Oral vs. LAI Antipsychotics: Metabolic Syndrome in Psychotic Disorders
VerifiedAdded on 2023/06/30
|6
|5737
|364
Report
AI Summary
This research report investigates the prevalence and risk factors of metabolic syndrome (MetS) in patients with chronic psychotic disorders, specifically schizophrenia (Sz) and schizoaffective disorder (SzAff), treated with oral and long-acting injectable (LAI) antipsychotics. The study, involving 151 patients, compares the metabolic health indices between Sz and SzAff patients and assesses the impact of different antipsychotic treatments on MetS. The findings indicate that SzAff diagnosis and higher antipsychotic doses are associated with increased MetS risk, while the mode of administration (oral vs. LAI) does not significantly influence MetS risk. The study identifies specific antipsychotics with higher MetS risk, such as quetiapine and clozapine, and highlights the importance of monitoring metabolic health in patients with severe mental illnesses. The research contributes to understanding the complex relationship between psychotic disorders, antipsychotic treatments, and metabolic complications.
ORIGINAL RESEARCH
published: 16 January 2019
doi: 10.3389/fpsyt.2018.00744
Frontiers in Psychiatry | www.frontiersin.org 1 January 2019 | Volume 9 | Article 744
Edited by:
Andrea Fiorillo,
Università degliStudidella Campania
“LuigiVanvitelli” Naples, Italy
Reviewed by:
Francesco Bartoli,
Università deglistudidi Milano
Bicocca, Italy
Steve Simpson Jr,
The University of Melbourne, Australia
Beth McGinty,
Johns Hopkins University,
United States
*Correspondence:
Antonio Ventriglio
a.ventriglio@libero.it
Specialty section:
This article was submitted to
Psychosomatic Medicine,
a section of the journal
Frontiers in Psychiatry
Received: 22 August 2018
Accepted: 17 December 2018
Published: 16 January 2019
Citation:
Ventriglio A, BaldessariniRJ, VitraniG,
Bonfitto I, Cecere AC, RinaldiA,
Petito A and Bellomo A (2019)
Metabolic Syndrome in Psychotic
Disorder Patients Treated With Oral
and Long-Acting Injected
Antipsychotics.
Front. Psychiatry 9:744.
doi: 10.3389/fpsyt.2018.00744
Metabolic Syndrome in Psychotic
Disorder Patients Treated With Oral
and Long-Acting Injected
Antipsychotics
Antonio Ventriglio1
*, Ross J. Baldessarini2,3, Giovanna Vitrani1, Iris Bonfitto1,
Angela Chiara Cecere1, Angelo Rinaldi1, Annamaria Petito1 and Antonello Bellomo1
1 Department of Clinicaland ExperimentalMedicine, University of Foggia, Foggia, Italy,2 InternationalConsortium for
Psychotic & Mood Disorder Research, McLean Hospital, Belmont, MA, United States,3 Department of Psychiatry, Harvard
MedicalSchool, McLean Hospital, Boston, MA, United States
Background: Severe mentalillnesses are associated with increased risks for metabolic
syndrome (MetS)and other medicaldisorders, often with unfavorable outcomes. MetS
may be more likely with schizoaffective disorder (SzAff)than schizophrenia (Sz).MetS
is associated with long-term antipsychotic drug treatment,but relative risk with orally
administered vs. long-acting injected (LAI) antipsychotics is uncertain.
Methods: Subjects (n = 151 with a DSM-IV-TR chronic psychotic disorder: 89 Sz, 62
SzAff),treated with oralor LAI antipsychotics were compared for risk ofMetS,initially
with bivariate comparisons and then by multivariate regression modeling.
Results: Aside from measures on which diagnosis of MetS is based, factors prelimina
associated with MetS included antipsychotic drug dose,“high-risk”antipsychotics
associated with weight-gain, older age and female sex. Defining factors associated w
diagnosis ofMetS ranked in multivariate regression as:higherfasting glucose,lower
LDL cholesterol,higherdiastolic blood pressure,and higherBMI. Risk of MetS with
antipsychotics ranked: quetiapine ≥ clozapine ≥ paliperidone ≥ olanzapine ≥ risper
≥ haloperidol≥ aripiprazole.Otherassociated risk factors in multivariate modeling
ranked: higher antipsychotic dose, older age, and SzAff diagnosis, but not oralvs. LAI
antipsychotics
Conclusions: SzAffdiagnosis and higher antipsychotic doses were associated with
MetS, whereas orally vs. injected antipsychotics did not differ in risk of MetS.
Keywords: metabolic syndrome, antipsychotics, long-acting injected, schizoaffective, schizophrenia
INTRODUCTION
Personswith severe mentalillnesseshave increased risk formetabolic disorders,including
metabolic syndrome (MetS), characterized by obesity, type 2 diabetes mellitus, dyslipide
hypertension (1). Such disorders appear to be related to an unhealthy diet, lack of regul
adverse effects of psychotropic drugs,and possibly to undefined risk factors associated with the
illnesses themselves (2,3).Much of the research on this topic has involved patients diagnose
with chronic psychotic or mood disorders,particularly schizophrenia (Sz) and bipolar disorder
published: 16 January 2019
doi: 10.3389/fpsyt.2018.00744
Frontiers in Psychiatry | www.frontiersin.org 1 January 2019 | Volume 9 | Article 744
Edited by:
Andrea Fiorillo,
Università degliStudidella Campania
“LuigiVanvitelli” Naples, Italy
Reviewed by:
Francesco Bartoli,
Università deglistudidi Milano
Bicocca, Italy
Steve Simpson Jr,
The University of Melbourne, Australia
Beth McGinty,
Johns Hopkins University,
United States
*Correspondence:
Antonio Ventriglio
a.ventriglio@libero.it
Specialty section:
This article was submitted to
Psychosomatic Medicine,
a section of the journal
Frontiers in Psychiatry
Received: 22 August 2018
Accepted: 17 December 2018
Published: 16 January 2019
Citation:
Ventriglio A, BaldessariniRJ, VitraniG,
Bonfitto I, Cecere AC, RinaldiA,
Petito A and Bellomo A (2019)
Metabolic Syndrome in Psychotic
Disorder Patients Treated With Oral
and Long-Acting Injected
Antipsychotics.
Front. Psychiatry 9:744.
doi: 10.3389/fpsyt.2018.00744
Metabolic Syndrome in Psychotic
Disorder Patients Treated With Oral
and Long-Acting Injected
Antipsychotics
Antonio Ventriglio1
*, Ross J. Baldessarini2,3, Giovanna Vitrani1, Iris Bonfitto1,
Angela Chiara Cecere1, Angelo Rinaldi1, Annamaria Petito1 and Antonello Bellomo1
1 Department of Clinicaland ExperimentalMedicine, University of Foggia, Foggia, Italy,2 InternationalConsortium for
Psychotic & Mood Disorder Research, McLean Hospital, Belmont, MA, United States,3 Department of Psychiatry, Harvard
MedicalSchool, McLean Hospital, Boston, MA, United States
Background: Severe mentalillnesses are associated with increased risks for metabolic
syndrome (MetS)and other medicaldisorders, often with unfavorable outcomes. MetS
may be more likely with schizoaffective disorder (SzAff)than schizophrenia (Sz).MetS
is associated with long-term antipsychotic drug treatment,but relative risk with orally
administered vs. long-acting injected (LAI) antipsychotics is uncertain.
Methods: Subjects (n = 151 with a DSM-IV-TR chronic psychotic disorder: 89 Sz, 62
SzAff),treated with oralor LAI antipsychotics were compared for risk ofMetS,initially
with bivariate comparisons and then by multivariate regression modeling.
Results: Aside from measures on which diagnosis of MetS is based, factors prelimina
associated with MetS included antipsychotic drug dose,“high-risk”antipsychotics
associated with weight-gain, older age and female sex. Defining factors associated w
diagnosis ofMetS ranked in multivariate regression as:higherfasting glucose,lower
LDL cholesterol,higherdiastolic blood pressure,and higherBMI. Risk of MetS with
antipsychotics ranked: quetiapine ≥ clozapine ≥ paliperidone ≥ olanzapine ≥ risper
≥ haloperidol≥ aripiprazole.Otherassociated risk factors in multivariate modeling
ranked: higher antipsychotic dose, older age, and SzAff diagnosis, but not oralvs. LAI
antipsychotics
Conclusions: SzAffdiagnosis and higher antipsychotic doses were associated with
MetS, whereas orally vs. injected antipsychotics did not differ in risk of MetS.
Keywords: metabolic syndrome, antipsychotics, long-acting injected, schizoaffective, schizophrenia
INTRODUCTION
Personswith severe mentalillnesseshave increased risk formetabolic disorders,including
metabolic syndrome (MetS), characterized by obesity, type 2 diabetes mellitus, dyslipide
hypertension (1). Such disorders appear to be related to an unhealthy diet, lack of regul
adverse effects of psychotropic drugs,and possibly to undefined risk factors associated with the
illnesses themselves (2,3).Much of the research on this topic has involved patients diagnose
with chronic psychotic or mood disorders,particularly schizophrenia (Sz) and bipolar disorder
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Ventriglio et al. Metabolic Problems: Effects of Diagnosis and Treatment
(2,4–6).Few studies have compared physical health of subjects
diagnosed with schizoaffective disorder (SzAff) to that of other
patients with other psychotic-disorder diagnoses,including Sz,
but SzAff patientsmay havea greaterrisk of MetS than
those with other major psychiatric disorders (6).SzAff patients
are characterized by emotionaland behavioralinstability over
time as well as psychoticfeatures,and often are treated
with relatively complex pharmacologicalregimens(7). Both
emotional instability and complex treatments may contribute to
an increased risk of metabolic disorders (1).
