NUR2200 Mental Health Across the Lifespan: MSE Report
VerifiedAdded on 2023/01/07
|7
|2360
|66
Report
AI Summary
This report presents a comprehensive Mental State Examination (MSE) of a 16-year-old male, Peter Smith, admitted to an adolescent mental health unit. The assessment covers general appearance, behavior, speech, mood, affect, thought process, thought content, perception, cognition, insight, and judgment. Peter presents with a cachexic appearance, low BMI, and signs of anorexia nervosa, including body image concerns and impaired nutritional intake. The report details nursing interventions, including behavioral modifications and meal supervision to address nutritional deficiencies and body image issues. It also includes a nursing report using the SHARED handover tool, outlining Peter's medical history, current condition, risks (including suicidal ideation), and required interventions, such as 24-hour observation and regular medical reviews. The report references several studies related to mental health and adolescent eating disorders.
Assessment name NUR2200 Mental Health Across
the Lifespan
Mental State Examination
Assessment
MENTAL STATE EXAMINATION
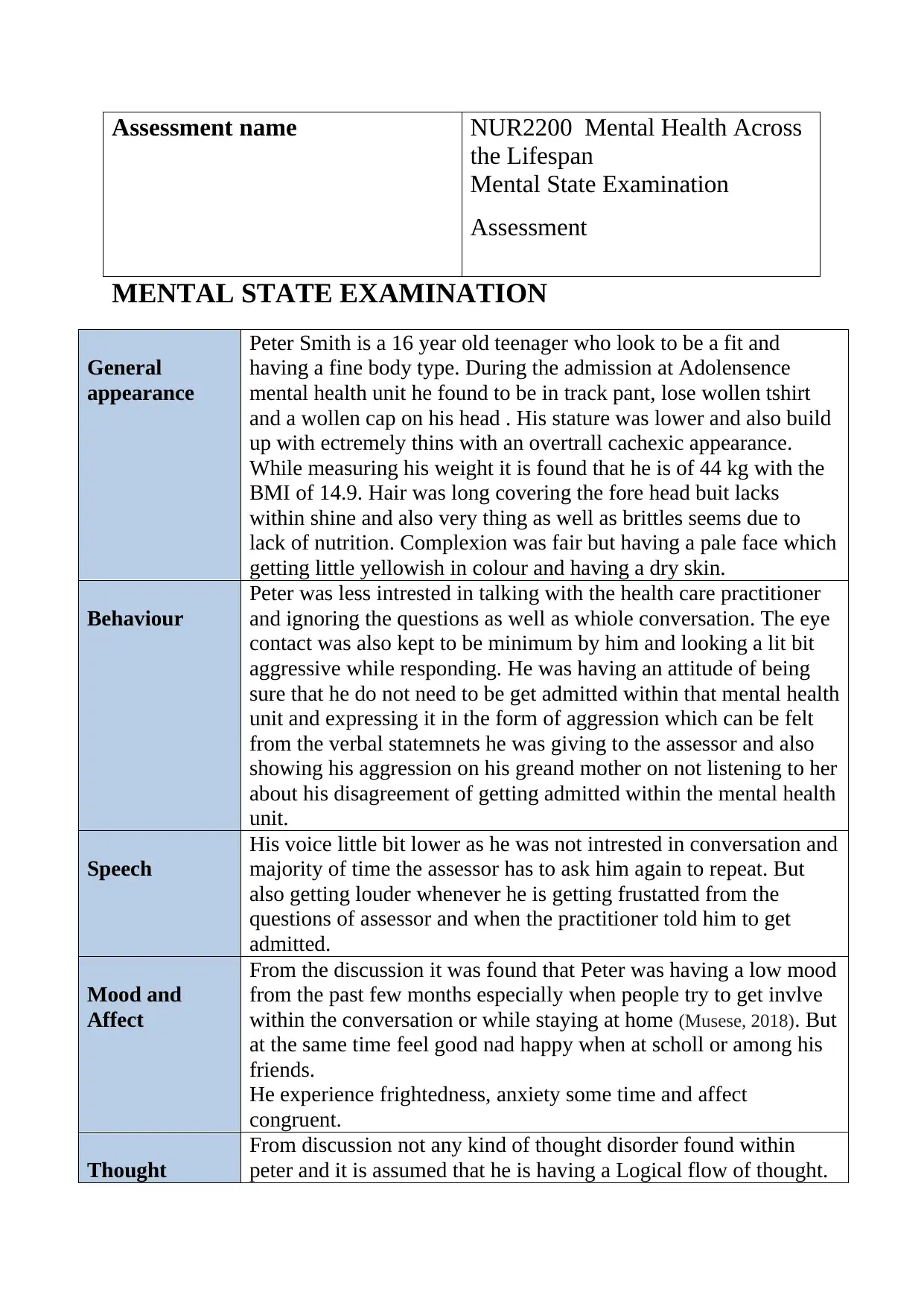
General
appearance
Peter Smith is a 16 year old teenager who look to be a fit and
having a fine body type. During the admission at Adolensence
mental health unit he found to be in track pant, lose wollen tshirt
and a wollen cap on his head . His stature was lower and also build
up with ectremely thins with an overtrall cachexic appearance.
