Nur331 Complex Care - Assessment Task 1B Case Study
VerifiedAdded on 2022/11/10
|9
|2711
|111
AI Summary
This article discusses a case study of a patient with sepsis due to a wound in his left leg. It covers the systematic assessment, priorities of treatment, and discharge planning for the patient. The article emphasizes the importance of early recognition and management of sepsis to prevent life-threatening conditions.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Assessment Task 1B Case Study
Nur331 Complex Care
Student Name:……..
Student ID:…………
University:…….
Nur331 Complex Care
Student Name:……..
Student ID:…………
University:…….
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Nur331 Complex care – Assessment Task 1B 2
Introduction
I have chosen the Case 3 Sepsis. The case involves a patient named Peters (45 year old) who is
brought to emergency department for complaints of sepsis due to wound in his left leg. The
wound occurred two weeks ago and has developed green exudates with inflammation.
Systematic assessment:
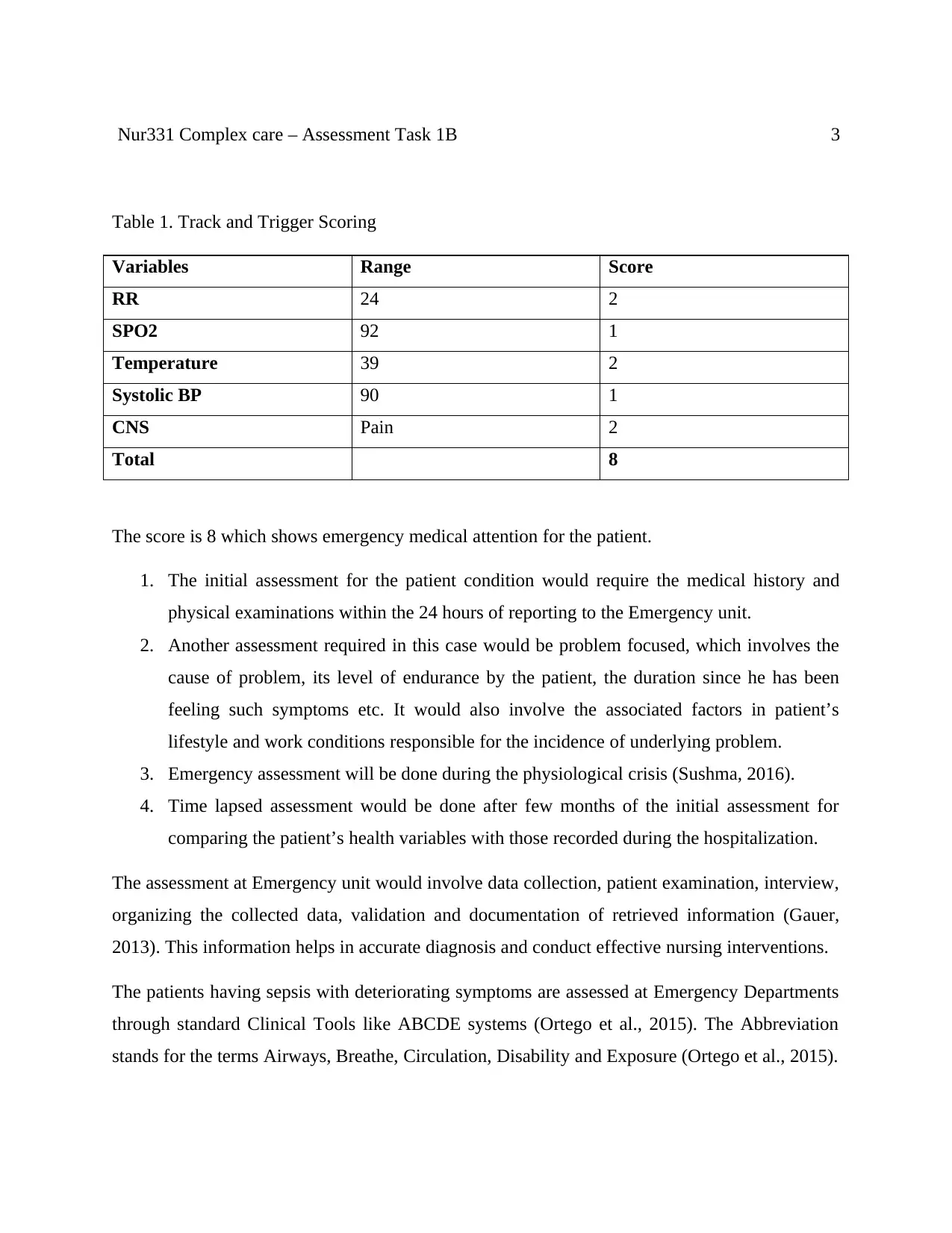
Diagnostic criteria process will be used to assess and identify the Sepsis. The process involves
documentation of infection through multiple parameters such as general variables, inflammation,
tissue perfusion, organ dysfunction and hemodynamics. Track and Trigger Scoring System may
be used to measure the severity of sepsis based on patient’s physiological derangement from the
normal ranges. The variables such as RR, SPO2, HR, BP, Temperature and CNS value can be
used to measure the score for Track and Trigger System.
CNS: I would check the CNS value. John is Alert, oriented, with clear speech. GCS= 15 shows
normal functioning of brain with Spontaneous Eye Opening, Oriented Verbal Response, Good
Motor Response (Obeys command).
CVS: HR 120, BP= 90/60, SPO2= 92%. Low BP leads to complications like decreasing the
blood supply to vital body organs. The heart works harder to meet the oxygen demands, thus
Heart rate increases in sepsis. A blood Oxygen level of 92% shows Hypoxemia.
