Nuclear Medicine Contribution to the Management of Lymphoedema
VerifiedAdded on 2023/04/21
|12
|2623
|256
Report
AI Summary
This report explores the contribution of nuclear medicine in managing suspected lymphoedema, a chronic condition causing swelling in body tissues due to lymphatic system dysfunction. It discusses lymphoscintigraphy and sentinel lymph node biopsy (SLNB) as key techniques, highlighting the benefit...

Running head: NUCLEAR MEDICINE
Contribution of nuclear medicine to suspected lymphoedema
Name of the Student
Name of the University
Author Note
Contribution of nuclear medicine to suspected lymphoedema
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1NUCLEAR MEDICINE
Introduction- The term nuclear medicine refers to the medical speciality that involves
application of certain radioactive substances for the identification, and treatment of any illness.
The history of nuclear medicine can be traced back to artificial radioactivity discovery in 1934,
followed by the production of several radio-nucleotides for usage in medicine in 1946, by the
Oak Ridge National laboratory (1). This form of medical speciality involves the usage of minute
amounts of radioactive substances, commonly referred to as radiotracers that are generally
injected into the bloodstream swallowed or inhaled, which then travel through the area that is
being investigated, and radiate energy in the form of gamma rays (2). This essay will elaborate
on the contribution of nuclear medicine in management of suspected lymphoedema, a chronic
condition that results in swelling of the body tissues. The condition particularly arises when the
lymphatic system fails to work in an effective manner, thereby creating difficulties in fighting
infection and removing excess body fluids.
Discussion- Lymphoscintigraphy also referred to as Sentinel Lymph Node (SLN)
mapping refers to an imaging technique that is particularly used for the identification of lymph
drainage basin, determination of the quantity of sentinel node, differentiation of subsequent
nodes from sentinel nodes, marking sentinel node over skin for the purpose of biopsy, and
locating sentinel nodes in unexpected regions (3). The benefits of nuclear medicine can be
accredited to the fact that conduction of a sentinel lymph node biopsy (SLNB) helps in
determining whether melanoma breast cancer in the patient has spread to others and lymph
nodes. SLNB has substituted axillary lymph node (ALN) dissection in recent years, and has
begun to be used as the chief stage staging modality for suspected breast cancer and melanoma.
Reports from recently conducted multicenter randomised trials that comprised of breast cancer
patients failed to demonstrate any significant differences in overall or disease free survival rates,
Introduction- The term nuclear medicine refers to the medical speciality that involves
application of certain radioactive substances for the identification, and treatment of any illness.
The history of nuclear medicine can be traced back to artificial radioactivity discovery in 1934,
followed by the production of several radio-nucleotides for usage in medicine in 1946, by the
Oak Ridge National laboratory (1). This form of medical speciality involves the usage of minute
amounts of radioactive substances, commonly referred to as radiotracers that are generally
injected into the bloodstream swallowed or inhaled, which then travel through the area that is
being investigated, and radiate energy in the form of gamma rays (2). This essay will elaborate
on the contribution of nuclear medicine in management of suspected lymphoedema, a chronic
condition that results in swelling of the body tissues. The condition particularly arises when the
lymphatic system fails to work in an effective manner, thereby creating difficulties in fighting
infection and removing excess body fluids.
Discussion- Lymphoscintigraphy also referred to as Sentinel Lymph Node (SLN)
mapping refers to an imaging technique that is particularly used for the identification of lymph
drainage basin, determination of the quantity of sentinel node, differentiation of subsequent
nodes from sentinel nodes, marking sentinel node over skin for the purpose of biopsy, and
locating sentinel nodes in unexpected regions (3). The benefits of nuclear medicine can be
accredited to the fact that conduction of a sentinel lymph node biopsy (SLNB) helps in
determining whether melanoma breast cancer in the patient has spread to others and lymph
nodes. SLNB has substituted axillary lymph node (ALN) dissection in recent years, and has
begun to be used as the chief stage staging modality for suspected breast cancer and melanoma.
Reports from recently conducted multicenter randomised trials that comprised of breast cancer
patients failed to demonstrate any significant differences in overall or disease free survival rates,
2NUCLEAR MEDICINE
between ALND and SLNB. Nonetheless, usage of nuclear medicine through SLNB was also
correlated with significant decline in the mortality rates, when compared to the other diagnostic
techniques. Low false negative rates were also found in studies that were associated with usage
of pre-operative lymphoscintigraphy, thus establishing the benefits of nuclear medicine in
diagnostic imaging (4).