While measuring his weight it is found that he is of 44 kg with the
BMI of 14.9. Hair was long covering the fore head buit lacks
within shine and also very thing as well as brittles seems due to
lack of nutrition. Complexion was fair but having a pale face which
getting little yellowish in colour and having a dry skin.
Behaviour
Peter was less intrested in talking with the health care practitioner
and ignoring the questions as well as whiole conversation. The eye
contact was also kept to be minimum by him and looking a lit bit
aggressive while responding. He was having an attitude of being
sure that he do not need to be get admitted within that mental health
unit and expressing it in the form of aggression which can be felt
from the verbal statemnets he was giving to the assessor and also
showing his aggression on his greand mother on not listening to her
about his disagreement of getting admitted within the mental health
unit.
Speech
His voice little bit lower as he was not intrested in conversation and
majority of time the assessor has to ask him again to repeat. But
also getting louder whenever he is getting frustatted from the
questions of assessor and when the practitioner told him to get
admitted.
Mood and
Affect
From the discussion it was found that Peter was having a low mood
from the past few months especially when people try to get invlve
within the conversation or while staying at home (Musese, 2018). But
at the same time feel good nad happy when at scholl or among his
friends.
He experience frightedness, anxiety some time and affect
congruent.
Thought
From discussion not any kind of thought disorder found within
peter and it is assumed that he is having a Logical flow of thought.
the Lifespan
Mental State Examination
Assessment
MENTAL STATE EXAMINATION
General
appearance
Peter Smith is a 16 year old teenager who look to be a fit and
having a fine body type. During the admission at Adolensence
mental health unit he found to be in track pant, lose wollen tshirt
and a wollen cap on his head . His stature was lower and also build
up with ectremely thins with an overtrall cachexic appearance.
While measuring his weight it is found that he is of 44 kg with the
BMI of 14.9. Hair was long covering the fore head buit lacks
within shine and also very thing as well as brittles seems due to
lack of nutrition. Complexion was fair but having a pale face which
getting little yellowish in colour and having a dry skin.
Behaviour
Peter was less intrested in talking with the health care practitioner
and ignoring the questions as well as whiole conversation. The eye
contact was also kept to be minimum by him and looking a lit bit
aggressive while responding. He was having an attitude of being
sure that he do not need to be get admitted within that mental health
unit and expressing it in the form of aggression which can be felt
from the verbal statemnets he was giving to the assessor and also
showing his aggression on his greand mother on not listening to her
about his disagreement of getting admitted within the mental health
unit.
Speech
His voice little bit lower as he was not intrested in conversation and
majority of time the assessor has to ask him again to repeat. But
also getting louder whenever he is getting frustatted from the
questions of assessor and when the practitioner told him to get
admitted.
Mood and
Affect
From the discussion it was found that Peter was having a low mood
from the past few months especially when people try to get invlve
within the conversation or while staying at home (Musese, 2018). But
at the same time feel good nad happy when at scholl or among his
friends.
He experience frightedness, anxiety some time and affect
congruent.
