Enhance Mental Health of Vulnerable Patients within BMI Healthcare in the UK
VerifiedAdded on 2023/06/06
|21
|8270
|395
AI Summary
This article discusses the notion of mental health of vulnerable patients within BMI Healthcare in the UK, the causes and impact that render upon mental health of vulnerable patients within BMI Healthcare in the UK, and the intervention or strategies used by healthcare leaders and care nurses to reduce impact and enhance mental health of vulnerable patients.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
Service Innovation and
Improvement Project
Improvement Project
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Table of Contents
TITLE..............................................................................................................................................3
INTRODUCTION...........................................................................................................................3
AIM..................................................................................................................................................4
OBJECTIVE....................................................................................................................................4
LITERATURE REVIEW................................................................................................................4
Notion of mental health of vulnerable patient within BMI Healthcare in the UK.................4
Causes and impact that render upon mental health of vulnerable patient within BMI
Healthcare in the UK..............................................................................................................6
Intervention or strategies used by healthcare leaders and care nurses to reduce impact and
enhance mental health of vulnerable patients.........................................................................9
THEORETICAL FRAMEWORK.................................................................................................11
Project life cycle (PLC)........................................................................................................11
Kotter’s 8 step Change Model..............................................................................................13
Contingency theory..............................................................................................................14
PROJECT PLAN METHODOLOGY...........................................................................................15
Gantt chart............................................................................................................................15
Scope....................................................................................................................................16
Resources..............................................................................................................................16
Communication....................................................................................................................16
Risk.......................................................................................................................................17
CONCLUSION..............................................................................................................................17
REFERENCES..............................................................................................................................18
TITLE..............................................................................................................................................3
INTRODUCTION...........................................................................................................................3
AIM..................................................................................................................................................4
OBJECTIVE....................................................................................................................................4
LITERATURE REVIEW................................................................................................................4
Notion of mental health of vulnerable patient within BMI Healthcare in the UK.................4
Causes and impact that render upon mental health of vulnerable patient within BMI
Healthcare in the UK..............................................................................................................6
Intervention or strategies used by healthcare leaders and care nurses to reduce impact and
enhance mental health of vulnerable patients.........................................................................9
THEORETICAL FRAMEWORK.................................................................................................11
Project life cycle (PLC)........................................................................................................11
Kotter’s 8 step Change Model..............................................................................................13
Contingency theory..............................................................................................................14
PROJECT PLAN METHODOLOGY...........................................................................................15
Gantt chart............................................................................................................................15
Scope....................................................................................................................................16
Resources..............................................................................................................................16
Communication....................................................................................................................16
Risk.......................................................................................................................................17
CONCLUSION..............................................................................................................................17
REFERENCES..............................................................................................................................18
TITLE
"Enhance Mental health of vulnerable patient within BMI Healthcare in the UK."
INTRODUCTION
There are large number of patients who are not able to take care of their health and should
not able to protect themselves within UK. This lead to create the situation of vulnerability to that
patient due to not able to protect themselves towards any risk of harm or neglect. Vulnerable
patient is the one who are highly exposed towards any type of harm or neglect within the
healthcare premises. When any patient is not able to take care of themselves and may get highly
exposed towards any harm or neglect and respond against those. These may lead to create the
risk of vulnerability to them. Here, vulnerable patient is not able to protect themselves that may
lead to create high impact on their safety (Stevens, 2020). This can also lead to impact their
mental health which are highly associated with their proper care. Vulnerable patient is at the
higher risk of getting declining mental health in which they are not able to protect themselves
from any type of harm or neglect. This impact their physical as well as their mental health. In
this, each and every healthcare premises need to take care of the better and effective response
towards the taking care of the better response in proper manner. BMI healthcare refers to the
independent provider in healthcare provide that are offered healthcare treatment to patient, NHS
patient and injured patient. It has 54 private healthcare organization that offer different
healthcare facilities within UK. It has headquarters in London. In December 2019, it acquired by
Circle Health and was replaced by Circle Health Group in 2022 (Paramore and et. al., 2020).
BMI healthcare have the responsibility to take care of their vulnerable patient and should take
effective step towards reducing the risk of declining their mental health and should take care
about their improved mental health. In this, BMI healthcare need to make some policies and
should be implemented effectively that can help to provide better and effective response towards
it. This can also help in getting better care for their vulnerable patient that can enable them to
improve their physical as well as their mental health in better way. Vulnerable patient should be
effectively taken care and all the nursing staff should ensure that they should not get any type of
neglect that may impact their mental and physical health. In this, it is also necessary to take
effective initiative that can be effective and may help vulnerable patient to get better and
effective care (Livingston and et. al., 2020). This can also enable them to improve in their mental
"Enhance Mental health of vulnerable patient within BMI Healthcare in the UK."
INTRODUCTION
There are large number of patients who are not able to take care of their health and should
not able to protect themselves within UK. This lead to create the situation of vulnerability to that
patient due to not able to protect themselves towards any risk of harm or neglect. Vulnerable
patient is the one who are highly exposed towards any type of harm or neglect within the
healthcare premises. When any patient is not able to take care of themselves and may get highly
exposed towards any harm or neglect and respond against those. These may lead to create the
risk of vulnerability to them. Here, vulnerable patient is not able to protect themselves that may
lead to create high impact on their safety (Stevens, 2020). This can also lead to impact their
mental health which are highly associated with their proper care. Vulnerable patient is at the
higher risk of getting declining mental health in which they are not able to protect themselves
from any type of harm or neglect. This impact their physical as well as their mental health. In
this, each and every healthcare premises need to take care of the better and effective response
towards the taking care of the better response in proper manner. BMI healthcare refers to the
independent provider in healthcare provide that are offered healthcare treatment to patient, NHS
patient and injured patient. It has 54 private healthcare organization that offer different
healthcare facilities within UK. It has headquarters in London. In December 2019, it acquired by
Circle Health and was replaced by Circle Health Group in 2022 (Paramore and et. al., 2020).
BMI healthcare have the responsibility to take care of their vulnerable patient and should take
effective step towards reducing the risk of declining their mental health and should take care
about their improved mental health. In this, BMI healthcare need to make some policies and
should be implemented effectively that can help to provide better and effective response towards
it. This can also help in getting better care for their vulnerable patient that can enable them to
improve their physical as well as their mental health in better way. Vulnerable patient should be
effectively taken care and all the nursing staff should ensure that they should not get any type of
neglect that may impact their mental and physical health. In this, it is also necessary to take
effective initiative that can be effective and may help vulnerable patient to get better and
effective care (Livingston and et. al., 2020). This can also enable them to improve in their mental
health that are associated with providing better environment within the BMI healthcare. It is
essential to take different measures and initiative that are effective and may lead to create high
impact on their mental health improvement. BMI healthcare should ensure about safeguarding of
their vulnerable patient which should be highly effective and may help in taking care of their
health that includes their mental health. Safeguarding can be effective which help to ensure that
individual is safe at any place and are not exposed to any type of harm or neglect. In this, it is
also need to take care that any individual should not harm their patient that can help to provide
them better physical environment at the healthcare premises. This can also enable patient to get
some improvement in their mental health. There are many patients who are not good at taking
care of themselves which is due to their bad mental health (Gilbody and et. al., 2019). There is
discussion about the enhancing mental health of vulnerable patient within BMI healthcare in UK.
There is are discussion about the notion of mental health of vulnerable patient, evaluation and
causes with their impact on vulnerable people mental health within UK. There is also discussion
about the intervention or strategies which can be effective in enhancing mental health of
vulnerable patient in UK. In this, BMI healthcare should take care of their health and ensure their
safeguarding that can be effective and may help in improving their mental health in better way.
AIM
To enhance mental health of vulnerable patients within BMI Healthcare in the UK.
OBJECTIVE
To analyse the notion of mental health of vulnerable patient within BMI Healthcare in the
UK
To evaluate the causes and impact that render upon mental health of vulnerable patient
within BMI Healthcare in the UK.
To examine the intervention or strategies used by healthcare leaders and care nurses to
reduce impact and enhance mental health of vulnerable patients.
LITERATURE REVIEW
Notion of mental health of vulnerable patient within BMI Healthcare in the UK
there are large number of patients who are not able to take care of their health and protect
themselves from any type of harm or neglect. They are also not able to make their own decision
which can be effective and may help them in getting better health support. These are the patient
essential to take different measures and initiative that are effective and may lead to create high
impact on their mental health improvement. BMI healthcare should ensure about safeguarding of
their vulnerable patient which should be highly effective and may help in taking care of their
health that includes their mental health. Safeguarding can be effective which help to ensure that
individual is safe at any place and are not exposed to any type of harm or neglect. In this, it is
also need to take care that any individual should not harm their patient that can help to provide
them better physical environment at the healthcare premises. This can also enable patient to get
some improvement in their mental health. There are many patients who are not good at taking
care of themselves which is due to their bad mental health (Gilbody and et. al., 2019). There is
discussion about the enhancing mental health of vulnerable patient within BMI healthcare in UK.
There is are discussion about the notion of mental health of vulnerable patient, evaluation and
causes with their impact on vulnerable people mental health within UK. There is also discussion
about the intervention or strategies which can be effective in enhancing mental health of
vulnerable patient in UK. In this, BMI healthcare should take care of their health and ensure their
safeguarding that can be effective and may help in improving their mental health in better way.
AIM
To enhance mental health of vulnerable patients within BMI Healthcare in the UK.
OBJECTIVE
To analyse the notion of mental health of vulnerable patient within BMI Healthcare in the
UK
To evaluate the causes and impact that render upon mental health of vulnerable patient
within BMI Healthcare in the UK.
To examine the intervention or strategies used by healthcare leaders and care nurses to
reduce impact and enhance mental health of vulnerable patients.
