NUR250 Assessment 1 S2 2018 Assignment Template
VerifiedAdded on 2023/06/07
|14
|3949
|478
AI Summary
This article provides a template for NUR250 Assessment 1 S2 2018 that includes patient assessment, care planning, and activity intolerance. It also includes nursing interventions, rationale, and indicators for each nursing problem. The article is relevant for nursing students and professionals.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

NUR250 Assessment 1 S2 2018
Assignment template
Do not delete the heading and the information below.
Please note: As indicated in Assessment 1 information, a cover sheet, title, and
contents pages are not required
Before you begin take a minute to fill in your details in the footer to ensure your document is
identifiable. To access the footer, double click on the grey writing “Last name….” at the bottom of
the page above. Once you have done that, double click here to come back to this page.
Information about the required line spacing and font size and type is in the Assessment 1
information document in the Assessment 1 folder on NUR250 Learnline. Take a minute to check that
this document meets those requirements.
To avoid or minimise problems with formatting, it is recommended you
Use the headings provided
Don’t copy from another document onto this template
Don’t delete the section breaks on the document
Submission of your assignment means you have read and understood the
University policies and procedures related to academic integrity
Assessment 1 presentation guidelines
Start to write your assignment here. Word count is calculated from this point.
Task 1: Patient assessment
The appropriate nursing assessment in this patient will include a complete cardiovascular
assessment, pain assessment and assessment of risk factors (Brunner, 2010). These are the priority
assessments in this patient presenting with features of heart failure in a previous myocardial
infarction. They are at increased risk of recurrence of cardiovascular disease hence risk factors that
precipitate heart failure or worsen morbidity need to be assessed (Elliott & Coventry, 2012). Pain
is a vital component of cardiovascular ischemia and in-hospital stay hence assessment of pain is
warranted.
The cardiovascular examination involves physical, functional and psychosocial assessment by
collecting objective and subjective data. Physical assessment starts by measuring the blood pressure,
heart rate, assessment of edema, peripheral circulation, followed by inspection, palpation, and
1
Double click here to fill in this footer
Last name__ _student number_NUR250 S2 2018 Assessment 1
Assignment template
Do not delete the heading and the information below.
Please note: As indicated in Assessment 1 information, a cover sheet, title, and
contents pages are not required
Before you begin take a minute to fill in your details in the footer to ensure your document is
identifiable. To access the footer, double click on the grey writing “Last name….” at the bottom of
the page above. Once you have done that, double click here to come back to this page.
Information about the required line spacing and font size and type is in the Assessment 1
information document in the Assessment 1 folder on NUR250 Learnline. Take a minute to check that
this document meets those requirements.
To avoid or minimise problems with formatting, it is recommended you
Use the headings provided
Don’t copy from another document onto this template
Don’t delete the section breaks on the document
Submission of your assignment means you have read and understood the
University policies and procedures related to academic integrity
Assessment 1 presentation guidelines
Start to write your assignment here. Word count is calculated from this point.
Task 1: Patient assessment
The appropriate nursing assessment in this patient will include a complete cardiovascular
assessment, pain assessment and assessment of risk factors (Brunner, 2010). These are the priority
assessments in this patient presenting with features of heart failure in a previous myocardial
infarction. They are at increased risk of recurrence of cardiovascular disease hence risk factors that
precipitate heart failure or worsen morbidity need to be assessed (Elliott & Coventry, 2012). Pain
is a vital component of cardiovascular ischemia and in-hospital stay hence assessment of pain is
warranted.
The cardiovascular examination involves physical, functional and psychosocial assessment by
collecting objective and subjective data. Physical assessment starts by measuring the blood pressure,
heart rate, assessment of edema, peripheral circulation, followed by inspection, palpation, and
1
Double click here to fill in this footer
Last name__ _student number_NUR250 S2 2018 Assessment 1
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
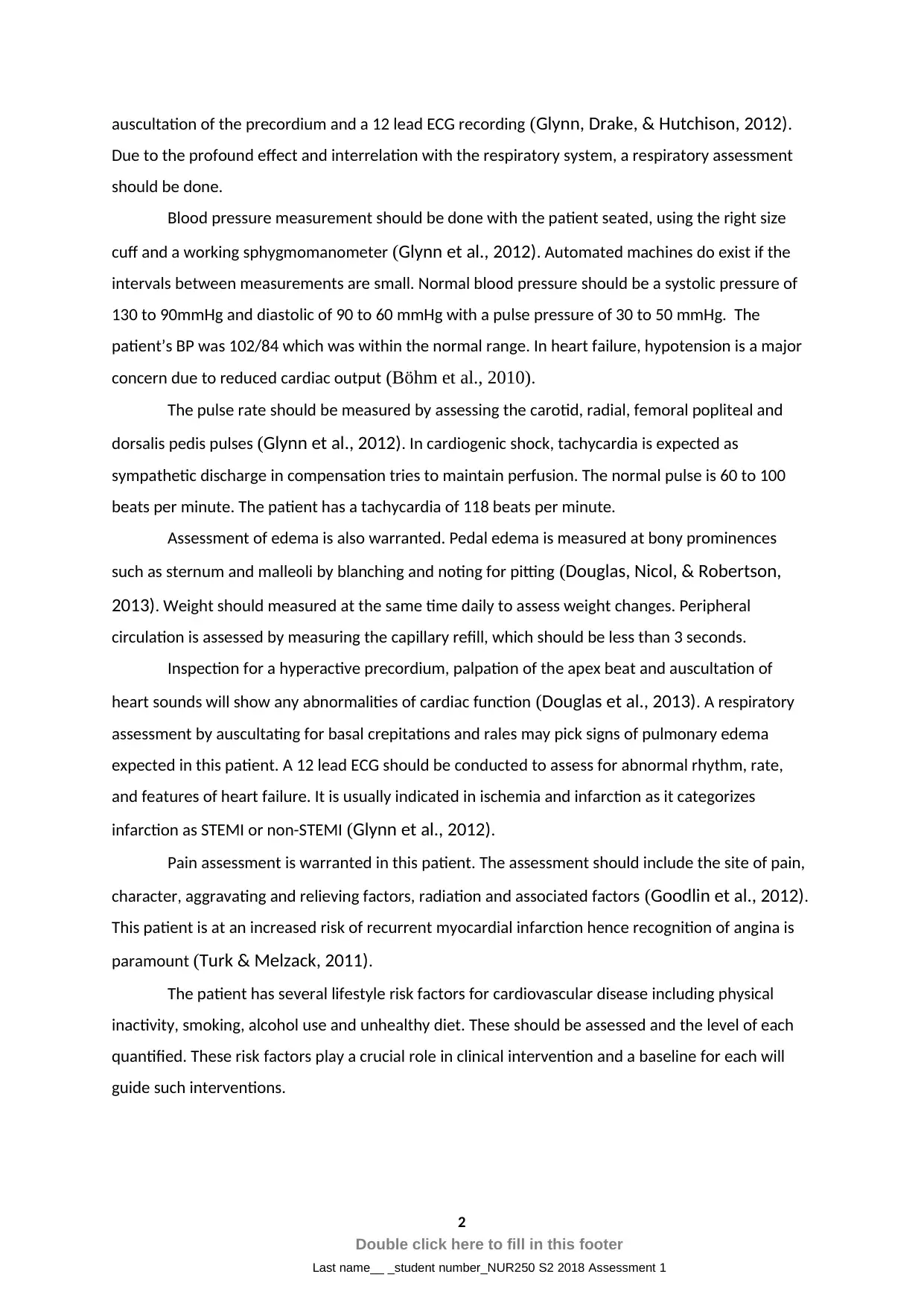
auscultation of the precordium and a 12 lead ECG recording (Glynn, Drake, & Hutchison, 2012).
Due to the profound effect and interrelation with the respiratory system, a respiratory assessment
should be done.
Blood pressure measurement should be done with the patient seated, using the right size
cuff and a working sphygmomanometer (Glynn et al., 2012). Automated machines do exist if the
intervals between measurements are small. Normal blood pressure should be a systolic pressure of
130 to 90mmHg and diastolic of 90 to 60 mmHg with a pulse pressure of 30 to 50 mmHg. The
patient’s BP was 102/84 which was within the normal range. In heart failure, hypotension is a major
concern due to reduced cardiac output (Böhm et al., 2010).
