can join two or more
other patients in non-stimulating
activities such as drawings, cards)
2. Nurses should engage the patient in
short solitary activities such as walking
RATIONALES
1. This can help to improve the focus and
social contact. Stimulating activities, such
as competitive activities can increase the
psychomotor activity and failure can again
develop a sense of self-resentment in the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7MENTAL HEALTH
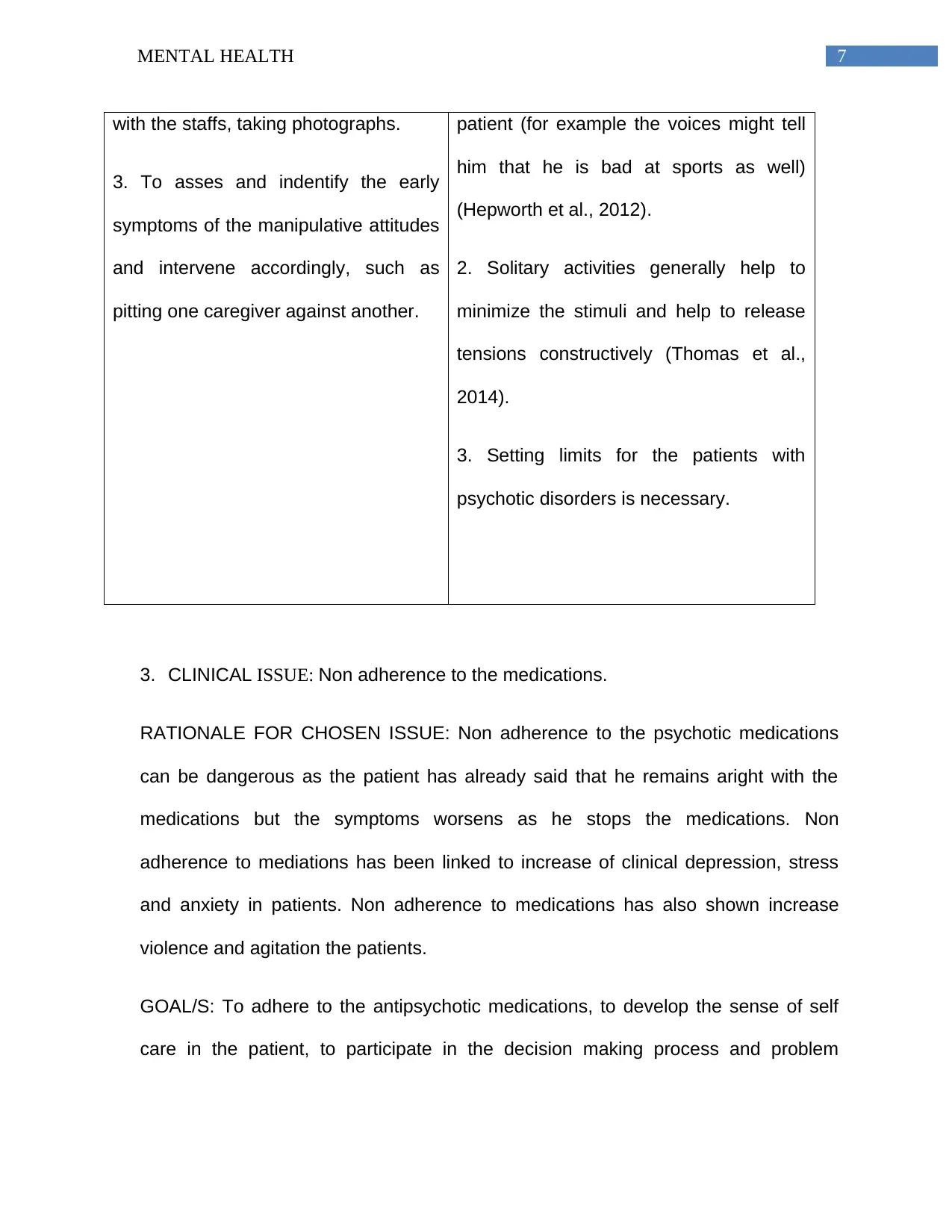
with the staffs, taking photographs.
