Detailed Case Study: Mental Status Examination of Patient Dimitrie
VerifiedAdded on 2021/09/10
|9
|2414
|61
Case Study
AI Summary
This case study presents a mental status examination of a patient named Dimitrie, detailing his appearance, behavior, affect, mood, speech, thought process, thought content, perception, cognition, and insight. The assessment reveals symptoms consistent with delusional thinking and auditory hallucinations. The examination highlights Dimitrie's distress, anxiety, and disruptions in thought. A care plan is proposed, emphasizing the importance of antipsychotic medication management, the development of a therapeutic relationship, and interventions to address the patient's delusions. The critique of the interview highlights the nurse's use of active listening skills and the barriers to communication. The document also includes a reference list of supporting literature.
1. Mental Status Examination
APPEARANCE- The early insight into Dimitrie’s appearance follows at the mental
health clinic, discovering he was sitting in a chair in an upright position, appearing to be
dazed and nervous. Dimitrie is a young man with black hair above the shoulders, with
Asian descent, wearing reading glasses, having a small build, moustache, and fair
complexion. Dimitrie wore a long sleeve flannel and pants; clothing appeared tidy,
which indicated a typical level of personal hygiene and self-care. Dimitrie did not have
any visible tattoos or piercings. Consequent to Dimitrie’s arrival at the clinic he emerges
as very tense at times and his facial expressions change rapidly from fixated to
disorientated which depicts his poor poise.
BEHAVIOUR- It was clear Dimitrie was distraught and anxious as he became agitated
with the voices that were in his head as they were ‘criticising’ him. Dimitrie presents
reduced eye contact to the mental health nurse, though he is able to build rapport and is
slow to engage with the clinician; he is co-operative and showing signs of compliance
as he mostly answers the nurse’s questions, appropriately. Signs of psychomotor
agitation can be shown as the patient shows episodes temporary inattentiveness, and
responds to the voices he is hearing; as he says ‘sorry what was the question again’ or in
response to his writing ‘I will finish it, so shut up’ which also demonstrates his negative
attitude and outlook. Dimitrie is unable to focus either looking into space or distracted
by saying ‘just leave me alone’ to the voices he hears.
AFFECT- Dimitrie produces some emotional responsiveness, suggested from his
anxious facial expressions; Dimitrie has also shown an impediment in terminating an
emotional response when triggered by voices, or discussing a sensitive topic; which
APPEARANCE- The early insight into Dimitrie’s appearance follows at the mental
health clinic, discovering he was sitting in a chair in an upright position, appearing to be
dazed and nervous. Dimitrie is a young man with black hair above the shoulders, with
Asian descent, wearing reading glasses, having a small build, moustache, and fair
complexion. Dimitrie wore a long sleeve flannel and pants; clothing appeared tidy,
which indicated a typical level of personal hygiene and self-care. Dimitrie did not have
any visible tattoos or piercings. Consequent to Dimitrie’s arrival at the clinic he emerges
as very tense at times and his facial expressions change rapidly from fixated to
disorientated which depicts his poor poise.
BEHAVIOUR- It was clear Dimitrie was distraught and anxious as he became agitated
with the voices that were in his head as they were ‘criticising’ him. Dimitrie presents
reduced eye contact to the mental health nurse, though he is able to build rapport and is
slow to engage with the clinician; he is co-operative and showing signs of compliance
as he mostly answers the nurse’s questions, appropriately. Signs of psychomotor
agitation can be shown as the patient shows episodes temporary inattentiveness, and
responds to the voices he is hearing; as he says ‘sorry what was the question again’ or in
response to his writing ‘I will finish it, so shut up’ which also demonstrates his negative
attitude and outlook. Dimitrie is unable to focus either looking into space or distracted
by saying ‘just leave me alone’ to the voices he hears.
AFFECT- Dimitrie produces some emotional responsiveness, suggested from his
anxious facial expressions; Dimitrie has also shown an impediment in terminating an
emotional response when triggered by voices, or discussing a sensitive topic; which
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
portrays a labile affect, when switching from listening to the nurse and the voices. When
asked questions from the nurse, the patient acts accordingly and appropriately; when not
restricted by the voices. This particular patient was showing signs of delusional thinking
as he was frightened by the experiences and mentioned ‘they do stuff to me which isn’t
pleasant’.
