Molecular Technologies: Breast Cancer
VerifiedAdded on 2023/06/10
|17
|4444
|202
AI Summary
Breast cancer is a leading cause of death in developing countries. This paper discusses the different malignancies associated with breast cancer, molecular pathology, diagnostic methods, prognosis, and treatment. The molecular pathology of breast cancer is guided by the sporadic clonal evolution model and stem cell model. Immuno-histochemical techniques and fluorescent in-situ hybridization are used for the detection of cancerous cell lines. Hormonal therapy is used for the prevention of recurrence of breast cancer. The future of molecular diagnostic in breast cancer is aimed towards the detection of breast cancer via the use of biomarkers.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: BREAST CANCER
Molecular Technologies: Breast Cancer
Name of the Student
Name of the University
Author Note
Molecular Technologies: Breast Cancer
Name of the Student
Name of the University
Author Note
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1
BREAST CANCER
Abstract
. Breast cancers are mainly common among women in comparison to men. There are
different types of breast cancers. Some of the common type of breast cancer includes
Invasive Ductal Carcinoma (IDC), Invasive Lobular Carcinoma (ILC) and Ductal Carcinoma
(in-situ) (DCIS). The main molecular pathology of breast cancer is guided by sporadic clonal
evolution model and stem cell model. The pathology of the IDC is mainly guided by the
hypothesis of sporadic clonal evolution model. According to this model, the epithelial cells of
the breast can undergo random mutations leading to the development of cancer. In order to
detect the cancerous cell-line of the breast tissue immuno-histochemical (IHC) techniques are
used. Recently efforts have been undertaken in order to employ fluorescent in-situ
hybridization (FISH) for the detection of the cancerous cell line. Both FISH and IHC
employs ligand binding assays for the detection of breast cancer. The prognosis of breast
cancer is defined by several factors including age, stage of cancer, status of lymph node
propagation and status of the hormonal receptors on the breast cancer tissue. Surgery is not a
sole treatment for breast cancer. At present hormonal therapy is also used for the prevention
of recurrence of breast cancer. The future molecular diagnostic in breast cancer is mainly
aiming towards the detection of breast cancer via the use of biomarkers and this will pave the
way for the formulations of personalised medications
Keywords: Breast cancer, breast cancer markers, breast cancer types, breast cancer
pathology, breast cancer treatment
BREAST CANCER
Abstract
. Breast cancers are mainly common among women in comparison to men. There are
different types of breast cancers. Some of the common type of breast cancer includes
Invasive Ductal Carcinoma (IDC), Invasive Lobular Carcinoma (ILC) and Ductal Carcinoma
(in-situ) (DCIS). The main molecular pathology of breast cancer is guided by sporadic clonal
evolution model and stem cell model. The pathology of the IDC is mainly guided by the
hypothesis of sporadic clonal evolution model. According to this model, the epithelial cells of
the breast can undergo random mutations leading to the development of cancer. In order to
detect the cancerous cell-line of the breast tissue immuno-histochemical (IHC) techniques are
used. Recently efforts have been undertaken in order to employ fluorescent in-situ
hybridization (FISH) for the detection of the cancerous cell line. Both FISH and IHC
employs ligand binding assays for the detection of breast cancer. The prognosis of breast
cancer is defined by several factors including age, stage of cancer, status of lymph node
propagation and status of the hormonal receptors on the breast cancer tissue. Surgery is not a
sole treatment for breast cancer. At present hormonal therapy is also used for the prevention
of recurrence of breast cancer. The future molecular diagnostic in breast cancer is mainly
aiming towards the detection of breast cancer via the use of biomarkers and this will pave the
way for the formulations of personalised medications
Keywords: Breast cancer, breast cancer markers, breast cancer types, breast cancer
pathology, breast cancer treatment
2
BREAST CANCER
Table of Contents
Introduction................................................................................................................................3
Discussion..................................................................................................................................3
Different malignancies for the breast cancer.........................................................................3
Molecular pathology of breast cancer....................................................................................4
Molecular pathology of IDC..............................................................................................5
Molecular diagnostic method.................................................................................................6
Prognosis................................................................................................................................8
Treatment...............................................................................................................................9
Future of molecular diagnostic in the cancer.......................................................................10
Conclusion................................................................................................................................10
References................................................................................................................................11
BREAST CANCER
Table of Contents
Introduction................................................................................................................................3
Discussion..................................................................................................................................3
Different malignancies for the breast cancer.........................................................................3
Molecular pathology of breast cancer....................................................................................4
Molecular pathology of IDC..............................................................................................5
Molecular diagnostic method.................................................................................................6
Prognosis................................................................................................................................8
Treatment...............................................................................................................................9
Future of molecular diagnostic in the cancer.......................................................................10
Conclusion................................................................................................................................10
References................................................................................................................................11
3
BREAST CANCER
Introduction
Breast cancer is regarded as one of the leading causes of death in most of the
developing countries (Stephens et al., 2012). It affects mostly the female however; males are
also affected (DeSantis, Ma, Bryan & Jemal, 2014). The main reason which are highlighted
as the main causative agent of breast cancer include sudden genetic mutation and presence of
genetic pre-disposition for the development of breast cancer. All these are non-modifiable
factors underlying the development of breast cancer (Goldhirsch et al., 2014). The type of
breast cancer is mainly determined by the affected breast tissues (Alexandrov et al., 2013).
Based on the site of occurrence, breast cancer can be sub-divided into ductal carcinoma,
invasive ductal carcinoma and invasive lobular carcinoma (Jafari-Koshki, Schmid & Mahaki,
2014; Khamis et al., 2012; Buchsbaum & Oh, 2016). The following assignment aims to
provide a detailed overview of the breast cancer. The paper will initiate with highlighting
different malignancies which are associated with breast cancer. Then the paper will discuss
the molecular pathology underlying the breast-cancer with a special mention to the invasive
ductal carcinoma. Upon discussing the pathophysiology, the paper will highlight the common
molecular diagnostic methods which are used for the detection of breast cancer. At the end,
the paper will analyse how prognosis of breast cancer is associated with several different
factors, along with the possible method of treatment of this complex disease and future
projection of the advanced grade treatment.
