Congestive Heart Failure: Risk Factors, Symptoms, Treatment, and Nursing Interventions
VerifiedAdded on 2023/04/11
|10
|2079
|308
AI Summary
This document provides information on congestive heart failure, including its risk factors, symptoms, treatment options, and nursing interventions. It discusses the importance of medication adherence, monitoring vital signs, and promoting respiratory function. The document also highlights the role of ACE inhibitors in the treatment of congestive heart failure.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
Nrsg 353 Acute Care
1
1
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Q.1.
Congestive heart failure (CHF) is a diseased status in which heart loses its ability to pump the
necessary amount of blood. Insufficient quantity of blood pumping by heart mainly occurs
due to cardiovascular conditions like high blood pressure and constricted arteries (Povsic,
2018). CHF is associated with risk factors like demographic factor like age, social factor
like smoking and inadequate physical activity and biological factors like high blood pressure,
obesity, diabetes and raised levels of cholesterol (Dhingra et al., 2014). In case of Mckenzie
(77 years), age is one of the risk factors for the occurrence of CHF. Probability of CHF
increases with increase in the age of the person. 2 and 5 % individuals upto age 60 and 70
years respectively are at risk of CHF. Moreover, Mckenzie is associated with hypertension.
Hence, it also can contribute to the occurrence of CHF in her. Females with hypertension are
four times at more risk with CHF relative to the normal female. Male and female are 40 and
60 % respectively at risk of CHF (Maahmood and Wang, 2013). High and low levels of low-
density lipoproteins and high-density lipoproteins respectively are responsible for the
occurrence of CHF. More saturated fat intake and β-type natriuretic peptides are also risk
factors of CHF (Díaz-Toro,Verdejo, and Castro, 2015). Obesity (36 %) and smoking (20 %),
also are risk factor for CHF (Australian Institute of Health and Welfare (2014).
Individuals with cardiovascular abnormalities and dysfunctioning like cardiomyopathy,
coronary artery disease (CAD), myocarditis, arrhythmias, defective heart valves and
myocardial infraction (MI) are at higher risk of CHF. Since, Mckenzie is associated with MI;
she is at higher risk of CHF. Medication consumption like antidiabetic drugs, nonsteroidal
anti-inflammatory drugs (NSAIDs), anaesthetic and anticancer might lead to development of
CHF (Chow and Senderovich, 2018). Individuals with CHF might survive maximum upto
five years after its diagnosis and these individuals are with 10 % higher death rate relative to
the normal individuals (Australian Institute of Health and Welfare, 2014).
Mckenzie might not be able complete routine activities due to cardio-pulmonary
diseased condition. Hence, family members need to extend support to her to carry out these
activities; and observe and monitor her activities. It would be helpful in extending
psychological and emotional support to her. Diseased condition of Mckenzie might impart
psychological stress and economical load on family members. Both family and staff members
need to regulate her medicines, diet and risk factors to achieve her speedy recovery. Positive
2
Congestive heart failure (CHF) is a diseased status in which heart loses its ability to pump the
necessary amount of blood. Insufficient quantity of blood pumping by heart mainly occurs
due to cardiovascular conditions like high blood pressure and constricted arteries (Povsic,
2018). CHF is associated with risk factors like demographic factor like age, social factor
like smoking and inadequate physical activity and biological factors like high blood pressure,
obesity, diabetes and raised levels of cholesterol (Dhingra et al., 2014). In case of Mckenzie
(77 years), age is one of the risk factors for the occurrence of CHF. Probability of CHF
increases with increase in the age of the person. 2 and 5 % individuals upto age 60 and 70
years respectively are at risk of CHF. Moreover, Mckenzie is associated with hypertension.
Hence, it also can contribute to the occurrence of CHF in her. Females with hypertension are
four times at more risk with CHF relative to the normal female. Male and female are 40 and
60 % respectively at risk of CHF (Maahmood and Wang, 2013). High and low levels of low-
density lipoproteins and high-density lipoproteins respectively are responsible for the
occurrence of CHF. More saturated fat intake and β-type natriuretic peptides are also risk
factors of CHF (Díaz-Toro,Verdejo, and Castro, 2015). Obesity (36 %) and smoking (20 %),
also are risk factor for CHF (Australian Institute of Health and Welfare (2014).
Individuals with cardiovascular abnormalities and dysfunctioning like cardiomyopathy,
coronary artery disease (CAD), myocarditis, arrhythmias, defective heart valves and
myocardial infraction (MI) are at higher risk of CHF. Since, Mckenzie is associated with MI;
she is at higher risk of CHF. Medication consumption like antidiabetic drugs, nonsteroidal
anti-inflammatory drugs (NSAIDs), anaesthetic and anticancer might lead to development of
CHF (Chow and Senderovich, 2018). Individuals with CHF might survive maximum upto
five years after its diagnosis and these individuals are with 10 % higher death rate relative to
the normal individuals (Australian Institute of Health and Welfare, 2014).
Mckenzie might not be able complete routine activities due to cardio-pulmonary
diseased condition. Hence, family members need to extend support to her to carry out these
activities; and observe and monitor her activities. It would be helpful in extending
psychological and emotional support to her. Diseased condition of Mckenzie might impart
psychological stress and economical load on family members. Both family and staff members
need to regulate her medicines, diet and risk factors to achieve her speedy recovery. Positive
2
communication of family and staff members with Mckenzie would be helpful in achieving
her speedy recovery (Cooper, DeVore, and Michael Felker, 2015).
Q2.:
Symptom Pathophysiology
Dyspnoea Dyspnoea is a condition in which individual experience breathlessness.
Patients with CHF are usually associated with dyspnoea due to decreased
cardiac output. Reduced cardiac output lead to lessened blood supply to
skeletal muscles which results in the skeletal muscle dysfunction. Skeletal
muscle dysfunction results in the rise in the left ventricular pressure which
is helpful in increasing cardiac output. It leads to cascade of events like
pulmonary diffusion followed by interstitial oedema and finally
breathlessness. Raised ventricular pressure require more amount of energy
due to extra expenditure of energy. It results in the development of
myocardial ischemia and raised requirement of oxygen. (Güde, Brenner,
Störk, Hoes, and Rutten, 2014). As a result, there is development of
dyspnoea in Mckenzie due augmented oxygen requirement.
