Health Promotion Evidence Critique Report: Indigenous Australians
VerifiedAdded on 2022/08/21
|3
|1736
|13
Report
AI Summary
This report critically analyzes health promotion strategies, specifically focusing on the health challenges faced by Indigenous Australians. It examines the elevated burden of illness, including psychiatric disorders, and the unique mental health needs of this population. The report explores the use of proportional rate surrogate tests due to the lack of regional statistics, referencing the PRISMA approach for institutional search. It highlights the increased incidence of psychiatric illnesses and behavioral disorders in Indigenous communities. Furthermore, the report delves into the relevance of health promotion messages, the application of the Ottawa Charter's strategies (enable, mediate, advocate), and how this knowledge can be utilized in future nursing practice. The report also addresses the impact of suicide and non-suicidal self-injury, the importance of Mental Health First Aid, and the integration of cultural competencies in mental health treatment. It emphasizes the need for culturally appropriate curriculum design, audit mechanisms, and strategic effort by policy and health agencies to incorporate preparation. The report references various studies and guidelines, including those for supporting Indigenous Australians experiencing suicidal thoughts and behaviors, and non-suicidal self-injury.
Sed ut perspiciatis unde
omnis iste ntus rror sit
Company
Brochure
Contact@companyemail.com
8549 Primrose Rd.
Menomonee Falls, WI 53051
Call +1-202-555-0126
Contact us
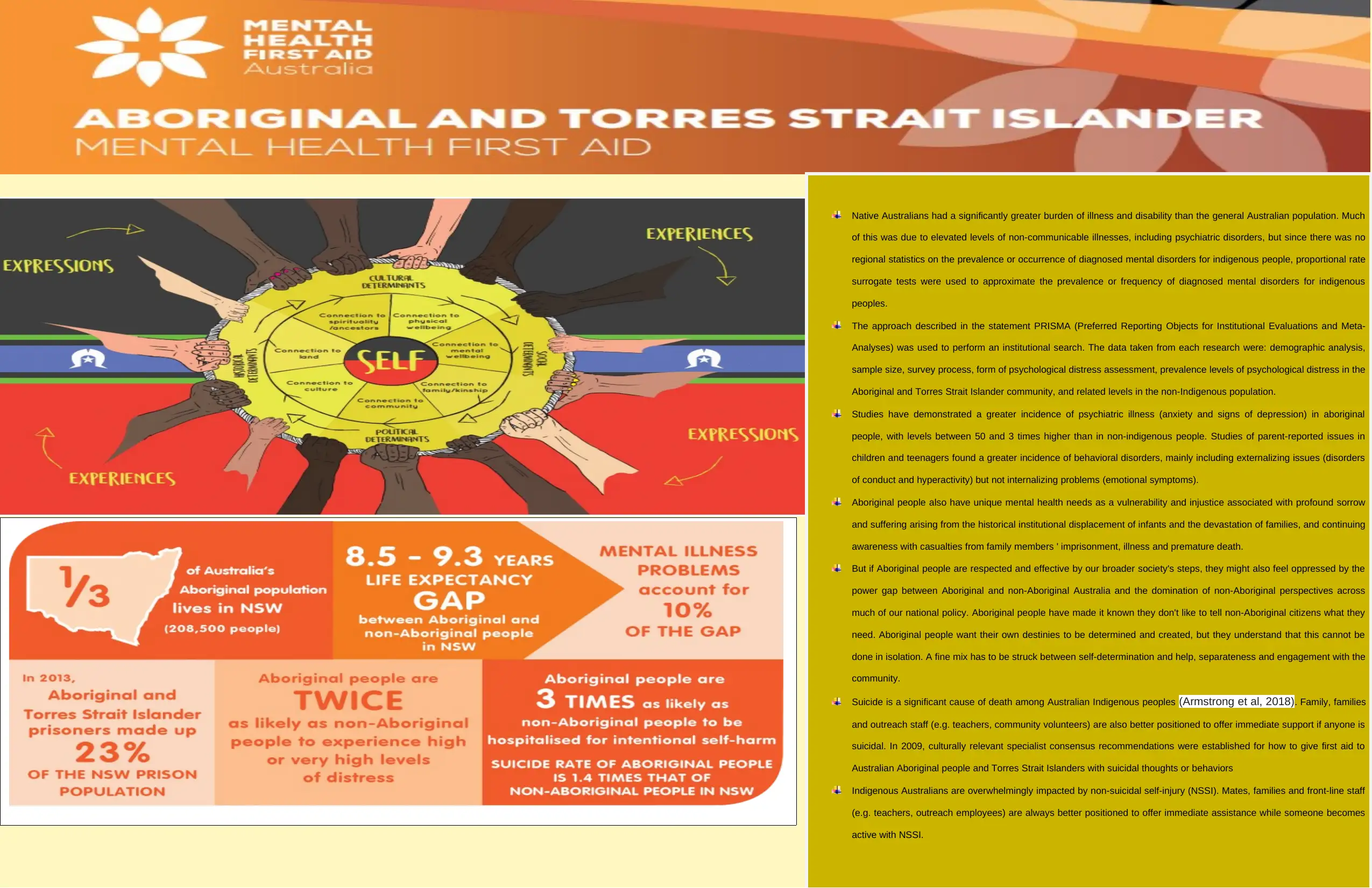
Native Australians had a significantly greater burden of illness and disability than the general Australian population. Much
of this was due to elevated levels of non-communicable illnesses, including psychiatric disorders, but since there was no
regional statistics on the prevalence or occurrence of diagnosed mental disorders for indigenous people, proportional rate
surrogate tests were used to approximate the prevalence or frequency of diagnosed mental disorders for indigenous
peoples.
The approach described in the statement PRISMA (Preferred Reporting Objects for Institutional Evaluations and Meta-
Analyses) was used to perform an institutional search. The data taken from each research were: demographic analysis,
sample size, survey process, form of psychological distress assessment, prevalence levels of psychological distress in the
Aboriginal and Torres Strait Islander community, and related levels in the non-Indigenous population.
Studies have demonstrated a greater incidence of psychiatric illness (anxiety and signs of depression) in aboriginal
people, with levels between 50 and 3 times higher than in non-indigenous people. Studies of parent-reported issues in
children and teenagers found a greater incidence of behavioral disorders, mainly including externalizing issues (disorders