Discussion
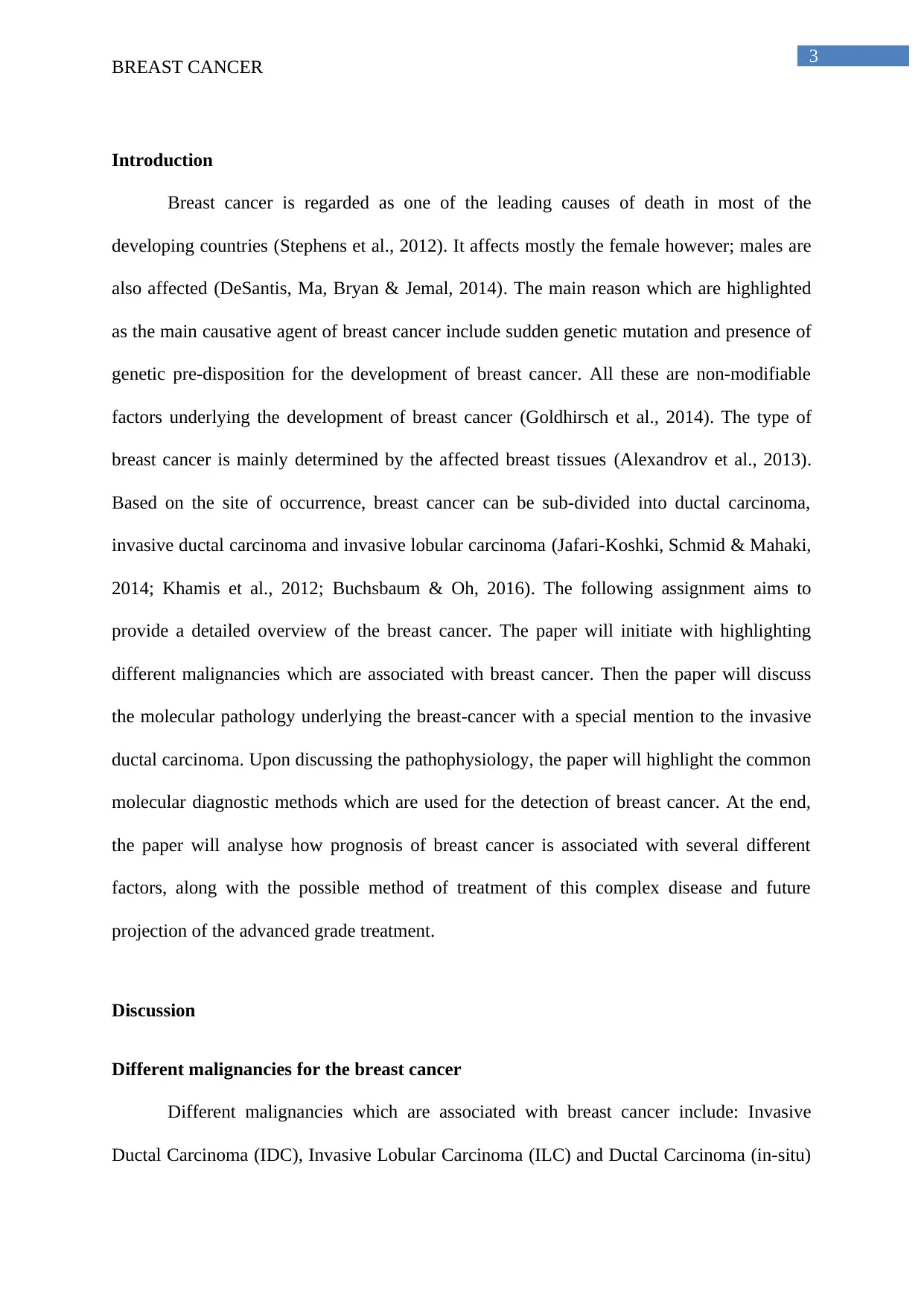
Different malignancies for the breast cancer
Different malignancies which are associated with breast cancer include: Invasive
Ductal Carcinoma (IDC), Invasive Lobular Carcinoma (ILC) and Ductal Carcinoma (in-situ)
BREAST CANCER
Introduction
Breast cancer is regarded as one of the leading causes of death in most of the
developing countries (Stephens et al., 2012). It affects mostly the female however; males are
also affected (DeSantis, Ma, Bryan & Jemal, 2014). The main reason which are highlighted
as the main causative agent of breast cancer include sudden genetic mutation and presence of
genetic pre-disposition for the development of breast cancer. All these are non-modifiable
factors underlying the development of breast cancer (Goldhirsch et al., 2014). The type of
breast cancer is mainly determined by the affected breast tissues (Alexandrov et al., 2013).
Based on the site of occurrence, breast cancer can be sub-divided into ductal carcinoma,
invasive ductal carcinoma and invasive lobular carcinoma (Jafari-Koshki, Schmid & Mahaki,
2014; Khamis et al., 2012; Buchsbaum & Oh, 2016). The following assignment aims to
provide a detailed overview of the breast cancer. The paper will initiate with highlighting
different malignancies which are associated with breast cancer. Then the paper will discuss
the molecular pathology underlying the breast-cancer with a special mention to the invasive
ductal carcinoma. Upon discussing the pathophysiology, the paper will highlight the common
molecular diagnostic methods which are used for the detection of breast cancer. At the end,
the paper will analyse how prognosis of breast cancer is associated with several different
factors, along with the possible method of treatment of this complex disease and future
projection of the advanced grade treatment.
Discussion
Different malignancies for the breast cancer
Different malignancies which are associated with breast cancer include: Invasive
Ductal Carcinoma (IDC), Invasive Lobular Carcinoma (ILC) and Ductal Carcinoma (in-situ)
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4
BREAST CANCER
(DCIS). IDC is further sub-divided into Tubular Carcinoma of the Breast, Medullary
Carcinoma of the Breast, Mucinous Carcinoma of the Breast, Papillary Carcinoma of the
Breast, Cribriform Carcinoma of the Breast (American Cancer Society, 2018). Other types of
breast cancer include inflammatory breast cancer, lobular carcinoma (in-situ), Paget’s disease
of the nipple, phyllodes tumors of the breast and metastatic breast cancer (American Cancer
Society, 2018).
(Source: American Cancer Society, 2018)
Molecular pathology of breast cancer
There are two leading models in order to discuss the molecular pathology underlying
the breast cancer. The sporadic clonal evolution model hypothesised that the breast epithelial
cell can undergo random mutations leading to the development of cancer. Alternatively
cancer stem cell model propose that only stem cell and the progenitor cells have the
capability to initiate and maintain the tumour progression (Bombonati & Sgroi, 2011). The
BREAST CANCER
(DCIS). IDC is further sub-divided into Tubular Carcinoma of the Breast, Medullary
Carcinoma of the Breast, Mucinous Carcinoma of the Breast, Papillary Carcinoma of the
Breast, Cribriform Carcinoma of the Breast (American Cancer Society, 2018). Other types of
breast cancer include inflammatory breast cancer, lobular carcinoma (in-situ), Paget’s disease
of the nipple, phyllodes tumors of the breast and metastatic breast cancer (American Cancer
Society, 2018).
(Source: American Cancer Society, 2018)
Molecular pathology of breast cancer
There are two leading models in order to discuss the molecular pathology underlying
the breast cancer. The sporadic clonal evolution model hypothesised that the breast epithelial
cell can undergo random mutations leading to the development of cancer. Alternatively
cancer stem cell model propose that only stem cell and the progenitor cells have the
capability to initiate and maintain the tumour progression (Bombonati & Sgroi, 2011). The
5
BREAST CANCER
main strength of the paper is it provides a distinct aspect of two different hypothesis of
underlying the pathophysiology of breast cancer however, fails to what is the probability that
one cancer cell line will follow sporadic clonal evolution model of stem cell model. A genetic
screening further will help to elucidate this topic further.
Basic molecular pathology of breast cancer underlines the concept of generation of
the cancerous differentiation among the cells of the mammary gland, initiated under the
action of the DNA or genetic mutation due to overexposure of estrogen or due to the
inheritance of faulty genes like BRCA1, BRCA2 and P52 (Allison, 2012). The study
undertaken by Allison (2012) employed advanced molecular testing technologies in order to
elucidate the underlying molecular pathology of breast cancer and this is the main strength of
their article and this validating the data further. However, the article failed to highlight the
controls, which are used in the molecular testing techniques.
Molecular pathology of IDC
Ductal Carcinoma (DCIS) is defined as the proliferation of the epithelial cells which
is separated from the breast stroma by an intact layer myoepithelial cells and its basement
membrane. This process is known as intraductal neoplastic proliferation. DCIS is defined as a
non-obligate precursor of IDC. Nearly 40% of the lesions of DCIS progress towards invasive
ductal disease if they are not treated in time. However, at present there are no technologies to
predict which DCIS is more susceptible in developing IDC. The reason behind this is, no
significant drivers of this invasive pathophysiology have been identified (Cowell et al.,
2013). However, the study conducted by Kim et al. (2015) highlighted that synchronous
DCIS and invasive form of breast cancer are significantly similar under qualitative analysis.