Swollen
ankle
Swollen ankle is condition in which there is swelling in the ankle. Fluid
build-up is the prominent factor for swelling. Reduced ventricular filling
and raised levels of natriuretic peptide and β-type natriuretic peptide are
accountable for vasodilation. Reduced cardiac preload and afterload mainly
occur due to vasodilation and reduced ventricular pressure. Subsequently, it
produces diminished blood back flow to the heart through the veins.
Diminished blood back flow mainly occurs due to constriction of the valve.
It led to the insufficient blood pumping by the heart (Eisen, 2014). In
McKenzie, swollen ankle mainly occurs due to cardiovascular abnormality
like diminished cardiac output.
Dizziness CHF characterised by the diminished supply of blood to organs comprising
of brain. Individuals with diminished supply of blood to brain tend to
develop dizziness due to inadequate supply of oxygen. Irregularity in the
cardiovascular parameters like heart rate and rhythm are the prominent
factors responsible for the development of dizziness in the CHF patients.
Six primary neurotransmitters of three-neuron arc regulate functions of
vestibulo-ocular reflex (VOR). Acetylcholine acts as an excitatory
3
her speedy recovery (Cooper, DeVore, and Michael Felker, 2015).
Q2.:
Symptom Pathophysiology
Dyspnoea Dyspnoea is a condition in which individual experience breathlessness.
Patients with CHF are usually associated with dyspnoea due to decreased
cardiac output. Reduced cardiac output lead to lessened blood supply to
skeletal muscles which results in the skeletal muscle dysfunction. Skeletal
muscle dysfunction results in the rise in the left ventricular pressure which
is helpful in increasing cardiac output. It leads to cascade of events like
pulmonary diffusion followed by interstitial oedema and finally
breathlessness. Raised ventricular pressure require more amount of energy
due to extra expenditure of energy. It results in the development of
myocardial ischemia and raised requirement of oxygen. (Güde, Brenner,
Störk, Hoes, and Rutten, 2014). As a result, there is development of
dyspnoea in Mckenzie due augmented oxygen requirement.
Swollen
ankle
Swollen ankle is condition in which there is swelling in the ankle. Fluid
build-up is the prominent factor for swelling. Reduced ventricular filling
and raised levels of natriuretic peptide and β-type natriuretic peptide are
accountable for vasodilation. Reduced cardiac preload and afterload mainly
occur due to vasodilation and reduced ventricular pressure. Subsequently, it
produces diminished blood back flow to the heart through the veins.
Diminished blood back flow mainly occurs due to constriction of the valve.
It led to the insufficient blood pumping by the heart (Eisen, 2014). In
McKenzie, swollen ankle mainly occurs due to cardiovascular abnormality
like diminished cardiac output.
Dizziness CHF characterised by the diminished supply of blood to organs comprising
of brain. Individuals with diminished supply of blood to brain tend to
develop dizziness due to inadequate supply of oxygen. Irregularity in the
cardiovascular parameters like heart rate and rhythm are the prominent
factors responsible for the development of dizziness in the CHF patients.
Six primary neurotransmitters of three-neuron arc regulate functions of
vestibulo-ocular reflex (VOR). Acetylcholine acts as an excitatory
3
neurotransmitter and regulate functioning of both peripheral and central
synapses. GABA is an inhibitory neurotransmitter and exhibits its action in
VOR and lateral and medical vestibular nucleus. Dopamine and
norepinephrine acts as accelerator and controller for vestibular
compensation respectively. Histamine role in the dizziness need to be fully
explored (Fife, 2017). Hence, McKenzie experiences dizziness due to
diminished cardiac output.
Q.3.
Cardiovascular patients like McKenzie need to be treated with Angiotensin-converting-
enzyme inhibitor (ACE inhibitor).
Mechanism of action of ACE inhibitors is inhibition of angiotensin-converting
enzyme. Angiotensin-converting enzyme in an essential component of renin–angiotensin-
aldosterone (RAAS) system. Disturbance in the physiological functioning of the RAAS
results in the development of hypertension. It is essential for ACE inhibitors to inhibit
Angiotensin I (ATI) conversion to Angiotensin II (ATII) to reduce hypertension.
Consequently, ACE inhibitors exhibit varied actions such as diminished cardiac output
diminished arteriolar resistance, diminished resistance in blood vessels and augmented
sodium excretion in the urine (Scott and Winters, 2015). Different effects of ACE inhibitors
like blood vessel relaxation and diminished blood volume are also responsible for its
antihypertensive effects. Consequently, it results in lessened both oxygen requirement and
consumption by the cardiovascular system (Dinicolantonio, Lavie, and O'Keefe, 2013).
Henceforth, ACE inhibitors like enalapril is the first choice of drug for the treatment of
patients like Mckenzie. Enalapril exhibited its effect in different cardiovascular conditions
like hypertension, asymptomatic left ventricular dysfunction and symptomatic heart failure
which are related to CHF.
Enalapril also exhibited its effect in chronic kidney failure and psychogenic
polydipsia. It is necessary to treat all these conditions in Mckenzie; since, these are the
predisposing factors for CHF (Sayer and Bhat, 2014).
Enalapril exhibit pharmacokinetic factors which are suitable for cardiovascular
patients because in cardiovascular patients’ drugs ADME properties alters due to alteration in
the blood flow and alteration in the kidney functions. Pharmacokinetic properties of enalapril
4
synapses. GABA is an inhibitory neurotransmitter and exhibits its action in
VOR and lateral and medical vestibular nucleus. Dopamine and
norepinephrine acts as accelerator and controller for vestibular
compensation respectively. Histamine role in the dizziness need to be fully
explored (Fife, 2017). Hence, McKenzie experiences dizziness due to
diminished cardiac output.
Q.3.
Cardiovascular patients like McKenzie need to be treated with Angiotensin-converting-
enzyme inhibitor (ACE inhibitor).
