Mental Health Case Management Plan: Assessing Josh's Needs and Care
VerifiedAdded on 2022/08/24
|13
|1828
|30
Case Study
AI Summary
This case management plan details the assessment and support strategies for a 20-year-old patient named Josh, who is facing a complex set of challenges including bipolar disorder, substance abuse (alcohol and cannabis), homelessness, and family conflicts. The plan outlines areas of need such as housing/safety, mental health, physiological, physical, belongingness, and self-actualization, with specific goals, strategies, barriers, and risk management strategies for each area. The plan also discusses the process of establishing cooperation with the patient by providing access to medical information and fostering open communication. Furthermore, the plan addresses service identification, engagement, and the avoidance of service duplication, emphasizing the importance of accurate patient identification. The plan references the patient's issues and the family issues, including unemployment, emotional distress, substance abuse, and family conflict. The plan also provides a detailed overview of the patient's health issues, including bipolar disorder and risky behaviors. The document also includes references to relevant literature on mental health and case management.

MENTAL HEALTH CASE MANAGEMENT 1
MENTAL HEALTH CASE MANAGEMENT
Student’s Name
Institutional Affiliation
Date
MENTAL HEALTH CASE MANAGEMENT
Student’s Name
Institutional Affiliation
Date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
MENTAL HEALTH CASE MANAGEMENT 2
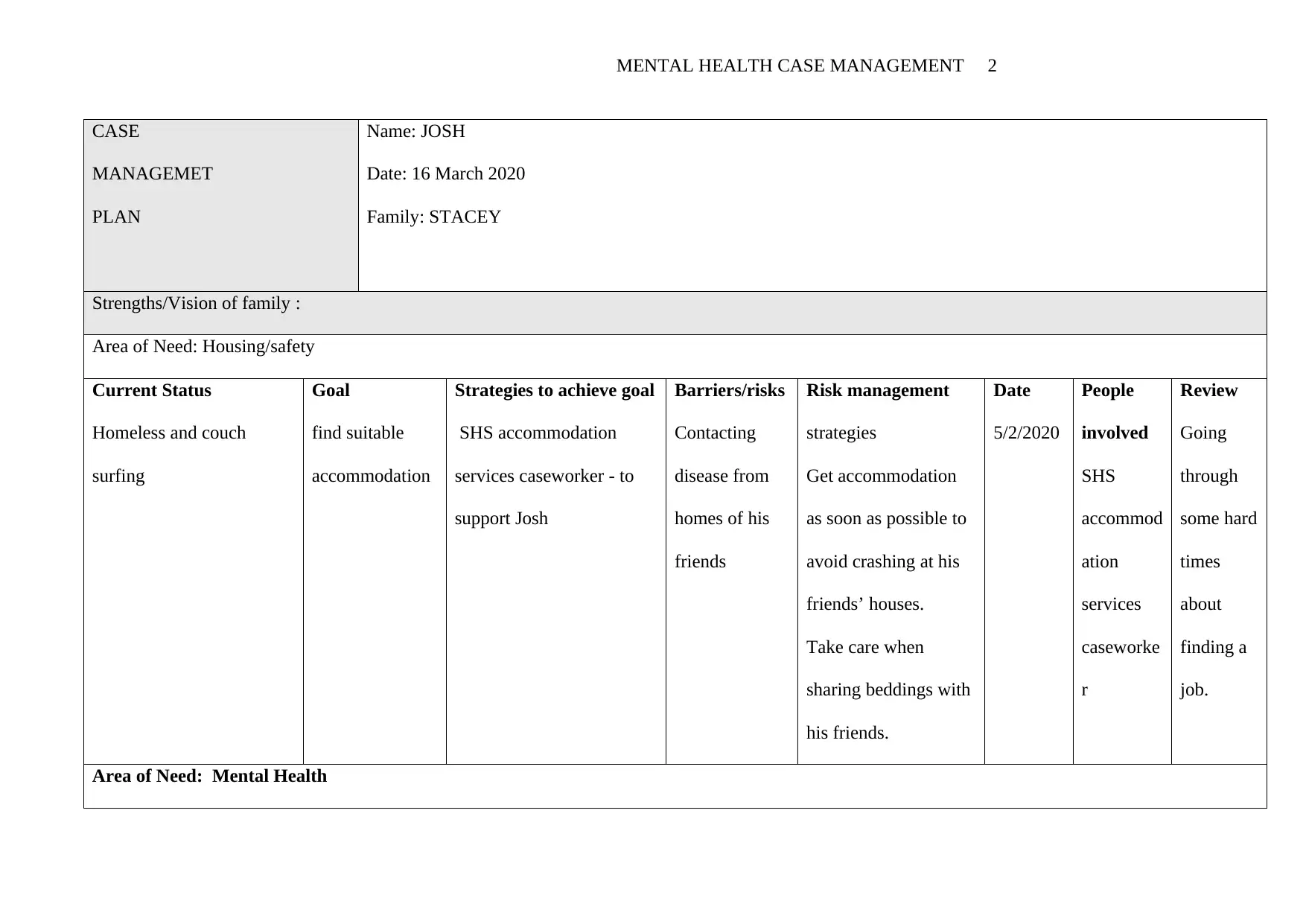
CASE
MANAGEMET
PLAN
Name: JOSH
Date: 16 March 2020
Family: STACEY
Strengths/Vision of family :
Area of Need: Housing/safety
Current Status
Homeless and couch
surfing
Goal
find suitable
accommodation
Strategies to achieve goal
SHS accommodation
services caseworker - to
support Josh
Barriers/risks
Contacting
disease from
homes of his
friends
Risk management
strategies
Get accommodation
as soon as possible to
avoid crashing at his
friends’ houses.