Inappropriate affect was shown when Dimitrie’s affect was incongruent with what he
was saying; for example when asked his job efforts he responded with ‘not really’ then
‘I’m a writer’ and ‘I will finish it, so shut up’, which lead to a flattened affect when
discussing impulses.
MOOD- The patient said he was ‘not entirely comfortable, because I am hearing voices’
and described the experience as ‘scary’. Dimitrie’s mood changes throughout the
meeting and seems to be fearful and worried, as a result of the voices. Overall emotional
tone was observed in the interview; there was spontaneous intense reactivity, by
Dimitrie from being distressed and when describing upsetting occurrences, he said ‘they
are very critical’ and ‘this is scary sometimes’ in reference to the voices.
SPEECH- Dimitrie speaks in a calm monotonous voice mostly to the nurse, unless he
starts hearing voices in his head; which shows him raising his voice ‘just leave me
alone’ to the voices. Dimitrie has a paucity of content in his speech, as his distracted by
the voices he is hearing, when talking to the nurse he has a clear normal prosody, and
lilt. The rate of speech was coerced with an inclination to emphasis on the deleterious
circumstances surrounding the voices.
THOUGHT FORM- Dimitrie is showing a poverty of ideas as is very vague when
asked about his writing; he also is exhibiting slow and hesitant thinking, and has goal
asked questions from the nurse, the patient acts accordingly and appropriately; when not
restricted by the voices. This particular patient was showing signs of delusional thinking
as he was frightened by the experiences and mentioned ‘they do stuff to me which isn’t
pleasant’.
Inappropriate affect was shown when Dimitrie’s affect was incongruent with what he
was saying; for example when asked his job efforts he responded with ‘not really’ then
‘I’m a writer’ and ‘I will finish it, so shut up’, which lead to a flattened affect when
discussing impulses.
MOOD- The patient said he was ‘not entirely comfortable, because I am hearing voices’
and described the experience as ‘scary’. Dimitrie’s mood changes throughout the
meeting and seems to be fearful and worried, as a result of the voices. Overall emotional
tone was observed in the interview; there was spontaneous intense reactivity, by
Dimitrie from being distressed and when describing upsetting occurrences, he said ‘they
are very critical’ and ‘this is scary sometimes’ in reference to the voices.
SPEECH- Dimitrie speaks in a calm monotonous voice mostly to the nurse, unless he
starts hearing voices in his head; which shows him raising his voice ‘just leave me
alone’ to the voices. Dimitrie has a paucity of content in his speech, as his distracted by
the voices he is hearing, when talking to the nurse he has a clear normal prosody, and
lilt. The rate of speech was coerced with an inclination to emphasis on the deleterious
circumstances surrounding the voices.
THOUGHT FORM- Dimitrie is showing a poverty of ideas as is very vague when
asked about his writing; he also is exhibiting slow and hesitant thinking, and has goal
directed thinking which is tangential ‘I’m still getting back to writing’ representing
loose associations. Dimitrie also encounters disruptions of the train of thought before an
idea has been finished; he also indicates a failure to recollect what was being said or
anticipated to be said. ‘Sorry, what was the question? ’ demonstrates his inarticulate and
unfathomable connections of thoughts resulting in a word salad, at times.
THOUGHT CONTENT- The patient is experiencing persecutory delusions as he is
hearing the voices ‘I haven’t had my medication in a while, so I’m hearing voices’, and
is specifying signs he is being harassed and in fear. He believes he ‘was fine till until the
last month’ of his holiday, for which he ran out of medications on his trip to Japan.
Dimitrie also said ‘I have friends, I guess I don’t see them much’, ‘on Facebook and
stuff’ which demonstrates he has anti-social urges.
PERCEPTION- During the interview Dimitrie appears to be suffering from auditory
phenomena without an authentic stimulus. This can be demonstrated when he gets side-
tracked and declares ‘I’m not crazy’, in response to the nurse asking about being
monitored in hospital; which is exhibiting the misinterpretations as wells as the feelings
of depersonalisation and derealisation by Dimitrie.
