Navigating Complexity in Patient Journeys
VerifiedAdded on 2019/11/29
|20
|3481
|236
Report
AI Summary
The case study highlights the challenges faced by Aboriginal patients in receiving healthcare services due to lack of responsive and flexible arrangements. Patients from rural areas need to travel long distances for hospital care, leading to poor health outcomes. The study emphasizes the importance of having a centre that provides specific information and services to support patient care. It also suggests that two approaches can be taken to manage complexity: planning and responsive approach, which involves predicting patient journeys and providing immediate responses; and managing problems and prices as they occur. The assignment highlights the need for coordination and tailored responses in healthcare services, particularly for Aboriginal patients.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: NURSING
Patient journey mapping
Name of the student:
Name of the university:
Author Note:
Patient journey mapping
Name of the student:
Name of the university:
Author Note:
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1NURSING
2NURSING
Patient journey mapping template
Introduction
The patient journey mapping is a type of a framework which is developed to analyse the model of health of aboriginal patients. This
framework is to identify the factors which affect all the needs of the aboriginal patients from Torres Strait Island. It is the interaction of the
factors which a country person is experiencing during the illness with the City Hospital in an aboriginal country.
Content
Narrative
A middle-aged man from Aborigine and Torres-strait Island is an employee in a local organization on a low pay, having 2 ceaseless
conditions which requires progressing care. That man was attended by the neighbourhood General Physician to see an expert in the city of
Adelaide for his increasing back pain. The time when he went to the Adelaide hospital (an excruciating five-hour travel every way), the doctor to
whom he was referred prompted that he required an alternate doctor and refused for his check up. Following a couple of months he came back to
Adelaide and, the second specialist recommended he have an X-ray (attractive reverberation imaging) examine (another trip) at that point return
for a moment conference (another outing). On each event the man and his accomplice flew out to Adelaide and return on the same day. They
didn't remain overnight in light of the fact that they had no family nearby, couldn't stand to pay for convenience and couldn't manage the cost of
Patient journey mapping template
Introduction
The patient journey mapping is a type of a framework which is developed to analyse the model of health of aboriginal patients. This
framework is to identify the factors which affect all the needs of the aboriginal patients from Torres Strait Island. It is the interaction of the
factors which a country person is experiencing during the illness with the City Hospital in an aboriginal country.
Content
Narrative
A middle-aged man from Aborigine and Torres-strait Island is an employee in a local organization on a low pay, having 2 ceaseless
conditions which requires progressing care. That man was attended by the neighbourhood General Physician to see an expert in the city of
Adelaide for his increasing back pain. The time when he went to the Adelaide hospital (an excruciating five-hour travel every way), the doctor to
whom he was referred prompted that he required an alternate doctor and refused for his check up. Following a couple of months he came back to
Adelaide and, the second specialist recommended he have an X-ray (attractive reverberation imaging) examine (another trip) at that point return
for a moment conference (another outing). On each event the man and his accomplice flew out to Adelaide and return on the same day. They
didn't remain overnight in light of the fact that they had no family nearby, couldn't stand to pay for convenience and couldn't manage the cost of

3NURSING
something beyond than one day away from work. The patient arranged mid-evening arrangements to enable time to drive to Adelaide and back
around the same time.
Despite the fact that accounts were tight, at one phase this patient chose to utilize the private wellbeing framework keeping in mind the
end goal to get human services and help from the pain more rapidly. He had an operation also, was returned home. After a month he returned via
auto for a subsequent MRI scan and pro visit. The expert verified that he required a second time operation, for which the patient had returned. A
subsequent MRI demonstrated issues that required additionally audit. The patient depicted the 'truly terrible' agony he encountered on these
rehashed trips. The specialist gave him content for torment help prescription and instructed him to take it as required.
The man did not understand he could progress toward becoming dependent on this prescription and saw the nearby GP for rehash
solutions as the outings and agony proceeded. The nearby GP did not have a considerable measure of time to spend on every counsel (there was
a GP deficiency in his district; the patient stated, 'you simply go in and out, not a ton of looking up') and these remedies proceeded for a few
months. The man felt that the authority specialists did not clarify or talk about his condition, treatment or drugs unmistakably and he found the
visits to experts threatening. Amid admission to the private healing centre he turned out to be forlorn. Staff given physical care instantly after the
operation, yet diminished their cooperation once the quiet was more portable. There were no AHLOs or, on the other hand Aboriginal staff in the
private framework. A family part remained with a cousin in the northern rural areas and went by amid the day. The rehashed treks to Adelaide
were time consuming and, filled with pain. The extra endless condition required costly prescriptions. The persistent turned out to be
something beyond than one day away from work. The patient arranged mid-evening arrangements to enable time to drive to Adelaide and back
around the same time.
Despite the fact that accounts were tight, at one phase this patient chose to utilize the private wellbeing framework keeping in mind the
end goal to get human services and help from the pain more rapidly. He had an operation also, was returned home. After a month he returned via
auto for a subsequent MRI scan and pro visit. The expert verified that he required a second time operation, for which the patient had returned. A
subsequent MRI demonstrated issues that required additionally audit. The patient depicted the 'truly terrible' agony he encountered on these
rehashed trips. The specialist gave him content for torment help prescription and instructed him to take it as required.
The man did not understand he could progress toward becoming dependent on this prescription and saw the nearby GP for rehash
solutions as the outings and agony proceeded. The nearby GP did not have a considerable measure of time to spend on every counsel (there was
a GP deficiency in his district; the patient stated, 'you simply go in and out, not a ton of looking up') and these remedies proceeded for a few
months. The man felt that the authority specialists did not clarify or talk about his condition, treatment or drugs unmistakably and he found the
visits to experts threatening. Amid admission to the private healing centre he turned out to be forlorn. Staff given physical care instantly after the
operation, yet diminished their cooperation once the quiet was more portable. There were no AHLOs or, on the other hand Aboriginal staff in the
private framework. A family part remained with a cousin in the northern rural areas and went by amid the day. The rehashed treks to Adelaide
were time consuming and, filled with pain. The extra endless condition required costly prescriptions. The persistent turned out to be
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4NURSING
progressively discouraged and one day endeavoured suicide, yet fortunately a family part happened to be adjacent and interceded. Together they
returned home and rang the psychological well-being line. The patient found the Rural also, Remote Mental Health Service (RRMHS) workers
extremely steady and took after their proposal that he be admitted to the closest doctor's facility, with the RRMHS group working with the
neighbourhood emotional well-being group to encourage this. The affirmation procedure was exceptionally smooth; the tolerant mirrored that
without this help he may have been sitting tight in crisis for quite a long time. A video chat was sorted out with an Adelaide therapist at RRMHS
and he valued the conversation with somebody whom he didn't know and who was not a relative. This patient is presently going to the
neighbourhood Aboriginal wellbeing administration, where he is looked after by a GP as well as by Aboriginal medical attendants and wellbeing
workers. He had not utilized this administration already, accepting that it was for social insurance card-holders as it were. The Native wellbeing
administration GP arranges his aggregate medicinal services, and clarifies inside and out about medications furthermore, treatment. The patient
has effectively pulled back from the opiates and qualities the facilitated medicinal services he gets for all his wellbeing concerns.
progressively discouraged and one day endeavoured suicide, yet fortunately a family part happened to be adjacent and interceded. Together they
returned home and rang the psychological well-being line. The patient found the Rural also, Remote Mental Health Service (RRMHS) workers
extremely steady and took after their proposal that he be admitted to the closest doctor's facility, with the RRMHS group working with the
neighbourhood emotional well-being group to encourage this. The affirmation procedure was exceptionally smooth; the tolerant mirrored that
without this help he may have been sitting tight in crisis for quite a long time. A video chat was sorted out with an Adelaide therapist at RRMHS
and he valued the conversation with somebody whom he didn't know and who was not a relative. This patient is presently going to the
neighbourhood Aboriginal wellbeing administration, where he is looked after by a GP as well as by Aboriginal medical attendants and wellbeing
workers. He had not utilized this administration already, accepting that it was for social insurance card-holders as it were. The Native wellbeing
administration GP arranges his aggregate medicinal services, and clarifies inside and out about medications furthermore, treatment. The patient
has effectively pulled back from the opiates and qualities the facilitated medicinal services he gets for all his wellbeing concerns.
