Psychology Case Study: Analyzing Eliza's Anxiety and Treatment Plan
VerifiedAdded on 2020/07/22
|11
|2458
|48
Case Study
AI Summary
This case study examines Eliza, a 25-year-old woman experiencing anxiety, referred for outpatient psychological services. The case study details her background, reason for referral, and a comprehensive assessment using both standardized and non-standardized tools, including interviews with Eliza and her husband. The assessment identifies factors contributing to her anxiety, such as interpersonal stressors and a history of childhood trauma. The planned intervention focuses on Cognitive Behavioral Therapy (CBT), including problem-solving training, cognitive restructuring, and relaxation techniques, aimed at modifying her thoughts, feelings, and behaviors. The intervention plan involves psychoeducation, CBT sessions, and relapse prevention strategies. The study evaluates the intervention's effectiveness through pre and post-treatment assessments, demonstrating a reduction in anxiety scores. Challenges encountered during implementation and the role of motivation in treatment adherence are also discussed. References to relevant literature are provided.
MOTIVATION AND
EMOTION
EMOTION
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Table of Contents
Background history......................................................................................................................1
Reason for referral.......................................................................................................................1
Assessment...................................................................................................................................1
Planned intervention....................................................................................................................2
Implementation and evaluation....................................................................................................4
REFERENCES................................................................................................................................5
Background history......................................................................................................................1
Reason for referral.......................................................................................................................1
Assessment...................................................................................................................................1
Planned intervention....................................................................................................................2
Implementation and evaluation....................................................................................................4
REFERENCES................................................................................................................................5
Background history
Eliza was 25 year old women and referred for outpatient psychological services. She
belongs to upper class and got married last year. Since from her teenage she had feeling tense
and worried. Along with this she described her symptom that her heart started shaken with
overwhelming worry about threatening event without any specific reason.
Reason for referral
Eliza was referred to outpatient psychological services and try to find out reason for her change
in behaviour and reason of getting tense. It was felt that cognitive behaviour therapy
interventions would assist aid her recovery.
Assessment
Aims of case study are as follows.
To encourage you to self-reflect upon the motivations behind your own behaviors.
To allow you to research and explore evidence-based methods for modifying a motivated
behavior.
To introduce you to the basic process clinicians work through when attempting to
understand and alter a motivated behavior
Eliza's cognitive behavior therapy assessment was undertaken with the use of different
standardized and non standardized tools. In formal assessment it includes interview with both
Eliza and her husband. Eliza started suffering from this behavioral problem since from her
teenage. Her condition was basically got chronic and mild and it becomes worse at the time
when she encounters from interpersonal stressor. She suffers from this problem because her
father died when she was at childhood stage and sign of anxiety started reflecting in her from the
age of adolescent. Therefore, when she got married her worry of losing her husband and children
increases. This lead to motivate her in changing her behavior (Jauhar and et.al., 2014).
In assessment the following points are identified:-
Eliza tense and worrying has significant impact of distress in her and her family. She gets
worried easily and frequently day to day. Specifically, at the time when she was slightly delayed
in returning home. One of the main reasons for her worrying thought is due to belief and image
1
Eliza was 25 year old women and referred for outpatient psychological services. She
belongs to upper class and got married last year. Since from her teenage she had feeling tense
and worried. Along with this she described her symptom that her heart started shaken with
overwhelming worry about threatening event without any specific reason.
Reason for referral
Eliza was referred to outpatient psychological services and try to find out reason for her change
in behaviour and reason of getting tense. It was felt that cognitive behaviour therapy
interventions would assist aid her recovery.
Assessment
Aims of case study are as follows.
To encourage you to self-reflect upon the motivations behind your own behaviors.
To allow you to research and explore evidence-based methods for modifying a motivated
behavior.