COGNITION & INTELLECTUAL FUNCTIONING- Dimitrie is aware of where he is
and his friend Cheryl who brought him to the clinic, although he does not have an
immediate recall of the date; which takes him some time to work out as he starts out by
stating ‘Ahh, its December’ and eventually remembers the medication he should be
taking, so he is somewhat orientated. When questioned about a mathematical
calculation he initially took some time and after two attempts he stated the voices are
‘telling me my math sucks’. The patient does not establish a clear ability to plan or
implement as he does not socialise, telling the nurse he usually goes to the ‘movies by
loose associations. Dimitrie also encounters disruptions of the train of thought before an
idea has been finished; he also indicates a failure to recollect what was being said or
anticipated to be said. ‘Sorry, what was the question? ’ demonstrates his inarticulate and
unfathomable connections of thoughts resulting in a word salad, at times.
THOUGHT CONTENT- The patient is experiencing persecutory delusions as he is
hearing the voices ‘I haven’t had my medication in a while, so I’m hearing voices’, and
is specifying signs he is being harassed and in fear. He believes he ‘was fine till until the
last month’ of his holiday, for which he ran out of medications on his trip to Japan.
Dimitrie also said ‘I have friends, I guess I don’t see them much’, ‘on Facebook and
stuff’ which demonstrates he has anti-social urges.
PERCEPTION- During the interview Dimitrie appears to be suffering from auditory
phenomena without an authentic stimulus. This can be demonstrated when he gets side-
tracked and declares ‘I’m not crazy’, in response to the nurse asking about being
monitored in hospital; which is exhibiting the misinterpretations as wells as the feelings
of depersonalisation and derealisation by Dimitrie.
COGNITION & INTELLECTUAL FUNCTIONING- Dimitrie is aware of where he is
and his friend Cheryl who brought him to the clinic, although he does not have an
immediate recall of the date; which takes him some time to work out as he starts out by
stating ‘Ahh, its December’ and eventually remembers the medication he should be
taking, so he is somewhat orientated. When questioned about a mathematical
calculation he initially took some time and after two attempts he stated the voices are
‘telling me my math sucks’. The patient does not establish a clear ability to plan or
implement as he does not socialise, telling the nurse he usually goes to the ‘movies by
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
myself’ or sees his mum ‘once every two weeks’. During Dimitrie’s interview a number
of sentences allude to disturbed thought content such as ‘I have friends, okay !!’.
Dimitrie’s thought content, illustrate frightening conditions that are beyond his control.
INSIGHT & JUDGEMENT- Acknowledgment and awareness is ultimately acquired,
that support is necessary, and finally an agreement with proposed help of the treating
doctor. Dimitrie is aware of the consequences, when not taking medication as he said
the voices wake him up sometimes with the nurse saying, ‘obviously you are unwell as
a result of not taking medication’.
Risks-
The patient is at risk of sleep deprivation or disturbances, as he said medication and
would help him but ‘they wake me up’ in reference to the voices. Dimitrie would also at
risk of financial difficulty as he mentioned ‘I’m still getting back’ to writing, and
specified he had no job when prompted by the clinician. The patient would be exposed
to a risk of malnutrition as he does not socialise, making it hard for him to go out to
purchase groceries; he also‘ran out of medication’ when questioned about this response
he said ‘I didn’t know how to’ which means he could also exhaust his food supplies,
and in sees his family twice in a month. Dimitrie could be a potential harm to others as
he thinks if the situation arose, he would need to defend himself; with the voices, his
behaviour could be unpredictable with the nature of his ideations.
of sentences allude to disturbed thought content such as ‘I have friends, okay !!’.
Dimitrie’s thought content, illustrate frightening conditions that are beyond his control.
INSIGHT & JUDGEMENT- Acknowledgment and awareness is ultimately acquired,
that support is necessary, and finally an agreement with proposed help of the treating
doctor. Dimitrie is aware of the consequences, when not taking medication as he said
the voices wake him up sometimes with the nurse saying, ‘obviously you are unwell as
a result of not taking medication’.
