Motivation and Emotion Case Study: University of Queensland
VerifiedAdded on 2023/06/08
|11
|2891
|162
Case Study
AI Summary
This case study focuses on a 20-year-old nursing student, Joe, experiencing insomnia and depressive symptoms following the death of her best friend. The assessment details Joe's behavioral issues, including difficulty sleeping, low energy, anxiety, and negative thoughts. The analysis explores the motivational factors behind these issues, attributing them to acute stress and the loss of a close friend. A hypothesis is proposed, linking the sleep disorder to depression and emphasizing the need for comprehensive treatment. The planned intervention involves both pharmacological and psychological approaches, including a non-benzodiazepine hypnotic drug and grief counseling sessions. The implementation and evaluation section describes the treatment process, the positive outcomes of the counseling, and the improvements in Joe's sleeping patterns and overall well-being. The study concludes with a critical analysis of ways to improve the intervention, suggesting the use of Cognitive Behavioral Therapy (CBT) and behavioral strategies like muscle relaxation and stress management.

Running Head: MOTIVATION AND EMOTION 1
Case study Motivation and Emotion
Author's Name
Institutional Affiliation
Case study Motivation and Emotion
Author's Name
Institutional Affiliation
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
MOTIVATION AND EMOTION 2
Reason for Referral
Joe is a 20 years old female, living at her home in Queensland, Australia with her parents
and her younger brother. Presently, she is pursuing her bachelor’s degree in nursing from the
University of Queensland. Joe is presently having difficulty falling asleep. She is neglecting her
social and physical actives of her regular life. This problem initiated two months ago when Joe
lost her best friend Momo who was suffering from a major ailment of heart. Neither Joe nor any
other members of her family have a previous record of depression or insomnia. Joe needs urgent
medical help here, or her situation can only get worse.
Assessment
Description of behavioral issue
Joe is not able to sleep properly and often remains awake at night. She has trouble falling asleep,
and when she wakes up, she feels drowsy and low on energy. Although she goes to bed at 10 pm,
she rains awake until 2 am. Even when she falls asleep, she wakes up at about 5.am. and is
unable to go back to sleep. She keeps lying in bed when she wakes up; she feels drowsy and low
on energy. She experiences anxiety at times and shows physical symptoms of dizziness. Joe is
unable to sleep and focus on her studies. As she feels low on energy, she does not feel like going
to the college Although her general health is good, she recalls a stressful event in her life, and it
is the untimely death of her best friend, Momo. She is showing symptoms of sleeping disorders
and depression. She looks uneasy, nervous and there is a stained look on her face. Her stress and
lack of sleep are interfering with her life and relationships. She complains of having negative
thoughts all the time and her mind is floodedwith the thoughts of her close friends and her death.
Reason for Referral
Joe is a 20 years old female, living at her home in Queensland, Australia with her parents
and her younger brother. Presently, she is pursuing her bachelor’s degree in nursing from the
University of Queensland. Joe is presently having difficulty falling asleep. She is neglecting her
social and physical actives of her regular life. This problem initiated two months ago when Joe
lost her best friend Momo who was suffering from a major ailment of heart. Neither Joe nor any
other members of her family have a previous record of depression or insomnia. Joe needs urgent
medical help here, or her situation can only get worse.
Assessment
Description of behavioral issue
Joe is not able to sleep properly and often remains awake at night. She has trouble falling asleep,
and when she wakes up, she feels drowsy and low on energy. Although she goes to bed at 10 pm,
she rains awake until 2 am. Even when she falls asleep, she wakes up at about 5.am. and is
unable to go back to sleep. She keeps lying in bed when she wakes up; she feels drowsy and low
on energy. She experiences anxiety at times and shows physical symptoms of dizziness. Joe is
unable to sleep and focus on her studies. As she feels low on energy, she does not feel like going
to the college Although her general health is good, she recalls a stressful event in her life, and it
is the untimely death of her best friend, Momo. She is showing symptoms of sleeping disorders
and depression. She looks uneasy, nervous and there is a stained look on her face. Her stress and
lack of sleep are interfering with her life and relationships. She complains of having negative
thoughts all the time and her mind is floodedwith the thoughts of her close friends and her death.
MOTIVATION AND EMOTION 3
Despite taking sleep medication, she still remains awake almost every night. Her family tried to
talk to her but, she refuses to respond or listen to them.