Mechanism of action of ACE inhibitors is inhibition of angiotensin-converting
enzyme. Angiotensin-converting enzyme in an essential component of renin–angiotensin-
aldosterone (RAAS) system. Disturbance in the physiological functioning of the RAAS
results in the development of hypertension. It is essential for ACE inhibitors to inhibit
Angiotensin I (ATI) conversion to Angiotensin II (ATII) to reduce hypertension.
Consequently, ACE inhibitors exhibit varied actions such as diminished cardiac output
diminished arteriolar resistance, diminished resistance in blood vessels and augmented
sodium excretion in the urine (Scott and Winters, 2015). Different effects of ACE inhibitors
like blood vessel relaxation and diminished blood volume are also responsible for its
antihypertensive effects. Consequently, it results in lessened both oxygen requirement and
consumption by the cardiovascular system (Dinicolantonio, Lavie, and O'Keefe, 2013).
Henceforth, ACE inhibitors like enalapril is the first choice of drug for the treatment of
patients like Mckenzie. Enalapril exhibited its effect in different cardiovascular conditions
like hypertension, asymptomatic left ventricular dysfunction and symptomatic heart failure
which are related to CHF.
Enalapril also exhibited its effect in chronic kidney failure and psychogenic
polydipsia. It is necessary to treat all these conditions in Mckenzie; since, these are the
predisposing factors for CHF (Sayer and Bhat, 2014).
Enalapril exhibit pharmacokinetic factors which are suitable for cardiovascular
patients because in cardiovascular patients’ drugs ADME properties alters due to alteration in
the blood flow and alteration in the kidney functions. Pharmacokinetic properties of enalapril
4
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
are as follows: onset of drug action is - 1-hour, it exhibits peak action between 4 – 6 hours,
oral bioavailability 60 % and total duration of action 12 – 24 hours. Enalapril is a prodrug.
Enalapril produce its effect through metabolite Enalaprilat (Opie and Gersh, 2011).
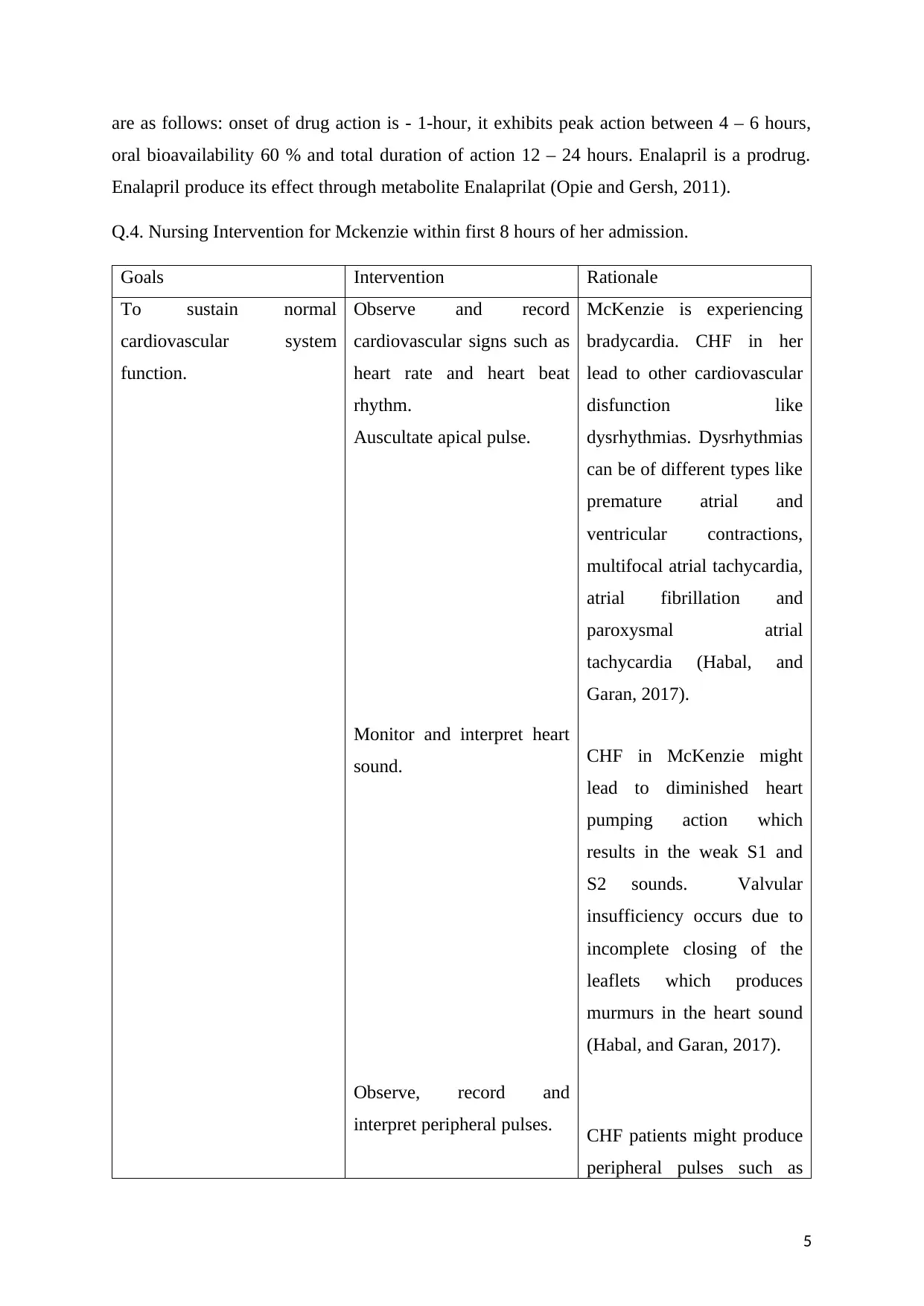
Q.4. Nursing Intervention for Mckenzie within first 8 hours of her admission.
Goals Intervention Rationale
To sustain normal
cardiovascular system
function.