The pulse rate should be measured by assessing the carotid, radial, femoral popliteal and
dorsalis pedis pulses (Glynn et al., 2012). In cardiogenic shock, tachycardia is expected as
sympathetic discharge in compensation tries to maintain perfusion. The normal pulse is 60 to 100
beats per minute. The patient has a tachycardia of 118 beats per minute.
Assessment of edema is also warranted. Pedal edema is measured at bony prominences
such as sternum and malleoli by blanching and noting for pitting (Douglas, Nicol, & Robertson,
2013). Weight should measured at the same time daily to assess weight changes. Peripheral
circulation is assessed by measuring the capillary refill, which should be less than 3 seconds.
Inspection for a hyperactive precordium, palpation of the apex beat and auscultation of
heart sounds will show any abnormalities of cardiac function (Douglas et al., 2013). A respiratory
assessment by auscultating for basal crepitations and rales may pick signs of pulmonary edema
expected in this patient. A 12 lead ECG should be conducted to assess for abnormal rhythm, rate,
and features of heart failure. It is usually indicated in ischemia and infarction as it categorizes
infarction as STEMI or non-STEMI (Glynn et al., 2012).
Pain assessment is warranted in this patient. The assessment should include the site of pain,
character, aggravating and relieving factors, radiation and associated factors (Goodlin et al., 2012).
This patient is at an increased risk of recurrent myocardial infarction hence recognition of angina is
paramount (Turk & Melzack, 2011).
The patient has several lifestyle risk factors for cardiovascular disease including physical
inactivity, smoking, alcohol use and unhealthy diet. These should be assessed and the level of each
quantified. These risk factors play a crucial role in clinical intervention and a baseline for each will
guide such interventions.
2
Double click here to fill in this footer
Last name__ _student number_NUR250 S2 2018 Assessment 1
Due to the profound effect and interrelation with the respiratory system, a respiratory assessment
should be done.
Blood pressure measurement should be done with the patient seated, using the right size
cuff and a working sphygmomanometer (Glynn et al., 2012). Automated machines do exist if the
intervals between measurements are small. Normal blood pressure should be a systolic pressure of
130 to 90mmHg and diastolic of 90 to 60 mmHg with a pulse pressure of 30 to 50 mmHg. The
patient’s BP was 102/84 which was within the normal range. In heart failure, hypotension is a major
concern due to reduced cardiac output (Böhm et al., 2010).
The pulse rate should be measured by assessing the carotid, radial, femoral popliteal and
dorsalis pedis pulses (Glynn et al., 2012). In cardiogenic shock, tachycardia is expected as
sympathetic discharge in compensation tries to maintain perfusion. The normal pulse is 60 to 100
beats per minute. The patient has a tachycardia of 118 beats per minute.
Assessment of edema is also warranted. Pedal edema is measured at bony prominences
such as sternum and malleoli by blanching and noting for pitting (Douglas, Nicol, & Robertson,
2013). Weight should measured at the same time daily to assess weight changes. Peripheral
circulation is assessed by measuring the capillary refill, which should be less than 3 seconds.
Inspection for a hyperactive precordium, palpation of the apex beat and auscultation of
heart sounds will show any abnormalities of cardiac function (Douglas et al., 2013). A respiratory
assessment by auscultating for basal crepitations and rales may pick signs of pulmonary edema
expected in this patient. A 12 lead ECG should be conducted to assess for abnormal rhythm, rate,
and features of heart failure. It is usually indicated in ischemia and infarction as it categorizes
infarction as STEMI or non-STEMI (Glynn et al., 2012).
Pain assessment is warranted in this patient. The assessment should include the site of pain,
character, aggravating and relieving factors, radiation and associated factors (Goodlin et al., 2012).
This patient is at an increased risk of recurrent myocardial infarction hence recognition of angina is
paramount (Turk & Melzack, 2011).
The patient has several lifestyle risk factors for cardiovascular disease including physical
inactivity, smoking, alcohol use and unhealthy diet. These should be assessed and the level of each
quantified. These risk factors play a crucial role in clinical intervention and a baseline for each will
guide such interventions.
2
Double click here to fill in this footer
Last name__ _student number_NUR250 S2 2018 Assessment 1

3
Double click here to fill in this footer
Last name__ _student number_NUR250 S2 2018 Assessment 1
Double click here to fill in this footer
Last name__ _student number_NUR250 S2 2018 Assessment 1
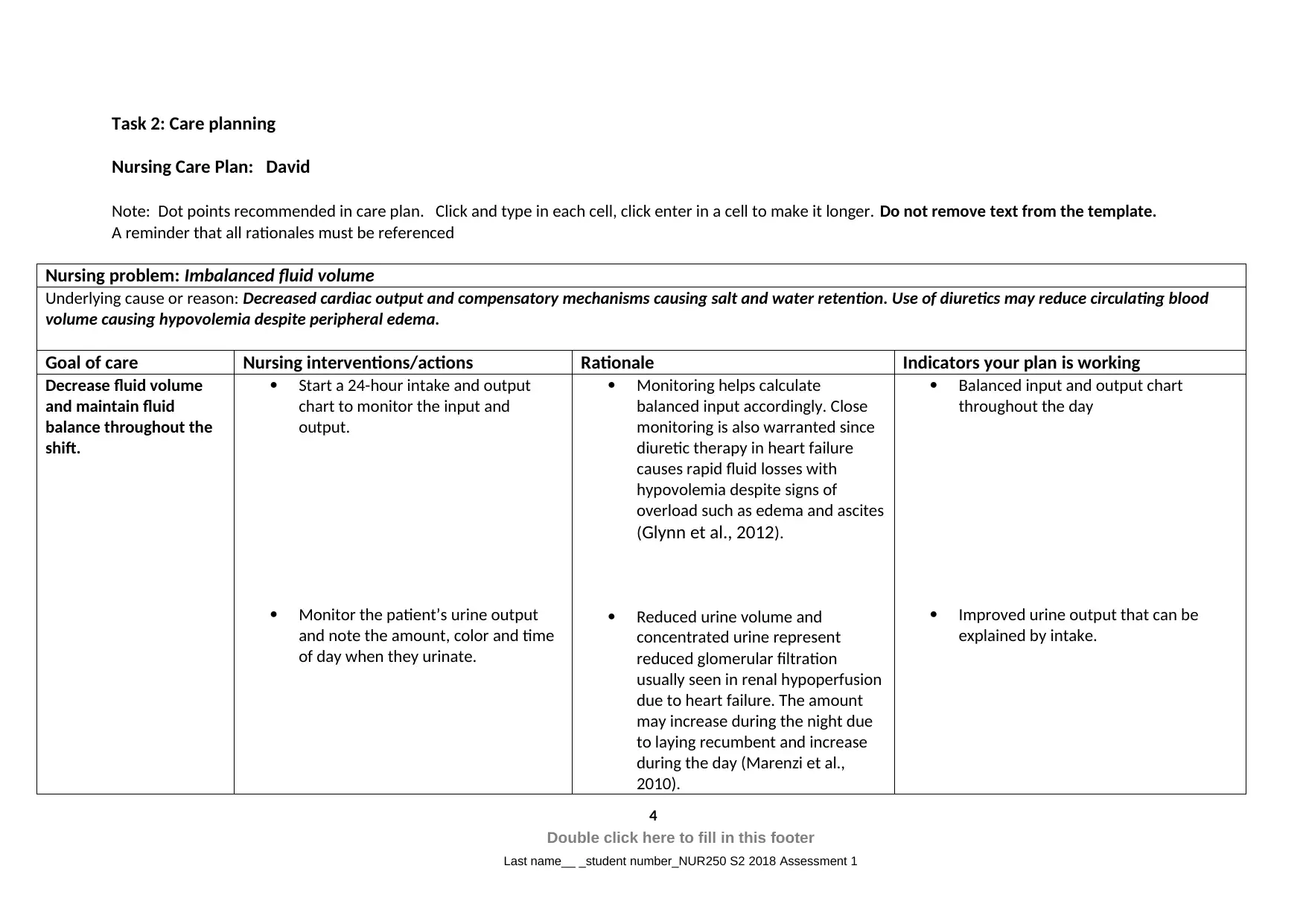
Task 2: Care planning
Nursing Care Plan: David
Note: Dot points recommended in care plan. Click and type in each cell, click enter in a cell to make it longer. Do not remove text from the template.