RESP: RR 24 bpm shows faster Respiratory Rate which is a serious health condition. Sepsis is
an infection which often results in rapid breathing.
ABDO: Pain 5/10 (Moderate pain)
RENAL: Unknown
OTHER: Temperature 39 (Mild Fever), Weight 88 kgs( obesity)
Introduction
I have chosen the Case 3 Sepsis. The case involves a patient named Peters (45 year old) who is
brought to emergency department for complaints of sepsis due to wound in his left leg. The
wound occurred two weeks ago and has developed green exudates with inflammation.
Systematic assessment:
Diagnostic criteria process will be used to assess and identify the Sepsis. The process involves
documentation of infection through multiple parameters such as general variables, inflammation,
tissue perfusion, organ dysfunction and hemodynamics. Track and Trigger Scoring System may
be used to measure the severity of sepsis based on patient’s physiological derangement from the
normal ranges. The variables such as RR, SPO2, HR, BP, Temperature and CNS value can be
used to measure the score for Track and Trigger System.
CNS: I would check the CNS value. John is Alert, oriented, with clear speech. GCS= 15 shows
normal functioning of brain with Spontaneous Eye Opening, Oriented Verbal Response, Good
Motor Response (Obeys command).
CVS: HR 120, BP= 90/60, SPO2= 92%. Low BP leads to complications like decreasing the
blood supply to vital body organs. The heart works harder to meet the oxygen demands, thus
Heart rate increases in sepsis. A blood Oxygen level of 92% shows Hypoxemia.
RESP: RR 24 bpm shows faster Respiratory Rate which is a serious health condition. Sepsis is
an infection which often results in rapid breathing.
ABDO: Pain 5/10 (Moderate pain)
RENAL: Unknown
OTHER: Temperature 39 (Mild Fever), Weight 88 kgs( obesity)
Nur331 Complex care – Assessment Task 1B 3
Table 1. Track and Trigger Scoring
Variables Range Score
RR 24 2
SPO2 92 1
Temperature 39 2
Systolic BP 90 1
CNS Pain 2
Total 8
The score is 8 which shows emergency medical attention for the patient.