Thought
From discussion not any kind of thought disorder found within
peter and it is assumed that he is having a Logical flow of thought.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
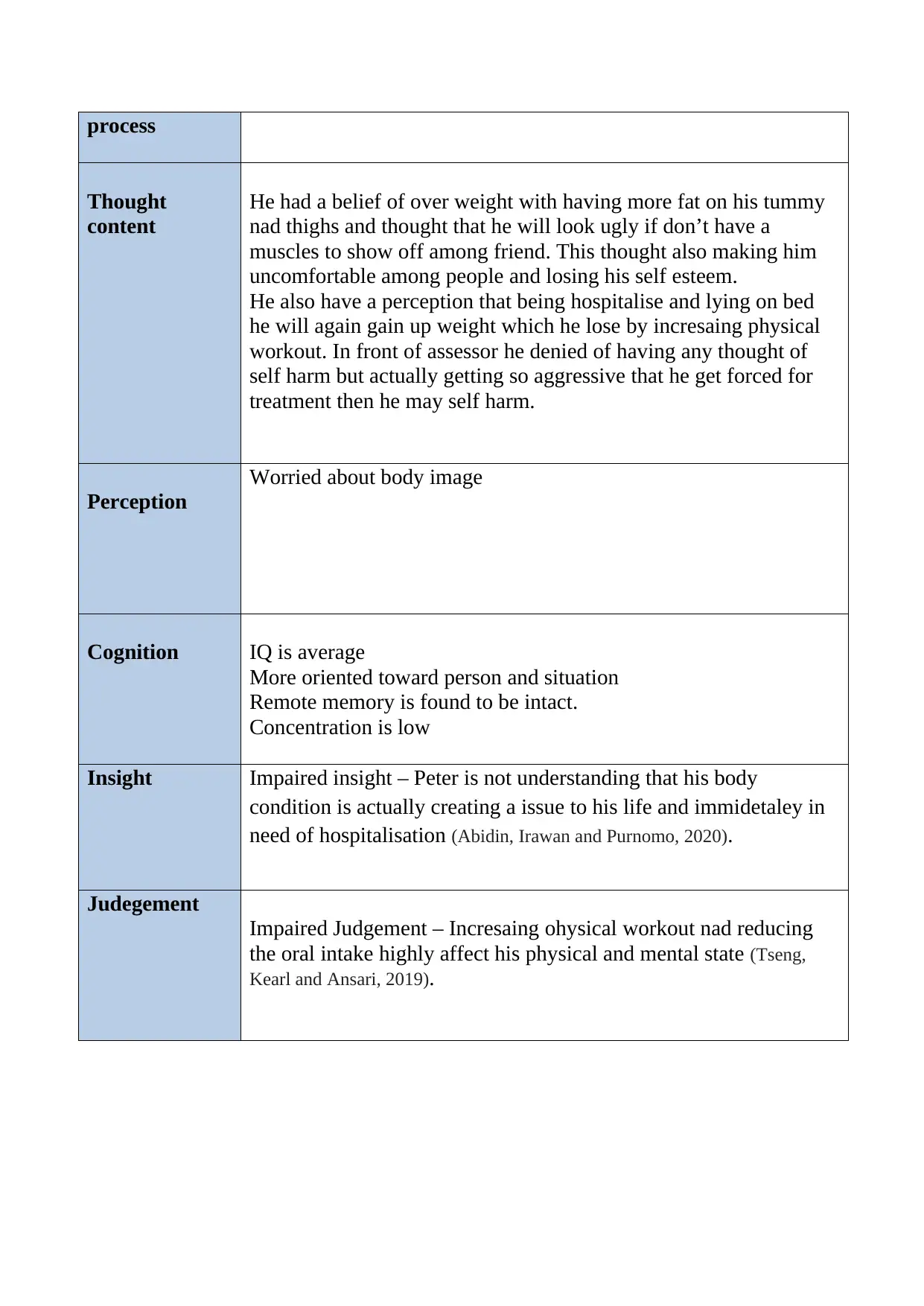
process
Thought
content
He had a belief of over weight with having more fat on his tummy
nad thighs and thought that he will look ugly if don’t have a
muscles to show off among friend. This thought also making him
uncomfortable among people and losing his self esteem.
He also have a perception that being hospitalise and lying on bed
he will again gain up weight which he lose by incresaing physical
workout. In front of assessor he denied of having any thought of
self harm but actually getting so aggressive that he get forced for
treatment then he may self harm.
Perception
Worried about body image
Cognition IQ is average
More oriented toward person and situation
Remote memory is found to be intact.
Concentration is low
Insight Impaired insight – Peter is not understanding that his body
condition is actually creating a issue to his life and immidetaley in
need of hospitalisation (Abidin, Irawan and Purnomo, 2020).
Judegement
Impaired Judgement – Incresaing ohysical workout nad reducing
the oral intake highly affect his physical and mental state (Tseng,
Kearl and Ansari, 2019).
Thought
content
He had a belief of over weight with having more fat on his tummy
nad thighs and thought that he will look ugly if don’t have a
muscles to show off among friend. This thought also making him
uncomfortable among people and losing his self esteem.
He also have a perception that being hospitalise and lying on bed
he will again gain up weight which he lose by incresaing physical
workout. In front of assessor he denied of having any thought of
self harm but actually getting so aggressive that he get forced for
treatment then he may self harm.
Perception
Worried about body image
Cognition IQ is average
More oriented toward person and situation
Remote memory is found to be intact.
Concentration is low
Insight Impaired insight – Peter is not understanding that his body
condition is actually creating a issue to his life and immidetaley in
need of hospitalisation (Abidin, Irawan and Purnomo, 2020).
Judegement
Impaired Judgement – Incresaing ohysical workout nad reducing
the oral intake highly affect his physical and mental state (Tseng,
Kearl and Ansari, 2019).