LITERATURE REVIEW
Notion of mental health of vulnerable patient within BMI Healthcare in the UK
there are large number of patients who are not able to take care of their health and protect
themselves from any type of harm or neglect. They are also not able to make their own decision
which can be effective and may help them in getting better health support. These are the patient
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
are vulnerable and may need better assistance and care that can allow to help them in getting
better mental health. There is higher chance that vulnerable patient is mentally weak or may not
have stable mental condition which lead them to risk of higher chance of vulnerability. There are
large number of patients who need proper assistance and care that can help to avoid the risk of
getting negative mental health impact (Hudon and et. al., 2018). Additionally, there is also need
to ensure about getting better response which are associated with ensuring about taking care of
good health. There is various reason due to which healthcare premises are not perform well
towards caring such type of vulnerable patient. Every healthcare provider should ensure about
taking care of each patient especially vulnerable patient (Cénat and et. al., 2020). In this, there
are many vulnerable patients who are mentally unstable and are not able make their own decision
should also have high risk of getting various restriction that may lead to provide bad
environment. With inclusion of good environment, it may influence healthcare staff member to
perform well and should take care of such patient more appropriately. There is risk of
discrimination which are effective and may lead to create variation in service delivery that may
also affect patient health. Vulnerable patient is having unstable mental health which should be
taken in care and have focus to provide better or improved mental health. This can be effective
and may help in delivery of better response toward the patient care and have better improvement
in their mental health. Through taking care of the mental illness, healthcare professional is able
to deliver better positive response in the health and provide health improvement to the vulnerable
patient (Kertesz and et. al., 2021). There is need to ensure about taking care of vulnerable patient
that should also provide positive impact on their health. It may also influence about delivery of
better and effective response which are associated with improving their mental health.
There are large number of vulnerable patients in UK who need proper care and support.
They are not physically or mentally strong in which they should provide proper safeguarding and
include various care service and techniques that are highly required in improving their mental
health. Healthcare service provider should ensure about taking care of such vulnerable people
and ensure about getting better and effective response which are associated with their mental
health. However, there may various reasons which can restrict healthcare staff to provide quality
of care or may lead to reason for neglect (Lebano and et. al., 2020). Here, neglect can be one of
the main reasons that may proceed to the declining mental health of patient. That can also be
effective and may lead to create high impact on their mental health. Here, healthcare serviced
better mental health. There is higher chance that vulnerable patient is mentally weak or may not
have stable mental condition which lead them to risk of higher chance of vulnerability. There are
large number of patients who need proper assistance and care that can help to avoid the risk of
getting negative mental health impact (Hudon and et. al., 2018). Additionally, there is also need
to ensure about getting better response which are associated with ensuring about taking care of
good health. There is various reason due to which healthcare premises are not perform well
towards caring such type of vulnerable patient. Every healthcare provider should ensure about
taking care of each patient especially vulnerable patient (Cénat and et. al., 2020). In this, there
are many vulnerable patients who are mentally unstable and are not able make their own decision
should also have high risk of getting various restriction that may lead to provide bad
environment. With inclusion of good environment, it may influence healthcare staff member to
perform well and should take care of such patient more appropriately. There is risk of
discrimination which are effective and may lead to create variation in service delivery that may
also affect patient health. Vulnerable patient is having unstable mental health which should be
taken in care and have focus to provide better or improved mental health. This can be effective
and may help in delivery of better response toward the patient care and have better improvement
in their mental health. Through taking care of the mental illness, healthcare professional is able
to deliver better positive response in the health and provide health improvement to the vulnerable
patient (Kertesz and et. al., 2021). There is need to ensure about taking care of vulnerable patient
that should also provide positive impact on their health. It may also influence about delivery of
better and effective response which are associated with improving their mental health.
There are large number of vulnerable patients in UK who need proper care and support.
They are not physically or mentally strong in which they should provide proper safeguarding and
include various care service and techniques that are highly required in improving their mental
health. Healthcare service provider should ensure about taking care of such vulnerable people
and ensure about getting better and effective response which are associated with their mental
health. However, there may various reasons which can restrict healthcare staff to provide quality
of care or may lead to reason for neglect (Lebano and et. al., 2020). Here, neglect can be one of
the main reasons that may proceed to the declining mental health of patient. That can also be
effective and may lead to create high impact on their mental health. Here, healthcare serviced
provider should ensure about using different techniques or theories which can be effective and
may lead to provide some positive aspect about delivery of care and mental health improvement.
There are large number of patients within healthcare where they are not able to take care of
themselves and may require proper care and support that can improve patient health. It is also
necessary to provide better and effective healthcare service which should be effective and may
help in better and effective healthcare services for better health improvement. Vulnerable people
are mentally weak and may need some support and proper care that can help in getting better
impact on delivery of proper response. Additionally, healthcare premises should have better
environment that can be effective and may provide better positive impact. There are many
healthcare professionals who are not able to provide proper care to vulnerable patient all the time
due to various reason (Kiselev and et. al., 2020). This reason may include time limitation,
inadequate staff members, busy schedule, large number of patients at a time and others. These
are highly effective and may lead to create the risk of not providing better care services to
patient. vulnerable patient is mentally weak and are not able to perform well and take care of
their health and protect themselves. In this, healthcare professional should ensure about proper
care and safety where safeguarding to those vulnerable patients is highly effective and may need
to ensure about proper care and support.
Vulnerable patient is highly at risk of harm or neglect where healthcare professional should
effectively take care of them in better way. They also need some special care and treatment
which can be effective and may help to reduce the risk of decreasing mental health. It is also
necessary to ensure about delivery of effective care where they should improve the care service
and their quality. This may help in improving their mental health. Vulnerable people are needed
for better assistance and care where they should be treated effectively. They should not face any
type of discrimination that may lead to create some consequences that are associated with
declining mental health (Saxe Zerden and et. al., 2019). There is need to ensure about taking care
of better and effective mental health which are also associated with ensuring about good mental
health. Here, healthcare service provider should work in better way through understanding the
situation and patient condition in better way and should provide training to their staff member
like nursing staff properly to handle the situation more effectively.
may lead to provide some positive aspect about delivery of care and mental health improvement.
There are large number of patients within healthcare where they are not able to take care of
themselves and may require proper care and support that can improve patient health. It is also
necessary to provide better and effective healthcare service which should be effective and may
help in better and effective healthcare services for better health improvement. Vulnerable people
are mentally weak and may need some support and proper care that can help in getting better
impact on delivery of proper response. Additionally, healthcare premises should have better
environment that can be effective and may provide better positive impact. There are many
healthcare professionals who are not able to provide proper care to vulnerable patient all the time
due to various reason (Kiselev and et. al., 2020). This reason may include time limitation,
inadequate staff members, busy schedule, large number of patients at a time and others. These
are highly effective and may lead to create the risk of not providing better care services to
patient. vulnerable patient is mentally weak and are not able to perform well and take care of
their health and protect themselves. In this, healthcare professional should ensure about proper
care and safety where safeguarding to those vulnerable patients is highly effective and may need
to ensure about proper care and support.
Vulnerable patient is highly at risk of harm or neglect where healthcare professional should
effectively take care of them in better way. They also need some special care and treatment
which can be effective and may help to reduce the risk of decreasing mental health. It is also
necessary to ensure about delivery of effective care where they should improve the care service
and their quality. This may help in improving their mental health. Vulnerable people are needed
for better assistance and care where they should be treated effectively. They should not face any
type of discrimination that may lead to create some consequences that are associated with
declining mental health (Saxe Zerden and et. al., 2019). There is need to ensure about taking care
of better and effective mental health which are also associated with ensuring about good mental
health. Here, healthcare service provider should work in better way through understanding the
situation and patient condition in better way and should provide training to their staff member
like nursing staff properly to handle the situation more effectively.
Causes and impact that render upon mental health of vulnerable patient within BMI Healthcare
in the UK
Vulnerable people face huge issue of stigmatisation and discrimination in healthcare facility.
Behaviour of healthcare providers towards vulnerable patient is the major aspect of developing
the risk of mental health within them. Negative attitude and rude behaviour can make them feel
worthless, useless, or helpless in any way. Such behaviour lead vulnerable people to lose their
self-esteem and confidence (Alegría and et. al., 2018). Such attitude put major negative impact
on their development as well as growth. It may result in causing mental health issues in some
individuals. Discriminative behaviour reduce motivation of getting well and lose hope for future.
Poor health care service, communication barrier, aggression or secondary unusual social
responses exhibit by healthcare workers can impact the mental health of vulnerable people in
BMI healthcare centre. Social isolation and loneliness within healthcare setting is also a
contributing factor is disturbing mental condition of a vulnerable patient. Social relationships are
important in everyone's life which help a person to share their problems, communicate about
issues, explore the opportunity of solutions but isolation keep them away from social love,
respect, and recognition. Within BMI healthcare setting, it is the responsibility of healthcare
providers to keep record of routine activities of an admitted individual and encourage the patient
to get socially involved and communicate with others. Bereavement and grief make people
vulnerable to mental health (Makwana, 2019). Feeling of sadness, hopeless, loneliness, and
anger are the emotions that bind people during grieving process. Bereavement may have
traumatic and stressful young people and even children. It may result in fluctuating down the
results at academic levels (in case of children), or office work (in case of adults), fall down of
confidence level, even including the risk of developing suicidal thoughts among individual.
Other major cause is having a long-term physical health condition which can lead to develop
stigma, make individual unable to go out which cause social isolation, lower down the self-
esteem. People generally get frustrated, stressed, worried, tired while dealing with pain,
treatments, isolation or flare-ups. Physically weak people are unable to do physical exercise
which leads to weight gain, weakens the strength, impact on physical posture can be observed.
Every individual has a different capability to deal with stressful conditions. Some people are so
weak and those are considered as weaker and more vulnerable to fall for mental health. It is
important for such people to practice exercise, yoga, meditation and develop an understanding
in the UK
Vulnerable people face huge issue of stigmatisation and discrimination in healthcare facility.
Behaviour of healthcare providers towards vulnerable patient is the major aspect of developing
the risk of mental health within them. Negative attitude and rude behaviour can make them feel
worthless, useless, or helpless in any way. Such behaviour lead vulnerable people to lose their
self-esteem and confidence (Alegría and et. al., 2018). Such attitude put major negative impact
on their development as well as growth. It may result in causing mental health issues in some
individuals. Discriminative behaviour reduce motivation of getting well and lose hope for future.
Poor health care service, communication barrier, aggression or secondary unusual social
responses exhibit by healthcare workers can impact the mental health of vulnerable people in
BMI healthcare centre. Social isolation and loneliness within healthcare setting is also a
contributing factor is disturbing mental condition of a vulnerable patient. Social relationships are
important in everyone's life which help a person to share their problems, communicate about
issues, explore the opportunity of solutions but isolation keep them away from social love,
respect, and recognition. Within BMI healthcare setting, it is the responsibility of healthcare
providers to keep record of routine activities of an admitted individual and encourage the patient
to get socially involved and communicate with others. Bereavement and grief make people
vulnerable to mental health (Makwana, 2019). Feeling of sadness, hopeless, loneliness, and
anger are the emotions that bind people during grieving process. Bereavement may have
traumatic and stressful young people and even children. It may result in fluctuating down the
results at academic levels (in case of children), or office work (in case of adults), fall down of
confidence level, even including the risk of developing suicidal thoughts among individual.
