MENTAL HEALTH ASSESSMENT TASK 2
VerifiedAdded on 2023/01/06
|12
|3305
|2
AI Summary
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
MENTAL HEALTH ASSESSMENT
TASK 2
1 | P a g e
TASK 2
1 | P a g e
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
PART 1: Holistic assessment and planning
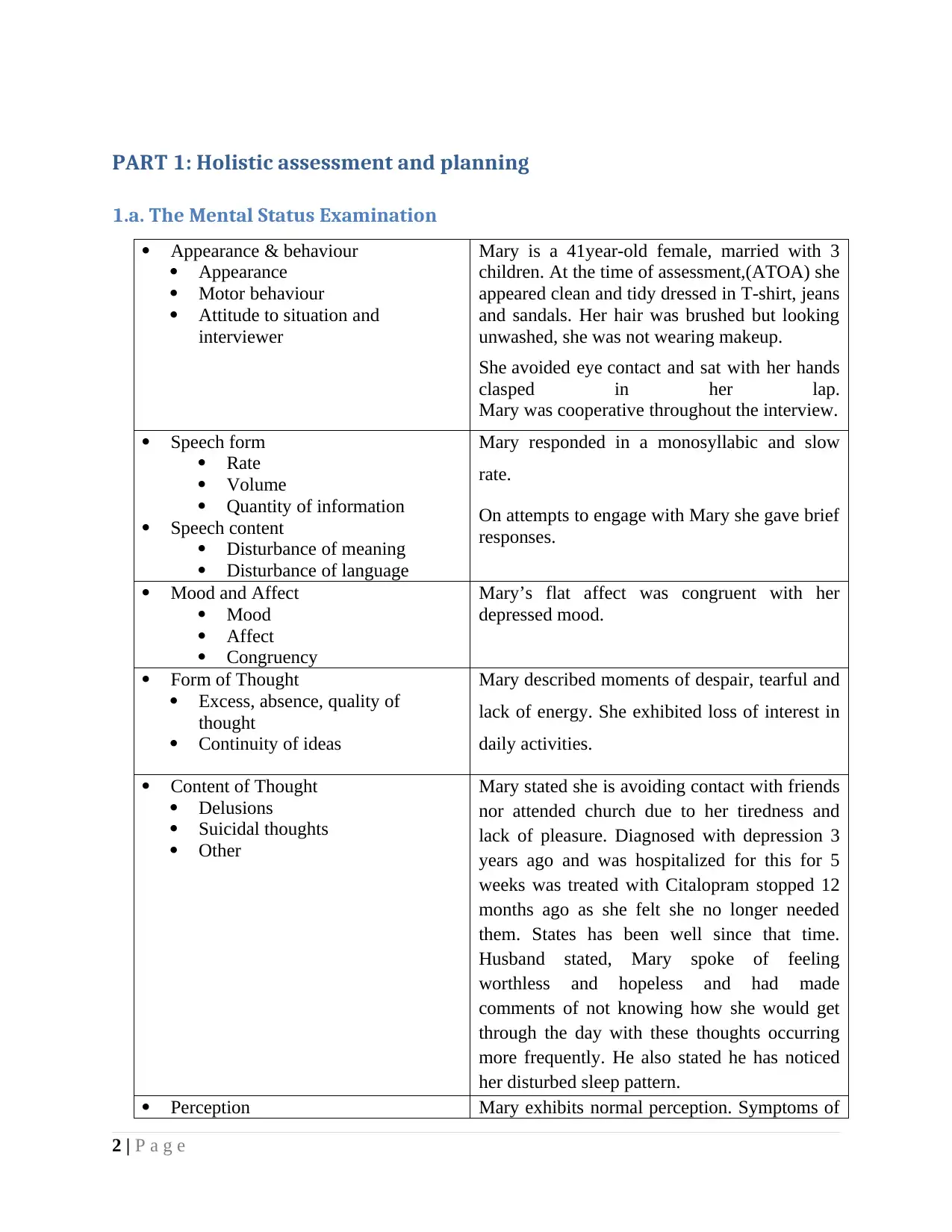
1.a. The Mental Status Examination
Appearance & behaviour
Appearance
Motor behaviour
Attitude to situation and
interviewer
Mary is a 41year-old female, married with 3
children. At the time of assessment,(ATOA) she
appeared clean and tidy dressed in T-shirt, jeans
and sandals. Her hair was brushed but looking
unwashed, she was not wearing makeup.
She avoided eye contact and sat with her hands
clasped in her lap.
Mary was cooperative throughout the interview.
Speech form
Rate
Volume
Quantity of information
Speech content
Disturbance of meaning
Disturbance of language
Mary responded in a monosyllabic and slow
rate.
On attempts to engage with Mary she gave brief
responses.
Mood and Affect
Mood
Affect
Congruency
Mary’s flat affect was congruent with her
depressed mood.
Form of Thought
Excess, absence, quality of
thought
Continuity of ideas
Mary described moments of despair, tearful and
lack of energy. She exhibited loss of interest in
daily activities.
Content of Thought
Delusions
Suicidal thoughts
Other
Mary stated she is avoiding contact with friends
nor attended church due to her tiredness and
lack of pleasure. Diagnosed with depression 3
years ago and was hospitalized for this for 5
weeks was treated with Citalopram stopped 12
months ago as she felt she no longer needed
them. States has been well since that time.
Husband stated, Mary spoke of feeling
worthless and hopeless and had made
comments of not knowing how she would get
through the day with these thoughts occurring
more frequently. He also stated he has noticed
her disturbed sleep pattern.
Perception Mary exhibits normal perception. Symptoms of
2 | P a g e
1.a. The Mental Status Examination
Appearance & behaviour
Appearance
Motor behaviour
Attitude to situation and
interviewer
Mary is a 41year-old female, married with 3
children. At the time of assessment,(ATOA) she
appeared clean and tidy dressed in T-shirt, jeans
and sandals. Her hair was brushed but looking
unwashed, she was not wearing makeup.
She avoided eye contact and sat with her hands
clasped in her lap.
Mary was cooperative throughout the interview.
Speech form
Rate
Volume
Quantity of information
Speech content
Disturbance of meaning
Disturbance of language
Mary responded in a monosyllabic and slow
rate.
On attempts to engage with Mary she gave brief
responses.
Mood and Affect
Mood
Affect
Congruency
Mary’s flat affect was congruent with her
depressed mood.
Form of Thought
Excess, absence, quality of
thought
Continuity of ideas
Mary described moments of despair, tearful and
lack of energy. She exhibited loss of interest in
daily activities.
Content of Thought
Delusions
Suicidal thoughts
Other
Mary stated she is avoiding contact with friends
nor attended church due to her tiredness and
lack of pleasure. Diagnosed with depression 3
years ago and was hospitalized for this for 5
weeks was treated with Citalopram stopped 12
months ago as she felt she no longer needed
them. States has been well since that time.