Analysis of motivational factors behind the behavioral issues
Joe’s problem with her sleep started after the death of her best friend. Earlier she had no
sleep problems. She was very close to Memo, who was diagnosed with a significant heart
ailment and unfortunately, she died with a massive heart attack at the age of 20 only. It is very
difficult for Joe to accept this stressful event in her life and she remembers her friend whenever
she is alone. Clearly, Joe is facing acute stress because of the loss of her very close friend. Joe’s
behavioral issues and lack of sleep have developed after the stressful life event. Even if the event
is gone and over, its impacts are manifesting as psychosocial stress and insomnia in Joe. Joe has
probably developed sleep patterns that link her sleep environment to anxiety and stress, Thus, her
sleep environment has become a stimulus for her sleep difficulties. When the bed time
approaches, she starts developing those thoughts and it results in increasing tension. The result is
that despite feeling sleepy, she is not able to sleep. The more she tries to sleep, the more difficult
it gets for her. Her GP prescribed a low-dose of Amitriptyline (tricyclic antidepressant) to lower
her stress and induce better sleep, but the medication leaves her even drowsier and her mouth
becomes dry. It is obvious that the medication prescribed by her GP is not effective. It is
essential to treat Momo as her symptoms are causing significant damage to her social and
academic life. Her physical and psychological health are likely to suffer if the patient is left
untreated.
Hypothesis
Despite taking sleep medication, she still remains awake almost every night. Her family tried to
talk to her but, she refuses to respond or listen to them.
Analysis of motivational factors behind the behavioral issues
Joe’s problem with her sleep started after the death of her best friend. Earlier she had no
sleep problems. She was very close to Memo, who was diagnosed with a significant heart
ailment and unfortunately, she died with a massive heart attack at the age of 20 only. It is very
difficult for Joe to accept this stressful event in her life and she remembers her friend whenever
she is alone. Clearly, Joe is facing acute stress because of the loss of her very close friend. Joe’s
behavioral issues and lack of sleep have developed after the stressful life event. Even if the event
is gone and over, its impacts are manifesting as psychosocial stress and insomnia in Joe. Joe has
probably developed sleep patterns that link her sleep environment to anxiety and stress, Thus, her
sleep environment has become a stimulus for her sleep difficulties. When the bed time
approaches, she starts developing those thoughts and it results in increasing tension. The result is
that despite feeling sleepy, she is not able to sleep. The more she tries to sleep, the more difficult
it gets for her. Her GP prescribed a low-dose of Amitriptyline (tricyclic antidepressant) to lower
her stress and induce better sleep, but the medication leaves her even drowsier and her mouth
becomes dry. It is obvious that the medication prescribed by her GP is not effective. It is
essential to treat Momo as her symptoms are causing significant damage to her social and
academic life. Her physical and psychological health are likely to suffer if the patient is left
untreated.
Hypothesis
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
MOTIVATION AND EMOTION 4
As sleep disorders and insomnia lead to a poor quality of life and weaker social and
workplace performance, they could further add to the stress levels. Lying awake in the dark
would encourage more negative thoughts to develop and can trigger the depression. Loss of
control over sleep or lack of sleep can make the individual feel helpless. In Joes’ case, the
traumatic event in her life has led to her depressive mood and sleep disorders that can further
aggravate the depression. It is essential to understand the relationship between depression and
insomnia. The treatment plans in her case should target both her depression and her sleeping
disorders. As it is the traumatic event that led to her sleeping disorders, it is not enough to treat
her insomnia but also look at the underlying cause behind her sleeping disorders and the cause of
her stress.
A simple baseline intervention has been selected to be most suitable in the case of Joe. As
it has been only two months that she is experiencing the problems, it would be easier to get rid of
the problems being faced by her
As individuals with depression show significant levels of insomnia, it is essential to treat
sleep disorders which could be a major health concern for the patient. A planned intervention and
treatment can help the patient get rid of her anxiety that is affecting her sleep.
Planned Intervention
Research review
Stress exposure can increase the psychophysiological vulnerabilities such as stress
disorders, depression, schizophrenia and the development of insomnia disorder (Drake, Pillai &
Roth,2014). Research indicates that the majority of individuals with depression show significant
levels of insomnia. Insomnia is the most prevalent sleep disorder and a significant public health
As sleep disorders and insomnia lead to a poor quality of life and weaker social and
workplace performance, they could further add to the stress levels. Lying awake in the dark
would encourage more negative thoughts to develop and can trigger the depression. Loss of
control over sleep or lack of sleep can make the individual feel helpless. In Joes’ case, the
traumatic event in her life has led to her depressive mood and sleep disorders that can further
aggravate the depression. It is essential to understand the relationship between depression and
insomnia. The treatment plans in her case should target both her depression and her sleeping
disorders. As it is the traumatic event that led to her sleeping disorders, it is not enough to treat
her insomnia but also look at the underlying cause behind her sleeping disorders and the cause of
her stress.