Other major cause is having a long-term physical health condition which can lead to develop
stigma, make individual unable to go out which cause social isolation, lower down the self-
esteem. People generally get frustrated, stressed, worried, tired while dealing with pain,
treatments, isolation or flare-ups. Physically weak people are unable to do physical exercise
which leads to weight gain, weakens the strength, impact on physical posture can be observed.
Every individual has a different capability to deal with stressful conditions. Some people are so
weak and those are considered as weaker and more vulnerable to fall for mental health. It is
important for such people to practice exercise, yoga, meditation and develop an understanding
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

about concern of mental and physical health. Healthcare workers at BMI should encourage
people to perform physical exercise on routine basis. Physical exercise lead human brain to
produce serotonin chemical which results to provide benefits of physical strength, refresh mood,
reduce stress and tension and considered to be good for overall well-being (Alonzi, La Torre and
Silverstein, 2020).
At some places, healthcare workers do not act responsibly which leads to impact the life of
people drastically. Physical causes like epilepsy, accident, or head injury may be responsible to
create a worst neurological condition which recorded to be highly impact the behaviour and
mood of the patient. Many lifestyle factors including drugs, improper diet, work stress, and lack
of sleep contributes to affect mental health. In BMI healthcare, healthcare workers should
prepare a diet chart of the vulnerable patients and prefer to provide them accordingly. Apart from
this, Healthcare centres must heir some professional counsellors. Association with professional
counsellors and therapists can help the patients to deal with the cause of mental problem. Proper
medication, suggestions to perform daily activities in order to reduce the stress, counselling and
therapy sessions can help them to cope up with the stressful conditions effectively (Orben,
Tomova, and Blakemore, 2020).
Alcohol and drug substance abuse is also a common cause among adults to suffer mental
problems. Tendency to use drugs and consume alcohol in order to overcome the depressing and
anxiety conditions make people addicted to these substances. Such substances contain
barbiturates and benzodiazepines which produce the calming and sedative effect on mind and
induce sleep within consumers. These drugs are so potential in producing addiction without
which it become impossible for abusers to survive and even if people try to withdraw these
drugs, then body can produce harmful withdrawal symptoms. Healthcare workers should be
concern about such patients and provide different treatment. Professional should timely monitor
for their blood to check whether the patient is still having drugs somehow. In BMI healthcare,
volunteers should take care and regularly check for patient's room to monitor that patient should
not be able to get drug supplies anyhow within BMI. Childhood abuse, trauma, long-term stress
and neglecting nature is also a cause of mental health condition within vulnerable people
(Arango and et. al., 2018). Such people are too vulnerable to get into traumatic condition again if
same incident get repeated again in their or somebody else's life.
people to perform physical exercise on routine basis. Physical exercise lead human brain to
produce serotonin chemical which results to provide benefits of physical strength, refresh mood,
reduce stress and tension and considered to be good for overall well-being (Alonzi, La Torre and
Silverstein, 2020).
At some places, healthcare workers do not act responsibly which leads to impact the life of
people drastically. Physical causes like epilepsy, accident, or head injury may be responsible to
create a worst neurological condition which recorded to be highly impact the behaviour and
mood of the patient. Many lifestyle factors including drugs, improper diet, work stress, and lack
of sleep contributes to affect mental health. In BMI healthcare, healthcare workers should
prepare a diet chart of the vulnerable patients and prefer to provide them accordingly. Apart from
this, Healthcare centres must heir some professional counsellors. Association with professional
counsellors and therapists can help the patients to deal with the cause of mental problem. Proper
medication, suggestions to perform daily activities in order to reduce the stress, counselling and
therapy sessions can help them to cope up with the stressful conditions effectively (Orben,
Tomova, and Blakemore, 2020).
Alcohol and drug substance abuse is also a common cause among adults to suffer mental
problems. Tendency to use drugs and consume alcohol in order to overcome the depressing and
anxiety conditions make people addicted to these substances. Such substances contain
barbiturates and benzodiazepines which produce the calming and sedative effect on mind and
induce sleep within consumers. These drugs are so potential in producing addiction without
which it become impossible for abusers to survive and even if people try to withdraw these
drugs, then body can produce harmful withdrawal symptoms. Healthcare workers should be
concern about such patients and provide different treatment. Professional should timely monitor
for their blood to check whether the patient is still having drugs somehow. In BMI healthcare,
volunteers should take care and regularly check for patient's room to monitor that patient should
not be able to get drug supplies anyhow within BMI. Childhood abuse, trauma, long-term stress
and neglecting nature is also a cause of mental health condition within vulnerable people
(Arango and et. al., 2018). Such people are too vulnerable to get into traumatic condition again if
same incident get repeated again in their or somebody else's life.
Proper diet, complete sleep, physical activity, burden free mind, proper medication course is
some of the sources which can help the vulnerable population to keep them safe or treat from
mental condition. Impact of medical condition on an individual mind can be worst. Those people
who suffer from such conditions need strength, and support both mentally and sometimes
physically to cope up with the situation. Proper planning and implementation of effective
strategies may help BMI healthcare organisation to operate and conduct their facilities in a
proper and effectively positive manner (Wang and et. al., 2018). Facilities at healthcare setting
which encourage people to participate in curriculum activities, fun activities, games, and indulge
them some activities may help patient to divert their mind from traumatic events or think about
depressing conditions. Facilities should not have environment of discrimination and
stigmatisation. Centres should be strictly free from such things; they must be investigated by
supervisors and professionals can monitor for recovering mental health condition of vulnerable
patients. It is of major concern of keep people away from factors that may accelerate the
condition of stress and anxiety among people.
Intervention or strategies used by healthcare leaders and care nurses to reduce impact and
enhance mental health of vulnerable patients
The intervention strategies used by the healthcare leaders and care nurses are cognitive-
behavioural, relaxation, social skills training, general behaviour, social support, mindfulness,
meditation, psycho-educational, acceptance, interpersonal psychotherapy, resilience as well as
forgiveness programs. Therefore, there are various intervention or strategies are used by the
healthcare leaders and nurses care in order to reduce or enhance the mental health of vulnerable
patient are mentioned such as:
Enhance social interaction or connection- As face-to-face interaction with other people
may help in reducing the stress as well as work as mood- booster power.
Stay active- As regular exercising or doing some regular activity can make a huge impact on
mental or emotional health such as helps in relieving stress, helps in improving memory as well
as in improving sleep.
Talk to someone- Regular talking to a friendly person is the most effective strategies as it
helps the vulnerable person to calm their nervous system as well as helps them in relieving
stress.
some of the sources which can help the vulnerable population to keep them safe or treat from
mental condition. Impact of medical condition on an individual mind can be worst. Those people
who suffer from such conditions need strength, and support both mentally and sometimes
physically to cope up with the situation. Proper planning and implementation of effective
strategies may help BMI healthcare organisation to operate and conduct their facilities in a
proper and effectively positive manner (Wang and et. al., 2018). Facilities at healthcare setting
which encourage people to participate in curriculum activities, fun activities, games, and indulge
them some activities may help patient to divert their mind from traumatic events or think about
depressing conditions. Facilities should not have environment of discrimination and
stigmatisation. Centres should be strictly free from such things; they must be investigated by
supervisors and professionals can monitor for recovering mental health condition of vulnerable
patients. It is of major concern of keep people away from factors that may accelerate the
condition of stress and anxiety among people.
Intervention or strategies used by healthcare leaders and care nurses to reduce impact and
enhance mental health of vulnerable patients
The intervention strategies used by the healthcare leaders and care nurses are cognitive-
behavioural, relaxation, social skills training, general behaviour, social support, mindfulness,
meditation, psycho-educational, acceptance, interpersonal psychotherapy, resilience as well as
forgiveness programs. Therefore, there are various intervention or strategies are used by the
healthcare leaders and nurses care in order to reduce or enhance the mental health of vulnerable
patient are mentioned such as:
Enhance social interaction or connection- As face-to-face interaction with other people
may help in reducing the stress as well as work as mood- booster power.
Stay active- As regular exercising or doing some regular activity can make a huge impact on
mental or emotional health such as helps in relieving stress, helps in improving memory as well
as in improving sleep.
Talk to someone- Regular talking to a friendly person is the most effective strategies as it
helps the vulnerable person to calm their nervous system as well as helps them in relieving
stress.
Appeal to your senses- doing some experiment to find the best solution for a vulnerable people in
order to enhance their mental health. The experiment involves listening some uplifting song
which can helps to feel calm, squeezing out the stress ball as it helps the patient to feel cantered,
talking about nature or enjoying sight as doing this activity can enhance some sensory response
(Courtenay and Perera., 2020).
Take up a relaxation practice- Involving the yoga, mindfulness, meditation as well as deep-
breathing in regular activity can help the vulnerable patient to reducing their stress level.
Make leisure and contemplation a priority- Having some leisure time is very important for
emotional and mental health such as having some time to relax, contemplate as well as pay
attention to the positive things even it is a small thing.
Eat healthy diet which support strong mental health- A healthy foods such as fatty fish rich in
omega-3s, nuts like walnuts, almonds, cashews and peanuts, avacados, beans, leafy green leaves
like spinach, kale and some brussels sprouts along with that includes some fresh fruits like
blueberries may elevate the mood and helps in enhancing the strong mental health.
Do not skimp on sleep- Having better sleep helps in reducing stress, helps in calming the
brain as well as helps in enhancing strong mental health. Therefore, the sleep process is to take a
break from stimulation of screening such as TV, phones, tablets or computers before two hours
to go at bedtime.
Find purpose and meaning- The motive and meaning is differed from person to person.
Therefore, following things need to do for enhancing mental health such as engage the person in
such work which makes them feel comfortable, increase spending time on those people who
matters the most (Grover and et.al., 2020).
The neurodevelopmental changes are occurring during young age make a period for both
vulnerability as well as the opportunity for mental health. There is research which indicate that
there are number of factors which influence the person's mental health from before birth to early
adulthood. The key component which supports optimal brain development, emotional regulation
and cognitive function is meeting the child's physical, psychological as well as social needs of
the children.
The successful treatments exist for mental health persons as by screening in early age
group. There is a study which conclude that adolescent or youth who receive routine wellness
check are not being screened of any depressive disorder. As timely intervention is insistent
order to enhance their mental health. The experiment involves listening some uplifting song
which can helps to feel calm, squeezing out the stress ball as it helps the patient to feel cantered,
talking about nature or enjoying sight as doing this activity can enhance some sensory response
(Courtenay and Perera., 2020).