3. To asses and indentify the early
symptoms of the manipulative attitudes
and intervene accordingly, such as
pitting one caregiver against another.
patient (for example the voices might tell
him that he is bad at sports as well)
(Hepworth et al., 2012).
2. Solitary activities generally help to
minimize the stimuli and help to release
tensions constructively (Thomas et al.,
2014).
3. Setting limits for the patients with
psychotic disorders is necessary.
3. CLINICAL ISSUE: Non adherence to the medications.
RATIONALE FOR CHOSEN ISSUE: Non adherence to the psychotic medications
can be dangerous as the patient has already said that he remains aright with the
medications but the symptoms worsens as he stops the medications. Non
adherence to mediations has been linked to increase of clinical depression, stress
and anxiety in patients. Non adherence to medications has also shown increase
violence and agitation the patients.
GOAL/S: To adhere to the antipsychotic medications, to develop the sense of self
care in the patient, to participate in the decision making process and problem
with the staffs, taking photographs.
3. To asses and indentify the early
symptoms of the manipulative attitudes
and intervene accordingly, such as
pitting one caregiver against another.
patient (for example the voices might tell
him that he is bad at sports as well)
(Hepworth et al., 2012).
2. Solitary activities generally help to
minimize the stimuli and help to release
tensions constructively (Thomas et al.,
2014).
3. Setting limits for the patients with
psychotic disorders is necessary.
3. CLINICAL ISSUE: Non adherence to the medications.
RATIONALE FOR CHOSEN ISSUE: Non adherence to the psychotic medications
can be dangerous as the patient has already said that he remains aright with the
medications but the symptoms worsens as he stops the medications. Non
adherence to mediations has been linked to increase of clinical depression, stress
and anxiety in patients. Non adherence to medications has also shown increase
violence and agitation the patients.
GOAL/S: To adhere to the antipsychotic medications, to develop the sense of self
care in the patient, to participate in the decision making process and problem
8MENTAL HEALTH
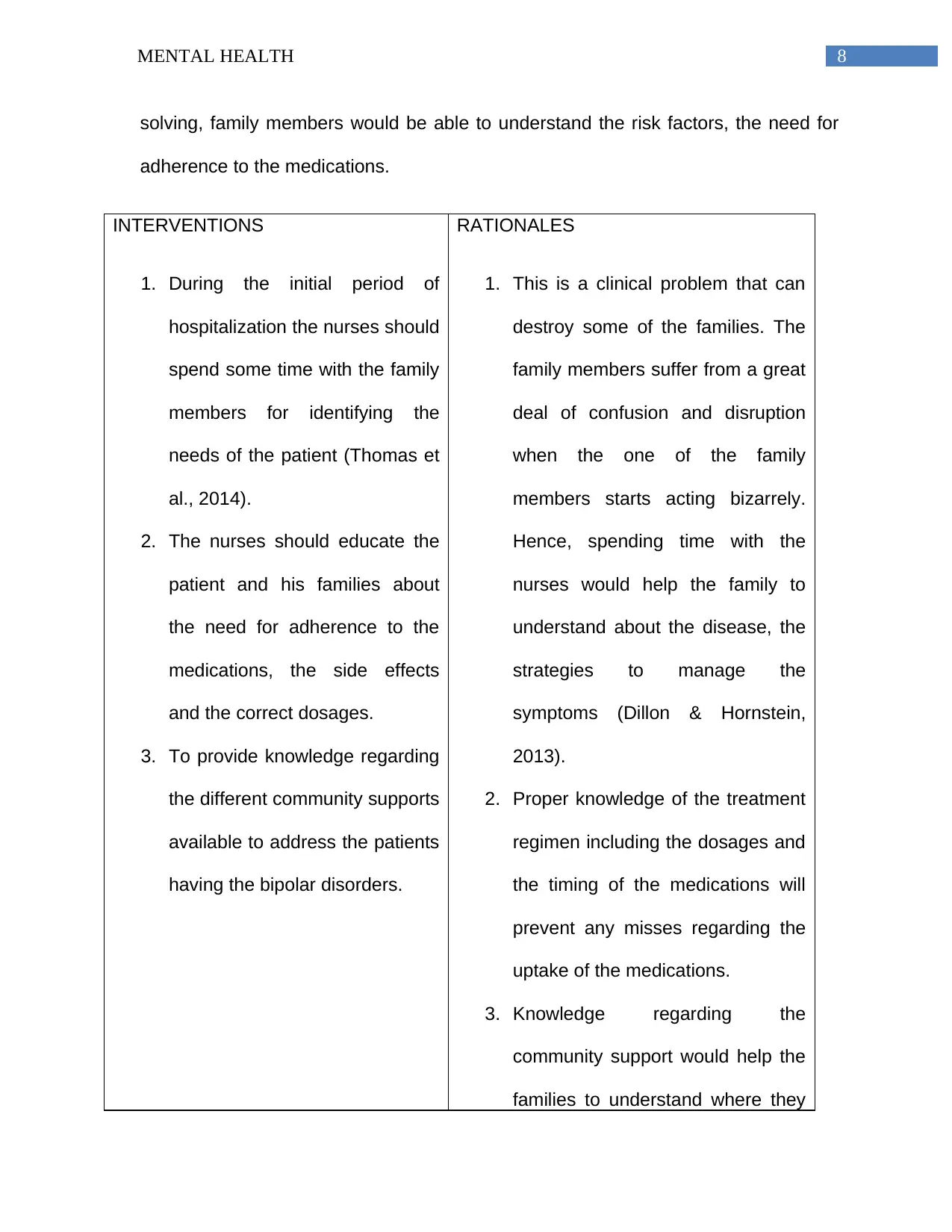
solving, family members would be able to understand the risk factors, the need for
adherence to the medications.
INTERVENTIONS