Research evidences also elaborate on the fact that metastatic nature of regional lymph
nodes is one of the most noteworthy prognostic factors in breast cancer melanoma, in contrast to
different solid tumours that have lymphatic spread. Pre-operative recognition of sentinel lymph
nodes has been conventionally performed with the use of radiotracer injection,
lymphoscintigraphy and Single Photon Emission Computed Tomography (SPECT). Owing to
the fact that use of radiocolloids such as nanocolloids facilitate greater rate of SLN detection
than conventional methods (as much as 95%), nuclear medicine can be used as an effective tool
for diagnostic purposes. The success of nuclear medicine can also be attributed to the capability
of radiocolloids to be retained for greater period of time, in the SLN, in combination with their
higher rates of detection (5). According to (6) upon investigating prognostic worth of qualitative
worth of lymphoscintigraphy, in relation to gynaecological cancer-associated lymphoedema, it
was found that an estimated 58.6% patients who underwent complex decongestive therapy
(CDT), manifested poor therapeutic response. This was concomitant with significant differences
between poor and good responders in therapy compliance, clinical status, pattern of lymphatic
vessel uptake, and dermal backflow severity, thus establishing lymphoscintigraphy beneficial in
predicting outcomes of such patients.
With the aim of exploring validity of quantitative lymphoscintigraphy for patients who
have undergone breast cancer surgery, 72 patients reporting lymphoedema were recruited,
between ALND and SLNB. Nonetheless, usage of nuclear medicine through SLNB was also
correlated with significant decline in the mortality rates, when compared to the other diagnostic
techniques. Low false negative rates were also found in studies that were associated with usage
of pre-operative lymphoscintigraphy, thus establishing the benefits of nuclear medicine in
diagnostic imaging (4).
Research evidences also elaborate on the fact that metastatic nature of regional lymph
nodes is one of the most noteworthy prognostic factors in breast cancer melanoma, in contrast to
different solid tumours that have lymphatic spread. Pre-operative recognition of sentinel lymph
nodes has been conventionally performed with the use of radiotracer injection,
lymphoscintigraphy and Single Photon Emission Computed Tomography (SPECT). Owing to
the fact that use of radiocolloids such as nanocolloids facilitate greater rate of SLN detection
than conventional methods (as much as 95%), nuclear medicine can be used as an effective tool
for diagnostic purposes. The success of nuclear medicine can also be attributed to the capability
of radiocolloids to be retained for greater period of time, in the SLN, in combination with their
higher rates of detection (5). According to (6) upon investigating prognostic worth of qualitative
worth of lymphoscintigraphy, in relation to gynaecological cancer-associated lymphoedema, it
was found that an estimated 58.6% patients who underwent complex decongestive therapy
(CDT), manifested poor therapeutic response. This was concomitant with significant differences
between poor and good responders in therapy compliance, clinical status, pattern of lymphatic
vessel uptake, and dermal backflow severity, thus establishing lymphoscintigraphy beneficial in
predicting outcomes of such patients.
With the aim of exploring validity of quantitative lymphoscintigraphy for patients who
have undergone breast cancer surgery, 72 patients reporting lymphoedema were recruited,
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

3NUCLEAR MEDICINE
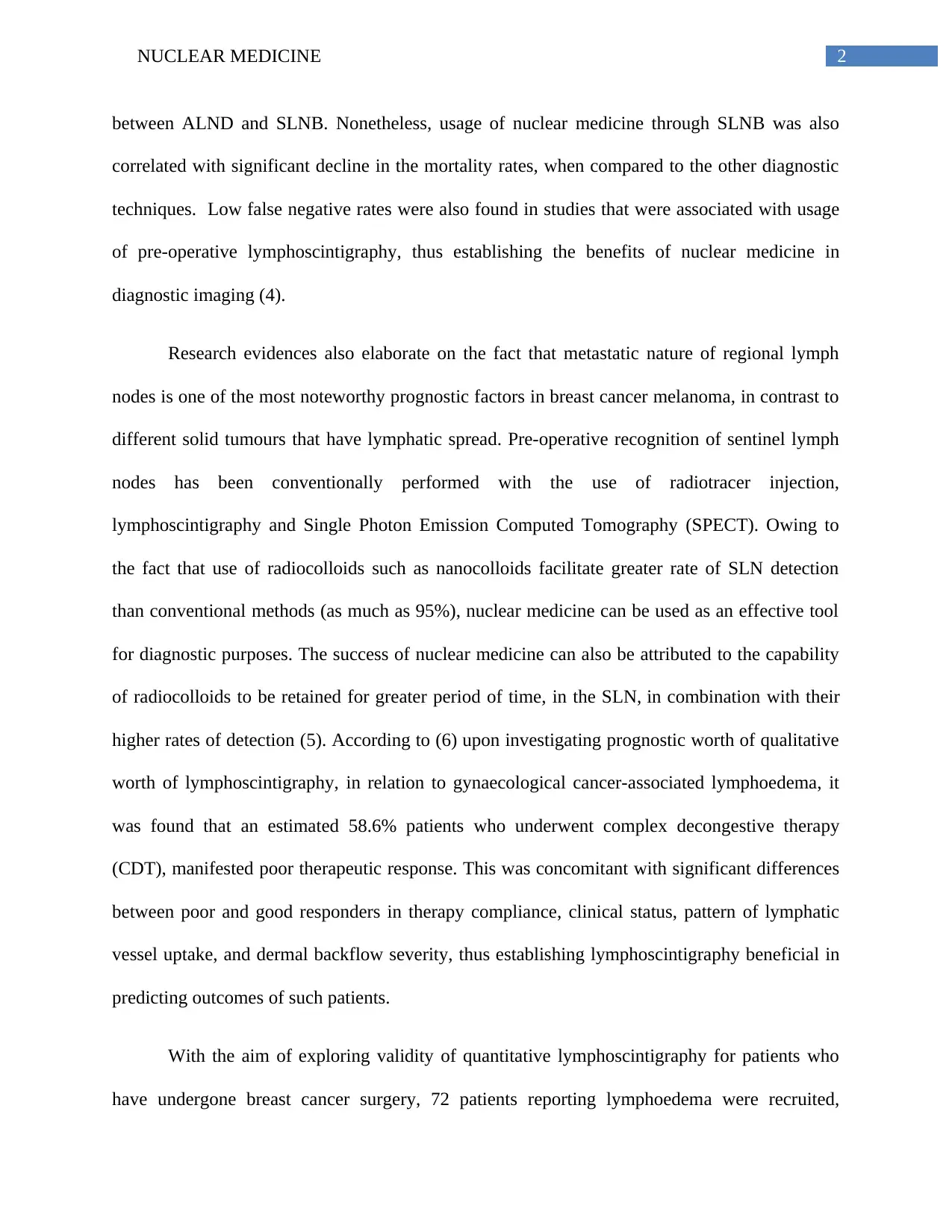
followed by implementation of quantitative asymmetry indices (QAI). Results suggested that
maximal circumference difference (MCD) was greater in qualitative obstruction patterns
