NUR251 Assignment 1: Assessing and Managing Diabetic Ketoacidosis
VerifiedAdded on 2022/08/20
|10
|2875
|17
Homework Assignment
AI Summary
This assignment focuses on the nursing management of a 15-year-old patient, Lily, admitted with diabetic ketoacidosis (DKA). The assessment encompasses vital signs, neurological behavior, blood glucose, urine analysis, and fluid balance. The solution details an initial care plan addressing fluid volume deficit, electrolyte imbalances, and unstable blood glucose levels. Nursing interventions include fluid administration, insulin therapy, dietary modifications, and patient education. The assignment also provides calculations for intravenous fluid rates and discusses the pharmacokinetics and side effects of insulin glargine and intravenous sodium chloride. The discharge plan emphasizes patient education on medication, diet, and blood glucose monitoring to prevent recurrence. The assignment highlights the importance of regular assessment, appropriate interventions, and comprehensive patient education in managing DKA.
NUR251 Assessment 1 S1 2020
Assessment One Template
Task 1
Diabetes ketoacidosis in children requires regular assessment of their vital signs, neurologic
behaviour, blood glucose level, glucose and ketones in the urine and fluid concentration. Lily is a 15
year old child who was diagnosed with diabetes mellitus at a young age and is now admitted to the
hospital due to diabetes ketoacidosis. The assessment should include documentation of the initial
care plan for the patient followed by changes in the assessment in progress notes. Further
assessment for preparing care plan for the patient must be according to the clinical judgement by
the nurse.
The nurse should check her vital signs where respiratory rate is high that is RR – 24 breaths
per minute (normal rate is 12 -20). Respiratory failure is directly correlated diabetes ketoacidosis.
High respiratory rate is associated with deficiency in potassium ions leading to hypokalemia, fall in
magnesium ions levels and lower serum levels of phosphorus due to hypophosphatemia. Lily’s
potassium level below normal (3-8 mmol/L) that is 2.4 mmol/L. If the potassium level is not
monitored and kept under normal range then increasing muscle weakness can occur thereby
affecting respiratory muscles and causing respiratory failure. High respiratory rate is an indication of
decreased potassium level (Gallo de Moraes & Surani, 2019). This respiratory assessment is
concentrated on measuring respiratory rate, depth and rhytm of the child that is number of breaths
taken by the child in one minute which must be recorded. This record must be compared with the
initial record of respiratory rate in the initial assessment (Rch.org.au, 2020).
Low sodium level in the serum is associated with diabetes ketoacidosis in children. This is
mainly caused by hyperglycemia that induces hyponatremia. It has been seen incase of Lily whose
serum level of sodium is below normal range ( 135-145 mEq/L) that is 128 mEq/L. The nurse should
measure the serum sodium level using osmometer that indicates plasma osmolality or Posm (Liamis
et al., 2015). Severe hyponatremia can cause fatigue, exhaustion and tiredness if the sodium level is
not balanced in the blood. Low sodium levels can also cause loss of appetite as seen in case of Lily
who is unwilling to eat. Gastrointestinal assessment criteria must be followed by the nurse to
inspect, the shape, size and abnormalities of the abdomen to understand the why Lily does not feel
like eating (Rch.org.au, 2020).
Another assessment for monitoring blood glucose level is done by monitoring HbAc1 (O
Ekpebegh et al., 2014). Hyperglycemia is a common condition in diabetes ketoacidosis. Normal level
1
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2020 Assessment 1
Assessment One Template
Task 1
Diabetes ketoacidosis in children requires regular assessment of their vital signs, neurologic
behaviour, blood glucose level, glucose and ketones in the urine and fluid concentration. Lily is a 15
year old child who was diagnosed with diabetes mellitus at a young age and is now admitted to the
hospital due to diabetes ketoacidosis. The assessment should include documentation of the initial
care plan for the patient followed by changes in the assessment in progress notes. Further
assessment for preparing care plan for the patient must be according to the clinical judgement by
the nurse.
The nurse should check her vital signs where respiratory rate is high that is RR – 24 breaths
per minute (normal rate is 12 -20). Respiratory failure is directly correlated diabetes ketoacidosis.
High respiratory rate is associated with deficiency in potassium ions leading to hypokalemia, fall in
magnesium ions levels and lower serum levels of phosphorus due to hypophosphatemia. Lily’s
potassium level below normal (3-8 mmol/L) that is 2.4 mmol/L. If the potassium level is not
monitored and kept under normal range then increasing muscle weakness can occur thereby
affecting respiratory muscles and causing respiratory failure. High respiratory rate is an indication of
decreased potassium level (Gallo de Moraes & Surani, 2019). This respiratory assessment is
concentrated on measuring respiratory rate, depth and rhytm of the child that is number of breaths
taken by the child in one minute which must be recorded. This record must be compared with the
initial record of respiratory rate in the initial assessment (Rch.org.au, 2020).