To introduce you to the basic process clinicians work through when attempting to
understand and alter a motivated behavior
Eliza's cognitive behavior therapy assessment was undertaken with the use of different
standardized and non standardized tools. In formal assessment it includes interview with both
Eliza and her husband. Eliza started suffering from this behavioral problem since from her
teenage. Her condition was basically got chronic and mild and it becomes worse at the time
when she encounters from interpersonal stressor. She suffers from this problem because her
father died when she was at childhood stage and sign of anxiety started reflecting in her from the
age of adolescent. Therefore, when she got married her worry of losing her husband and children
increases. This lead to motivate her in changing her behavior (Jauhar and et.al., 2014).
In assessment the following points are identified:-
Eliza tense and worrying has significant impact of distress in her and her family. She gets
worried easily and frequently day to day. Specifically, at the time when she was slightly delayed
in returning home. One of the main reasons for her worrying thought is due to belief and image
1
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
about her family and herself. It also occurs in certain situation such as Eliza get aggressive at the
time of dealing with stressful situation and get excessively conscientious. Her behavior change
because of her family member and she gets stressed at the time when her family members not
around. It frequently occurs at the time of carrying out daily working activity.
There are some factors due to which she emerged from the characteristic of worrying that
is a source of motivation, a positive personality traits, a way of preventing negative outcomes
and an aid to problem solving (Tarrier and Johnson, 2015). At the time when she gets highly
anxious her face became pale and her hands became cold. After performing such behavior her
family member get worried and unable to control her. Source of motivation for getting worried is
insecurity when she feels after staying far from home for longer time. Further self esteem worry
and future worry motivates her in changing her behavior. Worrying about future continue
reinforcing lead to create problem for
Eliza behavior get motivate at the time when she was unable to express her feeling in
front of her family members. Further she continuously thinks about her and her family future
which motivates her to work. Due to this behavior she felt difficulty in sleeping and awoke after
two to three hours. In intervention it is important to motivate Eliza so that she can overcome
from this problem (Andersson and et.al., 2014). Here in intervention cognitive behavioural
theories is applied because this theory suggest that anxiety disorder from which Eliza is suffering
is associated with distorted perception of danger related information. Eliza have lots of image of
fear in her mind which make her tense and worry and due to this reason she was unable to cope
up with her day to day activity leads to bring change in behavior.
Planned intervention
Intervention is the program or strategy that aims at changing the particular problematic
behavior of an individual. Thus, it is usually undertaken to address the behavioral problem of the
person so as to bring desired changes. Evidencing from the research of Khodarahimi and Pole,
(2010), it is stated that single baseline is the best way to evaluate changes in an individual
behavior. It is because, in this technique, clinicians use both baseline measures and results after
the intervention carried out so as to make comparative analysis. If after the treatment, significant
results found in individual behavior than it simply means that planned intervention is extremely
effective to bring change in particular problematic behavior. In this research, researcher also took
2
time of dealing with stressful situation and get excessively conscientious. Her behavior change
because of her family member and she gets stressed at the time when her family members not
around. It frequently occurs at the time of carrying out daily working activity.
There are some factors due to which she emerged from the characteristic of worrying that
is a source of motivation, a positive personality traits, a way of preventing negative outcomes
and an aid to problem solving (Tarrier and Johnson, 2015). At the time when she gets highly
anxious her face became pale and her hands became cold. After performing such behavior her
family member get worried and unable to control her. Source of motivation for getting worried is
insecurity when she feels after staying far from home for longer time. Further self esteem worry
and future worry motivates her in changing her behavior. Worrying about future continue
reinforcing lead to create problem for
Eliza behavior get motivate at the time when she was unable to express her feeling in
front of her family members. Further she continuously thinks about her and her family future
which motivates her to work. Due to this behavior she felt difficulty in sleeping and awoke after
two to three hours. In intervention it is important to motivate Eliza so that she can overcome
from this problem (Andersson and et.al., 2014). Here in intervention cognitive behavioural
theories is applied because this theory suggest that anxiety disorder from which Eliza is suffering
is associated with distorted perception of danger related information. Eliza have lots of image of
fear in her mind which make her tense and worry and due to this reason she was unable to cope
up with her day to day activity leads to bring change in behavior.
