NUR250 Assessment 1 S1: Pulmonary Function Testing
VerifiedAdded on 2022/08/25
|14
|3614
|16
Assignment
AI Summary
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
NUR250 Assessment 1 S1 2020 Assessment One
Template
Task 1
Analysis of the case scenario suggests that the patient Laura is suffering from
bronchitis and her presenting complaints include wheezing sound during expiration,
and increase respiratory rate, increased heart rate, elevated blood pressure, high
body temperature, and a sharp pain in her chest on inspiration. Bronchitis is
characterized by an inflammation of the medium and large size airways of bronchi
that are located in the lungs, which leads to coughing. Some of the common signs
and symptoms of bronchitis comprise of shortness of breath, pain in chest, coughing
up sputum and wheezing, most of which were reported by the patient (Jackwood &
de Wit, 2020). Bronchitis can be described as a result of severe inflammation of the
bronchi, and commonly occurs due to exposure to pollutants, allergens, or viral
infection.
The pathophysiology for this condition can be accredited to the excess
production and accumulation of mucus, as a response to signals of inflammation,
which is also known as mucus metaplasia. In patients suffering from bronchitis this
hypersecretion of mucus occurs due to the goblet cells and is primarily associated
with T cells. It is thought to be e correlated to the end production of the Th2 cells
(Gelb, Christenson & Nadel, 2016). Mucus metaplasia generally causes obstruction
of airflow by luminal occlusion. The epithelial layer gradually gets thickened and
intrudes the lumen, following which the mucus brings about an alteration in surface
tension of the airways. This in turn increases the risk of collapsing, and decreases
the capability of gaseous exchange and air flow to occur inside the lungs. This
eventually contributes to inability of a person to breathe out completely. A decrease
in flow of air occurs at the time of breathing out, since pressure in the chest leads to
compression of the airways during this time (Raju et al., 2016).
1
Double click here to fill in this footer
Last name__ _student number_NUR250 S1 2020 Assessment 1
Template
Task 1
Analysis of the case scenario suggests that the patient Laura is suffering from
bronchitis and her presenting complaints include wheezing sound during expiration,
and increase respiratory rate, increased heart rate, elevated blood pressure, high
body temperature, and a sharp pain in her chest on inspiration. Bronchitis is
characterized by an inflammation of the medium and large size airways of bronchi
that are located in the lungs, which leads to coughing. Some of the common signs
and symptoms of bronchitis comprise of shortness of breath, pain in chest, coughing
up sputum and wheezing, most of which were reported by the patient (Jackwood &
de Wit, 2020). Bronchitis can be described as a result of severe inflammation of the
bronchi, and commonly occurs due to exposure to pollutants, allergens, or viral
infection.
The pathophysiology for this condition can be accredited to the excess
production and accumulation of mucus, as a response to signals of inflammation,
which is also known as mucus metaplasia. In patients suffering from bronchitis this
hypersecretion of mucus occurs due to the goblet cells and is primarily associated
with T cells. It is thought to be e correlated to the end production of the Th2 cells
(Gelb, Christenson & Nadel, 2016). Mucus metaplasia generally causes obstruction
of airflow by luminal occlusion. The epithelial layer gradually gets thickened and
intrudes the lumen, following which the mucus brings about an alteration in surface
tension of the airways. This in turn increases the risk of collapsing, and decreases
the capability of gaseous exchange and air flow to occur inside the lungs. This
eventually contributes to inability of a person to breathe out completely. A decrease
in flow of air occurs at the time of breathing out, since pressure in the chest leads to
compression of the airways during this time (Raju et al., 2016).
1
Double click here to fill in this footer
Last name__ _student number_NUR250 S1 2020 Assessment 1
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
The current presentation of the patient Laura is associated with her medical
history of asthma, smoking habit, and obesity. Presence of asthma resulted in
inflammation of her airways, thus leading to chest tightness, shortness of breath, and
wheezing. It also triggered an inflammation of the bronchi, which in turn resulted in
respiratory condition and further exacerbated her health condition (Lai, Chen, Peng
& Zhan, 2017). Asthma is associated with bronchial hyperresponsiveness and
intermittent obstruction of air flow. Presentation of antigen by the dendritic cells with
cytokine and lymphocyte response also stimulated airway inflammation and resulted
in bronchitis. The inflammatory cells that are particularly associated with bronchitis
include macrophages and neutrophil granulocytes, both of which are white blood
cells.
Smokers have been found to contain an additional involvement of the Tc1
lymphocyte cells, and chemotactic factors act in the form of inflammatory mediators
and bring about the cell response. Additionally, her smoking habits might have
resulted in oxidative stress generated by the free radical concentration present in
tobacco smoke, thereby releasing inflammatory cells, and breaking down the
connective tissues present in the lungs, thus causing damage and emphysema
(Axelsson et al., 2016). This eventually contributed to poor airflow, and poor
respiratory exchange of gases. Obesity and being overweight have also been
associated with increased risk of bronchitis, since obesity results in mechanical
compression of lungs and chest cavity, thereby causing restrictive pulmonary
damage. Excess accumulation of fat also decreases compliance of the total
respiratory system, in consequence decreasing strength of the respiratory muscles
and increasing pulmonary resistance, and triggering bronchitis (Chandler, 2016).
2
Double click here to fill in this footer
Last name__ _student number_NUR250 S1 2020 Assessment 1
history of asthma, smoking habit, and obesity. Presence of asthma resulted in
inflammation of her airways, thus leading to chest tightness, shortness of breath, and
wheezing. It also triggered an inflammation of the bronchi, which in turn resulted in
respiratory condition and further exacerbated her health condition (Lai, Chen, Peng
& Zhan, 2017). Asthma is associated with bronchial hyperresponsiveness and
intermittent obstruction of air flow. Presentation of antigen by the dendritic cells with
cytokine and lymphocyte response also stimulated airway inflammation and resulted
in bronchitis. The inflammatory cells that are particularly associated with bronchitis
include macrophages and neutrophil granulocytes, both of which are white blood
cells.
Smokers have been found to contain an additional involvement of the Tc1
lymphocyte cells, and chemotactic factors act in the form of inflammatory mediators
and bring about the cell response. Additionally, her smoking habits might have
resulted in oxidative stress generated by the free radical concentration present in
tobacco smoke, thereby releasing inflammatory cells, and breaking down the
connective tissues present in the lungs, thus causing damage and emphysema
(Axelsson et al., 2016). This eventually contributed to poor airflow, and poor
respiratory exchange of gases. Obesity and being overweight have also been
associated with increased risk of bronchitis, since obesity results in mechanical
compression of lungs and chest cavity, thereby causing restrictive pulmonary
damage. Excess accumulation of fat also decreases compliance of the total
respiratory system, in consequence decreasing strength of the respiratory muscles
and increasing pulmonary resistance, and triggering bronchitis (Chandler, 2016).
