Myocardial Infarction: Case Study
VerifiedAdded on 2023/05/31
|7
|1654
|345
AI Summary
Read this case study on myocardial infarction and learn about the elements of deterioration, ISBAR communication, and pathophysiology of deleterious condition.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: MYOCARDIAL INFARCTION: CASE STUDY
Myocardial Infarction: Case Study
Name of student:
Name of university:
Author Note:
Myocardial Infarction: Case Study
Name of student:
Name of university:
Author Note:
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1MYOCARDIAL INFARCTION: CASE STUDY
Elements of deterioration
The patient, Mr. Lee was admitted with myocardial infarction with associated symptoms
of shortness of breath, lightheadedness and angina or chest pain. Early interventions and
diagnosis of the condition was done through performing electrocardiogram, which enabled initial
management of the cardiac discomfort. The patient was given nitroglycerin in sublingual form in
successive dosages along with morphine. This drug treatment, intended to improve the condition,
however, further resulted in deterioration of the patient’s condition with reduction of blood rate,
hypotension and reduced preload of myocardial oxygen demand followed by lethargy. A review
of the patient’s clinical condition confirmed that increased heart rate (HR 133), decreased blood
pressure (BP 87/53) and reduced level of myocardial oxygen saturation (SPO2 88%) are mainly
the elements of deterioration in the patient’s condition. According to NSW Health Between the
Flags, indication of these elements of deterioration require a clinical review by nursing officials
to assess the root of deterioration of clinical treatment (Hughes et al., 2014). Based on clinical
review in the given case study, an increased requirement of myocardial oxygen is required to
improve the hypoxic condition. The nursing assessment of the Mr. Lee needs to be performed to
identify whether the deterioration has occurred due to drug overdose or any new clinical
symptom. If these clinical review and identification of deteriorating causes do not result in
improved patient condition in the following one hour, then a rapid response team would be
required to handle the situation (Chen et al., 2014). In the given case study of Mr. Lee, frequent
assessment by nurses is essential for the following one hour post clinical review.
ISBAR communication
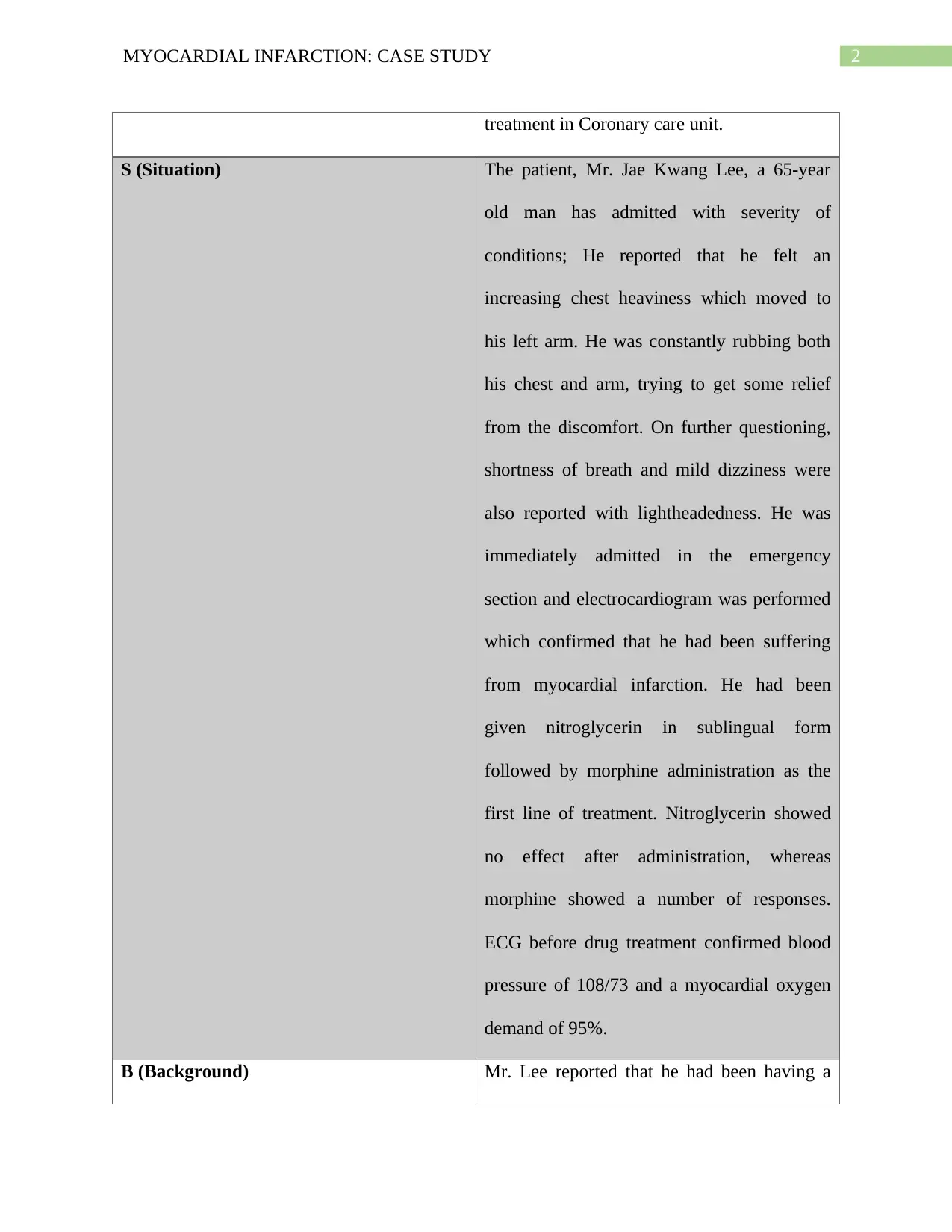
I (Identity) Health nurse attending Mr. Lee post drug
Elements of deterioration
The patient, Mr. Lee was admitted with myocardial infarction with associated symptoms