1. The initial assessment for the patient condition would require the medical history and
physical examinations within the 24 hours of reporting to the Emergency unit.
2. Another assessment required in this case would be problem focused, which involves the
cause of problem, its level of endurance by the patient, the duration since he has been
feeling such symptoms etc. It would also involve the associated factors in patient’s
lifestyle and work conditions responsible for the incidence of underlying problem.
3. Emergency assessment will be done during the physiological crisis (Sushma, 2016).
4. Time lapsed assessment would be done after few months of the initial assessment for
comparing the patient’s health variables with those recorded during the hospitalization.
The assessment at Emergency unit would involve data collection, patient examination, interview,
organizing the collected data, validation and documentation of retrieved information (Gauer,
2013). This information helps in accurate diagnosis and conduct effective nursing interventions.
The patients having sepsis with deteriorating symptoms are assessed at Emergency Departments
through standard Clinical Tools like ABCDE systems (Ortego et al., 2015). The Abbreviation
stands for the terms Airways, Breathe, Circulation, Disability and Exposure (Ortego et al., 2015).
Table 1. Track and Trigger Scoring
Variables Range Score
RR 24 2
SPO2 92 1
Temperature 39 2
Systolic BP 90 1
CNS Pain 2
Total 8
The score is 8 which shows emergency medical attention for the patient.
1. The initial assessment for the patient condition would require the medical history and
physical examinations within the 24 hours of reporting to the Emergency unit.
2. Another assessment required in this case would be problem focused, which involves the
cause of problem, its level of endurance by the patient, the duration since he has been
feeling such symptoms etc. It would also involve the associated factors in patient’s
lifestyle and work conditions responsible for the incidence of underlying problem.
3. Emergency assessment will be done during the physiological crisis (Sushma, 2016).
4. Time lapsed assessment would be done after few months of the initial assessment for
comparing the patient’s health variables with those recorded during the hospitalization.
The assessment at Emergency unit would involve data collection, patient examination, interview,
organizing the collected data, validation and documentation of retrieved information (Gauer,
2013). This information helps in accurate diagnosis and conduct effective nursing interventions.
The patients having sepsis with deteriorating symptoms are assessed at Emergency Departments
through standard Clinical Tools like ABCDE systems (Ortego et al., 2015). The Abbreviation
stands for the terms Airways, Breathe, Circulation, Disability and Exposure (Ortego et al., 2015).
Nur331 Complex care – Assessment Task 1B 4
Peters is awake, so there is reduced need to conduct the Airway Assessment. However, to
compensate the reduced Oxygen saturation in blood, the Oxygen can be administered. Breathing
assessment would identify the Respiratory Rate which is high in this case. Peters is in
Hypoxemia. Therefore it is recommended to administer bronchodilators and oxygen therapy
(Sushma, 2016). The assessment of circulation would identify the blood flow and Heart rate. The
patient may be assessed for skin color whether pale or faded. If the signs show worsening effect,
an Echocardiogram is recommended. The patient may feel agitated, so his blood sugar level may
be checked (Jones et al, 2015). Glasgow Coma Score (GCS) Assessment may be used to assess
the conscious level (Jones et al., 2015).
Patient should be checked for infection and its presence from head to toe. Peters has wound in
left leg. Abdomen can be checked for absence of bowel sounds or distension. Any indwelling
devices if found should be removed from the site of infection. Vital signs should be measured
periodically and the patient should be monitored continuously.
Moreover, his lifestyle is sedentary and he is obese. He drinks around 6 stubbies of beer during
night and smokes 1 packet of cigarettes in a day. He is doing this since last 30 years. He does
very little exercise however his job as a factory worker requires him to stand on feet whole day.
He is alone as he is divorced and has no children. He has low level of education and is unable to
read properly.
Priorities of treatment
The patients of sepsis are at high risk of developing organ dysfunction and death (Loots, 2017).