Also uncertain is whether specific types of medicines differ
appreciably in their associations with risks of metabolic disorders.
In particular,the extentto which relative metabolic risksof
modern or second-generation antipsychotics (SGAs) and their
long-acting injected (LAI) preparations differ from older or orally
administered antipsychotics remains uncertain (1, 8–10).
The preceding considerationsled us to compareclinical
measures, in particular indices of metabolic health, among SzAff
vs.Sz patient-subjects to identify factors associated specifically
with MetS, including comparison of orally administered vs. LAI
antipsychotics. We hypothesized that SzAff subjects would have
a higher risk of MetS than Sz subjects, and that the risk might be
lower with LAI antipsychotic treatments.
METHODS
From June 2014 to February 2017, we enrolled study subjects as
part of a program monitoring the health of psychotic disorder
patients attending the Day HospitalService for Severe Mental
Disorders in the Psychiatric Departmentat the University of
Foggia Medical Center. A total of 151 consecutive patients were
enrolled as study-subjects,including 89 diagnosed with Sz and
62 as SzAff by two expert clinicians (AB,AV) based on DSM-
IV-TR (Diagnostic and StatisticalManualof mentaldisorders-
Text Revision) criteria (11).Treatments were selected clinically
and included oralantipsychotics(n = 64, with or without
mood-stabilizers or antidepressants) as well as LAI antipsychotics
(n = 87, usually as monotherapy).
All subjects provided written informed consent to participate,
after study procedures approved by the University ofFoggia
medical center ethics committee were explained to them. Patients
were enrolled in a stable phase of their illness and treatments;
candidates who required psychiatric hospitalization, had revised
treatment protocols within the previous 6 months, were actively
abusing alcoholor drugs (confirmed by urine assays),or were
pregnant, were excluded from the study.
Currentpsychiatric morbidity was assessed and rated with
the Positive and Negative Syndrome Scale (PANSS) (12),and
Brief Psychiatric Rating Scale (BPRS) (13) by two experienced
psychiatrist-investigators (AB, AV). Raters were held unaware of
treatments given,and their ratings yielded high,independent,
interrateragreement(χ2 ≥ 0.90).Being considered “mildly
ill” corresponded to a PANSS totalscoreof ≤58 or BPRS
score of ≤31,“moderately ill” corresponded to PANSS ratings
of 59–75 or BPRS scoresof 32–40,“moderately severely ill”
corresponded to PANSS of 76–95 or BPRS of 41–53, and “severely
ill” corresponded to a PANSS of96–116 or BPRS of54–126
(12, 13).
We also collecteddata on: demographics(sex, age,
employmentstatus), current pharmacologicaltreatments
(oral or LAI antipsychotics,mood stabilizers[MSs], and
antidepressants[ADs]),and theirdoses;anthropometric and
metabolic measures (height [cm] and weight [kg] for body-m
index [BMI]),systolic and diastolic blood pressure (mm Hg),
pulse (beats/min); serum concentrations of fasting glucose (F
mg/dL),%-glycated hemoglobin (Hgb-A1c),totalcholesterol
(mg/dL),low density lipoproteins (LDL;mg/dL),high density
lipoproteins(HDL; mg/dL), triglycerides(mg/dL); waist
circumference(cm), electrocardiographicrate-corrected QT
repolarization interval(QTc,msec);serum levels ofprolactin
(ng/dL),thyroid stimulating hormone (TSH,mIU/L),and free
thyroxin and triiodothyronine. We also recorded adverse even
associated with treatment,and rated treatment-adherence with
the 30-item Drug Attitude Inventory (DAI-30) (14).
We rated subjectsfor the presenceof MetS defined by
current, revised International Diabetes Federation (IDF) criter
American Heart Association and InternationalAssociation for
the Study of Obesity (15,16).MetS required meeting ≥3 of the
following 5 criteria:[a] large waist circumference (≥102 cm in
men, ≥88 cm in women); [b] elevated serum triglycerides (≥
ng/dL); [c] low HDL-cholesterol (<40 mg/dL in men and <50 i
women); high blood pressure (≥130 mm Hg systolic or ≥85 m
diastolic);elevated glucose as fasting blood sugar (FBS >100
mg/dL).
To facilitate comparisons,we converted antipsychotic doses
to approximate oral daily mg-chlorpromazine-equivalents (CP
eq); LAI antipsychotic doses were estimated as total mg dose
days of injection cycles for conversion to CPZ-eq (17,18).For
MSs, we converted dosages to approximate daily mg-equivale
of lithium carbonate (Li-eq) (18, 19). Antidepressants were no
as being prescribed or not.
We compared measures collected among subjects diagnos
with SzAff and Sz,treated with LAIand oralantipsychotics,
emphasizing comparisonsof subjectswith vs.withoutMetS.
Data analyses used commercialstatisticalprograms (Statview-
5, SAS Corp.,Cary,North Carolina,USA for spreadsheets;
Stata.13.0,Stata Corp.,College Station,Texas,USA). Data are
presented as means ± standard deviation (SD)or with 95%
confidence intervals (CI),or as percentages (%),unless stated
otherwise. Continuous data were compared using nonparame
Mann-Whitneyrank-sum test(z-score)to avoid problems
of non-normaldistribution ofvalues,and categoricaldata
weretested with contingencytables(χ2). Factorsyielding
p < 0.10 in preliminary bivariate comparisons were considere
multivariate logistic regression modeling, with presence of Me
as the outcome measure.
RESULTS
Sample Characteristics and Treatments
The 151 patient-subjects were aged 42.1 ± 12.4 years;52.9%
were men, 18.5% were employed. Diagnoses included Sz (n =
58.9%) and SzAff (n = 62; 41.1%). More men than women we
Frontiers in Psychiatry | www.frontiersin.org 2 January 2019 | Volume 9 | Article 744
(2,4–6).Few studies have compared physical health of subjects
diagnosed with schizoaffective disorder (SzAff) to that of other
patients with other psychotic-disorder diagnoses,including Sz,
but SzAff patientsmay havea greaterrisk of MetS than
those with other major psychiatric disorders (6).SzAff patients
are characterized by emotionaland behavioralinstability over
time as well as psychoticfeatures,and often are treated
with relatively complex pharmacologicalregimens(7). Both
emotional instability and complex treatments may contribute to
an increased risk of metabolic disorders (1).
Also uncertain is whether specific types of medicines differ
appreciably in their associations with risks of metabolic disorders.
In particular,the extentto which relative metabolic risksof
modern or second-generation antipsychotics (SGAs) and their
long-acting injected (LAI) preparations differ from older or orally
administered antipsychotics remains uncertain (1, 8–10).
The preceding considerationsled us to compareclinical
measures, in particular indices of metabolic health, among SzAff
vs.Sz patient-subjects to identify factors associated specifically
with MetS, including comparison of orally administered vs. LAI
antipsychotics. We hypothesized that SzAff subjects would have
a higher risk of MetS than Sz subjects, and that the risk might be
lower with LAI antipsychotic treatments.
METHODS
From June 2014 to February 2017, we enrolled study subjects as
part of a program monitoring the health of psychotic disorder
patients attending the Day HospitalService for Severe Mental
Disorders in the Psychiatric Departmentat the University of
Foggia Medical Center. A total of 151 consecutive patients were
enrolled as study-subjects,including 89 diagnosed with Sz and
62 as SzAff by two expert clinicians (AB,AV) based on DSM-
IV-TR (Diagnostic and StatisticalManualof mentaldisorders-
Text Revision) criteria (11).Treatments were selected clinically
and included oralantipsychotics(n = 64, with or without
mood-stabilizers or antidepressants) as well as LAI antipsychotics
(n = 87, usually as monotherapy).
All subjects provided written informed consent to participate,
after study procedures approved by the University ofFoggia
medical center ethics committee were explained to them. Patients
were enrolled in a stable phase of their illness and treatments;
candidates who required psychiatric hospitalization, had revised
treatment protocols within the previous 6 months, were actively
abusing alcoholor drugs (confirmed by urine assays),or were
pregnant, were excluded from the study.
Currentpsychiatric morbidity was assessed and rated with
the Positive and Negative Syndrome Scale (PANSS) (12),and
Brief Psychiatric Rating Scale (BPRS) (13) by two experienced
psychiatrist-investigators (AB, AV). Raters were held unaware of
treatments given,and their ratings yielded high,independent,
interrateragreement(χ2 ≥ 0.90).Being considered “mildly
ill” corresponded to a PANSS totalscoreof ≤58 or BPRS
score of ≤31,“moderately ill” corresponded to PANSS ratings
of 59–75 or BPRS scoresof 32–40,“moderately severely ill”
corresponded to PANSS of 76–95 or BPRS of 41–53, and “severely
ill” corresponded to a PANSS of96–116 or BPRS of54–126
(12, 13).
We also collecteddata on: demographics(sex, age,
employmentstatus), current pharmacologicaltreatments
(oral or LAI antipsychotics,mood stabilizers[MSs], and
antidepressants[ADs]),and theirdoses;anthropometric and
metabolic measures (height [cm] and weight [kg] for body-m
index [BMI]),systolic and diastolic blood pressure (mm Hg),
pulse (beats/min); serum concentrations of fasting glucose (F
mg/dL),%-glycated hemoglobin (Hgb-A1c),totalcholesterol
(mg/dL),low density lipoproteins (LDL;mg/dL),high density
lipoproteins(HDL; mg/dL), triglycerides(mg/dL); waist
circumference(cm), electrocardiographicrate-corrected QT
repolarization interval(QTc,msec);serum levels ofprolactin
(ng/dL),thyroid stimulating hormone (TSH,mIU/L),and free
thyroxin and triiodothyronine. We also recorded adverse even
associated with treatment,and rated treatment-adherence with
the 30-item Drug Attitude Inventory (DAI-30) (14).