of shortness of breath, lightheadedness and angina or chest pain. Early interventions and
diagnosis of the condition was done through performing electrocardiogram, which enabled initial
management of the cardiac discomfort. The patient was given nitroglycerin in sublingual form in
successive dosages along with morphine. This drug treatment, intended to improve the condition,
however, further resulted in deterioration of the patient’s condition with reduction of blood rate,
hypotension and reduced preload of myocardial oxygen demand followed by lethargy. A review
of the patient’s clinical condition confirmed that increased heart rate (HR 133), decreased blood
pressure (BP 87/53) and reduced level of myocardial oxygen saturation (SPO2 88%) are mainly
the elements of deterioration in the patient’s condition. According to NSW Health Between the
Flags, indication of these elements of deterioration require a clinical review by nursing officials
to assess the root of deterioration of clinical treatment (Hughes et al., 2014). Based on clinical
review in the given case study, an increased requirement of myocardial oxygen is required to
improve the hypoxic condition. The nursing assessment of the Mr. Lee needs to be performed to
identify whether the deterioration has occurred due to drug overdose or any new clinical
symptom. If these clinical review and identification of deteriorating causes do not result in
improved patient condition in the following one hour, then a rapid response team would be
required to handle the situation (Chen et al., 2014). In the given case study of Mr. Lee, frequent
assessment by nurses is essential for the following one hour post clinical review.
ISBAR communication
I (Identity) Health nurse attending Mr. Lee post drug
2MYOCARDIAL INFARCTION: CASE STUDY
treatment in Coronary care unit.
S (Situation) The patient, Mr. Jae Kwang Lee, a 65-year
old man has admitted with severity of
conditions; He reported that he felt an
increasing chest heaviness which moved to
his left arm. He was constantly rubbing both
his chest and arm, trying to get some relief
from the discomfort. On further questioning,
shortness of breath and mild dizziness were
also reported with lightheadedness. He was
immediately admitted in the emergency
section and electrocardiogram was performed
which confirmed that he had been suffering
from myocardial infarction. He had been
given nitroglycerin in sublingual form
followed by morphine administration as the
first line of treatment. Nitroglycerin showed
no effect after administration, whereas
morphine showed a number of responses.