Take care when
sharing beddings with
his friends.
Date
5/2/2020
People
involved
SHS
accommod
ation
services
caseworke
r
Review
Going
through
some hard
times
about
finding a
job.
Area of Need: Mental Health
CASE
MANAGEMET
PLAN
Name: JOSH
Date: 16 March 2020
Family: STACEY
Strengths/Vision of family :
Area of Need: Housing/safety
Current Status
Homeless and couch
surfing
Goal
find suitable
accommodation
Strategies to achieve goal
SHS accommodation
services caseworker - to
support Josh
Barriers/risks
Contacting
disease from
homes of his
friends
Risk management
strategies
Get accommodation
as soon as possible to
avoid crashing at his
friends’ houses.
Take care when
sharing beddings with
his friends.
Date
5/2/2020
People
involved
SHS
accommod
ation
services
caseworke
r
Review
Going
through
some hard
times
about
finding a
job.
Area of Need: Mental Health
MENTAL HEALTH CASE MANAGEMENT 3
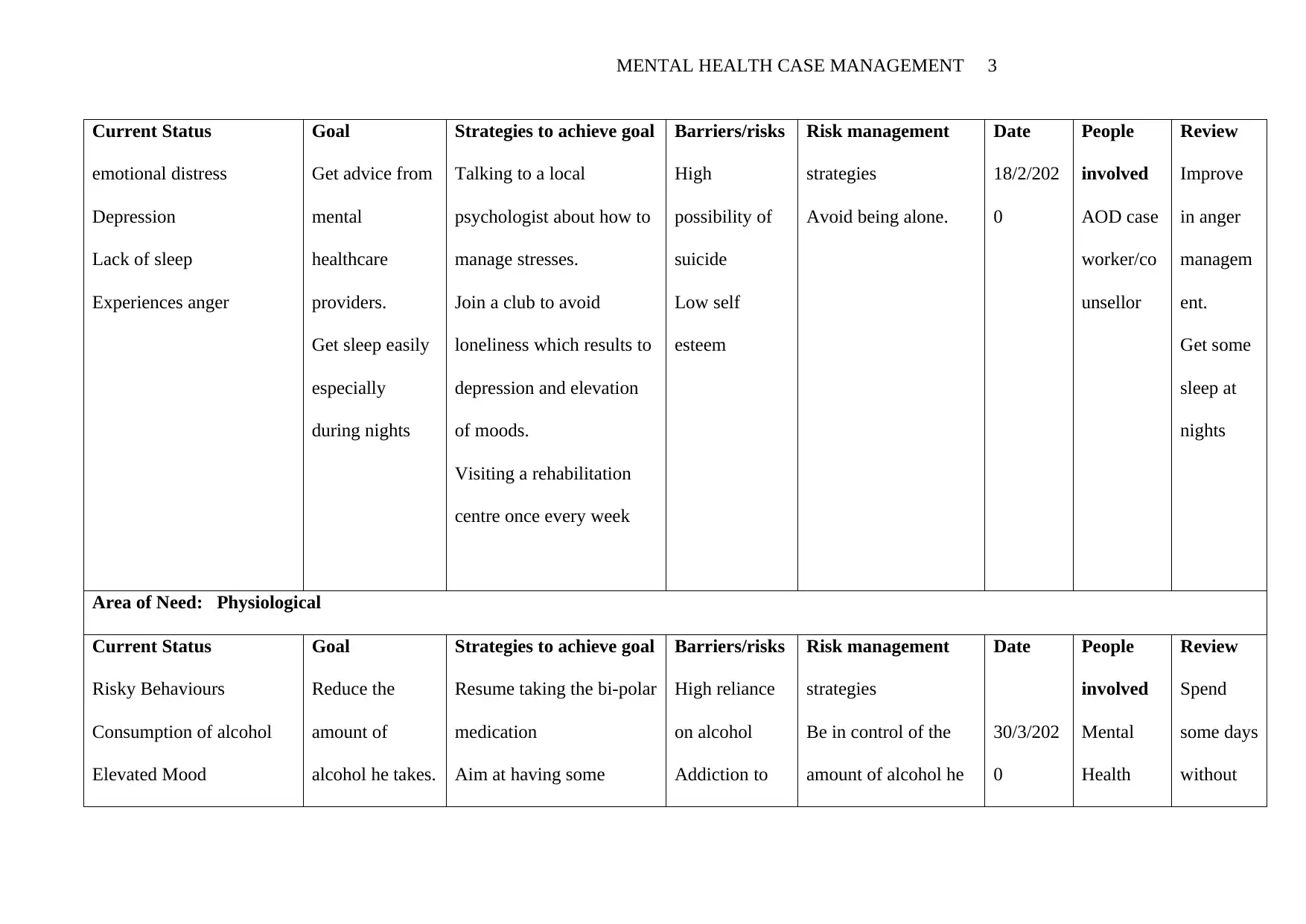
Current Status
emotional distress
Depression
Lack of sleep
Experiences anger
Goal
Get advice from
mental
healthcare
providers.