1. During the initial period of
hospitalization the nurses should
spend some time with the family
members for identifying the
needs of the patient (Thomas et
al., 2014).
2. The nurses should educate the
patient and his families about
the need for adherence to the
medications, the side effects
and the correct dosages.
3. To provide knowledge regarding
the different community supports
available to address the patients
having the bipolar disorders.
RATIONALES
1. This is a clinical problem that can
destroy some of the families. The
family members suffer from a great
deal of confusion and disruption
when the one of the family
members starts acting bizarrely.
Hence, spending time with the
nurses would help the family to
understand about the disease, the
strategies to manage the
symptoms (Dillon & Hornstein,
2013).
2. Proper knowledge of the treatment
regimen including the dosages and
the timing of the medications will
prevent any misses regarding the
uptake of the medications.
3. Knowledge regarding the
community support would help the
families to understand where they
solving, family members would be able to understand the risk factors, the need for
adherence to the medications.
INTERVENTIONS
1. During the initial period of
hospitalization the nurses should
spend some time with the family
members for identifying the
needs of the patient (Thomas et
al., 2014).
2. The nurses should educate the
patient and his families about
the need for adherence to the
medications, the side effects
and the correct dosages.
3. To provide knowledge regarding
the different community supports
available to address the patients
having the bipolar disorders.
RATIONALES
1. This is a clinical problem that can
destroy some of the families. The
family members suffer from a great
deal of confusion and disruption
when the one of the family
members starts acting bizarrely.
Hence, spending time with the
nurses would help the family to
understand about the disease, the
strategies to manage the
symptoms (Dillon & Hornstein,
2013).
2. Proper knowledge of the treatment
regimen including the dosages and
the timing of the medications will
prevent any misses regarding the
uptake of the medications.
3. Knowledge regarding the
community support would help the
families to understand where they
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9MENTAL HEALTH
have to go for help for their
individual issues (Dillon &
Hornstein, 2013).