ECG before drug treatment confirmed blood
pressure of 108/73 and a myocardial oxygen
demand of 95%.
B (Background) Mr. Lee reported that he had been having a
treatment in Coronary care unit.
S (Situation) The patient, Mr. Jae Kwang Lee, a 65-year
old man has admitted with severity of
conditions; He reported that he felt an
increasing chest heaviness which moved to
his left arm. He was constantly rubbing both
his chest and arm, trying to get some relief
from the discomfort. On further questioning,
shortness of breath and mild dizziness were
also reported with lightheadedness. He was
immediately admitted in the emergency
section and electrocardiogram was performed
which confirmed that he had been suffering
from myocardial infarction. He had been
given nitroglycerin in sublingual form
followed by morphine administration as the
first line of treatment. Nitroglycerin showed
no effect after administration, whereas
morphine showed a number of responses.
ECG before drug treatment confirmed blood
pressure of 108/73 and a myocardial oxygen
demand of 95%.
B (Background) Mr. Lee reported that he had been having a
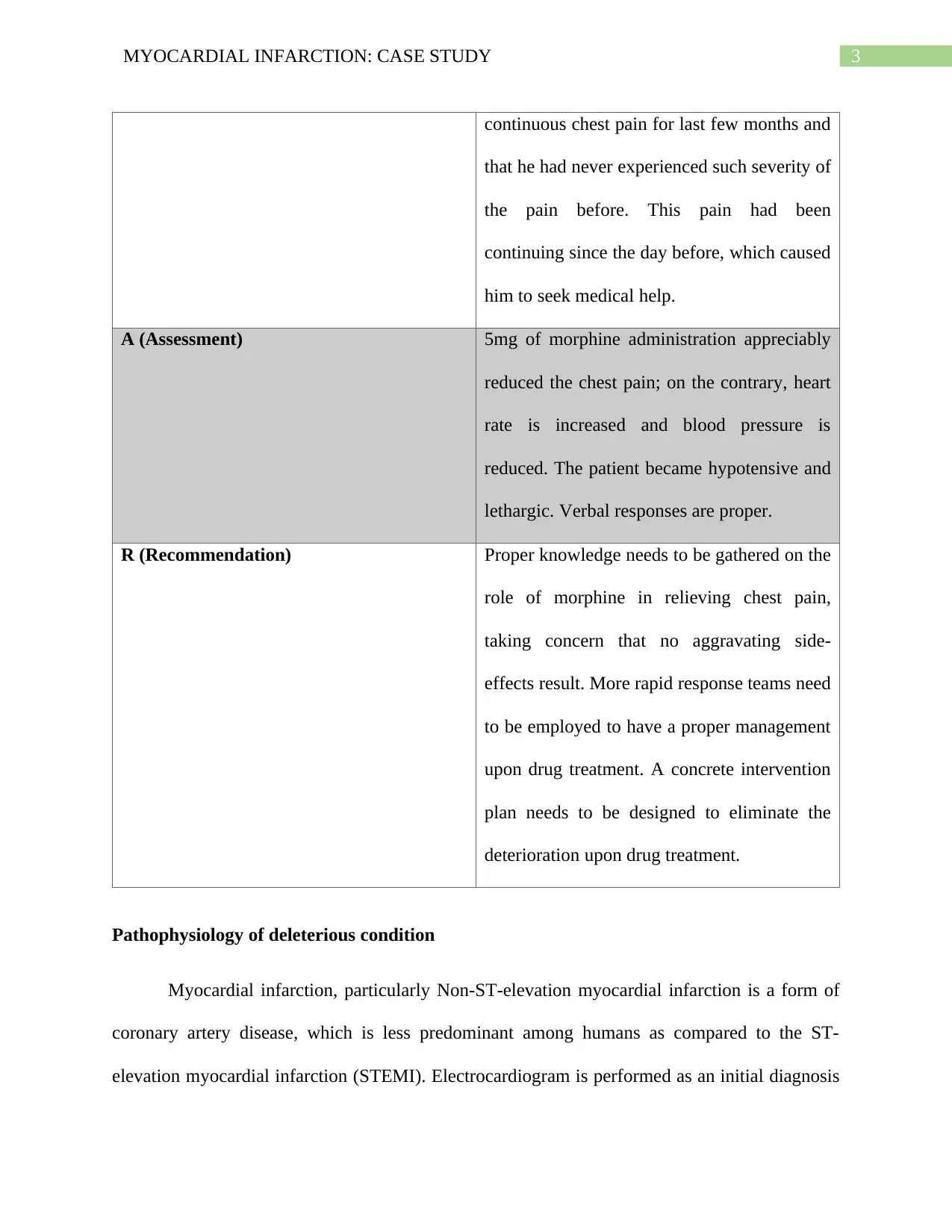
3MYOCARDIAL INFARCTION: CASE STUDY
continuous chest pain for last few months and
that he had never experienced such severity of
the pain before. This pain had been
continuing since the day before, which caused
him to seek medical help.