This similarity can be explained under the domain of intra-tumour genetic heterogeneity
which is mainly visible under subsets of DCIS. Kim et al. (2015) are of the opinion that the
process of disease progression is the “evolutionary bottleneck” which results in the selection
BREAST CANCER
main strength of the paper is it provides a distinct aspect of two different hypothesis of
underlying the pathophysiology of breast cancer however, fails to what is the probability that
one cancer cell line will follow sporadic clonal evolution model of stem cell model. A genetic
screening further will help to elucidate this topic further.
Basic molecular pathology of breast cancer underlines the concept of generation of
the cancerous differentiation among the cells of the mammary gland, initiated under the
action of the DNA or genetic mutation due to overexposure of estrogen or due to the
inheritance of faulty genes like BRCA1, BRCA2 and P52 (Allison, 2012). The study
undertaken by Allison (2012) employed advanced molecular testing technologies in order to
elucidate the underlying molecular pathology of breast cancer and this is the main strength of
their article and this validating the data further. However, the article failed to highlight the
controls, which are used in the molecular testing techniques.
Molecular pathology of IDC
Ductal Carcinoma (DCIS) is defined as the proliferation of the epithelial cells which
is separated from the breast stroma by an intact layer myoepithelial cells and its basement
membrane. This process is known as intraductal neoplastic proliferation. DCIS is defined as a
non-obligate precursor of IDC. Nearly 40% of the lesions of DCIS progress towards invasive
ductal disease if they are not treated in time. However, at present there are no technologies to
predict which DCIS is more susceptible in developing IDC. The reason behind this is, no
significant drivers of this invasive pathophysiology have been identified (Cowell et al.,
2013). However, the study conducted by Kim et al. (2015) highlighted that synchronous
DCIS and invasive form of breast cancer are significantly similar under qualitative analysis.
This similarity can be explained under the domain of intra-tumour genetic heterogeneity
which is mainly visible under subsets of DCIS. Kim et al. (2015) are of the opinion that the
process of disease progression is the “evolutionary bottleneck” which results in the selection
6
BREAST CANCER
of specific sub-sets of tumour cells with specific epigenetic aberrations. These epigenetic
aberrations are mainly conducted through chromosomal aberrations or through change in the
copy number of the gene leading to invasive disease progression. This change in the copy
number of the gene or the chromosomal aberration as detected by the comparative genomics
hybridization clear states the hypothesis highlighted by the sporadic clonal evolution model
(Cowell et al., 2013). The study conducted by Kim et al. is helpful in providing genomic
difference and difference in the exponential multiplication underlying pure ductal carcinoma
and synchronous carcinoma in-situ in invasive breast cancer but the authors failed to
highlight how the tissues were collected and the nature of the samples used for the collection
of the cancerous tissues.
However, the research conducted by Kreso and Dick (2014) highlighted that main
pathophysiology of the development of the breast cancer is mainly guided by the principle of
the stem cell model. Kreso and Dick (2014) are of the opinion that the mutations, which are
responsible for the promotion of the breast cancer originates from the stem cell at the germ,
line however, these mutations remain dormant and becomes vulnerable towards expression
with age or under the action of certain clonal mutations. The main strength of the study
conducted by Kreso and Dick (2014) is they integrated cancer stem cell approach with cancer
genetic data in order to drive the genetic heterogeneity. Kreso and Dick (2014) provided a
detailed description about the tissue or the cell line use for the study and this is can be defined
as additional strength of their study.
Molecular diagnostic method
Molecular diagnostic test used to screen breast cancer is screening of estrogen (ER)
and progesterone receptors (PR). The presence of hormonal receptor is assessed in the clinic
via the process of ligand binding assay or via immune histo-chemical staining (IHC) of tissue
sections (terHoeve et al., 2017). The immune histochemical staining is defined under the
BREAST CANCER
of specific sub-sets of tumour cells with specific epigenetic aberrations. These epigenetic
aberrations are mainly conducted through chromosomal aberrations or through change in the
copy number of the gene leading to invasive disease progression. This change in the copy
number of the gene or the chromosomal aberration as detected by the comparative genomics
hybridization clear states the hypothesis highlighted by the sporadic clonal evolution model
(Cowell et al., 2013). The study conducted by Kim et al. is helpful in providing genomic
difference and difference in the exponential multiplication underlying pure ductal carcinoma
and synchronous carcinoma in-situ in invasive breast cancer but the authors failed to
highlight how the tissues were collected and the nature of the samples used for the collection
of the cancerous tissues.
However, the research conducted by Kreso and Dick (2014) highlighted that main
pathophysiology of the development of the breast cancer is mainly guided by the principle of
the stem cell model. Kreso and Dick (2014) are of the opinion that the mutations, which are
responsible for the promotion of the breast cancer originates from the stem cell at the germ,
line however, these mutations remain dormant and becomes vulnerable towards expression
with age or under the action of certain clonal mutations. The main strength of the study
conducted by Kreso and Dick (2014) is they integrated cancer stem cell approach with cancer
genetic data in order to drive the genetic heterogeneity. Kreso and Dick (2014) provided a
detailed description about the tissue or the cell line use for the study and this is can be defined
as additional strength of their study.
Molecular diagnostic method
Molecular diagnostic test used to screen breast cancer is screening of estrogen (ER)
and progesterone receptors (PR). The presence of hormonal receptor is assessed in the clinic
via the process of ligand binding assay or via immune histo-chemical staining (IHC) of tissue
sections (terHoeve et al., 2017). The immune histochemical staining is defined under the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
BREAST CANCER
concept of immunohistochemistry (IHC). In immune-histochemistry, fine sections of the
malignant tissues are produced and then hormone markers are used to bind to the prepared set
of tissues. The binding of the markers with the set of hormones (estrogen and progesterone)
helps to determinate the stage and grade of cancer along with the identification of the cell
type.