5NURSING
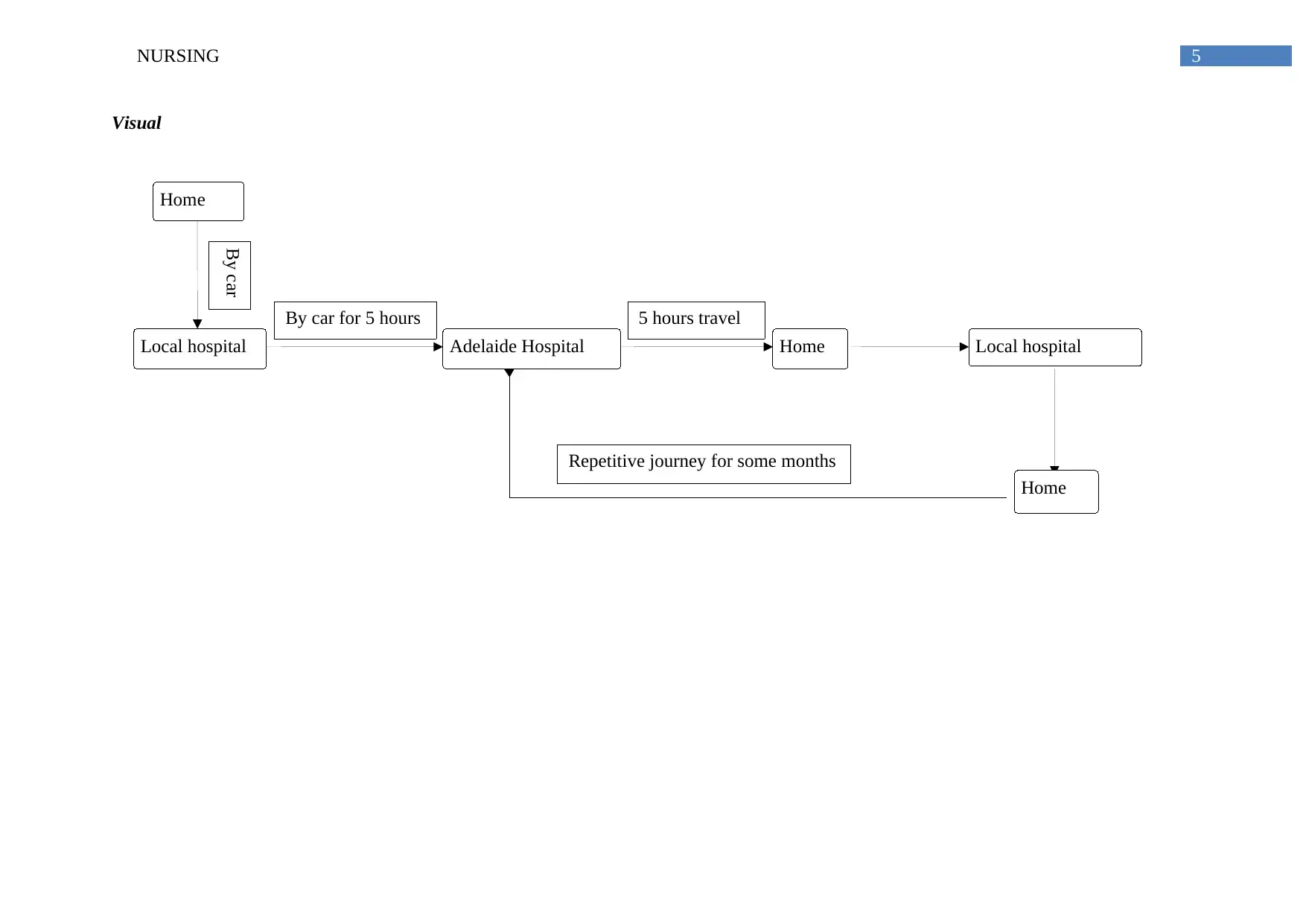
Visual
Local hospital
Home
Adelaide Hospital Home Local hospital
By car
By car for 5 hours 5 hours travel
Home
Repetitive journey for some months
Visual
Local hospital
Home
Adelaide Hospital Home Local hospital
By car
By car for 5 hours 5 hours travel
Home
Repetitive journey for some months
6NURSING
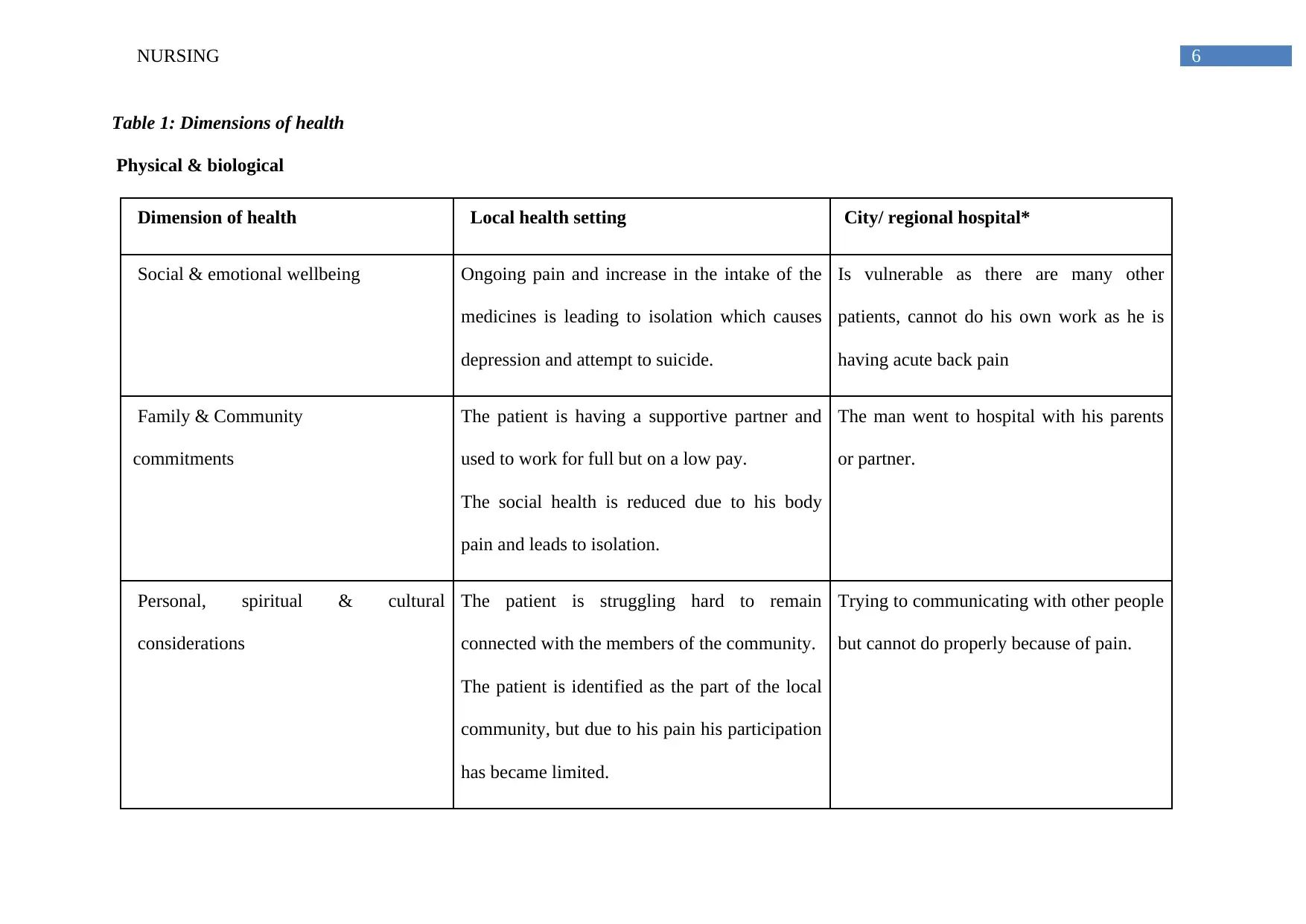
Table 1: Dimensions of health
Physical & biological
Dimension of health Local health setting City/ regional hospital*
Social & emotional wellbeing Ongoing pain and increase in the intake of the
medicines is leading to isolation which causes
depression and attempt to suicide.