of conduct and hyperactivity) but not internalizing problems (emotional symptoms).
Aboriginal people also have unique mental health needs as a vulnerability and injustice associated with profound sorrow
and suffering arising from the historical institutional displacement of infants and the devastation of families, and continuing
awareness with casualties from family members ' imprisonment, illness and premature death.
But if Aboriginal people are respected and effective by our broader society's steps, they might also feel oppressed by the
power gap between Aboriginal and non-Aboriginal Australia and the domination of non-Aboriginal perspectives across
much of our national policy. Aboriginal people have made it known they don't like to tell non-Aboriginal citizens what they
need. Aboriginal people want their own destinies to be determined and created, but they understand that this cannot be
done in isolation. A fine mix has to be struck between self-determination and help, separateness and engagement with the
community.
Suicide is a significant cause of death among Australian Indigenous peoples (Armstrong et al, 2018). Family, families
and outreach staff (e.g. teachers, community volunteers) are also better positioned to offer immediate support if anyone is
suicidal. In 2009, culturally relevant specialist consensus recommendations were established for how to give first aid to
Australian Aboriginal people and Torres Strait Islanders with suicidal thoughts or behaviors
Indigenous Australians are overwhelmingly impacted by non-suicidal self-injury (NSSI). Mates, families and front-line staff
(e.g. teachers, outreach employees) are always better positioned to offer immediate assistance while someone becomes
active with NSSI.
omnis iste ntus rror sit
Company
Brochure
Contact@companyemail.com
8549 Primrose Rd.
Menomonee Falls, WI 53051
Call +1-202-555-0126
Contact us
Native Australians had a significantly greater burden of illness and disability than the general Australian population. Much
of this was due to elevated levels of non-communicable illnesses, including psychiatric disorders, but since there was no
regional statistics on the prevalence or occurrence of diagnosed mental disorders for indigenous people, proportional rate
surrogate tests were used to approximate the prevalence or frequency of diagnosed mental disorders for indigenous
peoples.
The approach described in the statement PRISMA (Preferred Reporting Objects for Institutional Evaluations and Meta-
Analyses) was used to perform an institutional search. The data taken from each research were: demographic analysis,
sample size, survey process, form of psychological distress assessment, prevalence levels of psychological distress in the
Aboriginal and Torres Strait Islander community, and related levels in the non-Indigenous population.