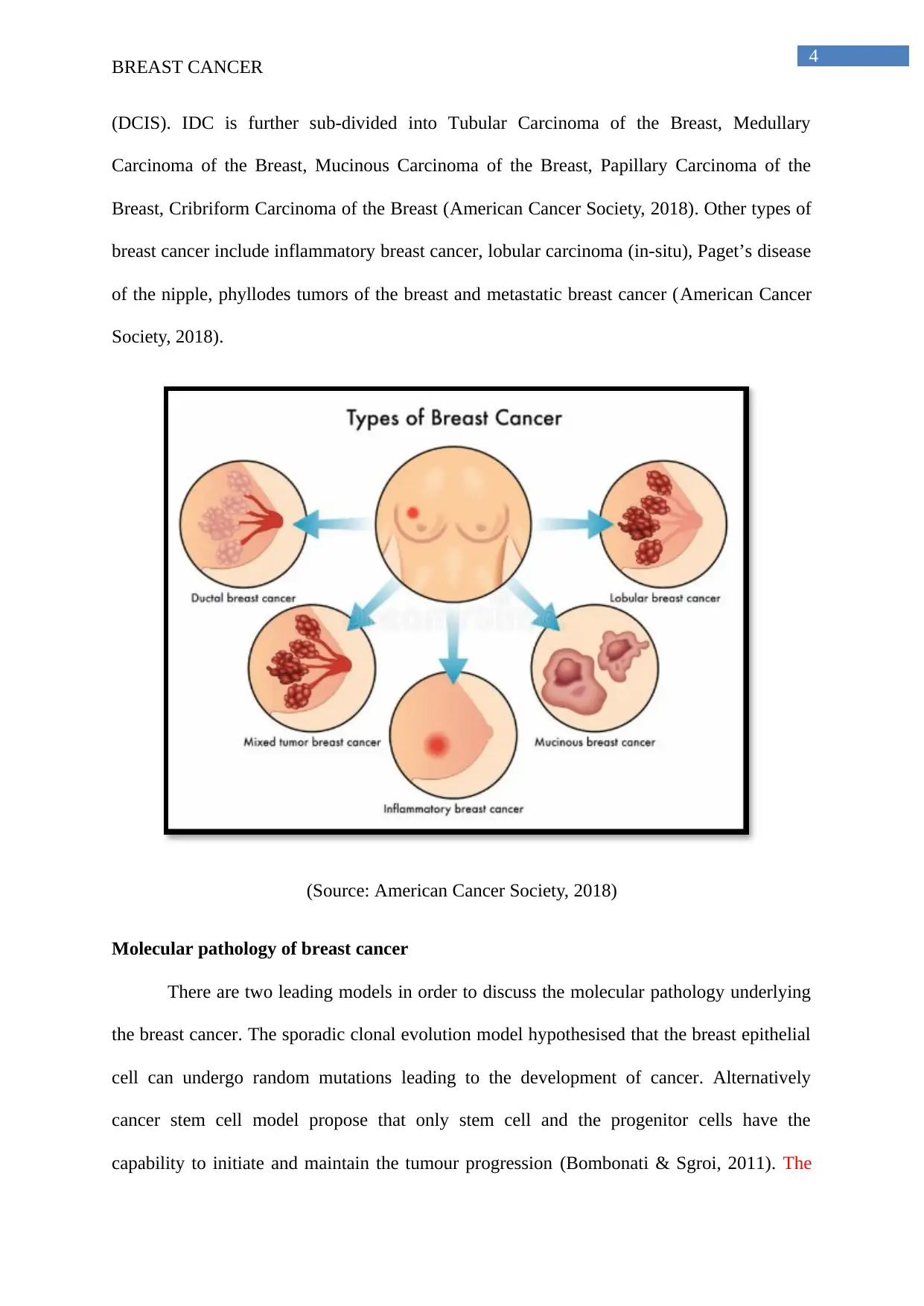
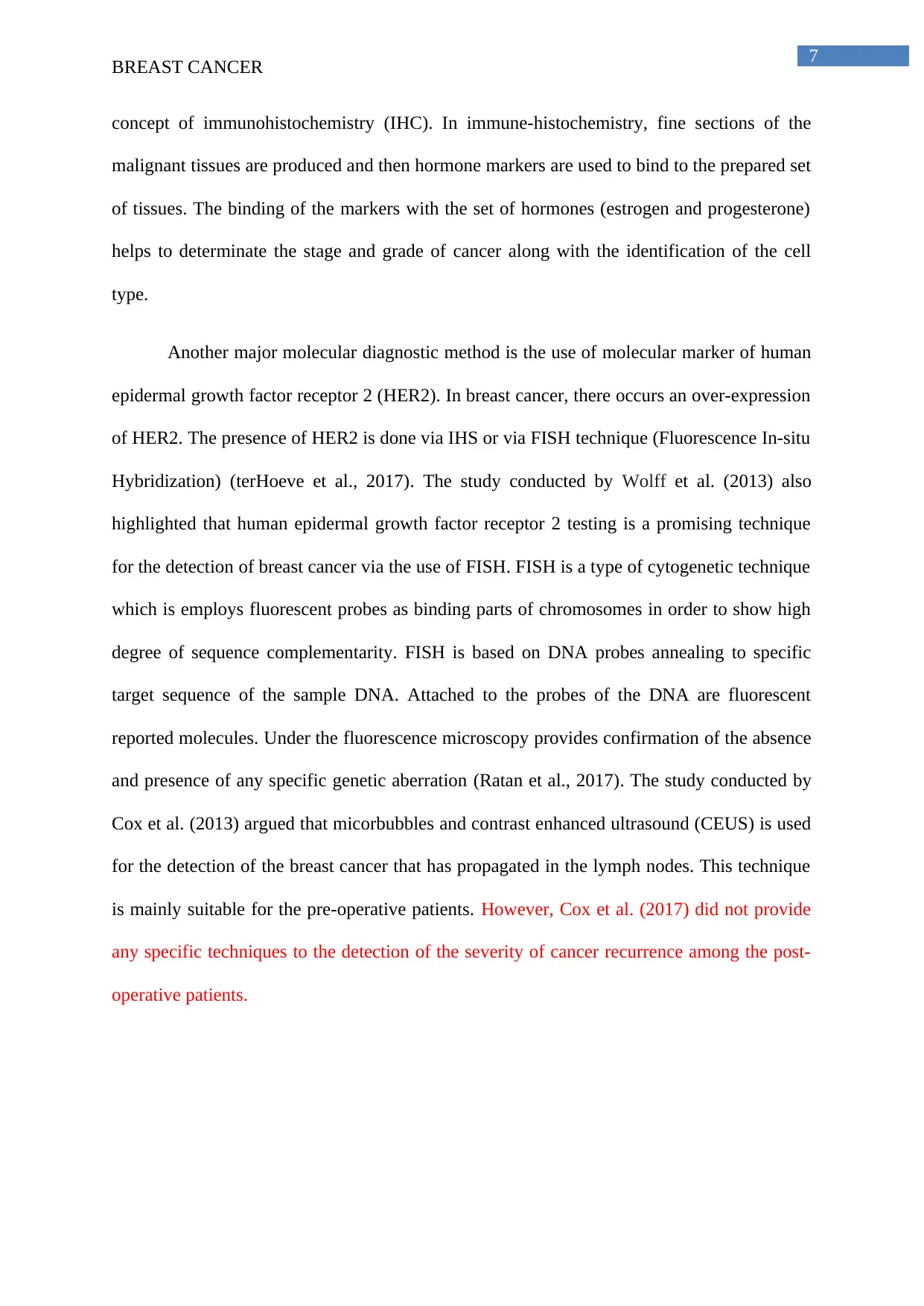
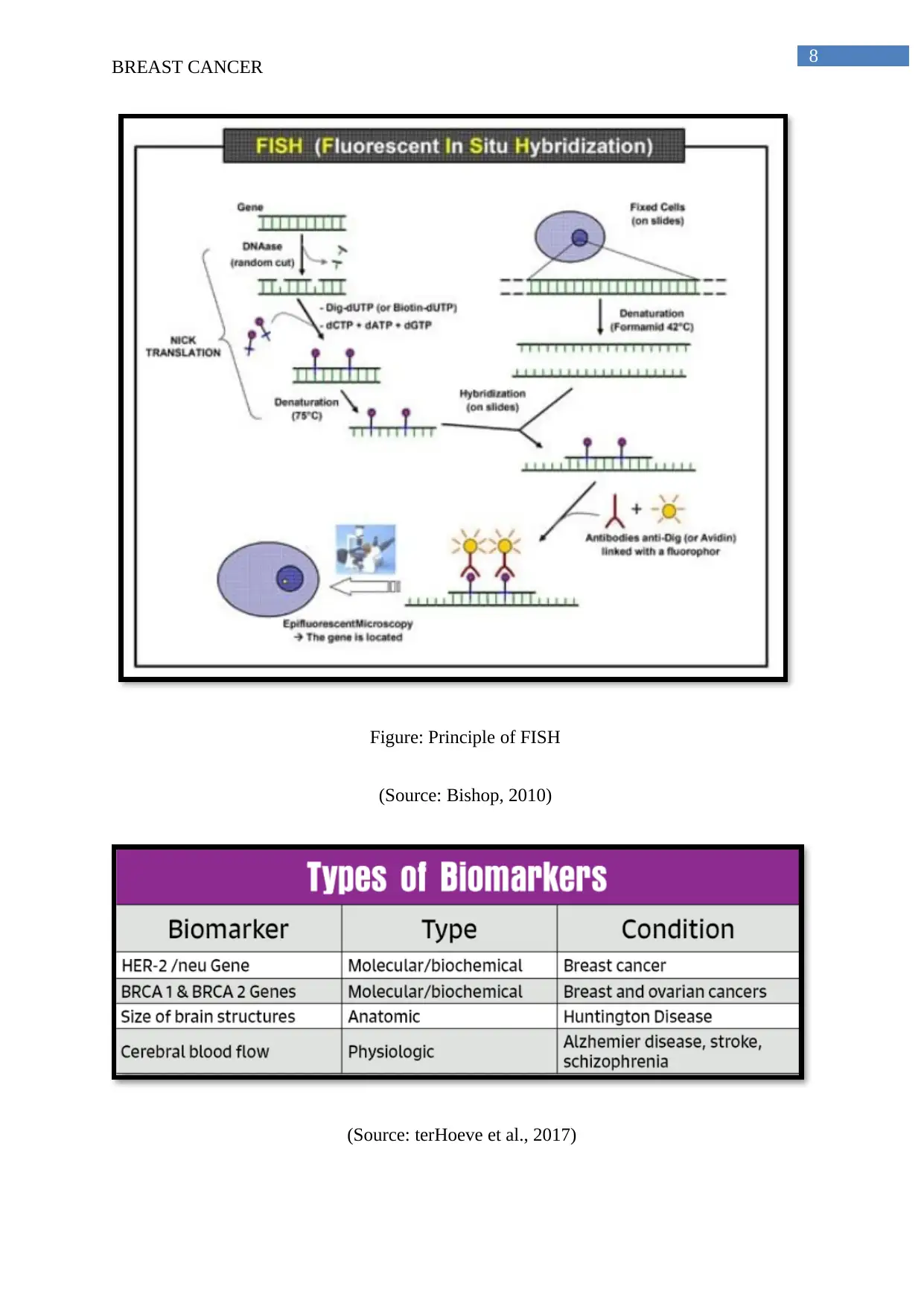
Another major molecular diagnostic method is the use of molecular marker of human
epidermal growth factor receptor 2 (HER2). In breast cancer, there occurs an over-expression
of HER2. The presence of HER2 is done via IHS or via FISH technique (Fluorescence In-situ
Hybridization) (terHoeve et al., 2017). The study conducted by Wolff et al. (2013) also
highlighted that human epidermal growth factor receptor 2 testing is a promising technique
for the detection of breast cancer via the use of FISH. FISH is a type of cytogenetic technique
which is employs fluorescent probes as binding parts of chromosomes in order to show high
degree of sequence complementarity. FISH is based on DNA probes annealing to specific
target sequence of the sample DNA. Attached to the probes of the DNA are fluorescent
reported molecules. Under the fluorescence microscopy provides confirmation of the absence
and presence of any specific genetic aberration (Ratan et al., 2017). The study conducted by
Cox et al. (2013) argued that micorbubbles and contrast enhanced ultrasound (CEUS) is used
for the detection of the breast cancer that has propagated in the lymph nodes. This technique
is mainly suitable for the pre-operative patients. However, Cox et al. (2017) did not provide
any specific techniques to the detection of the severity of cancer recurrence among the post-
operative patients.
BREAST CANCER
concept of immunohistochemistry (IHC). In immune-histochemistry, fine sections of the
malignant tissues are produced and then hormone markers are used to bind to the prepared set
of tissues. The binding of the markers with the set of hormones (estrogen and progesterone)
helps to determinate the stage and grade of cancer along with the identification of the cell
type.
Another major molecular diagnostic method is the use of molecular marker of human
epidermal growth factor receptor 2 (HER2). In breast cancer, there occurs an over-expression
of HER2. The presence of HER2 is done via IHS or via FISH technique (Fluorescence In-situ
Hybridization) (terHoeve et al., 2017). The study conducted by Wolff et al. (2013) also
highlighted that human epidermal growth factor receptor 2 testing is a promising technique
for the detection of breast cancer via the use of FISH. FISH is a type of cytogenetic technique
which is employs fluorescent probes as binding parts of chromosomes in order to show high
degree of sequence complementarity. FISH is based on DNA probes annealing to specific
target sequence of the sample DNA. Attached to the probes of the DNA are fluorescent
reported molecules. Under the fluorescence microscopy provides confirmation of the absence
and presence of any specific genetic aberration (Ratan et al., 2017). The study conducted by
Cox et al. (2013) argued that micorbubbles and contrast enhanced ultrasound (CEUS) is used
for the detection of the breast cancer that has propagated in the lymph nodes. This technique
is mainly suitable for the pre-operative patients. However, Cox et al. (2017) did not provide
any specific techniques to the detection of the severity of cancer recurrence among the post-
operative patients.
8
BREAST CANCER
Figure: Principle of FISH
(Source: Bishop, 2010)
(Source: terHoeve et al., 2017)
BREAST CANCER
Figure: Principle of FISH
(Source: Bishop, 2010)
(Source: terHoeve et al., 2017)
9
BREAST CANCER
Prognosis
The prognosis of breast cancer depends on the type of breast cancer, the grade or the
stage of breast cancer, the size of tumour, the status of the lymph node of the breast cancer,
the overall status of the ER and HER2 (Assi et al., 2013). Stage is the first prognosis factor
underlying breast cancer. According to Assi et al. (2013), there is comparatively lesser risk
that early stage breast cancer will return back thus it has more favourable prognosis. The
diagnosis of the breast cancer at later stages of life has higher risk of recurrence and thus