Observe and record
cardiovascular signs such as
heart rate and heart beat
rhythm.
Auscultate apical pulse.
Monitor and interpret heart
sound.
Observe, record and
interpret peripheral pulses.
McKenzie is experiencing
bradycardia. CHF in her
lead to other cardiovascular
disfunction like
dysrhythmias. Dysrhythmias
can be of different types like
premature atrial and
ventricular contractions,
multifocal atrial tachycardia,
atrial fibrillation and
paroxysmal atrial
tachycardia (Habal, and
Garan, 2017).
CHF in McKenzie might
lead to diminished heart
pumping action which
results in the weak S1 and
S2 sounds. Valvular
insufficiency occurs due to
incomplete closing of the
leaflets which produces
murmurs in the heart sound
(Habal, and Garan, 2017).
CHF patients might produce
peripheral pulses such as
5
oral bioavailability 60 % and total duration of action 12 – 24 hours. Enalapril is a prodrug.
Enalapril produce its effect through metabolite Enalaprilat (Opie and Gersh, 2011).
Q.4. Nursing Intervention for Mckenzie within first 8 hours of her admission.
Goals Intervention Rationale
To sustain normal
cardiovascular system
function.
Observe and record
cardiovascular signs such as
heart rate and heart beat
rhythm.
Auscultate apical pulse.
Monitor and interpret heart
sound.
Observe, record and
interpret peripheral pulses.
McKenzie is experiencing
bradycardia. CHF in her
lead to other cardiovascular
disfunction like
dysrhythmias. Dysrhythmias
can be of different types like
premature atrial and
ventricular contractions,
multifocal atrial tachycardia,
atrial fibrillation and
paroxysmal atrial
tachycardia (Habal, and
Garan, 2017).
CHF in McKenzie might
lead to diminished heart
pumping action which
results in the weak S1 and
S2 sounds. Valvular
insufficiency occurs due to
incomplete closing of the
leaflets which produces
murmurs in the heart sound
(Habal, and Garan, 2017).
CHF patients might produce
peripheral pulses such as
5
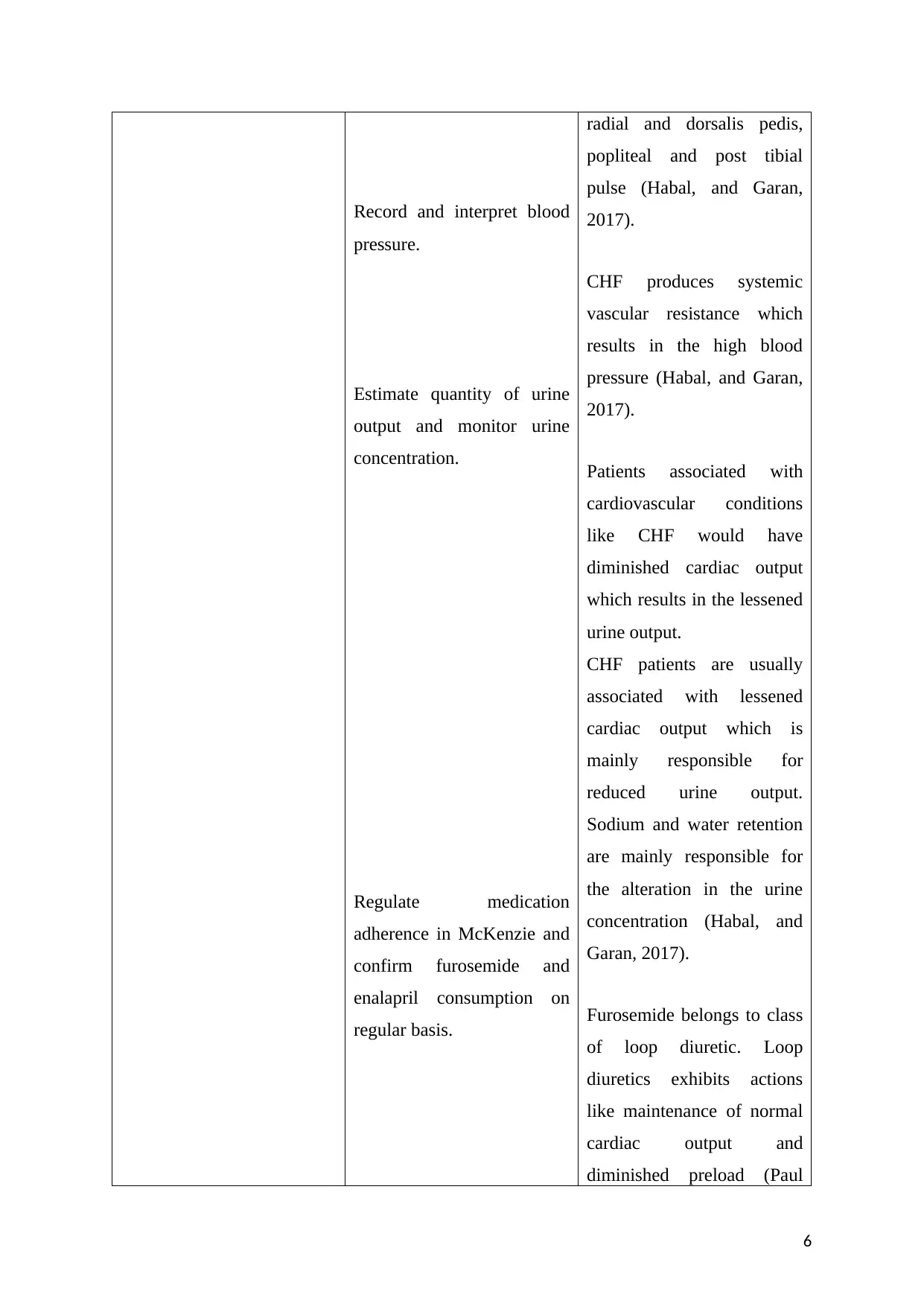
Record and interpret blood
pressure.
Estimate quantity of urine
output and monitor urine
concentration.