Husband stated, Mary spoke of feeling
worthless and hopeless and had made
comments of not knowing how she would get
through the day with these thoughts occurring
more frequently. He also stated he has noticed
her disturbed sleep pattern.
Perception Mary exhibits normal perception. Symptoms of
2 | P a g e
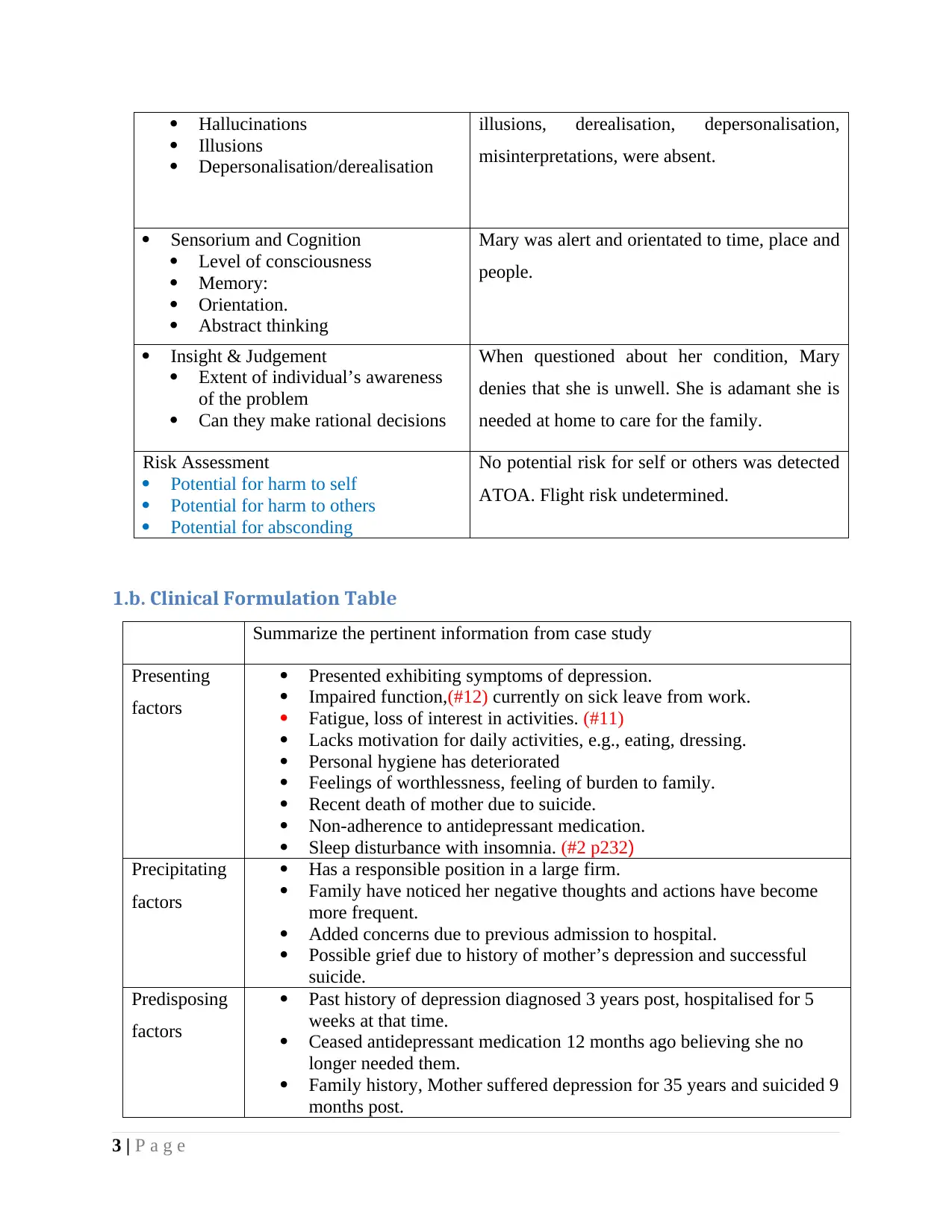
Hallucinations
Illusions
Depersonalisation/derealisation
illusions, derealisation, depersonalisation,
misinterpretations, were absent.
Sensorium and Cognition
Level of consciousness
Memory:
Orientation.
Abstract thinking
Mary was alert and orientated to time, place and
people.
Insight & Judgement
Extent of individual’s awareness
of the problem
Can they make rational decisions
When questioned about her condition, Mary
denies that she is unwell. She is adamant she is
needed at home to care for the family.
Risk Assessment
Potential for harm to self
Potential for harm to others
Potential for absconding
No potential risk for self or others was detected
ATOA. Flight risk undetermined.
1.b. Clinical Formulation Table
Summarize the pertinent information from case study
Presenting
factors
Presented exhibiting symptoms of depression.
Impaired function,(#12) currently on sick leave from work.
Fatigue, loss of interest in activities. (#11)
Lacks motivation for daily activities, e.g., eating, dressing.
Personal hygiene has deteriorated
Feelings of worthlessness, feeling of burden to family.
Recent death of mother due to suicide.
Non-adherence to antidepressant medication.
Sleep disturbance with insomnia. (#2 p232)
Precipitating
factors
Has a responsible position in a large firm.
Family have noticed her negative thoughts and actions have become
more frequent.
Added concerns due to previous admission to hospital.
Possible grief due to history of mother’s depression and successful
suicide.
Predisposing
factors
Past history of depression diagnosed 3 years post, hospitalised for 5
weeks at that time.
Ceased antidepressant medication 12 months ago believing she no
longer needed them.
Family history, Mother suffered depression for 35 years and suicided 9
months post.
3 | P a g e
Illusions
Depersonalisation/derealisation
illusions, derealisation, depersonalisation,
misinterpretations, were absent.
Sensorium and Cognition
Level of consciousness
Memory:
Orientation.
Abstract thinking
Mary was alert and orientated to time, place and
people.
Insight & Judgement
Extent of individual’s awareness
of the problem
Can they make rational decisions
When questioned about her condition, Mary
denies that she is unwell. She is adamant she is
needed at home to care for the family.
Risk Assessment
Potential for harm to self
Potential for harm to others
Potential for absconding
No potential risk for self or others was detected
ATOA. Flight risk undetermined.
1.b. Clinical Formulation Table
Summarize the pertinent information from case study
Presenting
factors
Presented exhibiting symptoms of depression.
Impaired function,(#12) currently on sick leave from work.
Fatigue, loss of interest in activities. (#11)
Lacks motivation for daily activities, e.g., eating, dressing.
Personal hygiene has deteriorated
Feelings of worthlessness, feeling of burden to family.
Recent death of mother due to suicide.
Non-adherence to antidepressant medication.
Sleep disturbance with insomnia. (#2 p232)
Precipitating
factors
Has a responsible position in a large firm.
Family have noticed her negative thoughts and actions have become
more frequent.