A reminder that all rationales must be referenced
Nursing problem: Imbalanced fluid volume
Underlying cause or reason: Decreased cardiac output and compensatory mechanisms causing salt and water retention. Use of diuretics may reduce circulating blood
volume causing hypovolemia despite peripheral edema.
Goal of care Nursing interventions/actions Rationale Indicators your plan is working
Decrease fluid volume
and maintain fluid
balance throughout the
shift.
Start a 24-hour intake and output
chart to monitor the input and
output.
Monitor the patient’s urine output
and note the amount, color and time
of day when they urinate.
Monitoring helps calculate
balanced input accordingly. Close
monitoring is also warranted since
diuretic therapy in heart failure
causes rapid fluid losses with
hypovolemia despite signs of
overload such as edema and ascites
(Glynn et al., 2012).
Reduced urine volume and
concentrated urine represent
reduced glomerular filtration
usually seen in renal hypoperfusion
due to heart failure. The amount
may increase during the night due
to laying recumbent and increase
during the day (Marenzi et al.,
2010).
Balanced input and output chart
throughout the day
Improved urine output that can be
explained by intake.
4
Double click here to fill in this footer
Last name__ _student number_NUR250 S2 2018 Assessment 1
Nursing Care Plan: David
Note: Dot points recommended in care plan. Click and type in each cell, click enter in a cell to make it longer. Do not remove text from the template.
A reminder that all rationales must be referenced
Nursing problem: Imbalanced fluid volume
Underlying cause or reason: Decreased cardiac output and compensatory mechanisms causing salt and water retention. Use of diuretics may reduce circulating blood
volume causing hypovolemia despite peripheral edema.
Goal of care Nursing interventions/actions Rationale Indicators your plan is working
Decrease fluid volume
and maintain fluid
balance throughout the
shift.
Start a 24-hour intake and output
chart to monitor the input and
output.
Monitor the patient’s urine output
and note the amount, color and time
of day when they urinate.
Monitoring helps calculate
balanced input accordingly. Close
monitoring is also warranted since
diuretic therapy in heart failure
causes rapid fluid losses with
hypovolemia despite signs of
overload such as edema and ascites
(Glynn et al., 2012).
Reduced urine volume and
concentrated urine represent
reduced glomerular filtration
usually seen in renal hypoperfusion
due to heart failure. The amount
may increase during the night due
to laying recumbent and increase
during the day (Marenzi et al.,
2010).
Balanced input and output chart
throughout the day
Improved urine output that can be
explained by intake.
4
Double click here to fill in this footer
Last name__ _student number_NUR250 S2 2018 Assessment 1
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Maintain the patient in a semi-
Fowler's position during bed rest or
maintain chair rest.
Weight the patient at the same time
daily.
Assess for signs of fluid overload
including distended neck veins,
ascites, pedal edema with or without
pitting and anasarca.
Assess the patients breathing by
auscultating the breath sounds noting
any added sounds such as wheeze,
crackles, rales or decreased air entry.
Note for dyspnoea, orthopnoea,
cough and paroxysmal nocturnal
dyspnoea.
Laying recumbent usually increases
the glomerular filtration rate and is
thought to decrease ADH
production. This enhances urine
production and reduces fluid
overload (Marenzi et al., 2010).
This helps in monitoring changes in
edema. Diuretics can also cause
sudden shifts in fluid status (Glynn
et al., 2012).
Heart failure causes salt and water
causing fluid overload that will
manifest venous engorgement and
the formation of edema. With
increased congestion associated
right heart failure causes systemic
edema that manifests as anasarca
(Glynn et al., 2012).
These represent signs of pulmonary
edema and congestion and
represent left heart failure. They
may be slow in onset in right heart
failure (Glynn et al., 2012).
Hypotension represents
cardiogenic shock with a reduction
Improved urine output throughout the
day.
Constant weight without sudden shifts
in the figures.
Resolution of edema, distended veins,
and ascites.
Normal breathing without adventitious
sounds.
5
Double click here to fill in this footer
Last name__ _student number_NUR250 S2 2018 Assessment 1
Fowler's position during bed rest or
maintain chair rest.
Weight the patient at the same time
daily.
Assess for signs of fluid overload
including distended neck veins,
ascites, pedal edema with or without
pitting and anasarca.
Assess the patients breathing by
auscultating the breath sounds noting
any added sounds such as wheeze,
crackles, rales or decreased air entry.
Note for dyspnoea, orthopnoea,
cough and paroxysmal nocturnal
dyspnoea.
Laying recumbent usually increases
the glomerular filtration rate and is
thought to decrease ADH
production. This enhances urine
production and reduces fluid
overload (Marenzi et al., 2010).
This helps in monitoring changes in
edema. Diuretics can also cause
sudden shifts in fluid status (Glynn
et al., 2012).
Heart failure causes salt and water
causing fluid overload that will
manifest venous engorgement and
the formation of edema. With
increased congestion associated
right heart failure causes systemic
edema that manifests as anasarca
(Glynn et al., 2012).
These represent signs of pulmonary
edema and congestion and
represent left heart failure. They
may be slow in onset in right heart
failure (Glynn et al., 2012).
Hypotension represents
cardiogenic shock with a reduction
Improved urine output throughout the
day.
Constant weight without sudden shifts
in the figures.
Resolution of edema, distended veins,
and ascites.
Normal breathing without adventitious
sounds.
5
Double click here to fill in this footer
Last name__ _student number_NUR250 S2 2018 Assessment 1
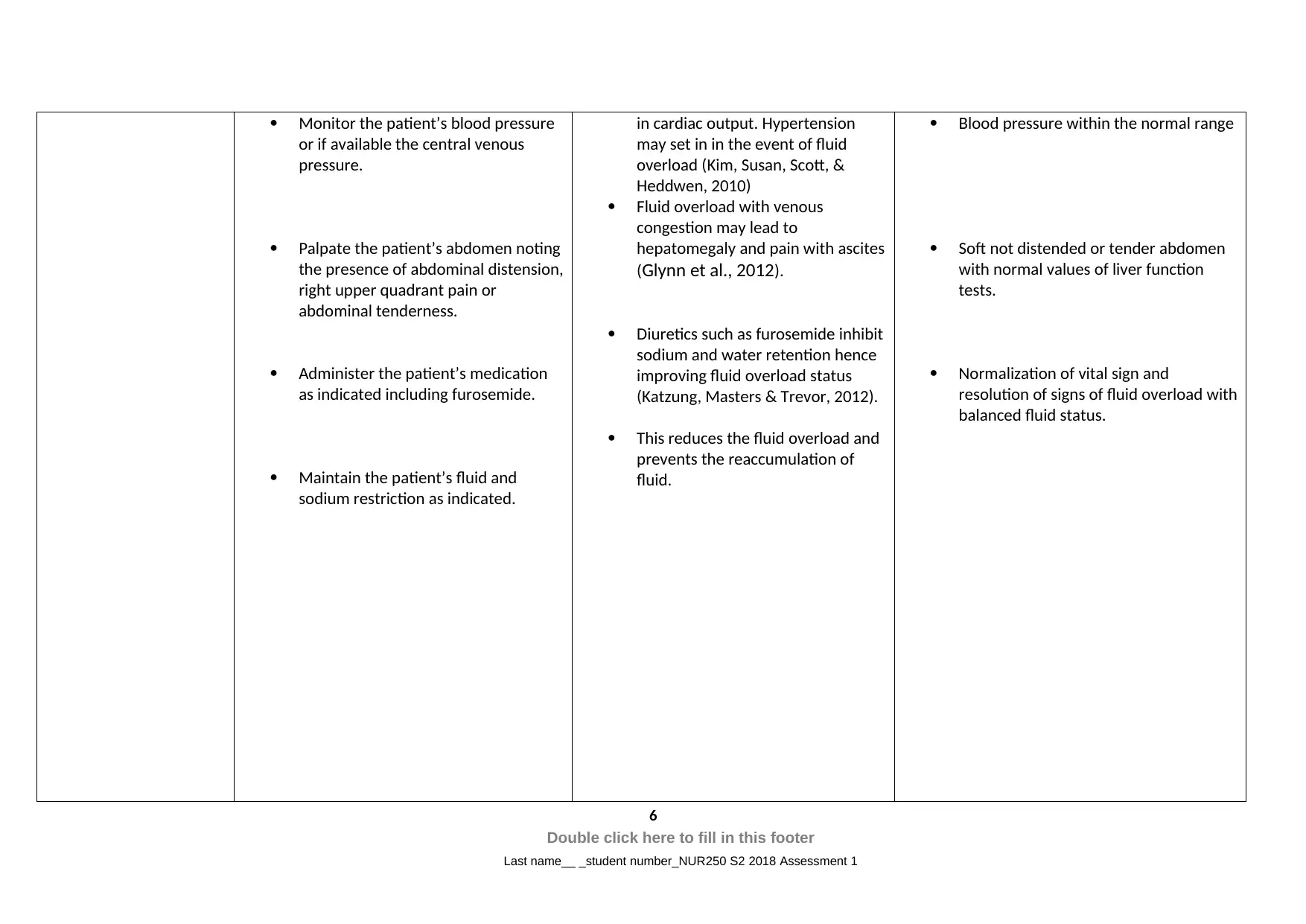
Monitor the patient’s blood pressure
or if available the central venous
pressure.