A (Assessment) 5mg of morphine administration appreciably
reduced the chest pain; on the contrary, heart
rate is increased and blood pressure is
reduced. The patient became hypotensive and
lethargic. Verbal responses are proper.
R (Recommendation) Proper knowledge needs to be gathered on the
role of morphine in relieving chest pain,
taking concern that no aggravating side-
effects result. More rapid response teams need
to be employed to have a proper management
upon drug treatment. A concrete intervention
plan needs to be designed to eliminate the
deterioration upon drug treatment.
Pathophysiology of deleterious condition
Myocardial infarction, particularly Non-ST-elevation myocardial infarction is a form of
coronary artery disease, which is less predominant among humans as compared to the ST-
elevation myocardial infarction (STEMI). Electrocardiogram is performed as an initial diagnosis
continuous chest pain for last few months and
that he had never experienced such severity of
the pain before. This pain had been
continuing since the day before, which caused
him to seek medical help.
A (Assessment) 5mg of morphine administration appreciably
reduced the chest pain; on the contrary, heart
rate is increased and blood pressure is
reduced. The patient became hypotensive and
lethargic. Verbal responses are proper.
R (Recommendation) Proper knowledge needs to be gathered on the
role of morphine in relieving chest pain,
taking concern that no aggravating side-
effects result. More rapid response teams need
to be employed to have a proper management
upon drug treatment. A concrete intervention
plan needs to be designed to eliminate the
deterioration upon drug treatment.
Pathophysiology of deleterious condition
Myocardial infarction, particularly Non-ST-elevation myocardial infarction is a form of
coronary artery disease, which is less predominant among humans as compared to the ST-
elevation myocardial infarction (STEMI). Electrocardiogram is performed as an initial diagnosis
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4MYOCARDIAL INFARCTION: CASE STUDY
in both the forms of heart attack. In non-ST elevation myocardial infarction, the
electrocardiogram does not show any alteration in the ST segment, which indicates that the
patient is suffering from temporary or partial blockages of coronary arteries and is unlikely to be
serious as compared to the ST-elevation myocardial infarction. Chest discomfort or ischemic
pain which is not localized is a common symptom as have been reported in the given case study.
Shortness of breath, mental dizziness, lightheadedness are commonly noted during the
pathological condition. Chest discomfort and shortness of breath continues for a while; therefore
relieving the chest discomfort or angina is the primary concern in treating myocardial infarction.
High blood pressure or bradycardia is observed which causes discomfort to the patient. Initial
diagnosis involves performing an electrocardiogram (ECG) which shows the severity of the
condition, depending on which medications are prescribed.