Is vulnerable as there are many other
patients, cannot do his own work as he is
having acute back pain
Family & Community
commitments
The patient is having a supportive partner and
used to work for full but on a low pay.
The social health is reduced due to his body
pain and leads to isolation.
The man went to hospital with his parents
or partner.
Personal, spiritual & cultural
considerations
The patient is struggling hard to remain
connected with the members of the community.
The patient is identified as the part of the local
community, but due to his pain his participation
has became limited.
Trying to communicating with other people
but cannot do properly because of pain.
Table 1: Dimensions of health
Physical & biological
Dimension of health Local health setting City/ regional hospital*
Social & emotional wellbeing Ongoing pain and increase in the intake of the
medicines is leading to isolation which causes
depression and attempt to suicide.
Is vulnerable as there are many other
patients, cannot do his own work as he is
having acute back pain
Family & Community
commitments
The patient is having a supportive partner and
used to work for full but on a low pay.
The social health is reduced due to his body
pain and leads to isolation.
The man went to hospital with his parents
or partner.
Personal, spiritual & cultural
considerations
The patient is struggling hard to remain
connected with the members of the community.
The patient is identified as the part of the local
community, but due to his pain his participation
has became limited.
Trying to communicating with other people
but cannot do properly because of pain.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7NURSING
Physical & biological Ongoing back pain and additional chronic
condition and drug dependence.
The patient is travelling for long distances,
which is very painful for the patient
Not eating properly
Anxious for the operation
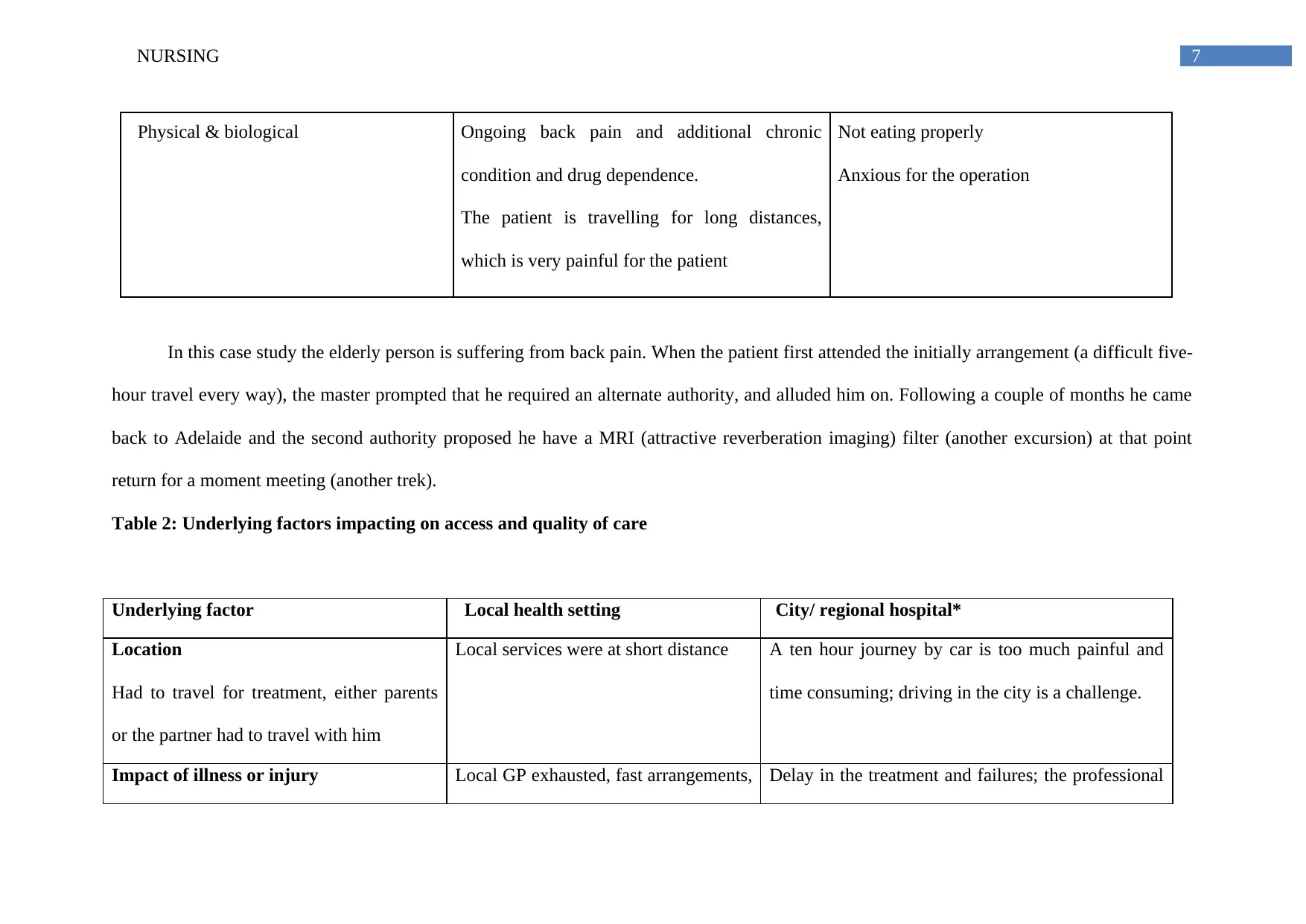
In this case study the elderly person is suffering from back pain. When the patient first attended the initially arrangement (a difficult five-
hour travel every way), the master prompted that he required an alternate authority, and alluded him on. Following a couple of months he came
back to Adelaide and the second authority proposed he have a MRI (attractive reverberation imaging) filter (another excursion) at that point
return for a moment meeting (another trek).
Table 2: Underlying factors impacting on access and quality of care
Underlying factor Local health setting City/ regional hospital*
Location
Had to travel for treatment, either parents
or the partner had to travel with him
Local services were at short distance A ten hour journey by car is too much painful and
time consuming; driving in the city is a challenge.
Impact of illness or injury Local GP exhausted, fast arrangements, Delay in the treatment and failures; the professional
Physical & biological Ongoing back pain and additional chronic
condition and drug dependence.
The patient is travelling for long distances,
which is very painful for the patient
Not eating properly
Anxious for the operation
In this case study the elderly person is suffering from back pain. When the patient first attended the initially arrangement (a difficult five-
hour travel every way), the master prompted that he required an alternate authority, and alluded him on. Following a couple of months he came
back to Adelaide and the second authority proposed he have a MRI (attractive reverberation imaging) filter (another excursion) at that point
return for a moment meeting (another trek).
Table 2: Underlying factors impacting on access and quality of care
Underlying factor Local health setting City/ regional hospital*
Location
Had to travel for treatment, either parents
or the partner had to travel with him
Local services were at short distance A ten hour journey by car is too much painful and
time consuming; driving in the city is a challenge.