Studies have demonstrated a greater incidence of psychiatric illness (anxiety and signs of depression) in aboriginal
people, with levels between 50 and 3 times higher than in non-indigenous people. Studies of parent-reported issues in
children and teenagers found a greater incidence of behavioral disorders, mainly including externalizing issues (disorders
of conduct and hyperactivity) but not internalizing problems (emotional symptoms).
Aboriginal people also have unique mental health needs as a vulnerability and injustice associated with profound sorrow
and suffering arising from the historical institutional displacement of infants and the devastation of families, and continuing
awareness with casualties from family members ' imprisonment, illness and premature death.
But if Aboriginal people are respected and effective by our broader society's steps, they might also feel oppressed by the
power gap between Aboriginal and non-Aboriginal Australia and the domination of non-Aboriginal perspectives across
much of our national policy. Aboriginal people have made it known they don't like to tell non-Aboriginal citizens what they
need. Aboriginal people want their own destinies to be determined and created, but they understand that this cannot be
done in isolation. A fine mix has to be struck between self-determination and help, separateness and engagement with the
community.
Suicide is a significant cause of death among Australian Indigenous peoples (Armstrong et al, 2018). Family, families
and outreach staff (e.g. teachers, community volunteers) are also better positioned to offer immediate support if anyone is
suicidal. In 2009, culturally relevant specialist consensus recommendations were established for how to give first aid to
Australian Aboriginal people and Torres Strait Islanders with suicidal thoughts or behaviors
Indigenous Australians are overwhelmingly impacted by non-suicidal self-injury (NSSI). Mates, families and front-line staff
(e.g. teachers, outreach employees) are always better positioned to offer immediate assistance while someone becomes
active with NSSI.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
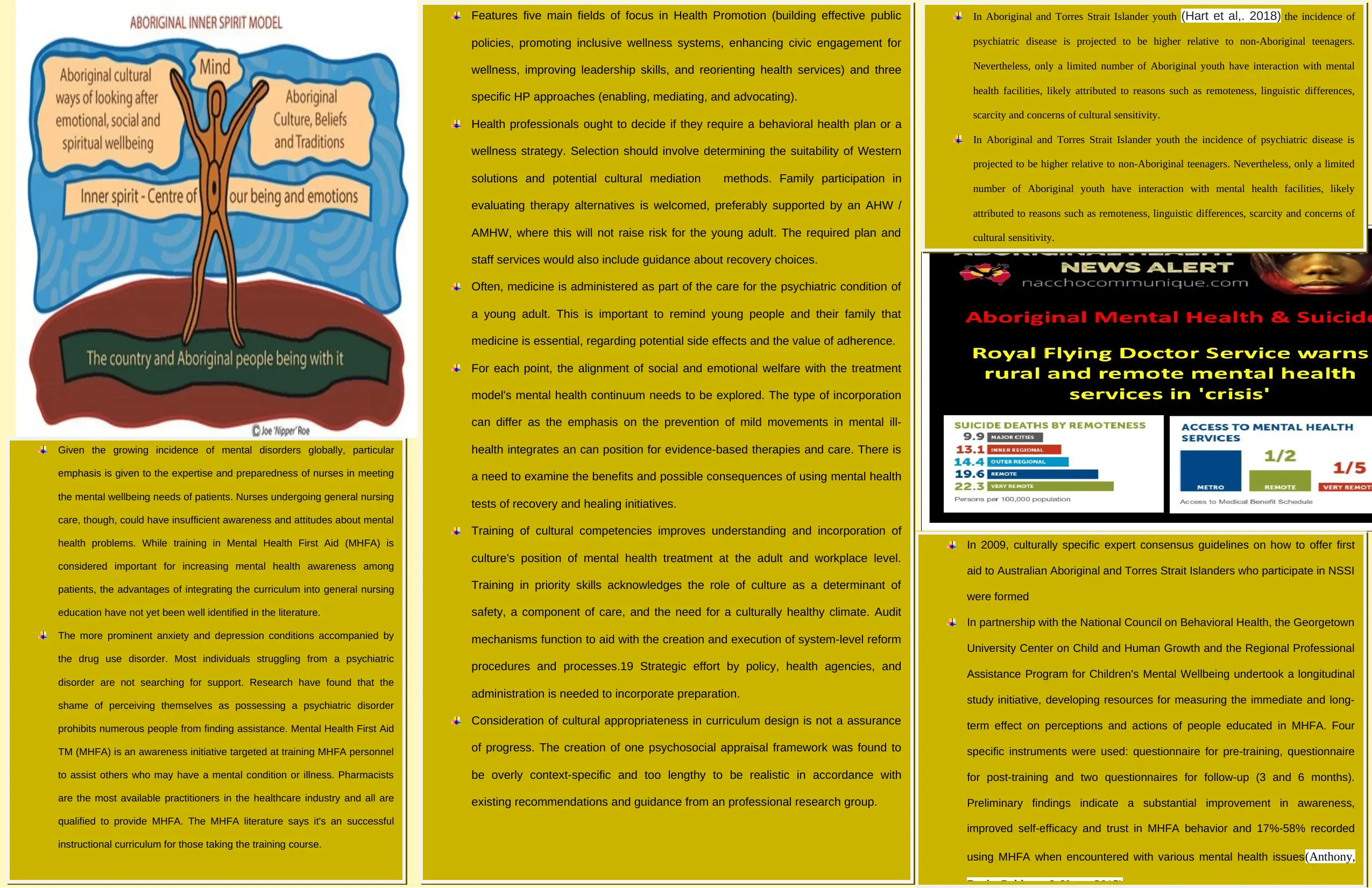
Features five main fields of focus in Health Promotion (building effective public
policies, promoting inclusive wellness systems, enhancing civic engagement for
wellness, improving leadership skills, and reorienting health services) and three
specific HP approaches (enabling, mediating, and advocating).
Health professionals ought to decide if they require a behavioral health plan or a
wellness strategy. Selection should involve determining the suitability of Western
solutions and potential cultural mediation methods. Family participation in
evaluating therapy alternatives is welcomed, preferably supported by an AHW /
AMHW, where this will not raise risk for the young adult. The required plan and