Take up a relaxation practice- Involving the yoga, mindfulness, meditation as well as deep-
breathing in regular activity can help the vulnerable patient to reducing their stress level.
Make leisure and contemplation a priority- Having some leisure time is very important for
emotional and mental health such as having some time to relax, contemplate as well as pay
attention to the positive things even it is a small thing.
Eat healthy diet which support strong mental health- A healthy foods such as fatty fish rich in
omega-3s, nuts like walnuts, almonds, cashews and peanuts, avacados, beans, leafy green leaves
like spinach, kale and some brussels sprouts along with that includes some fresh fruits like
blueberries may elevate the mood and helps in enhancing the strong mental health.
Do not skimp on sleep- Having better sleep helps in reducing stress, helps in calming the
brain as well as helps in enhancing strong mental health. Therefore, the sleep process is to take a
break from stimulation of screening such as TV, phones, tablets or computers before two hours
to go at bedtime.
Find purpose and meaning- The motive and meaning is differed from person to person.
Therefore, following things need to do for enhancing mental health such as engage the person in
such work which makes them feel comfortable, increase spending time on those people who
matters the most (Grover and et.al., 2020).
The neurodevelopmental changes are occurring during young age make a period for both
vulnerability as well as the opportunity for mental health. There is research which indicate that
there are number of factors which influence the person's mental health from before birth to early
adulthood. The key component which supports optimal brain development, emotional regulation
and cognitive function is meeting the child's physical, psychological as well as social needs of
the children.
The successful treatments exist for mental health persons as by screening in early age
group. There is a study which conclude that adolescent or youth who receive routine wellness
check are not being screened of any depressive disorder. As timely intervention is insistent
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
whereas in case of late diagnosis it could lead to difficult to treat chronic mental health
throughout the adulthood.
There are several mental health theories which are used as intervention in case of enhancement
of mental health or for vulnerable persons are mentioned such as behaviourism, biological,
psychodynamic, cognitive as well as humanistic. As psychodynamic theory helps the people to
look at their subconscious mind (Yau and et.al., 2021).
The most prominent strategy which has been purpoted in order to assist individuals in enacting
the mental health patient intentions and countering the gap between the intentions and the
behaviour implementation intentions. Self-regulation strategy is an implementation intention in
which the individual augments their intentions with a cue-initiated plan. It is a mental act which
build link between the anticipated critical situation with the appropriate intended response.
Therefore, cue is the most appropriate conditions, time or place where the action can be taken.
As nurses’ interaction is important in many settings including schools, community as
well as public health settings, outpatient clinics. Therefore, nurses must have to be educated on
the meet the needs of vulnerable population and mental health illness and utilize each
opportunity in order to identified mental health issues. In case of assessment of patient, the
nurses must have to be aware of some specific finding which identified the symptoms of mental
health issues or their increased risk (Tiller and Reynolds., 2020).
The effectiveness is dependent on individuals’ motivation as individuals must have sufficient
motivation in order to engage in the behaviour. The furthermore, proposed mechanisms which
effects the mental simulations on behaviour change by activation or make some salient certain
action which are mindset oriented as well as behavioural oriented. The mental simulations may
work as a bridge between the thoughts as well as the goal directed behaviour. The intervention is
based on the hypothesis which combine mental simulations intervention. It promotes motivation
with an implementation intention by optimizing participation in their health behaviour.
The healthcare professional more often sees vulnerable patient in school, public health
agency, urgent care setting due to limited access to routine healthcare. Therefore, the healthcare
leaders made ensure that nurses should have sufficient knowledge to assess or intervene even in
case as they are not trained mental health professionals. During the assessment of patient, the
nurses have a duty to assess all the information from the friends, their families and get to know
throughout the adulthood.
There are several mental health theories which are used as intervention in case of enhancement
of mental health or for vulnerable persons are mentioned such as behaviourism, biological,
psychodynamic, cognitive as well as humanistic. As psychodynamic theory helps the people to
look at their subconscious mind (Yau and et.al., 2021).
The most prominent strategy which has been purpoted in order to assist individuals in enacting
the mental health patient intentions and countering the gap between the intentions and the
behaviour implementation intentions. Self-regulation strategy is an implementation intention in
which the individual augments their intentions with a cue-initiated plan. It is a mental act which
build link between the anticipated critical situation with the appropriate intended response.
Therefore, cue is the most appropriate conditions, time or place where the action can be taken.
As nurses’ interaction is important in many settings including schools, community as
well as public health settings, outpatient clinics. Therefore, nurses must have to be educated on
the meet the needs of vulnerable population and mental health illness and utilize each
opportunity in order to identified mental health issues. In case of assessment of patient, the
nurses must have to be aware of some specific finding which identified the symptoms of mental
health issues or their increased risk (Tiller and Reynolds., 2020).
The effectiveness is dependent on individuals’ motivation as individuals must have sufficient
motivation in order to engage in the behaviour. The furthermore, proposed mechanisms which
effects the mental simulations on behaviour change by activation or make some salient certain
action which are mindset oriented as well as behavioural oriented. The mental simulations may
work as a bridge between the thoughts as well as the goal directed behaviour. The intervention is
based on the hypothesis which combine mental simulations intervention. It promotes motivation
with an implementation intention by optimizing participation in their health behaviour.
The healthcare professional more often sees vulnerable patient in school, public health
agency, urgent care setting due to limited access to routine healthcare. Therefore, the healthcare
leaders made ensure that nurses should have sufficient knowledge to assess or intervene even in
case as they are not trained mental health professionals. During the assessment of patient, the
nurses have a duty to assess all the information from the friends, their families and get to know
the history and the family dynamics as well as the provided education and the resources
(Perregrini., 2019).
There are some of the gaps in like implementing some policy and regulation that should be
implemented in better way. Each and every staff member should follow those policies strictly
that can help to ensure about avoid the risk of harm or neglect within the healthcare premises and
should provide better improvement in their health. This can also help to reduce the risk of
declining mental health of vulnerable patient.
THEORETICAL FRAMEWORK
Project life cycle (PLC)
The project life cycle is basically aimed on the project management which are includes
the project management phases, processes, tools as well as techniques for the effective
management of the projects. These project cycles consider some steps for the appropriate
development of the projects which are essential for the project supervisor to effectively manage
this project from start to end. The project is based on the increasing the mental health of
vulnerable person within the BMI healthcare organization. This cycle is including some steps
which are mentioned blow:
Project initiation: This is the starting phase of the project life cycle and this phase is
associated with the determining the aim or objective and stakeholder register of the project. The
main objective of the project is evaluating the condition of the mental health of vulnerable
people in the BMI healthcare in the UK (Wibowo and Uda, 2018). There is also determine the
causes and impact of this on the patient and evaluate the interventions as well as plans which are
used by the healthcare professional and the leaders of the patients.
Project planning: After the completion of the project initiation phase the planning of the
project is carry out. This is the second stage of the project life cycle which are considers the
plans, strategies and the interventions to increase the mental health in the patient in the
healthcare organization. This is considering the roadmap with the detailed description of the
strategies.
Project executing: This is the third step of the project life cycle which are considers the
budget allocation and most of the project deliverables are produced. This is also considering the
(Perregrini., 2019).
There are some of the gaps in like implementing some policy and regulation that should be
implemented in better way. Each and every staff member should follow those policies strictly
that can help to ensure about avoid the risk of harm or neglect within the healthcare premises and
should provide better improvement in their health. This can also help to reduce the risk of
declining mental health of vulnerable patient.
THEORETICAL FRAMEWORK
Project life cycle (PLC)
The project life cycle is basically aimed on the project management which are includes
the project management phases, processes, tools as well as techniques for the effective
management of the projects. These project cycles consider some steps for the appropriate
development of the projects which are essential for the project supervisor to effectively manage
this project from start to end. The project is based on the increasing the mental health of
vulnerable person within the BMI healthcare organization. This cycle is including some steps
which are mentioned blow:
Project initiation: This is the starting phase of the project life cycle and this phase is
associated with the determining the aim or objective and stakeholder register of the project. The
main objective of the project is evaluating the condition of the mental health of vulnerable
people in the BMI healthcare in the UK (Wibowo and Uda, 2018). There is also determine the
causes and impact of this on the patient and evaluate the interventions as well as plans which are
used by the healthcare professional and the leaders of the patients.
Project planning: After the completion of the project initiation phase the planning of the
project is carry out. This is the second stage of the project life cycle which are considers the
plans, strategies and the interventions to increase the mental health in the patient in the
healthcare organization. This is considering the roadmap with the detailed description of the
strategies.
Project executing: This is the third step of the project life cycle which are considers the
budget allocation and most of the project deliverables are produced. This is also considering the
development of the team, engagement of the managers or supervisor and investors as well as the
quality assurance activities.
Project monitoring or controlling: The project monitoring and controlling phase is
associated with the actual or current progress of the project with the implementation of the
strategies and planning. These all are associated with the taking the appropriate action where it is
essential (Maphanga and Nel, 2020).
Project closing: This is the last and final step of the project life cycle which are
considers the project delivering, achieving the project records, acknowledgment of the
achievement and officially disbanding and releasing the teams. This is the simple steps for the
checking the project completion. This is the necessary step for the formal complete the project
and determine the secure approval form the patients, nurses, leaders and the healthcare
professionals.
Kotter’s 8 step Change Model
The Kotter's 8 step change model is used for the assisting the healthcare leaders for
successfully implement organization change. This model is mainly aimed on the creating the
urgency in order to make a change happen. This model is developed by the John P. Kotter which
is provides an easy-to-follow roadmap for change managers, even if they are not expert. The
includes 8 steps which are explained as:
Creating urgency: This step is including the evaluation of the needs of the projects for
the patients and determine the current problems with the teams and get their opinion. This is also
considering the assessment of the threats which are arise during the projects (Tan and et. al.,
2019). It helps to identity need which should create in further and may impact the future aspect.
It also includes about finding the potential impact and issues and further try to find the solution.
Forming powerful Guiding coalitions: This step is including the assessment of the
weak areas of the projects and compensate them by increasing the persons in the several
departments. These is also identifying the change healthcare leaders and investors in the BMI
healthcare organization. Here, BMI healthcare professional should influence towards change that
is necessary for improvement in mental health of vulnerable people.
Developing a vision or strategies: This step is also involving with the development of
the clear objective and vision for the BMI healthcare's initiative as well as planning for the
quality assurance activities.