We rated subjectsfor the presenceof MetS defined by
current, revised International Diabetes Federation (IDF) criter
American Heart Association and InternationalAssociation for
the Study of Obesity (15,16).MetS required meeting ≥3 of the
following 5 criteria:[a] large waist circumference (≥102 cm in
men, ≥88 cm in women); [b] elevated serum triglycerides (≥
ng/dL); [c] low HDL-cholesterol (<40 mg/dL in men and <50 i
women); high blood pressure (≥130 mm Hg systolic or ≥85 m
diastolic);elevated glucose as fasting blood sugar (FBS >100
mg/dL).
To facilitate comparisons,we converted antipsychotic doses
to approximate oral daily mg-chlorpromazine-equivalents (CP
eq); LAI antipsychotic doses were estimated as total mg dose
days of injection cycles for conversion to CPZ-eq (17,18).For
MSs, we converted dosages to approximate daily mg-equivale
of lithium carbonate (Li-eq) (18, 19). Antidepressants were no
as being prescribed or not.
We compared measures collected among subjects diagnos
with SzAff and Sz,treated with LAIand oralantipsychotics,
emphasizing comparisonsof subjectswith vs.withoutMetS.
Data analyses used commercialstatisticalprograms (Statview-
5, SAS Corp.,Cary,North Carolina,USA for spreadsheets;
Stata.13.0,Stata Corp.,College Station,Texas,USA). Data are
presented as means ± standard deviation (SD)or with 95%
confidence intervals (CI),or as percentages (%),unless stated
otherwise. Continuous data were compared using nonparame
Mann-Whitneyrank-sum test(z-score)to avoid problems
of non-normaldistribution ofvalues,and categoricaldata
weretested with contingencytables(χ2). Factorsyielding
p < 0.10 in preliminary bivariate comparisons were considere
multivariate logistic regression modeling, with presence of Me
as the outcome measure.
RESULTS
Sample Characteristics and Treatments
The 151 patient-subjects were aged 42.1 ± 12.4 years;52.9%
were men, 18.5% were employed. Diagnoses included Sz (n =
58.9%) and SzAff (n = 62; 41.1%). More men than women we
Frontiers in Psychiatry | www.frontiersin.org 2 January 2019 | Volume 9 | Article 744
Ventriglio et al. Metabolic Problems: Effects of Diagnosis and Treatment
diagnosed with Sz (χ2 = 6.76; p = 0.009). Treatments included
oralantipsychotics in 42.3%,and LAI antipsychotics in 57.7%
(none received both). Antipsychotics were combined with mood-
stabilizers (MSs) in only 14.5%,or with antidepressants (ADs)
in 12.3% (ranking by use: duloxetine > paroxetine > citalopram
or S-citalopram > sertraline).Both adjunctive treatments were
given selectively with oralantipsychotics,by 6.4- (MSs) or 7.0-
times more (ADs; both p ≤ 0.006) among SzAff than Sz subjects.
Antipsychotic doses averaged 313 ± 329 mg/day CPZ-eq,and
MS (carbamazepine,lithium carbonate,sodium valproate) total
daily Li-eq doses averaged 650 ± 244 mg. Overall, clinical ratings
averaged 75.0 ± 34.7 for PANSS and 51.6 ± 23.6 for BPRS; both
indicate moderate symptomatic severity, even though all patients
reported clinical and treatment stability for at least six continuous
preceding months. Prolonged, stable dosing assured that even the
LAI antipsychotics were at pharmacokinetic steady-state.
Subjectswho receivedLAI vs. oral antipsychoticshad
significantly lowerlevelsof symptomaticmorbidity.PANSS
scores were, respectively, 58.0 ± 27.6 vs. 98.1 ± 29.9, and BPRS
scores averaged 40.1 ± 15.0 vs. 67.1 ± 24.5 (z-scores = 7.76 and
6.85, both p < 0.0001).
No subject was considered to have a substance-use disorder,
as was supportedby urine drug assays,consistentwith
current substance abuse as an exclusion criterion. Adherence to
prescribed treatments was considered good,as supported by a
DAI-30 score of 9.64 ± 2.19 (of a total maximum of 30).There
was a moderate rate of reported,treatment-associated,adverse
events (19.8%),most of which involved motor slowing or mild
tremor.
Risk and Measures Associated With
Metabolic Syndrome
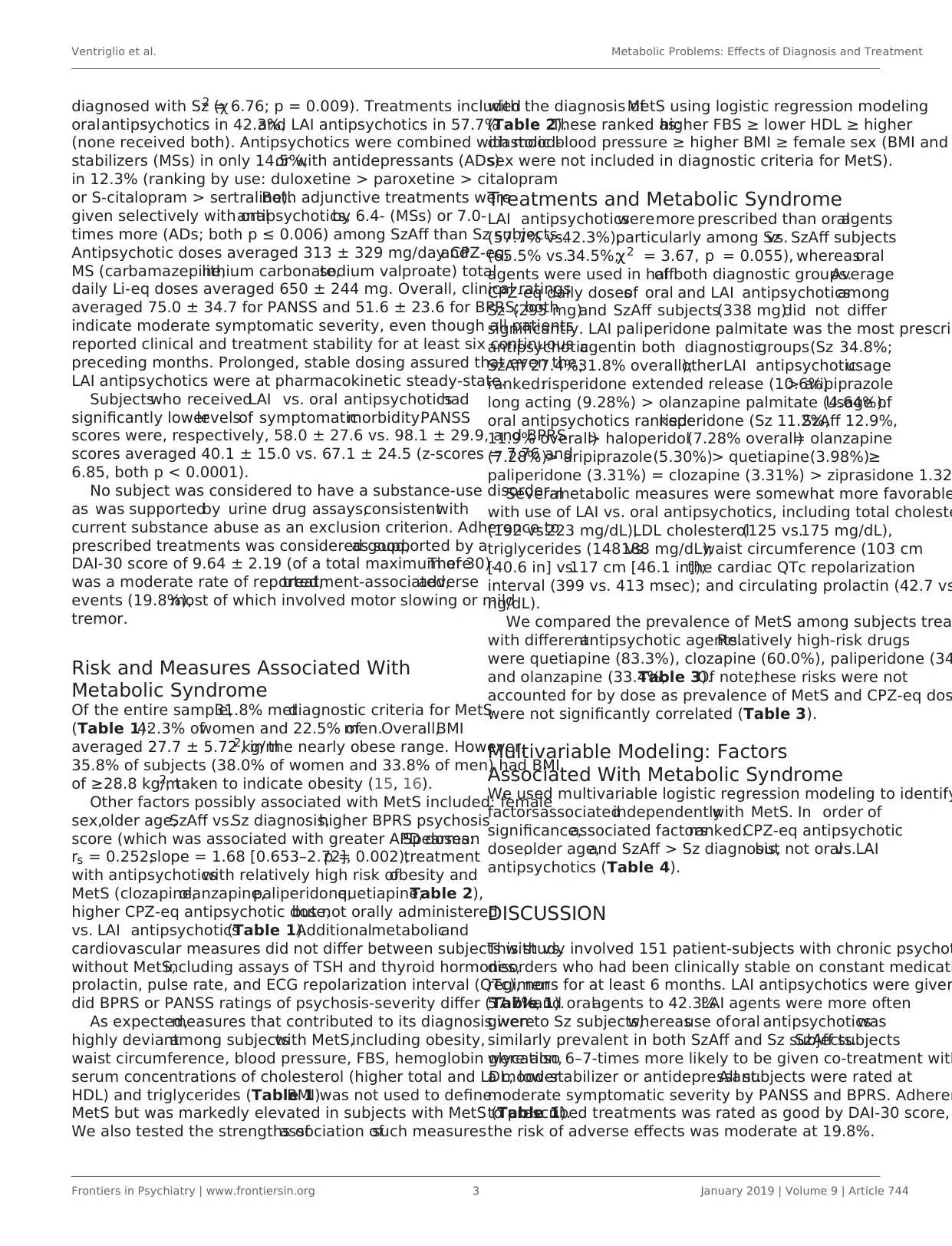
Of the entire sample,31.8% metdiagnostic criteria for MetS
(Table 1):42.3% ofwomen and 22.5% ofmen.Overall,BMI
averaged 27.7 ± 5.72 kg/m2, in the nearly obese range. However,
35.8% of subjects (38.0% of women and 33.8% of men) had BMI
of ≥28.8 kg/m2, taken to indicate obesity (15, 16).
Other factors possibly associated with MetS included: female
sex,older age,SzAff vs.Sz diagnosis,higher BPRS psychosis
score (which was associated with greater APD doses:Spearman
rs = 0.252,slope = 1.68 [0.653–2.72],p = 0.002),treatment
with antipsychoticswith relatively high risk ofobesity and
MetS (clozapine,olanzapine,paliperidone,quetiapine;Table 2),
higher CPZ-eq antipsychotic dose,but not orally administered
vs. LAI antipsychotics(Table 1).Additionalmetabolicand
cardiovascular measures did not differ between subjects with vs.
without MetS,including assays of TSH and thyroid hormones,
prolactin, pulse rate, and ECG repolarization interval (QTc), nor
did BPRS or PANSS ratings of psychosis-severity differ (Table 1).
As expected,measures that contributed to its diagnosis were
highly deviantamong subjectswith MetS,including obesity,
waist circumference, blood pressure, FBS, hemoglobin glycation,
serum concentrations of cholesterol (higher total and LDL, lower
HDL) and triglycerides (Table 1).BMI was not used to define
MetS but was markedly elevated in subjects with MetS (Table 1).