Impact of illness or injury Local GP exhausted, fast arrangements, Delay in the treatment and failures; the professional
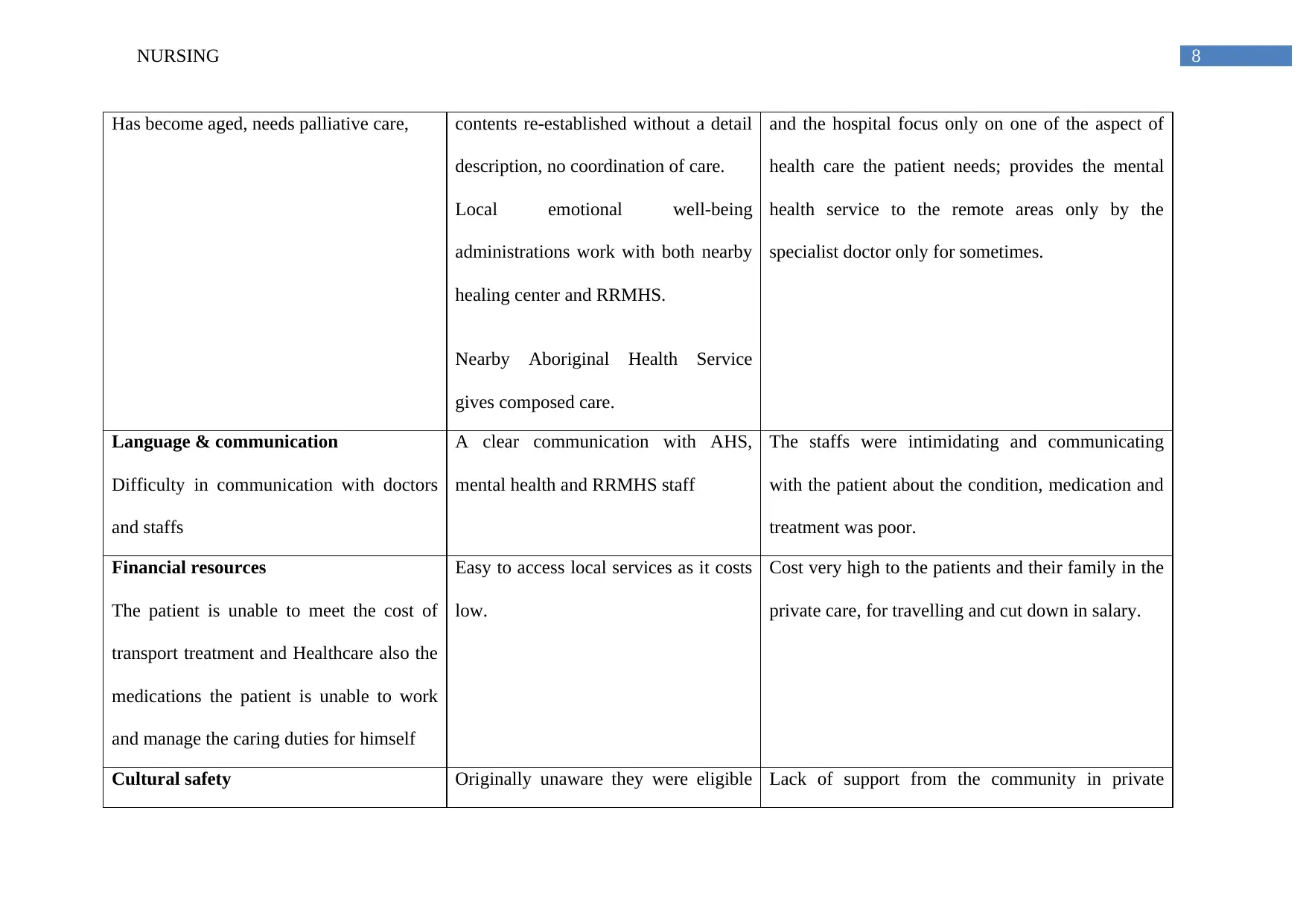
8NURSING
Has become aged, needs palliative care, contents re-established without a detail
description, no coordination of care.
Local emotional well-being
administrations work with both nearby
healing center and RRMHS.
Nearby Aboriginal Health Service
gives composed care.
and the hospital focus only on one of the aspect of
health care the patient needs; provides the mental
health service to the remote areas only by the
specialist doctor only for sometimes.
Language & communication
Difficulty in communication with doctors
and staffs
A clear communication with AHS,
mental health and RRMHS staff
The staffs were intimidating and communicating
with the patient about the condition, medication and
treatment was poor.
Financial resources
The patient is unable to meet the cost of
transport treatment and Healthcare also the
medications the patient is unable to work
and manage the caring duties for himself
Easy to access local services as it costs
low.
Cost very high to the patients and their family in the
private care, for travelling and cut down in salary.
Cultural safety Originally unaware they were eligible Lack of support from the community in private
Has become aged, needs palliative care, contents re-established without a detail
description, no coordination of care.
Local emotional well-being
administrations work with both nearby
healing center and RRMHS.
Nearby Aboriginal Health Service
gives composed care.
and the hospital focus only on one of the aspect of
health care the patient needs; provides the mental
health service to the remote areas only by the
specialist doctor only for sometimes.
Language & communication
Difficulty in communication with doctors
and staffs
A clear communication with AHS,
mental health and RRMHS staff
The staffs were intimidating and communicating
with the patient about the condition, medication and
treatment was poor.
Financial resources
The patient is unable to meet the cost of
transport treatment and Healthcare also the
medications the patient is unable to work
and manage the caring duties for himself
Easy to access local services as it costs
low.
Cost very high to the patients and their family in the
private care, for travelling and cut down in salary.
Cultural safety Originally unaware they were eligible Lack of support from the community in private
9NURSING
In the treatment of an aboriginal person is
ethics and culture safety must be
maintained
to use local Aboriginal health service.
Later AHS provided coordinated and
timely care.
hospital; lack of social interaction with staff.
We at that point considered how the five variables affected both locally and when he made a trip to the city for mind. The man felt that
the expert specialists did not clarify or talk about his condition, treatment or solutions unmistakably and he found the visits to pros scaring. Amid
admission to the private healing facility he turned out to be forlorn. Staff gave physical care instantly after the operation, however decreased
their communication once the patient was more versatile. There were no AHLOs or Aboriginal staff in the private framework. A relative
remained with a cousin in the northern rural areas and went to amid the day.
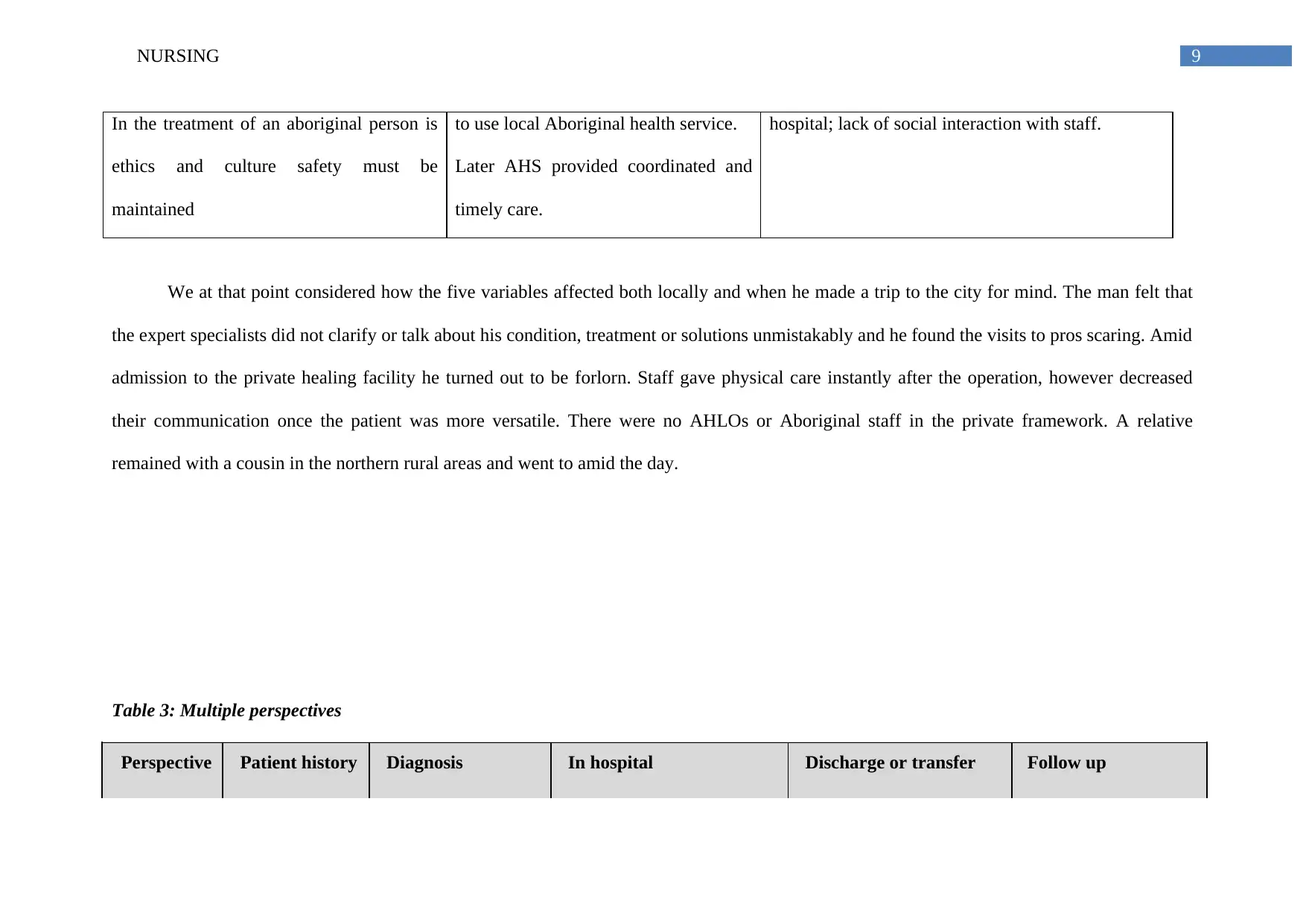
Table 3: Multiple perspectives
Perspective Patient history Diagnosis In hospital Discharge or transfer Follow up
In the treatment of an aboriginal person is
ethics and culture safety must be
maintained
to use local Aboriginal health service.