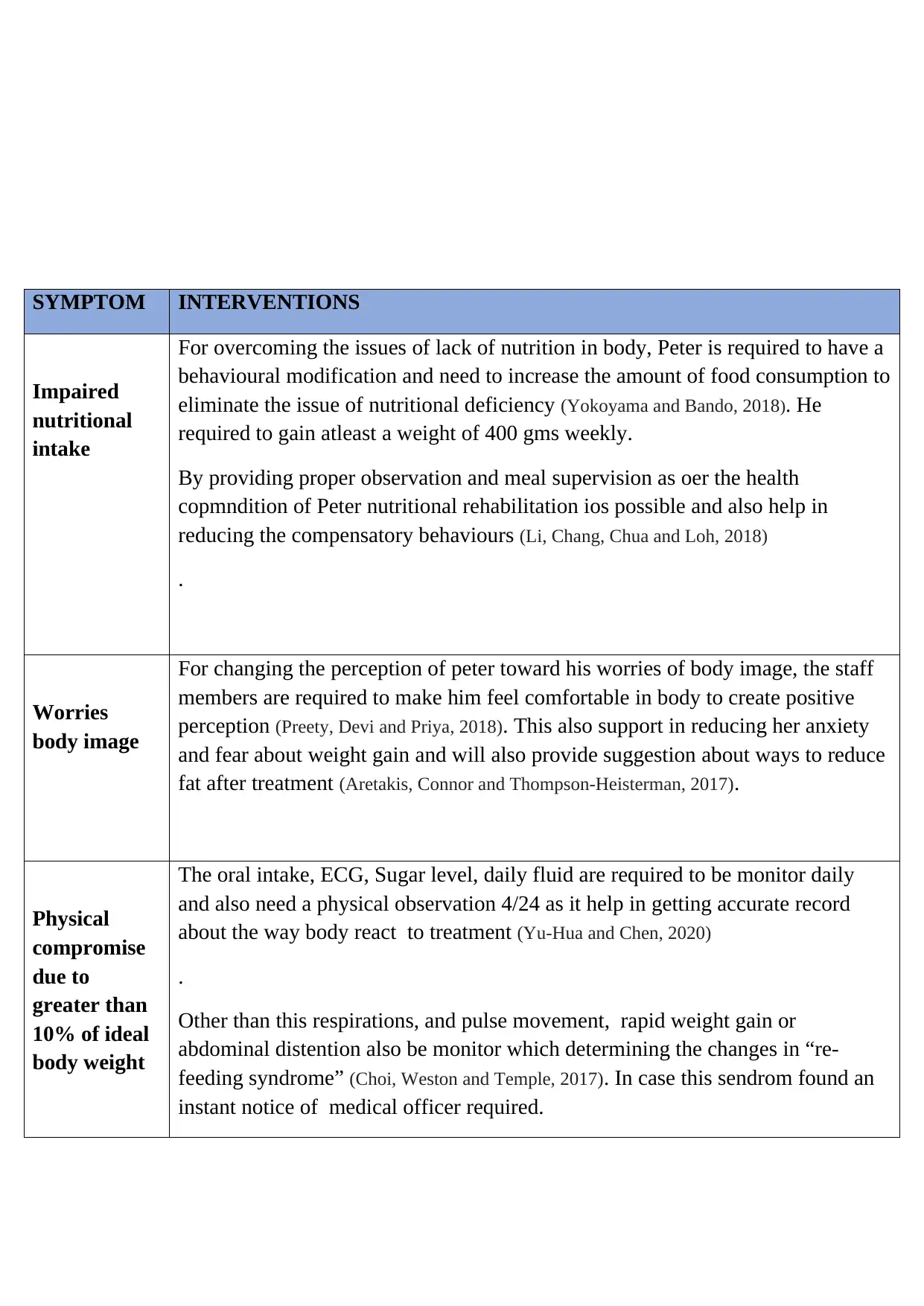
SYMPTOM INTERVENTIONS
Impaired
nutritional
intake
For overcoming the issues of lack of nutrition in body, Peter is required to have a
behavioural modification and need to increase the amount of food consumption to
eliminate the issue of nutritional deficiency (Yokoyama and Bando, 2018). He
required to gain atleast a weight of 400 gms weekly.
By providing proper observation and meal supervision as oer the health
copmndition of Peter nutritional rehabilitation ios possible and also help in
reducing the compensatory behaviours (Li, Chang, Chua and Loh, 2018)
.
Worries
body image
For changing the perception of peter toward his worries of body image, the staff
members are required to make him feel comfortable in body to create positive
perception (Preety, Devi and Priya, 2018). This also support in reducing her anxiety
and fear about weight gain and will also provide suggestion about ways to reduce
fat after treatment (Aretakis, Connor and Thompson-Heisterman, 2017).