staff services would also include guidance about recovery choices.
Often, medicine is administered as part of the care for the psychiatric condition of
a young adult. This is important to remind young people and their family that
medicine is essential, regarding potential side effects and the value of adherence.
For each point, the alignment of social and emotional welfare with the treatment
model's mental health continuum needs to be explored. The type of incorporation
can differ as the emphasis on the prevention of mild movements in mental ill-
health integrates an can position for evidence-based therapies and care. There is
a need to examine the benefits and possible consequences of using mental health
tests of recovery and healing initiatives.
Training of cultural competencies improves understanding and incorporation of
culture's position of mental health treatment at the adult and workplace level.
Training in priority skills acknowledges the role of culture as a determinant of
safety, a component of care, and the need for a culturally healthy climate. Audit
mechanisms function to aid with the creation and execution of system-level reform
procedures and processes.19 Strategic effort by policy, health agencies, and
administration is needed to incorporate preparation.
Consideration of cultural appropriateness in curriculum design is not a assurance
of progress. The creation of one psychosocial appraisal framework was found to
be overly context-specific and too lengthy to be realistic in accordance with
existing recommendations and guidance from an professional research group.
Given the growing incidence of mental disorders globally, particular
emphasis is given to the expertise and preparedness of nurses in meeting
the mental wellbeing needs of patients. Nurses undergoing general nursing
care, though, could have insufficient awareness and attitudes about mental
health problems. While training in Mental Health First Aid (MHFA) is
considered important for increasing mental health awareness among
patients, the advantages of integrating the curriculum into general nursing
education have not yet been well identified in the literature.
The more prominent anxiety and depression conditions accompanied by
the drug use disorder. Most individuals struggling from a psychiatric
disorder are not searching for support. Research have found that the
shame of perceiving themselves as possessing a psychiatric disorder
prohibits numerous people from finding assistance. Mental Health First Aid
TM (MHFA) is an awareness initiative targeted at training MHFA personnel
to assist others who may have a mental condition or illness. Pharmacists
are the most available practitioners in the healthcare industry and all are
qualified to provide MHFA. The MHFA literature says it's an successful
instructional curriculum for those taking the training course.