Palpate the patient’s abdomen noting
the presence of abdominal distension,
right upper quadrant pain or
abdominal tenderness.
Administer the patient’s medication
as indicated including furosemide.
Maintain the patient’s fluid and
sodium restriction as indicated.
in cardiac output. Hypertension
may set in in the event of fluid
overload (Kim, Susan, Scott, &
Heddwen, 2010)
Fluid overload with venous
congestion may lead to
hepatomegaly and pain with ascites
(Glynn et al., 2012).
Diuretics such as furosemide inhibit
sodium and water retention hence
improving fluid overload status
(Katzung, Masters & Trevor, 2012).
This reduces the fluid overload and
prevents the reaccumulation of
fluid.
Blood pressure within the normal range
Soft not distended or tender abdomen
with normal values of liver function
tests.
Normalization of vital sign and
resolution of signs of fluid overload with
balanced fluid status.
6
Double click here to fill in this footer
Last name__ _student number_NUR250 S2 2018 Assessment 1
or if available the central venous
pressure.
Palpate the patient’s abdomen noting
the presence of abdominal distension,
right upper quadrant pain or
abdominal tenderness.
Administer the patient’s medication
as indicated including furosemide.
Maintain the patient’s fluid and
sodium restriction as indicated.
in cardiac output. Hypertension
may set in in the event of fluid
overload (Kim, Susan, Scott, &
Heddwen, 2010)
Fluid overload with venous
congestion may lead to
hepatomegaly and pain with ascites
(Glynn et al., 2012).
Diuretics such as furosemide inhibit
sodium and water retention hence
improving fluid overload status
(Katzung, Masters & Trevor, 2012).
This reduces the fluid overload and
prevents the reaccumulation of
fluid.
Blood pressure within the normal range
Soft not distended or tender abdomen
with normal values of liver function
tests.
Normalization of vital sign and
resolution of signs of fluid overload with
balanced fluid status.
6
Double click here to fill in this footer
Last name__ _student number_NUR250 S2 2018 Assessment 1
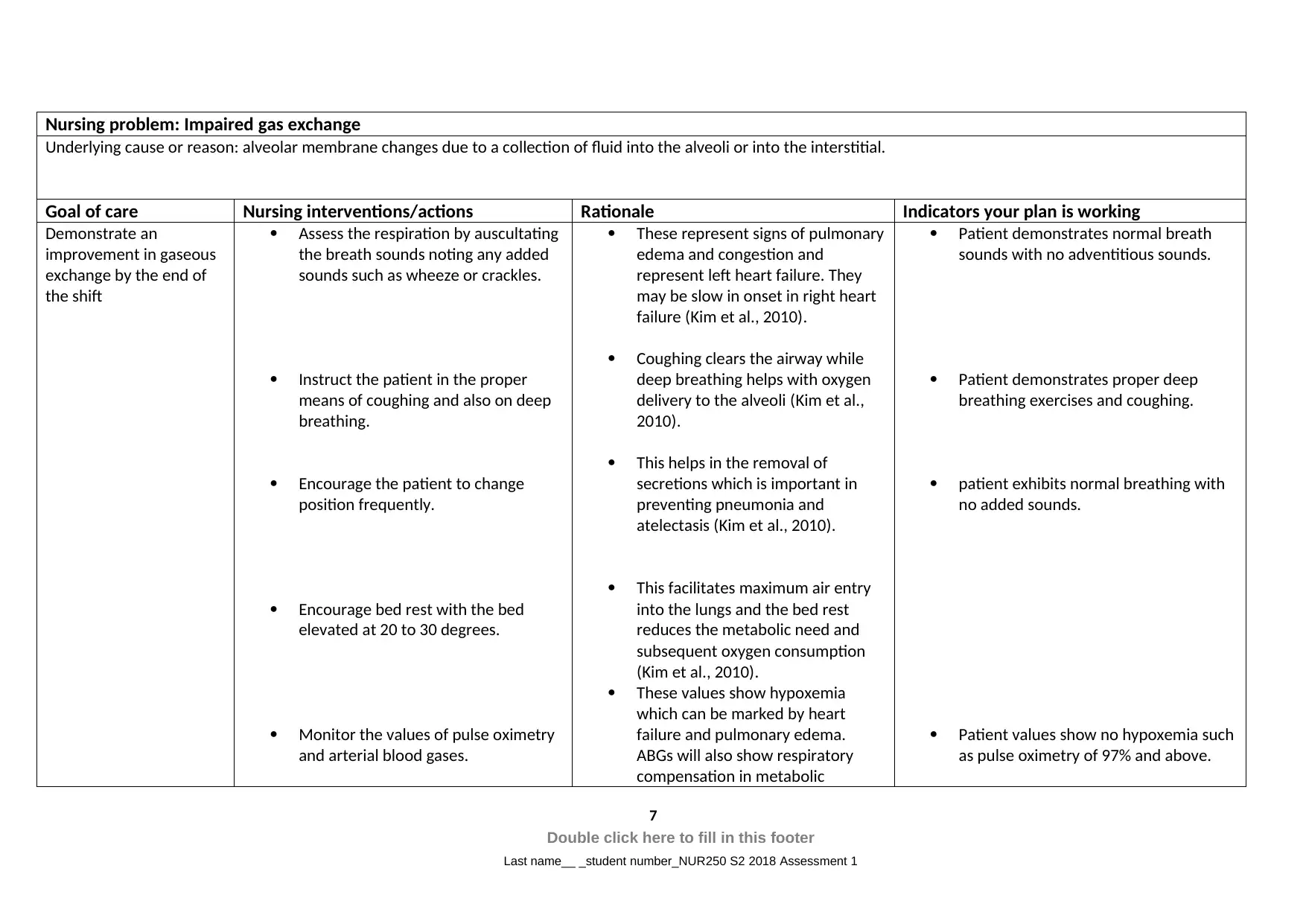
Nursing problem: Impaired gas exchange
Underlying cause or reason: alveolar membrane changes due to a collection of fluid into the alveoli or into the interstitial.
Goal of care Nursing interventions/actions Rationale Indicators your plan is working
Demonstrate an
improvement in gaseous
exchange by the end of
the shift
Assess the respiration by auscultating
the breath sounds noting any added
sounds such as wheeze or crackles.
Instruct the patient in the proper
means of coughing and also on deep
breathing.
Encourage the patient to change
position frequently.
Encourage bed rest with the bed
elevated at 20 to 30 degrees.
Monitor the values of pulse oximetry
and arterial blood gases.
These represent signs of pulmonary
edema and congestion and
represent left heart failure. They
may be slow in onset in right heart
failure (Kim et al., 2010).
Coughing clears the airway while
deep breathing helps with oxygen
delivery to the alveoli (Kim et al.,
2010).
This helps in the removal of
secretions which is important in
preventing pneumonia and
atelectasis (Kim et al., 2010).