Planned intervention
Intervention is the program or strategy that aims at changing the particular problematic
behavior of an individual. Thus, it is usually undertaken to address the behavioral problem of the
person so as to bring desired changes. Evidencing from the research of Khodarahimi and Pole,
(2010), it is stated that single baseline is the best way to evaluate changes in an individual
behavior. It is because, in this technique, clinicians use both baseline measures and results after
the intervention carried out so as to make comparative analysis. If after the treatment, significant
results found in individual behavior than it simply means that planned intervention is extremely
effective to bring change in particular problematic behavior. In this research, researcher also took
2
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

regular follow up from the patient suffering from overwhelming worry and tension to examine
that whether applied intervention plan sought problematic behavior or not by changing client’s
behavior.
In the presented case study, Eliza is experiencing several behavioral difficulties i.e.
tension and overwhelming worry for the unobvious dangerous and threatening events results in
high level of distress. Thus, over-consciousness, embarrassing, upset, headache, breathing issues
and sweetening are several health care issues experiencing by her. There are different kinds of
design that might be used for designing an intervention plan to cure her from her behavioral
difficulties such as simple design (i.e. single baseline) and complex design (i.e. reversal and
multiple baseline) (Yardley and et.al., 2015). Tracking record of client’s behavior to address the
duration, intensity of incidents and its tendencies are known as baseline measures. It works as a
standard with which identified changes in the individual behavior after implementation of
intervention will be compared to examine its effectiveness (Zipfel and et.al., 2014). Therefore,
single baseline measures will be used as a design under planned intervention to bring change in
her behavior so as to reduce problems of excessive tension, unobvious worry about dangerous &
threatening events. Thus, the key goal of the intervention plan covering cognitive behavioral
therapy (CBT) and generalized anxiety disorder (GAD) is to change individual feelings, thoughts
and behavior (Wagner, Horn and Maercker, 2014). In this, she will be provided with problem
solving training along with the cognitive restructuring for the treatment. Moreover, clinicians
will give relaxation training to change her behavior. Under the PST treatment, client will be
educated about her problems and their catastrophic impact. Brainstorming sessions will be
conducted to instruct client how to resolve their difficulties and obtain productive solutions
(Epton and et.al., 2015). Cognitive restructuring technique will facilitate Eliza to address her
adverse cognitive issues i.e. belief, expectations, excessive worry, belief, self-statement and
others (Dutil and et.al., 2014). It will be carry out in four stages (1). Elicit automatic thoughts (2)
Finding out underlying reasons behind imitational belief in the patient (3). Challenging
behavioral issues (4). Replacement behavior, in which, her problem behavior will be replaced by
suitable alternative.
Procedure of intervention plan
3
that whether applied intervention plan sought problematic behavior or not by changing client’s
behavior.
In the presented case study, Eliza is experiencing several behavioral difficulties i.e.
tension and overwhelming worry for the unobvious dangerous and threatening events results in
high level of distress. Thus, over-consciousness, embarrassing, upset, headache, breathing issues
and sweetening are several health care issues experiencing by her. There are different kinds of
design that might be used for designing an intervention plan to cure her from her behavioral
difficulties such as simple design (i.e. single baseline) and complex design (i.e. reversal and
multiple baseline) (Yardley and et.al., 2015). Tracking record of client’s behavior to address the
duration, intensity of incidents and its tendencies are known as baseline measures. It works as a
standard with which identified changes in the individual behavior after implementation of
intervention will be compared to examine its effectiveness (Zipfel and et.al., 2014). Therefore,
single baseline measures will be used as a design under planned intervention to bring change in
her behavior so as to reduce problems of excessive tension, unobvious worry about dangerous &
threatening events. Thus, the key goal of the intervention plan covering cognitive behavioral
therapy (CBT) and generalized anxiety disorder (GAD) is to change individual feelings, thoughts
and behavior (Wagner, Horn and Maercker, 2014). In this, she will be provided with problem
solving training along with the cognitive restructuring for the treatment. Moreover, clinicians
will give relaxation training to change her behavior. Under the PST treatment, client will be
educated about her problems and their catastrophic impact. Brainstorming sessions will be
conducted to instruct client how to resolve their difficulties and obtain productive solutions
(Epton and et.al., 2015). Cognitive restructuring technique will facilitate Eliza to address her
adverse cognitive issues i.e. belief, expectations, excessive worry, belief, self-statement and
others (Dutil and et.al., 2014). It will be carry out in four stages (1). Elicit automatic thoughts (2)
Finding out underlying reasons behind imitational belief in the patient (3). Challenging
behavioral issues (4). Replacement behavior, in which, her problem behavior will be replaced by
suitable alternative.