Regulate medication
adherence in McKenzie and
confirm furosemide and
enalapril consumption on
regular basis.
radial and dorsalis pedis,
popliteal and post tibial
pulse (Habal, and Garan,
2017).
CHF produces systemic
vascular resistance which
results in the high blood
pressure (Habal, and Garan,
2017).
Patients associated with
cardiovascular conditions
like CHF would have
diminished cardiac output
which results in the lessened
urine output.
CHF patients are usually
associated with lessened
cardiac output which is
mainly responsible for
reduced urine output.
Sodium and water retention
are mainly responsible for
the alteration in the urine
concentration (Habal, and
Garan, 2017).
Furosemide belongs to class
of loop diuretic. Loop
diuretics exhibits actions
like maintenance of normal
cardiac output and
diminished preload (Paul
6
pressure.
Estimate quantity of urine
output and monitor urine
concentration.
Regulate medication
adherence in McKenzie and
confirm furosemide and
enalapril consumption on
regular basis.
radial and dorsalis pedis,
popliteal and post tibial
pulse (Habal, and Garan,
2017).
CHF produces systemic
vascular resistance which
results in the high blood
pressure (Habal, and Garan,
2017).
Patients associated with
cardiovascular conditions
like CHF would have
diminished cardiac output
which results in the lessened
urine output.
CHF patients are usually
associated with lessened
cardiac output which is
mainly responsible for
reduced urine output.
Sodium and water retention
are mainly responsible for
the alteration in the urine
concentration (Habal, and
Garan, 2017).
Furosemide belongs to class
of loop diuretic. Loop
diuretics exhibits actions
like maintenance of normal
cardiac output and
diminished preload (Paul
6
and Hice, 2014)
Mechanism of action of
enalapril is ACE inhibition.
ACE inhibitors produces its
action by raising ventricular
filling pressure and cardiac
output (Paul and Hice,
2014).
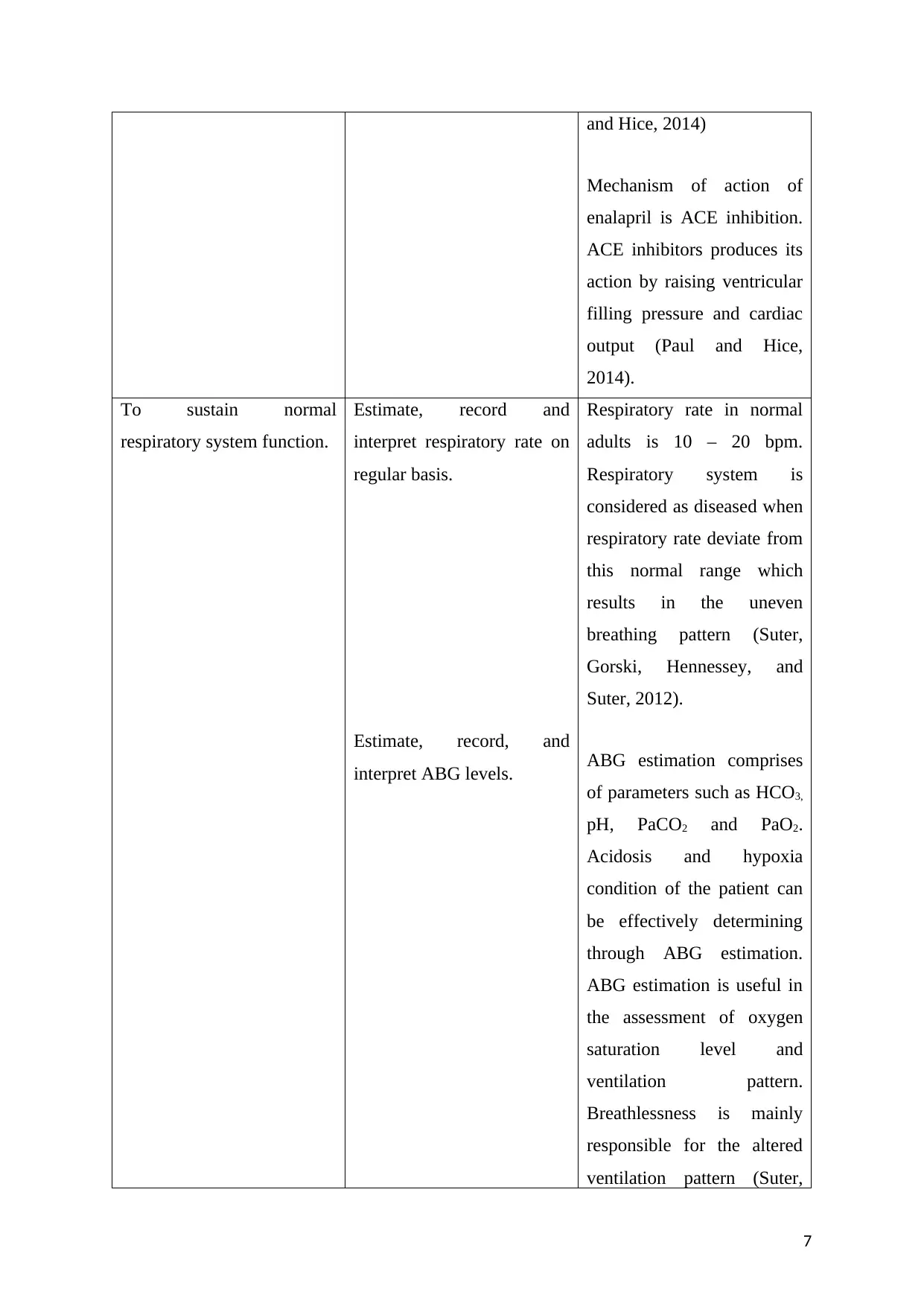
To sustain normal
respiratory system function.
Estimate, record and
interpret respiratory rate on
regular basis.
Estimate, record, and
interpret ABG levels.
Respiratory rate in normal
adults is 10 – 20 bpm.
Respiratory system is
considered as diseased when
respiratory rate deviate from
this normal range which
results in the uneven
breathing pattern (Suter,
Gorski, Hennessey, and
Suter, 2012).