(2.76±2.48), which was significantly different from decreased function pattern (1.65±1.17) and
normal pattern (0.69±0.78). With an increase in QAI of axillary LN, a significant decrease was
observed in MCD, which in turn was accompanied by high obstruction pattern of QAI in the
upper limbs (3.12±3.07). The findings of the study confirmed the use of quantitative
lymphoscintigraphy as an alternative diagnostic tool for identification of lymphoedema,
following breast cancer surgery (7).
Figure 1- Typical images of quantitative lymphoscintigraphic analysis of the upper
limb of a patient with breast cancer surgery including axillary lymph node (LN) dissection.
Source- (7)
Findings from another study that comprised of two groups having 16 patients with upper
limb/trunk melanoma for axillary SLN biopsy as the study subjects, and 10 healthy volunteers as
the control, respectively, demonstrated noteworthy differences. Asymmetry indices for
followed by implementation of quantitative asymmetry indices (QAI). Results suggested that
maximal circumference difference (MCD) was greater in qualitative obstruction patterns
(2.76±2.48), which was significantly different from decreased function pattern (1.65±1.17) and
normal pattern (0.69±0.78). With an increase in QAI of axillary LN, a significant decrease was
observed in MCD, which in turn was accompanied by high obstruction pattern of QAI in the
upper limbs (3.12±3.07). The findings of the study confirmed the use of quantitative
lymphoscintigraphy as an alternative diagnostic tool for identification of lymphoedema,
following breast cancer surgery (7).
Figure 1- Typical images of quantitative lymphoscintigraphic analysis of the upper
limb of a patient with breast cancer surgery including axillary lymph node (LN) dissection.
Source- (7)
Findings from another study that comprised of two groups having 16 patients with upper
limb/trunk melanoma for axillary SLN biopsy as the study subjects, and 10 healthy volunteers as
the control, respectively, demonstrated noteworthy differences. Asymmetry indices for
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4NUCLEAR MEDICINE
lymphoscintigraphic patterns were observed in 37.5% of the patients in study group, and 50%
patients in control group, with type III being the most prevalent pattern. The researchers failed to
demonstrate any major correlation between the patterns and clinical variables, which resulted in
lack of evidence on the possible advantages of nuclear medicine in lymphoedema (8).
Guidelines- According to the guidelines formulated and proposed by the Society of
Nuclear Medicine and Molecular Imaging (SNMMI) and the European Association of Nuclear
Medicine (EANM), indications for SLN procedures have been established for T1 or T2 tumour,
DCIS with mastectomy, obesity, older age, male breast cancer, and before preoperative systemic
therapy. However, there are controversies regarding implementation of this domain of nuclear
medicine in T3 or T4 tumour, multicentric or multifocal tumour, DCIS without mastectomy,
suspicious, axillary nodes, pregnancy, internal mammary lymph node evaluation, and prior non-
oncological breast surgery (9). According to (10) the practice guidelines also state that SLNB
can be easily performed in melanoma of the trunk or extremities. In the neck and head area, the
method is more challenging owing to several intricacies of the patterns of lymphatic drainage,
the shine-through phenomenon, and the complexities of local anatomy. The authors also
illustrated the fact that SLNB can be used amid patients who have been suspected with
intermediate thickness tumour. Nonetheless, the technique cannot be assessed for instances such
as, shave biopsy. It is also not recommended under circumstances when laser, cryotherapy or
cauterizations have been conducted on similar lesions, prior to diagnosis of a melanoma.