Procedure of intervention plan
3
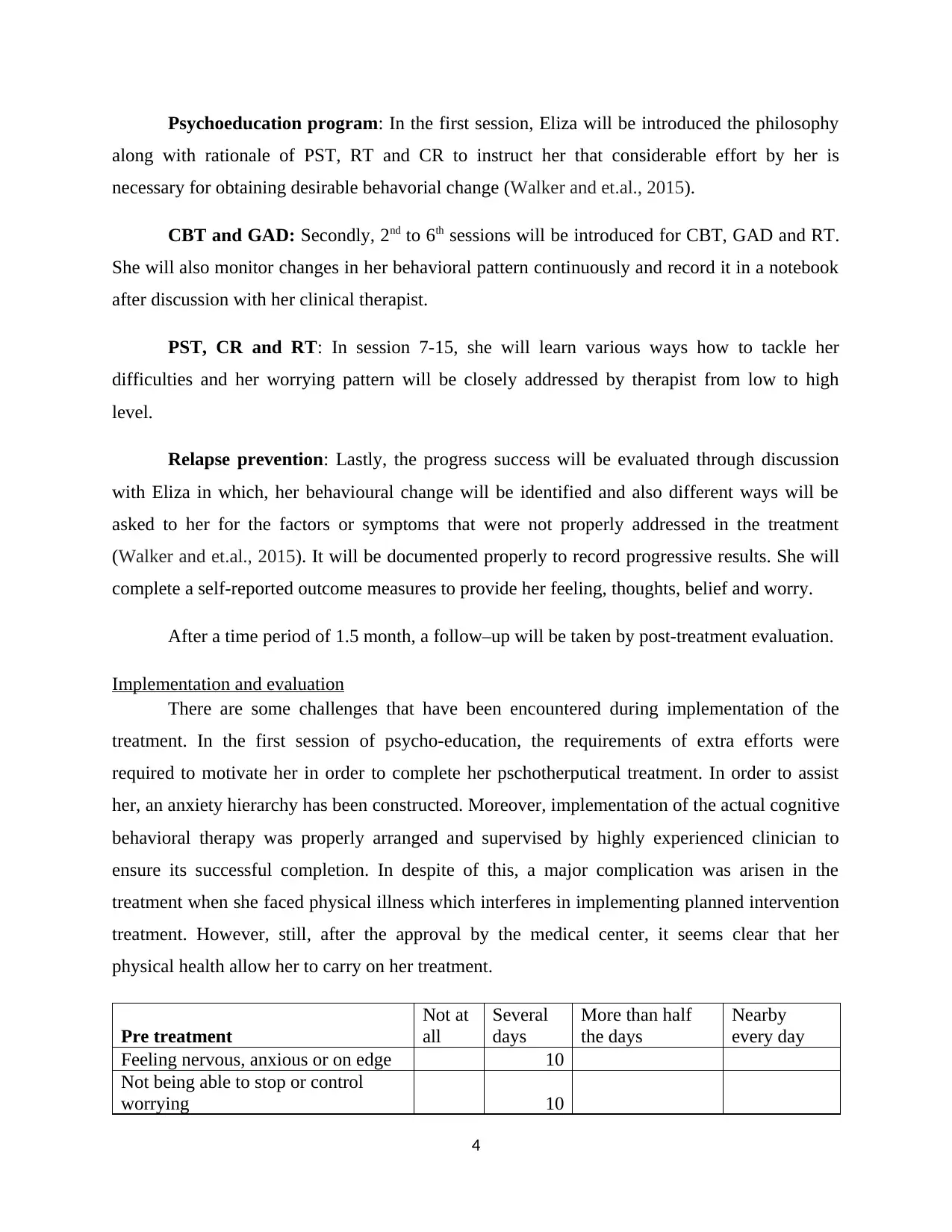
Psychoeducation program: In the first session, Eliza will be introduced the philosophy
along with rationale of PST, RT and CR to instruct her that considerable effort by her is
necessary for obtaining desirable behavorial change (Walker and et.al., 2015).