A simple baseline intervention has been selected to be most suitable in the case of Joe. As
it has been only two months that she is experiencing the problems, it would be easier to get rid of
the problems being faced by her
As individuals with depression show significant levels of insomnia, it is essential to treat
sleep disorders which could be a major health concern for the patient. A planned intervention and
treatment can help the patient get rid of her anxiety that is affecting her sleep.
Planned Intervention
Research review
Stress exposure can increase the psychophysiological vulnerabilities such as stress
disorders, depression, schizophrenia and the development of insomnia disorder (Drake, Pillai &
Roth,2014). Research indicates that the majority of individuals with depression show significant
levels of insomnia. Insomnia is the most prevalent sleep disorder and a significant public health
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
MOTIVATION AND EMOTION 5
implication that leads to lower productivity due to increased absenteeism and health care costs.
The patient suffers worse quality of life and is associated with poor mental and physical health
(Vgontzas Fernandez-Mendoza, Liao, & Bixler,2013). Sleep health is a strong indicator of other
disorders and is used as a useful reference by the healthcare administrators (Buysse., 2014).
Poor quality of sleep can disturb the health stimulating functions that lead to poor health
outcomes like stroke, obesity, diabetes, and depression have been linked to poor sleep (Johnson
et al., 2016). Insomnia and depression are connected deeply as they share several intersection
points. Disturbed sleep patterns become a risk for subsequent depression. It is essential to treat
both depression and insomnia to maximize positive outcomes (Scogin et al., 2018). Psychosocial
stressors are linked with lack of sleep.
The first line of treatment for insomnia is pharmacological interventions. US Food and
Drug Administration advocates certain drugs such as zaleplon and amelteon for sleep
maintenance problems (Pillai et al., 2015). Pharmacotherapy is one of the major approaches to
treatment for insomnia, while cognitive behavioral therapies are considered an alternative. The
clinicians must continue to exercise their clinical judgment based on their clinical experience,
patient response, and preferences, plus any potential adverse effects of the treatment (Sateia et
al., 2017). Cognitive behavioral therapy for insomnia (CBTI) remains underutilized when it
comes to targeting chronic insomnia and sleep disturbances as stated by Arnedt et al. (2013).
Although insomnia and depression are common comorbidities, the patient is usually treated for
depression. Research has evidences that counseling is as effective as CBT for depression. The
most commonly used psychological interventions for the treatment of depressive disorder are
interpersonal therapy, cognitive behavioral therapy and supportive therapy (Health Quality
implication that leads to lower productivity due to increased absenteeism and health care costs.
The patient suffers worse quality of life and is associated with poor mental and physical health
(Vgontzas Fernandez-Mendoza, Liao, & Bixler,2013). Sleep health is a strong indicator of other
disorders and is used as a useful reference by the healthcare administrators (Buysse., 2014).
Poor quality of sleep can disturb the health stimulating functions that lead to poor health
outcomes like stroke, obesity, diabetes, and depression have been linked to poor sleep (Johnson
et al., 2016). Insomnia and depression are connected deeply as they share several intersection
points. Disturbed sleep patterns become a risk for subsequent depression. It is essential to treat
both depression and insomnia to maximize positive outcomes (Scogin et al., 2018). Psychosocial
stressors are linked with lack of sleep.
The first line of treatment for insomnia is pharmacological interventions. US Food and
Drug Administration advocates certain drugs such as zaleplon and amelteon for sleep
maintenance problems (Pillai et al., 2015). Pharmacotherapy is one of the major approaches to
treatment for insomnia, while cognitive behavioral therapies are considered an alternative. The
clinicians must continue to exercise their clinical judgment based on their clinical experience,
patient response, and preferences, plus any potential adverse effects of the treatment (Sateia et
al., 2017). Cognitive behavioral therapy for insomnia (CBTI) remains underutilized when it
comes to targeting chronic insomnia and sleep disturbances as stated by Arnedt et al. (2013).
Although insomnia and depression are common comorbidities, the patient is usually treated for
depression. Research has evidences that counseling is as effective as CBT for depression. The
most commonly used psychological interventions for the treatment of depressive disorder are
interpersonal therapy, cognitive behavioral therapy and supportive therapy (Health Quality
MOTIVATION AND EMOTION 6
Ontario. 2017). These therapies reduce depression symptoms while CBT is known to reduce
anxiety symptoms in the patient.