Low sodium level in the serum is associated with diabetes ketoacidosis in children. This is
mainly caused by hyperglycemia that induces hyponatremia. It has been seen incase of Lily whose
serum level of sodium is below normal range ( 135-145 mEq/L) that is 128 mEq/L. The nurse should
measure the serum sodium level using osmometer that indicates plasma osmolality or Posm (Liamis
et al., 2015). Severe hyponatremia can cause fatigue, exhaustion and tiredness if the sodium level is
not balanced in the blood. Low sodium levels can also cause loss of appetite as seen in case of Lily
who is unwilling to eat. Gastrointestinal assessment criteria must be followed by the nurse to
inspect, the shape, size and abnormalities of the abdomen to understand the why Lily does not feel
like eating (Rch.org.au, 2020).
Another assessment for monitoring blood glucose level is done by monitoring HbAc1 (O
Ekpebegh et al., 2014). Hyperglycemia is a common condition in diabetes ketoacidosis. Normal level
1
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2020 Assessment 1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
of blood glucose is the between 4 and 8 mmol/L but in case of Lily the blood glucose level is 12
mmol/L, which is very high signifying increased glucose in the blood due to lack of insulin to control
glucose level and this is an indicator of type 1 diabetes. Glucose level is increased in patients like Lily
if it is not monitored and can lead to many complications such as obesity, kidney failure and
impairment of vision. Urinalysis can be performed for assessing the presence of ketones and glucose
in the urine with the help of urine dipstick. Presence of ketone in the body is an important indicator
of ketoacidosis where the ketones as byproduct of lipid metabolism are released in increased
amount with the urine (Siafarikas & O’Connell, 2010). Any abnormal finding during urinalysis such as
presence of ketones must be documented with the initial pathology results to identify the
abnormalities and preparing appropriate nursing action (Rch.org.au, 2020).
2
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2020 Assessment 1
mmol/L, which is very high signifying increased glucose in the blood due to lack of insulin to control
glucose level and this is an indicator of type 1 diabetes. Glucose level is increased in patients like Lily
if it is not monitored and can lead to many complications such as obesity, kidney failure and
impairment of vision. Urinalysis can be performed for assessing the presence of ketones and glucose
in the urine with the help of urine dipstick. Presence of ketone in the body is an important indicator
of ketoacidosis where the ketones as byproduct of lipid metabolism are released in increased
amount with the urine (Siafarikas & O’Connell, 2010). Any abnormal finding during urinalysis such as
presence of ketones must be documented with the initial pathology results to identify the
abnormalities and preparing appropriate nursing action (Rch.org.au, 2020).
2
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2020 Assessment 1
Task 2
Nursing Care Plan: Mrs Lily Orange
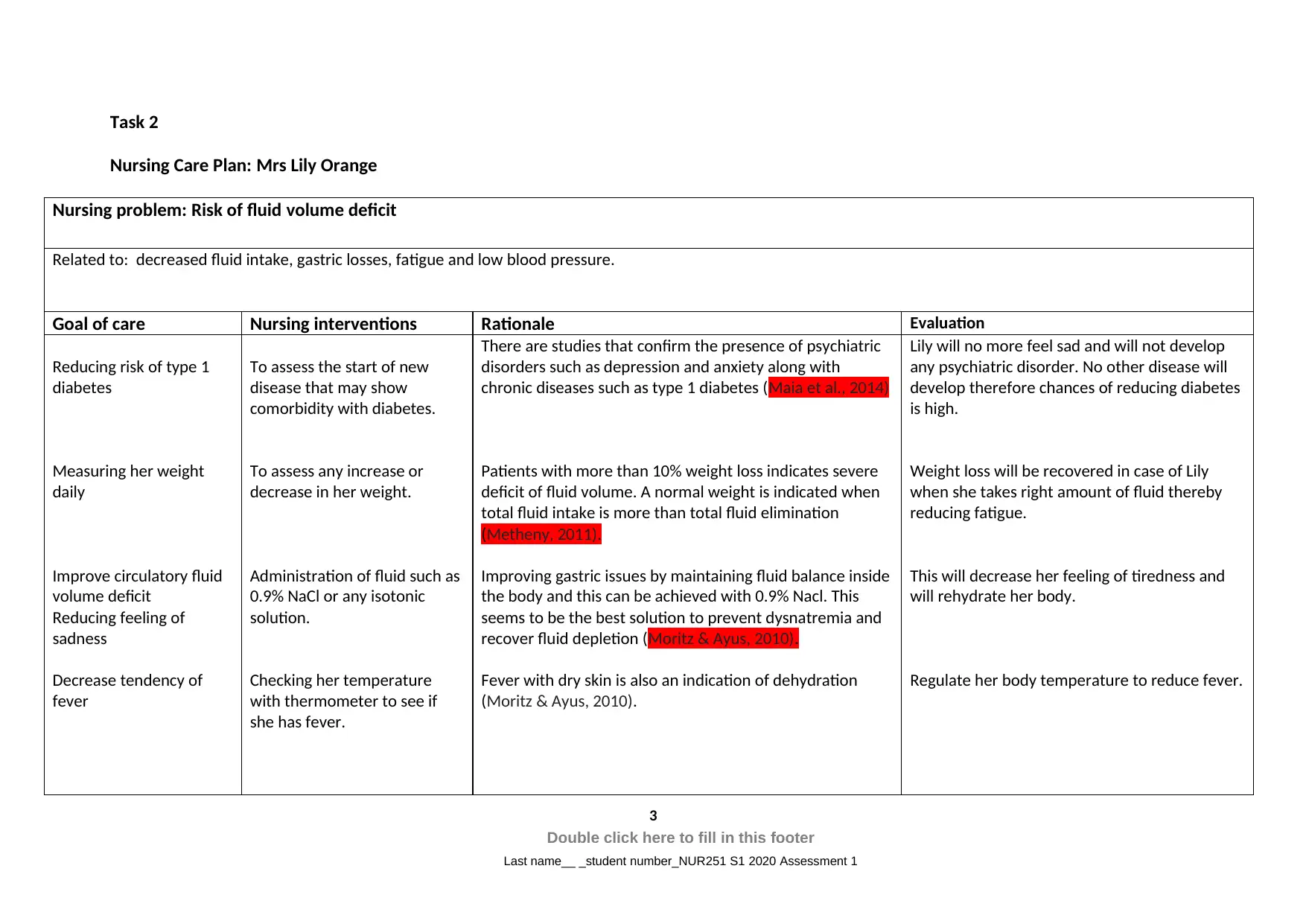
Nursing problem: Risk of fluid volume deficit
Related to: decreased fluid intake, gastric losses, fatigue and low blood pressure.