Get sleep easily
especially
during nights
Strategies to achieve goal
Talking to a local
psychologist about how to
manage stresses.
Join a club to avoid
loneliness which results to
depression and elevation
of moods.
Visiting a rehabilitation
centre once every week
Barriers/risks
High
possibility of
suicide
Low self
esteem
Risk management
strategies
Avoid being alone.
Date
18/2/202
0
People
involved
AOD case
worker/co
unsellor
Review
Improve
in anger
managem
ent.
Get some
sleep at
nights
Area of Need: Physiological
Current Status
Risky Behaviours
Consumption of alcohol
Elevated Mood
Goal
Reduce the
amount of
alcohol he takes.
Strategies to achieve goal
Resume taking the bi-polar
medication
Aim at having some
Barriers/risks
High reliance
on alcohol
Addiction to
Risk management
strategies
Be in control of the
amount of alcohol he
Date
30/3/202
0
People
involved
Mental
Health
Review
Spend
some days
without
Current Status
emotional distress
Depression
Lack of sleep
Experiences anger
Goal
Get advice from
mental
healthcare
providers.
Get sleep easily
especially
during nights
Strategies to achieve goal
Talking to a local
psychologist about how to
manage stresses.
Join a club to avoid
loneliness which results to
depression and elevation
of moods.
Visiting a rehabilitation
centre once every week
Barriers/risks
High
possibility of
suicide
Low self
esteem
Risk management
strategies
Avoid being alone.
Date
18/2/202
0
People
involved
AOD case
worker/co
unsellor
Review
Improve
in anger
managem
ent.
Get some
sleep at
nights
Area of Need: Physiological
Current Status
Risky Behaviours
Consumption of alcohol
Elevated Mood
Goal
Reduce the
amount of
alcohol he takes.
Strategies to achieve goal
Resume taking the bi-polar
medication
Aim at having some
Barriers/risks
High reliance
on alcohol
Addiction to
Risk management
strategies
Be in control of the
amount of alcohol he
Date
30/3/202
0
People
involved
Mental
Health
Review
Spend
some days
without
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
MENTAL HEALTH CASE MANAGEMENT 4
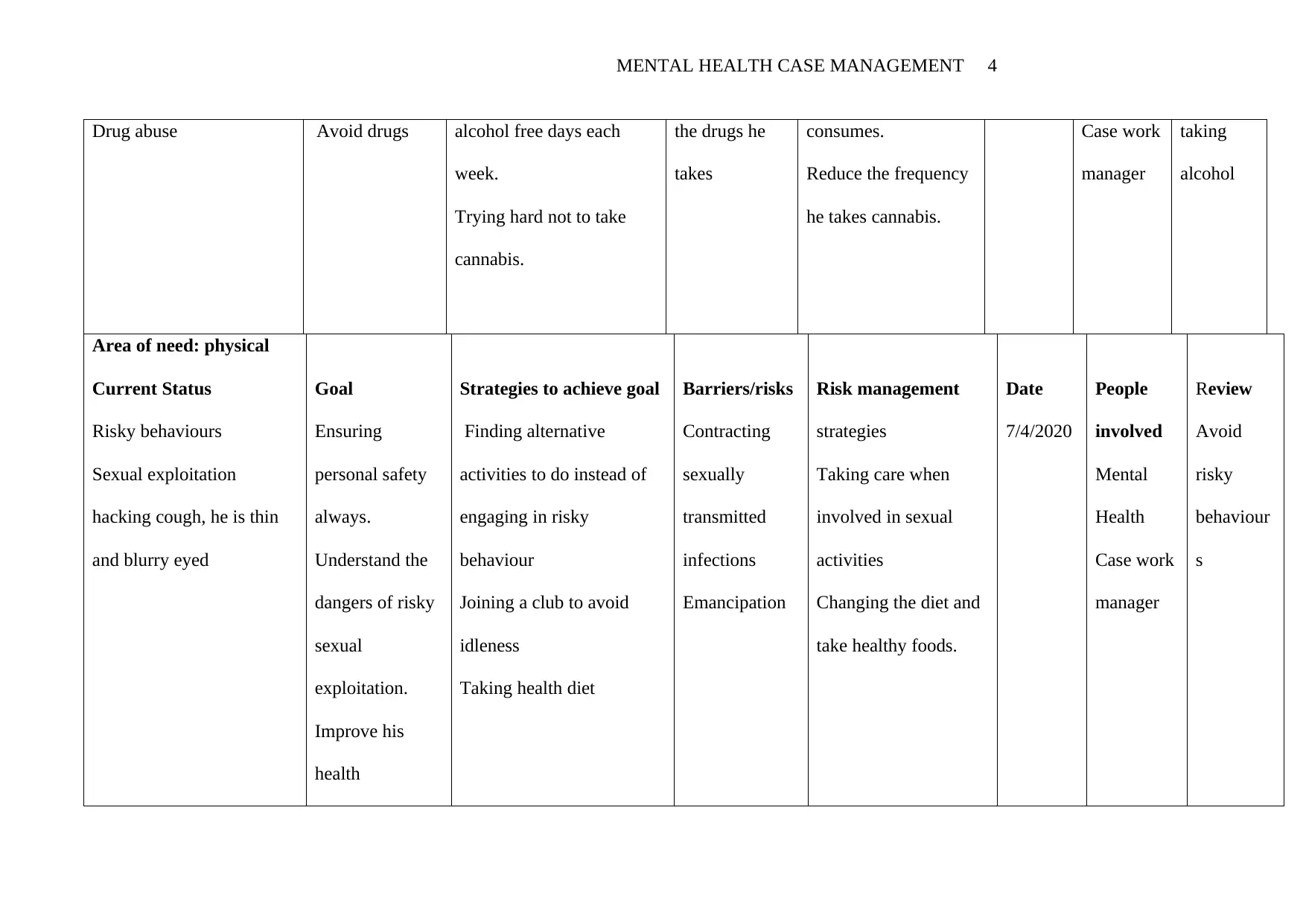
Drug abuse Avoid drugs alcohol free days each
week.