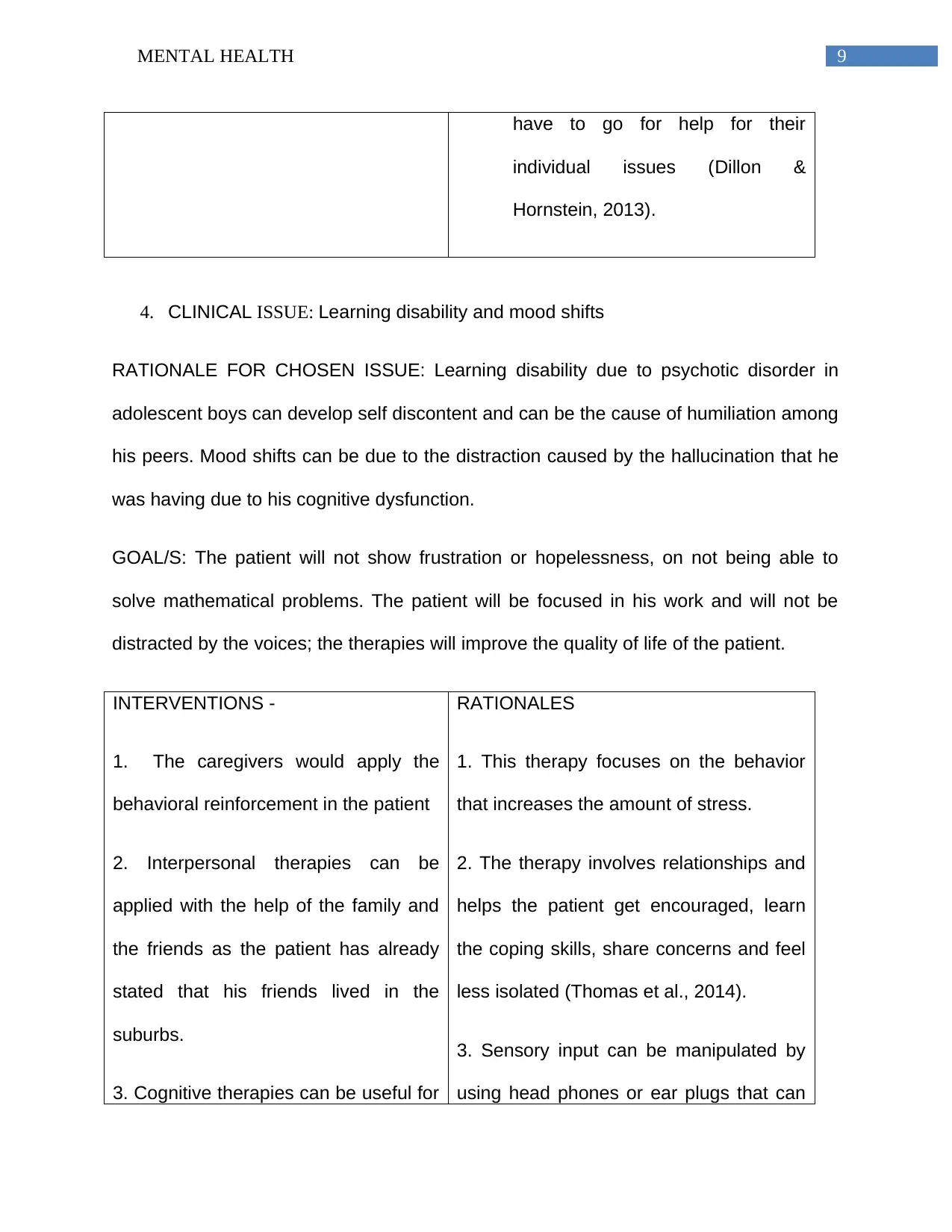
4. CLINICAL ISSUE: Learning disability and mood shifts
RATIONALE FOR CHOSEN ISSUE: Learning disability due to psychotic disorder in
adolescent boys can develop self discontent and can be the cause of humiliation among
his peers. Mood shifts can be due to the distraction caused by the hallucination that he
was having due to his cognitive dysfunction.
GOAL/S: The patient will not show frustration or hopelessness, on not being able to
solve mathematical problems. The patient will be focused in his work and will not be
distracted by the voices; the therapies will improve the quality of life of the patient.
INTERVENTIONS -
1. The caregivers would apply the
behavioral reinforcement in the patient
2. Interpersonal therapies can be
applied with the help of the family and
the friends as the patient has already
stated that his friends lived in the
suburbs.