We also tested the strengths ofassociation ofsuch measures
with the diagnosis ofMetS using logistic regression modeling
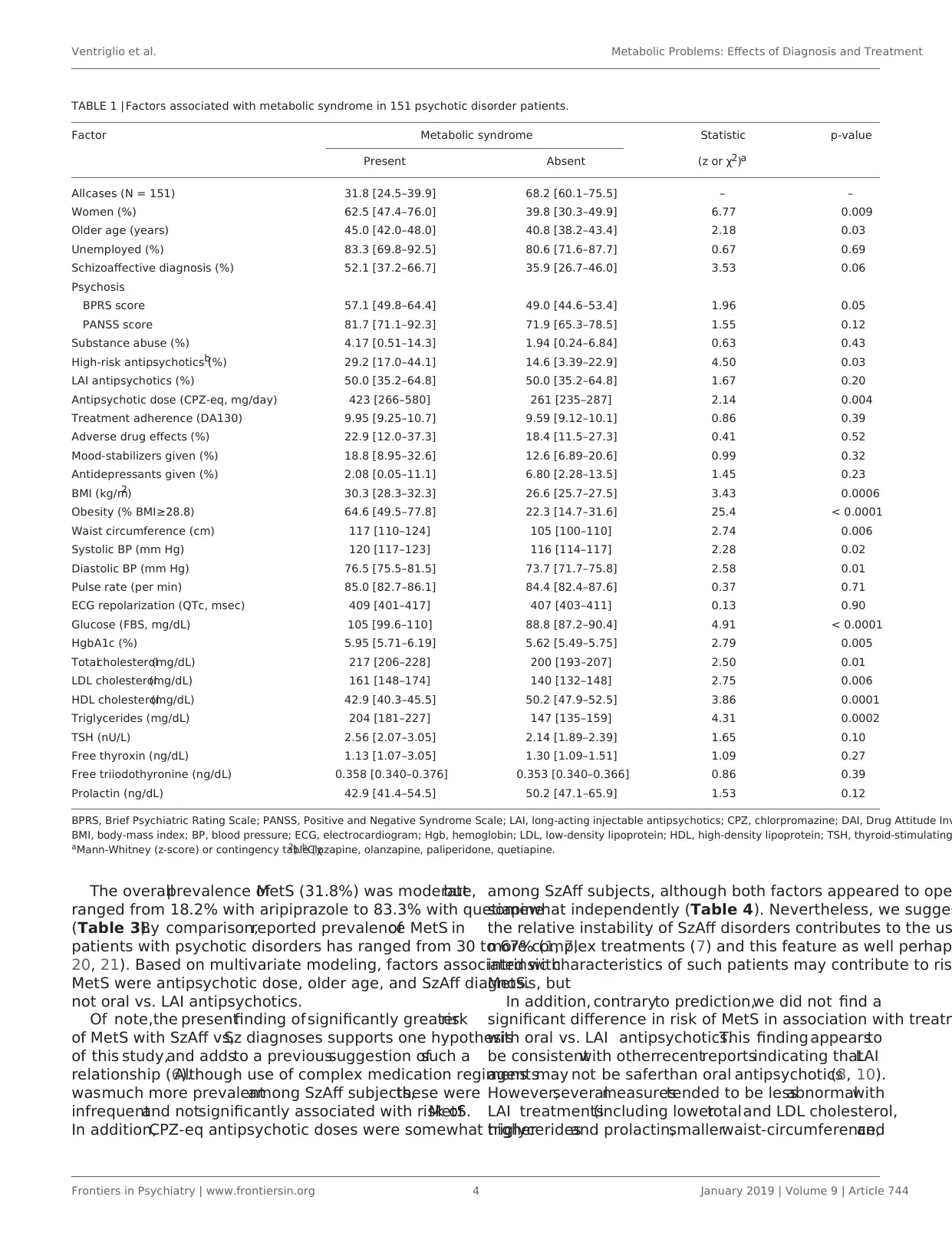
(Table 2).These ranked as:higher FBS ≥ lower HDL ≥ higher
diastolic blood pressure ≥ higher BMI ≥ female sex (BMI and
sex were not included in diagnostic criteria for MetS).
Treatments and Metabolic Syndrome
LAI antipsychoticsweremore prescribed than oralagents
(57.7% vs.42.3%),particularly among Szvs. SzAff subjects
(65.5% vs.34.5%;χ2 = 3.67, p = 0.055), whereasoral
agents were used in halfof both diagnostic groups.Average
CPZ-eq daily dosesof oral and LAI antipsychoticsamong
Sz (295 mg)and SzAff subjects(338 mg)did not differ
significantly. LAI paliperidone palmitate was the most prescrib
antipsychoticagentin both diagnosticgroups(Sz 34.8%;
SzAff 27.4%;31.8% overall);otherLAI antipsychoticusage
ranked:risperidone extended release (10.6%)> aripiprazole
long acting (9.28%) > olanzapine palmitate (4.64%).Usage of
oral antipsychotics ranked:risperidone (Sz 11.2%,SzAff 12.9%,
11.9% overall)> haloperidol(7.28% overall)= olanzapine
(7.28%)> aripiprazole(5.30%)> quetiapine(3.98%)≥
paliperidone (3.31%) = clozapine (3.31%) > ziprasidone 1.32
Severalmetabolic measures were somewhat more favorable
with use of LAI vs. oral antipsychotics, including total choleste
(192 vs.223 mg/dL),LDL cholesterol(125 vs.175 mg/dL),
triglycerides (148 vs.188 mg/dL);waist circumference (103 cm
[40.6 in] vs.117 cm [46.1 in]);the cardiac QTc repolarization
interval (399 vs. 413 msec); and circulating prolactin (42.7 vs
ng/dL).
We compared the prevalence of MetS among subjects trea
with differentantipsychotic agents.Relatively high-risk drugs
were quetiapine (83.3%), clozapine (60.0%), paliperidone (34
and olanzapine (33.4%;Table 3).Of note,these risks were not
accounted for by dose as prevalence of MetS and CPZ-eq dos
were not significantly correlated (Table 3).
Multivariable Modeling: Factors
Associated With Metabolic Syndrome
We used multivariable logistic regression modeling to identify
factorsassociatedindependentlywith MetS. In order of
significance,associated factorsranked:CPZ-eq antipsychotic
dose,older age,and SzAff > Sz diagnosis,but not oralvs.LAI
antipsychotics (Table 4).
DISCUSSION
This study involved 151 patient-subjects with chronic psychot
disorders who had been clinically stable on constant medicati
regimens for at least 6 months. LAI antipsychotics were given
57.7%,and oralagents to 42.3%.LAI agents were more often
given to Sz subjects,whereasuse oforal antipsychoticswas
similarly prevalent in both SzAff and Sz subjects.SzAff subjects
were also 6–7-times more likely to be given co-treatment with
a mood-stabilizer or antidepressant.All subjects were rated at
moderate symptomatic severity by PANSS and BPRS. Adheren
to prescribed treatments was rated as good by DAI-30 score,
the risk of adverse effects was moderate at 19.8%.
Frontiers in Psychiatry | www.frontiersin.org 3 January 2019 | Volume 9 | Article 744
diagnosed with Sz (χ2 = 6.76; p = 0.009). Treatments included
oralantipsychotics in 42.3%,and LAI antipsychotics in 57.7%
(none received both). Antipsychotics were combined with mood-
stabilizers (MSs) in only 14.5%,or with antidepressants (ADs)
in 12.3% (ranking by use: duloxetine > paroxetine > citalopram
or S-citalopram > sertraline).Both adjunctive treatments were
given selectively with oralantipsychotics,by 6.4- (MSs) or 7.0-
times more (ADs; both p ≤ 0.006) among SzAff than Sz subjects.
Antipsychotic doses averaged 313 ± 329 mg/day CPZ-eq,and
MS (carbamazepine,lithium carbonate,sodium valproate) total
daily Li-eq doses averaged 650 ± 244 mg. Overall, clinical ratings
averaged 75.0 ± 34.7 for PANSS and 51.6 ± 23.6 for BPRS; both
indicate moderate symptomatic severity, even though all patients
reported clinical and treatment stability for at least six continuous
preceding months. Prolonged, stable dosing assured that even the
LAI antipsychotics were at pharmacokinetic steady-state.
Subjectswho receivedLAI vs. oral antipsychoticshad
significantly lowerlevelsof symptomaticmorbidity.PANSS
scores were, respectively, 58.0 ± 27.6 vs. 98.1 ± 29.9, and BPRS
scores averaged 40.1 ± 15.0 vs. 67.1 ± 24.5 (z-scores = 7.76 and
6.85, both p < 0.0001).
No subject was considered to have a substance-use disorder,
as was supportedby urine drug assays,consistentwith
current substance abuse as an exclusion criterion. Adherence to
prescribed treatments was considered good,as supported by a
DAI-30 score of 9.64 ± 2.19 (of a total maximum of 30).There
was a moderate rate of reported,treatment-associated,adverse
events (19.8%),most of which involved motor slowing or mild
tremor.
Risk and Measures Associated With
Metabolic Syndrome
Of the entire sample,31.8% metdiagnostic criteria for MetS
(Table 1):42.3% ofwomen and 22.5% ofmen.Overall,BMI
averaged 27.7 ± 5.72 kg/m2, in the nearly obese range. However,
35.8% of subjects (38.0% of women and 33.8% of men) had BMI
of ≥28.8 kg/m2, taken to indicate obesity (15, 16).
Other factors possibly associated with MetS included: female
sex,older age,SzAff vs.Sz diagnosis,higher BPRS psychosis
score (which was associated with greater APD doses:Spearman
rs = 0.252,slope = 1.68 [0.653–2.72],p = 0.002),treatment
with antipsychoticswith relatively high risk ofobesity and
MetS (clozapine,olanzapine,paliperidone,quetiapine;Table 2),
higher CPZ-eq antipsychotic dose,but not orally administered
vs. LAI antipsychotics(Table 1).Additionalmetabolicand
cardiovascular measures did not differ between subjects with vs.
without MetS,including assays of TSH and thyroid hormones,
prolactin, pulse rate, and ECG repolarization interval (QTc), nor
did BPRS or PANSS ratings of psychosis-severity differ (Table 1).