Trying hard not to take
cannabis.
the drugs he
takes
consumes.
Reduce the frequency
he takes cannabis.
Case work
manager
taking
alcohol
Area of need: physical
Current Status
Risky behaviours
Sexual exploitation
hacking cough, he is thin
and blurry eyed
Goal
Ensuring
personal safety
always.
Understand the
dangers of risky
sexual
exploitation.
Improve his
health
Strategies to achieve goal
Finding alternative
activities to do instead of
engaging in risky
behaviour
Joining a club to avoid
idleness
Taking health diet
Barriers/risks
Contracting
sexually
transmitted
infections
Emancipation
Risk management
strategies
Taking care when
involved in sexual
activities
Changing the diet and
take healthy foods.
Date
7/4/2020
People
involved
Mental
Health
Case work
manager
Review
Avoid
risky
behaviour
s
Drug abuse Avoid drugs alcohol free days each
week.
Trying hard not to take
cannabis.
the drugs he
takes
consumes.
Reduce the frequency
he takes cannabis.
Case work
manager
taking
alcohol
Area of need: physical
Current Status
Risky behaviours
Sexual exploitation
hacking cough, he is thin
and blurry eyed
Goal
Ensuring
personal safety
always.
Understand the
dangers of risky
sexual
exploitation.
Improve his
health
Strategies to achieve goal
Finding alternative
activities to do instead of
engaging in risky
behaviour
Joining a club to avoid
idleness
Taking health diet
Barriers/risks
Contracting
sexually
transmitted
infections
Emancipation
Risk management
strategies
Taking care when
involved in sexual
activities
Changing the diet and
take healthy foods.
Date
7/4/2020
People
involved
Mental
Health
Case work
manager
Review
Avoid
risky
behaviour
s
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
MENTAL HEALTH CASE MANAGEMENT 5
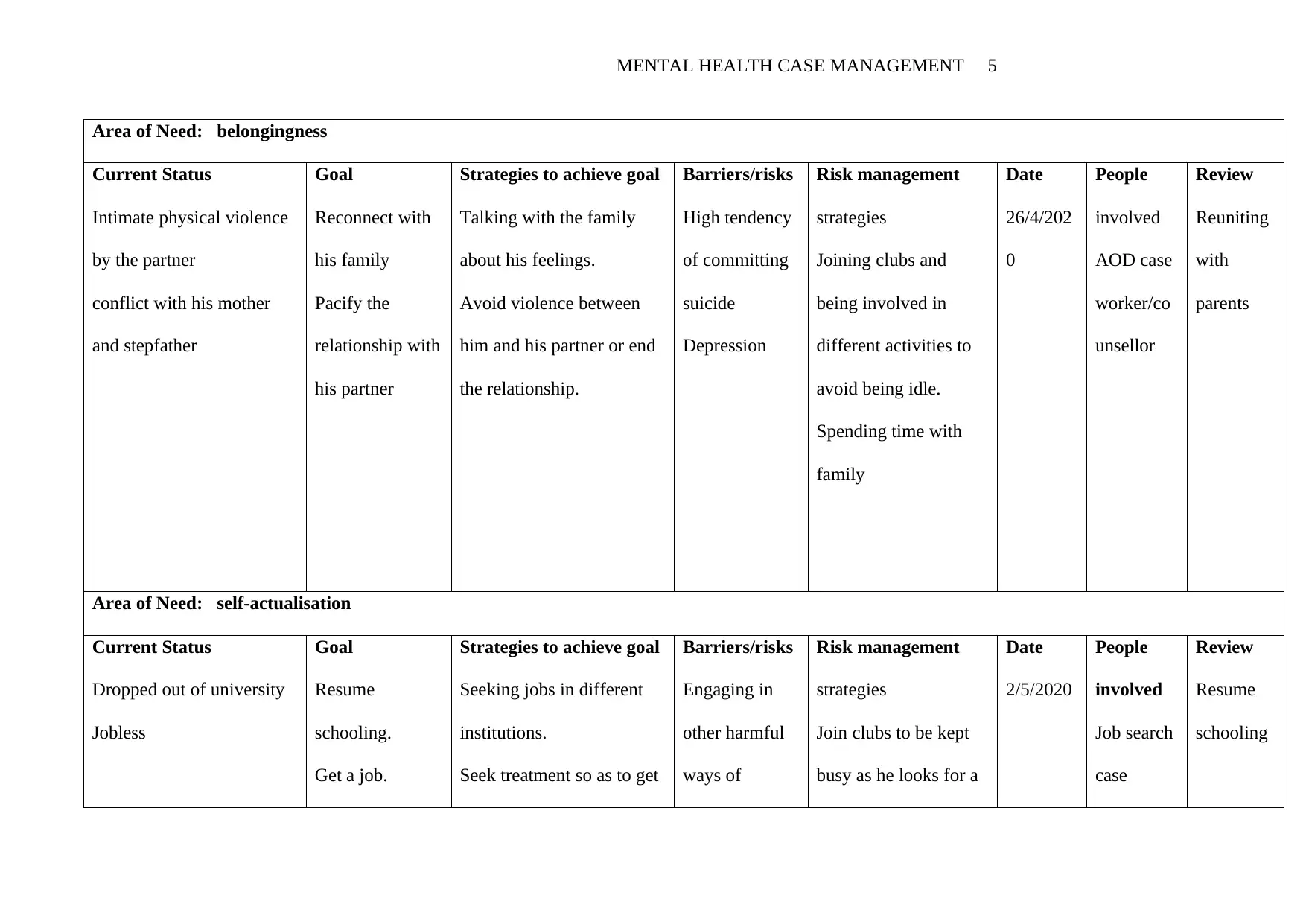
Area of Need: belongingness