To identify the source or causative organ for infection, the blood samples are collected for the
patient as earlier as possible prior to administration of antibiotics (Loots, 2017).
Initial Nursing Priorities of treatment during the first 1-2 hours of care at ED would be: (1) to
provide adequate oxygen through nasal oxygen and ventilation support; (2) to support the Blood
Pressure; (3) To provide antibiotic solution over the wound, and give injections for further
prevention of infection (4) Pharmacological Interventions to control temperature and pain.
Peters is awake, so there is reduced need to conduct the Airway Assessment. However, to
compensate the reduced Oxygen saturation in blood, the Oxygen can be administered. Breathing
assessment would identify the Respiratory Rate which is high in this case. Peters is in
Hypoxemia. Therefore it is recommended to administer bronchodilators and oxygen therapy
(Sushma, 2016). The assessment of circulation would identify the blood flow and Heart rate. The
patient may be assessed for skin color whether pale or faded. If the signs show worsening effect,
an Echocardiogram is recommended. The patient may feel agitated, so his blood sugar level may
be checked (Jones et al, 2015). Glasgow Coma Score (GCS) Assessment may be used to assess
the conscious level (Jones et al., 2015).
Patient should be checked for infection and its presence from head to toe. Peters has wound in
left leg. Abdomen can be checked for absence of bowel sounds or distension. Any indwelling
devices if found should be removed from the site of infection. Vital signs should be measured
periodically and the patient should be monitored continuously.
Moreover, his lifestyle is sedentary and he is obese. He drinks around 6 stubbies of beer during
night and smokes 1 packet of cigarettes in a day. He is doing this since last 30 years. He does
very little exercise however his job as a factory worker requires him to stand on feet whole day.
He is alone as he is divorced and has no children. He has low level of education and is unable to
read properly.
Priorities of treatment
The patients of sepsis are at high risk of developing organ dysfunction and death (Loots, 2017).
To identify the source or causative organ for infection, the blood samples are collected for the
patient as earlier as possible prior to administration of antibiotics (Loots, 2017).
Initial Nursing Priorities of treatment during the first 1-2 hours of care at ED would be: (1) to
provide adequate oxygen through nasal oxygen and ventilation support; (2) to support the Blood
Pressure; (3) To provide antibiotic solution over the wound, and give injections for further
prevention of infection (4) Pharmacological Interventions to control temperature and pain.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Nur331 Complex care – Assessment Task 1B 5
The patient requires immediate medical attention. The emergency nurses are the first
professionals who meet the patients in the hospital and interact with them (Dennison, 2016). The
Nurses would be accountable for the immediate assessment and management of the symptoms in
this case. They identify the issues with the patient’s health according to the predefined protocols
of the hospital and coordinate with the patient satisfaction and effective outcomes (Coopersmith,
2018).
The nurse would apply oxygen therapy to reduce hypoxia and maintain sufficient oxygen level in
the body by selecting correct flow rate and the device of delivery (WHO, 2012). The intervention
would aim to reduce the shortness of breath and maintain effective use of oxygen by the body
cells. Peters do not require intense administration of Oxygen therapy for prolonged duration
since is SPO2 is at the borderline.
The nurse can increase the IV flow of fluids to increase the BP and can administer medications
for that. To treat the wound with exudates and inflammation, the antibiotics and medications can
be applied after cleaning the wound. He may be given antibiotic injection to cure the wound.
Nurse may educate the patient regarding the management of wound and prevent sepsis in future.
He may be educated to follow a healthy lifestyle to reduce obesity and treat the low BP with non
pharmacological interventions at home. Nurse may asses the practice and cultural beliefs of
patient which may influence the adherence to medications and care (Coopersmith, 2018). Nurse
may discuss the concerns of the patient and can clarify his misunderstandings.