Goal of care Nursing interventions Rationale Evaluation
Reducing risk of type 1
diabetes
Measuring her weight
daily
Improve circulatory fluid
volume deficit
Reducing feeling of
sadness
Decrease tendency of
fever
To assess the start of new
disease that may show
comorbidity with diabetes.
To assess any increase or
decrease in her weight.
Administration of fluid such as
0.9% NaCl or any isotonic
solution.
Checking her temperature
with thermometer to see if
she has fever.
There are studies that confirm the presence of psychiatric
disorders such as depression and anxiety along with
chronic diseases such as type 1 diabetes (Maia et al., 2014)
Patients with more than 10% weight loss indicates severe
deficit of fluid volume. A normal weight is indicated when
total fluid intake is more than total fluid elimination
(Metheny, 2011).
Improving gastric issues by maintaining fluid balance inside
the body and this can be achieved with 0.9% Nacl. This
seems to be the best solution to prevent dysnatremia and
recover fluid depletion (Moritz & Ayus, 2010).
Fever with dry skin is also an indication of dehydration
(Moritz & Ayus, 2010).
Lily will no more feel sad and will not develop
any psychiatric disorder. No other disease will
develop therefore chances of reducing diabetes
is high.
Weight loss will be recovered in case of Lily
when she takes right amount of fluid thereby
reducing fatigue.
This will decrease her feeling of tiredness and
will rehydrate her body.
Regulate her body temperature to reduce fever.
3
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2020 Assessment 1
Nursing Care Plan: Mrs Lily Orange
Nursing problem: Risk of fluid volume deficit
Related to: decreased fluid intake, gastric losses, fatigue and low blood pressure.
Goal of care Nursing interventions Rationale Evaluation
Reducing risk of type 1
diabetes
Measuring her weight
daily
Improve circulatory fluid
volume deficit
Reducing feeling of
sadness
Decrease tendency of
fever
To assess the start of new
disease that may show
comorbidity with diabetes.
To assess any increase or
decrease in her weight.
Administration of fluid such as
0.9% NaCl or any isotonic
solution.
Checking her temperature
with thermometer to see if
she has fever.
There are studies that confirm the presence of psychiatric
disorders such as depression and anxiety along with
chronic diseases such as type 1 diabetes (Maia et al., 2014)
Patients with more than 10% weight loss indicates severe
deficit of fluid volume. A normal weight is indicated when
total fluid intake is more than total fluid elimination
(Metheny, 2011).
Improving gastric issues by maintaining fluid balance inside
the body and this can be achieved with 0.9% Nacl. This
seems to be the best solution to prevent dysnatremia and
recover fluid depletion (Moritz & Ayus, 2010).
Fever with dry skin is also an indication of dehydration
(Moritz & Ayus, 2010).
Lily will no more feel sad and will not develop
any psychiatric disorder. No other disease will
develop therefore chances of reducing diabetes
is high.
Weight loss will be recovered in case of Lily
when she takes right amount of fluid thereby
reducing fatigue.
This will decrease her feeling of tiredness and
will rehydrate her body.
Regulate her body temperature to reduce fever.