CBT and GAD: Secondly, 2nd to 6th sessions will be introduced for CBT, GAD and RT.
She will also monitor changes in her behavioral pattern continuously and record it in a notebook
after discussion with her clinical therapist.
PST, CR and RT: In session 7-15, she will learn various ways how to tackle her
difficulties and her worrying pattern will be closely addressed by therapist from low to high
level.
Relapse prevention: Lastly, the progress success will be evaluated through discussion
with Eliza in which, her behavioural change will be identified and also different ways will be
asked to her for the factors or symptoms that were not properly addressed in the treatment
(Walker and et.al., 2015). It will be documented properly to record progressive results. She will
complete a self-reported outcome measures to provide her feeling, thoughts, belief and worry.
After a time period of 1.5 month, a follow–up will be taken by post-treatment evaluation.
Implementation and evaluation
There are some challenges that have been encountered during implementation of the
treatment. In the first session of psycho-education, the requirements of extra efforts were
required to motivate her in order to complete her pschotherputical treatment. In order to assist
her, an anxiety hierarchy has been constructed. Moreover, implementation of the actual cognitive
behavioral therapy was properly arranged and supervised by highly experienced clinician to
ensure its successful completion. In despite of this, a major complication was arisen in the
treatment when she faced physical illness which interferes in implementing planned intervention
treatment. However, still, after the approval by the medical center, it seems clear that her
physical health allow her to carry on her treatment.
Pre treatment
Not at
all
Several
days
More than half
the days
Nearby
every day
Feeling nervous, anxious or on edge 10
Not being able to stop or control
worrying 10
4
along with rationale of PST, RT and CR to instruct her that considerable effort by her is
necessary for obtaining desirable behavorial change (Walker and et.al., 2015).
CBT and GAD: Secondly, 2nd to 6th sessions will be introduced for CBT, GAD and RT.
She will also monitor changes in her behavioral pattern continuously and record it in a notebook
after discussion with her clinical therapist.
PST, CR and RT: In session 7-15, she will learn various ways how to tackle her
difficulties and her worrying pattern will be closely addressed by therapist from low to high
level.
Relapse prevention: Lastly, the progress success will be evaluated through discussion
with Eliza in which, her behavioural change will be identified and also different ways will be
asked to her for the factors or symptoms that were not properly addressed in the treatment
(Walker and et.al., 2015). It will be documented properly to record progressive results. She will
complete a self-reported outcome measures to provide her feeling, thoughts, belief and worry.
After a time period of 1.5 month, a follow–up will be taken by post-treatment evaluation.
Implementation and evaluation
There are some challenges that have been encountered during implementation of the
treatment. In the first session of psycho-education, the requirements of extra efforts were
required to motivate her in order to complete her pschotherputical treatment. In order to assist
her, an anxiety hierarchy has been constructed. Moreover, implementation of the actual cognitive
behavioral therapy was properly arranged and supervised by highly experienced clinician to
ensure its successful completion. In despite of this, a major complication was arisen in the
treatment when she faced physical illness which interferes in implementing planned intervention
treatment. However, still, after the approval by the medical center, it seems clear that her
physical health allow her to carry on her treatment.