Later AHS provided coordinated and
timely care.
hospital; lack of social interaction with staff.
We at that point considered how the five variables affected both locally and when he made a trip to the city for mind. The man felt that
the expert specialists did not clarify or talk about his condition, treatment or solutions unmistakably and he found the visits to pros scaring. Amid
admission to the private healing facility he turned out to be forlorn. Staff gave physical care instantly after the operation, however decreased
their communication once the patient was more versatile. There were no AHLOs or Aboriginal staff in the private framework. A relative
remained with a cousin in the northern rural areas and went to amid the day.
Table 3: Multiple perspectives
Perspective Patient history Diagnosis In hospital Discharge or transfer Follow up
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
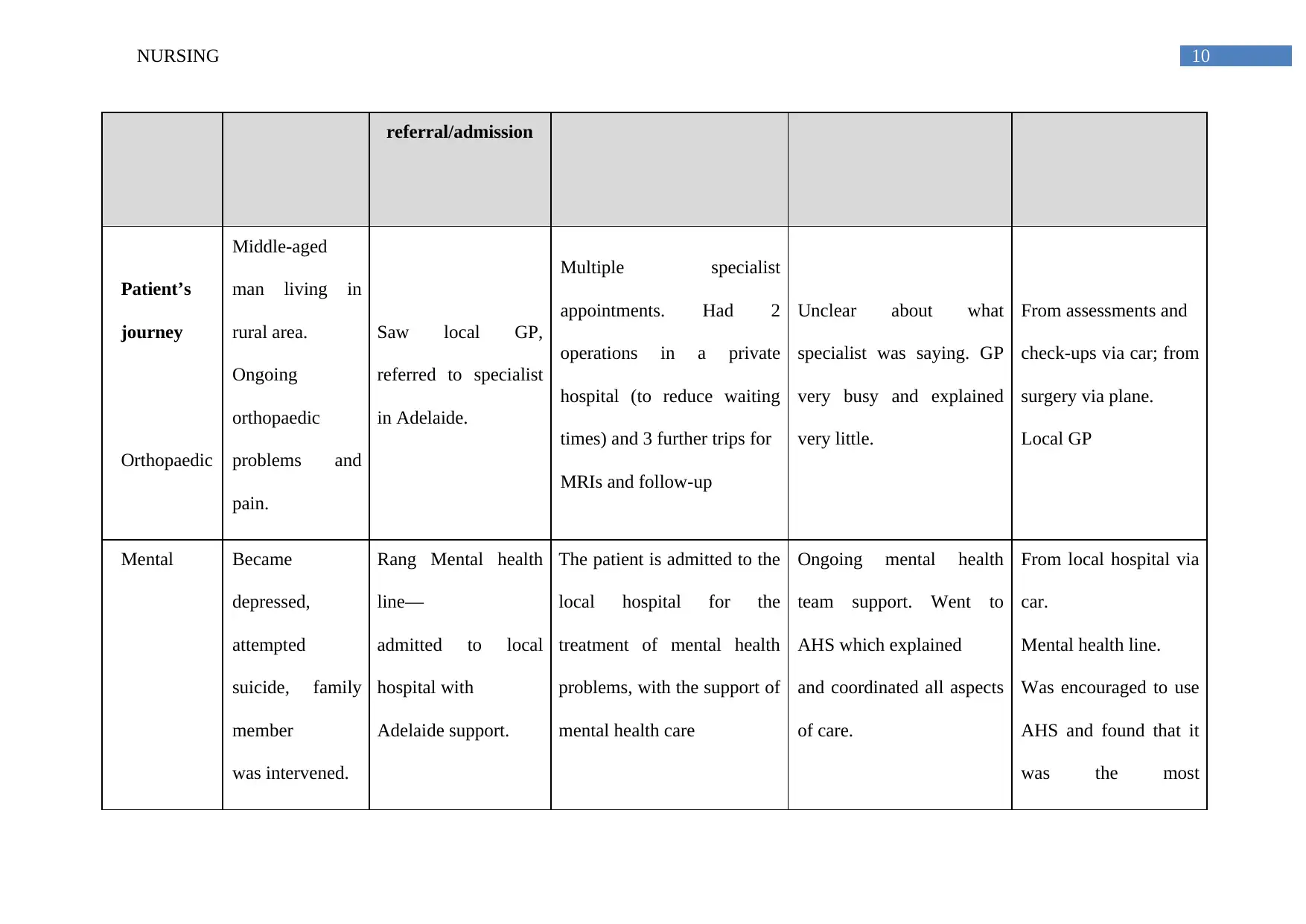
10NURSING
referral/admission
Patient’s
journey
Orthopaedic
Middle-aged
man living in
rural area.
Ongoing
orthopaedic
problems and
pain.
Saw local GP,
referred to specialist
in Adelaide.
Multiple specialist
appointments. Had 2
operations in a private
hospital (to reduce waiting
times) and 3 further trips for
MRIs and follow-up
Unclear about what
specialist was saying. GP
very busy and explained
very little.
From assessments and
check-ups via car; from
surgery via plane.
Local GP
Mental Became
depressed,
attempted
suicide, family
member
was intervened.
Rang Mental health
line—
admitted to local
hospital with
Adelaide support.
The patient is admitted to the
local hospital for the
treatment of mental health
problems, with the support of
mental health care
Ongoing mental health
team support. Went to
AHS which explained
and coordinated all aspects
of care.
From local hospital via
car.
Mental health line.
Was encouraged to use
AHS and found that it
was the most
referral/admission
Patient’s
journey
Orthopaedic
Middle-aged
man living in
rural area.
Ongoing
orthopaedic
problems and
pain.
Saw local GP,
referred to specialist
in Adelaide.
Multiple specialist
appointments. Had 2
operations in a private
hospital (to reduce waiting
times) and 3 further trips for
MRIs and follow-up
Unclear about what
specialist was saying. GP
very busy and explained
very little.
From assessments and
check-ups via car; from
surgery via plane.
Local GP
Mental Became
depressed,
attempted
suicide, family
member
was intervened.
Rang Mental health
line—
admitted to local
hospital with
Adelaide support.
The patient is admitted to the
local hospital for the
treatment of mental health
problems, with the support of
mental health care
Ongoing mental health
team support. Went to
AHS which explained
and coordinated all aspects
of care.
From local hospital via
car.
Mental health line.