Risks-
The patient is at risk of sleep deprivation or disturbances, as he said medication and
would help him but ‘they wake me up’ in reference to the voices. Dimitrie would also at
risk of financial difficulty as he mentioned ‘I’m still getting back’ to writing, and
specified he had no job when prompted by the clinician. The patient would be exposed
to a risk of malnutrition as he does not socialise, making it hard for him to go out to
purchase groceries; he also‘ran out of medication’ when questioned about this response
he said ‘I didn’t know how to’ which means he could also exhaust his food supplies,
and in sees his family twice in a month. Dimitrie could be a potential harm to others as
he thinks if the situation arose, he would need to defend himself; with the voices, his
behaviour could be unpredictable with the nature of his ideations.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2. Care Plan
CLINICAL ISSUE: Delusional Thinking
RATIONALE FOR CHOSEN ISSUE: The predetermined attitudes that are not
amenable to change, in light of contradictory substantiation, are described as delusions
which are shown throughout Dimitrie’s case (Bortolotti, 2018). Current literature
suggests beliefs negatively influenced patients’ well-being and the condition of life
(Asensio-Aguerri et al., 2019). Delusional thinking is the highest priority as it has arisen
from clinical judgement, in the interview; the patient states he finds the voices ‘scary’
and they wake him up. Delusional thinking can cause compelling instinctive feelings
and pessimistic representations of disappointment, despair, and vulnerability, evidently
correlated to the patients’ mood disorders, thus nursing interventions are required for
this predicament (Chaudhury & Kiran, 2019).
GOAL/S : To reduce delusional thinking in order to improve the outcomes of the
patient which are more beneficial and positive, through upkeep and promotion of
reality-based thoughts. To ensure Dimitrie contributes to the actual environment and
genuine conversations. To confirm the patient does not continue to hear voices through
the appropriate nursing interventions.
INTERVENTIONS
1. Distribute and manage
antipsychotic medications as
prescribed by treating doctor e.g.,
olanzapine on a regular basis to
RATIONALES
1. Dispensing medications of an antipsychotic
kind and ensuring Dimitrie’s obedience
reduces psychotic symptoms such as voices
(González-Rodríguez, Guàrdia, Palao, Labad
CLINICAL ISSUE: Delusional Thinking
RATIONALE FOR CHOSEN ISSUE: The predetermined attitudes that are not
amenable to change, in light of contradictory substantiation, are described as delusions
which are shown throughout Dimitrie’s case (Bortolotti, 2018). Current literature
suggests beliefs negatively influenced patients’ well-being and the condition of life
(Asensio-Aguerri et al., 2019). Delusional thinking is the highest priority as it has arisen
from clinical judgement, in the interview; the patient states he finds the voices ‘scary’
and they wake him up. Delusional thinking can cause compelling instinctive feelings
and pessimistic representations of disappointment, despair, and vulnerability, evidently
correlated to the patients’ mood disorders, thus nursing interventions are required for
this predicament (Chaudhury & Kiran, 2019).
GOAL/S : To reduce delusional thinking in order to improve the outcomes of the
patient which are more beneficial and positive, through upkeep and promotion of
reality-based thoughts. To ensure Dimitrie contributes to the actual environment and
genuine conversations. To confirm the patient does not continue to hear voices through
the appropriate nursing interventions.