Pre treatment
Not at
all
Several
days
More than half
the days
Nearby
every day
Feeling nervous, anxious or on edge 10
Not being able to stop or control
worrying 10
4
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
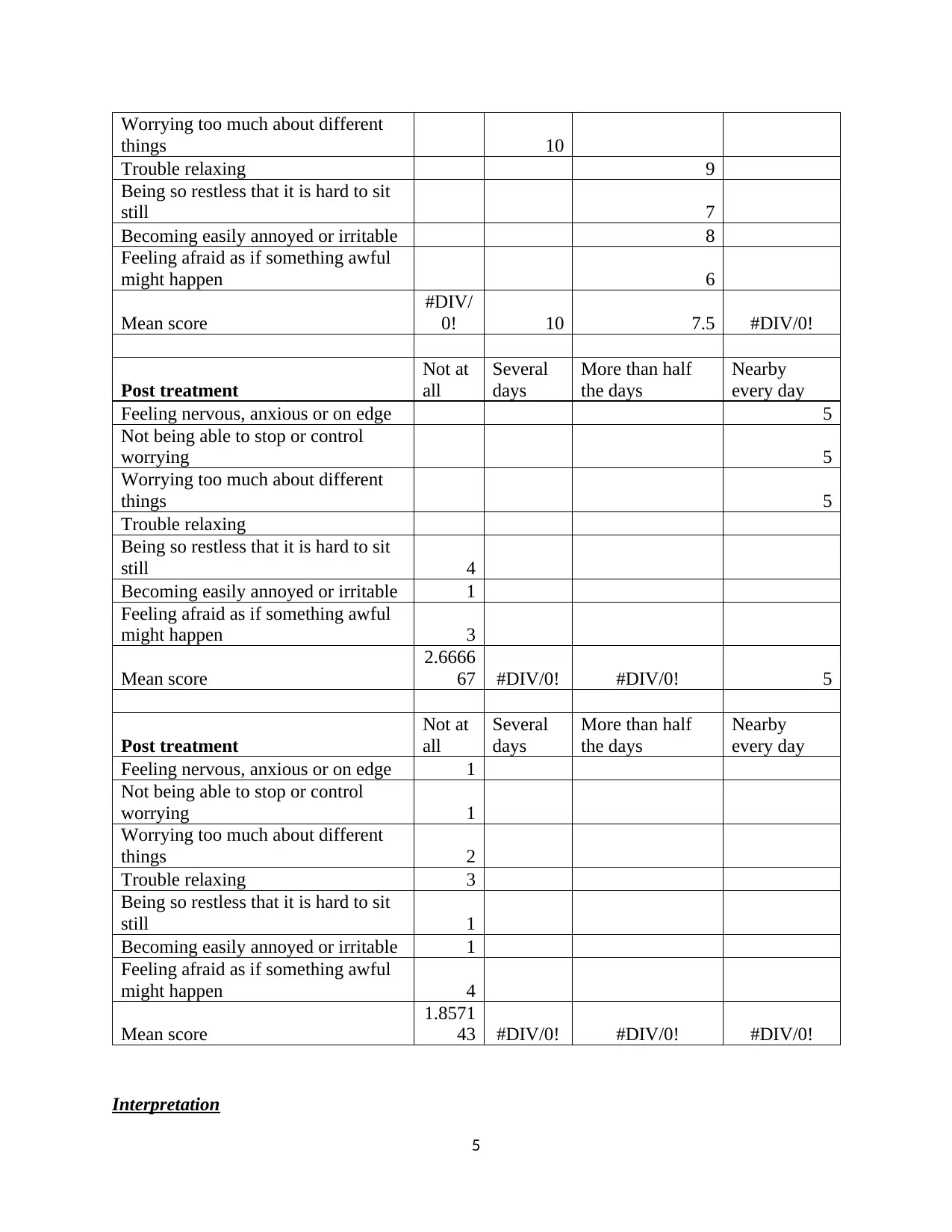
Worrying too much about different
things 10
Trouble relaxing 9
Being so restless that it is hard to sit
still 7
Becoming easily annoyed or irritable 8
Feeling afraid as if something awful
might happen 6
Mean score
#DIV/
0! 10 7.5 #DIV/0!