The patient, Mr. Lee has been administered with short term dosage of nitroglycerine in
the form of sublingual tablet or spray of GTN in order to relieve the chest pain the patient was
suffering from. However, the nitroglycerin produced no noticeable effect in ameliorating the
patient’s symptoms. After two doses of sublingual GTN, Mr. Lee was administered with 5mg of
morphine. Nitroglycerine alone or in combination with morphine is the first line of therapy in
myocardial infarction (Bellandi et al., 2016). Morphine showed considerable effects in the
patient’s level of discomfort within 2 hours of administration. Morphine is administered to
reduce the chest pain or angina, which is achieved in the reported case of Mr. Lee. However, the
patient Mr. Lee suffers from cardiogenic shock after drug treatment as confirmed through
assessment post drug administration. A deterioration of the patient condition has been observed;
bradycardia which is reduced blood pressure, hypotensive nature and a reduced myocardial
demand of oxygen with pO2 being 88% are concerning signs of cardiogenic shock. Cardiogenic
in both the forms of heart attack. In non-ST elevation myocardial infarction, the
electrocardiogram does not show any alteration in the ST segment, which indicates that the
patient is suffering from temporary or partial blockages of coronary arteries and is unlikely to be
serious as compared to the ST-elevation myocardial infarction. Chest discomfort or ischemic
pain which is not localized is a common symptom as have been reported in the given case study.
Shortness of breath, mental dizziness, lightheadedness are commonly noted during the
pathological condition. Chest discomfort and shortness of breath continues for a while; therefore
relieving the chest discomfort or angina is the primary concern in treating myocardial infarction.
High blood pressure or bradycardia is observed which causes discomfort to the patient. Initial
diagnosis involves performing an electrocardiogram (ECG) which shows the severity of the
condition, depending on which medications are prescribed.
The patient, Mr. Lee has been administered with short term dosage of nitroglycerine in
the form of sublingual tablet or spray of GTN in order to relieve the chest pain the patient was
suffering from. However, the nitroglycerin produced no noticeable effect in ameliorating the
patient’s symptoms. After two doses of sublingual GTN, Mr. Lee was administered with 5mg of
morphine. Nitroglycerine alone or in combination with morphine is the first line of therapy in
myocardial infarction (Bellandi et al., 2016). Morphine showed considerable effects in the
patient’s level of discomfort within 2 hours of administration. Morphine is administered to
reduce the chest pain or angina, which is achieved in the reported case of Mr. Lee. However, the
patient Mr. Lee suffers from cardiogenic shock after drug treatment as confirmed through
assessment post drug administration. A deterioration of the patient condition has been observed;
bradycardia which is reduced blood pressure, hypotensive nature and a reduced myocardial
demand of oxygen with pO2 being 88% are concerning signs of cardiogenic shock. Cardiogenic
5MYOCARDIAL INFARCTION: CASE STUDY
shock in myocardial infarction occurs as a result of cardiac dysfunction involving both systolic
and diastolic dysfunction. In myocardial infarction, the left ventricular diastole shows an
increased pressure. Myocardial perfusion continues during diastolic event and is dependent on
the pressure difference between aortic diastole and left ventricle (Heusch & Gersh, 2016). As a
result of myocardial infarction, coronary perfusion shows a decreasing trend due to decreased
pressure in aortic diastole and subsequent increase in left ventricular pressure. This is associated
with a progressive event of ischemia. In response to decreased coronary perfusion, the heart rate
increases in order to increase the myocardial demand of oxygen (Cooper & Panza, 2013). In
relation to Mr. Lee’s condition, increased heart rate (HR 133) occurs to increase the oxygen
demand in the hypoxic condition. Increased heart rate, in turn directly affects coronary perfusion.
Dilation of coronary blood vessels reduces the blood pressure (bradycardia) (Kubica et al.,
2015). In relation to the given case study, lower blood pressure reduces the cardiac preload of
oxygen, minimizing the pO2 at 88% as observed in Mr. Lee. The time of diastolic event
increases with the increase in heart rate. Therefore, the time of tissue perfusion dramatically
decreases leading to further manifestation of ischemia of inner membrane of the heart. Hypoxic
condition and lethargy in Mr. Lee are the resultant of the pathophysiological cycle of cardiogenic
shock.
shock in myocardial infarction occurs as a result of cardiac dysfunction involving both systolic
and diastolic dysfunction. In myocardial infarction, the left ventricular diastole shows an
increased pressure. Myocardial perfusion continues during diastolic event and is dependent on
the pressure difference between aortic diastole and left ventricle (Heusch & Gersh, 2016). As a
result of myocardial infarction, coronary perfusion shows a decreasing trend due to decreased
pressure in aortic diastole and subsequent increase in left ventricular pressure. This is associated
with a progressive event of ischemia. In response to decreased coronary perfusion, the heart rate
increases in order to increase the myocardial demand of oxygen (Cooper & Panza, 2013). In
relation to Mr. Lee’s condition, increased heart rate (HR 133) occurs to increase the oxygen
demand in the hypoxic condition. Increased heart rate, in turn directly affects coronary perfusion.