INTERVENTIONS
1. Distribute and manage
antipsychotic medications as
prescribed by treating doctor e.g.,
olanzapine on a regular basis to
RATIONALES
1. Dispensing medications of an antipsychotic
kind and ensuring Dimitrie’s obedience
reduces psychotic symptoms such as voices
(González-Rodríguez, Guàrdia, Palao, Labad
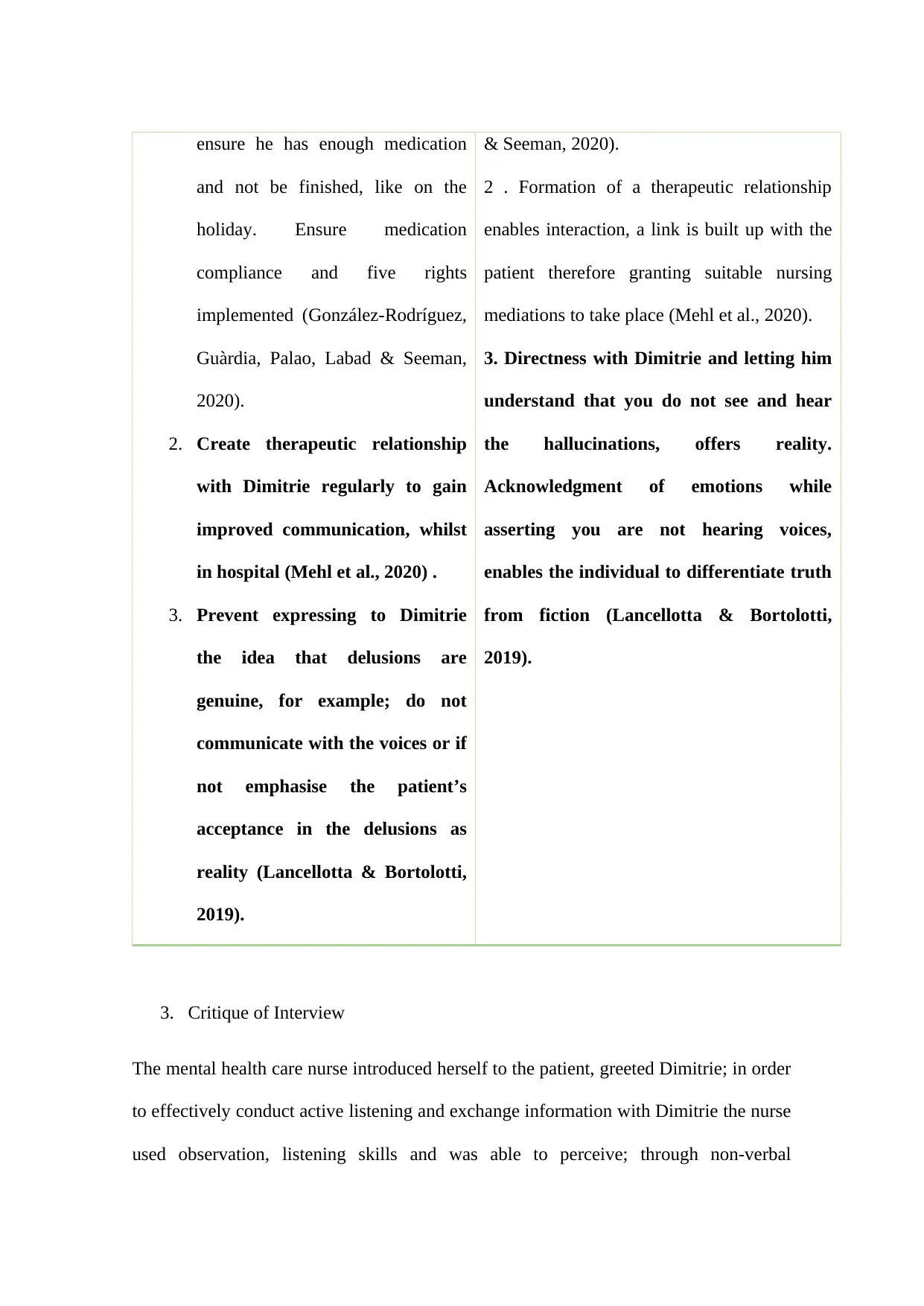
ensure he has enough medication
and not be finished, like on the
holiday. Ensure medication
compliance and five rights
implemented (González-Rodríguez,
Guàrdia, Palao, Labad & Seeman,
2020).
2. Create therapeutic relationship
with Dimitrie regularly to gain
improved communication, whilst
in hospital (Mehl et al., 2020) .
3. Prevent expressing to Dimitrie
the idea that delusions are
genuine, for example; do not
communicate with the voices or if
not emphasise the patient’s
acceptance in the delusions as
reality (Lancellotta & Bortolotti,
2019).