Project monitoring or controlling: The project monitoring and controlling phase is
associated with the actual or current progress of the project with the implementation of the
strategies and planning. These all are associated with the taking the appropriate action where it is
essential (Maphanga and Nel, 2020).
Project closing: This is the last and final step of the project life cycle which are
considers the project delivering, achieving the project records, acknowledgment of the
achievement and officially disbanding and releasing the teams. This is the simple steps for the
checking the project completion. This is the necessary step for the formal complete the project
and determine the secure approval form the patients, nurses, leaders and the healthcare
professionals.
Kotter’s 8 step Change Model
The Kotter's 8 step change model is used for the assisting the healthcare leaders for
successfully implement organization change. This model is mainly aimed on the creating the
urgency in order to make a change happen. This model is developed by the John P. Kotter which
is provides an easy-to-follow roadmap for change managers, even if they are not expert. The
includes 8 steps which are explained as:
Creating urgency: This step is including the evaluation of the needs of the projects for
the patients and determine the current problems with the teams and get their opinion. This is also
considering the assessment of the threats which are arise during the projects (Tan and et. al.,
2019). It helps to identity need which should create in further and may impact the future aspect.
It also includes about finding the potential impact and issues and further try to find the solution.
Forming powerful Guiding coalitions: This step is including the assessment of the
weak areas of the projects and compensate them by increasing the persons in the several
departments. These is also identifying the change healthcare leaders and investors in the BMI
healthcare organization. Here, BMI healthcare professional should influence towards change that
is necessary for improvement in mental health of vulnerable people.
Developing a vision or strategies: This step is also involving with the development of
the clear objective and vision for the BMI healthcare's initiative as well as planning for the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
effective strategies to assist the team in achieving it. Here, BMI healthcare management need to
focus on the developing strategy to resolve the identified issue.
Communicating the vision: The main aim of this step is associated with the
communicate the objectives or vision in a effective manner that are assist in the encourage the
healthcare leaders and nurses to support the changes (Galli, 2019). BMI healthcare professional
should communicate those strategies with staff member to get connected and understand the
change needs.
Removing the Obstacles: The development of the organization at the wide range will
increase the many obstacles. This stage is associated with the guiding the healthcare for
concentrate on removing every obstacle which are slowing down the progress of the
organization. BMI healthcare professional should ensure the implementation of strategy through
removing obstacle to implement those.
Creating the Short-term wins: This is playing an important role in the in the
development of the short-term goals and celebrate early in the change process to build and
maintain the momentum of the healthcare centre (Lundquist and Haaheim, 2020). Through
implementing those in BMI healthcare, there is need to create short term wins to motivate
themselves.
Consolidating Gains: This step is associated with the determination of the aspects which
are good or bad at the healthcare centre. These are ensuring that the teams are working hard to
achieve the objectives.
Anchoring change in the corporate culture: This is the final step of this model which
are ensure that it is integrated into the healthcare organization. These are considering the time,
change in leadership as well as change in the nurses and leaders that can change the impact
quickly and easily. BMI healthcare should include effective that can help to effectivel implement
change more effectively.
Contingency theory
The contingency theory is associated with the management theory which are explains the
proper aspects for the management which are completely depend on the current condition. The
supervisor which are associated with this theory are basically pay their attention to the condition
focus on the developing strategy to resolve the identified issue.
Communicating the vision: The main aim of this step is associated with the
communicate the objectives or vision in a effective manner that are assist in the encourage the
healthcare leaders and nurses to support the changes (Galli, 2019). BMI healthcare professional
should communicate those strategies with staff member to get connected and understand the
change needs.
Removing the Obstacles: The development of the organization at the wide range will
increase the many obstacles. This stage is associated with the guiding the healthcare for
concentrate on removing every obstacle which are slowing down the progress of the
organization. BMI healthcare professional should ensure the implementation of strategy through
removing obstacle to implement those.
Creating the Short-term wins: This is playing an important role in the in the
development of the short-term goals and celebrate early in the change process to build and
maintain the momentum of the healthcare centre (Lundquist and Haaheim, 2020). Through
implementing those in BMI healthcare, there is need to create short term wins to motivate
themselves.
Consolidating Gains: This step is associated with the determination of the aspects which
are good or bad at the healthcare centre. These are ensuring that the teams are working hard to
achieve the objectives.
Anchoring change in the corporate culture: This is the final step of this model which
are ensure that it is integrated into the healthcare organization. These are considering the time,
change in leadership as well as change in the nurses and leaders that can change the impact
quickly and easily. BMI healthcare should include effective that can help to effectivel implement
change more effectively.
Contingency theory
The contingency theory is associated with the management theory which are explains the
proper aspects for the management which are completely depend on the current condition. The
supervisor which are associated with this theory are basically pay their attention to the condition
and their style and these are make efforts to ensure the both are effectively interact (Csaszar and
Ostler, 2020).
The contingency theory has advantages in the healthcare organization which are
associated with the potential for the learning for the particular situation. There is every leader
have their personal leadership style which are associated with the various factors of the
workplace. According to this theory, the healthcare leaders are always finding the specific
condition that are become challenging for them and they must be consenting to declare that their
success partially which are depend on their condition. The nurses, managers and healthcare
leaders are requiring to adapt their leadership style to the specific situation. This theory is also
having advantages for the understanding of the leadership style which are includes the several
impacts of the conditions on leaders. This is also assisting the leader what can do in the critical
or the specific condition (McAdam, Miller and McSorley, 2019).
PROJECT PLAN METHODOLOGY
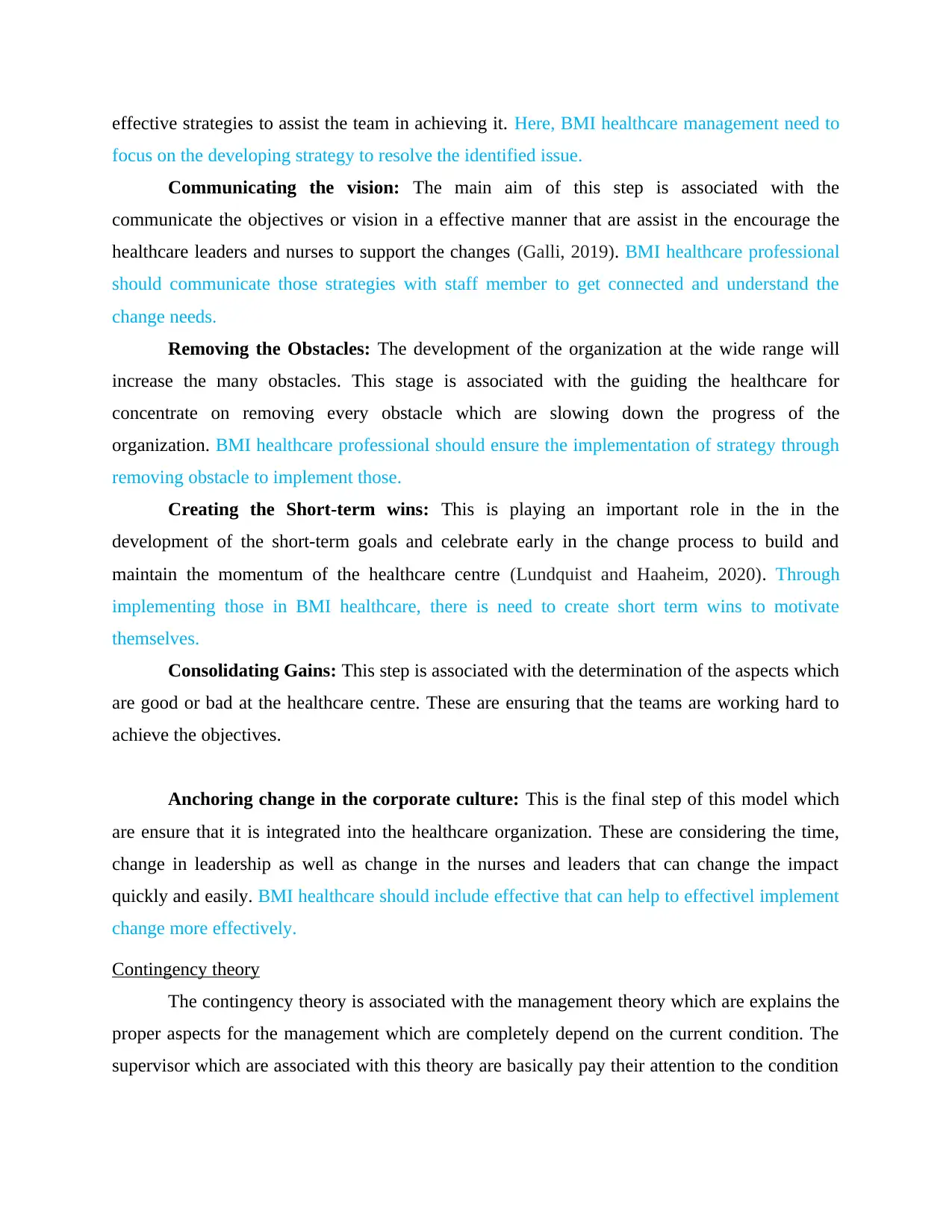
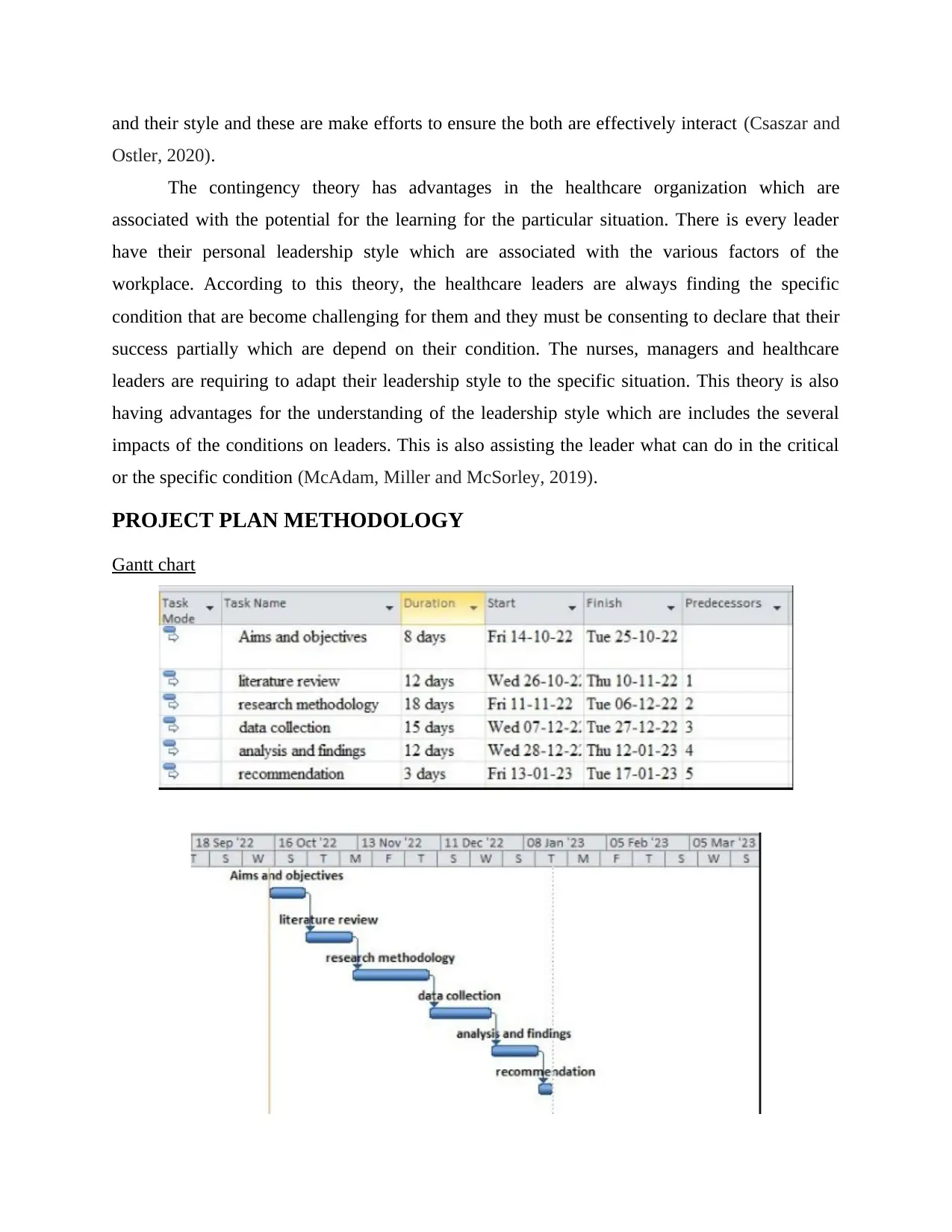
Gantt chart
Ostler, 2020).