Was encouraged to use
AHS and found that it
was the most
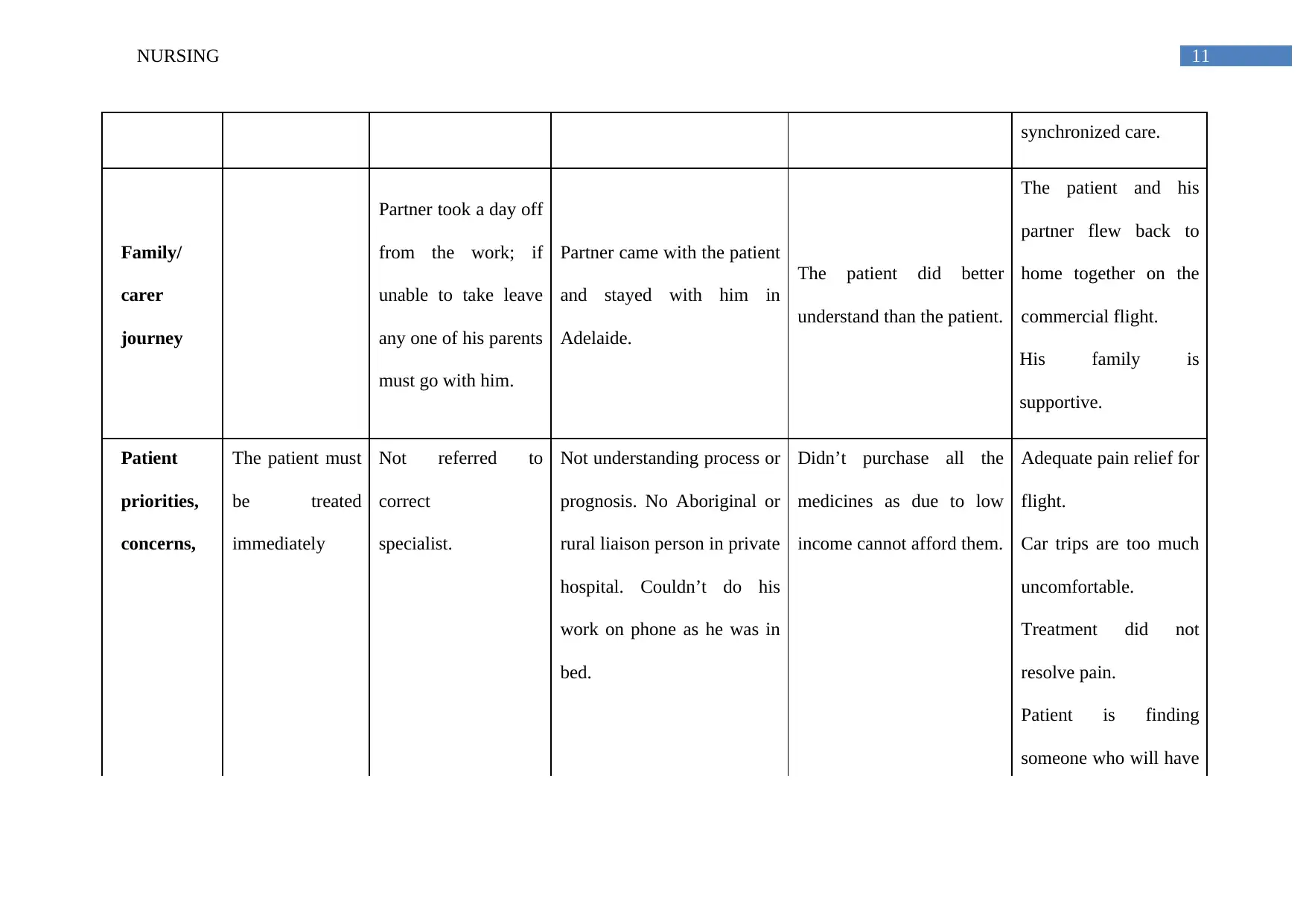
11NURSING
synchronized care.
Family/
carer
journey
Partner took a day off
from the work; if
unable to take leave
any one of his parents
must go with him.
Partner came with the patient
and stayed with him in
Adelaide.
The patient did better
understand than the patient.
The patient and his
partner flew back to
home together on the
commercial flight.
His family is
supportive.
Patient
priorities,
concerns,
The patient must
be treated
immediately
Not referred to
correct
specialist.
Not understanding process or
prognosis. No Aboriginal or
rural liaison person in private
hospital. Couldn’t do his
work on phone as he was in
bed.
Didn’t purchase all the
medicines as due to low
income cannot afford them.
Adequate pain relief for
flight.
Car trips are too much
uncomfortable.
Treatment did not
resolve pain.
Patient is finding
someone who will have
synchronized care.
Family/
carer
journey
Partner took a day off
from the work; if
unable to take leave
any one of his parents
must go with him.
Partner came with the patient
and stayed with him in
Adelaide.
The patient did better
understand than the patient.
The patient and his
partner flew back to
home together on the
commercial flight.
His family is
supportive.
Patient
priorities,
concerns,
The patient must
be treated
immediately
Not referred to
correct
specialist.
Not understanding process or
prognosis. No Aboriginal or
rural liaison person in private
hospital. Couldn’t do his
work on phone as he was in
bed.
Didn’t purchase all the
medicines as due to low
income cannot afford them.
Adequate pain relief for
flight.
Car trips are too much
uncomfortable.
Treatment did not
resolve pain.
Patient is finding
someone who will have
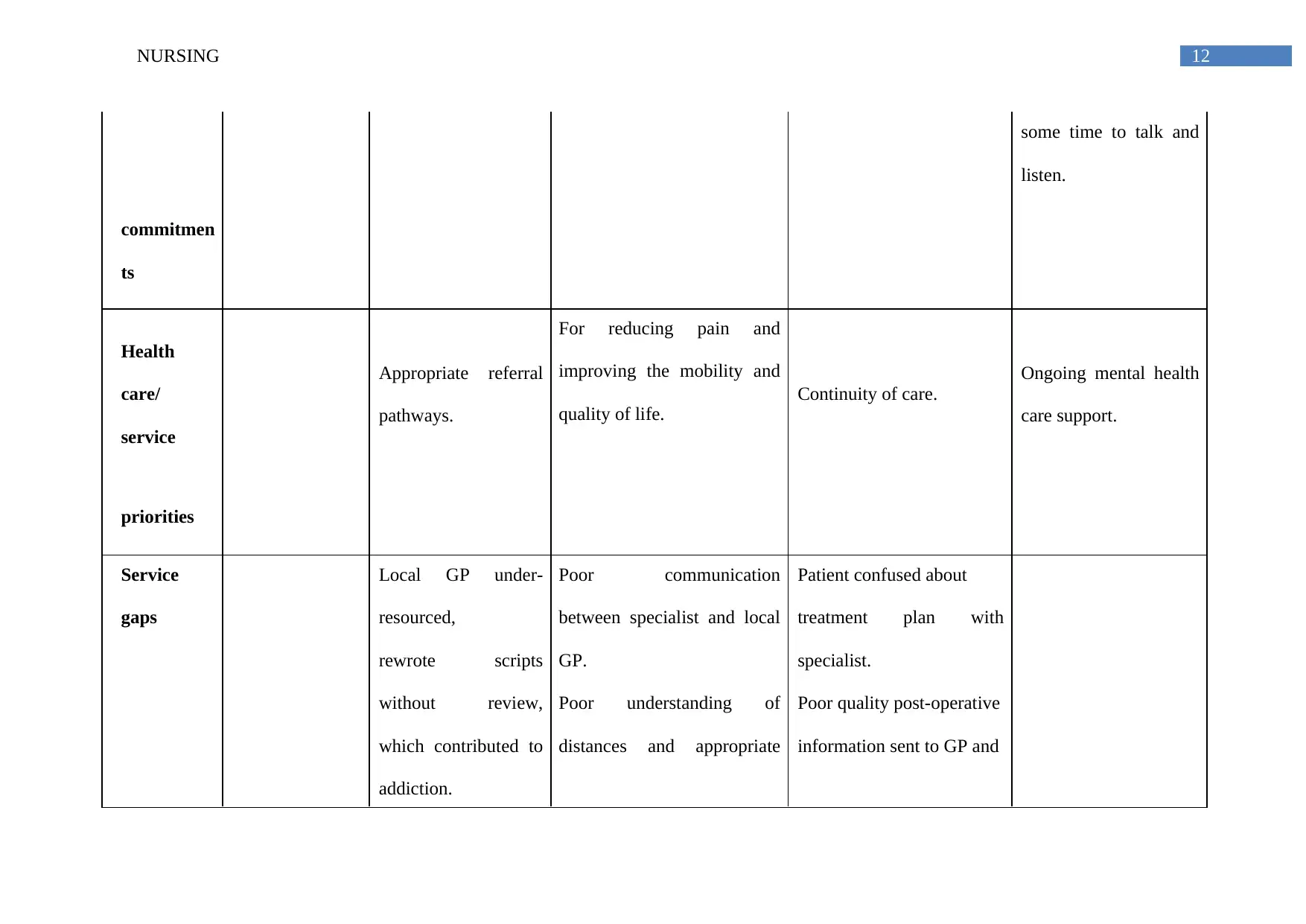
12NURSING
some time to talk and
listen.
commitmen
ts
Health
care/
service
Appropriate referral
pathways.
For reducing pain and
improving the mobility and
quality of life.
Continuity of care.
Ongoing mental health
care support.
priorities
Service
gaps
Local GP under-
resourced,
rewrote scripts
without review,
which contributed to
addiction.
Poor communication
between specialist and local
GP.
Poor understanding of
distances and appropriate
Patient confused about
treatment plan with
specialist.