The patient needs to be educated and increased awareness about the potential implications of
taking alcohol and smoking regularly. The patient needs education to improve his living
standards by reducing the weight. He needs to include exercises and yoga in his daily routine,
along with healthy diet and proper balance of work and rest. His diet should be rich in calcium
and protein to support his job requirements where he need to stand whole day.
The pharmacological interventions for treating the pain and temperature would involve analgesic
like paracetamol and ibuprofen for the mild pain (Dennison, 2016). If the pain severity anyhow
increases, he may be given opioids (Dennison, 2016).
The patient requires immediate medical attention. The emergency nurses are the first
professionals who meet the patients in the hospital and interact with them (Dennison, 2016). The
Nurses would be accountable for the immediate assessment and management of the symptoms in
this case. They identify the issues with the patient’s health according to the predefined protocols
of the hospital and coordinate with the patient satisfaction and effective outcomes (Coopersmith,
2018).
The nurse would apply oxygen therapy to reduce hypoxia and maintain sufficient oxygen level in
the body by selecting correct flow rate and the device of delivery (WHO, 2012). The intervention
would aim to reduce the shortness of breath and maintain effective use of oxygen by the body
cells. Peters do not require intense administration of Oxygen therapy for prolonged duration
since is SPO2 is at the borderline.
The nurse can increase the IV flow of fluids to increase the BP and can administer medications
for that. To treat the wound with exudates and inflammation, the antibiotics and medications can
be applied after cleaning the wound. He may be given antibiotic injection to cure the wound.
Nurse may educate the patient regarding the management of wound and prevent sepsis in future.
He may be educated to follow a healthy lifestyle to reduce obesity and treat the low BP with non
pharmacological interventions at home. Nurse may asses the practice and cultural beliefs of
patient which may influence the adherence to medications and care (Coopersmith, 2018). Nurse
may discuss the concerns of the patient and can clarify his misunderstandings.
The patient needs to be educated and increased awareness about the potential implications of
taking alcohol and smoking regularly. The patient needs education to improve his living
standards by reducing the weight. He needs to include exercises and yoga in his daily routine,
along with healthy diet and proper balance of work and rest. His diet should be rich in calcium
and protein to support his job requirements where he need to stand whole day.
The pharmacological interventions for treating the pain and temperature would involve analgesic
like paracetamol and ibuprofen for the mild pain (Dennison, 2016). If the pain severity anyhow
increases, he may be given opioids (Dennison, 2016).
Nur331 Complex care – Assessment Task 1B 6
The signs and symptoms of the sepsis patient should be identified early through proper
assessments at ED. The nurses need to adopt effective way of maintaining healthy trustworthy
relationship with the the patients so that the patients could follow their advice and adhere to the
instructions (Loots, 2017). The Nurses make the documentation and report on the basis of which
the doctors decide the treatment plan of the patient.
Sepsis may take the form of life threatening condition if the symptoms are left unnoticed and
untreated (WHO, 2012). The leg of the patient can be further infected transmitting the infection
to other internal organs. The condition may influence the circulatory system of the body
lowering down the blood pressure suddenly further affecting the functioning of multiple organs
of the body. The condition is called as Septic shock.
Most common bacterial sources of infection in sepsis are Streptococcus pneumonia, S.pyogenes,
Staphylococcus aureus, and E.coli (Sushma, 2016). Sepsis can also be cause by the less common
microbes like Klebseilla, Anaerobes, and fungus (Ortego et al., 2015). Wound infection is one of
the major causes of sepsis (National Guideline Centre (UK), 2016). Wound healing is very
important part of tissue restoration after the infection. The complications like delayed healing
and disruption can pose serious issues for the patient.
The inflammation in sepsis is mediated by the increased production of acute phase proteins
known as inflammatory cytokines (Jones et al., 2015). Wound healing demands sufficient
nutrient supply in the body. Thus patient should be given adequate nutrition. Proper wound
cleansing should be done while adequate hydration and nutrition should be maintained. Systemic
treatments would necessitate the intake of oral antibiotics along with local infection control
protocols. Topical antibiotics may be used to treat localized infection. Debridement should be
done to remove the devitalized tissue and green debris because these things lower down the
process of healing (Wound source, 2019).