have less favourable prognosis. Mainly the side of lymph nodes and the size of tumour are
considered while analysing the prognosis of the breast cancer. If the breast cancer has
propagated in the lymph nodes then there is higher risk of recurrence and this signifies less
chances of prognosis. The second important prognosis factor is the size of the tumour. The
tumours of the breast which are larger than 5 cm are more likely to come back and thus less
favourable prognosis. The grade of the tumour is also considered while determining the
prognosis of breast cancer. Low-grade tumours are less likely to spread throughout the tissues
and thus have better prognosis than high-grade tumour. The hormone receptor-positive
tumours mainly have good prognosis as they are less aggressive. The presence of the HER2
gene also alters the prognosis of breast cancer. HER2-positive breast cancer signifies that the
cancer cells make too many copies or has higher risk of over-expression and thus decreasing
the overall prognosis. The age of the individual also affects the prognosis of the breast
cancer. Women who are younger than 35 years of age are more likely to get diagnosed with
aggressive breast cancer with high grade tumours. This breast cancers are mainly advanced
grade cancer at the time of diagnosis and are more likely to re-occur and thus has less rate of
prognosis in comparison to the post menopausal women who more than 35 years of age (Assi
et al., 2013). However, contrasting results were highlighted in the study conducted by Hughes
et al. (2013), the authors here are of the opinion that severity of the detection of breast-cancer
BREAST CANCER
Prognosis
The prognosis of breast cancer depends on the type of breast cancer, the grade or the
stage of breast cancer, the size of tumour, the status of the lymph node of the breast cancer,
the overall status of the ER and HER2 (Assi et al., 2013). Stage is the first prognosis factor
underlying breast cancer. According to Assi et al. (2013), there is comparatively lesser risk
that early stage breast cancer will return back thus it has more favourable prognosis. The
diagnosis of the breast cancer at later stages of life has higher risk of recurrence and thus
have less favourable prognosis. Mainly the side of lymph nodes and the size of tumour are
considered while analysing the prognosis of the breast cancer. If the breast cancer has
propagated in the lymph nodes then there is higher risk of recurrence and this signifies less
chances of prognosis. The second important prognosis factor is the size of the tumour. The
tumours of the breast which are larger than 5 cm are more likely to come back and thus less
favourable prognosis. The grade of the tumour is also considered while determining the
prognosis of breast cancer. Low-grade tumours are less likely to spread throughout the tissues
and thus have better prognosis than high-grade tumour. The hormone receptor-positive
tumours mainly have good prognosis as they are less aggressive. The presence of the HER2
gene also alters the prognosis of breast cancer. HER2-positive breast cancer signifies that the
cancer cells make too many copies or has higher risk of over-expression and thus decreasing
the overall prognosis. The age of the individual also affects the prognosis of the breast
cancer. Women who are younger than 35 years of age are more likely to get diagnosed with
aggressive breast cancer with high grade tumours. This breast cancers are mainly advanced
grade cancer at the time of diagnosis and are more likely to re-occur and thus has less rate of
prognosis in comparison to the post menopausal women who more than 35 years of age (Assi
et al., 2013). However, contrasting results were highlighted in the study conducted by Hughes
et al. (2013), the authors here are of the opinion that severity of the detection of breast-cancer
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10
BREAST CANCER
is also higher among the women who are 70 years old. Successful lumpectomy and periodic
application of tamoxifen at times failed to reduce the vulnerability of recurrence.