This facilitates maximum air entry
into the lungs and the bed rest
reduces the metabolic need and
subsequent oxygen consumption
(Kim et al., 2010).
These values show hypoxemia
which can be marked by heart
failure and pulmonary edema.
ABGs will also show respiratory
compensation in metabolic
Patient demonstrates normal breath
sounds with no adventitious sounds.
Patient demonstrates proper deep
breathing exercises and coughing.
patient exhibits normal breathing with
no added sounds.
Patient values show no hypoxemia such
as pulse oximetry of 97% and above.
7
Double click here to fill in this footer
Last name__ _student number_NUR250 S2 2018 Assessment 1
Underlying cause or reason: alveolar membrane changes due to a collection of fluid into the alveoli or into the interstitial.
Goal of care Nursing interventions/actions Rationale Indicators your plan is working
Demonstrate an
improvement in gaseous
exchange by the end of
the shift
Assess the respiration by auscultating
the breath sounds noting any added
sounds such as wheeze or crackles.
Instruct the patient in the proper
means of coughing and also on deep
breathing.
Encourage the patient to change
position frequently.
Encourage bed rest with the bed
elevated at 20 to 30 degrees.
Monitor the values of pulse oximetry
and arterial blood gases.
These represent signs of pulmonary
edema and congestion and
represent left heart failure. They
may be slow in onset in right heart
failure (Kim et al., 2010).
Coughing clears the airway while
deep breathing helps with oxygen
delivery to the alveoli (Kim et al.,
2010).
This helps in the removal of
secretions which is important in
preventing pneumonia and
atelectasis (Kim et al., 2010).
This facilitates maximum air entry
into the lungs and the bed rest
reduces the metabolic need and
subsequent oxygen consumption
(Kim et al., 2010).
These values show hypoxemia
which can be marked by heart
failure and pulmonary edema.
ABGs will also show respiratory
compensation in metabolic
Patient demonstrates normal breath
sounds with no adventitious sounds.
Patient demonstrates proper deep
breathing exercises and coughing.
patient exhibits normal breathing with
no added sounds.
Patient values show no hypoxemia such
as pulse oximetry of 97% and above.
7
Double click here to fill in this footer
Last name__ _student number_NUR250 S2 2018 Assessment 1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
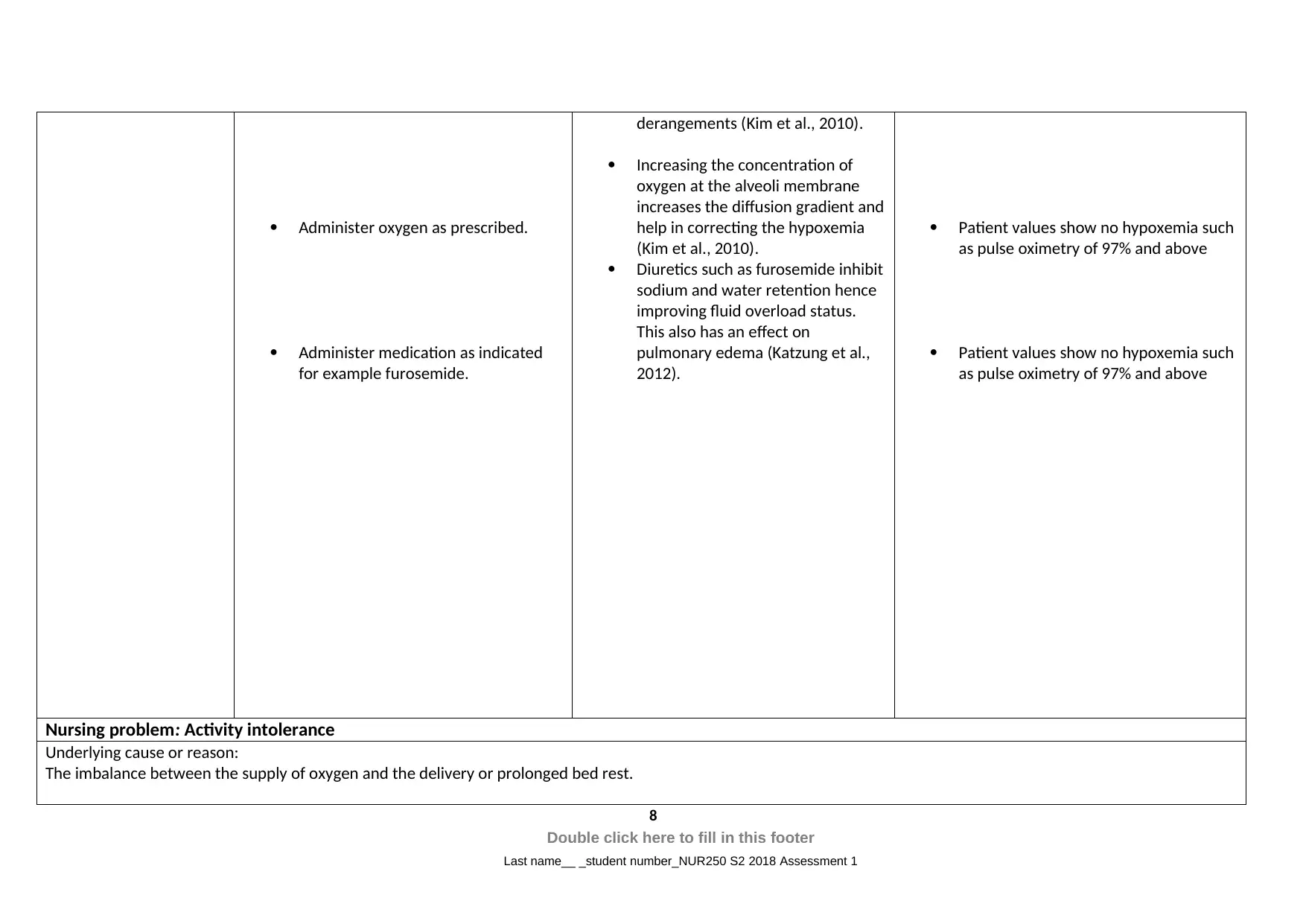
Administer oxygen as prescribed.
Administer medication as indicated
for example furosemide.
derangements (Kim et al., 2010).
Increasing the concentration of
oxygen at the alveoli membrane
increases the diffusion gradient and
help in correcting the hypoxemia
(Kim et al., 2010).
Diuretics such as furosemide inhibit
sodium and water retention hence
improving fluid overload status.
This also has an effect on
pulmonary edema (Katzung et al.,
2012).
Patient values show no hypoxemia such
as pulse oximetry of 97% and above
Patient values show no hypoxemia such
as pulse oximetry of 97% and above
Nursing problem: Activity intolerance
Underlying cause or reason:
The imbalance between the supply of oxygen and the delivery or prolonged bed rest.
8
Double click here to fill in this footer
Last name__ _student number_NUR250 S2 2018 Assessment 1
Administer medication as indicated
for example furosemide.
derangements (Kim et al., 2010).
Increasing the concentration of
oxygen at the alveoli membrane
increases the diffusion gradient and
help in correcting the hypoxemia
(Kim et al., 2010).
Diuretics such as furosemide inhibit
sodium and water retention hence
improving fluid overload status.
This also has an effect on
pulmonary edema (Katzung et al.,
2012).
Patient values show no hypoxemia such
as pulse oximetry of 97% and above
Patient values show no hypoxemia such
as pulse oximetry of 97% and above
Nursing problem: Activity intolerance
Underlying cause or reason:
The imbalance between the supply of oxygen and the delivery or prolonged bed rest.