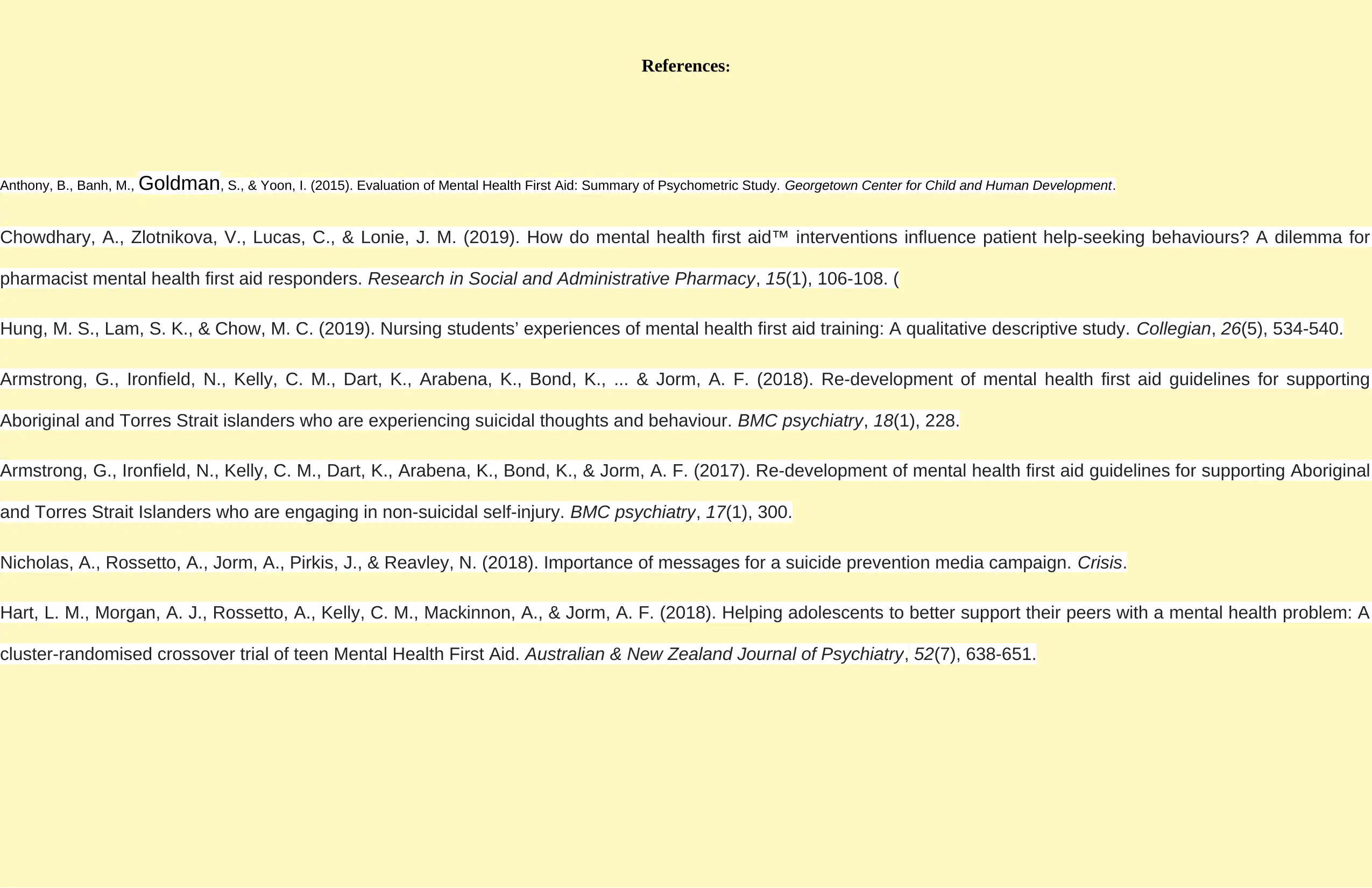
In 2009, culturally specific expert consensus guidelines on how to offer first
aid to Australian Aboriginal and Torres Strait Islanders who participate in NSSI
were formed
In partnership with the National Council on Behavioral Health, the Georgetown
University Center on Child and Human Growth and the Regional Professional
Assistance Program for Children's Mental Wellbeing undertook a longitudinal
study initiative, developing resources for measuring the immediate and long-
term effect on perceptions and actions of people educated in MHFA. Four
specific instruments were used: questionnaire for pre-training, questionnaire
for post-training and two questionnaires for follow-up (3 and 6 months).