Disadvantages- Some potential pitfalls that might arise during the use of nuclear
medicine for SLN procedure are skin contamination, and misinterpretation of second-echelon
nodes as SLN. Skin contamination typically arises due to injection or urinary contamination, and
is often wrongly diagnosed as lymph nodes, which can be identified by obtaining planar images
lymphoscintigraphic patterns were observed in 37.5% of the patients in study group, and 50%
patients in control group, with type III being the most prevalent pattern. The researchers failed to
demonstrate any major correlation between the patterns and clinical variables, which resulted in
lack of evidence on the possible advantages of nuclear medicine in lymphoedema (8).
Guidelines- According to the guidelines formulated and proposed by the Society of
Nuclear Medicine and Molecular Imaging (SNMMI) and the European Association of Nuclear
Medicine (EANM), indications for SLN procedures have been established for T1 or T2 tumour,
DCIS with mastectomy, obesity, older age, male breast cancer, and before preoperative systemic
therapy. However, there are controversies regarding implementation of this domain of nuclear
medicine in T3 or T4 tumour, multicentric or multifocal tumour, DCIS without mastectomy,
suspicious, axillary nodes, pregnancy, internal mammary lymph node evaluation, and prior non-
oncological breast surgery (9). According to (10) the practice guidelines also state that SLNB
can be easily performed in melanoma of the trunk or extremities. In the neck and head area, the
method is more challenging owing to several intricacies of the patterns of lymphatic drainage,
the shine-through phenomenon, and the complexities of local anatomy. The authors also
illustrated the fact that SLNB can be used amid patients who have been suspected with
intermediate thickness tumour. Nonetheless, the technique cannot be assessed for instances such
as, shave biopsy. It is also not recommended under circumstances when laser, cryotherapy or
cauterizations have been conducted on similar lesions, prior to diagnosis of a melanoma.
Disadvantages- Some potential pitfalls that might arise during the use of nuclear
medicine for SLN procedure are skin contamination, and misinterpretation of second-echelon
nodes as SLN. Skin contamination typically arises due to injection or urinary contamination, and
is often wrongly diagnosed as lymph nodes, which can be identified by obtaining planar images
5NUCLEAR MEDICINE
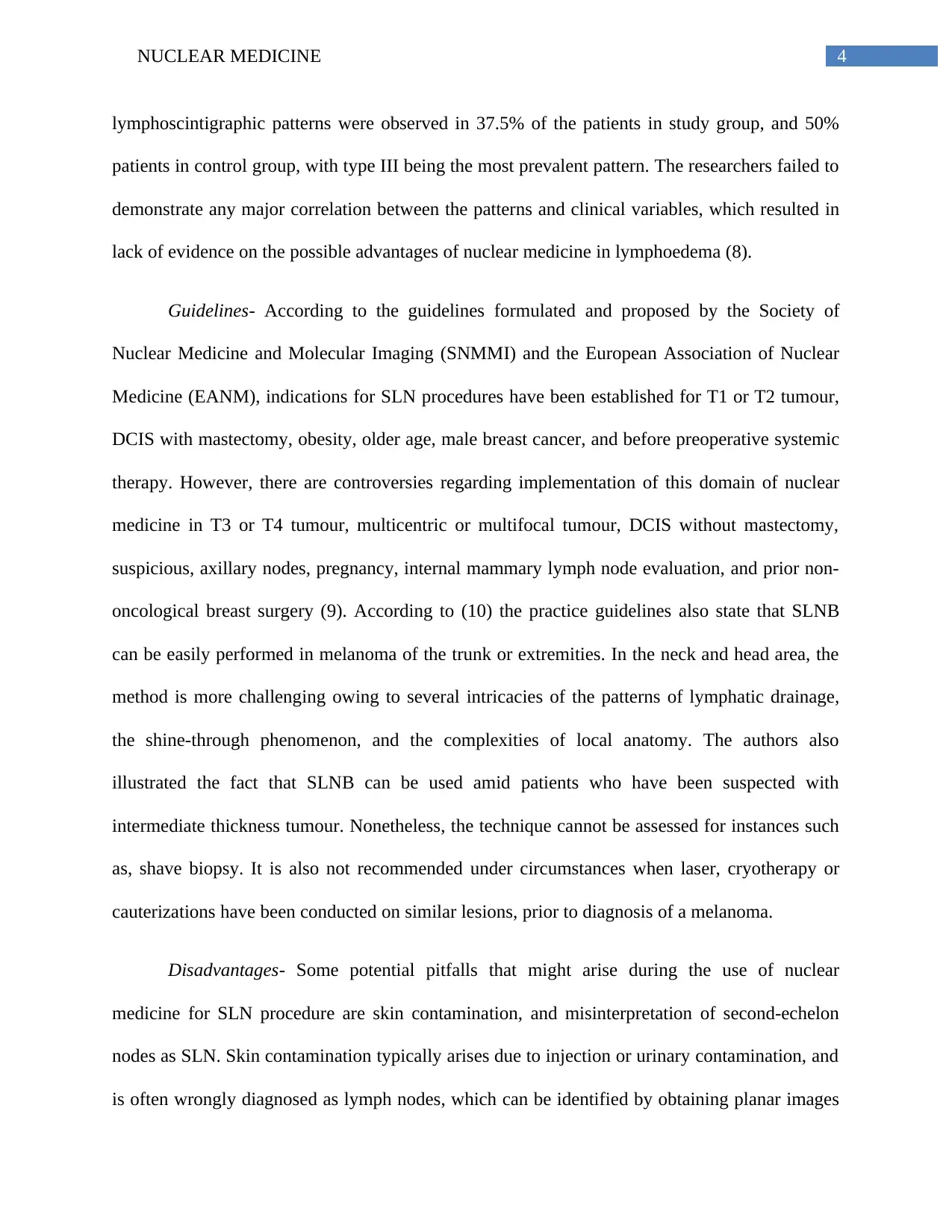
from a range of views, and by conducting SPECT/CT. Another potential drawback is the fact
that lymphatic lakes or lymphangioma are also often misinterpreted to be lymph nodes (11).