Physical
compromise
due to
greater than
10% of ideal
body weight
The oral intake, ECG, Sugar level, daily fluid are required to be monitor daily
and also need a physical observation 4/24 as it help in getting accurate record
about the way body react to treatment (Yu-Hua and Chen, 2020)
.
Other than this respirations, and pulse movement, rapid weight gain or
abdominal distention also be monitor which determining the changes in “re-
feeding syndrome” (Choi, Weston and Temple, 2017). In case this sendrom found an
instant notice of medical officer required.
Impaired
nutritional
intake
For overcoming the issues of lack of nutrition in body, Peter is required to have a
behavioural modification and need to increase the amount of food consumption to
eliminate the issue of nutritional deficiency (Yokoyama and Bando, 2018). He
required to gain atleast a weight of 400 gms weekly.
By providing proper observation and meal supervision as oer the health
copmndition of Peter nutritional rehabilitation ios possible and also help in
reducing the compensatory behaviours (Li, Chang, Chua and Loh, 2018)
.
Worries
body image
For changing the perception of peter toward his worries of body image, the staff
members are required to make him feel comfortable in body to create positive
perception (Preety, Devi and Priya, 2018). This also support in reducing her anxiety
and fear about weight gain and will also provide suggestion about ways to reduce
fat after treatment (Aretakis, Connor and Thompson-Heisterman, 2017).
Physical
compromise
due to
greater than
10% of ideal
body weight
The oral intake, ECG, Sugar level, daily fluid are required to be monitor daily
and also need a physical observation 4/24 as it help in getting accurate record
about the way body react to treatment (Yu-Hua and Chen, 2020)
.
Other than this respirations, and pulse movement, rapid weight gain or
abdominal distention also be monitor which determining the changes in “re-
feeding syndrome” (Choi, Weston and Temple, 2017). In case this sendrom found an
instant notice of medical officer required.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
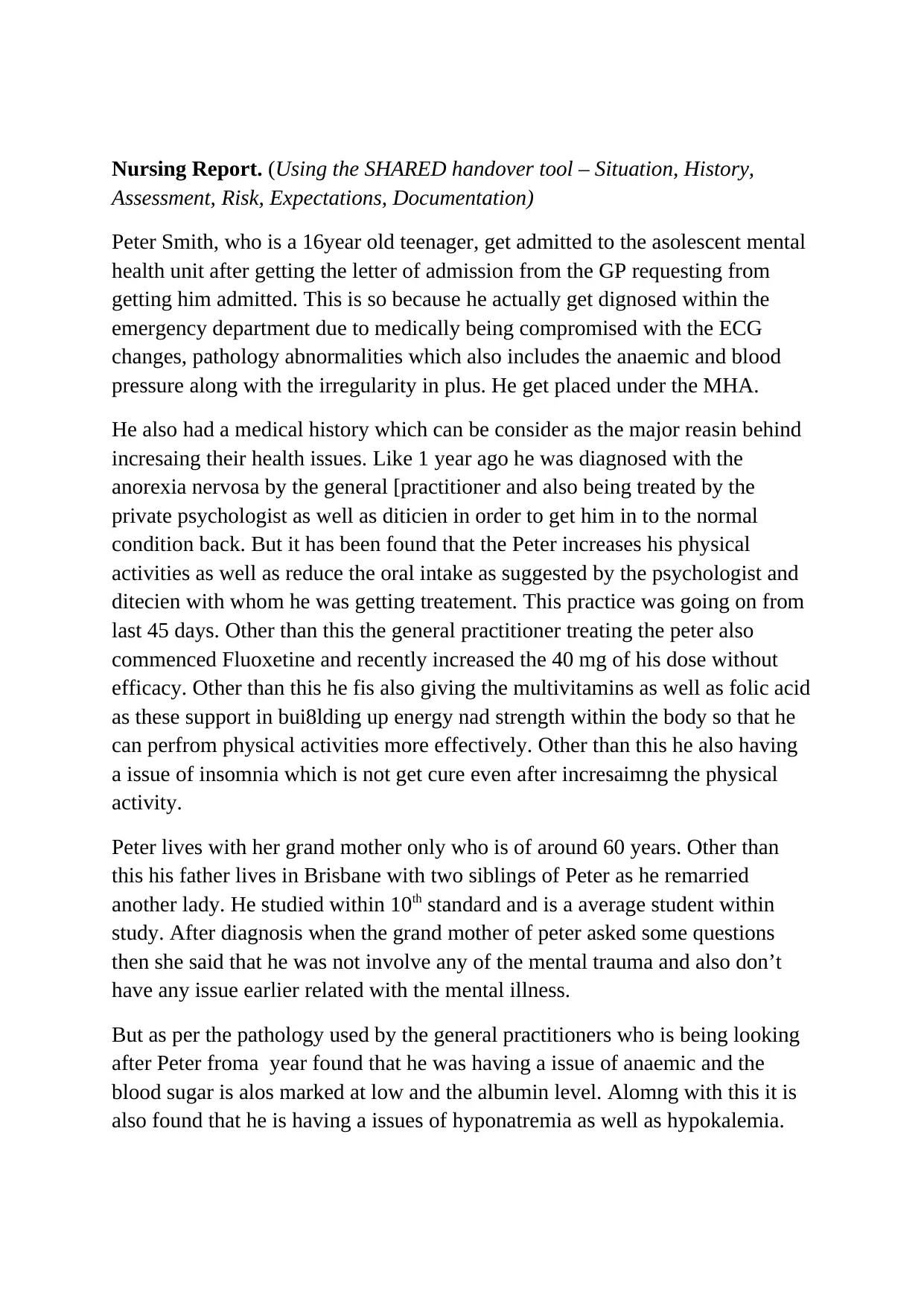
Nursing Report. (Using the SHARED handover tool – Situation, History,
Assessment, Risk, Expectations, Documentation)
Peter Smith, who is a 16year old teenager, get admitted to the asolescent mental
health unit after getting the letter of admission from the GP requesting from
getting him admitted. This is so because he actually get dignosed within the
emergency department due to medically being compromised with the ECG
changes, pathology abnormalities which also includes the anaemic and blood
pressure along with the irregularity in plus. He get placed under the MHA.
He also had a medical history which can be consider as the major reasin behind
incresaing their health issues. Like 1 year ago he was diagnosed with the
anorexia nervosa by the general [practitioner and also being treated by the
private psychologist as well as diticien in order to get him in to the normal
condition back. But it has been found that the Peter increases his physical
activities as well as reduce the oral intake as suggested by the psychologist and
ditecien with whom he was getting treatement. This practice was going on from