Preliminary findings indicate a substantial improvement in awareness,
improved self-efficacy and trust in MHFA behavior and 17%-58% recorded
using MHFA when encountered with various mental health issues(Anthony,
In Aboriginal and Torres Strait Islander youth (Hart et al,. 2018) the incidence of
psychiatric disease is projected to be higher relative to non-Aboriginal teenagers.
Nevertheless, only a limited number of Aboriginal youth have interaction with mental
health facilities, likely attributed to reasons such as remoteness, linguistic differences,
scarcity and concerns of cultural sensitivity.
In Aboriginal and Torres Strait Islander youth the incidence of psychiatric disease is
projected to be higher relative to non-Aboriginal teenagers. Nevertheless, only a limited
number of Aboriginal youth have interaction with mental health facilities, likely
attributed to reasons such as remoteness, linguistic differences, scarcity and concerns of
cultural sensitivity.
policies, promoting inclusive wellness systems, enhancing civic engagement for
wellness, improving leadership skills, and reorienting health services) and three
specific HP approaches (enabling, mediating, and advocating).
Health professionals ought to decide if they require a behavioral health plan or a
wellness strategy. Selection should involve determining the suitability of Western
solutions and potential cultural mediation methods. Family participation in
evaluating therapy alternatives is welcomed, preferably supported by an AHW /
AMHW, where this will not raise risk for the young adult. The required plan and
staff services would also include guidance about recovery choices.
Often, medicine is administered as part of the care for the psychiatric condition of
a young adult. This is important to remind young people and their family that
medicine is essential, regarding potential side effects and the value of adherence.
For each point, the alignment of social and emotional welfare with the treatment
model's mental health continuum needs to be explored. The type of incorporation
can differ as the emphasis on the prevention of mild movements in mental ill-
health integrates an can position for evidence-based therapies and care. There is
a need to examine the benefits and possible consequences of using mental health
tests of recovery and healing initiatives.
Training of cultural competencies improves understanding and incorporation of
culture's position of mental health treatment at the adult and workplace level.
Training in priority skills acknowledges the role of culture as a determinant of
safety, a component of care, and the need for a culturally healthy climate. Audit
mechanisms function to aid with the creation and execution of system-level reform
procedures and processes.19 Strategic effort by policy, health agencies, and
administration is needed to incorporate preparation.
Consideration of cultural appropriateness in curriculum design is not a assurance
of progress. The creation of one psychosocial appraisal framework was found to
be overly context-specific and too lengthy to be realistic in accordance with
existing recommendations and guidance from an professional research group.
Given the growing incidence of mental disorders globally, particular
emphasis is given to the expertise and preparedness of nurses in meeting
the mental wellbeing needs of patients. Nurses undergoing general nursing
care, though, could have insufficient awareness and attitudes about mental
health problems. While training in Mental Health First Aid (MHFA) is
considered important for increasing mental health awareness among
patients, the advantages of integrating the curriculum into general nursing
education have not yet been well identified in the literature.
The more prominent anxiety and depression conditions accompanied by
the drug use disorder. Most individuals struggling from a psychiatric
disorder are not searching for support. Research have found that the
shame of perceiving themselves as possessing a psychiatric disorder
prohibits numerous people from finding assistance. Mental Health First Aid
TM (MHFA) is an awareness initiative targeted at training MHFA personnel
to assist others who may have a mental condition or illness. Pharmacists
are the most available practitioners in the healthcare industry and all are
qualified to provide MHFA. The MHFA literature says it's an successful
instructional curriculum for those taking the training course.
In 2009, culturally specific expert consensus guidelines on how to offer first
aid to Australian Aboriginal and Torres Strait Islanders who participate in NSSI
were formed
In partnership with the National Council on Behavioral Health, the Georgetown
University Center on Child and Human Growth and the Regional Professional
Assistance Program for Children's Mental Wellbeing undertook a longitudinal
study initiative, developing resources for measuring the immediate and long-
term effect on perceptions and actions of people educated in MHFA. Four
specific instruments were used: questionnaire for pre-training, questionnaire
for post-training and two questionnaires for follow-up (3 and 6 months).
Preliminary findings indicate a substantial improvement in awareness,
improved self-efficacy and trust in MHFA behavior and 17%-58% recorded
using MHFA when encountered with various mental health issues(Anthony,
In Aboriginal and Torres Strait Islander youth (Hart et al,. 2018) the incidence of
psychiatric disease is projected to be higher relative to non-Aboriginal teenagers.