3
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2020 Assessment 1
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
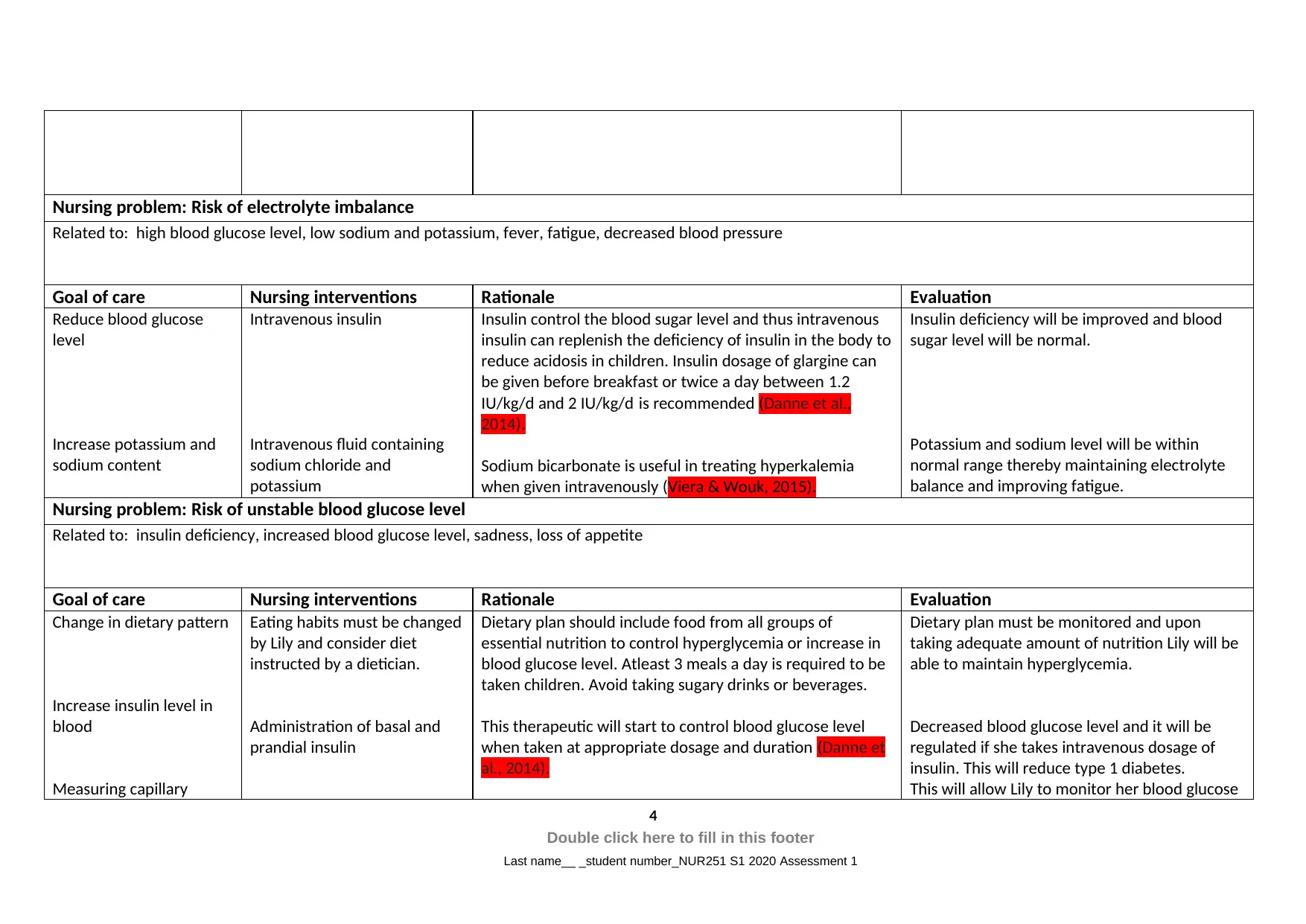
Nursing problem: Risk of electrolyte imbalance
Related to: high blood glucose level, low sodium and potassium, fever, fatigue, decreased blood pressure
Goal of care Nursing interventions Rationale Evaluation
Reduce blood glucose
level
Increase potassium and
sodium content
Intravenous insulin
Intravenous fluid containing
sodium chloride and
potassium
Insulin control the blood sugar level and thus intravenous
insulin can replenish the deficiency of insulin in the body to
reduce acidosis in children. Insulin dosage of glargine can
be given before breakfast or twice a day between 1.2
IU/kg/d and 2 IU/kg/d is recommended (Danne et al.,
2014).
Sodium bicarbonate is useful in treating hyperkalemia
when given intravenously (Viera & Wouk, 2015).
Insulin deficiency will be improved and blood
sugar level will be normal.
Potassium and sodium level will be within
normal range thereby maintaining electrolyte
balance and improving fatigue.
Nursing problem: Risk of unstable blood glucose level
Related to: insulin deficiency, increased blood glucose level, sadness, loss of appetite
Goal of care Nursing interventions Rationale Evaluation
Change in dietary pattern
Increase insulin level in
blood
Measuring capillary
Eating habits must be changed
by Lily and consider diet
instructed by a dietician.
Administration of basal and
prandial insulin
Dietary plan should include food from all groups of
essential nutrition to control hyperglycemia or increase in
blood glucose level. Atleast 3 meals a day is required to be
taken children. Avoid taking sugary drinks or beverages.
This therapeutic will start to control blood glucose level
when taken at appropriate dosage and duration (Danne et
al., 2014).
Dietary plan must be monitored and upon
taking adequate amount of nutrition Lily will be
able to maintain hyperglycemia.
Decreased blood glucose level and it will be
regulated if she takes intravenous dosage of
insulin. This will reduce type 1 diabetes.