last 45 days. Other than this the general practitioner treating the peter also
commenced Fluoxetine and recently increased the 40 mg of his dose without
efficacy. Other than this he fis also giving the multivitamins as well as folic acid
as these support in bui8lding up energy nad strength within the body so that he
can perfrom physical activities more effectively. Other than this he also having
a issue of insomnia which is not get cure even after incresaimng the physical
activity.
Peter lives with her grand mother only who is of around 60 years. Other than
this his father lives in Brisbane with two siblings of Peter as he remarried
another lady. He studied within 10th standard and is a average student within
study. After diagnosis when the grand mother of peter asked some questions
then she said that he was not involve any of the mental trauma and also don’t
have any issue earlier related with the mental illness.
But as per the pathology used by the general practitioners who is being looking
after Peter froma year found that he was having a issue of anaemic and the
blood sugar is alos marked at low and the albumin level. Alomng with this it is
also found that he is having a issues of hyponatremia as well as hypokalemia.
Assessment, Risk, Expectations, Documentation)
Peter Smith, who is a 16year old teenager, get admitted to the asolescent mental
health unit after getting the letter of admission from the GP requesting from
getting him admitted. This is so because he actually get dignosed within the
emergency department due to medically being compromised with the ECG
changes, pathology abnormalities which also includes the anaemic and blood
pressure along with the irregularity in plus. He get placed under the MHA.
He also had a medical history which can be consider as the major reasin behind
incresaing their health issues. Like 1 year ago he was diagnosed with the
anorexia nervosa by the general [practitioner and also being treated by the
private psychologist as well as diticien in order to get him in to the normal
condition back. But it has been found that the Peter increases his physical
activities as well as reduce the oral intake as suggested by the psychologist and
ditecien with whom he was getting treatement. This practice was going on from
last 45 days. Other than this the general practitioner treating the peter also
commenced Fluoxetine and recently increased the 40 mg of his dose without
efficacy. Other than this he fis also giving the multivitamins as well as folic acid
as these support in bui8lding up energy nad strength within the body so that he
can perfrom physical activities more effectively. Other than this he also having
a issue of insomnia which is not get cure even after incresaimng the physical
activity.
Peter lives with her grand mother only who is of around 60 years. Other than
this his father lives in Brisbane with two siblings of Peter as he remarried
another lady. He studied within 10th standard and is a average student within
study. After diagnosis when the grand mother of peter asked some questions
then she said that he was not involve any of the mental trauma and also don’t
have any issue earlier related with the mental illness.