As expected,measures that contributed to its diagnosis were
highly deviantamong subjectswith MetS,including obesity,
waist circumference, blood pressure, FBS, hemoglobin glycation,
serum concentrations of cholesterol (higher total and LDL, lower
HDL) and triglycerides (Table 1).BMI was not used to define
MetS but was markedly elevated in subjects with MetS (Table 1).
We also tested the strengths ofassociation ofsuch measures
with the diagnosis ofMetS using logistic regression modeling
(Table 2).These ranked as:higher FBS ≥ lower HDL ≥ higher
diastolic blood pressure ≥ higher BMI ≥ female sex (BMI and
sex were not included in diagnostic criteria for MetS).
Treatments and Metabolic Syndrome
LAI antipsychoticsweremore prescribed than oralagents
(57.7% vs.42.3%),particularly among Szvs. SzAff subjects
(65.5% vs.34.5%;χ2 = 3.67, p = 0.055), whereasoral
agents were used in halfof both diagnostic groups.Average
CPZ-eq daily dosesof oral and LAI antipsychoticsamong
Sz (295 mg)and SzAff subjects(338 mg)did not differ
significantly. LAI paliperidone palmitate was the most prescrib
antipsychoticagentin both diagnosticgroups(Sz 34.8%;
SzAff 27.4%;31.8% overall);otherLAI antipsychoticusage
ranked:risperidone extended release (10.6%)> aripiprazole
long acting (9.28%) > olanzapine palmitate (4.64%).Usage of
oral antipsychotics ranked:risperidone (Sz 11.2%,SzAff 12.9%,
11.9% overall)> haloperidol(7.28% overall)= olanzapine
(7.28%)> aripiprazole(5.30%)> quetiapine(3.98%)≥
paliperidone (3.31%) = clozapine (3.31%) > ziprasidone 1.32
Severalmetabolic measures were somewhat more favorable
with use of LAI vs. oral antipsychotics, including total choleste
(192 vs.223 mg/dL),LDL cholesterol(125 vs.175 mg/dL),
triglycerides (148 vs.188 mg/dL);waist circumference (103 cm
[40.6 in] vs.117 cm [46.1 in]);the cardiac QTc repolarization
interval (399 vs. 413 msec); and circulating prolactin (42.7 vs
ng/dL).
We compared the prevalence of MetS among subjects trea
with differentantipsychotic agents.Relatively high-risk drugs
were quetiapine (83.3%), clozapine (60.0%), paliperidone (34
and olanzapine (33.4%;Table 3).Of note,these risks were not
accounted for by dose as prevalence of MetS and CPZ-eq dos
were not significantly correlated (Table 3).
Multivariable Modeling: Factors
Associated With Metabolic Syndrome
We used multivariable logistic regression modeling to identify
factorsassociatedindependentlywith MetS. In order of
significance,associated factorsranked:CPZ-eq antipsychotic
dose,older age,and SzAff > Sz diagnosis,but not oralvs.LAI
antipsychotics (Table 4).
DISCUSSION
This study involved 151 patient-subjects with chronic psychot
disorders who had been clinically stable on constant medicati
regimens for at least 6 months. LAI antipsychotics were given
57.7%,and oralagents to 42.3%.LAI agents were more often
given to Sz subjects,whereasuse oforal antipsychoticswas
similarly prevalent in both SzAff and Sz subjects.SzAff subjects
were also 6–7-times more likely to be given co-treatment with
a mood-stabilizer or antidepressant.All subjects were rated at
moderate symptomatic severity by PANSS and BPRS. Adheren
to prescribed treatments was rated as good by DAI-30 score,
the risk of adverse effects was moderate at 19.8%.
Frontiers in Psychiatry | www.frontiersin.org 3 January 2019 | Volume 9 | Article 744
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Ventriglio et al. Metabolic Problems: Effects of Diagnosis and Treatment
TABLE 1 | Factors associated with metabolic syndrome in 151 psychotic disorder patients.
Factor Metabolic syndrome Statistic p-value
Present Absent (z or χ2)a
Allcases (N = 151) 31.8 [24.5–39.9] 68.2 [60.1–75.5] – –
Women (%) 62.5 [47.4–76.0] 39.8 [30.3–49.9] 6.77 0.009
Older age (years) 45.0 [42.0–48.0] 40.8 [38.2–43.4] 2.18 0.03
Unemployed (%) 83.3 [69.8–92.5] 80.6 [71.6–87.7] 0.67 0.69
Schizoaffective diagnosis (%) 52.1 [37.2–66.7] 35.9 [26.7–46.0] 3.53 0.06
Psychosis
BPRS score 57.1 [49.8–64.4] 49.0 [44.6–53.4] 1.96 0.05
PANSS score 81.7 [71.1–92.3] 71.9 [65.3–78.5] 1.55 0.12
Substance abuse (%) 4.17 [0.51–14.3] 1.94 [0.24–6.84] 0.63 0.43
High-risk antipsychotics (%)b 29.2 [17.0–44.1] 14.6 [3.39–22.9] 4.50 0.03
LAI antipsychotics (%) 50.0 [35.2–64.8] 50.0 [35.2–64.8] 1.67 0.20
Antipsychotic dose (CPZ-eq, mg/day) 423 [266–580] 261 [235–287] 2.14 0.004
Treatment adherence (DA130) 9.95 [9.25–10.7] 9.59 [9.12–10.1] 0.86 0.39
Adverse drug effects (%) 22.9 [12.0–37.3] 18.4 [11.5–27.3] 0.41 0.52
Mood-stabilizers given (%) 18.8 [8.95–32.6] 12.6 [6.89–20.6] 0.99 0.32
Antidepressants given (%) 2.08 [0.05–11.1] 6.80 [2.28–13.5] 1.45 0.23
BMI (kg/m2) 30.3 [28.3–32.3] 26.6 [25.7–27.5] 3.43 0.0006
Obesity (% BMI≥28.8) 64.6 [49.5–77.8] 22.3 [14.7–31.6] 25.4 < 0.0001
Waist circumference (cm) 117 [110–124] 105 [100–110] 2.74 0.006
Systolic BP (mm Hg) 120 [117–123] 116 [114–117] 2.28 0.02
Diastolic BP (mm Hg) 76.5 [75.5–81.5] 73.7 [71.7–75.8] 2.58 0.01
Pulse rate (per min) 85.0 [82.7–86.1] 84.4 [82.4–87.6] 0.37 0.71
ECG repolarization (QTc, msec) 409 [401–417] 407 [403–411] 0.13 0.90
Glucose (FBS, mg/dL) 105 [99.6–110] 88.8 [87.2–90.4] 4.91 < 0.0001
HgbA1c (%) 5.95 [5.71–6.19] 5.62 [5.49–5.75] 2.79 0.005
Totalcholesterol(mg/dL) 217 [206–228] 200 [193–207] 2.50 0.01
LDL cholesterol(mg/dL) 161 [148–174] 140 [132–148] 2.75 0.006
HDL cholesterol(mg/dL) 42.9 [40.3–45.5] 50.2 [47.9–52.5] 3.86 0.0001
Triglycerides (mg/dL) 204 [181–227] 147 [135–159] 4.31 0.0002
TSH (nU/L) 2.56 [2.07–3.05] 2.14 [1.89–2.39] 1.65 0.10
Free thyroxin (ng/dL) 1.13 [1.07–3.05] 1.30 [1.09–1.51] 1.09 0.27
Free triiodothyronine (ng/dL) 0.358 [0.340–0.376] 0.353 [0.340–0.366] 0.86 0.39
Prolactin (ng/dL) 42.9 [41.4–54.5] 50.2 [47.1–65.9] 1.53 0.12
BPRS, Brief Psychiatric Rating Scale; PANSS, Positive and Negative Syndrome Scale; LAI, long-acting injectable antipsychotics; CPZ, chlorpromazine; DAI, Drug Attitude Inv
BMI, body-mass index; BP, blood pressure; ECG, electrocardiogram; Hgb, hemoglobin; LDL, low-density lipoprotein; HDL, high-density lipoprotein; TSH, thyroid-stimulating
aMann-Whitney (z-score) or contingency table (χ2). bClozapine, olanzapine, paliperidone, quetiapine.
The overallprevalence ofMetS (31.8%) was moderate,but
ranged from 18.2% with aripiprazole to 83.3% with quetiapine
(Table 3).By comparison,reported prevalenceof MetS in
patients with psychotic disorders has ranged from 30 to 67% (1, 7,
20, 21). Based on multivariate modeling, factors associated with
MetS were antipsychotic dose, older age, and SzAff diagnosis, but
not oral vs. LAI antipsychotics.
Of note,the presentfinding of significantly greaterrisk
of MetS with SzAff vs,Sz diagnoses supports one hypothesis
of this study,and addsto a previoussuggestion ofsuch a
relationship (6).Although use of complex medication regimens
wasmuch more prevalentamong SzAff subjects,these were
infrequentand notsignificantly associated with risk ofMetS.
In addition,CPZ-eq antipsychotic doses were somewhat higher
among SzAff subjects, although both factors appeared to ope
somewhat independently (Table 4). Nevertheless, we sugges
the relative instability of SzAff disorders contributes to the us
more complex treatments (7) and this feature as well perhap
intrinsic characteristics of such patients may contribute to ris
MetS.