.
Discharge Planning
The signs and symptoms of the sepsis patient should be identified early through proper
assessments at ED. The nurses need to adopt effective way of maintaining healthy trustworthy
relationship with the the patients so that the patients could follow their advice and adhere to the
instructions (Loots, 2017). The Nurses make the documentation and report on the basis of which
the doctors decide the treatment plan of the patient.
Sepsis may take the form of life threatening condition if the symptoms are left unnoticed and
untreated (WHO, 2012). The leg of the patient can be further infected transmitting the infection
to other internal organs. The condition may influence the circulatory system of the body
lowering down the blood pressure suddenly further affecting the functioning of multiple organs
of the body. The condition is called as Septic shock.
Most common bacterial sources of infection in sepsis are Streptococcus pneumonia, S.pyogenes,
Staphylococcus aureus, and E.coli (Sushma, 2016). Sepsis can also be cause by the less common
microbes like Klebseilla, Anaerobes, and fungus (Ortego et al., 2015). Wound infection is one of
the major causes of sepsis (National Guideline Centre (UK), 2016). Wound healing is very
important part of tissue restoration after the infection. The complications like delayed healing
and disruption can pose serious issues for the patient.
The inflammation in sepsis is mediated by the increased production of acute phase proteins
known as inflammatory cytokines (Jones et al., 2015). Wound healing demands sufficient
nutrient supply in the body. Thus patient should be given adequate nutrition. Proper wound
cleansing should be done while adequate hydration and nutrition should be maintained. Systemic
treatments would necessitate the intake of oral antibiotics along with local infection control
protocols. Topical antibiotics may be used to treat localized infection. Debridement should be
done to remove the devitalized tissue and green debris because these things lower down the
process of healing (Wound source, 2019).
.
Discharge Planning
Nur331 Complex care – Assessment Task 1B 7
As per the Social Justice Framework, the discharge planning for Peters should involve four basic
steps: Assessment of patient, Discharge plan development, Service provision including the
family and patient education and referrals, and follow up evaluation (Yam, 2012).
The assessment of Peter’s physiological, cultural, psychological and social needs should be done
in first stage. Peters is divorced and lives alone. He has no children. Peters may be talked about
his other family members and the family support that he can assess during his home stay.
A list of medications would be there in the discharge sheet that Peters has to take regularly for a
specific period of time. The medicines would be to treat pain, infection, swelling, and prevent the
blood clotting. The patient would be educated to take care of his wound and body, to adopt
healthy lifestyle, daily exercise, balanced diet, adequate rest while coming back home from job,
and drink enough fluids. He needs to call the physician if he finds that the condition anyhow
deteriorates further.
The cause of sepsis as identified in the interview was during the fishing. The patient would be
directed to take precautions from those potential causes of infection to prevent recurrence. He
would be told about the follow up appointments after one week and the tests he need to get done
after one month, to reassess the implications of infection in long term.
He would need home care, so he should take help of any family members to help him at home
after discharge in management of his daily routine care and wound cleaning. He does not need
any extra services like physical or occupational services, as the wound would heal, he would be
better in his health and can resume work. He should restrict the intense physical activities and
standing whole day during the job, at least for one month to allow complete healing and infection
control. Peters need to watch for the complications in future, associated with similar symptoms
like fever, pain in wound, fatigue etc and should report to the doctor immediately. He need to
restrict the alcohol and smoking.
As during discharge, he is having no pain, Peters should take pain medicines only when he feels
pain. Self care at home would require wound caring, cleansing with the ointment and antibiotic
fluid provided by the hospital, and tie a clean bandage on it every time after cleaning. If the
wound does not heal for 10 days more, Peters should report to the doctor.