But as per the pathology used by the general practitioners who is being looking
after Peter froma year found that he was having a issue of anaemic and the
blood sugar is alos marked at low and the albumin level. Alomng with this it is
also found that he is having a issues of hyponatremia as well as hypokalemia.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
After hearing about that he is suggfested to shift to the adolescence mental
health unit he get anxious and also frightened after hearing about it. This was a
difficult case to being engage with in spercially during the admission process of
peter as his voicing was seems to be having a suicidal ideation in case she were
put to weight on. He was experience a fat over his body like he saod that he
perceive her stomach as wella s thighs are getting too much fatty and heavier as
a result of which he instantly losse his self esteem at that point.
If we talk about the physical appearance of peter, then it kee through a anorexia
nervosa diagnosis along with the cathexic appearance which involve a low body
weight which was about 44 kg along with the BMI which was marked at the
14.9. Other then this the lanugo has also being evident on his face as well as her
hair which get brittle. At the time of admission to the adolescence mental health
unit he was waering a losse and over sized t shirt which was actually a kind of
warmer as he said he was feeling little bit cold at that time and also found at the
temeperature of around 35.4.
His decision toward getting restricted to the incresaing the physical exerecise as
well as reducing the oral intake is also impaired that get correlated with the lack
of insight within rhe current physical condition as well as also his body is
getting so much affected that he required the hospitalisation instantlty. This is
so because she actually get tired and lower energy to stant effectively, it was
actually relasied from the declining of the concentration and as he was not
taking much attension or was found to be disappear somewhere when he do not
responde after attempting to call agaian and again.
By having discussion with her about her easiness and daily routine to know how
the things are going on within her life or what kind of health issues he is facing.
While this conversation he said that he was very happy at school, he had good
friends with whom he talks and enjoy a lot. But sometimes he feels low within
his mood but rest of the time he use to be ok. After that he get angry that the he
is ok and he is forcefully being hospitalised by the doctor and by staying at
hospital over bed he will not be able to loose weight he gained in order to get
her goal of losing weight till 40 kg and also voiced about the ideal of attempt
suicide.
So from the scenario it can be said that the risk realetd with the aggression as
well as violence are lower in case of peter, but the chances for the suicide as
wella s self harm is tend to be moderate. This is so because he is also at the risk
health unit he get anxious and also frightened after hearing about it. This was a
difficult case to being engage with in spercially during the admission process of
peter as his voicing was seems to be having a suicidal ideation in case she were
put to weight on. He was experience a fat over his body like he saod that he
perceive her stomach as wella s thighs are getting too much fatty and heavier as
a result of which he instantly losse his self esteem at that point.
If we talk about the physical appearance of peter, then it kee through a anorexia
nervosa diagnosis along with the cathexic appearance which involve a low body
weight which was about 44 kg along with the BMI which was marked at the
14.9. Other then this the lanugo has also being evident on his face as well as her
hair which get brittle. At the time of admission to the adolescence mental health
unit he was waering a losse and over sized t shirt which was actually a kind of
warmer as he said he was feeling little bit cold at that time and also found at the
temeperature of around 35.4.
His decision toward getting restricted to the incresaing the physical exerecise as
well as reducing the oral intake is also impaired that get correlated with the lack
of insight within rhe current physical condition as well as also his body is
getting so much affected that he required the hospitalisation instantlty. This is
so because she actually get tired and lower energy to stant effectively, it was
actually relasied from the declining of the concentration and as he was not
taking much attension or was found to be disappear somewhere when he do not
responde after attempting to call agaian and again.
By having discussion with her about her easiness and daily routine to know how
the things are going on within her life or what kind of health issues he is facing.
While this conversation he said that he was very happy at school, he had good
friends with whom he talks and enjoy a lot. But sometimes he feels low within
his mood but rest of the time he use to be ok. After that he get angry that the he
is ok and he is forcefully being hospitalised by the doctor and by staying at
hospital over bed he will not be able to loose weight he gained in order to get
her goal of losing weight till 40 kg and also voiced about the ideal of attempt
suicide.
So from the scenario it can be said that the risk realetd with the aggression as
well as violence are lower in case of peter, but the chances for the suicide as
wella s self harm is tend to be moderate. This is so because he is also at the risk
of sabotaging about her meal program which is due to the impaired decision
making. As a result of which the RMO ordered that the staff memebesr must
keep their eye 24 hour on peter so that he won’t get any chance to run awaty or
harm himself in any maner. Other than this it was also oredre to have an eye on
him specially at the time of meal nd after the meal till 60 minute. Do by getting
under the MHA, daily review by the consultant as well as registrar, the risk
assessment done on regular basis. Other this the medical officers are also
requiresent for daily measuring the ECG as well as BSL and 4/24 observation
with standing as well as sitting P and BP measures along with the daily
pathology.