Current Status
Intimate physical violence
by the partner
conflict with his mother
and stepfather
Goal
Reconnect with
his family
Pacify the
relationship with
his partner
Strategies to achieve goal
Talking with the family
about his feelings.
Avoid violence between
him and his partner or end
the relationship.
Barriers/risks
High tendency
of committing
suicide
Depression
Risk management
strategies
Joining clubs and
being involved in
different activities to
avoid being idle.
Spending time with
family
Date
26/4/202
0
People
involved
AOD case
worker/co
unsellor
Review
Reuniting
with
parents
Area of Need: self-actualisation
Current Status
Dropped out of university
Jobless
Goal
Resume
schooling.
Get a job.
Strategies to achieve goal
Seeking jobs in different
institutions.
Seek treatment so as to get
Barriers/risks
Engaging in
other harmful
ways of
Risk management
strategies
Join clubs to be kept
busy as he looks for a
Date
2/5/2020
People
involved
Job search
case
Review
Resume
schooling
Area of Need: belongingness
Current Status
Intimate physical violence
by the partner
conflict with his mother
and stepfather
Goal
Reconnect with
his family
Pacify the
relationship with
his partner
Strategies to achieve goal
Talking with the family
about his feelings.
Avoid violence between
him and his partner or end
the relationship.
Barriers/risks
High tendency
of committing
suicide
Depression
Risk management
strategies
Joining clubs and
being involved in
different activities to
avoid being idle.
Spending time with
family
Date
26/4/202
0
People
involved
AOD case
worker/co
unsellor
Review
Reuniting
with
parents
Area of Need: self-actualisation
Current Status
Dropped out of university
Jobless
Goal
Resume
schooling.
Get a job.
Strategies to achieve goal
Seeking jobs in different
institutions.