Intervention goals
The objective of intervention for the current case is to improve her sleep patterns so that
she is able to lead a normal and active life. In the current case, Joe is under acute stress due to the
sudden death of her best friend, Momo. She is suffering from acute insomnia and shows signs of
depression. Her treatment should focus on both insomnia and depression. The goal of the
intervention plan is to lower her stress levels and anxiety and improve her quality of sleep. Joe’s
main goal in participating in this treatment was to overcome her depressed moods and insomnia.
Design and procedure
A simple baseline intervention has been selected here that includes both pharmacological
and psychological treatment. Her current psychological stresses and depression symptoms must
be adequately explored.
As the patient is unable to tolerate the low-dose of Amitriptyline (tricyclic
antidepressant) prescribed by her GP, a non-benzodiazepine hypnotic drug,
Zalepon (of Andante brand) is suggested for four weeks.
Joe needs grief counselling sessions for at least three to four months and
education on good sleep hygiene. Her counselor would discuss her emotions and
the connection between her thoughts and emotions. He may suggest aerobic
exercises and brain stimulation exercises to keep her body and mind active.
Ontario. 2017). These therapies reduce depression symptoms while CBT is known to reduce
anxiety symptoms in the patient.
Intervention goals
The objective of intervention for the current case is to improve her sleep patterns so that
she is able to lead a normal and active life. In the current case, Joe is under acute stress due to the
sudden death of her best friend, Momo. She is suffering from acute insomnia and shows signs of
depression. Her treatment should focus on both insomnia and depression. The goal of the
intervention plan is to lower her stress levels and anxiety and improve her quality of sleep. Joe’s
main goal in participating in this treatment was to overcome her depressed moods and insomnia.
Design and procedure
A simple baseline intervention has been selected here that includes both pharmacological
and psychological treatment. Her current psychological stresses and depression symptoms must
be adequately explored.
As the patient is unable to tolerate the low-dose of Amitriptyline (tricyclic
antidepressant) prescribed by her GP, a non-benzodiazepine hypnotic drug,
Zalepon (of Andante brand) is suggested for four weeks.
Joe needs grief counselling sessions for at least three to four months and