ABG estimation comprises
of parameters such as HCO3,
pH, PaCO2 and PaO2.
Acidosis and hypoxia
condition of the patient can
be effectively determining
through ABG estimation.
ABG estimation is useful in
the assessment of oxygen
saturation level and
ventilation pattern.
Breathlessness is mainly
responsible for the altered
ventilation pattern (Suter,
7
Mechanism of action of
enalapril is ACE inhibition.
ACE inhibitors produces its
action by raising ventricular
filling pressure and cardiac
output (Paul and Hice,
2014).
To sustain normal
respiratory system function.
Estimate, record and
interpret respiratory rate on
regular basis.
Estimate, record, and
interpret ABG levels.
Respiratory rate in normal
adults is 10 – 20 bpm.
Respiratory system is
considered as diseased when
respiratory rate deviate from
this normal range which
results in the uneven
breathing pattern (Suter,
Gorski, Hennessey, and
Suter, 2012).
ABG estimation comprises
of parameters such as HCO3,
pH, PaCO2 and PaO2.
Acidosis and hypoxia
condition of the patient can
be effectively determining
through ABG estimation.
ABG estimation is useful in
the assessment of oxygen
saturation level and
ventilation pattern.
Breathlessness is mainly
responsible for the altered
ventilation pattern (Suter,
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
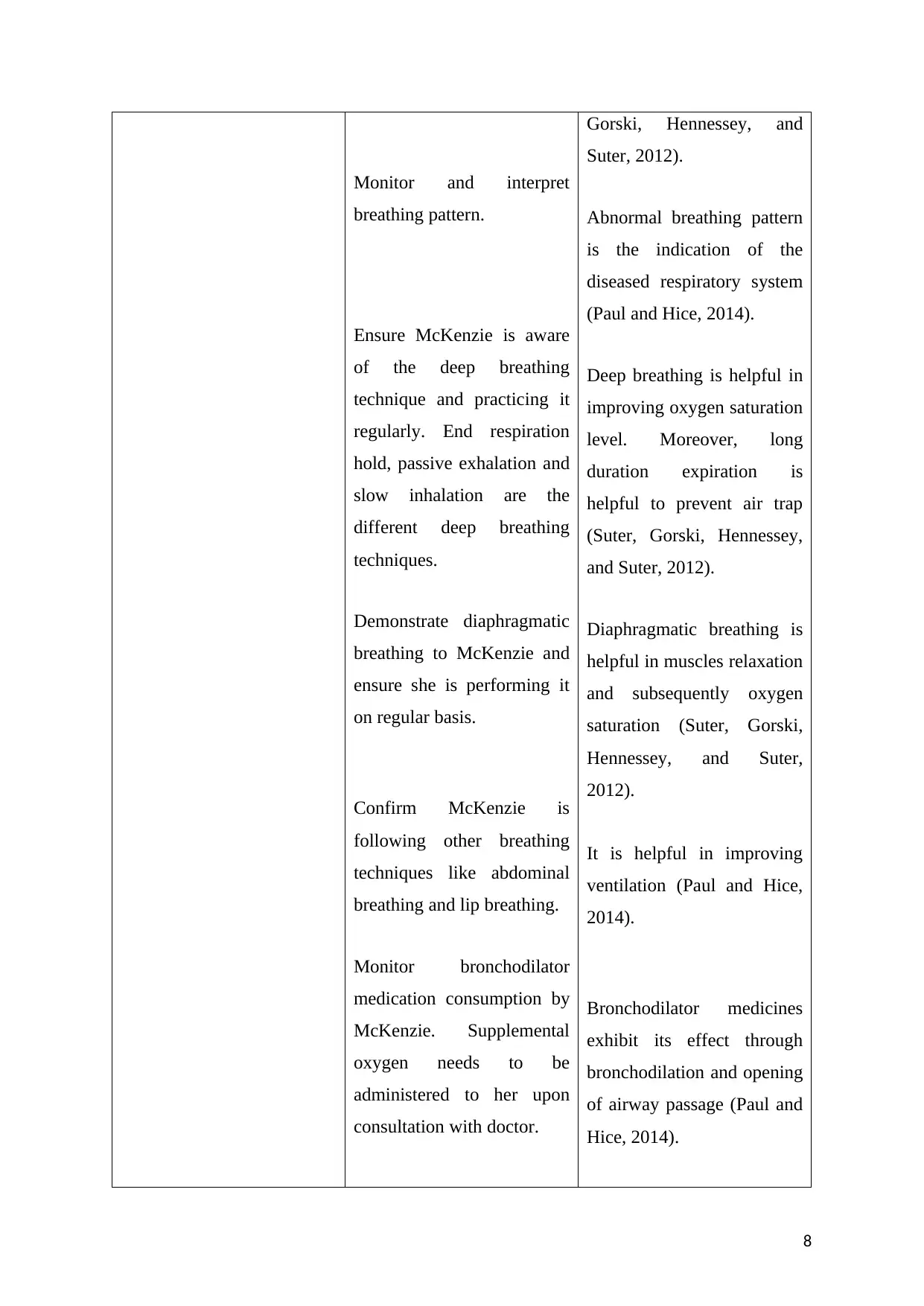
Monitor and interpret
breathing pattern.
Ensure McKenzie is aware
of the deep breathing
technique and practicing it
regularly. End respiration
hold, passive exhalation and
slow inhalation are the
different deep breathing
techniques.
Demonstrate diaphragmatic
breathing to McKenzie and
ensure she is performing it
on regular basis.
Confirm McKenzie is
following other breathing
techniques like abdominal
breathing and lip breathing.
Monitor bronchodilator
medication consumption by
McKenzie. Supplemental
oxygen needs to be
administered to her upon
consultation with doctor.
Gorski, Hennessey, and
Suter, 2012).
Abnormal breathing pattern
is the indication of the
diseased respiratory system
(Paul and Hice, 2014).
Deep breathing is helpful in
improving oxygen saturation
level. Moreover, long
duration expiration is
helpful to prevent air trap
(Suter, Gorski, Hennessey,
and Suter, 2012).