Seek treatment so as to get
Barriers/risks
Engaging in
other harmful
ways of
Risk management
strategies
Join clubs to be kept
busy as he looks for a
Date
2/5/2020
People
involved
Job search
case
Review
Resume
schooling
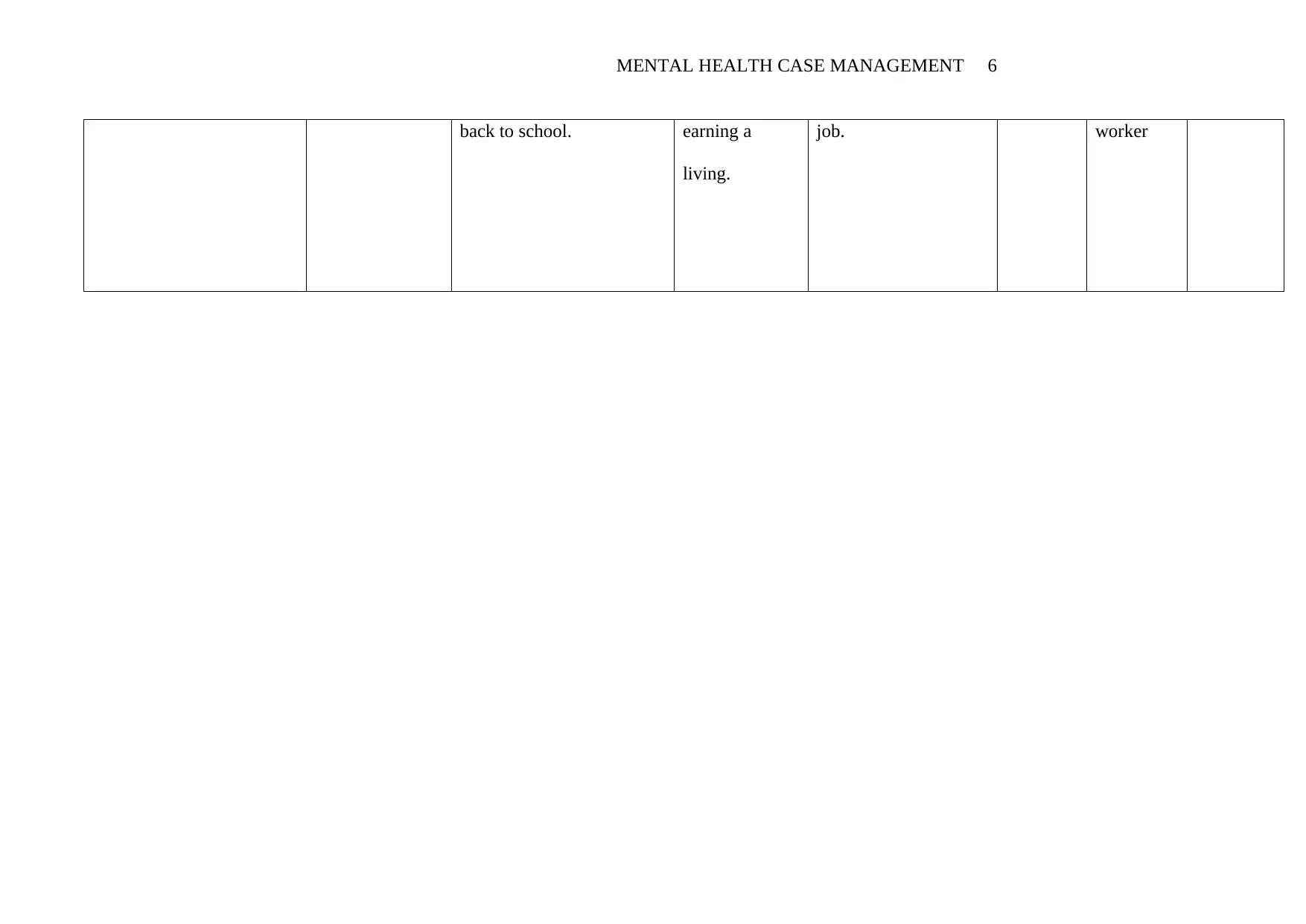
MENTAL HEALTH CASE MANAGEMENT 6
back to school. earning a
living.
job. worker
back to school. earning a
living.
job. worker
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
MENTAL HEALTH CASE MANAGEMENT 7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
MENTAL HEALTH CASE MANAGEMENT 8
Process of establishing and explaining the function of the co-ordination role with
the person.
The Quality Chasm's health care quality framework addresses the need for better care
coordination between the health provider and the patient as well as the provider
communication and collaboration to achieve the above plan. To establish cooperation with
the patient I would give him unfettered access to his own medical information and clinical
knowledge. To achieve this I have to have effective communication with the patient and
share all the information that he should have for the proper cooperation during the execution
of the whole plan. Informal communication with the patient is also important in enhancing
cooperation with the patient. This would help in creating trust with my patient. I would
achieve this by spending more time with the patients or visiting the patient frequently if time
is limited. Care coordination is the outcome of effective collaboration between the care
provider and the patient (Unutzer, Harbin, and Schoenbaum& Druss 2013). Establishment of
cooperation does not waste the patient's time or the resources of the health care system.
According to Bishop, Press, Keyhan &Pincus (2014), it promotes accurate diagnosis and
treatment because the patient is always aware of the actions taken by the health provider. This
makes cooperation between the patient and the health care provider very vital
Process of identifying and engaging services in line with the case management plan.
To identify, source and engage the services to the patient in line to this management
plan I would consider the condition of the patient. Different services to be offered depend on
the health condition the patient involved is in. it is always important to start by knowing the
patient well and the problems he has been facing. The information about the patient can be
got from the patient through direct chatting or through observation of the patient. The family
and friends of the patient are also very important when getting to know the patient ( Kroenke
Process of establishing and explaining the function of the co-ordination role with
the person.
The Quality Chasm's health care quality framework addresses the need for better care
coordination between the health provider and the patient as well as the provider
communication and collaboration to achieve the above plan. To establish cooperation with
the patient I would give him unfettered access to his own medical information and clinical
knowledge. To achieve this I have to have effective communication with the patient and
share all the information that he should have for the proper cooperation during the execution
of the whole plan. Informal communication with the patient is also important in enhancing
cooperation with the patient. This would help in creating trust with my patient. I would
achieve this by spending more time with the patients or visiting the patient frequently if time
is limited. Care coordination is the outcome of effective collaboration between the care
provider and the patient (Unutzer, Harbin, and Schoenbaum& Druss 2013). Establishment of
cooperation does not waste the patient's time or the resources of the health care system.