In addition, contraryto prediction,we did not find a
significant difference in risk of MetS in association with treatm
with oral vs. LAI antipsychotics.This finding appearsto
be consistentwith otherrecentreportsindicating thatLAI
agentsmay not be saferthan oral antipsychotics(8, 10).
However,severalmeasurestended to be lessabnormalwith
LAI treatments(including lowertotaland LDL cholesterol,
triglyceridesand prolactin,smallerwaist-circumference,and
Frontiers in Psychiatry | www.frontiersin.org 4 January 2019 | Volume 9 | Article 744
TABLE 1 | Factors associated with metabolic syndrome in 151 psychotic disorder patients.
Factor Metabolic syndrome Statistic p-value
Present Absent (z or χ2)a
Allcases (N = 151) 31.8 [24.5–39.9] 68.2 [60.1–75.5] – –
Women (%) 62.5 [47.4–76.0] 39.8 [30.3–49.9] 6.77 0.009
Older age (years) 45.0 [42.0–48.0] 40.8 [38.2–43.4] 2.18 0.03
Unemployed (%) 83.3 [69.8–92.5] 80.6 [71.6–87.7] 0.67 0.69
Schizoaffective diagnosis (%) 52.1 [37.2–66.7] 35.9 [26.7–46.0] 3.53 0.06
Psychosis
BPRS score 57.1 [49.8–64.4] 49.0 [44.6–53.4] 1.96 0.05
PANSS score 81.7 [71.1–92.3] 71.9 [65.3–78.5] 1.55 0.12
Substance abuse (%) 4.17 [0.51–14.3] 1.94 [0.24–6.84] 0.63 0.43
High-risk antipsychotics (%)b 29.2 [17.0–44.1] 14.6 [3.39–22.9] 4.50 0.03
LAI antipsychotics (%) 50.0 [35.2–64.8] 50.0 [35.2–64.8] 1.67 0.20
Antipsychotic dose (CPZ-eq, mg/day) 423 [266–580] 261 [235–287] 2.14 0.004
Treatment adherence (DA130) 9.95 [9.25–10.7] 9.59 [9.12–10.1] 0.86 0.39
Adverse drug effects (%) 22.9 [12.0–37.3] 18.4 [11.5–27.3] 0.41 0.52
Mood-stabilizers given (%) 18.8 [8.95–32.6] 12.6 [6.89–20.6] 0.99 0.32
Antidepressants given (%) 2.08 [0.05–11.1] 6.80 [2.28–13.5] 1.45 0.23
BMI (kg/m2) 30.3 [28.3–32.3] 26.6 [25.7–27.5] 3.43 0.0006
Obesity (% BMI≥28.8) 64.6 [49.5–77.8] 22.3 [14.7–31.6] 25.4 < 0.0001
Waist circumference (cm) 117 [110–124] 105 [100–110] 2.74 0.006
Systolic BP (mm Hg) 120 [117–123] 116 [114–117] 2.28 0.02
Diastolic BP (mm Hg) 76.5 [75.5–81.5] 73.7 [71.7–75.8] 2.58 0.01
Pulse rate (per min) 85.0 [82.7–86.1] 84.4 [82.4–87.6] 0.37 0.71
ECG repolarization (QTc, msec) 409 [401–417] 407 [403–411] 0.13 0.90
Glucose (FBS, mg/dL) 105 [99.6–110] 88.8 [87.2–90.4] 4.91 < 0.0001
HgbA1c (%) 5.95 [5.71–6.19] 5.62 [5.49–5.75] 2.79 0.005
Totalcholesterol(mg/dL) 217 [206–228] 200 [193–207] 2.50 0.01
LDL cholesterol(mg/dL) 161 [148–174] 140 [132–148] 2.75 0.006
HDL cholesterol(mg/dL) 42.9 [40.3–45.5] 50.2 [47.9–52.5] 3.86 0.0001
Triglycerides (mg/dL) 204 [181–227] 147 [135–159] 4.31 0.0002
TSH (nU/L) 2.56 [2.07–3.05] 2.14 [1.89–2.39] 1.65 0.10
Free thyroxin (ng/dL) 1.13 [1.07–3.05] 1.30 [1.09–1.51] 1.09 0.27
Free triiodothyronine (ng/dL) 0.358 [0.340–0.376] 0.353 [0.340–0.366] 0.86 0.39
Prolactin (ng/dL) 42.9 [41.4–54.5] 50.2 [47.1–65.9] 1.53 0.12
BPRS, Brief Psychiatric Rating Scale; PANSS, Positive and Negative Syndrome Scale; LAI, long-acting injectable antipsychotics; CPZ, chlorpromazine; DAI, Drug Attitude Inv
BMI, body-mass index; BP, blood pressure; ECG, electrocardiogram; Hgb, hemoglobin; LDL, low-density lipoprotein; HDL, high-density lipoprotein; TSH, thyroid-stimulating
aMann-Whitney (z-score) or contingency table (χ2). bClozapine, olanzapine, paliperidone, quetiapine.
The overallprevalence ofMetS (31.8%) was moderate,but
ranged from 18.2% with aripiprazole to 83.3% with quetiapine
(Table 3).By comparison,reported prevalenceof MetS in
patients with psychotic disorders has ranged from 30 to 67% (1, 7,
20, 21). Based on multivariate modeling, factors associated with
MetS were antipsychotic dose, older age, and SzAff diagnosis, but
not oral vs. LAI antipsychotics.
Of note,the presentfinding of significantly greaterrisk
of MetS with SzAff vs,Sz diagnoses supports one hypothesis
of this study,and addsto a previoussuggestion ofsuch a
relationship (6).Although use of complex medication regimens
wasmuch more prevalentamong SzAff subjects,these were
infrequentand notsignificantly associated with risk ofMetS.
In addition,CPZ-eq antipsychotic doses were somewhat higher
among SzAff subjects, although both factors appeared to ope
somewhat independently (Table 4). Nevertheless, we sugges
the relative instability of SzAff disorders contributes to the us
more complex treatments (7) and this feature as well perhap
intrinsic characteristics of such patients may contribute to ris
MetS.
In addition, contraryto prediction,we did not find a
significant difference in risk of MetS in association with treatm
with oral vs. LAI antipsychotics.This finding appearsto
be consistentwith otherrecentreportsindicating thatLAI
agentsmay not be saferthan oral antipsychotics(8, 10).
However,severalmeasurestended to be lessabnormalwith
LAI treatments(including lowertotaland LDL cholesterol,
triglyceridesand prolactin,smallerwaist-circumference,and
Frontiers in Psychiatry | www.frontiersin.org 4 January 2019 | Volume 9 | Article 744
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Ventriglio et al. Metabolic Problems: Effects of Diagnosis and Treatment
TABLE 2 | Multivariable logistic regression modeling: diagnostic measures
associated with metabolic syndrome.
Measure OR [95% CI] χ2 p-value
Higher FBS 1.12 [1.07–1.17] 25.2 <0.0001
Lower HDL 1.16 [1.08–1.24] 17.0 <0.0001
Diastolic blood pressure 1.10 [1.04–1.16] 10.3 0.001
Higher BMI 1.17 [1.06–1.29] 9.53 0.002
Female sex 5.72 [1.85–17.7] 9.21 0.002
Modelfit χ2 = 93,5, p < 0.0001. Not associated, age, LDL level, waist-circumference.
TABLE 3 | Risk of metabolic syndrome: antipsychotic agents and doses.
Drug Metabolic Syndrome Daily dose
Prevalence (% [CI]) (CPZ-eq mg [CI])
Quetiapine 83.3 [35.9–99.6] 229 [89.9–368]
Clozapine 60.0 [14,7–94.7] 615 [196–1034]
Paliperidone 34.0 [21.5–48.3] 298 [265–330]
Olanzapine 33.4 [13.3–59.0] 378 [309–448]
Risperidone 23.5 [10.7–41.2] 266 [232–301]
Haloperidol 18.2 [2.28–51.8] 259 [197–321]
Aripiprazole 18.2 [5.19–40.3] 121 [95.4–146]
Risk ofMetS is notsignificantly associated with CPZ-eq dose (Spearman rs = 0.402,
p = 0.325), but the drugs differ overall(χ2 = 13.4, p = 0.04). Relatively high-risk drugs
are quetiapine, clozapine, paliperidone and olanzapine.
TABLE 4 | Multivariable logistic regression modeling: risk factors associated with
metabolic syndrome.
Factor OR [95% CI] χ2 p-value
Antipsychotic dose (CPZ-eq) 1.003 [1.001–1.005] 4.80 0.028
Older age 1.03 [1.01–1.07] 4.76 0.029
Diagnosis: Schizoaffective 2.28 [1.06–4.90] 4.46 0.035
Oralvs. LAI antipsychotics 1.01 [0.46–2.24] 0.001 0.98
Modelfit χ2 = 17.9, p = 0.001. Not associated, sex, diagnosis, psychosis severity.
(BPRS rating).
shorter QTc interval). In addition, we found marked differences
in risk of MetS between particular antipsychotic agents,with
higher risk associated with quetiapine,clozapine,paliperidone,
and olanzapine, which are known to be associated with relativ
high risks of weight-gain (1, 2, 18, 22, 23).
Limitations
The study included a relatively smallnumber ofsubjects and
its findings may not generalize to other sites.Its cross-sectional
design supports associations with MetS,but precludes causal
inferences.In addition,estimatesof CPZ-eq dosesof LAI
antipsychoticsare not adjusted forprobablebut uncertain
differences in bioavailability of injected vs.orally administered
drugs.
CONCLUSIONS
This observationalstudy of151 patient-subjects with chronic
psychoticdisordersfound a moderateprevalenceof MetS
(31.8%),which was associated with being overweight or obese
and with antipsychotic agents prone to leading to weight-gain
as wellas higher antipsychotic CPZ-eq doses,and older age.