Diaphragmatic breathing is
helpful in muscles relaxation
and subsequently oxygen
saturation (Suter, Gorski,
Hennessey, and Suter,
2012).
It is helpful in improving
ventilation (Paul and Hice,
2014).
Bronchodilator medicines
exhibit its effect through
bronchodilation and opening
of airway passage (Paul and
Hice, 2014).
8
breathing pattern.
Ensure McKenzie is aware
of the deep breathing
technique and practicing it
regularly. End respiration
hold, passive exhalation and
slow inhalation are the
different deep breathing
techniques.
Demonstrate diaphragmatic
breathing to McKenzie and
ensure she is performing it
on regular basis.
Confirm McKenzie is
following other breathing
techniques like abdominal
breathing and lip breathing.
Monitor bronchodilator
medication consumption by
McKenzie. Supplemental
oxygen needs to be
administered to her upon
consultation with doctor.
Gorski, Hennessey, and
Suter, 2012).
Abnormal breathing pattern
is the indication of the
diseased respiratory system
(Paul and Hice, 2014).
Deep breathing is helpful in
improving oxygen saturation
level. Moreover, long
duration expiration is
helpful to prevent air trap
(Suter, Gorski, Hennessey,
and Suter, 2012).
Diaphragmatic breathing is
helpful in muscles relaxation
and subsequently oxygen
saturation (Suter, Gorski,
Hennessey, and Suter,
2012).
It is helpful in improving
ventilation (Paul and Hice,
2014).
Bronchodilator medicines
exhibit its effect through
bronchodilation and opening
of airway passage (Paul and
Hice, 2014).
8
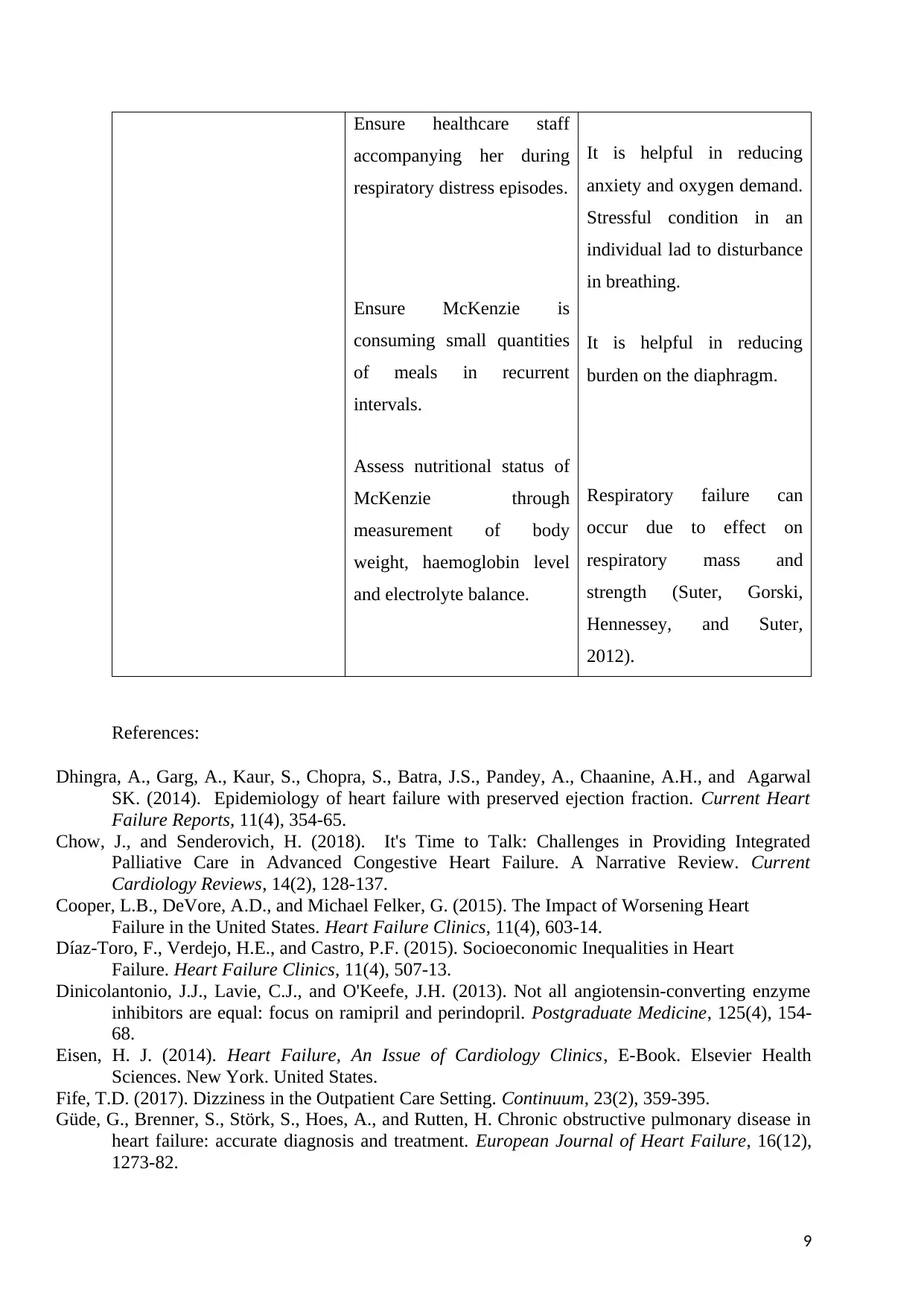
Ensure healthcare staff
accompanying her during
respiratory distress episodes.
Ensure McKenzie is
consuming small quantities
of meals in recurrent
intervals.
Assess nutritional status of
McKenzie through
measurement of body
weight, haemoglobin level
and electrolyte balance.
It is helpful in reducing
anxiety and oxygen demand.
Stressful condition in an
individual lad to disturbance
in breathing.
It is helpful in reducing
burden on the diaphragm.
Respiratory failure can
occur due to effect on
respiratory mass and
strength (Suter, Gorski,
Hennessey, and Suter,
2012).