This will allow Lily to monitor her blood glucose
4
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2020 Assessment 1
Related to: high blood glucose level, low sodium and potassium, fever, fatigue, decreased blood pressure
Goal of care Nursing interventions Rationale Evaluation
Reduce blood glucose
level
Increase potassium and
sodium content
Intravenous insulin
Intravenous fluid containing
sodium chloride and
potassium
Insulin control the blood sugar level and thus intravenous
insulin can replenish the deficiency of insulin in the body to
reduce acidosis in children. Insulin dosage of glargine can
be given before breakfast or twice a day between 1.2
IU/kg/d and 2 IU/kg/d is recommended (Danne et al.,
2014).
Sodium bicarbonate is useful in treating hyperkalemia
when given intravenously (Viera & Wouk, 2015).
Insulin deficiency will be improved and blood
sugar level will be normal.
Potassium and sodium level will be within
normal range thereby maintaining electrolyte
balance and improving fatigue.
Nursing problem: Risk of unstable blood glucose level
Related to: insulin deficiency, increased blood glucose level, sadness, loss of appetite
Goal of care Nursing interventions Rationale Evaluation
Change in dietary pattern
Increase insulin level in
blood
Measuring capillary
Eating habits must be changed
by Lily and consider diet
instructed by a dietician.
Administration of basal and
prandial insulin
Dietary plan should include food from all groups of
essential nutrition to control hyperglycemia or increase in
blood glucose level. Atleast 3 meals a day is required to be
taken children. Avoid taking sugary drinks or beverages.
This therapeutic will start to control blood glucose level
when taken at appropriate dosage and duration (Danne et
al., 2014).
Dietary plan must be monitored and upon
taking adequate amount of nutrition Lily will be
able to maintain hyperglycemia.
Decreased blood glucose level and it will be
regulated if she takes intravenous dosage of
insulin. This will reduce type 1 diabetes.
This will allow Lily to monitor her blood glucose
4
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2020 Assessment 1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
glucose in blood Teaching patient to measure
their own capillary blood
glucose level
Using capillary technique of devices that measure blood
glucose at any point of time giving instant result that is
displayed digitally. It can be useful because patients can
themselves monitor blood glucose that will be accurate
(Laffel, 2016).
level at any time and control her dietary plan
according to it. This will ensure whether the
medications are effective in reducing her blood
glucose level.
5
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2020 Assessment 1
their own capillary blood
glucose level
Using capillary technique of devices that measure blood
glucose at any point of time giving instant result that is
displayed digitally. It can be useful because patients can
themselves monitor blood glucose that will be accurate
(Laffel, 2016).
level at any time and control her dietary plan
according to it. This will ensure whether the
medications are effective in reducing her blood
glucose level.
5
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2020 Assessment 1
Task 3
The discharge plan should include the information on the condition of the Lily with all
the details of the assessment process and medication chart regarding the dosage, type of
medication along with its duration (Ahrq.gov, 2020). The details on the condition of Lily could
be presented in the form of medical report that can be carried home by Lily and her family.
The medication chart should include the process of administrating the medication. The
medication chart should also contain details of how insulin should be injected intravenously
through the ACF region where the IVC were inserted and what dosage of insulin should be
given to Lily either once or twice daily. An important information should include monitoring
of blood glucose level with the help of blood sugar meter that displays the level of glucose as
digital reading and if the glucose level is high then blood ketones should also be monitored.
Blood sugar level monitoring procedure must be explained in the patient information chart
and it should be monitored three times a day. The normal range for blood glucose level and
ketones in the body should be mentioned. Lily can check her urine and breath for fruity
smell, an indicator of increased ketones in the body fluid (lson, 2010). All of these
information must be explained as a part of patient education to Lily and her family so that
they follow the medication guideline regularly.
Another strategy to control or prevent the recurrence of ketoacidosis in Lily is
providing her a dietary chart that includes the kind of nutrition she will intake to reduce her
chances of developing ketoacidosis. Dietary plan should include nutrition that is restrictive
and adequate nutrition to control hyperglycemia (Souto & Rosado, 2010).This should provide
information on the number of meals per day and the food items contained in the meal. Her
meal should also include salt substitutes to maintain her fluid and electrolyte balance. She
should have enough water and her fluid intake must be more than the fluid output. Her meal
should exclude simple carbohydrates that will maintain her insulin-to-carb ratio (Rewers,
2012). Therefore Lily and her parents should be educated by the nurse on the diet plan of Lily
before she is discharged from the hospital and that will include the importance of this diet
plan prepared on Lily’s condition.
6
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2020 Assessment 1
The discharge plan should include the information on the condition of the Lily with all
the details of the assessment process and medication chart regarding the dosage, type of
medication along with its duration (Ahrq.gov, 2020). The details on the condition of Lily could
be presented in the form of medical report that can be carried home by Lily and her family.
The medication chart should include the process of administrating the medication. The
medication chart should also contain details of how insulin should be injected intravenously
through the ACF region where the IVC were inserted and what dosage of insulin should be
given to Lily either once or twice daily. An important information should include monitoring
of blood glucose level with the help of blood sugar meter that displays the level of glucose as
digital reading and if the glucose level is high then blood ketones should also be monitored.