education on good sleep hygiene. Her counselor would discuss her emotions and
the connection between her thoughts and emotions. He may suggest aerobic
exercises and brain stimulation exercises to keep her body and mind active.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
MOTIVATION AND EMOTION 7
The treatment should be planned based on her preferences and how she responds to the
treatment. It will be beneficial if her family and friends remain in close contact with her so that
she can interact and share her feelings. The emotional support would help her get back faster to
her regular life and deal with her trauma effectively. It essential in such cases to follow up and
keep a check that the trouble in falling asleep can take a chronic course of action and develop
into chronic psychophysiological insomnia.
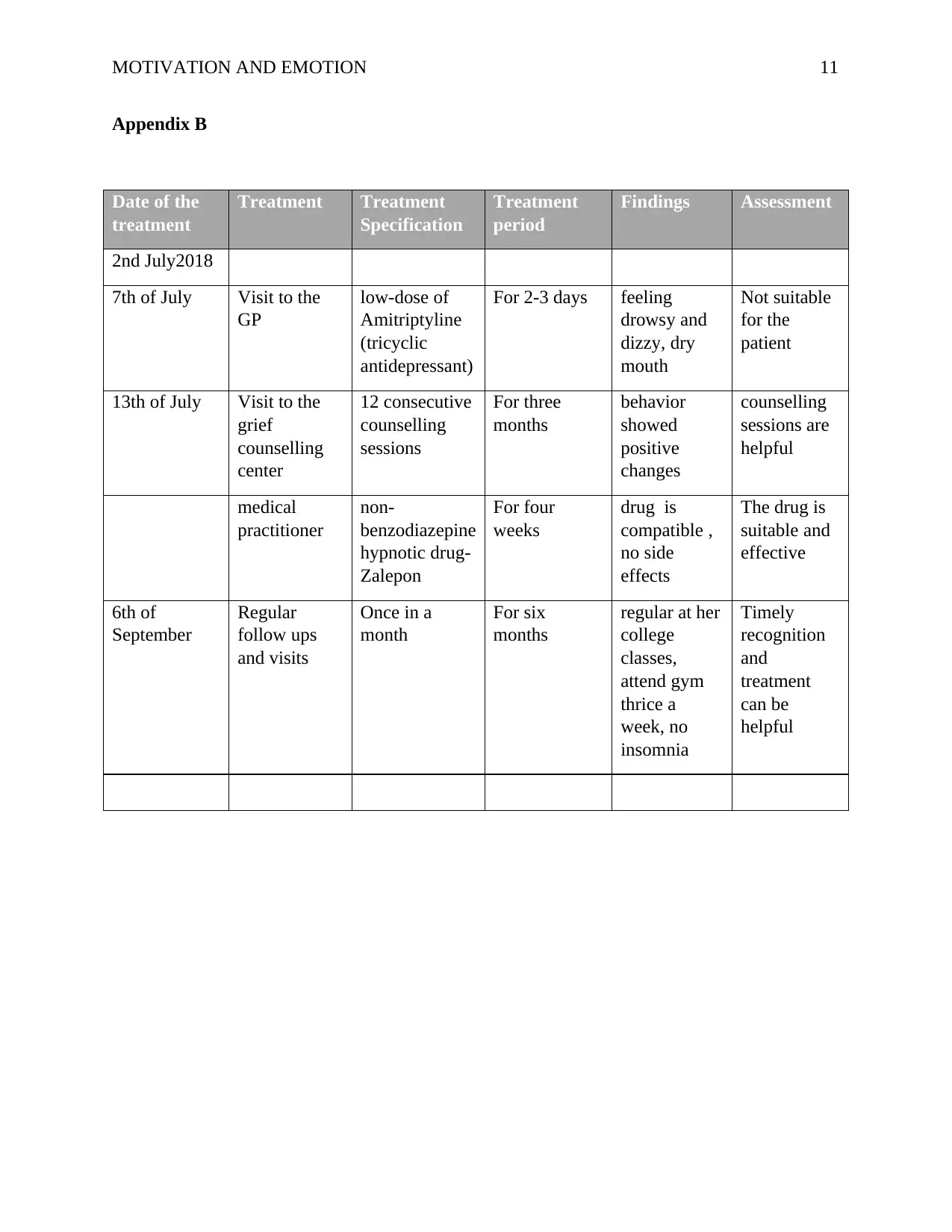
Implementation and Evaluation
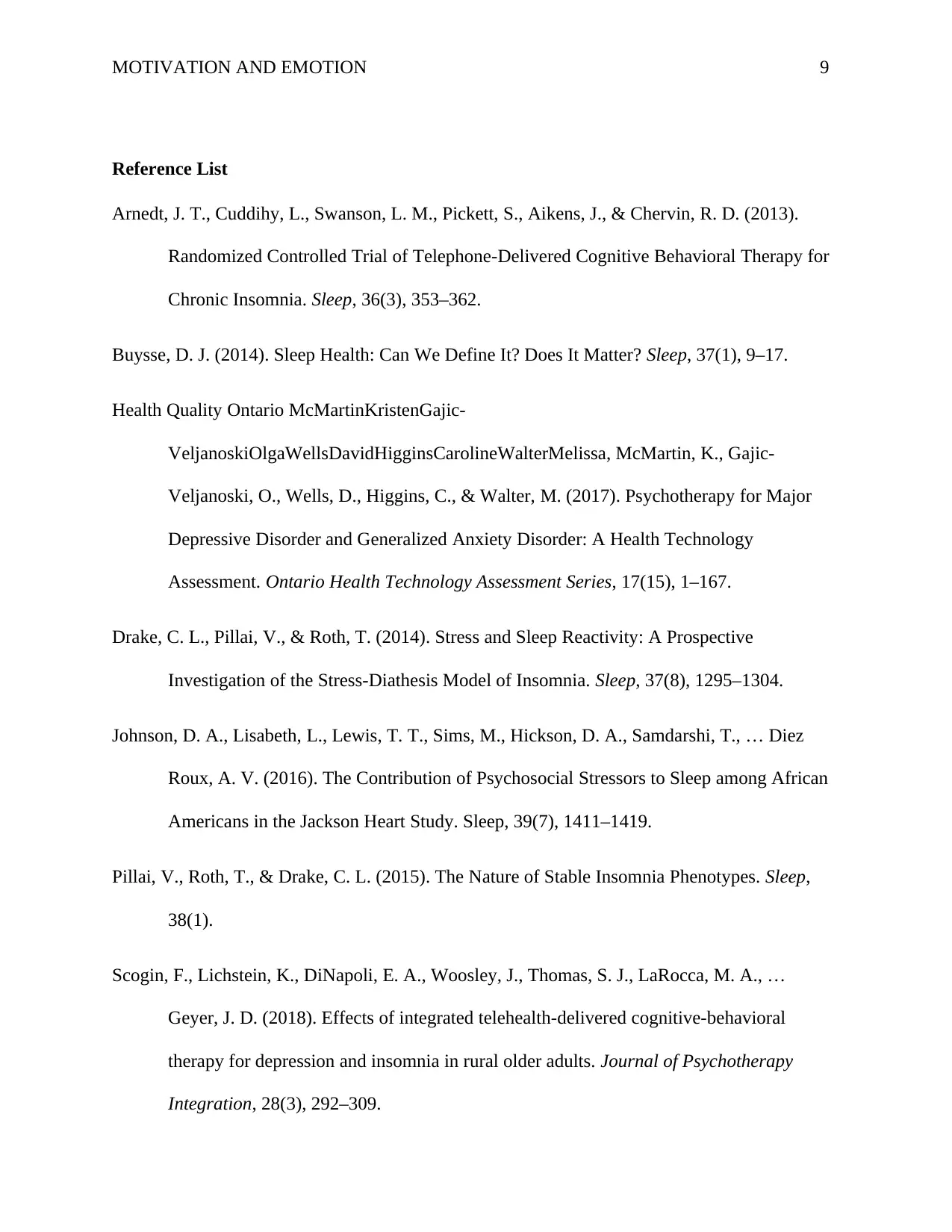
Joe’s treatment commenced on the 2nd July 2018, and she was taken to the GP on the 7th
of July, 2018. However, as the prescribed medicines by the GP did not work out, she was taken
to the grief counselling center on 13th of July. Mr. Hary, the counsellor conducted for her
psychometric tests and scheduled for the 12 consecutive counselling sessions for Joe. The total
time frame of this treatment was set to be three months. For these three months, Joe needs to
attend the sessions every Friday. A medical practitioner gave her medicines comprising of a
non-benzodiazepine hypnotic drug, Zalepon (of Andante brand) and asked her to continue the
drug for four weeks.
Critical evaluation
The counselling sessions by Mr. Hary was proven to be very much helpful for Joe.
Counselling by the psychiatrist and the support of her family and friends showed positive
improvements in Joe. After attaining two or three sessions, Joe’s behavior showed positive
changes. Gradually, she overcame the massive trauma of losing her best friend and her sleeping
patterns improved. Moreover, this time this drug was much compatible with Joe. By the end of
her 10th session she had almost overcome the trauma and was getting back to her regular course
of life. The last two sessions took care of all her small issues regarding overcoming this life
The treatment should be planned based on her preferences and how she responds to the
treatment. It will be beneficial if her family and friends remain in close contact with her so that
she can interact and share her feelings. The emotional support would help her get back faster to
her regular life and deal with her trauma effectively. It essential in such cases to follow up and