The contingency theory has advantages in the healthcare organization which are
associated with the potential for the learning for the particular situation. There is every leader
have their personal leadership style which are associated with the various factors of the
workplace. According to this theory, the healthcare leaders are always finding the specific
condition that are become challenging for them and they must be consenting to declare that their
success partially which are depend on their condition. The nurses, managers and healthcare
leaders are requiring to adapt their leadership style to the specific situation. This theory is also
having advantages for the understanding of the leadership style which are includes the several
impacts of the conditions on leaders. This is also assisting the leader what can do in the critical
or the specific condition (McAdam, Miller and McSorley, 2019).
PROJECT PLAN METHODOLOGY
Gantt chart

Scope
The scope of the study mainly describes the extent to which the investigation area will be
explored among the work and can depict the specific parameters within the research that will be
operating. In this, the scope generally denotes that in which part a person will have to describe
what the study is generally going to cover as well as what it will be focusing over. It is generally
important to have a scope of the project as it can efficiently provide a person and a reader’s
significant outlines as well as can aid them to keep on track while doing the research. In addition
to this, it can give a depth knowledge to the study issues more effectively. Here, the selected
topic of scope is generally to enhance the mental health of vulnerable patients within BMI
Healthcare in the UK. It is determined that the mental health mainly includes psychological,
emotional as well as the social health of the vulnerable patients. It can mainly influence how a
vulnerable patient can think, feel as well as act. It can generally aid to identify how an individual
can handle stress, associated to others as well as make choices. In addition to this, the mental
well-being is generally essential at every stage of the living, from the childhood and adolescence
via the adulthood.
Resources
The resources in the research are mainly described as both the primary and secondary
sources. In this, the primary sources are mainly the first-hand information of the accurate events
mainly written by the original literacy or an eyewitness also. A primary source is particularly a
document or can be a record, generally a peer reviewed Journal articles which can significantly
reports research, experiments and the specific events or else the several phenomena more
particularly the first hand. Within the study, conducting a search strategy is generally based on to
enhance the mental health of the vulnerable patients within BMI healthcare in the UK. To gather
the sufficient information as well as its selection which is effectively linked with the selected
The scope of the study mainly describes the extent to which the investigation area will be
explored among the work and can depict the specific parameters within the research that will be
operating. In this, the scope generally denotes that in which part a person will have to describe
what the study is generally going to cover as well as what it will be focusing over. It is generally
important to have a scope of the project as it can efficiently provide a person and a reader’s
significant outlines as well as can aid them to keep on track while doing the research. In addition
to this, it can give a depth knowledge to the study issues more effectively. Here, the selected
topic of scope is generally to enhance the mental health of vulnerable patients within BMI
Healthcare in the UK. It is determined that the mental health mainly includes psychological,
emotional as well as the social health of the vulnerable patients. It can mainly influence how a
vulnerable patient can think, feel as well as act. It can generally aid to identify how an individual
can handle stress, associated to others as well as make choices. In addition to this, the mental
well-being is generally essential at every stage of the living, from the childhood and adolescence
via the adulthood.
Resources
The resources in the research are mainly described as both the primary and secondary
sources. In this, the primary sources are mainly the first-hand information of the accurate events
mainly written by the original literacy or an eyewitness also. A primary source is particularly a
document or can be a record, generally a peer reviewed Journal articles which can significantly
reports research, experiments and the specific events or else the several phenomena more
particularly the first hand. Within the study, conducting a search strategy is generally based on to
enhance the mental health of the vulnerable patients within BMI healthcare in the UK. To gather
the sufficient information as well as its selection which is effectively linked with the selected
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

title is generally based over various websites. However, there are several websites as well as the
search engines which are particularly available in which the most relevant and validated article
are being selected for the selection and review as well as can also gather some additional
information from the selected article. Here, the articles such as PubMed and PMC are effectively
being selected as a high aspect of information collection platform which is validated from the
investigation process. In addition to this, these such sources are mainly considered as a high
source of information that can significantly benefit the gathering of data which is needed for
further study.
Communication
It is generally necessary for the people to know additionally about the study topic like
improving mental health of the vulnerable patients within the BMI healthcare in the UK. In this,
the healthcare professionals and care nurses are mainly responsible for providing the effective
healthcare services to the vulnerable patients in order to enhance their well-being. In addition to
this, the care nurse role mainly requires the contemporary information over choosing the topic
such as enhancing mental health of the vulnerable patients within BMI healthcare across UK. In
order to prevent or reduce the prevalence of various issues such as anxiety, depression among
vulnerable patients, the healthcare professionals and care nurses should give an effective
information towards their vulnerable patient as well as their family members about anxiety,
depression due to mental issues. The concept of mental health is quite necessary for overall well-
being such that physical and mental health are equally essential element of overall well-being.
Like depression generally enhances the possible risks for various types of the physical well-
being issues, mainly the long-lasting conditions such as cardiovascular illness, diabetes and the
stroke as well. similarly, the presence of all the acute conditions can significantly enhances the
potential risk for mental disorders among vulnerable patients.
It is essential to communicate with other healthcare professional which are effective and
lead to create high impact to provide better care services for improving mental health of
vulnerable people. Communication table enable BMI healthcare to effectively perform their role
towards mental health improvement.
Target Audience Goals Tools Time table
Program
implementation team
To implement
program effective for
Meeting with proper
document and
Monthly
search engines which are particularly available in which the most relevant and validated article
are being selected for the selection and review as well as can also gather some additional
information from the selected article. Here, the articles such as PubMed and PMC are effectively
being selected as a high aspect of information collection platform which is validated from the
investigation process. In addition to this, these such sources are mainly considered as a high
source of information that can significantly benefit the gathering of data which is needed for
further study.
Communication
It is generally necessary for the people to know additionally about the study topic like
improving mental health of the vulnerable patients within the BMI healthcare in the UK. In this,
the healthcare professionals and care nurses are mainly responsible for providing the effective
healthcare services to the vulnerable patients in order to enhance their well-being. In addition to
this, the care nurse role mainly requires the contemporary information over choosing the topic
such as enhancing mental health of the vulnerable patients within BMI healthcare across UK. In
order to prevent or reduce the prevalence of various issues such as anxiety, depression among
vulnerable patients, the healthcare professionals and care nurses should give an effective
information towards their vulnerable patient as well as their family members about anxiety,
depression due to mental issues. The concept of mental health is quite necessary for overall well-
being such that physical and mental health are equally essential element of overall well-being.
Like depression generally enhances the possible risks for various types of the physical well-
being issues, mainly the long-lasting conditions such as cardiovascular illness, diabetes and the
stroke as well. similarly, the presence of all the acute conditions can significantly enhances the
potential risk for mental disorders among vulnerable patients.
It is essential to communicate with other healthcare professional which are effective and
lead to create high impact to provide better care services for improving mental health of
vulnerable people. Communication table enable BMI healthcare to effectively perform their role
towards mental health improvement.