8
Double click here to fill in this footer
Last name__ _student number_NUR250 S2 2018 Assessment 1
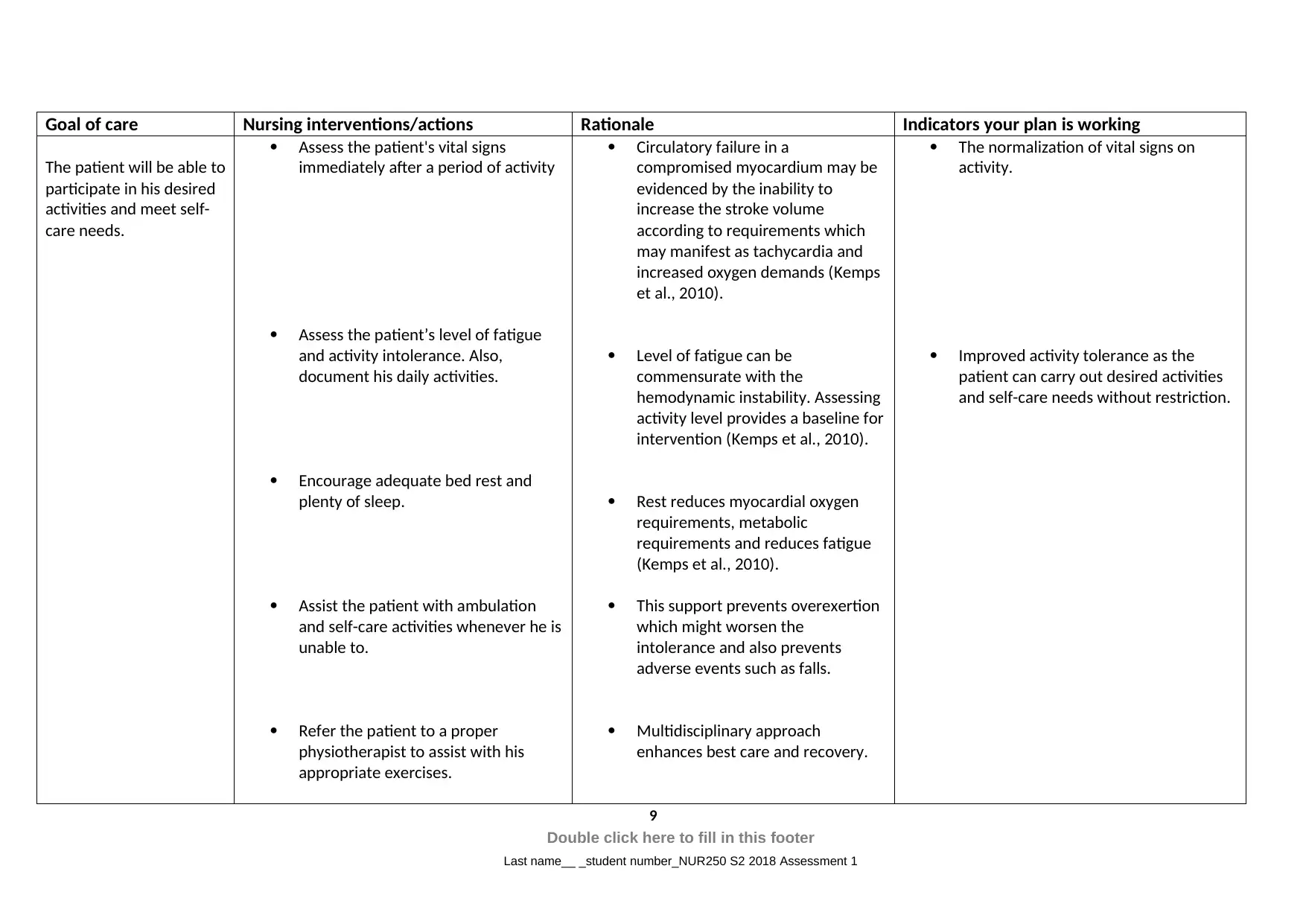
Goal of care Nursing interventions/actions Rationale Indicators your plan is working
The patient will be able to
participate in his desired
activities and meet self-
care needs.
Assess the patient's vital signs
immediately after a period of activity
Assess the patient’s level of fatigue
and activity intolerance. Also,
document his daily activities.
Encourage adequate bed rest and
plenty of sleep.
Assist the patient with ambulation
and self-care activities whenever he is
unable to.
Refer the patient to a proper
physiotherapist to assist with his
appropriate exercises.
Circulatory failure in a
compromised myocardium may be
evidenced by the inability to
increase the stroke volume
according to requirements which
may manifest as tachycardia and
increased oxygen demands (Kemps
et al., 2010).
Level of fatigue can be
commensurate with the
hemodynamic instability. Assessing
activity level provides a baseline for
intervention (Kemps et al., 2010).
Rest reduces myocardial oxygen
requirements, metabolic
requirements and reduces fatigue
(Kemps et al., 2010).
This support prevents overexertion
which might worsen the
intolerance and also prevents
adverse events such as falls.
Multidisciplinary approach
enhances best care and recovery.
The normalization of vital signs on
activity.
Improved activity tolerance as the
patient can carry out desired activities
and self-care needs without restriction.
9
Double click here to fill in this footer
Last name__ _student number_NUR250 S2 2018 Assessment 1
The patient will be able to
participate in his desired
activities and meet self-
care needs.
Assess the patient's vital signs
immediately after a period of activity
Assess the patient’s level of fatigue
and activity intolerance. Also,
document his daily activities.
Encourage adequate bed rest and
plenty of sleep.
Assist the patient with ambulation
and self-care activities whenever he is
unable to.
Refer the patient to a proper
physiotherapist to assist with his
appropriate exercises.
Circulatory failure in a
compromised myocardium may be
evidenced by the inability to
increase the stroke volume
according to requirements which
may manifest as tachycardia and
increased oxygen demands (Kemps
et al., 2010).
Level of fatigue can be
commensurate with the
hemodynamic instability. Assessing
activity level provides a baseline for
intervention (Kemps et al., 2010).
Rest reduces myocardial oxygen
requirements, metabolic
requirements and reduces fatigue
(Kemps et al., 2010).
This support prevents overexertion
which might worsen the
intolerance and also prevents
adverse events such as falls.
Multidisciplinary approach
enhances best care and recovery.
The normalization of vital signs on
activity.
Improved activity tolerance as the
patient can carry out desired activities
and self-care needs without restriction.
9
Double click here to fill in this footer
Last name__ _student number_NUR250 S2 2018 Assessment 1
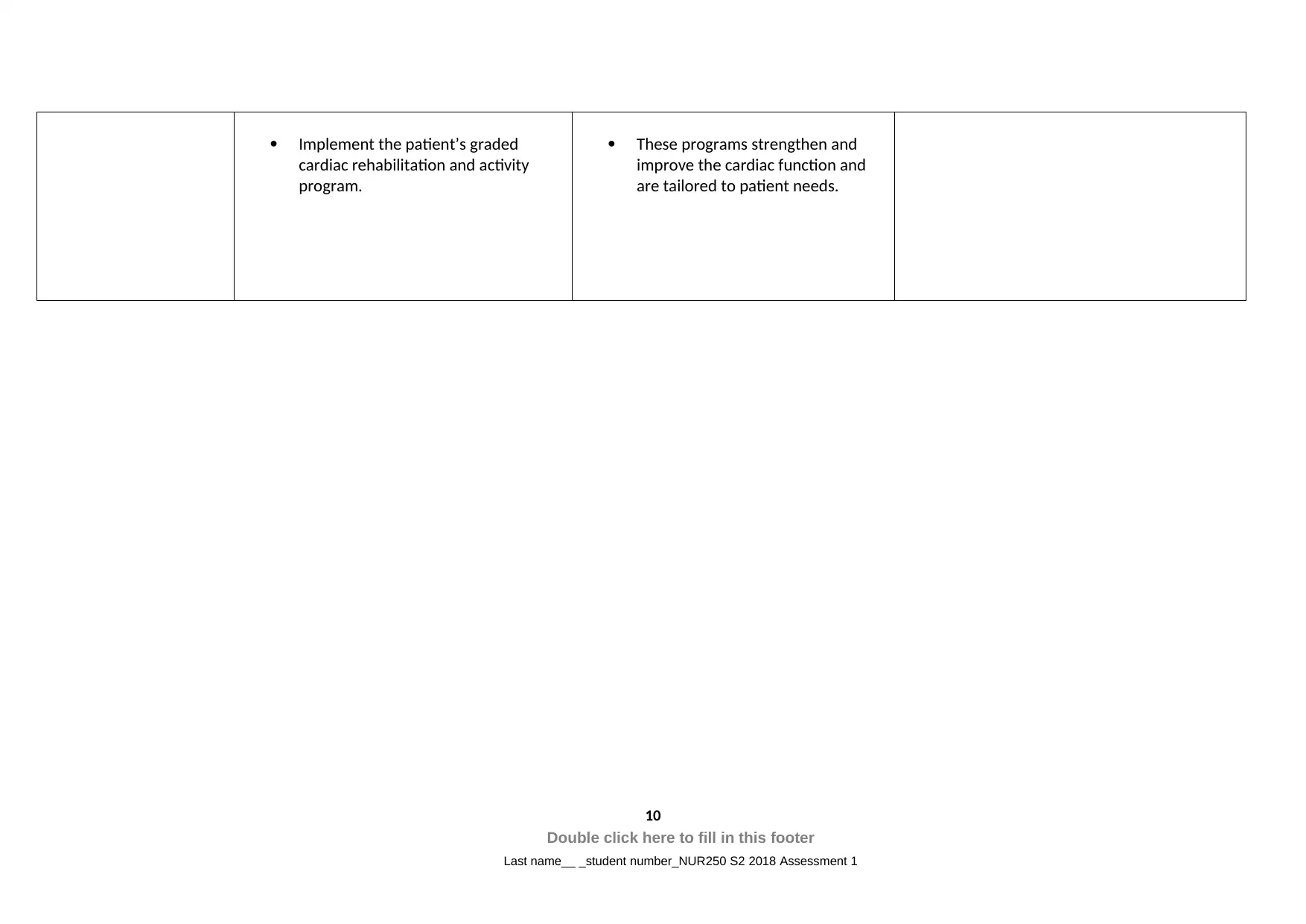
Implement the patient’s graded
cardiac rehabilitation and activity
program.