Dilation of coronary blood vessels reduces the blood pressure (bradycardia) (Kubica et al.,
2015). In relation to the given case study, lower blood pressure reduces the cardiac preload of
oxygen, minimizing the pO2 at 88% as observed in Mr. Lee. The time of diastolic event
increases with the increase in heart rate. Therefore, the time of tissue perfusion dramatically
decreases leading to further manifestation of ischemia of inner membrane of the heart. Hypoxic
condition and lethargy in Mr. Lee are the resultant of the pathophysiological cycle of cardiogenic
shock.
6MYOCARDIAL INFARCTION: CASE STUDY
References
Bellandi, B., Zocchi, C., Xanthopoulou, I., Scudiero, F., Valenti, R., Migliorini, A.,. & Parodi, G.
(2016). Morphine use and myocardial reperfusion in patients with acute myocardial
infarction treated with primary PCI. International journal of cardiology, 221, 567-571.
Chen, J., Ou, L., Hillman, K., Flabouris, A., Bellomo, R., Hollis, S. J., & Assareh, H. (2014).
The impact of implementing a rapid response system: a comparison of cardiopulmonary
arrests and mortality among four teaching hospitals in Australia. Resuscitation, 85(9),
1275-1281.
Cooper, H. A., & Panza, J. A. (2013). Cardiogenic shock. Cardiology clinics, 31(4), 567-580.
Heusch, G., & Gersh, B. J. (2016). The pathophysiology of acute myocardial infarction and
strategies of protection beyond reperfusion: a continual challenge. European heart
journal, 38(11), 774-784.
Hughes, C., Pain, C., Braithwaite, J., & Hillman, K. (2014). ‘Between the flags’: implementing a
rapid response system at scale. BMJ Qual Saf, bmjqs-2014.
Kubica, J., Adamski, P., Ostrowska, M., Sikora, J., Kubica, J. M., Sroka, W. D., & Siller-Matula,
J. M. (2015). Morphine delays and attenuates ticagrelor exposure and action in patients
with myocardial infarction: the randomized, double-blind, placebo-controlled
IMPRESSION trial. European heart journal, 37(3), 245-252.
References
Bellandi, B., Zocchi, C., Xanthopoulou, I., Scudiero, F., Valenti, R., Migliorini, A.,. & Parodi, G.
(2016). Morphine use and myocardial reperfusion in patients with acute myocardial
infarction treated with primary PCI. International journal of cardiology, 221, 567-571.
Chen, J., Ou, L., Hillman, K., Flabouris, A., Bellomo, R., Hollis, S. J., & Assareh, H. (2014).
The impact of implementing a rapid response system: a comparison of cardiopulmonary
arrests and mortality among four teaching hospitals in Australia. Resuscitation, 85(9),
1275-1281.
Cooper, H. A., & Panza, J. A. (2013). Cardiogenic shock. Cardiology clinics, 31(4), 567-580.
Heusch, G., & Gersh, B. J. (2016). The pathophysiology of acute myocardial infarction and
strategies of protection beyond reperfusion: a continual challenge. European heart
journal, 38(11), 774-784.
Hughes, C., Pain, C., Braithwaite, J., & Hillman, K. (2014). ‘Between the flags’: implementing a
rapid response system at scale. BMJ Qual Saf, bmjqs-2014.
Kubica, J., Adamski, P., Ostrowska, M., Sikora, J., Kubica, J. M., Sroka, W. D., & Siller-Matula,
J. M. (2015). Morphine delays and attenuates ticagrelor exposure and action in patients
with myocardial infarction: the randomized, double-blind, placebo-controlled
IMPRESSION trial. European heart journal, 37(3), 245-252.
1 out of 7
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