Added concerns due to previous admission to hospital.
Possible grief due to history of mother’s depression and successful
suicide.
Predisposing
factors
Past history of depression diagnosed 3 years post, hospitalised for 5
weeks at that time.
Ceased antidepressant medication 12 months ago believing she no
longer needed them.
Family history, Mother suffered depression for 35 years and suicided 9
months post.
3 | P a g e
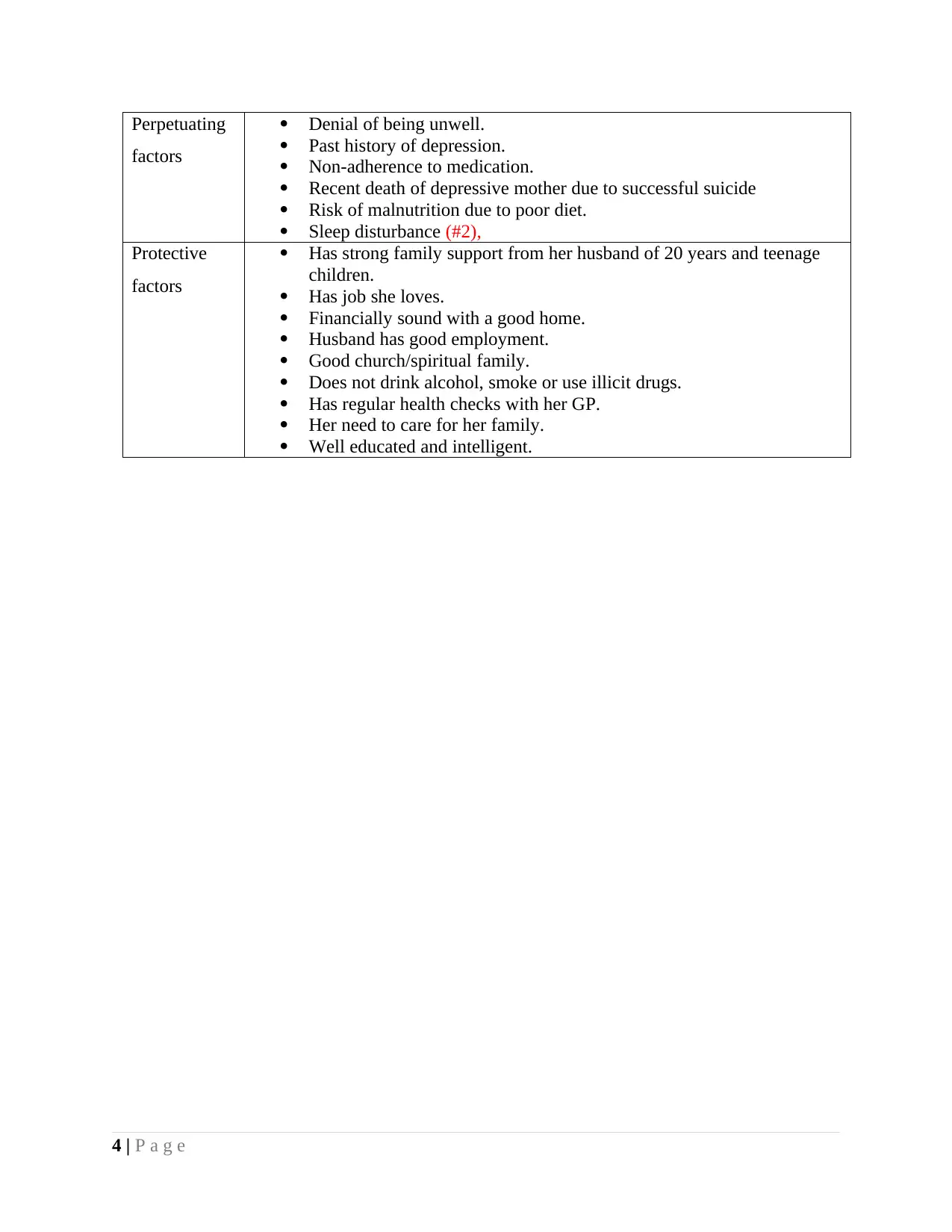
Perpetuating
factors
Denial of being unwell.
Past history of depression.
Non-adherence to medication.
Recent death of depressive mother due to successful suicide
Risk of malnutrition due to poor diet.
Sleep disturbance (#2),
Protective
factors
Has strong family support from her husband of 20 years and teenage
children.
Has job she loves.
Financially sound with a good home.
Husband has good employment.
Good church/spiritual family.
Does not drink alcohol, smoke or use illicit drugs.
Has regular health checks with her GP.
Her need to care for her family.
Well educated and intelligent.
4 | P a g e
factors
Denial of being unwell.
Past history of depression.
Non-adherence to medication.
Recent death of depressive mother due to successful suicide
Risk of malnutrition due to poor diet.
Sleep disturbance (#2),
Protective
factors
Has strong family support from her husband of 20 years and teenage
children.
Has job she loves.
Financially sound with a good home.
Husband has good employment.
Good church/spiritual family.
Does not drink alcohol, smoke or use illicit drugs.
Has regular health checks with her GP.
Her need to care for her family.
Well educated and intelligent.