Blood sugar level monitoring procedure must be explained in the patient information chart
and it should be monitored three times a day. The normal range for blood glucose level and
ketones in the body should be mentioned. Lily can check her urine and breath for fruity
smell, an indicator of increased ketones in the body fluid (lson, 2010). All of these
information must be explained as a part of patient education to Lily and her family so that
they follow the medication guideline regularly.
Another strategy to control or prevent the recurrence of ketoacidosis in Lily is
providing her a dietary chart that includes the kind of nutrition she will intake to reduce her
chances of developing ketoacidosis. Dietary plan should include nutrition that is restrictive
and adequate nutrition to control hyperglycemia (Souto & Rosado, 2010).This should provide
information on the number of meals per day and the food items contained in the meal. Her
meal should also include salt substitutes to maintain her fluid and electrolyte balance. She
should have enough water and her fluid intake must be more than the fluid output. Her meal
should exclude simple carbohydrates that will maintain her insulin-to-carb ratio (Rewers,
2012). Therefore Lily and her parents should be educated by the nurse on the diet plan of Lily
before she is discharged from the hospital and that will include the importance of this diet
plan prepared on Lily’s condition.
6
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2020 Assessment 1
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Task 4
To calculate the hourly rate of the intravenous fluid the following formulas are to be used
Drip Rate = Volume (mL) / Time (h) .
Time (hours) = Volume (mL) Drip Rate (mL/hour) (Lor.usq.edu.au, 2020).
For sodium lactate- 500ml over 2 hours
Drip rate= 500/2
= 250 ml/hr
Time= 500/250
= 2 hours
For sodium chloride-
Drip rate- 1000ml/ 8 hrs = 125
Time= 1000/125
= 8 hours.
Insulin glargine and intravenous sodium chloride 1000ml/8 hrs are chosen-
Insulin glargine:
Pharmacokinetics- after subcutaneous administration of the insulin in diabetic patients, the
drug acts as slow acting thereby longer absorption time along with constant
concentration/time in 24 hours is seen. Glargine is not completely metabolised from the
carboxy end of its B chain in the subcutaneous layer forming two metabolites that are not
further degraded.
Reason for prescription- to treat Lily with the insulin for controlling blood glucose level or
hyperglycemia that occurs during Diabetes ketoacidosis.
Side effects- one of the adverse effects of glargin is development of allergies on the site of
injection and hypoglycaemia when used for a prolonged period (Tga.gov.au, 2020).
Intravenous sodium chloride:
7
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2020 Assessment 1
To calculate the hourly rate of the intravenous fluid the following formulas are to be used
Drip Rate = Volume (mL) / Time (h) .
Time (hours) = Volume (mL) Drip Rate (mL/hour) (Lor.usq.edu.au, 2020).
For sodium lactate- 500ml over 2 hours
Drip rate= 500/2
= 250 ml/hr
Time= 500/250
= 2 hours
For sodium chloride-
Drip rate- 1000ml/ 8 hrs = 125
Time= 1000/125
= 8 hours.
Insulin glargine and intravenous sodium chloride 1000ml/8 hrs are chosen-
Insulin glargine:
Pharmacokinetics- after subcutaneous administration of the insulin in diabetic patients, the
drug acts as slow acting thereby longer absorption time along with constant
concentration/time in 24 hours is seen. Glargine is not completely metabolised from the
carboxy end of its B chain in the subcutaneous layer forming two metabolites that are not
further degraded.
Reason for prescription- to treat Lily with the insulin for controlling blood glucose level or
hyperglycemia that occurs during Diabetes ketoacidosis.
Side effects- one of the adverse effects of glargin is development of allergies on the site of
injection and hypoglycaemia when used for a prolonged period (Tga.gov.au, 2020).
Intravenous sodium chloride:
7
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2020 Assessment 1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Pharmacokinetics- the bioavailability of the intravenous sodium chloride is 100% because it
is directly injected into the blood therefore does not require absorption. Excess of salt is
eliminated through the kidneys and very small amount is lost as sweat and through faeces.
Reason for prescription- for restoring electrolytes in the body of Lily, because her sodium
level is low. It will also increase the level of extracellular fluid thereby preventing fluid
imbalance.
Side effects- if the infusion is for a long time then the injection site may causes clots in the
blood and block veins, a condition called thrombophlebitis. Excessive use may also cause
hypernatraemia and hypokalaemia, or may increase acidosis in patients suffering from diabetic
ketoacidosis (Secure.healthlinks.net.au, 2020).
Keyword:
ACF- antecubital fossa
IVC- Intravenous catheter
8
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2020 Assessment 1
is directly injected into the blood therefore does not require absorption. Excess of salt is
eliminated through the kidneys and very small amount is lost as sweat and through faeces.
Reason for prescription- for restoring electrolytes in the body of Lily, because her sodium
level is low. It will also increase the level of extracellular fluid thereby preventing fluid
imbalance.