Post treatment
Not at
all
Several
days
More than half
the days
Nearby
every day
Feeling nervous, anxious or on edge 5
Not being able to stop or control
worrying 5
Worrying too much about different
things 5
Trouble relaxing
Being so restless that it is hard to sit
still 4
Becoming easily annoyed or irritable 1
Feeling afraid as if something awful
might happen 3
Mean score
2.6666
67 #DIV/0! #DIV/0! 5
Post treatment
Not at
all
Several
days
More than half
the days
Nearby
every day
Feeling nervous, anxious or on edge 1
Not being able to stop or control
worrying 1
Worrying too much about different
things 2
Trouble relaxing 3
Being so restless that it is hard to sit
still 1
Becoming easily annoyed or irritable 1
Feeling afraid as if something awful
might happen 4
Mean score
1.8571
43 #DIV/0! #DIV/0! #DIV/0!
Interpretation
5
things 10
Trouble relaxing 9
Being so restless that it is hard to sit
still 7
Becoming easily annoyed or irritable 8
Feeling afraid as if something awful
might happen 6
Mean score
#DIV/
0! 10 7.5 #DIV/0!
Post treatment
Not at
all
Several
days
More than half
the days
Nearby
every day
Feeling nervous, anxious or on edge 5
Not being able to stop or control
worrying 5
Worrying too much about different
things 5
Trouble relaxing
Being so restless that it is hard to sit
still 4
Becoming easily annoyed or irritable 1
Feeling afraid as if something awful
might happen 3
Mean score
2.6666
67 #DIV/0! #DIV/0! 5
Post treatment
Not at
all
Several
days
More than half
the days
Nearby
every day
Feeling nervous, anxious or on edge 1
Not being able to stop or control
worrying 1
Worrying too much about different
things 2
Trouble relaxing 3
Being so restless that it is hard to sit
still 1
Becoming easily annoyed or irritable 1
Feeling afraid as if something awful
might happen 4
Mean score
1.8571
43 #DIV/0! #DIV/0! #DIV/0!
Interpretation
5
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Facts are clearly reflecting that before CBT test anxiety score was much high as score
was 10 across all parameters which reflect that anxiety level for several days was high. In case of
trouble relaxing and other variables anxiety score is nearby in range of 6 to 9. It can be said that
anxiety was observed by individual most of days before treatment. Post treatment mean value
reduced to 2.66 and 5 and shift to not at all and nearby every day. Anxiety score are less than 5
and reflect that after treatment behavior of individual get improved. After post treatment again
data gathered and it is identified that individual shift to not all category from class of nearby
every day. Mean score of anxiety reduced to 1.85 from 2.66 and this reflect that consistency
comes in behavior of individual
6
was 10 across all parameters which reflect that anxiety level for several days was high. In case of
trouble relaxing and other variables anxiety score is nearby in range of 6 to 9. It can be said that
anxiety was observed by individual most of days before treatment. Post treatment mean value
reduced to 2.66 and 5 and shift to not at all and nearby every day. Anxiety score are less than 5
and reflect that after treatment behavior of individual get improved. After post treatment again
data gathered and it is identified that individual shift to not all category from class of nearby
every day. Mean score of anxiety reduced to 1.85 from 2.66 and this reflect that consistency
comes in behavior of individual
6
REFERENCES
Books and Journals
Tarrier, N., & Johnson, J. (2015). Case formulation in cognitive behaviour therapy: The
treatment of challenging and complex cases. Routledge.
Zipfel, S. & et.al. (2014). Focal psychodynamic therapy, cognitive behaviour therapy, and
optimised treatment as usual in outpatients with anorexia nervosa (ANTOP study):
randomised controlled trial. The Lancet. 383(9912). pp.127-137.