4 | P a g e
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
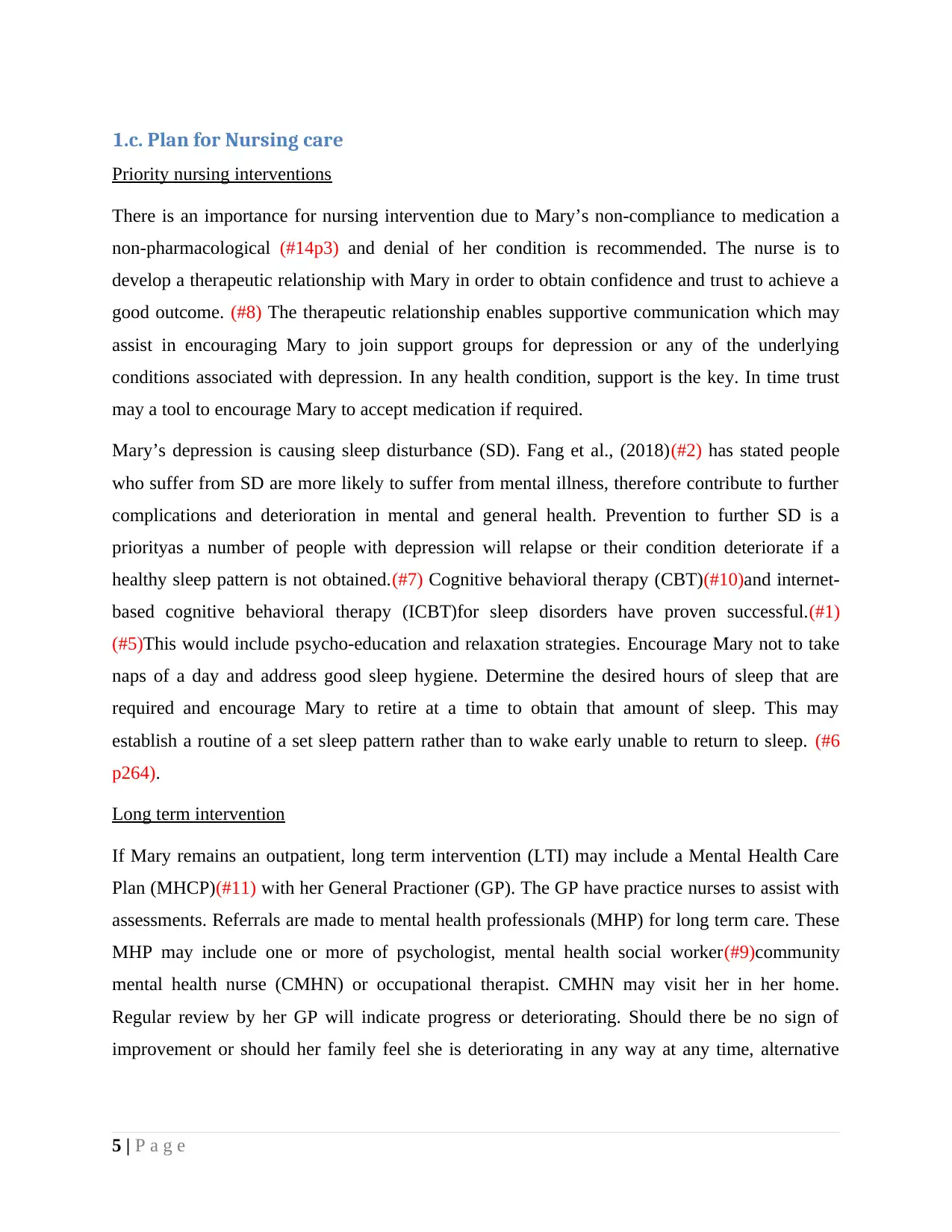
1.c. Plan for Nursing care
Priority nursing interventions
There is an importance for nursing intervention due to Mary’s non-compliance to medication a
non-pharmacological (#14p3) and denial of her condition is recommended. The nurse is to
develop a therapeutic relationship with Mary in order to obtain confidence and trust to achieve a
good outcome. (#8) The therapeutic relationship enables supportive communication which may
assist in encouraging Mary to join support groups for depression or any of the underlying
conditions associated with depression. In any health condition, support is the key. In time trust
may a tool to encourage Mary to accept medication if required.
Mary’s depression is causing sleep disturbance (SD). Fang et al., (2018)(#2) has stated people
who suffer from SD are more likely to suffer from mental illness, therefore contribute to further
complications and deterioration in mental and general health. Prevention to further SD is a
priorityas a number of people with depression will relapse or their condition deteriorate if a
healthy sleep pattern is not obtained.(#7) Cognitive behavioral therapy (CBT)(#10)and internet-
based cognitive behavioral therapy (ICBT)for sleep disorders have proven successful.(#1)
(#5)This would include psycho-education and relaxation strategies. Encourage Mary not to take
naps of a day and address good sleep hygiene. Determine the desired hours of sleep that are
required and encourage Mary to retire at a time to obtain that amount of sleep. This may
establish a routine of a set sleep pattern rather than to wake early unable to return to sleep. (#6
p264).
Long term intervention
If Mary remains an outpatient, long term intervention (LTI) may include a Mental Health Care
Plan (MHCP)(#11) with her General Practioner (GP). The GP have practice nurses to assist with
assessments. Referrals are made to mental health professionals (MHP) for long term care. These
MHP may include one or more of psychologist, mental health social worker(#9)community
mental health nurse (CMHN) or occupational therapist. CMHN may visit her in her home.
Regular review by her GP will indicate progress or deteriorating. Should there be no sign of
improvement or should her family feel she is deteriorating in any way at any time, alternative
5 | P a g e
Priority nursing interventions
There is an importance for nursing intervention due to Mary’s non-compliance to medication a
non-pharmacological (#14p3) and denial of her condition is recommended. The nurse is to
develop a therapeutic relationship with Mary in order to obtain confidence and trust to achieve a
good outcome. (#8) The therapeutic relationship enables supportive communication which may
assist in encouraging Mary to join support groups for depression or any of the underlying
conditions associated with depression. In any health condition, support is the key. In time trust
may a tool to encourage Mary to accept medication if required.
Mary’s depression is causing sleep disturbance (SD). Fang et al., (2018)(#2) has stated people
who suffer from SD are more likely to suffer from mental illness, therefore contribute to further
complications and deterioration in mental and general health. Prevention to further SD is a
priorityas a number of people with depression will relapse or their condition deteriorate if a
healthy sleep pattern is not obtained.(#7) Cognitive behavioral therapy (CBT)(#10)and internet-
based cognitive behavioral therapy (ICBT)for sleep disorders have proven successful.(#1)
(#5)This would include psycho-education and relaxation strategies. Encourage Mary not to take
naps of a day and address good sleep hygiene. Determine the desired hours of sleep that are
required and encourage Mary to retire at a time to obtain that amount of sleep. This may
establish a routine of a set sleep pattern rather than to wake early unable to return to sleep. (#6
p264).
Long term intervention
If Mary remains an outpatient, long term intervention (LTI) may include a Mental Health Care
Plan (MHCP)(#11) with her General Practioner (GP). The GP have practice nurses to assist with
assessments. Referrals are made to mental health professionals (MHP) for long term care. These
MHP may include one or more of psychologist, mental health social worker(#9)community
mental health nurse (CMHN) or occupational therapist. CMHN may visit her in her home.