Side effects- if the infusion is for a long time then the injection site may causes clots in the
blood and block veins, a condition called thrombophlebitis. Excessive use may also cause
hypernatraemia and hypokalaemia, or may increase acidosis in patients suffering from diabetic
ketoacidosis (Secure.healthlinks.net.au, 2020).
Keyword:
ACF- antecubital fossa
IVC- Intravenous catheter
8
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2020 Assessment 1
References:
Ahrq.gov. (2020). IDEAL Discharge Planning Overview, Process, and Checklist. Ahrq.gov. Retrieved 29
March 2020, from
https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/systems/hospital/
engagingfamilies/strategy4/Strat4_Tool_1_IDEAL_chklst_508.pdf.
Danne, T., Bangstad, H. J., Deeb, L., Jarosz Chobot, P., Mungaie, L., Saboo, B., ... & Hanas, R. (2014).‐
Insulin treatment in children and adolescents with diabetes. Pediatric diabetes, 15(S20), 115-
134. https://doi.org/10.1186/s13643-019-1171-9
Gallo de Moraes, A., & Surani, S. (2019). Effects of diabetic ketoacidosis in the respiratory
system. World journal of diabetes, 10(1), 16–22. https://doi.org/10.4239/wjd.v10.i1.16
Laffel, L. (2016). Improved accuracy of continuous glucose monitoring systems in pediatric patients
with diabetes mellitus: results from two studies. Diabetes technology & therapeutics, 18(S2),
S2-23.
Liamis, G., Tsimihodimos, V., & Elisaf, M. (2015). Hyponatremia in diabetes mellitus: clues to
diagnosis and treatment. J Diabetes Metab, 6(5), 559-61.
https://doi.org/10.1089/dia.2015.0380
Lor.usq.edu.au. (2020). Intravenous Infusion Calculations. Lor.usq.edu.au. Retrieved 29 March 2020,
from https://lor.usq.edu.au/usq/file/d7126477-43e3-402f-a988-e61a3dbe28ec/1/
IVCalculation%20_2018.pdf.
Maia, A. C. C., Braga, A. D. A., Paes, F., Machado, S., Nardi, A. E., & Silva, A. C. D. (2014). Psychiatric
comorbidity in diabetes type 1: a cross-sectional observational study. Revista da Associação
Médica Brasileira, 60(1), 59-62. https://doi.org10.1590/1806-9282.60.01.013
Metheny, N. (2011). Fluid and electrolyte balance. Jones & Bartlett Publishers. Retrieved from
ISBN:978-0-7637-8164-4
Moritz, M. L., & Ayus, J. C. (2010). Improving intravenous fluid therapy in children with
gastroenteritis. Pediatric Nephrology, 25(8), 1383-1384. https://doi.org/10.1007/s00467-
010-1505-2
O Ekpebegh, C., Longo-Mbenza, B., & Blanco-Blanco, E. (2014). Glycosylated haemoglobin is markedly
elevated in new and known diabetes patients with hyperglycaemic ketoacidosis. African
health sciences, 14(3), 526–532. https://doi.org/10.4314/ahs.v14i3.5
Rch.org.au. (2020). Clinical Guidelines (Nursing) : Nursing assessment. Rch.org.au. Retrieved 29
March 2020, from
https://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Nursing_assessment/.
9
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2020 Assessment 1
Ahrq.gov. (2020). IDEAL Discharge Planning Overview, Process, and Checklist. Ahrq.gov. Retrieved 29
March 2020, from
https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/systems/hospital/
engagingfamilies/strategy4/Strat4_Tool_1_IDEAL_chklst_508.pdf.
Danne, T., Bangstad, H. J., Deeb, L., Jarosz Chobot, P., Mungaie, L., Saboo, B., ... & Hanas, R. (2014).‐
Insulin treatment in children and adolescents with diabetes. Pediatric diabetes, 15(S20), 115-
134. https://doi.org/10.1186/s13643-019-1171-9
Gallo de Moraes, A., & Surani, S. (2019). Effects of diabetic ketoacidosis in the respiratory
system. World journal of diabetes, 10(1), 16–22. https://doi.org/10.4239/wjd.v10.i1.16
Laffel, L. (2016). Improved accuracy of continuous glucose monitoring systems in pediatric patients
with diabetes mellitus: results from two studies. Diabetes technology & therapeutics, 18(S2),
S2-23.
Liamis, G., Tsimihodimos, V., & Elisaf, M. (2015). Hyponatremia in diabetes mellitus: clues to
diagnosis and treatment. J Diabetes Metab, 6(5), 559-61.
https://doi.org/10.1089/dia.2015.0380
Lor.usq.edu.au. (2020). Intravenous Infusion Calculations. Lor.usq.edu.au. Retrieved 29 March 2020,
from https://lor.usq.edu.au/usq/file/d7126477-43e3-402f-a988-e61a3dbe28ec/1/
IVCalculation%20_2018.pdf.