As per the Social Justice Framework, the discharge planning for Peters should involve four basic
steps: Assessment of patient, Discharge plan development, Service provision including the
family and patient education and referrals, and follow up evaluation (Yam, 2012).
The assessment of Peter’s physiological, cultural, psychological and social needs should be done
in first stage. Peters is divorced and lives alone. He has no children. Peters may be talked about
his other family members and the family support that he can assess during his home stay.
A list of medications would be there in the discharge sheet that Peters has to take regularly for a
specific period of time. The medicines would be to treat pain, infection, swelling, and prevent the
blood clotting. The patient would be educated to take care of his wound and body, to adopt
healthy lifestyle, daily exercise, balanced diet, adequate rest while coming back home from job,
and drink enough fluids. He needs to call the physician if he finds that the condition anyhow
deteriorates further.
The cause of sepsis as identified in the interview was during the fishing. The patient would be
directed to take precautions from those potential causes of infection to prevent recurrence. He
would be told about the follow up appointments after one week and the tests he need to get done
after one month, to reassess the implications of infection in long term.
He would need home care, so he should take help of any family members to help him at home
after discharge in management of his daily routine care and wound cleaning. He does not need
any extra services like physical or occupational services, as the wound would heal, he would be
better in his health and can resume work. He should restrict the intense physical activities and
standing whole day during the job, at least for one month to allow complete healing and infection
control. Peters need to watch for the complications in future, associated with similar symptoms
like fever, pain in wound, fatigue etc and should report to the doctor immediately. He need to
restrict the alcohol and smoking.
As during discharge, he is having no pain, Peters should take pain medicines only when he feels
pain. Self care at home would require wound caring, cleansing with the ointment and antibiotic
fluid provided by the hospital, and tie a clean bandage on it every time after cleaning. If the
wound does not heal for 10 days more, Peters should report to the doctor.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Nur331 Complex care – Assessment Task 1B 8
The patients of sepsis may get readmissions due to another acute condition after 15 days of
discharge (Ortego et al., 2015). Therefore Peters should adhere to all the instructions written in
discharge slip to prevent high risk conditions.
References
Coopersmith,C. (2018). Surviving sepsis campaign: research priorities for sepsis and septic
shock. Intensive Care Medicine. 44(9). 1400-1426. DOI: https://doi.org/10.1007/s00134-018-
5175-z
WHO (2012). Guidelines on the Pharmacological Treatment of Persisting Pain in Children with
Medical Illnesses. Available from: https://www.ncbi.nlm.nih.gov/books/NBK138349/
Dennison, C.R.(2016). Expanding the Role of Nurses to Improve Hypertension Care and Control
Globally. 82(2). 243-253. https://doi.org/10.1016/j.aogh.2016.02.003
Gauer, R.L.(2013). Early Recognition and Management of Sepsis in Adults: The First Six Hours
. Am Fam Physician. 88(1). 44-53. Available from https://www.aafp.org/afp/2013/0701/p44.html
Jones, T. K., Fuchs, B. D., Small, D. S., Halpern, S. D., Hanish, A., Umscheid, C. A., …
Mikkelsen, M. E. (2015). Post-Acute Care Use and Hospital Readmission after Sepsis. Annals of
the American Thoracic Society, 12(6), 904–913. doi:10.1513/AnnalsATS.201411-504OC
Loots, F. J., Arpots, R., van den Berg, R., Hopstaken, R. M., Giesen, P., & Smits, M. (2017).
Recognition of sepsis in primary care: a survey among GPs. BJGP open, 1(2),
bjgpopen17X100965. doi:10.3399/bjgpopen17X100965
National Guideline Centre (UK) (2016). Sepsis: Recognition, Assessment and Early
Management. Available from: https://www.ncbi.nlm.nih.gov/books/NBK385343/
The patients of sepsis may get readmissions due to another acute condition after 15 days of
discharge (Ortego et al., 2015). Therefore Peters should adhere to all the instructions written in
discharge slip to prevent high risk conditions.