Image reading might also get intricate due to adjacent tissues that contain radioactivity.
Likewise, although the identification rate is greater and false-negative rates (FNR) are lower,
when two mapping techniques of radiocolloid and blue dyes are used together, there is lack of
consensus on the technique that should be used. Researchers have proposed a general agreement
that administration of a radiocolloid that measures 100-200 nm is the best compromise between
optimal retention in SLN and fast lymphatic drainage (12).
Figure 2- Planar images and anterior (a) and lateral projections (b) of a
lymphoscintigraphy of a 55-year-old woman with a breast cancer in the right ULQ.
Source- (11)
Furthermore, there are controversies over the usage of SLNB amid patients with pre-
operative DCIS diagnosis. Uses of radioactive iodine in the form of essential urgent treatment
from a range of views, and by conducting SPECT/CT. Another potential drawback is the fact
that lymphatic lakes or lymphangioma are also often misinterpreted to be lymph nodes (11).
Image reading might also get intricate due to adjacent tissues that contain radioactivity.
Likewise, although the identification rate is greater and false-negative rates (FNR) are lower,
when two mapping techniques of radiocolloid and blue dyes are used together, there is lack of
consensus on the technique that should be used. Researchers have proposed a general agreement
that administration of a radiocolloid that measures 100-200 nm is the best compromise between
optimal retention in SLN and fast lymphatic drainage (12).
Figure 2- Planar images and anterior (a) and lateral projections (b) of a
lymphoscintigraphy of a 55-year-old woman with a breast cancer in the right ULQ.
Source- (11)
Furthermore, there are controversies over the usage of SLNB amid patients with pre-
operative DCIS diagnosis. Uses of radioactive iodine in the form of essential urgent treatment
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6NUCLEAR MEDICINE
method, following thyroidectomy among patients suffering from differentiated thyroid
carcinoma, has also been associated with certain latent side effects that have been classified as
late and early complications. Early complications comprise of radiation thyroiditis,
gastrointestinal symptoms, suppression of bone marrow, gonadal damage, nasolacrimal duct
obstruction, dry eye, and xerostomia/ sialadenitis. In contrast, late complications of this nuclear
medicine application include pulmonary fibrosis, secondary cancer, genetic effects, and
permanent suppression of bone marrow (13).
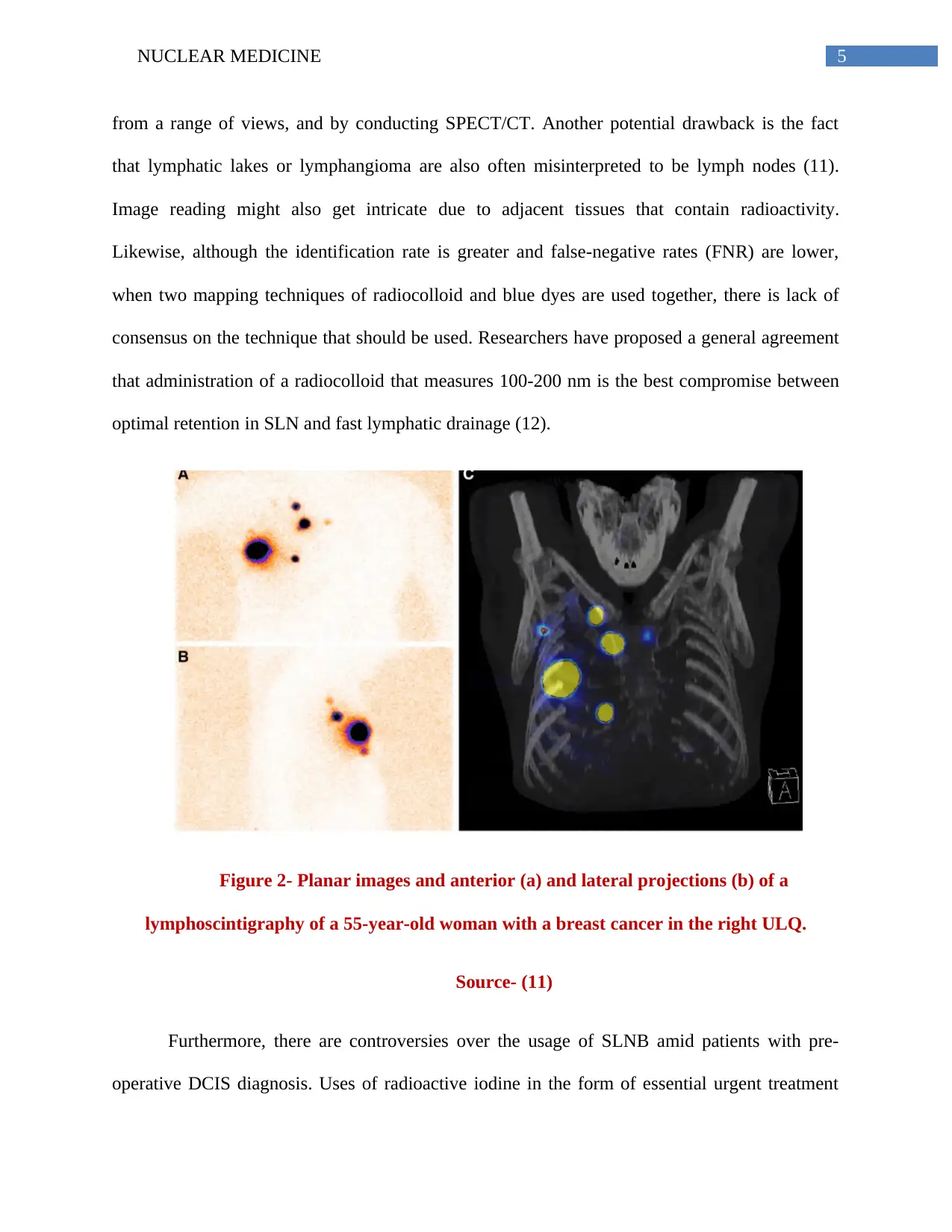
Another major impediment of nuclear medicine includes post-radioembolization
syndrome that typically comprises of abdominal pain and discomfort, fatigue, nausea, vomiting,
and cachexia. Although the patients do not actually require hospitalization, they are commonly
administered antinauseants such as, ondasetron, prior to their treatment. Complications due to
radioactive procedures have also been associated with pre-existing dysfunction of the liver that
often gives rise to a potentially grave incident, referred to as radiation-induced liver disease