2
Double click here to fill in this footer
Last name__ _student number_NUR250 S1 2020 Assessment 1
Task 2
Nursing Care Plan: (type in your patient’s name here and then delete these instructions)
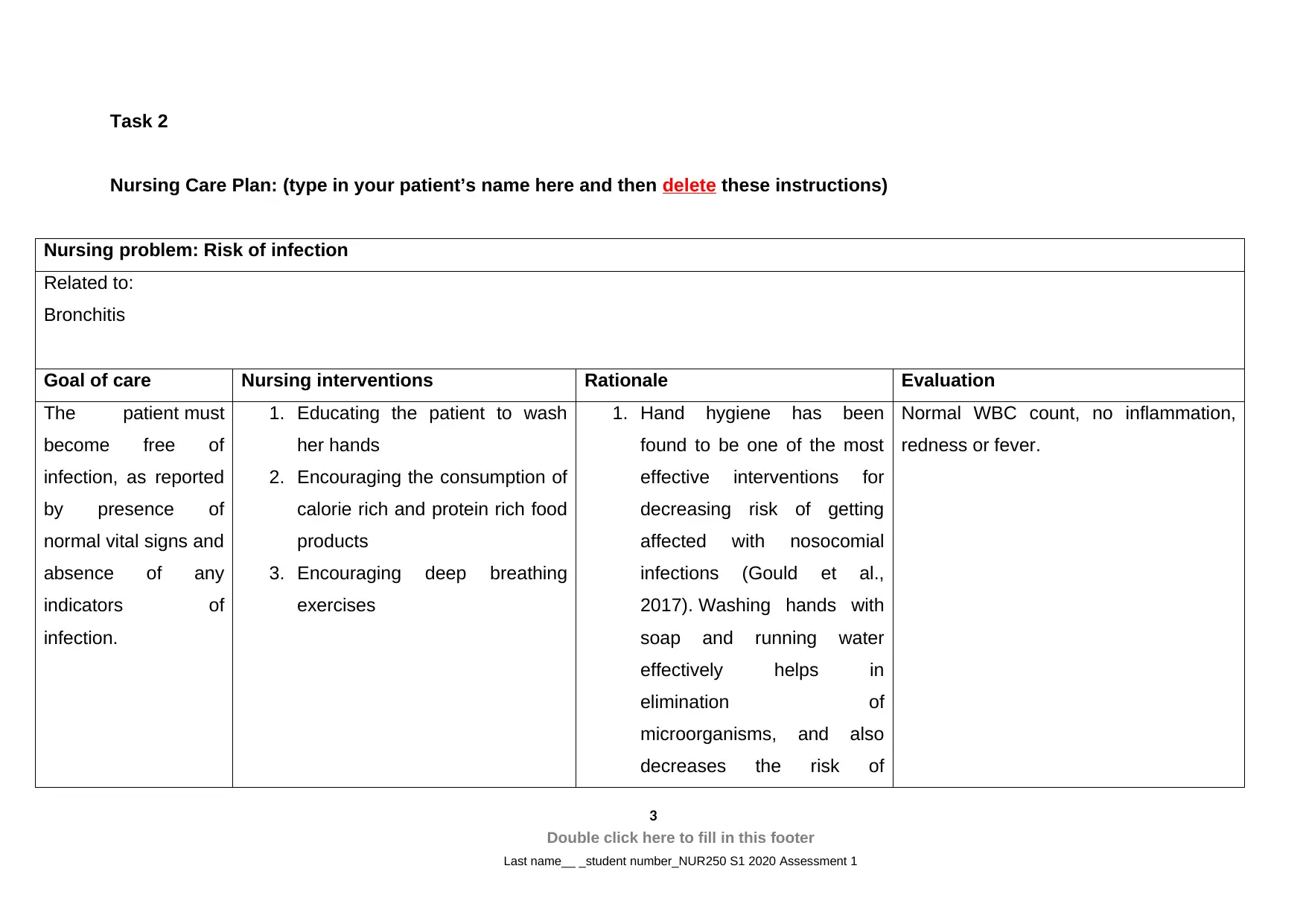
Nursing problem: Risk of infection
Related to:
Bronchitis
Goal of care Nursing interventions Rationale Evaluation
The patient must
become free of
infection, as reported
by presence of
normal vital signs and
absence of any
indicators of
infection.
1. Educating the patient to wash
her hands
2. Encouraging the consumption of
calorie rich and protein rich food
products
3. Encouraging deep breathing
exercises
1. Hand hygiene has been
found to be one of the most
effective interventions for
decreasing risk of getting
affected with nosocomial
infections (Gould et al.,
2017). Washing hands with
soap and running water
effectively helps in
elimination of
microorganisms, and also
decreases the risk of
Normal WBC count, no inflammation,
redness or fever.
3
Double click here to fill in this footer
Last name__ _student number_NUR250 S1 2020 Assessment 1
Nursing Care Plan: (type in your patient’s name here and then delete these instructions)
Nursing problem: Risk of infection
Related to:
Bronchitis
Goal of care Nursing interventions Rationale Evaluation
The patient must
become free of
infection, as reported
by presence of
normal vital signs and
absence of any
indicators of
infection.
1. Educating the patient to wash
her hands
2. Encouraging the consumption of
calorie rich and protein rich food
products
3. Encouraging deep breathing
exercises
1. Hand hygiene has been
found to be one of the most
effective interventions for
decreasing risk of getting
affected with nosocomial
infections (Gould et al.,
2017). Washing hands with
soap and running water
effectively helps in
elimination of
microorganisms, and also
decreases the risk of
Normal WBC count, no inflammation,
redness or fever.
3
Double click here to fill in this footer
Last name__ _student number_NUR250 S1 2020 Assessment 1
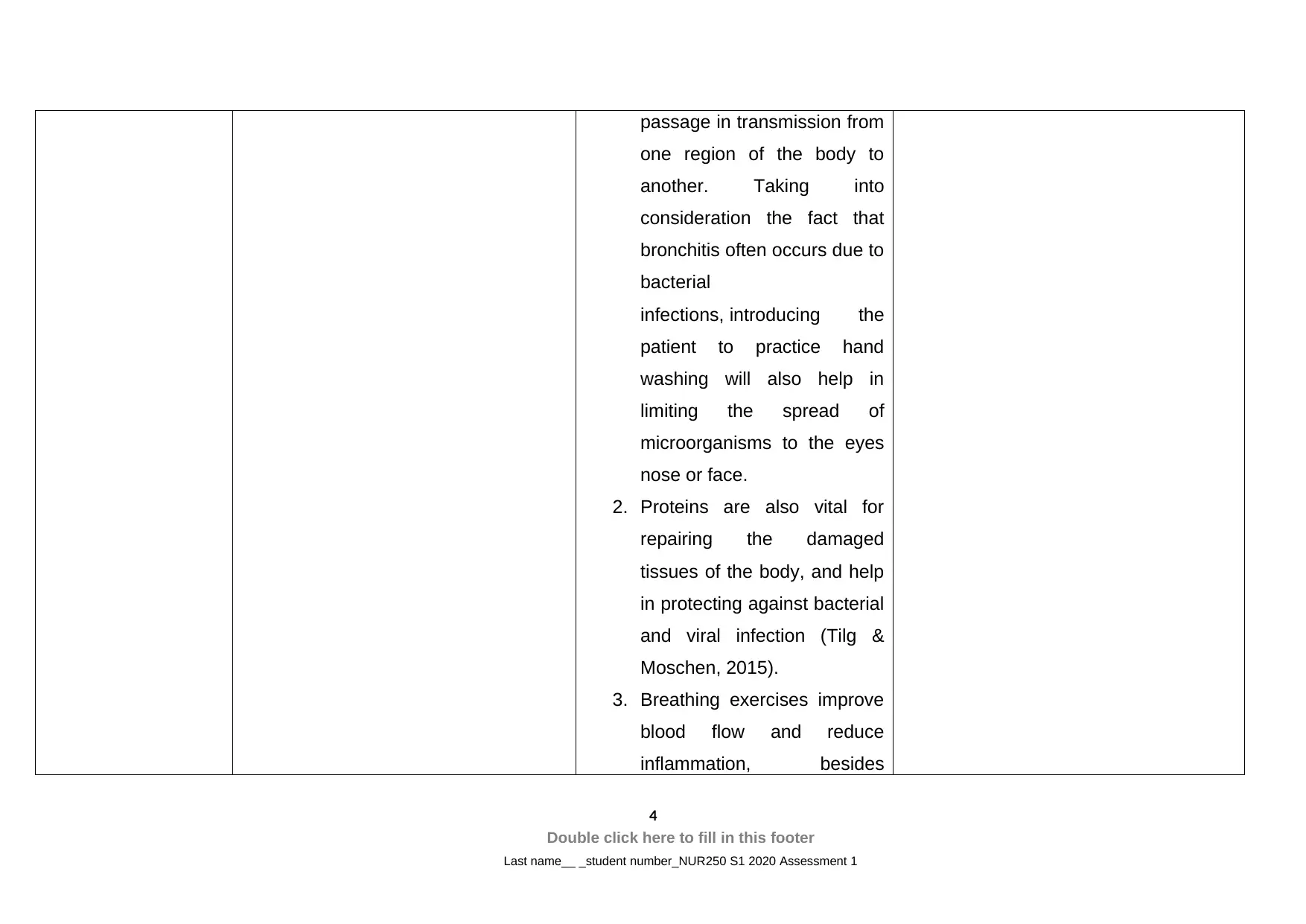
passage in transmission from
one region of the body to
another. Taking into
consideration the fact that
bronchitis often occurs due to
bacterial
infections, introducing the
patient to practice hand
washing will also help in
limiting the spread of
microorganisms to the eyes
nose or face.