REFERENCE LIST
Abidin, D.S., Irawan, R. and Purnomo, W., 2020. Effect of Nutritional Status, Hemoglobin
Levels and Psychosocial Emotional Behavior with Cognitive Function of Female
Teenager. Indian Journal of Public Health Research & Development, 11(1),
pp.1040-1044.
Li, P., Chang, L., Chua, T.H.H. and Loh, R.S.M., 2018. “Likes” as KPI: An examination of
teenage girls’ perspective on peer feedback on Instagram and its influence on coping
response. Telematics and Informatics, 35(7), pp.1994-2005.
Aretakis, D.A., Connor, A. and Thompson-Heisterman, A., 2017. Poverty, Homelessness,
Teen Pregnancy, and Mental Illness. Foundations for Population Health in
Community/Public Health Nursing-E-Book, p.392.
Yu-Hua, C. and Chen, J., 2020. A corpus-based study of depressive language in online teen
health communications. working paper, unpublished.
Choi, H.J., Weston, R. and Temple, J.R., 2017. A three-step latent class analysis to identify
how different patterns of teen dating violence and psychosocial factors influence
mental health. Journal of youth and adolescence, 46(4), pp.854-866.
Preety, R., Devi, R.G. and Priya, A.J., 2018. Sleep deprivation and cell phone usage among
teenagers. Drug Invention Today, 10(10).
Yokoyama, T. and Bando, H., 2018. The Egogram Feature of Late Teenager in the Internet
Generation. Clinical Research in Psychology, 1(2).
Tseng, P., Kearl, Y.L. and Ansari, A., 2019. Roller Coaster–Induced Subdural Hematoma in
a Previously Healthy Teenager. Pediatric emergency care, 35(4), pp.e76-e78.
Balgir, R.S. and et. al., 2016. Distribution of psychiatric morbidity among school going
adolescents in a district of North India. International Journal of Medical Research &
Health Sciences, 5(5), pp.1-9.
Musese, A.N., 2018. Mental health and coping strategies of teenage mothers in the Kavango
regions (Doctoral dissertation, University of Namibia).
making. As a result of which the RMO ordered that the staff memebesr must
keep their eye 24 hour on peter so that he won’t get any chance to run awaty or
harm himself in any maner. Other than this it was also oredre to have an eye on
him specially at the time of meal nd after the meal till 60 minute. Do by getting
under the MHA, daily review by the consultant as well as registrar, the risk
assessment done on regular basis. Other this the medical officers are also
requiresent for daily measuring the ECG as well as BSL and 4/24 observation
with standing as well as sitting P and BP measures along with the daily
pathology.
REFERENCE LIST
Abidin, D.S., Irawan, R. and Purnomo, W., 2020. Effect of Nutritional Status, Hemoglobin
Levels and Psychosocial Emotional Behavior with Cognitive Function of Female
Teenager. Indian Journal of Public Health Research & Development, 11(1),
pp.1040-1044.
Li, P., Chang, L., Chua, T.H.H. and Loh, R.S.M., 2018. “Likes” as KPI: An examination of
teenage girls’ perspective on peer feedback on Instagram and its influence on coping
response. Telematics and Informatics, 35(7), pp.1994-2005.
Aretakis, D.A., Connor, A. and Thompson-Heisterman, A., 2017. Poverty, Homelessness,
Teen Pregnancy, and Mental Illness. Foundations for Population Health in
Community/Public Health Nursing-E-Book, p.392.
Yu-Hua, C. and Chen, J., 2020. A corpus-based study of depressive language in online teen
health communications. working paper, unpublished.
Choi, H.J., Weston, R. and Temple, J.R., 2017. A three-step latent class analysis to identify
how different patterns of teen dating violence and psychosocial factors influence
mental health. Journal of youth and adolescence, 46(4), pp.854-866.
Preety, R., Devi, R.G. and Priya, A.J., 2018. Sleep deprivation and cell phone usage among
teenagers. Drug Invention Today, 10(10).
Yokoyama, T. and Bando, H., 2018. The Egogram Feature of Late Teenager in the Internet
Generation. Clinical Research in Psychology, 1(2).
Tseng, P., Kearl, Y.L. and Ansari, A., 2019. Roller Coaster–Induced Subdural Hematoma in
a Previously Healthy Teenager. Pediatric emergency care, 35(4), pp.e76-e78.
Balgir, R.S. and et. al., 2016. Distribution of psychiatric morbidity among school going
adolescents in a district of North India. International Journal of Medical Research &
Health Sciences, 5(5), pp.1-9.
Musese, A.N., 2018. Mental health and coping strategies of teenage mothers in the Kavango
regions (Doctoral dissertation, University of Namibia).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

1 out of 7
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