Treatment
The treatment of breast cancer is mainly based on hormonal therapy and
chemotherapy. Hormonal therapy for breast cancer is mainly used after surgery as a form of
adjuvant therapy. Hormonal therapy helps to reduce the overall risk recurrence of the disease.
At times, the hormonal therapy is initiated before surgery in the form of neo-adjuvant therapy
and is usually continued for 5 years (Burstein, Lacchetti & Griggs, 2016). According to
Burstein, Lacchetti and Griggs (2016), 2 out of 3 breast cancers are hormone receptor-
positive. Hormone receptor-positive cells have receptor proteins that bind to the hormones
estrogen or hormone progesterone. Binding with the hormones helps the cancerous cell to
grow fast. So in hormone therapy, the hormonal receptors of the cancerous cells are blocked
and thereby preventing the cancerous cell from growing. In the majority of the hormonal
therapy for the breast cancer, estrogen binding receptors are used. The main drugs which are
used for the hormonal therapy of the breast cancer include Tamoxifen. Tamoxifen mainly
blocks the estrogen receptor present on the breast cancer cells. This in turn prevents estrogen
from connecting to the cancer cell and thereby preventing them to divide and grow.
Toremifene or Fareston also works in similar way like Tamoxifen but is used less often and is
only used for the treatment for metastatic breast cancer. There drugs are mainly taken orally
and are also associated with side-effects like hot flashes, vaginal dryness or discharge and
mood swing (Burstein, Lacchetti & Griggs, 2016). The main strength of the study conducted
by Burstein, Lacchetti and Griggs (2016) is structure of the study. The authors opted for
systematic review of the randomized control trials. However, they only selected two articles
for the review this might be regarded as one of the drawback of the study.
BREAST CANCER
is also higher among the women who are 70 years old. Successful lumpectomy and periodic
application of tamoxifen at times failed to reduce the vulnerability of recurrence.
Treatment
The treatment of breast cancer is mainly based on hormonal therapy and
chemotherapy. Hormonal therapy for breast cancer is mainly used after surgery as a form of
adjuvant therapy. Hormonal therapy helps to reduce the overall risk recurrence of the disease.
At times, the hormonal therapy is initiated before surgery in the form of neo-adjuvant therapy
and is usually continued for 5 years (Burstein, Lacchetti & Griggs, 2016). According to
Burstein, Lacchetti and Griggs (2016), 2 out of 3 breast cancers are hormone receptor-
positive. Hormone receptor-positive cells have receptor proteins that bind to the hormones
estrogen or hormone progesterone. Binding with the hormones helps the cancerous cell to
grow fast. So in hormone therapy, the hormonal receptors of the cancerous cells are blocked
and thereby preventing the cancerous cell from growing. In the majority of the hormonal
therapy for the breast cancer, estrogen binding receptors are used. The main drugs which are
used for the hormonal therapy of the breast cancer include Tamoxifen. Tamoxifen mainly
blocks the estrogen receptor present on the breast cancer cells. This in turn prevents estrogen
from connecting to the cancer cell and thereby preventing them to divide and grow.
Toremifene or Fareston also works in similar way like Tamoxifen but is used less often and is
only used for the treatment for metastatic breast cancer. There drugs are mainly taken orally
and are also associated with side-effects like hot flashes, vaginal dryness or discharge and
mood swing (Burstein, Lacchetti & Griggs, 2016). The main strength of the study conducted
by Burstein, Lacchetti and Griggs (2016) is structure of the study. The authors opted for
systematic review of the randomized control trials. However, they only selected two articles
for the review this might be regarded as one of the drawback of the study.
11
BREAST CANCER
Recently the researchers are planning to target the PI3K/AKT/mTOR and
Raf/MEK/ERK pathways for the treatment of breast cancer (Saini et al., 2013). The targets of
these pathways are most done by the chemotherapeutic drugs which will act as an antagonist
to one of the components of the pathway. This hampers the downstream signalling of the
pathway and thereby causing cessation of the pathway and its effect on the malignant
proliferation of the breast cancer tissue (Saini et al., 2013).
Future of molecular diagnostic in the cancer
The future molecular diagnosis of breast cancer is mainly based on the designing of
the biomarkers for the effective detection of the stage and the type of breast cancer. The
prognostic biomarkers will selectively aim to identify the somatic germ line mutations, level
of DNA methylation and the levels of micro RNA and circulating tumour cells in breast
cancer (Kalia, 2015). Use of the biomarkers for the detection of the somatic germ line
mutations will help in the generation of the personalised medicines. According to Kalia
(2015) personalised medicine is an emerging practice of medicine that employs the genetic
profile of an individual for disease treatment. However, study conducted by Kalia has sudden
limitations like it mainly used to identified somatic cell mutations and not the germ-line
mutations. The study conducted by Piva, Spandidos and Gambari (2013) highlighted that
microRNA functions and microRNA therapeutics are now used to design novel drug targets
for breast cancer treatment. The main strength of their study is, the authors utilised the
expression profile of oncogenic miRNAs and tumor suppressor miRNAs and this helped
them to obtain case specific data.
Conclusion
Thus from the above discussion, it can be concluded that breast cancer is a complex
disease with several different variation in the disease occurrence and requires thorough
BREAST CANCER
Recently the researchers are planning to target the PI3K/AKT/mTOR and
Raf/MEK/ERK pathways for the treatment of breast cancer (Saini et al., 2013). The targets of
these pathways are most done by the chemotherapeutic drugs which will act as an antagonist
to one of the components of the pathway. This hampers the downstream signalling of the
pathway and thereby causing cessation of the pathway and its effect on the malignant
proliferation of the breast cancer tissue (Saini et al., 2013).
