Non Medical Prescribing: Case Study Reflection Template
This publication by The King’s Fund explores the importance of shared decision-making in the health system in England and offers resources to help improve it.
12 Pages2706 Words227 Views
Added on 2022-11-28
About This Document
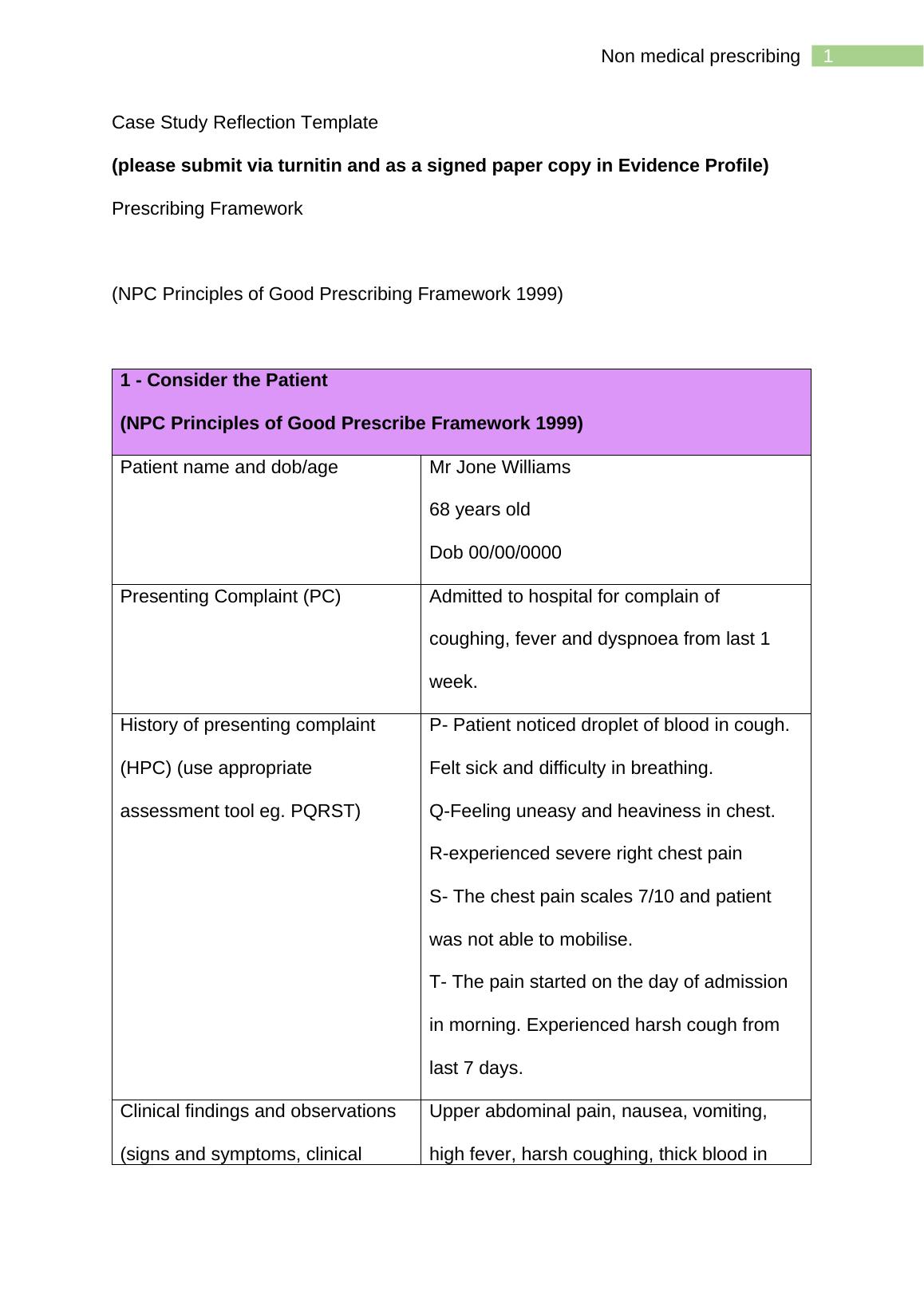
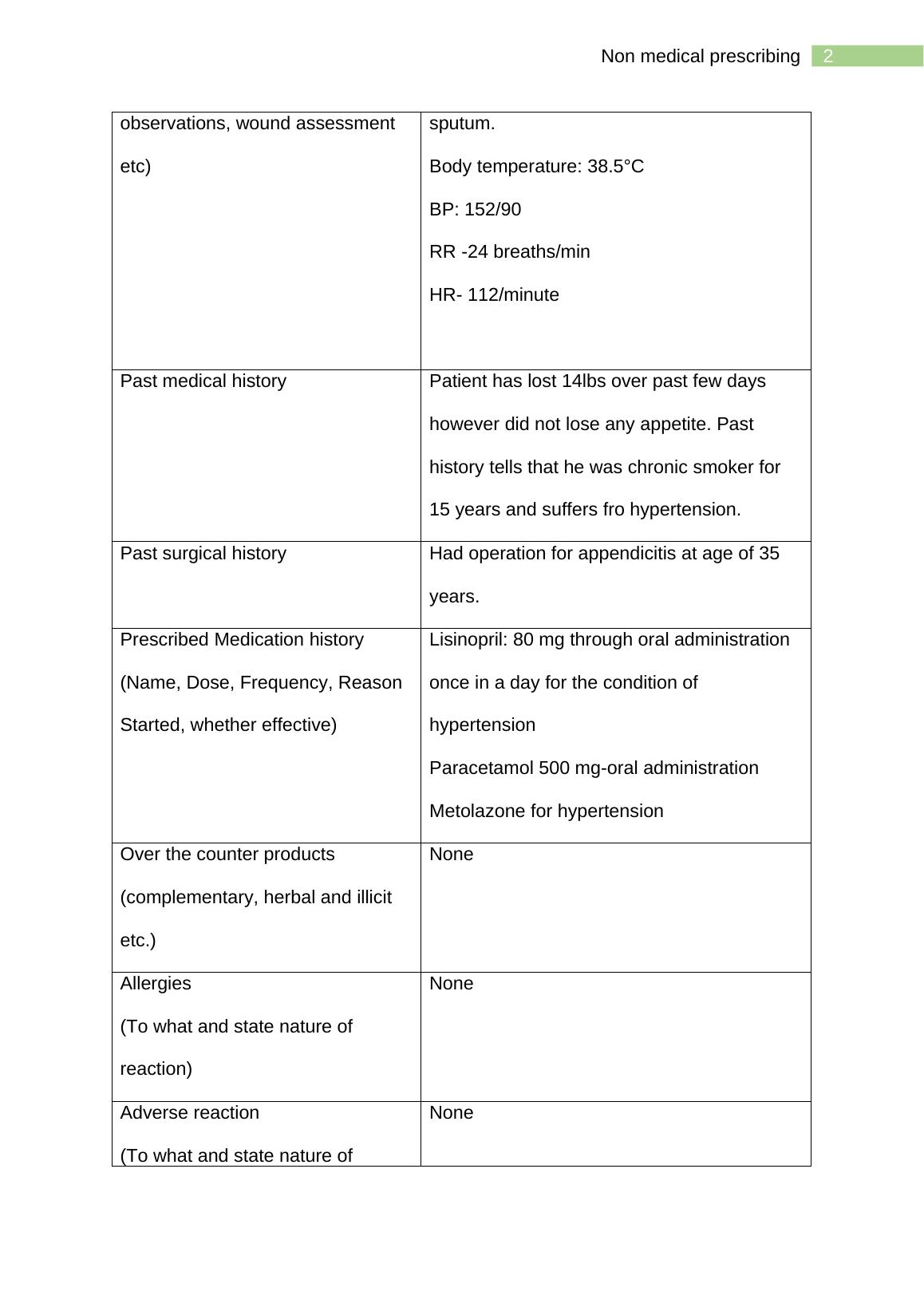
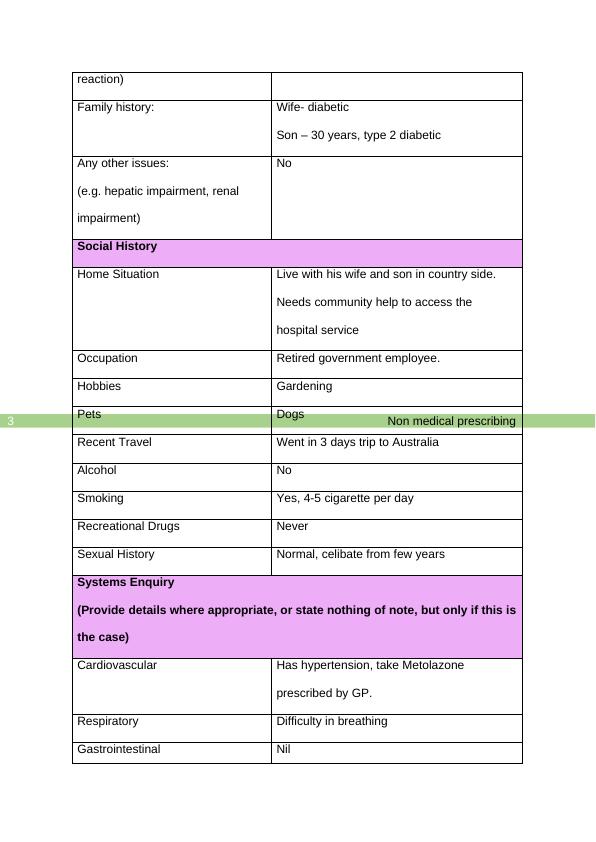
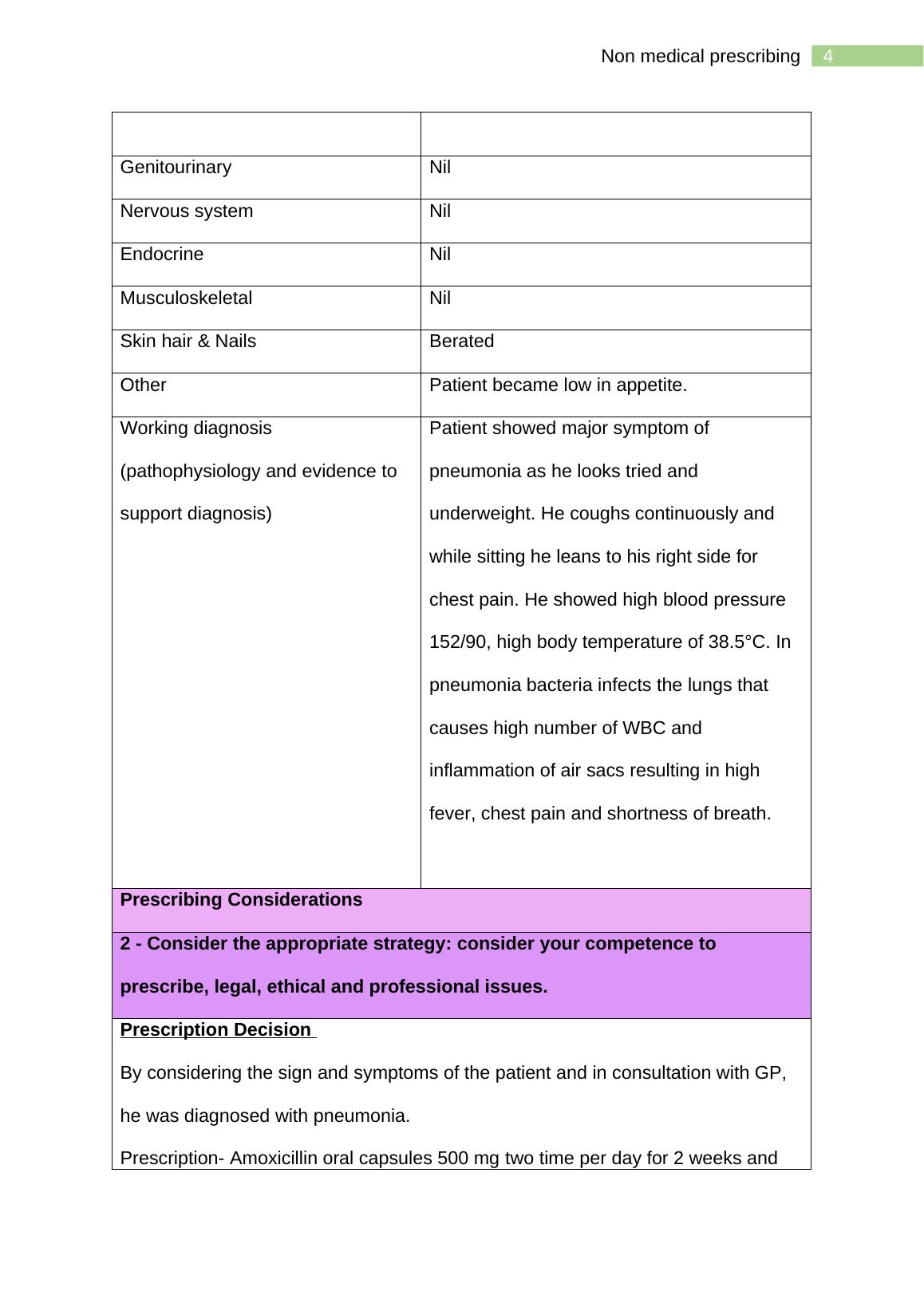
This document is a case study reflection template for non medical prescribing. It includes a prescribing framework, patient information, clinical findings, past medical history, prescribed medication history, and more.
Non Medical Prescribing: Case Study Reflection Template
This publication by The King’s Fund explores the importance of shared decision-making in the health system in England and offers resources to help improve it.
Added on 2022-11-28
ShareRelated Documents
End of preview
Want to access all the pages? Upload your documents or become a member.
Prescribing Considerations
|13
|3155
|53
Case Study Reflection Template
|15
|3773
|26
Nursing Case Study on Sepsis: Pathophysiology, Assessment, and Management
|14
|3573
|231
Case Scenario of an Older Patient.
|17
|4367
|24
Nursing Case Study Analysis | Report
|11
|2938
|32
Case Study: Nursing Care for CHF Exacerbation in an Elderly Patient
|11
|3122
|67