(RILD) (14). Implementation of nuclear medicine has also been associated with futile efforts to
minimise the risk that are nonexistent, which are considered a major source of the onset of
persistent radiophobia. Radiophobia has been found to be detrimental to all patients, which
results in stress, and thereby leads to avoidance of imaging and suboptimal image quality. This in
turn increases the likelihood of misdiagnosis of health condition, and consequently harms the
patients, while not offering them any compensating benefits (15).
method, following thyroidectomy among patients suffering from differentiated thyroid
carcinoma, has also been associated with certain latent side effects that have been classified as
late and early complications. Early complications comprise of radiation thyroiditis,
gastrointestinal symptoms, suppression of bone marrow, gonadal damage, nasolacrimal duct
obstruction, dry eye, and xerostomia/ sialadenitis. In contrast, late complications of this nuclear
medicine application include pulmonary fibrosis, secondary cancer, genetic effects, and
permanent suppression of bone marrow (13).
Another major impediment of nuclear medicine includes post-radioembolization
syndrome that typically comprises of abdominal pain and discomfort, fatigue, nausea, vomiting,
and cachexia. Although the patients do not actually require hospitalization, they are commonly
administered antinauseants such as, ondasetron, prior to their treatment. Complications due to
radioactive procedures have also been associated with pre-existing dysfunction of the liver that
often gives rise to a potentially grave incident, referred to as radiation-induced liver disease
(RILD) (14). Implementation of nuclear medicine has also been associated with futile efforts to
minimise the risk that are nonexistent, which are considered a major source of the onset of
persistent radiophobia. Radiophobia has been found to be detrimental to all patients, which
results in stress, and thereby leads to avoidance of imaging and suboptimal image quality. This in
turn increases the likelihood of misdiagnosis of health condition, and consequently harms the
patients, while not offering them any compensating benefits (15).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7NUCLEAR MEDICINE
Figure 3- Planar Tc-99m MAA scan demonstrating high LSF (76%).
Source- (14)
Conclusion- To conclude it can be stated that uses of nuclear medicine helps in the
production of functional images that provide valuable information to doctors, regarding the
particular ways in which organs function. Another major advantage of nuclear medicine imaging
can be accredited to the fact that it helps in analysis of the whole body thereby facilitating
identification of lesions in several places such as dissemination of cancer, or presence of
infectious lesions, or suspicion of infectious lesions. I hold the opinion that combination of high
sensitivity nuclear imaging with precision in anatomical image localisation, helps in proper
detection of lymphoedema and melanoma. However, it comes with several health risks among
Figure 3- Planar Tc-99m MAA scan demonstrating high LSF (76%).