Regular review by her GP will indicate progress or deteriorating. Should there be no sign of
improvement or should her family feel she is deteriorating in any way at any time, alternative
5 | P a g e
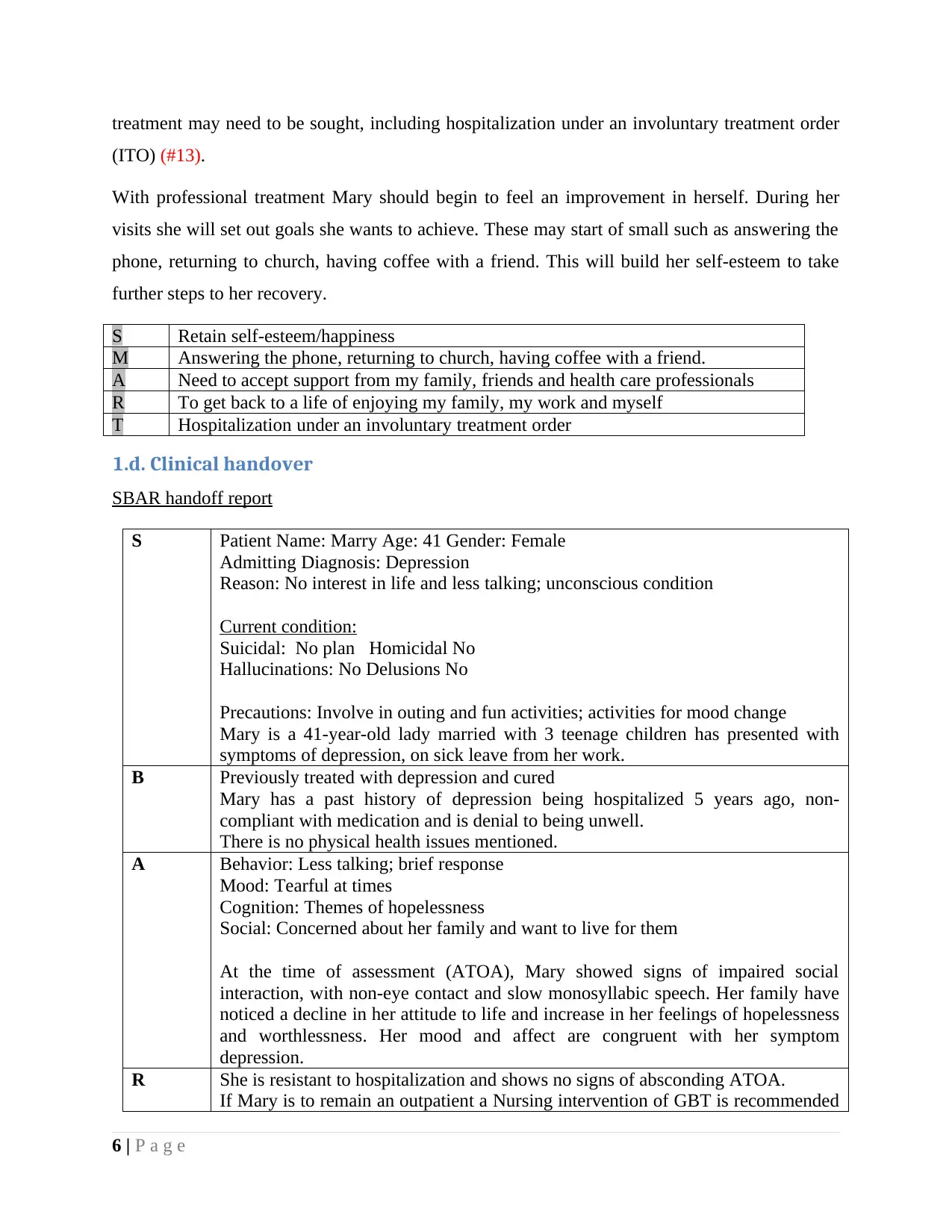
treatment may need to be sought, including hospitalization under an involuntary treatment order
(ITO) (#13).
With professional treatment Mary should begin to feel an improvement in herself. During her
visits she will set out goals she wants to achieve. These may start of small such as answering the
phone, returning to church, having coffee with a friend. This will build her self-esteem to take
further steps to her recovery.
S Retain self-esteem/happiness
M Answering the phone, returning to church, having coffee with a friend.
A Need to accept support from my family, friends and health care professionals
R To get back to a life of enjoying my family, my work and myself
T Hospitalization under an involuntary treatment order
1.d. Clinical handover
SBAR handoff report
S Patient Name: Marry Age: 41 Gender: Female
Admitting Diagnosis: Depression
Reason: No interest in life and less talking; unconscious condition
Current condition:
Suicidal: No plan Homicidal No
Hallucinations: No Delusions No
Precautions: Involve in outing and fun activities; activities for mood change
Mary is a 41-year-old lady married with 3 teenage children has presented with
symptoms of depression, on sick leave from her work.
B Previously treated with depression and cured
Mary has a past history of depression being hospitalized 5 years ago, non-
compliant with medication and is denial to being unwell.
There is no physical health issues mentioned.
A Behavior: Less talking; brief response
Mood: Tearful at times
Cognition: Themes of hopelessness
Social: Concerned about her family and want to live for them
At the time of assessment (ATOA), Mary showed signs of impaired social
interaction, with non-eye contact and slow monosyllabic speech. Her family have
noticed a decline in her attitude to life and increase in her feelings of hopelessness
and worthlessness. Her mood and affect are congruent with her symptom
depression.
R She is resistant to hospitalization and shows no signs of absconding ATOA.
If Mary is to remain an outpatient a Nursing intervention of GBT is recommended
6 | P a g e
(ITO) (#13).
With professional treatment Mary should begin to feel an improvement in herself. During her
visits she will set out goals she wants to achieve. These may start of small such as answering the
phone, returning to church, having coffee with a friend. This will build her self-esteem to take
further steps to her recovery.
S Retain self-esteem/happiness
M Answering the phone, returning to church, having coffee with a friend.
A Need to accept support from my family, friends and health care professionals
R To get back to a life of enjoying my family, my work and myself
T Hospitalization under an involuntary treatment order
1.d. Clinical handover
SBAR handoff report
S Patient Name: Marry Age: 41 Gender: Female
Admitting Diagnosis: Depression
Reason: No interest in life and less talking; unconscious condition
Current condition:
Suicidal: No plan Homicidal No
Hallucinations: No Delusions No
Precautions: Involve in outing and fun activities; activities for mood change
Mary is a 41-year-old lady married with 3 teenage children has presented with
symptoms of depression, on sick leave from her work.
B Previously treated with depression and cured
Mary has a past history of depression being hospitalized 5 years ago, non-
compliant with medication and is denial to being unwell.
There is no physical health issues mentioned.
A Behavior: Less talking; brief response
Mood: Tearful at times
Cognition: Themes of hopelessness
Social: Concerned about her family and want to live for them
At the time of assessment (ATOA), Mary showed signs of impaired social
interaction, with non-eye contact and slow monosyllabic speech. Her family have
noticed a decline in her attitude to life and increase in her feelings of hopelessness
and worthlessness. Her mood and affect are congruent with her symptom
depression.
R She is resistant to hospitalization and shows no signs of absconding ATOA.
If Mary is to remain an outpatient a Nursing intervention of GBT is recommended
6 | P a g e
and GPMHCP.
7 | P a g e
7 | P a g e
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Part 2: Therapeutic engagement and clinical interpretation
2.a. Strategy to develop a therapeutic relationship with Marry
The therapeutic relationship is central to all nursing practice. For example, in mental health and
community nursing, the therapeutic relationship may be the primary intervention to promote
awareness and growth and/or to work through difficulties. Clinical guidance promotes the quiet
specialist relationship as a fundamental component of excellent people-centered care for
depressed patients. However, patients can struggle to interact with experts, and experts have
shown they need more guidance on how to build successful relationships with their patients.