References:
Dhingra, A., Garg, A., Kaur, S., Chopra, S., Batra, J.S., Pandey, A., Chaanine, A.H., and Agarwal
SK. (2014). Epidemiology of heart failure with preserved ejection fraction. Current Heart
Failure Reports, 11(4), 354-65.
Chow, J., and Senderovich, H. (2018). It's Time to Talk: Challenges in Providing Integrated
Palliative Care in Advanced Congestive Heart Failure. A Narrative Review. Current
Cardiology Reviews, 14(2), 128-137.
Cooper, L.B., DeVore, A.D., and Michael Felker, G. (2015). The Impact of Worsening Heart
Failure in the United States. Heart Failure Clinics, 11(4), 603-14.
Díaz-Toro, F., Verdejo, H.E., and Castro, P.F. (2015). Socioeconomic Inequalities in Heart
Failure. Heart Failure Clinics, 11(4), 507-13.
Dinicolantonio, J.J., Lavie, C.J., and O'Keefe, J.H. (2013). Not all angiotensin-converting enzyme
inhibitors are equal: focus on ramipril and perindopril. Postgraduate Medicine, 125(4), 154-
68.
Eisen, H. J. (2014). Heart Failure, An Issue of Cardiology Clinics, E-Book. Elsevier Health
Sciences. New York. United States.
Fife, T.D. (2017). Dizziness in the Outpatient Care Setting. Continuum, 23(2), 359-395.
Güde, G., Brenner, S., Störk, S., Hoes, A., and Rutten, H. Chronic obstructive pulmonary disease in
heart failure: accurate diagnosis and treatment. European Journal of Heart Failure, 16(12),
1273-82.
9
accompanying her during
respiratory distress episodes.
Ensure McKenzie is
consuming small quantities
of meals in recurrent
intervals.
Assess nutritional status of
McKenzie through
measurement of body
weight, haemoglobin level
and electrolyte balance.
It is helpful in reducing
anxiety and oxygen demand.
Stressful condition in an
individual lad to disturbance
in breathing.
It is helpful in reducing
burden on the diaphragm.
Respiratory failure can
occur due to effect on
respiratory mass and
strength (Suter, Gorski,
Hennessey, and Suter,
2012).
References:
Dhingra, A., Garg, A., Kaur, S., Chopra, S., Batra, J.S., Pandey, A., Chaanine, A.H., and Agarwal
SK. (2014). Epidemiology of heart failure with preserved ejection fraction. Current Heart
Failure Reports, 11(4), 354-65.
Chow, J., and Senderovich, H. (2018). It's Time to Talk: Challenges in Providing Integrated
Palliative Care in Advanced Congestive Heart Failure. A Narrative Review. Current
Cardiology Reviews, 14(2), 128-137.
Cooper, L.B., DeVore, A.D., and Michael Felker, G. (2015). The Impact of Worsening Heart
Failure in the United States. Heart Failure Clinics, 11(4), 603-14.
Díaz-Toro, F., Verdejo, H.E., and Castro, P.F. (2015). Socioeconomic Inequalities in Heart
Failure. Heart Failure Clinics, 11(4), 507-13.
Dinicolantonio, J.J., Lavie, C.J., and O'Keefe, J.H. (2013). Not all angiotensin-converting enzyme
inhibitors are equal: focus on ramipril and perindopril. Postgraduate Medicine, 125(4), 154-
68.
Eisen, H. J. (2014). Heart Failure, An Issue of Cardiology Clinics, E-Book. Elsevier Health
Sciences. New York. United States.
Fife, T.D. (2017). Dizziness in the Outpatient Care Setting. Continuum, 23(2), 359-395.
Güde, G., Brenner, S., Störk, S., Hoes, A., and Rutten, H. Chronic obstructive pulmonary disease in
heart failure: accurate diagnosis and treatment. European Journal of Heart Failure, 16(12),
1273-82.
9
Habal, M.V., and Garan, A.R. (2017). Long-term management of end-stage heart failure. Best
Practice & Research: Clinical Anaesthesiology, 31(2), 153-166.
Mahmood, S. S., and Wang, T. J. (2013). The epidemiology of congestive heart failure: the
Framingham Heart Study perspective. Global Heart, 8(1), 77–82.
Opie, L. H., and Gersh, B. J. (2011). Drugs for the Heart E-Book. Elsevier Health Sciences. New
York. United States.
Paul, S., and Hice, A. (2014). Role of the acute care nurse in managing patients with heart
failure using evidence-based care. Critical Care Nursing Q, 37(4), 357-76.
Povsic, T.J. (2018). Emerging Therapies for Congestive Heart Failure. Clinical Pharmacology &
Therapeutics, 103(1), 77-87.
Sayer, G., and Bhat, G. (2014). The renin-angiotensin-aldosterone system and heart failure.
Cardiology Clinics, 32(1), 21-32.
Scott, M.C., and Winters, M.E. (2015). Congestive Heart Failure. Emergency Medicine
Clinics of North America, 33(3), 553-62.
10
Practice & Research: Clinical Anaesthesiology, 31(2), 153-166.
Mahmood, S. S., and Wang, T. J. (2013). The epidemiology of congestive heart failure: the
Framingham Heart Study perspective. Global Heart, 8(1), 77–82.
Opie, L. H., and Gersh, B. J. (2011). Drugs for the Heart E-Book. Elsevier Health Sciences. New
York. United States.
Paul, S., and Hice, A. (2014). Role of the acute care nurse in managing patients with heart
failure using evidence-based care. Critical Care Nursing Q, 37(4), 357-76.
Povsic, T.J. (2018). Emerging Therapies for Congestive Heart Failure. Clinical Pharmacology &
Therapeutics, 103(1), 77-87.
Sayer, G., and Bhat, G. (2014). The renin-angiotensin-aldosterone system and heart failure.
Cardiology Clinics, 32(1), 21-32.
Scott, M.C., and Winters, M.E. (2015). Congestive Heart Failure. Emergency Medicine
Clinics of North America, 33(3), 553-62.
10
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