Nevertheless, only a limited number of Aboriginal youth have interaction with mental
health facilities, likely attributed to reasons such as remoteness, linguistic differences,
scarcity and concerns of cultural sensitivity.
In Aboriginal and Torres Strait Islander youth the incidence of psychiatric disease is
projected to be higher relative to non-Aboriginal teenagers. Nevertheless, only a limited
number of Aboriginal youth have interaction with mental health facilities, likely
attributed to reasons such as remoteness, linguistic differences, scarcity and concerns of
cultural sensitivity.
References:
Anthony, B., Banh, M., Goldman, S., & Yoon, I. (2015). Evaluation of Mental Health First Aid: Summary of Psychometric Study. Georgetown Center for Child and Human Development.
Chowdhary, A., Zlotnikova, V., Lucas, C., & Lonie, J. M. (2019). How do mental health first aid™ interventions influence patient help-seeking behaviours? A dilemma for
pharmacist mental health first aid responders. Research in Social and Administrative Pharmacy, 15(1), 106-108. (
Hung, M. S., Lam, S. K., & Chow, M. C. (2019). Nursing students’ experiences of mental health first aid training: A qualitative descriptive study. Collegian, 26(5), 534-540.
Armstrong, G., Ironfield, N., Kelly, C. M., Dart, K., Arabena, K., Bond, K., ... & Jorm, A. F. (2018). Re-development of mental health first aid guidelines for supporting
Aboriginal and Torres Strait islanders who are experiencing suicidal thoughts and behaviour. BMC psychiatry, 18(1), 228.
Armstrong, G., Ironfield, N., Kelly, C. M., Dart, K., Arabena, K., Bond, K., & Jorm, A. F. (2017). Re-development of mental health first aid guidelines for supporting Aboriginal
and Torres Strait Islanders who are engaging in non-suicidal self-injury. BMC psychiatry, 17(1), 300.
Nicholas, A., Rossetto, A., Jorm, A., Pirkis, J., & Reavley, N. (2018). Importance of messages for a suicide prevention media campaign. Crisis.
Hart, L. M., Morgan, A. J., Rossetto, A., Kelly, C. M., Mackinnon, A., & Jorm, A. F. (2018). Helping adolescents to better support their peers with a mental health problem: A
cluster-randomised crossover trial of teen Mental Health First Aid. Australian & New Zealand Journal of Psychiatry, 52(7), 638-651.
Anthony, B., Banh, M., Goldman, S., & Yoon, I. (2015). Evaluation of Mental Health First Aid: Summary of Psychometric Study. Georgetown Center for Child and Human Development.
Chowdhary, A., Zlotnikova, V., Lucas, C., & Lonie, J. M. (2019). How do mental health first aid™ interventions influence patient help-seeking behaviours? A dilemma for
pharmacist mental health first aid responders. Research in Social and Administrative Pharmacy, 15(1), 106-108. (
Hung, M. S., Lam, S. K., & Chow, M. C. (2019). Nursing students’ experiences of mental health first aid training: A qualitative descriptive study. Collegian, 26(5), 534-540.
Armstrong, G., Ironfield, N., Kelly, C. M., Dart, K., Arabena, K., Bond, K., ... & Jorm, A. F. (2018). Re-development of mental health first aid guidelines for supporting
Aboriginal and Torres Strait islanders who are experiencing suicidal thoughts and behaviour. BMC psychiatry, 18(1), 228.
Armstrong, G., Ironfield, N., Kelly, C. M., Dart, K., Arabena, K., Bond, K., & Jorm, A. F. (2017). Re-development of mental health first aid guidelines for supporting Aboriginal
and Torres Strait Islanders who are engaging in non-suicidal self-injury. BMC psychiatry, 17(1), 300.
Nicholas, A., Rossetto, A., Jorm, A., Pirkis, J., & Reavley, N. (2018). Importance of messages for a suicide prevention media campaign. Crisis.
Hart, L. M., Morgan, A. J., Rossetto, A., Kelly, C. M., Mackinnon, A., & Jorm, A. F. (2018). Helping adolescents to better support their peers with a mental health problem: A
cluster-randomised crossover trial of teen Mental Health First Aid. Australian & New Zealand Journal of Psychiatry, 52(7), 638-651.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 3
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