Notably,risk of MetS was somewhat greater among SzAff than
Sz subjects,butdid notdiffer significantly between treatment
with oral and LAI antipsychoticsnor with the relatively
infrequent use of adjunctive mood-stabilizers or antidepressa
However, several metabolic measures tended to be less abno
among SzAff than Sz subjects.The association ofMetS with
SzAff (more than with Sz)probably reflectsthe complexity
of SzAff disordersand their pharmacologicaltreatment,
includingsomewhathigherantipsychoticdosesand more
co-treatmentwith mood-stabilizersand antidepressants,but
may also reflect other unknown characteristics of the disorde
themselves.
AUTHOR CONTRIBUTIONS
AV, GV, IB, AC, AR, and AP recruited patients and collected da
AV and RB wrote the paper. AB supervised clinical work and t
manuscript drafting.
FUNDING
Supported by Department of Clinical and Experimental Medic
of University ofFoggia.Supported,in part,by a grantfrom
the Bruce J.Anderson Foundation and by the McLean Private
Donors Psychopharmacology Research Fund (to RB).
REFERENCES
1. De Hert M, Dekker JM, Wood D, Kahl KG, Holt RI, Möller
HJ. Cardiovasculardiseaseand diabetesin people with severe
mental illness position statementfrom the European Psychiatric
Association(EPA), supportedby the EuropeanAssociationfor the
Study of Diabetes(EASD) and the EuropeanSocietyof Cardiology
(ESC). Eur Psychiatry(2009) 24:412–24.doi: 10.1016/j.eurpsy.2009.
01.005
2. Ventriglio A,Gentile A,Stella E,Bellomo A.Metabolic issues in patients
affected by schizophrenia:clinicalcharacteristics and medicalmanagement.
Front Neurosci. (2015) 9:297–303. doi: 10.3389/fnins.2015.00297
3. De Hert M,Detraux J,Vancampfort D.The intriguing relationship between
coronary heartdisease and mentaldisorders.Dialog Clin Neurosci.(2018)
20:31–40.
4. VancampfortD, VansteelandtK, Correll CU, Mitchell AJ, De Herdt
A, SienaertP, et al. Metabolicsyndromeand metabolicabnormalities
in bipolar disorder:meta-analysisof prevalenceratesand moderators.
Am J Psychiatry(2013) 170:265–74.doi: 10.1176/appi.ajp.2012.120
50620
5. Ventriglio A,Gentile A,BaldessariniRJ, Martone S,VitraniG, La Marca
A, et al. Improvementsin metabolicabnormalitiesamongoverweight
schizophrenia and bipolar disorder patients. Eur Psychiatry (2014) 29:402–
doi: 10.1016/j.eurpsy.2013.11.005
Frontiers in Psychiatry | www.frontiersin.org 5 January 2019 | Volume 9 | Article 744
TABLE 2 | Multivariable logistic regression modeling: diagnostic measures
associated with metabolic syndrome.
Measure OR [95% CI] χ2 p-value
Higher FBS 1.12 [1.07–1.17] 25.2 <0.0001
Lower HDL 1.16 [1.08–1.24] 17.0 <0.0001
Diastolic blood pressure 1.10 [1.04–1.16] 10.3 0.001
Higher BMI 1.17 [1.06–1.29] 9.53 0.002
Female sex 5.72 [1.85–17.7] 9.21 0.002
Modelfit χ2 = 93,5, p < 0.0001. Not associated, age, LDL level, waist-circumference.
TABLE 3 | Risk of metabolic syndrome: antipsychotic agents and doses.
Drug Metabolic Syndrome Daily dose
Prevalence (% [CI]) (CPZ-eq mg [CI])
Quetiapine 83.3 [35.9–99.6] 229 [89.9–368]
Clozapine 60.0 [14,7–94.7] 615 [196–1034]
Paliperidone 34.0 [21.5–48.3] 298 [265–330]
Olanzapine 33.4 [13.3–59.0] 378 [309–448]
Risperidone 23.5 [10.7–41.2] 266 [232–301]
Haloperidol 18.2 [2.28–51.8] 259 [197–321]
Aripiprazole 18.2 [5.19–40.3] 121 [95.4–146]
Risk ofMetS is notsignificantly associated with CPZ-eq dose (Spearman rs = 0.402,
p = 0.325), but the drugs differ overall(χ2 = 13.4, p = 0.04). Relatively high-risk drugs
are quetiapine, clozapine, paliperidone and olanzapine.
TABLE 4 | Multivariable logistic regression modeling: risk factors associated with
metabolic syndrome.
Factor OR [95% CI] χ2 p-value
Antipsychotic dose (CPZ-eq) 1.003 [1.001–1.005] 4.80 0.028
Older age 1.03 [1.01–1.07] 4.76 0.029
Diagnosis: Schizoaffective 2.28 [1.06–4.90] 4.46 0.035
Oralvs. LAI antipsychotics 1.01 [0.46–2.24] 0.001 0.98
Modelfit χ2 = 17.9, p = 0.001. Not associated, sex, diagnosis, psychosis severity.
(BPRS rating).
shorter QTc interval). In addition, we found marked differences
in risk of MetS between particular antipsychotic agents,with
higher risk associated with quetiapine,clozapine,paliperidone,
and olanzapine, which are known to be associated with relativ
high risks of weight-gain (1, 2, 18, 22, 23).
Limitations
The study included a relatively smallnumber ofsubjects and
its findings may not generalize to other sites.Its cross-sectional
design supports associations with MetS,but precludes causal
inferences.In addition,estimatesof CPZ-eq dosesof LAI
antipsychoticsare not adjusted forprobablebut uncertain
differences in bioavailability of injected vs.orally administered
drugs.
CONCLUSIONS
This observationalstudy of151 patient-subjects with chronic
psychoticdisordersfound a moderateprevalenceof MetS
(31.8%),which was associated with being overweight or obese
and with antipsychotic agents prone to leading to weight-gain
as wellas higher antipsychotic CPZ-eq doses,and older age.
Notably,risk of MetS was somewhat greater among SzAff than
Sz subjects,butdid notdiffer significantly between treatment
with oral and LAI antipsychoticsnor with the relatively
infrequent use of adjunctive mood-stabilizers or antidepressa
However, several metabolic measures tended to be less abno
among SzAff than Sz subjects.The association ofMetS with
SzAff (more than with Sz)probably reflectsthe complexity
of SzAff disordersand their pharmacologicaltreatment,
includingsomewhathigherantipsychoticdosesand more
co-treatmentwith mood-stabilizersand antidepressants,but
may also reflect other unknown characteristics of the disorde
themselves.
AUTHOR CONTRIBUTIONS
AV, GV, IB, AC, AR, and AP recruited patients and collected da
AV and RB wrote the paper. AB supervised clinical work and t
manuscript drafting.
FUNDING
Supported by Department of Clinical and Experimental Medic
of University ofFoggia.Supported,in part,by a grantfrom
the Bruce J.Anderson Foundation and by the McLean Private
Donors Psychopharmacology Research Fund (to RB).
REFERENCES
1. De Hert M, Dekker JM, Wood D, Kahl KG, Holt RI, Möller
HJ. Cardiovasculardiseaseand diabetesin people with severe
mental illness position statementfrom the European Psychiatric
Association(EPA), supportedby the EuropeanAssociationfor the
Study of Diabetes(EASD) and the EuropeanSocietyof Cardiology
(ESC). Eur Psychiatry(2009) 24:412–24.doi: 10.1016/j.eurpsy.2009.
01.005
2. Ventriglio A,Gentile A,Stella E,Bellomo A.Metabolic issues in patients
affected by schizophrenia:clinicalcharacteristics and medicalmanagement.
Front Neurosci. (2015) 9:297–303. doi: 10.3389/fnins.2015.00297
3. De Hert M,Detraux J,Vancampfort D.The intriguing relationship between
coronary heartdisease and mentaldisorders.Dialog Clin Neurosci.(2018)
20:31–40.
4. VancampfortD, VansteelandtK, Correll CU, Mitchell AJ, De Herdt
A, SienaertP, et al. Metabolicsyndromeand metabolicabnormalities
in bipolar disorder:meta-analysisof prevalenceratesand moderators.
Am J Psychiatry(2013) 170:265–74.doi: 10.1176/appi.ajp.2012.120
50620
5. Ventriglio A,Gentile A,BaldessariniRJ, Martone S,VitraniG, La Marca
A, et al. Improvementsin metabolicabnormalitiesamongoverweight
schizophrenia and bipolar disorder patients. Eur Psychiatry (2014) 29:402–
doi: 10.1016/j.eurpsy.2013.11.005
Frontiers in Psychiatry | www.frontiersin.org 5 January 2019 | Volume 9 | Article 744
Ventriglio et al. Metabolic Problems: Effects of Diagnosis and Treatment
6. Bartoli F, Crocamo C, Caslini M, Clerici M, Carrà G. Schizoaffective disorder
and metabolicsyndrome:meta-analyticcomparison with schizophrenia
and othernonaffective psychoses.J PsychiatrRes.(2015)66–67:127–34.
doi: 10.1016/j.jpsychires.2015.04.028
7. Chouinard VA, Pingali SM, Chouinard G, Henderson DC, Mallya SG, Cypess
AM, et al.Factors associated with overweight and obesity in schizophrenia,
schizoaffective and bipolardisorders.Psychiatry Res.(2016)237:304–10.
doi: 10.1016/j.psychres.2016.01.024
8. Gentile S.Safety concerns associated with second-generation antipsychotic
long-acting injection treatment.A systematic update.Horm MolBiolClin
Investig. (2017). doi: 10.1515/hmbci-2017-0004. [Epub ahead of print].