& Seeman, 2020).
2 . Formation of a therapeutic relationship
enables interaction, a link is built up with the
patient therefore granting suitable nursing
mediations to take place (Mehl et al., 2020).
3. Directness with Dimitrie and letting him
understand that you do not see and hear
the hallucinations, offers reality.
Acknowledgment of emotions while
asserting you are not hearing voices,
enables the individual to differentiate truth
from fiction (Lancellotta & Bortolotti,
2019).
3. Critique of Interview
The mental health care nurse introduced herself to the patient, greeted Dimitrie; in order
to effectively conduct active listening and exchange information with Dimitrie the nurse
used observation, listening skills and was able to perceive; through non-verbal
and not be finished, like on the
holiday. Ensure medication
compliance and five rights
implemented (González-Rodríguez,
Guàrdia, Palao, Labad & Seeman,
2020).
2. Create therapeutic relationship
with Dimitrie regularly to gain
improved communication, whilst
in hospital (Mehl et al., 2020) .
3. Prevent expressing to Dimitrie
the idea that delusions are
genuine, for example; do not
communicate with the voices or if
not emphasise the patient’s
acceptance in the delusions as
reality (Lancellotta & Bortolotti,
2019).
& Seeman, 2020).
2 . Formation of a therapeutic relationship
enables interaction, a link is built up with the
patient therefore granting suitable nursing
mediations to take place (Mehl et al., 2020).
3. Directness with Dimitrie and letting him
understand that you do not see and hear
the hallucinations, offers reality.
Acknowledgment of emotions while
asserting you are not hearing voices,
enables the individual to differentiate truth
from fiction (Lancellotta & Bortolotti,
2019).
3. Critique of Interview
The mental health care nurse introduced herself to the patient, greeted Dimitrie; in order
to effectively conduct active listening and exchange information with Dimitrie the nurse
used observation, listening skills and was able to perceive; through non-verbal
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
communication cues such as eye contact (when appropriate), good, open, relaxed body
posture, which Dimitrie to express his feelings and emotional state and build a
therapeutic relationship (Stein-Parbury, 2017). Reassurance for instance, soft
murmuring ‘Mmm’ and nodding was demonstrated to illustrate attention and sincerity,
letting Dimitrie feel understood and feelings of value and recognition (Stein-Parbury,
2017).
Although there were numerous methods of positive interactions exhibited, there can be
barriers with Dimitrie had which affected the interaction negatively. In this particular
case the patient was unable to listening attentively and the delusions also affected the
congruent conversation which distorted the responses (Stein-Parbury, 2017).
To establish effective fundamental relationships, the use of listening skills for the
development of a comprehensive understanding of Dimitrie’s situation the nurse
responded according to meet his needs such as ‘What are they saying to you?’ which is
an example of an open-ended question (Stein-Parbury, 2017).
The negative interactions include an absence of empathy and deprived information
provision, as Dimitrie was reluctant to stay in hospital. Absenteeism of guidance about
additional support was portrayed, when Dimitrie was questioned about staying in
hospital; which led to him feeling distressed, and isolated thus it is important that nurses
are more approachable and accessible (Gilbert, Ussher, Perz, Hobbs & Kirsten, 2018).
posture, which Dimitrie to express his feelings and emotional state and build a
therapeutic relationship (Stein-Parbury, 2017). Reassurance for instance, soft
murmuring ‘Mmm’ and nodding was demonstrated to illustrate attention and sincerity,
letting Dimitrie feel understood and feelings of value and recognition (Stein-Parbury,
2017).
Although there were numerous methods of positive interactions exhibited, there can be
barriers with Dimitrie had which affected the interaction negatively. In this particular
case the patient was unable to listening attentively and the delusions also affected the
congruent conversation which distorted the responses (Stein-Parbury, 2017).
To establish effective fundamental relationships, the use of listening skills for the
development of a comprehensive understanding of Dimitrie’s situation the nurse
responded according to meet his needs such as ‘What are they saying to you?’ which is
an example of an open-ended question (Stein-Parbury, 2017).