Maia, A. C. C., Braga, A. D. A., Paes, F., Machado, S., Nardi, A. E., & Silva, A. C. D. (2014). Psychiatric
comorbidity in diabetes type 1: a cross-sectional observational study. Revista da Associação
Médica Brasileira, 60(1), 59-62. https://doi.org10.1590/1806-9282.60.01.013
Metheny, N. (2011). Fluid and electrolyte balance. Jones & Bartlett Publishers. Retrieved from
ISBN:978-0-7637-8164-4
Moritz, M. L., & Ayus, J. C. (2010). Improving intravenous fluid therapy in children with
gastroenteritis. Pediatric Nephrology, 25(8), 1383-1384. https://doi.org/10.1007/s00467-
010-1505-2
O Ekpebegh, C., Longo-Mbenza, B., & Blanco-Blanco, E. (2014). Glycosylated haemoglobin is markedly
elevated in new and known diabetes patients with hyperglycaemic ketoacidosis. African
health sciences, 14(3), 526–532. https://doi.org/10.4314/ahs.v14i3.5
Rch.org.au. (2020). Clinical Guidelines (Nursing) : Nursing assessment. Rch.org.au. Retrieved 29
March 2020, from
https://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Nursing_assessment/.
9
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2020 Assessment 1
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Rewers, A. (2012). Current concepts and controversies in prevention and treatment of diabetic
ketoacidosis in children. Current diabetes reports, 12(5), 524-532.
https://doi.org/10.1007/s11892-012-0307-2
Secure.healthlinks.net.au. (2020). AUSTRALIAN PRODUCT INFORMATION – SODIUM CHLORIDE
INJECTION 0.9% BP SODIUM CHLORIDE INTRAVENOUS INFUSION 0.9% BP (SODIUM
CHLORIDE). Secure.healthlinks.net.au. Retrieved 29 March 2020, from
http://secure.healthlinks.net.au/content/pf/retriever.cfm?product=pfpsodii10612.
Siafarikas, A., & O’Connell, S. (2010). Type 1 diabetes in children: Emergency
management. Australian family physician, 39(5), 290. Retrieved from
https://www.ncbi.nlm.nih.gov/pubmed/20485715
Smart, C. E., Annan, F., Bruno, L. P., Higgins, L. A., & Acerini, C. L. (2014). Nutritional management in
children and adolescents with diabetes. Pediatric diabetes, 15(S20), 135-153.
https://doi.org/10.1111/pedi.12175
Souto, D. L., & Rosado, E. L. (2010). Use of carb counting in the dietary treatment of diabetes
mellitus. Nutricion hospitalaria, 25(1), 18-25. https://doi.org/10.3305/nh.2010.25.1.4324
Tga.gov.au. (2020). Australian Public Assessment Report for Insulin glargine. Tga.gov.au. Retrieved 2
April 2020, from https://www.tga.gov.au/sites/default/files/auspar-insulin-glargine-150828.pdf.
Viera, A. J., & Wouk, N. (2015). Potassium disorders: hypokalemia and hyperkalemia. American
family physician, 92(6), 487-495. Retrieved from
https://www.aafp.org/afp/2015/0915/p487.html
Wilson, J. F. (2010). Diabetic ketoacidosis. Annals of internal medicine, 152(1), ITC1-1.
https://doi.org/10.7326/0003-4819-152-1-201001050-01001
10
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2020 Assessment 1
ketoacidosis in children. Current diabetes reports, 12(5), 524-532.
https://doi.org/10.1007/s11892-012-0307-2
Secure.healthlinks.net.au. (2020). AUSTRALIAN PRODUCT INFORMATION – SODIUM CHLORIDE
INJECTION 0.9% BP SODIUM CHLORIDE INTRAVENOUS INFUSION 0.9% BP (SODIUM
CHLORIDE). Secure.healthlinks.net.au. Retrieved 29 March 2020, from
http://secure.healthlinks.net.au/content/pf/retriever.cfm?product=pfpsodii10612.
Siafarikas, A., & O’Connell, S. (2010). Type 1 diabetes in children: Emergency
management. Australian family physician, 39(5), 290. Retrieved from
https://www.ncbi.nlm.nih.gov/pubmed/20485715
Smart, C. E., Annan, F., Bruno, L. P., Higgins, L. A., & Acerini, C. L. (2014). Nutritional management in
children and adolescents with diabetes. Pediatric diabetes, 15(S20), 135-153.
https://doi.org/10.1111/pedi.12175
Souto, D. L., & Rosado, E. L. (2010). Use of carb counting in the dietary treatment of diabetes
mellitus. Nutricion hospitalaria, 25(1), 18-25. https://doi.org/10.3305/nh.2010.25.1.4324
Tga.gov.au. (2020). Australian Public Assessment Report for Insulin glargine. Tga.gov.au. Retrieved 2
April 2020, from https://www.tga.gov.au/sites/default/files/auspar-insulin-glargine-150828.pdf.
Viera, A. J., & Wouk, N. (2015). Potassium disorders: hypokalemia and hyperkalemia. American
family physician, 92(6), 487-495. Retrieved from
https://www.aafp.org/afp/2015/0915/p487.html
Wilson, J. F. (2010). Diabetic ketoacidosis. Annals of internal medicine, 152(1), ITC1-1.
https://doi.org/10.7326/0003-4819-152-1-201001050-01001
10
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2020 Assessment 1
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