Target Audience Goals Tools Time table
Program
implementation team
To implement
program effective for
Meeting with proper
document and
Monthly
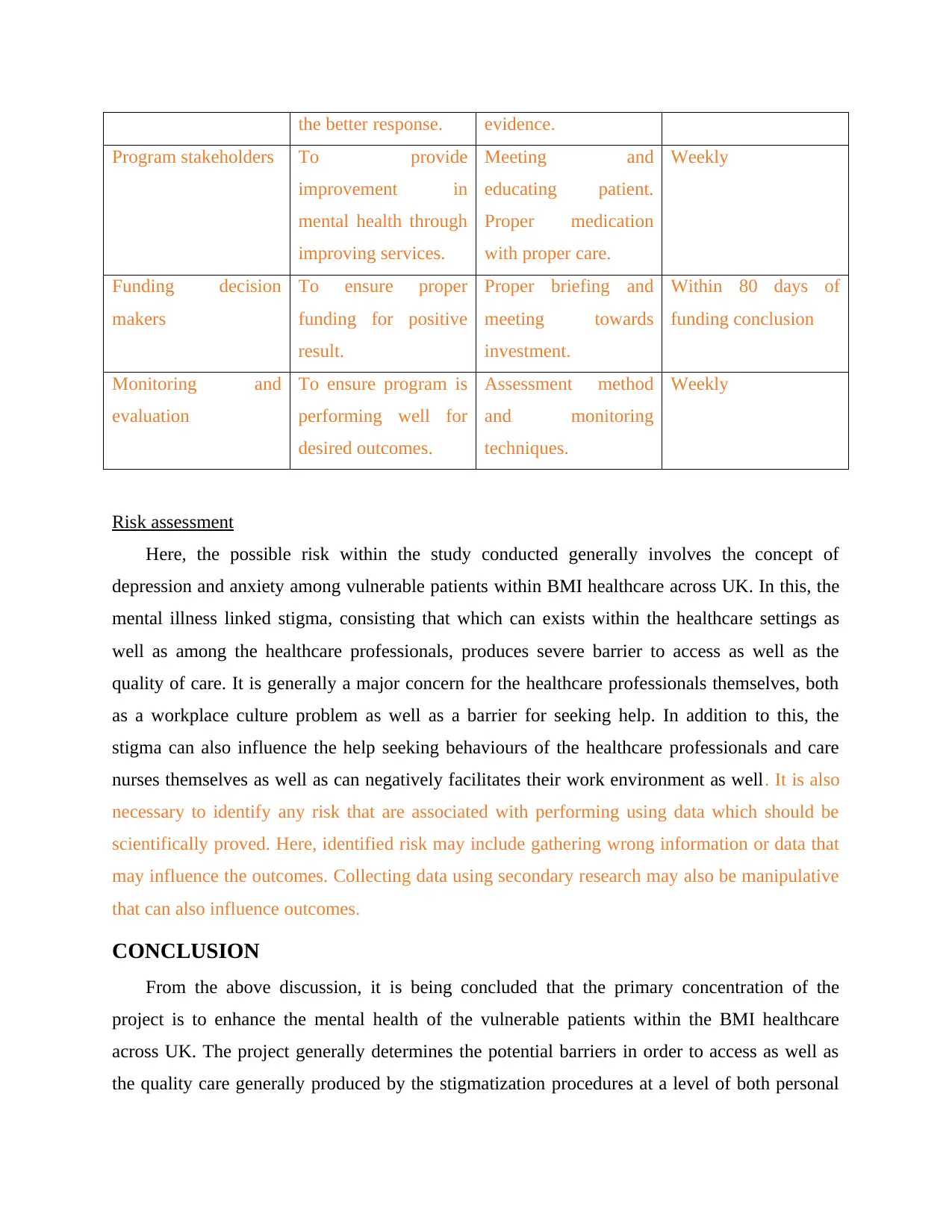
the better response. evidence.
Program stakeholders To provide
improvement in
mental health through
improving services.
Meeting and
educating patient.
Proper medication
with proper care.
Weekly
Funding decision
makers
To ensure proper
funding for positive
result.
Proper briefing and
meeting towards
investment.
Within 80 days of
funding conclusion
Monitoring and
evaluation
To ensure program is
performing well for
desired outcomes.
Assessment method
and monitoring
techniques.
Weekly
Risk assessment
Here, the possible risk within the study conducted generally involves the concept of
depression and anxiety among vulnerable patients within BMI healthcare across UK. In this, the
mental illness linked stigma, consisting that which can exists within the healthcare settings as
well as among the healthcare professionals, produces severe barrier to access as well as the
quality of care. It is generally a major concern for the healthcare professionals themselves, both
as a workplace culture problem as well as a barrier for seeking help. In addition to this, the
stigma can also influence the help seeking behaviours of the healthcare professionals and care
nurses themselves as well as can negatively facilitates their work environment as well. It is also
necessary to identify any risk that are associated with performing using data which should be
scientifically proved. Here, identified risk may include gathering wrong information or data that
may influence the outcomes. Collecting data using secondary research may also be manipulative
that can also influence outcomes.
CONCLUSION
From the above discussion, it is being concluded that the primary concentration of the
project is to enhance the mental health of the vulnerable patients within the BMI healthcare
across UK. The project generally determines the potential barriers in order to access as well as
the quality care generally produced by the stigmatization procedures at a level of both personal
Program stakeholders To provide
improvement in
mental health through
improving services.
Meeting and
educating patient.
Proper medication
with proper care.
Weekly
Funding decision
makers
To ensure proper
funding for positive
result.
Proper briefing and
meeting towards
investment.
Within 80 days of
funding conclusion
Monitoring and
evaluation
To ensure program is
performing well for
desired outcomes.
Assessment method
and monitoring
techniques.
Weekly
Risk assessment
Here, the possible risk within the study conducted generally involves the concept of
depression and anxiety among vulnerable patients within BMI healthcare across UK. In this, the
mental illness linked stigma, consisting that which can exists within the healthcare settings as
well as among the healthcare professionals, produces severe barrier to access as well as the
quality of care. It is generally a major concern for the healthcare professionals themselves, both
as a workplace culture problem as well as a barrier for seeking help. In addition to this, the
stigma can also influence the help seeking behaviours of the healthcare professionals and care
nurses themselves as well as can negatively facilitates their work environment as well. It is also
necessary to identify any risk that are associated with performing using data which should be
scientifically proved. Here, identified risk may include gathering wrong information or data that
may influence the outcomes. Collecting data using secondary research may also be manipulative
that can also influence outcomes.
CONCLUSION
From the above discussion, it is being concluded that the primary concentration of the
project is to enhance the mental health of the vulnerable patients within the BMI healthcare
across UK. The project generally determines the potential barriers in order to access as well as
the quality care generally produced by the stigmatization procedures at a level of both personal

as well as the interpersonal stigma and to determine the effective solutions which can effectively
executed within the healthcare industry as well. Within this, a key limitation of the evidence
illustrated in the above discussion is that various anti-stigma interventions are effectively
evaluated using the providers-based results more typically the behaviours and the attitudes
intentions of the well-being care providers. In addition to this, there is generally required more
study which can target the influence of the stigma reduction initiatives over the experience of the
patients as well as the significant care practices. Furthermore, the culture of a healthcare
organization which can encourage the well-being of vulnerable patients and staff well-being as
well as is efficiently committed towards combating the stigma within patient care is more likely
to have a positive influence over the staff and the safety of the vulnerable patients along with the
financial conditions.
executed within the healthcare industry as well. Within this, a key limitation of the evidence
illustrated in the above discussion is that various anti-stigma interventions are effectively
evaluated using the providers-based results more typically the behaviours and the attitudes
intentions of the well-being care providers. In addition to this, there is generally required more
study which can target the influence of the stigma reduction initiatives over the experience of the
patients as well as the significant care practices. Furthermore, the culture of a healthcare
organization which can encourage the well-being of vulnerable patients and staff well-being as
well as is efficiently committed towards combating the stigma within patient care is more likely
to have a positive influence over the staff and the safety of the vulnerable patients along with the
financial conditions.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
REFERENCES
Books and Journals
Alegría, M., NeMoyer, A., Falgàs Bagué, I., Wang, Y. and Alvarez, K., 2018. Social
determinants of mental health: where we are and where we need to go. Current psychiatry
reports, 20(11), pp.1-13.
Alonzi, S., La Torre, A. and Silverstein, M.W., 2020. The psychological impact of preexisting
mental and physical health conditions during the COVID-19 pandemic. Psychological
trauma: theory, research, practice, and policy, 12(S1), p.S236.
Arango, C., Díaz-Caneja, C.M., McGorry, P.D., Rapoport, J., Sommer, I.E., Vorstman, J.A.,
McDaid, D., Marín, O., Serrano-Drozdowskyj, E., Freedman, R. and Carpenter, W., 2018.
Preventive strategies for mental health. The Lancet Psychiatry, 5(7), pp.591-604.
Cénat, J.M., Felix, N., Blais-Rochette, C., Rousseau, C., Bukaka, J., Derivois, D., Noorishad,
P.G. and Birangui, J.P., 2020. Prevalence of mental health problems in populations
affected by the Ebola virus disease: A systematic review and meta-analysis. Psychiatry
research, 289, p.113033.
Courtenay, K. and Perera, B., 2020. COVID-19 and people with intellectual disability: impacts
of a pandemic. Irish Journal of Psychological Medicine, 37(3), pp.231-236.
Csaszar, F.A. and Ostler, J., 2020. A contingency theory of representational complexity in
organizations. Organization Science, 31(5), pp.1198-1219.
Galli, B.J., 2019. An engineering manager's guide for commonly used change management
approaches—from one practitioner's experience. IEEE Engineering Management
Review, 47(3), pp.118-126.
Gilbody, S., Peckham, E., Bailey, D., Arundel, C., Heron, P., Crosland, S., Fairhurst, C., Hewitt,
C., Li, J., Parrott, S. and Bradshaw, T., 2019. Smoking cessation for people with severe
mental illness (SCIMITAR+): a pragmatic randomised controlled trial. The Lancet
Psychiatry, 6(5), pp.379-390.
Grover, S., Dua, D., Sahoo, S., Mehra, A., Nehra, R. and Chakrabarti, S., 2020. Why all
COVID-19 hospitals should have mental health professionals: The importance of
mental health in a worldwide crisis!. Asian journal of psychiatry, 51, p.102147.
Hudon, C., Chouinard, M.C., Dubois, M.F., Roberge, P., Loignon, C., Tchouaket, É., Lambert,
M., Hudon, É., Diadiou, F. and Bouliane, D., 2018. Case management in primary care for
frequent users of health care services: a mixed methods study. The Annals of Family
Medicine, 16(3), pp.232-239.
Kertesz, S.G., deRussy, A.J., Kim, Y.I., Hoge, A.E., Austin, E.L., Gordon, A.J., Gelberg, L.,
Gabrielian, S.E., Riggs, K.R., Blosnich, J.R. and Montgomery, A.E., 2021. Comparison
of patient experience between primary care settings tailored for homeless clientele and
mainstream care settings. Medical care, 59(6), p.495.
Kiselev, N., Pfaltz, M., Haas, F., Schick, M., Kappen, M., Sijbrandij, M., De Graaff, A.M., Bird,
M., Hansen, P., Ventevogel, P. and Fuhr, D.C., 2020. Structural and socio-cultural
barriers to accessing mental healthcare among Syrian refugees and asylum seekers in
Switzerland. European journal of psychotraumatology, 11(1), p.1717825.