3. Cognitive therapies can be useful for
RATIONALES
1. This therapy focuses on the behavior
that increases the amount of stress.
2. The therapy involves relationships and
helps the patient get encouraged, learn
the coping skills, share concerns and feel
less isolated (Thomas et al., 2014).
3. Sensory input can be manipulated by
using head phones or ear plugs that can
have to go for help for their
individual issues (Dillon &
Hornstein, 2013).
4. CLINICAL ISSUE: Learning disability and mood shifts
RATIONALE FOR CHOSEN ISSUE: Learning disability due to psychotic disorder in
adolescent boys can develop self discontent and can be the cause of humiliation among
his peers. Mood shifts can be due to the distraction caused by the hallucination that he
was having due to his cognitive dysfunction.
GOAL/S: The patient will not show frustration or hopelessness, on not being able to
solve mathematical problems. The patient will be focused in his work and will not be
distracted by the voices; the therapies will improve the quality of life of the patient.
INTERVENTIONS -
1. The caregivers would apply the
behavioral reinforcement in the patient
2. Interpersonal therapies can be
applied with the help of the family and
the friends as the patient has already
stated that his friends lived in the
suburbs.
3. Cognitive therapies can be useful for
RATIONALES
1. This therapy focuses on the behavior
that increases the amount of stress.
2. The therapy involves relationships and
helps the patient get encouraged, learn
the coping skills, share concerns and feel
less isolated (Thomas et al., 2014).
3. Sensory input can be manipulated by
using head phones or ear plugs that can
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
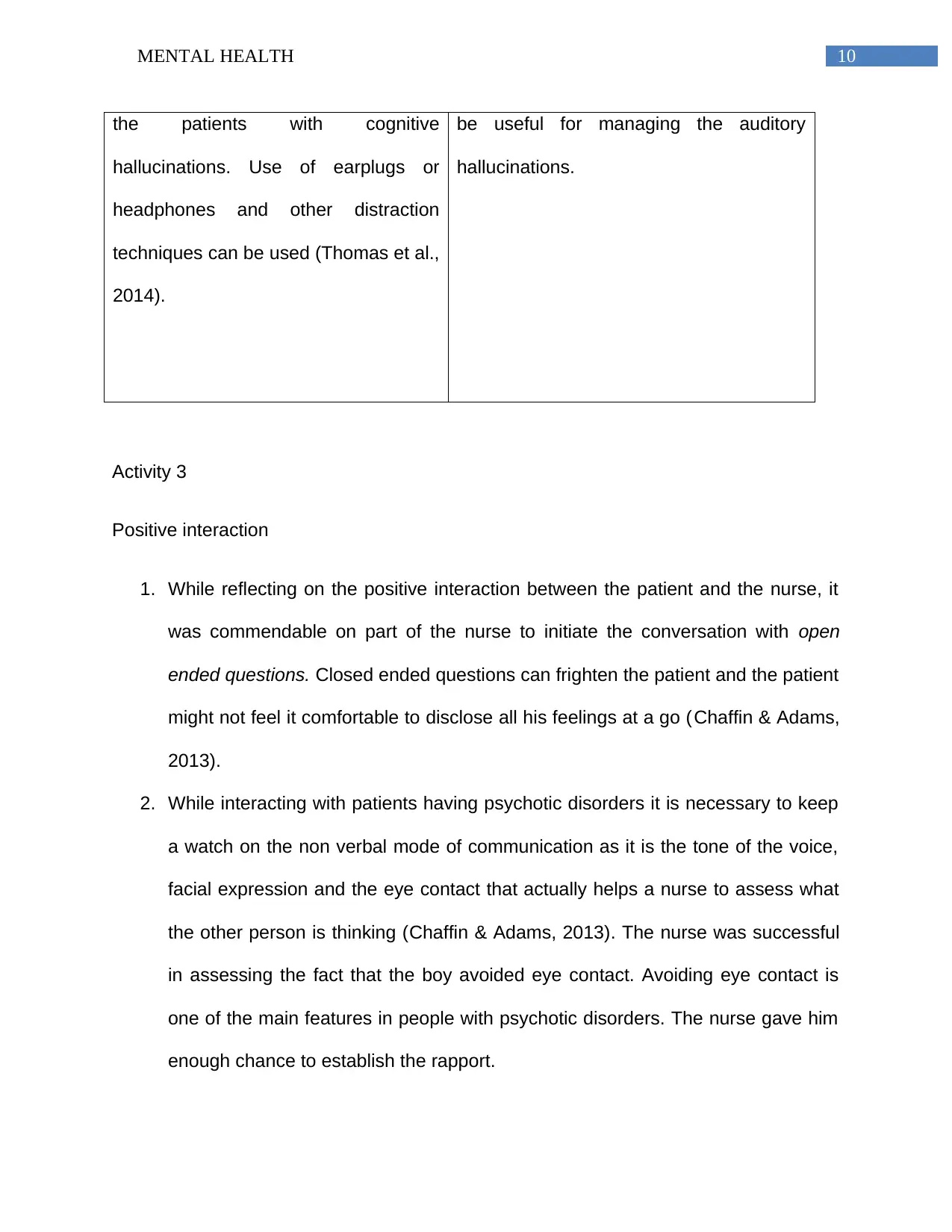
10MENTAL HEALTH
the patients with cognitive
hallucinations. Use of earplugs or
headphones and other distraction
techniques can be used (Thomas et al.,
2014).
be useful for managing the auditory
hallucinations.