2. Proteins are also vital for
repairing the damaged
tissues of the body, and help
in protecting against bacterial
and viral infection (Tilg &
Moschen, 2015).
3. Breathing exercises improve
blood flow and reduce
inflammation, besides
4
Double click here to fill in this footer
Last name__ _student number_NUR250 S1 2020 Assessment 1
one region of the body to
another. Taking into
consideration the fact that
bronchitis often occurs due to
bacterial
infections, introducing the
patient to practice hand
washing will also help in
limiting the spread of
microorganisms to the eyes
nose or face.
2. Proteins are also vital for
repairing the damaged
tissues of the body, and help
in protecting against bacterial
and viral infection (Tilg &
Moschen, 2015).
3. Breathing exercises improve
blood flow and reduce
inflammation, besides
4
Double click here to fill in this footer
Last name__ _student number_NUR250 S1 2020 Assessment 1
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
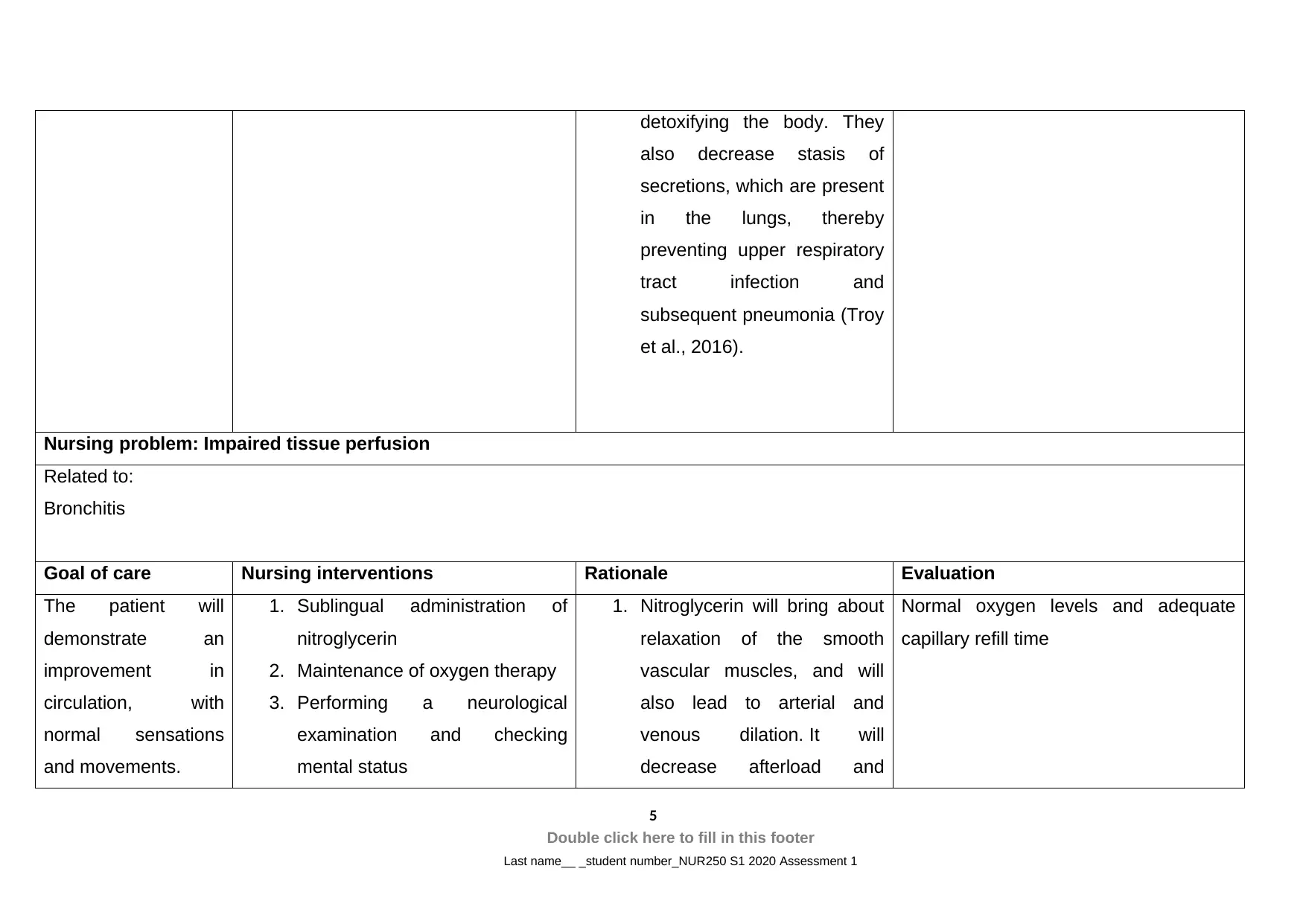
detoxifying the body. They
also decrease stasis of
secretions, which are present
in the lungs, thereby
preventing upper respiratory
tract infection and
subsequent pneumonia (Troy
et al., 2016).
Nursing problem: Impaired tissue perfusion
Related to:
Bronchitis
Goal of care Nursing interventions Rationale Evaluation
The patient will
demonstrate an
improvement in
circulation, with
normal sensations
and movements.
1. Sublingual administration of
nitroglycerin
2. Maintenance of oxygen therapy
3. Performing a neurological
examination and checking
mental status
1. Nitroglycerin will bring about
relaxation of the smooth
vascular muscles, and will
also lead to arterial and
venous dilation. It will
decrease afterload and
Normal oxygen levels and adequate
capillary refill time
5
Double click here to fill in this footer
Last name__ _student number_NUR250 S1 2020 Assessment 1
also decrease stasis of
secretions, which are present
in the lungs, thereby
preventing upper respiratory
tract infection and
subsequent pneumonia (Troy
et al., 2016).
Nursing problem: Impaired tissue perfusion
Related to:
Bronchitis
Goal of care Nursing interventions Rationale Evaluation
The patient will
demonstrate an
improvement in
circulation, with
normal sensations
and movements.