9. BrissosS, Ruiz VeguillaM, Taylor D, Balanzá-MartinezV. Role of
long-acting injectable antipsychoticsin schizophrenia:a criticalappraisal
Ther Adv Psychopharmacol.(2014)4:198–219.doi: 10.1177/20451253145
40297
10. Sanchez-Martinez V,Romero-Rubio D,Abad-Perez MJ,Descalzo-Cabades
MA, Alonso-GutierrezS, Salazar-FraileJ, et al. Metabolicsyndrome
and cardiovascularrisk in people treatedwith long-actinginjectable
antipsychotics. Endocr Metab Immune Disord Drug Targets (2018) 18:379–87.
doi: 10.2174/1871530317666171120151201
11. American Psychiatric Association (APA).Diagnostic and StatisticalManual
of Mental Disorders.4th ed.Text Revision (DSM-IV-TR).Washington,DC:
American Psychiatric Publishing (2000).
12. Kay SR, Fiszbein A, Opler LA. The positiveand negativesyndrome
scalefor schizophrenia(PANSS).Schizophrenia Bull.(1987)13:261–76.
doi: 10.1093/schbul/13.2.261
13. Overall JE,Gorham DR.The Brief Psychiatric Rating Scale (BPRS).Psychol
Rep. (1962) 10:799–812. doi: 10.2466/pr0.1962.10.3.799
14. Hogan TP, Awad AG, EastwoodR. Self-reportscale predictiveof
drug compliancein schizophrenics:reliability and discriminative
validity. PsycholMed. (1983) 13:177–83.doi: 10.1017/S00332917000
50182
15. Alberti KG, ZimmetP, Shaw J. Metabolicsyndrome-anew worldwide
definition: consensusstatementfrom the InternationalDiabetes
Federation.Diabet Med.(2006) 23:469–80.doi:10.1111/j.1464-5491.2006.0
1858.x
16. AlbertiKG, EckelRH, Grundy SM,Zimmet PZ,Cleeman JI,Donato KA,
et al.Harmonizing the metabolic syndrome.Circulation (2009) 120:1640–5.
doi: 10.1161/CIRCULATIONAHA.109.192644
17. Gardner D,Murphy A,BaldessariniRJ. Equivalentdoses ofantipsychotic
agents: findings from an international Delphi survey. Am J Psychiatry (2010
167:686–93. doi: 10.1176/appi.ajp.2009.09060802
18. Baldessarini RJ. Chemotherapy in Psychiatry. 3rd ed. New York, NY: Spring
Press (2013).
19. Centorrino F,Sani G,Fogarty KV,Salvatore P,Talamo A,Cincotta SL,et al.
Combinations of mood-stabilizers with antipsychotics as treatment strateg
in hospitalized psychiatric patients. Clin Neuropsychiatry (2006) 3:322–26.
20. Centorrino F,Masters G,BaldessariniRJ, Öngür D.Metabolic syndrome
in psychiatricallyhospitalizedpatients treated with antipsychotics
and other psychotropics.Hum Psychopharmacol.(2012) 27:521–6.
doi: 10.1002/hup.2257
21. Correll CU, Frederickson AM,Kane JM, Manu P. Metabolic syndrome
and the risk of coronaryheartdiseasein 367 patientstreated with
second generation antipsychotic drugs.J Clin Psychiatry (2006) 67:575–83.
doi: 10.4088/JCP.v67n0408
22. Musil R, ObermeierM, Russ P, Hamerle M. Weight-gainand
antipsychotis;drug safety review.Expert Opin Drug Safety (2015) 14:73–96.
doi: 10.1517/14740338.2015.974549
23. Cascade E,KalaliAH, Buckley P.Treatmentof schizoaffective disorder.
Psychiatry (2009) 6:15–7.
Conflictof InterestStatement:The authorsdeclarethat the research was
conducted in the absence of any commercial or financial relationships that cou
be construed as a potential conflict of interest.
Copyright© 2019 Ventriglio,Baldessarini,Vitrani,Bonfitto,Cecere,Rinaldi,
Petito and Bellomo.This is an open-accessarticle distributed under the terms
of the Creative Commons Attribution License (CC BY).The use,distribution or
reproduction in other forums is permitted, provided the original author(s) and
copyrightowner(s) are credited and that the originalpublication in this journal
is cited,in accordance with accepted academic practice.No use,distribution or
reproduction is permitted which does not comply with these terms.
Frontiers in Psychiatry | www.frontiersin.org 6 January 2019 | Volume 9 | Article 744
6. Bartoli F, Crocamo C, Caslini M, Clerici M, Carrà G. Schizoaffective disorder
and metabolicsyndrome:meta-analyticcomparison with schizophrenia
and othernonaffective psychoses.J PsychiatrRes.(2015)66–67:127–34.
doi: 10.1016/j.jpsychires.2015.04.028
7. Chouinard VA, Pingali SM, Chouinard G, Henderson DC, Mallya SG, Cypess
AM, et al.Factors associated with overweight and obesity in schizophrenia,
schizoaffective and bipolardisorders.Psychiatry Res.(2016)237:304–10.
doi: 10.1016/j.psychres.2016.01.024
8. Gentile S.Safety concerns associated with second-generation antipsychotic
long-acting injection treatment.A systematic update.Horm MolBiolClin
Investig. (2017). doi: 10.1515/hmbci-2017-0004. [Epub ahead of print].
9. BrissosS, Ruiz VeguillaM, Taylor D, Balanzá-MartinezV. Role of
long-acting injectable antipsychoticsin schizophrenia:a criticalappraisal
Ther Adv Psychopharmacol.(2014)4:198–219.doi: 10.1177/20451253145
40297
10. Sanchez-Martinez V,Romero-Rubio D,Abad-Perez MJ,Descalzo-Cabades
MA, Alonso-GutierrezS, Salazar-FraileJ, et al. Metabolicsyndrome
and cardiovascularrisk in people treatedwith long-actinginjectable
antipsychotics. Endocr Metab Immune Disord Drug Targets (2018) 18:379–87.
doi: 10.2174/1871530317666171120151201
11. American Psychiatric Association (APA).Diagnostic and StatisticalManual
of Mental Disorders.4th ed.Text Revision (DSM-IV-TR).Washington,DC:
American Psychiatric Publishing (2000).
12. Kay SR, Fiszbein A, Opler LA. The positiveand negativesyndrome
scalefor schizophrenia(PANSS).Schizophrenia Bull.(1987)13:261–76.
doi: 10.1093/schbul/13.2.261
13. Overall JE,Gorham DR.The Brief Psychiatric Rating Scale (BPRS).Psychol
Rep. (1962) 10:799–812. doi: 10.2466/pr0.1962.10.3.799
14. Hogan TP, Awad AG, EastwoodR. Self-reportscale predictiveof
drug compliancein schizophrenics:reliability and discriminative
validity. PsycholMed. (1983) 13:177–83.doi: 10.1017/S00332917000
50182
15. Alberti KG, ZimmetP, Shaw J. Metabolicsyndrome-anew worldwide
definition: consensusstatementfrom the InternationalDiabetes
Federation.Diabet Med.(2006) 23:469–80.doi:10.1111/j.1464-5491.2006.0
1858.x
16. AlbertiKG, EckelRH, Grundy SM,Zimmet PZ,Cleeman JI,Donato KA,
et al.Harmonizing the metabolic syndrome.Circulation (2009) 120:1640–5.
doi: 10.1161/CIRCULATIONAHA.109.192644
17. Gardner D,Murphy A,BaldessariniRJ. Equivalentdoses ofantipsychotic
agents: findings from an international Delphi survey. Am J Psychiatry (2010
167:686–93. doi: 10.1176/appi.ajp.2009.09060802
18. Baldessarini RJ. Chemotherapy in Psychiatry. 3rd ed. New York, NY: Spring
Press (2013).
19. Centorrino F,Sani G,Fogarty KV,Salvatore P,Talamo A,Cincotta SL,et al.
Combinations of mood-stabilizers with antipsychotics as treatment strateg
in hospitalized psychiatric patients. Clin Neuropsychiatry (2006) 3:322–26.
20. Centorrino F,Masters G,BaldessariniRJ, Öngür D.Metabolic syndrome
in psychiatricallyhospitalizedpatients treated with antipsychotics
and other psychotropics.Hum Psychopharmacol.(2012) 27:521–6.
doi: 10.1002/hup.2257
21. Correll CU, Frederickson AM,Kane JM, Manu P. Metabolic syndrome
and the risk of coronaryheartdiseasein 367 patientstreated with
second generation antipsychotic drugs.J Clin Psychiatry (2006) 67:575–83.
doi: 10.4088/JCP.v67n0408
22. Musil R, ObermeierM, Russ P, Hamerle M. Weight-gainand
antipsychotis;drug safety review.Expert Opin Drug Safety (2015) 14:73–96.
doi: 10.1517/14740338.2015.974549
23. Cascade E,KalaliAH, Buckley P.Treatmentof schizoaffective disorder.
Psychiatry (2009) 6:15–7.
Conflictof InterestStatement:The authorsdeclarethat the research was
conducted in the absence of any commercial or financial relationships that cou
be construed as a potential conflict of interest.
Copyright© 2019 Ventriglio,Baldessarini,Vitrani,Bonfitto,Cecere,Rinaldi,
Petito and Bellomo.This is an open-accessarticle distributed under the terms
of the Creative Commons Attribution License (CC BY).The use,distribution or
reproduction in other forums is permitted, provided the original author(s) and
copyrightowner(s) are credited and that the originalpublication in this journal
is cited,in accordance with accepted academic practice.No use,distribution or
reproduction is permitted which does not comply with these terms.
Frontiers in Psychiatry | www.frontiersin.org 6 January 2019 | Volume 9 | Article 744
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 6
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.