Poor quality post-operative
information sent to GP and
some time to talk and
listen.
commitmen
ts
Health
care/
service
Appropriate referral
pathways.
For reducing pain and
improving the mobility and
quality of life.
Continuity of care.
Ongoing mental health
care support.
priorities
Service
gaps
Local GP under-
resourced,
rewrote scripts
without review,
which contributed to
addiction.
Poor communication
between specialist and local
GP.
Poor understanding of
distances and appropriate
Patient confused about
treatment plan with
specialist.
Poor quality post-operative
information sent to GP and
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
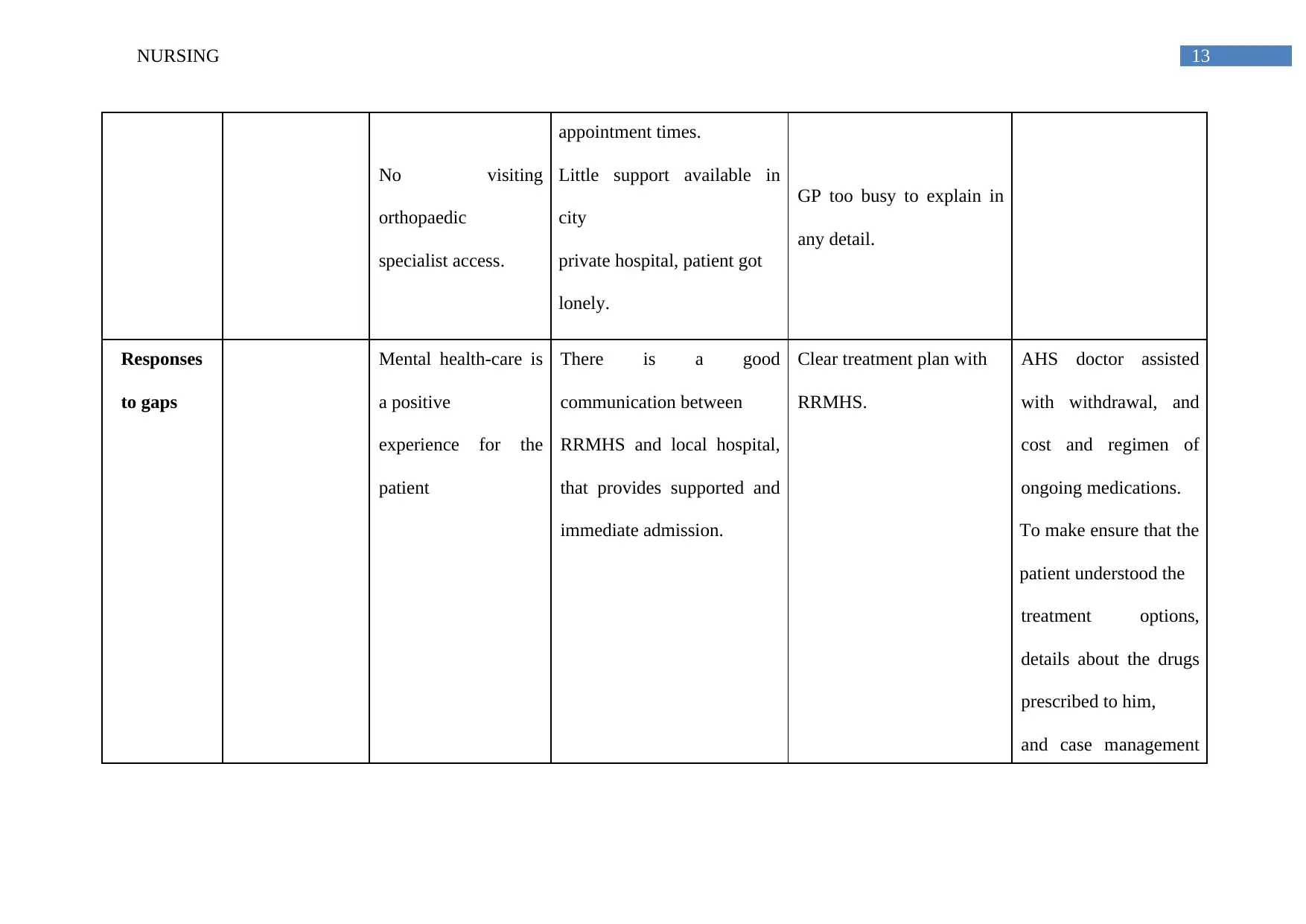
13NURSING
No visiting
orthopaedic
specialist access.
appointment times.
Little support available in
city
private hospital, patient got
lonely.
GP too busy to explain in
any detail.
Responses
to gaps
Mental health-care is
a positive
experience for the
patient
There is a good
communication between
RRMHS and local hospital,
that provides supported and
immediate admission.
Clear treatment plan with
RRMHS.
AHS doctor assisted
with withdrawal, and
cost and regimen of
ongoing medications.
To make ensure that the
patient understood the
treatment options,
details about the drugs
prescribed to him,
and case management
No visiting
orthopaedic
specialist access.
appointment times.
Little support available in
city
private hospital, patient got
lonely.
GP too busy to explain in
any detail.
Responses
to gaps
Mental health-care is
a positive
experience for the
patient
There is a good
communication between
RRMHS and local hospital,
that provides supported and
immediate admission.
Clear treatment plan with
RRMHS.
AHS doctor assisted
with withdrawal, and
cost and regimen of
ongoing medications.
To make ensure that the
patient understood the
treatment options,
details about the drugs
prescribed to him,
and case management
14NURSING
plans
Improvement plan:
There are 5 things which I want to improve for the indigenous patients. They are:
To provide access to the specialist care in regional centres and making arrangements for the outpatient so that they can accommodate the
people were travelling from long distances.
Helping them to use the technology so that they can reduce travel and delay in diagnosis and care
Providing the better support for the travel requirements and improving the interpersonal skills and knowledge among the hospital staff
Allowing them the better accommodations options in the City
Conclusion
The above assignment describes what are the strengths and weaknesses of the health system The case study highlighted that hospital and
support service arrangements which work well for the city patients and not so much responsive are flexible to respond to the aboriginal patients
when any country is aboriginal patients need the help of the hospital care they had to do a long journey on which becomes complex for them due
to the impact most of the time the patients are remain untreated and they leads to death. Although medical complexity of the city patients are
plans
Improvement plan:
There are 5 things which I want to improve for the indigenous patients. They are:
To provide access to the specialist care in regional centres and making arrangements for the outpatient so that they can accommodate the
people were travelling from long distances.
Helping them to use the technology so that they can reduce travel and delay in diagnosis and care
Providing the better support for the travel requirements and improving the interpersonal skills and knowledge among the hospital staff
Allowing them the better accommodations options in the City
Conclusion
The above assignment describes what are the strengths and weaknesses of the health system The case study highlighted that hospital and
support service arrangements which work well for the city patients and not so much responsive are flexible to respond to the aboriginal patients
when any country is aboriginal patients need the help of the hospital care they had to do a long journey on which becomes complex for them due
to the impact most of the time the patients are remain untreated and they leads to death. Although medical complexity of the city patients are
15NURSING
handled by the hospitals they become very narrow in case of the aboriginal patients this means that the patient without the needed care and can
experience poor quality also my face on necessary stress. the patients their families communities hospitals and the local country Health Services
used to be the financial cost of complexity of the aboriginal patients it is a very difficult problem which may require both the availability of
specific interventions and services to support the names of a patient it has been provided that there must be a centre who could spur provide the
specific information and services for implementing responses to the patient care. Although not all the other innovation triggers tailored responses
in complexity but in most of the cases it is usually expected study indicate that the complexity can be managed in two ways planning and
responsive approach which can predict the complexity and does immediate responses and second is by managing the problems and prices when
they occur.