Activity 3
Positive interaction
1. While reflecting on the positive interaction between the patient and the nurse, it
was commendable on part of the nurse to initiate the conversation with open
ended questions. Closed ended questions can frighten the patient and the patient
might not feel it comfortable to disclose all his feelings at a go (Chaffin & Adams,
2013).
2. While interacting with patients having psychotic disorders it is necessary to keep
a watch on the non verbal mode of communication as it is the tone of the voice,
facial expression and the eye contact that actually helps a nurse to assess what
the other person is thinking (Chaffin & Adams, 2013). The nurse was successful
in assessing the fact that the boy avoided eye contact. Avoiding eye contact is
one of the main features in people with psychotic disorders. The nurse gave him
enough chance to establish the rapport.
the patients with cognitive
hallucinations. Use of earplugs or
headphones and other distraction
techniques can be used (Thomas et al.,
2014).
be useful for managing the auditory
hallucinations.
Activity 3
Positive interaction
1. While reflecting on the positive interaction between the patient and the nurse, it
was commendable on part of the nurse to initiate the conversation with open
ended questions. Closed ended questions can frighten the patient and the patient
might not feel it comfortable to disclose all his feelings at a go (Chaffin & Adams,
2013).
2. While interacting with patients having psychotic disorders it is necessary to keep
a watch on the non verbal mode of communication as it is the tone of the voice,
facial expression and the eye contact that actually helps a nurse to assess what
the other person is thinking (Chaffin & Adams, 2013). The nurse was successful
in assessing the fact that the boy avoided eye contact. Avoiding eye contact is
one of the main features in people with psychotic disorders. The nurse gave him
enough chance to establish the rapport.