1. Sublingual administration of
nitroglycerin
2. Maintenance of oxygen therapy
3. Performing a neurological
examination and checking
mental status
1. Nitroglycerin will bring about
relaxation of the smooth
vascular muscles, and will
also lead to arterial and
venous dilation. It will
decrease afterload and
Normal oxygen levels and adequate
capillary refill time
5
Double click here to fill in this footer
Last name__ _student number_NUR250 S1 2020 Assessment 1
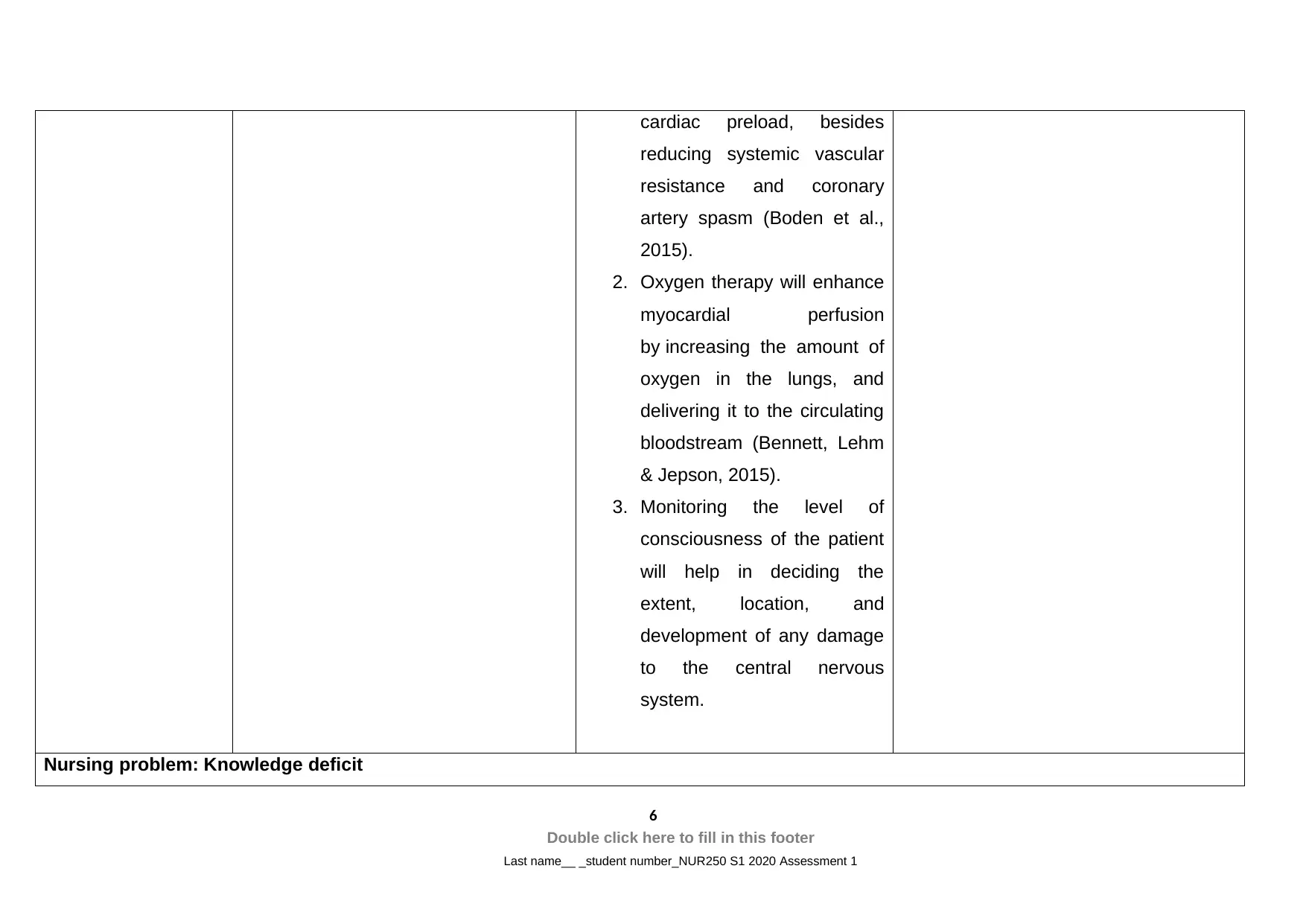
cardiac preload, besides
reducing systemic vascular
resistance and coronary
artery spasm (Boden et al.,
2015).
2. Oxygen therapy will enhance
myocardial perfusion
by increasing the amount of
oxygen in the lungs, and
delivering it to the circulating
bloodstream (Bennett, Lehm
& Jepson, 2015).
3. Monitoring the level of
consciousness of the patient
will help in deciding the
extent, location, and
development of any damage
to the central nervous
system.
Nursing problem: Knowledge deficit
6
Double click here to fill in this footer
Last name__ _student number_NUR250 S1 2020 Assessment 1
reducing systemic vascular
resistance and coronary
artery spasm (Boden et al.,
2015).
2. Oxygen therapy will enhance
myocardial perfusion
by increasing the amount of
oxygen in the lungs, and
delivering it to the circulating
bloodstream (Bennett, Lehm
& Jepson, 2015).
3. Monitoring the level of
consciousness of the patient
will help in deciding the
extent, location, and
development of any damage
to the central nervous
system.
Nursing problem: Knowledge deficit
6
Double click here to fill in this footer
Last name__ _student number_NUR250 S1 2020 Assessment 1
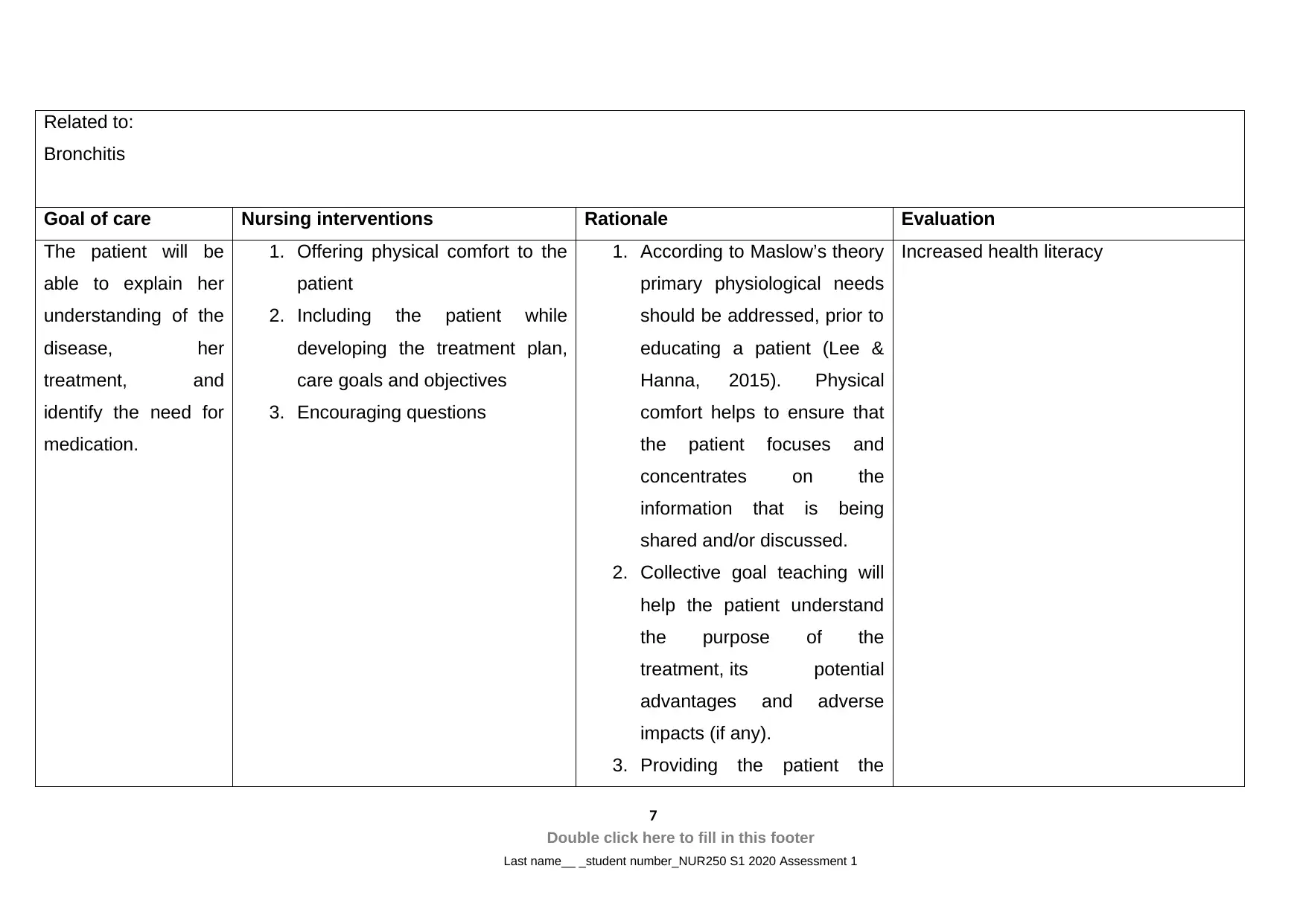
Related to:
Bronchitis
Goal of care Nursing interventions Rationale Evaluation
The patient will be
able to explain her
understanding of the
disease, her
treatment, and
identify the need for
medication.