In this, the first option is based on prediction and the preparation of the patient journey mainly the possibility that some of the patients
journey will become complex as compared to other patients. It could be found that the clinical units is established for preparing and responding
to the admission of the country and have aboriginal patients. It has been observed that every clinical unit have a specific number of aboriginal
patients that we cared for and each is having a specific coordinator who plays a part of the clinical team his rolls where to work with the hospital,
to take care of the primary health, to interpret and to provide the support services. Nation wellbeing administrations associated with these cases
considers were more probable than city administrations to pay thoughtfulness regarding tending to complexities all together to guarantee access
to the required watch over their patients.
handled by the hospitals they become very narrow in case of the aboriginal patients this means that the patient without the needed care and can
experience poor quality also my face on necessary stress. the patients their families communities hospitals and the local country Health Services
used to be the financial cost of complexity of the aboriginal patients it is a very difficult problem which may require both the availability of
specific interventions and services to support the names of a patient it has been provided that there must be a centre who could spur provide the
specific information and services for implementing responses to the patient care. Although not all the other innovation triggers tailored responses
in complexity but in most of the cases it is usually expected study indicate that the complexity can be managed in two ways planning and
responsive approach which can predict the complexity and does immediate responses and second is by managing the problems and prices when
they occur.
In this, the first option is based on prediction and the preparation of the patient journey mainly the possibility that some of the patients
journey will become complex as compared to other patients. It could be found that the clinical units is established for preparing and responding
to the admission of the country and have aboriginal patients. It has been observed that every clinical unit have a specific number of aboriginal
patients that we cared for and each is having a specific coordinator who plays a part of the clinical team his rolls where to work with the hospital,
to take care of the primary health, to interpret and to provide the support services. Nation wellbeing administrations associated with these cases
considers were more probable than city administrations to pay thoughtfulness regarding tending to complexities all together to guarantee access
to the required watch over their patients.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
16NURSING
Coordination of these complex trips is a continuous essential for good care. Not every Aboriginal patient who are admitted to city healing
facilities have critical extra expenses related with their pre-affirmation and post-release ventures. Consequently, a framework that reacts to
many-sided quality by expecting high expenses and complexities for all patients is liable to be wasteful. Rather, the ability to tailor reactions as
indicated by the anticipated complexities is required. In clinical units that treat critical quantities of nation Aboriginal patients, a committed
facilitator part (full-or low maintenance) is required. For clinical units that concede few nation Aboriginal patients, planning limit could live in
the doctor's facility based AHLO and additionally Aboriginal Understanding Pathway Officer group, gave that an distinguished individual from
the clinical unit group takes duty regarding correspondence and contact with those specialists.
Coordination of these complex trips is a continuous essential for good care. Not every Aboriginal patient who are admitted to city healing
facilities have critical extra expenses related with their pre-affirmation and post-release ventures. Consequently, a framework that reacts to
many-sided quality by expecting high expenses and complexities for all patients is liable to be wasteful. Rather, the ability to tailor reactions as
indicated by the anticipated complexities is required. In clinical units that treat critical quantities of nation Aboriginal patients, a committed
facilitator part (full-or low maintenance) is required. For clinical units that concede few nation Aboriginal patients, planning limit could live in
the doctor's facility based AHLO and additionally Aboriginal Understanding Pathway Officer group, gave that an distinguished individual from
the clinical unit group takes duty regarding correspondence and contact with those specialists.

17NURSING
18NURSING
References
Ajmi, I., Gammoudi, L., Carruel, M., Zgaya, H., Hammadi, S. and Renard, J.M., 2014, September. Mapping patient flow in the Jeanne de
Flandres Hospital's operating rooms. In Emerging Technology and Factory Automation (ETFA), 2014 IEEE (pp. 1-5). IEEE.
Green, A., Abbott, P., Delaney, P., Patradoon-Ho, P., Delaney, J., Davidson, P.M. and DiGiacomo, M., 2016. Navigating the journey of
Aboriginal childhood disability: a qualitative study of carers’ interface with services. BMC health services research, 16(1), p.680.
Hägglund, M., Bolin, P. and Koch, S., 2015. Experiences as input to eHealth design-a hip surgery patient journey case. In MIE (pp. 672-674).
Kelly, J., 2017. Using mapping tools to improve aboriginal patient journeys. Australian Nursing and Midwifery Journal, 24(9), p.43.
Kelly, J., Dwyer, J., Mackean, T., O’Donnell, K. and Willis, E., 2016. Coproducing Aboriginal patient journey mapping tools for improved
quality and coordination of care. Australian journal of primary health.
Kelly, J., Dwyer, J., Pekarsky, B., Mackean, T., Willis, E., De Crespigny, C., Perkins, S., O'Donnell, K., King, R., Mackean, L. and Brown, A.,
2015.
References
Ajmi, I., Gammoudi, L., Carruel, M., Zgaya, H., Hammadi, S. and Renard, J.M., 2014, September. Mapping patient flow in the Jeanne de
Flandres Hospital's operating rooms. In Emerging Technology and Factory Automation (ETFA), 2014 IEEE (pp. 1-5). IEEE.
Green, A., Abbott, P., Delaney, P., Patradoon-Ho, P., Delaney, J., Davidson, P.M. and DiGiacomo, M., 2016. Navigating the journey of
Aboriginal childhood disability: a qualitative study of carers’ interface with services. BMC health services research, 16(1), p.680.
Hägglund, M., Bolin, P. and Koch, S., 2015. Experiences as input to eHealth design-a hip surgery patient journey case. In MIE (pp. 672-674).
Kelly, J., 2017. Using mapping tools to improve aboriginal patient journeys. Australian Nursing and Midwifery Journal, 24(9), p.43.
Kelly, J., Dwyer, J., Mackean, T., O’Donnell, K. and Willis, E., 2016. Coproducing Aboriginal patient journey mapping tools for improved
quality and coordination of care. Australian journal of primary health.
Kelly, J., Dwyer, J., Pekarsky, B., Mackean, T., Willis, E., De Crespigny, C., Perkins, S., O'Donnell, K., King, R., Mackean, L. and Brown, A.,
2015.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
19NURSING
Managing Two Worlds Together: Stage 3: Improving Aboriginal Patient Journeys-Study Report. Managing Two Worlds Together: Stage 3:
Improving Aboriginal Patient Journeys-Study Report, p.vi.
Kelly, J., Ramage, M., Perry, D., Tinsley, J., Auckram, H., Corkhill, W., Wyatt, S. and McCabe, N., 2015. Managing Two Worlds Together:
Stage 3: Improving Aboriginal Patient Journeys-Cardiac Case Studies. Managing Two Worlds Together: Stage 3: Improving Aboriginal Patient
Journeys-Cardiac Case Studies, p.vi.
Kelly, J., Wilden, C., Chamney, M., Martin, G., Herman, K. and Russell, C., 2016. Improving cultural and clinical competency and safety of
renal nurse education. Renal Society of Australasia Journal, 12(3), p.106.
Kelly, J., Wilden, C., Herman, K., Martin, G., Russell, C. and Brown, S., 2016. Bottling knowledge and sharing it-using patient journey mapping
to build evidence and improve Aboriginal renal patient care. Renal Society of Australasia Journal, 12(2), p.48.
McCarthy, S., O’Raghallaigh, P., Woodworth, S., Lim, Y.L., Kenny, L.C. and Adam, F., 2016. An integrated patient journey mapping tool for
embedding quality in healthcare service reform. Journal of Decision Systems, 25(sup1), pp.354-368.
Managing Two Worlds Together: Stage 3: Improving Aboriginal Patient Journeys-Study Report. Managing Two Worlds Together: Stage 3:
Improving Aboriginal Patient Journeys-Study Report, p.vi.
Kelly, J., Ramage, M., Perry, D., Tinsley, J., Auckram, H., Corkhill, W., Wyatt, S. and McCabe, N., 2015. Managing Two Worlds Together:
Stage 3: Improving Aboriginal Patient Journeys-Cardiac Case Studies. Managing Two Worlds Together: Stage 3: Improving Aboriginal Patient
Journeys-Cardiac Case Studies, p.vi.
Kelly, J., Wilden, C., Chamney, M., Martin, G., Herman, K. and Russell, C., 2016. Improving cultural and clinical competency and safety of
renal nurse education. Renal Society of Australasia Journal, 12(3), p.106.
Kelly, J., Wilden, C., Herman, K., Martin, G., Russell, C. and Brown, S., 2016. Bottling knowledge and sharing it-using patient journey mapping
to build evidence and improve Aboriginal renal patient care. Renal Society of Australasia Journal, 12(2), p.48.
McCarthy, S., O’Raghallaigh, P., Woodworth, S., Lim, Y.L., Kenny, L.C. and Adam, F., 2016. An integrated patient journey mapping tool for
embedding quality in healthcare service reform. Journal of Decision Systems, 25(sup1), pp.354-368.
1 out of 20
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.