keep a check that the trouble in falling asleep can take a chronic course of action and develop
into chronic psychophysiological insomnia.
Implementation and Evaluation
Joe’s treatment commenced on the 2nd July 2018, and she was taken to the GP on the 7th
of July, 2018. However, as the prescribed medicines by the GP did not work out, she was taken
to the grief counselling center on 13th of July. Mr. Hary, the counsellor conducted for her
psychometric tests and scheduled for the 12 consecutive counselling sessions for Joe. The total
time frame of this treatment was set to be three months. For these three months, Joe needs to
attend the sessions every Friday. A medical practitioner gave her medicines comprising of a
non-benzodiazepine hypnotic drug, Zalepon (of Andante brand) and asked her to continue the
drug for four weeks.
Critical evaluation
The counselling sessions by Mr. Hary was proven to be very much helpful for Joe.
Counselling by the psychiatrist and the support of her family and friends showed positive
improvements in Joe. After attaining two or three sessions, Joe’s behavior showed positive
changes. Gradually, she overcame the massive trauma of losing her best friend and her sleeping
patterns improved. Moreover, this time this drug was much compatible with Joe. By the end of
her 10th session she had almost overcome the trauma and was getting back to her regular course
of life. The last two sessions took care of all her small issues regarding overcoming this life
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
MOTIVATION AND EMOTION 8
event. Moreover, after the completion of the treatment, her issues were completely gone, and she
went back to her regular course of life. Today, as on the 6th of September, 2018 Joe is leading a
normal college life. She is regular at her college classes, attend gym thrice a week and gives
adequate time to her family and friends. She visits her counselor once in a month as a follow up
and to assess any further conditions.
Critical analysis of ways to improve intervention
Cognitive behavioral therapy (CBT) can be used to improve the treatment intervention
for Joe. CBT can help the patient to get rid of unrealistic expectations about her sleep and get
more practical. Her counselor can discuss those issues and reassure her. She needs to understand
that fundamental causes behind her sleep disorders or insomnia. The intervention can further
improve if she is instructed to keep a sleep diary and taught several behavioral strategies like
muscle relaxation, meditation and stress management.