According to Bishop, Press, Keyhan &Pincus (2014), it promotes accurate diagnosis and
treatment because the patient is always aware of the actions taken by the health provider. This
makes cooperation between the patient and the health care provider very vital
Process of identifying and engaging services in line with the case management plan.
To identify, source and engage the services to the patient in line to this management
plan I would consider the condition of the patient. Different services to be offered depend on
the health condition the patient involved is in. it is always important to start by knowing the
patient well and the problems he has been facing. The information about the patient can be
got from the patient through direct chatting or through observation of the patient. The family
and friends of the patient are also very important when getting to know the patient ( Kroenke
MENTAL HEALTH CASE MANAGEMENT 9
& Unutzer 2017). After I have all information it becomes easy to identify the services to
apply to the patient. . It also helps to observe how the patient responds to the first services
and this is essential in determining the services to be offered next. I would also assess the
seriousness of the patient’s condition so as to determine the best services to be offered to the
patient.
Reducing service duplication
Precise patient ID consistently has been basic to giving the best patient consideration. "Yet,
in the present computerized clinical record world, it is very hard to provide best services to
patients especially if the names are regular (Mechanic 2012). Regardless of developing
spotlight on the issue of copy clinical records, the issue proceeds. Druss, Esenwein, &
Compton (2010) says that clinics everywhere throughout the world are battling with this
overwhelming problem as well as the wellbeing and money related consequences that can
happen if a patient is really misidentified. 7-10% of patients are misidentified when their
Enterprise Master Patient Index (EMPI) and electronic wellbeing records (EHR) are looked
(Katon &Unutzer 2013). Of this gathering, 9% experience an antagonistic occasion. As per a
report directed by the American Health Information Management Association (AHIMA),
somewhere in the range of 8% and 12% of EHR records are duplicates. Still more patients
may endure clinical blunders because of missing wellbeing data in their records, or overlays
that blend various patients' records together.
To avoid service duplication when dealing with Josh, I would abstain from hurrying
during the enlistment procedure, in any event and when patients are in numbers. This helps in
avoiding confusion that happens when the patients to be attendant are numerous (Schmidt,
Worrack & Korff 2016). I also would also confirm the patient’s names from his documents as
well as associating with the patient severally so as to know the names of the patient from
himself. This is very important especially if there are several patients with similar names. In
& Unutzer 2017). After I have all information it becomes easy to identify the services to
apply to the patient. . It also helps to observe how the patient responds to the first services
and this is essential in determining the services to be offered next. I would also assess the
seriousness of the patient’s condition so as to determine the best services to be offered to the
patient.
Reducing service duplication
Precise patient ID consistently has been basic to giving the best patient consideration. "Yet,
in the present computerized clinical record world, it is very hard to provide best services to
patients especially if the names are regular (Mechanic 2012). Regardless of developing
spotlight on the issue of copy clinical records, the issue proceeds. Druss, Esenwein, &
Compton (2010) says that clinics everywhere throughout the world are battling with this
overwhelming problem as well as the wellbeing and money related consequences that can
happen if a patient is really misidentified. 7-10% of patients are misidentified when their
Enterprise Master Patient Index (EMPI) and electronic wellbeing records (EHR) are looked
(Katon &Unutzer 2013). Of this gathering, 9% experience an antagonistic occasion. As per a
report directed by the American Health Information Management Association (AHIMA),
somewhere in the range of 8% and 12% of EHR records are duplicates. Still more patients
may endure clinical blunders because of missing wellbeing data in their records, or overlays
that blend various patients' records together.
To avoid service duplication when dealing with Josh, I would abstain from hurrying
during the enlistment procedure, in any event and when patients are in numbers. This helps in
avoiding confusion that happens when the patients to be attendant are numerous (Schmidt,
Worrack & Korff 2016). I also would also confirm the patient’s names from his documents as
well as associating with the patient severally so as to know the names of the patient from
himself. This is very important especially if there are several patients with similar names. In
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

MENTAL HEALTH CASE MANAGEMENT 10
addition, keeping the health records of the patient safely and organized would ensure that the
records are easily accessed when needed and this would enable different health personnel to
attend to the patient easily.
addition, keeping the health records of the patient safely and organized would ensure that the
records are easily accessed when needed and this would enable different health personnel to
attend to the patient easily.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
MENTAL HEALTH CASE MANAGEMENT 11
References
Bishop, T., Press, m., Keyhan, S. &Pincus, A. 2014. Acceptance of insurance by psychiatrists
And the implications for access to mental health care. JAMA Psychiatry [Online]
Available at :< https://pubmed.ncbi.nlm.nih.gov/24337499/ > [Accessed 21 March
2020].
Croft, B. &Parish, S. 2013. Care integration in the patient protection and affordable care act:
Implications for behavioral health. Administration and policy in mental health and
mental health services research [Online] Available at :<
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3888027/> [Accessed 21 march
2020].