References
Coopersmith,C. (2018). Surviving sepsis campaign: research priorities for sepsis and septic
shock. Intensive Care Medicine. 44(9). 1400-1426. DOI: https://doi.org/10.1007/s00134-018-
5175-z
WHO (2012). Guidelines on the Pharmacological Treatment of Persisting Pain in Children with
Medical Illnesses. Available from: https://www.ncbi.nlm.nih.gov/books/NBK138349/
Dennison, C.R.(2016). Expanding the Role of Nurses to Improve Hypertension Care and Control
Globally. 82(2). 243-253. https://doi.org/10.1016/j.aogh.2016.02.003
Gauer, R.L.(2013). Early Recognition and Management of Sepsis in Adults: The First Six Hours
. Am Fam Physician. 88(1). 44-53. Available from https://www.aafp.org/afp/2013/0701/p44.html
Jones, T. K., Fuchs, B. D., Small, D. S., Halpern, S. D., Hanish, A., Umscheid, C. A., …
Mikkelsen, M. E. (2015). Post-Acute Care Use and Hospital Readmission after Sepsis. Annals of
the American Thoracic Society, 12(6), 904–913. doi:10.1513/AnnalsATS.201411-504OC
Loots, F. J., Arpots, R., van den Berg, R., Hopstaken, R. M., Giesen, P., & Smits, M. (2017).
Recognition of sepsis in primary care: a survey among GPs. BJGP open, 1(2),
bjgpopen17X100965. doi:10.3399/bjgpopen17X100965
National Guideline Centre (UK) (2016). Sepsis: Recognition, Assessment and Early
Management. Available from: https://www.ncbi.nlm.nih.gov/books/NBK385343/
Nur331 Complex care – Assessment Task 1B 9
Ortego, A., Gaieski, D. F., Fuchs, B. D., Jones, T., Halpern, S. D., Small, D. S., … Mikkelsen,
M. E. (2015). Hospital-based acute care use in survivors of septic shock. Critical care
medicine, 43(4), 729–737. doi:10.1097/CCM.0000000000000693
Sushma,S.(2016). IDENTIFYING AND ASSESSING PATIENT’S SEPSIS BY NURSES IN
AN EMERGENCY DEPARTMENT: A Literature Review. Available from
https://pdfs.semanticscholar.org/5f6b/ae4b7da43287d43fea14edf73fb0ca4b5bbf.pdf
Wound Source(2019). Infected wounds. Available from
https://www.woundsource.com/patientcondition/infected-wounds
Yam (2012). Framework and components for effective discharge planning system: a delphi
methodology. BMC Health Services Researchvolume 12, Article number: 396 (2012) . Available
from https://bmchealthservres.biomedcentral.com/articles/10.1186/1472-6963-12-396
Ortego, A., Gaieski, D. F., Fuchs, B. D., Jones, T., Halpern, S. D., Small, D. S., … Mikkelsen,
M. E. (2015). Hospital-based acute care use in survivors of septic shock. Critical care
medicine, 43(4), 729–737. doi:10.1097/CCM.0000000000000693
Sushma,S.(2016). IDENTIFYING AND ASSESSING PATIENT’S SEPSIS BY NURSES IN
AN EMERGENCY DEPARTMENT: A Literature Review. Available from
https://pdfs.semanticscholar.org/5f6b/ae4b7da43287d43fea14edf73fb0ca4b5bbf.pdf
Wound Source(2019). Infected wounds. Available from
https://www.woundsource.com/patientcondition/infected-wounds
Yam (2012). Framework and components for effective discharge planning system: a delphi
methodology. BMC Health Services Researchvolume 12, Article number: 396 (2012) . Available
from https://bmchealthservres.biomedcentral.com/articles/10.1186/1472-6963-12-396
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