Future of molecular diagnostic in the cancer
The future molecular diagnosis of breast cancer is mainly based on the designing of
the biomarkers for the effective detection of the stage and the type of breast cancer. The
prognostic biomarkers will selectively aim to identify the somatic germ line mutations, level
of DNA methylation and the levels of micro RNA and circulating tumour cells in breast
cancer (Kalia, 2015). Use of the biomarkers for the detection of the somatic germ line
mutations will help in the generation of the personalised medicines. According to Kalia
(2015) personalised medicine is an emerging practice of medicine that employs the genetic
profile of an individual for disease treatment. However, study conducted by Kalia has sudden
limitations like it mainly used to identified somatic cell mutations and not the germ-line
mutations. The study conducted by Piva, Spandidos and Gambari (2013) highlighted that
microRNA functions and microRNA therapeutics are now used to design novel drug targets
for breast cancer treatment. The main strength of their study is, the authors utilised the
expression profile of oncogenic miRNAs and tumor suppressor miRNAs and this helped
them to obtain case specific data.
Conclusion
Thus from the above discussion, it can be concluded that breast cancer is a complex
disease with several different variation in the disease occurrence and requires thorough

12
BREAST CANCER
treatment along with regular monitoring for better health outcomes. Some of the common and
widely known breast-cancers include invasive ductal carcinoma, invasive lobular carcinoma
and ductal carcinoma in-situ. The underlying pathology of breast cancer is mainly guided by
the two different hypotheses. One hypothesis is guided by sporadic clonal evolution model
and another hypothesis is guided by the cancer stem cell model. The popular molecular
diagnostic approaches which are used for the detection of breast cancer include immuno-
histochemical techniques, fluorescence in-situ hybridization and ligand binding assays for the
detection of human epidermal growth factor. Early detection of the breast cancer promotes
quality prognosis along with providing the basis of the thorough therapy plan. The treatment
of breast cancer mainly includes surgery and hormonal therapy. Future molecular diagnostic
methods are mainly targeting the use of biomarkers for devising personalised medicines.
BREAST CANCER
treatment along with regular monitoring for better health outcomes. Some of the common and
widely known breast-cancers include invasive ductal carcinoma, invasive lobular carcinoma
and ductal carcinoma in-situ. The underlying pathology of breast cancer is mainly guided by
the two different hypotheses. One hypothesis is guided by sporadic clonal evolution model
and another hypothesis is guided by the cancer stem cell model. The popular molecular
diagnostic approaches which are used for the detection of breast cancer include immuno-
histochemical techniques, fluorescence in-situ hybridization and ligand binding assays for the
detection of human epidermal growth factor. Early detection of the breast cancer promotes
quality prognosis along with providing the basis of the thorough therapy plan. The treatment
of breast cancer mainly includes surgery and hormonal therapy. Future molecular diagnostic
methods are mainly targeting the use of biomarkers for devising personalised medicines.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
13
BREAST CANCER
References
Alexandrov, L. B., Nik-Zainal, S., Wedge, D. C., Aparicio, S. A., Behjati, S., Biankin, A.
V., ... & Boyault, S. (2013). Signatures of mutational processes in human
cancer. Nature, 500(7463), 415.
Allison, K. H. (2012). Molecular pathology of breast cancer: what a pathologist needs to
know. American journal of clinical pathology, 138(6), 770-780.
American Cancer Society.(2018).Types of Breast Cancer.Access date: 12th July 2018.
Retrieved from: https://www.cancer.org/cancer/breast-cancer/understanding-a-breast-
cancer-diagnosis/types-of-breast-cancer.html
Assi, H. A., Khoury, K. E., Dbouk, H., Khalil, L. E., Mouhieddine, T. H., & El Saghir, N. S.,
(2013). Epidemiology and prognosis of breast cancer in young women. Journal of
thoracic disease, 5(Suppl 1), S2.
Bishop, R. (2010). Applications of fluorescence in situ hybridization (FISH) in detecting
genetic aberrations of medical significance. Bioscience Horizons, 3(1), 85-95.
Bombonati, A. &Sgroi, D.C., (2011).The molecular pathology of breast cancer
progression. The Journal of pathology, 223(2), pp.308-318.
Buchsbaum, R. J., & Oh, S. Y. (2016). Breast cancer-associated fibroblasts: where we are and
where we need to go. Cancers, 8(2), 19.
Burstein, H. J., Lacchetti, C., & Griggs, J. J. (2016). Adjuvant Endocrine Therapy for Women
With Hormone Receptor–Positive Breast Cancer: American Society of Clinical
Oncology Clinical Practice Guideline Update on Ovarian Suppression
Summary. Journal of oncology practice, 12(4), 390-393.
BREAST CANCER
References
Alexandrov, L. B., Nik-Zainal, S., Wedge, D. C., Aparicio, S. A., Behjati, S., Biankin, A.
V., ... & Boyault, S. (2013). Signatures of mutational processes in human
cancer. Nature, 500(7463), 415.
Allison, K. H. (2012). Molecular pathology of breast cancer: what a pathologist needs to
know. American journal of clinical pathology, 138(6), 770-780.
American Cancer Society.(2018).Types of Breast Cancer.Access date: 12th July 2018.
Retrieved from: https://www.cancer.org/cancer/breast-cancer/understanding-a-breast-
cancer-diagnosis/types-of-breast-cancer.html
Assi, H. A., Khoury, K. E., Dbouk, H., Khalil, L. E., Mouhieddine, T. H., & El Saghir, N. S.,
(2013). Epidemiology and prognosis of breast cancer in young women. Journal of
thoracic disease, 5(Suppl 1), S2.
Bishop, R. (2010). Applications of fluorescence in situ hybridization (FISH) in detecting
genetic aberrations of medical significance. Bioscience Horizons, 3(1), 85-95.
Bombonati, A. &Sgroi, D.C., (2011).The molecular pathology of breast cancer
progression. The Journal of pathology, 223(2), pp.308-318.
Buchsbaum, R. J., & Oh, S. Y. (2016). Breast cancer-associated fibroblasts: where we are and
where we need to go. Cancers, 8(2), 19.
Burstein, H. J., Lacchetti, C., & Griggs, J. J. (2016). Adjuvant Endocrine Therapy for Women
With Hormone Receptor–Positive Breast Cancer: American Society of Clinical
Oncology Clinical Practice Guideline Update on Ovarian Suppression
Summary. Journal of oncology practice, 12(4), 390-393.
14
BREAST CANCER
Cowell, C. F., Weigelt, B., Sakr, R. A., Ng, C. K., Hicks, J., King, T. A., & Reis-Filho, J. S.
(2013). Progression from ductal carcinoma in situ to invasive breast cancer:
revisited. Molecular oncology, 7(5), 859-869.
Cox, K., Sever, A., Jones, S., Weeks, J., Mills, P., Devalia, H., ... & Jones, P. (2013).
Validation of a technique using microbubbles and contrast enhanced ultrasound
(CEUS) to biopsy sentinel lymph nodes (SLN) in pre-operative breast cancer patients
with a normal grey-scale axillary ultrasound. European Journal of Surgical Oncology
(EJSO), 39(7), 760-765.
DeSantis, C., Ma, J., Bryan, L., & Jemal, A. (2014). Breast cancer statistics, 2013. CA: a
cancer journal for clinicians, 64(1), 52-62.
Goldhirsch, A., Winer, E. P., Coates, A. S., Gelber, R. D., Piccart-Gebhart, M., Thürlimann,
B., ... & Bergh, J. (2013). Personalizing the treatment of women with early breast
cancer: highlights of the St Gallen International Expert Consensus on the Primary
Therapy of Early Breast Cancer 2013. Annals of oncology, 24(9), 2206-2223.