The negative interactions include an absence of empathy and deprived information
provision, as Dimitrie was reluctant to stay in hospital. Absenteeism of guidance about
additional support was portrayed, when Dimitrie was questioned about staying in
hospital; which led to him feeling distressed, and isolated thus it is important that nurses
are more approachable and accessible (Gilbert, Ussher, Perz, Hobbs & Kirsten, 2018).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Reference List
Asensio-Aguerri, L., Beato-Fernández, L., Stavraki, M., Rodríguez-Cano, T., Bajo, M.,
& Díaz, D. (2019). Paranoid Thinking and Wellbeing. The Role of Doubt in
Pharmacological and Metacognitive Therapies. Frontiers In Psychology, 10.
doi: 10.3389/fpsyg.2019.02099
Bortolotti, L. (2018). Delusions in Context (1st ed. 2018. ed.).
Chaudhury, S., & Kiran, C. (2019). Understanding delusions. Industrial Psychiatry
Journal, 18(1), 3. doi: 10.4103/0972-6748.57851
Gilbert, E., Ussher, J., Perz, J., Hobbs, K., & Kirsten, L. (2018). Positive and Negative
Interactions With Health Professionals. Cancer Nursing, 33(6), E1-E9. doi:
10.1097/ncc.0b013e3181da365d
González-Rodríguez, A., Guàrdia, A., Palao, D., Labad, J., & Seeman, M. (2020).
Moderators and mediators of antipsychotic response in delusional disorder:
Further steps are needed. World Journal Of Psychiatry, 10(4), 34-45. doi:
10.5498/wjp.v10.i4.34
Lancellotta, E., & Bortolotti, L. (2019). Are clinical delusions adaptive?. Wiley
Interdisciplinary Reviews: Cognitive Science, e1502. doi: 10.1002/wcs.1502
Asensio-Aguerri, L., Beato-Fernández, L., Stavraki, M., Rodríguez-Cano, T., Bajo, M.,
& Díaz, D. (2019). Paranoid Thinking and Wellbeing. The Role of Doubt in
Pharmacological and Metacognitive Therapies. Frontiers In Psychology, 10.
doi: 10.3389/fpsyg.2019.02099
Bortolotti, L. (2018). Delusions in Context (1st ed. 2018. ed.).
Chaudhury, S., & Kiran, C. (2019). Understanding delusions. Industrial Psychiatry
Journal, 18(1), 3. doi: 10.4103/0972-6748.57851
Gilbert, E., Ussher, J., Perz, J., Hobbs, K., & Kirsten, L. (2018). Positive and Negative
Interactions With Health Professionals. Cancer Nursing, 33(6), E1-E9. doi:
10.1097/ncc.0b013e3181da365d
González-Rodríguez, A., Guàrdia, A., Palao, D., Labad, J., & Seeman, M. (2020).
Moderators and mediators of antipsychotic response in delusional disorder:
Further steps are needed. World Journal Of Psychiatry, 10(4), 34-45. doi:
10.5498/wjp.v10.i4.34
Lancellotta, E., & Bortolotti, L. (2019). Are clinical delusions adaptive?. Wiley
Interdisciplinary Reviews: Cognitive Science, e1502. doi: 10.1002/wcs.1502
Mehl, S., Hesse, K., Schmidt, A., Landsberg, M., Soll, D., & Bechdolf, A. et al. (2020).
Theory of mind, emotion recognition, delusions and the quality of the
therapeutic relationship in patients with psychosis – a secondary analysis of a
randomized-controlled therapy trial. BMC Psychiatry, 20(1). doi:
10.1186/s12888-020-2482-z
Stein-Parbury, J. (2017).Patient and person. 6th ed. Sydney: Elsevier Churchill
Livingstone.
Theory of mind, emotion recognition, delusions and the quality of the
therapeutic relationship in patients with psychosis – a secondary analysis of a
randomized-controlled therapy trial. BMC Psychiatry, 20(1). doi:
10.1186/s12888-020-2482-z
Stein-Parbury, J. (2017).Patient and person. 6th ed. Sydney: Elsevier Churchill
Livingstone.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