1. Offering physical comfort to the
patient
2. Including the patient while
developing the treatment plan,
care goals and objectives
3. Encouraging questions
1. According to Maslow’s theory
primary physiological needs
should be addressed, prior to
educating a patient (Lee &
Hanna, 2015). Physical
comfort helps to ensure that
the patient focuses and
concentrates on the
information that is being
shared and/or discussed.
2. Collective goal teaching will
help the patient understand
the purpose of the
treatment, its potential
advantages and adverse
impacts (if any).
3. Providing the patient the
Increased health literacy
7
Double click here to fill in this footer
Last name__ _student number_NUR250 S1 2020 Assessment 1
Bronchitis
Goal of care Nursing interventions Rationale Evaluation
The patient will be
able to explain her
understanding of the
disease, her
treatment, and
identify the need for
medication.
1. Offering physical comfort to the
patient
2. Including the patient while
developing the treatment plan,
care goals and objectives
3. Encouraging questions
1. According to Maslow’s theory
primary physiological needs
should be addressed, prior to
educating a patient (Lee &
Hanna, 2015). Physical
comfort helps to ensure that
the patient focuses and
concentrates on the
information that is being
shared and/or discussed.
2. Collective goal teaching will
help the patient understand
the purpose of the
treatment, its potential
advantages and adverse
impacts (if any).
3. Providing the patient the
Increased health literacy
7
Double click here to fill in this footer
Last name__ _student number_NUR250 S1 2020 Assessment 1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
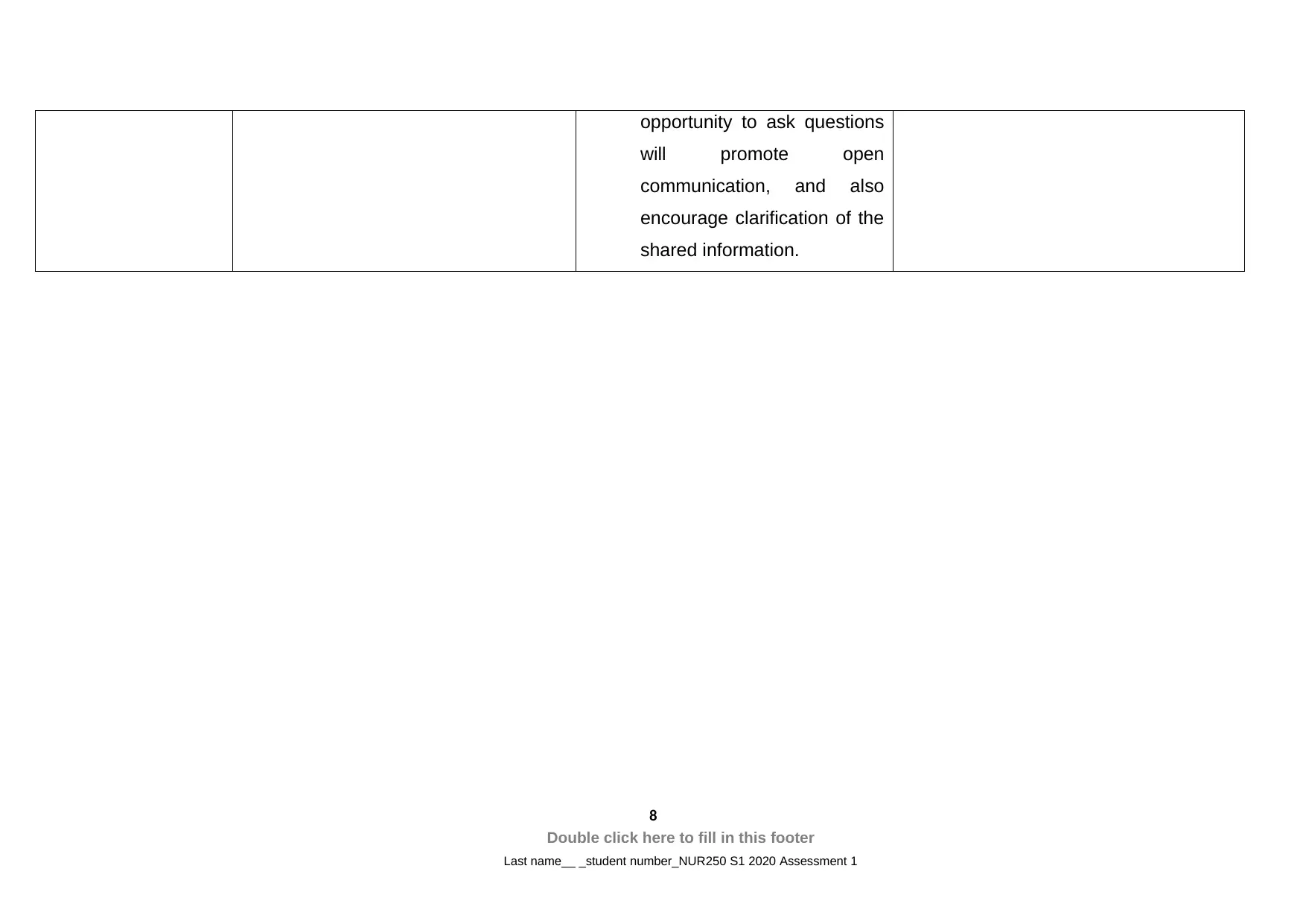
opportunity to ask questions
will promote open
communication, and also
encourage clarification of the
shared information.
8
Double click here to fill in this footer
Last name__ _student number_NUR250 S1 2020 Assessment 1
will promote open
communication, and also
encourage clarification of the
shared information.
8
Double click here to fill in this footer
Last name__ _student number_NUR250 S1 2020 Assessment 1
Task 3
Discharge planning typically involves the healthcare professionals, patients,
and family members, making appropriate arrangements for ensuring smooth
transition of the patient from the healthcare facility to home, and takes into
consideration several factors like, follow-up appointment, tests, and personal health
objectives (Gonçalves‐Bradley et al., 2016). Two significant points that will be
included in preparation of the patient for discharge are namely, understanding her
health condition and recovery from bronchitis.