The useful relationship is a fundamental messenger, of all psychiatric nursing treatments,
regardless of the exact point. The key is to create a sensible relationship between the caregiver
and the client. The relationship between a medical assistant and a client will surely be protected,
categorized, rigid and in line with clear materials and boundaries. The facts show that problems
with true natural science and hereditary components like schizophrenia and major motivational
factors cannot be alleviated with help. Nonetheless, some of the carer's intense themes such as
helpless mental self-esteem and low confidence are greatly improved through the union of health
or relationship messengers. Establishing a worthwhile partnership or customer relationship
requires a huge investment. The abilities across this land are slightly enhanced and at the same
time improve with the guidance of those with additional skills and experience.
First of all, empathy is an idea that medical assistants need to understand how to build useful
relationships. Compassion is about watching, drawing attention, understanding and participating.
"It belongs to the person with real, psychological and inner (Usher et al. 2005). Sympathy allows
Lauren to understand Mrs. Mary’s situation and what happened to her right now and has passed
on sensitively developing the relationship between the medical helper and the patient Along with
empathy a rehabilitative relationship considers the helper talking to the patient without making
any decisions. .the patient can feel recognized and the relationship can be strengthened (Rana
and Upton, 2009) A strong relationship based on trust can push patients to gather testimonials
and talk directly about the problems with their doctor through the implementation of these
systems of reformed friendship Mrs. Mary could be help to gain the abilities she has to achieve
his goals and a solution plan powerful realization.
8 | P a g e
2.a. Strategy to develop a therapeutic relationship with Marry
The therapeutic relationship is central to all nursing practice. For example, in mental health and
community nursing, the therapeutic relationship may be the primary intervention to promote
awareness and growth and/or to work through difficulties. Clinical guidance promotes the quiet
specialist relationship as a fundamental component of excellent people-centered care for
depressed patients. However, patients can struggle to interact with experts, and experts have
shown they need more guidance on how to build successful relationships with their patients.
The useful relationship is a fundamental messenger, of all psychiatric nursing treatments,
regardless of the exact point. The key is to create a sensible relationship between the caregiver
and the client. The relationship between a medical assistant and a client will surely be protected,
categorized, rigid and in line with clear materials and boundaries. The facts show that problems
with true natural science and hereditary components like schizophrenia and major motivational
factors cannot be alleviated with help. Nonetheless, some of the carer's intense themes such as
helpless mental self-esteem and low confidence are greatly improved through the union of health
or relationship messengers. Establishing a worthwhile partnership or customer relationship
requires a huge investment. The abilities across this land are slightly enhanced and at the same
time improve with the guidance of those with additional skills and experience.
First of all, empathy is an idea that medical assistants need to understand how to build useful
relationships. Compassion is about watching, drawing attention, understanding and participating.
"It belongs to the person with real, psychological and inner (Usher et al. 2005). Sympathy allows
Lauren to understand Mrs. Mary’s situation and what happened to her right now and has passed
on sensitively developing the relationship between the medical helper and the patient Along with
empathy a rehabilitative relationship considers the helper talking to the patient without making
any decisions. .the patient can feel recognized and the relationship can be strengthened (Rana
and Upton, 2009) A strong relationship based on trust can push patients to gather testimonials
and talk directly about the problems with their doctor through the implementation of these
systems of reformed friendship Mrs. Mary could be help to gain the abilities she has to achieve
his goals and a solution plan powerful realization.
8 | P a g e

2.b Describe how the specific nursing strategy relates to the Recovery
model in mental health
Despite evidence for the centrality of the doctor–patient relationship specializing in functional
manipulation of the mind, the perspective of studying the flow of the mind has given limited
consideration to the function of sympathetic human understanding in routine mental treatment,
remembering for conditions strong strategies or techniques for working compassionately with
psychiatric patients in routine practice.
Supporting people with psychological instability involves exercising compassionate skills
through working on it, remembering situations where emotional well-being is legitimately
involved with people's commitment to seek help, the ability to frame by seeing someone or the
ability to speak to others in a sensible and internal way. Neurobiological testing is expanding due
to the importance of passionate and relative treatment components for patients with emotional
wellbeing disorders. In each case, there is a trade-off that clinical empathy involves
understanding a patient's perspective, realistic awakening, and communicating awareness and
responsibility, some of the times referred to. as an intellectual, full of emotion and a behavioral
measure of empathy.
In psychiatric writing, there are many episodic and philosophical explanations for
communicating with patients. In fact, thoughts of empathy in psychotherapy have placed a
balance between empathy as a means of treating the patient and empathy as a means of
understanding the patient in order to develop treatment.
2.c. Challenge while working with Mary
Diagnosis of specific psychiatric disorders would be difficult in the primary care because of high
rate of co-morbidity amongst various disorders. It has become apparent that the proportion of
patients in critical thinking is unresponsive to a clear mental disorder, usually conceptualized
using patients found in supportive or tertiary thinking. Additionally, many people with load
symptoms have a variety of physical or mental problems. This physical and mental empathy
would provide suggestions for the order, treatment, and outcome of the burdensome disease. As
a result, under diagnosis and incomplete administration result in persistent symptoms, use of
abundant wellness management, and loss of working capacity.
9 | P a g e
model in mental health
Despite evidence for the centrality of the doctor–patient relationship specializing in functional
manipulation of the mind, the perspective of studying the flow of the mind has given limited
consideration to the function of sympathetic human understanding in routine mental treatment,
remembering for conditions strong strategies or techniques for working compassionately with
psychiatric patients in routine practice.
Supporting people with psychological instability involves exercising compassionate skills
through working on it, remembering situations where emotional well-being is legitimately
involved with people's commitment to seek help, the ability to frame by seeing someone or the
ability to speak to others in a sensible and internal way. Neurobiological testing is expanding due
to the importance of passionate and relative treatment components for patients with emotional
wellbeing disorders. In each case, there is a trade-off that clinical empathy involves
understanding a patient's perspective, realistic awakening, and communicating awareness and
responsibility, some of the times referred to. as an intellectual, full of emotion and a behavioral
measure of empathy.
In psychiatric writing, there are many episodic and philosophical explanations for
communicating with patients. In fact, thoughts of empathy in psychotherapy have placed a
balance between empathy as a means of treating the patient and empathy as a means of
understanding the patient in order to develop treatment.
2.c. Challenge while working with Mary
Diagnosis of specific psychiatric disorders would be difficult in the primary care because of high
rate of co-morbidity amongst various disorders. It has become apparent that the proportion of
patients in critical thinking is unresponsive to a clear mental disorder, usually conceptualized
using patients found in supportive or tertiary thinking. Additionally, many people with load
symptoms have a variety of physical or mental problems. This physical and mental empathy
would provide suggestions for the order, treatment, and outcome of the burdensome disease. As
a result, under diagnosis and incomplete administration result in persistent symptoms, use of
abundant wellness management, and loss of working capacity.