These programs strengthen and
improve the cardiac function and
are tailored to patient needs.
10
Double click here to fill in this footer
Last name__ _student number_NUR250 S2 2018 Assessment 1
cardiac rehabilitation and activity
program.
These programs strengthen and
improve the cardiac function and
are tailored to patient needs.
10
Double click here to fill in this footer
Last name__ _student number_NUR250 S2 2018 Assessment 1
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

Task 3: Medication management
The patient is on anti-failure medication with ramipril, digoxin, and furosemide. These are
among the drugs recommended for management of heart failure.
Furosemide 40mg PO twice daily
Furosemide is a loop-diuretic that functions to reduce fluid overload in heat failure. It
functions as a diuretic at the kidney to enhance salt and water excretion thus reducing fluid
accumulation (Katzung et al., 2012). Nursing responsibility during medication with furosemide
should include assessment of fluid balance and appropriate dosing. Drug allergy should be asked for
and any contraindications such as kidney disease and liver disease noted. Side effects include
nausea, vomiting, dizziness, and bleeding.
Digoxin 62.5mcg PO daily
Cardiac glycosides have been used in heart failure for years, with digoxin being one of them.
It is a positive inotrope that improves cardiac contractility thus improving cardiac output and
perfusion in heart failure (Katzung et al., 2012). Digitalis toxicity is a recognized adverse effect when
using this drug and can be fatal. Monitoring of dosage and adverse effects is an important nursing
responsibility. They include a headache, dizziness, arrhythmias, blurred vision and confusion. The
patient should be instructed to verbalize any of these side effects if they occur.
Ramipril 5mg PO twice daily
Ramipril is an angiotensin-converting enzyme blocker with profound action on smooth
muscle causing vasodilation. It inhibits the formation of angiotensin II which is a vasoconstrictor thus
causing vasodilation (Katzung et al., 2012). It has a role in heart failure as it improves perfusion by
eliminating reflex vasoconstriction. The nurse should ensure no drug allergies in the patient exist and
no contraindication are present in the patient. Dosage and monitoring of therapy should also be
done.
Task 4: Patient education
Smoking is among the modifiable risk factors for most cardiovascular diseases. Smoking
cessation should be considered in any patient with or without cardiovascular disease as it is
unhealthy and has been implicated in many systemic diseases and cancers (US Department of Health
and Human Services, 2014). The patient could enroll in a rehabilitation program that is equipped
with support and medication to ensure smoking cessation, combating of withdrawal and positive
behavior modification (Thomas, 2012; Stead et al., 2013). To make sure David understand the
teaching, a teach-back method of patient education should be employed (Tamura-Lis, 2013). In this
method, the patient is taught the health effects of smoking, complications, and hazards and given
11
Double click here to fill in this footer
Last name__ _student number_NUR250 S2 2018 Assessment 1
The patient is on anti-failure medication with ramipril, digoxin, and furosemide. These are
among the drugs recommended for management of heart failure.
Furosemide 40mg PO twice daily
Furosemide is a loop-diuretic that functions to reduce fluid overload in heat failure. It
functions as a diuretic at the kidney to enhance salt and water excretion thus reducing fluid
accumulation (Katzung et al., 2012). Nursing responsibility during medication with furosemide
should include assessment of fluid balance and appropriate dosing. Drug allergy should be asked for
and any contraindications such as kidney disease and liver disease noted. Side effects include
nausea, vomiting, dizziness, and bleeding.
Digoxin 62.5mcg PO daily
Cardiac glycosides have been used in heart failure for years, with digoxin being one of them.
It is a positive inotrope that improves cardiac contractility thus improving cardiac output and
perfusion in heart failure (Katzung et al., 2012). Digitalis toxicity is a recognized adverse effect when
using this drug and can be fatal. Monitoring of dosage and adverse effects is an important nursing
responsibility. They include a headache, dizziness, arrhythmias, blurred vision and confusion. The
patient should be instructed to verbalize any of these side effects if they occur.
Ramipril 5mg PO twice daily
Ramipril is an angiotensin-converting enzyme blocker with profound action on smooth
muscle causing vasodilation. It inhibits the formation of angiotensin II which is a vasoconstrictor thus
causing vasodilation (Katzung et al., 2012). It has a role in heart failure as it improves perfusion by
eliminating reflex vasoconstriction. The nurse should ensure no drug allergies in the patient exist and
no contraindication are present in the patient. Dosage and monitoring of therapy should also be
done.
Task 4: Patient education
Smoking is among the modifiable risk factors for most cardiovascular diseases. Smoking
cessation should be considered in any patient with or without cardiovascular disease as it is
unhealthy and has been implicated in many systemic diseases and cancers (US Department of Health
and Human Services, 2014). The patient could enroll in a rehabilitation program that is equipped
with support and medication to ensure smoking cessation, combating of withdrawal and positive
behavior modification (Thomas, 2012; Stead et al., 2013). To make sure David understand the
teaching, a teach-back method of patient education should be employed (Tamura-Lis, 2013). In this
method, the patient is taught the health effects of smoking, complications, and hazards and given
11
Double click here to fill in this footer
Last name__ _student number_NUR250 S2 2018 Assessment 1
alternatives and options. They are then instructed to teach the health professional what they have
learned. Effective understanding is considered to be achieved if David can correctly teach the nurse
what he learned.
Task 5: ISBAR handover
Introduction
I am ------------------ a registered nurse in this department handing over Mr. David Parker, a patient
who was referred from the cardiology clinic under Dr-------------------- with a diagnosis of chronic
heart failure after presenting with dyspnoea at rest.
Situation
The patient was received unstable in the ward following the referral from cardiology.
Background
He is a patient who had been in our cared before due to a myocardial infarction. He had been
discharged through a rehabilitation facility. However, he refused to attend the program and also
refused diet guidelines as he did not eat the low-fat diet prepared by his wife. Other directives which
he ignored included cessation of smoking and alcohol use. His medication included ramipril, digoxin
and furosemide.
Assessment
His vitals were as follows: tachycardia of 118 beats per minute, tachypnoea of 24 breaths per minute
with a low oxygen saturation of 92%. His other vitals were within normal with a blood pressure of
102/84 and temperature of 36.5oC. He had dyspnoea at rest, a cough and was fatigued.
Recommendation and plan
The patient was put on 1000 ml fluid restriction which should be maintained. Monitor input and
output and administer medication as charted
12
Double click here to fill in this footer
Last name__ _student number_NUR250 S2 2018 Assessment 1
learned. Effective understanding is considered to be achieved if David can correctly teach the nurse
what he learned.