The patient Laura will be educated that most cases of bronchitis are self
limited, and typically resolve within a few weeks by themselves. However, pain
medications might help with providing relief to the symptoms. She will be provided an
explanation on the prognosis of bronchitis, which lasts for a few days or weeks. It
might closely follow or accompany flu or cold, or might occur on its own. The signs
and symptoms that should be taken into consideration after discharge from the
hospital are dry cough, together with waking up at night. The patient will be asked to
keep a check on symptoms of productive or wet cough, which might be accompanied
by headache and fever (Chang et al., 2016). On observing such symptoms, in
addition to mucus production with blood she should immediately report to the
healthcare professional and seek medical help.
In relation to recovery from bronchitis, Laura will be explained that the
symptoms can be effectively managed by improving adherence to the recommended
treatment plan. In order to recover from bronchitis, she should show adherence to the
medications that have been prescribed. The patient will be shown how to use inhaler
that will make breathing easier, and lead to less coughing. She will also be educated
that the inhaler administers medicine in the form of a mist, such that it can be easily
taken into the lungs (Pothirat et al., 2015). She will be taught to ensure that the
correct amount of medicine is being administered through the inhaler, and will be
recommended to breathe in her mouth at a steady and slow rate. Instructions will
also be provided to clean the inhaler at least once in a week. She will also be taught
about different lifestyle modifications that with help in taking care of her health like
smoking cessation, avoiding alcohol consumption, drinking more liquid, consumption
9
Double click here to fill in this footer
Last name__ _student number_NUR250 S1 2020 Assessment 1
Discharge planning typically involves the healthcare professionals, patients,
and family members, making appropriate arrangements for ensuring smooth
transition of the patient from the healthcare facility to home, and takes into
consideration several factors like, follow-up appointment, tests, and personal health
objectives (Gonçalves‐Bradley et al., 2016). Two significant points that will be
included in preparation of the patient for discharge are namely, understanding her
health condition and recovery from bronchitis.
The patient Laura will be educated that most cases of bronchitis are self
limited, and typically resolve within a few weeks by themselves. However, pain
medications might help with providing relief to the symptoms. She will be provided an
explanation on the prognosis of bronchitis, which lasts for a few days or weeks. It
might closely follow or accompany flu or cold, or might occur on its own. The signs
and symptoms that should be taken into consideration after discharge from the
hospital are dry cough, together with waking up at night. The patient will be asked to
keep a check on symptoms of productive or wet cough, which might be accompanied
by headache and fever (Chang et al., 2016). On observing such symptoms, in
addition to mucus production with blood she should immediately report to the
healthcare professional and seek medical help.
In relation to recovery from bronchitis, Laura will be explained that the
symptoms can be effectively managed by improving adherence to the recommended
treatment plan. In order to recover from bronchitis, she should show adherence to the
medications that have been prescribed. The patient will be shown how to use inhaler
that will make breathing easier, and lead to less coughing. She will also be educated
that the inhaler administers medicine in the form of a mist, such that it can be easily
taken into the lungs (Pothirat et al., 2015). She will be taught to ensure that the
correct amount of medicine is being administered through the inhaler, and will be
recommended to breathe in her mouth at a steady and slow rate. Instructions will
also be provided to clean the inhaler at least once in a week. She will also be taught
about different lifestyle modifications that with help in taking care of her health like
smoking cessation, avoiding alcohol consumption, drinking more liquid, consumption
9
Double click here to fill in this footer
Last name__ _student number_NUR250 S1 2020 Assessment 1
of healthy food, and use of a cool mist humidifier for increasing air moisture in her
residence (Singh, Avula & Zahn, 2019).
One education strategy that will be used for helping the patient implement the
information shared in her daily routine is the dissemination of brochures and leaflets
on bronchitis and its management. These printed resources will cover extensive
information on the health ailment that the patient is suffering from, and will also
provide a snapshot of the steps that need to be followed, post discharge from the
hospital. They will contain contact information of the healthcare personnel under
circumstances of sudden exacerbation of the symptoms. Brochures contain
information in an illustrative format that will increase understanding of the patient,
and will particularly prove beneficial in capturing undivided attention. Not only will it
graphically illustrate the benefits of showing adherence to the recommendations, but
will also help the patient implement the strategies accurately in her daily practice.
Task 4
A usual medication is ipratropium bromide MDI 21mcg INH. Also sold under
the name of atrovent, this medication has been prescribed to the patient, since it
brings about an opening of the large and medium airways located in the lungs, and is
used for the management of asthma and/or chronic obstructive pulmonary disease
(COPD). In its chemical form, ipratropium bromide is present as of quaternary
ammonium compound, generated from the action of isopropyl bromide and atropine.
The drug has been found to exhibit broncholytic action by bringing about a decrease
in cholinergic influence on the musculature of the bronchi. It leads to a blockage of
the muscarinic acetylcholine receptors, thus promoting cyclic guanosine
monophosphate (cGMP) degradation, and leading to a reduction in the
cGMP intracellular concentration (Koumbourlis & Mastropietro, 2015). This eventually
reduces smooth muscle vasculature in the lungs, thus preventing additional secretion
of mucus and bronchoconstriction. The drug belongs to the category of muscarinic
antagonist, and fails to diffuse in the circulating bloodstream, thereby preventing any
systemic adverse effects. However, if inhaled in minimal amount, side effects that
resemble anticholinergics might be observed. It can lead to sedation and dry
mouth. Other probable side effects are tachycardia nausea, palpitation, skin flushing,
10
Double click here to fill in this footer
Last name__ _student number_NUR250 S1 2020 Assessment 1
residence (Singh, Avula & Zahn, 2019).
One education strategy that will be used for helping the patient implement the
information shared in her daily routine is the dissemination of brochures and leaflets
on bronchitis and its management. These printed resources will cover extensive
information on the health ailment that the patient is suffering from, and will also
provide a snapshot of the steps that need to be followed, post discharge from the
hospital. They will contain contact information of the healthcare personnel under
circumstances of sudden exacerbation of the symptoms. Brochures contain
information in an illustrative format that will increase understanding of the patient,
and will particularly prove beneficial in capturing undivided attention. Not only will it
graphically illustrate the benefits of showing adherence to the recommendations, but
will also help the patient implement the strategies accurately in her daily practice.
Task 4
A usual medication is ipratropium bromide MDI 21mcg INH. Also sold under
the name of atrovent, this medication has been prescribed to the patient, since it
brings about an opening of the large and medium airways located in the lungs, and is
used for the management of asthma and/or chronic obstructive pulmonary disease
(COPD). In its chemical form, ipratropium bromide is present as of quaternary
ammonium compound, generated from the action of isopropyl bromide and atropine.
The drug has been found to exhibit broncholytic action by bringing about a decrease
in cholinergic influence on the musculature of the bronchi. It leads to a blockage of
the muscarinic acetylcholine receptors, thus promoting cyclic guanosine
monophosphate (cGMP) degradation, and leading to a reduction in the
cGMP intracellular concentration (Koumbourlis & Mastropietro, 2015). This eventually
reduces smooth muscle vasculature in the lungs, thus preventing additional secretion
of mucus and bronchoconstriction. The drug belongs to the category of muscarinic
antagonist, and fails to diffuse in the circulating bloodstream, thereby preventing any
systemic adverse effects. However, if inhaled in minimal amount, side effects that
resemble anticholinergics might be observed. It can lead to sedation and dry
mouth. Other probable side effects are tachycardia nausea, palpitation, skin flushing,
10
Double click here to fill in this footer
Last name__ _student number_NUR250 S1 2020 Assessment 1
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
headache, and acute angle closure glaucoma. Urinary retention is also reported by
some patients who are administered this drug with the help of a nebulizer (Mukherjee
et al., 2015).