Hughes, K. S., Schnaper, L. A., Bellon, J. R., Cirrincione, C. T., Berry, D. A., McCormick,
B., ... & Wood, W. C. (2013). Lumpectomy plus tamoxifen with or without irradiation
in women age 70 years or older with early breast cancer: long-term follow-up of
CALGB 9343. Journal of Clinical Oncology, 31(19), 2382.
Jafari-Koshki, T., Schmid, V. J., & Mahaki, B. (2014). Trends of breast cancer incidence in
Iran during 2004-2008: a Bayesian space-time model. Asian Pac J Cancer
Prev, 15(4), 1557-61.
Kalia, M., (2015).Biomarkers for personalized oncology: recent advances and future
challenges. Metabolism, 64(3), S16-S21.
BREAST CANCER
Cowell, C. F., Weigelt, B., Sakr, R. A., Ng, C. K., Hicks, J., King, T. A., & Reis-Filho, J. S.
(2013). Progression from ductal carcinoma in situ to invasive breast cancer:
revisited. Molecular oncology, 7(5), 859-869.
Cox, K., Sever, A., Jones, S., Weeks, J., Mills, P., Devalia, H., ... & Jones, P. (2013).
Validation of a technique using microbubbles and contrast enhanced ultrasound
(CEUS) to biopsy sentinel lymph nodes (SLN) in pre-operative breast cancer patients
with a normal grey-scale axillary ultrasound. European Journal of Surgical Oncology
(EJSO), 39(7), 760-765.
DeSantis, C., Ma, J., Bryan, L., & Jemal, A. (2014). Breast cancer statistics, 2013. CA: a
cancer journal for clinicians, 64(1), 52-62.
Goldhirsch, A., Winer, E. P., Coates, A. S., Gelber, R. D., Piccart-Gebhart, M., Thürlimann,
B., ... & Bergh, J. (2013). Personalizing the treatment of women with early breast
cancer: highlights of the St Gallen International Expert Consensus on the Primary
Therapy of Early Breast Cancer 2013. Annals of oncology, 24(9), 2206-2223.
Hughes, K. S., Schnaper, L. A., Bellon, J. R., Cirrincione, C. T., Berry, D. A., McCormick,
B., ... & Wood, W. C. (2013). Lumpectomy plus tamoxifen with or without irradiation
in women age 70 years or older with early breast cancer: long-term follow-up of
CALGB 9343. Journal of Clinical Oncology, 31(19), 2382.
Jafari-Koshki, T., Schmid, V. J., & Mahaki, B. (2014). Trends of breast cancer incidence in
Iran during 2004-2008: a Bayesian space-time model. Asian Pac J Cancer
Prev, 15(4), 1557-61.
Kalia, M., (2015).Biomarkers for personalized oncology: recent advances and future
challenges. Metabolism, 64(3), S16-S21.
15
BREAST CANCER
Khamis, Z. I., Sahab, Z. J., & Sang, Q. X. A. (2012). Active roles of tumor stroma in breast
cancer metastasis. International journal of breast cancer, 2012.
Kim, S. Y., Jung, S. H., Kim, M. S., Baek, I. P., Lee, S. H., Kim, T. M., ... & Lee, S. H.
(2015). Genomic differences between pure ductal carcinoma in situ and synchronous
ductal carcinoma in situ with invasive breast cancer. Oncotarget, 6(10), 7597.
Kreso, A., & Dick, J. E. (2014). Evolution of the cancer stem cell model. Cell stem
cell, 14(3), 275-291.
Piva, R., Spandidos, D. A., & Gambari, R. (2013). From microRNA functions to microRNA
therapeutics: novel targets and novel drugs in breast cancer research and
treatment. International journal of oncology, 43(4), 985-994.
Ratan, Z. A., Zaman, S. B., Mehta, V., Haidere, M. F., Runa, N. J., & Akter, N. (2017).
Application of Fluorescence in situ Hybridization (FISH) technique for the detection
of genetic aberration in medical science. Cureus, 9(6).
Saini, K. S., Loi, S., de Azambuja, E., Metzger-Filho, O., Saini, M. L., Ignatiadis,
M., ...&Piccart-Gebhart, M. J. (2013). Targeting the PI3K/AKT/mTOR and
Raf/MEK/ERK pathways in the treatment of breast cancer. Cancer treatment
reviews, 39(8), 935-946.
Stephens, P. J., Tarpey, P. S., Davies, H., Van Loo, P., Greenman, C., Wedge, D. C., ... &
Yates, L. R. (2012). The landscape of cancer genes and mutational processes in breast
cancer. Nature, 486(7403), 400.
terHoeve, N.D., Moelans, C.B., Schrijver, W.A., de Leng, W. & van Diest, P.J., (2017).
Molecular diagnostics in breast cancer routine practice. European Oncology and
Haematology, 13(1), pp.74-79.
BREAST CANCER
Khamis, Z. I., Sahab, Z. J., & Sang, Q. X. A. (2012). Active roles of tumor stroma in breast
cancer metastasis. International journal of breast cancer, 2012.
Kim, S. Y., Jung, S. H., Kim, M. S., Baek, I. P., Lee, S. H., Kim, T. M., ... & Lee, S. H.
(2015). Genomic differences between pure ductal carcinoma in situ and synchronous
ductal carcinoma in situ with invasive breast cancer. Oncotarget, 6(10), 7597.
Kreso, A., & Dick, J. E. (2014). Evolution of the cancer stem cell model. Cell stem
cell, 14(3), 275-291.
Piva, R., Spandidos, D. A., & Gambari, R. (2013). From microRNA functions to microRNA
therapeutics: novel targets and novel drugs in breast cancer research and
treatment. International journal of oncology, 43(4), 985-994.
Ratan, Z. A., Zaman, S. B., Mehta, V., Haidere, M. F., Runa, N. J., & Akter, N. (2017).
Application of Fluorescence in situ Hybridization (FISH) technique for the detection
of genetic aberration in medical science. Cureus, 9(6).
Saini, K. S., Loi, S., de Azambuja, E., Metzger-Filho, O., Saini, M. L., Ignatiadis,
M., ...&Piccart-Gebhart, M. J. (2013). Targeting the PI3K/AKT/mTOR and
Raf/MEK/ERK pathways in the treatment of breast cancer. Cancer treatment
reviews, 39(8), 935-946.
Stephens, P. J., Tarpey, P. S., Davies, H., Van Loo, P., Greenman, C., Wedge, D. C., ... &
Yates, L. R. (2012). The landscape of cancer genes and mutational processes in breast
cancer. Nature, 486(7403), 400.
terHoeve, N.D., Moelans, C.B., Schrijver, W.A., de Leng, W. & van Diest, P.J., (2017).
Molecular diagnostics in breast cancer routine practice. European Oncology and
Haematology, 13(1), pp.74-79.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
16
BREAST CANCER
Wolff, A. C., Hammond, M. E. H., Hicks, D. G., Dowsett, M., McShane, L. M., Allison, K.
H., ... & Hanna, W. (2013). Recommendations for human epidermal growth factor
receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of
American Pathologists clinical practice guideline update. Archives of Pathology and
Laboratory Medicine, 138(2), 241-256.
BREAST CANCER
Wolff, A. C., Hammond, M. E. H., Hicks, D. G., Dowsett, M., McShane, L. M., Allison, K.
H., ... & Hanna, W. (2013). Recommendations for human epidermal growth factor
receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of
American Pathologists clinical practice guideline update. Archives of Pathology and
Laboratory Medicine, 138(2), 241-256.
1 out of 17
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.