Andersson, G. & et.al., (2014). Guided Internet based vs. face to face cognitive behavior therapy
for psychiatric and somatic disorders: a systematic review and meta‐analysis. World
Psychiatry. 13(3). pp.288-295.
Jauhar, S. & et.al., (2014). Cognitive-behavioural therapy for the symptoms of schizophrenia:
systematic review and meta-analysis with examination of potential bias. The British
Journal of Psychiatry. 204(1). pp.20-29.
Wagner, B., Horn, A. B., & Maercker, A. (2014). Internet-based versus face-to-face cognitive-
behavioral intervention for depression: a randomized controlled non-inferiority
trial. Journal of affective disorder., 152(12). 113-121.
Walker, K. & et.al., (2015). Desistance from intimate partner violence: A conceptual model and
framework for practitioners for managing the process of change. Journal of interpersonal
violence. 30(15). 2726-2750.
Dutil, Y. & et.al., (2014). Modeling phase change materials behavior in building applications:
Comments on material characterization and model validation. Renewable Energy. 61(7).
pp.132-135.
Epton, T. & et.al., (2015). The impact of self-affirmation on health-behavior change: a meta-
analysis. Health Psychology. 34(3). pp.187-196.
7
Books and Journals
Tarrier, N., & Johnson, J. (2015). Case formulation in cognitive behaviour therapy: The
treatment of challenging and complex cases. Routledge.
Zipfel, S. & et.al. (2014). Focal psychodynamic therapy, cognitive behaviour therapy, and
optimised treatment as usual in outpatients with anorexia nervosa (ANTOP study):
randomised controlled trial. The Lancet. 383(9912). pp.127-137.
Andersson, G. & et.al., (2014). Guided Internet based vs. face to face cognitive behavior therapy
for psychiatric and somatic disorders: a systematic review and meta‐analysis. World
Psychiatry. 13(3). pp.288-295.
Jauhar, S. & et.al., (2014). Cognitive-behavioural therapy for the symptoms of schizophrenia:
systematic review and meta-analysis with examination of potential bias. The British
Journal of Psychiatry. 204(1). pp.20-29.
Wagner, B., Horn, A. B., & Maercker, A. (2014). Internet-based versus face-to-face cognitive-
behavioral intervention for depression: a randomized controlled non-inferiority
trial. Journal of affective disorder., 152(12). 113-121.
Walker, K. & et.al., (2015). Desistance from intimate partner violence: A conceptual model and
framework for practitioners for managing the process of change. Journal of interpersonal
violence. 30(15). 2726-2750.
Dutil, Y. & et.al., (2014). Modeling phase change materials behavior in building applications:
Comments on material characterization and model validation. Renewable Energy. 61(7).
pp.132-135.
Epton, T. & et.al., (2015). The impact of self-affirmation on health-behavior change: a meta-
analysis. Health Psychology. 34(3). pp.187-196.
7
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Yardley, L. & et.al., (2015). The person-based approach to intervention development:
application to digital health-related behavior change interventions. Journal of medical
Internet research. 17(1). pp.14-39.
McCracken, L. M., & Vowles, K. E. (2014). Acceptance and commitment therapy and
mindfulness for chronic pain: Model, process, and progress. American Psychologist.
69(2). pp.178-183.
Khodarahimi, S., & Pole, N. (2010). Cognitive behavior therapy and worry reduction in an
outpatient with generalized anxiety disorder. Clinical Case Studies. 9(1). pp.53-62.
8
application to digital health-related behavior change interventions. Journal of medical
Internet research. 17(1). pp.14-39.
McCracken, L. M., & Vowles, K. E. (2014). Acceptance and commitment therapy and
mindfulness for chronic pain: Model, process, and progress. American Psychologist.
69(2). pp.178-183.
Khodarahimi, S., & Pole, N. (2010). Cognitive behavior therapy and worry reduction in an
outpatient with generalized anxiety disorder. Clinical Case Studies. 9(1). pp.53-62.
8
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

9
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