In the case of Joe, it is seen that she was very much traumatized because of the sudden
death of her best friend. She was under stress because of the very traumatic event in her life
which was like an extreme trauma that was making her restless and unable to sleep at night. It
only by designing the right treatment plans and interventions that can help Joe and help her
overcome here traumas, stress and the sleeping disorders. Timely recognition of Joe’s problem
by her parents, their active support, and the proper treatment of the issue, Joe was able to recover
soon, and resume her regular course of life by overcoming her trauma
event. Moreover, after the completion of the treatment, her issues were completely gone, and she
went back to her regular course of life. Today, as on the 6th of September, 2018 Joe is leading a
normal college life. She is regular at her college classes, attend gym thrice a week and gives
adequate time to her family and friends. She visits her counselor once in a month as a follow up
and to assess any further conditions.
Critical analysis of ways to improve intervention
Cognitive behavioral therapy (CBT) can be used to improve the treatment intervention
for Joe. CBT can help the patient to get rid of unrealistic expectations about her sleep and get
more practical. Her counselor can discuss those issues and reassure her. She needs to understand
that fundamental causes behind her sleep disorders or insomnia. The intervention can further
improve if she is instructed to keep a sleep diary and taught several behavioral strategies like
muscle relaxation, meditation and stress management.
In the case of Joe, it is seen that she was very much traumatized because of the sudden
death of her best friend. She was under stress because of the very traumatic event in her life
which was like an extreme trauma that was making her restless and unable to sleep at night. It
only by designing the right treatment plans and interventions that can help Joe and help her
overcome here traumas, stress and the sleeping disorders. Timely recognition of Joe’s problem
by her parents, their active support, and the proper treatment of the issue, Joe was able to recover
soon, and resume her regular course of life by overcoming her trauma
MOTIVATION AND EMOTION 9
Reference List
Arnedt, J. T., Cuddihy, L., Swanson, L. M., Pickett, S., Aikens, J., & Chervin, R. D. (2013).
Randomized Controlled Trial of Telephone-Delivered Cognitive Behavioral Therapy for
Chronic Insomnia. Sleep, 36(3), 353–362.
Buysse, D. J. (2014). Sleep Health: Can We Define It? Does It Matter? Sleep, 37(1), 9–17.
Health Quality Ontario McMartinKristenGajic-
VeljanoskiOlgaWellsDavidHigginsCarolineWalterMelissa, McMartin, K., Gajic-
Veljanoski, O., Wells, D., Higgins, C., & Walter, M. (2017). Psychotherapy for Major
Depressive Disorder and Generalized Anxiety Disorder: A Health Technology
Assessment. Ontario Health Technology Assessment Series, 17(15), 1–167.
Drake, C. L., Pillai, V., & Roth, T. (2014). Stress and Sleep Reactivity: A Prospective
Investigation of the Stress-Diathesis Model of Insomnia. Sleep, 37(8), 1295–1304.
Johnson, D. A., Lisabeth, L., Lewis, T. T., Sims, M., Hickson, D. A., Samdarshi, T., … Diez
Roux, A. V. (2016). The Contribution of Psychosocial Stressors to Sleep among African
Americans in the Jackson Heart Study. Sleep, 39(7), 1411–1419.
Pillai, V., Roth, T., & Drake, C. L. (2015). The Nature of Stable Insomnia Phenotypes. Sleep,
38(1).
Scogin, F., Lichstein, K., DiNapoli, E. A., Woosley, J., Thomas, S. J., LaRocca, M. A., …
Geyer, J. D. (2018). Effects of integrated telehealth-delivered cognitive-behavioral
therapy for depression and insomnia in rural older adults. Journal of Psychotherapy
Integration, 28(3), 292–309.
Reference List
Arnedt, J. T., Cuddihy, L., Swanson, L. M., Pickett, S., Aikens, J., & Chervin, R. D. (2013).
Randomized Controlled Trial of Telephone-Delivered Cognitive Behavioral Therapy for
Chronic Insomnia. Sleep, 36(3), 353–362.
Buysse, D. J. (2014). Sleep Health: Can We Define It? Does It Matter? Sleep, 37(1), 9–17.
Health Quality Ontario McMartinKristenGajic-
VeljanoskiOlgaWellsDavidHigginsCarolineWalterMelissa, McMartin, K., Gajic-
Veljanoski, O., Wells, D., Higgins, C., & Walter, M. (2017). Psychotherapy for Major
Depressive Disorder and Generalized Anxiety Disorder: A Health Technology
Assessment. Ontario Health Technology Assessment Series, 17(15), 1–167.