Lebano, A., Hamed, S., Bradby, H., Gil-Salmerón, A., Durá-Ferrandis, E., Garcés-Ferrer, J.,
Azzedine, F., Riza, E., Karnaki, P., Zota, D. and Linos, A., 2020. Migrants’ and refugees’
Books and Journals
Alegría, M., NeMoyer, A., Falgàs Bagué, I., Wang, Y. and Alvarez, K., 2018. Social
determinants of mental health: where we are and where we need to go. Current psychiatry
reports, 20(11), pp.1-13.
Alonzi, S., La Torre, A. and Silverstein, M.W., 2020. The psychological impact of preexisting
mental and physical health conditions during the COVID-19 pandemic. Psychological
trauma: theory, research, practice, and policy, 12(S1), p.S236.
Arango, C., Díaz-Caneja, C.M., McGorry, P.D., Rapoport, J., Sommer, I.E., Vorstman, J.A.,
McDaid, D., Marín, O., Serrano-Drozdowskyj, E., Freedman, R. and Carpenter, W., 2018.
Preventive strategies for mental health. The Lancet Psychiatry, 5(7), pp.591-604.
Cénat, J.M., Felix, N., Blais-Rochette, C., Rousseau, C., Bukaka, J., Derivois, D., Noorishad,
P.G. and Birangui, J.P., 2020. Prevalence of mental health problems in populations
affected by the Ebola virus disease: A systematic review and meta-analysis. Psychiatry
research, 289, p.113033.
Courtenay, K. and Perera, B., 2020. COVID-19 and people with intellectual disability: impacts
of a pandemic. Irish Journal of Psychological Medicine, 37(3), pp.231-236.
Csaszar, F.A. and Ostler, J., 2020. A contingency theory of representational complexity in
organizations. Organization Science, 31(5), pp.1198-1219.
Galli, B.J., 2019. An engineering manager's guide for commonly used change management
approaches—from one practitioner's experience. IEEE Engineering Management
Review, 47(3), pp.118-126.
Gilbody, S., Peckham, E., Bailey, D., Arundel, C., Heron, P., Crosland, S., Fairhurst, C., Hewitt,
C., Li, J., Parrott, S. and Bradshaw, T., 2019. Smoking cessation for people with severe
mental illness (SCIMITAR+): a pragmatic randomised controlled trial. The Lancet
Psychiatry, 6(5), pp.379-390.
Grover, S., Dua, D., Sahoo, S., Mehra, A., Nehra, R. and Chakrabarti, S., 2020. Why all
COVID-19 hospitals should have mental health professionals: The importance of
mental health in a worldwide crisis!. Asian journal of psychiatry, 51, p.102147.
Hudon, C., Chouinard, M.C., Dubois, M.F., Roberge, P., Loignon, C., Tchouaket, É., Lambert,
M., Hudon, É., Diadiou, F. and Bouliane, D., 2018. Case management in primary care for
frequent users of health care services: a mixed methods study. The Annals of Family
Medicine, 16(3), pp.232-239.
Kertesz, S.G., deRussy, A.J., Kim, Y.I., Hoge, A.E., Austin, E.L., Gordon, A.J., Gelberg, L.,
Gabrielian, S.E., Riggs, K.R., Blosnich, J.R. and Montgomery, A.E., 2021. Comparison
of patient experience between primary care settings tailored for homeless clientele and
mainstream care settings. Medical care, 59(6), p.495.
Kiselev, N., Pfaltz, M., Haas, F., Schick, M., Kappen, M., Sijbrandij, M., De Graaff, A.M., Bird,
M., Hansen, P., Ventevogel, P. and Fuhr, D.C., 2020. Structural and socio-cultural
barriers to accessing mental healthcare among Syrian refugees and asylum seekers in
Switzerland. European journal of psychotraumatology, 11(1), p.1717825.
Lebano, A., Hamed, S., Bradby, H., Gil-Salmerón, A., Durá-Ferrandis, E., Garcés-Ferrer, J.,
Azzedine, F., Riza, E., Karnaki, P., Zota, D. and Linos, A., 2020. Migrants’ and refugees’
health status and healthcare in Europe: a scoping literature review. BMC Public
Health, 20(1), pp.1-22.
Livingston, G., Rostamipour, H., Gallagher, P., Kalafatis, C., Shastri, A., Huzzey, L., Liu, K.,
Sommerlad, A. and Marston, L., 2020. Prevalence, management, and outcomes of SARS-
CoV-2 infections in older people and those with dementia in mental health wards in
London, UK: a retrospective observational study. The Lancet Psychiatry, 7(12), pp.1054-
1063.
Lundquist, A. and Haaheim, R., 2020. A review of Kotter's eight-step change model: Enlightened
by the case of the implementation of a new feed technology in Norway Royal
Salmon (Master's thesis, NTNU).
Makwana, N., 2019. Disaster and its impact on mental health: A narrative review. Journal of
family medicine and primary care, 8(10), p.3090.
Maphanga, P. and Nel, H., 2020. Identification of stakeholders in the project life cycle of a
capital project for a State-Owned enterprise in South Africa.
McAdam, R., Miller, K. and McSorley, C., 2019. Towards a contingency theory perspective of
quality management in enabling strategic alignment. International Journal of Production
Economics, 207, pp.195-209.
Orben, A., Tomova, L. and Blakemore, S.J., 2020. The effects of social deprivation on
adolescent development and mental health. The Lancet Child & Adolescent Health, 4(8),
pp.634-640.
Paramore, L., Yang, B., Abdelmotagly, Y., Noureldin, M., McLean, D., Rajkumar, G., Adamson,
A., Emara, A., White, C., Hindley, R. and Nedas, T., 2020. Delivering urgent urological
surgery during the COVID‐19 pandemic in the UK: Outcomes from our initial 52
patients. Bju International, 126(2), p.248.
Perregrini, M., 2019. Combating compassion fatigue. Nursing2021, 49(2), pp.50-54.
Saxe Zerden, L.D., Lombardi, B.M. and Jones, A., 2019. Social workers in integrated health
care: Improving care throughout the life course. Social Work in Health Care, 58(1),
pp.142-149.
Stevens, A.J., 2020. How can we meet the health needs of child refugees, asylum seekers and
undocumented migrants?. Archives of Disease in Childhood, 105(2), pp.191-196.
Tan, T.K., Gn, Y.M. and Goh, S.Y., 2019. ESRA19-0096 Implementing a regional anaesthesia
(RA) time-out procedure (TO) in our hospital: applying kotter’s ‘8 step change
management’(a management model).
Tiller, J. and Reynolds, S., 2020. Human trafficking in the emergency department: improving
our response to a vulnerable population. Western journal of emergency medicine, 21(3),
p.549.
Wang, J., Mann, F., Lloyd-Evans, B., Ma, R. and Johnson, S., 2018. Associations between
loneliness and perceived social support and outcomes of mental health problems: a
systematic review. BMC psychiatry, 18(1), pp.1-16.
Wibowo, M.A. and Uda, S.A.K., 2018. Reducing carbon emission in construction base on
project life cycle (PLC). In MATEC Web of Conferences (Vol. 195, p. 06002). EDP
Sciences.
Yau, B., Vijh, R., Prairie, J., McKee, G. and Schwandt, M., 2021. Lived experiences of frontline
workers and leaders during COVID-19 outbreaks in long-term care: A qualitative
study. American journal of infection control, 49(8), pp.978-984.
Health, 20(1), pp.1-22.
Livingston, G., Rostamipour, H., Gallagher, P., Kalafatis, C., Shastri, A., Huzzey, L., Liu, K.,
Sommerlad, A. and Marston, L., 2020. Prevalence, management, and outcomes of SARS-
CoV-2 infections in older people and those with dementia in mental health wards in
London, UK: a retrospective observational study. The Lancet Psychiatry, 7(12), pp.1054-
1063.
Lundquist, A. and Haaheim, R., 2020. A review of Kotter's eight-step change model: Enlightened
by the case of the implementation of a new feed technology in Norway Royal
Salmon (Master's thesis, NTNU).
Makwana, N., 2019. Disaster and its impact on mental health: A narrative review. Journal of
family medicine and primary care, 8(10), p.3090.
Maphanga, P. and Nel, H., 2020. Identification of stakeholders in the project life cycle of a
capital project for a State-Owned enterprise in South Africa.
McAdam, R., Miller, K. and McSorley, C., 2019. Towards a contingency theory perspective of
quality management in enabling strategic alignment. International Journal of Production
Economics, 207, pp.195-209.
Orben, A., Tomova, L. and Blakemore, S.J., 2020. The effects of social deprivation on
adolescent development and mental health. The Lancet Child & Adolescent Health, 4(8),
pp.634-640.
Paramore, L., Yang, B., Abdelmotagly, Y., Noureldin, M., McLean, D., Rajkumar, G., Adamson,
A., Emara, A., White, C., Hindley, R. and Nedas, T., 2020. Delivering urgent urological
surgery during the COVID‐19 pandemic in the UK: Outcomes from our initial 52
patients. Bju International, 126(2), p.248.
Perregrini, M., 2019. Combating compassion fatigue. Nursing2021, 49(2), pp.50-54.
Saxe Zerden, L.D., Lombardi, B.M. and Jones, A., 2019. Social workers in integrated health
care: Improving care throughout the life course. Social Work in Health Care, 58(1),
pp.142-149.
Stevens, A.J., 2020. How can we meet the health needs of child refugees, asylum seekers and
undocumented migrants?. Archives of Disease in Childhood, 105(2), pp.191-196.
Tan, T.K., Gn, Y.M. and Goh, S.Y., 2019. ESRA19-0096 Implementing a regional anaesthesia
(RA) time-out procedure (TO) in our hospital: applying kotter’s ‘8 step change
management’(a management model).
Tiller, J. and Reynolds, S., 2020. Human trafficking in the emergency department: improving
our response to a vulnerable population. Western journal of emergency medicine, 21(3),
p.549.
Wang, J., Mann, F., Lloyd-Evans, B., Ma, R. and Johnson, S., 2018. Associations between
loneliness and perceived social support and outcomes of mental health problems: a
systematic review. BMC psychiatry, 18(1), pp.1-16.
Wibowo, M.A. and Uda, S.A.K., 2018. Reducing carbon emission in construction base on
project life cycle (PLC). In MATEC Web of Conferences (Vol. 195, p. 06002). EDP
Sciences.
Yau, B., Vijh, R., Prairie, J., McKee, G. and Schwandt, M., 2021. Lived experiences of frontline
workers and leaders during COVID-19 outbreaks in long-term care: A qualitative
study. American journal of infection control, 49(8), pp.978-984.
1 out of 21
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