One new medication is Prednisolone 25mg OD PO. It has been prescribed
since this is medication is used for the treatment of inflammatory conditions,
allergies, and autoimmune disorders. In other words, prednisolone acts in the form of
a steroid, by preventing release of chemical substances that cause inflammation in
the body. The lipophilic structure of this drug acts as glucocorticoid and facilitates
easy passage through the plasma membrane, following which it binds to the
corresponding glucocorticoid receptor (GCR) that is present in the cytoplasm. After
this binding, a GC/GCR complex gets formed that eventually leads to chaperone
protein dissociation from the receptorsb thereby allowing translocation of the
GC/GCR complex inside the nucleus. On entering the nucleusb particular DNA
binding sites referred to as glucocorticoid response elements (GREs) bind to the
complex and lead to inhibition or expression (Karthikeyan & Sai Koushik, 2016). Anti-
inflammatory proteins are synthesized when the binding occurs to positive GREs,
and the binding to negative GRE leads to implemented in gene transcription
blockage, thus preventing for the exacerbation of the symptoms. Short term impacts
of this drug might include reduce vasodilatation and capillary permeability, in addition
to a decrease in migration of leukocytes to reaction of the inflammation. It might also
inhibit neutrophil apoptosis, thereby inhibiting phospholipase A2, which eventually
decreases arachidonic acid derivatives formation, and production of anti-
inflammatory genes. However other adverse effects associated with this drug might
consist of increased risk of infection, increased appetite, nausea, weight gain, cardio
vascular complications, hyperglycemia, increasing blood pressure, skeletal and
muscular abnormality, neurological effects like headache, convulsion and vertigo,
perforation of nasal septum, and behavioural disturbances (Morshed, 2015). The
drug is also associated with a decrease in potassium, increased thirst and urination,
tingling or numbness sensation, fluid retention, and stomach discomfort or bloating.
11
Double click here to fill in this footer
Last name__ _student number_NUR250 S1 2020 Assessment 1
some patients who are administered this drug with the help of a nebulizer (Mukherjee
et al., 2015).
One new medication is Prednisolone 25mg OD PO. It has been prescribed
since this is medication is used for the treatment of inflammatory conditions,
allergies, and autoimmune disorders. In other words, prednisolone acts in the form of
a steroid, by preventing release of chemical substances that cause inflammation in
the body. The lipophilic structure of this drug acts as glucocorticoid and facilitates
easy passage through the plasma membrane, following which it binds to the
corresponding glucocorticoid receptor (GCR) that is present in the cytoplasm. After
this binding, a GC/GCR complex gets formed that eventually leads to chaperone
protein dissociation from the receptorsb thereby allowing translocation of the
GC/GCR complex inside the nucleus. On entering the nucleusb particular DNA
binding sites referred to as glucocorticoid response elements (GREs) bind to the
complex and lead to inhibition or expression (Karthikeyan & Sai Koushik, 2016). Anti-
inflammatory proteins are synthesized when the binding occurs to positive GREs,
and the binding to negative GRE leads to implemented in gene transcription
blockage, thus preventing for the exacerbation of the symptoms. Short term impacts
of this drug might include reduce vasodilatation and capillary permeability, in addition
to a decrease in migration of leukocytes to reaction of the inflammation. It might also
inhibit neutrophil apoptosis, thereby inhibiting phospholipase A2, which eventually
decreases arachidonic acid derivatives formation, and production of anti-
inflammatory genes. However other adverse effects associated with this drug might
consist of increased risk of infection, increased appetite, nausea, weight gain, cardio
vascular complications, hyperglycemia, increasing blood pressure, skeletal and
muscular abnormality, neurological effects like headache, convulsion and vertigo,
perforation of nasal septum, and behavioural disturbances (Morshed, 2015). The
drug is also associated with a decrease in potassium, increased thirst and urination,
tingling or numbness sensation, fluid retention, and stomach discomfort or bloating.
11
Double click here to fill in this footer
Last name__ _student number_NUR250 S1 2020 Assessment 1
References
Axelsson, M., Ekerljung, L., Eriksson, J., Hagstad, S., Rönmark, E., Lötvall, J., &
Lundbäck, B. (2016). Chronic bronchitis in West Sweden–a matter of smoking
and social class. European clinical respiratory journal, 3(1), 30319.
https://doi.org/10.3402/ecrj.v3.30319
Bennett, M. H., Lehm, J. P., & Jepson, N. (2015). Hyperbaric oxygen therapy for
acute coronary syndrome. Cochrane Database of Systematic Reviews, (7).
https://doi.org/10.1002/14651858.CD004818.pub4
Boden, W. E., Padala, S. K., Cabral, K. P., Buschmann, I. R., & Sidhu, M. S. (2015).
Role of short-acting nitroglycerin in the management of ischemic heart
disease. Drug design, development and therapy, 9, 4793.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4548722/pdf/dddt-9-
4793.pdf
Chandler, M. L. (2016). Impact of obesity on cardiopulmonary disease. Veterinary
Clinics: Small Animal Practice, 46(5), 817-830.
https://doi.org/10.1016/j.cvsm.2016.04.005
Chang, A. B., Upham, J. W., Masters, I. B., Redding, G. R., Gibson, P. G., Marchant,
J. M., & Grimwood, K. (2016). Protracted bacterial bronchitis: the last decade
and the road ahead. Pediatric pulmonology, 51(3), 225-242.
https://doi.org/10.1002/ppul.23351
Gelb, A. F., Christenson, S. A., & Nadel, J. A. (2016). Understanding the
pathophysiology of the asthma–chronic obstructive pulmonary disease overlap
syndrome. Current opinion in pulmonary medicine, 22(2), 100-105.
10.1097/MCP.0000000000000236
Gonçalves‐Bradley, D. C., Lannin, N. A., Clemson, L. M., Cameron, I. D., &
Shepperd, S. (2016). Discharge planning from hospital. Cochrane database of
systematic reviews, (1). https://doi.org/10.1002/14651858.CD000313.pub5
Gould, D. J., Moralejo, D., Drey, N., Chudleigh, J. H., & Taljaard, M. (2017).
Interventions to improve hand hygiene compliance in patient care. Cochrane
database of systematic reviews, (9).
https://doi.org/10.1002/14651858.CD005186.pub4
Jackwood, M. W., & de Wit, S. (2020). Infectious bronchitis. Diseases of poultry, 167-
188. https://doi.org/10.1002/9781119371199.ch4
12
Double click here to fill in this footer
Last name__ _student number_NUR250 S1 2020 Assessment 1
Axelsson, M., Ekerljung, L., Eriksson, J., Hagstad, S., Rönmark, E., Lötvall, J., &
Lundbäck, B. (2016). Chronic bronchitis in West Sweden–a matter of smoking
and social class. European clinical respiratory journal, 3(1), 30319.
https://doi.org/10.3402/ecrj.v3.30319
Bennett, M. H., Lehm, J. P., & Jepson, N. (2015). Hyperbaric oxygen therapy for
acute coronary syndrome. Cochrane Database of Systematic Reviews, (7).
https://doi.org/10.1002/14651858.CD004818.pub4
Boden, W. E., Padala, S. K., Cabral, K. P., Buschmann, I. R., & Sidhu, M. S. (2015).