Drake, C. L., Pillai, V., & Roth, T. (2014). Stress and Sleep Reactivity: A Prospective
Investigation of the Stress-Diathesis Model of Insomnia. Sleep, 37(8), 1295–1304.
Johnson, D. A., Lisabeth, L., Lewis, T. T., Sims, M., Hickson, D. A., Samdarshi, T., … Diez
Roux, A. V. (2016). The Contribution of Psychosocial Stressors to Sleep among African
Americans in the Jackson Heart Study. Sleep, 39(7), 1411–1419.
Pillai, V., Roth, T., & Drake, C. L. (2015). The Nature of Stable Insomnia Phenotypes. Sleep,
38(1).
Scogin, F., Lichstein, K., DiNapoli, E. A., Woosley, J., Thomas, S. J., LaRocca, M. A., …
Geyer, J. D. (2018). Effects of integrated telehealth-delivered cognitive-behavioral
therapy for depression and insomnia in rural older adults. Journal of Psychotherapy
Integration, 28(3), 292–309.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

MOTIVATION AND EMOTION 10
Sateia, M. J., Buysse, D. J., Krystal, A. D., Neubauer, D. N., & Heald, J. L. (2017). Clinical
Practice Guideline for the Pharmacologic Treatment of Chronic Insomnia in Adults: An
American Academy of Sleep Medicine Clinical Practice Guideline. Journal of Clinical
Sleep Medicine : JCSM : Official Publication of the American Academy of Sleep
Medicine, 13(2), 307–349.
Vgontzas, A. N., Fernandez-Mendoza, J., Liao, D., & Bixler, E. O. (2013). Insomnia with
Objective Short Sleep Duration: the Most Biologically Severe Phenotype of the Disorder.
Sleep Medicine Reviews, 17(4), 241–254.
Appendix A
Sateia, M. J., Buysse, D. J., Krystal, A. D., Neubauer, D. N., & Heald, J. L. (2017). Clinical
Practice Guideline for the Pharmacologic Treatment of Chronic Insomnia in Adults: An
American Academy of Sleep Medicine Clinical Practice Guideline. Journal of Clinical
Sleep Medicine : JCSM : Official Publication of the American Academy of Sleep
Medicine, 13(2), 307–349.
Vgontzas, A. N., Fernandez-Mendoza, J., Liao, D., & Bixler, E. O. (2013). Insomnia with
Objective Short Sleep Duration: the Most Biologically Severe Phenotype of the Disorder.
Sleep Medicine Reviews, 17(4), 241–254.
Appendix A
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
MOTIVATION AND EMOTION 11
Appendix B
Date of the
treatment
Treatment Treatment
Specification
Treatment
period
Findings Assessment
2nd July2018
7th of July Visit to the
GP
low-dose of
Amitriptyline
(tricyclic
antidepressant)
For 2-3 days feeling
drowsy and
dizzy, dry
mouth
Not suitable
for the
patient
13th of July Visit to the
grief
counselling
center
12 consecutive
counselling
sessions
For three
months
behavior
showed
positive
changes
counselling
sessions are
helpful
medical
practitioner
non-
benzodiazepine
hypnotic drug-
Zalepon
For four
weeks
drug is
compatible ,
no side
effects
The drug is
suitable and
effective
6th of
September
Regular
follow ups
and visits
Once in a
month
For six
months
regular at her
college
classes,
attend gym
thrice a
week, no
insomnia
Timely
recognition
and
treatment
can be
helpful
Appendix B
Date of the
treatment
Treatment Treatment
Specification
Treatment
period
Findings Assessment
2nd July2018
7th of July Visit to the
GP
low-dose of
Amitriptyline
(tricyclic
antidepressant)
For 2-3 days feeling
drowsy and
dizzy, dry
mouth
Not suitable
for the
patient
13th of July Visit to the
grief
counselling
center
12 consecutive
counselling
sessions
For three
months
behavior
showed
positive
changes
counselling
sessions are
helpful
medical
practitioner
non-
benzodiazepine
hypnotic drug-
Zalepon
For four
weeks
drug is
compatible ,
no side
effects
The drug is
suitable and
effective
6th of
September
Regular
follow ups
and visits
Once in a
month
For six
months
regular at her
college
classes,
attend gym
thrice a
week, no
insomnia
Timely
recognition
and
treatment
can be
helpful
1 out of 11
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.