9 | P a g e

2.d. Strategy to overcome this challenge
Johnson and allies provided evidence for effectiveness of enhanced care by community health
workers in improving treatment adherence to antidepressant medication in rural women with
major depression. Treatment with power orders controlled by the physician in the medical care
community was essential. However, additional information was provided such as initiation of
psycho education, occasional reconnaissance, support and assistance to proceed with treatment in
the “enhanced therapy”. This was led by the four network wellbeing staffs who were experienced
in working in the network wellbeing program. Develop managed care through these networked
welfare workers trained for bereaved women in the province translated into more care and less
deception, but the impact could not be demonstrated in the result of a severe problem. This
review showed that emergency but effective donation from the medical services framework
could lead to treatment. In addition, the trial was proposed to examine the impact of better
observation in a meeting of more empowered individuals but with less access to the medical
services office.
10 | P a g e
Johnson and allies provided evidence for effectiveness of enhanced care by community health
workers in improving treatment adherence to antidepressant medication in rural women with
major depression. Treatment with power orders controlled by the physician in the medical care
community was essential. However, additional information was provided such as initiation of
psycho education, occasional reconnaissance, support and assistance to proceed with treatment in
the “enhanced therapy”. This was led by the four network wellbeing staffs who were experienced
in working in the network wellbeing program. Develop managed care through these networked
welfare workers trained for bereaved women in the province translated into more care and less
deception, but the impact could not be demonstrated in the result of a severe problem. This
review showed that emergency but effective donation from the medical services framework
could lead to treatment. In addition, the trial was proposed to examine the impact of better
observation in a meeting of more empowered individuals but with less access to the medical
services office.
10 | P a g e
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
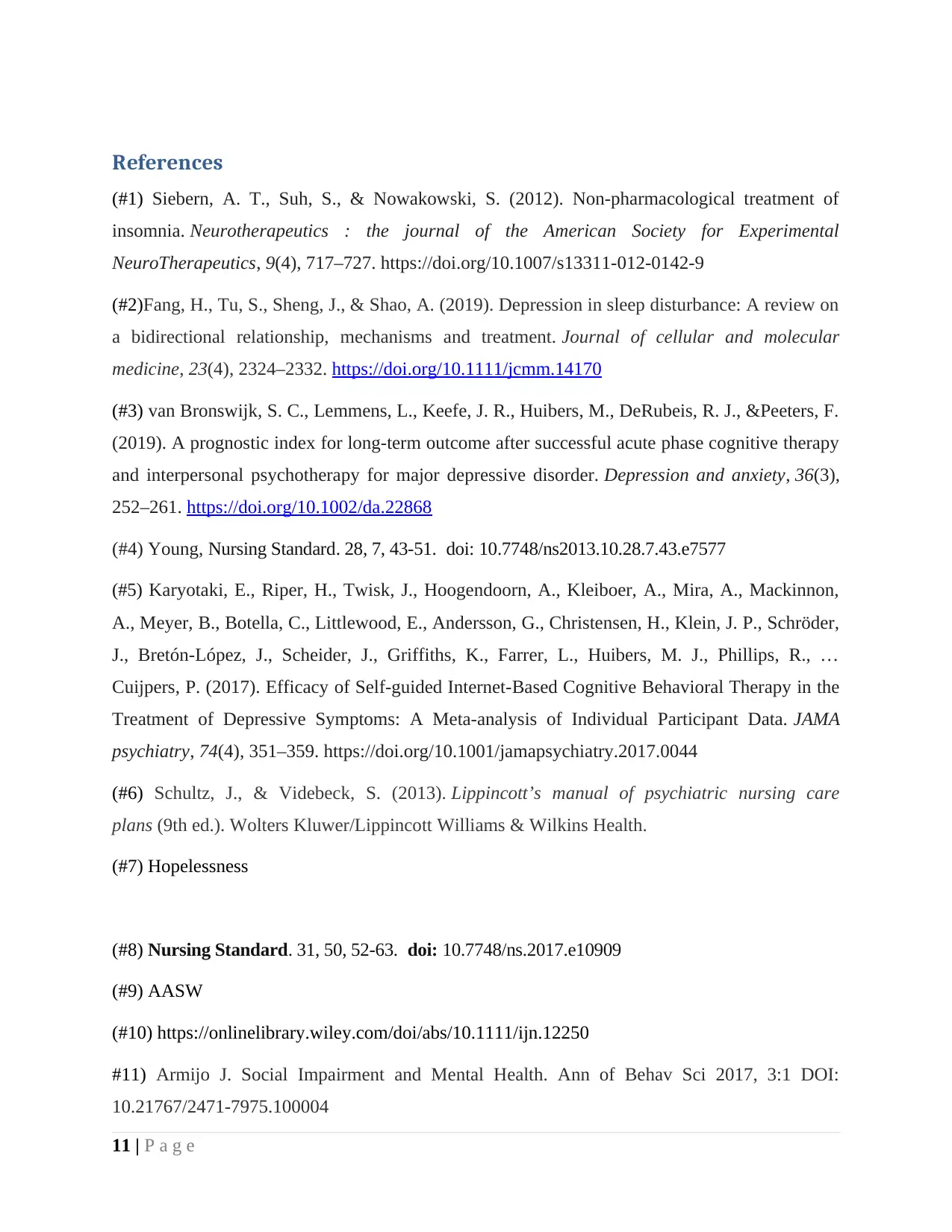
References
(#1) Siebern, A. T., Suh, S., & Nowakowski, S. (2012). Non-pharmacological treatment of
insomnia. Neurotherapeutics : the journal of the American Society for Experimental
NeuroTherapeutics, 9(4), 717–727. https://doi.org/10.1007/s13311-012-0142-9
(#2)Fang, H., Tu, S., Sheng, J., & Shao, A. (2019). Depression in sleep disturbance: A review on
a bidirectional relationship, mechanisms and treatment. Journal of cellular and molecular
medicine, 23(4), 2324–2332. https://doi.org/10.1111/jcmm.14170
(#3) van Bronswijk, S. C., Lemmens, L., Keefe, J. R., Huibers, M., DeRubeis, R. J., &Peeters, F.
(2019). A prognostic index for long-term outcome after successful acute phase cognitive therapy
and interpersonal psychotherapy for major depressive disorder. Depression and anxiety, 36(3),
252–261. https://doi.org/10.1002/da.22868
(#4) Young, Nursing Standard. 28, 7, 43-51. doi: 10.7748/ns2013.10.28.7.43.e7577
(#5) Karyotaki, E., Riper, H., Twisk, J., Hoogendoorn, A., Kleiboer, A., Mira, A., Mackinnon,
A., Meyer, B., Botella, C., Littlewood, E., Andersson, G., Christensen, H., Klein, J. P., Schröder,
J., Bretón-López, J., Scheider, J., Griffiths, K., Farrer, L., Huibers, M. J., Phillips, R., …
Cuijpers, P. (2017). Efficacy of Self-guided Internet-Based Cognitive Behavioral Therapy in the
Treatment of Depressive Symptoms: A Meta-analysis of Individual Participant Data. JAMA
psychiatry, 74(4), 351–359. https://doi.org/10.1001/jamapsychiatry.2017.0044
(#6) Schultz, J., & Videbeck, S. (2013). Lippincott’s manual of psychiatric nursing care
plans (9th ed.). Wolters Kluwer/Lippincott Williams & Wilkins Health.