Role of short-acting nitroglycerin in the management of ischemic heart
disease. Drug design, development and therapy, 9, 4793.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4548722/pdf/dddt-9-
4793.pdf
Chandler, M. L. (2016). Impact of obesity on cardiopulmonary disease. Veterinary
Clinics: Small Animal Practice, 46(5), 817-830.
https://doi.org/10.1016/j.cvsm.2016.04.005
Chang, A. B., Upham, J. W., Masters, I. B., Redding, G. R., Gibson, P. G., Marchant,
J. M., & Grimwood, K. (2016). Protracted bacterial bronchitis: the last decade
and the road ahead. Pediatric pulmonology, 51(3), 225-242.
https://doi.org/10.1002/ppul.23351
Gelb, A. F., Christenson, S. A., & Nadel, J. A. (2016). Understanding the
pathophysiology of the asthma–chronic obstructive pulmonary disease overlap
syndrome. Current opinion in pulmonary medicine, 22(2), 100-105.
10.1097/MCP.0000000000000236
Gonçalves‐Bradley, D. C., Lannin, N. A., Clemson, L. M., Cameron, I. D., &
Shepperd, S. (2016). Discharge planning from hospital. Cochrane database of
systematic reviews, (1). https://doi.org/10.1002/14651858.CD000313.pub5
Gould, D. J., Moralejo, D., Drey, N., Chudleigh, J. H., & Taljaard, M. (2017).
Interventions to improve hand hygiene compliance in patient care. Cochrane
database of systematic reviews, (9).
https://doi.org/10.1002/14651858.CD005186.pub4
Jackwood, M. W., & de Wit, S. (2020). Infectious bronchitis. Diseases of poultry, 167-
188. https://doi.org/10.1002/9781119371199.ch4
12
Double click here to fill in this footer
Last name__ _student number_NUR250 S1 2020 Assessment 1
Karthikeyan, R., & Sai Koushik, O. (2016). RajKumarPV. Biodistribution Study of
Pegylated Ppi Dendrimer Loaded with Prednisolone for Prolonged Release.
Nano Res Appl, 2, 2.
http://www.academia.edu/download/51452279/biodistribution-study-of-
ppi.pdf
Koumbourlis, A. C., & Mastropietro, C. (2015). Continuous Inhalation of Ipratropium
Bromide for Acute Asthma Refractory to β2-agonist Treatment. The Journal of
Pediatric Pharmacology and Therapeutics, 20(1), 66-69.
https://www.jppt.org/doi/abs/10.5863/1551-6776-20.1.66
Lai, K., Chen, R., Peng, W., & Zhan, W. (2017). Non-asthmatic eosinophilic
bronchitis and its relationship with asthma. Pulmonary pharmacology &
therapeutics, 47, 66-71. https://doi.org/10.1016/j.pupt.2017.07.002
Lee, J. M., & Hanna, S. D. (2015). Savings goals and saving behavior from a
perspective of Maslow's hierarchy of needs. Journal of Financial Counseling
and Planning, 26(2), 129-147.
10.1891/1052-3073.26.2.129
Morshed, N. (2015). Comparative evaluation of prednisolone 5MG tablets marketed
in Bangladesh. http://dspace.bracu.ac.bd/xmlui/handle/10361/4947
Mukherjee, S., Rutter, K., Watson, L., & Eisenhut, M. (2015). Adverse effects of
bronchodilators in infants with bronchiolitis. The Journal of Pediatric
Pharmacology and Therapeutics: JPPT, 20(1), 70.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4353204/pdf/i1551-6776-
20-1-70.pdf
Pothirat, C., Chaiwong, W., Phetsuk, N., Pisalthanapuna, S., Chetsadaphan, N., &
Choomuang, W. (2015). Evaluating inhaler use technique in COPD
patients. International journal of chronic obstructive pulmonary disease, 10,
1291. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4501446/pdf/copd-
10-1291.pdf
Raju, S. V., Kim, H., Byzek, S. A., Tang, L. P., Trombley, J. E., Jackson, P., ... &
Winter, L. (2016). A ferret model of COPD-related chronic bronchitis. JCI
insight, 1(15).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5033751/pdf/jciinsight-1-
87536.pdf
13
Double click here to fill in this footer
Last name__ _student number_NUR250 S1 2020 Assessment 1
Pegylated Ppi Dendrimer Loaded with Prednisolone for Prolonged Release.
Nano Res Appl, 2, 2.
http://www.academia.edu/download/51452279/biodistribution-study-of-
ppi.pdf
Koumbourlis, A. C., & Mastropietro, C. (2015). Continuous Inhalation of Ipratropium
Bromide for Acute Asthma Refractory to β2-agonist Treatment. The Journal of
Pediatric Pharmacology and Therapeutics, 20(1), 66-69.
https://www.jppt.org/doi/abs/10.5863/1551-6776-20.1.66
Lai, K., Chen, R., Peng, W., & Zhan, W. (2017). Non-asthmatic eosinophilic
bronchitis and its relationship with asthma. Pulmonary pharmacology &
therapeutics, 47, 66-71. https://doi.org/10.1016/j.pupt.2017.07.002
Lee, J. M., & Hanna, S. D. (2015). Savings goals and saving behavior from a
perspective of Maslow's hierarchy of needs. Journal of Financial Counseling
and Planning, 26(2), 129-147.
10.1891/1052-3073.26.2.129
Morshed, N. (2015). Comparative evaluation of prednisolone 5MG tablets marketed
in Bangladesh. http://dspace.bracu.ac.bd/xmlui/handle/10361/4947
Mukherjee, S., Rutter, K., Watson, L., & Eisenhut, M. (2015). Adverse effects of
bronchodilators in infants with bronchiolitis. The Journal of Pediatric
Pharmacology and Therapeutics: JPPT, 20(1), 70.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4353204/pdf/i1551-6776-
20-1-70.pdf
Pothirat, C., Chaiwong, W., Phetsuk, N., Pisalthanapuna, S., Chetsadaphan, N., &
Choomuang, W. (2015). Evaluating inhaler use technique in COPD
patients. International journal of chronic obstructive pulmonary disease, 10,
1291. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4501446/pdf/copd-
10-1291.pdf
Raju, S. V., Kim, H., Byzek, S. A., Tang, L. P., Trombley, J. E., Jackson, P., ... &
Winter, L. (2016). A ferret model of COPD-related chronic bronchitis. JCI
insight, 1(15).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5033751/pdf/jciinsight-1-
87536.pdf
13
Double click here to fill in this footer
Last name__ _student number_NUR250 S1 2020 Assessment 1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Singh, A., Avula, A., & Zahn, E. (2019). Acute Bronchitis.
https://europepmc.org/article/NBK/NBK448067
Tilg, H., & Moschen, A. R. (2015). Food, immunity, and the
microbiome. Gastroenterology, 148(6), 1107-1119.
https://doi.org/10.1053/j.gastro.2014.12.036
Troy, L. K., Young, I. H., Lau, E. M., & Corte, T. J. (2016). Exercise pathophysiology
and the role of oxygen therapy in idiopathic interstitial
pneumonia. Respirology, 21(6), 1005-1014.
https://doi.org/10.1111/resp.12650
14
Double click here to fill in this footer
Last name__ _student number_NUR250 S1 2020 Assessment 1
https://europepmc.org/article/NBK/NBK448067
Tilg, H., & Moschen, A. R. (2015). Food, immunity, and the
microbiome. Gastroenterology, 148(6), 1107-1119.
https://doi.org/10.1053/j.gastro.2014.12.036
Troy, L. K., Young, I. H., Lau, E. M., & Corte, T. J. (2016). Exercise pathophysiology
and the role of oxygen therapy in idiopathic interstitial
pneumonia. Respirology, 21(6), 1005-1014.
https://doi.org/10.1111/resp.12650
14
Double click here to fill in this footer
Last name__ _student number_NUR250 S1 2020 Assessment 1
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