Source- (14)
Conclusion- To conclude it can be stated that uses of nuclear medicine helps in the
production of functional images that provide valuable information to doctors, regarding the
particular ways in which organs function. Another major advantage of nuclear medicine imaging
can be accredited to the fact that it helps in analysis of the whole body thereby facilitating
identification of lesions in several places such as dissemination of cancer, or presence of
infectious lesions, or suspicion of infectious lesions. I hold the opinion that combination of high
sensitivity nuclear imaging with precision in anatomical image localisation, helps in proper
detection of lymphoedema and melanoma. However, it comes with several health risks among
8NUCLEAR MEDICINE
pregnant, young and elderly patients and has not promised a 100% guarantee in terms of medical
treatment.
pregnant, young and elderly patients and has not promised a 100% guarantee in terms of medical
treatment.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9NUCLEAR MEDICINE
References
1) Hine GJ, editor. Instrumentation in nuclear medicine. Academic Press; 2016 Jan 21.
2) Nakajima K, Matsumoto N, Kasai T, Matsuo S, Kiso K, Okuda K. Normal values and
standardization of parameters in nuclear cardiology: Japanese Society of Nuclear
Medicine working group database. Annals of nuclear medicine. 2016 Apr 1;30(3):188-
99.
3) Bluemel C, Herrmann K, Giammarile F, Nieweg OE, Dubreuil J, Testori A, Audisio RA,
Zoras O, Lassmann M, Chakera AH, Uren R. EANM practice guidelines for
lymphoscintigraphy and sentinel lymph node biopsy in melanoma. European journal of
nuclear medicine and molecular imaging. 2015 Oct 1;42(11):1750-66.
4) Moncayo VM, Aarsvold JN, Alazraki NP. Lymphoscintigraphy and sentinel nodes.
Journal of Nuclear Medicine. 2015 Jun 1;56(6):901-7.
5) Vidal-Sicart S, van Leeuwen FW, van den Berg NS, Olmos RA. Fluorescent
radiocolloids: are hybrid tracers the future for lymphatic mapping?. European Journal of
Nuclear Medicine and Molecular Imaging. 2015 Oct 1;42(11):1627-30.
6) Yoo J, Choi JY, Hwang JH, Kim DI, Kim YW, Choe YS, Lee KH, Kim BT. Prognostic
value of lymphoscintigraphy in patients with gynecological cancer‐related lymphedema.
Journal of surgical oncology. 2014 Jun;109(8):760-3.
7) Yoo JN, Cheong YS, Min YS, Lee SW, Park HY, Jung TD. Validity of quantitative
lymphoscintigraphy as a lymphedema assessment tool for patients with breast cancer.
Annals of rehabilitation medicine. 2015 Dec;39(6):931.
8) Rossi M, Grassi R, Costa R, Di Rosa L, D’arpa S, Moschella F, Cordova A. Evaluation
of the upper limb lymphatic system: A prospective lymphoscintigraphic study in
References
1) Hine GJ, editor. Instrumentation in nuclear medicine. Academic Press; 2016 Jan 21.
2) Nakajima K, Matsumoto N, Kasai T, Matsuo S, Kiso K, Okuda K. Normal values and
standardization of parameters in nuclear cardiology: Japanese Society of Nuclear
Medicine working group database. Annals of nuclear medicine. 2016 Apr 1;30(3):188-
99.
3) Bluemel C, Herrmann K, Giammarile F, Nieweg OE, Dubreuil J, Testori A, Audisio RA,
Zoras O, Lassmann M, Chakera AH, Uren R. EANM practice guidelines for
lymphoscintigraphy and sentinel lymph node biopsy in melanoma. European journal of
nuclear medicine and molecular imaging. 2015 Oct 1;42(11):1750-66.
4) Moncayo VM, Aarsvold JN, Alazraki NP. Lymphoscintigraphy and sentinel nodes.
Journal of Nuclear Medicine. 2015 Jun 1;56(6):901-7.
5) Vidal-Sicart S, van Leeuwen FW, van den Berg NS, Olmos RA. Fluorescent
radiocolloids: are hybrid tracers the future for lymphatic mapping?. European Journal of
Nuclear Medicine and Molecular Imaging. 2015 Oct 1;42(11):1627-30.
6) Yoo J, Choi JY, Hwang JH, Kim DI, Kim YW, Choe YS, Lee KH, Kim BT. Prognostic
value of lymphoscintigraphy in patients with gynecological cancer‐related lymphedema.
Journal of surgical oncology. 2014 Jun;109(8):760-3.
7) Yoo JN, Cheong YS, Min YS, Lee SW, Park HY, Jung TD. Validity of quantitative
lymphoscintigraphy as a lymphedema assessment tool for patients with breast cancer.
Annals of rehabilitation medicine. 2015 Dec;39(6):931.