Druss, B., Esenwein, S. & Compton, M. 2010. A randomized trial of medical care
management
For community mental health settings: the primary care access, referral and evaluation
(PCARE) study. American journal of psychiatry [Online] Available at
<https://www.semanticscholar.org/paper/A-randomized-trial-of-medical-care-
management-for-Druss-Esenwein/5f5ac65b76f3d99b8aa749666c2290b34936bb5d>
[Accessed 21 March 2020].
Katon, W. &Unutzer, J. 2013. Health reform and the affordable care act: the importance
Of mental health treatment to achieving the triple aim. Journal of psychosomatic
research[Online]Availableat:<https://scholar.google.com/scholar?
q=health+reform+and+affordable+care+act+
%3B+the+importance&hl=en&as_sdt=0&as_vis=1&oi=scholart#d=gs_qabs&u=
%23p%3DhgvmC_YIZtAJ> [Accessed 21 March 2020].
Kroenke, K. & Unutzer, J. 2017. Closing the false divide: sustainable approaches to
References
Bishop, T., Press, m., Keyhan, S. &Pincus, A. 2014. Acceptance of insurance by psychiatrists
And the implications for access to mental health care. JAMA Psychiatry [Online]
Available at :< https://pubmed.ncbi.nlm.nih.gov/24337499/ > [Accessed 21 March
2020].
Croft, B. &Parish, S. 2013. Care integration in the patient protection and affordable care act:
Implications for behavioral health. Administration and policy in mental health and
mental health services research [Online] Available at :<
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3888027/> [Accessed 21 march
2020].
Druss, B., Esenwein, S. & Compton, M. 2010. A randomized trial of medical care
management
For community mental health settings: the primary care access, referral and evaluation
(PCARE) study. American journal of psychiatry [Online] Available at
<https://www.semanticscholar.org/paper/A-randomized-trial-of-medical-care-
management-for-Druss-Esenwein/5f5ac65b76f3d99b8aa749666c2290b34936bb5d>
[Accessed 21 March 2020].
Katon, W. &Unutzer, J. 2013. Health reform and the affordable care act: the importance
Of mental health treatment to achieving the triple aim. Journal of psychosomatic
research[Online]Availableat:<https://scholar.google.com/scholar?
q=health+reform+and+affordable+care+act+
%3B+the+importance&hl=en&as_sdt=0&as_vis=1&oi=scholart#d=gs_qabs&u=
%23p%3DhgvmC_YIZtAJ> [Accessed 21 March 2020].
Kroenke, K. & Unutzer, J. 2017. Closing the false divide: sustainable approaches to
MENTAL HEALTH CASE MANAGEMENT 12
Integrating mental health services into primary care. Journal of general internal
medicine [Online] Available at :< https://pubmed.ncbi.nlm.nih.gov/28243873/>
[Accessed 21 March 2020].
Mechanic, D. 2012. Seizing opportunities under the affordable care act for transforming the
Mental and behavioral health system. Health affairs [Online] Available at :<
https://pubmed.ncbi.nlm.nih.gov/22323168/> [Accessed 21 March 2020].
Schmidt, K., Worrack, S. & Korff, M. 2016. Effect of a primary care management
Intervention on mental health- related quality of life among survivors of sepsis: a
randomized clinical trial. JAMA Psychiatry [Online] Available at :<
https://pubmed.ncbi.nlm.nih.gov/27367877/> [Accessed 21 March 2020].
Unutzer, J., Harbin, H., Schoenbaum, M. & Druss, D. 2013. The collaborative care model; an
Approach for integrating physical and mental health care in Medicaid health homes.
Health home information resource center [Online] Available
at:<https://scholar.google.com/scholar?q=the+collaborative+care+model+
%3Ban+approach+for+integrating&hl=en&as_sdt=0&as_vis=1&oi=scholart#d=gs_q
abs&u=%23p%3Duho48wOMlKcJ>[Accessed 21 March 2020].
Integrating mental health services into primary care. Journal of general internal
medicine [Online] Available at :< https://pubmed.ncbi.nlm.nih.gov/28243873/>
[Accessed 21 March 2020].
Mechanic, D. 2012. Seizing opportunities under the affordable care act for transforming the
Mental and behavioral health system. Health affairs [Online] Available at :<
https://pubmed.ncbi.nlm.nih.gov/22323168/> [Accessed 21 March 2020].
Schmidt, K., Worrack, S. & Korff, M. 2016. Effect of a primary care management
Intervention on mental health- related quality of life among survivors of sepsis: a
randomized clinical trial. JAMA Psychiatry [Online] Available at :<
https://pubmed.ncbi.nlm.nih.gov/27367877/> [Accessed 21 March 2020].
Unutzer, J., Harbin, H., Schoenbaum, M. & Druss, D. 2013. The collaborative care model; an
Approach for integrating physical and mental health care in Medicaid health homes.
Health home information resource center [Online] Available
at:<https://scholar.google.com/scholar?q=the+collaborative+care+model+
%3Ban+approach+for+integrating&hl=en&as_sdt=0&as_vis=1&oi=scholart#d=gs_q
abs&u=%23p%3Duho48wOMlKcJ>[Accessed 21 March 2020].
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.