Task 5: ISBAR handover
Introduction
I am ------------------ a registered nurse in this department handing over Mr. David Parker, a patient
who was referred from the cardiology clinic under Dr-------------------- with a diagnosis of chronic
heart failure after presenting with dyspnoea at rest.
Situation
The patient was received unstable in the ward following the referral from cardiology.
Background
He is a patient who had been in our cared before due to a myocardial infarction. He had been
discharged through a rehabilitation facility. However, he refused to attend the program and also
refused diet guidelines as he did not eat the low-fat diet prepared by his wife. Other directives which
he ignored included cessation of smoking and alcohol use. His medication included ramipril, digoxin
and furosemide.
Assessment
His vitals were as follows: tachycardia of 118 beats per minute, tachypnoea of 24 breaths per minute
with a low oxygen saturation of 92%. His other vitals were within normal with a blood pressure of
102/84 and temperature of 36.5oC. He had dyspnoea at rest, a cough and was fatigued.
Recommendation and plan
The patient was put on 1000 ml fluid restriction which should be maintained. Monitor input and
output and administer medication as charted
12
Double click here to fill in this footer
Last name__ _student number_NUR250 S2 2018 Assessment 1
References
Böhm, M., Swedberg, K., Komajda, M., Borer, J. S., Ford, I., Dubost-Brama, A., ... & SHIFT
Investigators. (2010). Heart rate as a risk factor in chronic heart failure (SHIFT): the
association between heart rate and outcomes in a randomized placebo-controlled trial. The
Lancet, 376(9744), 886-894.
Brunner, L. S. (2010). Brunner & Suddarth's textbook of medical-surgical nursing (Vol. 1). Lippincott
Williams & Wilkins.
Douglas, G., Nicol, F., & Robertson, C. (Eds.). (2013). Macleod's Clinical Examination E-Book. Elsevier
Health Sciences.
Elliott, M., & Coventry, A. (2012). Critical care: the eight vital signs of patient monitoring. British
Journal of Nursing, 21(10), 621-625.
Glynn, M., Drake, W. M., & Hutchison, R. (2012). Hutchison's clinical methods: an integrated
approach to clinical practice. Edinburgh: W.B. Saunder
Goodlin, S. J., Wingate, S., Albert, N. M., Pressler, S. J., Houser, J., Kwon, J., ... & PAIN-HF
Investigators. (2012). Investigating pain in heart failure patients: the pain assessment,
incidence, and nature in heart failure (PAIN-HF) study. Journal of cardiac failure, 18(10), 776-
783.
Katzung, B. G., Masters, S. B., & Trevor, A. J. (2012). Basic and Clinical Pharmacology (LANGE Basic
Science). McGraw-Hill Education.
Kemps, H. M., de Vries, W. R., Schmikli, S. L., Zonderland, M. L., Hoogeveen, A. R., Thijssen, E. J., &
Schep, G. (2010). Assessment of the effects of physical training in patients with chronic heart
failure: the utility of effort-independent exercise variables. European journal of applied
physiology, 108(3), 469-476.
Kemps, H. M., Schep, G., Zonderland, M. L., Thijssen, E. J., De Vries, W. R., Wessels, B., ... & Wijn, P. F.
(2010). Are oxygen uptake kinetics in chronic heart failure limited by oxygen delivery or
oxygen utilization? International journal of cardiology, 142(2), 138-144.
13
Double click here to fill in this footer
Last name__ _student number_NUR250 S2 2018 Assessment 1
Böhm, M., Swedberg, K., Komajda, M., Borer, J. S., Ford, I., Dubost-Brama, A., ... & SHIFT
Investigators. (2010). Heart rate as a risk factor in chronic heart failure (SHIFT): the
association between heart rate and outcomes in a randomized placebo-controlled trial. The
Lancet, 376(9744), 886-894.
Brunner, L. S. (2010). Brunner & Suddarth's textbook of medical-surgical nursing (Vol. 1). Lippincott
Williams & Wilkins.
Douglas, G., Nicol, F., & Robertson, C. (Eds.). (2013). Macleod's Clinical Examination E-Book. Elsevier
Health Sciences.
Elliott, M., & Coventry, A. (2012). Critical care: the eight vital signs of patient monitoring. British
Journal of Nursing, 21(10), 621-625.
Glynn, M., Drake, W. M., & Hutchison, R. (2012). Hutchison's clinical methods: an integrated
approach to clinical practice. Edinburgh: W.B. Saunder
Goodlin, S. J., Wingate, S., Albert, N. M., Pressler, S. J., Houser, J., Kwon, J., ... & PAIN-HF
Investigators. (2012). Investigating pain in heart failure patients: the pain assessment,
incidence, and nature in heart failure (PAIN-HF) study. Journal of cardiac failure, 18(10), 776-
783.
Katzung, B. G., Masters, S. B., & Trevor, A. J. (2012). Basic and Clinical Pharmacology (LANGE Basic
Science). McGraw-Hill Education.
Kemps, H. M., de Vries, W. R., Schmikli, S. L., Zonderland, M. L., Hoogeveen, A. R., Thijssen, E. J., &
Schep, G. (2010). Assessment of the effects of physical training in patients with chronic heart
failure: the utility of effort-independent exercise variables. European journal of applied
physiology, 108(3), 469-476.
Kemps, H. M., Schep, G., Zonderland, M. L., Thijssen, E. J., De Vries, W. R., Wessels, B., ... & Wijn, P. F.
(2010). Are oxygen uptake kinetics in chronic heart failure limited by oxygen delivery or
oxygen utilization? International journal of cardiology, 142(2), 138-144.
13
Double click here to fill in this footer
Last name__ _student number_NUR250 S2 2018 Assessment 1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Kim, E. B., Susan, M. B., Scott, B., & Heddwen, L. B. (2010). Ganong’s review of medical physiology.
Marenzi, G., Assanelli, E., Campodonico, J., De Metrio, M., Lauri, G., Marana, I., ... & Bartorelli, A. L.
(2010). Acute kidney injury in ST-segment elevation acute myocardial infarction complicated
by cardiogenic shock at admission. Critical care medicine, 38(2), 438-444
Stead, L. F., Buitrago, D., Preciado, N., Sanchez, G., Hartmann-Boyce, J., & Lancaster, T. (2013).
Physician advice for smoking cessation.
Tamura-Lis, W. (2013). Teach-back for quality education and patient safety. Urologic Nursing, 33(6),
267.
Thomas, D. (2012). Smoking and cardiovascular diseases. La Revue du praticien, 62(3), 339-343.
Turk, D. C., & Melzack, R. (Eds.). (2011). Handbook of pain assessment. Guilford Press.
US Department of Health and Human Services. (2014). The health consequences of smoking—50
years of progress: a report of the Surgeon General. Atlanta, GA: US Department of Health
and Human Services, Centers for Disease Control and Prevention, National Center for Chronic
Disease Prevention and Health Promotion, Office on Smoking and Health, 17.
14
Double click here to fill in this footer
Last name__ _student number_NUR250 S2 2018 Assessment 1
Marenzi, G., Assanelli, E., Campodonico, J., De Metrio, M., Lauri, G., Marana, I., ... & Bartorelli, A. L.
(2010). Acute kidney injury in ST-segment elevation acute myocardial infarction complicated
by cardiogenic shock at admission. Critical care medicine, 38(2), 438-444
Stead, L. F., Buitrago, D., Preciado, N., Sanchez, G., Hartmann-Boyce, J., & Lancaster, T. (2013).
Physician advice for smoking cessation.
Tamura-Lis, W. (2013). Teach-back for quality education and patient safety. Urologic Nursing, 33(6),
267.
Thomas, D. (2012). Smoking and cardiovascular diseases. La Revue du praticien, 62(3), 339-343.
Turk, D. C., & Melzack, R. (Eds.). (2011). Handbook of pain assessment. Guilford Press.
US Department of Health and Human Services. (2014). The health consequences of smoking—50
years of progress: a report of the Surgeon General. Atlanta, GA: US Department of Health
and Human Services, Centers for Disease Control and Prevention, National Center for Chronic
Disease Prevention and Health Promotion, Office on Smoking and Health, 17.
14
Double click here to fill in this footer
Last name__ _student number_NUR250 S2 2018 Assessment 1
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.