11MENTAL HEALTH
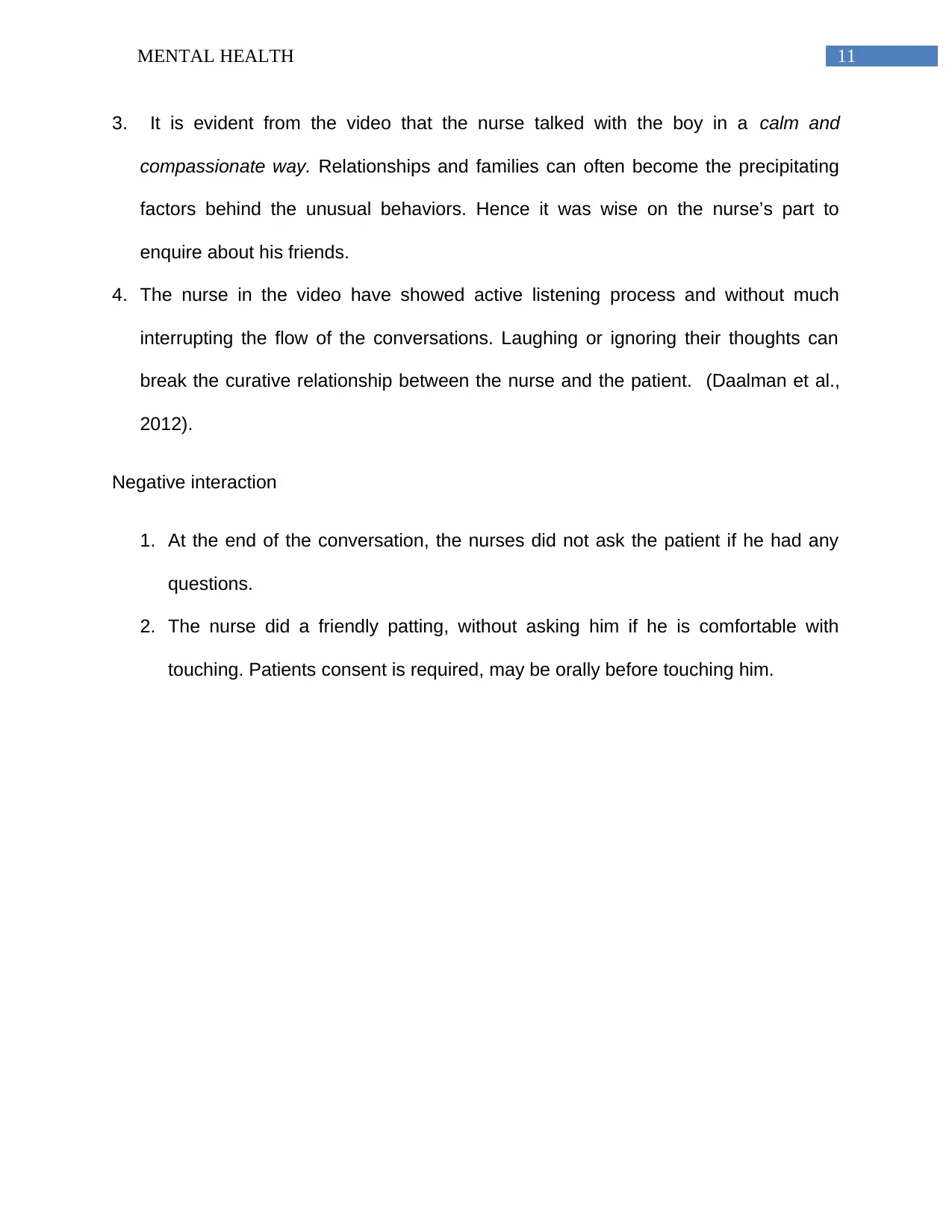
3. It is evident from the video that the nurse talked with the boy in a calm and
compassionate way. Relationships and families can often become the precipitating
factors behind the unusual behaviors. Hence it was wise on the nurse’s part to
enquire about his friends.
4. The nurse in the video have showed active listening process and without much
interrupting the flow of the conversations. Laughing or ignoring their thoughts can
break the curative relationship between the nurse and the patient. (Daalman et al.,
2012).
Negative interaction
1. At the end of the conversation, the nurses did not ask the patient if he had any
questions.
2. The nurse did a friendly patting, without asking him if he is comfortable with
touching. Patients consent is required, may be orally before touching him.
3. It is evident from the video that the nurse talked with the boy in a calm and
compassionate way. Relationships and families can often become the precipitating
factors behind the unusual behaviors. Hence it was wise on the nurse’s part to
enquire about his friends.
4. The nurse in the video have showed active listening process and without much
interrupting the flow of the conversations. Laughing or ignoring their thoughts can
break the curative relationship between the nurse and the patient. (Daalman et al.,
2012).
Negative interaction
1. At the end of the conversation, the nurses did not ask the patient if he had any
questions.
2. The nurse did a friendly patting, without asking him if he is comfortable with
touching. Patients consent is required, may be orally before touching him.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