8) Rossi M, Grassi R, Costa R, Di Rosa L, D’arpa S, Moschella F, Cordova A. Evaluation
of the upper limb lymphatic system: A prospective lymphoscintigraphic study in
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10NUCLEAR MEDICINE
melanoma patients and healthy controls. Plastic and reconstructive surgery. 2016 Dec
1;138(6):1321-31.
9) Giammarile F, Bozkurt MF, Cibula D, Pahisa J, Oyen WJ, Paredes P, Olmos RV, Sicart
SV. The EANM clinical and technical guidelines for lymphoscintigraphy and sentinel
node localization in gynaecological cancers. European journal of nuclear medicine and
molecular imaging. 2014 Jul 1;41(7):1463-77.
10) Bluemel C, Herrmann K, Giammarile F, Nieweg OE, Dubreuil J, Testori A, Audisio RA,
Zoras O, Lassmann M, Chakera AH, Uren R. EANM practice guidelines for
lymphoscintigraphy and sentinel lymph node biopsy in melanoma. European journal of
nuclear medicine and molecular imaging. 2015 Oct 1;42(11):1750-66.
11) Serrano-Vicente J, Rayo-Madrid JI, Domínguez-Grande ML, Infante-Torre JR, García-
Bernardo L, Moreno-Caballero M, Medina-Romero F, Durán-Barquero C. Role of
SPECT-CT in breast cancer sentinel node biopsy when internal mammary chain drainage
is observed. Clinical and Translational Oncology. 2016 Apr 1;18(4):418-25.
12) Manca G, Rubello D, Tardelli E, Giammarile F, Mazzarri S, Boni G, Chondrogiannis S,
Marzola MC, Chiacchio S, Ghilli M, Roncella M. Sentinel lymph node biopsy in breast
cancer: indications, contraindications, and controversies. Clinical nuclear medicine. 2016
Feb 1;41(2):126-33.
13) Fard-Esfahani A, Emami-Ardekani A, Fallahi B, Fard-Esfahani P, Beiki D, Hassanzadeh-
Rad A, Eftekhari M. Adverse effects of radioactive iodine-131 treatment for
differentiated thyroid carcinoma. Nuclear medicine communications. 2014 Aug
1;35(8):808-17.
melanoma patients and healthy controls. Plastic and reconstructive surgery. 2016 Dec
1;138(6):1321-31.
9) Giammarile F, Bozkurt MF, Cibula D, Pahisa J, Oyen WJ, Paredes P, Olmos RV, Sicart
SV. The EANM clinical and technical guidelines for lymphoscintigraphy and sentinel
node localization in gynaecological cancers. European journal of nuclear medicine and
molecular imaging. 2014 Jul 1;41(7):1463-77.
10) Bluemel C, Herrmann K, Giammarile F, Nieweg OE, Dubreuil J, Testori A, Audisio RA,
Zoras O, Lassmann M, Chakera AH, Uren R. EANM practice guidelines for
lymphoscintigraphy and sentinel lymph node biopsy in melanoma. European journal of
nuclear medicine and molecular imaging. 2015 Oct 1;42(11):1750-66.
11) Serrano-Vicente J, Rayo-Madrid JI, Domínguez-Grande ML, Infante-Torre JR, García-
Bernardo L, Moreno-Caballero M, Medina-Romero F, Durán-Barquero C. Role of
SPECT-CT in breast cancer sentinel node biopsy when internal mammary chain drainage
is observed. Clinical and Translational Oncology. 2016 Apr 1;18(4):418-25.
12) Manca G, Rubello D, Tardelli E, Giammarile F, Mazzarri S, Boni G, Chondrogiannis S,
Marzola MC, Chiacchio S, Ghilli M, Roncella M. Sentinel lymph node biopsy in breast
cancer: indications, contraindications, and controversies. Clinical nuclear medicine. 2016
Feb 1;41(2):126-33.
13) Fard-Esfahani A, Emami-Ardekani A, Fallahi B, Fard-Esfahani P, Beiki D, Hassanzadeh-
Rad A, Eftekhari M. Adverse effects of radioactive iodine-131 treatment for
differentiated thyroid carcinoma. Nuclear medicine communications. 2014 Aug
1;35(8):808-17.
11NUCLEAR MEDICINE
14) Riaz A, Awais R, Salem R. Side effects of yttrium-90 radioembolization. Frontiers in
oncology. 2014 Jul 29;4:198.
15) Siegel JA, Sacks B, Pennington CW, Welsh JS. Dose optimization to minimize radiation
risk for children undergoing CT and nuclear medicine imaging is misguided and
detrimental. Journal of Nuclear Medicine. 2017 Jun 1;58(6):865-8.
14) Riaz A, Awais R, Salem R. Side effects of yttrium-90 radioembolization. Frontiers in
oncology. 2014 Jul 29;4:198.
15) Siegel JA, Sacks B, Pennington CW, Welsh JS. Dose optimization to minimize radiation
risk for children undergoing CT and nuclear medicine imaging is misguided and
detrimental. Journal of Nuclear Medicine. 2017 Jun 1;58(6):865-8.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.