(#7) Hopelessness
(#8) Nursing Standard. 31, 50, 52-63. doi: 10.7748/ns.2017.e10909
(#9) AASW
(#10) https://onlinelibrary.wiley.com/doi/abs/10.1111/ijn.12250
#11) Armijo J. Social Impairment and Mental Health. Ann of Behav Sci 2017, 3:1 DOI:
10.21767/2471-7975.100004
11 | P a g e
(#1) Siebern, A. T., Suh, S., & Nowakowski, S. (2012). Non-pharmacological treatment of
insomnia. Neurotherapeutics : the journal of the American Society for Experimental
NeuroTherapeutics, 9(4), 717–727. https://doi.org/10.1007/s13311-012-0142-9
(#2)Fang, H., Tu, S., Sheng, J., & Shao, A. (2019). Depression in sleep disturbance: A review on
a bidirectional relationship, mechanisms and treatment. Journal of cellular and molecular
medicine, 23(4), 2324–2332. https://doi.org/10.1111/jcmm.14170
(#3) van Bronswijk, S. C., Lemmens, L., Keefe, J. R., Huibers, M., DeRubeis, R. J., &Peeters, F.
(2019). A prognostic index for long-term outcome after successful acute phase cognitive therapy
and interpersonal psychotherapy for major depressive disorder. Depression and anxiety, 36(3),
252–261. https://doi.org/10.1002/da.22868
(#4) Young, Nursing Standard. 28, 7, 43-51. doi: 10.7748/ns2013.10.28.7.43.e7577
(#5) Karyotaki, E., Riper, H., Twisk, J., Hoogendoorn, A., Kleiboer, A., Mira, A., Mackinnon,
A., Meyer, B., Botella, C., Littlewood, E., Andersson, G., Christensen, H., Klein, J. P., Schröder,
J., Bretón-López, J., Scheider, J., Griffiths, K., Farrer, L., Huibers, M. J., Phillips, R., …
Cuijpers, P. (2017). Efficacy of Self-guided Internet-Based Cognitive Behavioral Therapy in the
Treatment of Depressive Symptoms: A Meta-analysis of Individual Participant Data. JAMA
psychiatry, 74(4), 351–359. https://doi.org/10.1001/jamapsychiatry.2017.0044
(#6) Schultz, J., & Videbeck, S. (2013). Lippincott’s manual of psychiatric nursing care
plans (9th ed.). Wolters Kluwer/Lippincott Williams & Wilkins Health.
(#7) Hopelessness
(#8) Nursing Standard. 31, 50, 52-63. doi: 10.7748/ns.2017.e10909
(#9) AASW
(#10) https://onlinelibrary.wiley.com/doi/abs/10.1111/ijn.12250
#11) Armijo J. Social Impairment and Mental Health. Ann of Behav Sci 2017, 3:1 DOI:
10.21767/2471-7975.100004
11 | P a g e
(#12) Hammer-Helmich, L., Haro, J. M., Jönsson, B., Tanguy Melac, A., Di Nicola, S., Chollet,
J., Milea, D., Rive, B., &Saragoussi, D. (2018). Functional impairment in patients with major
depressive disorder: the 2-year PERFORM study. Neuropsychiatric disease and treatment, 14,
239–249. https://doi.org/10.2147/NDT.S146098
(#13) Wyder, M., Bland, R., Blythe, A., Matarasso, B., & Crompton, D. (2015). Therapeutic
relationships and involuntary treatment orders: service users' interactions with health-care
professionals on the ward. International journal of mental health nursing, 24(2), 181–189.
https://doi.org/10.1111/inm.12121
(#14) Lenora R, Kumar A, Uphoff E, Meader N, Furtado VA. Interventions for helping
people recognise early signs of recurrence in depression. Cochrane Database of Systematic
Reviews 2019, Issue 7. Art. No.: CD013383. DOI: 10.1002/14651858.CD013383.
(#15) Samantha Hartley, Jessica Raphael, Karina Lovell, Katherine Berry,
Effective nurse–patient relationships in mental health care: A systematic review of interventions
to improve the therapeutic alliance,
International Journal of Nursing Studies,
Volume 102,2020,103490,ISSN 0020-7489,https://doi.org/10.1016/j.ijnurstu.2019.103490.
(http://www.sciencedirect.com/science/article/pii/S0020748919302974)
https://www.health.qld.gov.au/news-events/news/what-is-mental-health-care-plan-how-to-
access-Queensland-Australia
Psychiatric and Mental Health Nursing, 4thEd. Chatswood, NSW: Elsevier, Australia Chapter 17
p 370
A guide what works for depression. Beyond Blue p 26
https://resources.beyondblue.org.au/prism/file?token=BL/0556
12 | P a g e
J., Milea, D., Rive, B., &Saragoussi, D. (2018). Functional impairment in patients with major
depressive disorder: the 2-year PERFORM study. Neuropsychiatric disease and treatment, 14,
239–249. https://doi.org/10.2147/NDT.S146098
(#13) Wyder, M., Bland, R., Blythe, A., Matarasso, B., & Crompton, D. (2015). Therapeutic
relationships and involuntary treatment orders: service users' interactions with health-care
professionals on the ward. International journal of mental health nursing, 24(2), 181–189.
https://doi.org/10.1111/inm.12121
(#14) Lenora R, Kumar A, Uphoff E, Meader N, Furtado VA. Interventions for helping
people recognise early signs of recurrence in depression. Cochrane Database of Systematic
Reviews 2019, Issue 7. Art. No.: CD013383. DOI: 10.1002/14651858.CD013383.
(#15) Samantha Hartley, Jessica Raphael, Karina Lovell, Katherine Berry,
Effective nurse–patient relationships in mental health care: A systematic review of interventions
to improve the therapeutic alliance,
International Journal of Nursing Studies,
Volume 102,2020,103490,ISSN 0020-7489,https://doi.org/10.1016/j.ijnurstu.2019.103490.
(http://www.sciencedirect.com/science/article/pii/S0020748919302974)
https://www.health.qld.gov.au/news-events/news/what-is-mental-health-care-plan-how-to-
access-Queensland-Australia
Psychiatric and Mental Health Nursing, 4thEd. Chatswood, NSW: Elsevier, Australia Chapter 17
p 370
A guide what works for depression. Beyond Blue p 26
https://resources.beyondblue.org.au/prism/file?token=BL/0556
12 | P a g e
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





